Enterobacteriacea e Enterobacteriacea A large family of bacteria

Enterobacteriacea e
Enterobacteriacea A large family of bacteria that includes many genera. They are classified on the basis of lactose fermentation into: lactose fermenters (coliforms) & non- lactose fermenters. Coliforms include; Escherichia, Klebsiella, Enterobacter, Serratia, and Citrobacter. Many species are members of the normal intestinal flora. Escherichia coli (E coli) is the most commonly isolated organism in the clinical laboratory.
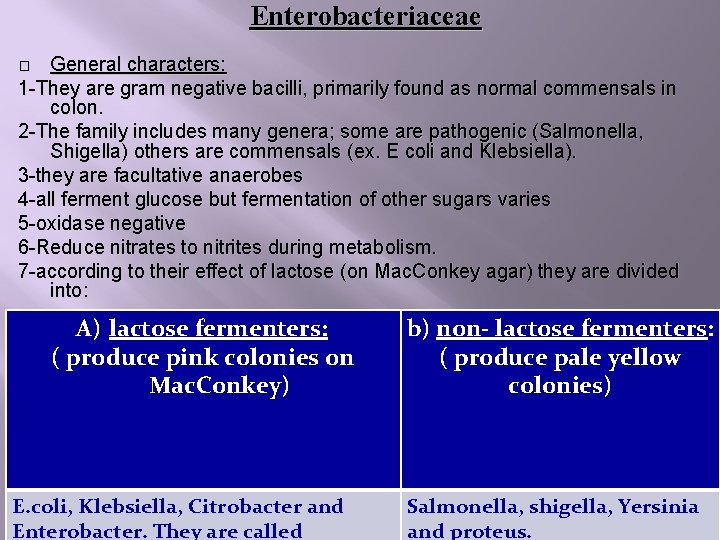
Enterobacteriaceae General characters: 1 -They are gram negative bacilli, primarily found as normal commensals in colon. 2 -The family includes many genera; some are pathogenic (Salmonella, Shigella) others are commensals (ex. E coli and Klebsiella). 3 -they are facultative anaerobes 4 -all ferment glucose but fermentation of other sugars varies 5 -oxidase negative 6 -Reduce nitrates to nitrites during metabolism. 7 -according to their effect of lactose (on Mac. Conkey agar) they are divided into: � A) lactose fermenters: ( produce pink colonies on Mac. Conkey) E. coli, Klebsiella, Citrobacter and Enterobacter. They are called b) non- lactose fermenters: ( produce pale yellow colonies) Salmonella, shigella, Yersinia and proteus.

Enterobacteriaceae Mac. Conkey agar Lactose fermenters (Rose pink colonies) E. coli, Klebsiella, Citrobacter, Enterobacter Lactose non fermenters (pale yellow) Salmonella, shigella, proteus, yersinia

Salmonella.
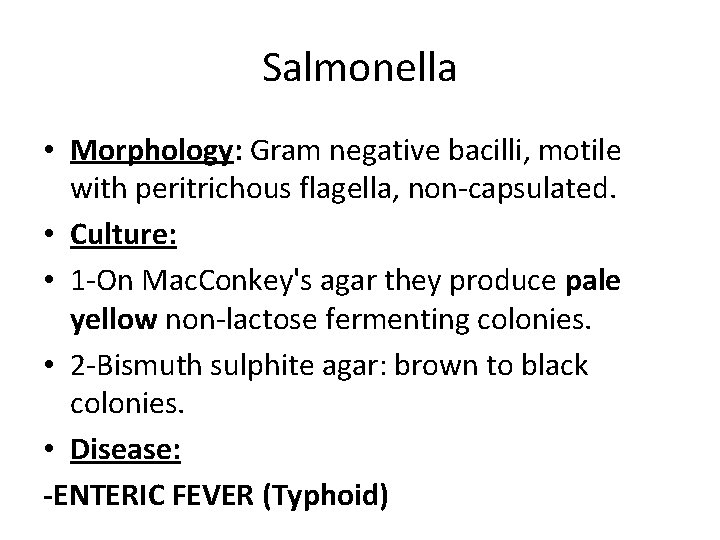
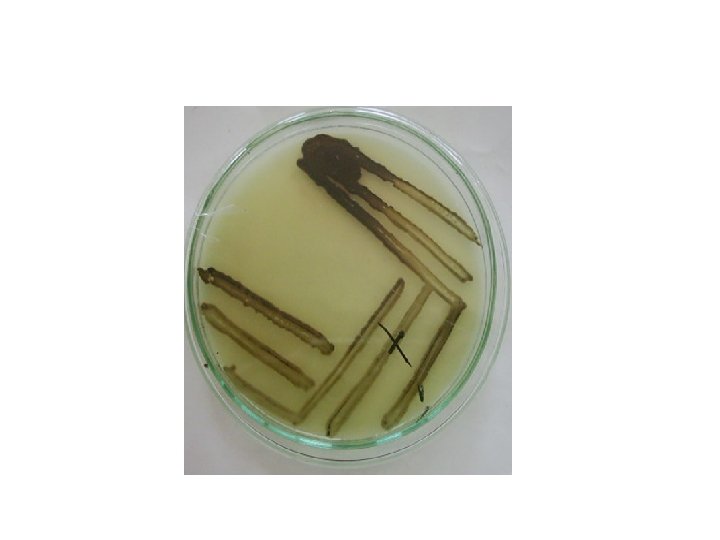
Salmonella • Morphology: Gram negative bacilli, motile with peritrichous flagella, non-capsulated. • Culture: • 1 -On Mac. Conkey's agar they produce pale yellow non-lactose fermenting colonies. • 2 -Bismuth sulphite agar: brown to black colonies. • Disease: -ENTERIC FEVER (Typhoid)
