Enhanced Recovery After Surgery What is it and
- Slides: 32
Enhanced Recovery After Surgery: What is it and is it worth the trouble? Andrew Hill Colorectal Surgeon Middlemore Hospital, University of Auckland Enhanced Recovery After Surgery Group
What is ERAS? • • AKA Fast-track or ERP Developed by Kehlet in Denmark in colonic surgery Gradually has gained world-wide acceptance Originally described in Open Surgery but same advantages seem to apply for Laparoscopy
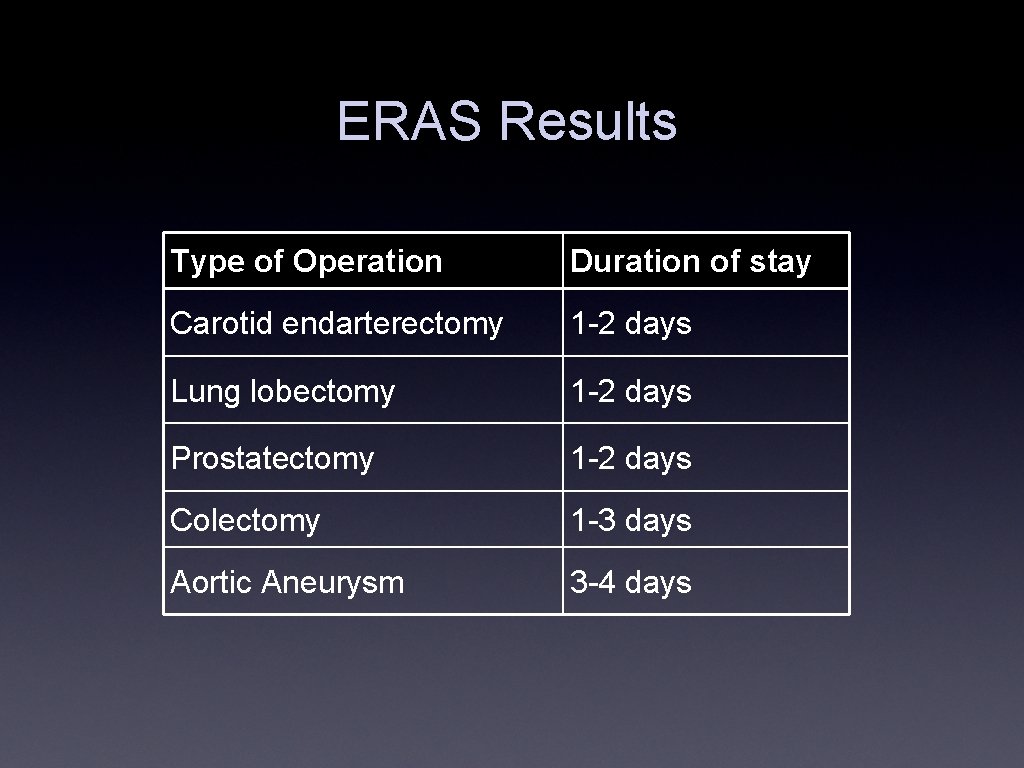
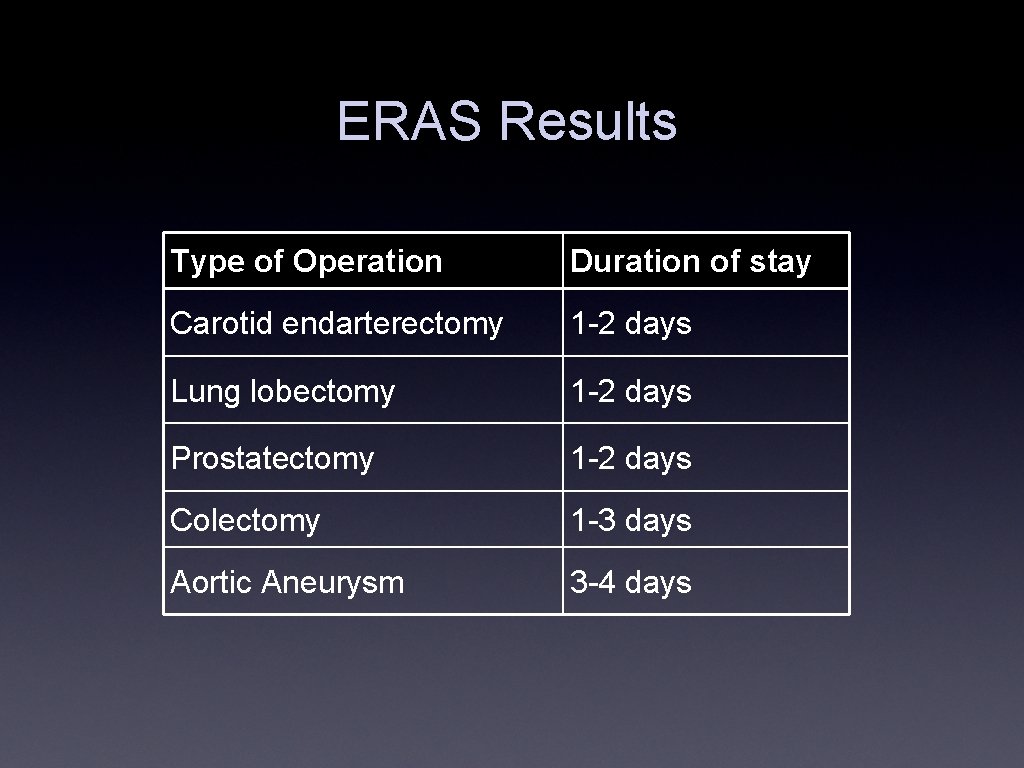
ERAS Results Type of Operation Duration of stay Carotid endarterectomy 1 -2 days Lung lobectomy 1 -2 days Prostatectomy 1 -2 days Colectomy 1 -3 days Aortic Aneurysm 3 -4 days
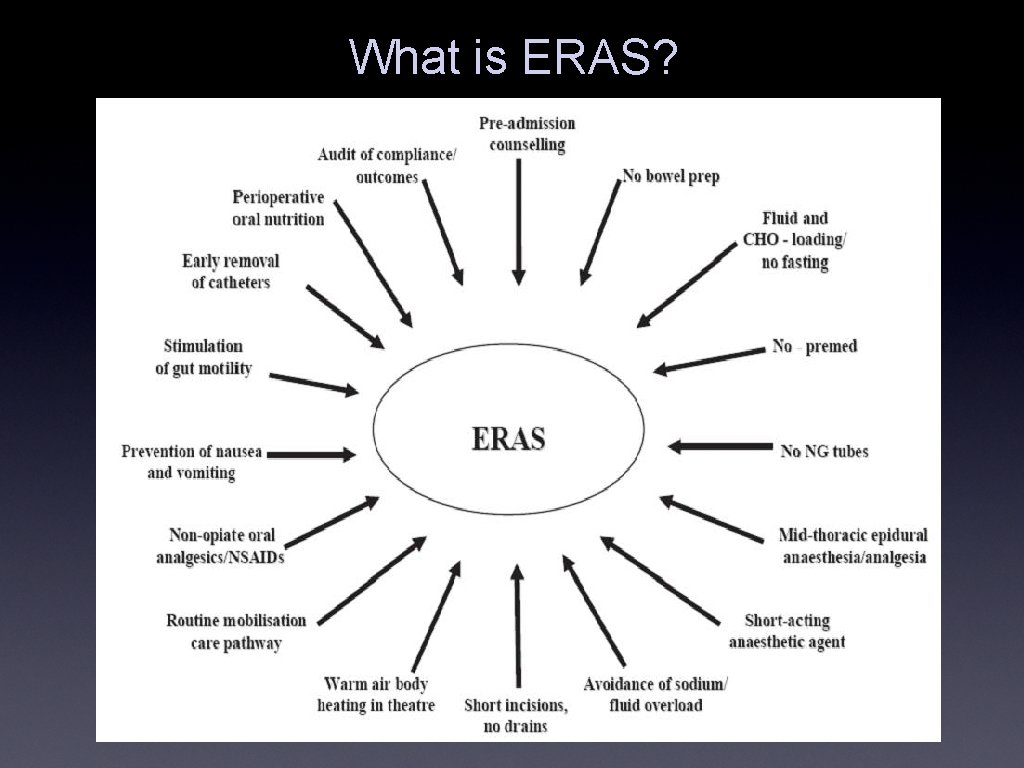
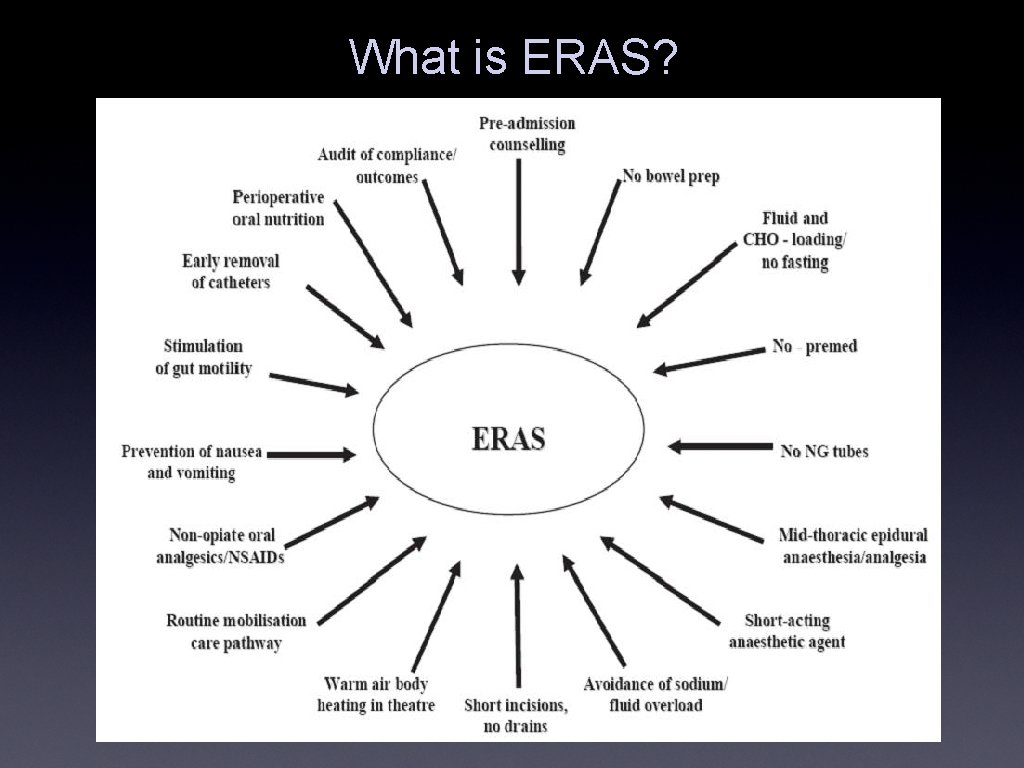
What is ERAS?
