End o Cryin about the Endocrine Lab Tests
End ‘o Cryin’ about the Endocrine Lab Tests ! Cheryl Morrow MD June 5, 2015
n o i s s ppre Su e n aso th e m exa D IG F 1 ? ? PTHr. P Cosyntro pin Test ? e d roi y h t ra Pa ? H on m or say s A
Learning Objectives: �Will be able to select appropriate diagnostic lab testing when presented with a case study representing the most common disorders of the pituitary, thyroid, adrenal and parathyroid glands, and arrive at a diagnosis based on properly interpreting the results. �Will be able to select and interpret lab test results that are used to manage/monitor the most common disorders of the pituitary, thyroid, adrenal and parathyroid glands. �Will be able to recognize and diagnose common autoimmune and paraneoplastic syndromes (ectopic hormones) that present as primary endocrine disorders

To Understand Endocrine Physiology and Pathology, and the lab tests we use for diagnosis and monitoring … we have to understand Negative Feedback Control
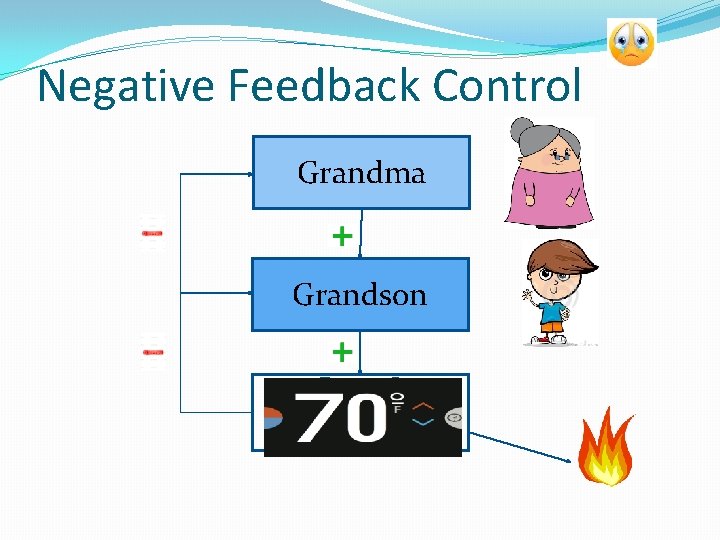
Negative Feedback Control Grandma Grandson
90 degrees !!
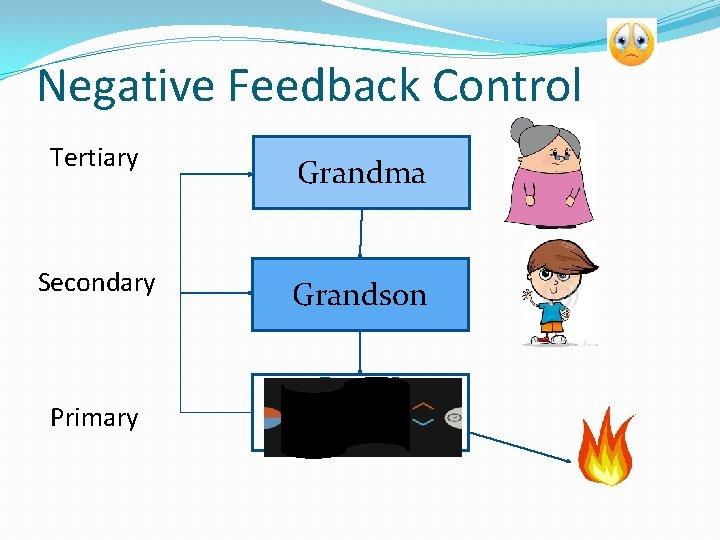
Negative Feedback Control Tertiary Grandma Secondary Grandson Primary
Negative Feedback Control Grandma Grandson
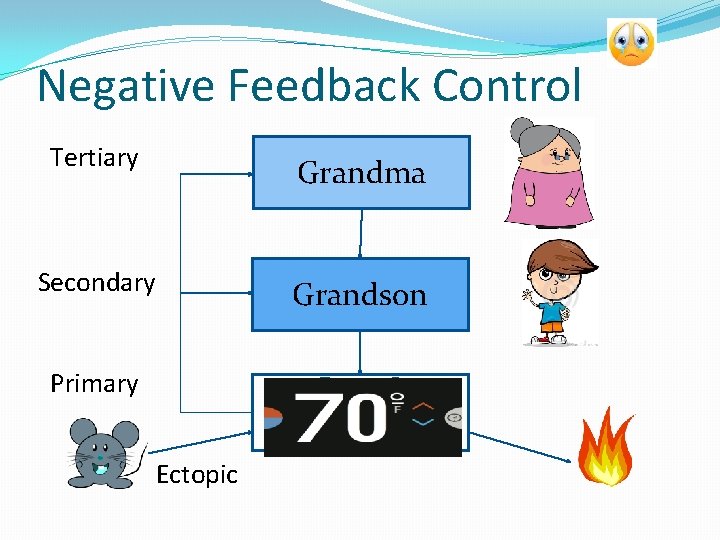
Negative Feedback Control Tertiary Grandma Secondary Grandson Primary Ectopic
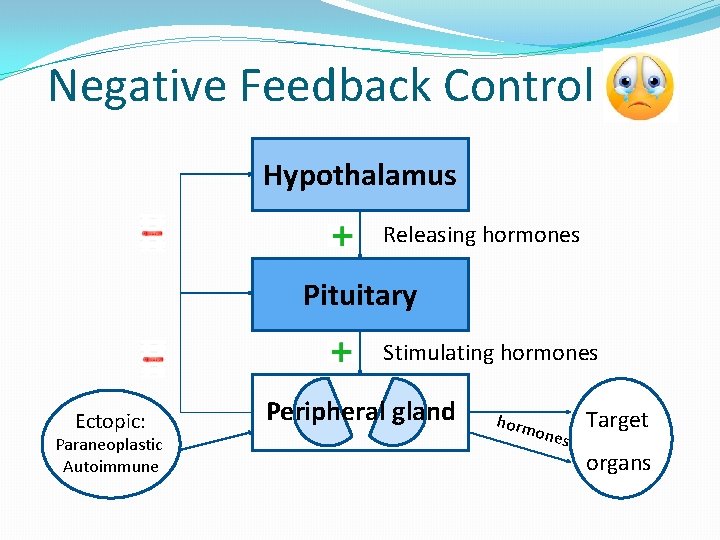
Negative Feedback Control Hypothalamus Releasing hormones Pituitary Stimulating hormones Ectopic: Paraneoplastic Autoimmune Peripheral gland horm ones Target organs
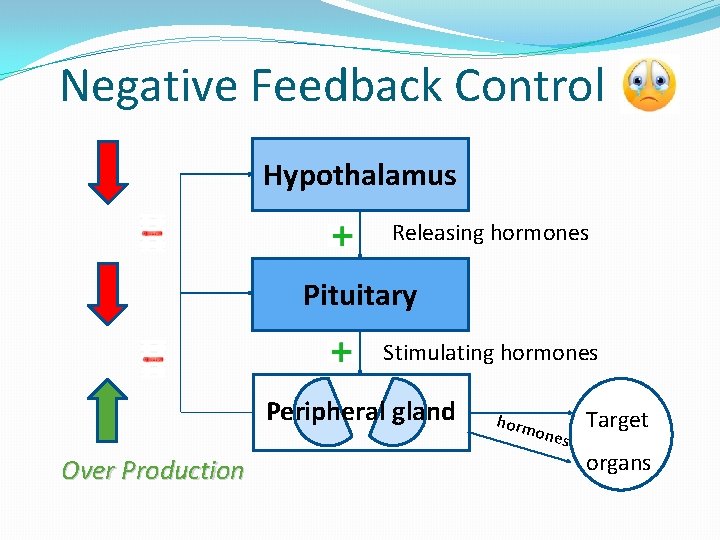
Negative Feedback Control Hypothalamus Releasing hormones Pituitary Stimulating hormones Peripheral gland Over Production horm ones Target organs
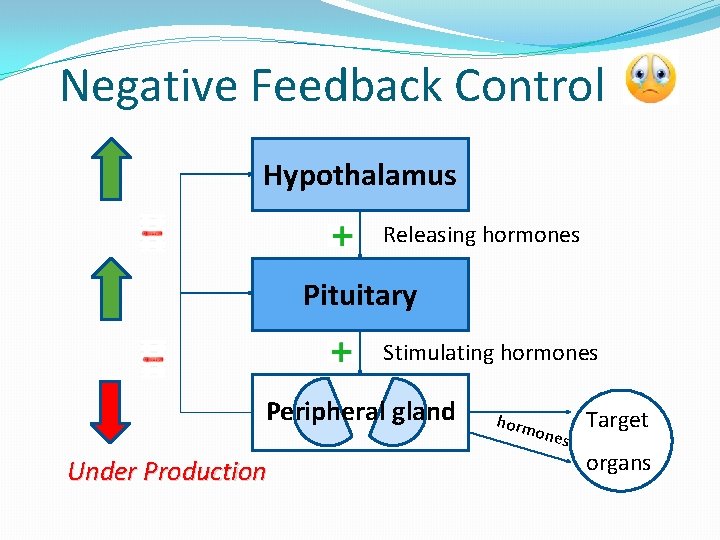
Negative Feedback Control Hypothalamus Releasing hormones Pituitary Stimulating hormones Peripheral gland Under Production horm ones Target organs
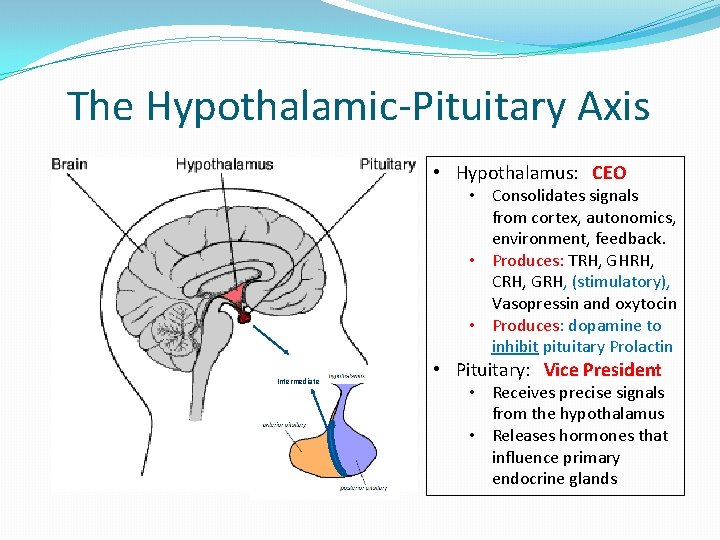
The Hypothalamic-Pituitary Axis • Hypothalamus: CEO • Consolidates signals from cortex, autonomics, environment, feedback. • Produces: TRH, GHRH, CRH, GRH, (stimulatory), Vasopressin and oxytocin • Produces: dopamine to inhibit pituitary Prolactin Intermediate • Pituitary: Vice President • Receives precise signals from the hypothalamus • Releases hormones that influence primary endocrine glands

Endocrine glands: /Ovaries The Pituitary Secretes: Anterior Lobe: (produces/secretes) • ACTH Adrenals • h. GH Liver, other • TSH Thyroid gland • FSH Gonads • LH Gonads • PRL(LTH) mammary; gonads Intermediate Lobe: (produc/secret) • MSH melanocytes Posterior Lobe: (secretes only) • ADH kidney, arteries • Oxytocin uterus, brain (will not be discussing post. Pituitary)
Hypothalamic Diseases: �No diseases of overproduction of releasing hormones, �Ectopic CRF: pulmonary carcinoid tumors Cushings Syndrome �Underproduction, leading to hypopituitarism, occurs with: �Mass lesions: craniopharyngiomas, metastases �Radiation damage: occurs when brain receives RT �Infiltrative lesions: ie. Sarcoidosis, histiocytosis �Infections: i. e. tuberculous meningitis-> hypothalamus �Traumatic brain injury Take Home Point: Hypopituitarism -> R/O Hypothalamic Dis.