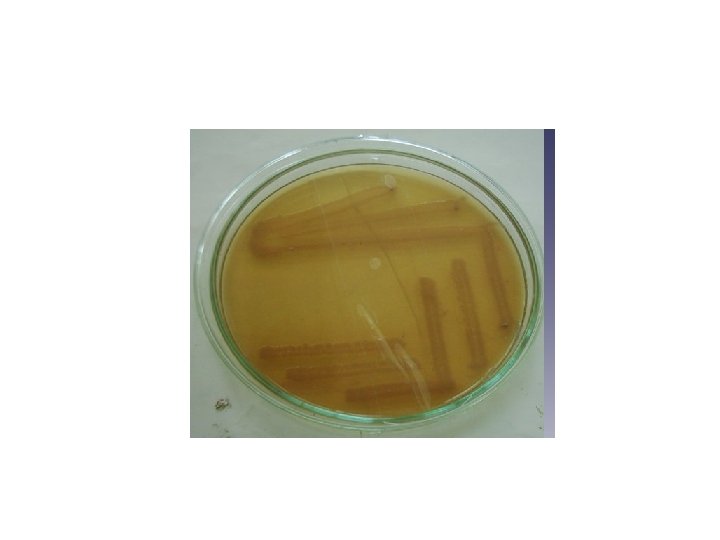
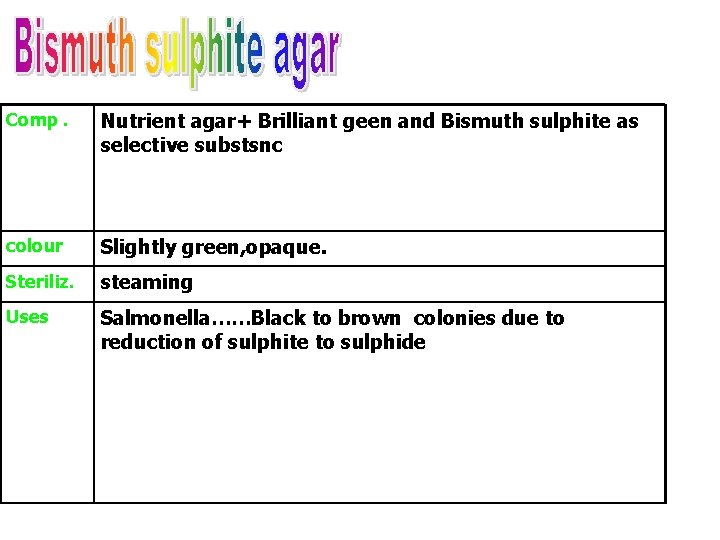
Comp. Nutrient agar+ Brilliant geen and Bismuth sulphite as selective substsnc colour Slightly green, opaque. Steriliz. steaming Uses Salmonella……Black to brown colonies due to reduction of sulphite to sulphide
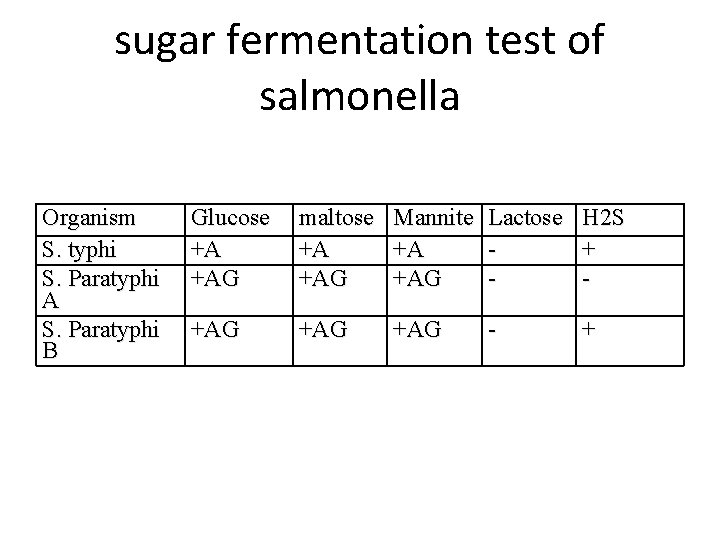
sugar fermentation test of salmonella Organism S. typhi S. Paratyphi A S. Paratyphi B Glucose +A +AG maltose Mannite Lactose H 2 S +A +A + +AG - +AG +AG - +
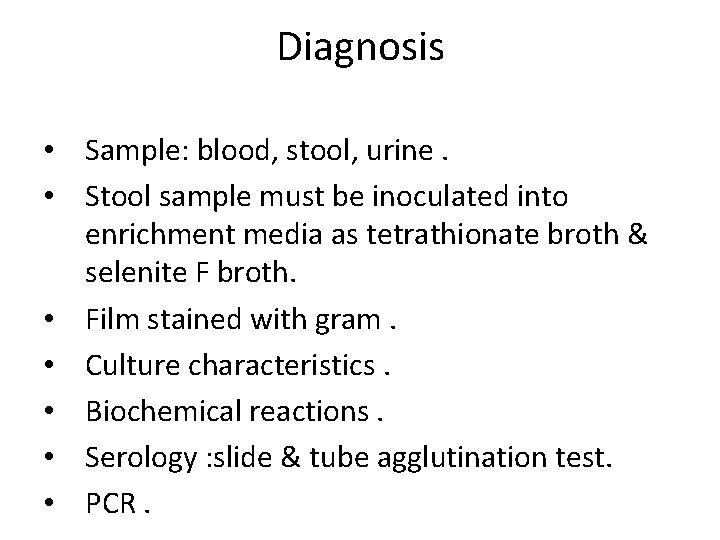
Diagnosis • Sample: blood, stool, urine. • Stool sample must be inoculated into enrichment media as tetrathionate broth & selenite F broth. • Film stained with gram. • Culture characteristics. • Biochemical reactions. • Serology : slide & tube agglutination test. • PCR.
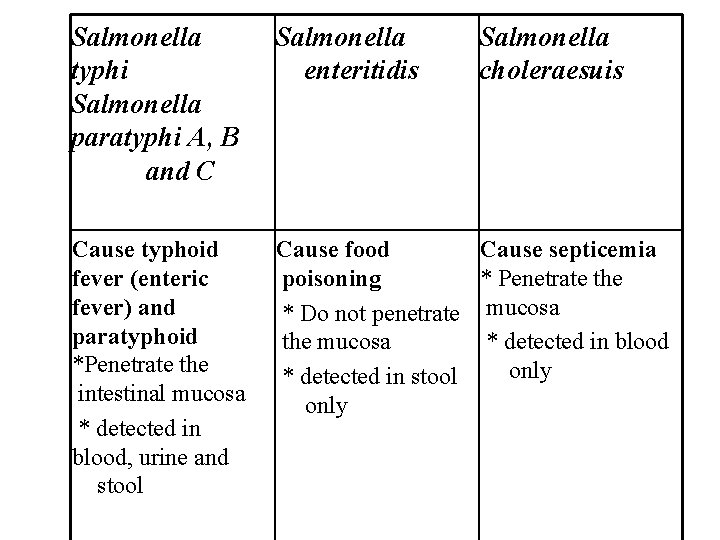
Salmonella typhi Salmonella paratyphi A, B and C Salmonella enteritidis Salmonella choleraesuis Cause typhoid fever (enteric fever) and paratyphoid *Penetrate the intestinal mucosa * detected in blood, urine and stool Cause food Cause septicemia poisoning * Penetrate the * Do not penetrate mucosa the mucosa * detected in blood only * detected in stool only
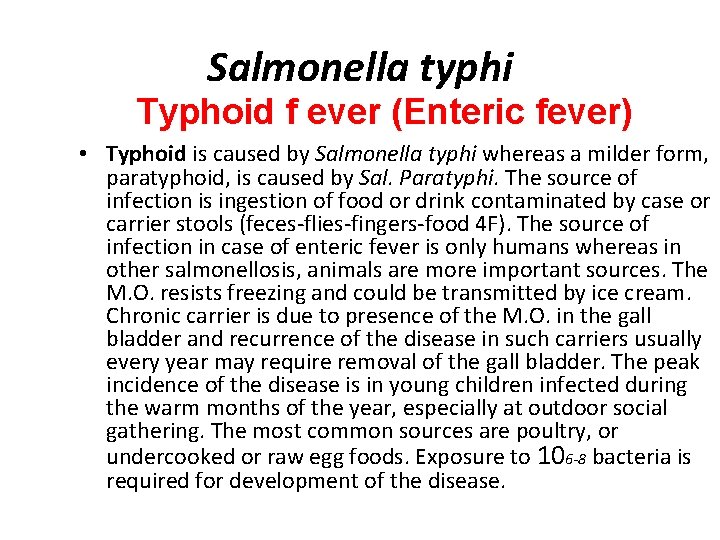
Salmonella typhi Typhoid f ever (Enteric fever) • Typhoid is caused by Salmonella typhi whereas a milder form, paratyphoid, is caused by Sal. Paratyphi. The source of infection is ingestion of food or drink contaminated by case or carrier stools (feces-flies-fingers-food 4 F). The source of infection in case of enteric fever is only humans whereas in other salmonellosis, animals are more important sources. The