Enterovirus Structure and composition The virion of enterovirus



- Slides: 27
Enterovirus

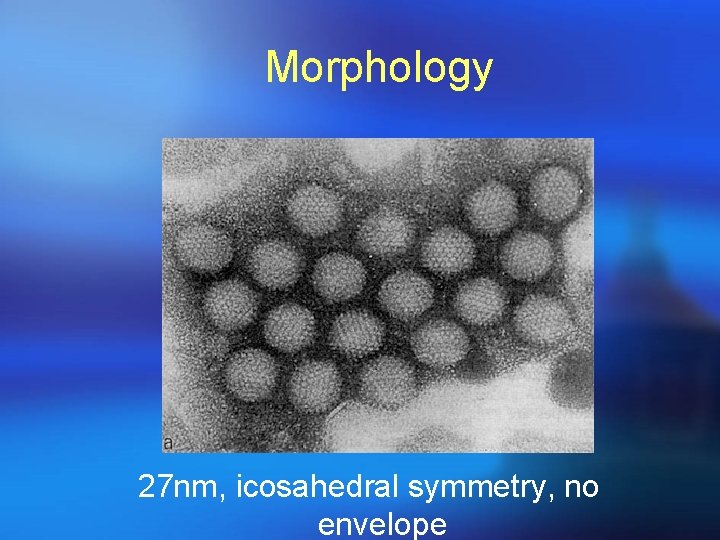
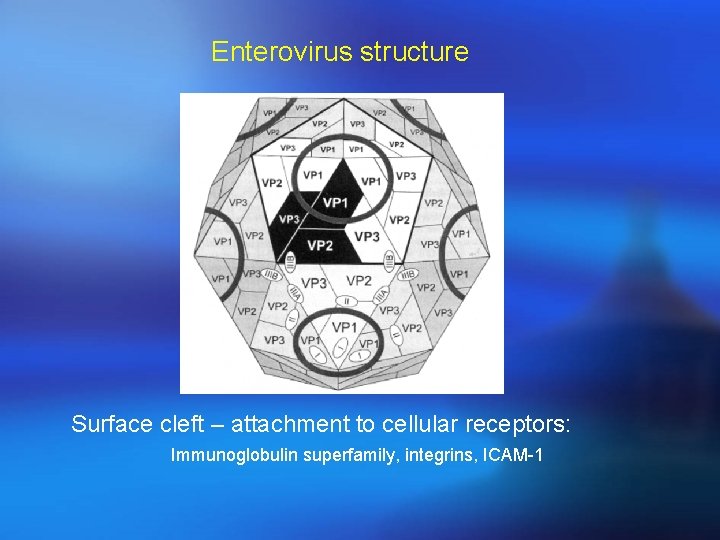
Structure and composition The virion of enterovirus consists of a capsid shell of 60 subunites , each of four proteins(vp 1 -vp 4)arranged with icosahedral symmetry around a genome made up of a single strand of positive –sense RNA.
