ENLS Version 4 0 Acute Ischemic Stroke Content


- Slides: 38
ENLS Version 4. 0 Acute Ischemic Stroke Content: Archana Hinduja, MD; Noah Grose, BSN, MSN, ACNP-BC; Deborah S. Tran, DNP, RN, NE-BC, CNRN, SCRN; Aaron Raleigh, BS, EMTP Slides: Nicholas A. Morris, MD

Presenter: Your name Your institution Conflicts: No conflicts
Editors’ Note: Global Considerations The intent of the editors, authors, and reviewers of this ENLS topic was not to address all the variations in international practice for the different diseases. We have discussed major practice variances (e. g. , the availability of diagnostic testing, or the type of medications used) and encourage learners to use the ENLS algorithms as a framework on which any relevant local practice guidelines can be incorporated.
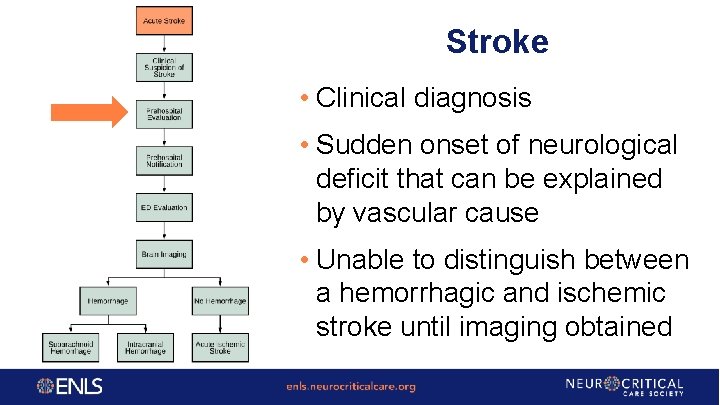
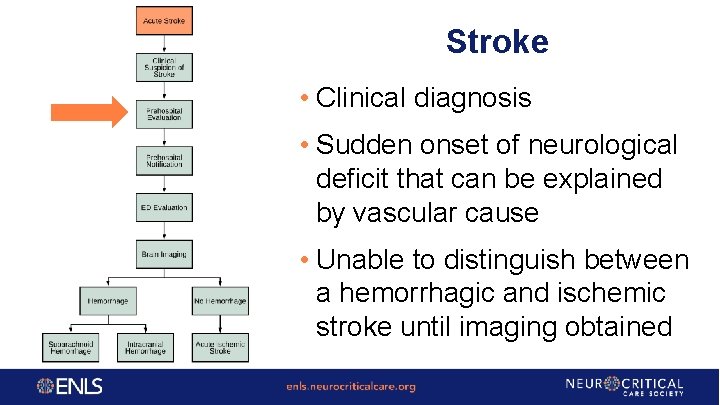
Stroke • Clinical diagnosis • Sudden onset of neurological deficit that can be explained by vascular cause • Unable to distinguish between a hemorrhagic and ischemic stroke until imaging obtained
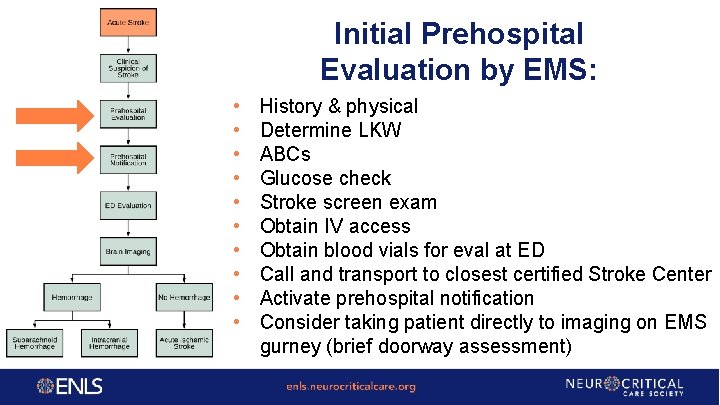
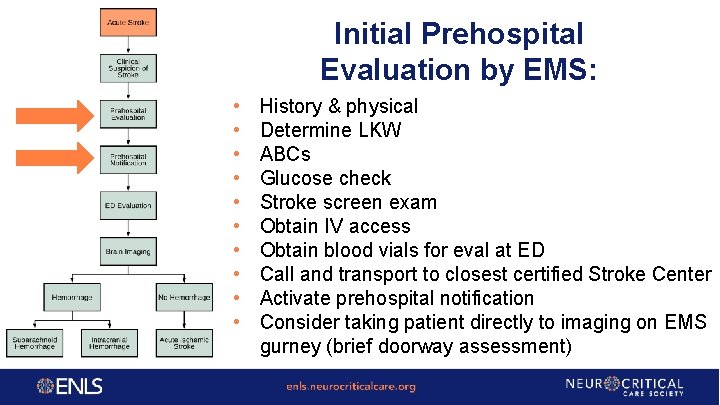
Initial Prehospital Evaluation by EMS: • • • History & physical Determine LKW ABCs Glucose check Stroke screen exam Obtain IV access Obtain blood vials for eval at ED Call and transport to closest certified Stroke Center Activate prehospital notification Consider taking patient directly to imaging on EMS gurney (brief doorway assessment)
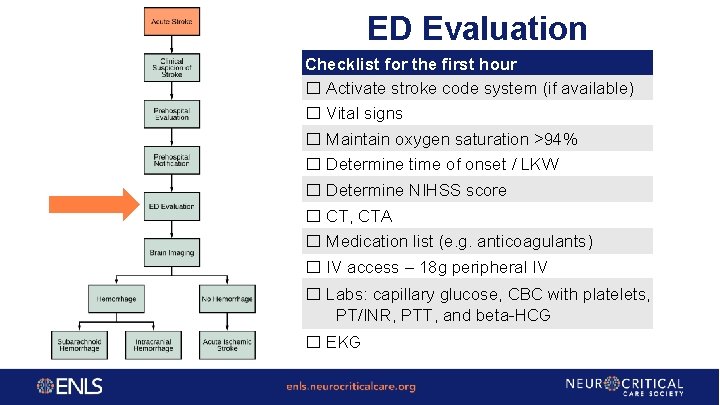
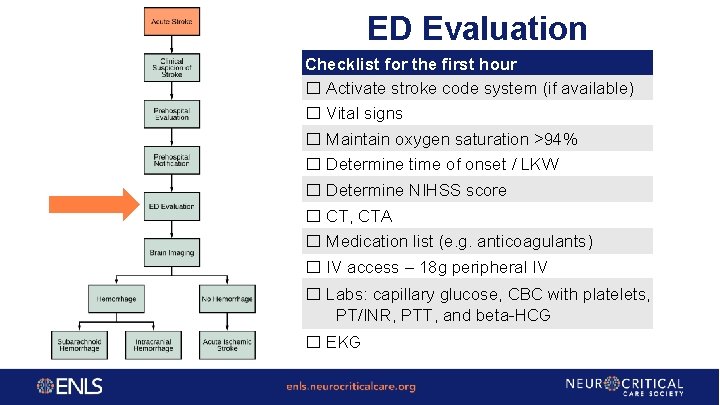