M. O. resists freezing and could be transmitted by ice cream. Chronic carrier is due to presence of the M. O. in the gall bladder and recurrence of the disease in such carriers usually every year may require removal of the gall bladder. The peak incidence of the disease is in young children infected during the warm months of the year, especially at outdoor social gathering. The most common sources are poultry, or undercooked or raw egg foods. Exposure to 106 -8 bacteria is required for development of the disease.
• The incubation period is 2 weeks, during which the M. O. multiplies in Peyer′s patches, then passes to the blood through the lymphatics resulting in bacteraemia that persists for one week. In the second week the M. O. passes to different organs including again the Peyer′s patches of the intestine causing ulcers, gall bladder, liver, kidneys and sometimes the bone marrow, rarely the lungs or meninges.
Clinical signs Fever, headache, malaise, delirium and tender abdomen with dough like touch. Sometimes rose spots appear Complications of the disease include intestinal hemorrhage and perforation Chronic carrier is due to presence of the M. O. in the gall bladder and recurrence in such carriers usually every year may require removal of the gall bladder
Laboratory diagnosis Depend on the stage of the disease The diagnosis done by: 1)Isolation of the organism 2)Serological diagnosis
Isolation of the organism Specimen: Blood (1 stweek), urine (2 ndweek), and stool (3 rdweek).
Isolation from the blood: . . In the first week. . 5 -10 ml of patient blood+50 -100 ml bile salt broth. . . subculture on: Mac. Conkeys agar (differential media): pale yellow colonies(NLF) DCA=deoxycholate and citrate agar (selective media) : pale colonies
