Endodontic Restoration of Endodontically Treated Teeth Part 1

- Slides: 18
Endodontic Restoration of Endodontically Treated Teeth Part 1
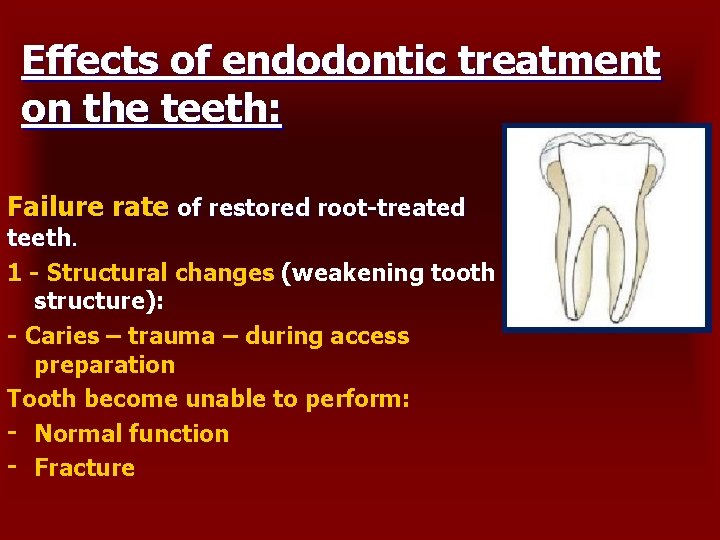
Effects of endodontic treatment on the teeth: Failure rate of restored root-treated teeth. 1 - Structural changes (weakening tooth structure): - Caries – trauma – during access preparation Tooth become unable to perform: - Normal function - Fracture
2 - Changes in dentin physical characteristic: • Irreversible changes + weakening. • Failure rate of restored RCT is higher. • Brittleness • Radicular dentin loose moisture than coronal dentin • Loose of moisture may due to aging , decrease of organic and increase in inorganic • Increase in the modulus of elasticity We should : Preserved useful remaining tooth structure Minimize stress within the tooth and restoration 3 - Esthetic consideration - Biochemical changes in dentin modify light reflection through the tooth - Incomplete clearing and shaping of root canal system - Sealer - Debris or filling left in the chamber
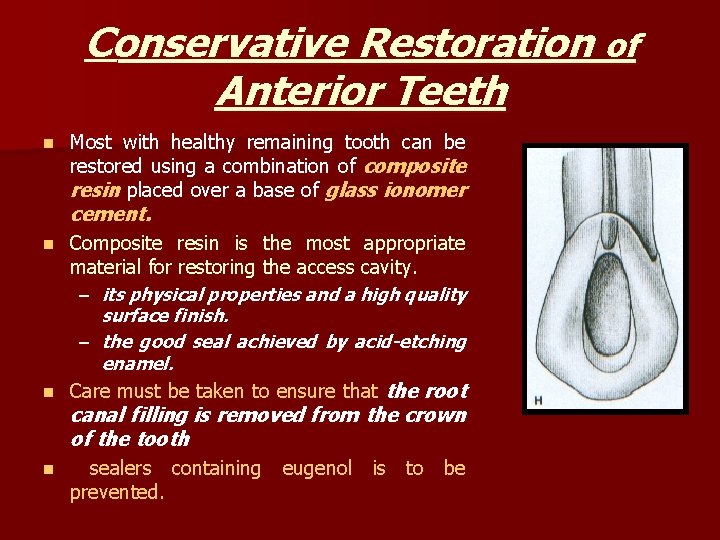
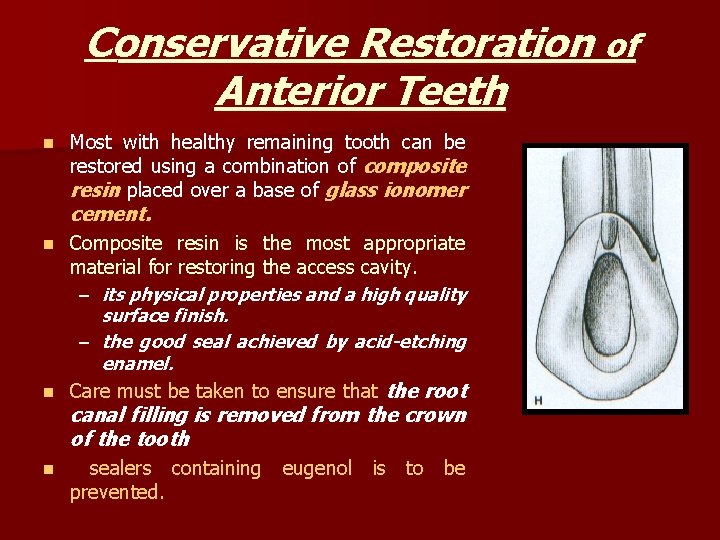
Conservative Restoration of Anterior Teeth n Most with healthy remaining tooth can be restored using a combination of composite resin placed over a base of glass ionomer cement. Composite resin is the most appropriate material for restoring the access cavity. – its physical properties and a high quality surface finish. – the good seal achieved by acid-etching enamel. n Care must be taken to ensure that the root n canal filling is removed from the crown of the tooth n sealers containing eugenol is to be prevented.
