Endocrine System Cellular Communication Types of Communication 1
- Slides: 75
Endocrine System
Cellular Communication Types of Communication 1. Direct Contact: exchange of materials between cells a. b. c. Plasmodesmata Gap junctions Surface to Surface contact: interaction of peripheral proteins on the cellular membrane (immune response)
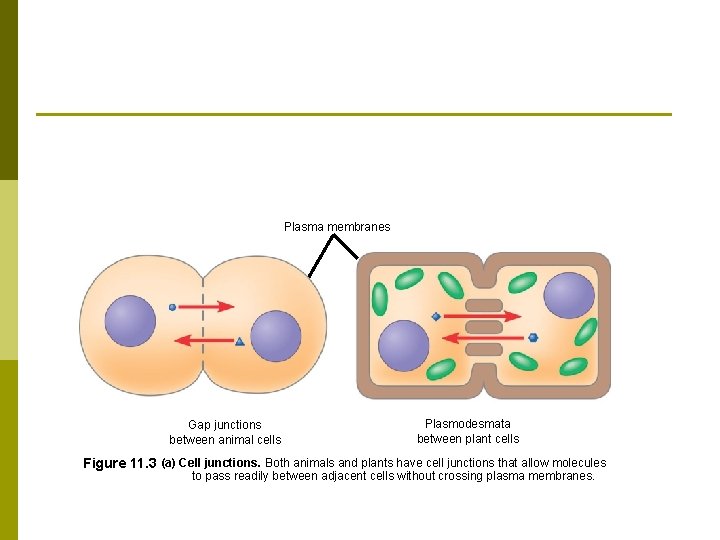
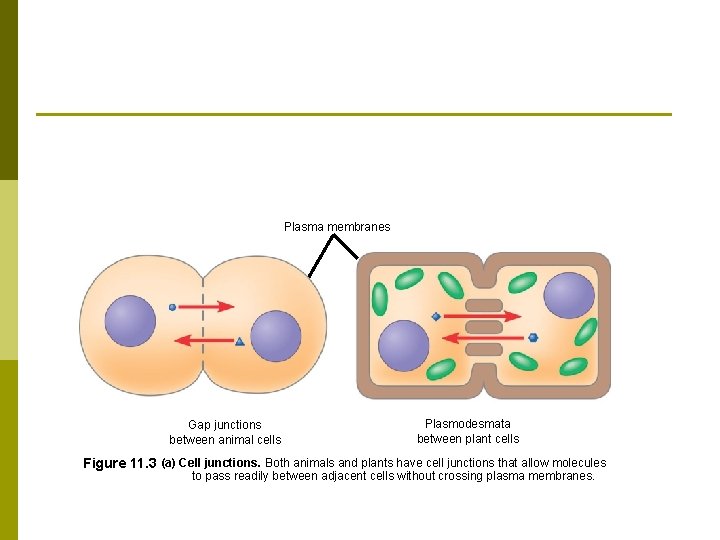
Plasma membranes Gap junctions between animal cells Plasmodesmata between plant cells Figure 11. 3 (a) Cell junctions. Both animals and plants have cell junctions that allow molecules to pass readily between adjacent cells without crossing plasma membranes.
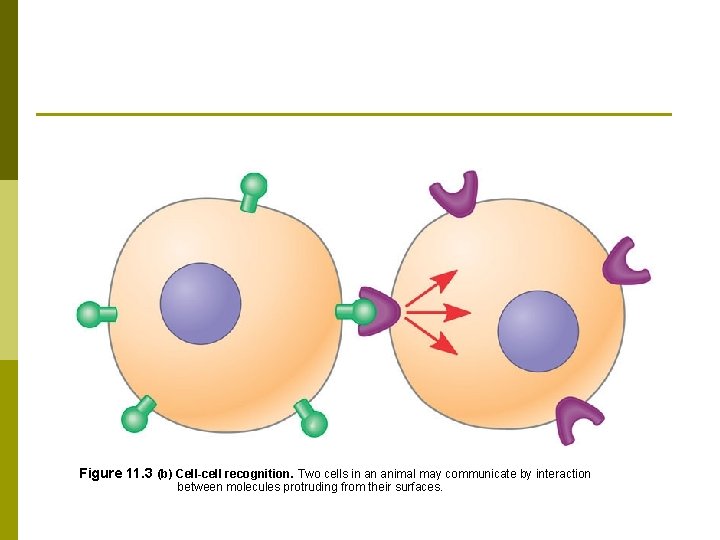
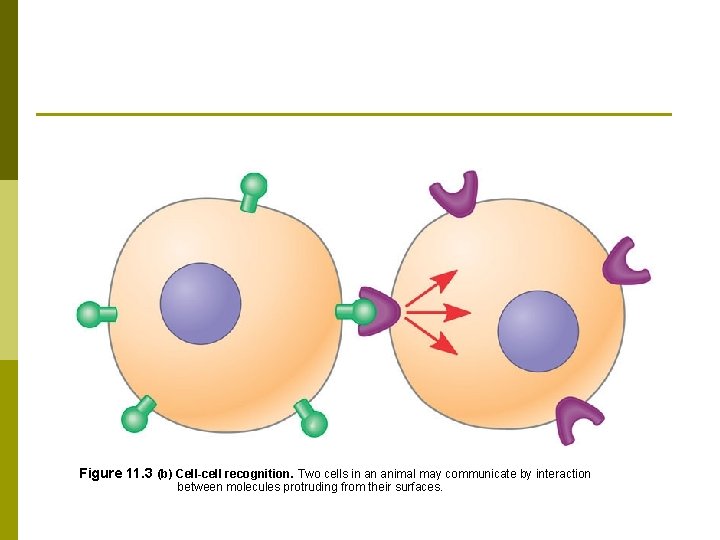
Figure 11. 3 (b) Cell-cell recognition. Two cells in an animal may communicate by interaction between molecules protruding from their surfaces.
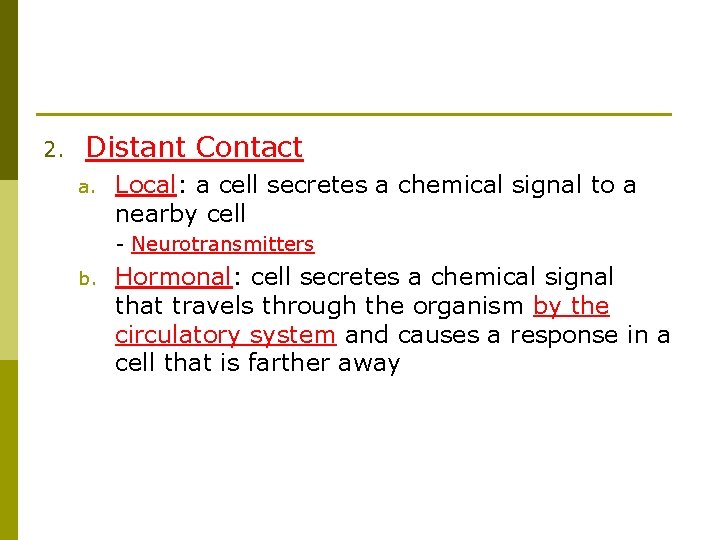
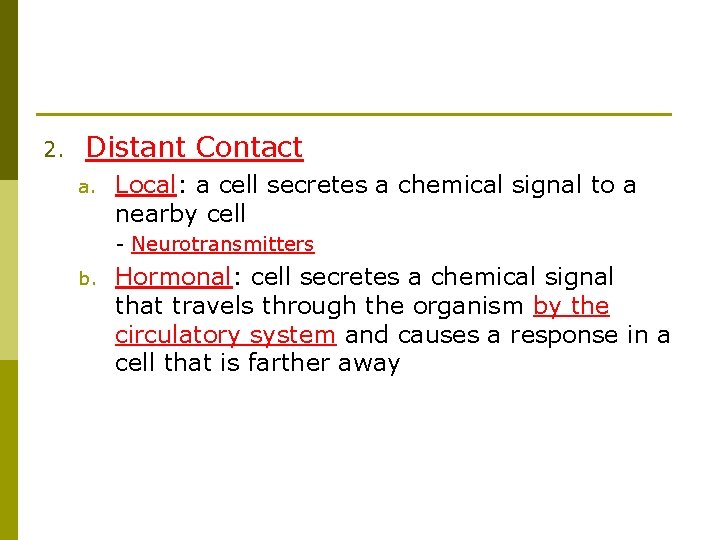
2. Distant Contact a. Local: a cell secretes a chemical signal to a nearby cell - Neurotransmitters b. Hormonal: cell secretes a chemical signal that travels through the organism by the circulatory system and causes a response in a cell that is farther away
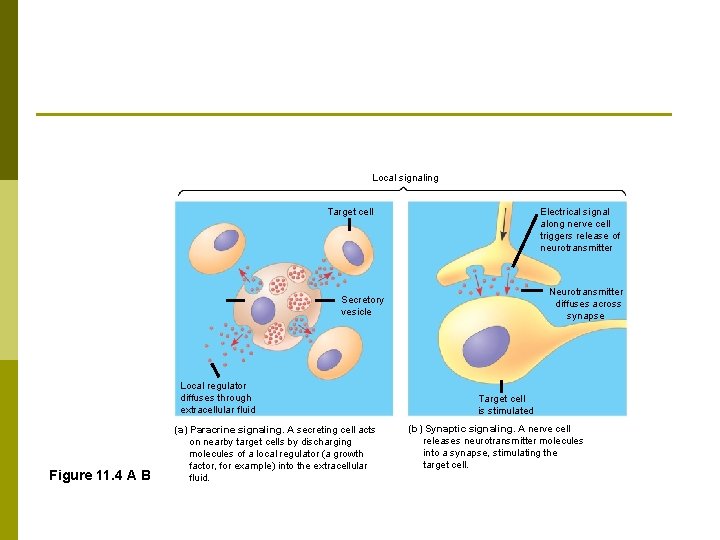
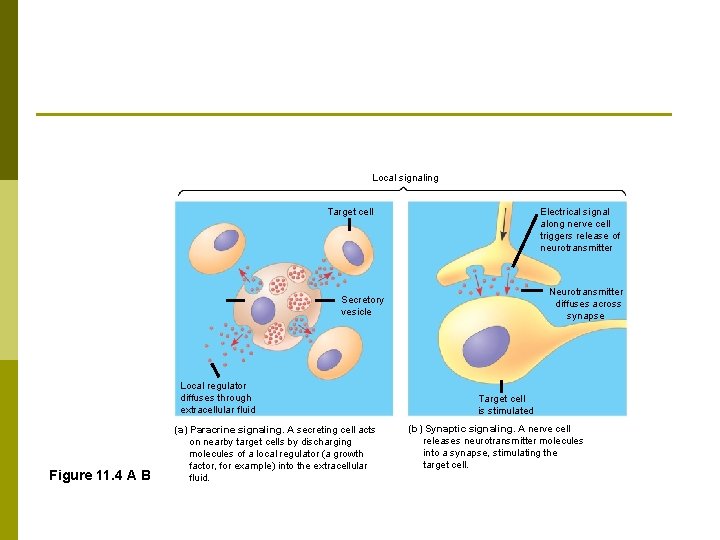
Local signaling Target cell Electrical signal along nerve cell triggers release of neurotransmitter Neurotransmitter diffuses across synapse Secretory vesicle Local regulator diffuses through extracellular fluid Figure 11. 4 A B (a) Paracrine signaling. A secreting cell acts on nearby target cells by discharging molecules of a local regulator (a growth factor, for example) into the extracellular fluid. Target cell is stimulated (b) Synaptic signaling. A nerve cell releases neurotransmitter molecules into a synapse, stimulating the target cell.
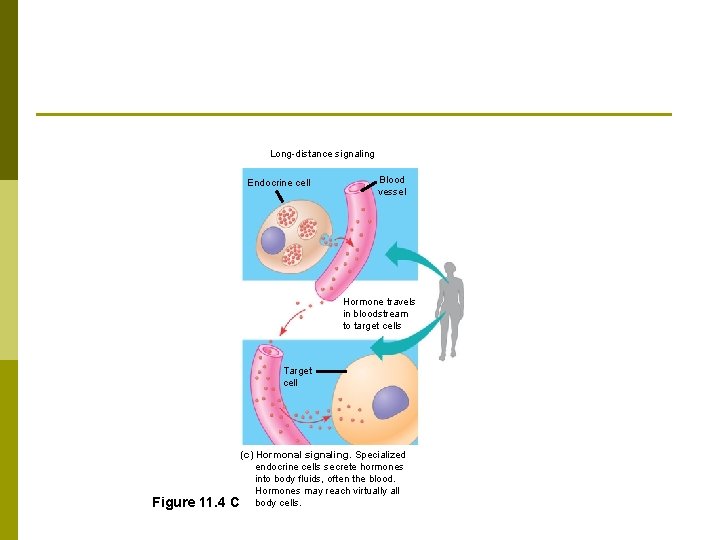
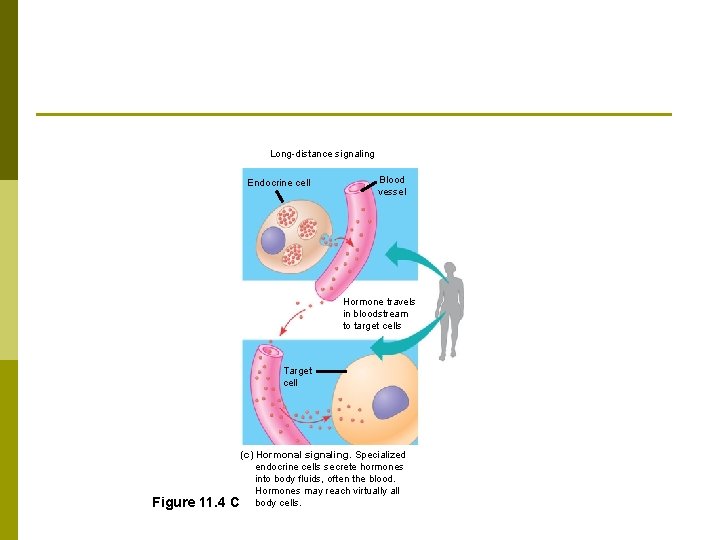
Long-distance signaling Endocrine cell Blood vessel Hormone travels in bloodstream to target cells Target cell Figure 11. 4 (c) Hormonal signaling. Specialized endocrine cells secrete hormones into body fluids, often the blood. Hormones may reach virtually all C body cells.