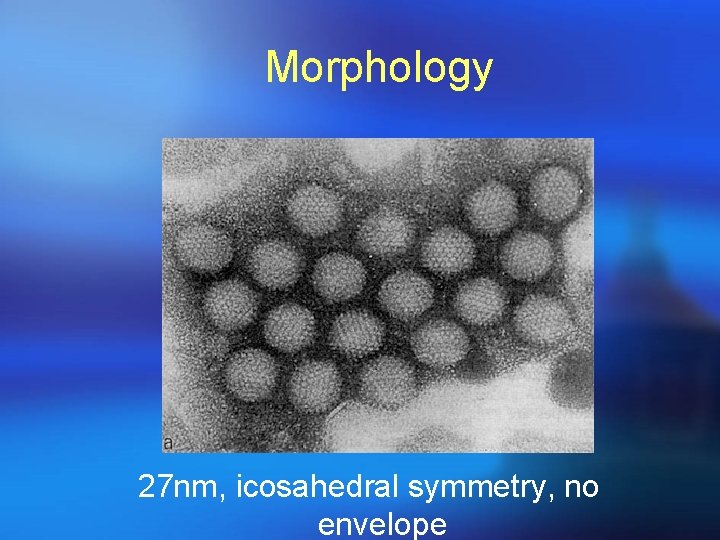
Morphology 27 nm, icosahedral symmetry, no envelope
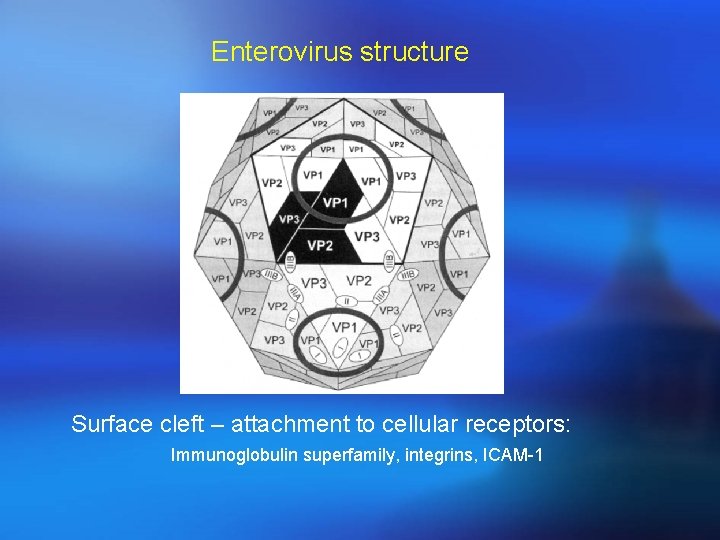
Enterovirus structure Surface cleft – attachment to cellular receptors: Immunoglobulin superfamily, integrins, ICAM-1
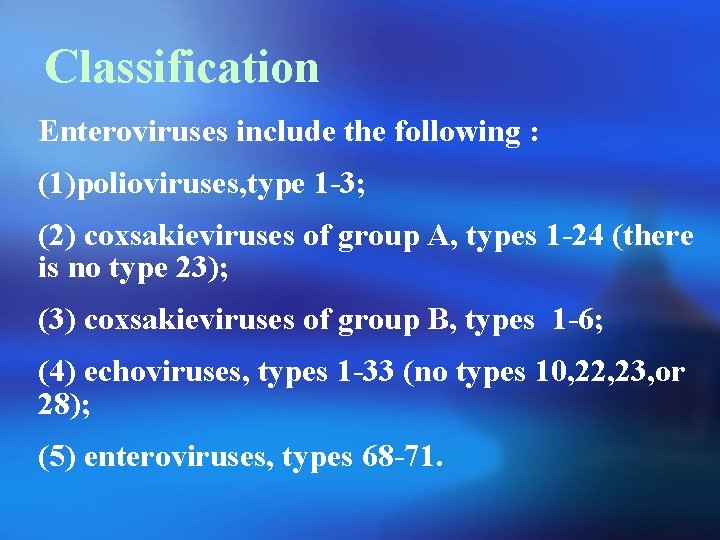
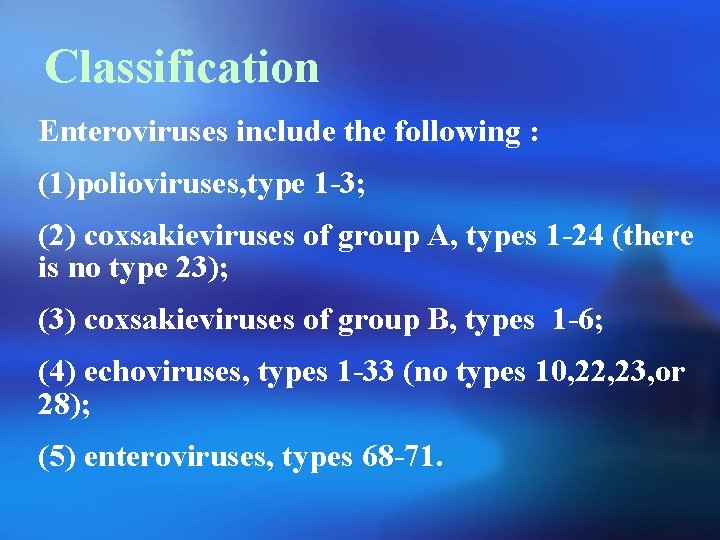
Classification Enteroviruses include the following : (1)polioviruses, type 1 -3; (2) coxsakieviruses of group A, types 1 -24 (there is no type 23); (3) coxsakieviruses of group B, types 1 -6; (4) echoviruses, types 1 -33 (no types 10, 22, 23, or 28); (5) enteroviruses, types 68 -71.
