ENTERAL AND PARENTERAL NUTRITION IN CRITICALLY ILL CHILDREN

- Slides: 46
ENTERAL AND PARENTERAL NUTRITION IN CRITICALLY ILL CHILDREN Mudit Mathur, M. D. SUNY Downstate Medical Center
LEARNING GOALS l Impact of Critical Illness l Importance of Nutrition l Goals of nutritional support l Nutritional requirements l Enteral vs Parenteral l When and how to initiate and advance Nutrition l Monitoring
IMPACT OF CRITICAL ILLNESS-1 l. Physiologic stress response : Catabolic phase increased caloric needs, urinary nitrogen losses l inadequate intake wasting of endogenous protein stores, gluconeogenesis l mass reduction of muscle-protein breakdown l
IMPACT OF CRITICAL ILLNESS-2 l Increased energy expenditure – Pain – Anxiety – Fever – Muscular effort-WOB, shivering
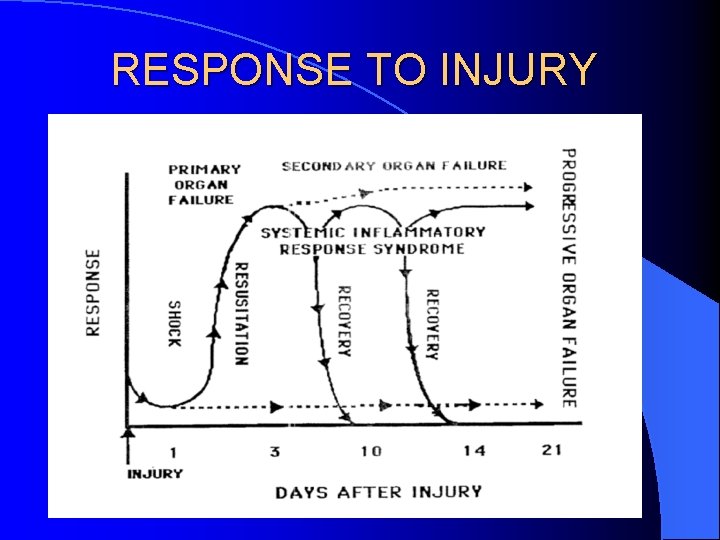
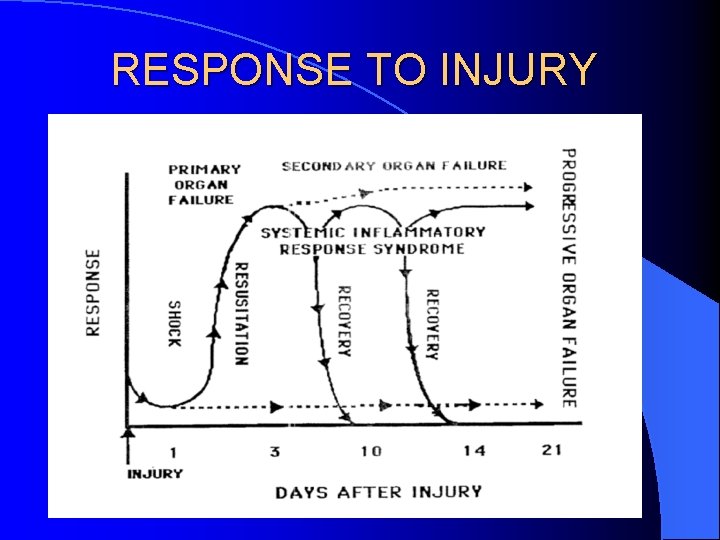
RESPONSE TO INJURY
WHY IS NUTRITION IMPORTANT CRITICAL ILLNESS + POOR NUTRITION = l Prolonged ventilator dependency l Prolonged ICU stay l Heightened susceptibility to nosocomial infections MSOF l Increased mortality with mild/moderate or severe malnutrition
NUTRITION: OVERALL GOALS ACCP Consensus statement, 1997 l Provide nutritional support appropriate for the individual patient’s – Medical condition – Nutritional status – Available routes for administration
NUTRITION: OVERALL GOALS l Prevent/treat macro/micronutrient deficiencies l Dose nutrients compatible with existing metabolism l Avoid complications l Improve patient outcomes
ENTERAL OR PARENTERAL