Pituitary Adenomas: 800, 000/yr US Prevalence in population: 16. 7%* ; May be part of MEN 1 �Overproduction of stim. /trophic hormones: �Somatotroph Adenoma: 27 % of pit. Adenomas � Produces GH which is pulsatile; don’t assay. IGF-1. (GH stimulates IGF-1) stable levels. Assay. � Acromegaly: excess growth bones, soft tissues � �Corticotroph Adenoma: 8% of pit. Adenomas � Produces ACTH, which in turn stimulates corticosteroids. This is Cushings Disease which will be discussed again under Adrenal Diseases. * Ezzat et. al. , Cancer. 2004, Aug 1; 101(3) 613 -9
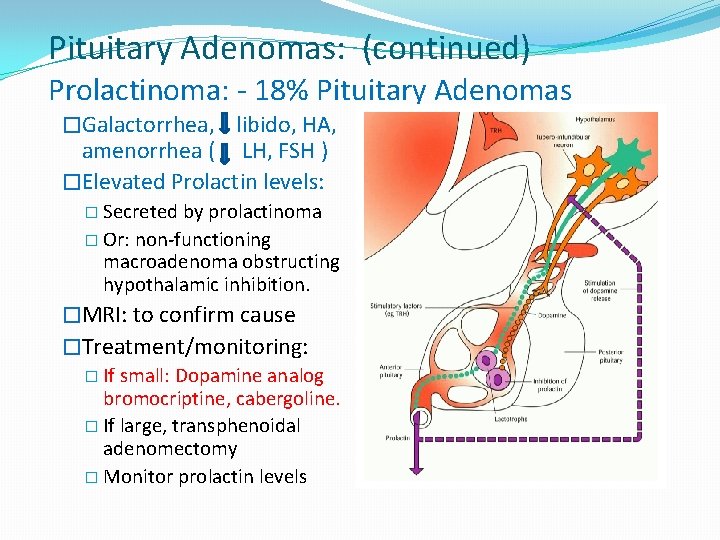
Pituitary Adenomas: (continued) Prolactinoma: - 18% Pituitary Adenomas �Galactorrhea, libido, HA, amenorrhea ( LH, FSH ) �Elevated Prolactin levels: � Secreted by prolactinoma � Or: non-functioning macroadenoma obstructing hypothalamic inhibition. �MRI: to confirm cause �Treatment/monitoring: � If small: Dopamine analog bromocriptine, cabergoline. � If large, transphenoidal adenomectomy � Monitor prolactin levels
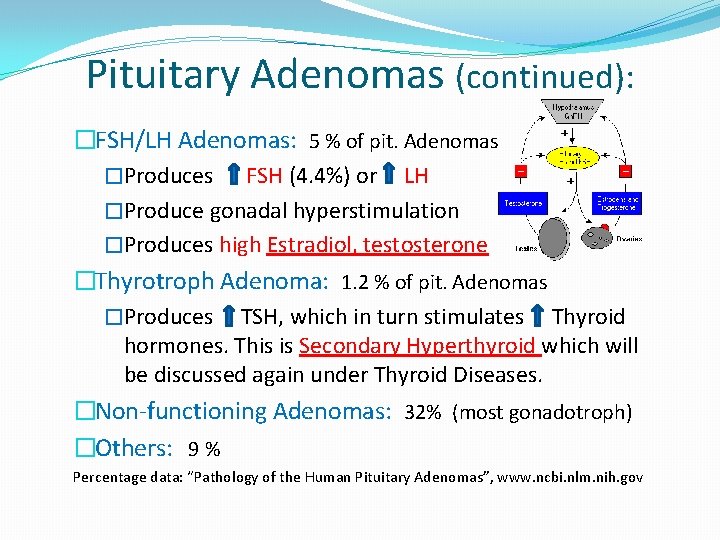
Pituitary Adenomas (continued): �FSH/LH Adenomas: 5 % of pit. Adenomas �Produces FSH (4. 4%) or LH �Produce gonadal hyperstimulation �Produces high Estradiol, testosterone �Thyrotroph Adenoma: 1. 2 % of pit. Adenomas �Produces TSH, which in turn stimulates Thyroid hormones. This is Secondary Hyperthyroid which will be discussed again under Thyroid Diseases. �Non-functioning Adenomas: 32% (most gonadotroph) �Others: 9 % Percentage data: “Pathology of the Human Pituitary Adenomas”, www. ncbi. nlm. nih. gov
Hypopituitarism �Global: �Sheehans – pituitary infarction after post-partum hemorrhage �Pituitary Apoplexy – sudden hemorrhage into pituitary � Bleed often occurs into a pituitary adenoma � Sudden onset of severe headache, diplopia, hypopituitarism � Sudden onset of ACTH defic cortisol hypotension, glucose �Other: radiation, infiltrative (hemochromatosis), granuloma, TBI, tumor/metastasis, infectious, autoimmune �Symptoms: pan-hypopit: Hypocortisolism, hypothyroid �Labs: prolactin, TSH, FT 4, IGF-1, ACTH, FSH, LH, cortisol and cosyntropin stimulation test (see Adrenal Insufficiency)
Hypopituitarism �Selective: Sx’s are same as hypo function of target organ �Causes: genetic/congenital, tumors, radiation, TBI, autoimmune, infarct �Lab tests: � Growth Hormone Deficiency: GH stimulation test; IGF-1 � Adrenal Corticotrophic Hormone Deficiency: early AM cortisol, Cosyntropin stimulation test, ACTH (see adrenal insufficiency) � Thyroid Stimulating Hormone Deficiency: TSH, FT 4, FT 3 � LH/FSH Deficiency: Rule out Prolactinoma ! � Women: � Pre-menopause: Estradiol, LH, FSH, abnormal periods � Post-menopause: LH, FSH � Men: LH, FSH and testosterone