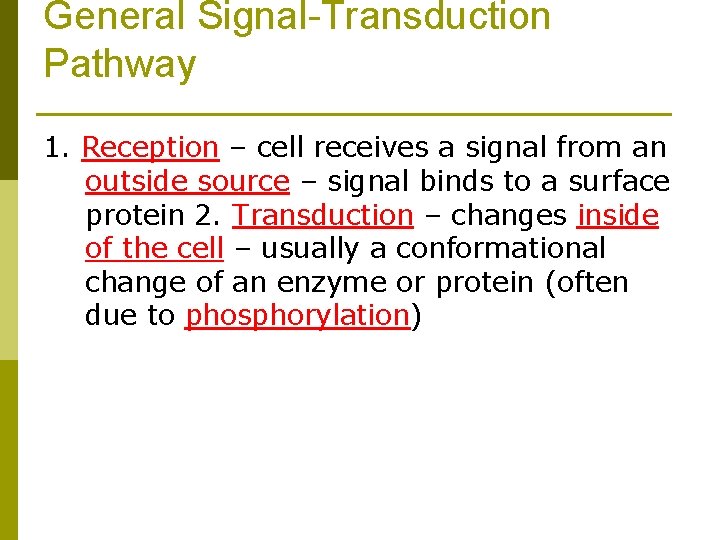
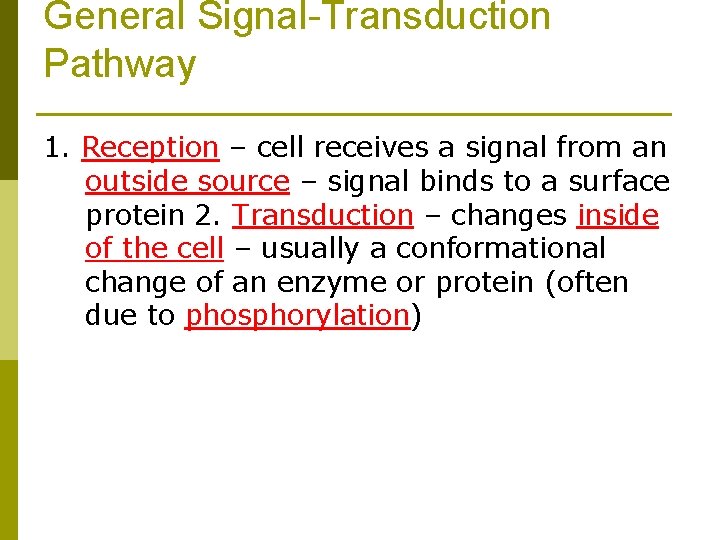
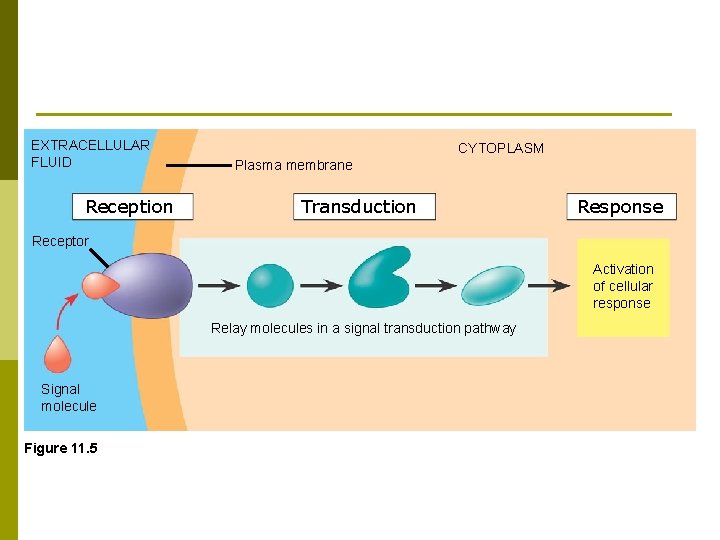
General Signal-Transduction Pathway 1. Reception – cell receives a signal from an outside source – signal binds to a surface protein 2. Transduction – changes inside of the cell – usually a conformational change of an enzyme or protein (often due to phosphorylation)
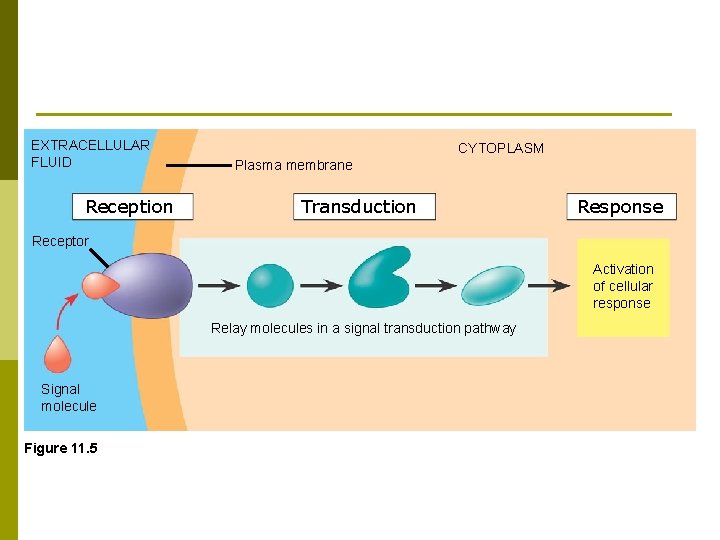
EXTRACELLULAR FLUID Reception CYTOPLASM Plasma membrane Transduction Response Receptor Activation of cellular response Relay molecules in a signal transduction pathway Signal molecule Figure 11. 5
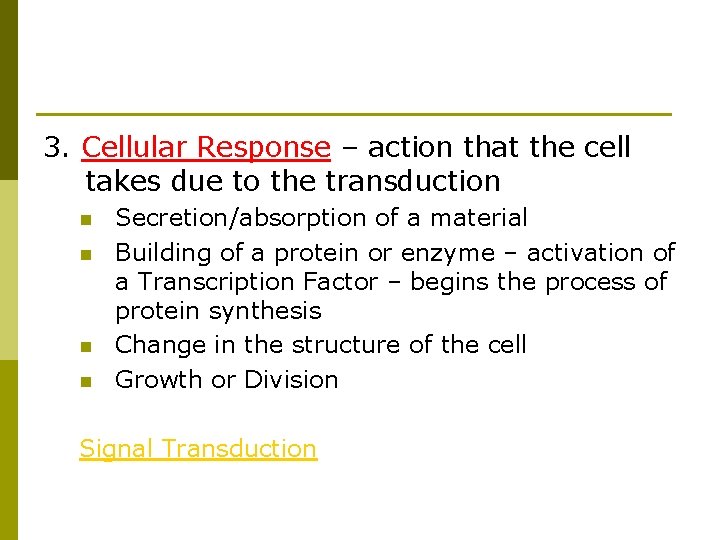
3. Cellular Response – action that the cell takes due to the transduction n n Secretion/absorption of a material Building of a protein or enzyme – activation of a Transcription Factor – begins the process of protein synthesis Change in the structure of the cell Growth or Division Signal Transduction
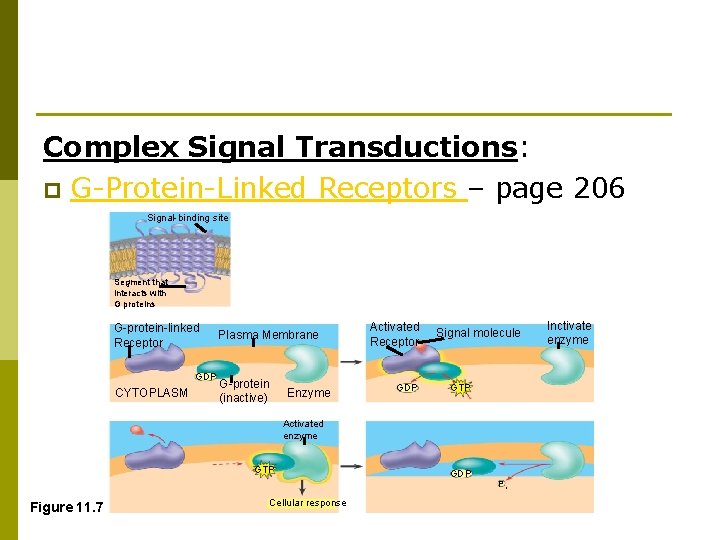
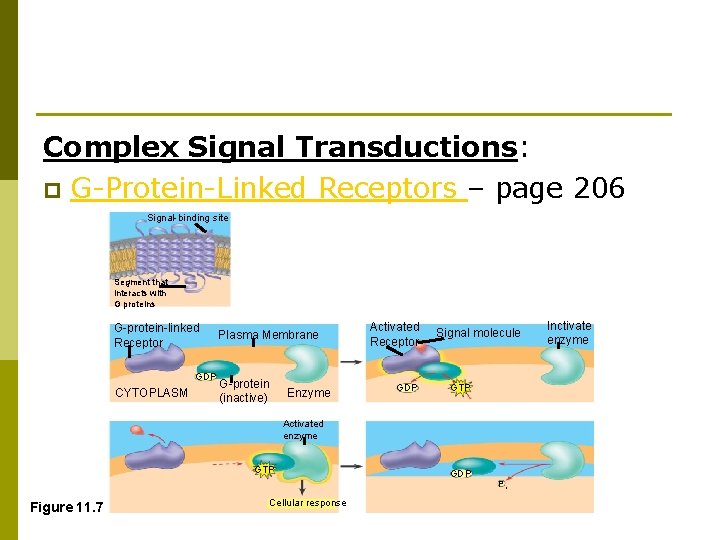
Complex Signal Transductions: p G-Protein-Linked Receptors – page 206 Signal-binding site Segment that interacts with G proteins G-protein-linked Receptor GDP CYTOPLASM Plasma Membrane G-protein (inactive) Enzyme Activated Receptor GDP Signal molecule GTP Activated enzyme GTP Figure 11. 7 Cellular response GDP Pi Inctivate enzyme
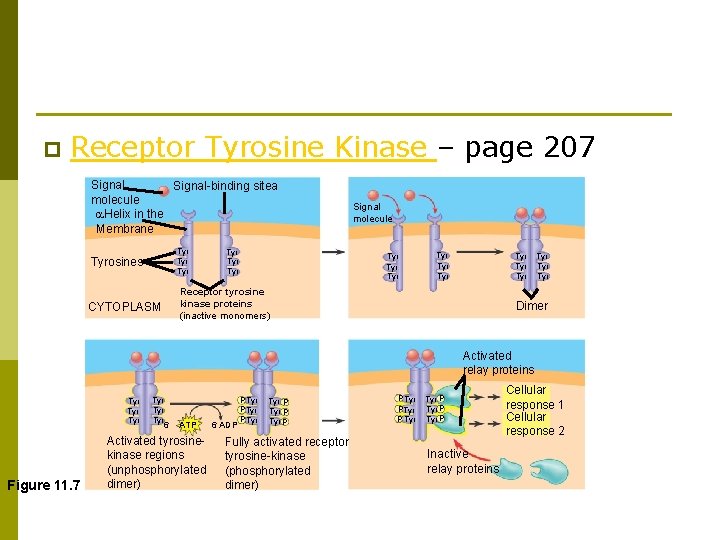
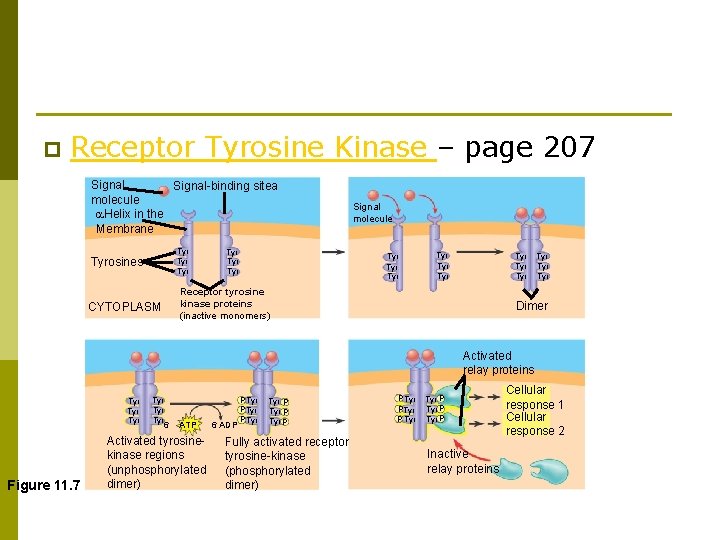
p Receptor Tyrosine Kinase – page 207 Signal-binding sitea molecule Helix in the Membrane Tyr Tyrosines Tyr Tyr Signal molecule Tyr Tyr Tyr Receptor tyrosine kinase proteins (inactive monomers) CYTOPLASM Tyr Tyr Dimer Activated relay proteins Tyr Tyr Figure 11. 7 Tyr Tyr 6 ATP Activated tyrosinekinase regions (unphosphorylated dimer) 6 ADP P Tyr P Tyr P Fully activated receptor tyrosine-kinase (phosphorylated dimer) P Tyr P Tyr P Inactive relay proteins Cellular response 1 Cellular response 2
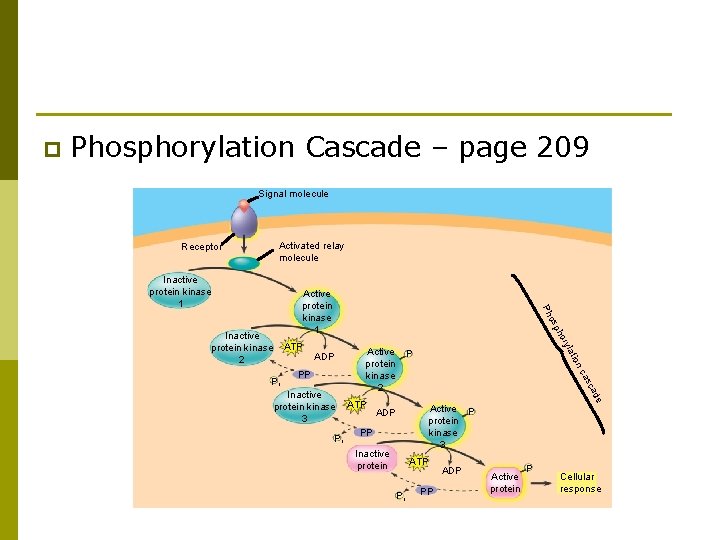
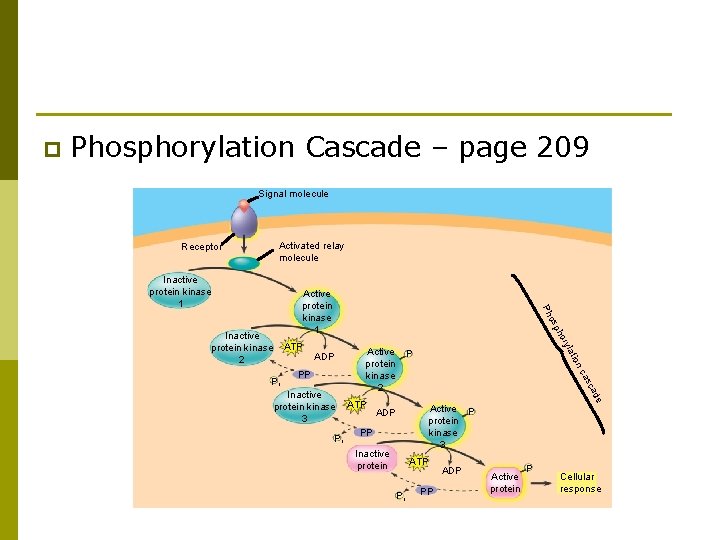
p Phosphorylation Cascade – page 209 Signal molecule Activated relay molecule Receptor Inactive protein kinase 1 de ca Pi ATP s ca Inactive protein kinase 3 P ion PP Active protein kinase 2 lat Pi ADP ry ho ATP p os Inactive protein kinase 2 Ph Active protein kinase 1 Active P protein kinase 3 ADP PP Inactive protein ATP Pi PP ADP Active protein P Cellular response
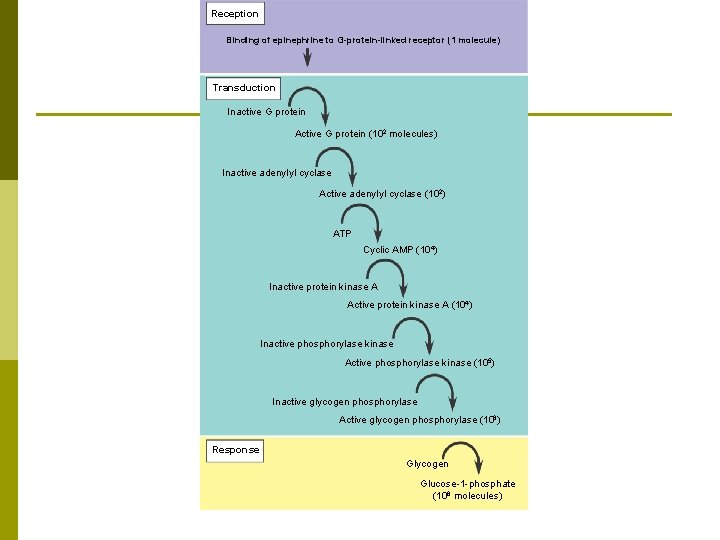
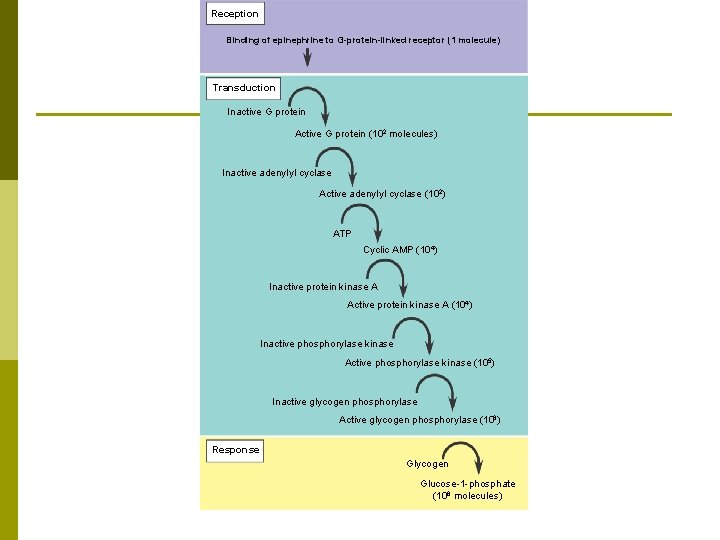
Reception Binding of epinephrine to G-protein-linked receptor (1 molecule) Transduction Inactive G protein Active G protein (102 molecules) Inactive adenylyl cyclase Active adenylyl cyclase (102) ATP Cyclic AMP (104) Inactive protein kinase A Active protein kinase A (104) Inactive phosphorylase kinase Active phosphorylase kinase (105) Inactive glycogen phosphorylase Active glycogen phosphorylase (106) Response Glycogen Glucose-1 -phosphate (108 molecules)
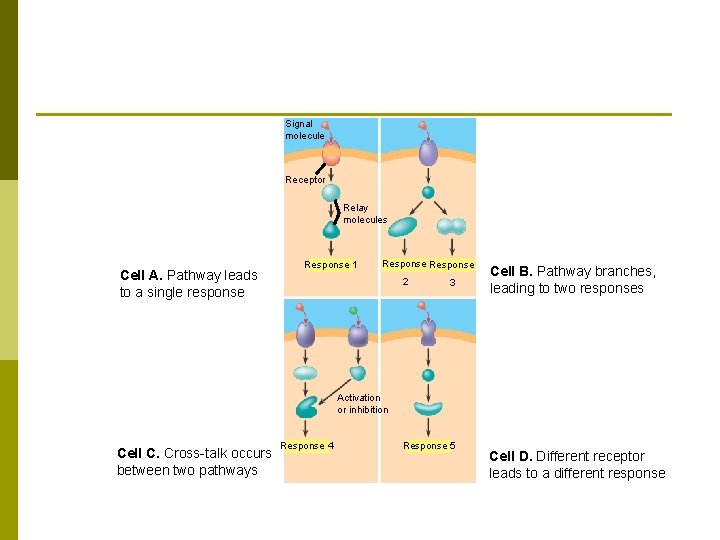
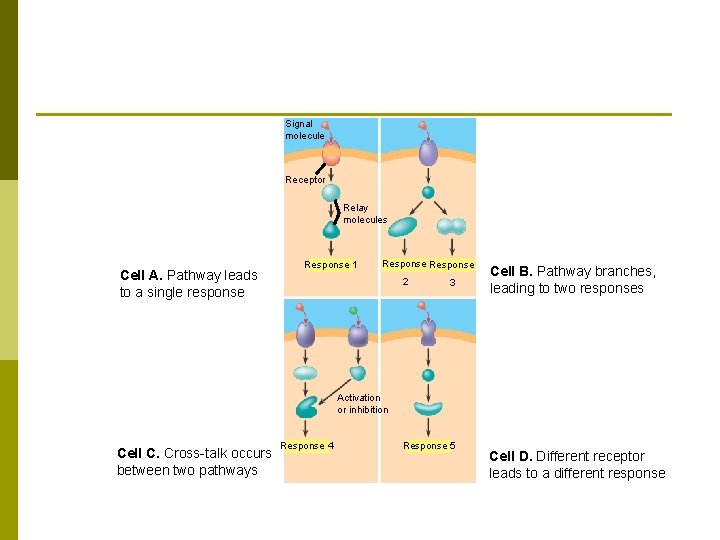
Signal molecule Receptor Relay molecules Cell A. Pathway leads to a single response Response 1 Response 2 3 Cell B. Pathway branches, leading to two responses Activation or inhibition Cell C. Cross-talk occurs between two pathways Response 4 Response 5 Cell D. Different receptor leads to a different response
p Cell Communication and Response
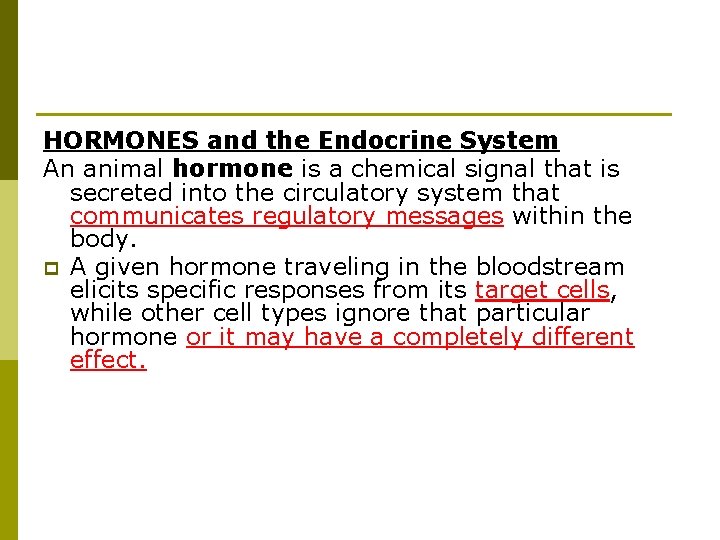
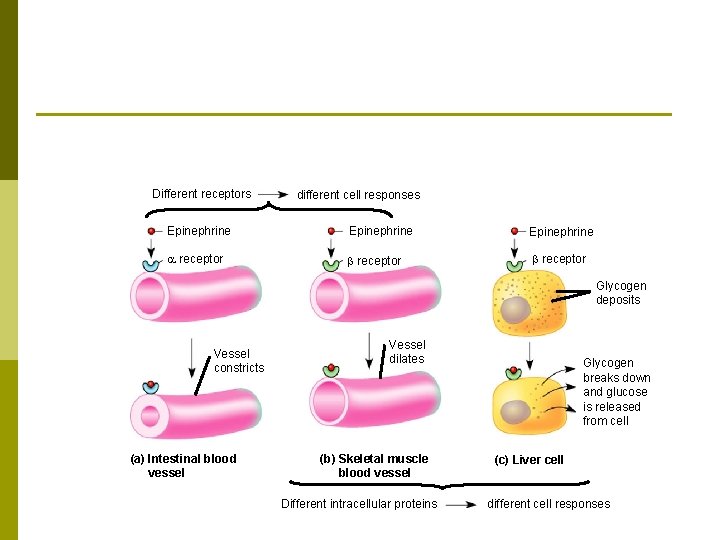
HORMONES and the Endocrine System An animal hormone is a chemical signal that is secreted into the circulatory system that communicates regulatory messages within the body. p A given hormone traveling in the bloodstream elicits specific responses from its target cells, while other cell types ignore that particular hormone or it may have a completely different effect.
