Encountering The Pediatric Patient Condell Medical Center EMS






















- Slides: 120
Encountering The Pediatric Patient Condell Medical Center EMS System November 2008 ECRN CE Module III Site Code #10 -7200 E 1208 Prepared by: Sharon Hopkins, RN, BSN, EMT-P
Objectives • Upon successful completion of this module, the ECRN should be able to: – Review and understand the components of the Pediatric Assessment Triangle (PAT) – Identify the difference between respiratory distress and respiratory failure – Choose the appropriate EMS field medication & dose to administer for a variety of conditions (Dextrose, Narcan, Albuterol, Valium, Epinephrine, Atropine, Adenosine, Versed, Benadryl)
– Calculate medication dosages given the patient’s weight – Calculate the GCS given the pt’s responses – Identify and appropriately state interventions for a variety of EKG rhythms specific to the pediatric population (VF, SVT, bradycardia) – Successfully complete the 10 question quiz with a score of 80% or better

Pediatric Assessment Triangle - PAT • Establishes a level of severity • Assists in determining urgency for life support • Identifies key physiological problems using observational & listening skills
General Assessment PAT • Performed when first approaching the child – Does not take the place of obtaining vital signs üCheck appearance üEvaluate work of breathing üAssess circulation to the skin
PAT - Appearance • Reflects adequacy of: üOxygenation üVentilation üBrain perfusion üHomeostasis üCNS function

Assessing Appearance • Evaluate as you cross the room and before you touch the child: . Muscle tone – can they sit up on own? . Mental status / interactivity level. Consolability. Eye contact or gaze – do they watch you? . Speech or cry
PAT - Breathing • Reflects adequacy of : oxygenation Ventilation ¤In children, work of breathing more accurate indicator of oxygenation & ventilation than respiratory rate or breath sounds (standards used in adults)
Assessing Breathing • Evaluate: . Body position. Visible movement of chest or abdominal walls . 6 -7 years-old & younger are primarily diaphragmatic (belly) breathers. Respiratory rate & effort. Audible breath sounds
PAT - Circulation • Reflects: Adequacy of cardiac output and perfusion of vital organs (core perfusion)
Assessing Circulation • Evaluate skin color: . Cyanosis reflects decreased oxygen levels in arterial blood. Cyanosis indicates vasoconstriction and respiratory failure. Trunk mottling indicates hypoxemia
Initial Assessment • Airway – is it open? • Breathing – how fast, effort being used, is it adequate? • Circulation – what is the central circulation status as well as peripheral? • Disability – AVPU and GCS • Expose – to complete a hands-on examination
Priority Patients & Transport Decisions • Decide what level of criticality this patient is • EMS to decide if the patient must go to the closest emergency department or if they have time to honor the family request if their hospital is not the closest
Additional Assessment • Includes: Focused history Physical exam Toe to head approach in the very young (infants, toddlers, preschoolers) Head to toe in the older child SAMPLE history