Poliovirus
Poliovirus was first identified in 1909 by inoculation of specimens into monkeys. The virus was first grown in cell culture in 1949 which became the basis for vaccines
Poliovirus may cause poliomyelitis , which is an infectious disease that in its serious form affects the central nervous system. However, most poliovirus infections are subclinical.
General properties: Poliovirus particle are typical enterovirus. They are inactivated when heated at 550 c for 30 min, by a chlorine concentration of 0. 1 ppm Poliovirus are not affected ether or sodium deoxycholate
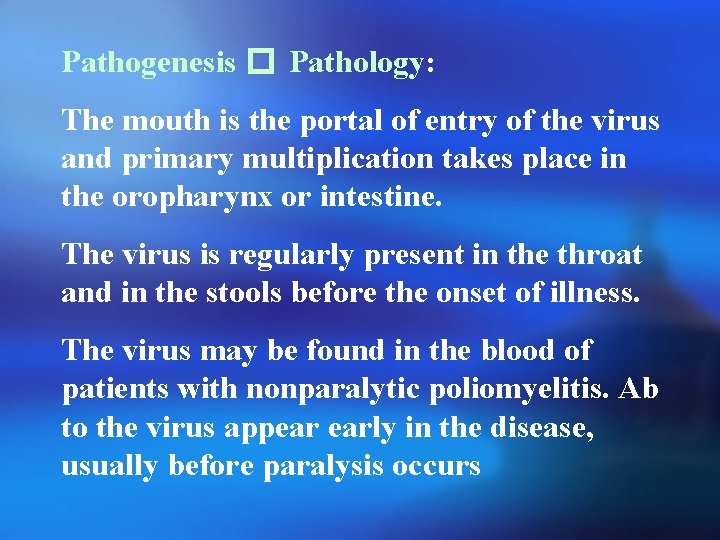
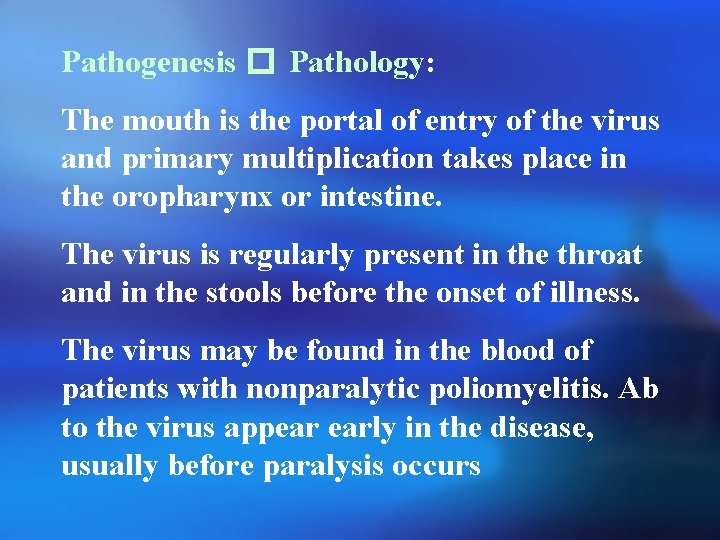
Pathogenesis � Pathology: The mouth is the portal of entry of the virus and primary multiplication takes place in the oropharynx or intestine. The virus is regularly present in the throat and in the stools before the onset of illness. The virus may be found in the blood of patients with nonparalytic poliomyelitis. Ab to the virus appear early in the disease, usually before paralysis occurs