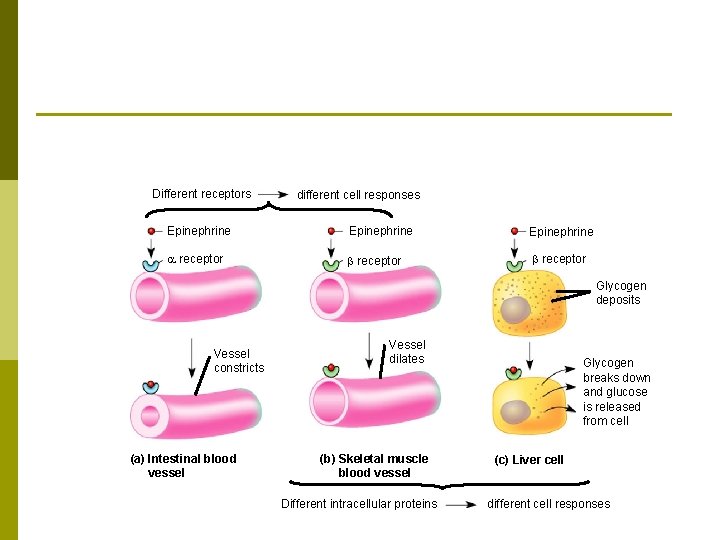
Different receptors different cell responses Epinephrine receptor b receptor Glycogen deposits Vessel constricts (a) Intestinal blood vessel Vessel dilates (b) Skeletal muscle blood vessel Different intracellular proteins Glycogen breaks down and glucose is released from cell (c) Liver cell different cell responses
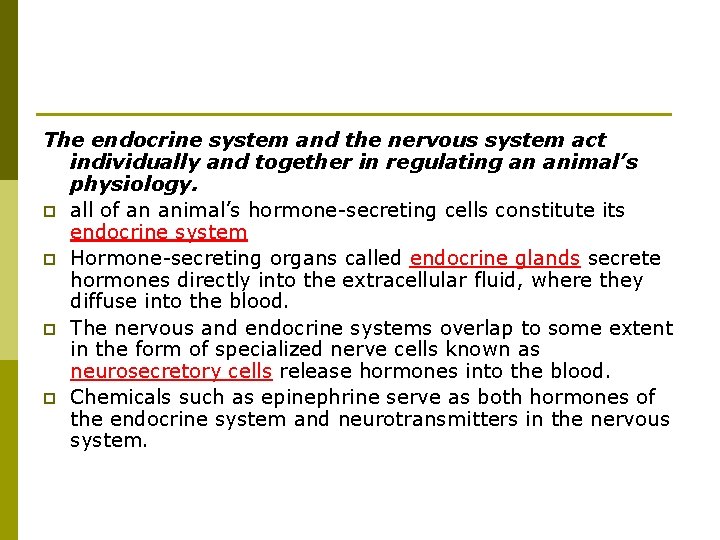
The endocrine system and the nervous system act individually and together in regulating an animal’s physiology. p all of an animal’s hormone-secreting cells constitute its endocrine system p Hormone-secreting organs called endocrine glands secrete hormones directly into the extracellular fluid, where they diffuse into the blood. p The nervous and endocrine systems overlap to some extent in the form of specialized nerve cells known as neurosecretory cells release hormones into the blood. p Chemicals such as epinephrine serve as both hormones of the endocrine system and neurotransmitters in the nervous system.
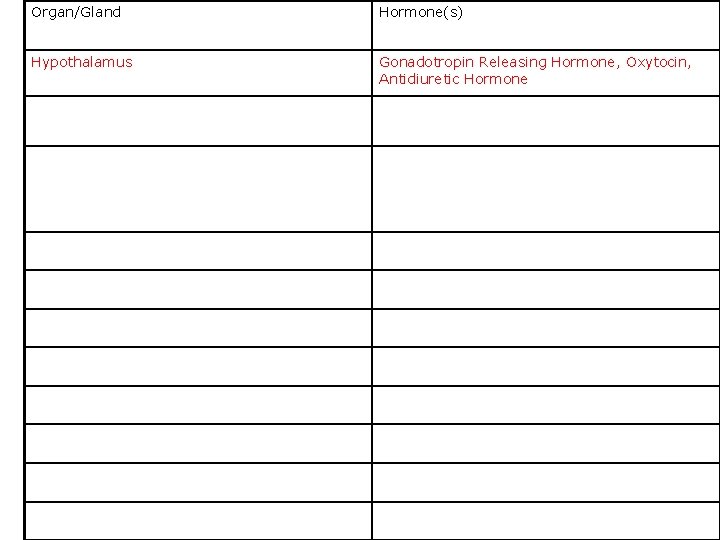
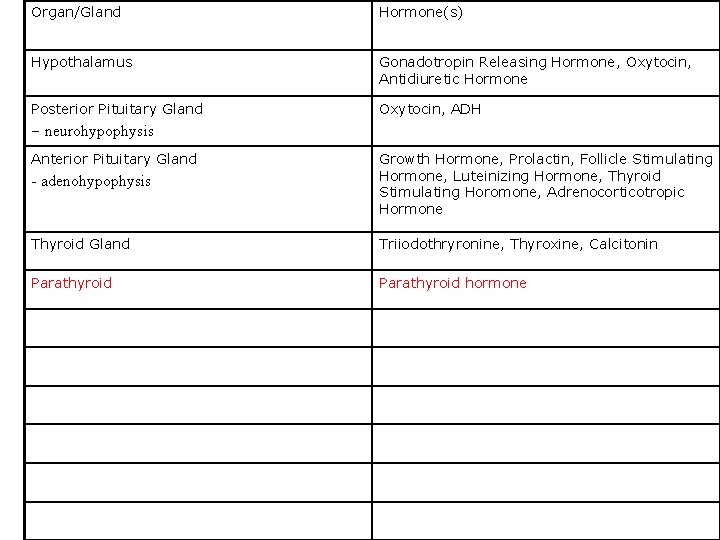
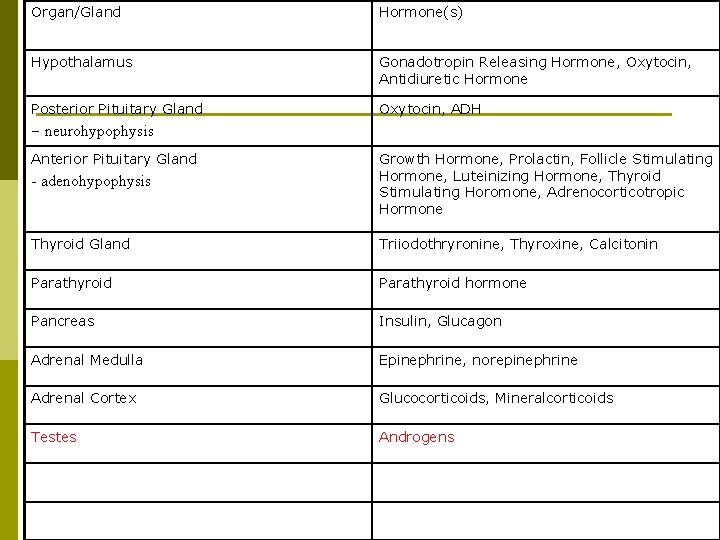
Organ/Gland Hormone(s)
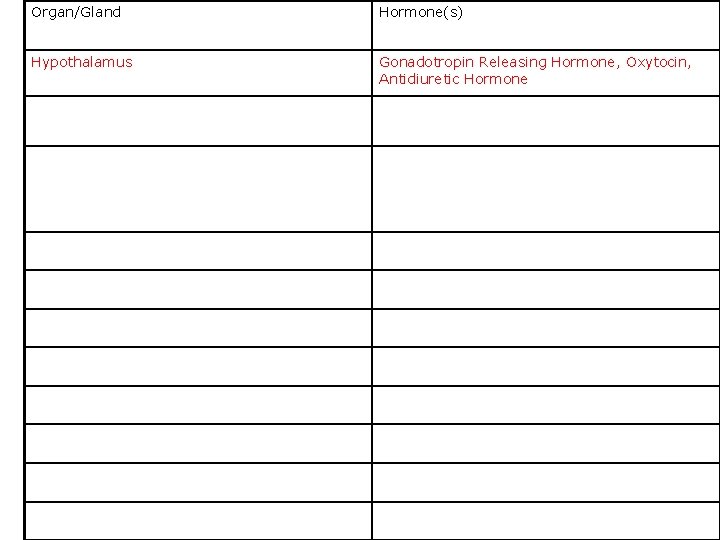
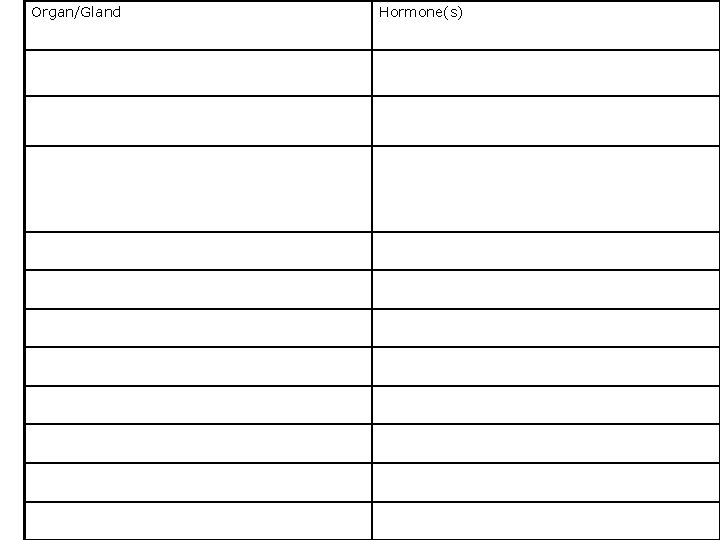
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone
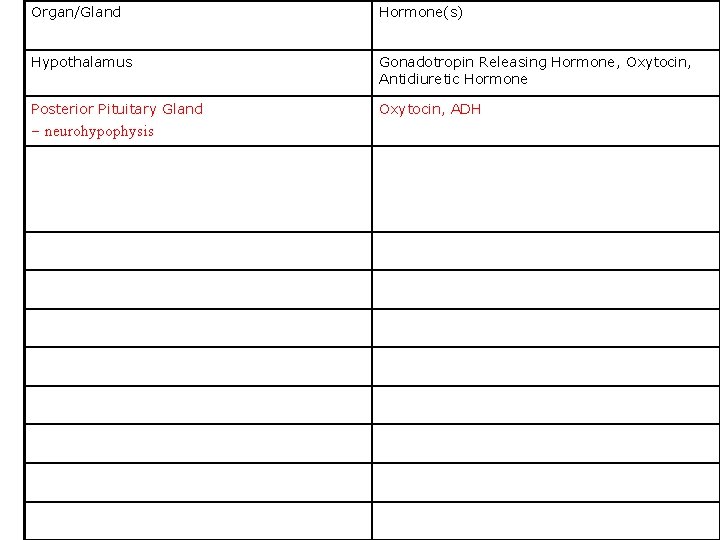
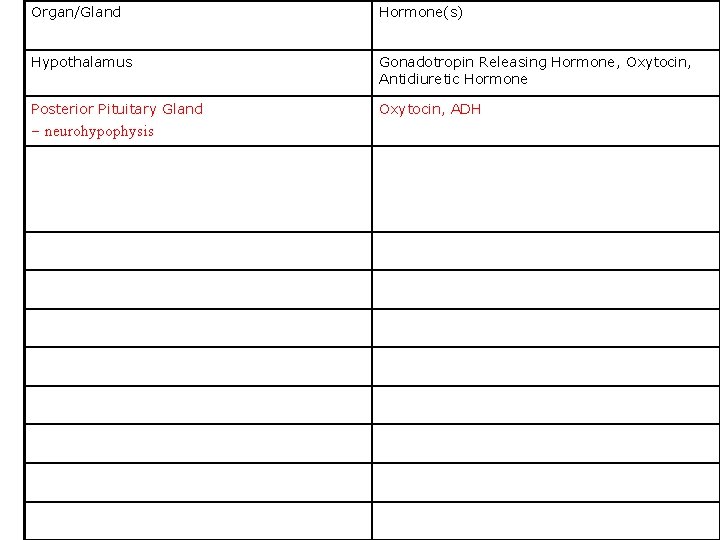
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis
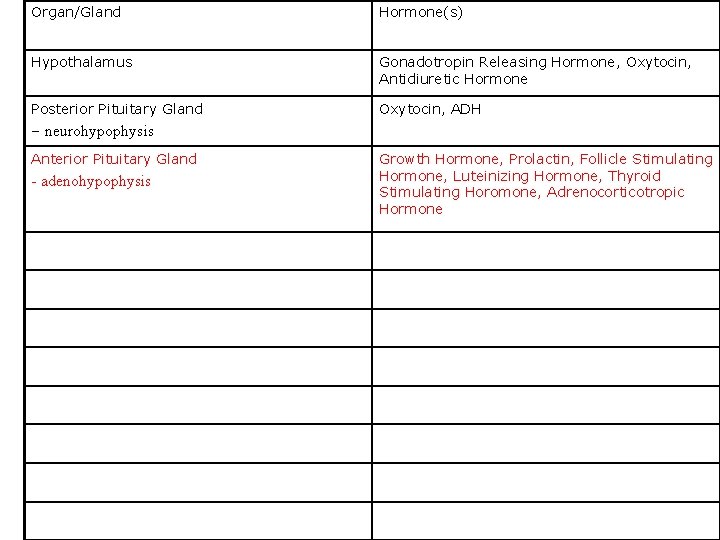
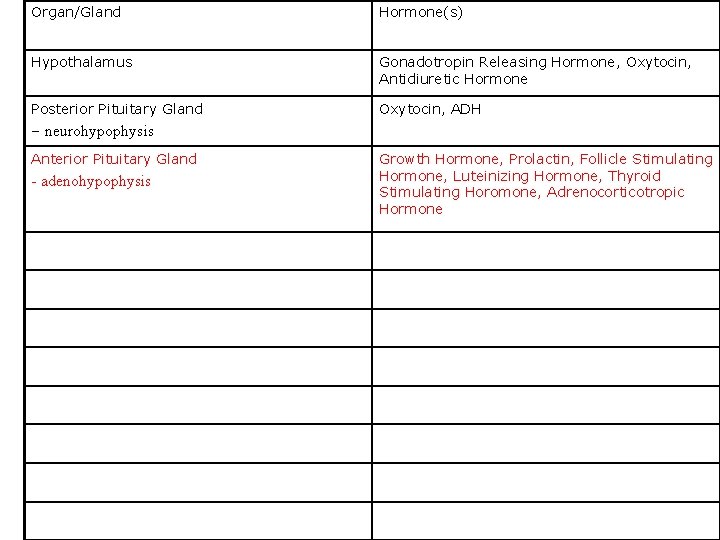
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone
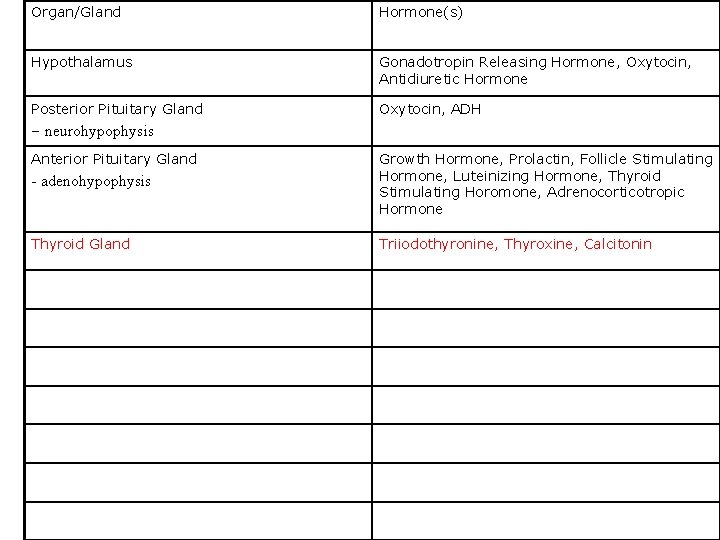
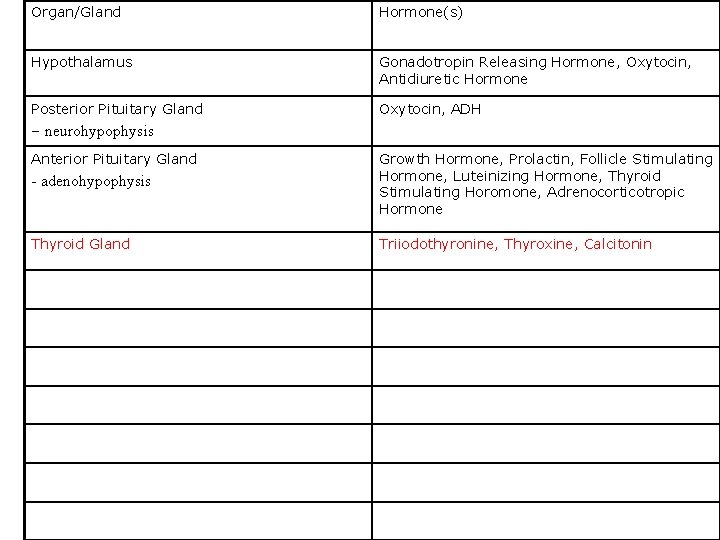
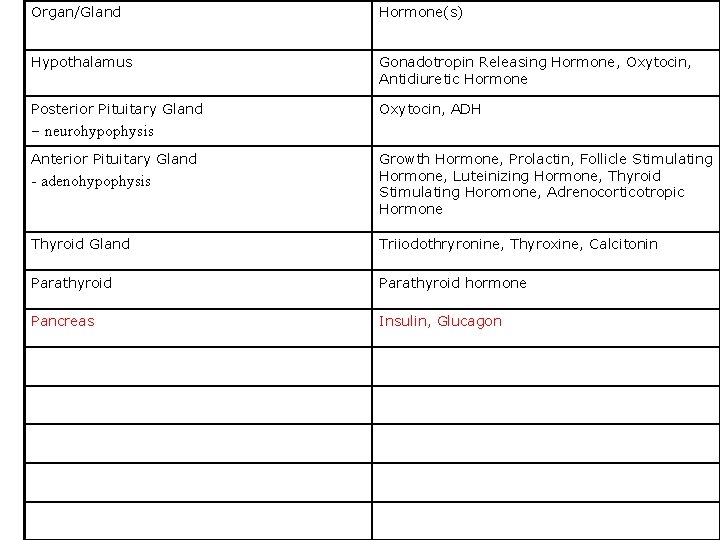
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothyronine, Thyroxine, Calcitonin
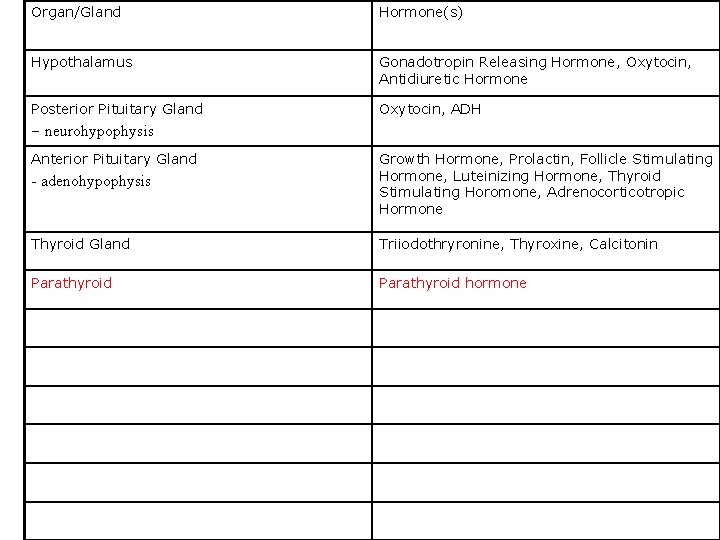
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothryronine, Thyroxine, Calcitonin Parathyroid hormone
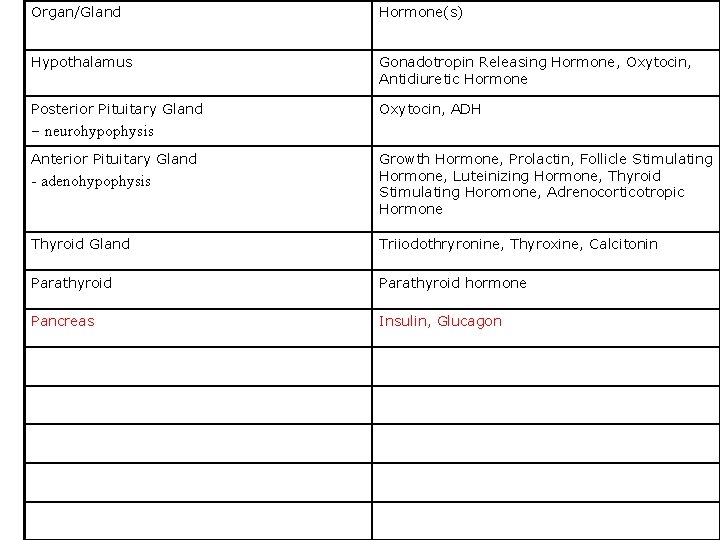
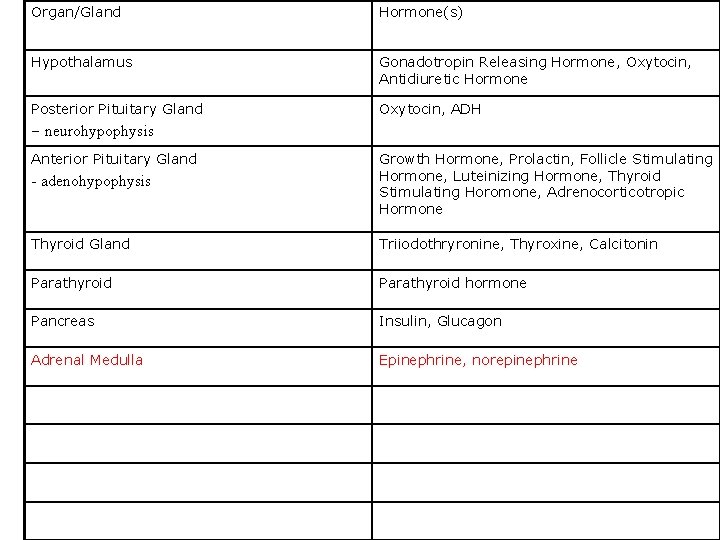
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothryronine, Thyroxine, Calcitonin Parathyroid hormone Pancreas Insulin, Glucagon
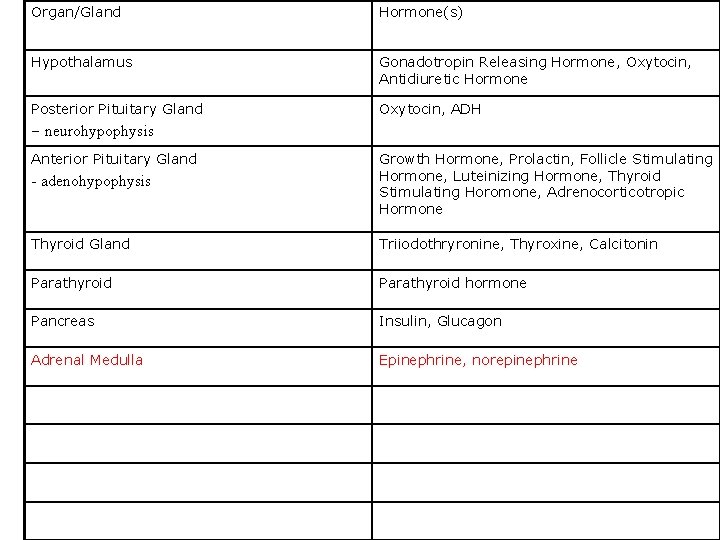
