ENLS Version 4 0 Status Epilepticus Content Karen


- Slides: 39
ENLS Version 4. 0 Status Epilepticus Content: Karen Berger, Pharm. D; Joshua N. Goldstein, MD, Ph. D; Sarah Peacock, DNP, APRN, ACNP-BC; AM Iqbal O’Meara, MD Slides: Brandon Francis, MD, MPH

Presenter: Your name Your institution Conflicts: No conflicts
Editors’ Note: Global Considerations The intent of the editors, authors, and reviewers of this ENLS topic was not to address all the variations in international practice for the different diseases. We have discussed major practice variances (e. g. , the availability of diagnostic testing, or the type of medications used) and encourage learners to use the ENLS algorithms as a framework on which any relevant local practice guidelines can be incorporated.
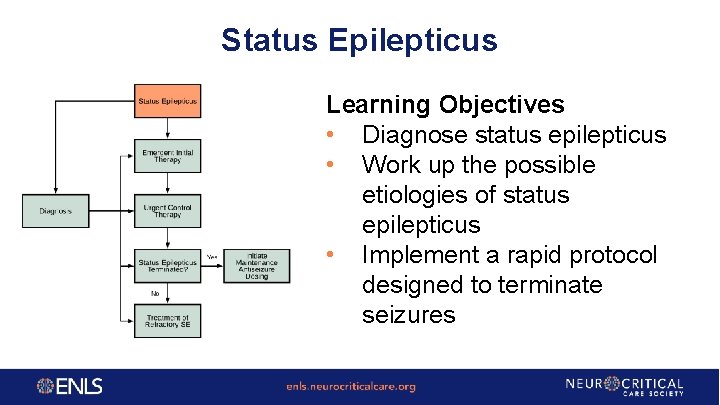
Status Epilepticus Learning Objectives • Diagnose status epilepticus • Work up the possible etiologies of status epilepticus • Implement a rapid protocol designed to terminate seizures
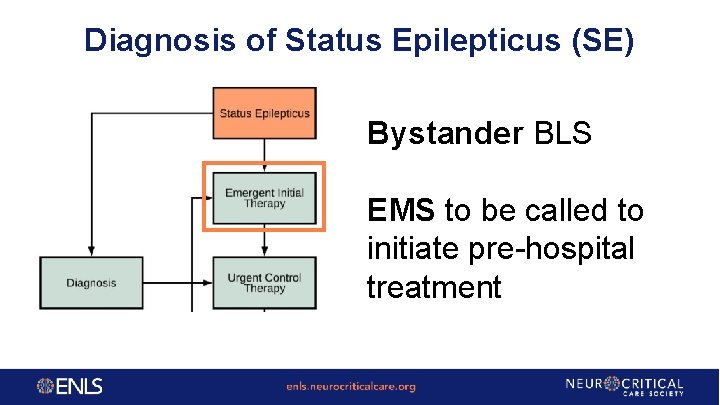
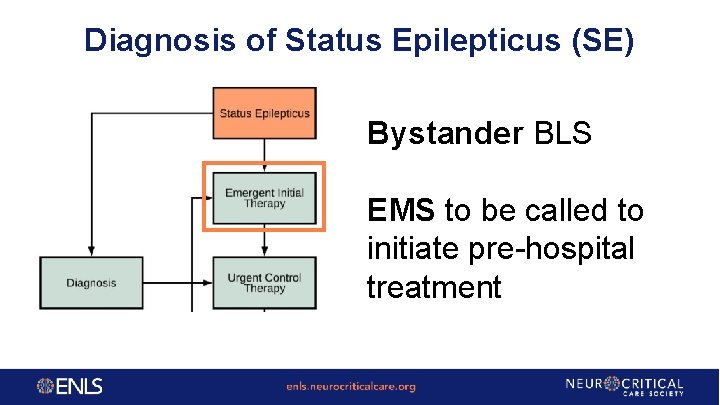
Diagnosis of Status Epilepticus (SE) Bystander BLS EMS to be called to initiate pre-hospital treatment
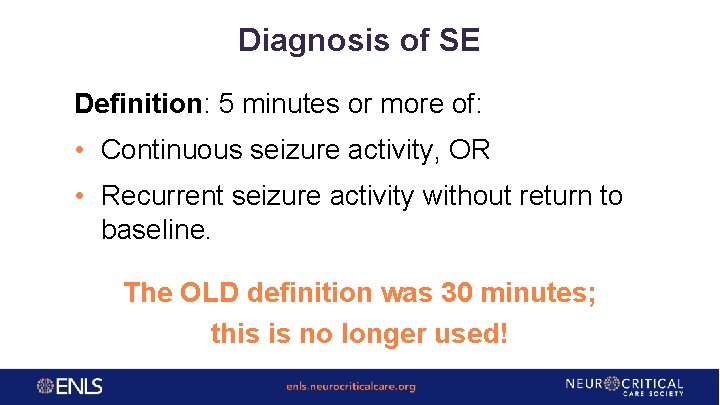
Diagnosis of SE Definition: 5 minutes or more of: • Continuous seizure activity, OR • Recurrent seizure activity without return to baseline. The OLD definition was 30 minutes; this is no longer used!
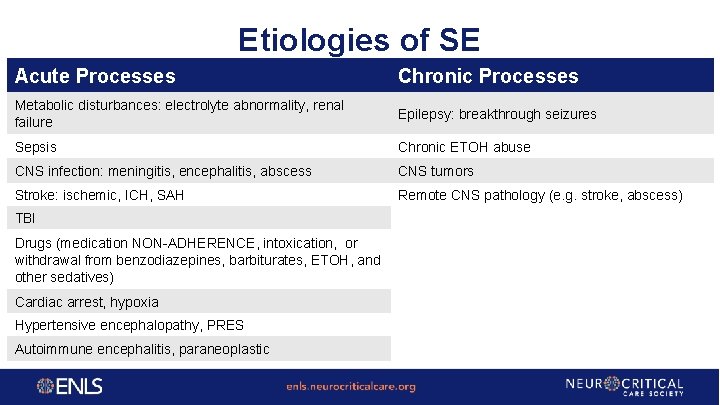
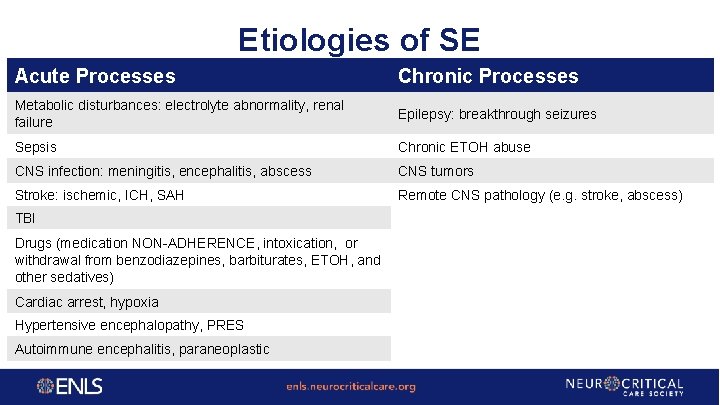