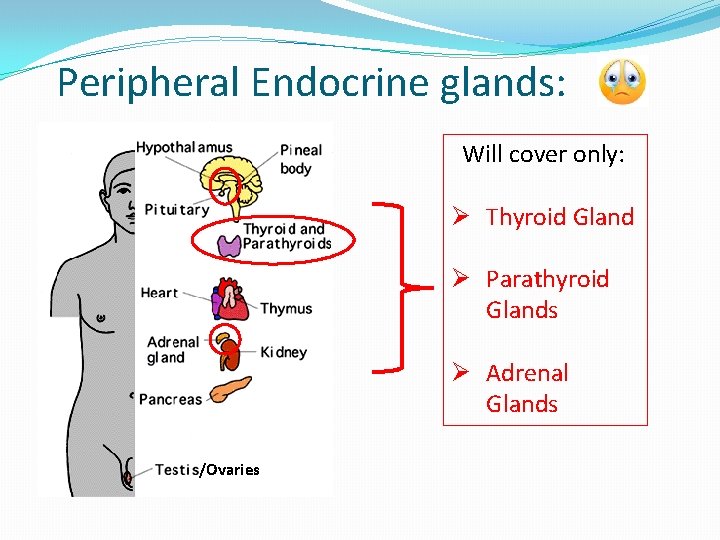
Peripheral Endocrine glands: Will cover only: Ø Thyroid Gland Ø Parathyroid Glands Ø Adrenal Glands /Ovaries
The Adrenal Glands ( Most complicated, so will cover first )
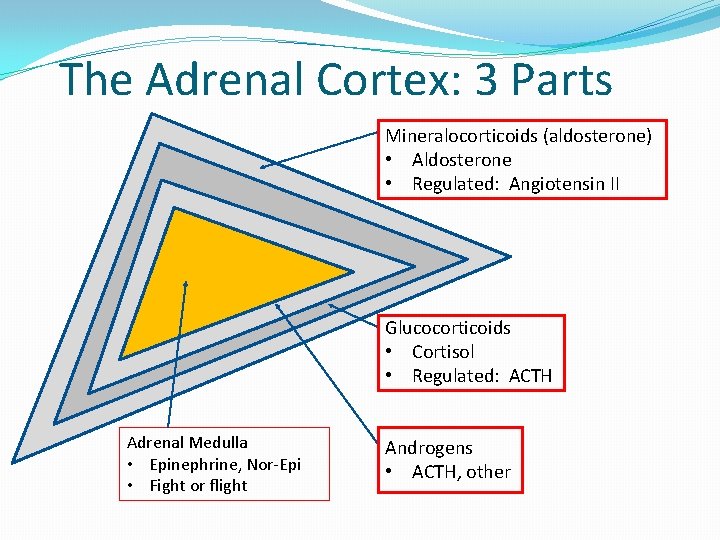
The Adrenal Cortex: 3 Parts Mineralocorticoids (aldosterone) • Aldosterone • Regulated: Angiotensin II Glucocorticoids • Cortisol • Regulated: ACTH Adrenal Medulla • Epinephrine, Nor-Epi • Fight or flight Androgens • ACTH, other
Diseases of Adrenal Cortex Hypercortisolism
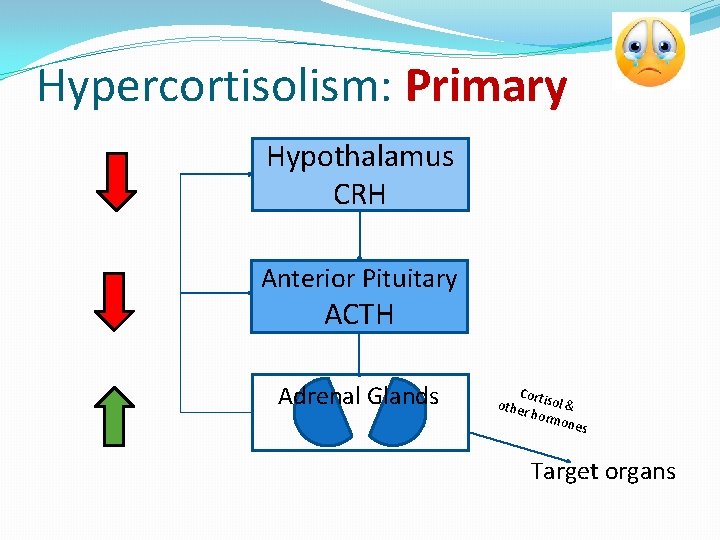
Hypercortisolism: Primary Hypothalamus CRH Anterior Pituitary ACTH Adrenal Glands Cor other tisol & horm ones Target organs
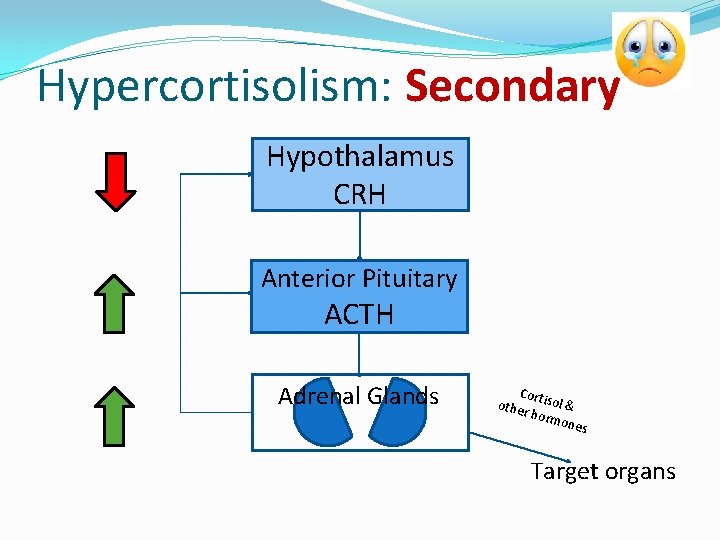
Hypercortisolism: Secondary Hypothalamus CRH Anterior Pituitary ACTH Adrenal Glands Cor other tisol & horm ones Target organs
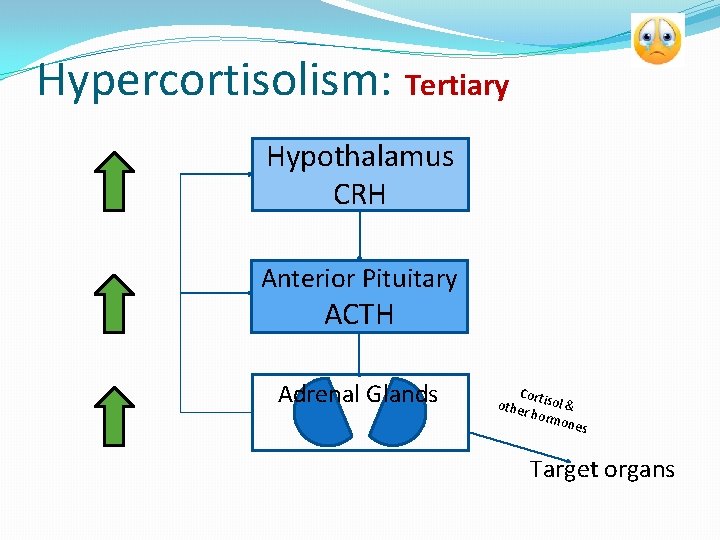
Hypercortisolism: Tertiary Hypothalamus CRH Anterior Pituitary ACTH Adrenal Glands Cor other tisol & horm ones Target organs
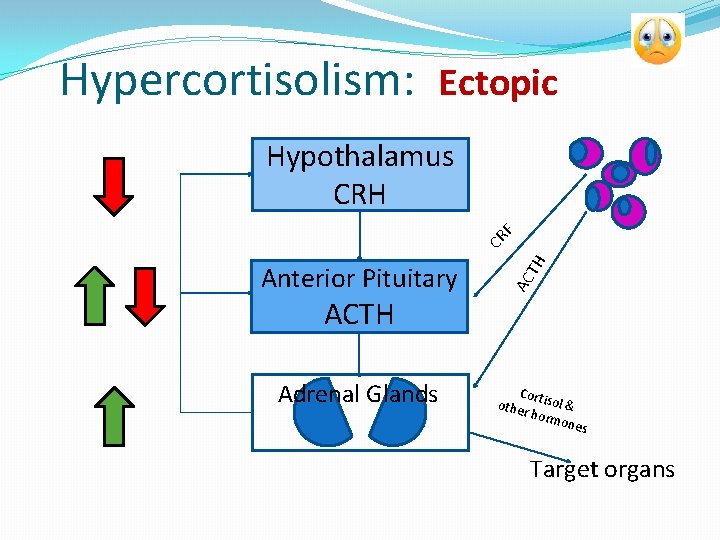
Hypercortisolism: Ectopic AC Anterior Pituitary TH CR F Hypothalamus CRH ACTH Adrenal Glands Cor other tisol & horm ones Target organs
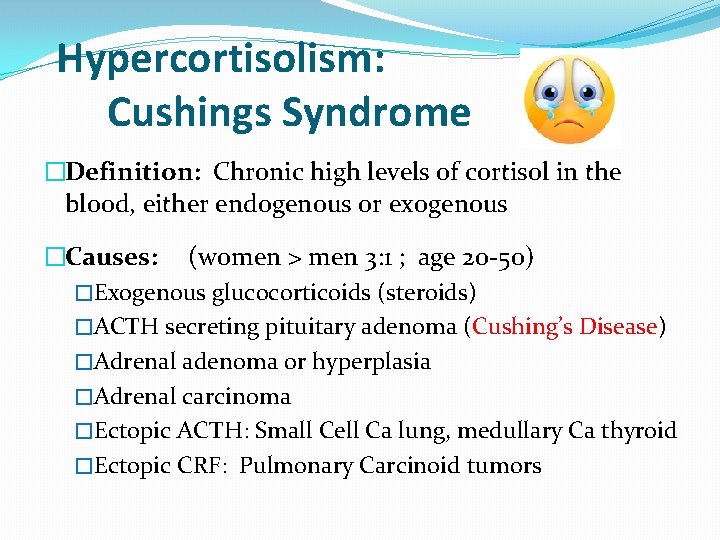
Hypercortisolism: Cushings Syndrome �Definition: Chronic high levels of cortisol in the blood, either endogenous or exogenous �Causes: (women > men 3: 1 ; age 20 -50) �Exogenous glucocorticoids (steroids) �ACTH secreting pituitary adenoma (Cushing’s Disease) �Adrenal adenoma or hyperplasia �Adrenal carcinoma �Ectopic ACTH: Small Cell Ca lung, medullary Ca thyroid �Ectopic CRF: Pulmonary Carcinoid tumors
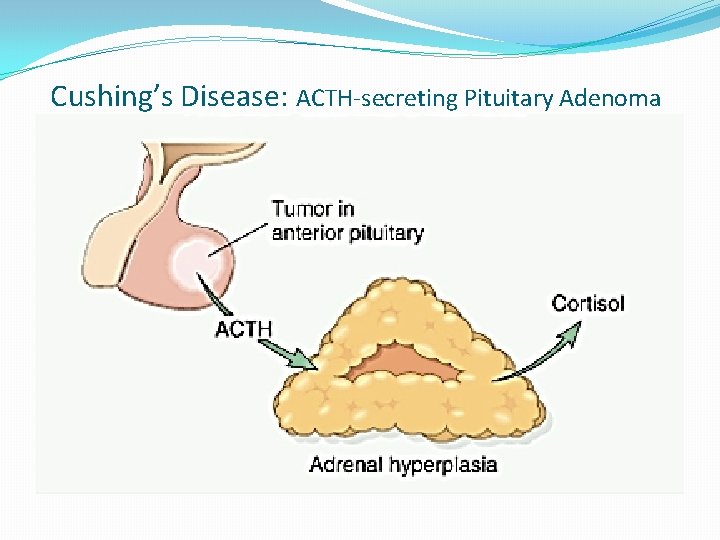
Cushing’s Disease: ACTH-secreting Pituitary Adenoma
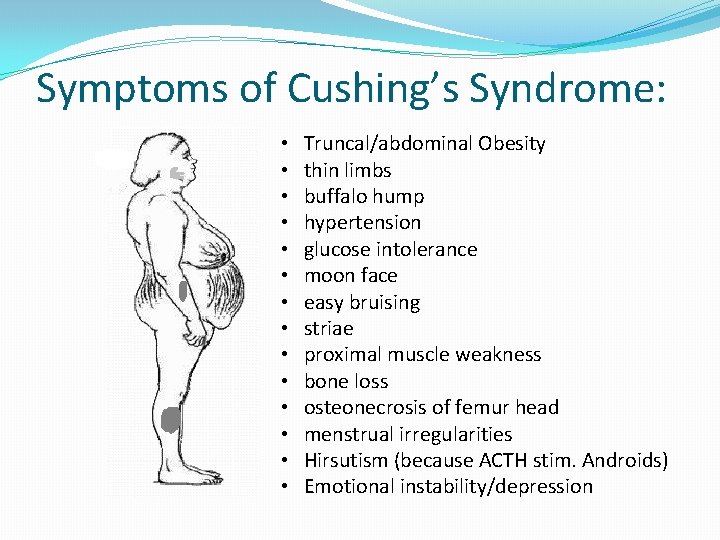
Symptoms of Cushing’s Syndrome: • • • • Truncal/abdominal Obesity thin limbs buffalo hump hypertension glucose intolerance moon face easy bruising striae proximal muscle weakness bone loss osteonecrosis of femur head menstrual irregularities Hirsutism (because ACTH stim. Androids) Emotional instability/depression
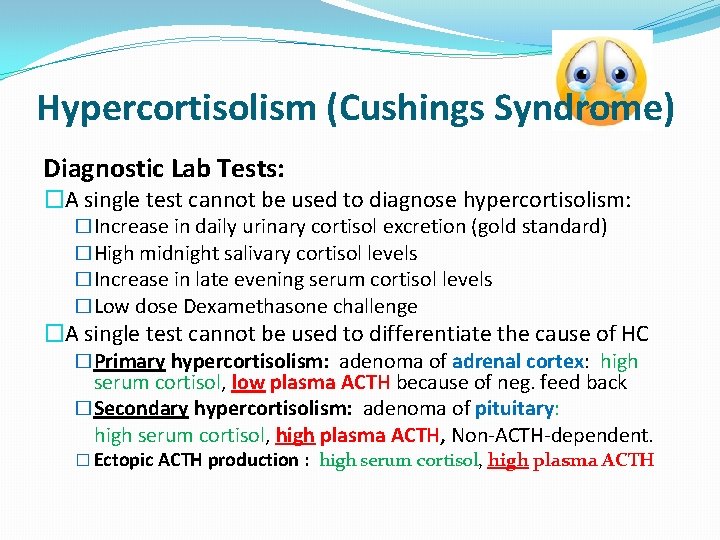
Hypercortisolism (Cushings Syndrome) Diagnostic Lab Tests: �A single test cannot be used to diagnose hypercortisolism: �Increase in daily urinary cortisol excretion (gold standard) �High midnight salivary cortisol levels �Increase in late evening serum cortisol levels �Low dose Dexamethasone challenge �A single test cannot be used to differentiate the cause of HC �Primary hypercortisolism: adenoma of adrenal cortex: high serum cortisol, low plasma ACTH because of neg. feed back �Secondary hypercortisolism: adenoma of pituitary: high serum cortisol, high plasma ACTH, Non-ACTH-dependent. � Ectopic ACTH production : high serum cortisol, high plasma ACTH