• M. O disappear from the blood shortly after chloramphenicol therapy……so bl. Culture has no value.
Isolation from urine: M. O is discharged in urine from 2 nd week onwards. Discharged intermittently so repeated samples are taken. Urine sample is centrifuged & the deposit is inoculated on Mac. Conkeys agar & DCA.
Isolation from stool M. O is found in the stool throughout the course of illness but best isolated during 2 nd & 3 rd ws of infection. Discharged intermittently so repeated samples are taken.
• Culture on enrichment medium (selenite F or tetrathionate) that inhibits coliforms and allow growth of Salmonella & Shigella. Then • Culture on selective medium (salmonella. Shigella{SS} or deoxycholate and citrate agar), which support the growth of both M. O. s. Then • Culture on differential medium {Mac. Conkey, or triple sugar iron agar}. White colonies-alkaline slope, acid butt
Isolated organism freom blood , urine or stool can be identified by: 1 - stain: Gram-negative rods motile with peritrichous flagella & non capsulated. 2 -culture: . . on bismuth sulphite media: salmonella form brown to black colonies due to reduction of sulphite to sulphide
Serological identification • 1 -serological typing: By slide agglutination method using anti salmonella serum. • 2 -serological diagnosis: To detect antibodies to salmonella by Widal agglutination reaction, positive from the second week and on
Widal test. . Serial dilutions of patient serum are prepared in serial sets of test tubes. . To each sets a different suspension of salm is added. . {O} antigen is shared between Sal. Typhi & paratyphi. . . Specific {H} antigen is used for each of Sal. Typhi & paratyphi Tubes incubated at 37 C 0 for 2 -4 hr then examined for agglutination with different suspension.