SAMPLE History • S – signs & symptoms • A – allergies • M – medications including herbal and over the counter (OTC) • P – past pertinent medical history • L – last oral intake (anything to eat or drink including water) • E – events leading up to the incident
Assessment & Interventions • Vital signs • Determine weight and age • Sa. O 2 reading preferably before & after O 2 administration • Cardiac monitor if applicable • Establish IV if indicated • Determine blood glucose if indicated • Reassess vital signs, Sa. O 2, patient condition
Detailed Physical Exam • Information gathered builds on the findings of the initial assessment and focused exam • Use the to head for infants, toddlers, and preschoolers

Putting It All Together • EMS is called to the scene for a 2 year-old who has fallen off the 2 nd floor porch. • The toddler landed in the grass • The toddler is unresponsive upon EMS arrival; there is a laceration to the right forehead and the right arm • is deformed
Putting It All Together Mechanism of Injury • Fall from height greater than 3 times the toddler’s height • For this 2 year-old, the mechanism of injury indicates a Category I trauma patient based on mechanism of injury (fall from height) and level of consciousness (unresponsiveness)

General Impression For This 2 year-old • Category I trauma patient with head & orthopedic injuries • EMS Region X SOP’s to follow – Spinal immobilization – Care of the airway with anticipation for need to be bagged or intubated – Hemorrhage control / interventions with IV/IO access needing to be obtained – Cardiac monitoring – Determining blood glucose level

What’s The Difference? ü Respiratory distress – The patient exhibits increased work of breathing but the patient is able to compensate for themselves • Increased respiratory effort in child who is alert, irritable, anxious, and restless • Evident use of accessory muscles – Intercostal retractions – Seesaw respirations (abdominal breathing) – Neck muscles straining
ü Respiratory failure – Energy reserves have been exhausted and the patient cannot maintain adequate oxygenation and ventilation (breathing) • Sleepy, intermittently combative or agitated child • Heart rate usually bradycardic as a result of hypoxia
Respiratory Distress • • • Stridor Grunting Gurgling Audible wheezing Tachypnea (increased respiratory rate) Mild tachycardia Head bobbing Abdominal breathing (normal < 6 -7 years-old) Nasal flaring Central cyanosis resolved with O 2
Stridor • Harsh, high-pitched sound heard on inspiration associated with upper airway obstruction • Sounds like high-pitched crowing or “seal-bark” sound on inspiration
Grunting • Compensatory mechanism to help maintain patency of small airways • A short, low-pitched sound heard at the end of exhalation • Patient trying to generate positive end-expiratory pressure (PEEP) by exhaling against a closed glottis • Prolongs the period of oxygen and carbon dioxide exchange
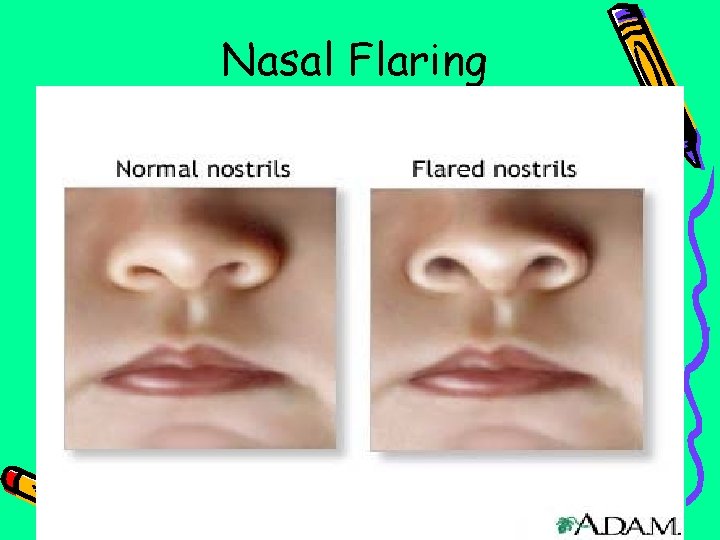
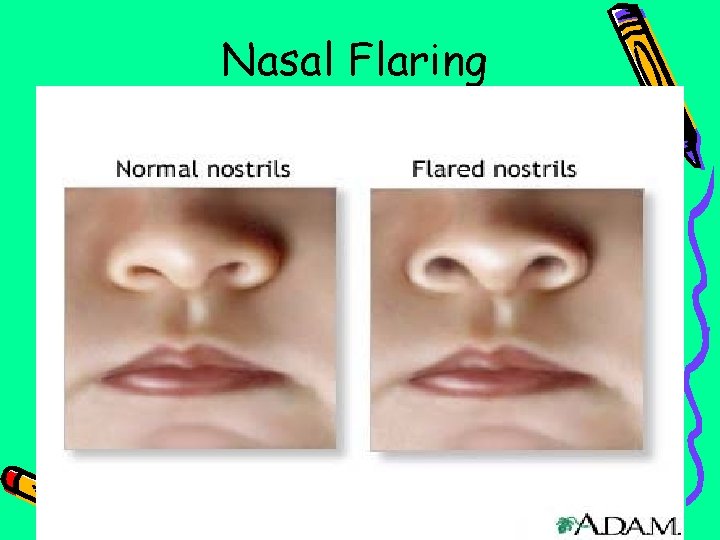
Nasal Flaring