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothryronine, Thyroxine, Calcitonin Parathyroid hormone Pancreas Insulin, Glucagon Adrenal Medulla Epinephrine, norepinephrine
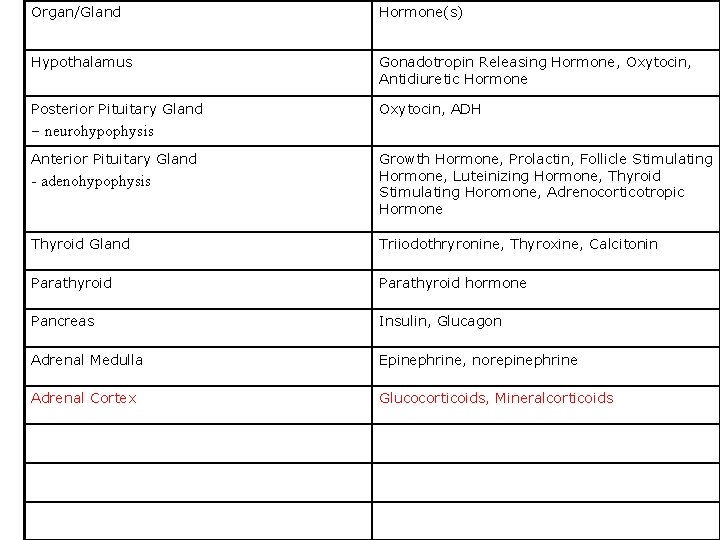
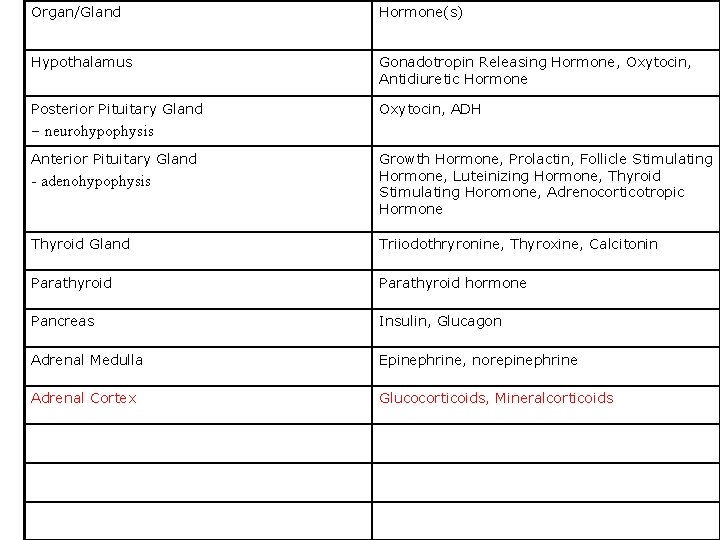
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothryronine, Thyroxine, Calcitonin Parathyroid hormone Pancreas Insulin, Glucagon Adrenal Medulla Epinephrine, norepinephrine Adrenal Cortex Glucocorticoids, Mineralcorticoids
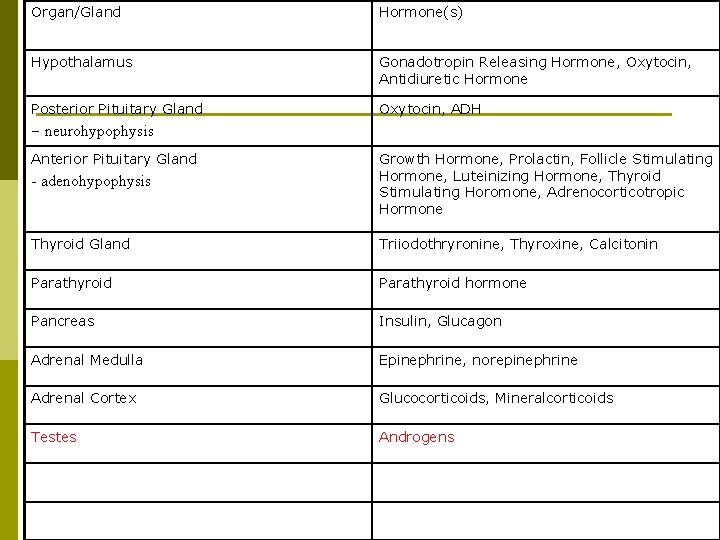
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothryronine, Thyroxine, Calcitonin Parathyroid hormone Pancreas Insulin, Glucagon Adrenal Medulla Epinephrine, norepinephrine Adrenal Cortex Glucocorticoids, Mineralcorticoids Testes Androgens
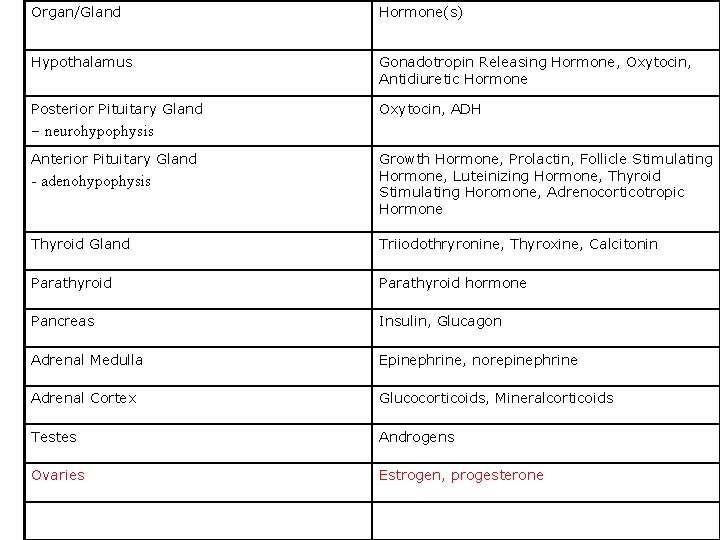
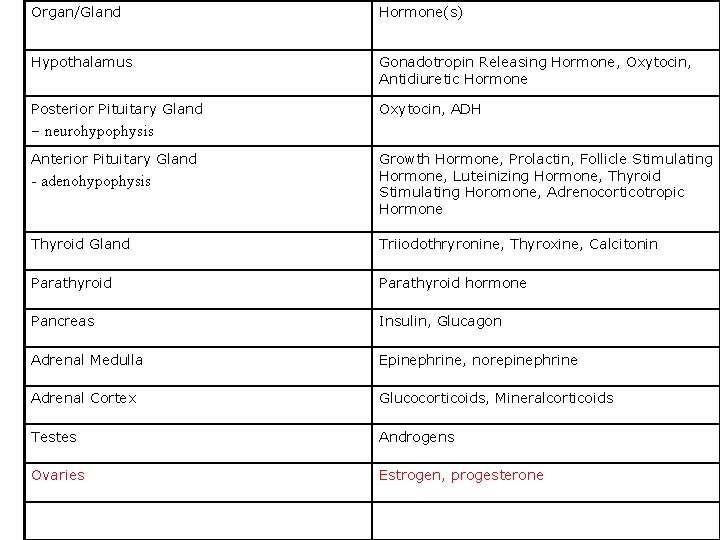
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothryronine, Thyroxine, Calcitonin Parathyroid hormone Pancreas Insulin, Glucagon Adrenal Medulla Epinephrine, norepinephrine Adrenal Cortex Glucocorticoids, Mineralcorticoids Testes Androgens Ovaries Estrogen, progesterone
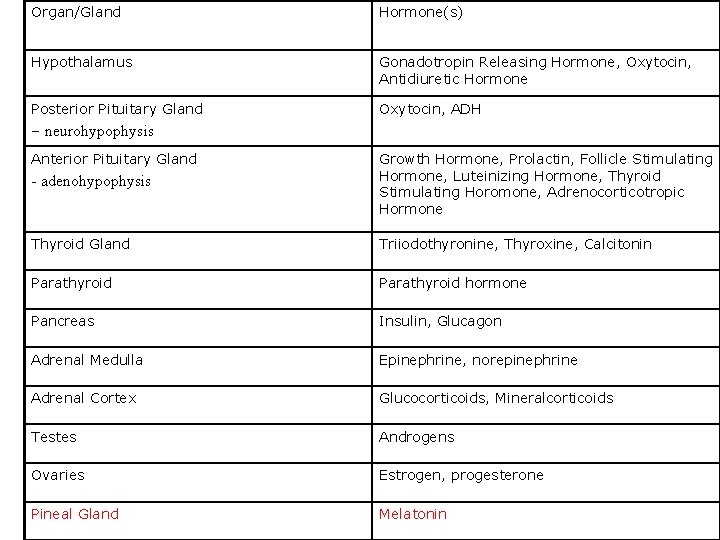
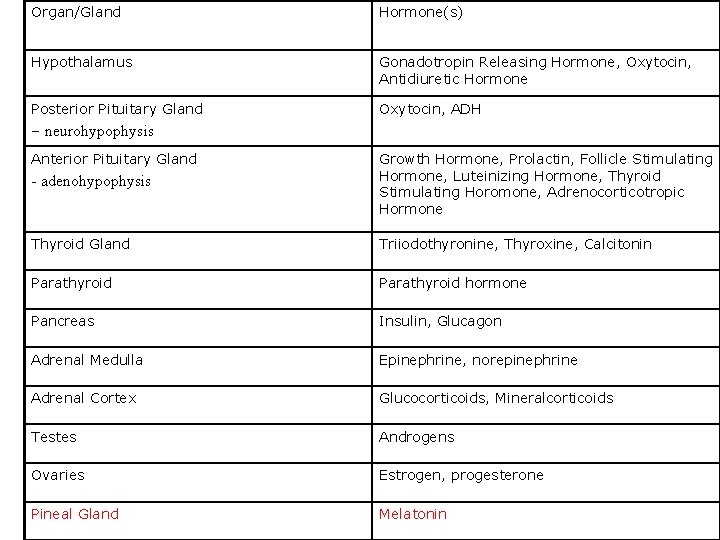
Organ/Gland Hormone(s) Hypothalamus Gonadotropin Releasing Hormone, Oxytocin, Antidiuretic Hormone Posterior Pituitary Gland Oxytocin, ADH – neurohypophysis Anterior Pituitary Gland - adenohypophysis Growth Hormone, Prolactin, Follicle Stimulating Hormone, Luteinizing Hormone, Thyroid Stimulating Horomone, Adrenocorticotropic Hormone Thyroid Gland Triiodothyronine, Thyroxine, Calcitonin Parathyroid hormone Pancreas Insulin, Glucagon Adrenal Medulla Epinephrine, norepinephrine Adrenal Cortex Glucocorticoids, Mineralcorticoids Testes Androgens Ovaries Estrogen, progesterone Pineal Gland Melatonin
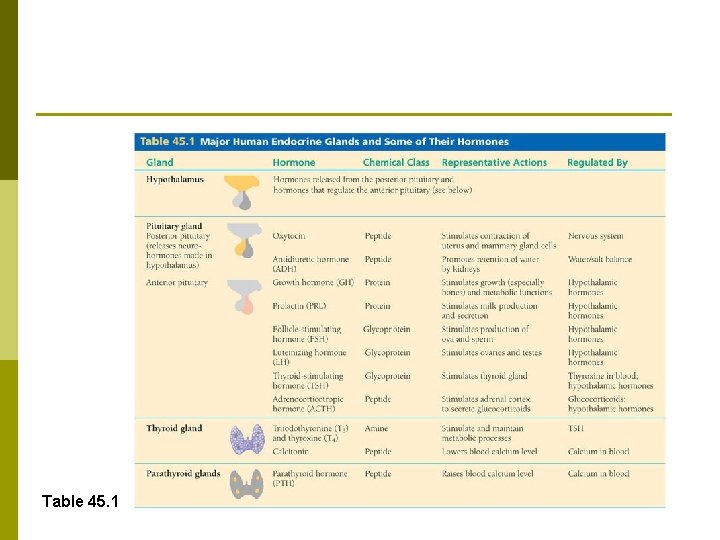
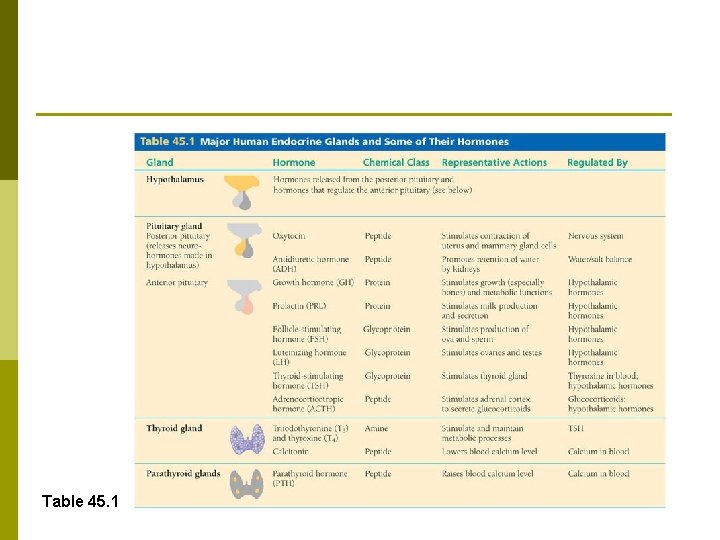
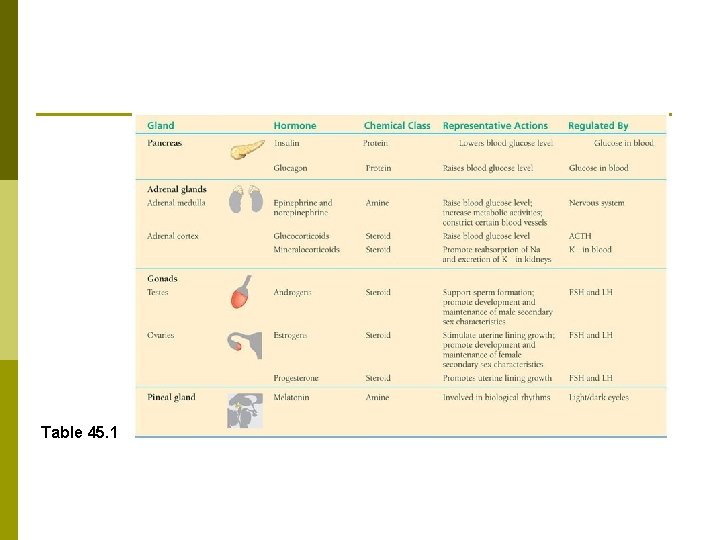
Table 45. 1
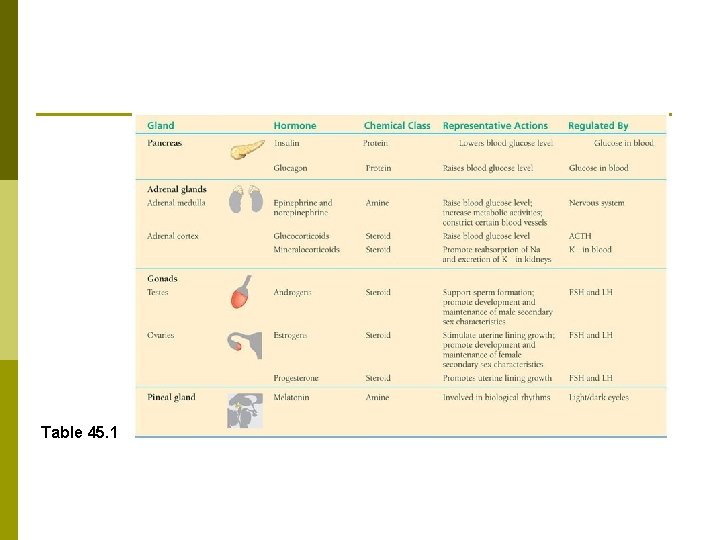
Table 45. 1
Endocrine Control: p A receptor, or sensor, detects a stimulus and sends information to a control center. p After comparing the incoming information to a set point, the control center sends out a signal that directs an effector to respond.