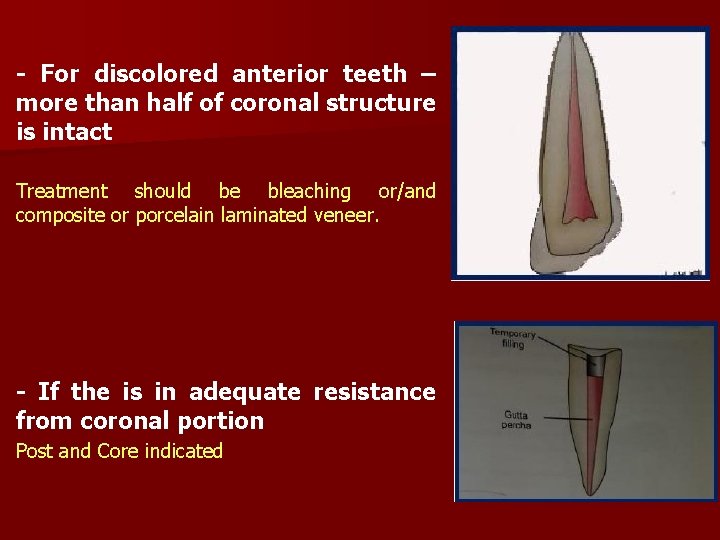
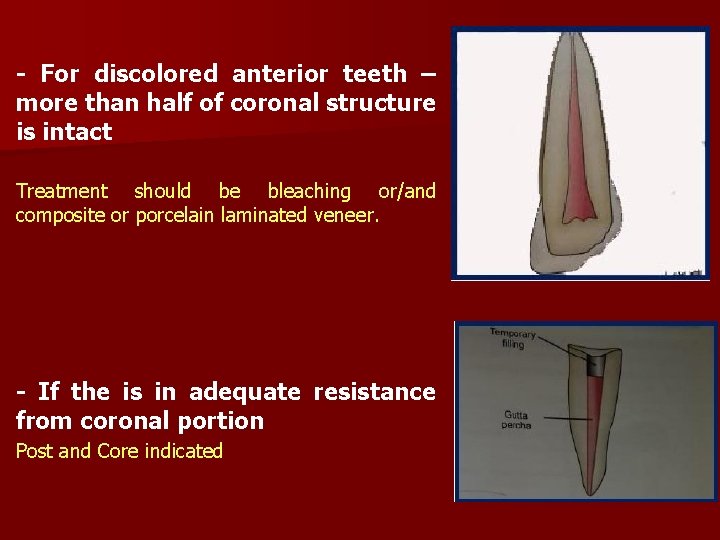
- For discolored anterior teeth – more than half of coronal structure is intact Treatment should be bleaching or/and composite or porcelain laminated veneer. - If the is in adequate resistance from coronal portion Post and Core indicated
Tooth Reinforcement? ? ? n There is no indication for the placement of a post within the root canal of intact anterior tooth. The idea that post reinforced tooth against fracture is untrue…. . Post provide retention for core n n With the increased range of adhesive techniques available for restoring anterior teeth. Give rise for the conservative approach to the restoration of even extensively damaged root-canal-treated anterior teeth.