ED Evaluation Checklist for the first hour ☐ Activate stroke code system (if available) ☐ Vital signs ☐ Maintain oxygen saturation >94% ☐ Determine time of onset / LKW ☐ Determine NIHSS score ☐ CT, CTA ☐ Medication list (e. g. anticoagulants) ☐ IV access – 18 g peripheral IV ☐ Labs: capillary glucose, CBC with platelets, PT/INR, PTT, and beta-HCG ☐ EKG
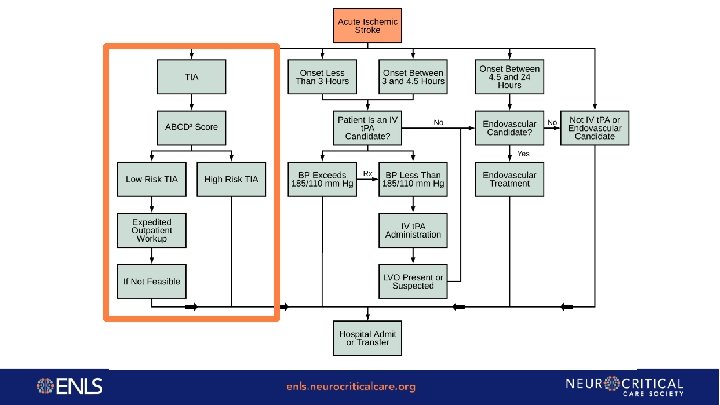
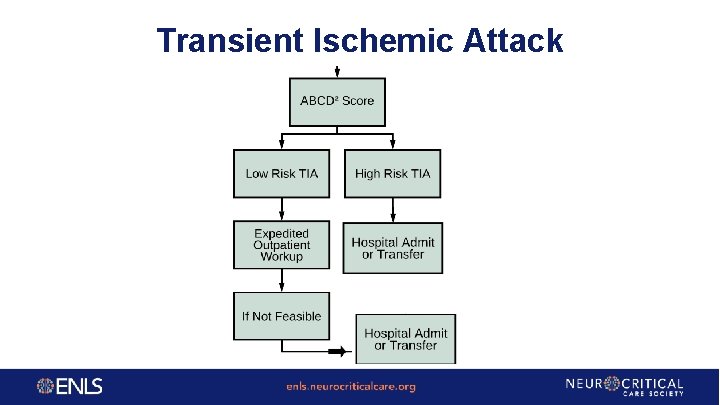
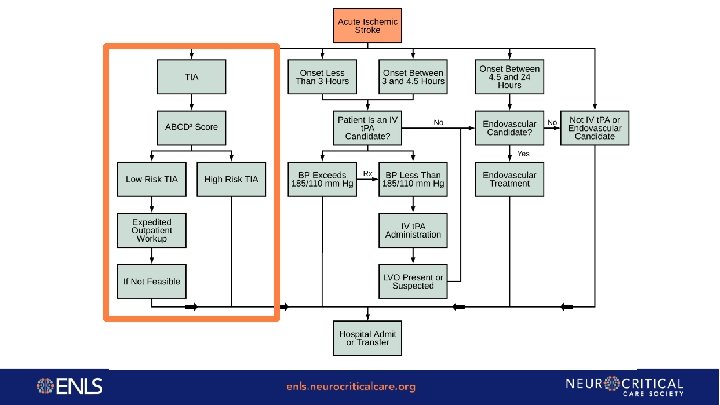
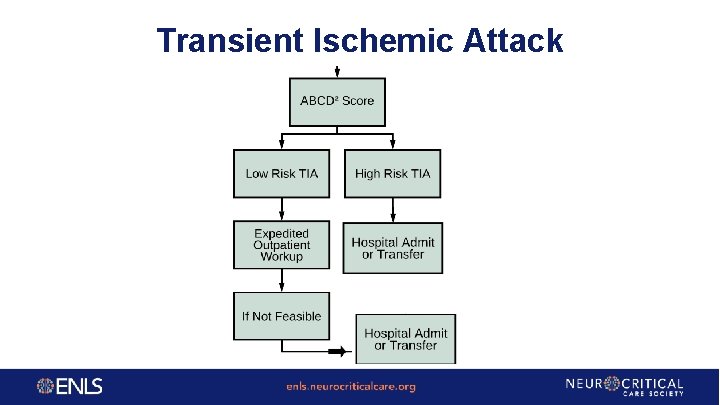
Transient Ischemic Attack
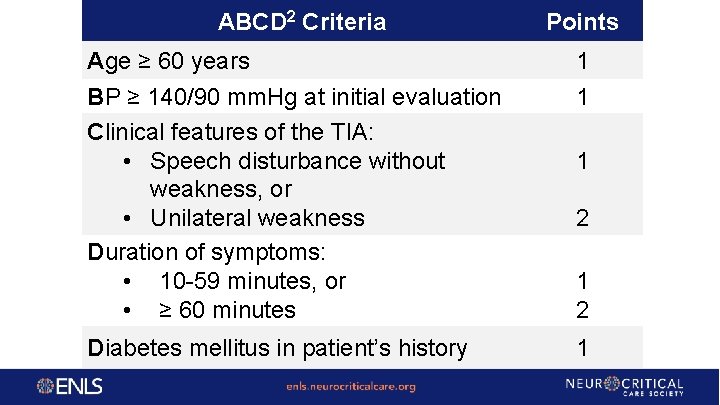
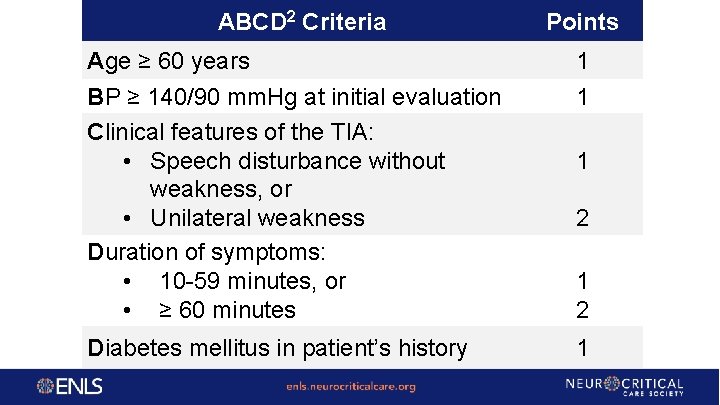
ABCD 2 Criteria Points Age ≥ 60 years 1 BP ≥ 140/90 mm. Hg at initial evaluation Clinical features of the TIA: • Speech disturbance without weakness, or • Unilateral weakness Duration of symptoms: • 10 -59 minutes, or • ≥ 60 minutes 1 Diabetes mellitus in patient’s history 1 1 2
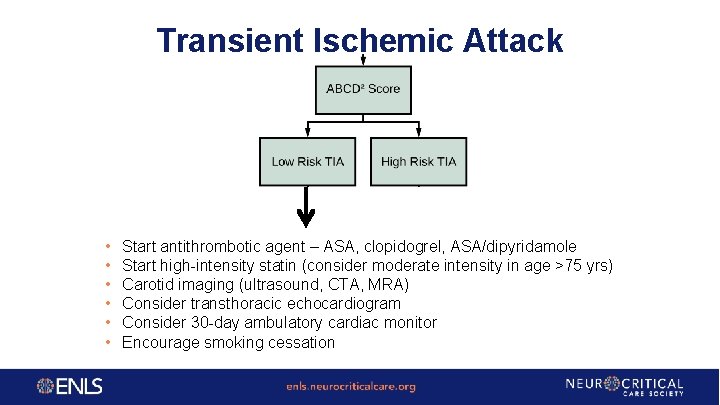
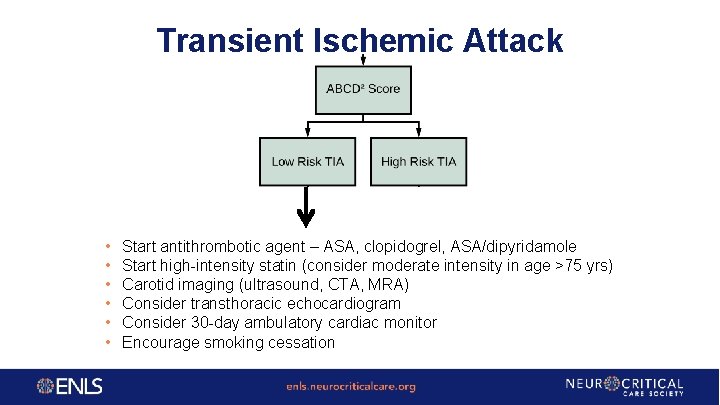
Transient Ischemic Attack • • • Start antithrombotic agent – ASA, clopidogrel, ASA/dipyridamole Start high-intensity statin (consider moderate intensity in age >75 yrs) Carotid imaging (ultrasound, CTA, MRA) Consider transthoracic echocardiogram Consider 30 -day ambulatory cardiac monitor Encourage smoking cessation
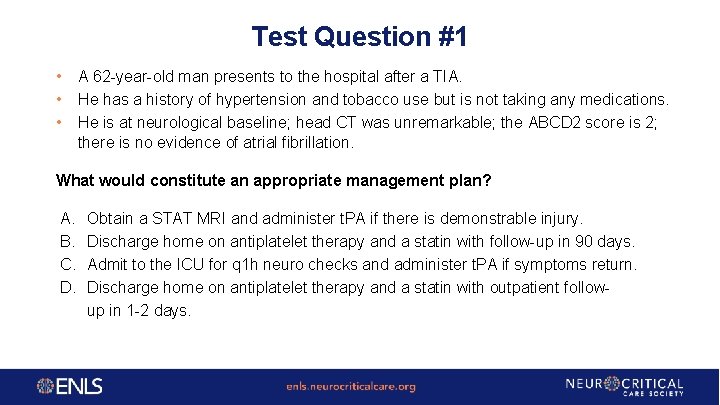
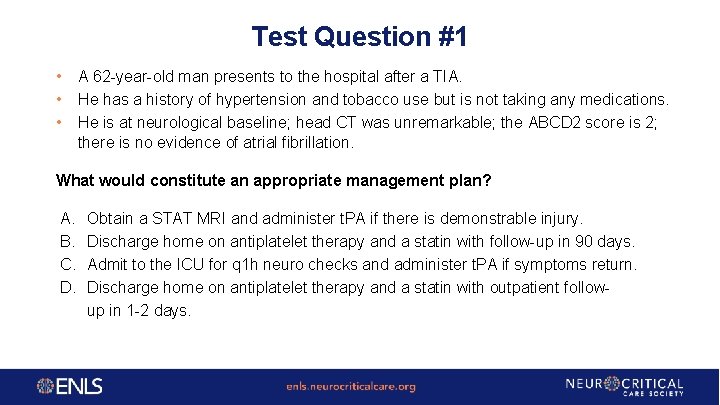
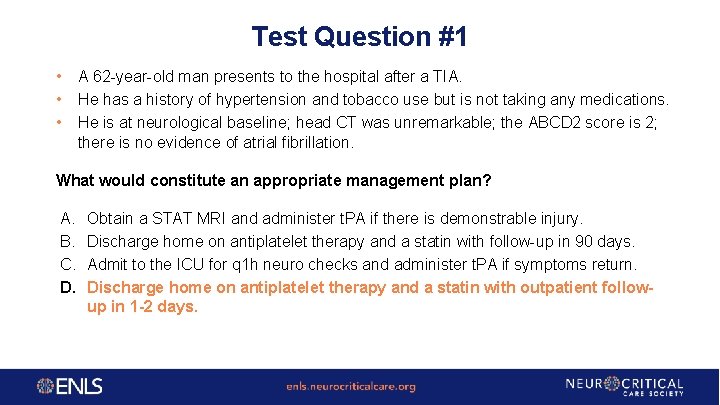
Test Question #1 • • • A 62 -year-old man presents to the hospital after a TIA. He has a history of hypertension and tobacco use but is not taking any medications. He is at neurological baseline; head CT was unremarkable; the ABCD 2 score is 2; there is no evidence of atrial fibrillation. What