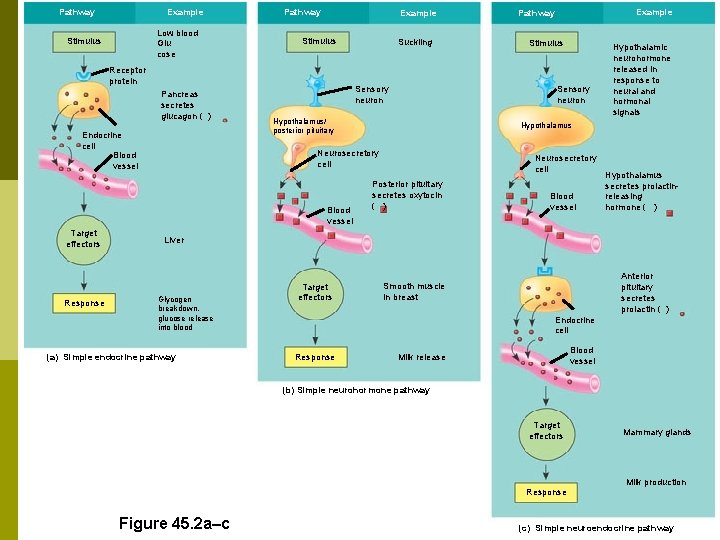
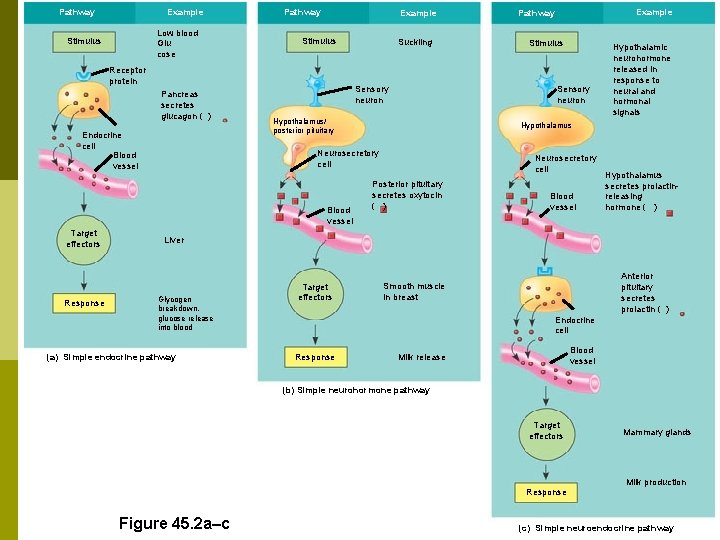
Pathway Example Low blood Glu cose Stimulus Pathway Example Stimulus Receptor protein Pancreas secretes glucagon ( ) Endocrine cell Blood vessel Response Stimulus Sensory neuron Hypothalamus/ posterior pituitary Hypothalamic neurohormone released in response to neural and hormonal signals Hypothalamus Neurosecretory cell Blood vessel Target effectors Suckling Example Pathway Neurosecretory cell Posterior pituitary secretes oxytocin ( ) Blood vessel Hypothalamus secretes prolactinreleasing hormone ( ) Liver Glycogen breakdown, glucose release into blood (a) Simple endocrine pathway Target effectors Anterior pituitary secretes prolactin ( ) Smooth muscle in breast Endocrine cell Response Blood vessel Milk release (b) Simple neurohormone pathway Target effectors Response Figure 45. 2 a–c Mammary glands Milk production (c) Simple neuroendocrine pathway
Hormones and other chemical signals bind to target cell receptors, initiating pathways that culminate in specific cell responses. p Three major classes of molecules function as hormones in vertebrates: proteins and peptides, amines, and steroids. p Most protein/peptides and amine hormones are water-soluble, unlike steroid hormones.
Chemical Signals and Their Modes of Action 1. Water-soluble hormones have cellsurface receptors. p The receptors for water-soluble hormones are embedded in the plasma membrane.
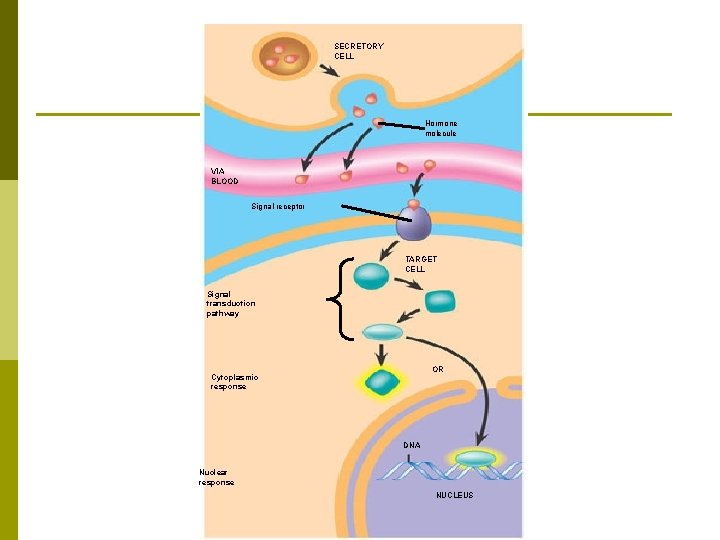
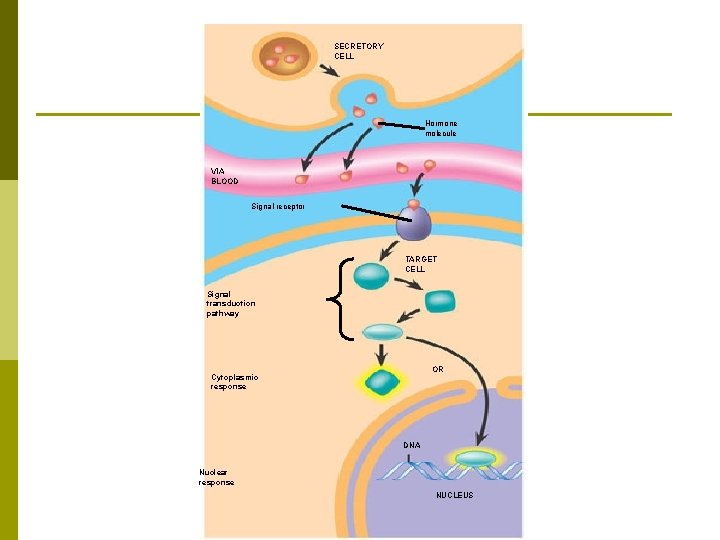
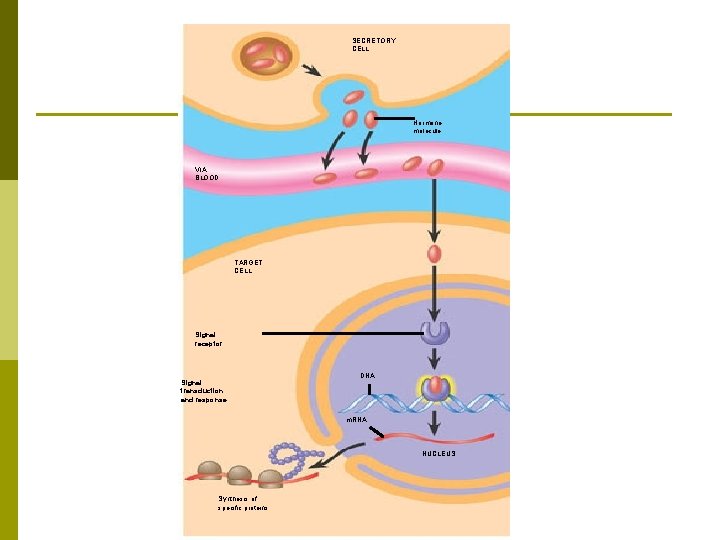
SECRETORY CELL Hormone molecule VIA BLOOD Signal receptor TARGET CELL Signal transduction pathway OR Cytoplasmic response DNA Nuclear response NUCLEUS
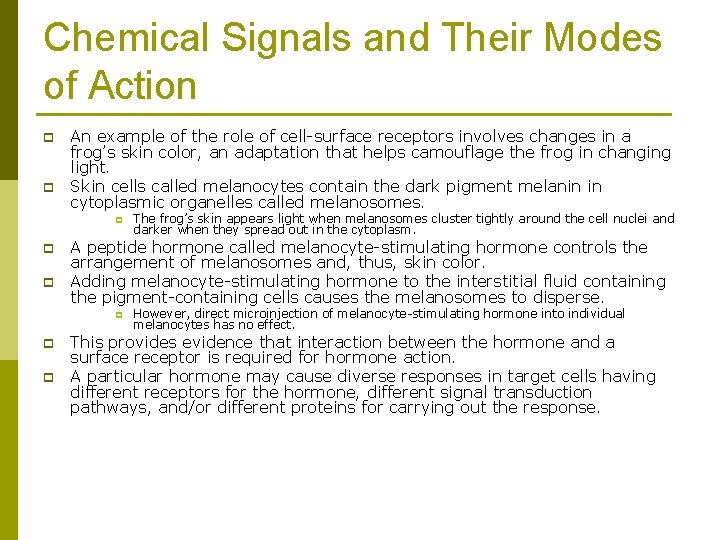
Chemical Signals and Their Modes of Action p p An example of the role of cell-surface receptors involves changes in a frog’s skin color, an adaptation that helps camouflage the frog in changing light. Skin cells called melanocytes contain the dark pigment melanin in cytoplasmic organelles called melanosomes. p p p A peptide hormone called melanocyte-stimulating hormone controls the arrangement of melanosomes and, thus, skin color. Adding melanocyte-stimulating hormone to the interstitial fluid containing the pigment-containing cells causes the melanosomes to disperse. p p p The frog’s skin appears light when melanosomes cluster tightly around the cell nuclei and darker when they spread out in the cytoplasm. However, direct microinjection of melanocyte-stimulating hormone into individual melanocytes has no effect. This provides evidence that interaction between the hormone and a surface receptor is required for hormone action. A particular hormone may cause diverse responses in target cells having different receptors for the hormone, different signal transduction pathways, and/or different proteins for carrying out the response.
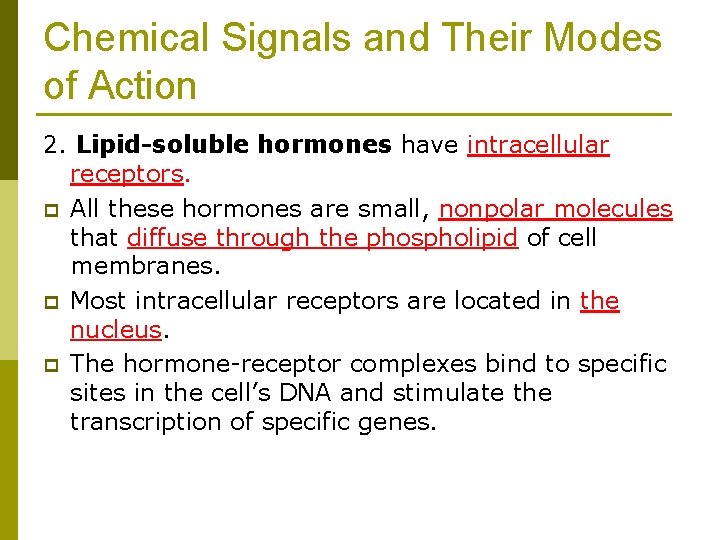
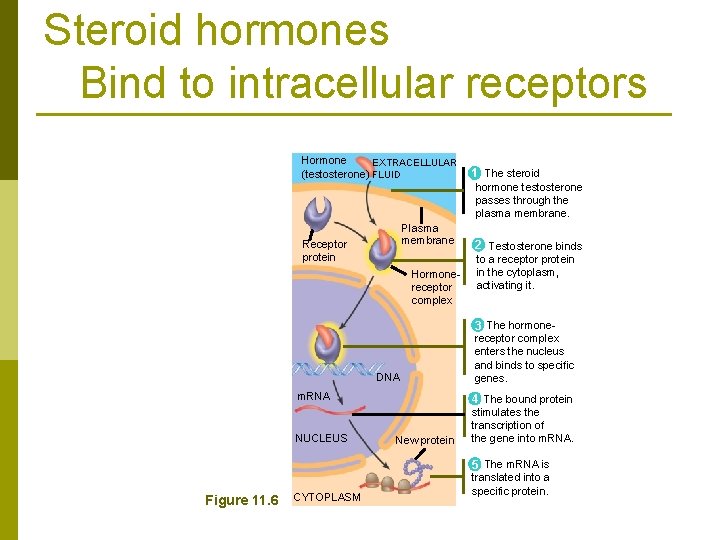
Chemical Signals and Their Modes of Action 2. Lipid-soluble hormones have intracellular receptors. p All these hormones are small, nonpolar molecules that diffuse through the phospholipid of cell membranes. p Most intracellular receptors are located in the nucleus. p The hormone-receptor complexes bind to specific sites in the cell’s DNA and stimulate the transcription of specific genes.
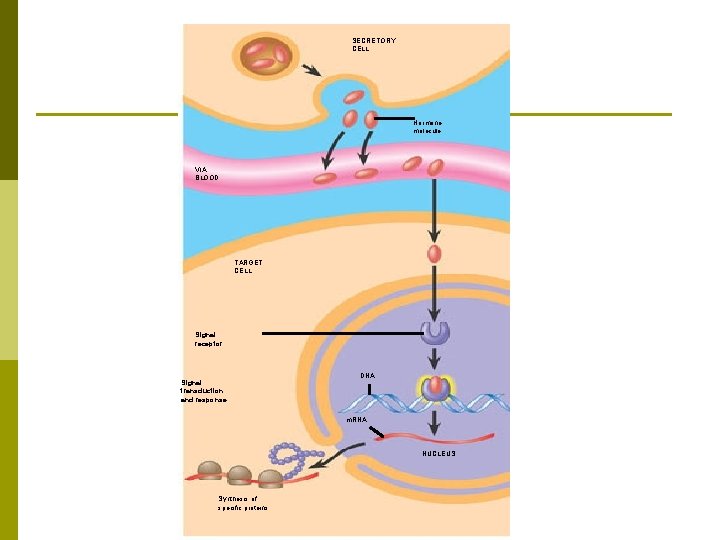
SECRETORY CELL Hormone molecule VIA BLOOD TARGET CELL Signal receptor Signal transduction and response DNA m. RNA NUCLEUS Synthesis of specific proteins
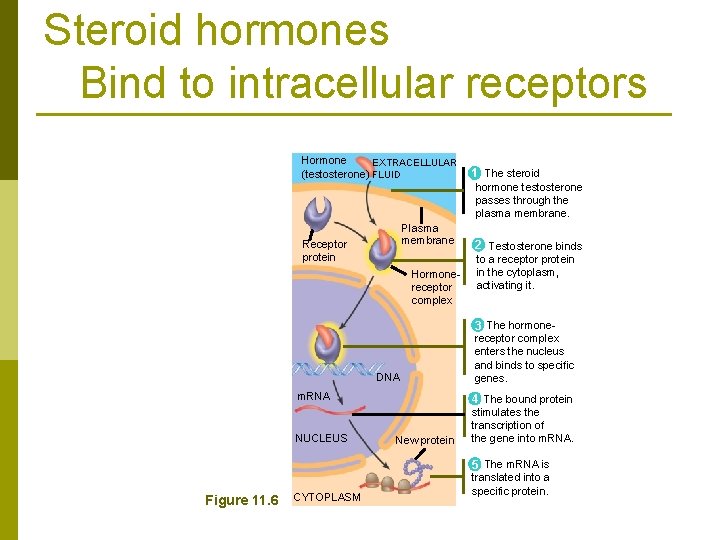
Steroid hormones Bind to intracellular receptors Hormone EXTRACELLULAR (testosterone) FLUID 1 The steroid hormone testosterone passes through the plasma membrane. Plasma membrane Receptor protein Hormonereceptor complex 2 Testosterone binds to a receptor protein in the cytoplasm, activating it. 3 The hormone- DNA Figure 11. 6 receptor complex enters the nucleus and binds to specific genes. m. RNA 4 The bound protein NUCLEUS stimulates the transcription of the gene into m. RNA. CYTOPLASM New protein 5 The m. RNA is translated into a specific protein.