Etiologies of SE Acute Processes Chronic Processes Metabolic disturbances: electrolyte abnormality, renal failure Epilepsy: breakthrough seizures Sepsis Chronic ETOH abuse CNS infection: meningitis, encephalitis, abscess CNS tumors Stroke: ischemic, ICH, SAH Remote CNS pathology (e. g. stroke, abscess) TBI Drugs (medication NON-ADHERENCE, intoxication, or withdrawal from benzodiazepines, barbiturates, ETOH, and other sedatives) Cardiac arrest, hypoxia Hypertensive encephalopathy, PRES Autoimmune encephalitis, paraneoplastic
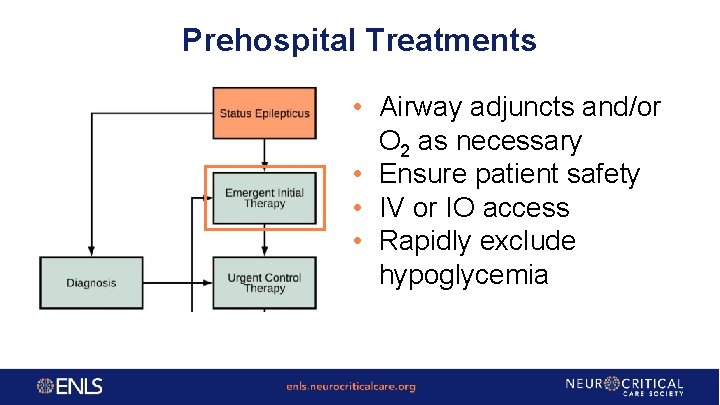
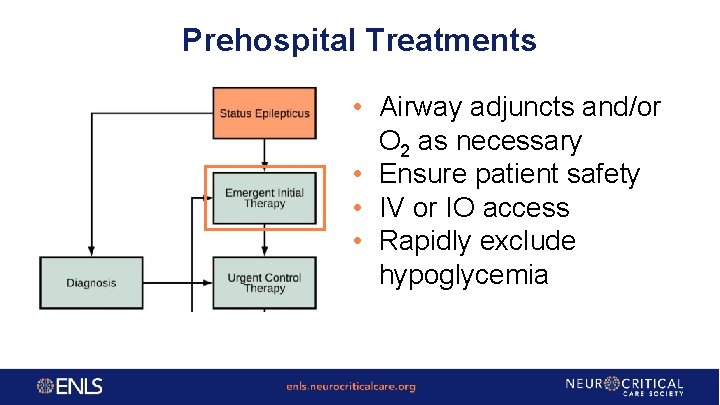
Prehospital Treatments • Airway adjuncts and/or O 2 as necessary • Ensure patient safety • IV or IO access • Rapidly exclude hypoglycemia
Case 1 • A 28 -year-old man with no known past medical history is brought by EMS to the emergency department after suffering a seizure at work. • EMS did not administer any medication in the field or en route to the hospital. • Seizure activity started approximately 22 minutes ago and continues. What is the appropriate first line pharmacologic agent to treat this patient's status epilepticus?
Case 1 A. B. C. D. E. Levetiracetam 1000 mg IV over 15 minutes Lorazepam 2 mg IVP Lorazepam 0. 1 mg/kg IVP Propofol 1 mg/kg IV push followed by infusion of 0. 5 mg/kg/hr Phenytoin 20 mg/kg IV push
Case 1 A. B. C. D. E. Levetiracetam 1000 mg IV over 15 minutes Lorazepam 2 mg IVP Lorazepam 0. 1 mg/kg IVP Propofol 1 mg/kg IV push followed by infusion of 0. 5 mg/kg/hr Phenytoin 20 mg/kg IV push The Veterans administration (VA) cooperative trial identified 0. 1 mg/kg of IV lorazepam as the preferred first line pharmacologic agent. IM midazolam may also be considered as a first line pharmacologic agent.
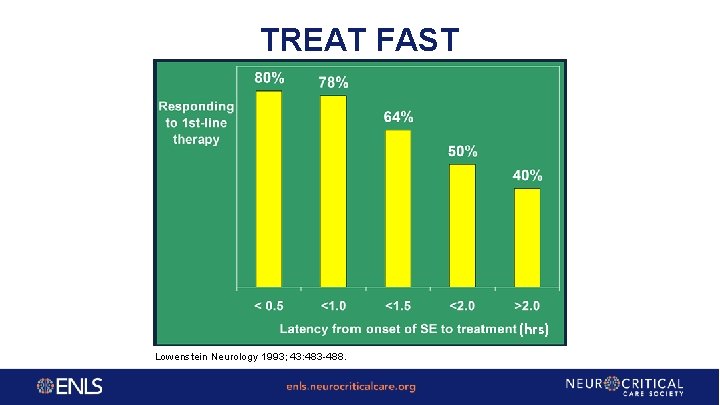
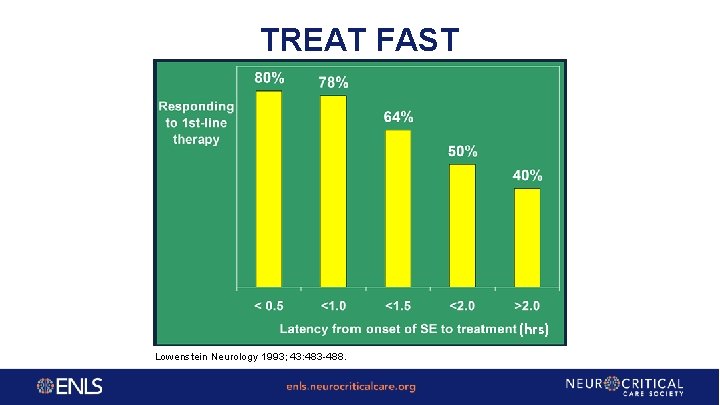
TREAT FAST (hrs) Lowenstein Neurology 1993; 43: 483 -488.