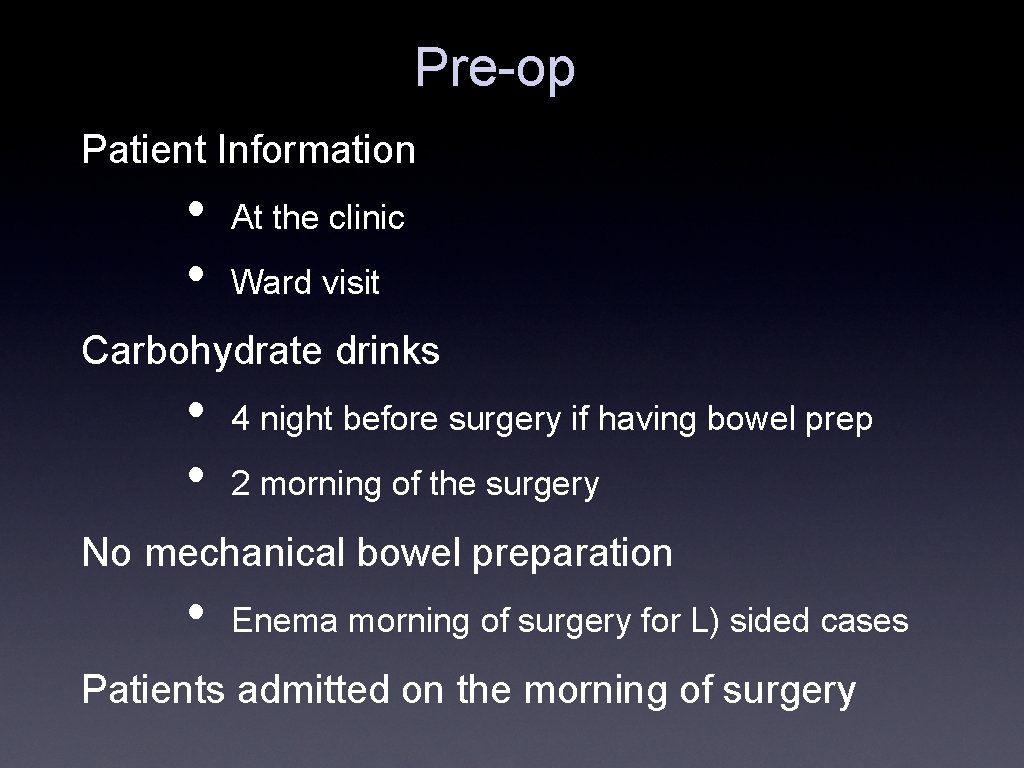
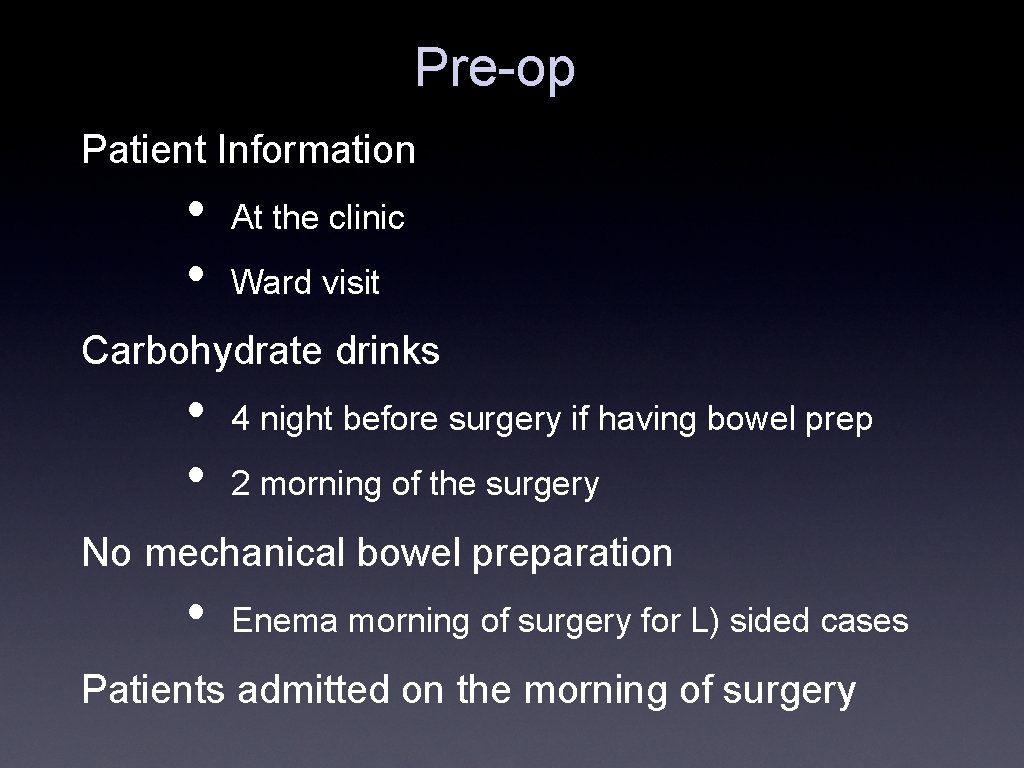
Pre-op Patient Information • • At the clinic Ward visit Carbohydrate drinks • • 4 night before surgery if having bowel prep 2 morning of the surgery No mechanical bowel preparation • Enema morning of surgery for L) sided cases Patients admitted on the morning of surgery
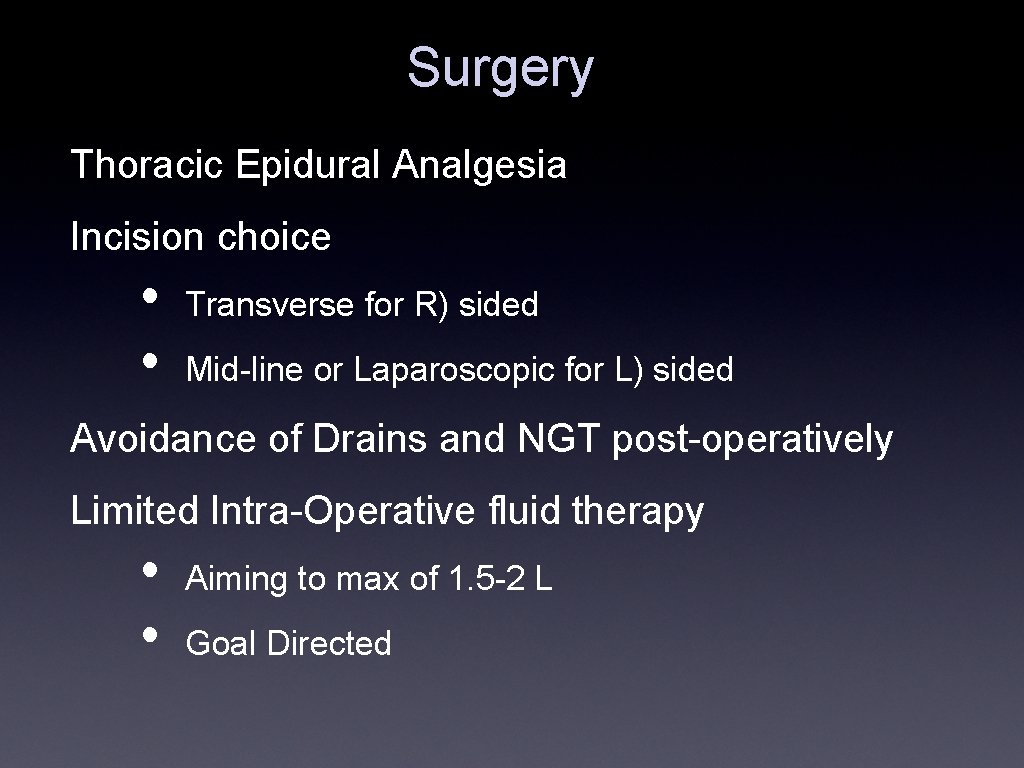
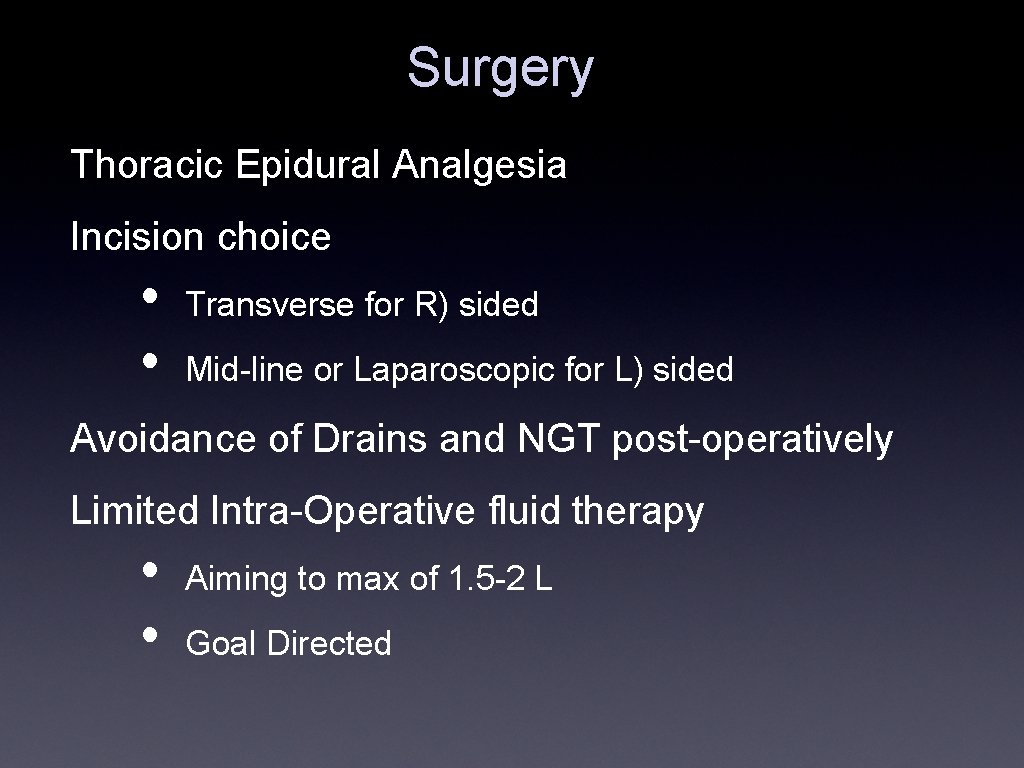
Surgery Thoracic Epidural Analgesia Incision choice • • Transverse for R) sided Mid-line or Laparoscopic for L) sided Avoidance of Drains and NGT post-operatively Limited Intra-Operative fluid therapy • • Aiming to max of 1. 5 -2 L Goal Directed
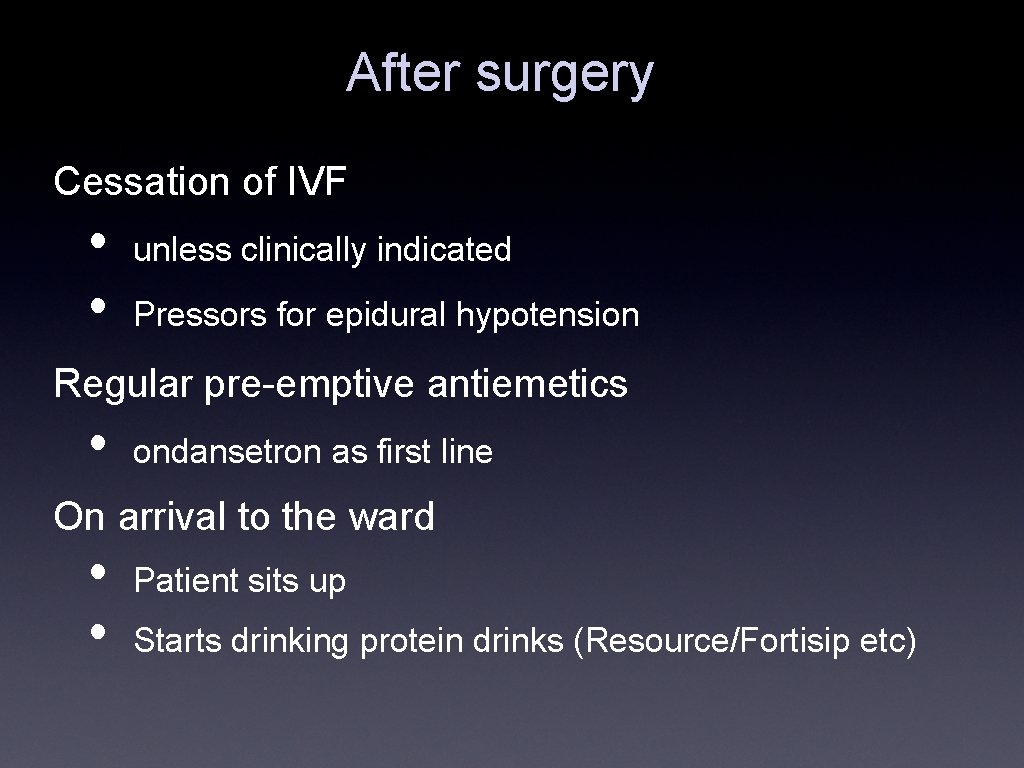
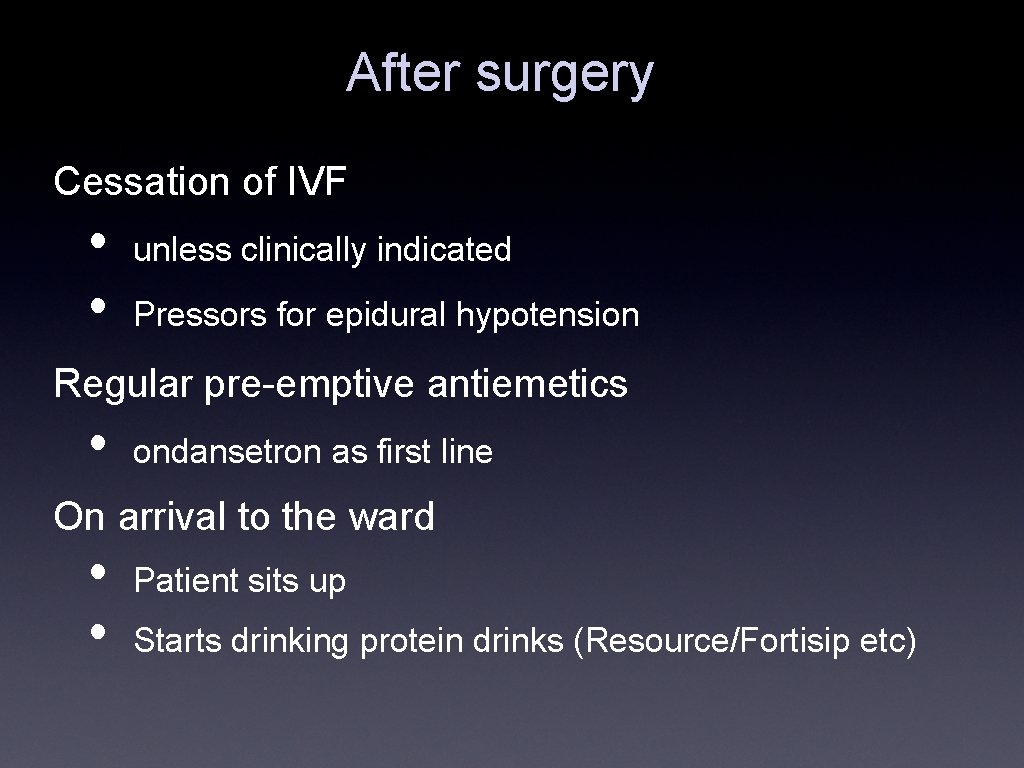
After surgery Cessation of IVF • • unless clinically indicated Pressors for epidural hypotension Regular pre-emptive antiemetics • ondansetron as first line On arrival to the ward • • Patient sits up Starts drinking protein drinks (Resource/Fortisip etc)