would constitute an appropriate management plan? A. B. C. D. Obtain a STAT MRI and administer t. PA if there is demonstrable injury. Discharge home on antiplatelet therapy and a statin with follow-up in 90 days. Admit to the ICU for q 1 h neuro checks and administer t. PA if symptoms return. Discharge home on antiplatelet therapy and a statin with outpatient followup in 1 -2 days.
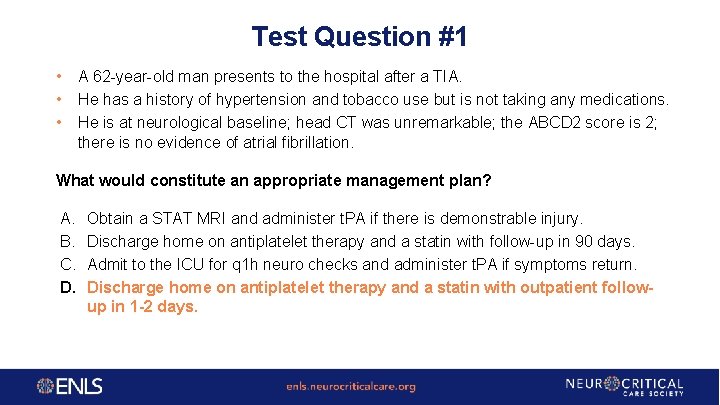
Test Question #1 • • • A 62 -year-old man presents to the hospital after a TIA. He has a history of hypertension and tobacco use but is not taking any medications. He is at neurological baseline; head CT was unremarkable; the ABCD 2 score is 2; there is no evidence of atrial fibrillation. What would constitute an appropriate management plan? A. B. C. D. Obtain a STAT MRI and administer t. PA if there is demonstrable injury. Discharge home on antiplatelet therapy and a statin with follow-up in 90 days. Admit to the ICU for q 1 h neuro checks and administer t. PA if symptoms return. Discharge home on antiplatelet therapy and a statin with outpatient followup in 1 -2 days.
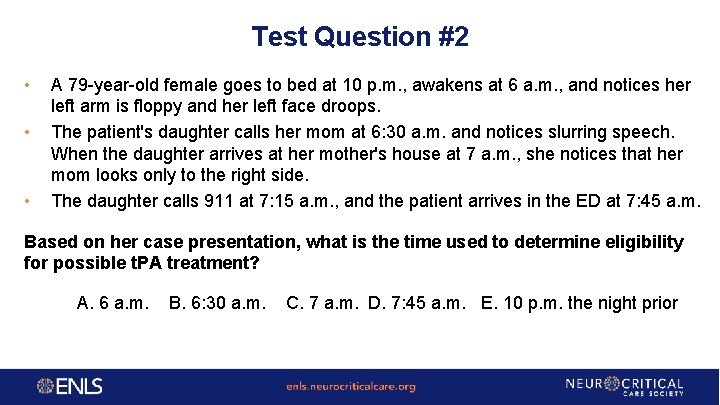
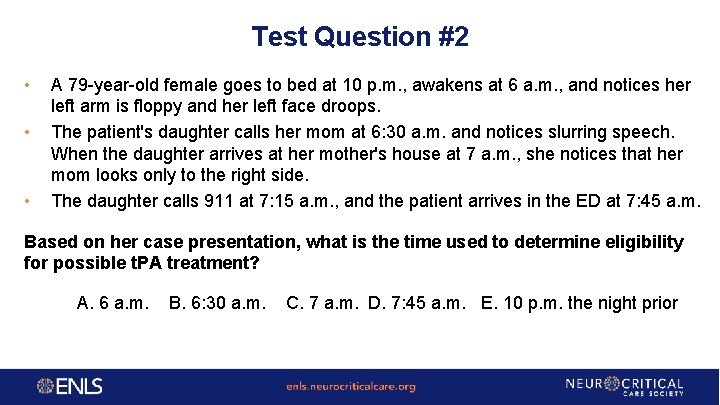
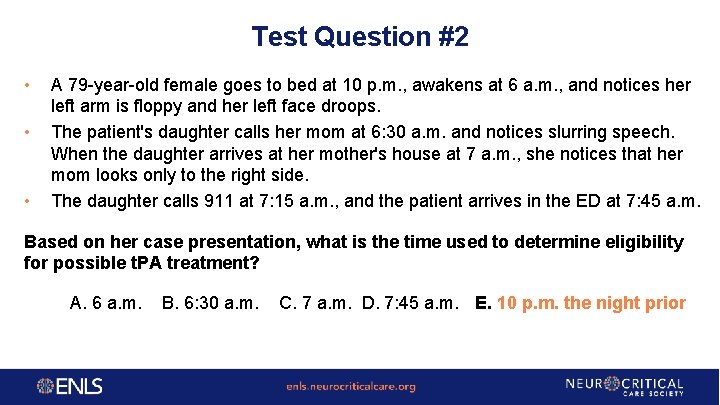
Test Question #2 • • • A 79 -year-old female goes to bed at 10 p. m. , awakens at 6 a. m. , and notices her left arm is floppy and her left face droops. The patient's daughter calls her mom at 6: 30 a. m. and notices slurring speech. When the daughter arrives at her mother's house at 7 a. m. , she notices that her mom looks only to the right side. The daughter calls 911 at 7: 15 a. m. , and the patient arrives in the ED at 7: 45 a. m. Based on her case presentation, what is the time used to determine eligibility for possible t. PA treatment? A. 6 a. m. B. 6: 30 a. m. C. 7 a. m. D. 7: 45 a. m. E. 10 p. m. the night prior
