Endotracheal IntubationExtubati on 1 Upper Airway Anatomy p
Endotracheal Intubation/Extubati on 1
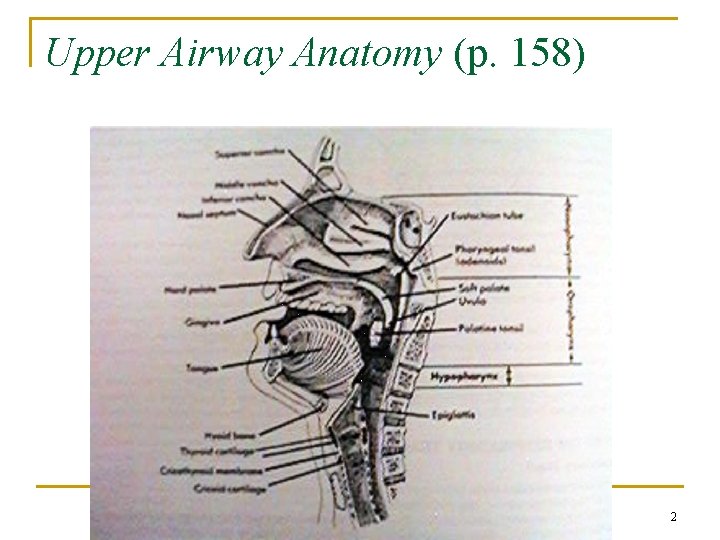
Upper Airway Anatomy (p. 158) 2
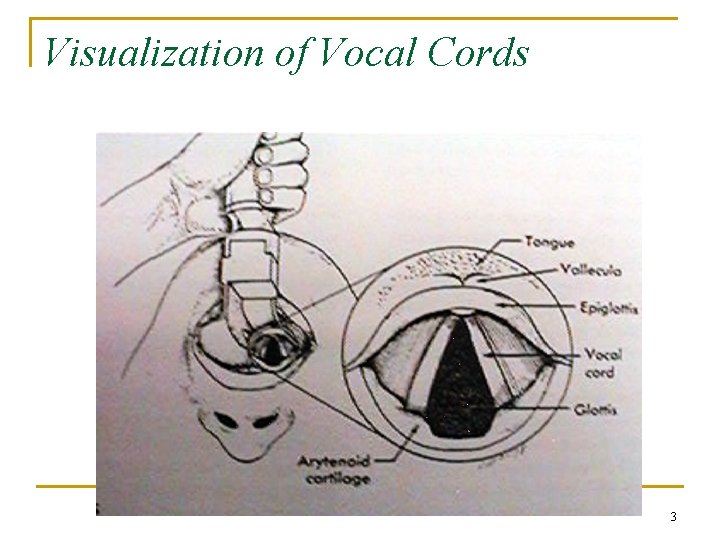
Visualization of Vocal Cords 3
Indications for Intubation n In conditions of, or leading to resp. failure, such as; - trauma to the chest or airway neurologic involvement from drugs myasthenia gravis, poisons, etc. -CV involvement leading to CNS impairment from strokes, tumors, infection, pulmonary emboli -CP arrest 4
Indications (cont’d) n n n Relief of airway obstruction Protection of airway (I. e. seizures) Evacuation of secretions by tracheal aspiration Prevention of aspiration Facilitation of positive press. ventilation 5
Relieving Airway Obstruction n Obstruction classified as upper ( above the glottis and includes the areas of the nasopharynx, oropharynx, and larynx) or lower (below the vocal cords) Can also be classified as partial or complete obstruction Causes include trauma, edema, tumors, changes in muscle tone or tissue support 6
