Enterobacteriaceae Dr mer Kkbasmac Enterobacteriaceae The largest most
Enterobacteriaceae Dr Ömer Küçükbasmacı
Enterobacteriaceae • The largest, most heterogeneous collection of medically important gram-negative rods • >40 genera and 150 species • Fewer than 20 species are responsible for more than 95% of the infections • Ubiquitous organisms, found worldwide in soil, water, and vegetation
Enterobacteriaceae • part of the normal intestinal flora • 30% to 35% of all septicemias, more than 70% of urinary tract infections (UTIs), and many intestinal infections • Salmonella typhi, Shigella species, Yersinia pestis • Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis
Enterobacteriaceae • become pathogenic when they acquire virulence factor • can originate from an animal • or from a human carrier • or through the endogenous spread of organisms
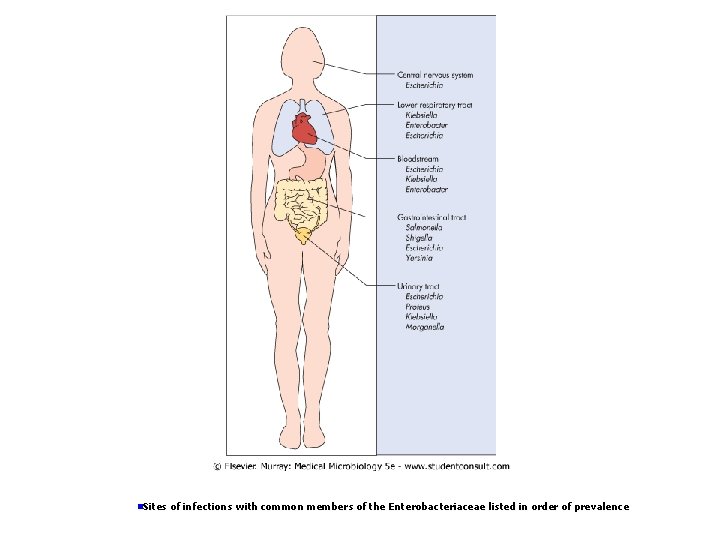
n. Sites of infections with common members of the Enterobacteriaceae listed in order of prevalence
Enterobacteriaceae • moderately sized (0. 3 -1. 0 × 1. 0 -6. 0 μm) • gram-negative rods • either nonmotile or motile with peritrichous flagella • do not form spores • facultative anaerobes • have simple nutritional requirements
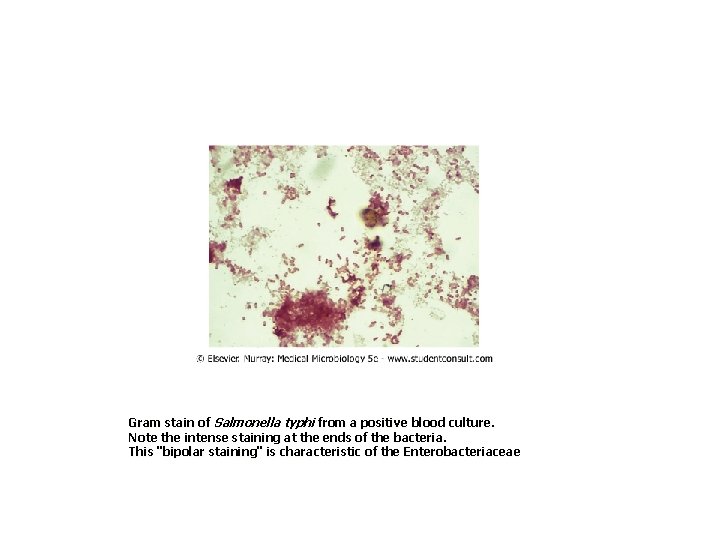
Gram stain of Salmonella typhi from a positive blood culture. Note the intense staining at the ends of the bacteria. This "bipolar staining" is characteristic of the Enterobacteriaceae
Enterobacteriaceae • ferment glucose, reduce nitrate • catalase positive and oxidase negative • the ability to ferment lactose Escherichia, Klebsiella, Enterobacter, Citrobacter, and Serratia spp • do not ferment lactose Proteus, Salmonella, Shigella, and Yersinia spp. • Some have prominent capsules
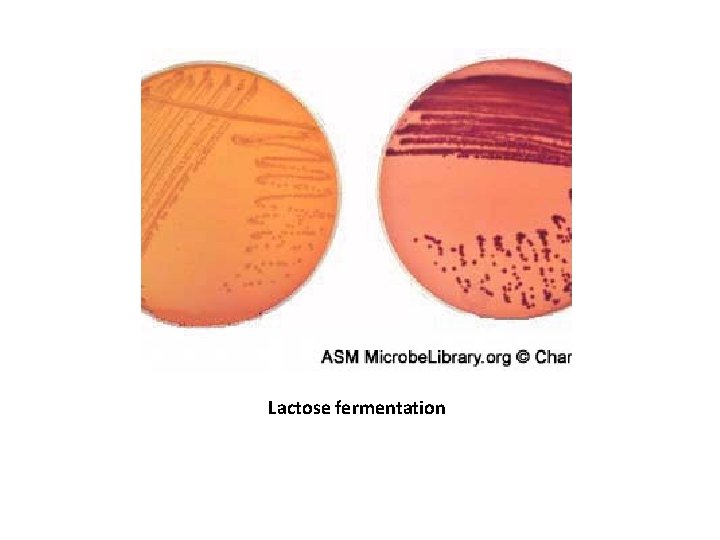
Lactose fermentation

Enterobacteriaceae • Resistance to bile salts • Some have capsules Common Medically Important Enterobacteriaceae • Citrobacter freundii, Citrobacter koseri • Enterobacter aerogenes, Enterobacter cloacae • Escherichia coli • Klebsiella pneumoniae, Klebsiella oxytoca • Morganella morganii • Proteus mirabilis, Proteus vulgaris • Salmonella enterica • Serratia marcescens • Shigella sonnei, Shigella flexneri • Yersinia pestis, Yersinia enterocolitica, Yersinia pseudotuberculosis