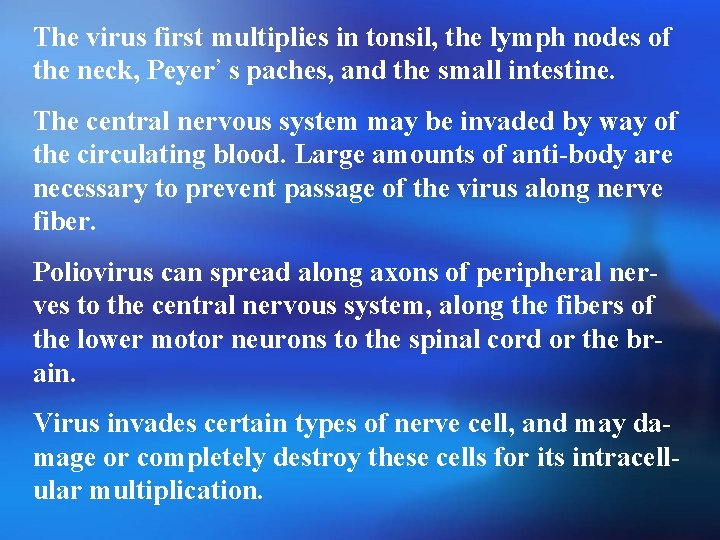
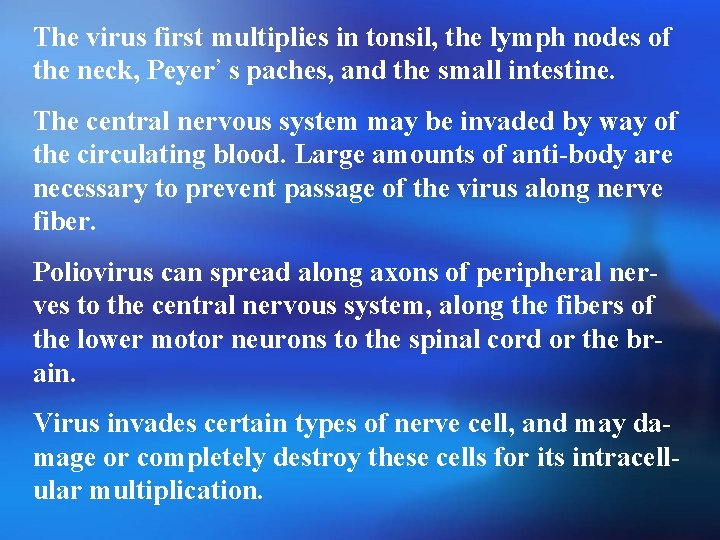
The virus first multiplies in tonsil, the lymph nodes of the neck, Peyer’ s paches, and the small intestine. The central nervous system may be invaded by way of the circulating blood. Large amounts of anti-body are necessary to prevent passage of the virus along nerve fiber. Poliovirus can spread along axons of peripheral nerves to the central nervous system, along the fibers of the lower motor neurons to the spinal cord or the brain. Virus invades certain types of nerve cell, and may damage or completely destroy these cells for its intracellular multiplication.
Transmission ¡Fecal – oral route via hands and objects via food and water contaminated with patient’s stool/oral secretion/urine.
Clinical findings: 1 -Abortive poliomyelitis 2 -Nonparalytic poliomyelitis 3 -Paralytic poliomyelitis 4 -Progressive postpoliomylitis muscle atrophy
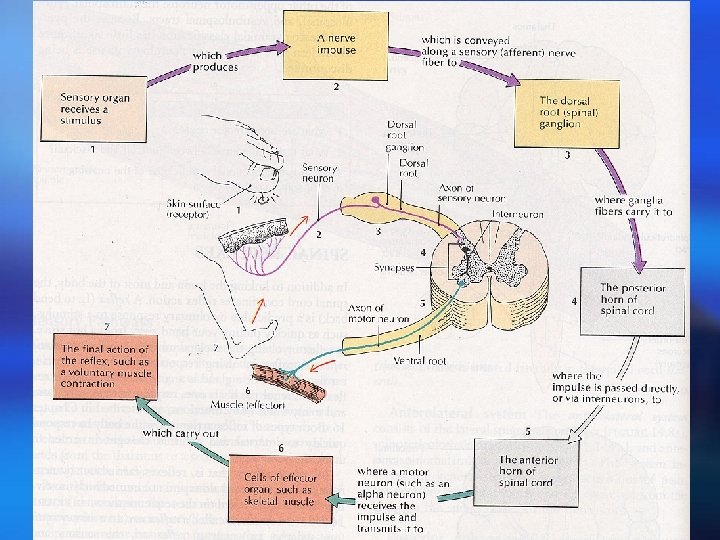
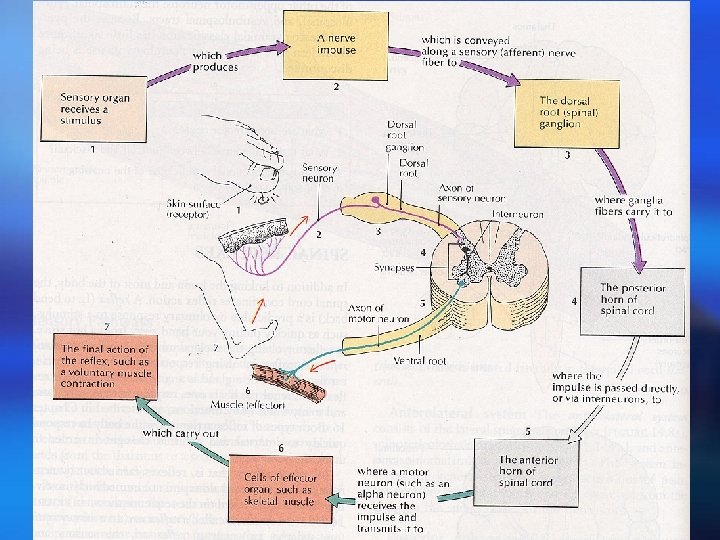