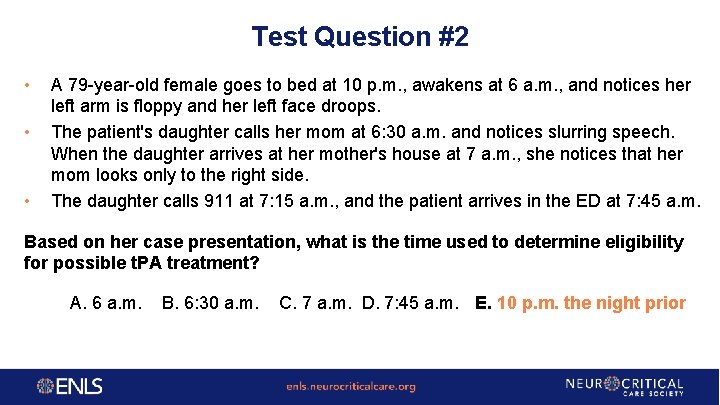
Test Question #2 • • • A 79 -year-old female goes to bed at 10 p. m. , awakens at 6 a. m. , and notices her left arm is floppy and her left face droops. The patient's daughter calls her mom at 6: 30 a. m. and notices slurring speech. When the daughter arrives at her mother's house at 7 a. m. , she notices that her mom looks only to the right side. The daughter calls 911 at 7: 15 a. m. , and the patient arrives in the ED at 7: 45 a. m. Based on her case presentation, what is the time used to determine eligibility for possible t. PA treatment? A. 6 a. m. B. 6: 30 a. m. C. 7 a. m. D. 7: 45 a. m. E. 10 p. m. the night prior
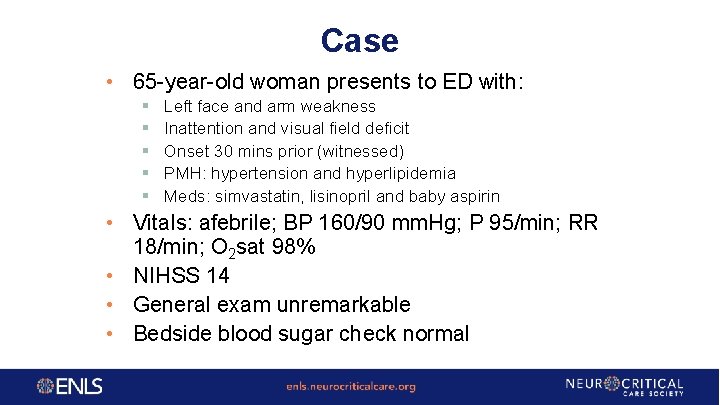
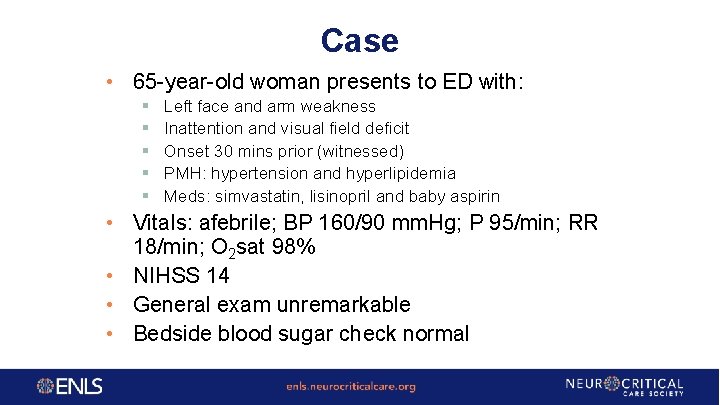
Case • 65 -year-old woman presents to ED with: § § § Left face and arm weakness Inattention and visual field deficit Onset 30 mins prior (witnessed) PMH: hypertension and hyperlipidemia Meds: simvastatin, lisinopril and baby aspirin • Vitals: afebrile; BP 160/90 mm. Hg; P 95/min; RR 18/min; O 2 sat 98% • NIHSS 14 • General exam unremarkable • Bedside blood sugar check normal
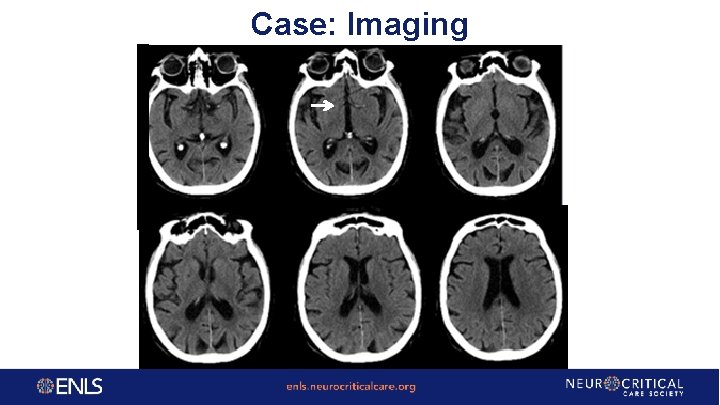
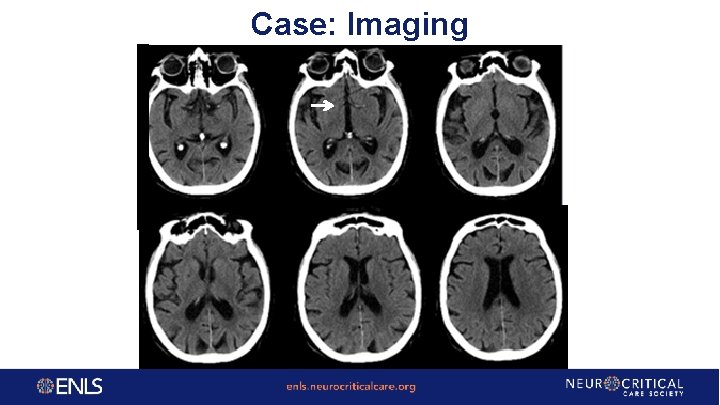
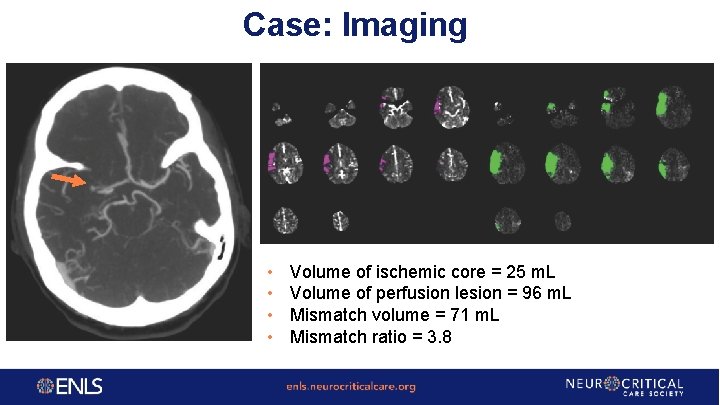
Case: Imaging
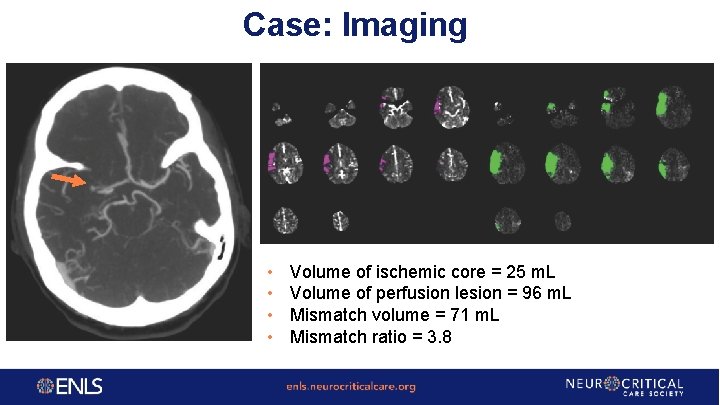
Case: Imaging • • Volume of ischemic core = 25 m. L Volume of perfusion lesion = 96 m. L Mismatch volume = 71 m. L Mismatch ratio = 3. 8