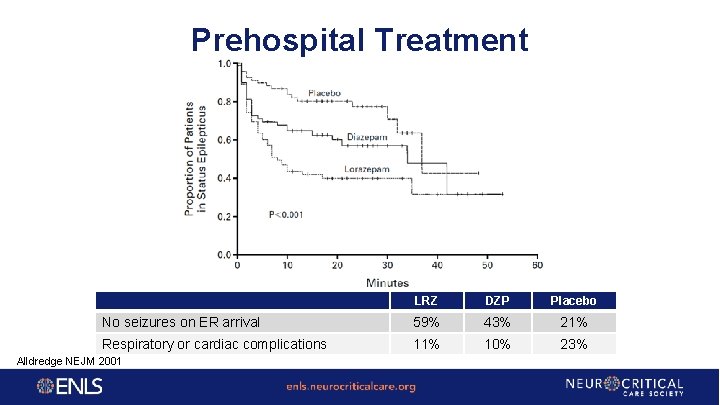
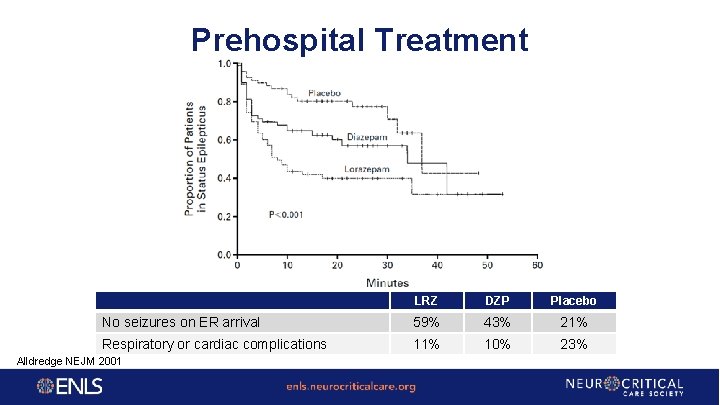
Prehospital Treatment LRZ DZP Placebo No seizures on ER arrival 59% 43% 21% Respiratory or cardiac complications 11% 10% 23% Alldredge NEJM 2001
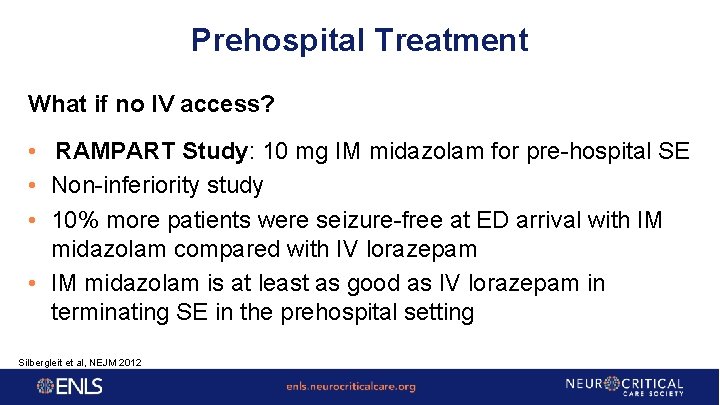
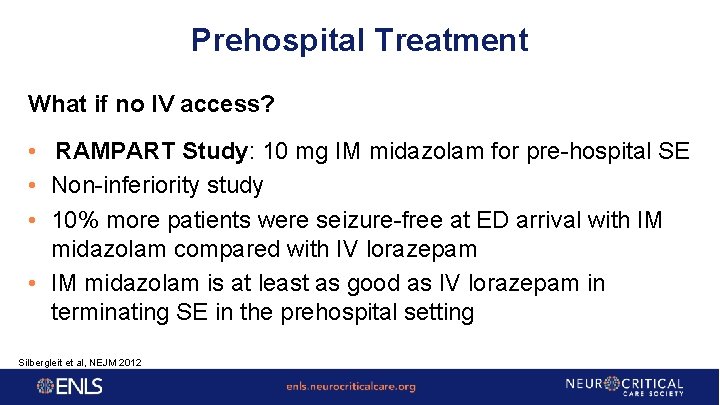
Prehospital Treatment What if no IV access? • RAMPART Study: 10 mg IM midazolam for pre-hospital SE • Non-inferiority study • 10% more patients were seizure-free at ED arrival with IM midazolam compared with IV lorazepam • IM midazolam is at least as good as IV lorazepam in terminating SE in the prehospital setting Silbergleit et al, NEJM 2012
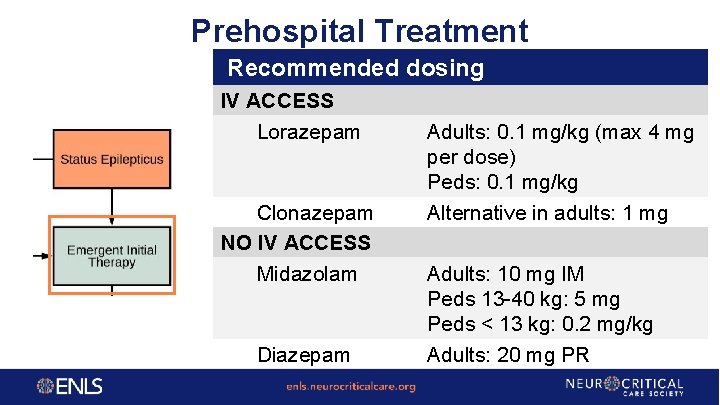
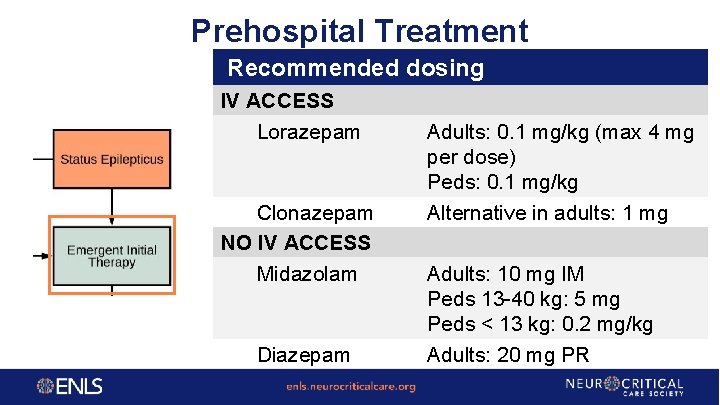
Prehospital Treatment Recommended dosing IV ACCESS Lorazepam Clonazepam NO IV ACCESS Midazolam Diazepam Adults: 0. 1 mg/kg (max 4 mg per dose) Peds: 0. 1 mg/kg Alternative in adults: 1 mg Adults: 10 mg IM Peds 13 -40 kg: 5 mg Peds < 13 kg: 0. 2 mg/kg Adults: 20 mg PR
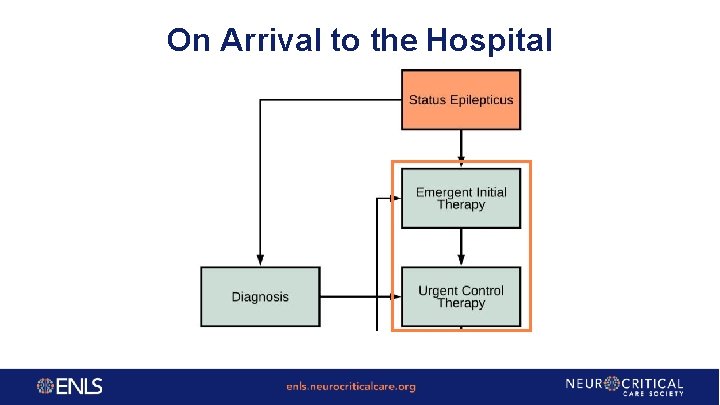
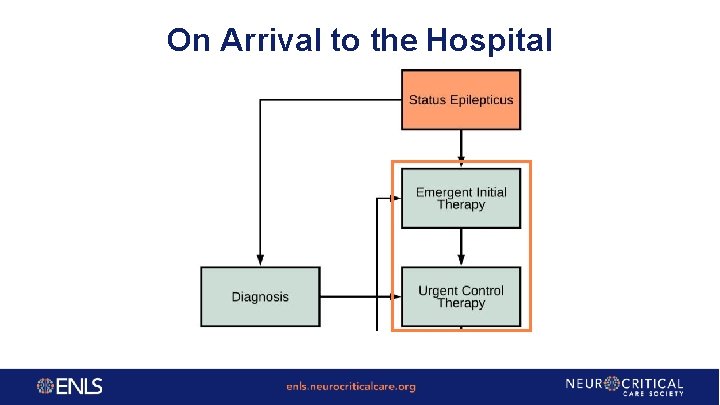
On Arrival to the Hospital ER
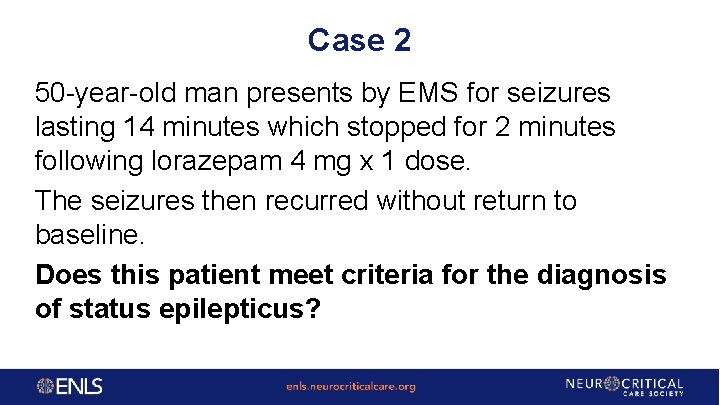
Case 2 50 -year-old man presents by EMS for seizures lasting 14 minutes which stopped for 2 minutes following lorazepam 4 mg x 1 dose. The seizures then recurred without return to baseline. Does this patient meet criteria for the diagnosis of status epilepticus?