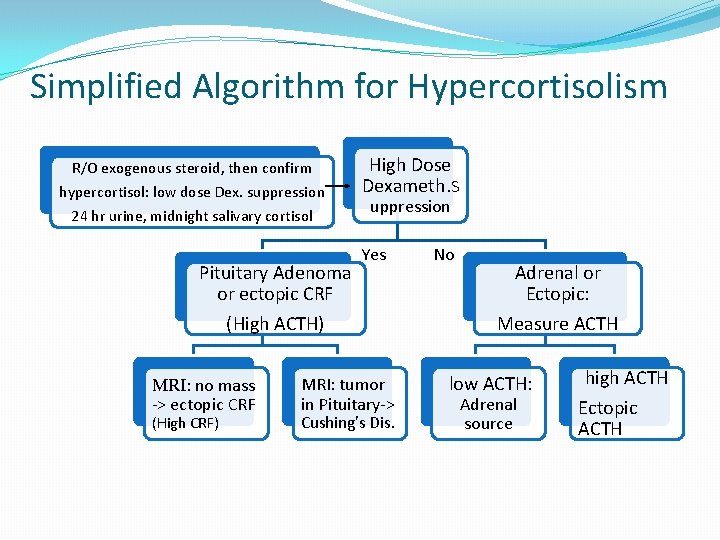
Simplified Algorithm for Hypercortisolism R/O exogenous steroid, then confirm hypercortisol: low dose Dex. suppression 24 hr urine, midnight salivary cortisol Pituitary Adenoma or ectopic CRF (High ACTH) MRI: no mass -> ectopic CRF (High CRF) High Dose Dexameth. S uppression Yes MRI: tumor in Pituitary-> Cushing’s Dis. No Adrenal or Ectopic: Measure ACTH low ACTH: Adrenal source high ACTH Ectopic ACTH
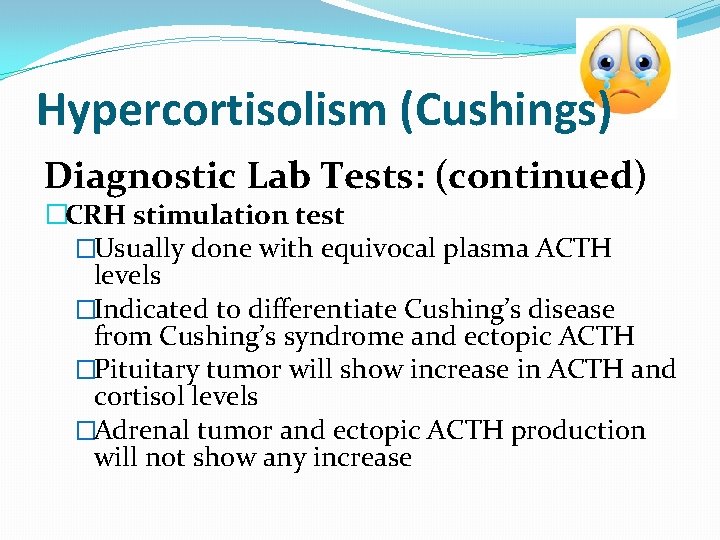
Hypercortisolism (Cushings) Diagnostic Lab Tests: (continued) �CRH stimulation test �Usually done with equivocal plasma ACTH levels �Indicated to differentiate Cushing’s disease from Cushing’s syndrome and ectopic ACTH �Pituitary tumor will show increase in ACTH and cortisol levels �Adrenal tumor and ectopic ACTH production will not show any increase
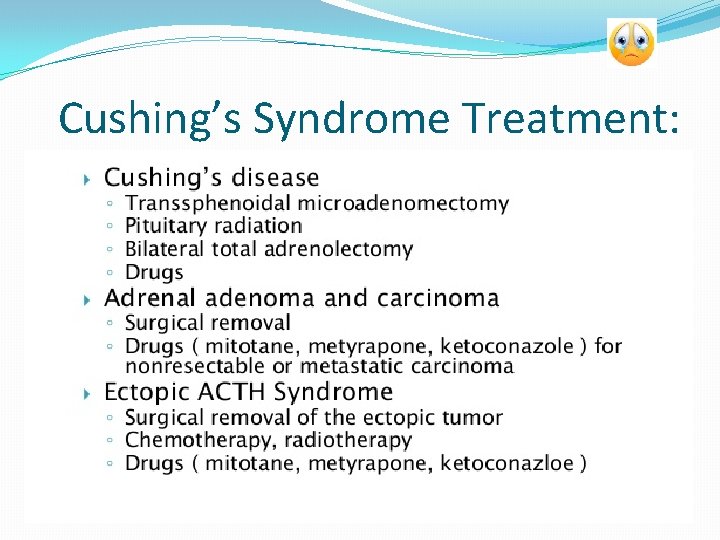
Cushing’s Syndrome Treatment:
Diseases affecting the Adrenal Gland Adrenal Insufficiency
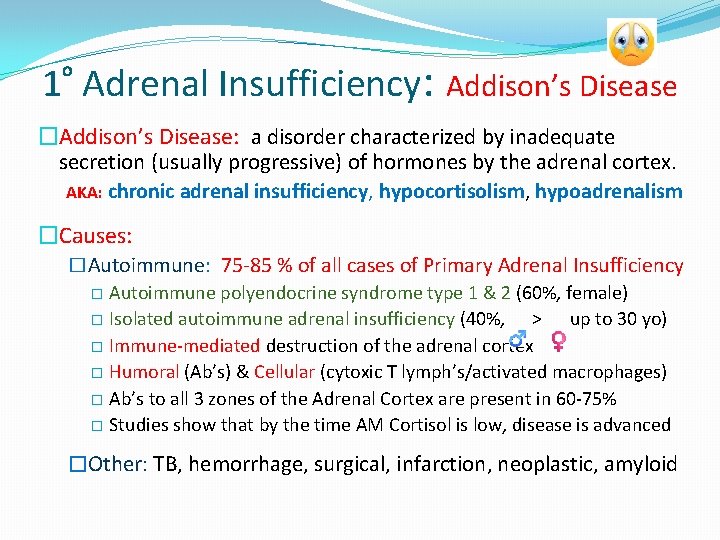
1 Adrenal Insufficiency: Addison’s Disease o �Addison’s Disease: a disorder characterized by inadequate secretion (usually progressive) of hormones by the adrenal cortex. AKA: chronic adrenal insufficiency, hypocortisolism, hypoadrenalism �Causes: �Autoimmune: 75 -85 % of all cases of Primary Adrenal Insufficiency � Autoimmune polyendocrine syndrome type 1 & 2 (60%, female) � Isolated autoimmune adrenal insufficiency (40%, > up to 30 yo) � Immune-mediated destruction of the adrenal cortex � Humoral (Ab’s) & Cellular (cytoxic T lymph’s/activated macrophages) � Ab’s to all 3 zones of the Adrenal Cortex are present in 60 -75% � Studies show that by the time AM Cortisol is low, disease is advanced �Other: TB, hemorrhage, surgical, infarction, neoplastic, amyloid
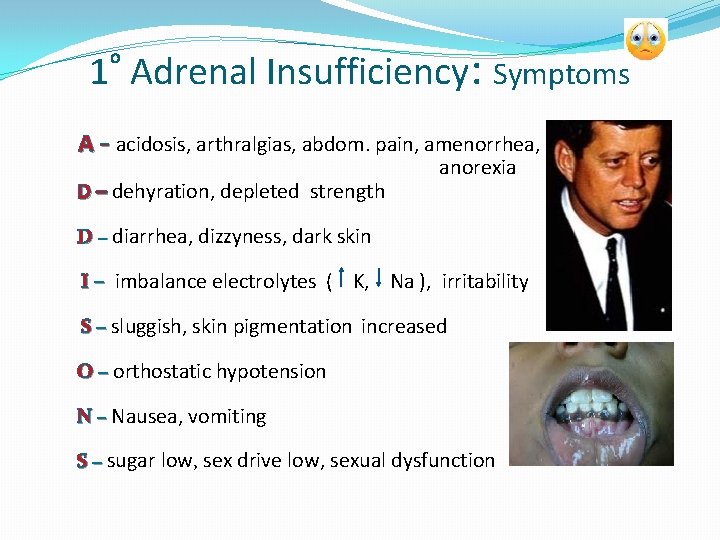
1 Adrenal Insufficiency: Symptoms o A - acidosis, arthralgias, abdom. pain, amenorrhea, D – dehyration, depleted strength anorexia D – diarrhea, dizzyness, dark skin I – imbalance electrolytes ( K, Na ), irritability S – sluggish, skin pigmentation increased O – orthostatic hypotension N – Nausea, vomiting S – sugar low, sex drive low, sexual dysfunction
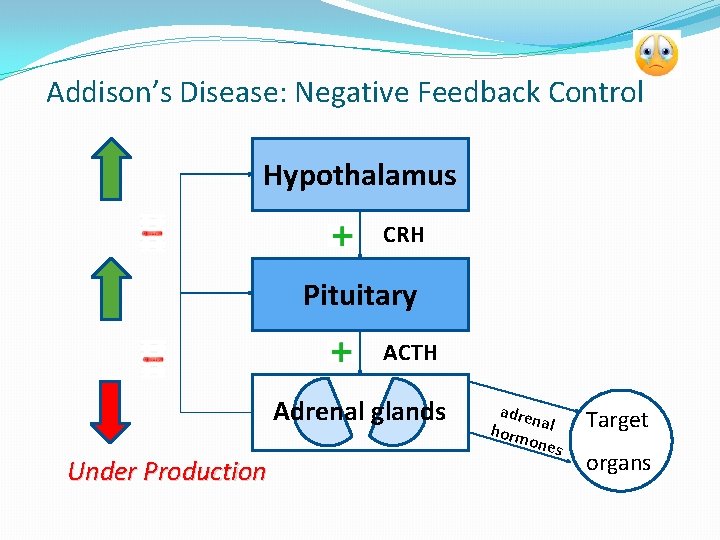
Addison’s Disease: Negative Feedback Control Hypothalamus CRH Pituitary ACTH Adrenal glands Under Production adre n horm al ones Target organs
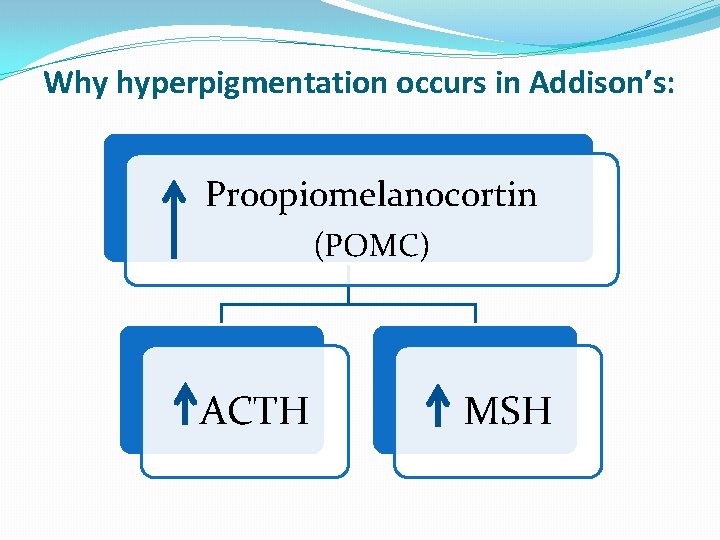
