Endocrine Organs Dr Zahiri The endocrine system includes

























- Slides: 57
Endocrine Organs Dr. Zahiri
� The endocrine system includes a number of different cells, structures, and organs which are not necessarily related at the gross anatomical level. � 1. Histologically the endocrine system includes all structures and organs that have endocrine secretory cells as the parenchymal tissue. � 2. Components of the endocrine system are functionally related in that they synthesize and secrete hormones (chemical messengers) which regulate, coordinate, and integrate functions of cells which are not in physical contact with the hormone producing cells.
a. Several categories of biological chemicals are used as hormones. � (1) Peptides, proteins, and glycoproteins (2) Steroids � (3) Amino acid analogues and derivatives � � b. Hormones are secreted into the tissue fluid in connective tissue, but in most cases the secretions quickly enter the circulatory system.
B. Endocrine glandular structures are classified according to cell type and arrangement of cells: 1. Unicellular endocrine units occur as single cells in another tissue. � 2. Neurosecretory endocrine units contain cells which are structurally similar to neurons. � 3. Cord and clump endocrine units contain cells arranged in linear arrays and/or clusters. � 4. Follicular endocrine units contain epithelial cells which form the walls of epithelial spheres with partially formed secretory product localized inside sphere. �

C. Cellular morphology of endocrine cells � varies depending on the chemical nature of the secretory product secreted by the cells. � 1. Protein and glycoprotein secreting cells contain extensive r. ER, have well-developed Golgi bodies, and frequently accumulate acidophilic secretory granules in their peripheral cytoplasm. � 2. Steroid secreting cells contain extensive s. ER, contain numerous mitochondria with tubular cristae, and often contain numerous lipid droplets. � 3. Amino acid and catecholamine secreting cells contain small secretory or storage granules similar to synaptic vesicles found in axonal endings in neurons, but lack extensive s. ER or r. ER.

E. Components (cells, structures, organs) comprising the endocrine "system" 1. Endocrine organs a. Thyroid gland b. Parathyroid gland c. Adrenal gland d. Pituitary gland (hypophysis) e. Pineal gland � 2. Endocrine cells within organs of other systems a. Islets of Langerhans in the pancreas b. b. Juxtaglomerular (JG) cells in the kidney c. c. Leydig interstitial cells in the testis d. d. Granulosa, thecal, and interstitial cells in the ovary e. e. Solitary endocrine (or neuroendocrine) cells in the walls of digestive and respiratory organs and the heart
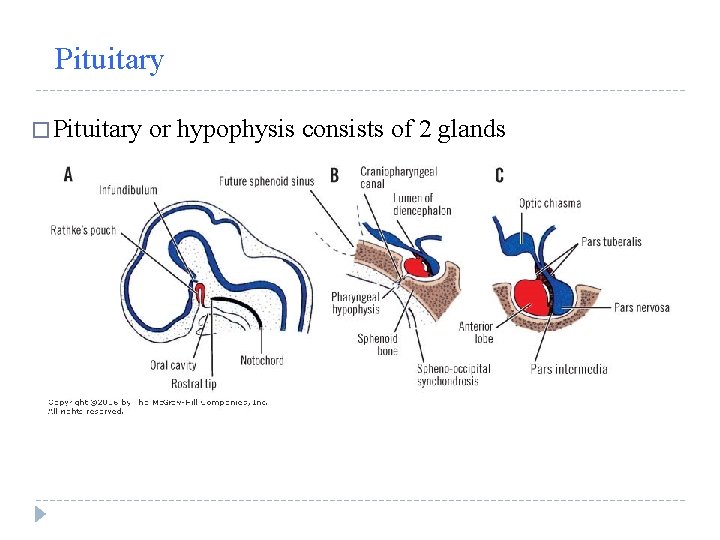
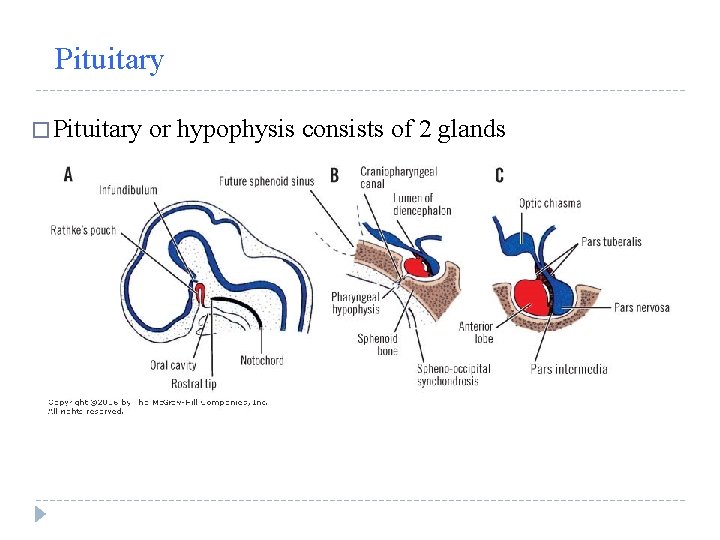
Pituitary � Pituitary or hypophysis consists of 2 glands
Pituitary � Pituitary or hypophysis consists of 2 glands � Neurohypophysis § § § (posterior pituitary) Median eminence Infundibulum Pars nervosa � Adenohypophysis o o o pars distalis (anterior lobe) pars tuberalis (around infundibulum) pars intermedia

