ENDOMETRIOSIS Clinical diagnosis The clinical symptoms of endometriosis

- Slides: 25
ENDOMETRIOSIS

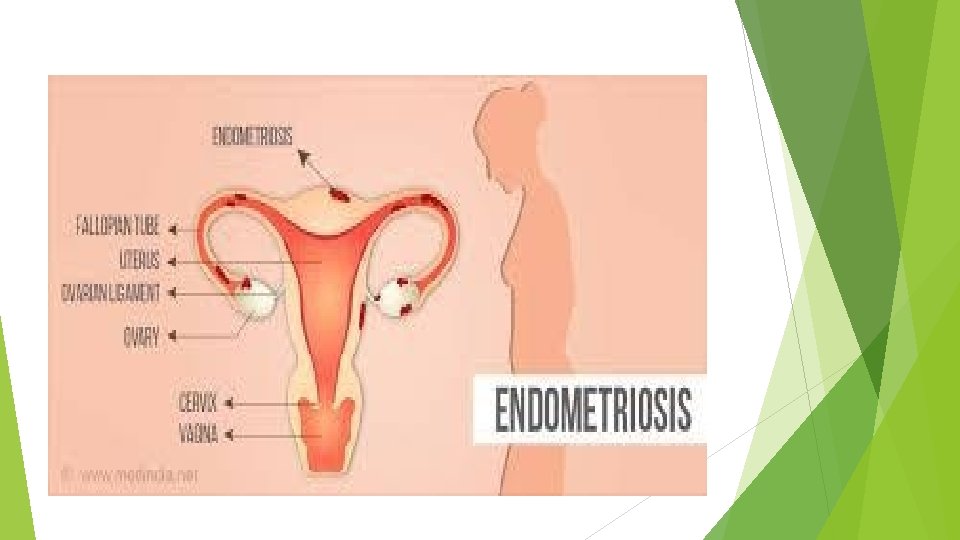
Clinical diagnosis
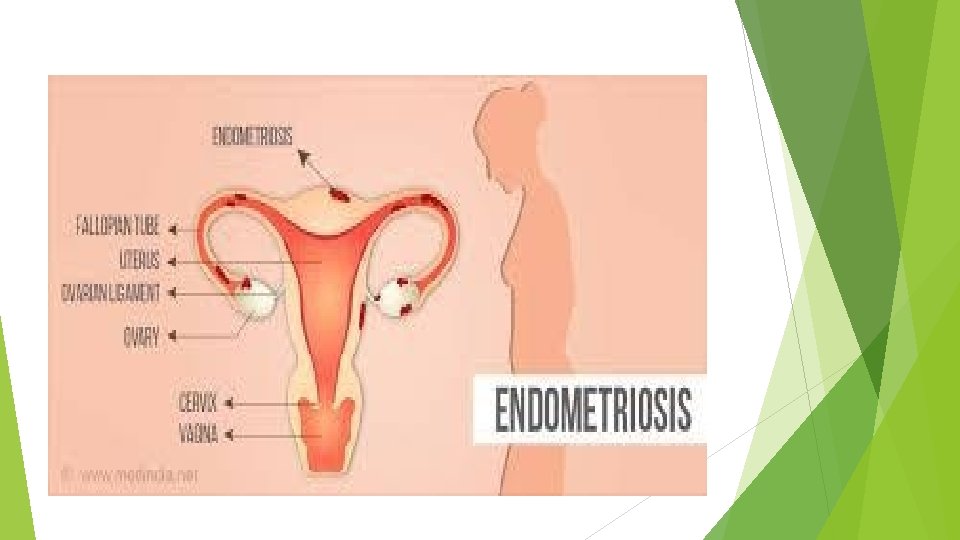
The clinical symptoms of endometriosis include dysmenorrhea, pain, dyspareunia, cyclic bowel or bladder symptoms, subfertility, abnormal bleeding, and chronic fatigue. They also reveal that endometriosis can coexist with or be misdiagnosed as irritable bowel syndrome or pelvic inflammatory disease. It is not surprising that diagnosis can be delayed, often for a period of years. The dysmenorrhea associated with endometriosis often begins before onset of menstrual flow and usually persists throughout menses, sometimes even beyond. The pain usually is diffuse, located deep in the pelvis, dull and aching, and may radiate to the back and thighs or be associated with rectal pressure, nausea, and episodic diarrhea. Pain may be more common, severe, and associated with dyspareunia and painful defecation in women with deeply infiltrating disease involving the cul-de-sac and rectovaginal septum
Physical findings in women with endometriosis vary widely and, when present, relate to the location and extent of disease. The extemal genitalia are typically normal. Occasionally, speculum examination may reveal characteristic blue-colored implants or red prolirerative lesions that bleed on contact, both usually in the posterior fornix. The uterus often is retroverted and can exhibit decreased mobility or fixation. Women with ovarian endometriomas can have a tender, fixed, adnexal mass. Focal tendemess, thickening, induration, and nodularity of the uterosacral ligaments are the most common, and frequently the only, physical finding
CA-125 Levels of CA-125 often are elevated in women with advanced endometriosis, but also during early pregnancy and normal menstruation, and in women with acute pelvic inflammatory disease or leiomyomata. Overall, the serum CA-125 concentration does nor have the necessary sensitivity to be an effective screen ing fest for the diagnosis of endometriosis. Whereas the serum CA-125 generally is not a reliable predictor of the effectiveness of medical therapy, a sustained elevation of serum CA-125 after surgical treatment predicts a relatively poor prognosis.