• titre: highst dilution of patient serum show agglutinatuion. . High anti {O} titer indicates active infection (160 or more). . . High anti {H} titer indicates post infection or vaccination & determine which type causing infection. . . High anti {Vi} titer indicates carrier (200 or more). . In Egypt titer of 80 is of no significance, since the disease is endemic.
. . false +ve results: 1 -in recent vaccinated individuals: however in this case agglutination occur with more than on suspension & if the vaccine was given long time ago…no agglutination occur with o suspension 2 -non enteric infection: Due to cross reacting Ab
. . False –ve result: 1 - if the test done in first week 2 -if the patient receive antibiotic early in the disease…Ab titre will be supressed So for proper Interpretion of the test, 2 serum samples 10 days apart are taken to detect rising Ab titre that indicates active enteric fever.
Diagnosis of carier • 1 -urinary carrier: the sample is urine • 2 - billiary carrier: do dudenal drainage or stool sample after giving a cholegogue to empty the GB Then do same previous steps +. . High anti {Vi} titer indicates carrier (200 or more). .
Control: • Proper sanitation of food and drink & Proper waste treatment of sewage • Examination of food handlers • Vaccination with TAB vaccine (heat killed phenol preserved Sal. Typhi and para typhi A & B. A live attenuated oral vaccine of avirulent strain of Sal. Typhi and a Vi capsular polysaccharide capsule proved to be more effective.
Treatment: • Chloramphenicol was the drug of choice. Ampicillin, quinolone (tarvid) and trimethoprim-sulphamethoxazole are effective. • Ceftriaxone is used for resistant strains
Proteus • It is widely distributed in the nature in manure, sewage, soil. • Important sp. are : Proteus vulgaris & p. mirabilis
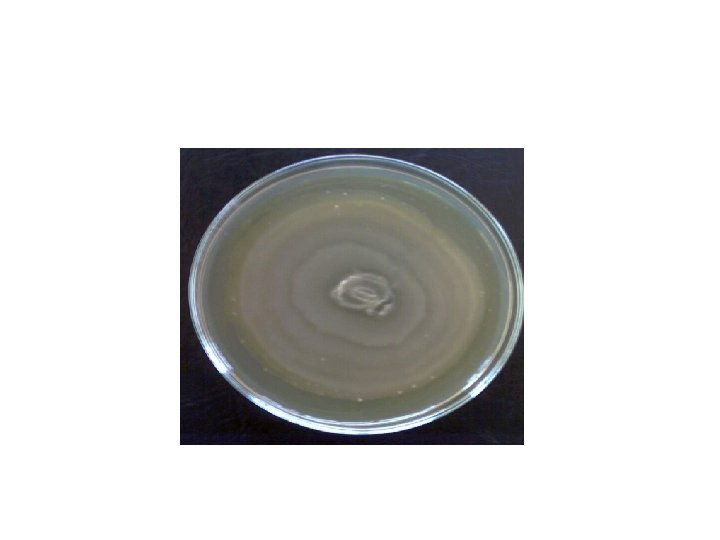
• Morphology: Gram negative bacilli, very pleomorphic and highly motile. • Culture: 1 - On Mac. Conkey's agar: they produce pale yellow non-lactose fermenting colonies. 2 - On nutrient agar: Due to their high motility, they give colonies which swarm in successive waves over the surface (swarming).
Biochemical reactions: • 1 - urease positive. • 2 -They produce H 2 S which blackens the butt of triple sugar iron (TSI) agar.
