Endocrine Diseases Pituitary Gland University of New England
- Slides: 24
Endocrine Diseases Pituitary Gland University of New England Physician Assistant Program J. B. Handler, M. D. 1
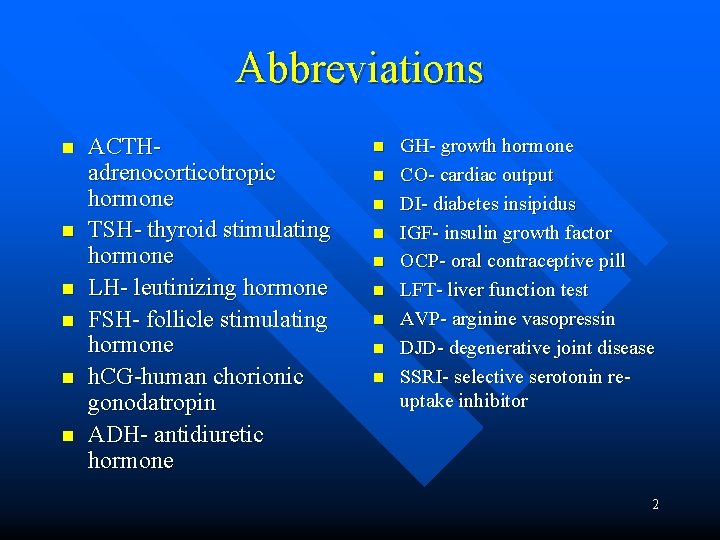
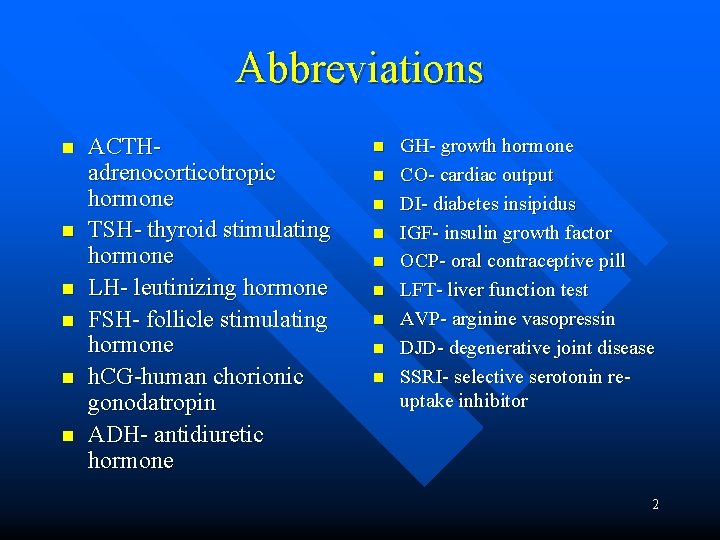
Abbreviations n n n ACTHadrenocorticotropic hormone TSH- thyroid stimulating hormone LH- leutinizing hormone FSH- follicle stimulating hormone h. CG-human chorionic gonodatropin ADH- antidiuretic hormone n n n n n GH- growth hormone CO- cardiac output DI- diabetes insipidus IGF- insulin growth factor OCP- oral contraceptive pill LFT- liver function test AVP- arginine vasopressin DJD- degenerative joint disease SSRI- selective serotonin reuptake inhibitor 2
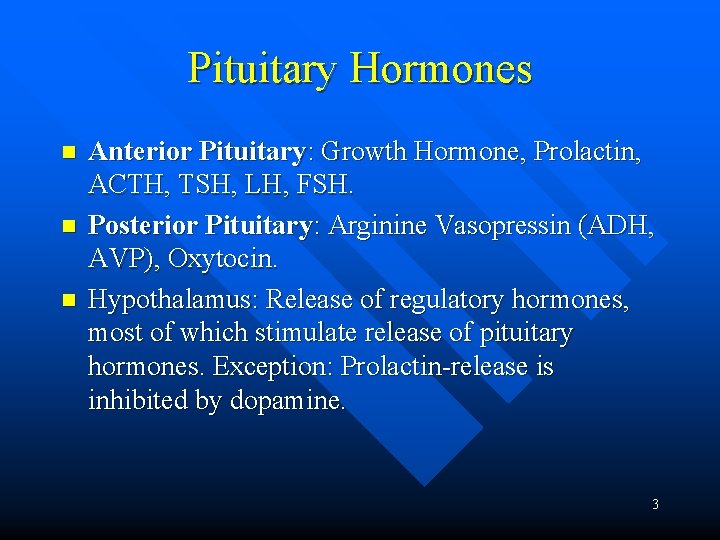
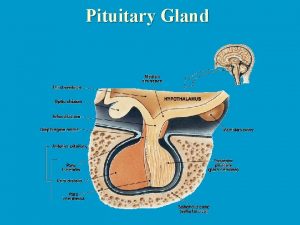
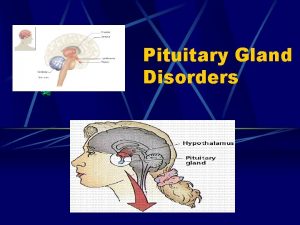
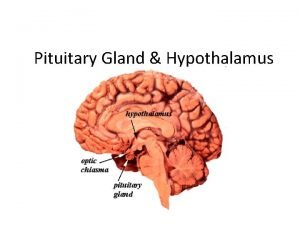
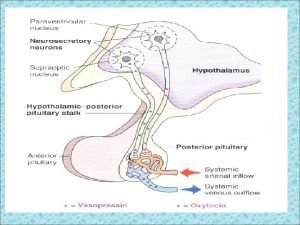
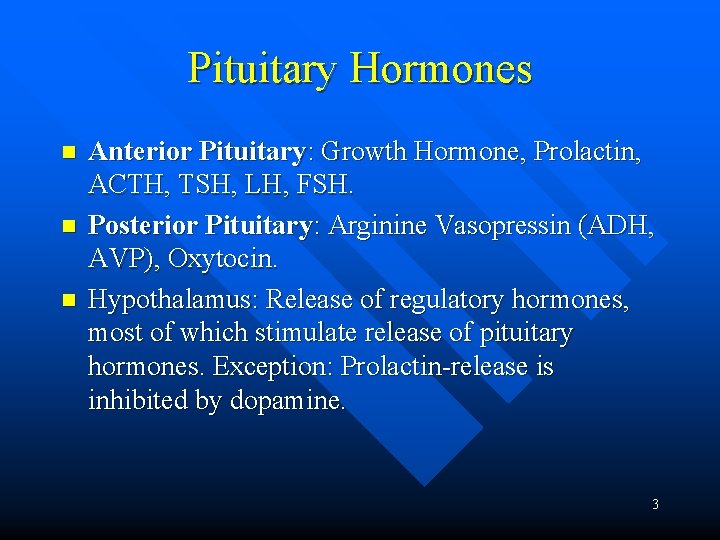
Pituitary Hormones n n n Anterior Pituitary: Growth Hormone, Prolactin, ACTH, TSH, LH, FSH. Posterior Pituitary: Arginine Vasopressin (ADH, AVP), Oxytocin. Hypothalamus: Release of regulatory hormones, most of which stimulate release of pituitary hormones. Exception: Prolactin-release is inhibited by dopamine. 3