Case 2 A. No, 30 minutes of continuous seizure activity is required before a patient is considered to be in status epilepticus B. No, the seizure stopped for a short period of time indicating recurrent seizures but not status epilepticus C. No, the diagnosis of status epilepticus cannot be reached without confirmatory EEG testing D. Yes, the patient's seizure activity lasted longer than 5 minutes without return to neurologic baseline E. Yes, the patient has a history of seizure activity and is therefore in status epilepticus
Case 2 A. No, 30 minutes of continuous seizure activity is required before a patient is considered to be in status epilepticus B. No, the seizure stopped for a short period of time indicating recurrent seizures but not status epilepticus C. No, the diagnosis of status epilepticus cannot be reached without confirmatory EEG testing D. Yes, the patient's seizure activity lasted longer than 5 minutes without return to neurologic baseline E. Yes, the patient has a history of seizure activity and is therefore in status epilepticus
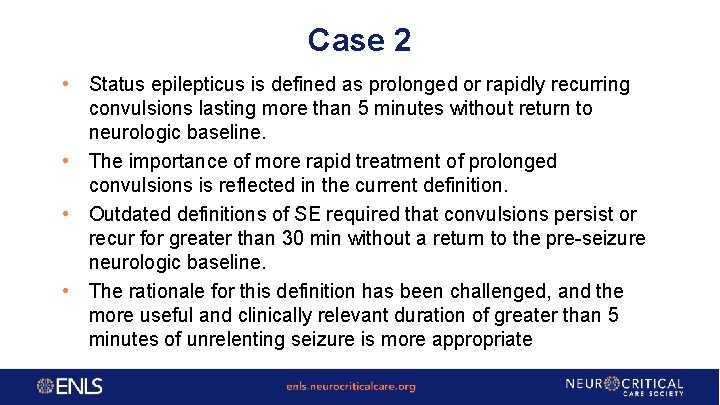
Case 2 • Status epilepticus is defined as prolonged or rapidly recurring convulsions lasting more than 5 minutes without return to neurologic baseline. • The importance of more rapid treatment of prolonged convulsions is reflected in the current definition. • Outdated definitions of SE required that convulsions persist or recur for greater than 30 min without a return to the pre-seizure neurologic baseline. • The rationale for this definition has been challenged, and the more useful and clinically relevant duration of greater than 5 minutes of unrelenting seizure is more appropriate
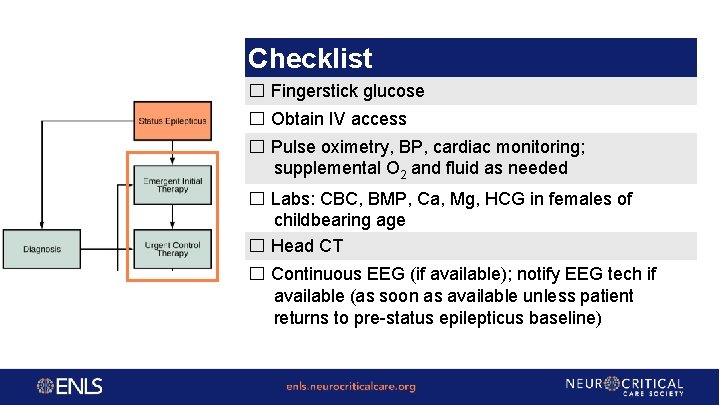