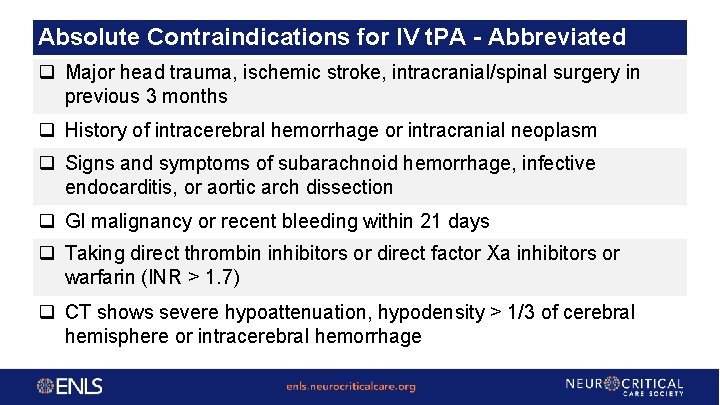
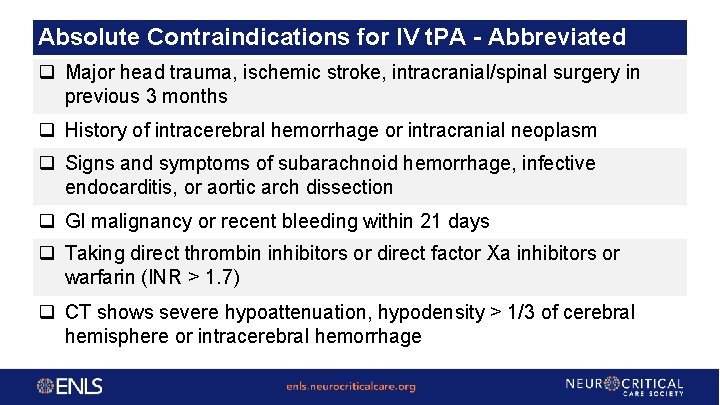
Absolute Contraindications for IV t. PA - Abbreviated q Major head trauma, ischemic stroke, intracranial/spinal surgery in previous 3 months q History of intracerebral hemorrhage or intracranial neoplasm q Signs and symptoms of subarachnoid hemorrhage, infective endocarditis, or aortic arch dissection q GI malignancy or recent bleeding within 21 days q Taking direct thrombin inhibitors or direct factor Xa inhibitors or warfarin (INR > 1. 7) q CT shows severe hypoattenuation, hypodensity > 1/3 of cerebral hemisphere or intracerebral hemorrhage
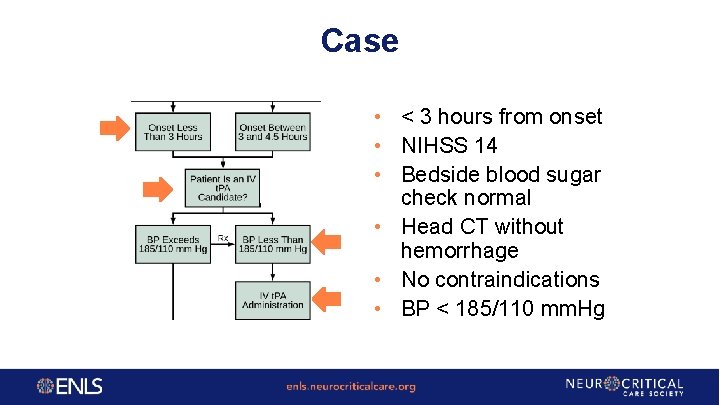
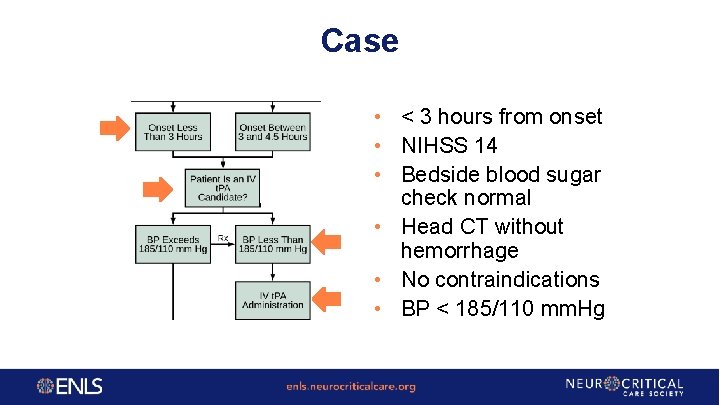
Case • < 3 hours from onset • NIHSS 14 • Bedside blood sugar check normal • Head CT without hemorrhage • No contraindications • BP < 185/110 mm. Hg
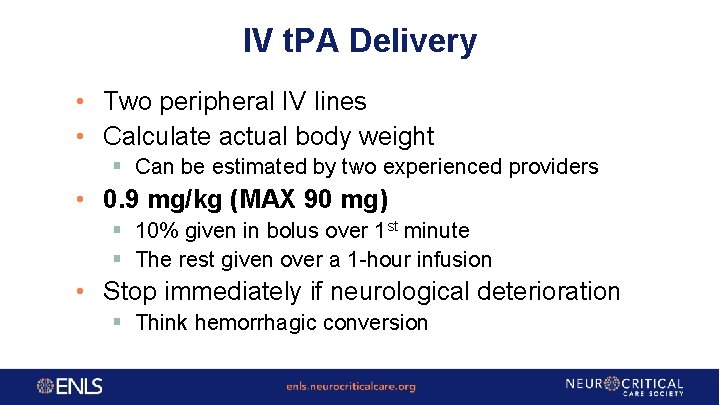
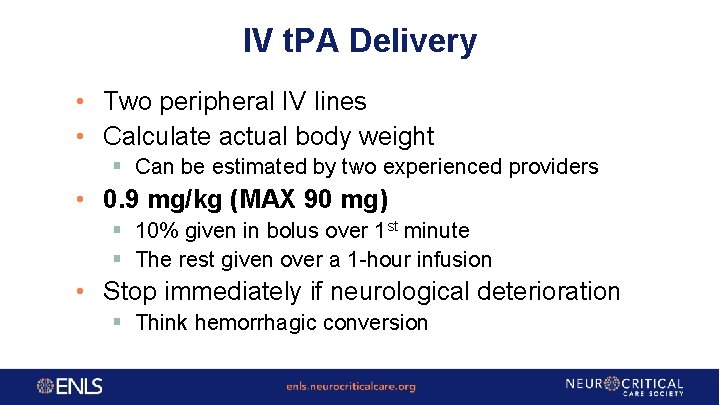
IV t. PA Delivery • Two peripheral IV lines • Calculate actual body weight § Can be estimated by two experienced providers • 0. 9 mg/kg (MAX 90 mg) § 10% given in bolus over 1 st minute § The rest given over a 1 -hour infusion • Stop immediately if neurological deterioration § Think hemorrhagic conversion
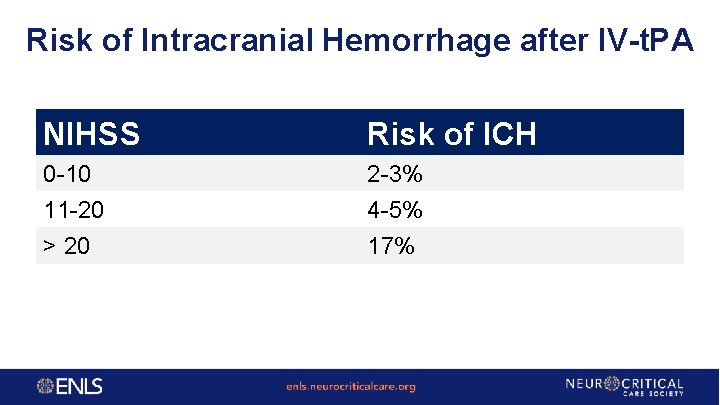
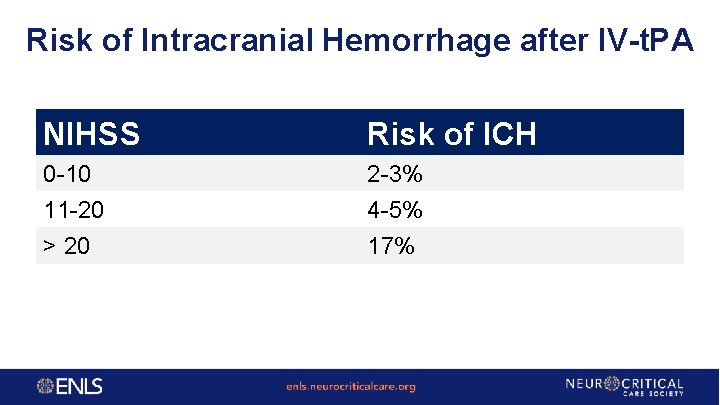
Risk of Intracranial Hemorrhage after IV-t. PA NIHSS Risk of ICH 0 -10 11 -20 > 20 2 -3% 4 -5% 17%
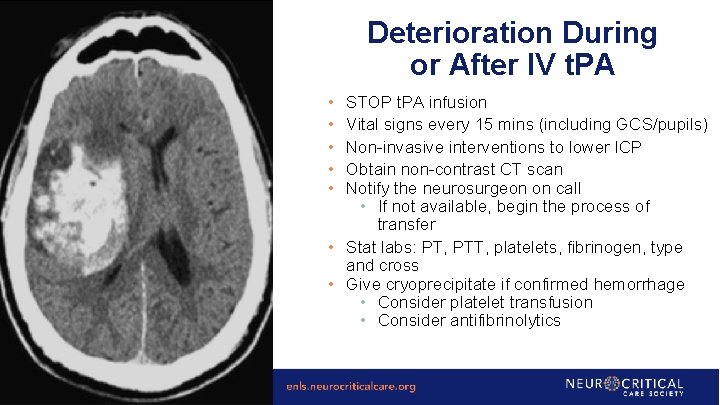
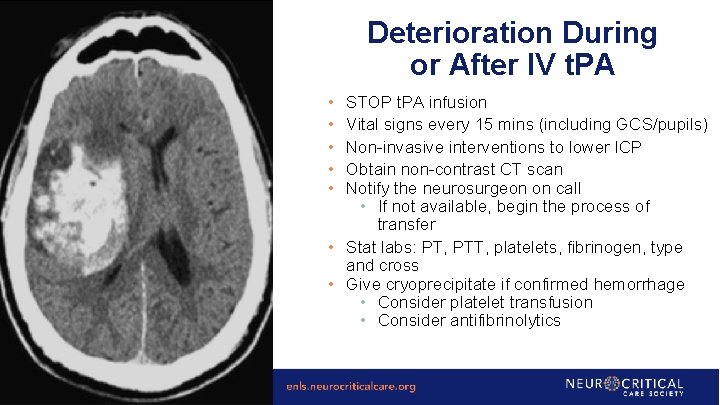