Hazards of tracheal tubes & cuffs n n n Infection Trauma Dehydration Obstruction Trauma 7
Hazards (cont’d) n n n Accidental intubation of the esophagus or right mainstem bronchus Bronchospasm, laryngospasm Cardiac arrhythmias resulting from stimulation of the vagus nerve Aspiration pneumonia Broken or loosened teeth 8
Later Complications of Intubation n n Paralysis of the tongue Ulcerations of the mouth Paralysis of the vocal cords Tissue stenosis and necrosis of the trachea 9
Routes for Intubation n Orotracheal Nasotracheal Tracheotomy 10
Oral Intubation 11
Advantages of Oral Intubation n n Larger tube can be inserted Tube can be inserted usually with more speed and ease with less trauma Easier suctioning Less airflow resistance Reduced risk of tube kinking 12
Disadvantages of Oral Intubation n n Gagging, coughing, salivation, and irritation can be induced with intact airway reflexes Tube fixation is difficult, self-extubation Gastric distention from frequent swallowing of air Mucosal irritation and ulcerations of mouth (change tube position) 13
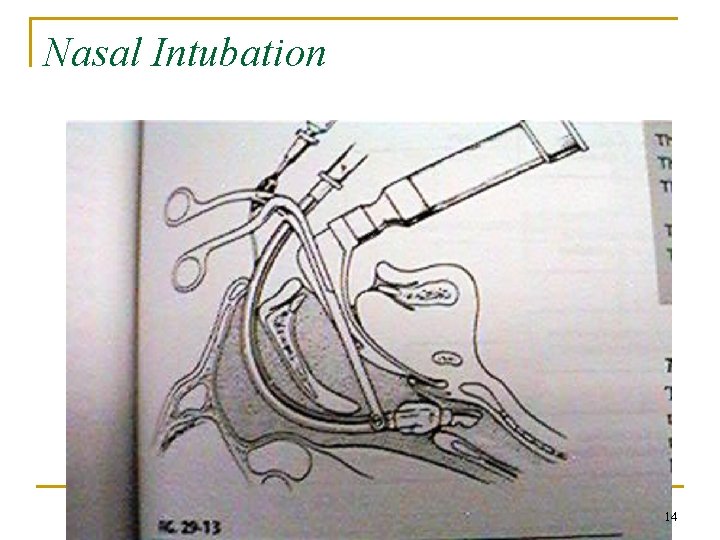
Nasal Intubation 14