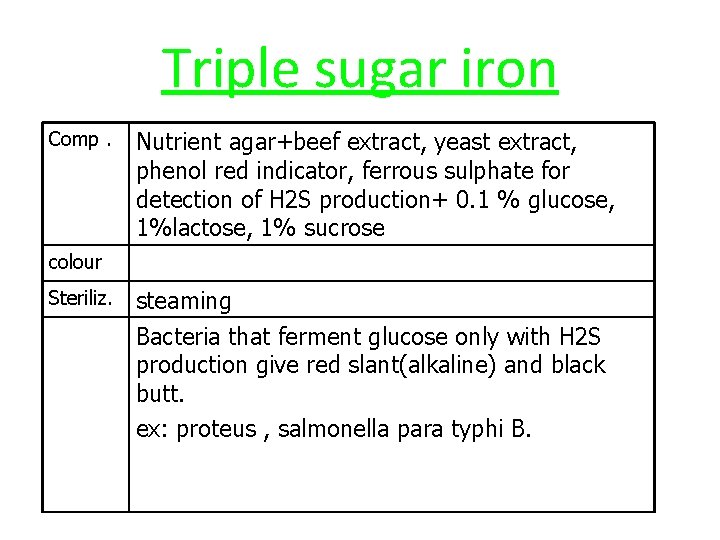
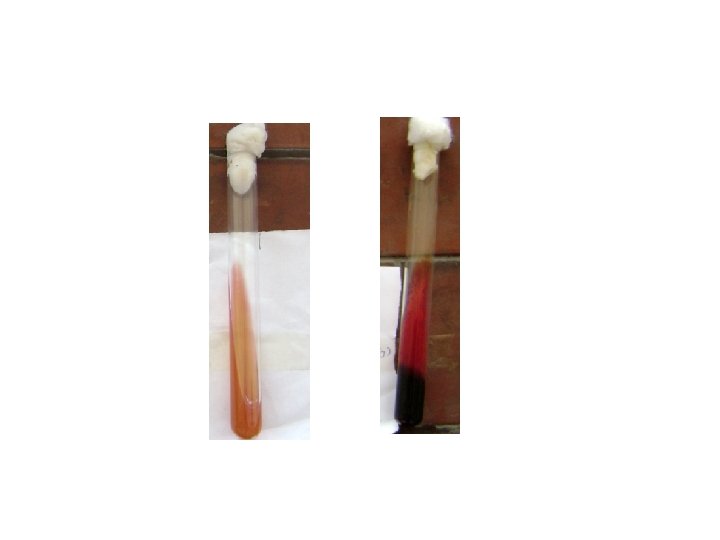
Triple sugar iron Comp. Nutrient agar+beef extract, yeast extract, phenol red indicator, ferrous sulphate for detection of H 2 S production+ 0. 1 % glucose, 1%lactose, 1% sucrose colour Steriliz. steaming Bacteria that ferment glucose only with H 2 S production give red slant(alkaline) and black butt. ex: proteus , salmonella para typhi B.
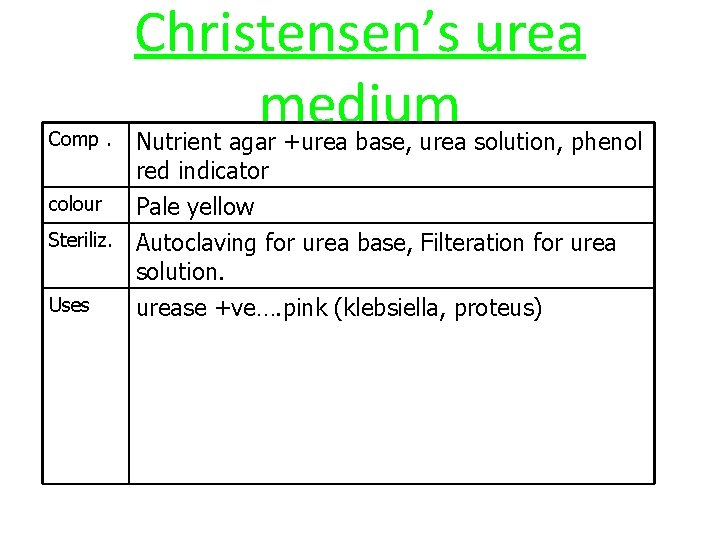
Comp. Christensen’s urea medium Nutrient agar +urea base, urea solution, phenol red indicator colour Pale yellow Steriliz. Autoclaving for urea base, Filteration for urea solution. Uses urease +ve…. pink (klebsiella, proteus)

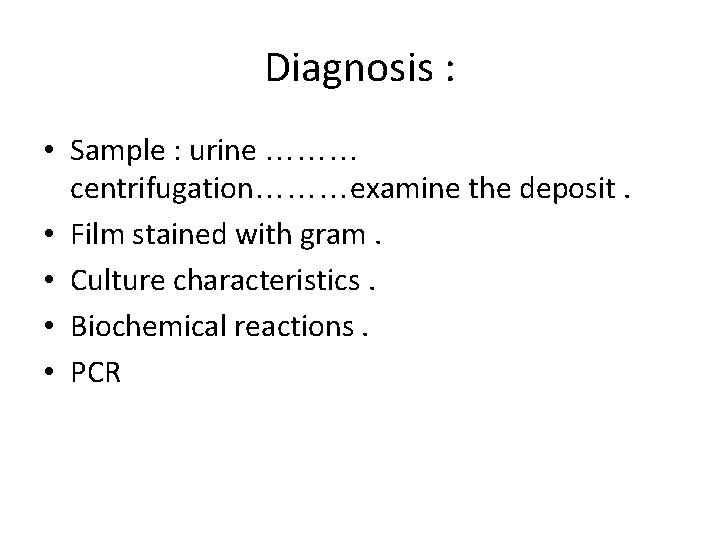
Diagnosis : • Sample : urine ……… centrifugation………examine the deposit. • Film stained with gram. • Culture characteristics. • Biochemical reactions. • PCR
SHIGELLA
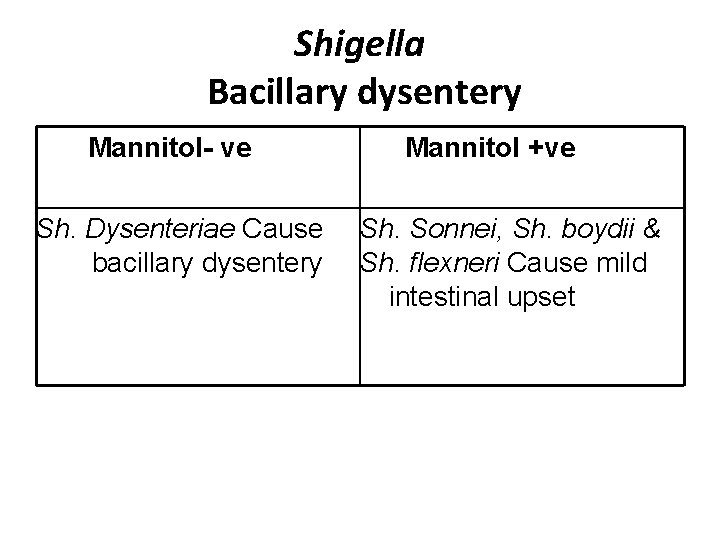
Shigella Bacillary dysentery Mannitol- ve Sh. Dysenteriae Cause bacillary dysentery Mannitol +ve Sh. Sonnei, Sh. boydii & Sh. flexneri Cause mild intestinal upset
• Bacillary dysentery is characterized by abdominal cramps and tenesmus, bloody diarrhea with abundant pus and fever. The disease is self-limiting. The incubation period varies between 1 to 3 days. Pathogenesis of