Clinical Manifestations ¡ Most infections asymptomatic, 95% ¡ Abortive polio (minor illness), 5%: fever, malaise, sore throat, myalgia, headache) ¡ Aseptic meningitis (non paralytic polio), 1% ¡ Paralytic polio (major illness), 0. 1%: asymetric flaccid paralysis / paresis. Lower, or upper extremities, thoracic, abdominal, bulbar. Involvement : spinal cord anterior horn cells, motor cortex, dorsal root ganglia neurologic sequela (2/3) ¡ Post-polio syndrome: progressive atrophy years later


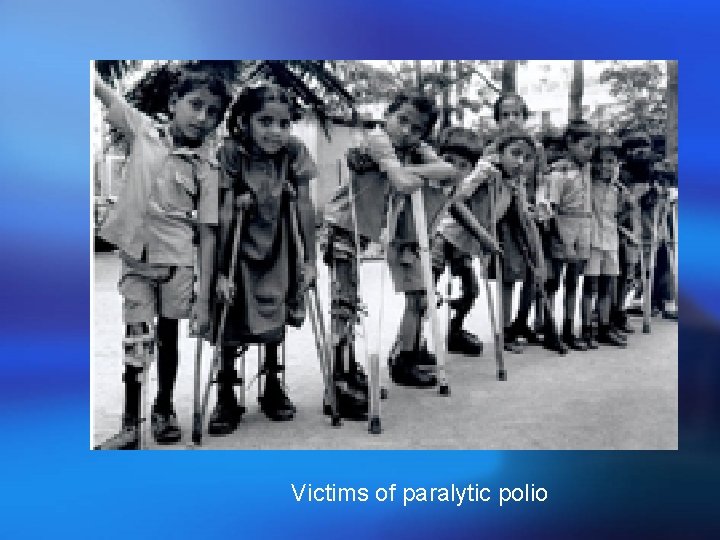
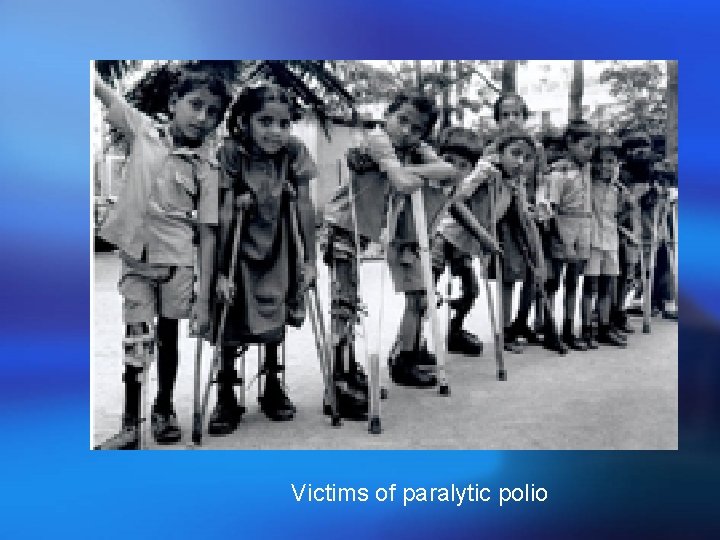
Victims of paralytic polio
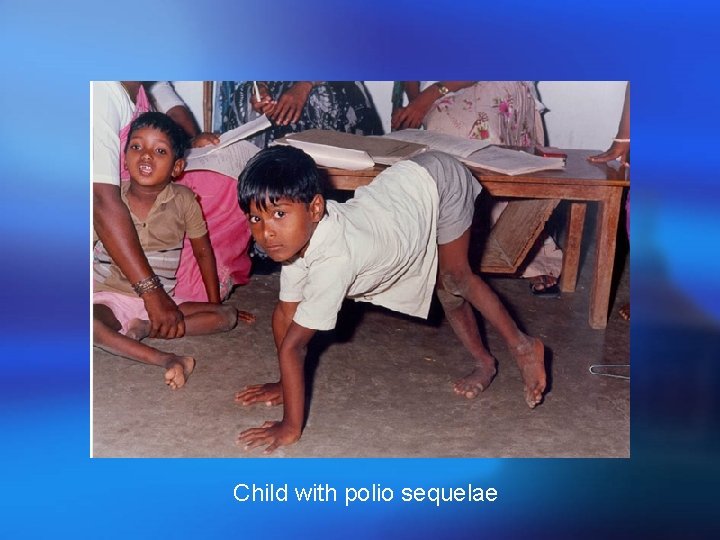
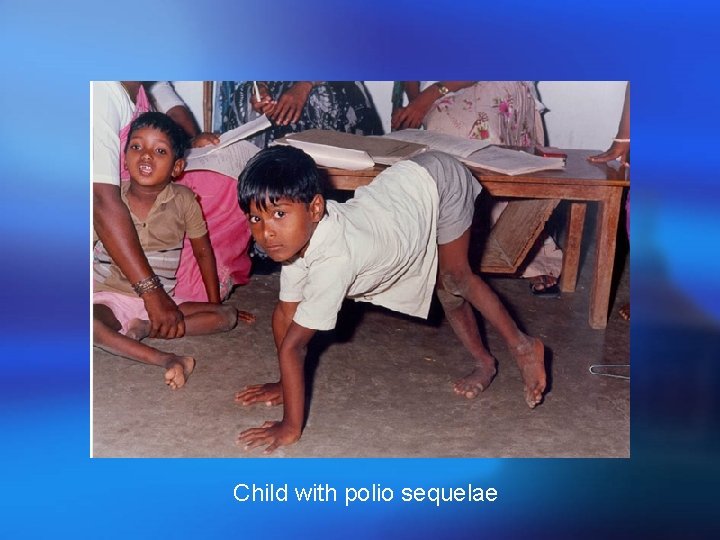
Child with polio sequelae
Laboratory diagnosis: The virus may be recovered from throat swabs, rectal swabs, or stool samples. Specimens should be kept frozen during transit to the laboratory Cultures of human or monkey cells Paired serum specimens are required to show rise in antibody titer during the course of disease.
Laboratory Diagnosis ¡ Virus Isolation Mainstay of diagnosis of poliovirus infection poliovirus can be readily isolated from throat swabs, faeces, and rectal swabs, but rarely from the CSF Can be readily grown and identified in cell culture Requires molecular techniques to differentiate between the wild type and the vaccine type ¡ Serology Very rarely used for diagnosis since cell culture is efficient. Occasionally used for immune status screening for immunocompromised individuals
Immunity: Immunity is permanent to the type causing the infection. Passive immunity is transferred from mother to offspring, which gradually disappear during the first 6 months of life. Virus-neutralizing antibody forms soon after exposure to the virus, often before the onset of illness.
Epidemiology: Poliomyelitis occurs worldwide – year-round in tropics and during summer and fall in temperate zone. Winter outbreaks are rare. The disease occurs in all age groups , but children are more susceptible than adult because of the acquired immunity of the adult population. Human are the only known reservoir of infection.