Advantages of Nasal Intubation n n n More comfort long term Decreased gagging Less salivation, easier to swallow Improved mouth care Better tube fixation Improved communication 15
Disadvantages of Nasal Intub. n n n n Pain and discomfort Nasal and paranasal complications, I. e. , epistaxis, sinusitis, otits More difficult procedure Smaller tube needed Increased airflow resistance Difficult suctioning Bacteremia 16
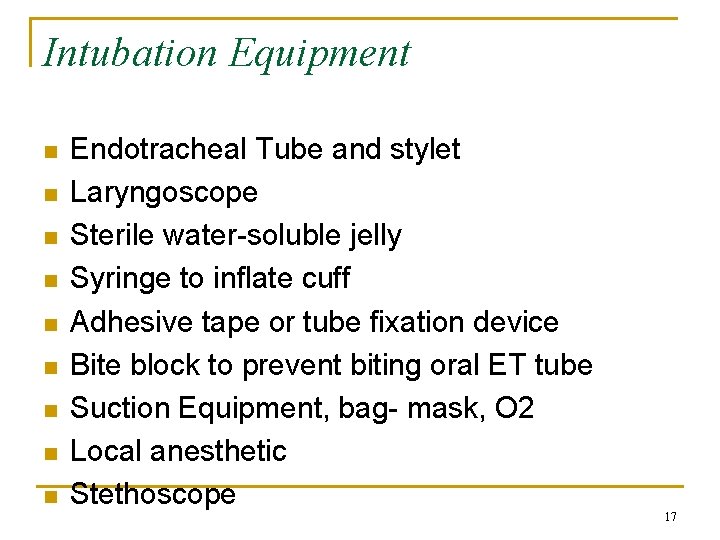
Intubation Equipment n n n n n Endotracheal Tube and stylet Laryngoscope Sterile water-soluble jelly Syringe to inflate cuff Adhesive tape or tube fixation device Bite block to prevent biting oral ET tube Suction Equipment, bag- mask, O 2 Local anesthetic Stethoscope 17
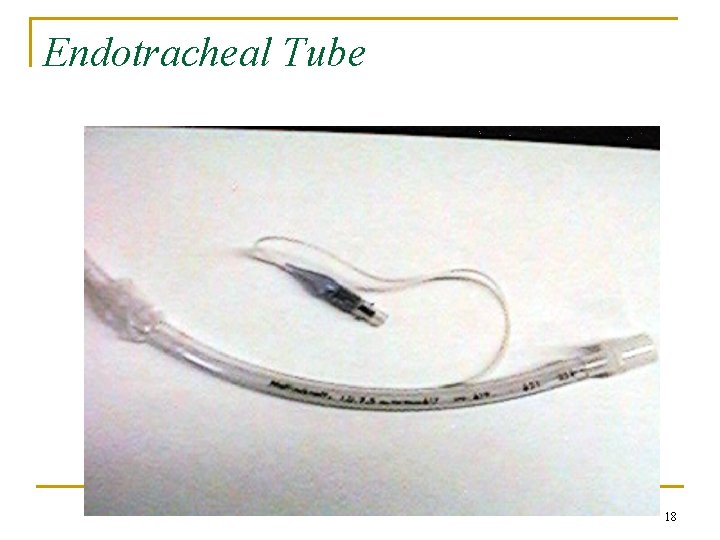
Endotracheal Tube 18
Endotracheal Tube n n n ET tube size and depth of insertion (see p. 594) For children older than 2 years - tube size = age/4 + 4 - depth = age/2 + 12 Adult - tube size female = 8. 0, male = 9. 0 - depth female = 19 -21 and 24 -26 male = 21 -23 and 26 -28 19
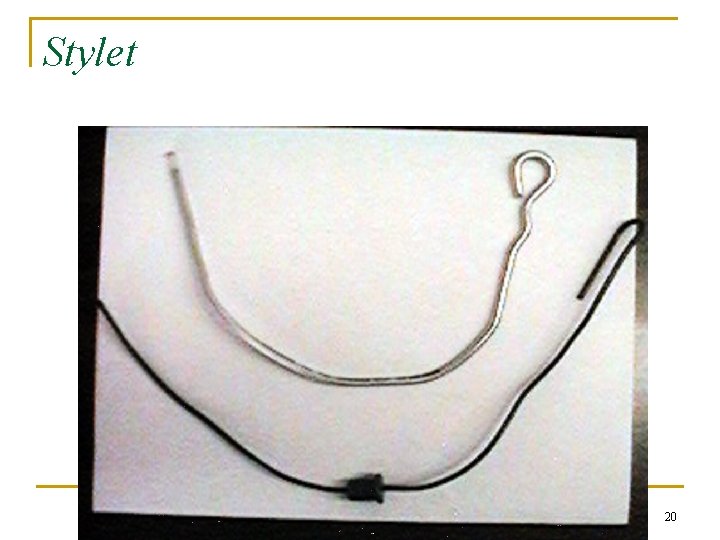
Stylet 20
Light stylet (light wand) 21

Laryngoscope 22