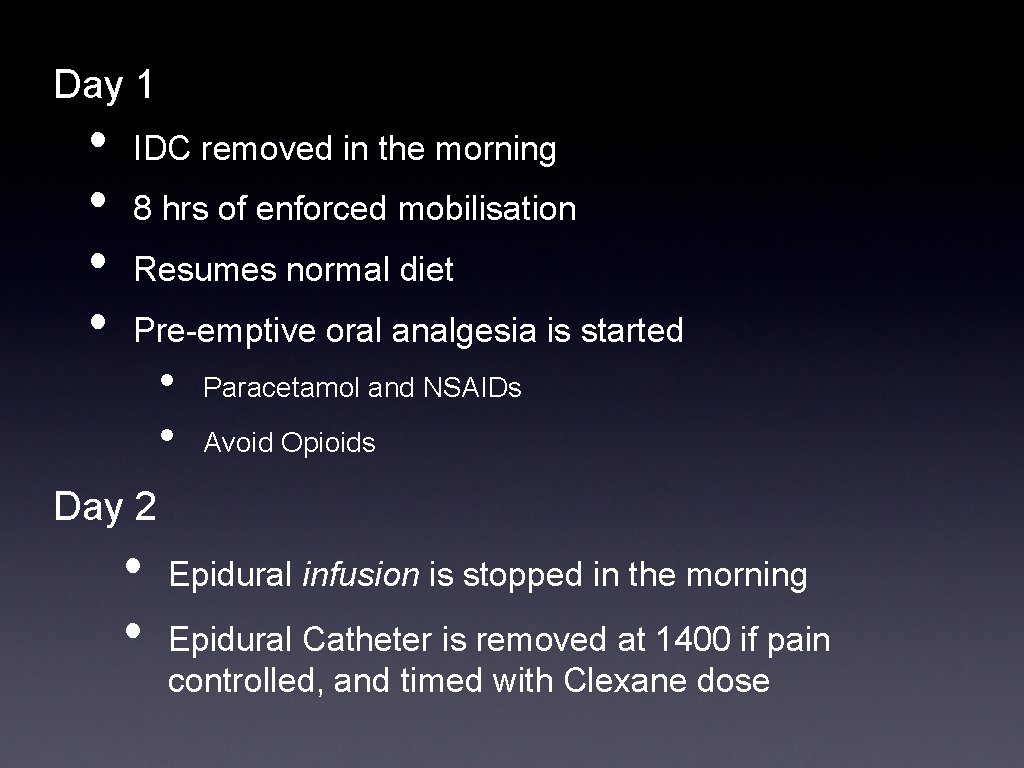
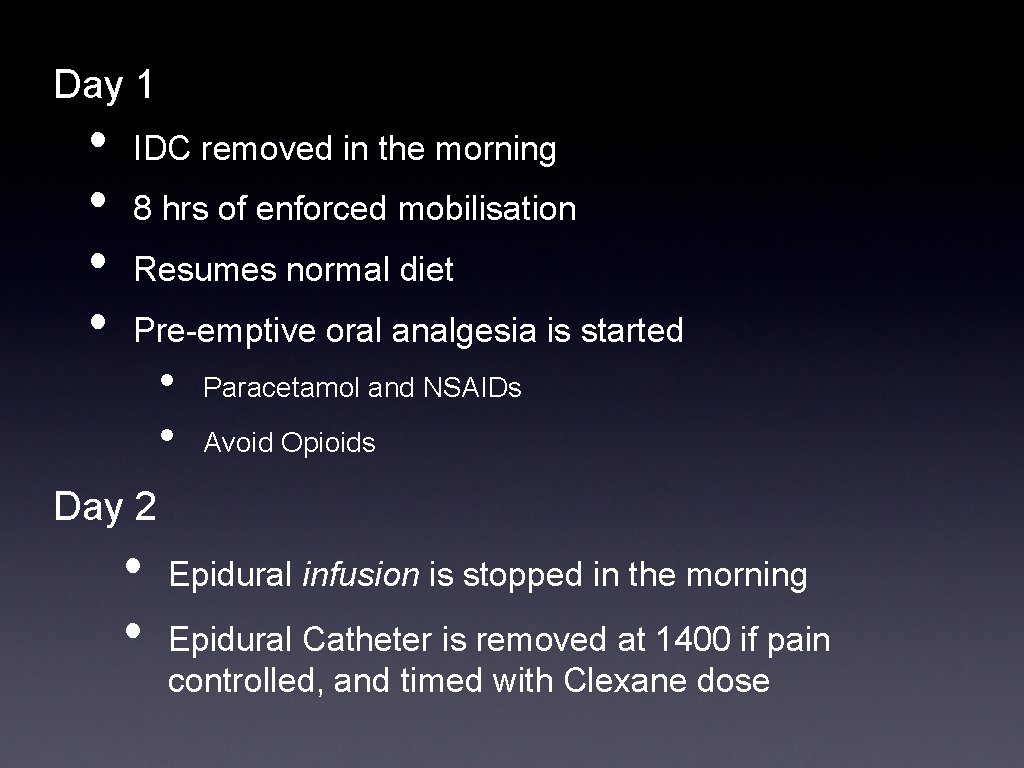
Day 1 • • IDC removed in the morning 8 hrs of enforced mobilisation Resumes normal diet Pre-emptive oral analgesia is started • • Paracetamol and NSAIDs Avoid Opioids Day 2 • • Epidural infusion is stopped in the morning Epidural Catheter is removed at 1400 if pain controlled, and timed with Clexane dose
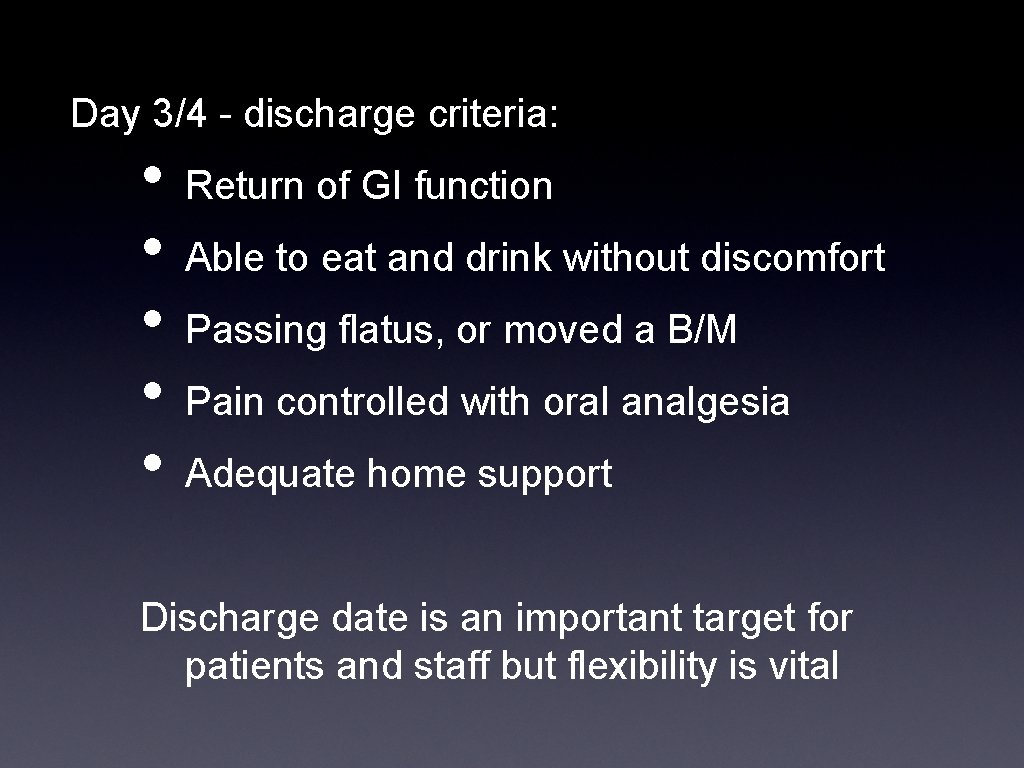
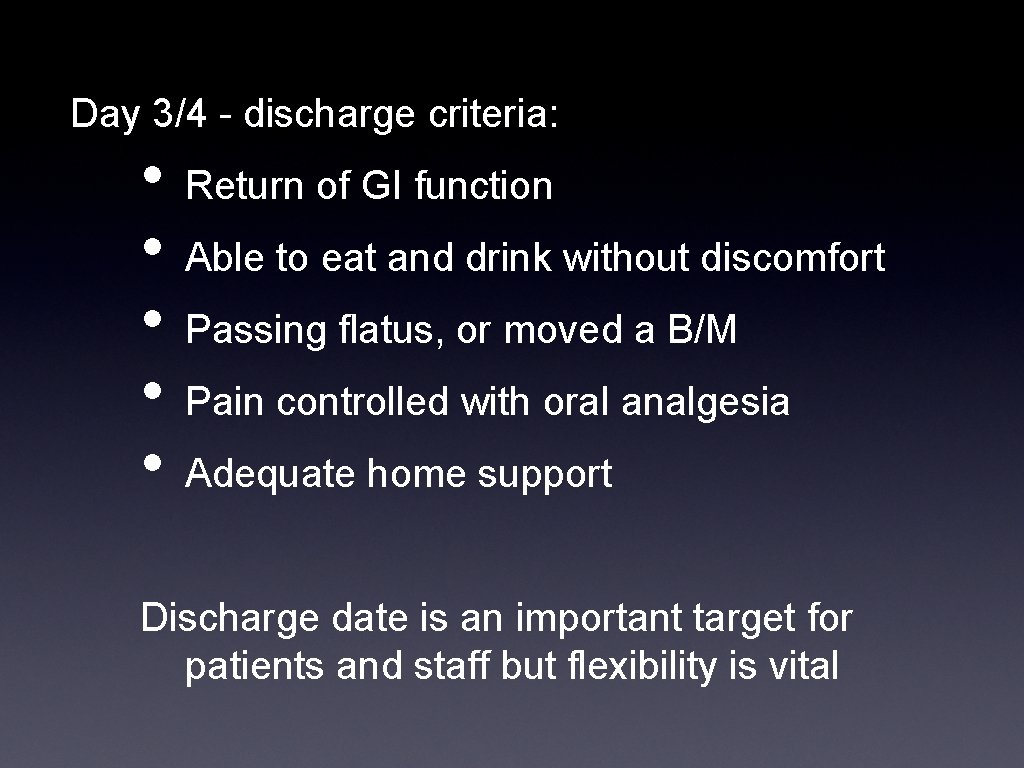
Day 3/4 - discharge criteria: • • • Return of GI function Able to eat and drink without discomfort Passing flatus, or moved a B/M Pain controlled with oral analgesia Adequate home support Discharge date is an important target for patients and staff but flexibility is vital
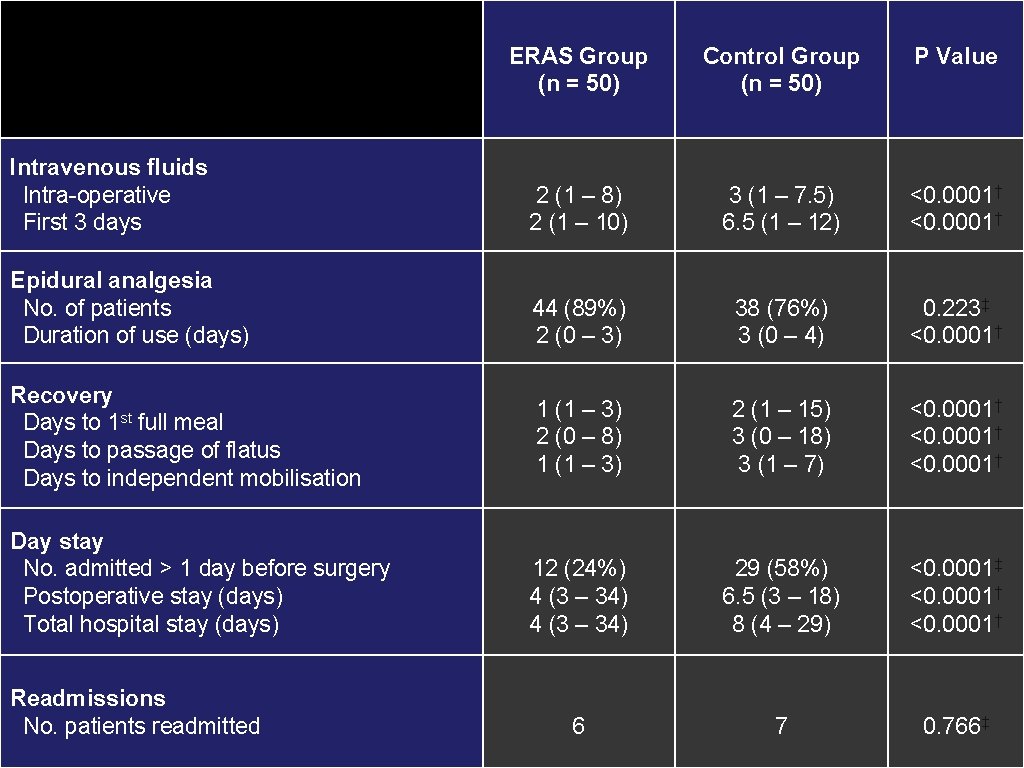
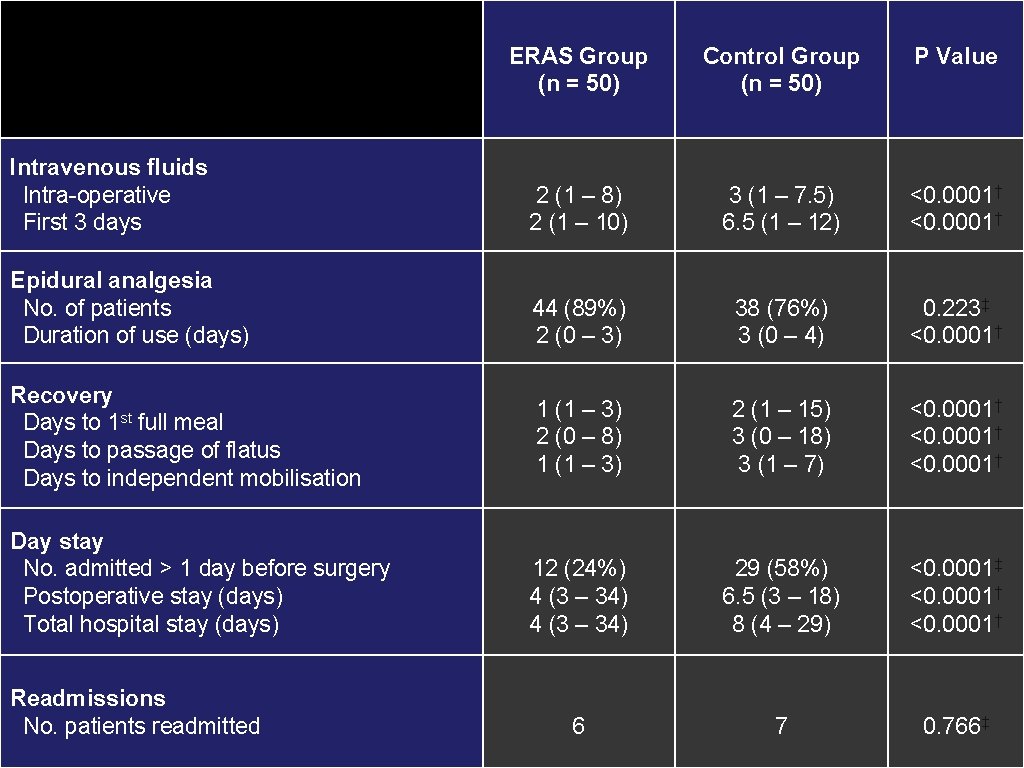