Shigella sp. is mainly due to invasion of the colon mucosa. The M. O. secretes an exotoxin causing ulceration of the intestinal mucosa with formation of pseudomembranes and bloody diarrhea. Sh. Dysenteriae shiga type produces the most potent exotoxin which act as enterotoxin and neurotoxin causing necrosis of the cells of the colon. The bacilli rarely penetrate beyond the intestinal mucosa
• Shigella infection is alwayes limited to GIT & blood stream invasion is very rare. • Shigella infection is highly communicable due to low dose of infection(10^3 org) while it is 10^5 -10^8 M. O for salmonella. • Epidemiology: 4 F transmission, usually spreads in low hygiene communities
Serotypes of shigella Shigella are divided into 4 groups according to O antigen: Group A: Sh. Dysenteriae(the most severe form of bacilliary dysentry) Group B: Sh. flexneri Group C: Sh. boydii Group D: Sh. Sonnei
Laboratory diagnosis • Specimen: Stool or rectal swab • Microscopic exam. Of fresh stool show large No. of leucocytes & RBCs • Stain: gram negative rods, non motile , non caps. , non spore forming. • Isolation of the M. O. on culture media (enrichment, selective and differential) as in salmonella. • Biochemical reaction: ferment glucose with acid production and is H 2 S negative so on TSI give acidic butt & alk. slant.