Enterobacteriaceae • LPS: Consists of three components: the outermost somatic O polysaccharide a core polysaccharide common to all Enterobacteriaceae (enterobacterial common antigen) lipid A
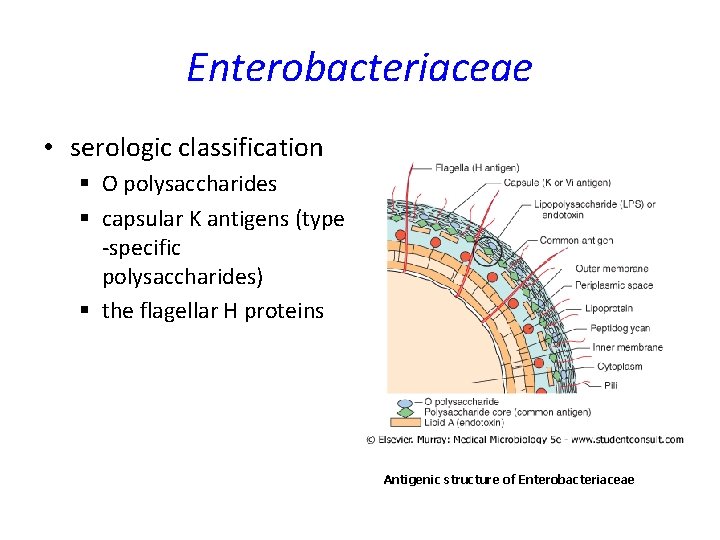
Enterobacteriaceae • serologic classification § O polysaccharides § capsular K antigens (type -specific polysaccharides) § the flagellar H proteins Antigenic structure of Enterobacteriaceae
Enterobacteriaceae • Common Virulence Factors Associated with Enterobacteriaceae § Endotoxin § Capsule § Antigenic phase variation § Type III secretion systems § Sequestration of growth factors § Resistance to serum killing § Antimicrobial resistance
Escherichia coli five species sepsis, UTIs, meningitis, gastroenteritis Gram-negative, facultative anaerobic rods Fermenter; oxidase negative Outer membrane makes the organisms susceptible to drying • Lipopolysaccharide consists of outer somatic O polysaccharide, core polysaccharide (common antigen), and lipid A (endotoxin) • • •
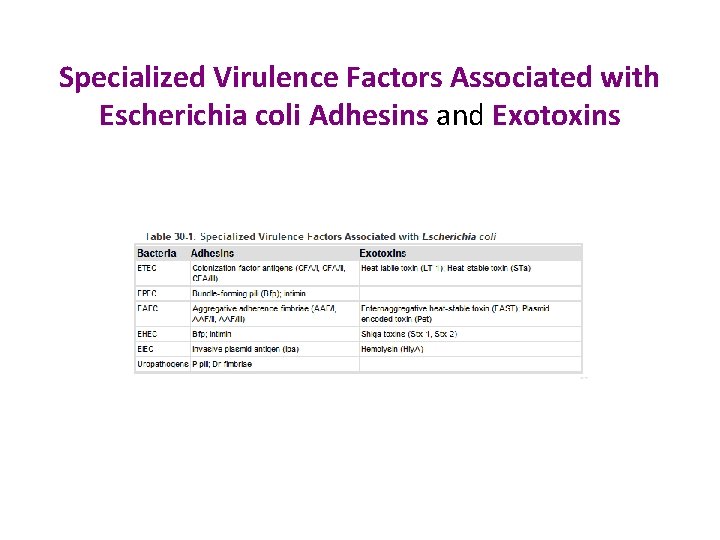
Specialized Virulence Factors Associated with Escherichia coli Adhesins and Exotoxins
Escherichia coli • the most common gram-negative rods isolated from patients with sepsis • responsible for causing more than 80% of all community-acquired UTIs • gastroenteritis in developing countries • Most infections are endogenous
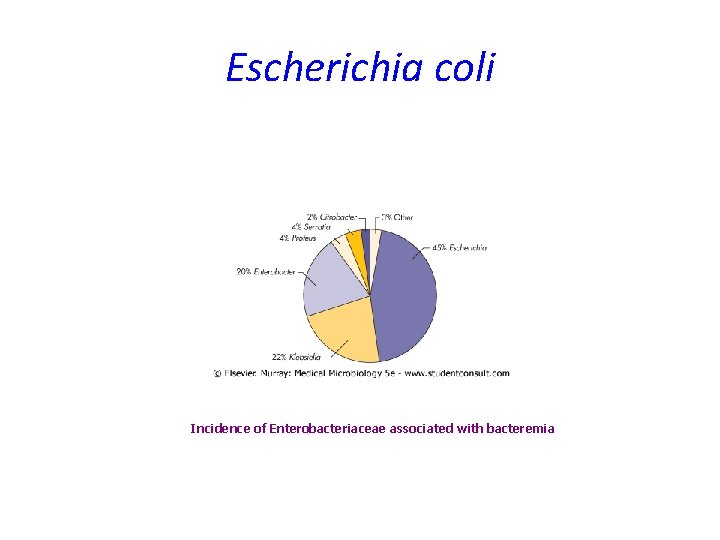
Escherichia coli Incidence of Enterobacteriaceae associated with bacteremia
Escherichia coli • Diseases – Bacteremia (most commonly isolated gram-negative rod) – Urinary tract infection (most common cause of bacterial UTIs); limited to bladder (cystitis) or can spread to kidneys (pyelonephritis) or prostate (prostatitis) – At least five different pathogenic groups cause gastroenteritis (EPEC, ETEC, EHEC, EIEC, EAEC); most cause diseases in developing countries, although EHEC is an important cause of hemorrhagic colitis (HC) and hemolytic uremic syndrome (HUS) – Neonatal meningitis (usually with strains carrying the K 1 capsular antigen) – Intraabdominal infections (associated with intestinal perforation) – Most infections are endogenous
Escherichia coli • Neonatal Meningitis: E. coli and group B streptococci • Gastroenteritis § § § enteropathogenic (EPEC) enterotoxigenic (ETEC) enterohemorrhagic (EHEC) enteroinvasive (EIEC) enteroaggregative (EAEC) E. coli
Escherichia coli • ETEC: Traveler's diarrhea; infant diarrhea in developing countries; watery diarrhea, vomiting, cramps, nausea, low-grade fever § Plasmid-mediated, heat-stable and/or heat-labile enterotoxins that stimulate hypersecretion of fluids and electrolytes § LT-1 similar to cholera toxin c. AMP GM 1 gangliosid § Enhanced secretion of chloride and dec absorption of sodium and chloride § STa c. GMP
Escherichia coli • EPEC: Infant diarrhea in underdeveloped countries; watery diarrhea and vomiting, nonbloody stools, per to per spread occurs § Person to person spread § Plasmid-mediated A/E histopathology with disruption of normal microvillus § Nonfimbrial adhesin, no LT or ST § Moderately invasive
Escherichia coli • EAEC: Infant diarrhea in underdeveloped countries; traveler's diarrhea, persistent or chronic diarrhea Plasmid-mediated aggregative adherence of rods Enteroaggregative heat stable toxin (EAST)
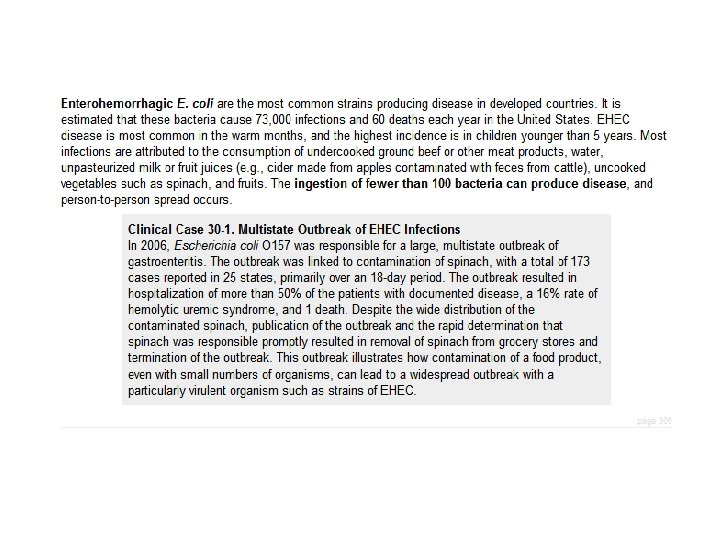
Escherichia coli • EHEC: Initial watery diarrhea, followed by grossly bloody diarrhea (hemorrhagic colitis) with abdominal cramps; little or no fever; may progress to hemolytic uremic syndrome (HUS) Mediated by cytotoxic Shiga toxins, which disrupt protein synthesis; lesions with destruction of intestinal microvillus resulting in decreased absorption, bacteriophage mediated
Escherichia coli • EIEC: Disease in underdeveloped countries; fever, cramping, watery diarrhea; may progress to dysentery with scant, bloody stools, fever, severe inflammation Plasmid-mediated invasion and destruction of epithelial cells Sereny test positive