Laryngoscope n n Blade and handle Blade - has a flange, spatula, light, and tip curved blade (Macintosh) straight blade (Miller, Wisconsin) Fiber optic vs. traditional laryngoscope Blade size: 0 - 1 infant, 2 from 2 -8 years 3 from age 10 - adult, 4 large adult 23
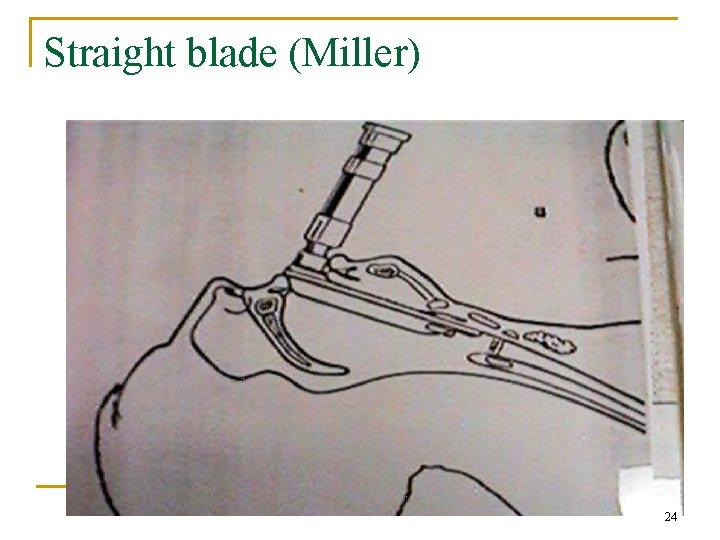
Straight blade (Miller) 24
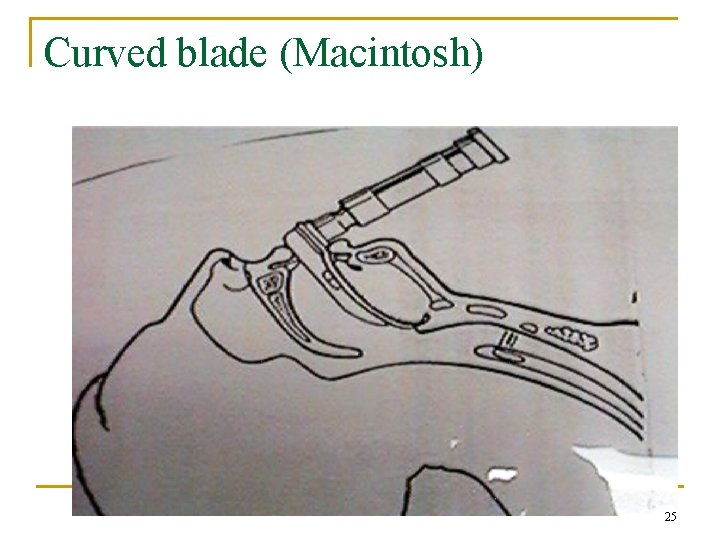
Curved blade (Macintosh) 25
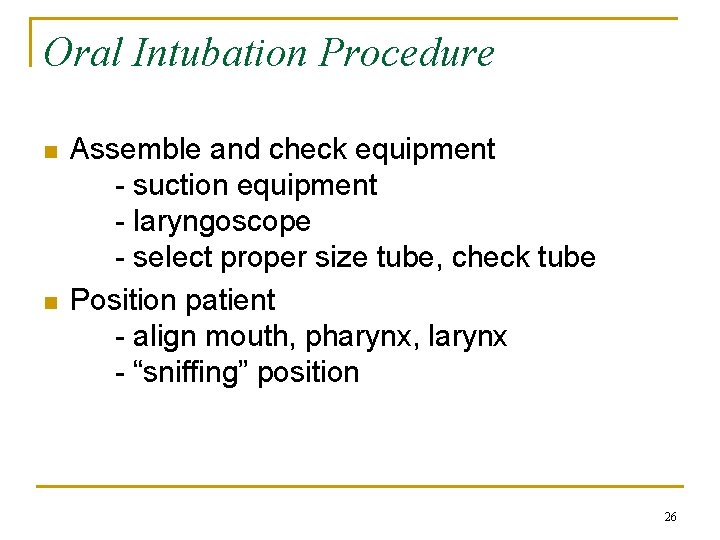
Oral Intubation Procedure n n Assemble and check equipment - suction equipment - laryngoscope - select proper size tube, check tube Position patient - align mouth, pharynx, larynx - “sniffing” position 26
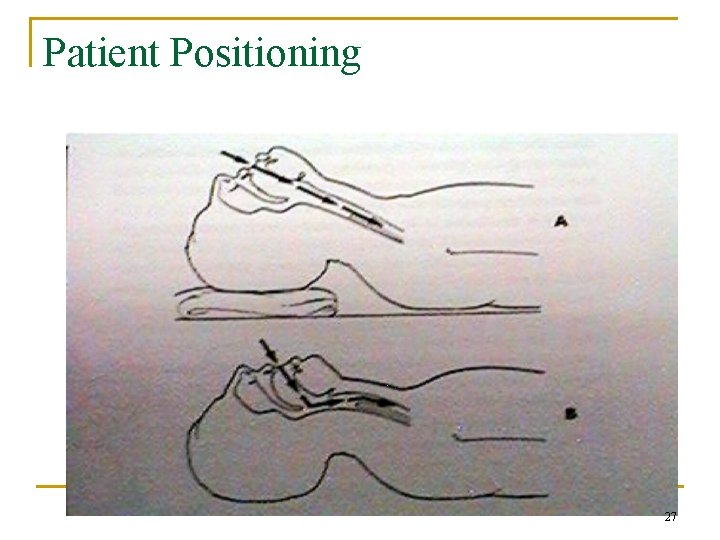
Patient Positioning 27
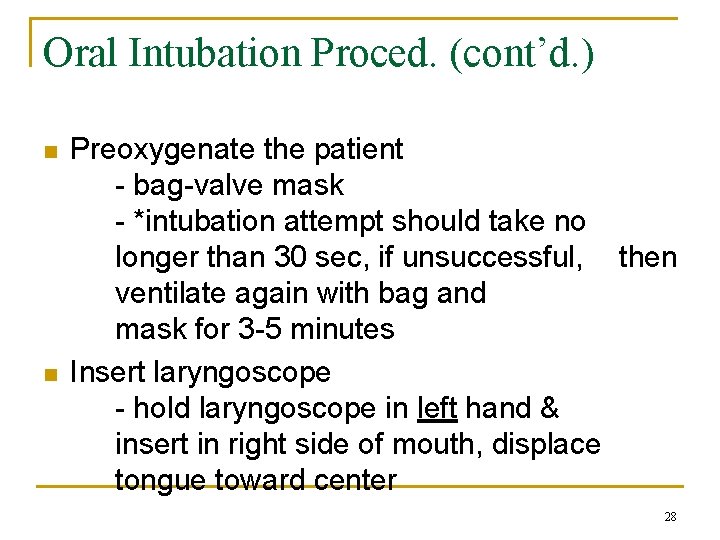
Oral Intubation Proced. (cont’d. ) n n Preoxygenate the patient - bag-valve mask - *intubation attempt should take no longer than 30 sec, if unsuccessful, then ventilate again with bag and mask for 3 -5 minutes Insert laryngoscope - hold laryngoscope in left hand & insert in right side of mouth, displace tongue toward center 28