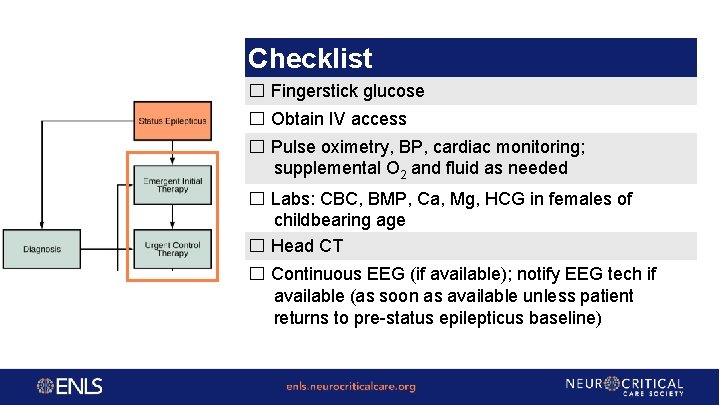
Checklist ☐ Fingerstick glucose ☐ Obtain IV access ☐ Pulse oximetry, BP, cardiac monitoring; supplemental O 2 and fluid as needed ☐ Labs: CBC, BMP, Ca, Mg, HCG in females of childbearing age ☐ Head CT ☐ Continuous EEG (if available); notify EEG tech if available (as soon as available unless patient returns to pre-status epilepticus baseline)
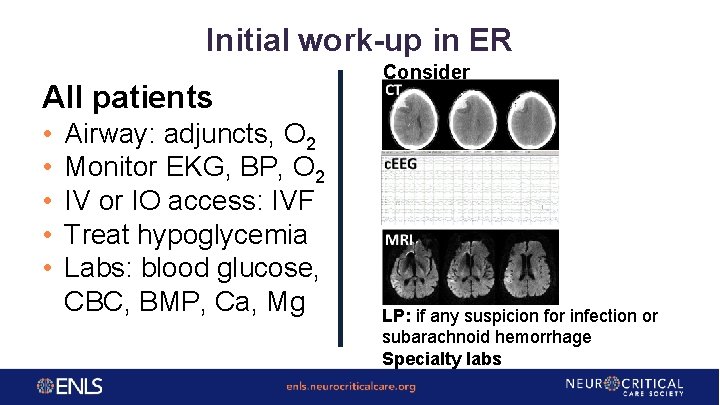
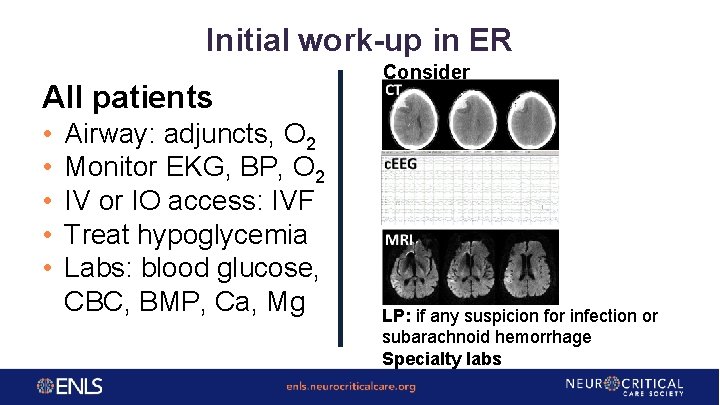
Initial work-up in ER All patients • • • CT • • Airway: adjuncts, O 2 Monitor EKG, BP, O 2 IV or IO access: IVF Treat hypoglycemia Labs: blood glucose, CBC, BMP, Ca, Mg Consider CT CT MRI LP: if any suspicion for infection or subarachnoid hemorrhage Specialty labs
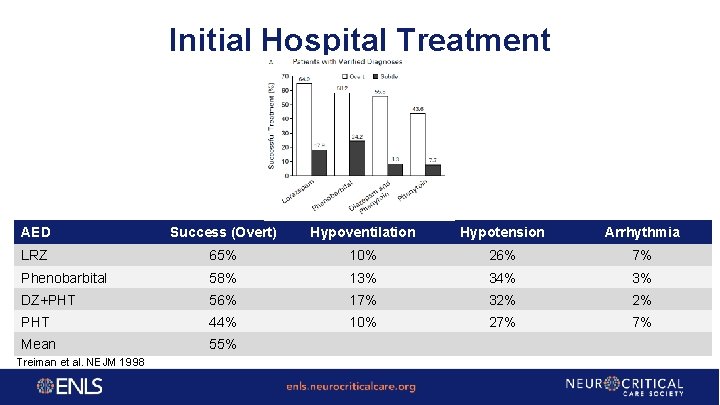
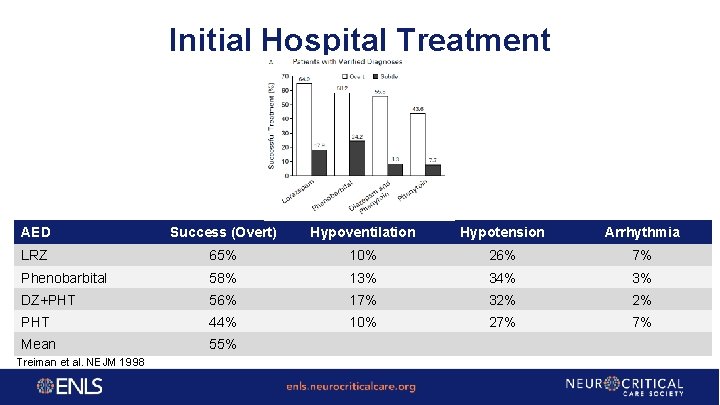
Initial Hospital Treatment AED Success (Overt) Hypoventilation Hypotension Arrhythmia LRZ 65% 10% 26% 7% Phenobarbital 58% 13% 34% 3% DZ+PHT 56% 17% 32% 2% PHT 44% 10% 27% 7% Mean 55% Treiman et al. NEJM 1998
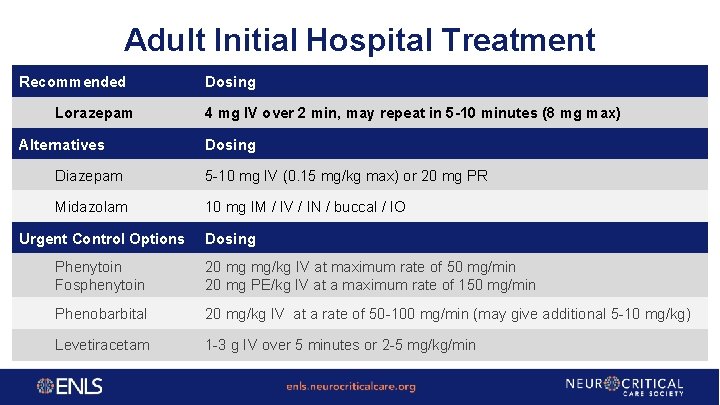
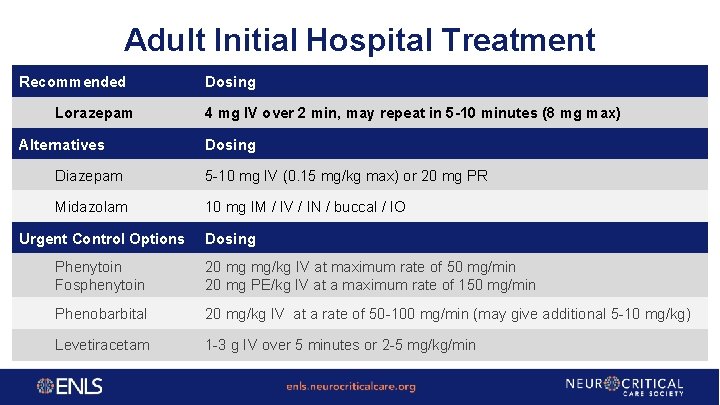
Adult Initial Hospital Treatment Recommended Lorazepam Alternatives Dosing 4 mg IV over 2 min, may repeat in 5 -10 minutes (8 mg max) Dosing Diazepam 5 -10 mg IV (0. 15 mg/kg max) or 20 mg PR Midazolam 10 mg IM / IV / IN / buccal / IO Urgent Control Options Dosing Phenytoin Fosphenytoin 20 mg mg/kg IV at maximum rate of 50 mg/min 20 mg PE/kg IV at a maximum rate of 150 mg/min Phenobarbital 20 mg/kg IV at a rate of 50 -100 mg/min (may give additional 5 -10 mg/kg) Levetiracetam 1 -3 g IV over 5 minutes or 2 -5 mg/kg/min
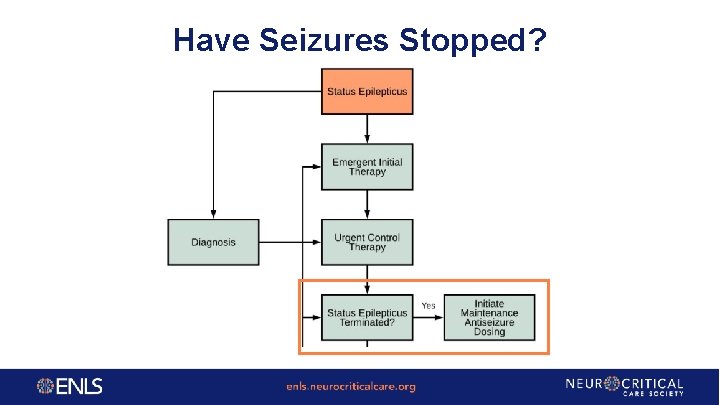
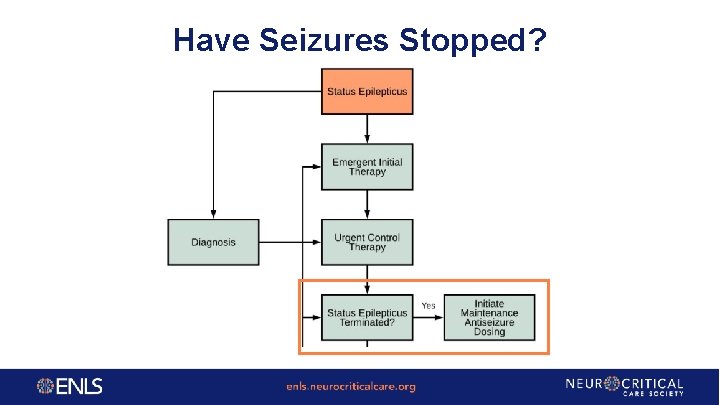
Have Seizures Stopped?