Retractions • A visible sign where the soft tissues sink in during inhalation • Most notable are in the areas above the sternum or clavicle, over the sternum, and between the rib spaces
Respiratory Failure • Decreased level of responsiveness or response to pain • Decreased muscle tone • Inadequate respiratory rate, effort, or chest excursion • Tachypnea with periods of bradypnea slowing to agonal breathing
IV Access • Peripheral access can be difficult to find in a child – More sub Q fat – Smaller targets – More fragile veins – Lack of our experience
Hint to Find Peds Veins • Hold your penlight across the skin to reflect the veins • Hold the penlight under the site to illuminate the veins
EMS IO Indications • Shock, arrest, or impending arrest • Unconscious/unresponsive to stimuli • 2 unsuccessful IV attempts or 90 second duration • Peds needle used for 3 – 39 kg (up to 88 lbs) - Peds needle 15 G 5/8 (G same as adult, length is shorter)
EZ IO Landmarks ü Proximal medial tibia • <39 kg (child) – tibial tuberosity often difficult to palpate & if not palpated – Go 2 finger breadths below patella and then on flat aspect of medial tibia • 40 kg (88 pounds or more) – 1 -2 finger breadths below patella (this is usually 1/2 (1 cm) distal to tibial tuberosity) – 1 finger breadth medially from the tibial – tuberosity

Tibial tuberosity
EZ IO Infusion • All patients need to have the IO flushed prior to connecting the IV solution • The primed extension tubing must be used with a syringe attached • Only the syringe is removed after flushing in preparation to attaching IV fluid • All IV bags need a pressure bag to • flow

EMS Altered Level of Consciousness SOP • If blood glucose level is <60 – < 1 year old – Dextrose 12. 5% 4 ml/kg – > 1 -15 years old – Dextrose 25% 2 ml/kg • If no IV/IO access – Glucagon 0. 1 mg/kg IM • Max dose up to 1 mg (max at adult dosage)
• If you suspect narcotic influence or as a diagnostic tool if blood sugar is okay or patient does not respond to Dextrose – Narcan EMS dosing ü<20 kg = 0. 1 mg/kg IVP/IO/IM ü>20 kg = 2 mg IVP/IO/IM • Max total dose is 2 mg
Dextrose • The brain is a very sensitive organ to inadequate levels of glucose • When the glucose levels drop the patient will have an altered level of consciousness • If glucose levels reach a critically low level, the patient may have a seizure
Narcan • Useful to reverse the effects of narcotics (respiratory depression and depression of the central nervous system) • Morphine, hydromorphine (Dilaudid), oxycodone, Demerol, heroin, codeine, percodan, fentanyl, darvon, methadone • Consider the children that get into other’s purses and have access to the medicine cabinet & other areas where drugs can be found
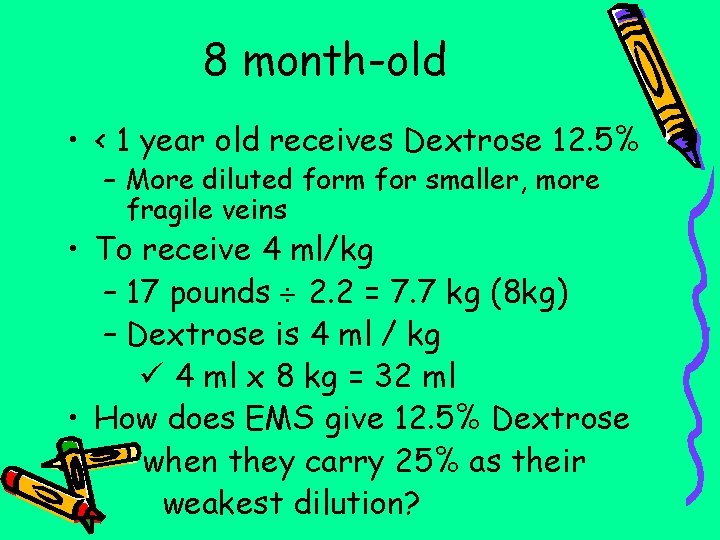
Calculation Practice • Your 8 month-old patient weighs 17 pounds • Which strength Dextrose should this patient receive by EMS and how much?
8 month-old • < 1 year old receives Dextrose 12. 5% – More diluted form for smaller, more fragile veins • To receive 4 ml/kg – 17 pounds 2. 2 = 7. 7 kg (8 kg) – Dextrose is 4 ml / kg ü 4 ml x 8 kg = 32 ml • How does EMS give 12. 5% Dextrose when they carry 25% as their weakest dilution?