Deterioration During or After IV t. PA • • • STOP t. PA infusion Vital signs every 15 mins (including GCS/pupils) Non-invasive interventions to lower ICP Obtain non-contrast CT scan Notify the neurosurgeon on call • If not available, begin the process of transfer • Stat labs: PT, PTT, platelets, fibrinogen, type and cross • Give cryoprecipitate if confirmed hemorrhage • Consider platelet transfusion • Consider antifibrinolytics
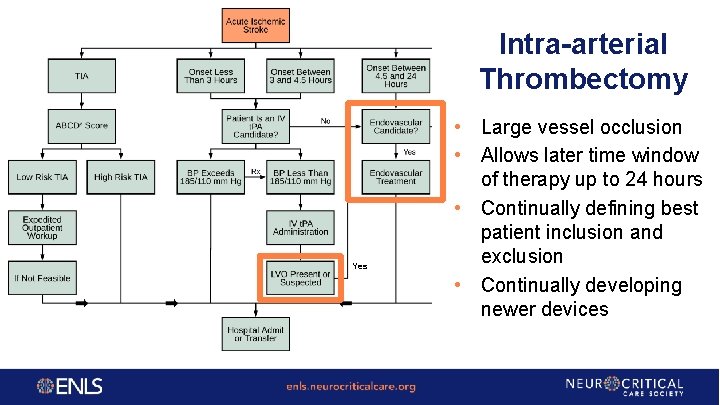
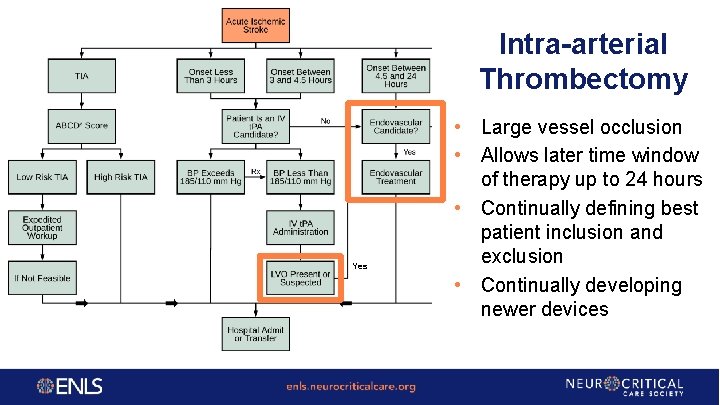
Intra-arterial Thrombectomy Yes • Large vessel occlusion • Allows later time window of therapy up to 24 hours • Continually defining best patient inclusion and exclusion • Continually developing newer devices
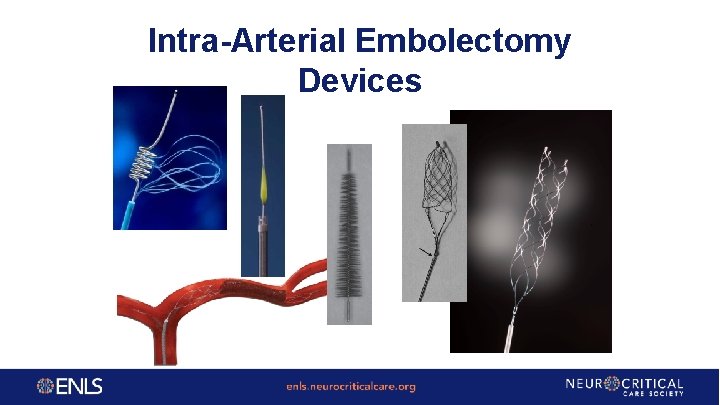
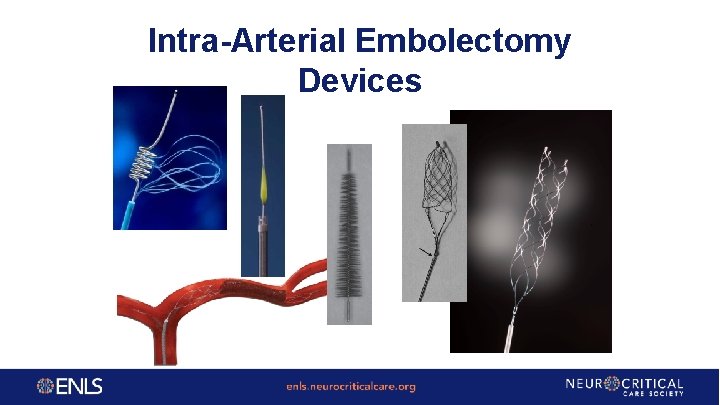
Intra-Arterial Embolectomy Devices
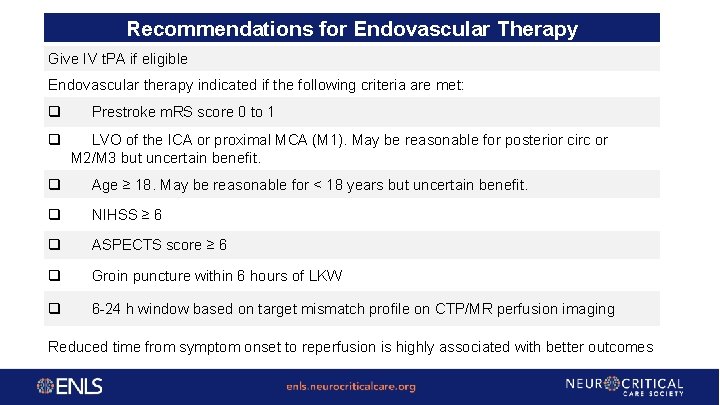
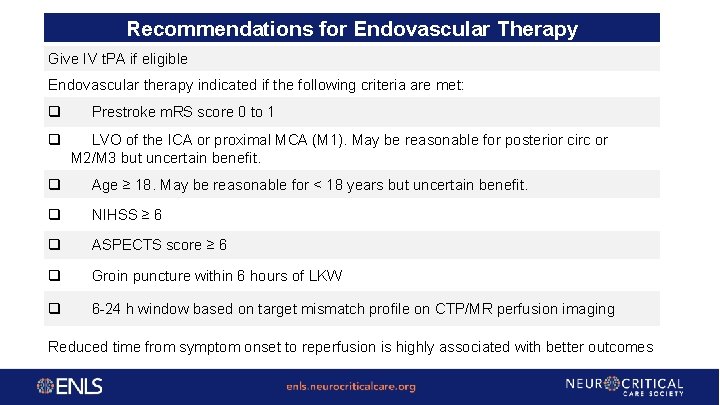
Recommendations for Endovascular Therapy Give IV t. PA if eligible Endovascular therapy indicated if the following criteria are met: q q Prestroke m. RS score 0 to 1 LVO of the ICA or proximal MCA (M 1). May be reasonable for posterior circ or M 2/M 3 but uncertain benefit. q Age ≥ 18. May be reasonable for < 18 years but uncertain benefit. q NIHSS ≥ 6 q ASPECTS score ≥ 6 q Groin puncture within 6 hours of LKW q 6 -24 h window based on target mismatch profile on CTP/MR perfusion imaging Reduced time from symptom onset to reperfusion is highly associated with better outcomes
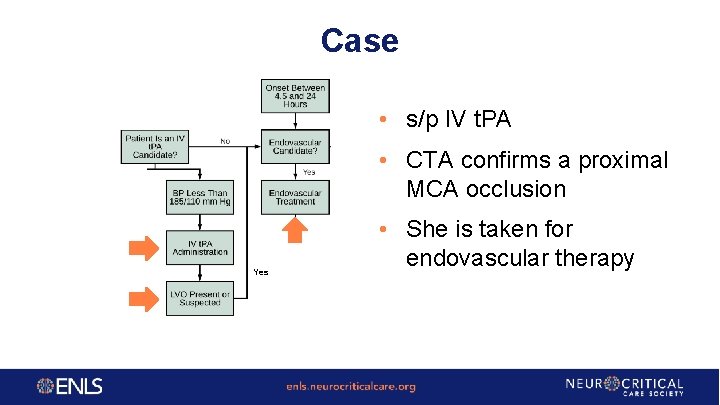
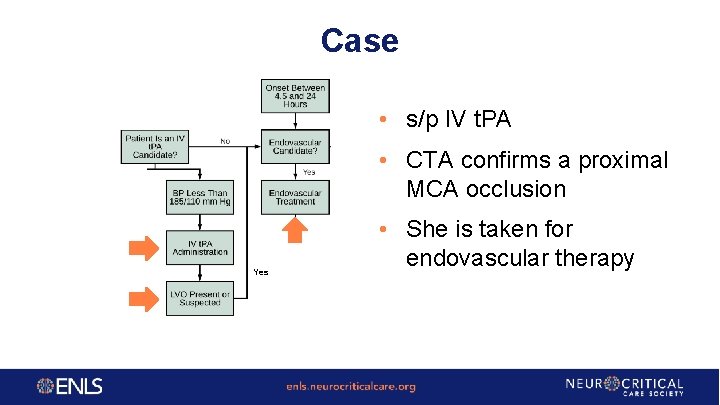
Case • s/p IV t. PA • CTA confirms a proximal MCA occlusion Yes • She is taken for endovascular therapy
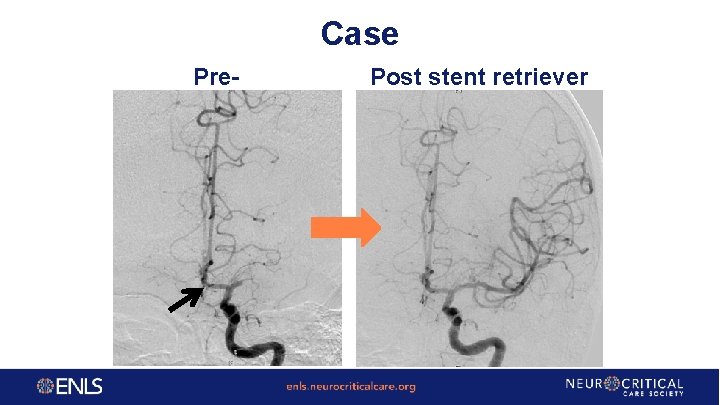