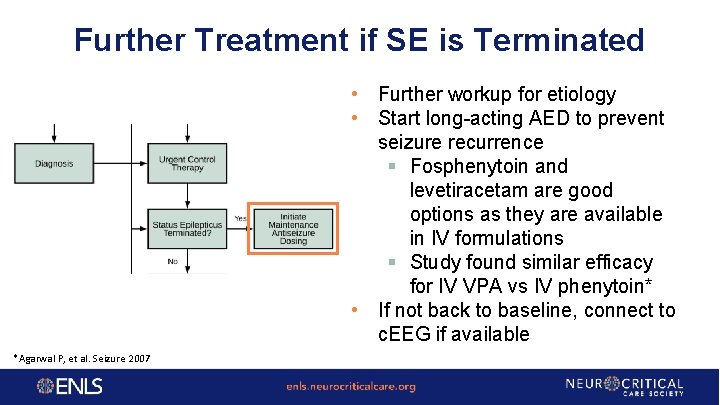
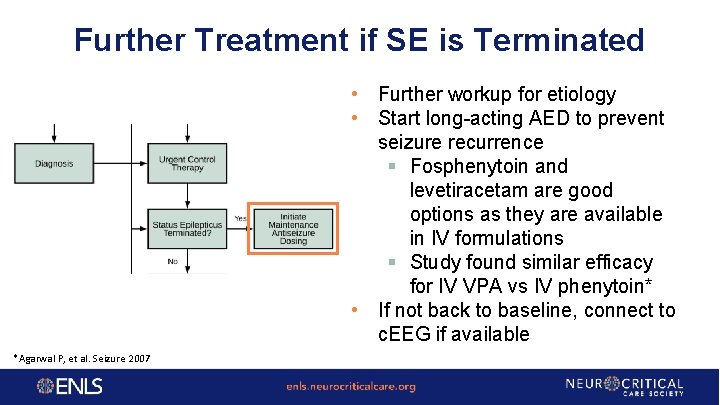
Further Treatment if SE is Terminated • Further workup for etiology • Start long-acting AED to prevent seizure recurrence § Fosphenytoin and levetiracetam are good options as they are available in IV formulations § Study found similar efficacy for IV VPA vs IV phenytoin* • If not back to baseline, connect to c. EEG if available *Agarwal P, et al. Seizure 2007
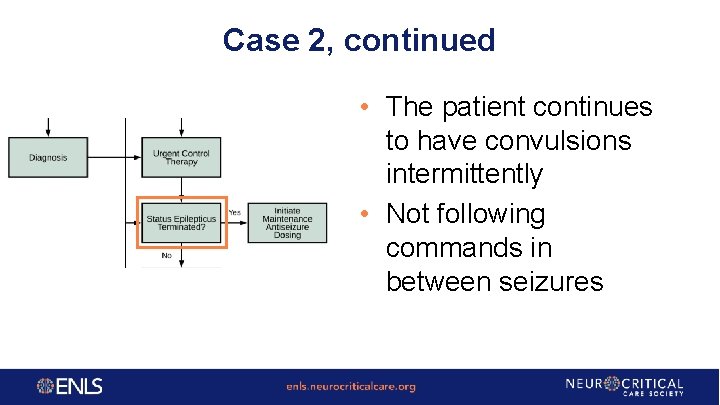
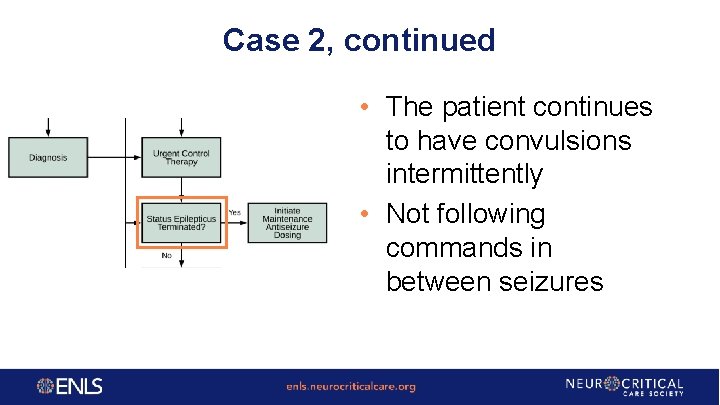
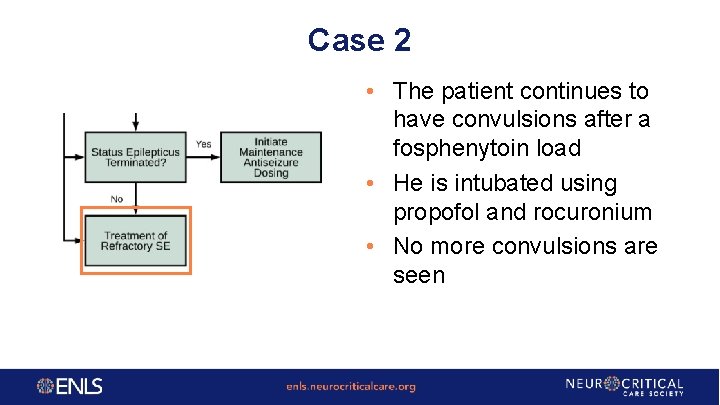
Case 2, continued • The patient continues to have convulsions intermittently • Not following commands in between seizures
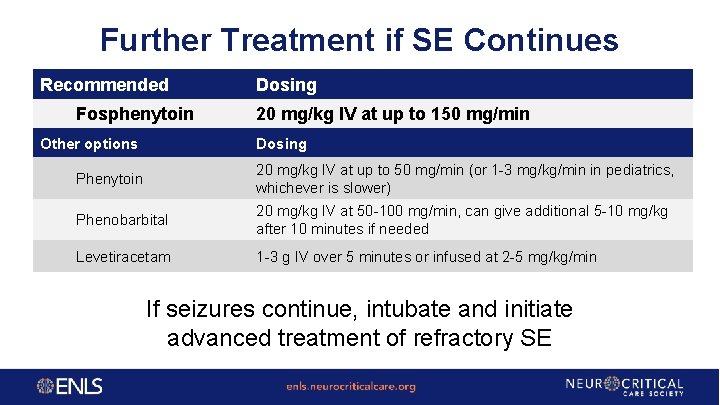
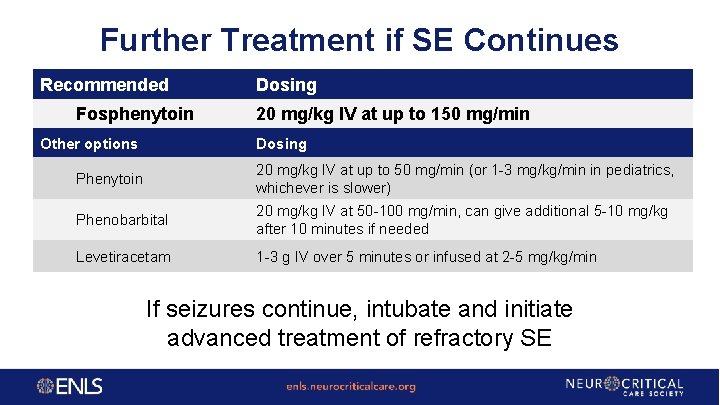
Further Treatment if SE Continues Recommended Fosphenytoin Other options Dosing 20 mg/kg IV at up to 150 mg/min Dosing Phenytoin 20 mg/kg IV at up to 50 mg/min (or 1 -3 mg/kg/min in pediatrics, whichever is slower) Phenobarbital 20 mg/kg IV at 50 -100 mg/min, can give additional 5 -10 mg/kg after 10 minutes if needed Levetiracetam 1 -3 g IV over 5 minutes or infused at 2 -5 mg/kg/min If seizures continue, intubate and initiate advanced treatment of refractory SE
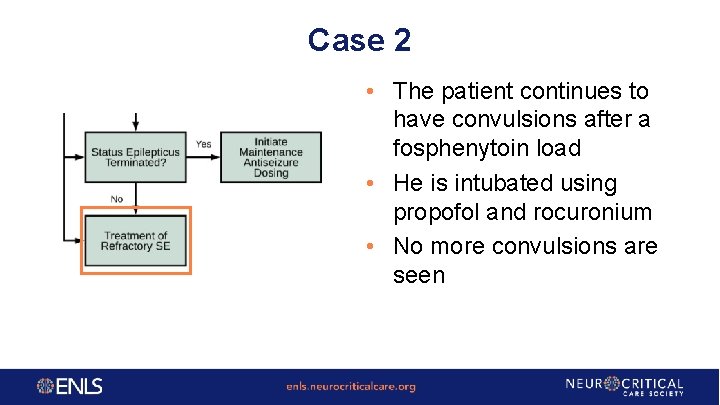
Case 2 • The patient continues to have convulsions after a fosphenytoin load • He is intubated using propofol and rocuronium • No more convulsions are seen
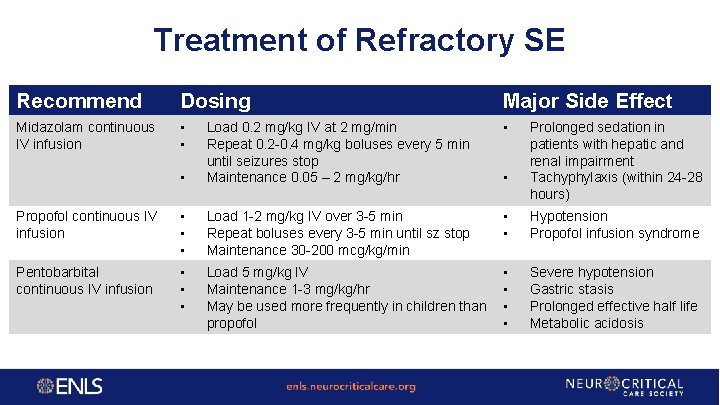
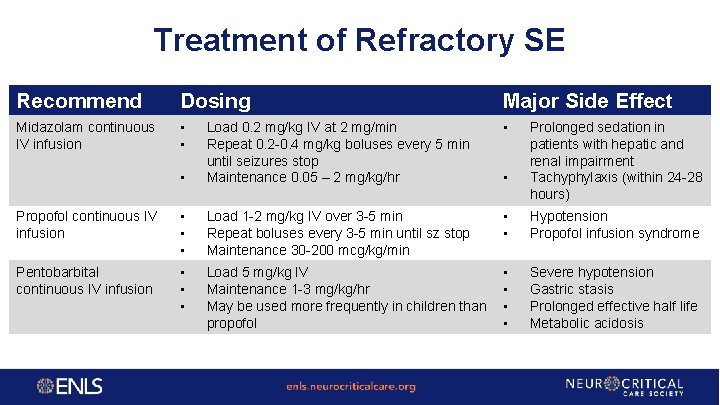