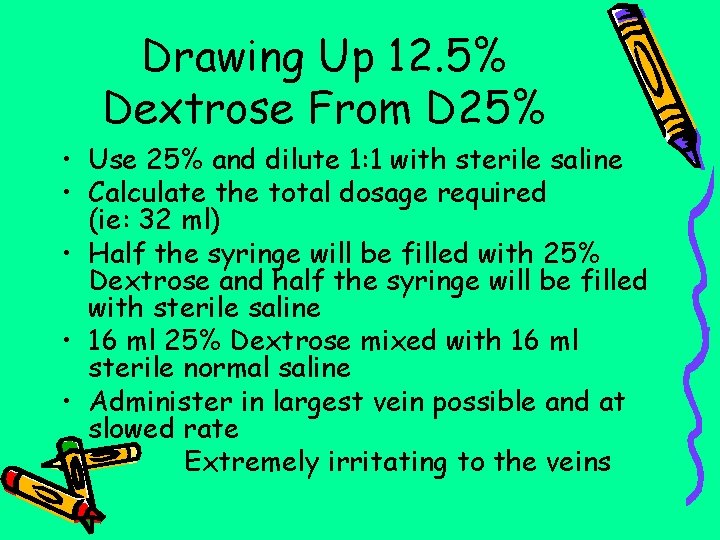
Drawing Up 12. 5% Dextrose From D 25% • Use 25% and dilute 1: 1 with sterile saline • Calculate the total dosage required (ie: 32 ml) • Half the syringe will be filled with 25% Dextrose and half the syringe will be filled with sterile saline • 16 ml 25% Dextrose mixed with 16 ml sterile normal saline • Administer in largest vein possible and at slowed rate – Extremely irritating to the veins
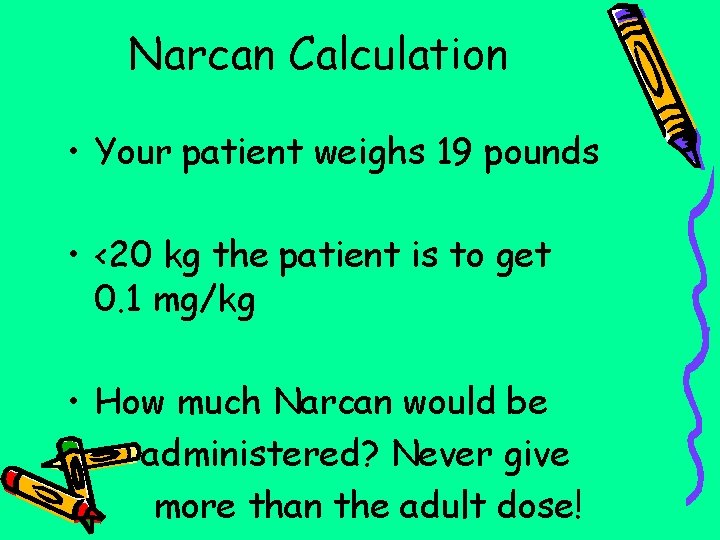
Narcan Calculation • Your patient weighs 19 pounds • <20 kg the patient is to get 0. 1 mg/kg • How much Narcan would be administered? Never give more than the adult dose!

Narcan for 19 Pound Infant • 19 pounds 2. 2 kg = 8. 6 kg (9 kg) • 9 kg x 0. 1 mg/kg = 0. 9 mg • (You still need to know how many ml’s to put into the syringe) • What type of syringe would you use? – Under 1 ml use a TB syringe – much more accurate to draw up medications
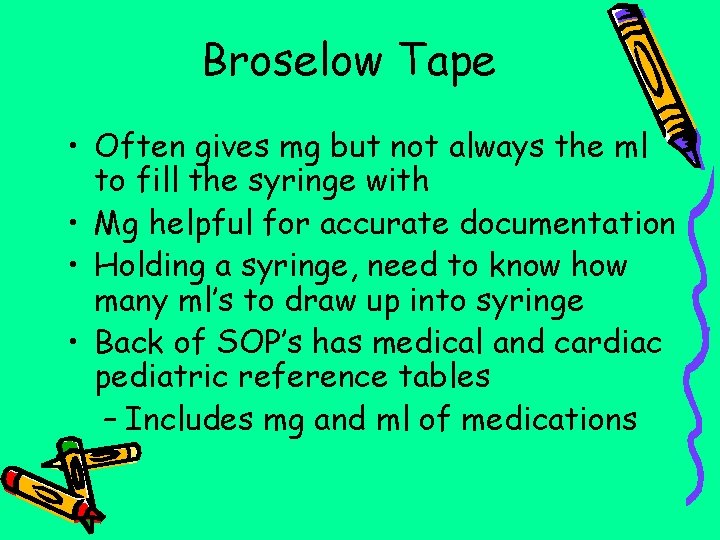
Broselow Tape • Often gives mg but not always the ml to fill the syringe with • Mg helpful for accurate documentation • Holding a syringe, need to know how many ml’s to draw up into syringe • Back of SOP’s has medical and cardiac pediatric reference tables – Includes mg and ml of medications

GCS For Pediatric Patient • Same tool used for the adult population with minor changes to accommodate the young nonverbal infant • Most accommodations made in the verbal section • Makes sense if this is for the non-verbal patient
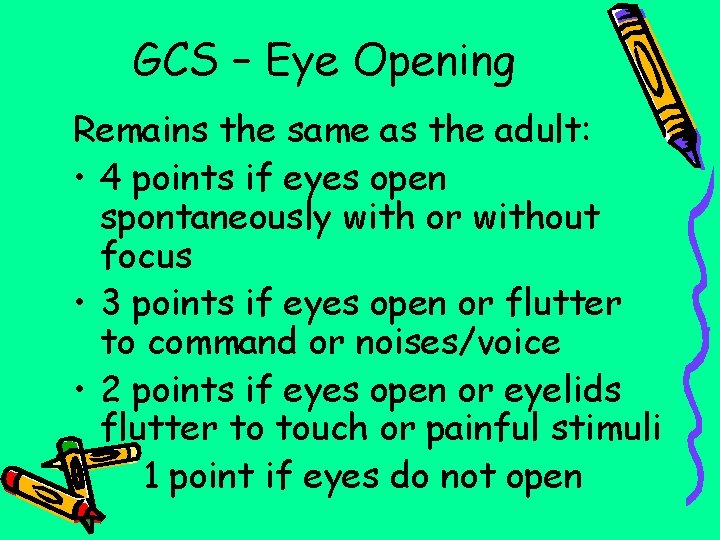