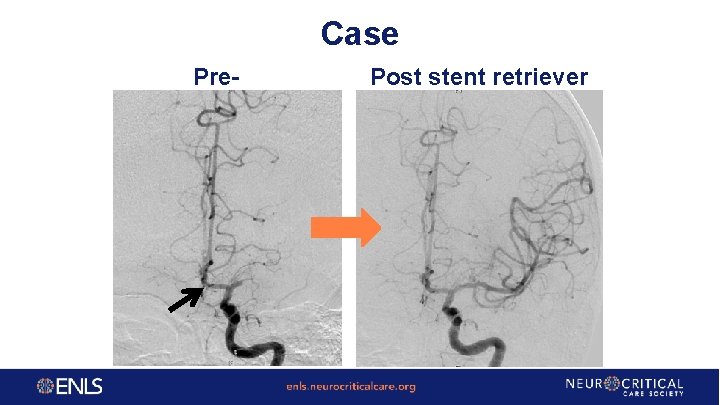
Case Pre- Post stent retriever
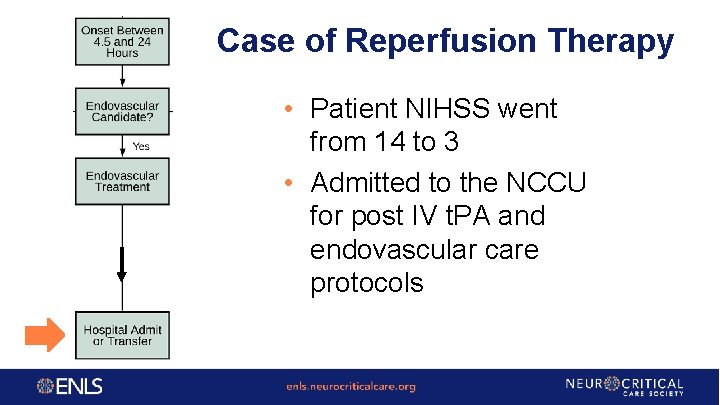
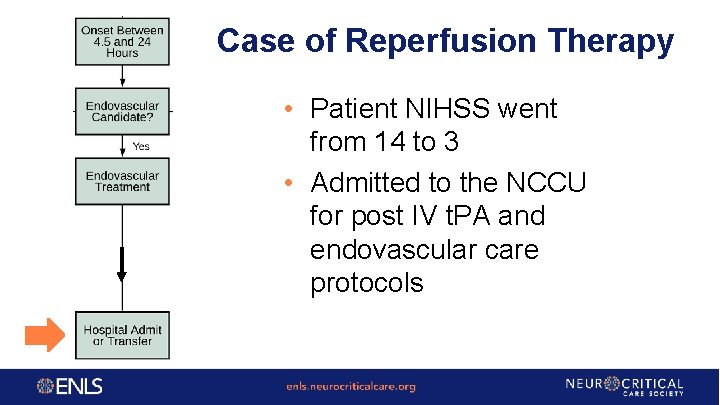
Case of Reperfusion Therapy • Patient NIHSS went from 14 to 3 • Admitted to the NCCU for post IV t. PA and endovascular care protocols
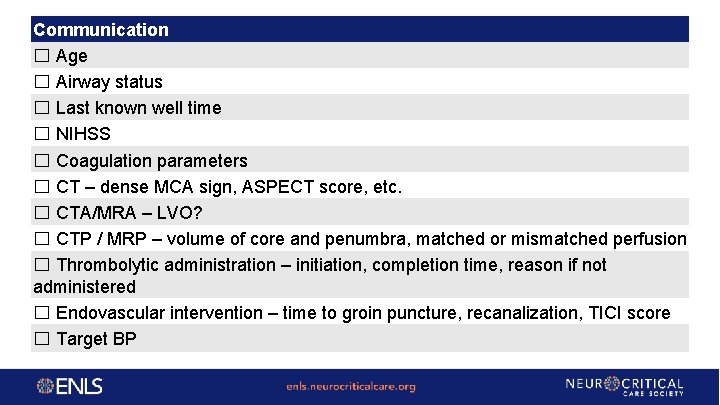
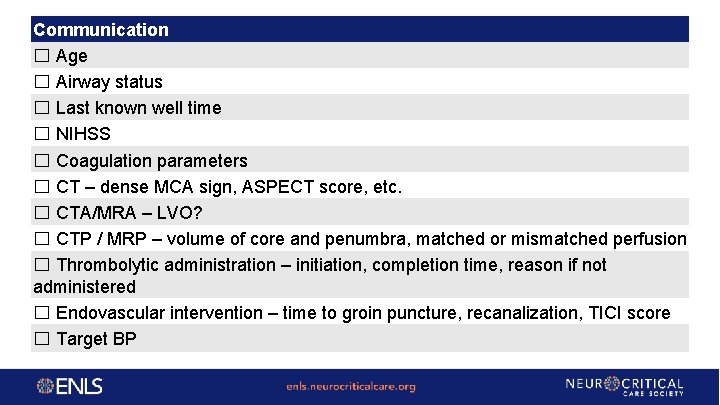
Communication ☐ Age ☐ Airway status ☐ Last known well time ☐ NIHSS ☐ Coagulation parameters ☐ CT – dense MCA sign, ASPECT score, etc. ☐ CTA/MRA – LVO? ☐ CTP / MRP – volume of core and penumbra, matched or mismatched perfusion ☐ Thrombolytic administration – initiation, completion time, reason if not administered ☐ Endovascular intervention – time to groin puncture, recanalization, TICI score ☐ Target BP
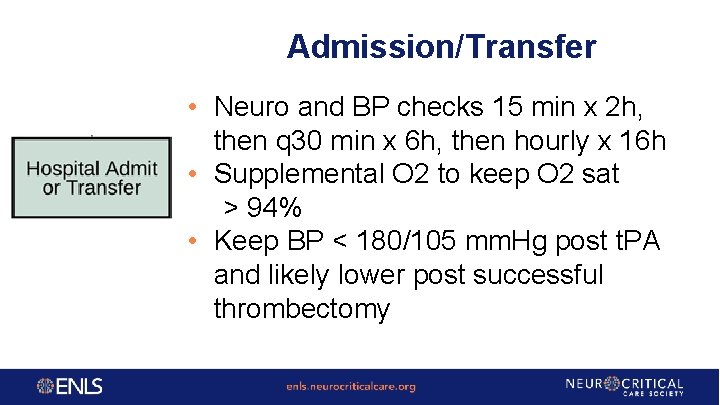
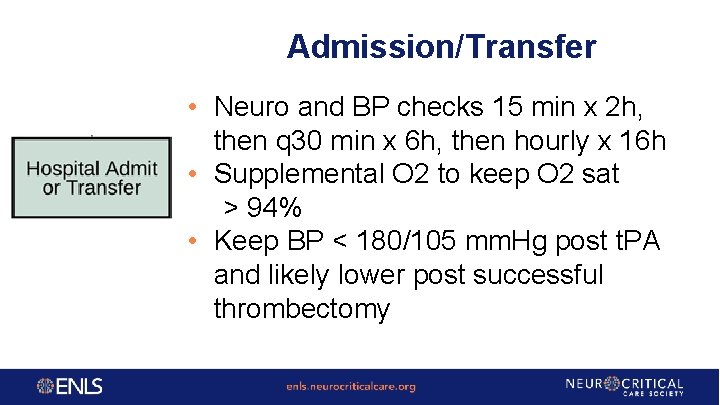
Admission/Transfer • Neuro and BP checks 15 min x 2 h, then q 30 min x 6 h, then hourly x 16 h • Supplemental O 2 to keep O 2 sat > 94% • Keep BP < 180/105 mm. Hg post t. PA and likely lower post successful thrombectomy
Admission/Transfer • • • Continuous telemetry IV normal saline – euvolemia Keep glucose 140 -180 mg/dl (7. 8 -10 mmol/L) Aggressive fever control If t. PA administered, § no anticoagulation or antiplatelets for 24 hours § avoid indwelling urinary catheters, nasogastric tubes and intra-arterial catheters for 4 hours • Swallow assessment before feeding