Escherichia coli-UTI • Colon contaminate urethra ascend into bladder and may migrate to kidney or prostate • UTIs: adhesins (primarily P pili, AAF/III, Dr) and hemolysin Hly. A
Escherichia coli-Neonatal Meningitis • E. coli and group B streptococci major CNS pathogens • K 1 capsular antigen • Commonly present in the GIS
Escherichia coli-Septicemia • May be originated from UT or GIS • Mortality is high
Salmonella • Salmonella enterica and Salmonella bongori • S. enterica is subdivided into six subspecies, S. enterica subsp. enterica • the two species have been subdivided into more than 2500 unique serotypes • S. enterica subspecies enterica serotype Typhimurium or S. Typhimurium
Salmonella • Physiology and Structure § Gram-negative, facultative anaerobic rods § Fermenter; oxidase negative § Outer membrane makes the organisms susceptible to drying § Lipopolysaccharide consists of outer somatic O polysaccharide, core polysaccharide (common antigen), and lipid A (endotoxin) § More than 2500 O serotypes (commonly referred to as individual Salmonella species)
• Enrichment broth: Tetrathionat, GN, selenit broth • Selective media: Mac Conkey, SS agar, Hektoen Enteric Agar, Bismuth sulfide agar
• • Human ( Typhi, paratyphi) Citrate (-) Vi antigen positive Gas from glucose negative
Salmonella • Tolerant to acids in phagocytic vesicles • Can survive in macrophages and spread from the intestine to other body sites (particularly true of S. typhi) • Endotoxin
Salmonella-Epidemiology • Most infections are acquired by eating contaminated food products • Direct fecal-oral spread in children • S. typhi and S. paratyphi are strict human pathogens • Individuals at risk for infection include those who eat improperly cooked poultry or eggs, patients with reduced gastric acid levels, and immunocompromised patients • Infections occur worldwide, particularly in the warm months of the year • Nontyphoid Salmonella %98