IMPACT OF STARVATION-1 l Negative nitrogen balance, further wt loss l Morphological changes in the gut – Mucosal thickness – Cell proliferation – Villus height l Functional changes – Increased permeability – Decreased absorption of amino acids
IMPACT OF STARVATION-2 l Enzymatic/Hormonal changes – Decreased sucrase and lactase l Impact on immunity – Cellular: Decreased T cells, atrophied germinal centers, mitogenic proliferation, differentiation, Th cell function, altered homing – Humoral: Complement, opsonins, Ig, secretory Ig. A – (70 -80% of all Ig produced is secretory Ig. A) – Increased bacterial translocation
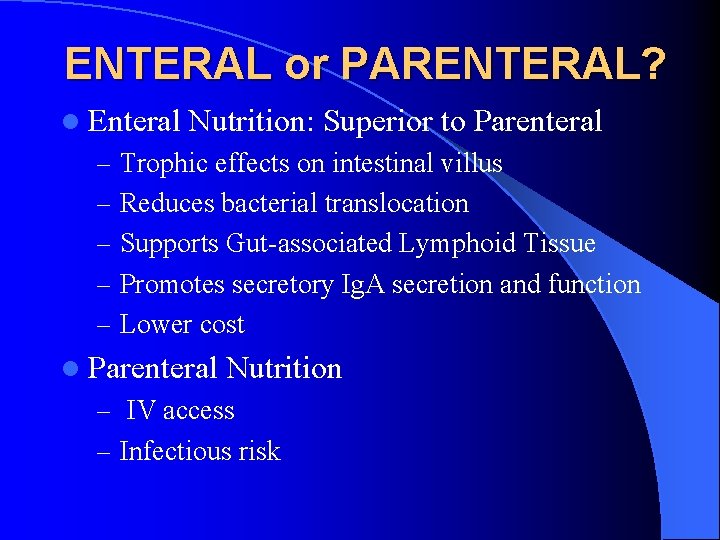
ENTERAL or PARENTERAL? l Enteral Nutrition: Superior to Parenteral – Trophic effects on intestinal villus – Reduces bacterial translocation – Supports Gut-associated Lymphoid Tissue – Promotes secretory Ig. A secretion and function – Lower cost l Parenteral Nutrition – IV access – Infectious risk
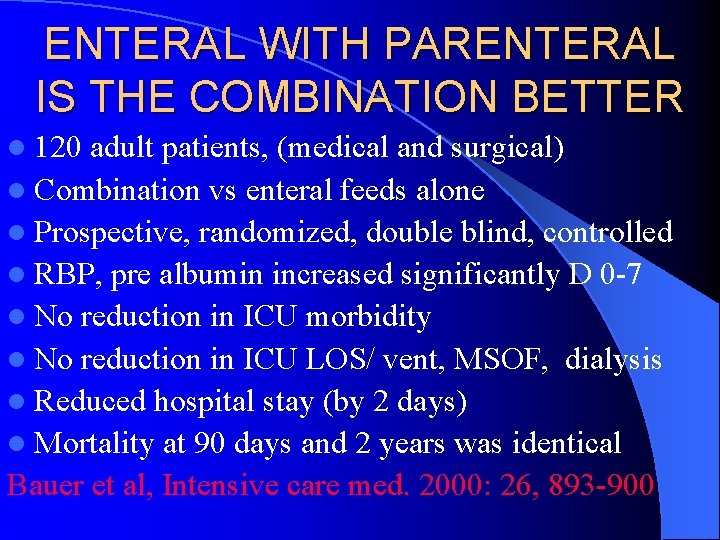
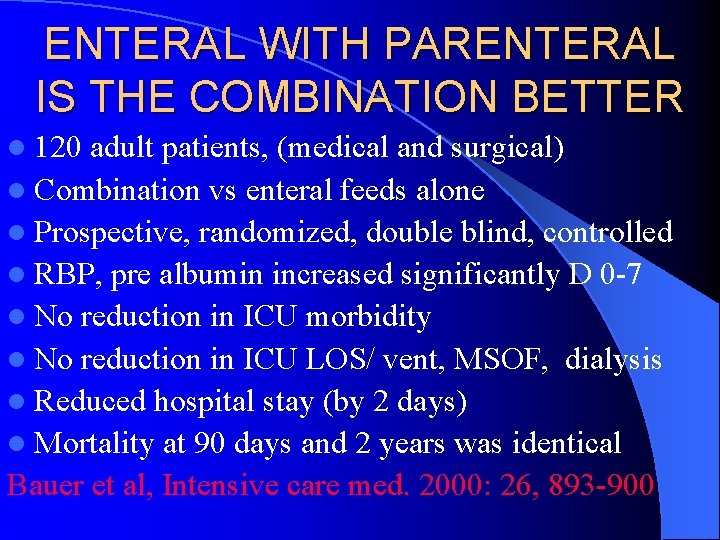
ENTERAL WITH PARENTERAL IS THE COMBINATION BETTER l 120 adult patients, (medical and surgical) l Combination vs enteral feeds alone l Prospective, randomized, double blind, controlled l RBP, pre albumin increased significantly D 0 -7 l No reduction in ICU morbidity l No reduction in ICU LOS/ vent, MSOF, dialysis l Reduced hospital stay (by 2 days) l Mortality at 90 days and 2 years was identical Bauer et al, Intensive care med. 2000: 26, 893 -900
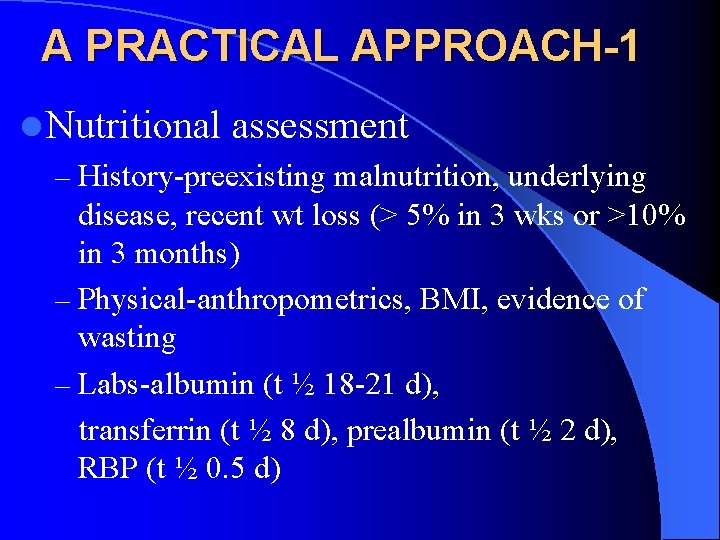
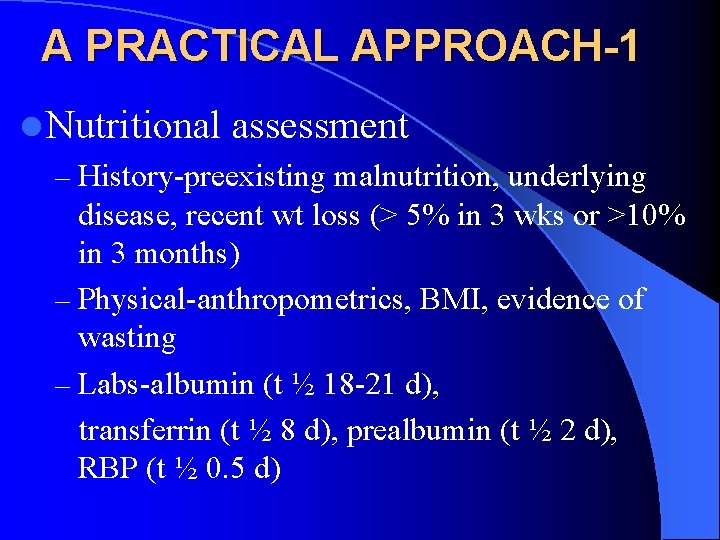