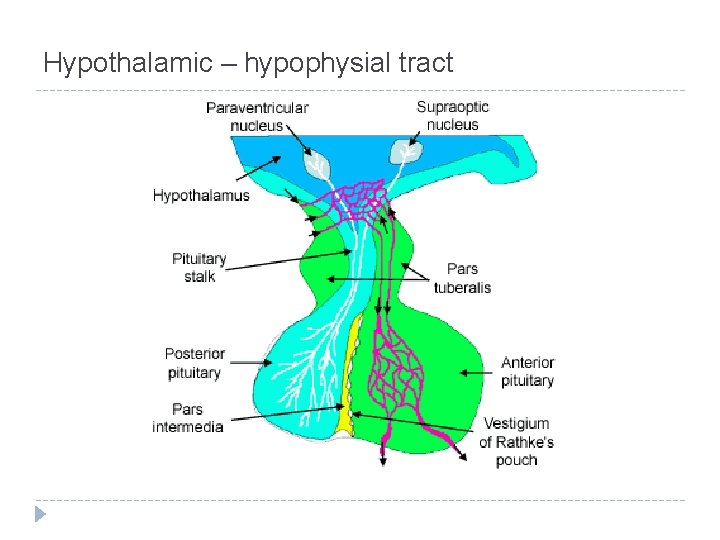
Pituitary Vasculature Hypothalmo-hypophyseal portal vessels delivers neurosecretory hormones from median eminence to the secondary capillary plexus of adenohypophysis � Ending of axons of neurons that originate in various portions of hypothalamus liberate releasing or inhibiting factors directly into primary capillary bed, in this way they differ from other nerve ending � Artery/vein system supplying and draining neurohypophysis �
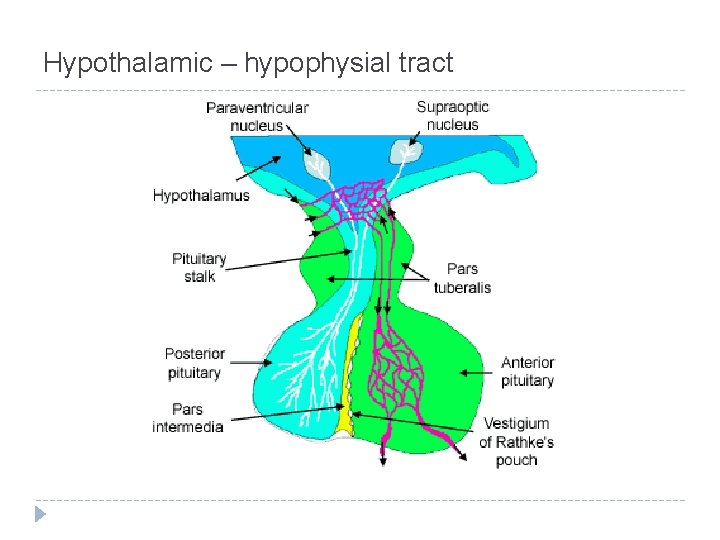
Hypothalamic – hypophysial tract
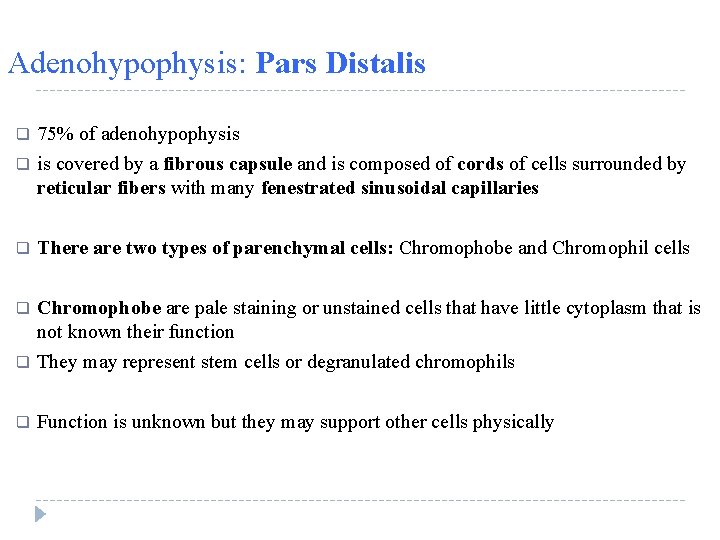
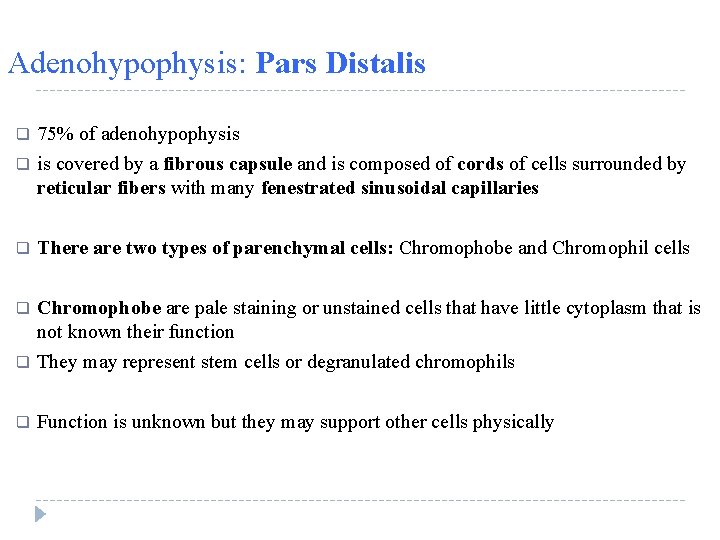
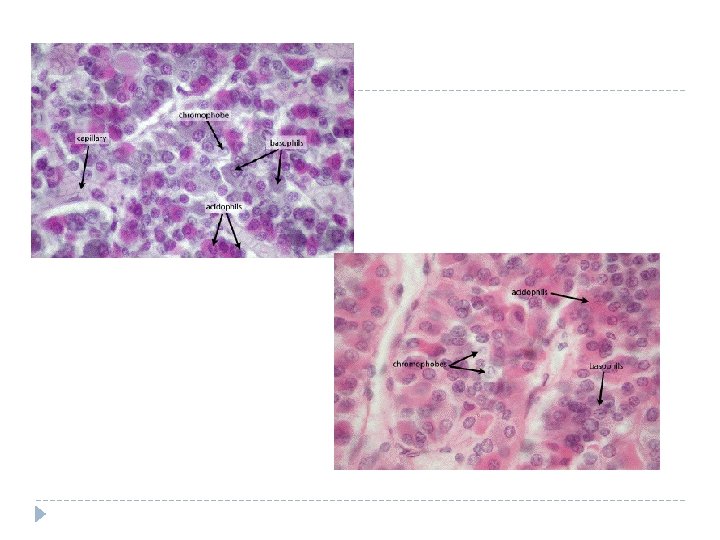
Adenohypophysis: Pars Distalis q 75% of adenohypophysis is covered by a fibrous capsule and is composed of cords of cells surrounded by reticular fibers with many fenestrated sinusoidal capillaries q There are two types of parenchymal cells: Chromophobe and Chromophil cells q q Chromophobe are pale staining or unstained cells that have little cytoplasm that is not known their function They may represent stem cells or degranulated chromophils q Function is unknown but they may support other cells physically q
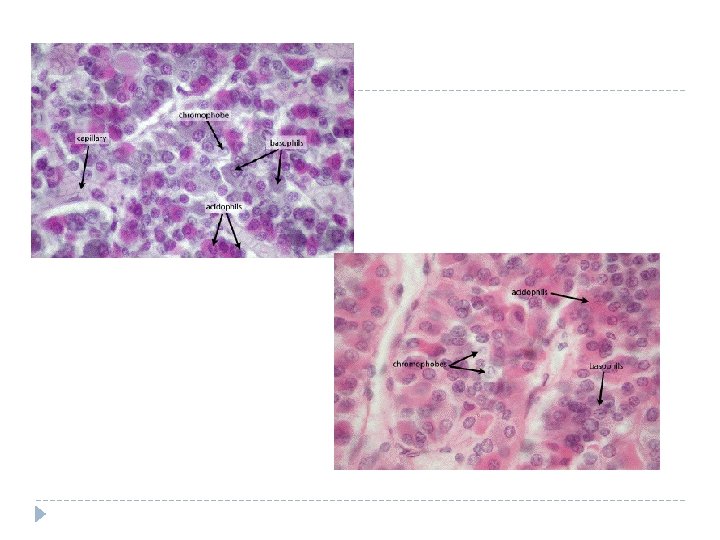