Pediatric Considerations • • • Not as common as adults (1. 6 -13/100 K children per year) More often presents with seizure Tends to occur in select population § Sickle cell disease § Cardiac abnormalities • • Pediatric NIHSS is validated tool Many stroke mimics (seizure, migraine) in children § MRI is generally the preferred imaging modality • IV t. PA not approved for < 18 years § Only case reports of its use in children § One clinical trial in children age 2 -18 was closed due to insufficient enrollment § Approach on case by case basis • Case reports only for endovascular therapy
Nursing Pearls • • • If acute neurological deficit, check fingerstick glucose and activate stroke team. CT should not be delayed for lab work. Obtain actual weight of patient. Obtain 18 g IV access for perfusion imaging and 2 nd IV if patient will be receiving thrombolytics or going for thrombectomy. t. PA is mixed with swirling, not shaking. t. PA dose should be double-checked with 2 nd clinician and BP and neuro status checked within 15 min prior to administration. Bolus dose, infusion dose, wasted t. PA, and follow-up flush post-t. PA should be documented. Patients not receiving t. PA may be allowed to have permissively higher blood pressure. Notify the provider immediately for decline in neuro status, acute hypertension, angioedema.
Clinical Pearls • • • LKW in wake-up stroke is time patient went to bed. In cases of stuttering symptoms, the clock is reset only if patient is 100% back to baseline. With patients on direct oral anticoagulation, determine the last time the patient took their medication. Low NIHSS is not a contraindication to thrombolysis. Observing patients after thrombolysis for response is not required prior to mechanical thrombectomy. Consider short-term dual antiplatelet therapy in patients with TIA and ischemic stroke.

Questions?