ERAS Group (n = 50) Control Group (n = 50) P Value Intravenous fluids Intra-operative First 3 days 2 (1 – 8) 2 (1 – 10) 3 (1 – 7. 5) 6. 5 (1 – 12) <0. 0001† Epidural analgesia No. of patients Duration of use (days) 44 (89%) 2 (0 – 3) 38 (76%) 3 (0 – 4) 0. 223‡ <0. 0001† 1 (1 – 3) 2 (0 – 8) 1 (1 – 3) 2 (1 – 15) 3 (0 – 18) 3 (1 – 7) <0. 0001† 12 (24%) 4 (3 – 34) 29 (58%) 6. 5 (3 – 18) 8 (4 – 29) <0. 0001‡ <0. 0001† 6 7 0. 766‡ Recovery Days to 1 st full meal Days to passage of flatus Days to independent mobilisation Day stay No. admitted > 1 day before surgery Postoperative stay (days) Total hospital stay (days) Readmissions No. patients readmitted
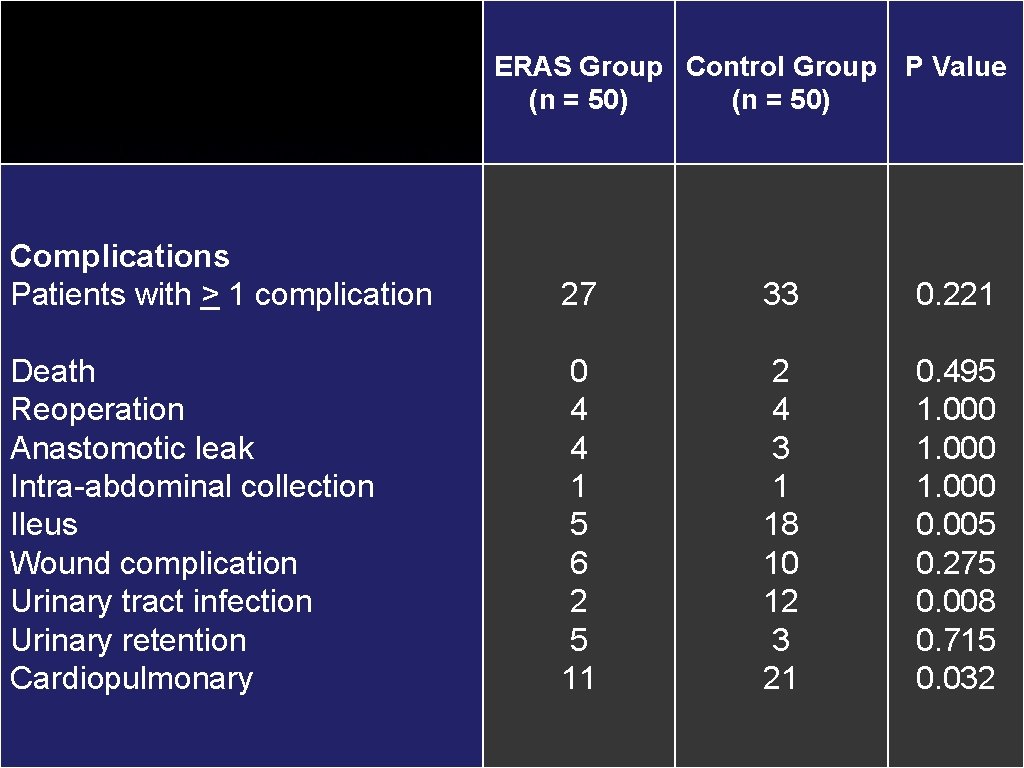
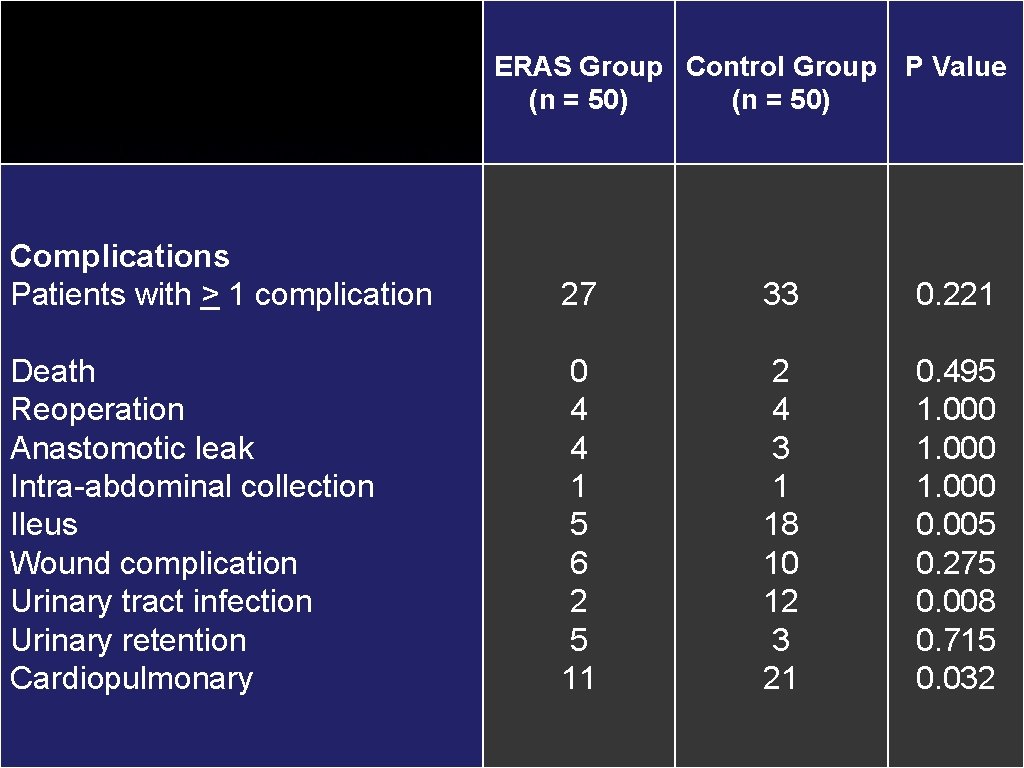
ERAS Group Control Group (n = 50) P Value Complications Patients with > 1 complication 27 33 0. 221 Death Reoperation Anastomotic leak Intra-abdominal collection Ileus Wound complication Urinary tract infection Urinary retention Cardiopulmonary 0 4 4 1 5 6 2 5 11 2 4 3 1 18 10 12 3 21 0. 495 1. 000 0. 005 0. 275 0. 008 0. 715 0. 032