Adenohypophysis: Pars Distalis q Chromophil cells are those cells that have affinity for dyes are two types: acidophils and basophils q Acidophils stain red or orange and more numerous than basophils, they are consist of: • Somatotrophs and mammotrophs q Basophils stain blue and located at periphery of pars distalis, they are consist of: • Thyrotrophs, gonadotrophs, corticotrophs
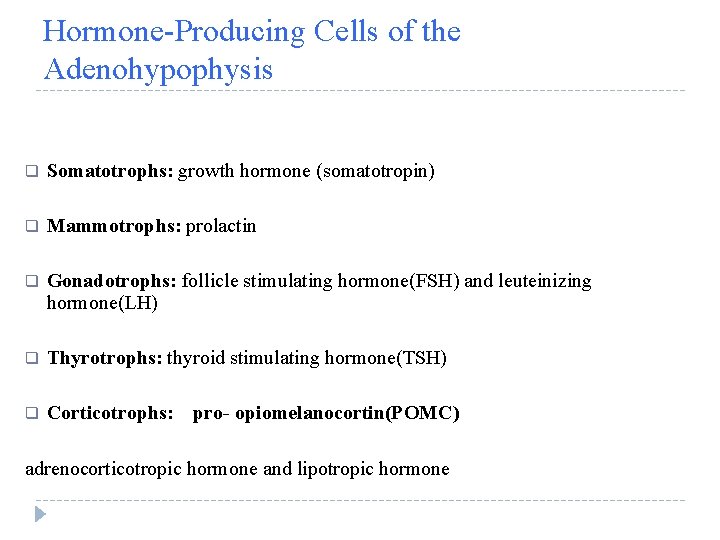
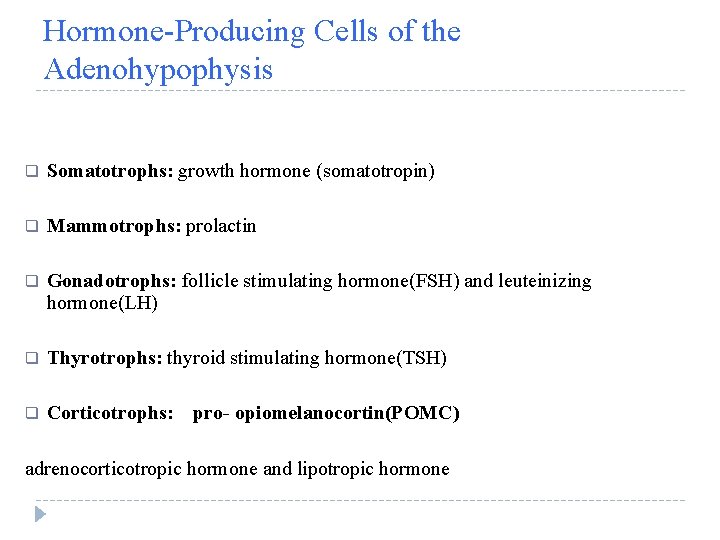
Hormone-Producing Cells of the Adenohypophysis q Somatotrophs: growth hormone (somatotropin) q Mammotrophs: prolactin q Gonadotrophs: follicle stimulating hormone(FSH) and leuteinizing hormone(LH) q Thyrotrophs: thyroid stimulating hormone(TSH) q Corticotrophs: pro- opiomelanocortin(POMC) adrenocorticotropic hormone and lipotropic hormone

Release and Release-Inhibiting Factors q Release and inhibiting factors are proteins and amino acid derivatives released into median eminence that flow to adenohypophysis via portal vessels and control pituitary cells or they are hormones which are released by target cells q SRH increases growth hormone Somatostatin decreases growth hormone PRH and oxytocin increases prolactin Dopamine and PIF decreases prolactin TRH increases tyrotropin (TSH) T 3 and T 4 decreases Tyrotropin (TSH) Gn. RH increases LH and FSH Hormones of testis and ovary decreases LH and FSH CRH increases ACTH q q q q

Pars tuberalis q Pars tuberalis surrounds infundibulum (hypophysial stalk) q It is composed of cuboidal to low columnar epithelial cells q These cells are basophilic and mostly gonadotrophs q Pars tuberalis do not secrete any specific hormone
Pars intermedia q Pars intermedia is rudimentary in humans q It is composed of cuboidal cell which are forming follicles containing colloid q Sometimes houses cords of basophils which are synthesizing proopiomelanocortin (POMC) that forms melanocyte stimulating hormone, melanocyte stimulating hormone (MSH) and ß-endorphin q In humans function is unknown; well-developed in other mammals

Neurohypophysis q Includes the infundibulum, median eminence, and pars nervosa q Pars nervosa is not an endocrine gland q In pars nervosa distal ends of unmyelinated axon of hypothalamohypophysial tracts terminate in vicinity of the fenestrated capillaries q The cell body of neurosecretory cells are located in hypothalamus q These axons supported by pituicytes which are astrocyte-like glial cells that occupy 25% of the volume of the pars nervosa q Herring bodies are distentions of the axons not only at their termini but also along their lenght which are representation of accumulation s of neuroseretory granules

q Vasopressin (ADH), Oxytocin, and a carrier protein known as neurophysin are produced in nuclei of hypothalamus( supra optic, paraventricular) and travel down to neurohypophysis q Vasopressin (ADH) is a vasoconstrictor and also affects collecting ducts of kidney and cause water resorption q Oxytocin has effect on smooth muscle cells contraction, especially during parturition, milk ejection, and sexual intercourse
Diabetes insipidus (DI) polyuria and polydipsia � deficiency of arginine vasopressin (AVP), also known as antidiuretic hormone (ADH).