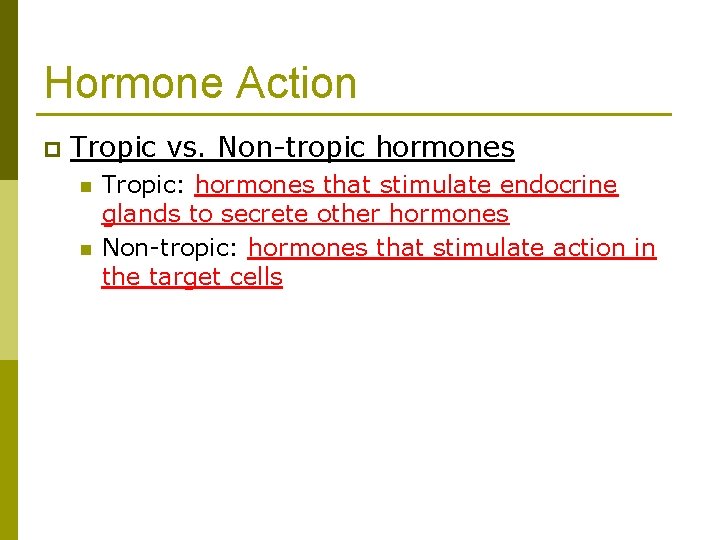
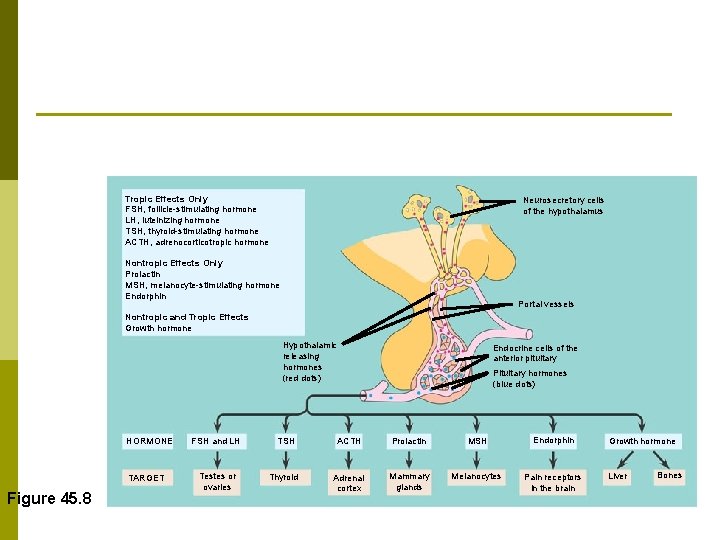
Hormone Action p Tropic vs. Non-tropic hormones n n Tropic: hormones that stimulate endocrine glands to secrete other hormones Non-tropic: hormones that stimulate action in the target cells
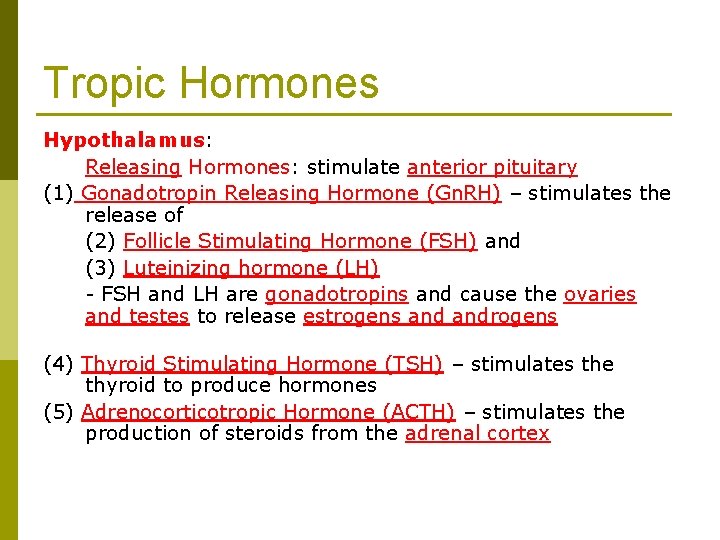
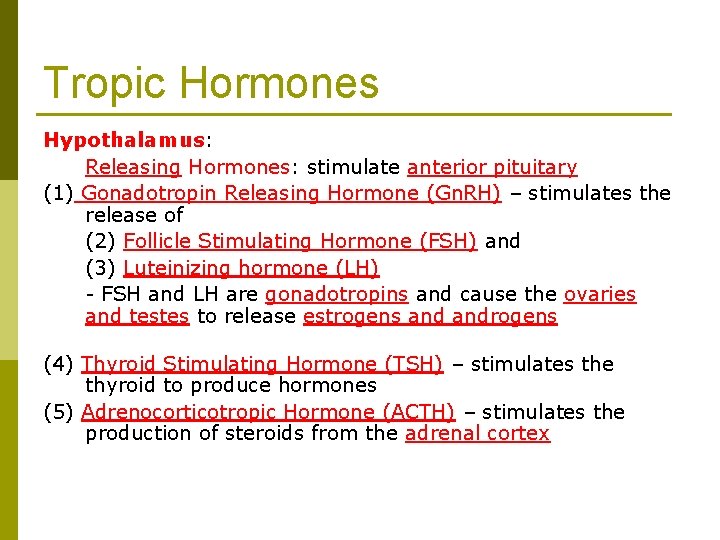
Tropic Hormones Hypothalamus: Releasing Hormones: stimulate anterior pituitary (1) Gonadotropin Releasing Hormone (Gn. RH) – stimulates the release of (2) Follicle Stimulating Hormone (FSH) and (3) Luteinizing hormone (LH) - FSH and LH are gonadotropins and cause the ovaries and testes to release estrogens androgens (4) Thyroid Stimulating Hormone (TSH) – stimulates the thyroid to produce hormones (5) Adrenocorticotropic Hormone (ACTH) – stimulates the production of steroids from the adrenal cortex
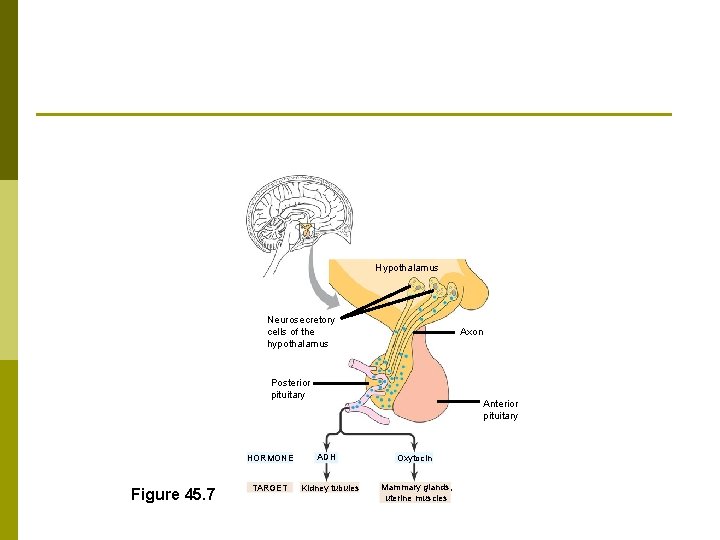
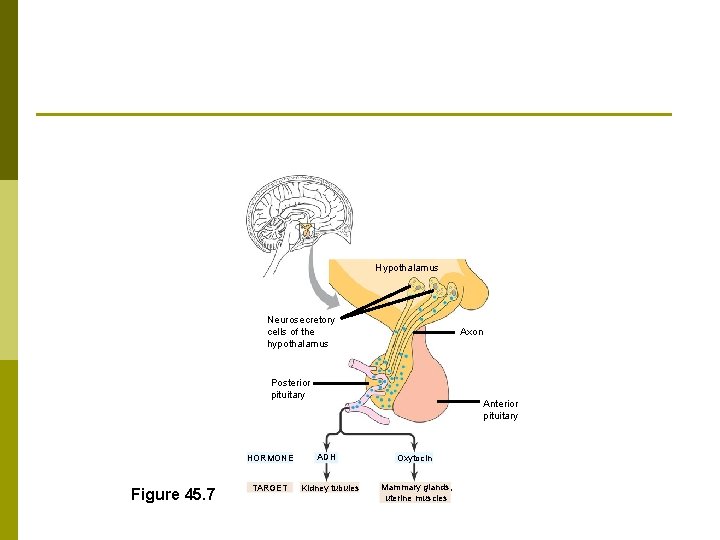
Hypothalamus Neurosecretory cells of the hypothalamus Axon Posterior pituitary HORMONE Figure 45. 7 TARGET Anterior pituitary ADH Kidney tubules Oxytocin Mammary glands, uterine muscles
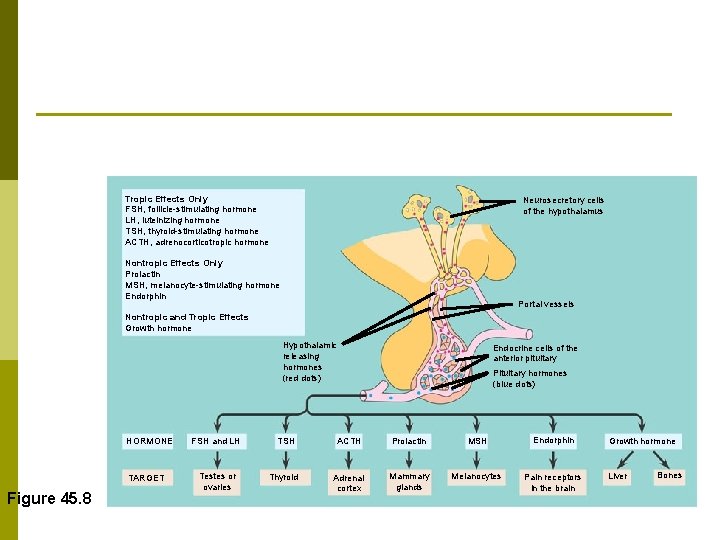
Tropic Effects Only FSH, follicle-stimulating hormone LH, luteinizing hormone TSH, thyroid-stimulating hormone ACTH, adrenocorticotropic hormone Neurosecretory cells of the hypothalamus Nontropic Effects Only Prolactin MSH, melanocyte-stimulating hormone Endorphin Portal vessels Nontropic and Tropic Effects Growth hormone Hypothalamic releasing hormones (red dots) HORMONE TARGET Figure 45. 8 FSH and LH Testes or ovaries TSH Thyroid Endocrine cells of the anterior pituitary Pituitary hormones (blue dots) ACTH Prolactin MSH Endorphin Adrenal cortex Mammary glands Melanocytes Pain receptors in the brain Growth hormone Liver Bones
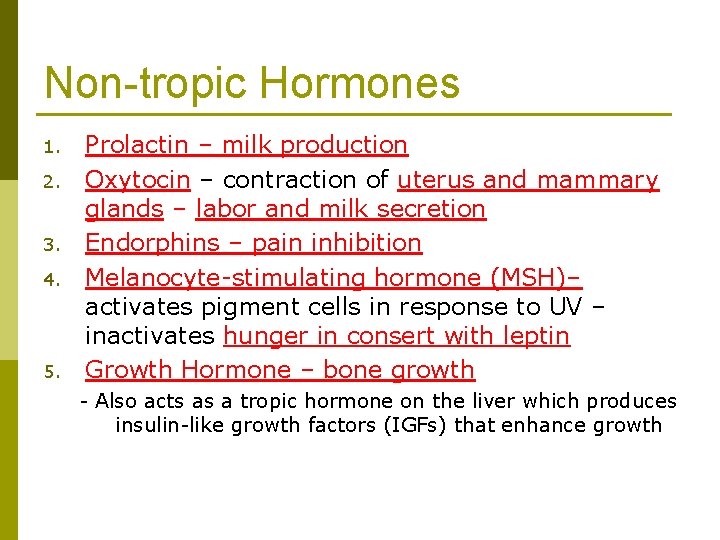
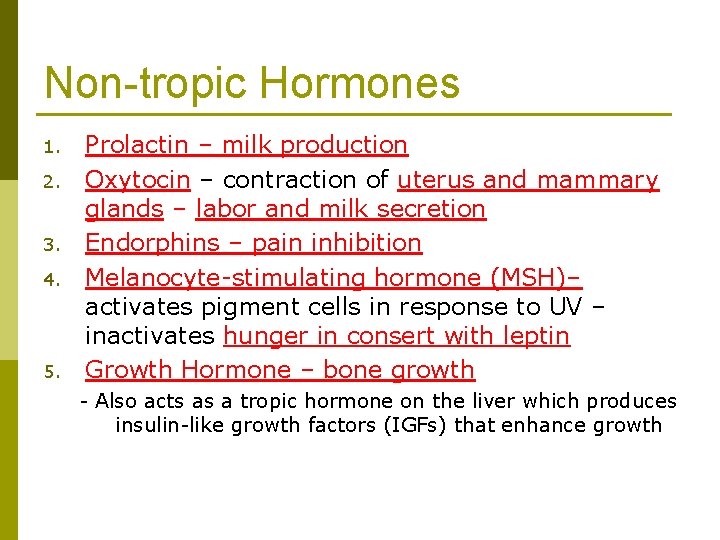
Non-tropic Hormones 1. 2. 3. 4. 5. Prolactin – milk production Oxytocin – contraction of uterus and mammary glands – labor and milk secretion Endorphins – pain inhibition Melanocyte-stimulating hormone (MSH)– activates pigment cells in response to UV – inactivates hunger in consert with leptin Growth Hormone – bone growth - Also acts as a tropic hormone on the liver which produces insulin-like growth factors (IGFs) that enhance growth
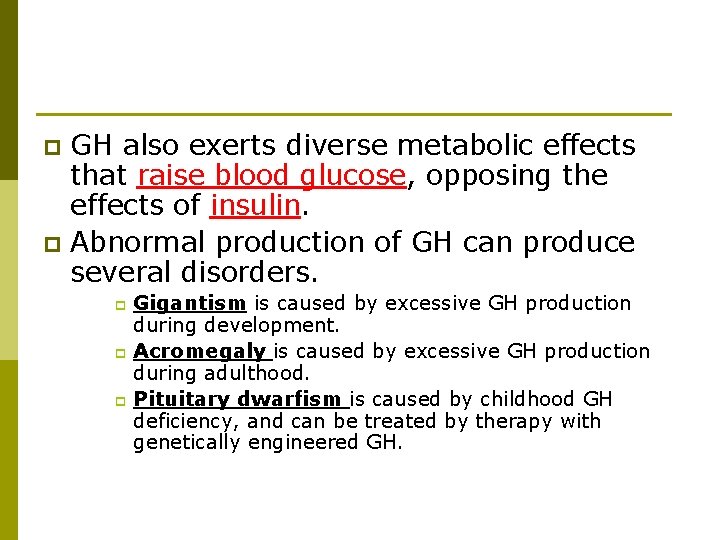
GH also exerts diverse metabolic effects that raise blood glucose, opposing the effects of insulin. p Abnormal production of GH can produce several disorders. p Gigantism is caused by excessive GH production during development. p Acromegaly is caused by excessive GH production during adulthood. p Pituitary dwarfism is caused by childhood GH deficiency, and can be treated by therapy with genetically engineered GH. p
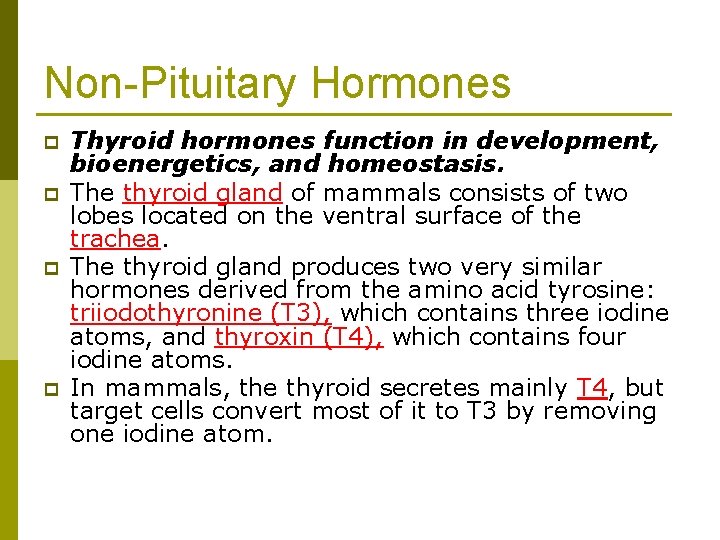
Non-Pituitary Hormones p p Thyroid hormones function in development, bioenergetics, and homeostasis. The thyroid gland of mammals consists of two lobes located on the ventral surface of the trachea. The thyroid gland produces two very similar hormones derived from the amino acid tyrosine: triiodothyronine (T 3), which contains three iodine atoms, and thyroxin (T 4), which contains four iodine atoms. In mammals, the thyroid secretes mainly T 4, but target cells convert most of it to T 3 by removing one iodine atom.