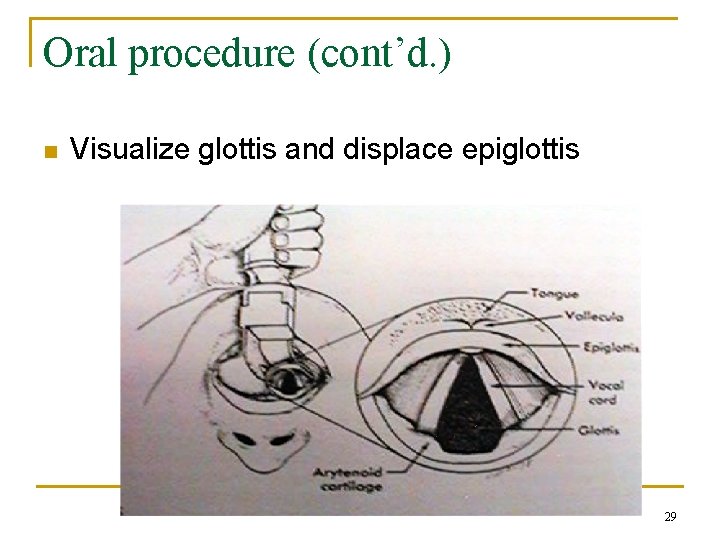
Oral procedure (cont’d. ) n Visualize glottis and displace epiglottis 29
Oral proced. (cont’d. ) n n Insert ET tube - do not use laryngoscope blade to guide tube once you see the tube pass the glottis, advance the cuff passed the cords by 2 -3 cm Hold tube with right hand remove laryngoscope & stylet - inflate cuff with 5 - 10 cc of air - ventilate with bag 30
Oral proced. (cont’d) n n Inflate cuff with 5 - 10 cc of air Ventilate with “bag” Assess tube position - auscultation of chest & epigastric - cm mark at teeth - capnometry/colorimetry - light “wand” Stabilize tube/Confirm placement - chest x-ray 31
Extubation n n Guidelines for extubation (see table, p. 613) Cuff-leak test 32
Extubation Procedure n n Assemble Equipment - intubation equipment - in addition to intubation equipment, O 2 device and humidity, SVN with racemic epi Suction ET tube Oxygenate patient Unsecure tube, deflate cuff 33
Extubation proced. (cont’d. ) n n n Place suction catheter down tube and remove ET tube as you suction Apply appropriate O 2 and humidity Assess/Reassess the patient 34
- Slides: 34