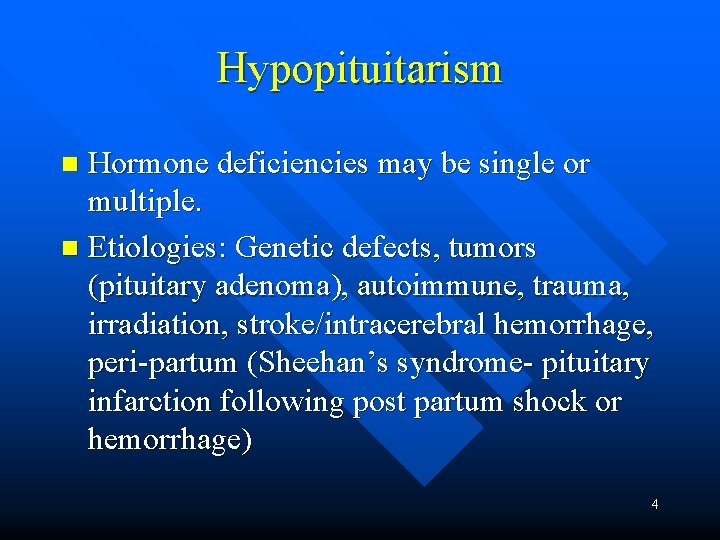
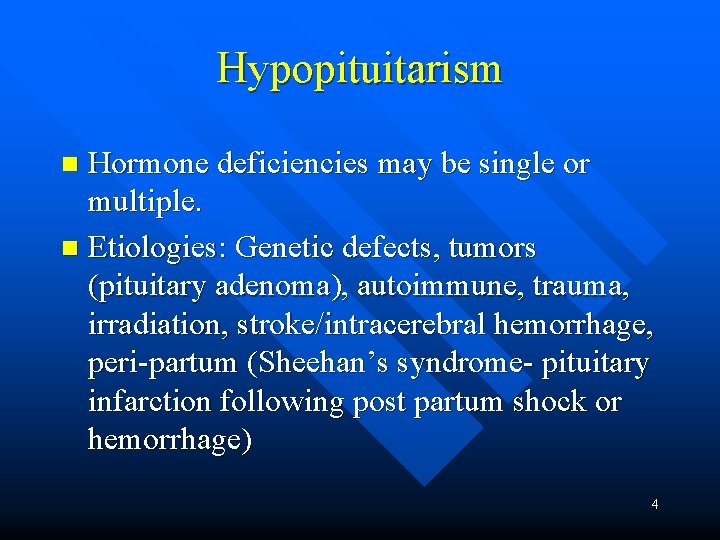
Hypopituitarism Hormone deficiencies may be single or multiple. n Etiologies: Genetic defects, tumors (pituitary adenoma), autoimmune, trauma, irradiation, stroke/intracerebral hemorrhage, peri-partum (Sheehan’s syndrome- pituitary infarction following post partum shock or hemorrhage) n 4
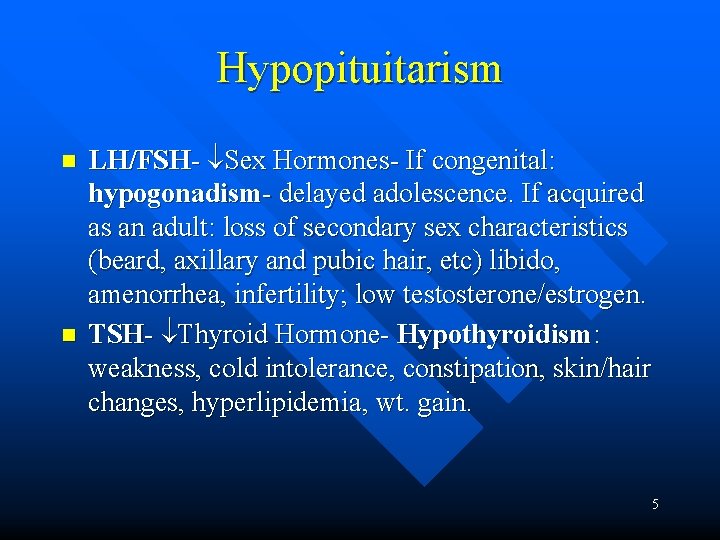
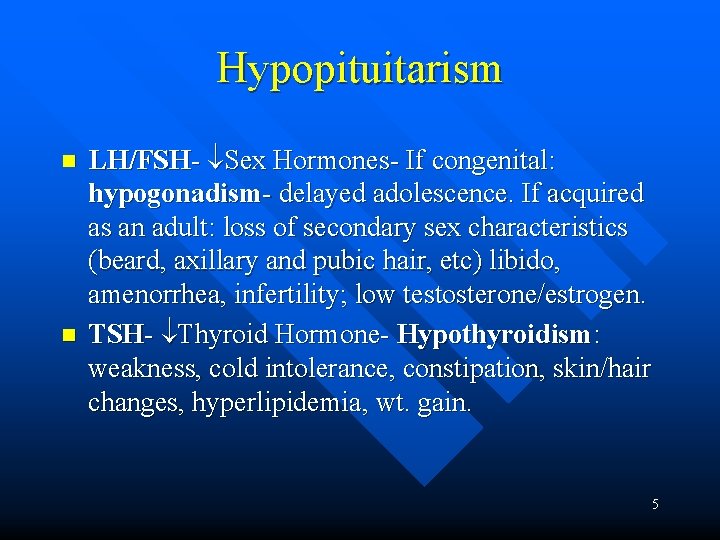
Hypopituitarism n n LH/FSH- Sex Hormones- If congenital: hypogonadism- delayed adolescence. If acquired as an adult: loss of secondary sex characteristics (beard, axillary and pubic hair, etc) libido, amenorrhea, infertility; low testosterone/estrogen. TSH- Thyroid Hormone- Hypothyroidism: weakness, cold intolerance, constipation, skin/hair changes, hyperlipidemia, wt. gain. 5
n n n ACTH- Cortisol-Adrenal insufficiency: Weakness, fatigue, weight loss, hypotension. Growth Hormone-In adults: obesity, asthenia, decreased CO. In children-serious growth disturbance. Panhypopituitarism-lack all of the anterior pituitary hormones. 6