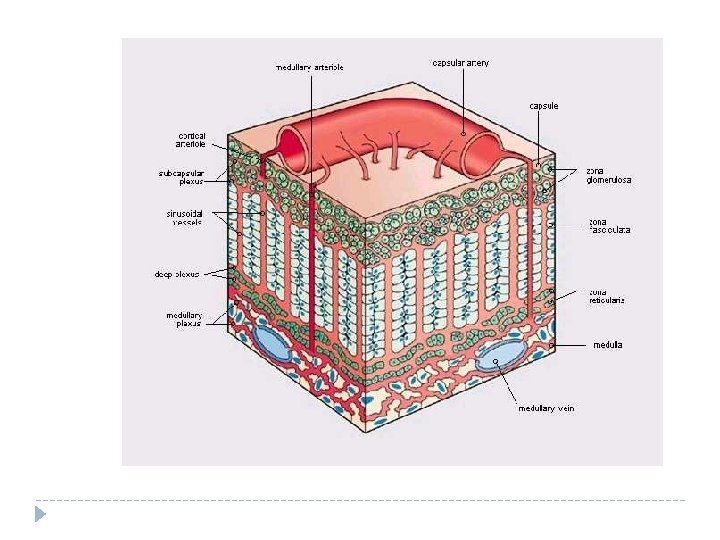
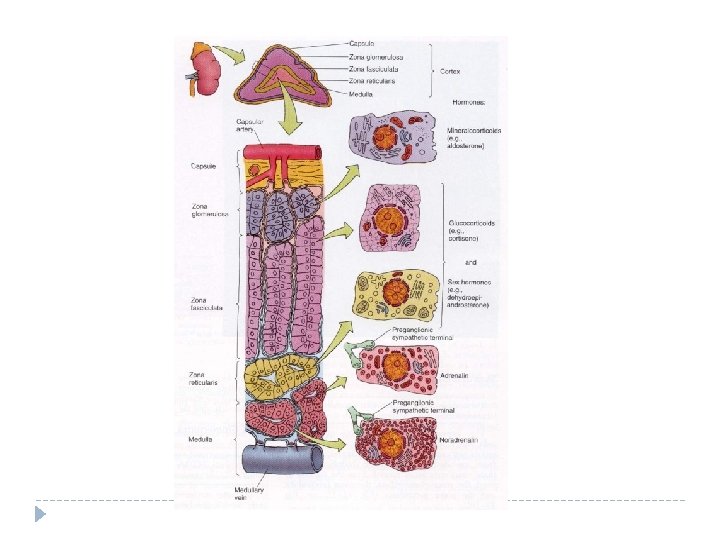
Adrenal Gland q q q Adrenal gland Lies at superior pole of kidney in peri-renal adipose tissue It has a capsule of dense irregular connective tissue with septa Stroma is consists of reticular fibers and fibroblasts q Adrenal gland has two distinct parts that are integrated into one organ Outer cortex and inner medulla q Cortex is mesodermal in origin produces steroid hormone Medulla is from neural crest (ectoderm) produces vasoactive amines Both areas are highly vascularized with fenestrated capillaries supplied by cortical arterioles and medullary arterioles with some communication between them q q
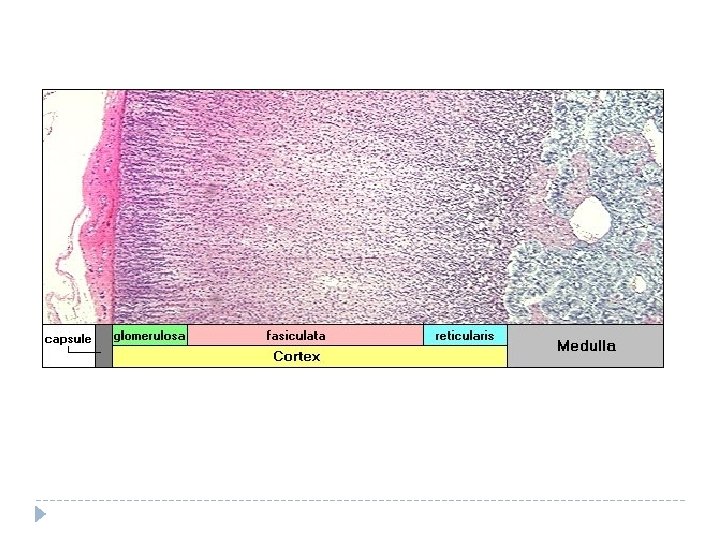
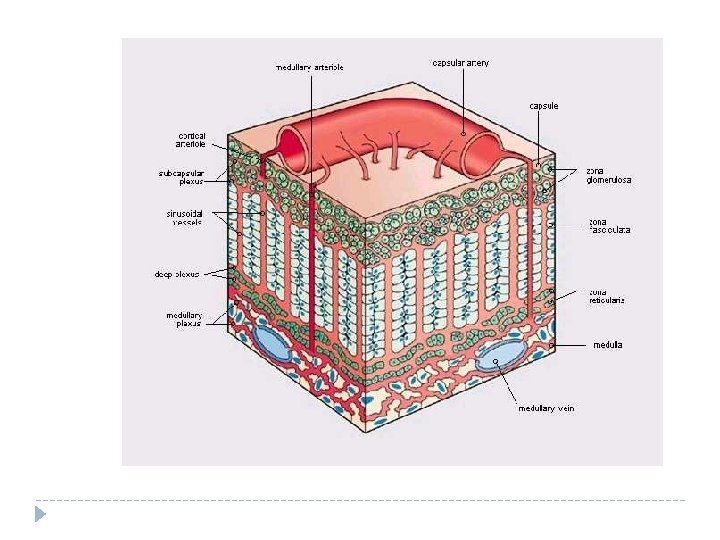
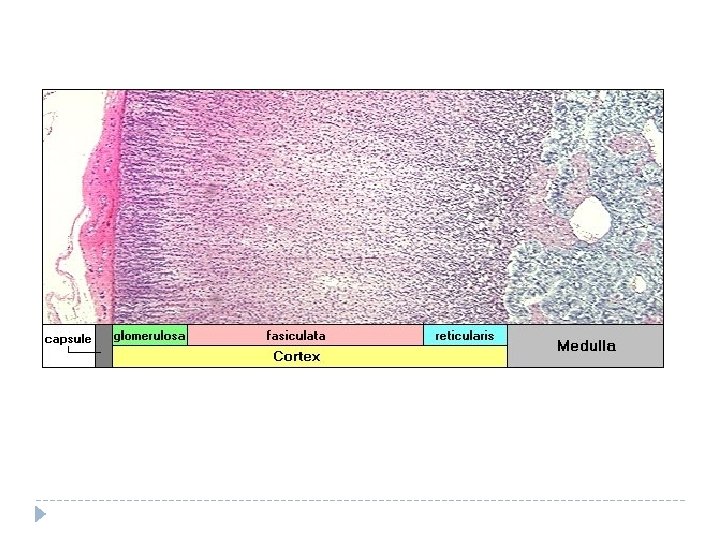
Adrenal Cortex q Adrenal cortex is composed of 3 distinct layers; although in humans these are not always easily distinguished q Zona glomerulosa: outer layer Zona fasciculata: middle layer Zona reticularis: inner layer q q
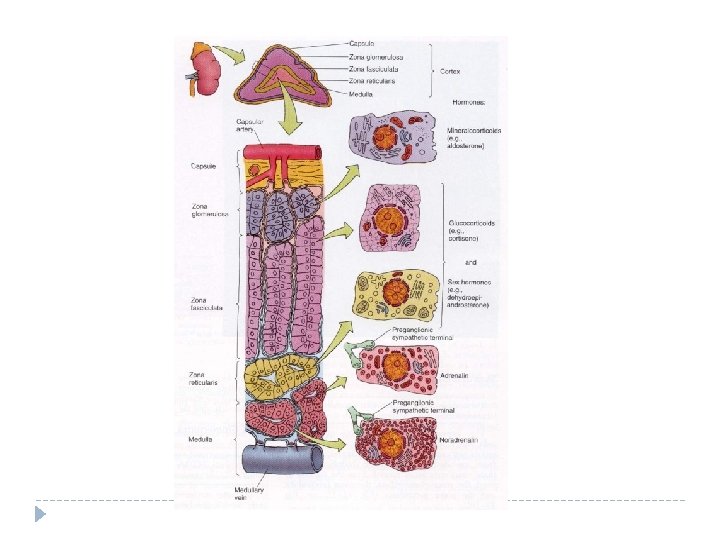
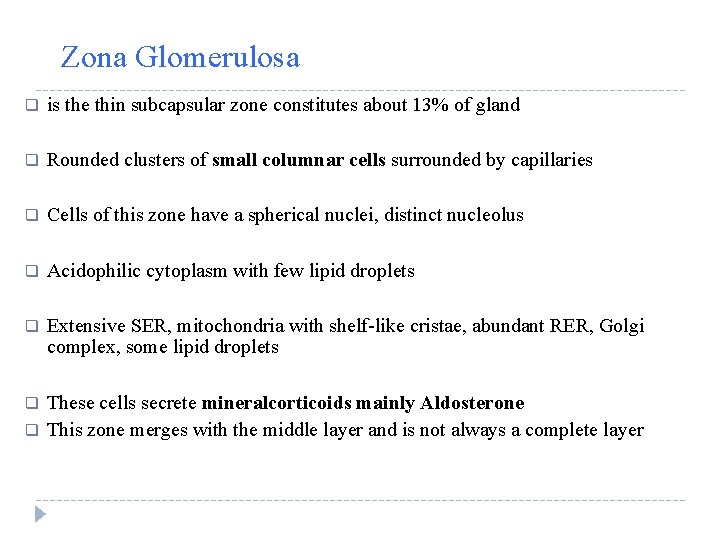
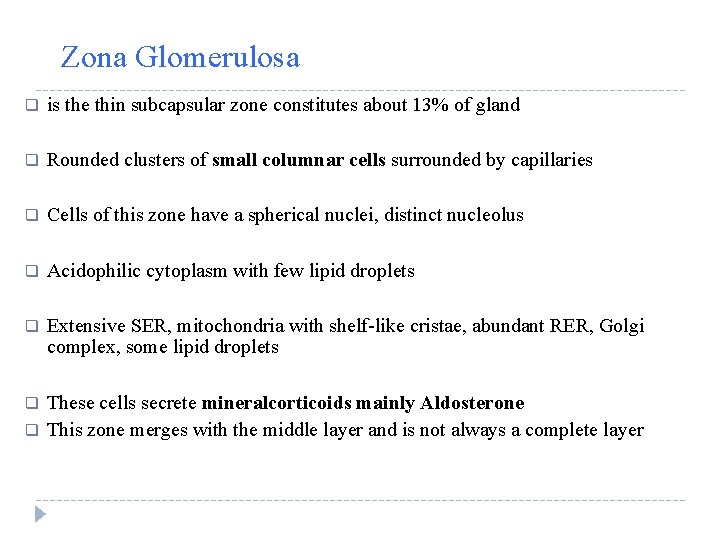
Zona Glomerulosa q is the thin subcapsular zone constitutes about 13% of gland q Rounded clusters of small columnar cells surrounded by capillaries q Cells of this zone have a spherical nuclei, distinct nucleolus q Acidophilic cytoplasm with few lipid droplets q Extensive SER, mitochondria with shelf-like cristae, abundant RER, Golgi complex, some lipid droplets q These cells secrete mineralcorticoids mainly Aldosterone This zone merges with the middle layer and is not always a complete layer q