A PRACTICAL APPROACH-1 l Nutritional assessment – History-preexisting malnutrition, underlying disease, recent wt loss (> 5% in 3 wks or >10% in 3 months) – Physical-anthropometrics, BMI, evidence of wasting – Labs-albumin (t ½ 18 -21 d), transferrin (t ½ 8 d), prealbumin (t ½ 2 d), RBP (t ½ 0. 5 d)
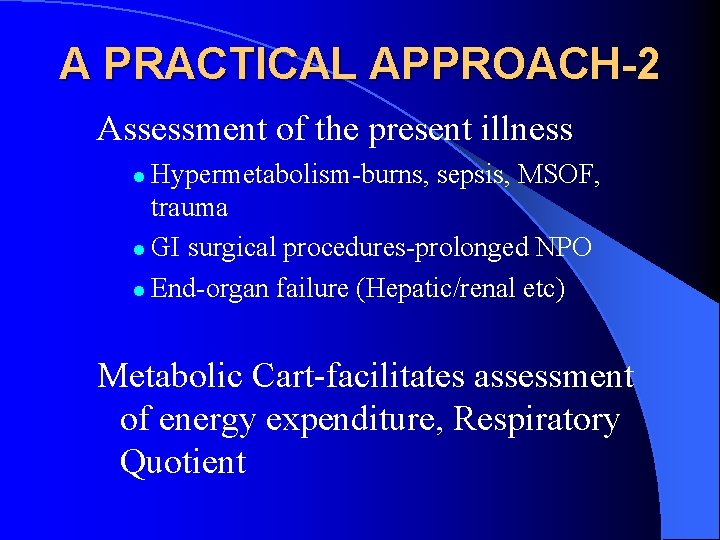
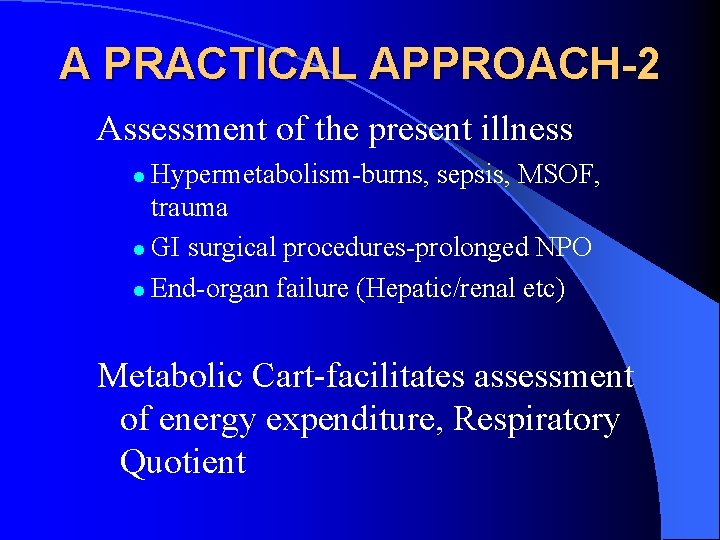
A PRACTICAL APPROACH-2 Assessment of the present illness Hypermetabolism-burns, sepsis, MSOF, trauma l GI surgical procedures-prolonged NPO l End-organ failure (Hepatic/renal etc) l Metabolic Cart-facilitates assessment of energy expenditure, Respiratory Quotient
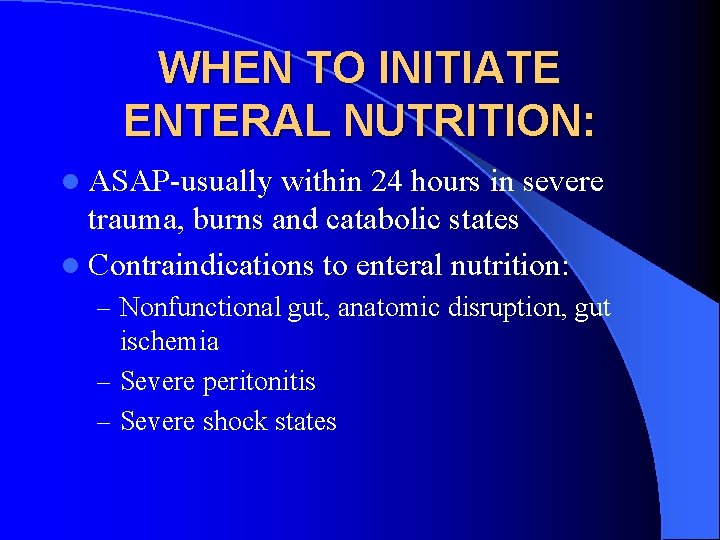
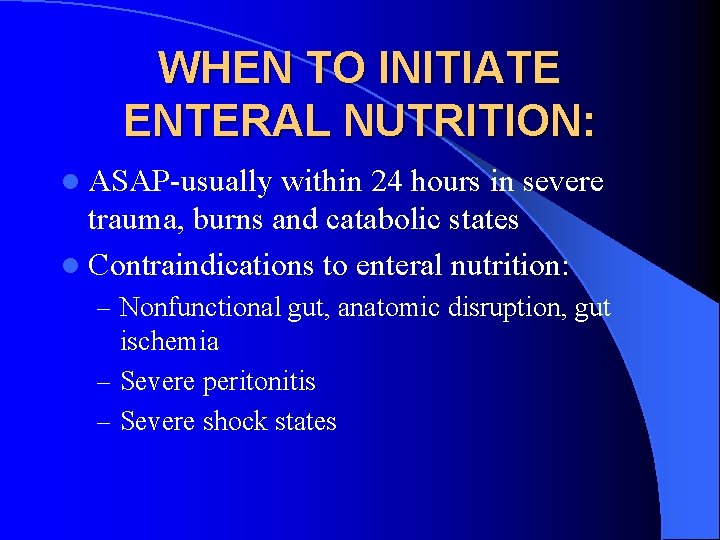
WHEN TO INITIATE ENTERAL NUTRITION: l ASAP-usually within 24 hours in severe trauma, burns and catabolic states l Contraindications to enteral nutrition: – Nonfunctional gut, anatomic disruption, gut ischemia – Severe peritonitis – Severe shock states
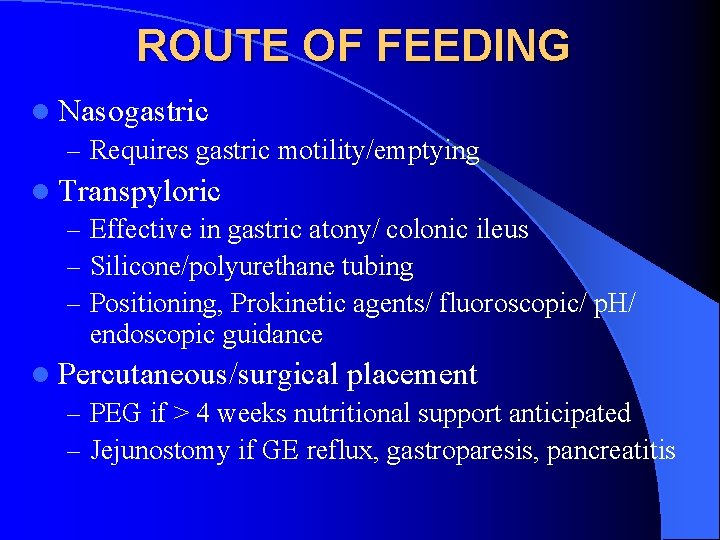
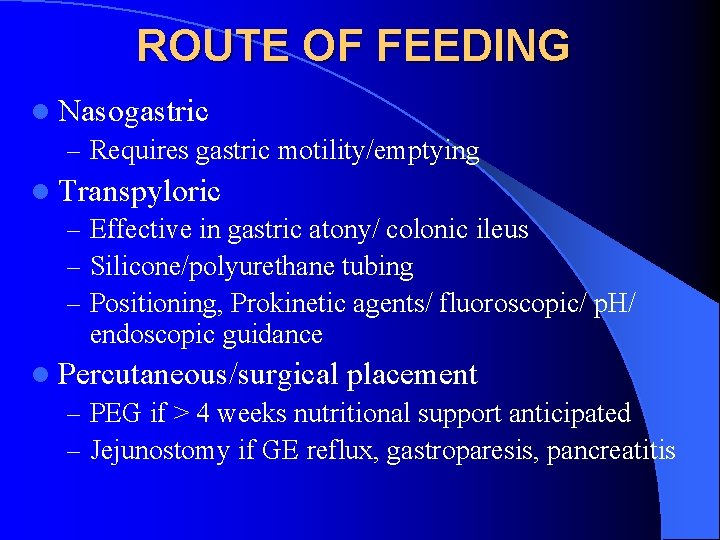
ROUTE OF FEEDING l Nasogastric – Requires gastric motility/emptying l Transpyloric – Effective in gastric atony/ colonic ileus – Silicone/polyurethane tubing – Positioning, Prokinetic agents/ fluoroscopic/ p. H/ endoscopic guidance l Percutaneous/surgical placement – PEG if > 4 weeks nutritional support anticipated – Jejunostomy if GE reflux, gastroparesis, pancreatitis
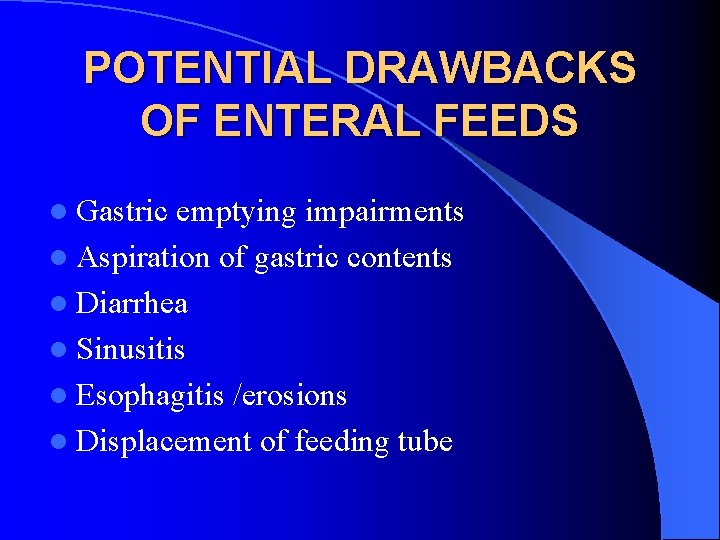
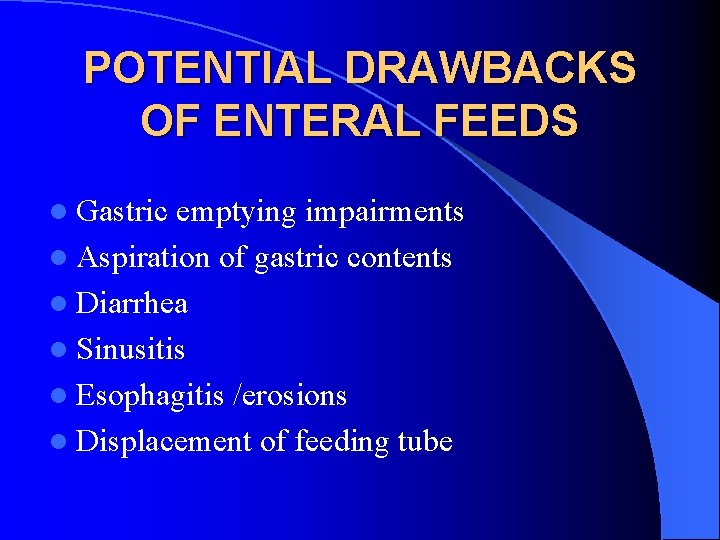
POTENTIAL DRAWBACKS OF ENTERAL FEEDS l Gastric emptying impairments l Aspiration of gastric contents l Diarrhea l Sinusitis l Esophagitis /erosions l Displacement of feeding tube