Clinical Manifestations • • • Gastroenteritis Enteric fever Bacteremia and vascular infections Localized infections Carrier state
Gastroenteritis • • • Incubation 6 -48 hours Watery diarrhea, nausea, vomiting Fever Neutrophil in stool Self limited 3 -7 days Mortality very low
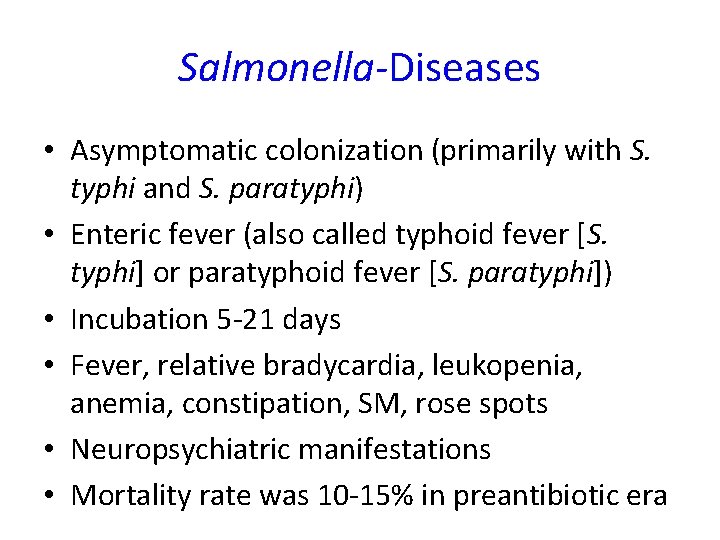
Salmonella-Diseases • Asymptomatic colonization (primarily with S. typhi and S. paratyphi) • Enteric fever (also called typhoid fever [S. typhi] or paratyphoid fever [S. paratyphi]) • Incubation 5 -21 days • Fever, relative bradycardia, leukopenia, anemia, constipation, SM, rose spots • Neuropsychiatric manifestations • Mortality rate was 10 -15% in preantibiotic era
Localized Infections • • Septic artritis Osteomyelitis Meningitis Abscess (splenic, hepatic)
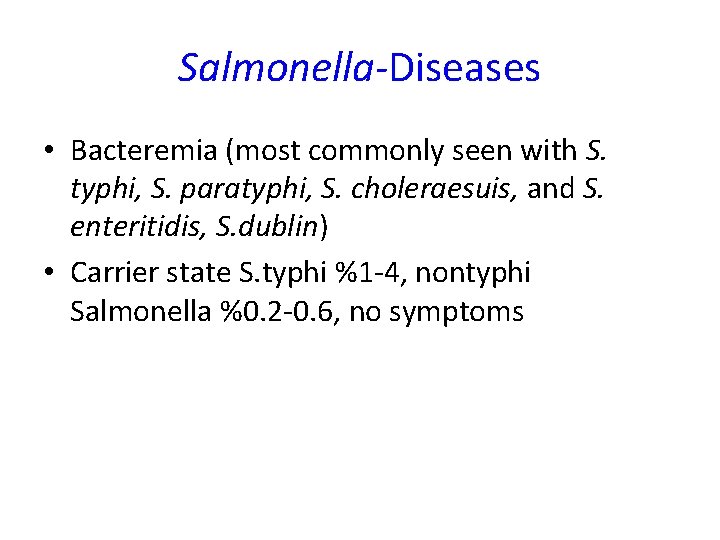
Salmonella-Diseases • Bacteremia (most commonly seen with S. typhi, S. paratyphi, S. choleraesuis, and S. enteritidis, S. dublin) • Carrier state S. typhi %1 -4, nontyphi Salmonella %0. 2 -0. 6, no symptoms
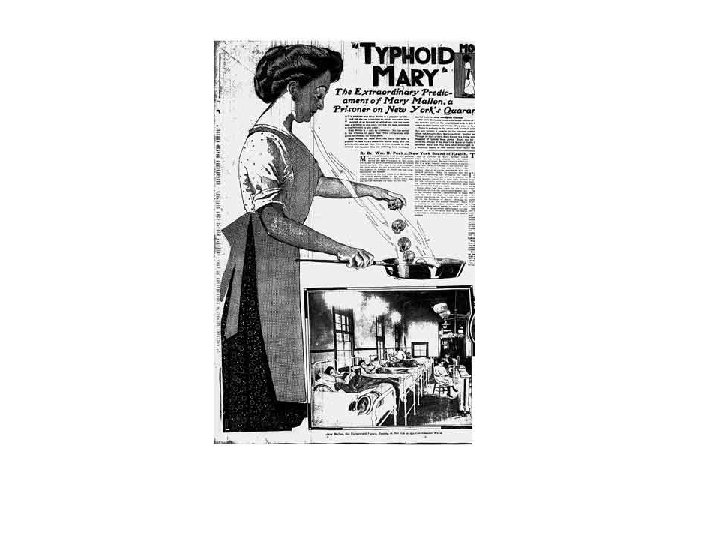
• What New York did about Typhoid Mary • By wildnewyork Mary Mallon was born in Irelend in 1869 and came to America at 16, working as a cook for wealthy families in Boston and New York. In the early 1900 s, several family members came down with typhoid —a potentially deadly bacterial infection spread through food when a carrier doesn’t wash his or her hands after using the bathroom. • Eventually a New York City typhoid researcher identified Mary as the source of all the infections. She denied having typhoid, but tests proved otherwise, and city health officials forced her into quarantine in a city hospital at North Brother Island in the East River. • A New York newspaper illustrates her plight in 1909. • After leaving quarantine and promising not to handle food, she went back to work as a cook, promptly infecting more people. Eventually she was brought back to the island, where she lived out her life. Mary died in 1938, a celebrity for being a healthy carrier of a lethal bacteria.