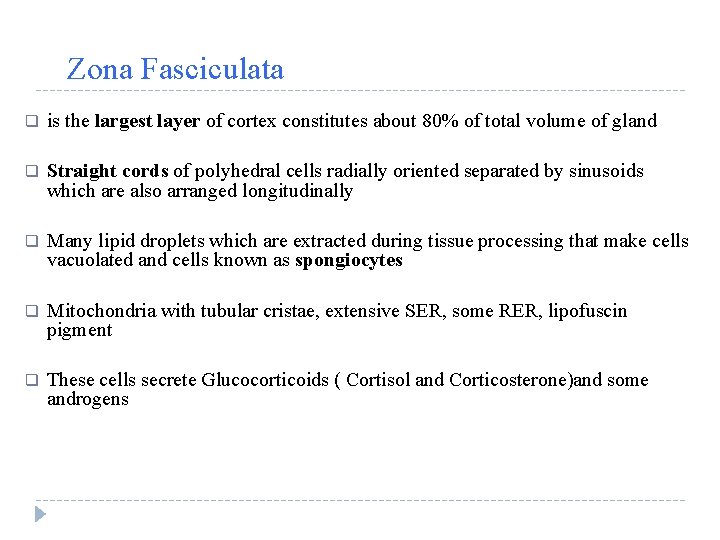
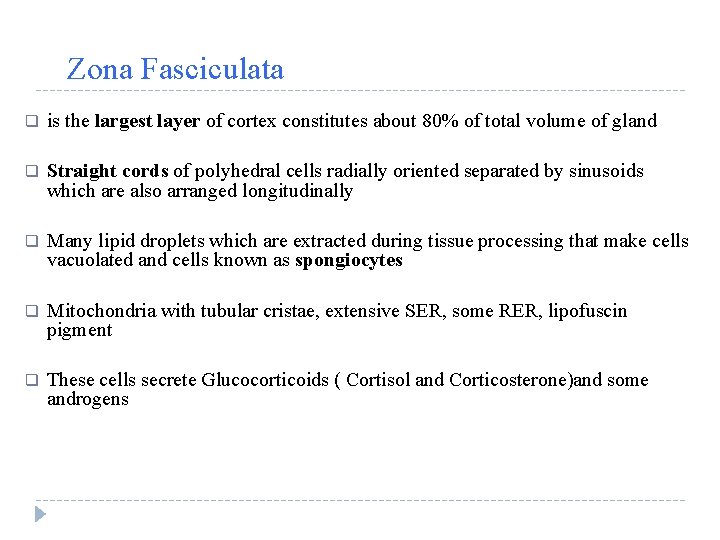
Zona Fasciculata q is the largest layer of cortex constitutes about 80% of total volume of gland q Straight cords of polyhedral cells radially oriented separated by sinusoids which are also arranged longitudinally q Many lipid droplets which are extracted during tissue processing that make cells vacuolated and cells known as spongiocytes q Mitochondria with tubular cristae, extensive SER, some RER, lipofuscin pigment q These cells secrete Glucocorticoids ( Cortisol and Corticosterone)and some androgens