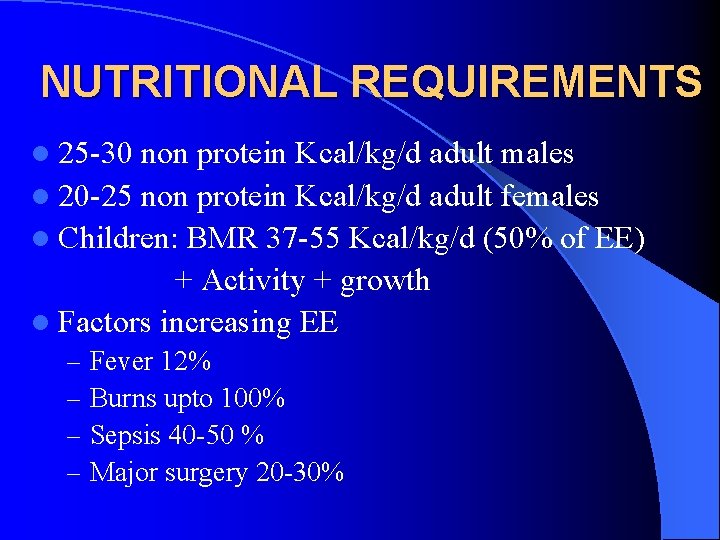
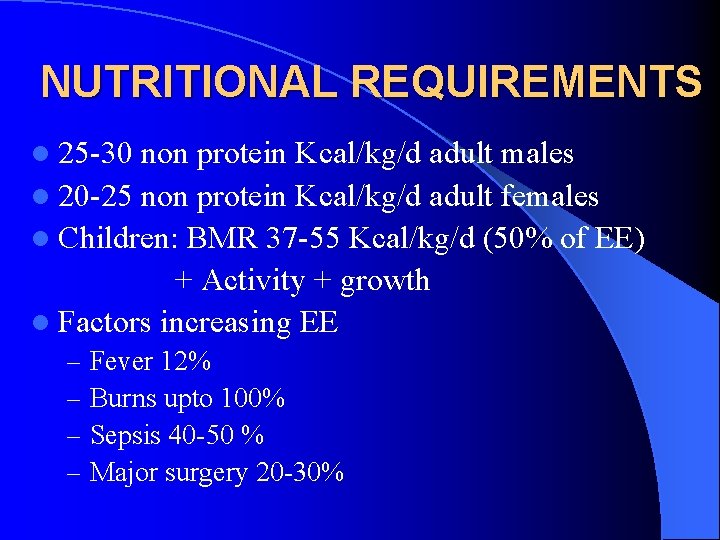
NUTRITIONAL REQUIREMENTS l 25 -30 non protein Kcal/kg/d adult males l 20 -25 non protein Kcal/kg/d adult females l Children: BMR 37 -55 Kcal/kg/d (50% of EE) + Activity + growth l Factors increasing EE – – Fever 12% Burns upto 100% Sepsis 40 -50 % Major surgery 20 -30%
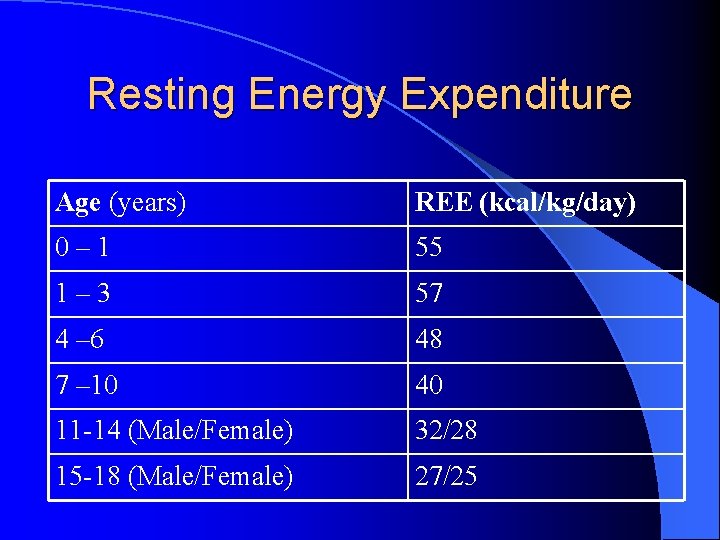
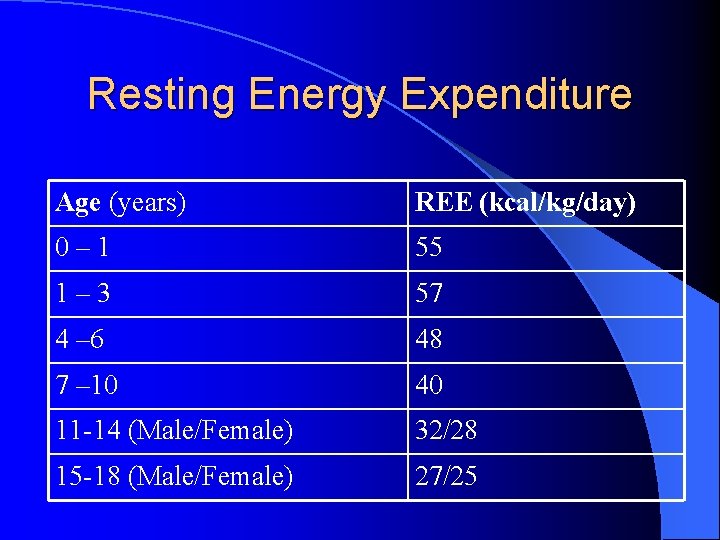
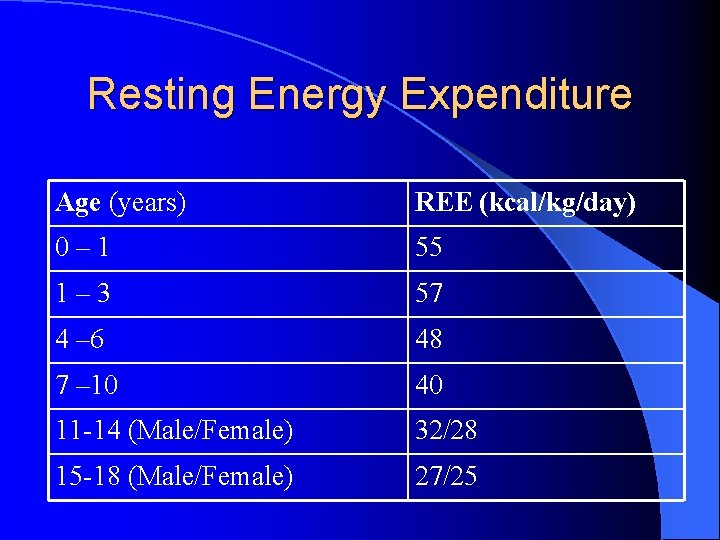
Resting Energy Expenditure Age (years) REE (kcal/kg/day) 0– 1 55 1– 3 57 4 – 6 48 7 – 10 40 11 -14 (Male/Female) 32/28 15 -18 (Male/Female) 27/25
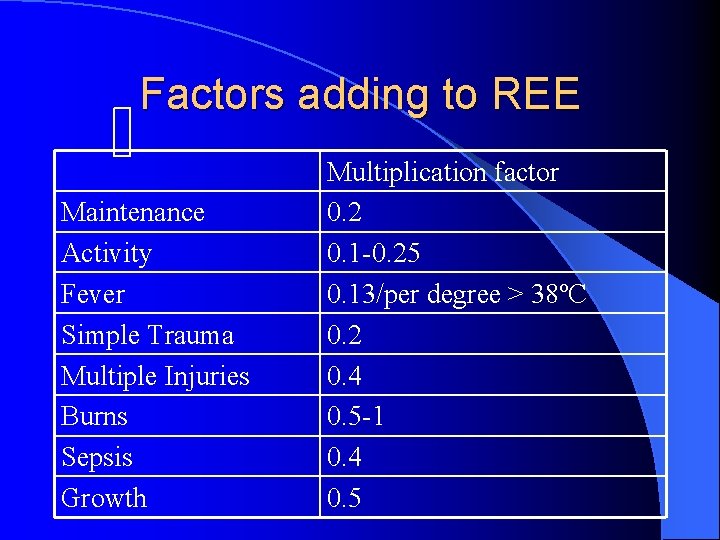
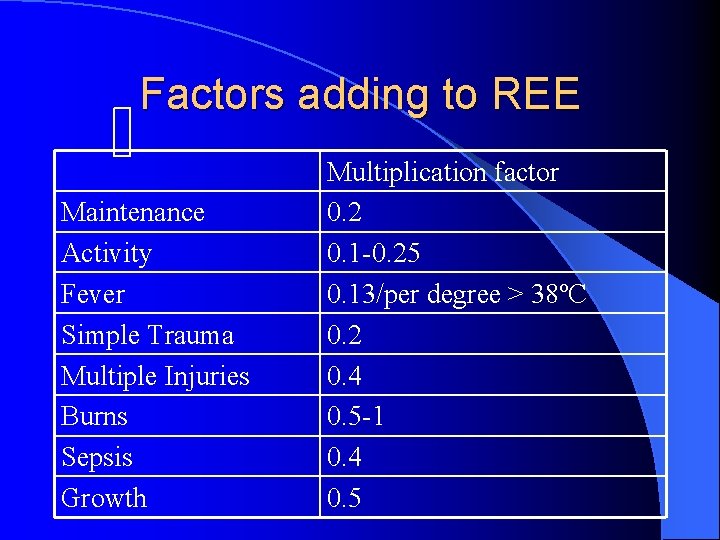
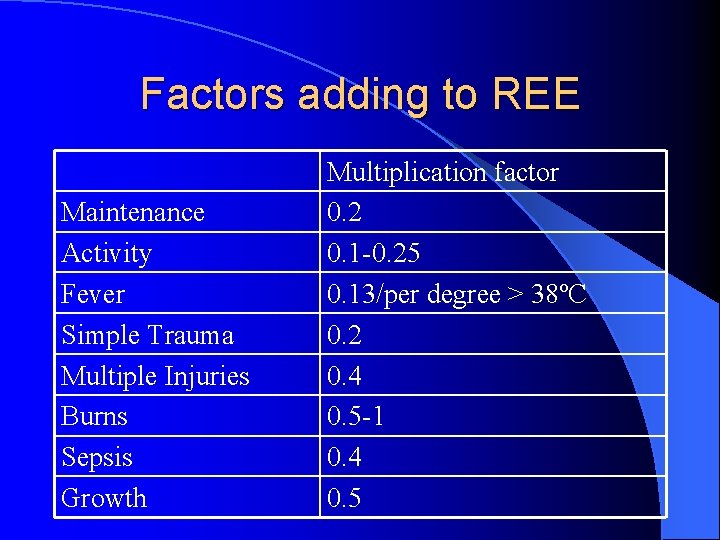
Factors adding to REE Maintenance Activity Fever Simple Trauma Multiple Injuries Burns Sepsis Growth Multiplication factor 0. 2 0. 1 -0. 25 0. 13/per degree > 38ºC 0. 2 0. 4 0. 5 -1 0. 4 0. 5
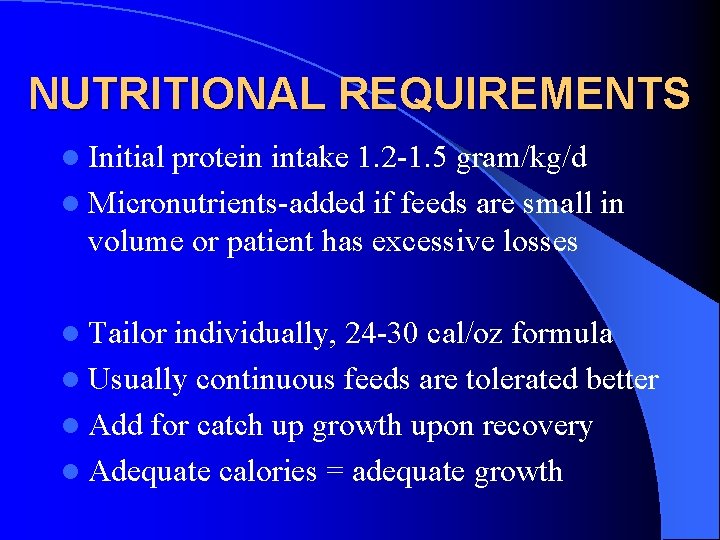
NUTRITIONAL REQUIREMENTS l Initial protein intake 1. 2 -1. 5 gram/kg/d l Micronutrients-added if feeds are small in volume or patient has excessive losses l Tailor individually, 24 -30 cal/oz formula l Usually continuous feeds are tolerated better l Add for catch up growth upon recovery l Adequate calories = adequate growth
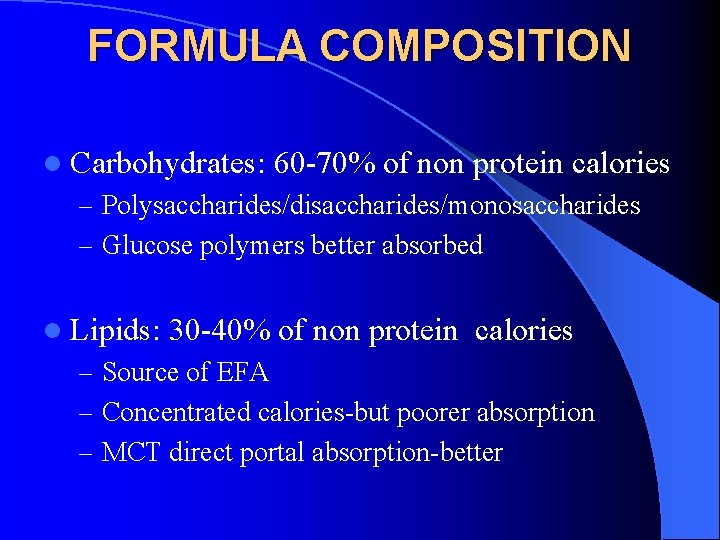
FORMULA COMPOSITION l Carbohydrates: 60 -70% of non protein calories – Polysaccharides/disaccharides/monosaccharides – Glucose polymers better absorbed l Lipids: 30 -40% of non protein calories – Source of EFA – Concentrated calories-but poorer absorption – MCT direct portal absorption-better