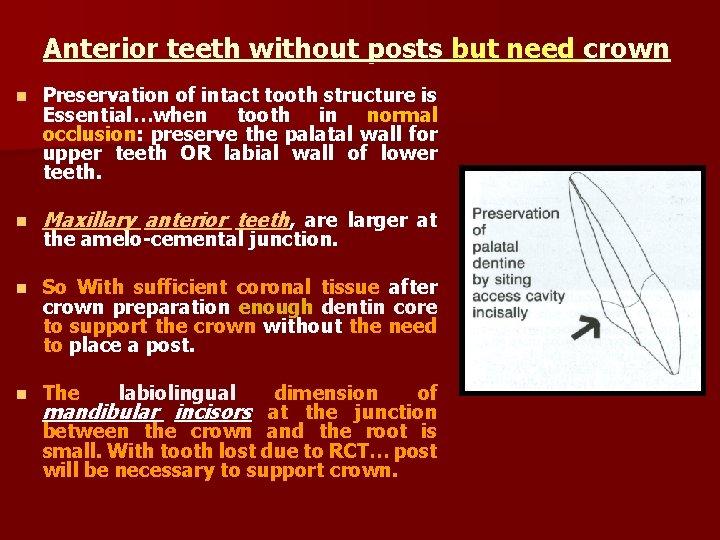
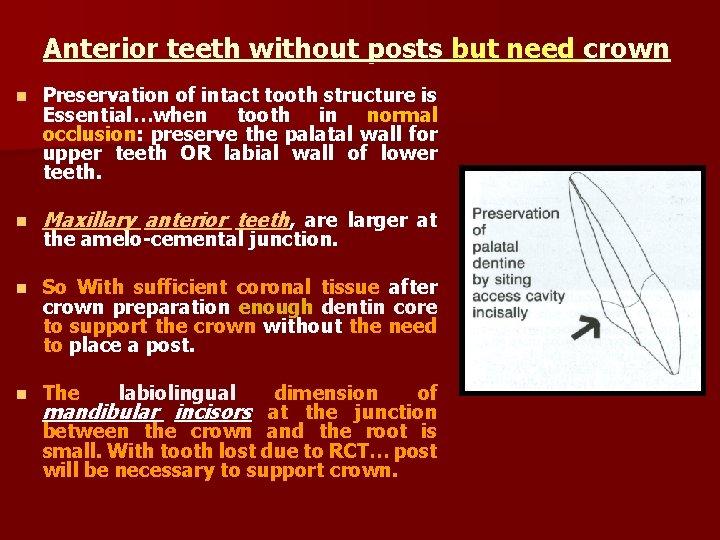
Anterior teeth without posts but need crown n Preservation of intact tooth structure is Essential…when tooth in normal occlusion: preserve the palatal wall for upper teeth OR labial wall of lower teeth. n Maxillary anterior teeth, are larger at n So With sufficient coronal tissue after crown preparation enough dentin core to support the crown without the need to place a post. n The the amelo-cemental junction. labiolingual dimension of mandibular incisors at the junction between the crown and the root is small. With tooth lost due to RCT… post will be necessary to support crown.