GCS – Eye Opening Remains the same as the adult: • 4 points if eyes open spontaneously with or without focus • 3 points if eyes open or flutter to command or noises/voice • 2 points if eyes open or eyelids flutter to touch or painful stimuli • 1 point if eyes do not open
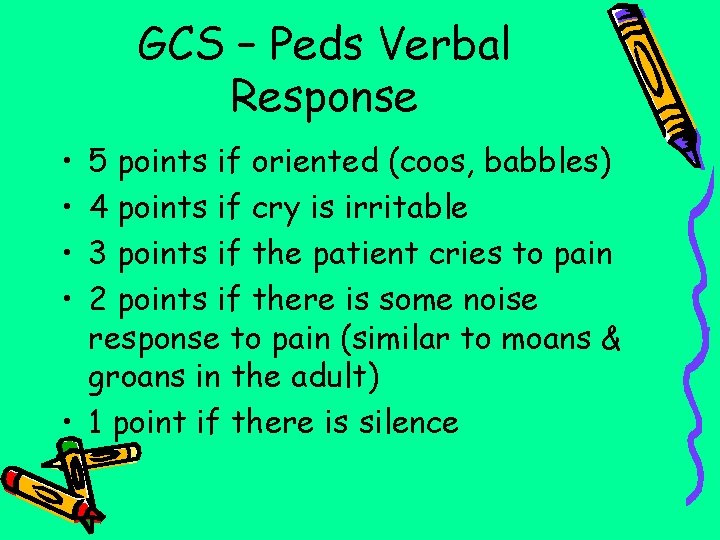
GCS – Peds Verbal Response • • 5 points if oriented (coos, babbles) 4 points if cry is irritable 3 points if the patient cries to pain 2 points if there is some noise response to pain (similar to moans & groans in the adult) • 1 point if there is silence
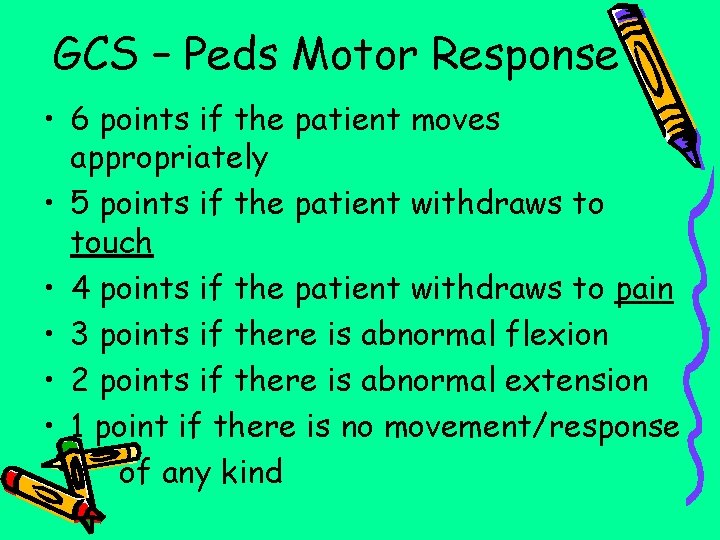
GCS – Peds Motor Response • 6 points if the patient moves appropriately • 5 points if the patient withdraws to touch • 4 points if the patient withdraws to pain • 3 points if there is abnormal flexion • 2 points if there is abnormal extension • 1 point if there is no movement/response of any kind
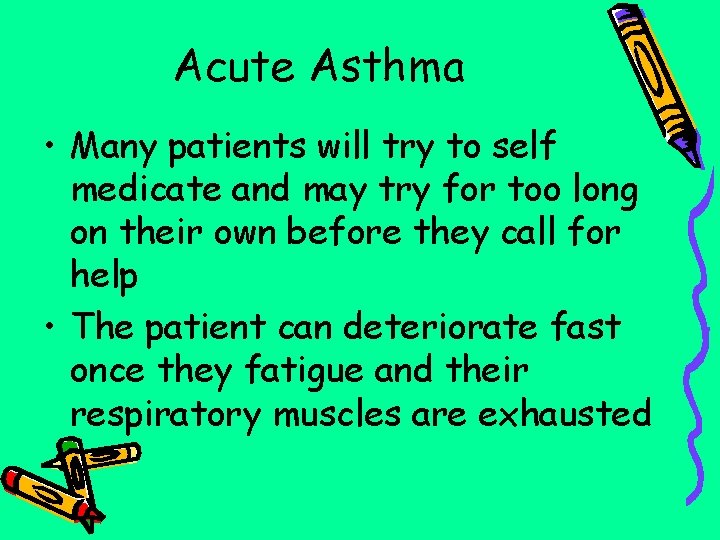
Acute Asthma • Many patients will try to self medicate and may try for too long on their own before they call for help • The patient can deteriorate fast once they fatigue and their respiratory muscles are exhausted
Why Albuterol? • Albuterol is a bronchodilator • Receptors are in the lungs • Opens up constricted bronchiole passages • Albuterol also triggers receptors in the heart and you may see an increase in heart • rate

EMS Albuterol Dosing • 2. 5 mg/3 ml for all patients • The drug will be more successful when the patient is coached through use of the nebulizer • The drug only works if it is inhaled deeply into the lungs • Short, shallow breaths will not help drug absorption