FORMULA COMPOSITION l Proteins – -polymeric (pancreatic enzymes required) or peptides – Small peptides from whey protein hydrolysis absorbed better than free AA l Fibers – Insoluble-reduce diarrhea, slower transit-better glycemic control – Degraded to SCFA-trophic to colon
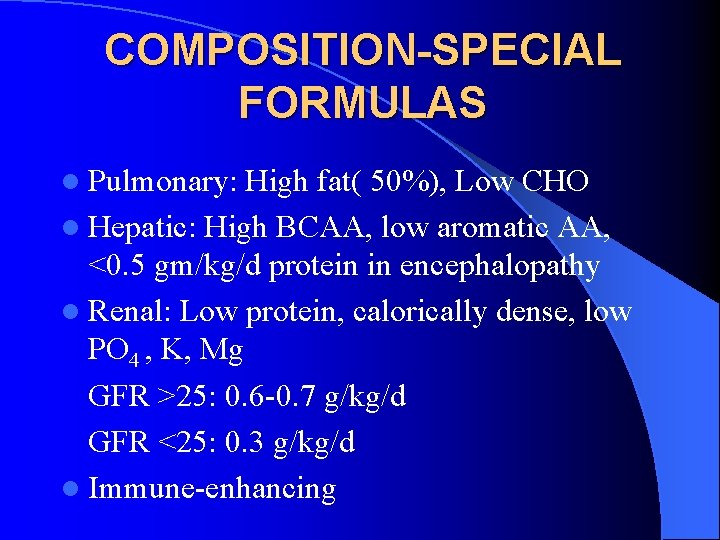
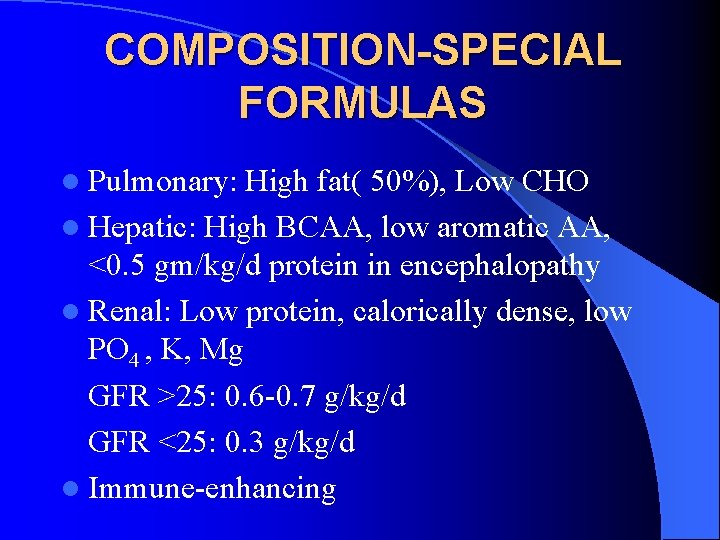
COMPOSITION-SPECIAL FORMULAS l Pulmonary: High fat( 50%), Low CHO l Hepatic: High BCAA, low aromatic AA, <0. 5 gm/kg/d protein in encephalopathy l Renal: Low protein, calorically dense, low PO 4 , K, Mg GFR >25: 0. 6 -0. 7 g/kg/d GFR <25: 0. 3 g/kg/d l Immune-enhancing
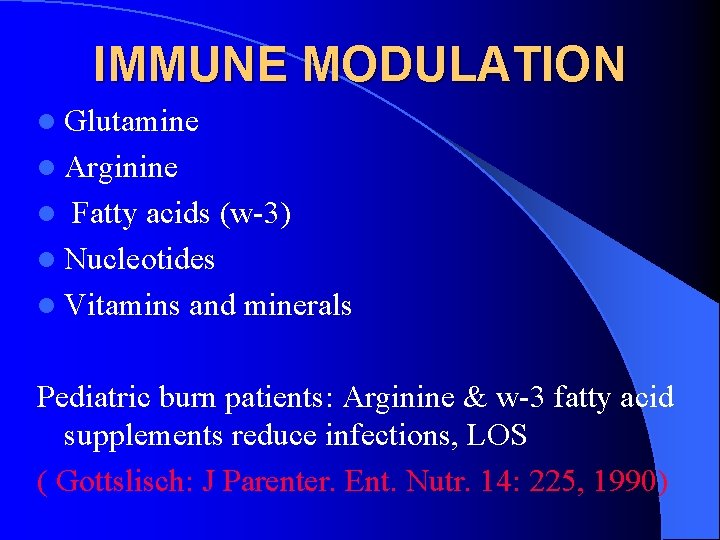
IMMUNE MODULATION l Glutamine l Arginine Fatty acids (w-3) l Nucleotides l Vitamins and minerals l Pediatric burn patients: Arginine & w-3 fatty acid supplements reduce infections, LOS ( Gottslisch: J Parenter. Ent. Nutr. 14: 225, 1990)
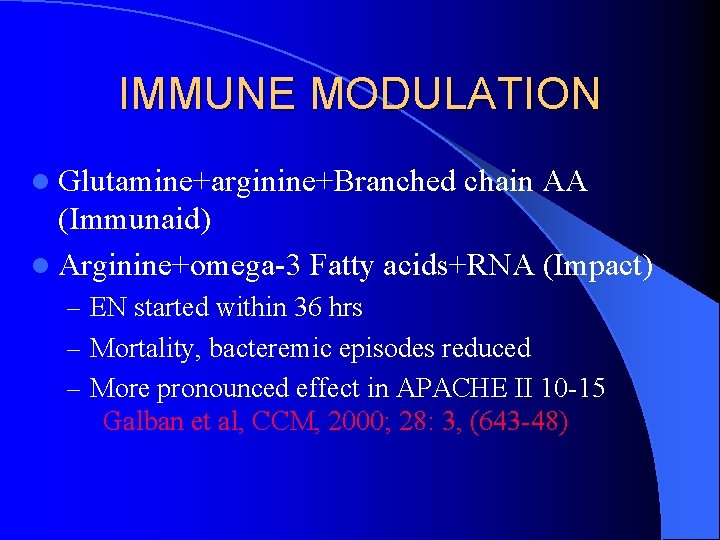
IMMUNE MODULATION l Glutamine+arginine+Branched chain AA (Immunaid) l Arginine+omega-3 Fatty acids+RNA (Impact) – EN started within 36 hrs – Mortality, bacteremic episodes reduced – More pronounced effect in APACHE II 10 -15 Galban et al, CCM, 2000; 28: 3, (643 -48)
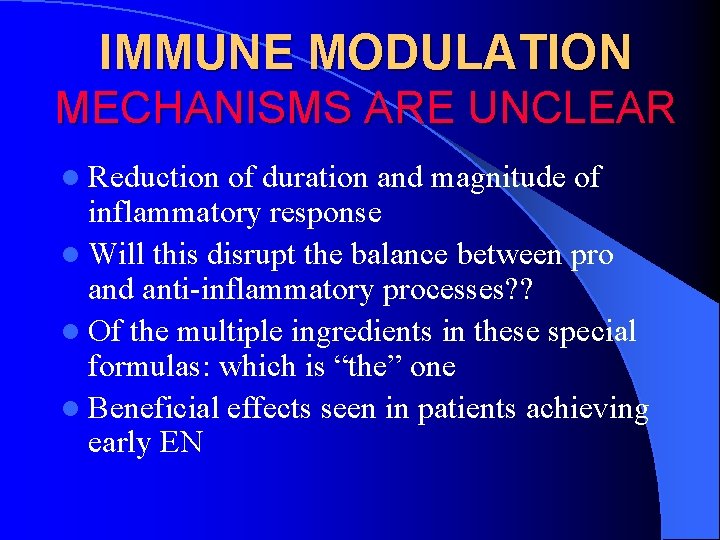
IMMUNE MODULATION MECHANISMS ARE UNCLEAR l Reduction of duration and magnitude of inflammatory response l Will this disrupt the balance between pro and anti-inflammatory processes? ? l Of the multiple ingredients in these special formulas: which is “the” one l Beneficial effects seen in patients achieving early EN