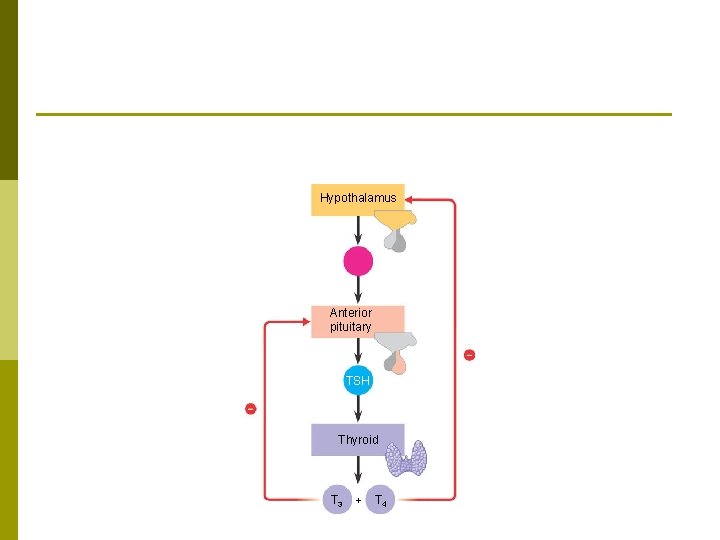
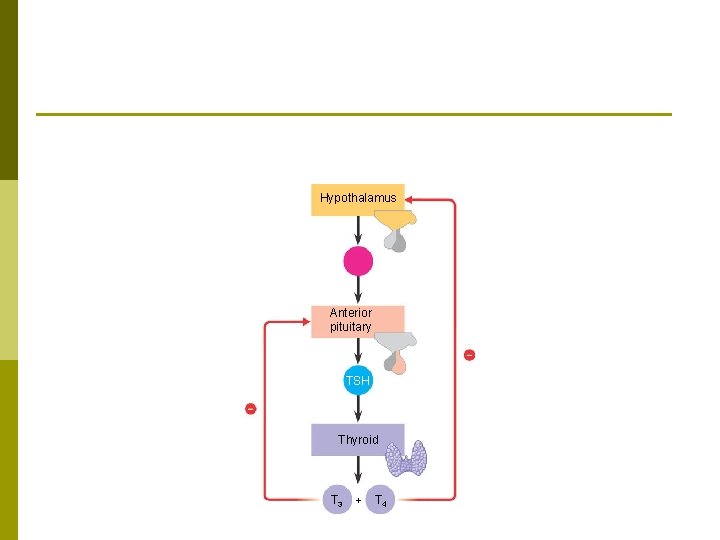
Hypothalamus Anterior pituitary TSH Thyroid T 3 + T 4
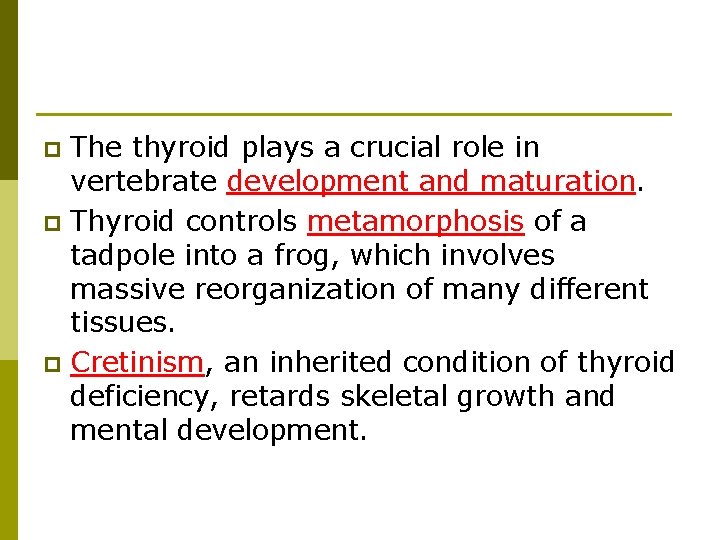
The thyroid plays a crucial role in vertebrate development and maturation. p Thyroid controls metamorphosis of a tadpole into a frog, which involves massive reorganization of many different tissues. p Cretinism, an inherited condition of thyroid deficiency, retards skeletal growth and mental development. p
The thyroid gland has important homeostatic functions. p In adult mammals, thyroid hormones help to maintain normal blood pressure, heart rate, muscle tone, digestion, and reproductive functions. p Throughout the body, T 3 and T 4 are important in bioenergetics, increasing the rate of oxygen consumption and cellular metabolism. p
Too much or too little of these hormones can cause serious metabolic disorders. p Hyperthyroidism is the excessive secretion of thyroid hormones, leading to high body temperature, profuse sweating, weight loss, irritability, and high blood pressure. p An insufficient amount of thyroid hormones is known as hypothyroidism. p This condition cause cretinism in infants. p Adult symptoms include weight gain, lethargy, and cold intolerance. p
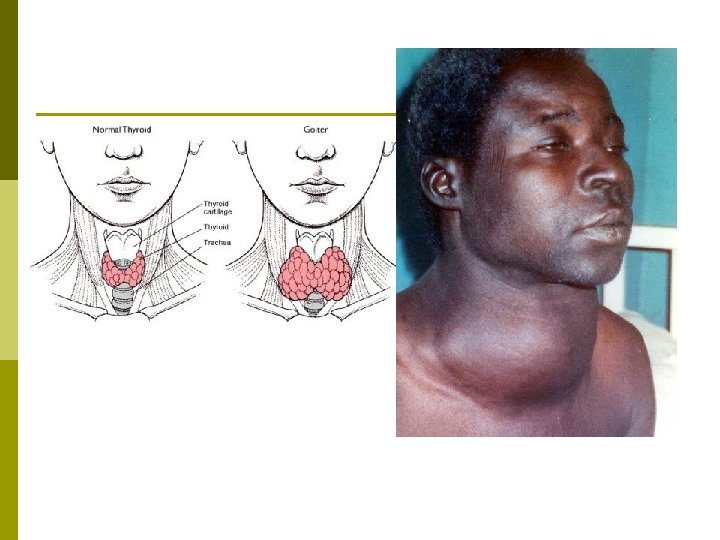
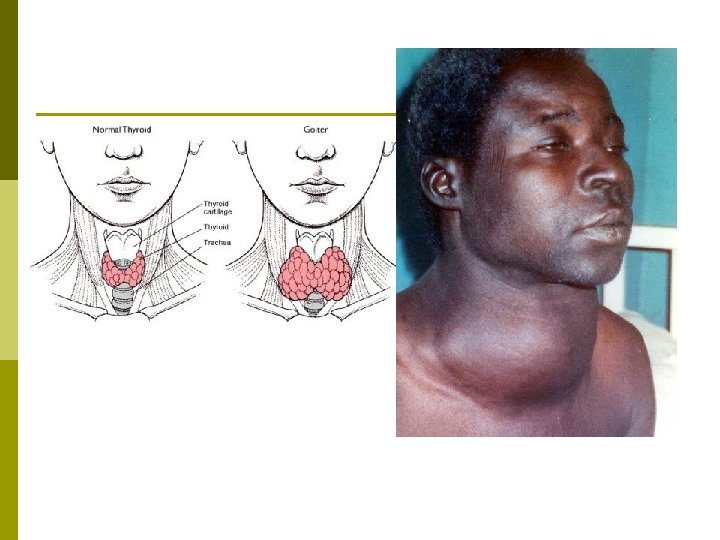
p A deficiency of iodine in the diet can result in goiter, an enlargement of the thyroid gland. Without sufficient iodine, the thyroid gland cannot synthesize adequate amounts of T 3 and T 4. p The resulting low blood levels of these hormones cannot exert negative feedback on the hypothalamus and anterior pituitary. p The pituitary continues to secrete TSH, elevating TSH levels and enlarging the thyroid. p
In addition to cells that produce T 3 and T 4, the mammalian thyroid gland produces calcitonin. p This hormone acts in conjunction with parathyroid hormone to maintain calcium homeostasis. p
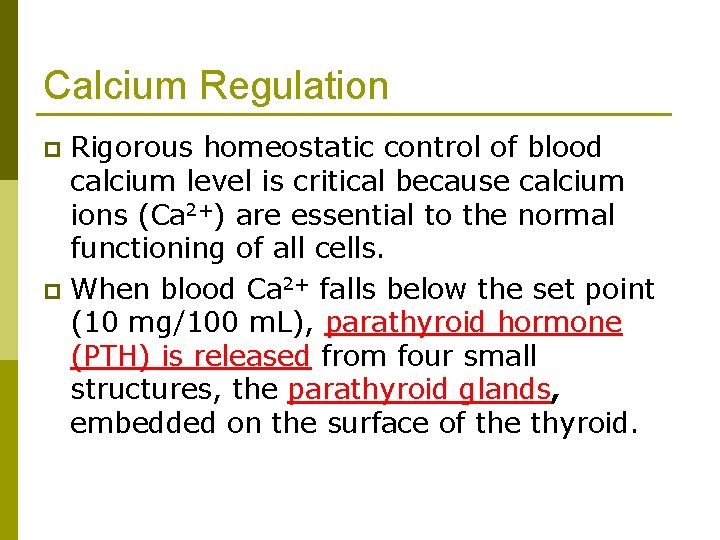
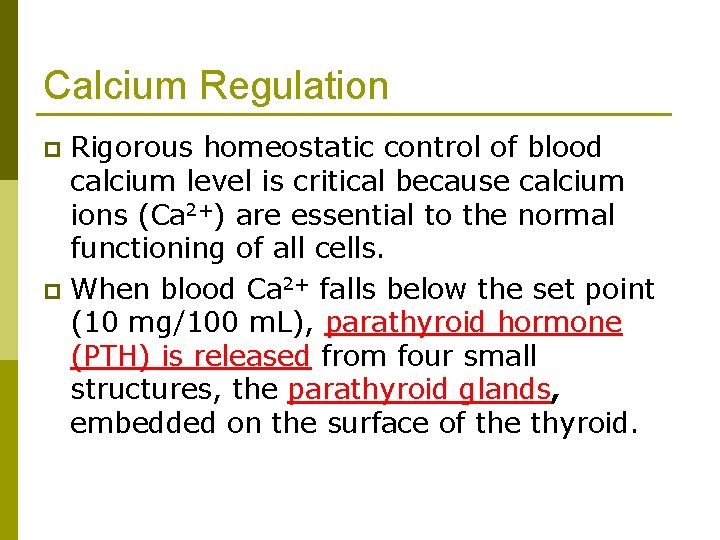
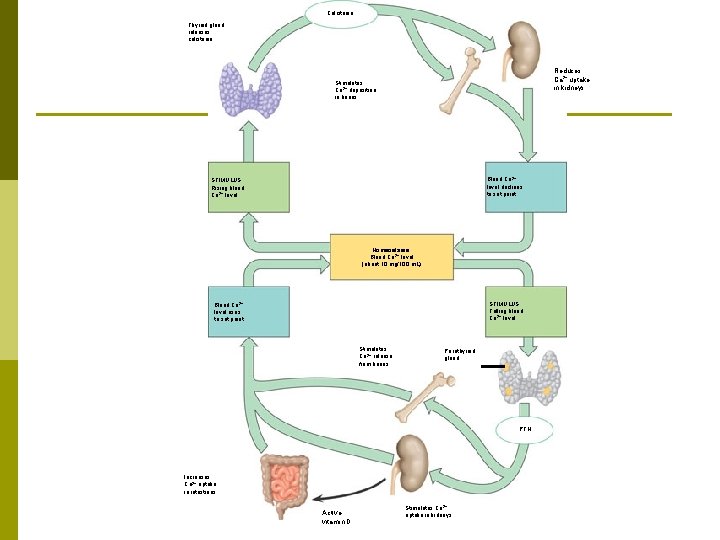
Calcium Regulation Rigorous homeostatic control of blood calcium level is critical because calcium ions (Ca 2+) are essential to the normal functioning of all cells. p When blood Ca 2+ falls below the set point (10 mg/100 m. L), parathyroid hormone (PTH) is released from four small structures, the parathyroid glands, embedded on the surface of the thyroid. p
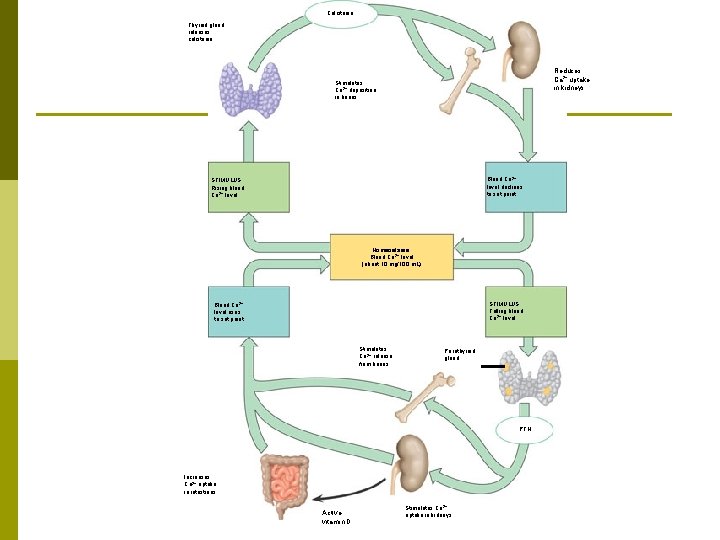
Calcitonin Thyroid gland releases calcitonin. Reduces Ca 2+ uptake in kidneys Stimulates Ca 2+ deposition in bones Blood Ca 2+ level declines to set point STIMULUS: Rising blood Ca 2+ level Homeostasis: Blood Ca 2+ level (about 10 mg/100 m. L) STIMULUS: Falling blood Ca 2+ level Blood Ca 2+ level rises to set point Stimulates Ca 2+ release from bones Parathyroid gland PTH Increases Ca 2+ uptake in intestines Active vitamin D Stimulates Ca 2+ uptake in kidneys
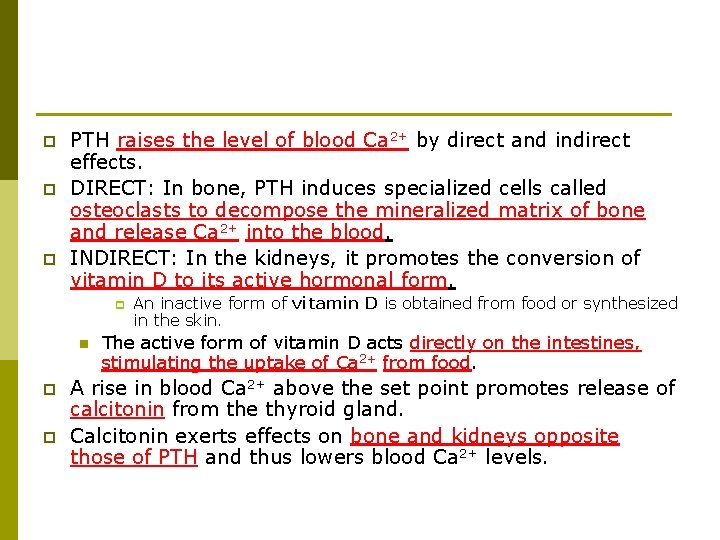
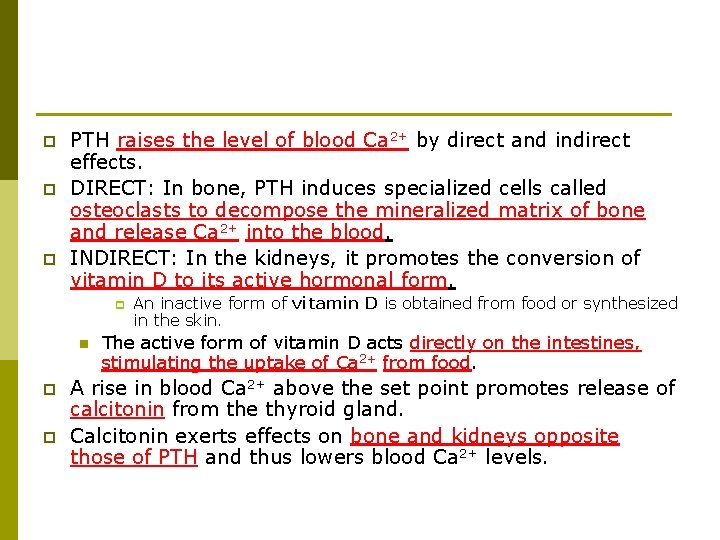
p p p PTH raises the level of blood Ca 2+ by direct and indirect effects. DIRECT: In bone, PTH induces specialized cells called osteoclasts to decompose the mineralized matrix of bone and release Ca 2+ into the blood. INDIRECT: In the kidneys, it promotes the conversion of vitamin D to its active hormonal form. p n p p An inactive form of vitamin D is obtained from food or synthesized in the skin. The active form of vitamin D acts directly on the intestines, stimulating the uptake of Ca 2+ from food. A rise in blood Ca 2+ above the set point promotes release of calcitonin from the thyroid gland. Calcitonin exerts effects on bone and kidneys opposite those of PTH and thus lowers blood Ca 2+ levels.
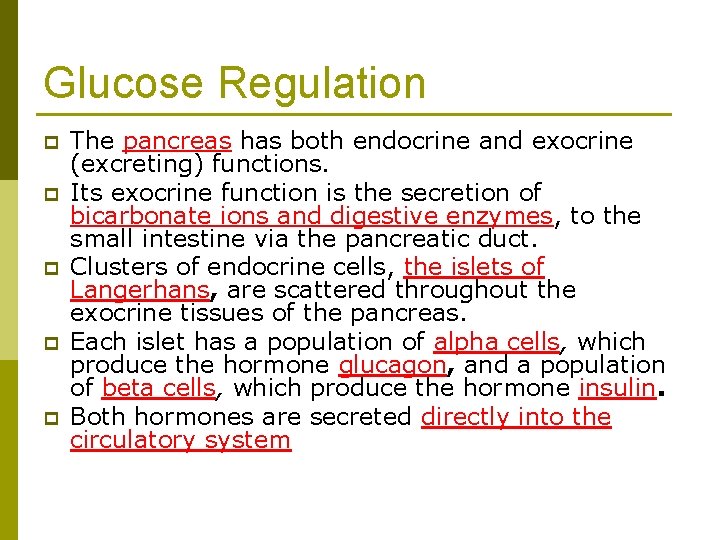
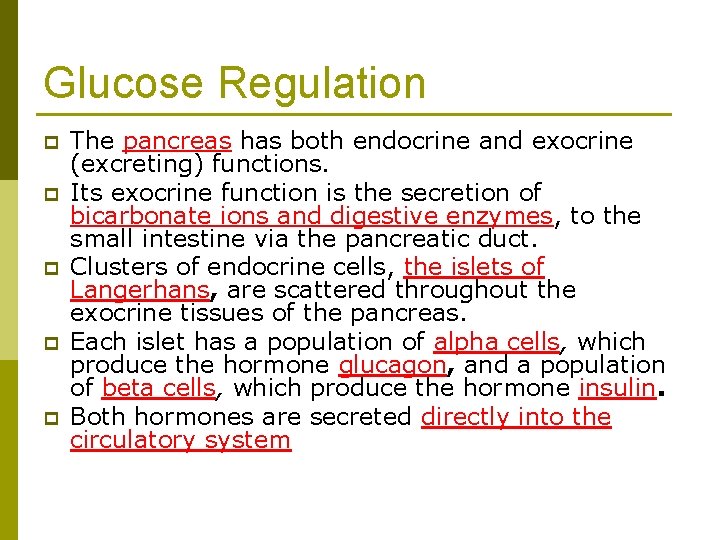
Glucose Regulation p p p The pancreas has both endocrine and exocrine (excreting) functions. Its exocrine function is the secretion of bicarbonate ions and digestive enzymes, to the small intestine via the pancreatic duct. Clusters of endocrine cells, the islets of Langerhans, are scattered throughout the exocrine tissues of the pancreas. Each islet has a population of alpha cells, which produce the hormone glucagon, and a population of beta cells, which produce the hormone insulin. Both hormones are secreted directly into the circulatory system
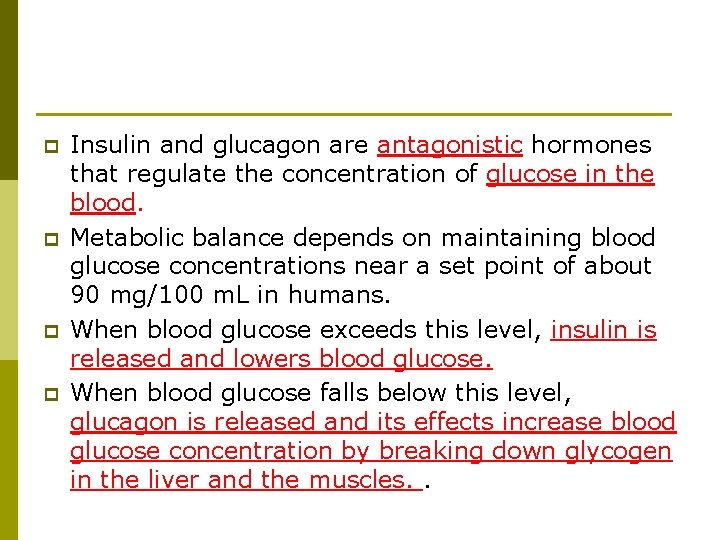
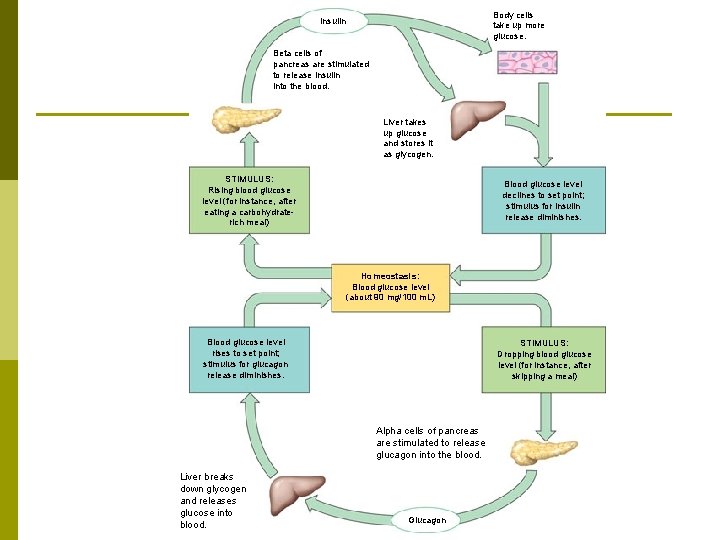
p p Insulin and glucagon are antagonistic hormones that regulate the concentration of glucose in the blood. Metabolic balance depends on maintaining blood glucose concentrations near a set point of about 90 mg/100 m. L in humans. When blood glucose exceeds this level, insulin is released and lowers blood glucose. When blood glucose falls below this level, glucagon is released and its effects increase blood glucose concentration by breaking down glycogen in the liver and the muscles. .