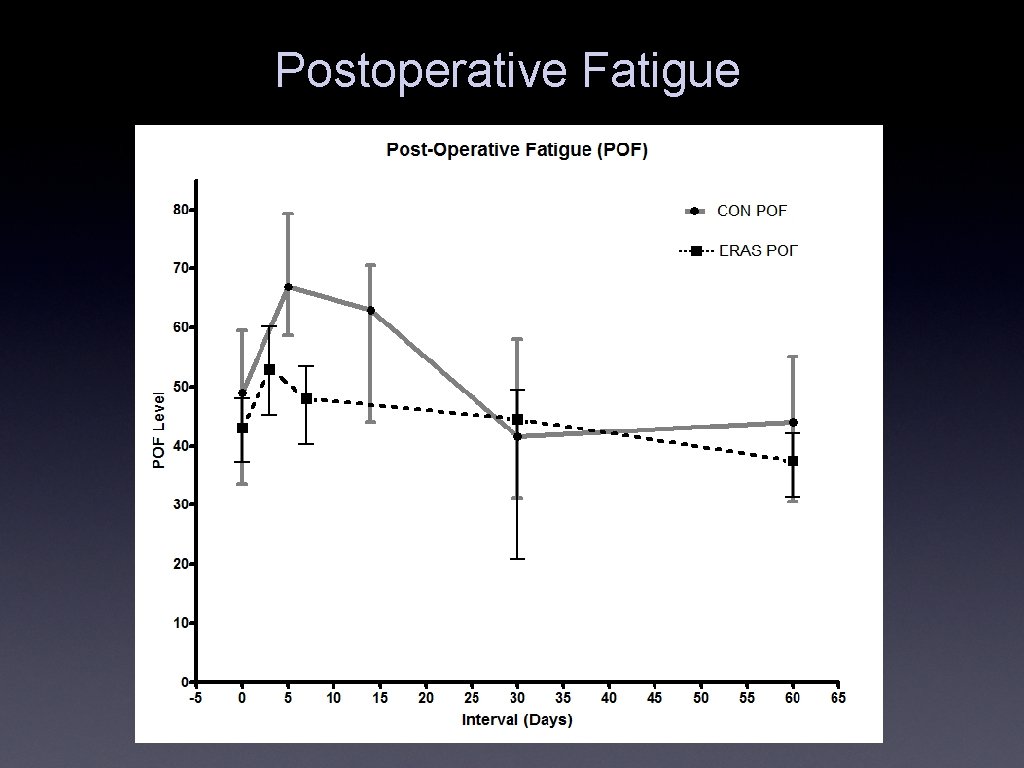
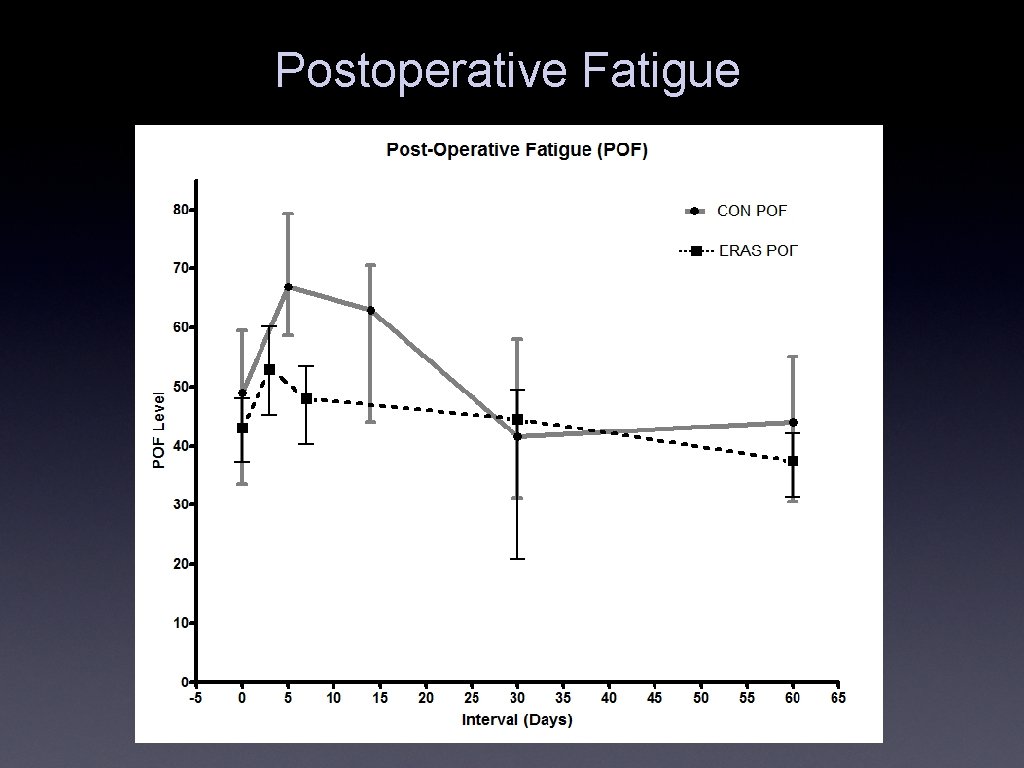
Postoperative Fatigue
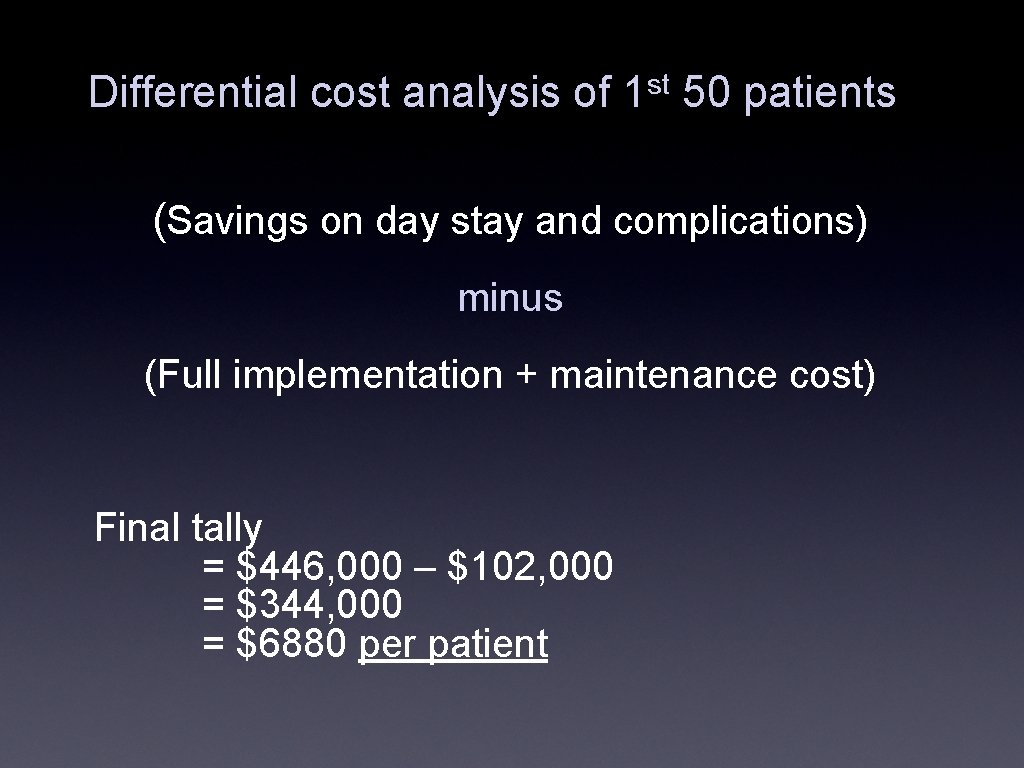
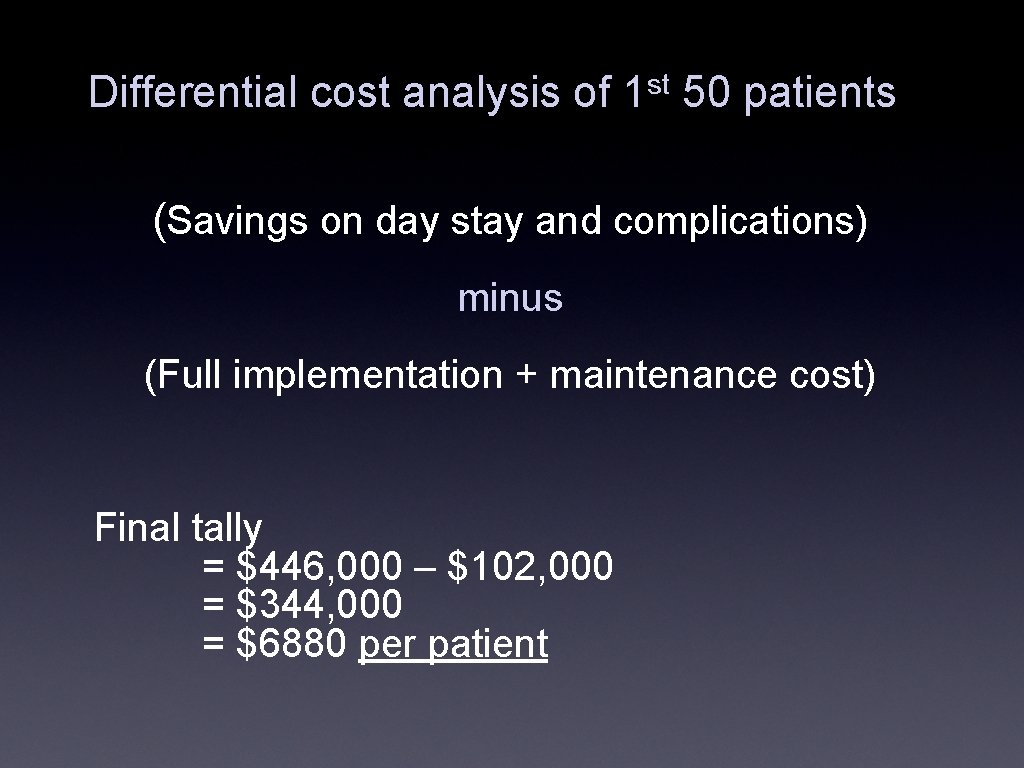
Differential cost analysis of 1 st 50 patients (Savings on day stay and complications) minus (Full implementation + maintenance cost) Final tally = $446, 000 – $102, 000 = $344, 000 = $6880 per patient
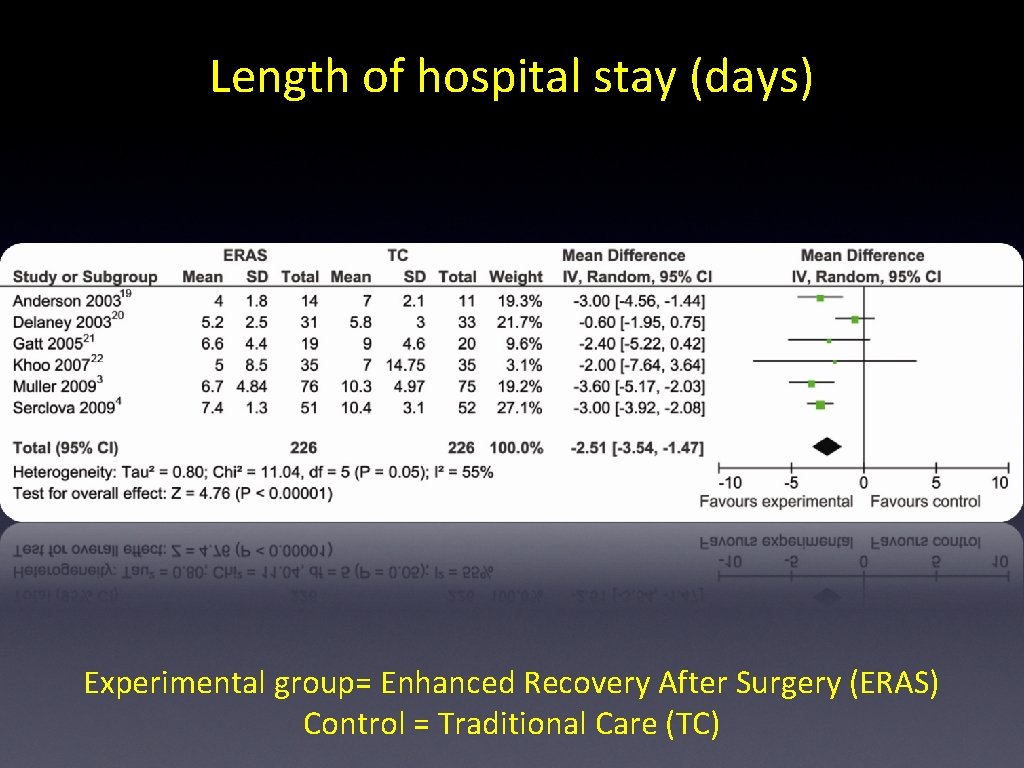
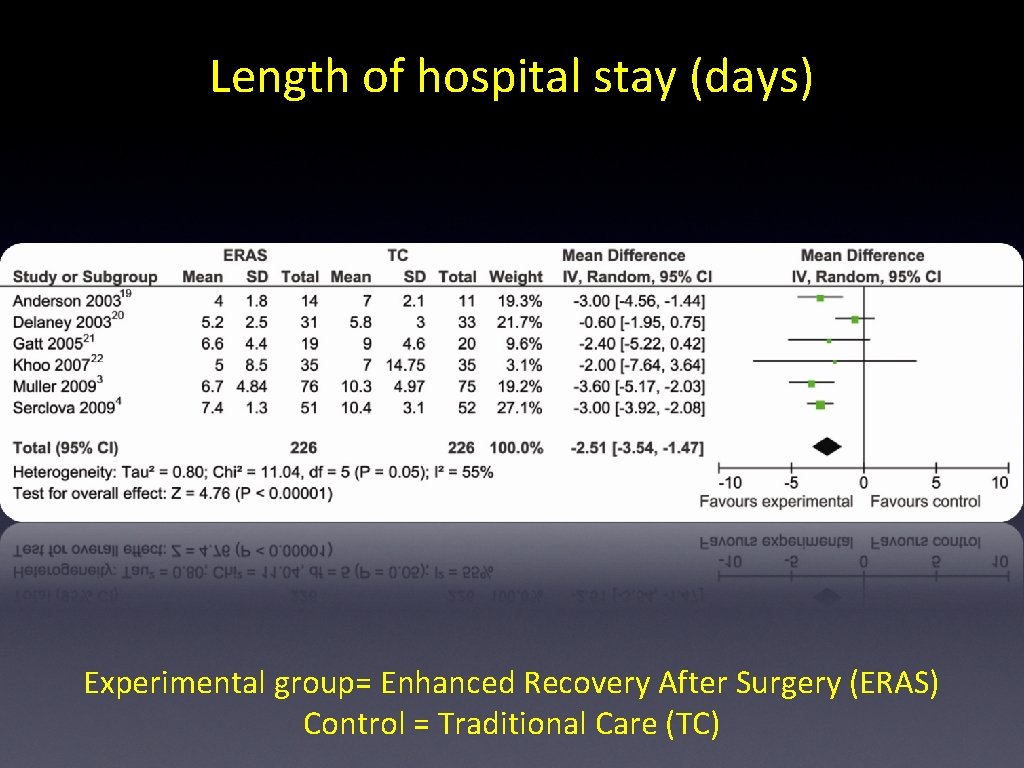
Length of hospital stay (days) Experimental group= Enhanced Recovery After Surgery (ERAS) Control = Traditional Care (TC)
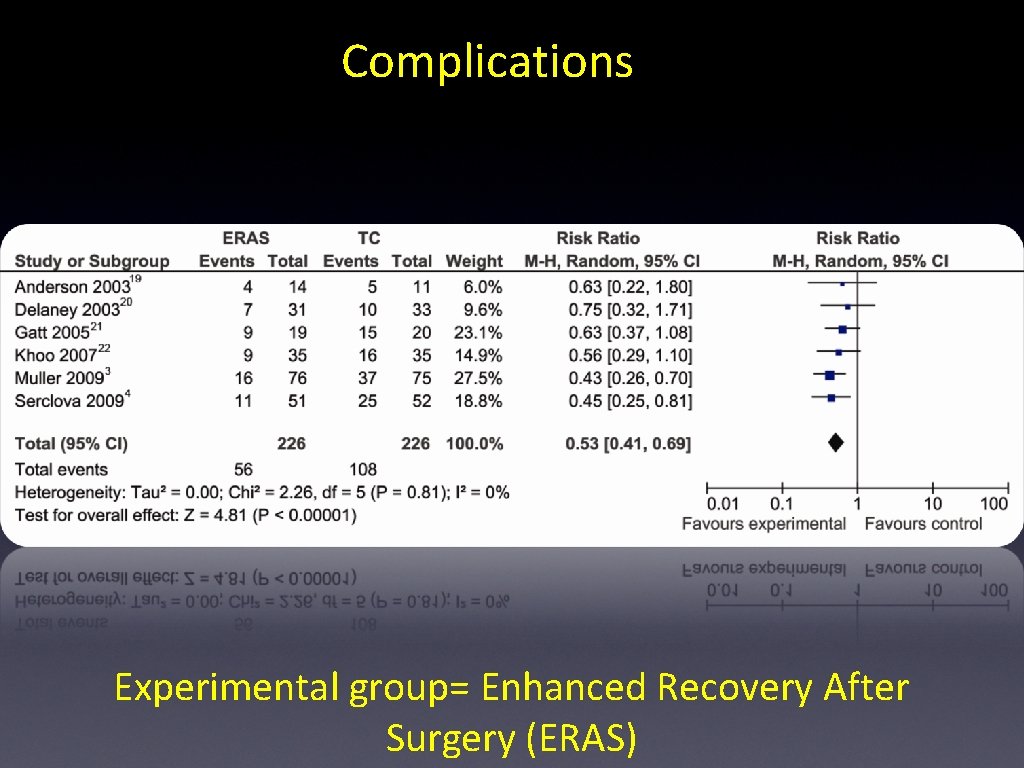
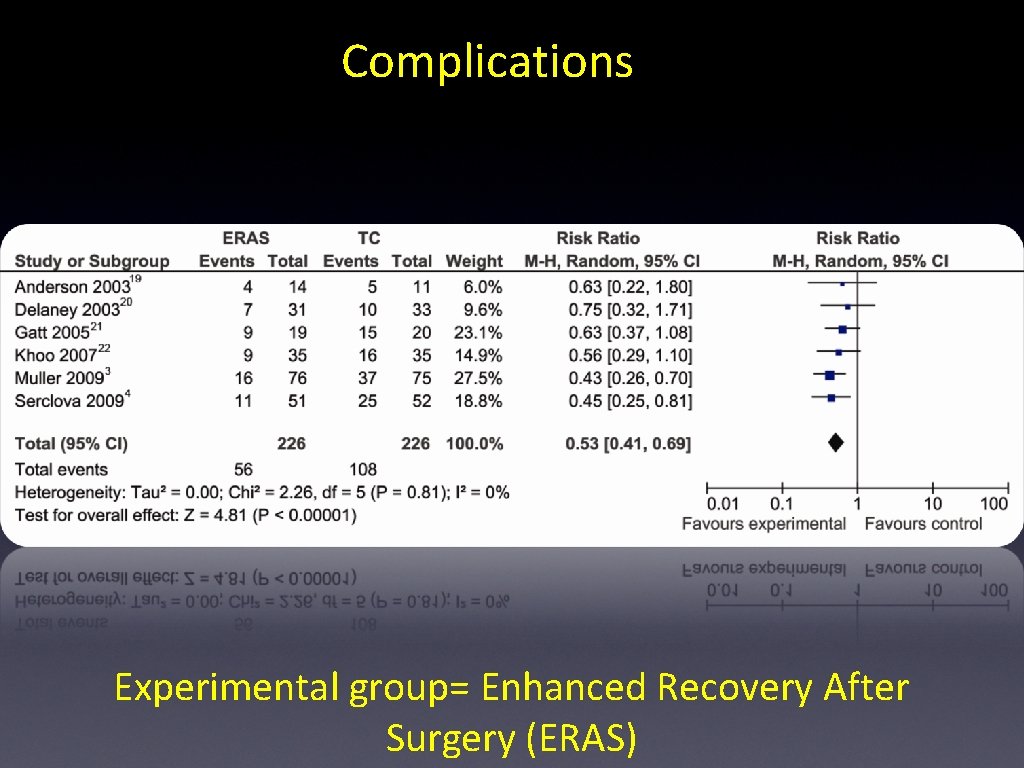
Complications Experimental group= Enhanced Recovery After Surgery (ERAS)
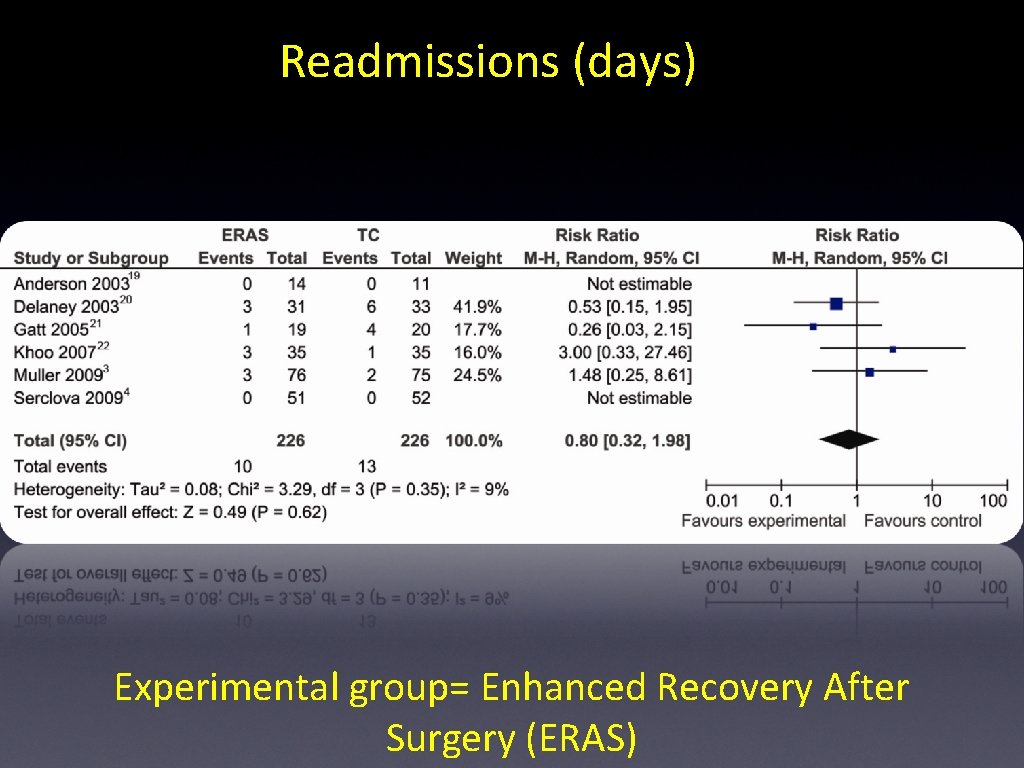
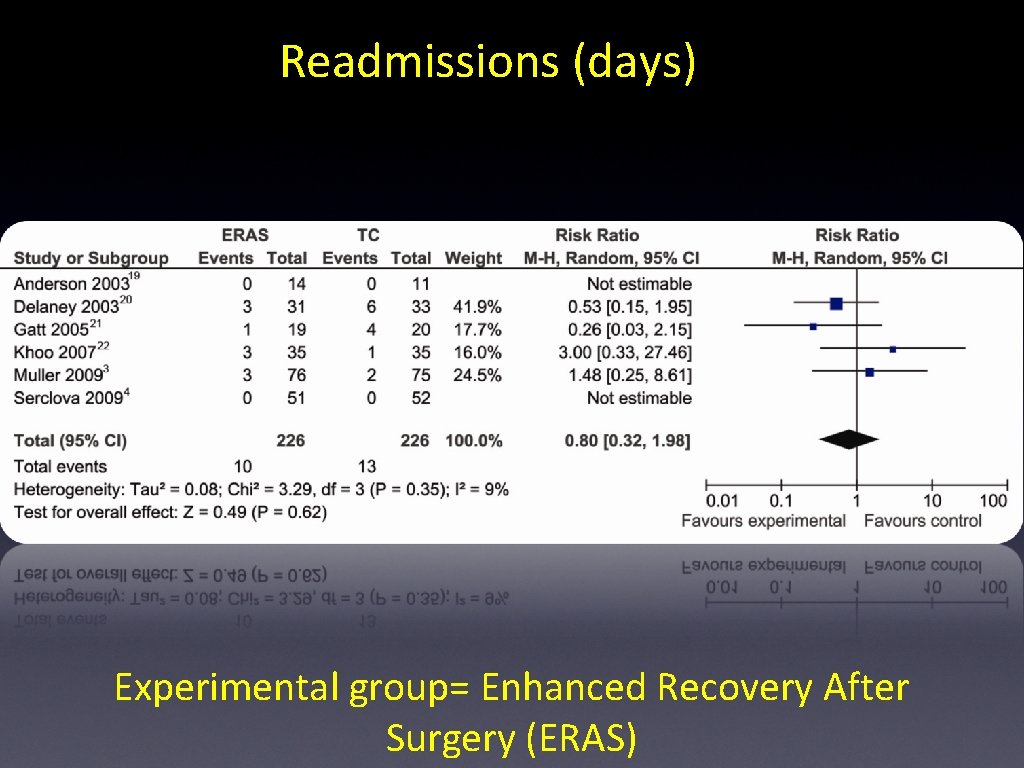
Readmissions (days) Experimental group= Enhanced Recovery After Surgery (ERAS)