IMMUNE MODULATION Conclusive studies, clear indications & Cost-benefit analysis are still needed
ENTERAL NUTRITION IN CRITICAL ILLNESS: l Maintains nutritional status l Prevents catabolism l Provides resistance to infection l Potential effect on immune modulation
PARENTERAL NUTRITION (PN) The PN formulation is based on: l Fluid Requirements l Energy Requirements l Vitamins l Trace elements l Other additives-Heparin, H 2 blocker etc
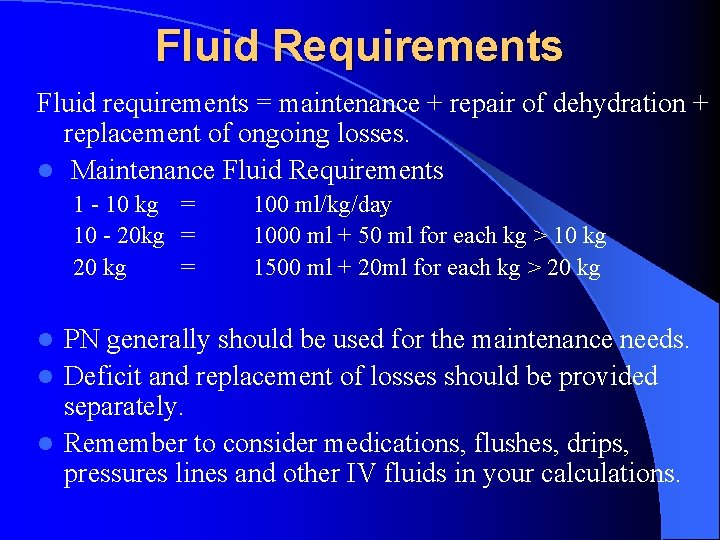
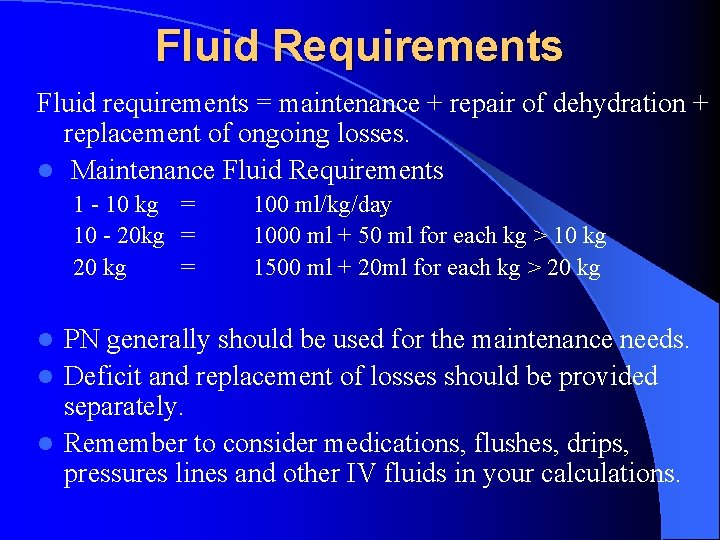
Fluid Requirements Fluid requirements = maintenance + repair of dehydration + replacement of ongoing losses. l Maintenance Fluid Requirements 1 - 10 kg = 10 - 20 kg = 20 kg = 100 ml/kg/day 1000 ml + 50 ml for each kg > 10 kg 1500 ml + 20 ml for each kg > 20 kg PN generally should be used for the maintenance needs. l Deficit and replacement of losses should be provided separately. l Remember to consider medications, flushes, drips, pressures lines and other IV fluids in your calculations. l
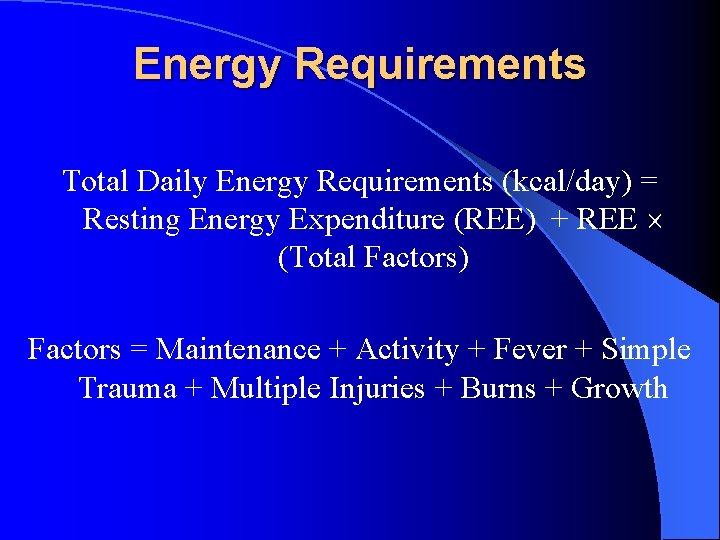
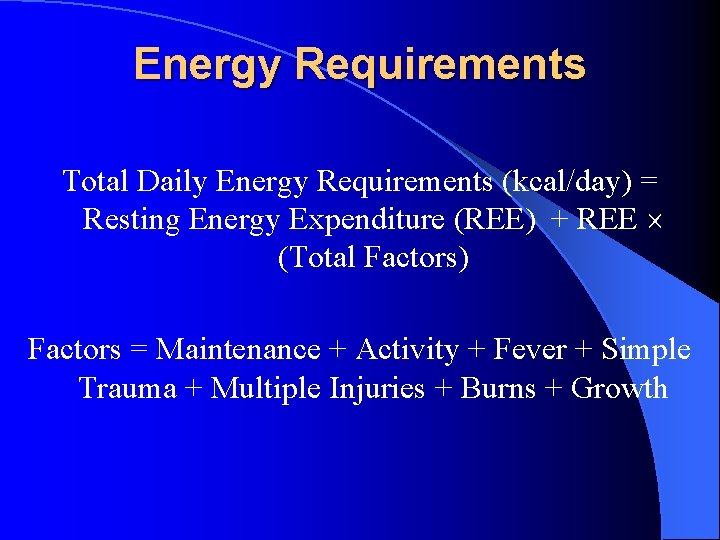
Energy Requirements Total Daily Energy Requirements (kcal/day) = Resting Energy Expenditure (REE) + REE (Total Factors) Factors = Maintenance + Activity + Fever + Simple Trauma + Multiple Injuries + Burns + Growth
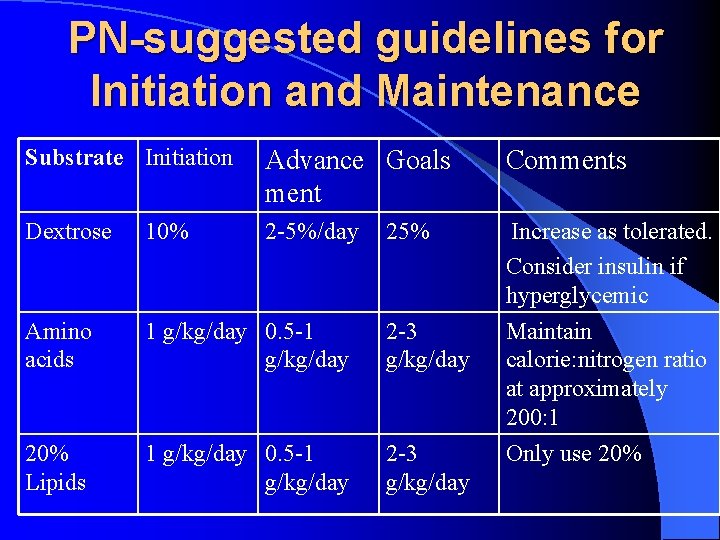
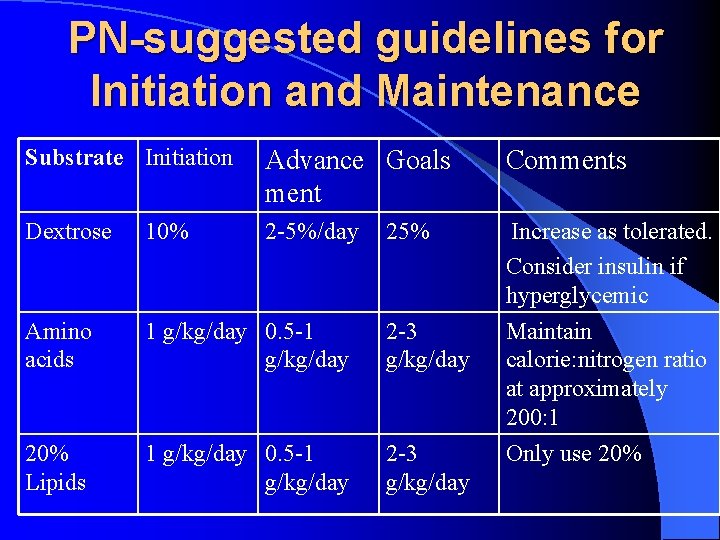
PN-suggested guidelines for Initiation and Maintenance Substrate Initiation Advance Goals ment Comments Dextrose 10% 2 -5%/day Amino acids 1 g/kg/day 0. 5 -1 g/kg/day 2 -3 g/kg/day 20% Lipids 1 g/kg/day 0. 5 -1 g/kg/day 2 -3 g/kg/day Increase as tolerated. Consider insulin if hyperglycemic Maintain calorie: nitrogen ratio at approximately 200: 1 Only use 20% 25%