Insulin lowers blood glucose levels by stimulating all body cells (except brain cells) to take up glucose from the blood. p Brain cells can take up glucose without insulin and, thus, have access to circulating fuel at all times. p
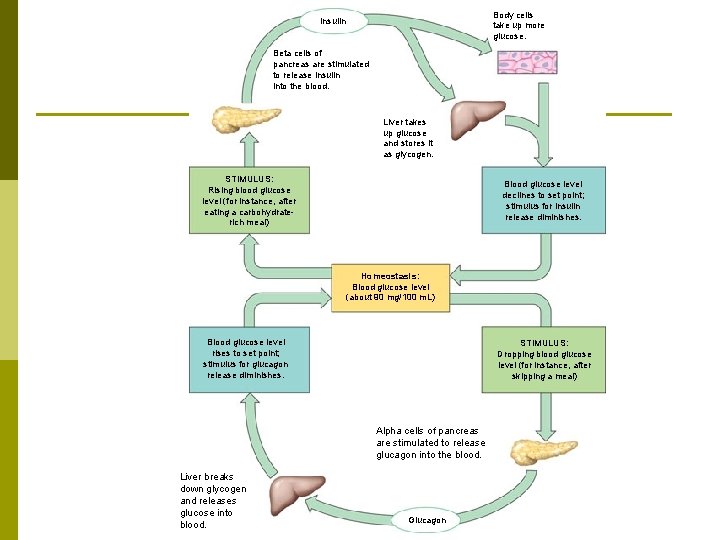
Body cells take up more glucose. Insulin Beta cells of pancreas are stimulated to release insulin into the blood. Liver takes up glucose and stores it as glycogen. STIMULUS: Rising blood glucose level (for instance, after eating a carbohydraterich meal) Blood glucose level declines to set point; stimulus for insulin release diminishes. Homeostasis: Blood glucose level (about 90 mg/100 m. L) Blood glucose level rises to set point; stimulus for glucagon release diminishes. STIMULUS: Dropping blood glucose level (for instance, after skipping a meal) Alpha cells of pancreas are stimulated to release glucagon into the blood. Liver breaks down glycogen and releases glucose into blood. Glucagon
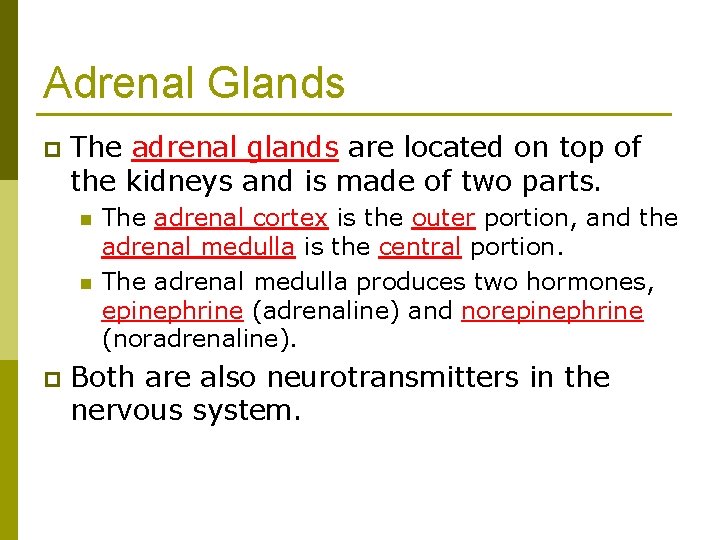
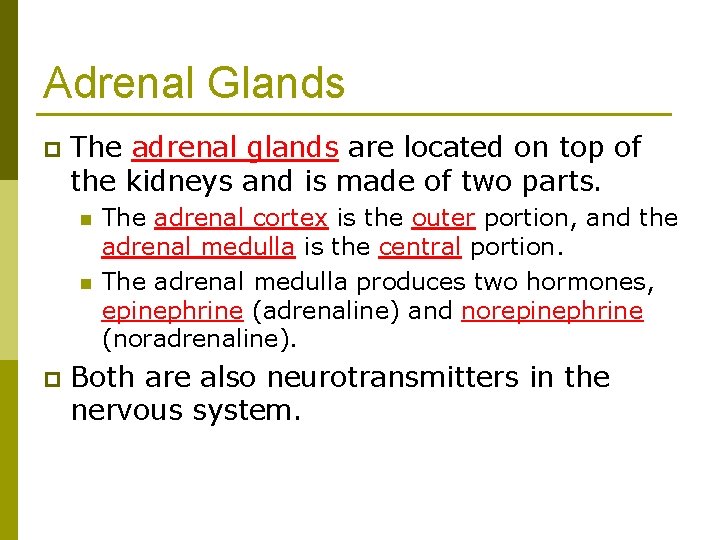
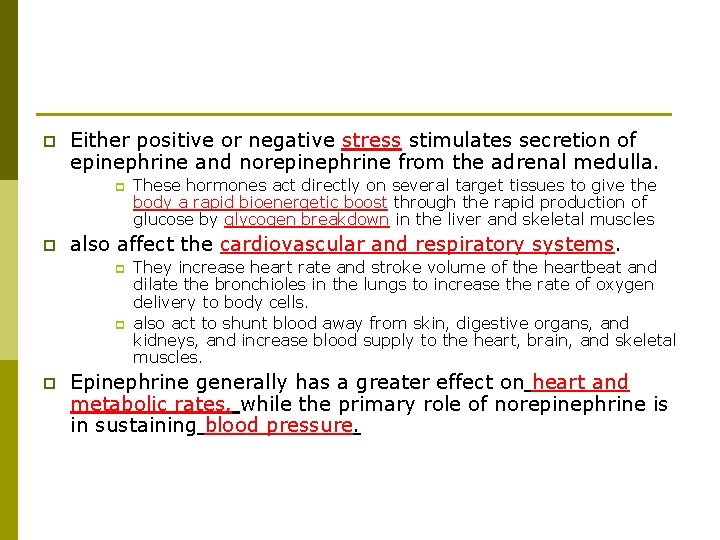
Adrenal Glands p The adrenal glands are located on top of the kidneys and is made of two parts. n n p The adrenal cortex is the outer portion, and the adrenal medulla is the central portion. The adrenal medulla produces two hormones, epinephrine (adrenaline) and norepinephrine (noradrenaline). Both are also neurotransmitters in the nervous system.
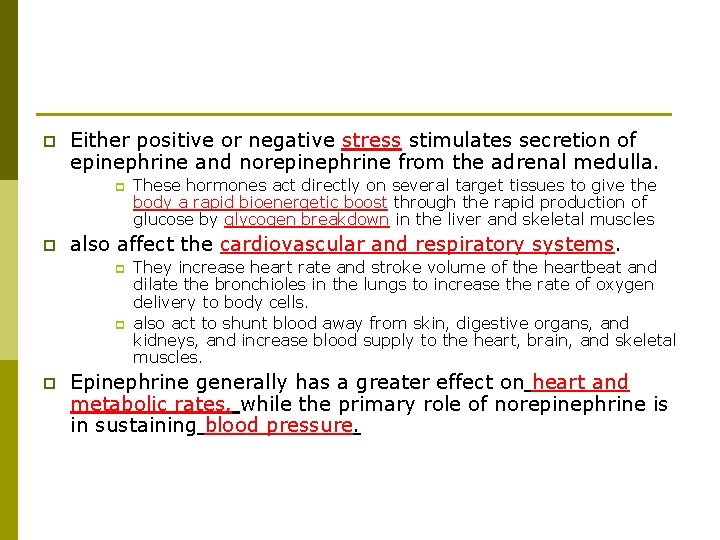
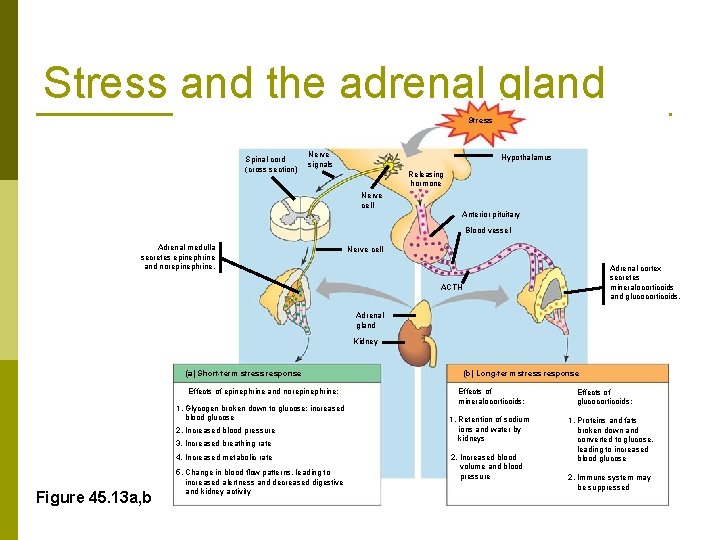
p Either positive or negative stress stimulates secretion of epinephrine and norepinephrine from the adrenal medulla. p p also affect the cardiovascular and respiratory systems. p p p These hormones act directly on several target tissues to give the body a rapid bioenergetic boost through the rapid production of glucose by glycogen breakdown in the liver and skeletal muscles They increase heart rate and stroke volume of the heartbeat and dilate the bronchioles in the lungs to increase the rate of oxygen delivery to body cells. also act to shunt blood away from skin, digestive organs, and kidneys, and increase blood supply to the heart, brain, and skeletal muscles. Epinephrine generally has a greater effect on heart and metabolic rates, while the primary role of norepinephrine is in sustaining blood pressure.
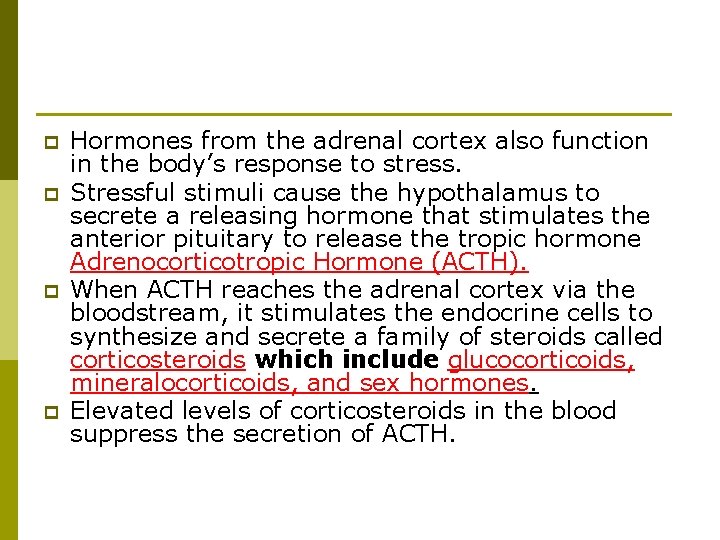
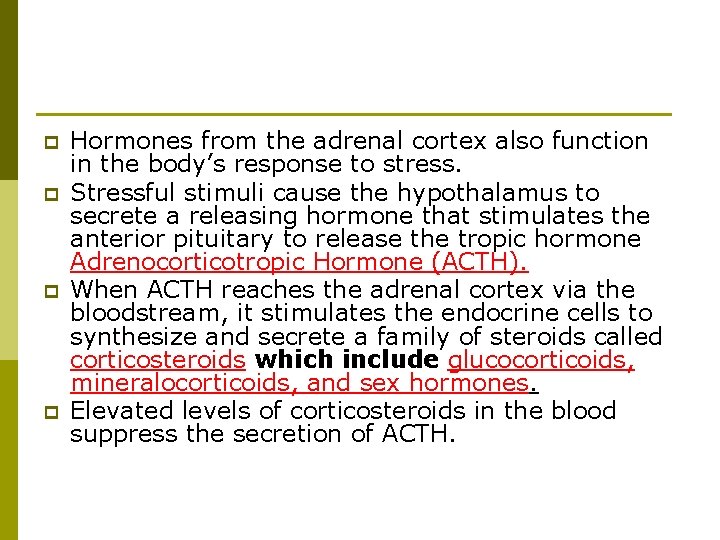
p p Hormones from the adrenal cortex also function in the body’s response to stress. Stressful stimuli cause the hypothalamus to secrete a releasing hormone that stimulates the anterior pituitary to release the tropic hormone Adrenocorticotropic Hormone (ACTH). When ACTH reaches the adrenal cortex via the bloodstream, it stimulates the endocrine cells to synthesize and secrete a family of steroids called corticosteroids which include glucocorticoids, mineralocorticoids, and sex hormones. Elevated levels of corticosteroids in the blood suppress the secretion of ACTH.
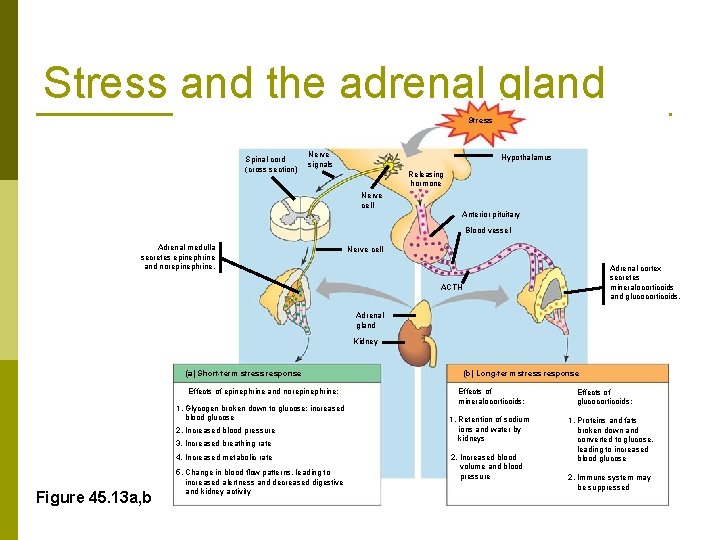
Stress and the adrenal gland Stress Spinal cord (cross section) Nerve signals Hypothalamus Releasing hormone Nerve cell Anterior pituitary Blood vessel Adrenal medulla secretes epinephrine and norepinephrine. Nerve cell Adrenal cortex secretes mineralocorticoids and glucocorticoids. ACTH Adrenal gland Kidney (a) Short-term stress response Effects of epinephrine and norepinephrine: 1. Glycogen broken down to glucose; increased blood glucose 2. Increased blood pressure 3. Increased breathing rate 4. Increased metabolic rate Figure 45. 13 a, b 5. Change in blood flow patterns, leading to increased alertness and decreased digestive and kidney activity (b) Long-term stress response Effects of mineralocorticoids: 1. Retention of sodium ions and water by kidneys 2. Increased blood volume and blood pressure Effects of glucocorticoids: 1. Proteins and fats broken down and converted to glucose, leading to increased blood glucose 2. Immune system may be suppressed
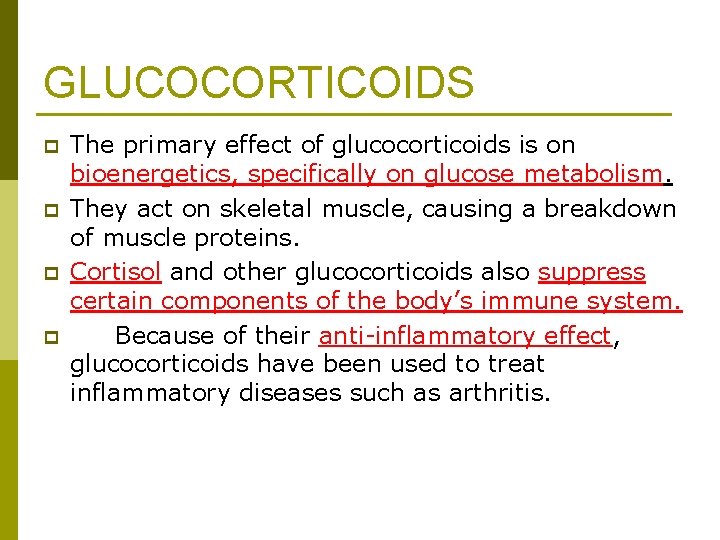
GLUCOCORTICOIDS p p The primary effect of glucocorticoids is on bioenergetics, specifically on glucose metabolism. They act on skeletal muscle, causing a breakdown of muscle proteins. Cortisol and other glucocorticoids also suppress certain components of the body’s immune system. Because of their anti-inflammatory effect, glucocorticoids have been used to treat inflammatory diseases such as arthritis.
Mineralocorticoids act principally on salt and water balance. p Aldosterone stimulates cells in the kidneys to reabsorb Na+ and water from filtrate, raising blood pressure and volume. p
p p Gonadal steroids regulate growth, development, reproductive cycles, and sexual behavior. The gonads are the primary source of the sex hormones. Their secretion is controlled by gonadotropins (FSH and LH) from the anterior pituitary gland. FSH and LH production is controlled by a releasing hormone from the hypothalamus, Gn. RH (gonadotropin-releasing hormone).
The gonads produce and secrete three major categories of steroid hormones: androgens, estrogens, and progestins. p All three types are found in males and females but in different proportions. p Sex hormones affect growth and development and regulate reproductive cycles and sexual behavior. p
ANDROGENS p p The testes primarily synthesize androgens, the main one being testosterone. Androgens promote development and maintenance of male sex characteristics. Androgens produced early in development determine whether a fetus develops as a male or a female. At puberty, high levels of androgens are responsible for the development of male secondary sex characteristics, including male patterns of hair growth, a low voice, and increased muscle mass and bone mass typical of males.
ESTROGEN Estrogens, the most important of which is estradiol, are responsible for the development and maintenance of the female reproductive system and the development of female secondary sex characteristics. p In mammals, progestins, which include progesterone, are involved in promoting uterine lining growth to support the growth and development of an embryo. p
Pineal Gland p p p The pineal gland is a small mass of tissue near the center of the mammalian brain. The pineal gland synthesizes and secretes the hormone melatonin. Depending on the species, the pineal gland contains lightsensitive cells or has nervous connections from the eyes that control its secretory activity. Melatonin regulates functions related to light and to seasons marked by changes in day length. Its primary functions are related to biological rhythms associated with reproduction. p p p Melatonin secretion is regulated by light/dark cycles. Melatonin is secreted at night, and the amount secreted depends on the length of the night. Thus, melatonin production is a link between a biological clock and daily or seasonal activities such as reproduction.