• Timeline: 1869 - Mary Mallon born, Country Tyrone, Irleand 1883 - Like many Irish women poverty forces Mallon to emigrate to the United States 1900 - 1906 Mallon works as a cook in New York City. At her places of employment (private homes), Mallon unknowingly infects two dozen people with typhoid. 1901 - Manhattan. Member's of Mallon's employer's family and her coworkers develop fevers and diarrhea. One laundress dies. 1906 - Long Island. Within two weeks of hiring Mallon as a cook, fourteen of twenty family members are ill with typhoid. Mallon quickly leaves the position. She is eventually identified by George Soper as a healthy carrier. 1908 -1911 Mallon is quaratined on North Brother Island at Riverside Hospital. She is released after some media attention and after she gives her promise not to work in the food industry. 1915 - Mallon returns to working as a cook. Using the pseudonym "Mary Brown" she is hired at the Sloan Maternity Hospital in New York. Twenty-five people are infected, two die. Mallon is returned to quarantine on North Brother Island. 1915 -1938 Mallon remains in quarantine for the rest of her life. She has her own cottage, makes her own meals, is occasionally interviewed by reporters and works as a lab assistant for a time. 1938, November 11 th: Mallon dies of pneumonia. An autopsy reveals live typhoid bacteria in her bladder.
Diagnosis • • Culture Stool, urine , blood, rose spots, bone marrow Selective media Typhoid fever 1. week blood culture ≥ 3. week stool culture
Diagnosis • Gruber Widal Anti-O Ab Anti-H Ab Anti-Vi Ab (Long term carriers)
Therapy • Replacement • Quinolones, ampicillin, Co-trimoxazole • Cephalosporin 1. , 2. Gen and aminoglycosides are ineffective • Oral attenue and Vi parenteral vaccines available
Shigella • S. dysenteriae, Shigella flexneri, Shigella boydii, and Shigella sonnei • S. sonnei is the most common cause of shigellosis in the industrial world • S. flexneri is the most common cause in developing countries • They are very much like Escherichia