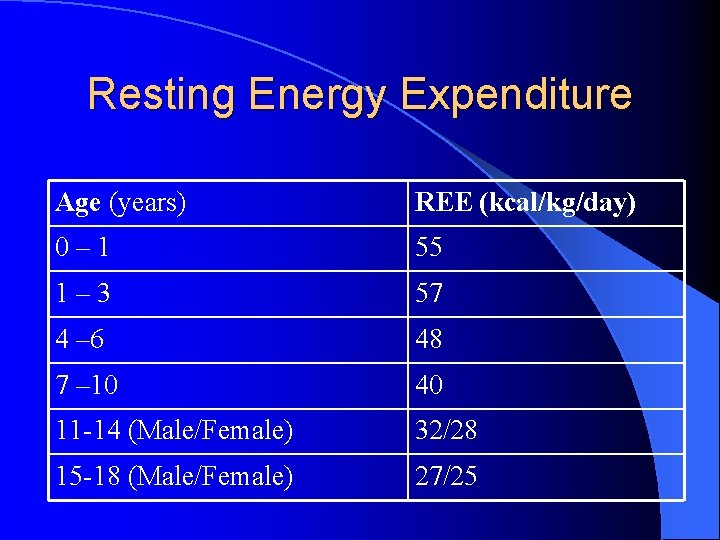
Resting Energy Expenditure Age (years) REE (kcal/kg/day) 0– 1 55 1– 3 57 4 – 6 48 7 – 10 40 11 -14 (Male/Female) 32/28 15 -18 (Male/Female) 27/25
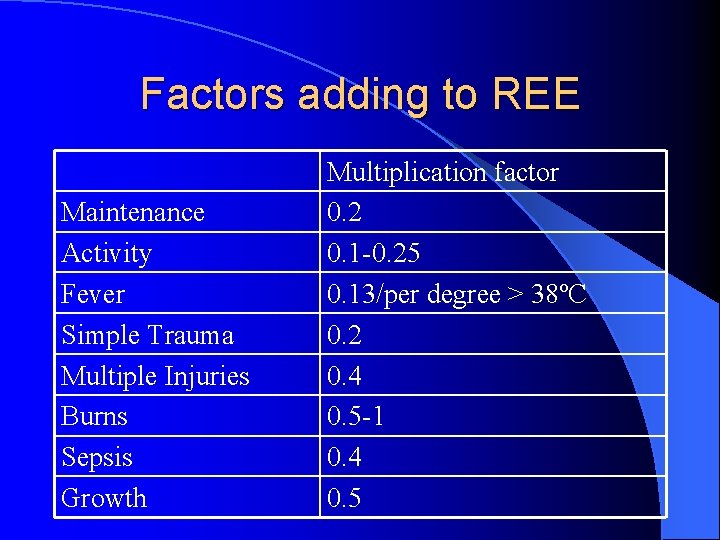
Factors adding to REE Maintenance Activity Fever Simple Trauma Multiple Injuries Burns Sepsis Growth Multiplication factor 0. 2 0. 1 -0. 25 0. 13/per degree > 38ºC 0. 2 0. 4 0. 5 -1 0. 4 0. 5
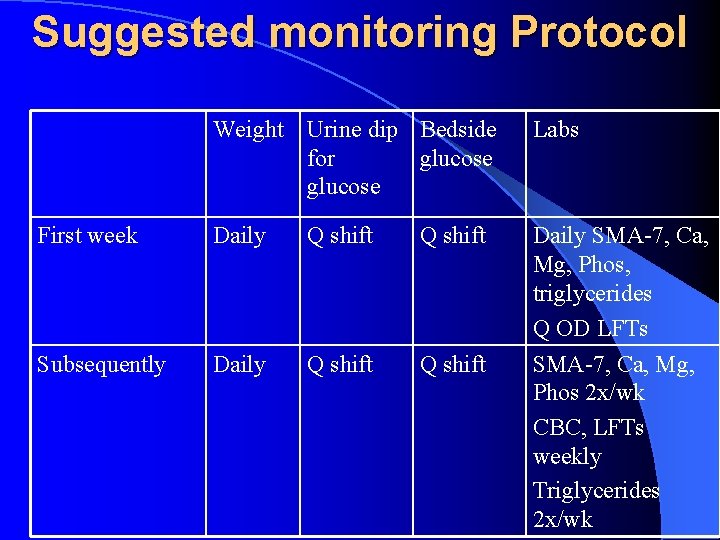
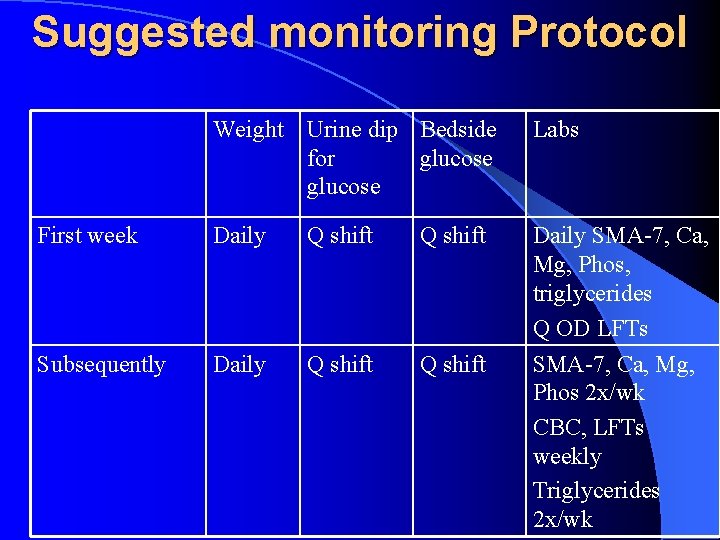
Suggested monitoring Protocol Weight Urine dip Bedside for glucose Labs First week Daily Q shift Subsequently Daily Q shift Daily SMA-7, Ca, Mg, Phos, triglycerides Q OD LFTs SMA-7, Ca, Mg, Phos 2 x/wk CBC, LFTs weekly Triglycerides 2 x/wk
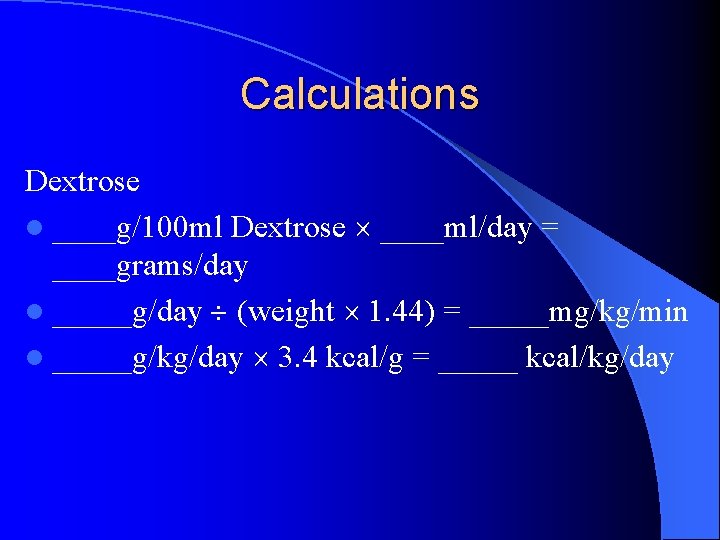
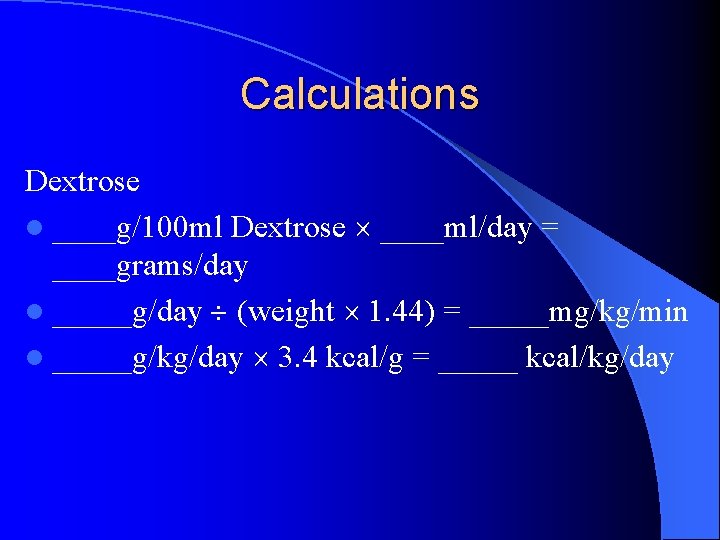
Calculations Dextrose l ____g/100 ml Dextrose ____ml/day = ____grams/day l _____g/day (weight 1. 44) = _____mg/kg/min l _____g/kg/day 3. 4 kcal/g = _____ kcal/kg/day
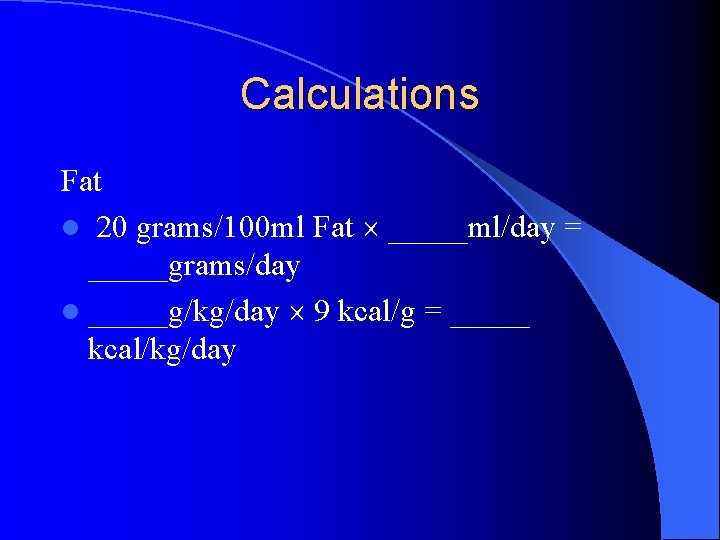
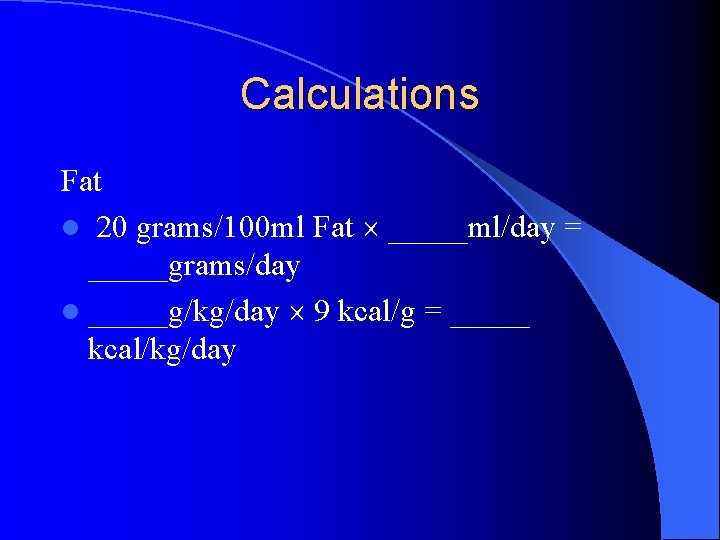
Calculations Fat l 20 grams/100 ml Fat _____ml/day = _____grams/day l _____g/kg/day 9 kcal/g = _____ kcal/kg/day
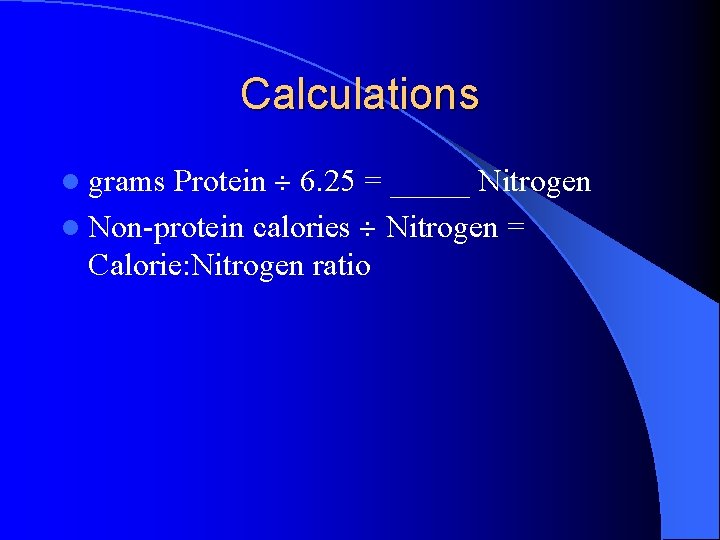
Calculations Protein 6. 25 = _____ Nitrogen l Non-protein calories Nitrogen = Calorie: Nitrogen ratio l grams