Zona Reticularis q q q q About 7% of gland volume Cells are alike to spongiocytes but smaller and have fewer lipid droplets mitochondria with tubular cristae, large amount of lipofuscin pigments Dark staining acidophilic cytoplasm Cells of this zone forming anastomosing cords Produce some androgens and glucocorticoids Some macrophages may be present

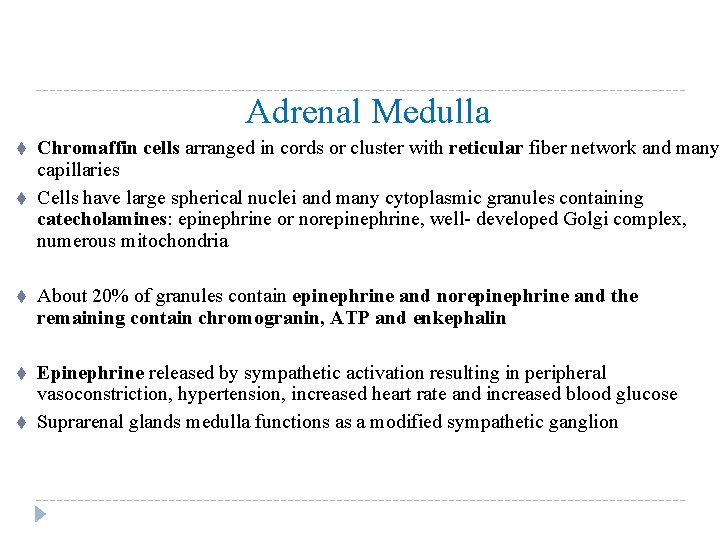
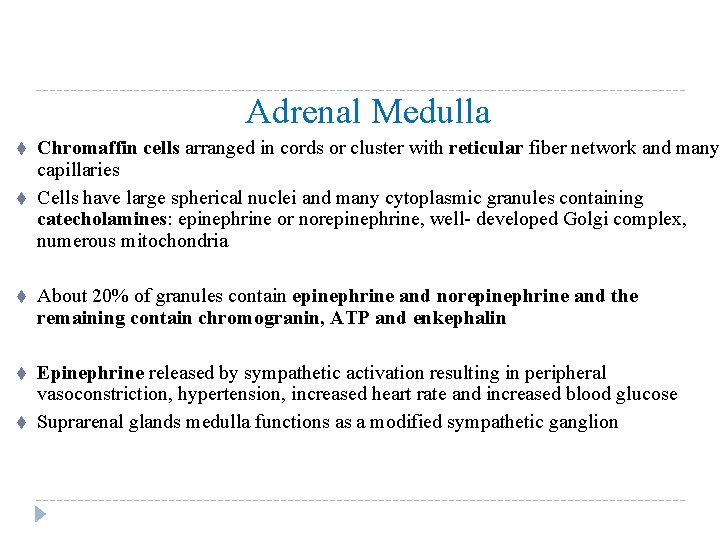
Adrenal Medulla t t Chromaffin cells arranged in cords or cluster with reticular fiber network and many capillaries Cells have large spherical nuclei and many cytoplasmic granules containing catecholamines: epinephrine or norepinephrine, well- developed Golgi complex, numerous mitochondria t About 20% of granules contain epinephrine and norepinephrine and the remaining contain chromogranin, ATP and enkephalin t Epinephrine released by sympathetic activation resulting in peripheral vasoconstriction, hypertension, increased heart rate and increased blood glucose Suprarenal glands medulla functions as a modified sympathetic ganglion t

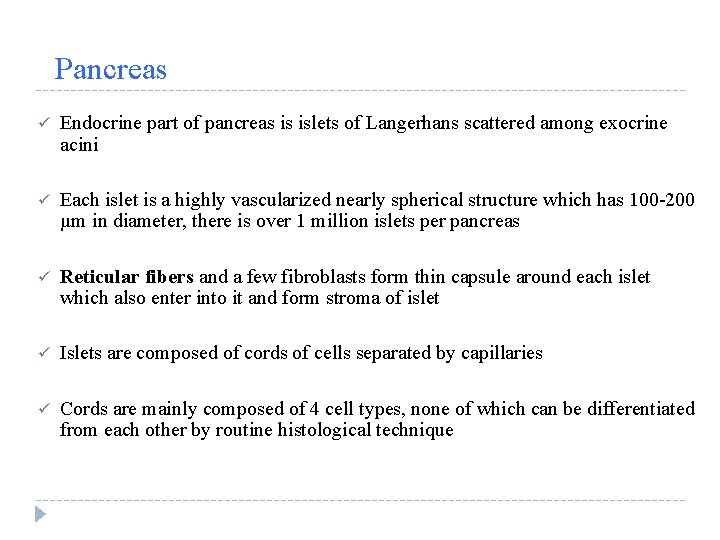
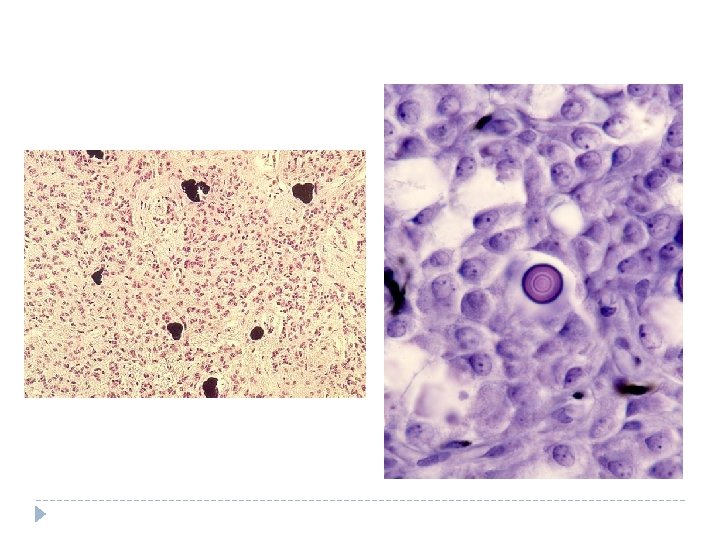
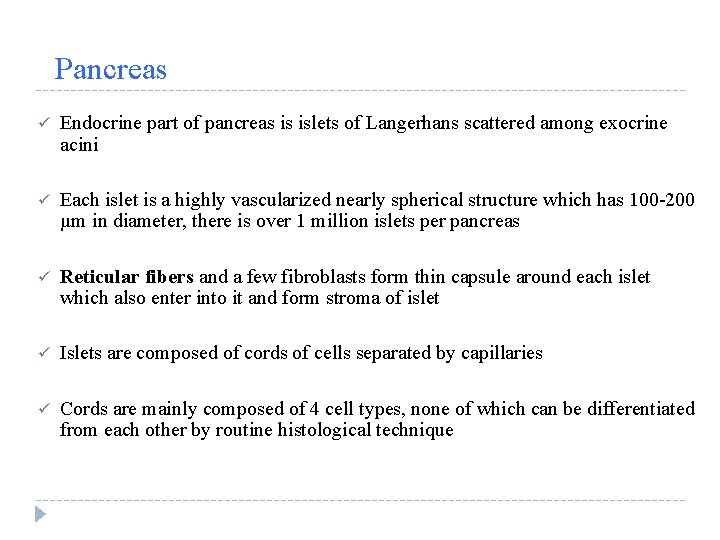
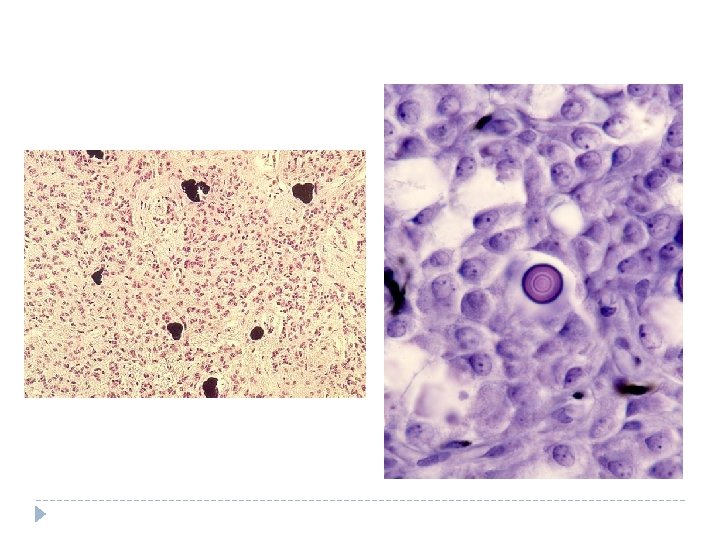
Pancreas ü Endocrine part of pancreas is islets of Langerhans scattered among exocrine acini ü Each islet is a highly vascularized nearly spherical structure which has 100 -200 µm in diameter, there is over 1 million islets per pancreas ü Reticular fibers and a few fibroblasts form thin capsule around each islet which also enter into it and form stroma of islet ü Islets are composed of cords of cells separated by capillaries ü Cords are mainly composed of 4 cell types, none of which can be differentiated from each other by routine histological technique