Lab, Diagnostics and Treatment n n n Possibilities: ACTH Cortisol hyponatremia, hypoglycemia; TSH free T 4; LH, FSH Testosterone, Estradiol. MRI- Visualization of Pituitary neoplasms and other CNS pathology. Transphenoidal pituitary surgery (if tumor) followed by endocrine replacement therapy: LThyroxin, Testosterone or Estrogen, Cortisol, h. GH. 7
Diabetes Insipidus n n Central: Deficiency of AVP/ADH Primary: Pituitary intact; familial forms (rare). Secondary: Damage to pituitary or pituitary stalk by tumor, surgery, anoxia. Nephrogenic: Inability of the kidneys to respond to ADH; congenital (lack ADH receptors) and acquired forms (pyelonephritis, post-obstructive, tubular interstitial disease, drug induced (demeclocycline, lithium), hypercalcemia, etc. ). 8
Signs, Symptoms & Diagnostics Intense thirst, polyuria (2 -20 L/d). n Lab: Serum- hypernatremia; urine- low specific gravity. n Other pituitary deficiencies may be present. n 9
Diagnostics Vasospressin challenge: Desmopressin administered SC or intranasal results in dramatic decrease in urine volume in central DI; no response with nephrogenic DI. n Differential Dx of polyuria/polydipsea: DI, Diabetes Mellitus, psychogenic polydypsia. n Complications: Severe dehydration, hypernatremia. n 10