Imaging Like transvaginal ultrasonography, magnetic resonance imaging (MRI) can be helpful for detection and differentiation of ovarian endometriomras from other cystic ovarian masses, but cannot reliably image small peritoneal lesions. For detection of peritoneal implants, MRI is superior to transvaginal ultrasonography but still identifies only 30 -40% of the lesions observed at surgery. For detection of disease documented by histopathology, MRI is approximately 70% sensitive and 75% specific.
Diagnosis by therapeutic trial A trial of treatment with a nonsteroidal anti-inflammatory drug (NSAID), ideally combined with an estrogen/progestin or progestin only contraceptive, is reasonable when the symptoms The results of the study demonstrate the diagnostic accuracy of rigorous clinical criteria and the efficacy of empiric lenprolide treatment in women with chronic pelvic pain, but do not support the conclusion thar the clinical response to treatment has diagnostic value.
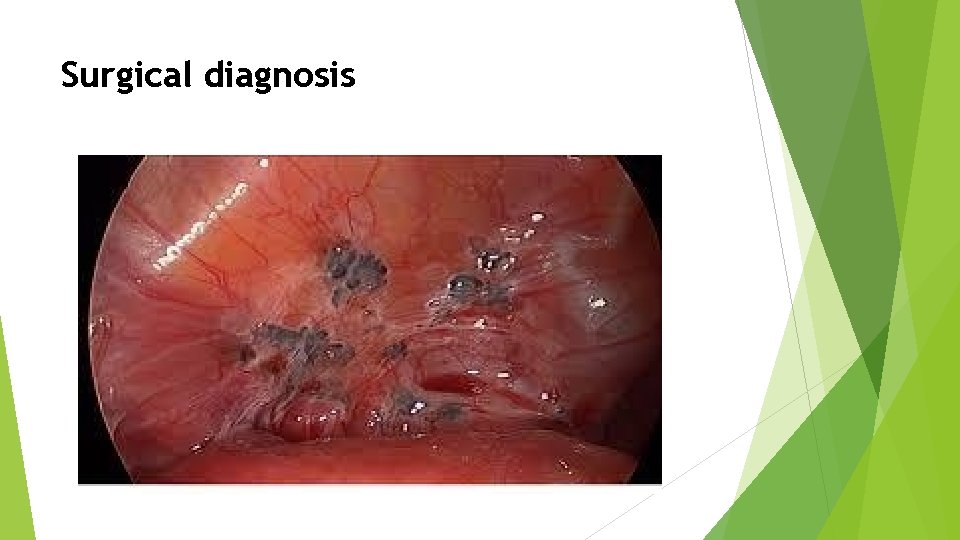
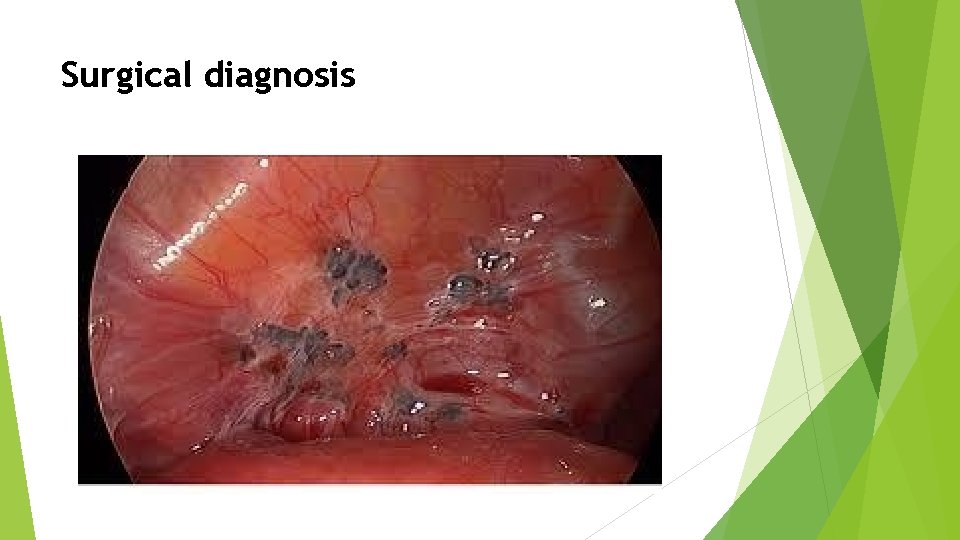
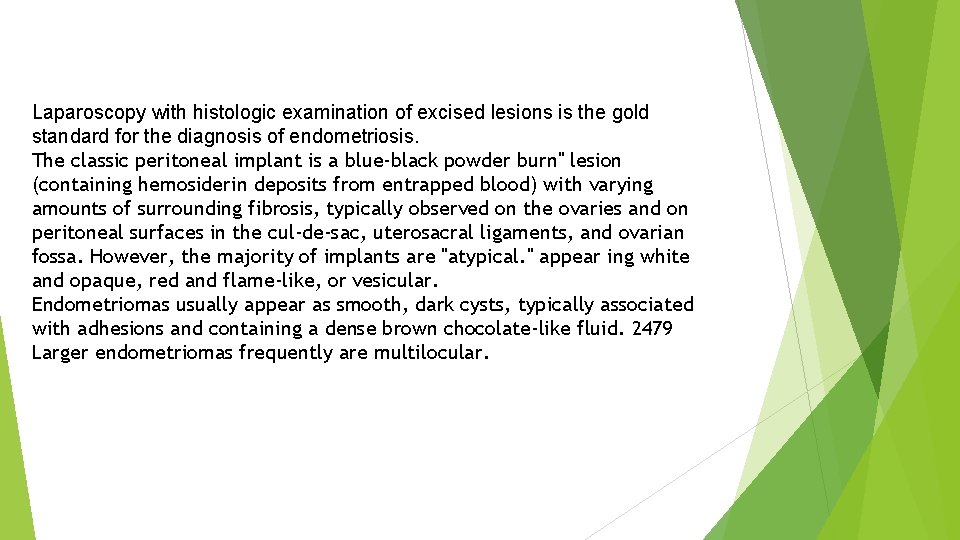
Surgical diagnosis
Laparoscopy with histologic examination of excised lesions is the gold standard for the diagnosis of endometriosis. The classic peritoneal implant is a blue-black powder burn" lesion (containing hemosiderin deposits from entrapped blood) with varying amounts of surrounding fibrosis, typically observed on the ovaries and on peritoneal surfaces in the cul-de-sac, uterosacral ligaments, and ovarian fossa. However, the majority of implants are "atypical. " appear ing white and opaque, red and flame-like, or vesicular. Endometriomas usually appear as smooth, dark cysts, typically associated with adhesions and containing a dense brown chocolate-like fluid. 2479 Larger endometriomas frequently are multilocular.
Classification and staging system • Minimal endometriosis - isolated superficial disease on the peritoneal surface with no significant associated adhesions. • Mild endometriosis - scattered superficial disease on the peritoneal surface and ovaries, totaling less than 5 cm in aggregate, with no significant associated adhesions. • Moderate endometriosis multifocal disease, both superficial and invasive, that may be associated with adhesions involving the fallopian tubes and/or the ovaries • Severe endometriosis multifocal disease, both superficial and invasive, including large ovarian endometriomas, usually associated with adhesions, both filmy and dense, involving the fallopian tubes, ovaries, and cul-de-sac.