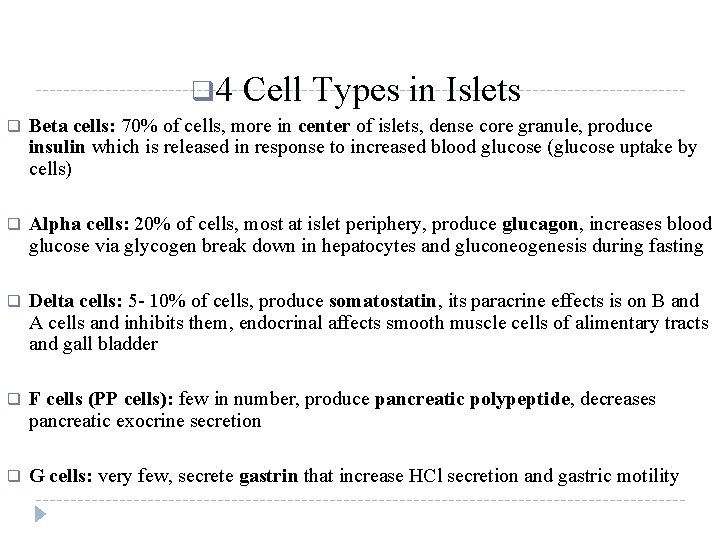
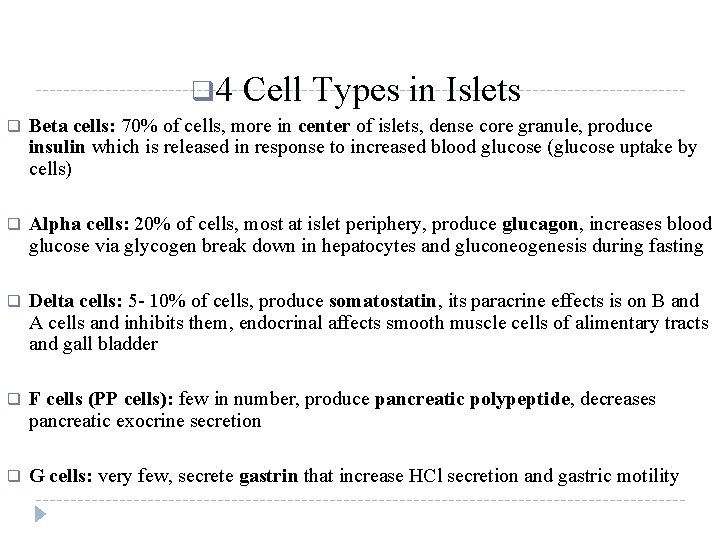
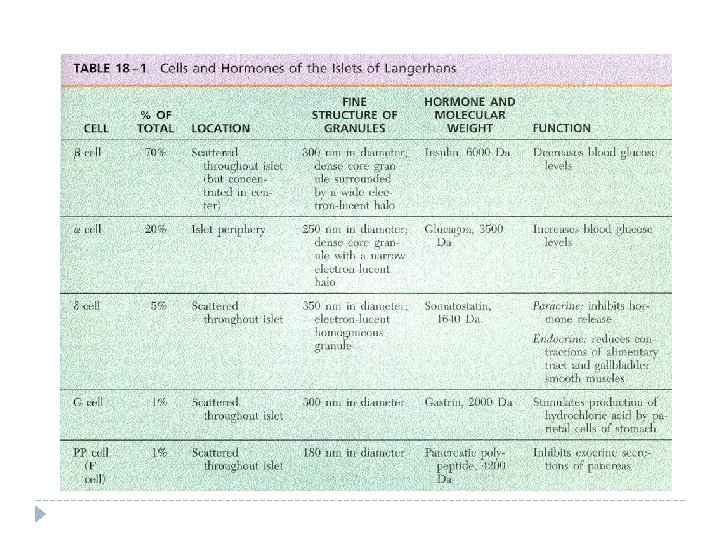
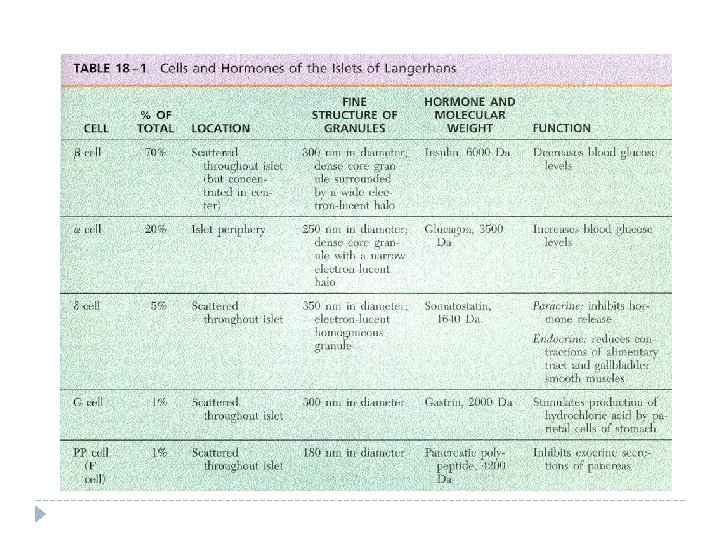
q 4 Cell Types in Islets q Beta cells: 70% of cells, more in center of islets, dense core granule, produce insulin which is released in response to increased blood glucose (glucose uptake by cells) q Alpha cells: 20% of cells, most at islet periphery, produce glucagon, increases blood glucose via glycogen break down in hepatocytes and gluconeogenesis during fasting q Delta cells: 5 - 10% of cells, produce somatostatin, its paracrine effects is on B and A cells and inhibits them, endocrinal affects smooth muscle cells of alimentary tracts and gall bladder q F cells (PP cells): few in number, produce pancreatic polypeptide, decreases pancreatic exocrine secretion q G cells: very few, secrete gastrin that increase HCl secretion and gastric motility