Treatment Central DI: Partial deficiency may require no treatment other than fluids. Complete deficiency: Desmopressin (SC, IM, oral, intranasal); lowest effective dose to avoid hyponatremia. n Nephrogenic DI: May respond to Indomethacin which increases renal sensitivity to AVP by blocking the action of prostaglandin E. n 11
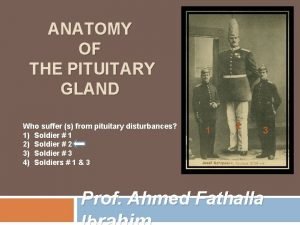
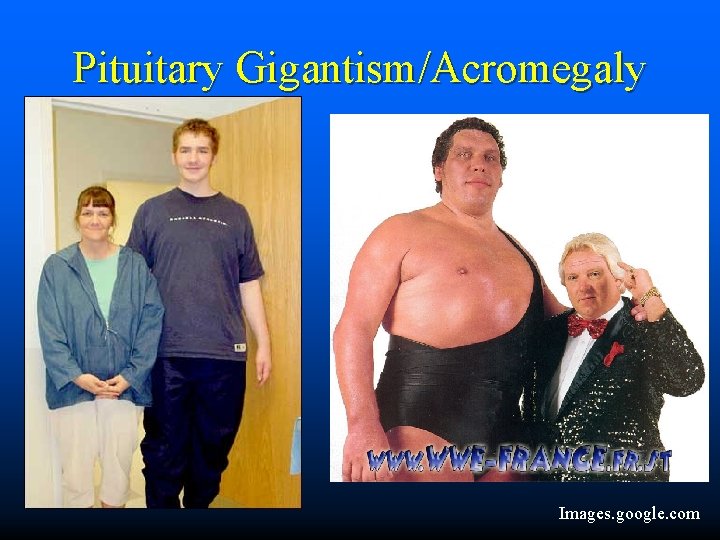
Acromegaly and Gigantism Excessive GH release, almost always from a pituitary adenoma. n GH effects mediated by increased production of IGF-I in liver. n These tumors often produce prolactin in addition to GH additional Sx (see below). n 12
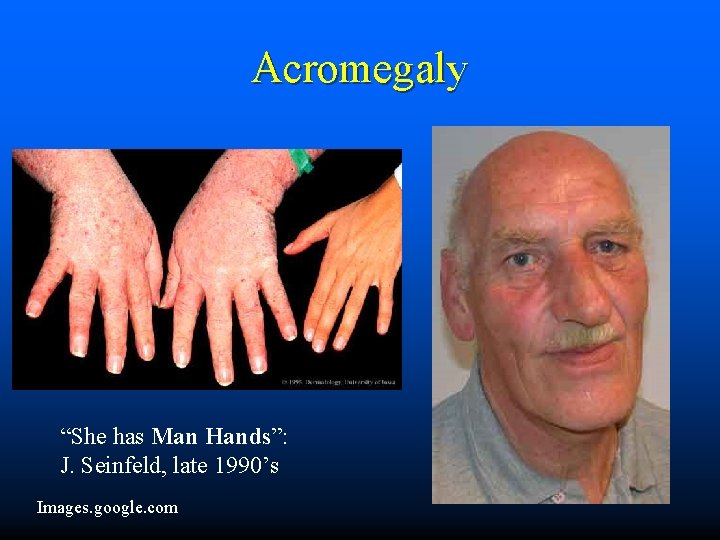
Signs and Symptoms Dependent on when the tumor develops. n If before closure of epiphyses: Gigantism n After epiphyseal closure: Acromegaly. Characterized by enlargement of the hands, jaw, feet; coarse facial features; bones of the skull enlarge; deep voice. n 13
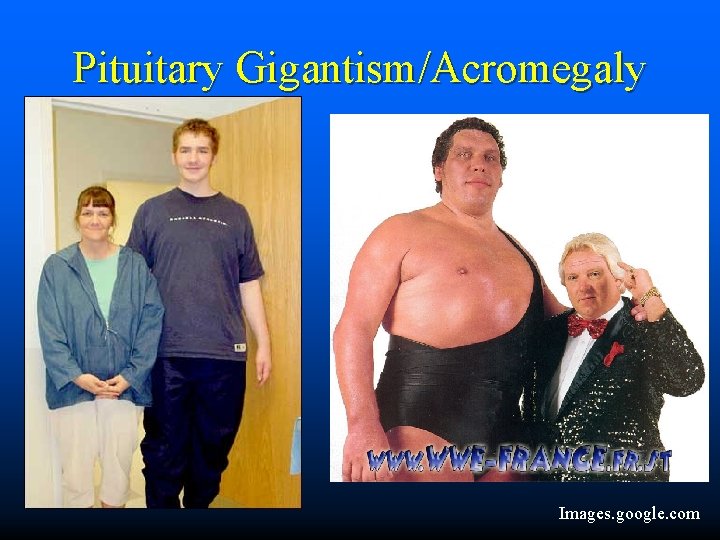
Pituitary Gigantism/Acromegaly Images. google. com
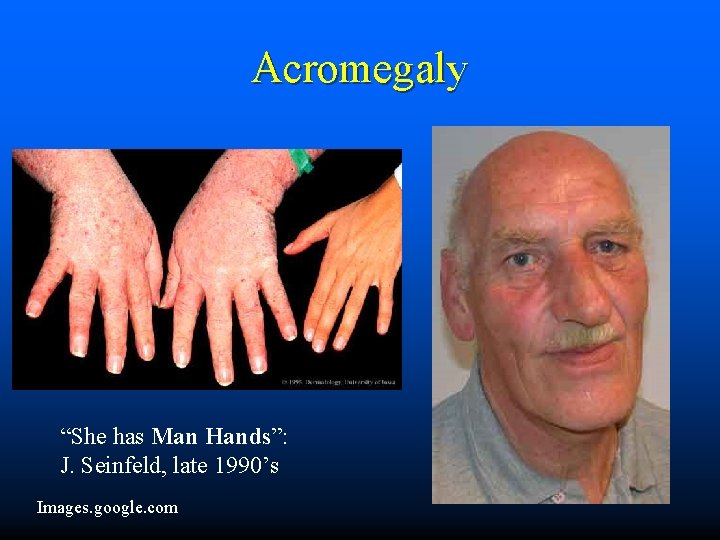
Acromegaly “She has Man Hands”: J. Seinfeld, late 1990’s Images. google. com
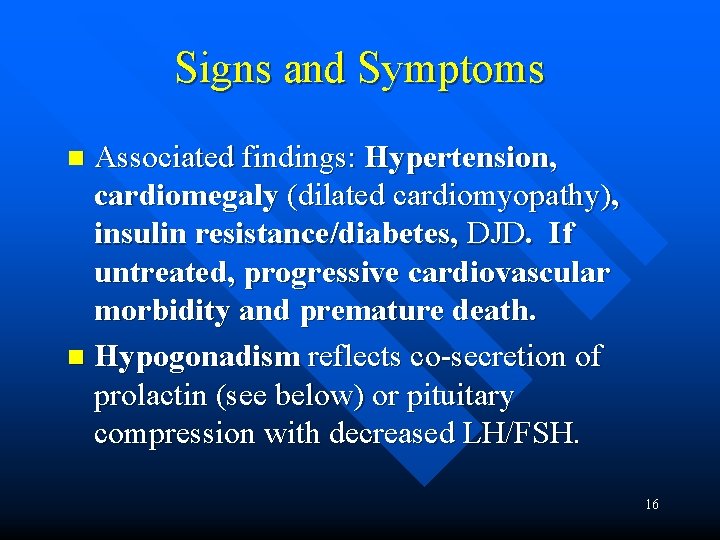
Signs and Symptoms Associated findings: Hypertension, cardiomegaly (dilated cardiomyopathy), insulin resistance/diabetes, DJD. If untreated, progressive cardiovascular morbidity and premature death. n Hypogonadism reflects co-secretion of prolactin (see below) or pituitary compression with decreased LH/FSH. n 16