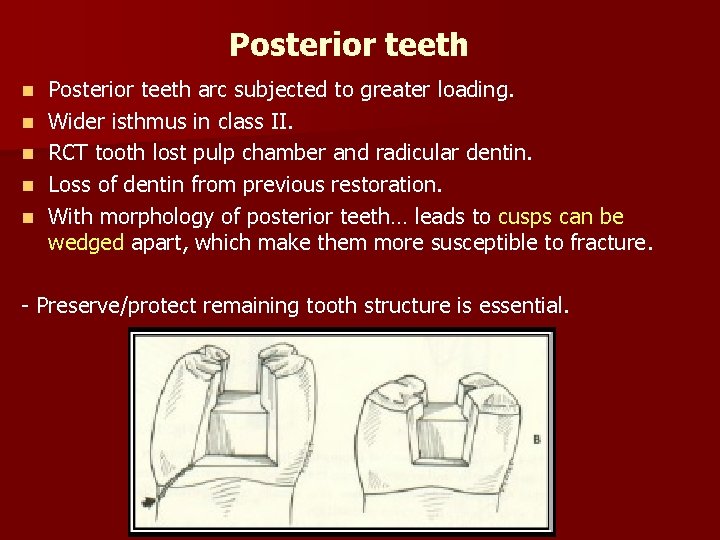
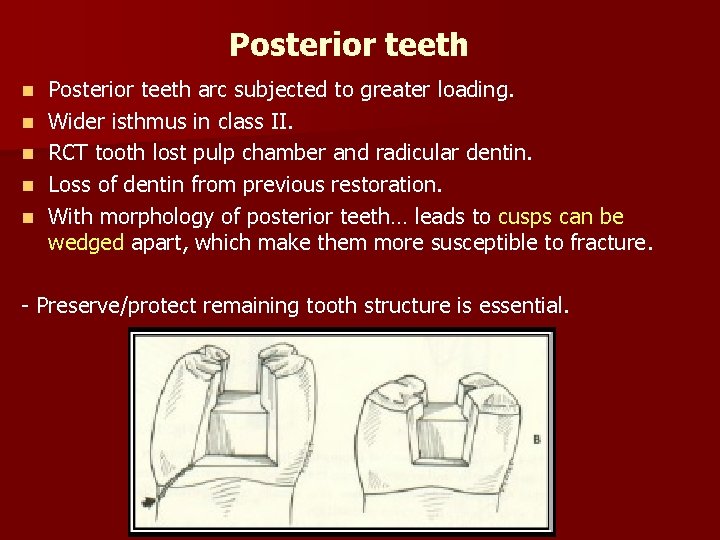
Posterior teeth n n n Posterior teeth arc subjected to greater loading. Wider isthmus in class II. RCT tooth lost pulp chamber and radicular dentin. Loss of dentin from previous restoration. With morphology of posterior teeth… leads to cusps can be wedged apart, which make them more susceptible to fracture. - Preserve/protect remaining tooth structure is essential.
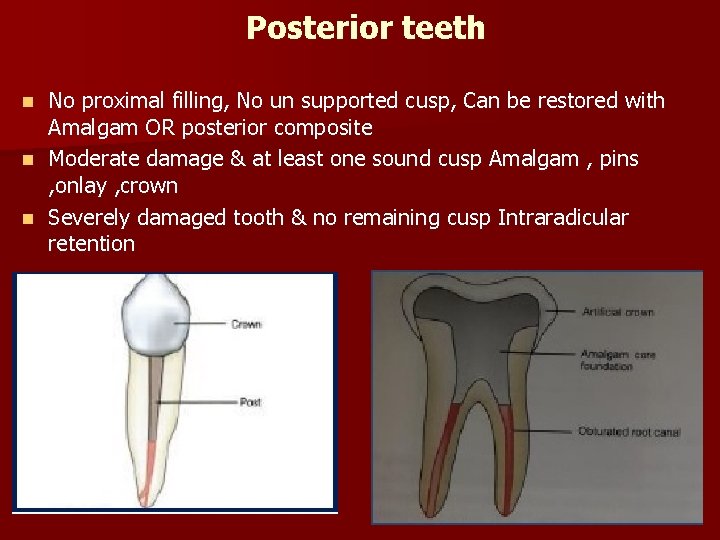
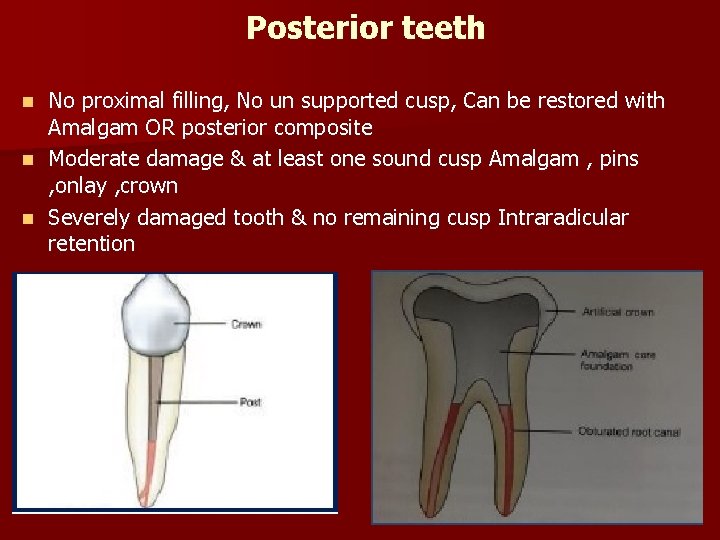
Posterior teeth No proximal filling, No un supported cusp, Can be restored with Amalgam OR posterior composite n Moderate damage & at least one sound cusp Amalgam , pins , onlay , crown n Severely damaged tooth & no remaining cusp Intraradicular retention n