Thyroid Gland q Thyroid gland forms from gut endoderm located just inferior to larynx q A thin slender dense irregular connective tissue surrounds the gland q Septa that are derived from the glands divide the glands into lobules q The parathyroid glands located in the posterior aspects of thyroid within its capsule q Thyroid gland produces, stores and secretes thyroxine and triiodothyronine which increase metabolic rate q Thyroid is composed of follicles that are lined by low cuboidal or squamous epithelium with lumen filled with colloid

q Between follicles are many fenestrated capillaries, some connective tissue q Parafollicular (C) cells: larger, pale staining, in follicle epithelium or in clusters between follicles but they don’t reach to the lumen of follicle, they are about 0. 1% of the epithelial cells q Secrete calcitonin which decreases blood calcium by decreasing bone resorption by osteoclasts and increasing bone formation by osteoblasts


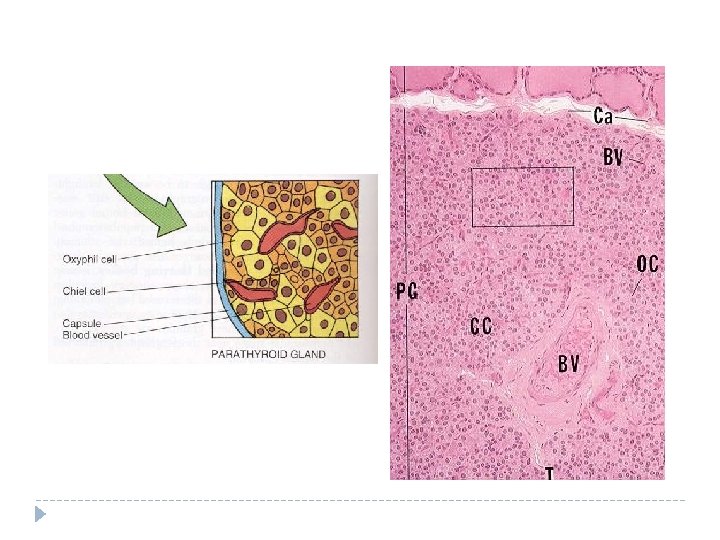
Parathyroid Glands q q q Parathyroid glands are 4 small glands that located on posterior side of thyroid Each gland is enveloped by its own thin connective tissue capsule The paranchymal cells of 3 cell types: Chief cells, Oxyphil cells, and adipocytes Adipocytes appear at puberty and gradually increase in number until about age 40 when most of the gland may be occupied by unilocular adipose tissue Chief and oxyphil cells are arranged in cords close to a network of capillaries
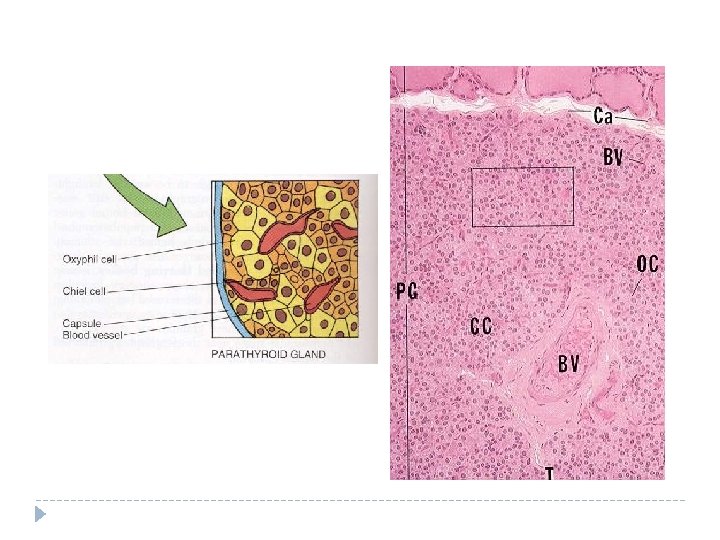
q q q Chief cell: most common, small polygonal cells with acidophilic cytoplasm and dark staining small nucleus secrete parathyroid hormone In healthy adult with normal calcium balance 80% of chief cells are in resting phase In secreting phase chief cells contain stack of RER, Golgi complex and parathyroid hormone granules arranged toward periphery of the cell In resting phase lipid and glycogen are more but less RER and small Golgi complex Parathyroid hormone stimulates increased osteoclast activity leading to increased blood calcium and phosphate

Parathyroid Gland Cells • Oxyphil cells are less common, larger than chief cells, acidophilic cytoplasm due to many mitochondria • Function unknown, may be a different physiological state of chief cell • They are rare before puberty, but increasing in numbers in early adult life


Pineal Body q q Pineal gland = epiphysis cerebri projected from the roof of diencephalon q It is covered by pia matter that form a capsule around the gland with septa which divide the gland into incomplete lobule q Paranchyma is made of Cell cords with many nerve fiber endings q Pinealocytes: basophilic cytoplasm with large irregular nucleus; RER, SER, numerous mitochondria , well developed cytoskeleton Pinealocytes produce melatonin (during darkness) and serotonin (during the day) q

q Inerestitial cells are astroglial cells q These cells have darker nucleus, long processes with glial filaments q Pineal gland may have concretions of calcium phosphate known as brain sand or corpora arenacea q Brain sands appear during childhood and increase in size q Postganglionic sympathetic nerve fibers synapses with pinealocytes q Melatonin inhibits gonad development in prepubertal humans, may regulate diurnal rhythmus, sleep/wake cycles,