Why hyperpigmentation occurs in Addison’s: Proopiomelanocortin (POMC) ACTH MSH
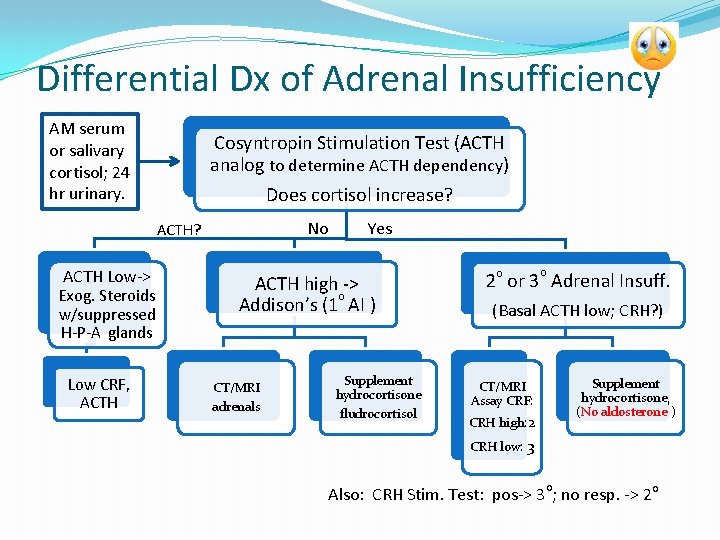
Differential Dx of Adrenal Insufficiency AM serum or salivary cortisol; 24 hr urinary. Cosyntropin Stimulation Test (ACTH analog to determine ACTH dependency) Does cortisol increase? No ACTH? ACTH Low-> Exog. Steroids w/suppressed H-P-A glands Low CRF, ACTH Yes ACTH high -> o Addison’s (1 AI ) CT/MRI adrenals Supplement hydrocortisone fludrocortisol o o 2 or 3 Adrenal Insuff. (Basal ACTH low; CRH? ) Supplement hydrocortisone, (No aldosterone ) CT/MRI Assay CRF: CRH high: 2 CRH low: 3 o Also: CRH Stim. Test: pos-> 3 ; no resp. -> 2 o
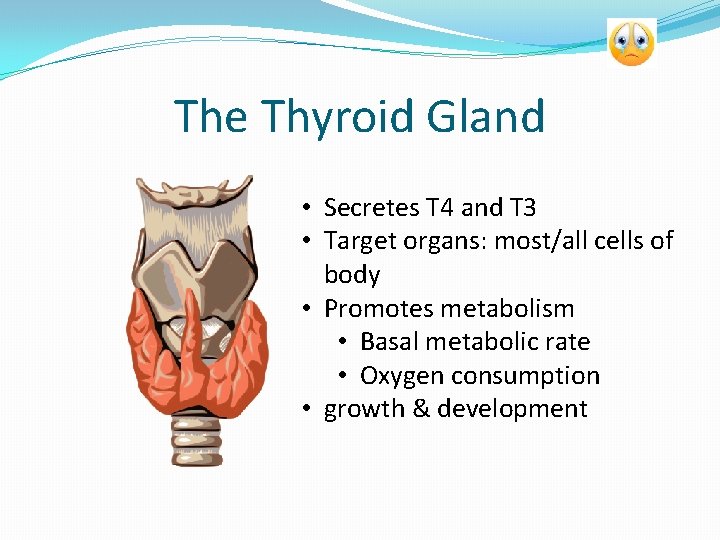
The Thyroid Gland • Secretes T 4 and T 3 • Target organs: most/all cells of body • Promotes metabolism • Basal metabolic rate • Oxygen consumption • growth & development
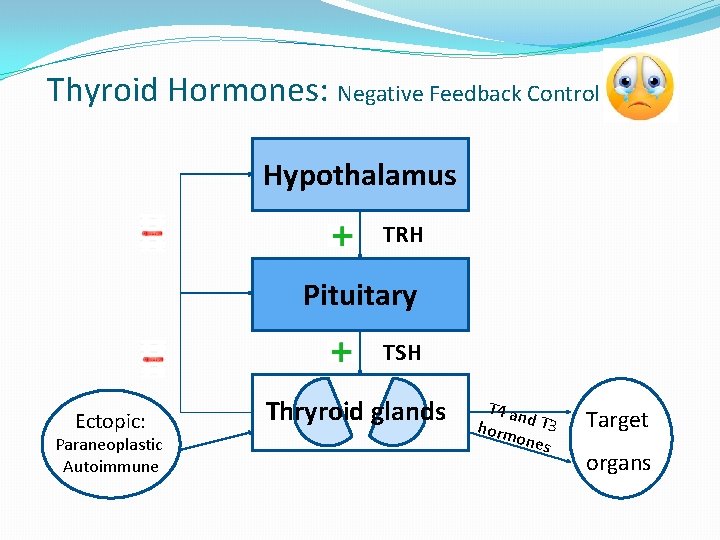
Thyroid Hormones: Negative Feedback Control Hypothalamus TRH Pituitary TSH Ectopic: Paraneoplastic Autoimmune Thryroid glands T 4 an horm d T 3 ones Target organs
Diseases of the Thyroid Gland Hyperthyroidism
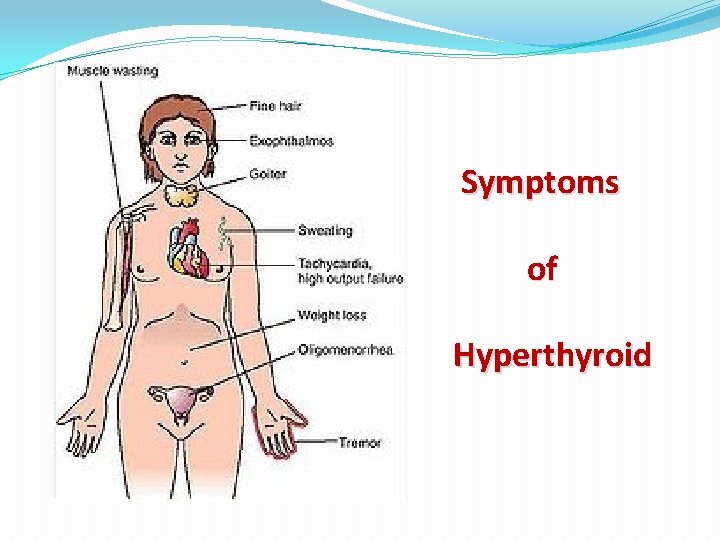
Symptoms of Hyperthyroid
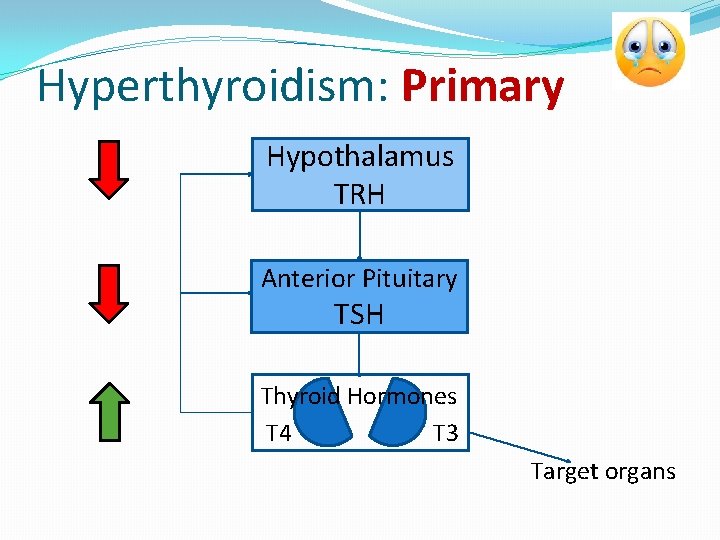
Hyperthyroidism: Primary Hypothalamus TRH Anterior Pituitary TSH Thyroid Hormones T 4 T 3 Target organs
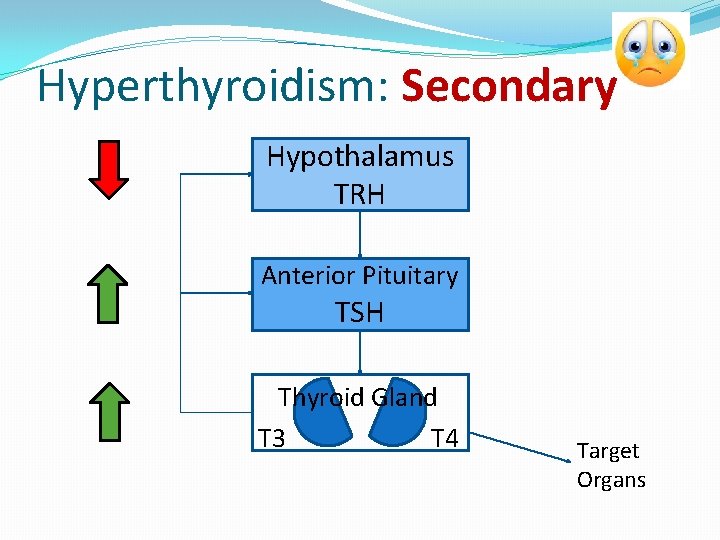
Hyperthyroidism: Secondary Hypothalamus TRH Anterior Pituitary TSH Thyroid Gland T 3 T 4 Target Organs
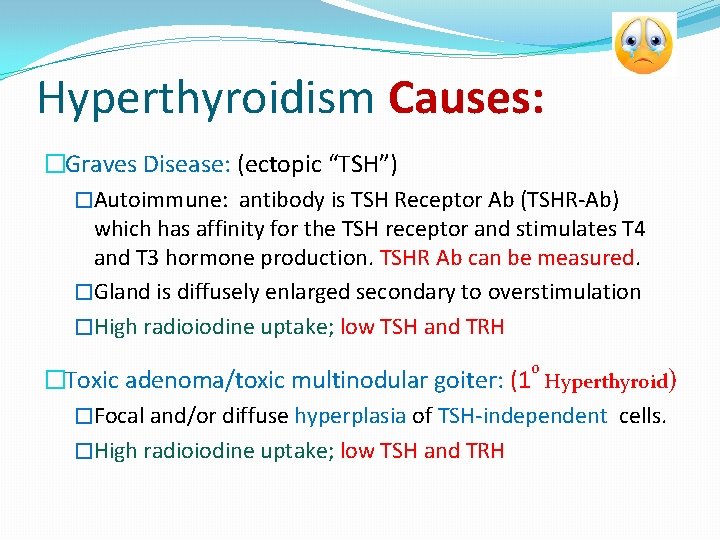
Hyperthyroidism Causes: �Graves Disease: (ectopic “TSH”) �Autoimmune: antibody is TSH Receptor Ab (TSHR-Ab) which has affinity for the TSH receptor and stimulates T 4 and T 3 hormone production. TSHR Ab can be measured. �Gland is diffusely enlarged secondary to overstimulation �High radioiodine uptake; low TSH and TRH o �Toxic adenoma/toxic multinodular goiter: (1 Hyperthyroid) �Focal and/or diffuse hyperplasia of TSH-independent cells. �High radioiodine uptake; low TSH and TRH
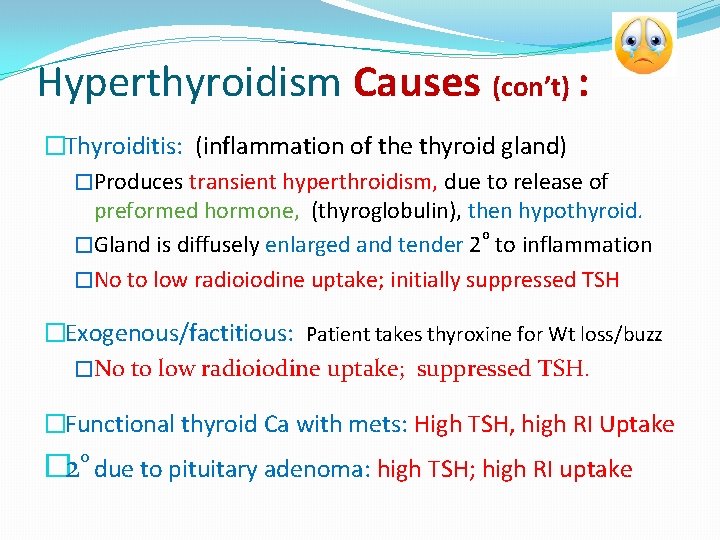
Hyperthyroidism Causes (con’t) : �Thyroiditis: (inflammation of the thyroid gland) �Produces transient hyperthroidism, due to release of preformed hormone, (thyroglobulin), then hypothyroid. o �Gland is diffusely enlarged and tender 2 to inflammation �No to low radioiodine uptake; initially suppressed TSH �Exogenous/factitious: Patient takes thyroxine for Wt loss/buzz �No to low radioiodine uptake; suppressed TSH. �Functional thyroid Ca with mets: High TSH, high RI Uptake o � 2 due to pituitary adenoma: high TSH; high RI uptake
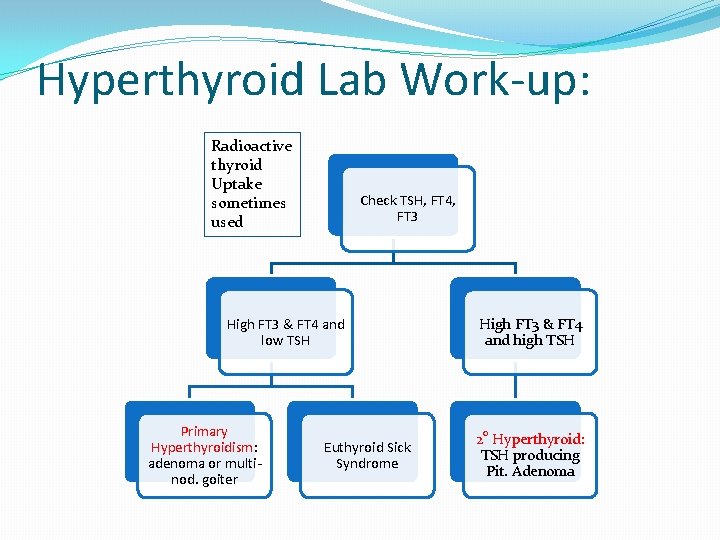