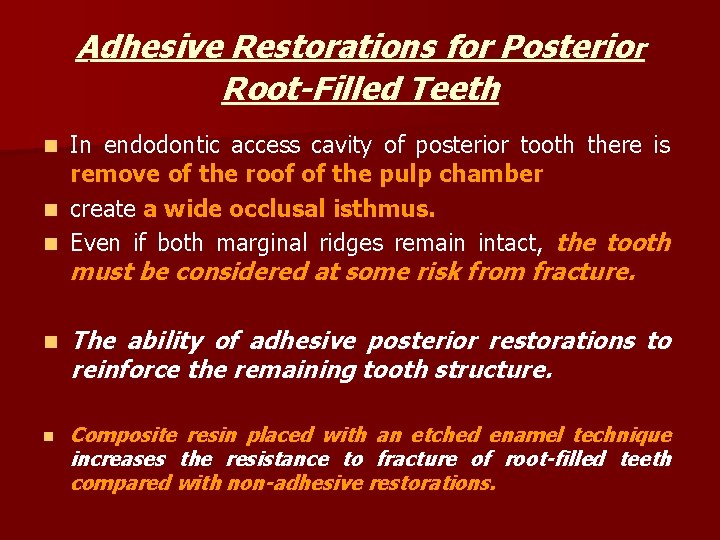
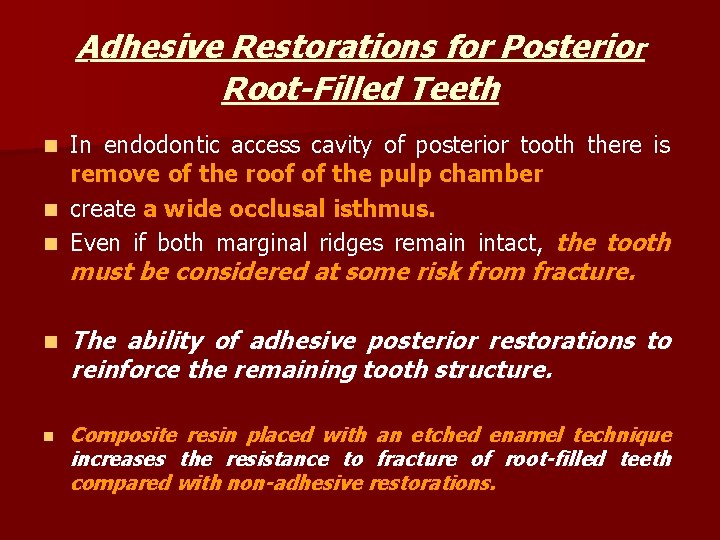
Adhesive Restorations for Posterior Root-Filled Teeth In endodontic access cavity of posterior tooth there is remove of the roof of the pulp chamber n create a wide occlusal isthmus. n Even if both marginal ridges remain intact, the tooth n must be considered at some risk from fracture. n The ability of adhesive posterior restorations to reinforce the remaining tooth structure. n Composite resin placed with an etched enamel technique increases the resistance to fracture of root-filled teeth compared with non-adhesive restorations.