Treatment of Refractory SE Recommend Dosing Major Side Effect Midazolam continuous IV infusion • • Load 0. 2 mg/kg IV at 2 mg/min Repeat 0. 2 -0. 4 mg/kg boluses every 5 min until seizures stop Maintenance 0. 05 – 2 mg/kg/hr Propofol continuous IV infusion • • • Load 1 -2 mg/kg IV over 3 -5 min Repeat boluses every 3 -5 min until sz stop Maintenance 30 -200 mcg/kg/min • • Hypotension Propofol infusion syndrome Pentobarbital continuous IV infusion • • • Load 5 mg/kg IV Maintenance 1 -3 mg/kg/hr May be used more frequently in children than propofol • • Severe hypotension Gastric stasis Prolonged effective half life Metabolic acidosis • Prolonged sedation in patients with hepatic and renal impairment Tachyphylaxis (within 24 -28 hours)
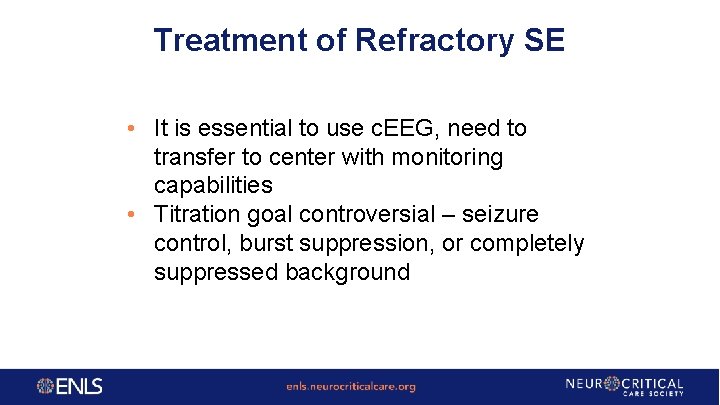
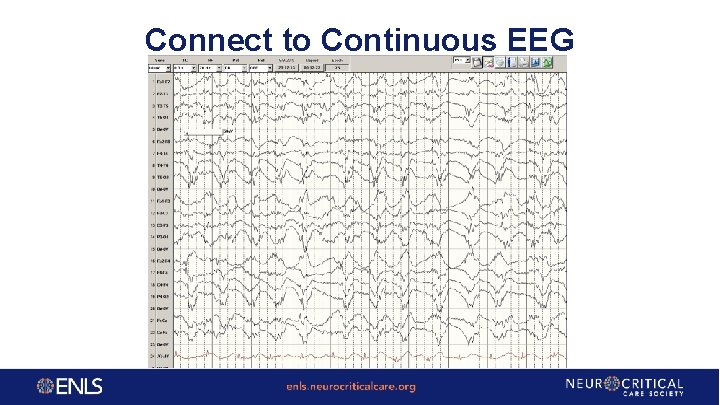
Treatment of Refractory SE • It is essential to use c. EEG, need to transfer to center with monitoring capabilities • Titration goal controversial – seizure control, burst suppression, or completely suppressed background
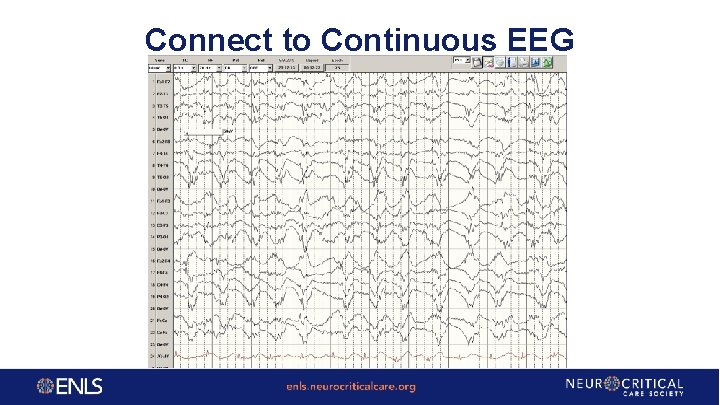
Connect to Continuous EEG
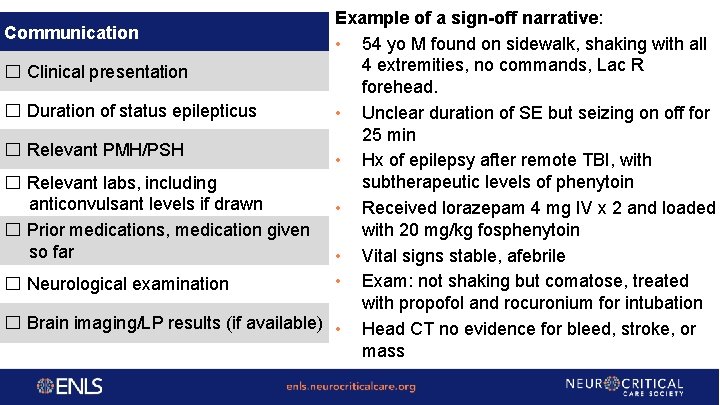
Example of a sign-off narrative: Communication • 54 yo M found on sidewalk, shaking with all 4 extremities, no commands, Lac R ☐ Clinical presentation forehead. ☐ Duration of status epilepticus • Unclear duration of SE but seizing on off for 25 min ☐ Relevant PMH/PSH • Hx of epilepsy after remote TBI, with subtherapeutic levels of phenytoin ☐ Relevant labs, including anticonvulsant levels if drawn • Received lorazepam 4 mg IV x 2 and loaded with 20 mg/kg fosphenytoin ☐ Prior medications, medication given so far • Vital signs stable, afebrile • Exam: not shaking but comatose, treated ☐ Neurological examination with propofol and rocuronium for intubation ☐ Brain imaging/LP results (if available) • Head CT no evidence for bleed, stroke, or mass