Medical Treatment Women with pelvic pain, suspected endometriosis, and no other indication for surgical treatment can be managed effectively with empiric medical treatment without establishing a surgical diagnosis. keeping in mind that a response to treatment does not establish the diagnosis of endometriosis. Empiric medical therapy may involve treatment with nonsteroidal antiinflammatory drugs (NSAIDs) or estrogen-progestin contraceptives for women with mild symptoms, or with a gonadotropin-releasing hormone (Gn. RH) agonist for those with moderate or severe pelvic pain.
Estrogen-Progestin Contraceptives Estrogen-progestin contraceptives, taken in a cyclic or continuous fashion, have been a mainstay of the medical treatment of symptomatic endometriosis. Estrogen-progestin contraceptives are a good initial choice for women with mild symp. toms who also need contraception. They can be expected to provide effective relief from pain associated with endometriosis in 75 -90% of affected women, particularly when taken continuously. They also might help to prevent progression of endometriosis.
Progestins Medroxyprogesterone acetate can be administered orally (20 -100 mg daily) or by injection (150 mg i. m. every 3 months). Side effects include nausea, weight gain, fluid retention, breast tenderness, irregular bleeding, and depression. Breakthrough bleeding is common (35 -50%) but generally well tolerated and usually can be eliminated by treatment with short courses of supplemental estrogen (conjugated estrogens 1. 25 mg or estradiol 2. 0 mg daily for 7 -10 days). Although progestins are effective treatment for pain associated with endometriosis, their adverse effects on fertility limit their utility in infertile women seeking pregnancy.
Gonadotropin-Releasing Hormone Agonists Long-acting Gn. RH agonists (leuprolide, nafarelin, goserelin, buscrelin, triptorelin) have the same effect. inducing a hypogonadotropic hypogonadal state that has been dubbed "pseudomenopause" or "medical oophorectomy, " although both terms are misnomers. After discontinuation of treatment, bone loss is slowly recovered, but not completely in all women. In efforts to prevent the bone mineral depletion that accompanies Gn. RH agonist therapy. a number of different "add-back" treatment strategies have been developed. Low-dose combined estrogen-progestin add-back regimens (conjugated estrogens 0. 625 mg and medroxyprogesterone acetate 2. 5 mg daily or norethindrone 5. 0 mg daily) are based on the notion that the level of estrogen required to support endometriosis is greater than is required to prevent vasomotor symptoms or bone mineral depletion. Results achieved with low-dose combined estrogen-progestin add-back regimens support this "estrogen threshold hypothesis
. Gonadotropin-Releasing Hormone Agonists However, estrogen-only add-back is inadvisable; a clinical trial (oral estradiol, 1 mg daily) was terminated early due to observations of recurrent pain in treated subjects Numerous other add-back regimens have been described, including progestins alone (norethindrone 2. 5 5 mg daily)'tibolone (2. 5 mg daily). bisphonates (cyclic ctidronate 400 mg daily for 2 weeks every 2 months: alendronate 10 mg daily), and the selective estrogen receptor modulator, raloxifene (60 mg daily). Combined estrogenprogestin add-back treatment regimers prefect bone and have the added advantage of preventing hur flushes and the development of genitourinary afrophy. Progestin only add-back regimens have been less consistently effective.
Danazol is the first drig ever approved for the treatment of endometriosis in the U. S. The amenorrhea that commonly results from danazol treatment also decreases new peritoneal seeding. Although danazol is effective for the treatment of pain associated with endometriosis, the recommended doses (400 -800 mg daily) have substantial androgenic and hypeestrogenic side effects that limir its clinical utility. The most common are weight gain, fluid retention, fatigue, decreased breast size, acne, oily skin, hirsutism, atrophic vaginitis, hot flushes, muscle cramps, and emotional lability.
Aromatase Inhibitors Although not approved for the treatment of endometriosis, aromatase inhibitors offer a new and promising approach to management of the disease. 14. Aromatase inhibitors effectively suppress estrogen production in the periphery (e. g. , brain, adipose) and in endometriotic tissues, as well as in the ovary. In numerous case reports and small series, aromatase inhibitors (anastrozole 1 mg daily, letrozole 2. 5 mg daily) have been found effective for the management of pain associated with endometriosis. Aromatase inhibitors can be expected to cause significant bone loss with prolonged use and cannot be used alone in premenopausal women because they stimulate FSH release, causing development of multiple ovarian cysts. To avoid the complication, they must be used in combination with a Gn. RH agonist or norethindrone acetate (5 mg daily) in premenopausal women.