Lab and Diagnostic Findings n n n Bloodwork (Following an overnight fast): serum IGF-I ( 5 x nl with Acromegaly), prolactin, glucose; all may be elevated. TSH/Thyroxin if low, suggests additional pituitary pathology. Glucose challenge post fast- Elevated GH levels help confirm the diagnosis (should normally be < 1 ng/m. L). MRI- Usually identifies a pituitary adenoma. 17
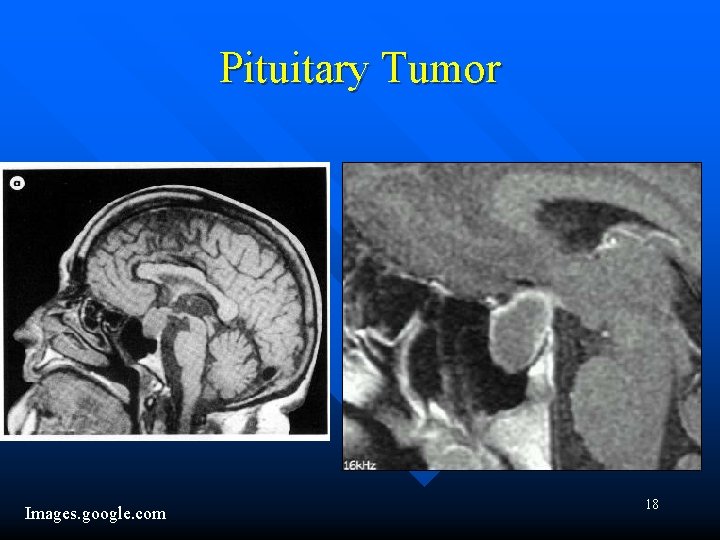
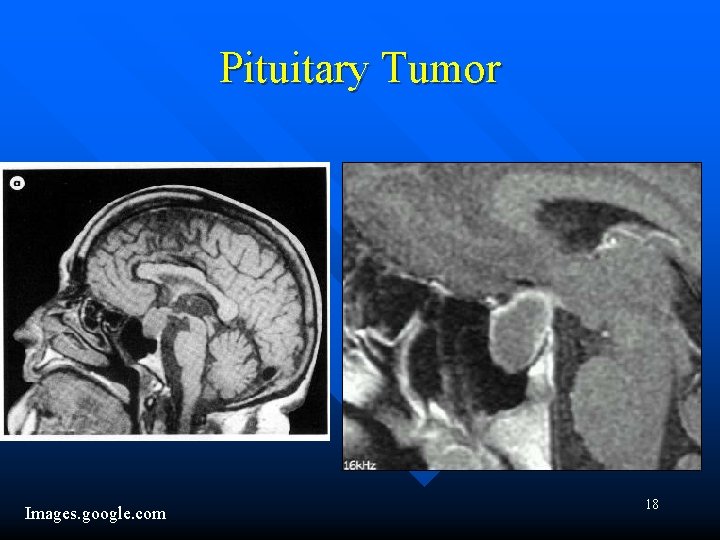
Pituitary Tumor Images. google. com 18
Treatment of Acromegaly n n Transphenoidal microsurgery, which may result in transient or permanent hypopituitarism. Octreotide-a somatostatin (somatotropin releaseinhibiting factor) analog. Suppresses GH secretion; used in patients who continue to have excessive GH release post-op; very expensive; injected shrinks some tumors – Dopaminergic agents (cabergoline, oral) useful especially if tumor co-secretes prolactin shrinks some tumors. – Pegvisomant- GH receptor antagonist, new. 19