Nebulizer Delivery • This route is most effective if there is someone “coaching” the patient during use – Have someone talk the patient through the process • Verbal encouragement essential to success – Encourage slower breaths for a few ventilations – Then encourage the breaths to be a bit deeper – Then encourage the deeper breaths to be held a bit longer to get the drug down into the lungs
In-line Albuterol • Any patient no longer able to take a deep breath or remain conscious needs this drug “forced” into the lungs • The drug must be given in-line – Attach nebulizer to the BVM mask as you start bagging the patient to get some drug into the lungs – Once intubated, the ambu bag will continue to force the drug into the airway and down into the lungs

What Are the Risk Factors That Expose Kids To Seizures? • • Fever – most common Hypoxia Infections Electrolyte imbalance Head trauma Hypoglycemia Toxic ingestions Tumor
Status Epilepticus • A series of one or more generalized seizures without any periods of consciousness • Concern is with periods of prolonged apnea that can lead to hypoxia
Assessment of Seizures • ALWAYS obtain a glucose level if level of consciousness is altered • Ask if there is a history of recent illness • Ask for description of the seizure activity – Jerking of both sides of the body, jerking limited to a particular part of the body, eye blinking, staring, lip smacking
EMS Seizure Intervention • Support the airway – Consider BVM if active seizure • To terminate current seizure – Valium 0. 2 mg/kg IVP – No IV access, Valium rectally 0. 5 mg/kg – Max total rectally 10 mg • Remove extra clothing if febrile • Cool cloths over patient, fan patient • Shivering will increase body temp!