Hyperthyroid Lab Work-up: Radioactive thyroid Uptake sometimes used Check TSH, FT 4, FT 3 High FT 3 & FT 4 and low TSH Primary Hyperthyroidism: adenoma or multinod. goiter Euthyroid Sick Syndrome High FT 3 & FT 4 and high TSH 2 o Hyperthyroid: TSH producing Pit. Adenoma
Hyperthyroid Treatment: �Pharmacologic: �Beta blockers (favors formation RT 3), anxiolytics, �Suppressive: PTU (use in Pregnancy); methimazole �Radioiodine ablation: will then need replacement therapy �Thyroidectomy: will then need replacement therapy �When monitoring suppressive or replacement therapy: check TSH, FT$ plus/minus FT 3
Diseases of the Thyroid Gland Hypothyroidism
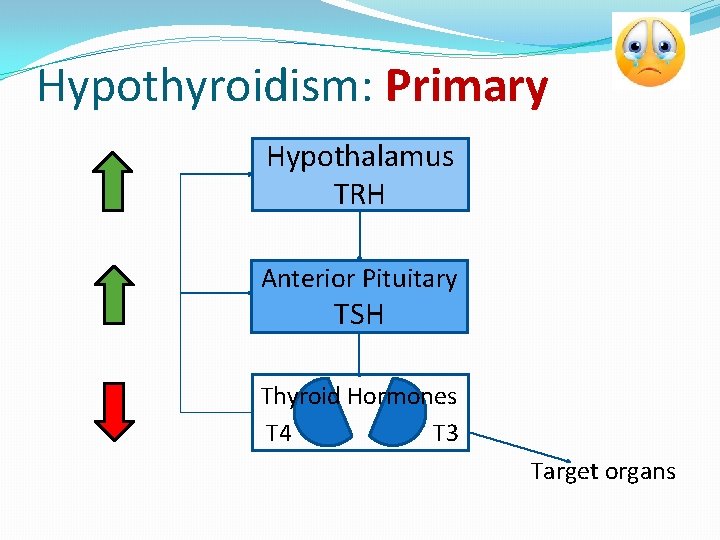
Hypothyroidism: Primary Hypothalamus TRH Anterior Pituitary TSH Thyroid Hormones T 4 T 3 Target organs
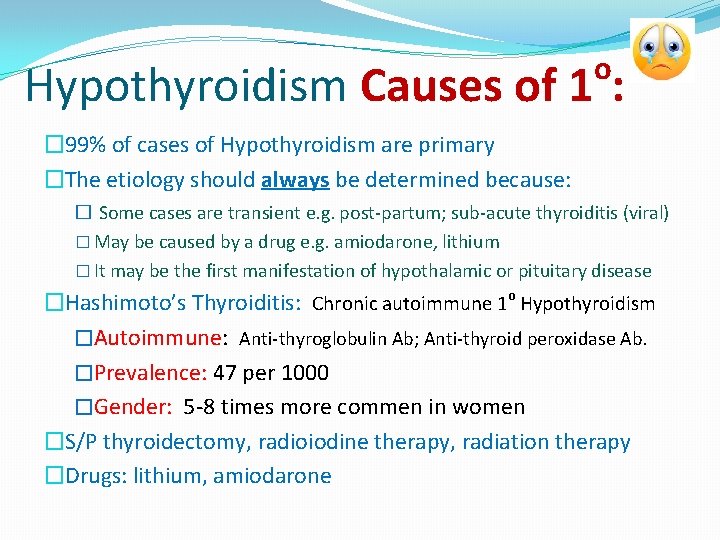
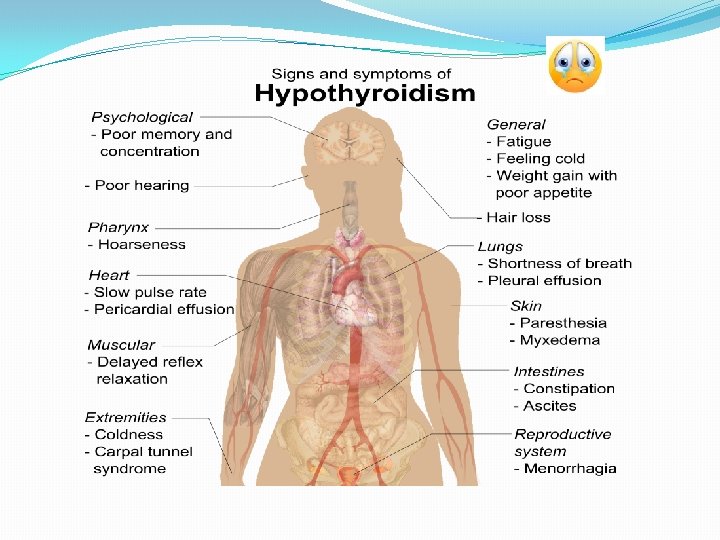
o Hypothyroidism Causes of 1 : � 99% of cases of Hypothyroidism are primary �The etiology should always be determined because: � Some cases are transient e. g. post-partum; sub-acute thyroiditis (viral) � May be caused by a drug e. g. amiodarone, lithium � It may be the first manifestation of hypothalamic or pituitary disease �Hashimoto’s Thyroiditis: Chronic autoimmune 1 o Hypothyroidism �Autoimmune: Anti-thyroglobulin Ab; Anti-thyroid peroxidase Ab. �Prevalence: 47 per 1000 �Gender: 5 -8 times more commen in women �S/P thyroidectomy, radioiodine therapy, radiation therapy �Drugs: lithium, amiodarone
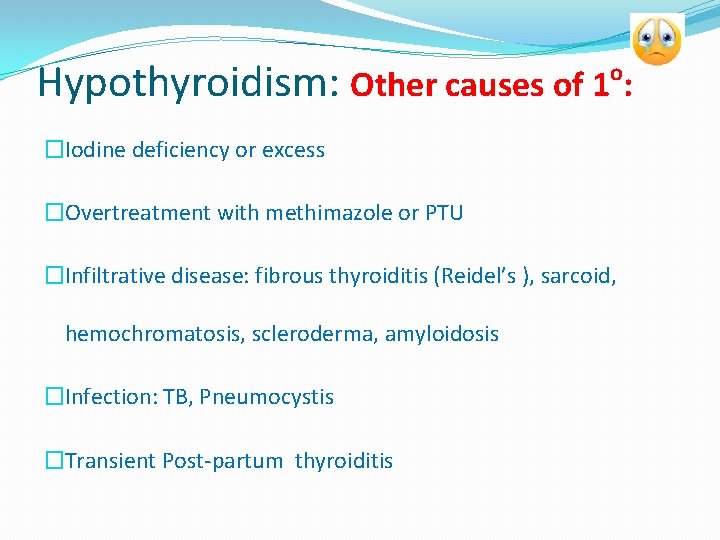
Hypothyroidism: Other causes of 1 : o �Iodine deficiency or excess �Overtreatment with methimazole or PTU �Infiltrative disease: fibrous thyroiditis (Reidel’s ), sarcoid, hemochromatosis, scleroderma, amyloidosis �Infection: TB, Pneumocystis �Transient Post-partum thyroiditis
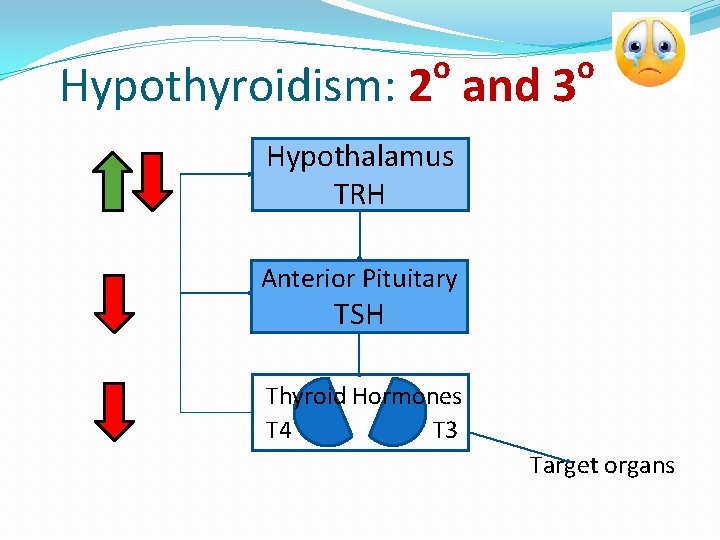
o Hypothyroidism: 2 and 3 o Hypothalamus TRH Anterior Pituitary TSH Thyroid Hormones T 4 T 3 Target organs
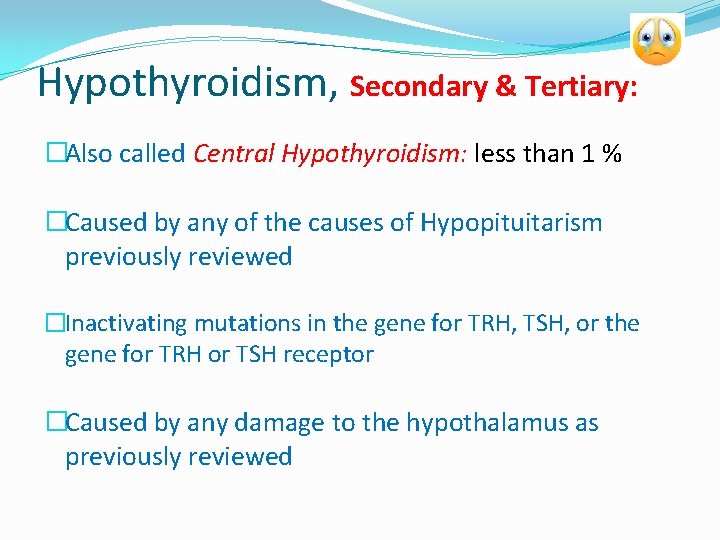
Hypothyroidism, Secondary & Tertiary: �Also called Central Hypothyroidism: less than 1 % �Caused by any of the causes of Hypopituitarism previously reviewed �Inactivating mutations in the gene for TRH, TSH, or the gene for TRH or TSH receptor �Caused by any damage to the hypothalamus as previously reviewed
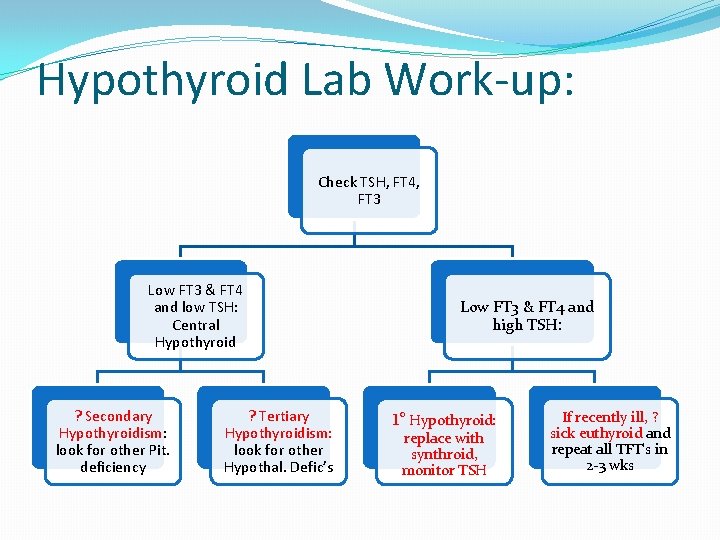
Hypothyroid Lab Work-up: Check TSH, FT 4, FT 3 Low FT 3 & FT 4 and low TSH: Central Hypothyroid ? Secondary Hypothyroidism: look for other Pit. deficiency ? Tertiary Hypothyroidism: look for other Hypothal. Defic’s Low FT 3 & FT 4 and high TSH: 1 o Hypothyroid: replace with synthroid, monitor TSH If recently ill, ? sick euthyroid and repeat all TFT’s in 2 -3 wks