Shigella • Nonmotile • Noncapsulated • H 2 S negative
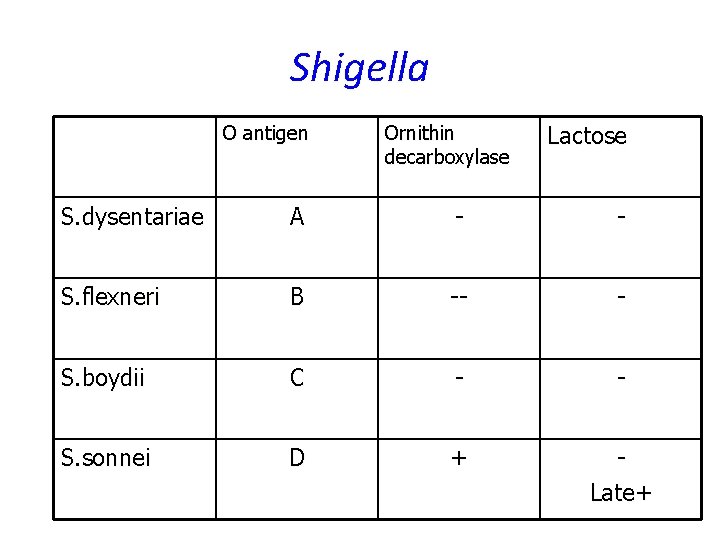
Shigella O antigen Ornithin decarboxylase Lactose S. dysentariae A - - S. flexneri B -- - S. boydii C - - S. sonnei D + Late+
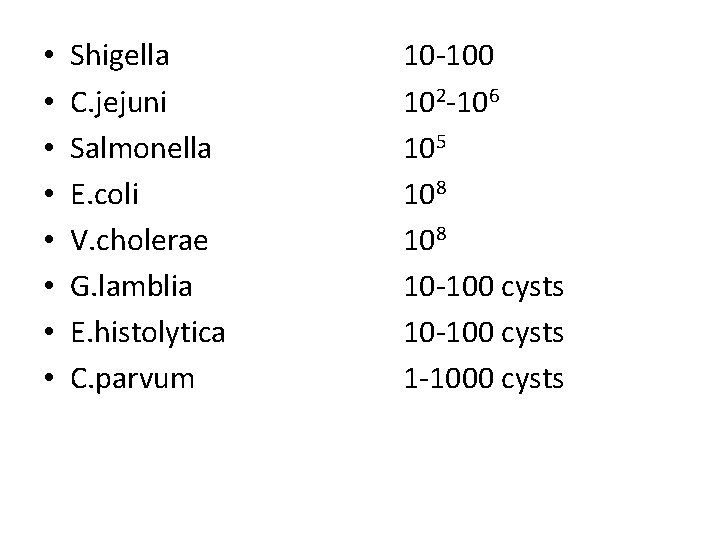
• • Shigella C. jejuni Salmonella E. coli V. cholerae G. lamblia E. histolytica C. parvum 10 -100 102 -106 105 108 10 -100 cysts 1 -1000 cysts
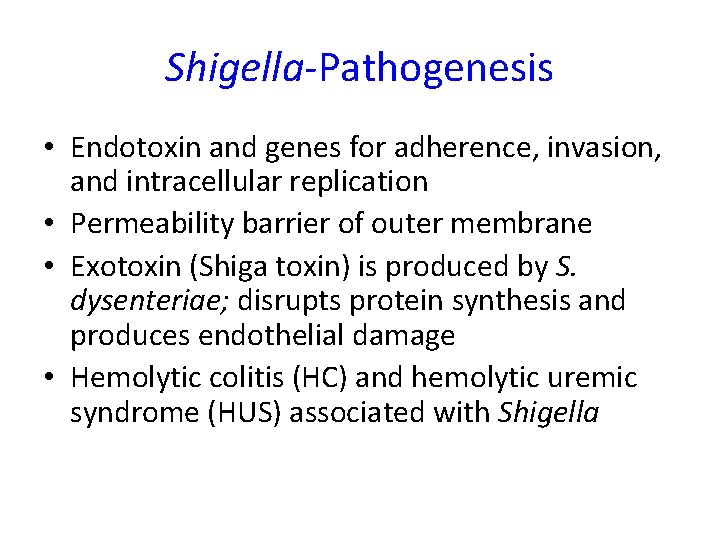
Shigella-Pathogenesis • Endotoxin and genes for adherence, invasion, and intracellular replication • Permeability barrier of outer membrane • Exotoxin (Shiga toxin) is produced by S. dysenteriae; disrupts protein synthesis and produces endothelial damage • Hemolytic colitis (HC) and hemolytic uremic syndrome (HUS) associated with Shigella
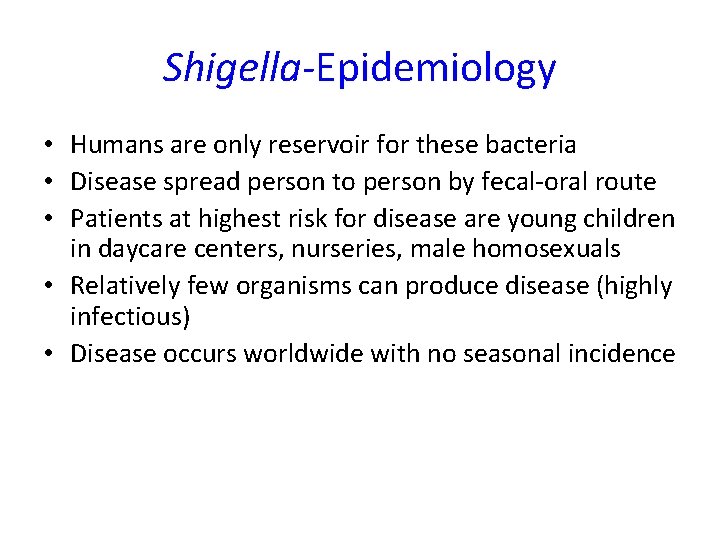
Shigella-Epidemiology • Humans are only reservoir for these bacteria • Disease spread person to person by fecal-oral route • Patients at highest risk for disease are young children in daycare centers, nurseries, male homosexuals • Relatively few organisms can produce disease (highly infectious) • Disease occurs worldwide with no seasonal incidence
Shigella-Diseases • Gastroenteritis (shigellosis) • Most common form is an initial watery diarrhea progressing within 1 to 2 days to abdominal cramps and tenesmus (with or without bloody stools) • Asymptomatic carriage develops in a small number of patients (reservoir for future infections) • A severe form of disease is caused by S. dysenteriae (bacterial dysentery)
Shigella-Diseases • Bloody diarrhae containing mucus, • Shigatoxin-an exotoxin B unit binds to host cell glycolipids and A cleaves the 28 S r. RNA , preventing the protein synthesis • Shigatoxin can mediate the damage to the glomeruşar endothelial calls, resulting in renal failure (HUS).