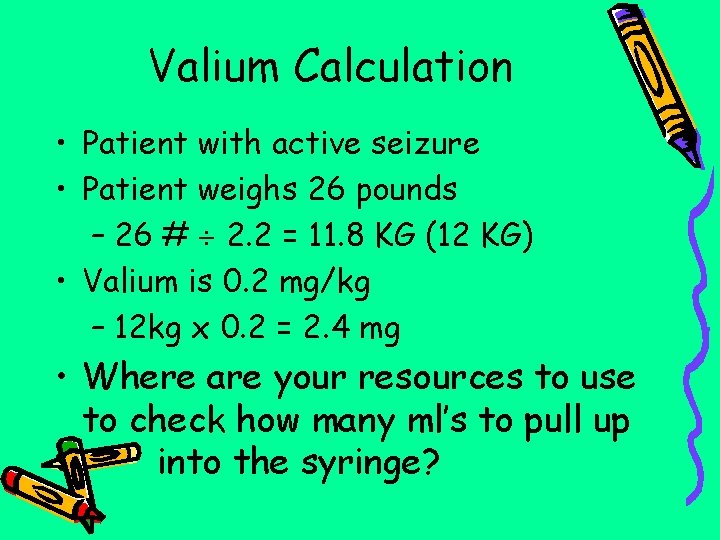
Valium Calculation • Patient with active seizure • Patient weighs 26 pounds – 26 # 2. 2 = 11. 8 KG (12 KG) • Valium is 0. 2 mg/kg – 12 kg x 0. 2 = 2. 4 mg • Where are your resources to use to check how many ml’s to pull up • into the syringe?
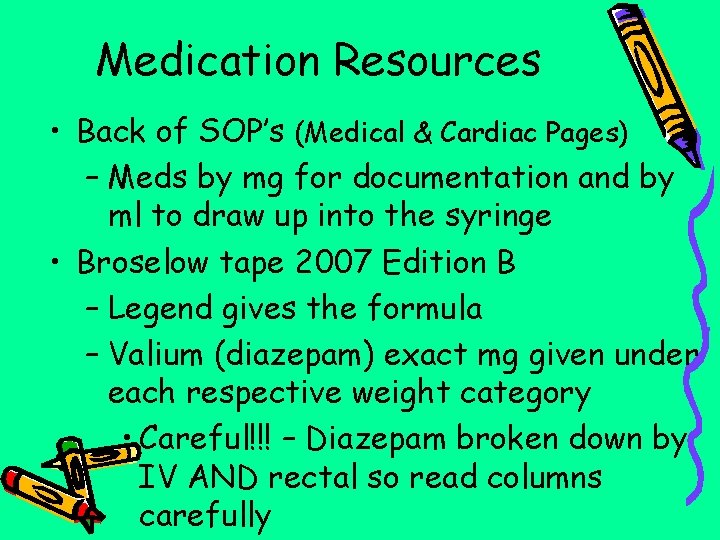
Medication Resources • Back of SOP’s (Medical & Cardiac Pages) – Meds by mg for documentation and by ml to draw up into the syringe • Broselow tape 2007 Edition B – Legend gives the formula – Valium (diazepam) exact mg given under each respective weight category • Careful!!! – Diazepam broken down by IV AND rectal so read columns carefully

Possible Causes of Critical Rhythms • 6 H’s – Hypovolemia – fluid challenge – Hypoxia – supplemental O 2 – Acidosis – ventilate to blow off CO 2 – Hyper/hypokalema – Hypothermia – warm core – Hypoglycemia – check glucose level