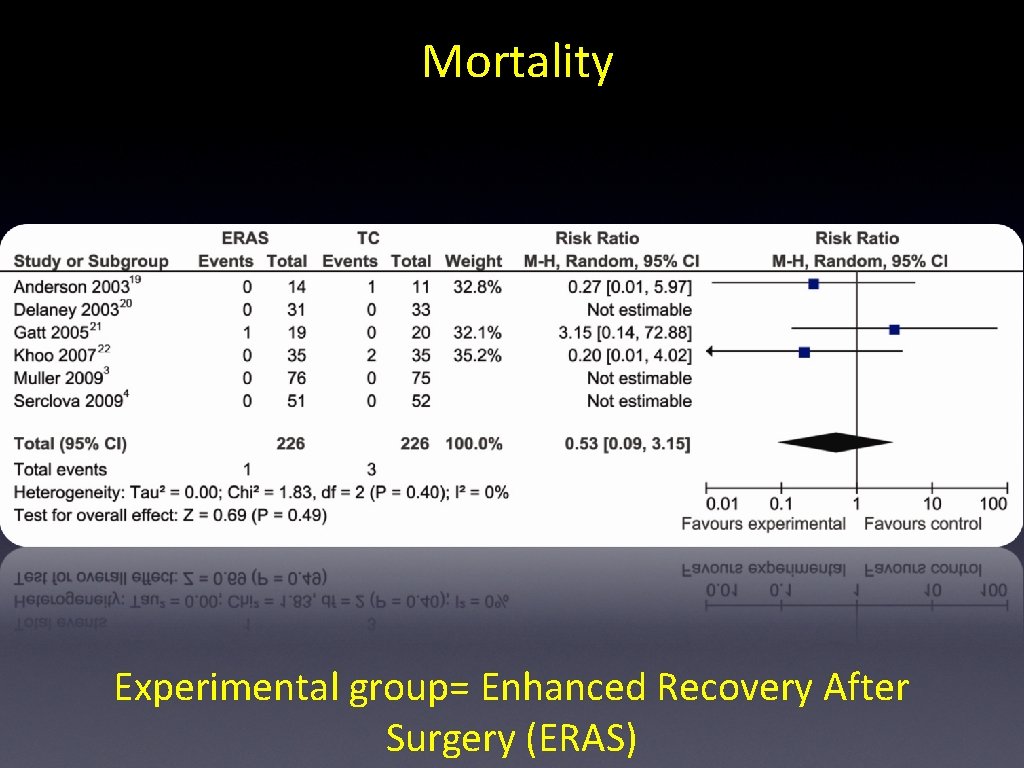
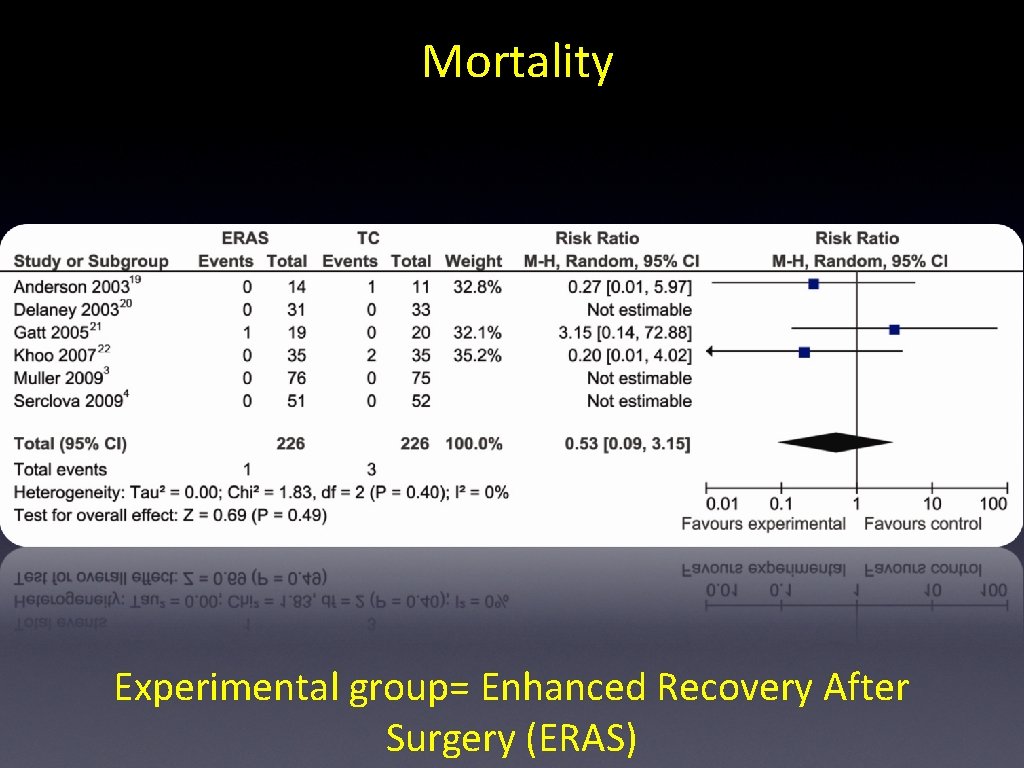
Mortality Experimental group= Enhanced Recovery After Surgery (ERAS)
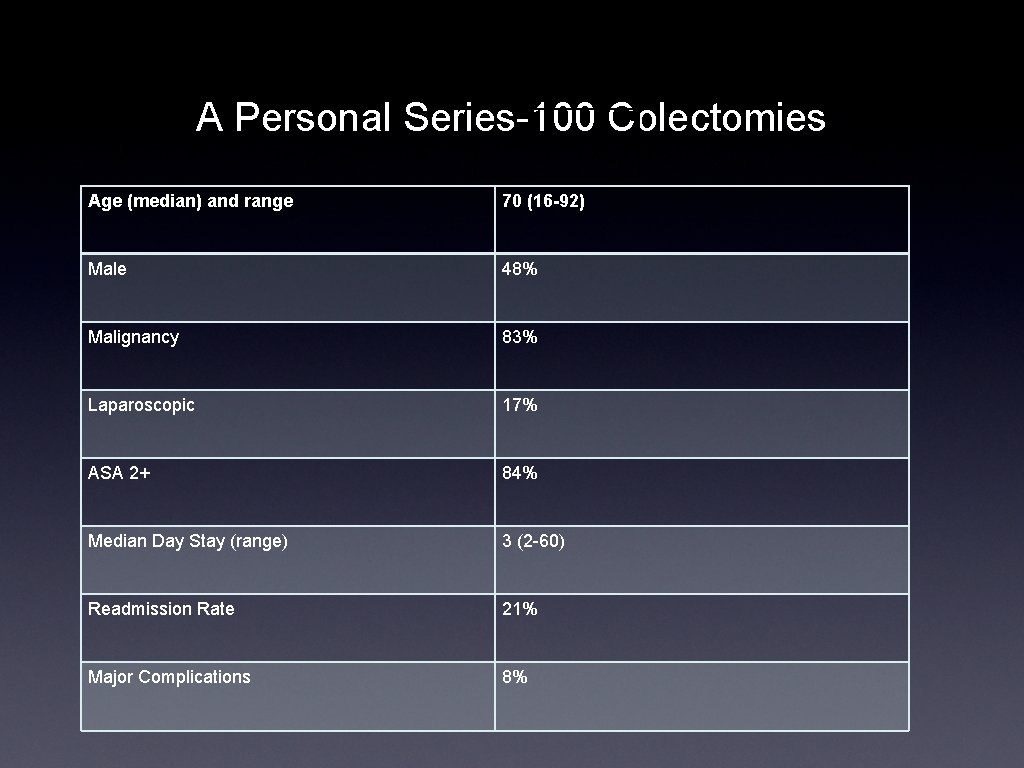
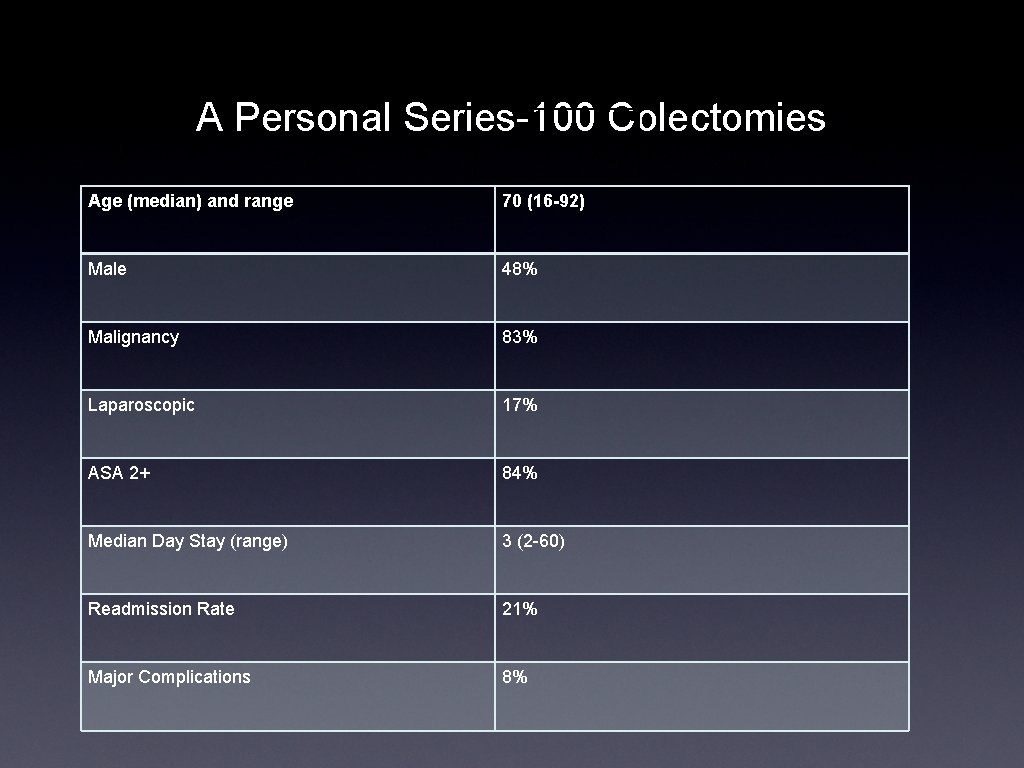
A Personal Series-100 Colectomies Age (median) and range 70 (16 -92) Male 48% Malignancy 83% Laparoscopic 17% ASA 2+ 84% Median Day Stay (range) 3 (2 -60) Readmission Rate 21% Major Complications 8%
ERAS in Bariatrics • Randomised Controlled Trial • 2 Arms • ERAS vs. Standard Perioperative Care
Population • • • Patients undergoing laparoscopic sleeve gastrectomy (LSG) for weight loss Eligibility Criteria • • Procedure at Manukau Surgery Centre (MSC) Consenting surgeon Exclusion Criteria • • Not at MSC Redo procedure
Intervention and Control • Perioperative care as per Bariatric Specific ERAS protocol VS. • Standard perioperative care