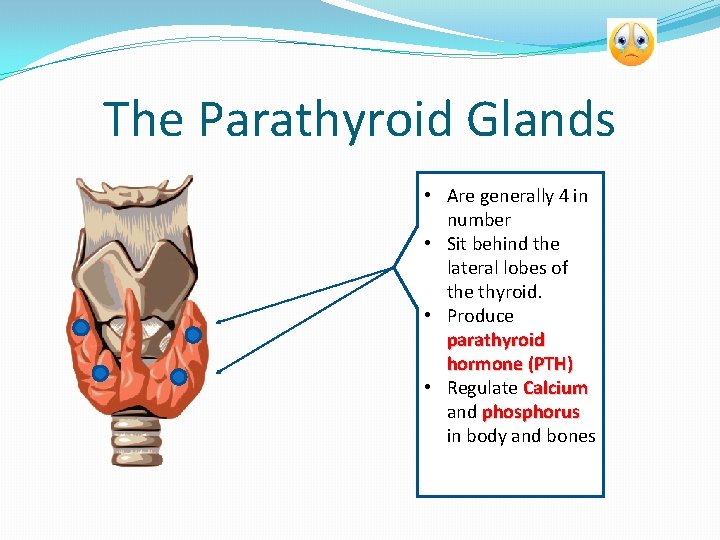
The Parathyroid Glands aare • Are generally 4 in number • Sit behind the lateral lobes of the thyroid. • Produce parathyroid hormone (PTH) • Regulate Calcium and phosphorus in body and bones
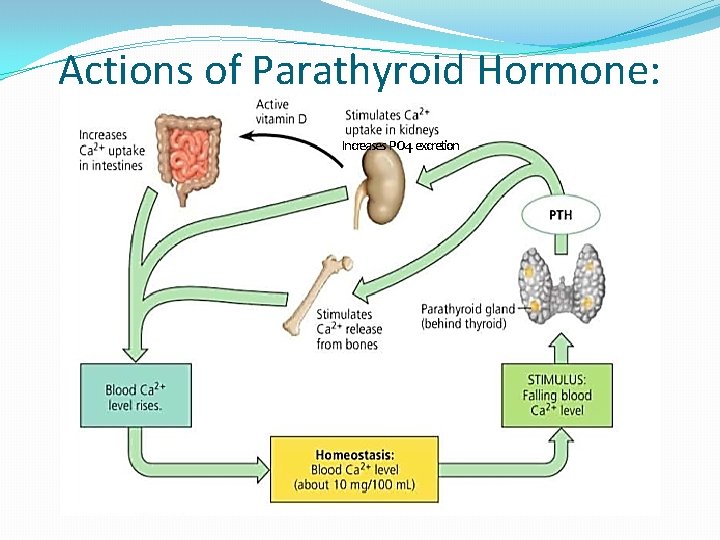
Actions of Parathyroid Hormone: Increases PO 4 excretion
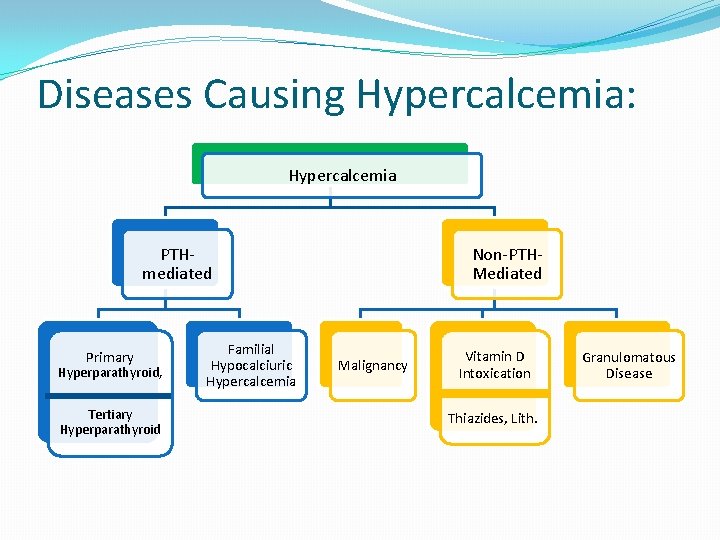
Diseases Causing Hypercalcemia: Hypercalcemia PTHmediated Primary Hyperparathyroid, Tertiary Hyperparathyroid Familial Hypocalciuric Hypercalcemia Non-PTHMediated Malignancy Vitamin D Intoxication Thiazides, Lith. Granulomatous Disease
Diseases Causing Hypercalcemia, PTH-mediated: Primary Hyperparathyroidism • Most commonly caused by solitary parathyroid adenoma • Results in increased PTH, increased Ca and decreased phosphorus • Primary Hyperparathyroidism and Malignancy (paraneoplastic) account for > 90 % of cases of hypercalcemia • Cured by surgical excision of adenoma
Diseases causing hypercalcemia, - PTH Mediated (cont’d): • Familial Hypocalciuric Hypercalcemia • • Calcium-sensing receptor mutation on Parathyroid Gland Causes increased PTH secretion Decreased urinary excretion of Ca++ Increased serum Calcium
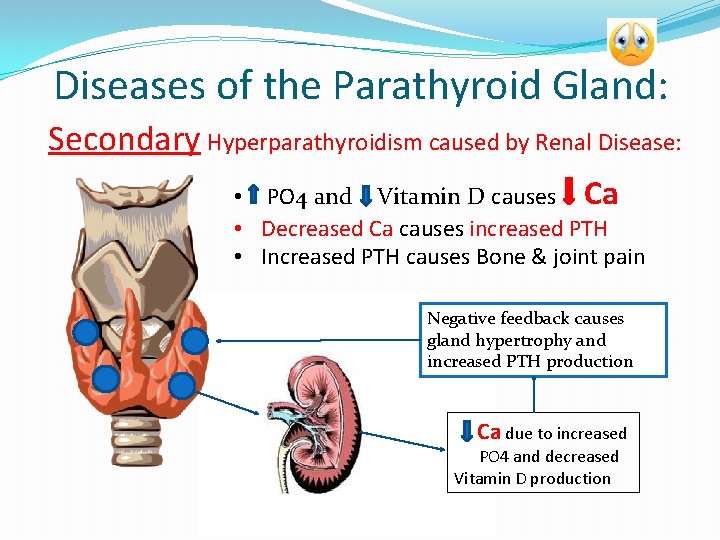
Diseases of the Parathyroid Gland: Secondary Hyperparathyroidism caused by Renal Disease: • PO 4 and Vitamin D causes Ca • Decreased Ca causes increased PTH • Increased PTH causes Bone & joint pain Negative feedback causes gland hypertrophy and increased PTH production Ca due to increased PO 4 and decreased Vitamin D production
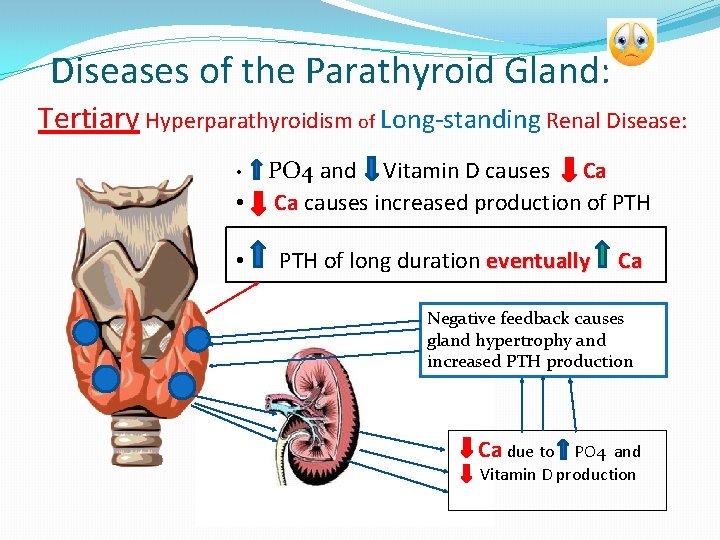
Diseases of the Parathyroid Gland: Tertiary Hyperparathyroidism of Long-standing Renal Disease: PO 4 and Vitamin D causes Ca • Ca causes increased production of PTH • • PTH of long duration eventually Ca Negative feedback causes gland hypertrophy and increased PTH production Ca due to PO 4 and Vitamin D production
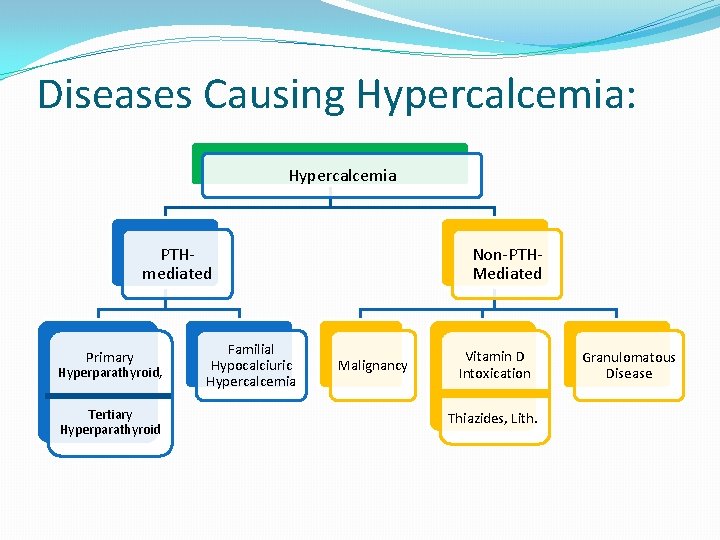
Diseases Causing Hypercalcemia: Hypercalcemia PTHmediated Primary Hyperparathyroid, Tertiary Hyperparathyroid Familial Hypocalciuric Hypercalcemia Non-PTHMediated Malignancy Vitamin D Intoxication Thiazides, Lith. Granulomatous Disease
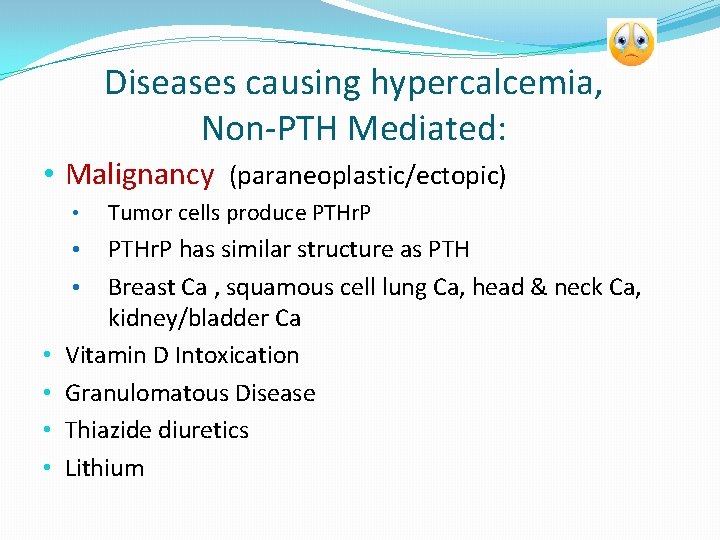
Diseases causing hypercalcemia, Non-PTH Mediated: • Malignancy (paraneoplastic/ectopic) • PTHr. P has similar structure as PTH • Breast Ca , squamous cell lung Ca, head & neck Ca, kidney/bladder Ca Vitamin D Intoxication Granulomatous Disease Thiazide diuretics Lithium • • • Tumor cells produce PTHr. P
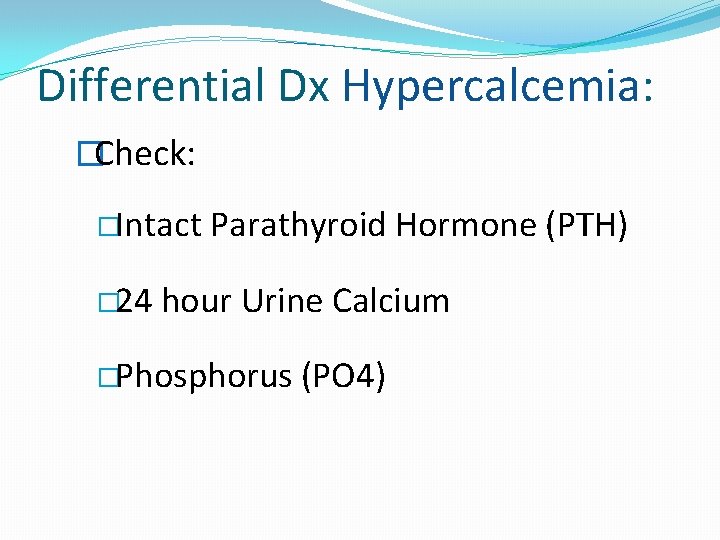