Shigella-Treatment, Prevention, and Control • Antibiotic therapy shortens the course of symptomatic disease and fecal shedding • Treatment should be guided by in vitro susceptibility tests • Empiric therapy can be initiated with a fluoroquinolone or trimethoprim-sulfamethoxazole • Appropriate infection control measures should be instituted to prevent spread of the organism
Yersinia • 11 species • Y. pestis, Yersinia enterocolitica, Yersinia pseudotuberculosis • Y. pestis is covered with a protein capsule • Some species (e. g. , Y. enterocolitica) can grow at cold temperatures
Yersinia • • • Y. pestis systemic disease with a high mortality Y. enterocolitica and Y. Pseudotuberculosis Capsule on Y. pestis is antiphagocytic Y. pestis is also resistant to serum killing Yersinia with genes for adherence, cytotoxic activity, inhibition of phagocytic migration and engulfment, and inhibition of platelet aggregation
Yersinia • Y. pestis is a zoonotic infection with humans the accidental host; natural reservoirs include rats, squirrels, rabbits, and domestic animals • Disease is spread by flea bites or direct contact with infected tissues or person to person by inhalation of infectious aerosols from a patient with pulmonary disease • Other Yersinia infections are spread through exposure to contaminated food products or blood products (Y. enterocolitica) • Colonization with other Yersinia species can occur
Yersinia • Y. pestis causes bubonic plague (most common) and pulmonary plague, both having a high mortality rate • Other Yersinia species cause gastroenteritis (acute watery diarrhea or chronic diarrhea) and transfusionrelated sepsis • Enteric disease in children may manifest as enlarge mesenteric lymph nodes and mimic acute appendicitis
Yersinia • • All Yersinia infections are zoonotic Urban plague, sylvatic plague Bubonic plague, pneumonic plague
Yersinia • Y. pestis infections are treated with streptomycin; tetracyclines, chloramphenicol , or trimethoprimsulfamethoxazole can be administered as alternative therapy • Enteric infections with other Yersinia species are usually selflimited. If antibiotic therapy is indicated, most organisms are susceptible to broad-spectrum cephalosporins, aminoglycosides, chloramphenicol , tetracyclines, and trimethoprim-sulfamethoxazole • Plague is controlled by reduction of the rodent population and vaccination of individuals at risk • Other Yersinia infections are controlled by the proper preparation of food products
Klebsiella • K. pneumoniae and Klebsiella oxytoca • Klebsiella rhinoscleromatis (causes a granulomatous disease of the nose) • Klebsiella ozaenae (causes chronic atrophic rhinitis) • K. granulomatis is the etiologic agent of granuloma inguinale
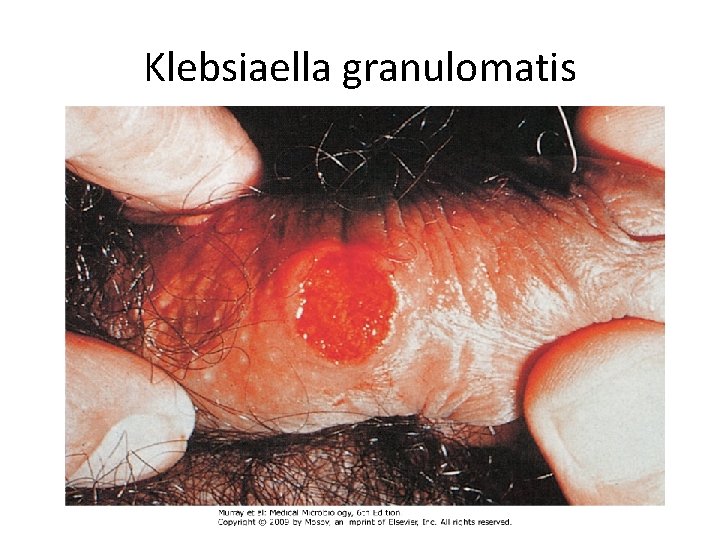
Klebsiaella granulomatis
Proteus • P. mirabilis • P. vulgaris
ENTEROBACTER, CITROBACTER, MORGANELLA, SERRATIA • Primary infections are rare • Citrobacter koseri has a predilection for causing meningitis and brain abscesses in neonates • Resistance is a particularly serious problem with Enterobacter species
Laboratory Diagnosis • Grow readily on culture media • Selective media (e. g. , Mac. Conkey agar, eosinmethylene blue [EMB] agar • Cold enrichment Y. enterocolitica • Biochemical identification • Serologic testing such as E. coli O 157 : H 7 or Y. enterocolitica O 8
• Az sayıda bol dışkı İB V. cholerae, ETEC, Shigella, Giardia • Çok sayıda az miktarda dışkı KB Shigella, Salmonella, Campylobacter, Entamoeba histolytica • Tenezm, acil dışkılama, dizanteri kolit Shigella, Salmonella, Campylobacter, Entamoeba histolytica
- Slides: 68