Outcomes • Primary outcome was initial median length of hospital stay (LOS) • Powered to detect a reduction in median LOS from 3 (current figure) to 1 (target from the literature) • α: 0. 05; β: 0. 8; Sample Size = 56 (28 in each arm)
Follow up time • 30 day follow up • Further analysis planned for longer term follow up on weight loss data
Results • 71 randomised • 11 post randomization exclusions • 60 patients included in analysis • 31 ERAS group • 29 Non ERAS group
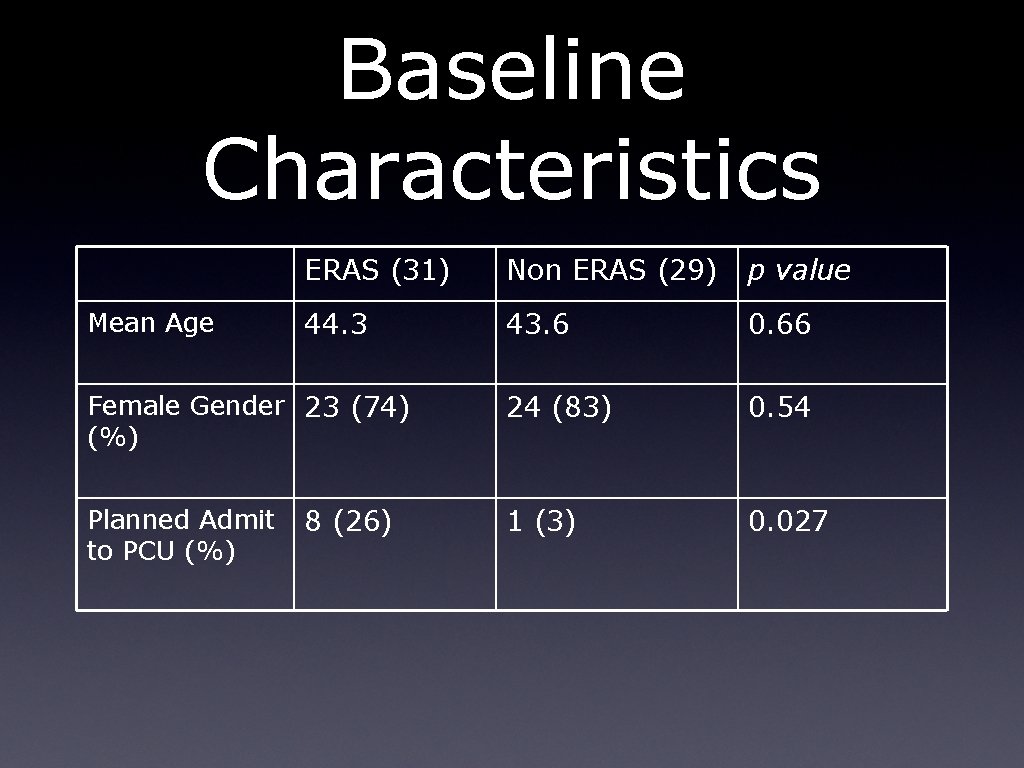
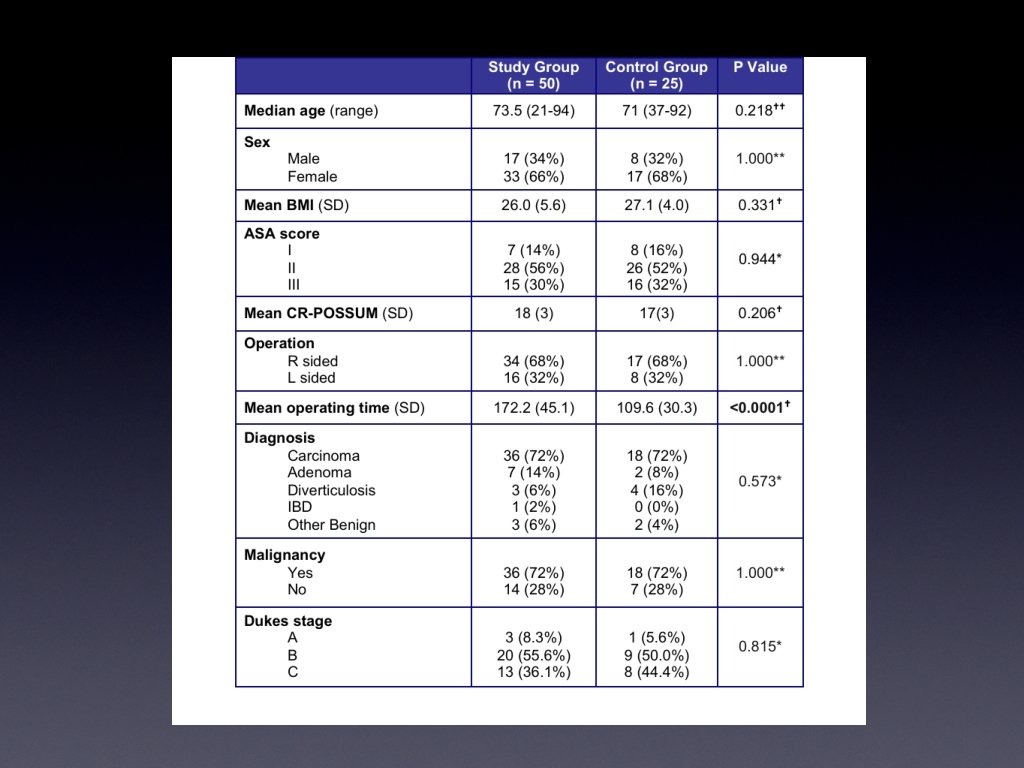
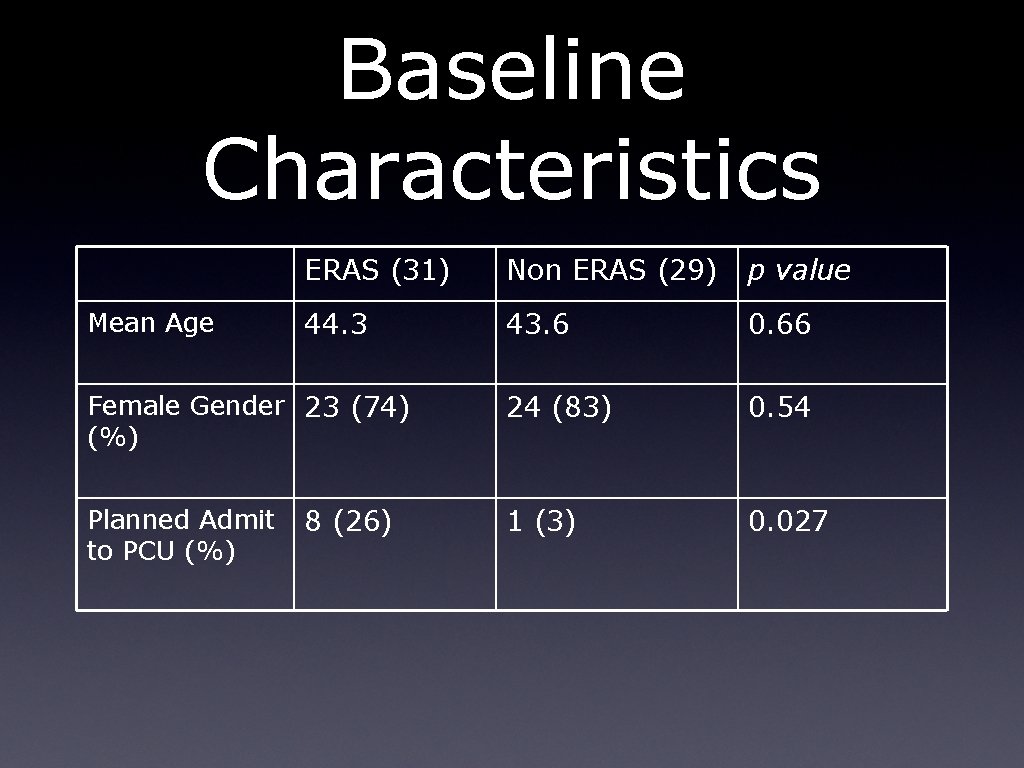
Baseline Characteristics Mean Age ERAS (31) Non ERAS (29) p value 44. 3 43. 6 0. 66 24 (83) 0. 54 1 (3) 0. 027 Female Gender 23 (74) (%) Planned Admit to PCU (%) 8 (26)
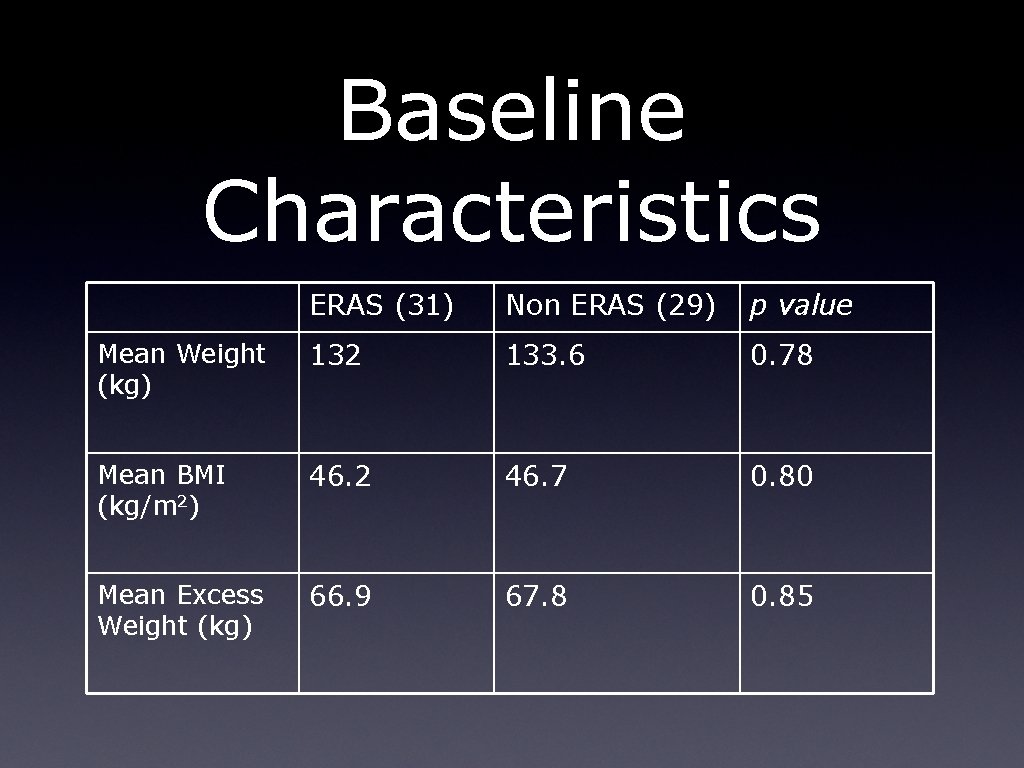
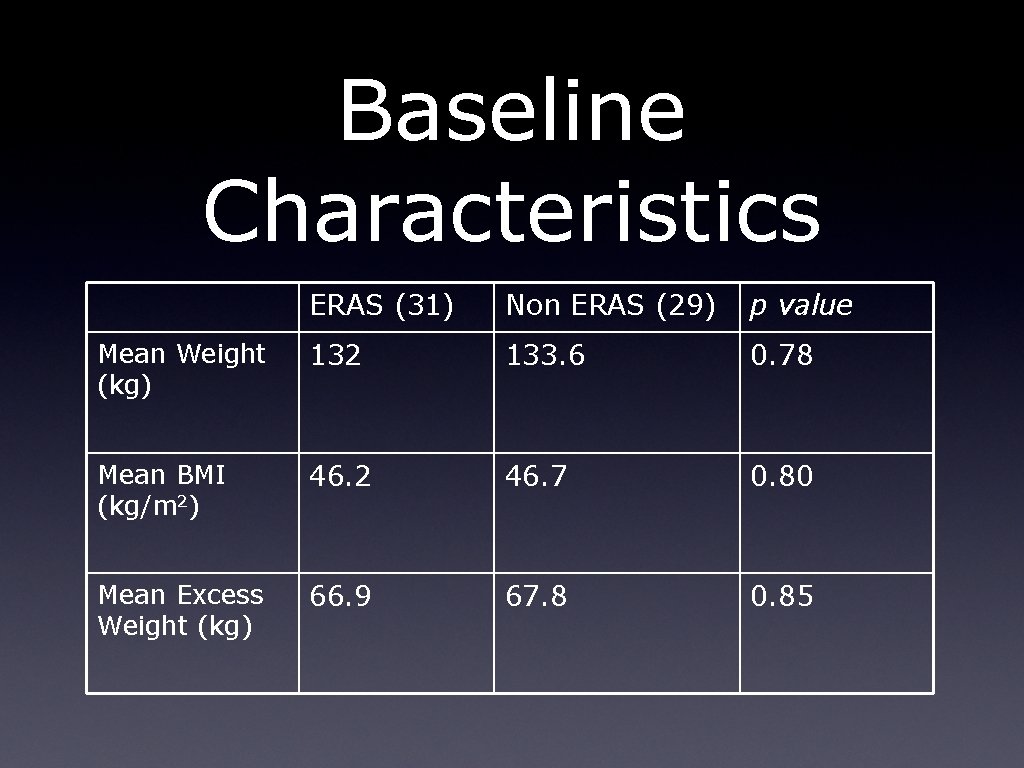
Baseline Characteristics ERAS (31) Non ERAS (29) p value Mean Weight (kg) 132 133. 6 0. 78 Mean BMI (kg/m 2) 46. 2 46. 7 0. 80 Mean Excess Weight (kg) 66. 9 67. 8 0. 85