DANGERS OF OVERFEEDING l Secretory diarrhea (with EN) l Hyperglycemia, glycosuria, dehydration, lipogenesis, fatty liver, liver dysfunction l Electrolyte abnormalities: PO 4 , K, Mg l Volume overload, CHF l CO 2 production- ventilatory demand l O 2 consumption l Increased mortality (in adult studies)

MONITORING Prevent Overfeeding l Carbohydrate: High RQ indicates CHO excess, stool reducing substances l Protein: Nitrogen balance l Fat: triglyceride l Visceral protein monitoring l Electrolytes, vitamin levels l Caloric requirement assessment by metabolic cart
CONCLUSIONS l Start nutrition early l Enteral route is preferred when available l Set goals for the individual patient l Dose nutrients compatible with existing metabolism l Appropriate monitoring is essential l Avoid overfeeding
QUESTION 1 l When should nutritional support be initiated in critically ill patients? – Only after extubation – After 3 days of NPO status – After 5 days of NPO status – After 7 days of NPO status – ASAP, preferrably within 24 hours of admission
QUESTION 2 l What would be the preferred mode for nutritional support in a 10 year old boy with head injury, raised ICP and aspiration pneumonia that developed after he vomited during intubation in the field. – Parenteral nutrition – Enteral nutrition – A combination of enteral and parenteral nutrition – IV fluids alone until ICP is better controlled.
QUESTION 3 l What would be the initial TPN composition for a 10 kg 18 month year old child – Glucose 10%, Protein 20 g/day, lipids 5 g/d – Glucose 10%, Protein 10 g/day, lipids 15 g/d – Glucose 15%, Protein 5 g/day, lipids 20 g/d – Glucose 12. 5%, Protein 20 g/day, lipids 10 g/d – Glucose 10%, Protein 10 g/day, lipids 10 g/d