Differential Dx Hypercalcemia: �Check: �Intact � 24 Parathyroid Hormone (PTH) hour Urine Calcium �Phosphorus (PO 4)
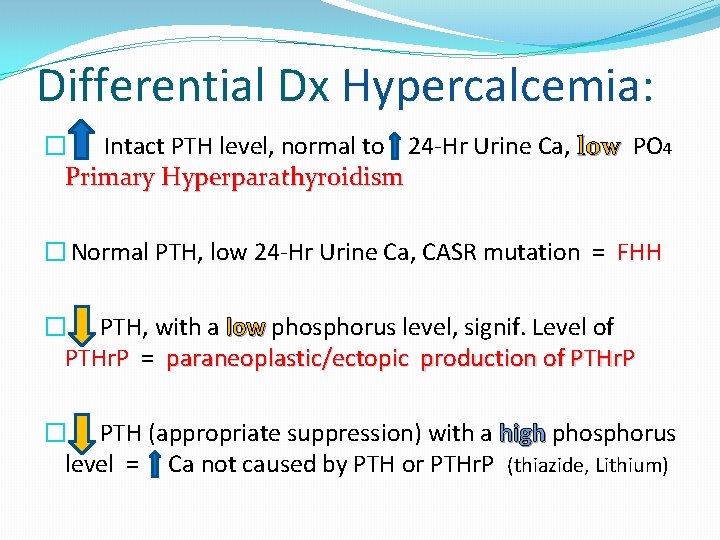
Differential Dx Hypercalcemia: � Intact PTH level, normal to 24 -Hr Urine Ca, low PO 4 Primary Hyperparathyroidism � Normal PTH, low 24 -Hr Urine Ca, CASR mutation = FHH � PTH, with a low phosphorus level, signif. Level of PTHr. P = paraneoplastic/ectopic production of PTHr. P � PTH (appropriate suppression) with a high phosphorus level = Ca not caused by PTH or PTHr. P (thiazide, Lithium)
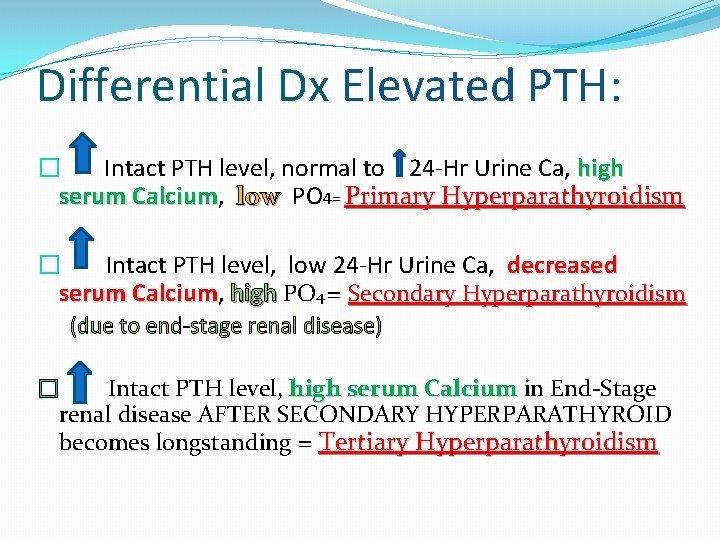
Differential Dx Elevated PTH: � Intact PTH level, normal to 24 -Hr Urine Ca, high serum Calcium, Calcium low PO 4= Primary Hyperparathyroidism � Intact PTH level, low 24 -Hr Urine Ca, decreased serum Calcium, Calcium high PO 4 = Secondary Hyperparathyroidism (due to end-stage renal disease) � Intact PTH level, high serum Calcium in End-Stage renal disease AFTER SECONDARY HYPERPARATHYROID becomes longstanding = Tertiary Hyperparathyroidism
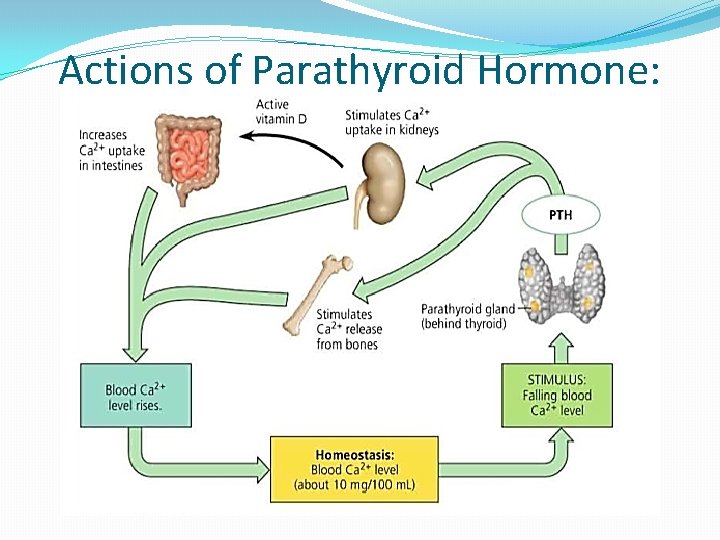
Actions of Parathyroid Hormone:
Diseases of the Parathyroid Gland Hypoparathyroidis m
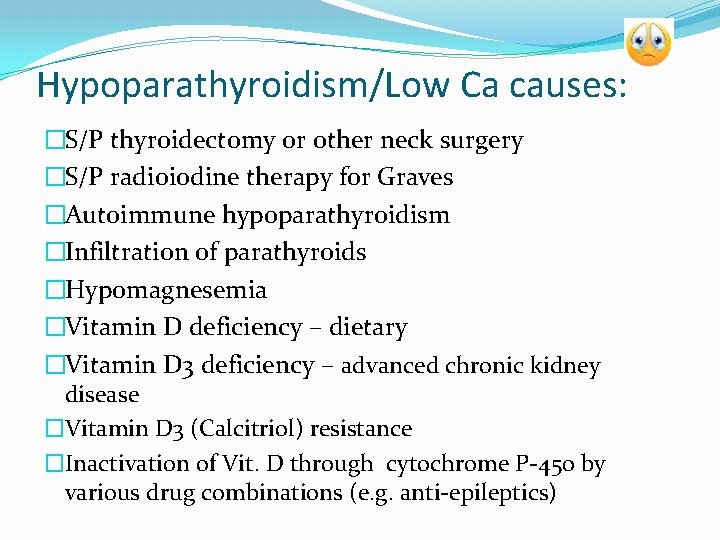
Hypoparathyroidism/Low Ca causes: �S/P thyroidectomy or other neck surgery �S/P radioiodine therapy for Graves �Autoimmune hypoparathyroidism �Infiltration of parathyroids �Hypomagnesemia �Vitamin D deficiency – dietary �Vitamin D 3 deficiency – advanced chronic kidney disease �Vitamin D 3 (Calcitriol) resistance �Inactivation of Vit. D through cytochrome P-450 by various drug combinations (e. g. anti-epileptics)

Lab Tests for Hypocalcemia and their interpretation: PTH PO 4 Hypoparathyroid Hypomagnesemia -- / -- PTH Resistance Vitamin D Defic. CKD Mg++ --- -- / Vit D 2 -- --/ -- Vit. D 3 -- / -- Creat. --- -- / -- variable --
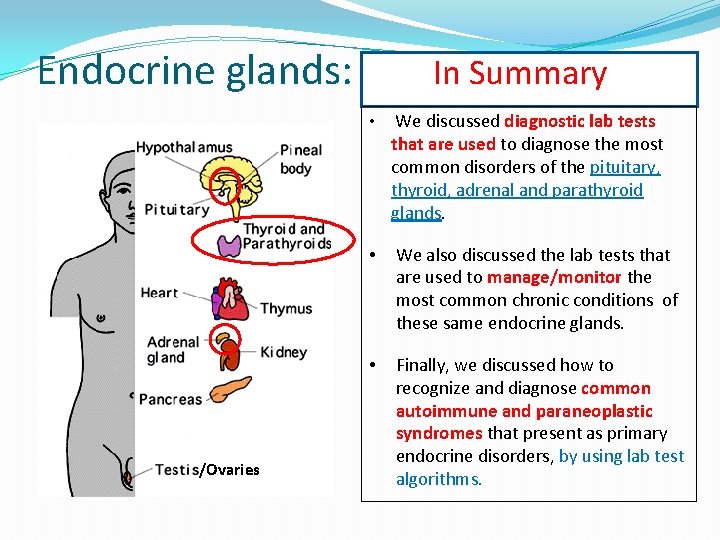
Endocrine glands: /Ovaries In Summary • We discussed diagnostic lab tests that are used to diagnose the most common disorders of the pituitary, thyroid, adrenal and parathyroid glands. • We also discussed the lab tests that are used to manage/monitor the most common chronic conditions of these same endocrine glands. • Finally, we discussed how to recognize and diagnose common autoimmune and paraneoplastic syndromes that present as primary endocrine disorders, by using lab test algorithms.
I am hopeful that I have provided you with some helpful tools to unwrap the mysteries of endocrine disorders. And, hopefully you have replaced this with this when you think about endocrine disorders !! Thank you for your attention. Questions ? ?
- Slides: 77