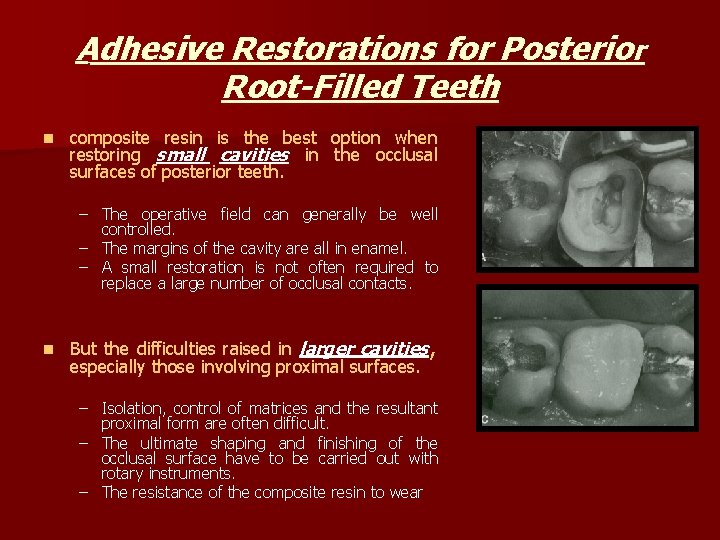
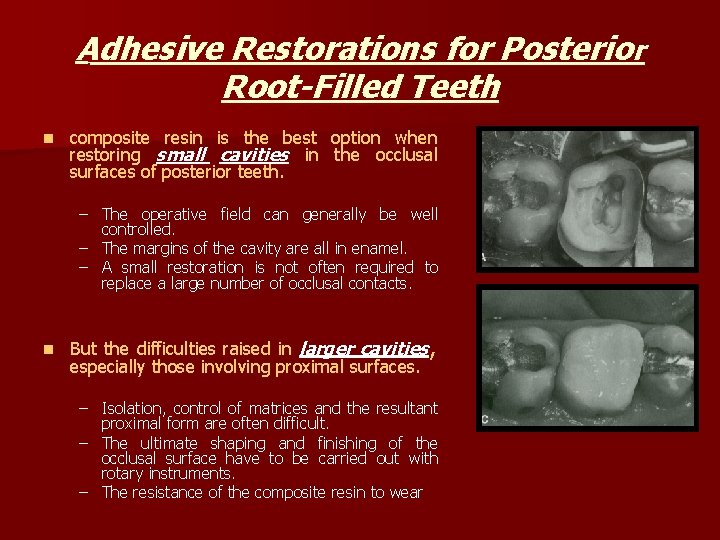
Adhesive Restorations for Posterior Root-Filled Teeth n composite resin is the best option when restoring small cavities in the occlusal surfaces of posterior teeth. – The operative field can generally be well controlled. – The margins of the cavity are all in enamel. – A small restoration is not often required to replace a large number of occlusal contacts. n But the difficulties raised in larger cavities, especially those involving proximal surfaces. – Isolation, control of matrices and the resultant proximal form are often difficult. – The ultimate shaping and finishing of the occlusal surface have to be carried out with rotary instruments. – The resistance of the composite resin to wear
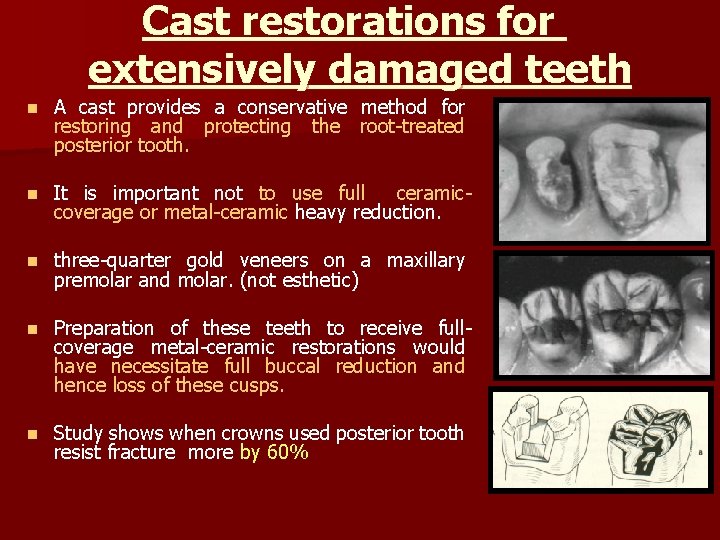
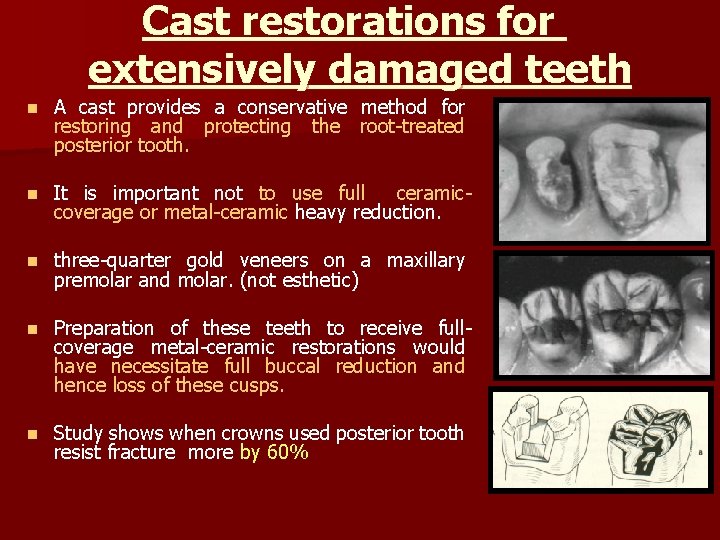
Cast restorations for extensively damaged teeth n A cast provides a conservative method for restoring and protecting the root-treated posterior tooth. n It is important not to use full ceramiccoverage or metal-ceramic heavy reduction. n three-quarter gold veneers on a maxillary premolar and molar. (not esthetic) n Preparation of these teeth to receive fullcoverage metal-ceramic restorations would have necessitate full buccal reduction and hence loss of these cusps. n Study shows when crowns used posterior tooth resist fracture more by 60%
Position of the Preparation Margin It is an important to distribute loads and minimize stress concentration, the margins of the final preparation should extend well onto sound tooth structure. n When different core use without crown fracture occur what ever core materials used n But when the margin placed 2 mm (ferrule effect) into sound tooth structure resistance increase with no difference what core material used. n This may sometimes a surgical crown-lengthening is done prior to crown preparation to provide visible tooth structure apical to the margins of the core. n
Timing the restorative procedure n How long to wait after root canal treatment before placing the final restoration? ? ? – There is no set answer to this and the following factors need to be considered. n Satisfactory final radiograph with the absence of symptoms, and the pulp had previously been vital; the final restoration can be proceeding immediately. In contrast, with n apical radiolucency prior to treatment n unsatisfactory root canal filling, In such cases, delay the final restoration until: n evidence of periradicular healing is seen radiographically. n This is true if further endodontic treatment is more complicated. after placement of a post n That is why the decision is taken to wait healing be seen radiographically for at least 6 months. n During this time, the remaining tooth structure must be protected.