Hyperprolactinemia Prolactin induces lactation during pregnancy (along with estrogen and progesterone). n Control of prolactin production is inhibitory, mediated by dopamine. n Etiologies: Pituitary microadenoma (may also produce GH), drugs (SSRI’s, thiazides, Cimetidine, Tricyclics, OCP, others); hypothyroidism, renal failure and cirrhosis. n 20
Signs and Symptoms n n n High prolactin levels suppress Gn. RH LH/FSH, resulting in hypogonatropic hypogonadism. Females: Pre-menopausal woman develop galactorrhea, oligo/amenorrhea and infertility, decreased libido, vaginal dryness. Males: Decreased libido, erectile dysfunction, gynecomastia, but no galactorrhea. 21
Lab and Diagnostic Findings Baseline labs should include h. CG, TSH, Free Thyroxine, Creatinine and BUN, LFT’s and Prolactin levels. n In the absence of pregnancy and renal failure, a Prolactin level >250 ng/m. L is highly suspicious/diagnostic of Prolactinoma. n Imaging- MRI n 22
Treatment DC offending drug if present. n Correct other possible etiologies. n Microprolactinomas grow very slowly and patients with mild symptoms can be followed without intervention. n 23
Treatment With symptoms of hypogonadism/infertility or larger tumors: Dopamine agonists (Cabergoline, Bromocriptine) can successfully treat symptoms, correct amenorrhea and galactorrhea, and shrink the tumor. n Transphenoidal pituitary surgery reserved for individuals with large macroadenomas that abut/compress the optic chiasm. n 24
 Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Janos lobe
Janos lobe Pituitary gland venous drainage
Pituitary gland venous drainage Division of pituitary gland
Division of pituitary gland Nerve supply to pituitary gland
Nerve supply to pituitary gland Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Hyperfunction of the pituitary gland in preadolescence
Hyperfunction of the pituitary gland in preadolescence Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Hypersecretion of prolactin
Hypersecretion of prolactin Circulação
Circulação Blood supply of pituitary gland
Blood supply of pituitary gland Evolution of pituitary gland
Evolution of pituitary gland Pituitary gland hormones
Pituitary gland hormones Brainstem glioma
Brainstem glioma Where is kidney pain felt diagram
Where is kidney pain felt diagram Tongue development
Tongue development Gland
Gland Pituitary gland thyroid
Pituitary gland thyroid Anterior pituitary
Anterior pituitary Pituitary gland embryonic origin
Pituitary gland embryonic origin Pituitary gland disorders
Pituitary gland disorders Pituitary gland
Pituitary gland Hypothalamus and pituitary gland connection
Hypothalamus and pituitary gland connection