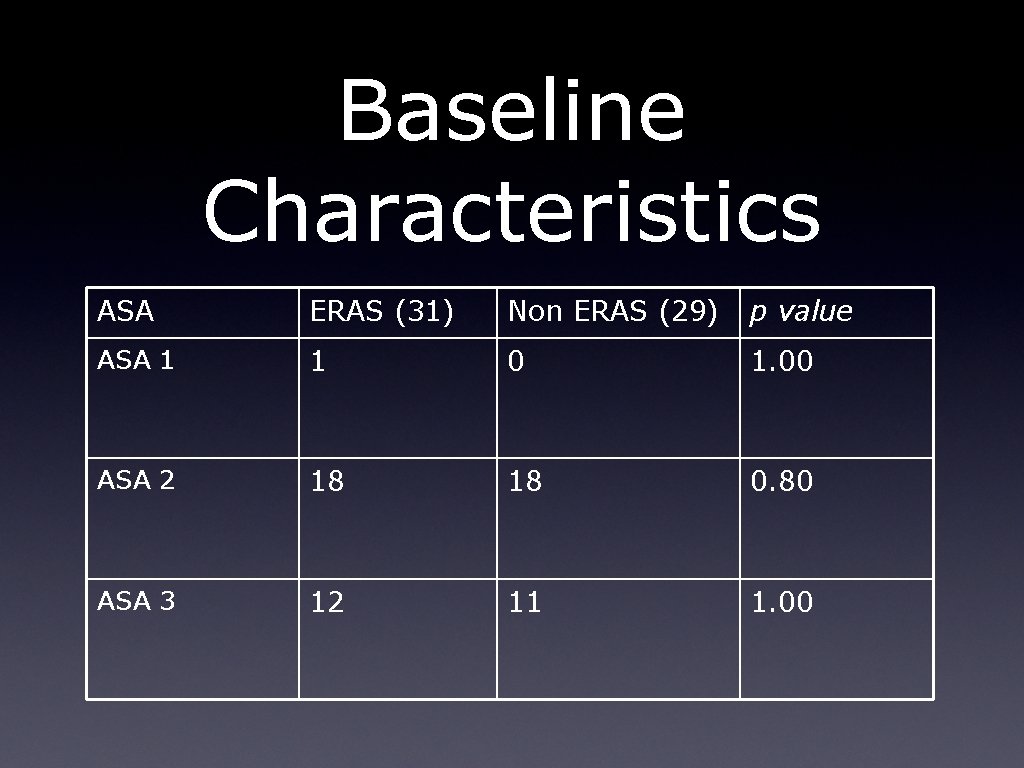
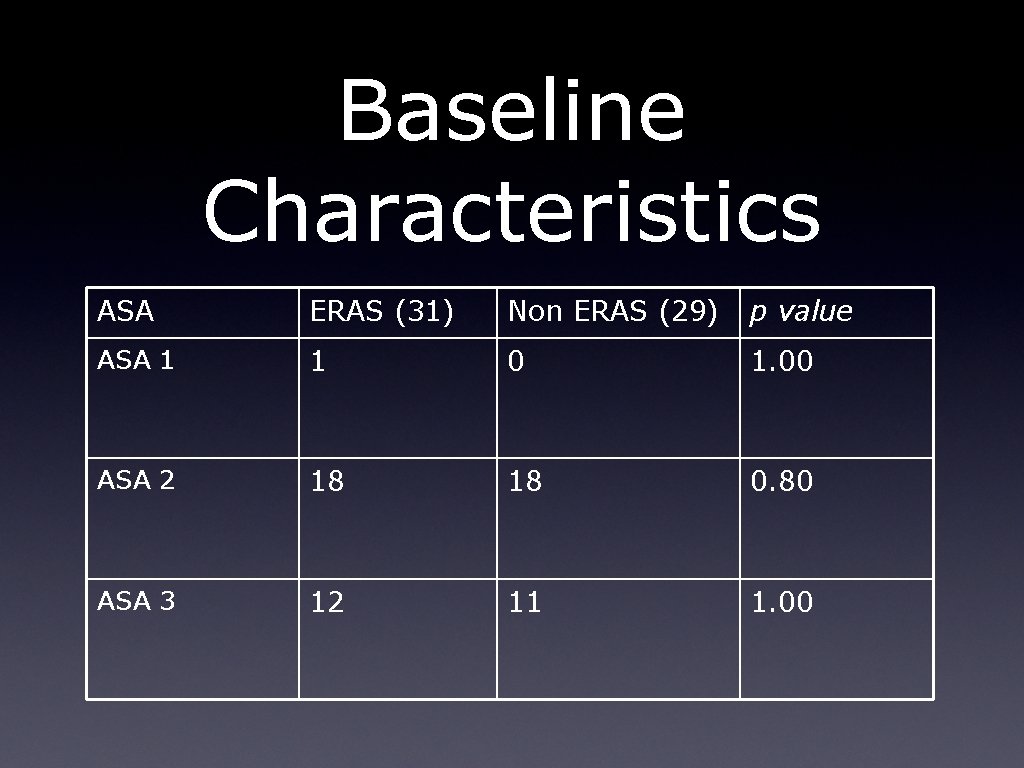
Baseline Characteristics ASA ERAS (31) Non ERAS (29) p value ASA 1 1 0 1. 00 ASA 2 18 18 0. 80 ASA 3 12 11 1. 00
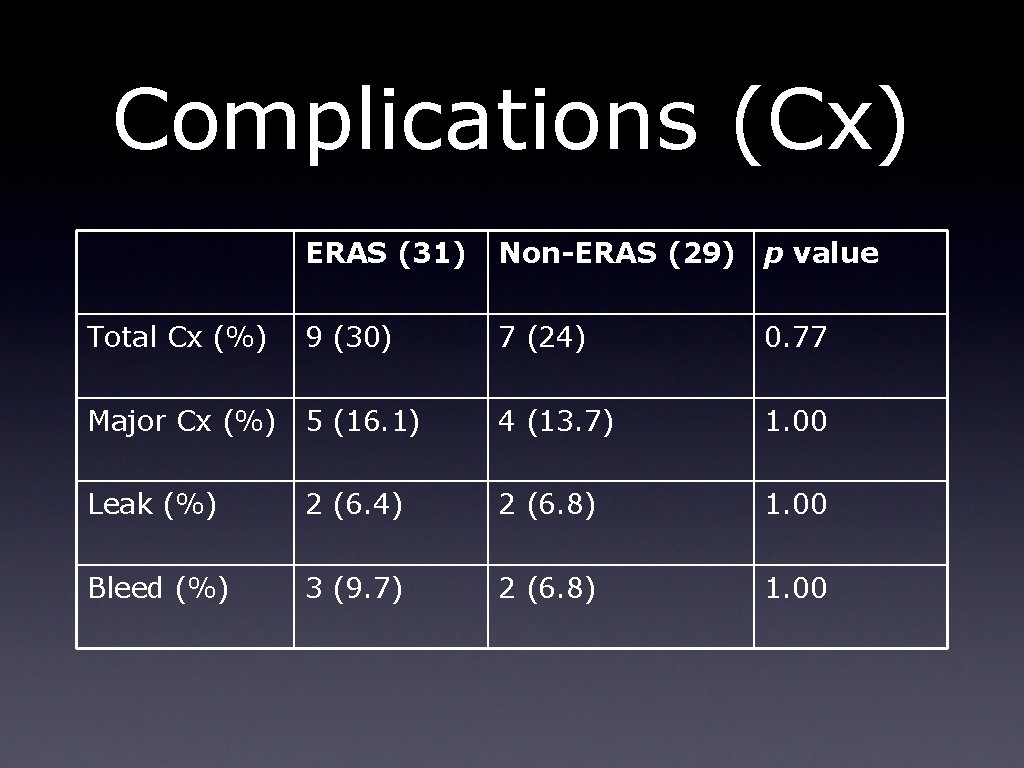
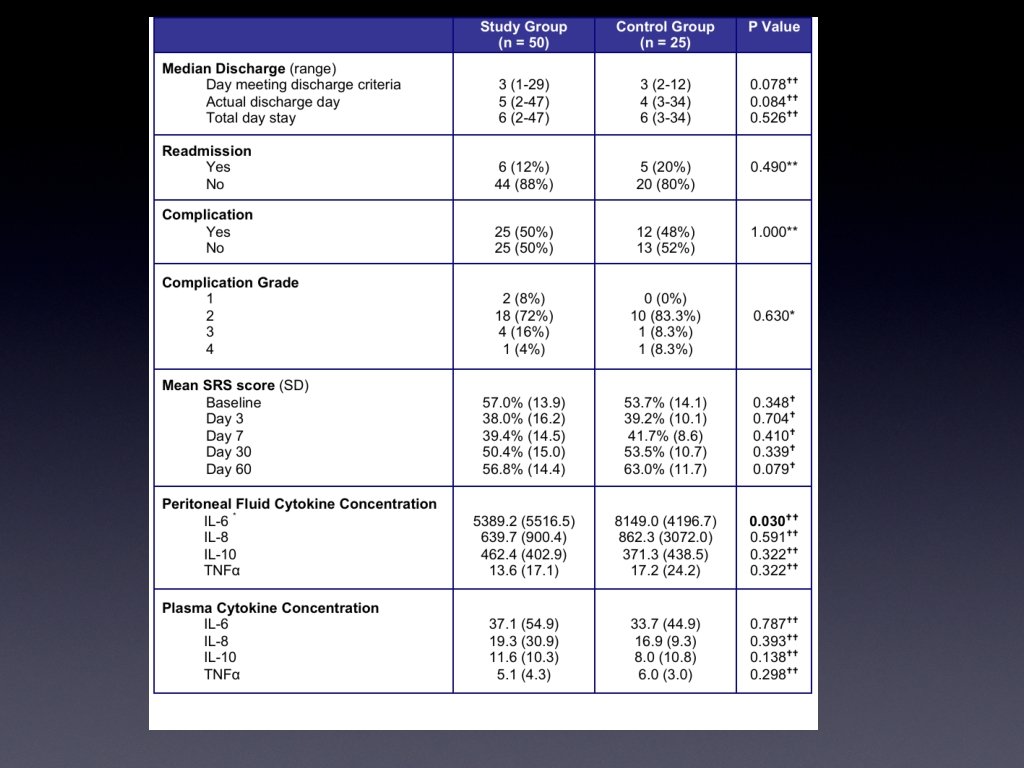
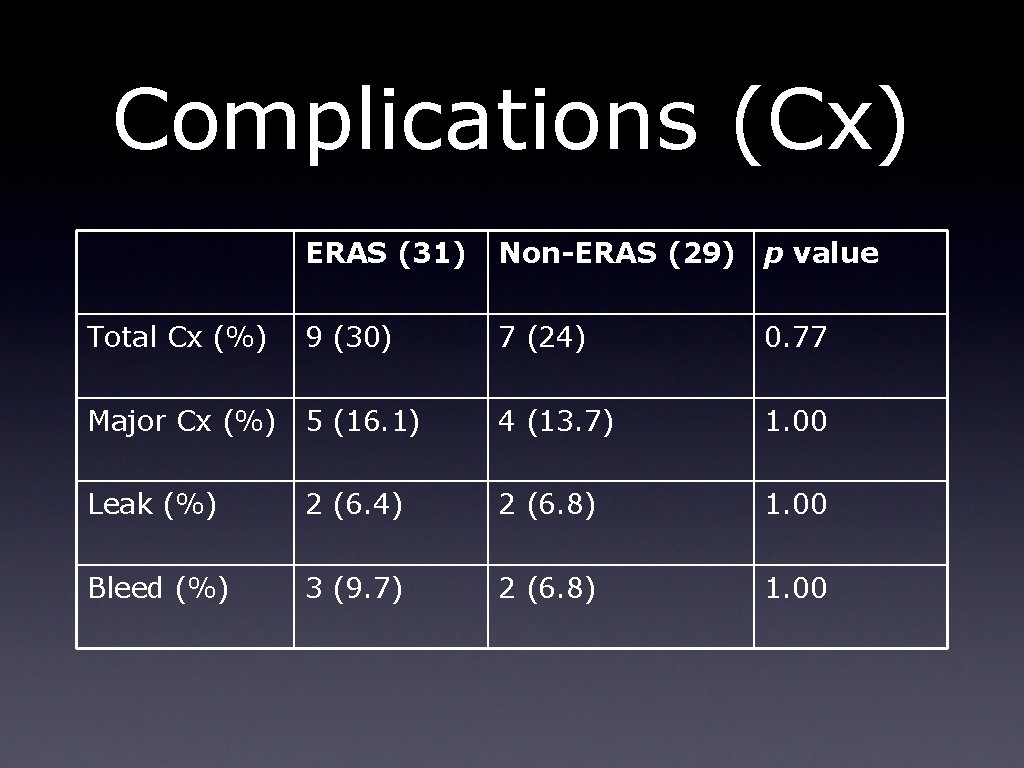
Complications (Cx) ERAS (31) Non-ERAS (29) p value 9 (30) 7 (24) 0. 77 Major Cx (%) 5 (16. 1) 4 (13. 7) 1. 00 Leak (%) 2 (6. 4) 2 (6. 8) 1. 00 Bleed (%) 3 (9. 7) 2 (6. 8) 1. 00 Total Cx (%)
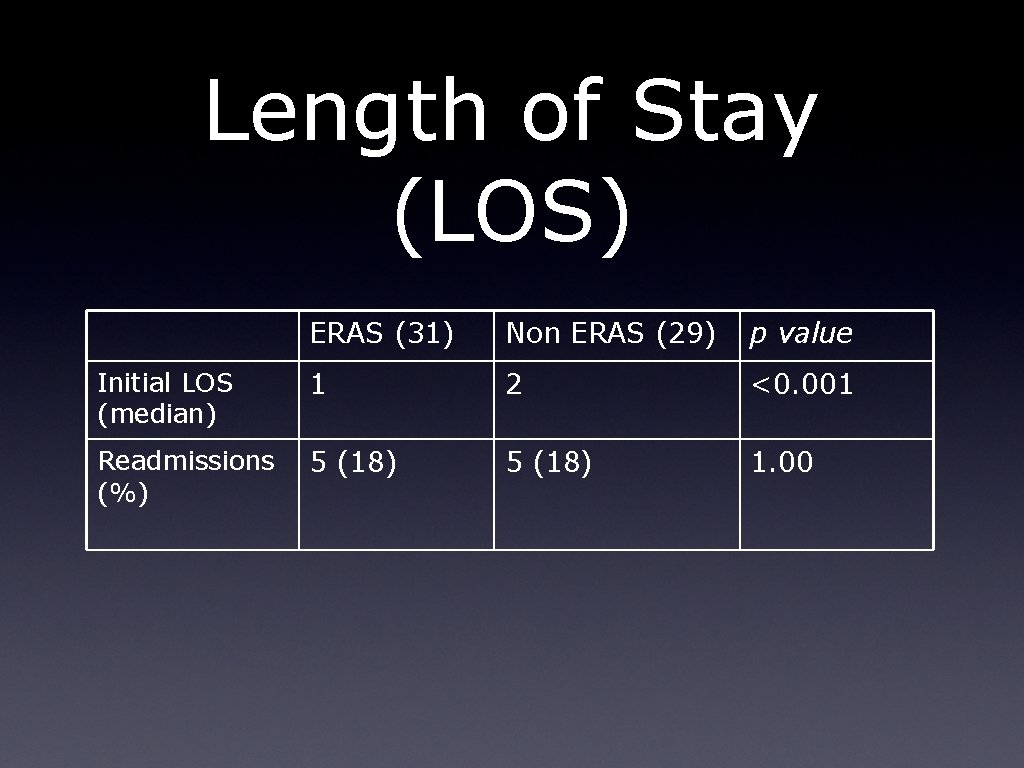
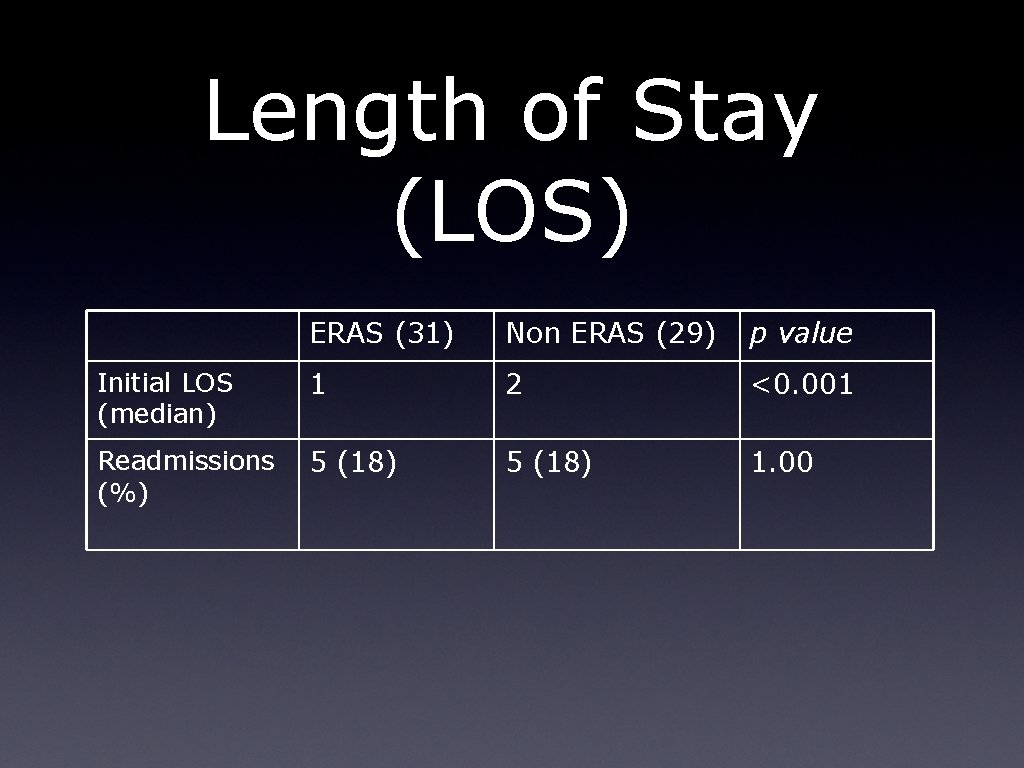
Length of Stay (LOS) ERAS (31) Non ERAS (29) p value Initial LOS (median) 1 2 <0. 001 Readmissions (%) 5 (18) 1. 00
Conclusion ERAS is possible in a New Zealand public hospital. ERAS is safe in a New Zealand Hospital ERAS enhances recovery in a New Zealand Hospital ERAS is cost-effective in a New Zealand Hospital ERAS is more than just Colorectal Surgery