Surgical Treatment The objectives of surgical treatment for endometriosis are to restore normal anatomical relationships, to excise or destroy all visible disease to the extent possible, and to prevent or delay recurrence. For women having moderate or severe endometriosis that distorts the reproductive anatomy and hoping to restore or preserve fertility, surgery is the treatment of choice because medical treatment cannot achieve the goal. When disease is less severe, medical treatment can effectively control pain in the large majority of women but has no effect on fertility: surgery is at least as effective as medical treatment for relieving pain and also may improve fertility,
Minimal and Mild Disease Peritoneal implants of endometriosis may be ablated with unipolar or bipolar electrosurgical instruments or lasers, or excised by sharp dissection. Unfortunately, as with medical treatment recurrent disease and pain after local excision or ablation of endometriosis are common symptoms recur in at least 10 -20% of treated women per year. The results suggest that approximately nine infertile women with minimal or mild endometriosis must undergo surgical treatment to achieve one additional pregnancy, a small bur potentially important effect.
Moderate and Severe Disease The optimum surgical management of ovarian endometriomas is somewhat controversial. Endometriosis have been treated by wedge resection, enucleation (stripping), and by drainage with and without ablation of the internal cyst wall. In women with advanced symptomatic endometriosis who have completed childbearing and those in whom medical and conservative surgical treatment fails, definitive surgical treatment deserves serious consideration.
Adjuvant Procedures Adjuvant presacral neurectomy and laparoscopic uterosacral nerve ablation (LUNA) have heen advocated for the management of dysmenorrhea and severe central pelvic pain unresponsive to medical or previous surgical treatment for endometriosis. Considering their uncertain benefits and potential risks, routine presacral neurectomy or LUNA at time of conservative surgery for endometriosis cannot be recommended, both procedures should be reserved for highly selected individuals, who must be counseled very carefully.
Pre- and Post-operative Medical Treatments Some advocate preoperative medical treatment with a Gn. RH agonist, believing it may offer certain advantages, including a decrease in the volume of disease requiring surgical treatment, elimination of functional ovarian cysts that may pose technical problems, greater convenience of surgical scheduling, and a better overall outcome. Postoperative medical suppressive therapy also has been controversial. Whereas some studies have observed a longer pain-free interval or higher pregnancy rates when surgical treatment is followed by an interval of medical treatment with a Gn. RH agonist, danazol, progestins, 17 or estrogen-progestin contraceptives, others have found no differences between the prevalence of recurrent pain or pregnancy rates 1 -3 years after surgical treatment in women who did and did not receive postoperative medical treatment. Considering that the highest pregnancy rates after conservative surgery in infertile women generally are observed in the first year after operation, most clinicians have been reluctant to use medical treatment that will prevent pregnancy after surgical treatment. When the primary objective of surgical treatment for endometriosis is relief from pain and pregnancy is not an immediate goal, postoperative medical treatment may have value, particularly in women with extensive disease and those with residual disease than could not be completely excised,
After conservative surgical treatment of endometriosis in infertile women, a choice between expectant management and active treatment must consider age, the surgical results, and the influence and severity of any other infertility factors. Considering the modestly increased fecundability of women with minimal and mild endometriosis after surgical treatment, young women with limited disease and otherwise unexplained infertility of relatively short duration might be treated expectantly, but not for longer than 6 -9 months. A more aggressive approach involving immediate further empiric treatment with a combination of clomiphene citrate or exogenous gonadotropins and intrauterine insemination or even IVF is justified in those with longer durations of infertility or more advanced endometriosis, and in older women After radical surgery (hysterectomy and bilateral salpingo-oophorectomy) for persistent or recurrent endometriosis, hormone therapy can begin immediately in most women with neg. eligible risk of inducing growth of residual disease and recurrent symptoms. However, in those with extensive disease, an interval without hormone treatment or progestin-only treatment may be prudent. Progestins may have value both for their direct suppressive effects on any residual foci of endometriosis and for alleviating the otherwise inevitable vasomotor symptoms that accompany removal of the ovaries, Low-dose combined estrogen-progestin treatment is strongly recommended over treatment with estrogen alone, even though the uferus is absent, because the numerous reports of adenocarcinoma arising from endometriosis in women treated with unopposed estrogen cannot be ignored.