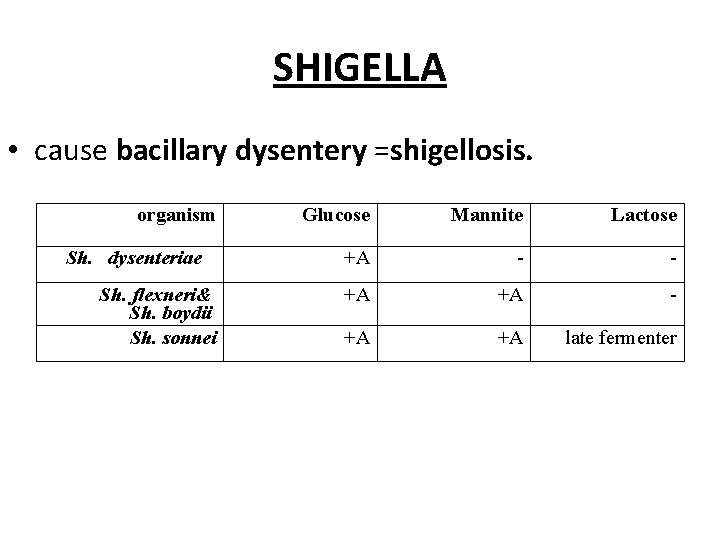
SHIGELLA • cause bacillary dysentery =shigellosis. organism Sh. dysenteriae Sh. flexneri& Sh. boydii Sh. sonnei Glucose Mannite Lactose +A - - +A +A late fermenter
• * Serological agglutination reaction: of little value !!!!! • Treatment: Ampicillin or tetracycline, • also trimethoprim + sulfamethoxazole
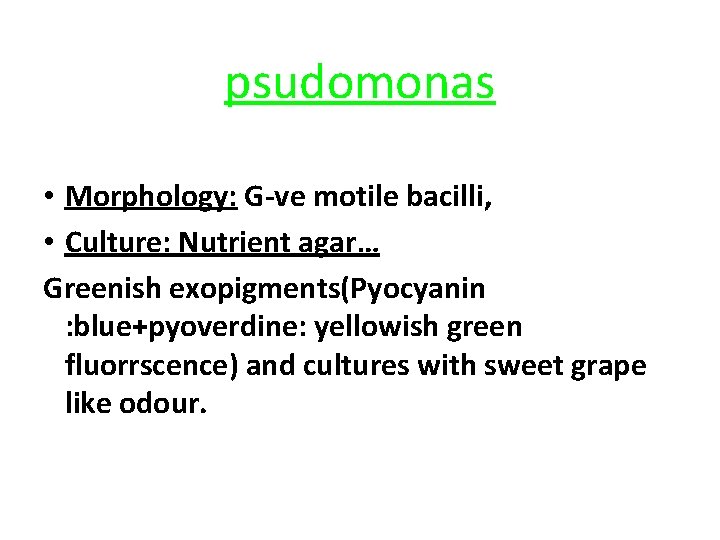
psudomonas • Morphology: G-ve motile bacilli, • Culture: Nutrient agar… Greenish exopigments(Pyocyanin : blue+pyoverdine: yellowish green fluorrscence) and cultures with sweet grape like odour.

b- – greenish exopigment of Pseudomonas
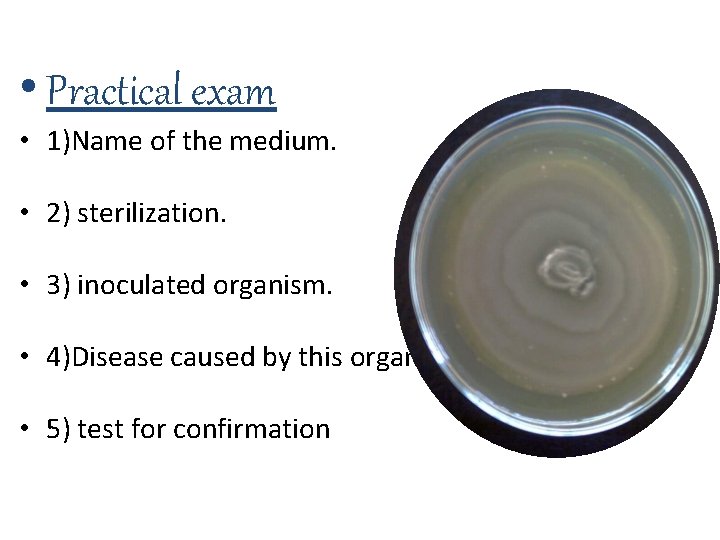
• Practical exam • 1)Name of the medium. • 2) sterilization. • 3) inoculated organism. • 4)Disease caused by this organism. • 5) test for confirmation
- Slides: 53