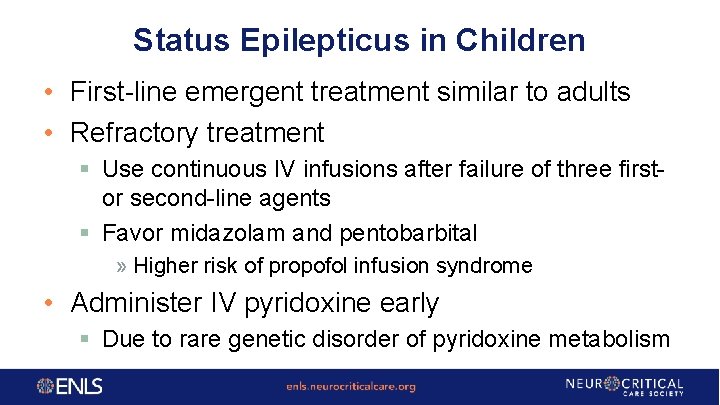
Status Epilepticus in Children • First-line emergent treatment similar to adults • Refractory treatment § Use continuous IV infusions after failure of three firstor second-line agents § Favor midazolam and pentobarbital » Higher risk of propofol infusion syndrome • Administer IV pyridoxine early § Due to rare genetic disorder of pyridoxine metabolism
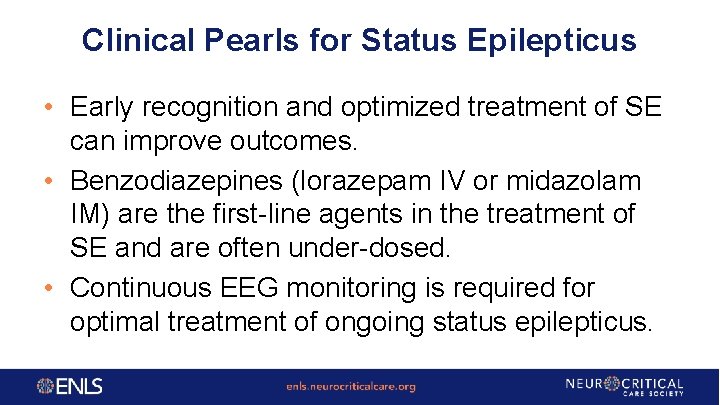
Clinical Pearls for Status Epilepticus • Early recognition and optimized treatment of SE can improve outcomes. • Benzodiazepines (lorazepam IV or midazolam IM) are the first-line agents in the treatment of SE and are often under-dosed. • Continuous EEG monitoring is required for optimal treatment of ongoing status epilepticus.
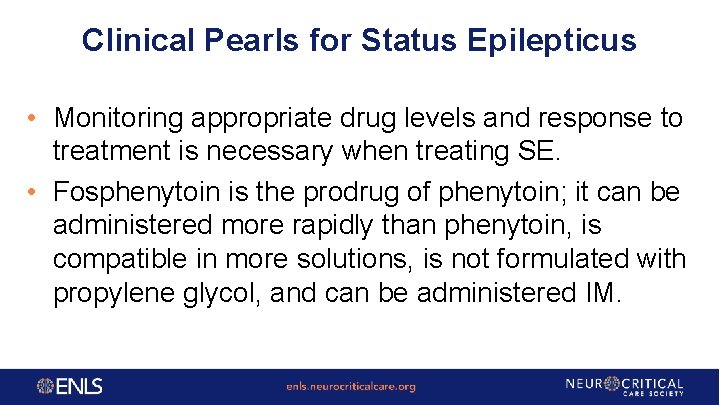
Clinical Pearls for Status Epilepticus • Monitoring appropriate drug levels and response to treatment is necessary when treating SE. • Fosphenytoin is the prodrug of phenytoin; it can be administered more rapidly than phenytoin, is compatible in more solutions, is not formulated with propylene glycol, and can be administered IM.
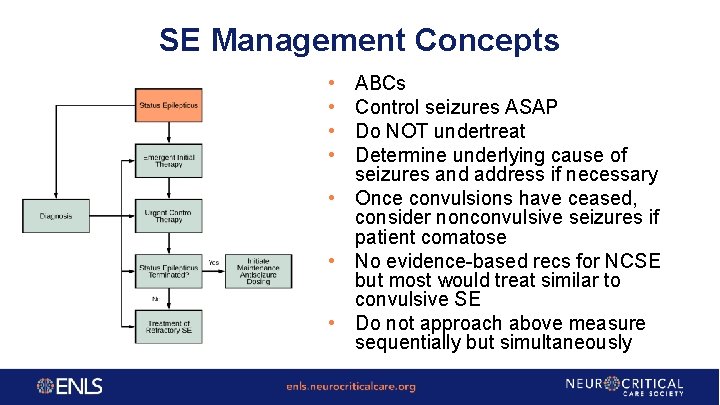
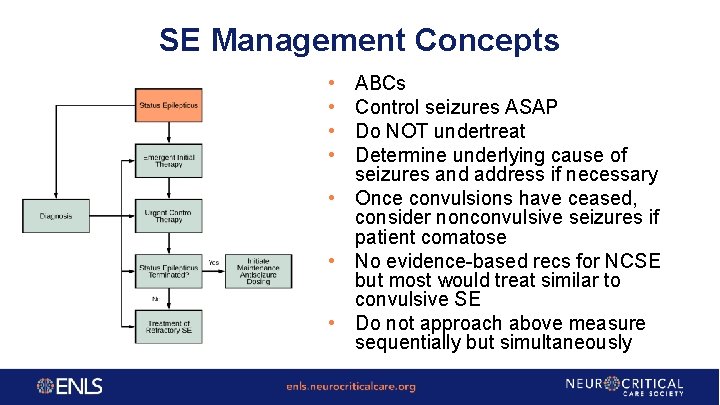
SE Management Concepts • • ABCs Control seizures ASAP Do NOT undertreat Determine underlying cause of seizures and address if necessary • Once convulsions have ceased, consider nonconvulsive seizures if patient comatose • No evidence-based recs for NCSE but most would treat similar to convulsive SE • Do not approach above measure sequentially but simultaneously

Questions?