Prevention � control: Both live-virus and killed-virus vaccines are available. They induce antibody and protect the central nervous system from subsequent invasion by wild virus. A potential limiting factor for oral vaccine is interference, and for vaccine-associated disease, a switch to the use of only inactivated poliovaccine (four doses) for children Immune globulin can provide protection for a few weeks against the paralytic disease but does not prevent subclinical infection. The application of recombinant DNA
Vaccination ¡ Intramuscular Poliovirus Vaccine (IPV) consists of formalin inactivated virus of all 3 poliovirus serotypes (Salk) Produces serum antibodies only: does not induce local immunity and thus will not prevent local infection of the gut However, it will prevent paralytic poliomyelitis since viraemia is essential for the pathogenesis of the disease ¡ Oral Poliovirus Vaccine (OPV) Consists of live attenuated virus of all 3 serotypes (Sabin). Produces local immunity through the induction of an Ig. A response as well as systemic immunity Rarely causes paralytic poliomyelitis, around 1 in 3 million doses
¡ Most countries use OPV because of its ability to induce local immunity and also it is much cheaper to produce than IPV ¡ The normal response rate to OPV is close to 100%. ¡ OPV is used for the WHO poliovirus eradication campaign ¡ Because of the slight risk of paralytic poliomyelitis, some Scandinavian countries have reverted to using IPV. Because of the lack of local immunity, small community outbreaks of poliovirus infections have been reported
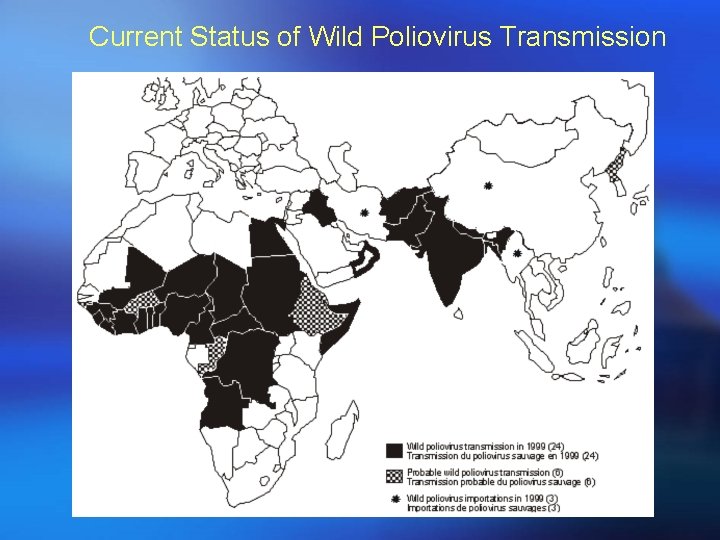
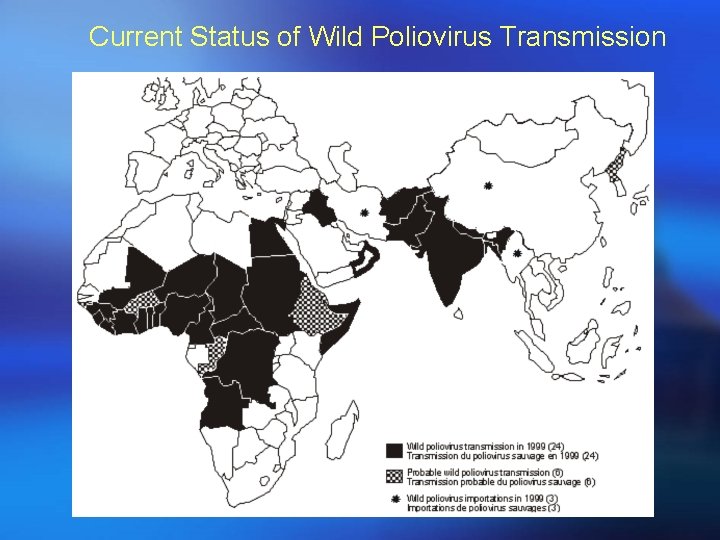
Current Status of Wild Poliovirus Transmission