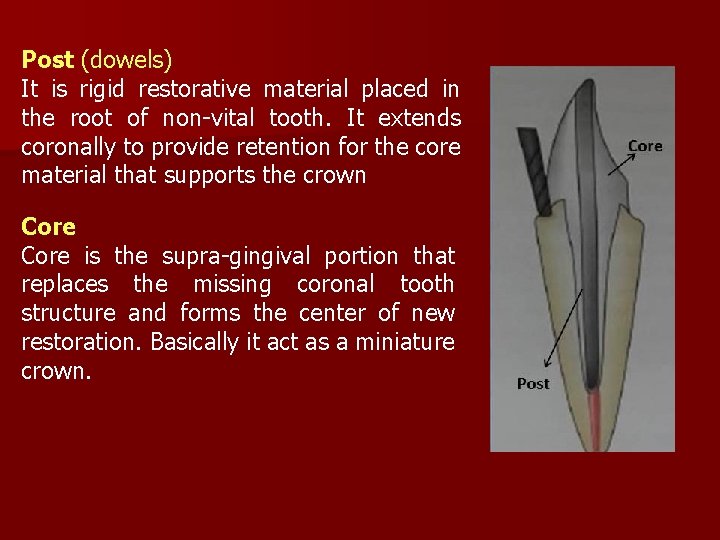
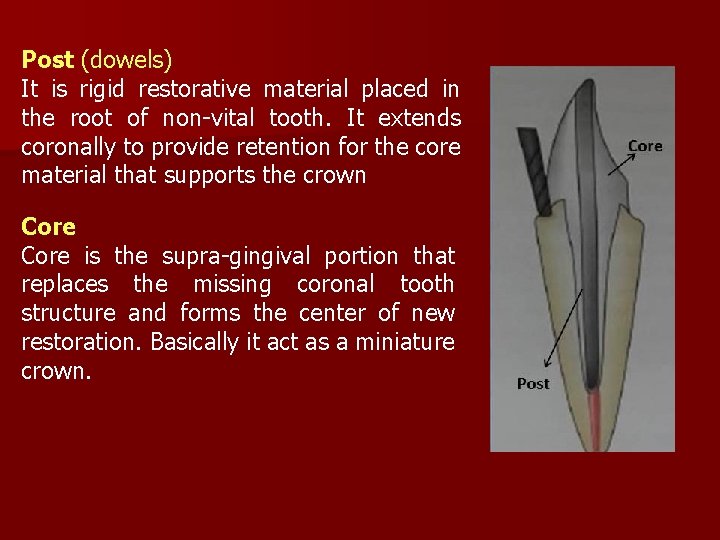
Post (dowels) It is rigid restorative material placed in the root of non-vital tooth. It extends coronally to provide retention for the core material that supports the crown Core is the supra-gingival portion that replaces the missing coronal tooth structure and forms the center of new restoration. Basically it act as a miniature crown.

Features Evaluated before going for Post and Core: *Restorability of the tooth *Role of tooth in the month *Periodontal considerations *Functional loading Requirements of a Tooth to Accept a Post and Core: *Optimal apical seal *Absence of fistula or exudate *Absence of active inflammation *No sensitivity to percussion *Absence of associated periodontal disease *Sufficient bone support around the root. *Sound tooth structure coronal to alveolar crest *Absence of any fracture of root.
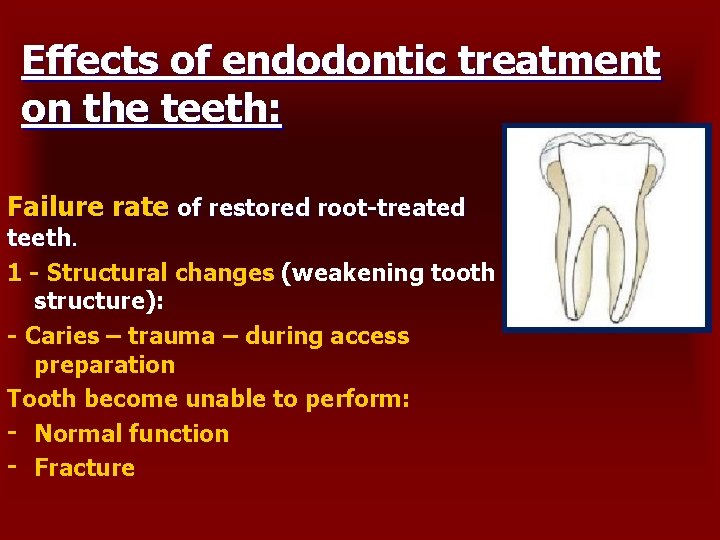
Conditions where post should NOT be given: 1. Any sign of endodontic failures are evident, i. e. tooth exhibits • Poor apical seal and poor quality obturation • Active inflammation • Presence of fistula or sinus • Tender on percussion 2. If adequate retention of core can be achieved by natural undercuts of crown. 3. If there are horizontal cracks in the coronal portion of the teeth. 4. When tooth is subjected to excursive occlusal stresses such as when there is presence of lateral stresses of bruxism or heavy incisal guidance.