• 5 T’s – Tablets – drug overdose – Tamponade – supportive care in field – Tension pneumothorax – needle decompression – Thrombosis, coronary or pulmonary – Trauma
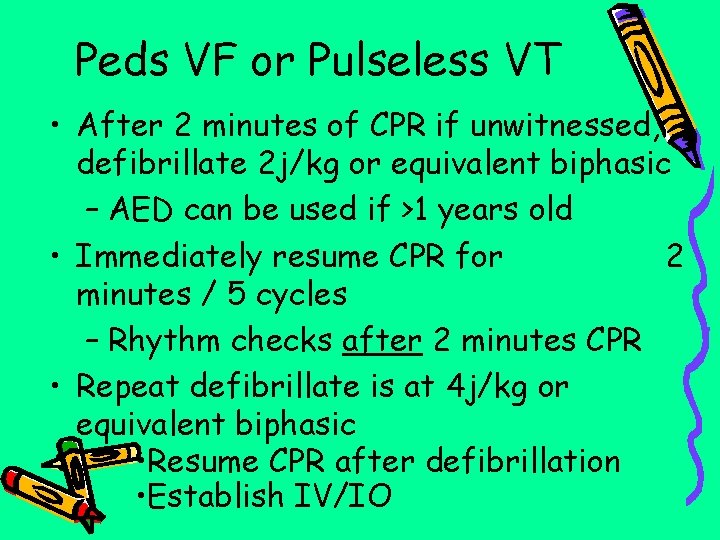
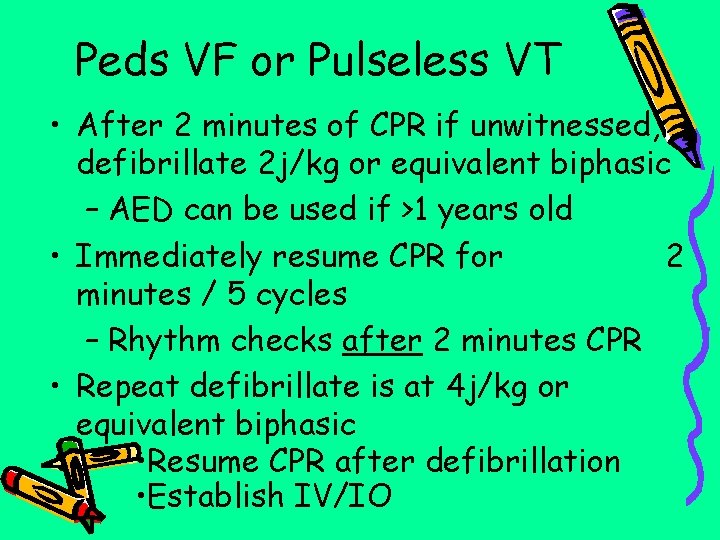
Peds VF or Pulseless VT • After 2 minutes of CPR if unwitnessed, defibrillate 2 j/kg or equivalent biphasic – AED can be used if >1 years old • Immediately resume CPR for 2 minutes / 5 cycles – Rhythm checks after 2 minutes CPR • Repeat defibrillate is at 4 j/kg or equivalent biphasic • Resume CPR after defibrillation • Establish IV/IO
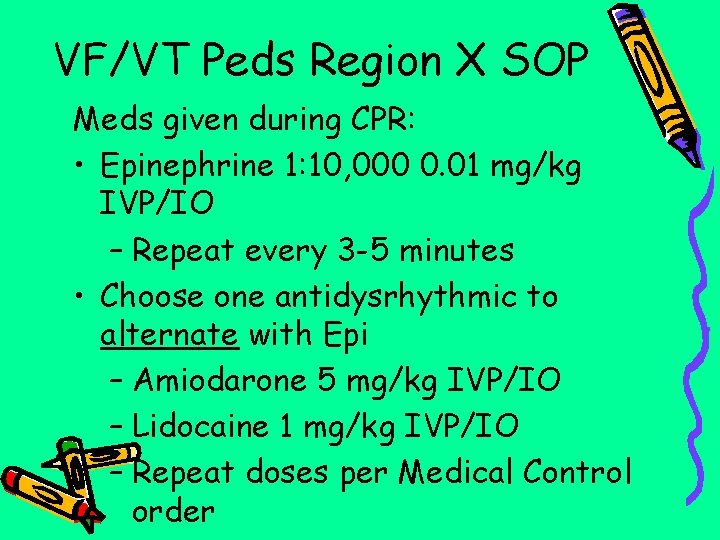
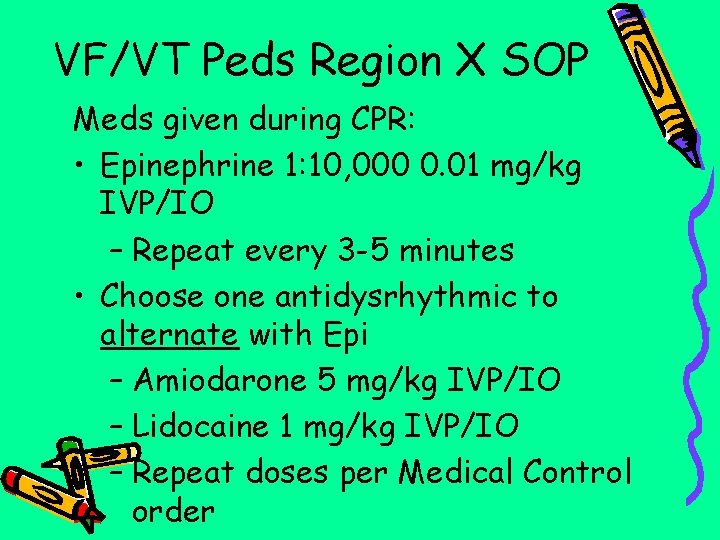
VF/VT Peds Region X SOP Meds given during CPR: • Epinephrine 1: 10, 000 0. 01 mg/kg IVP/IO – Repeat every 3 -5 minutes • Choose one antidysrhythmic to alternate with Epi – Amiodarone 5 mg/kg IVP/IO – Lidocaine 1 mg/kg IVP/IO – Repeat doses per Medical Control order
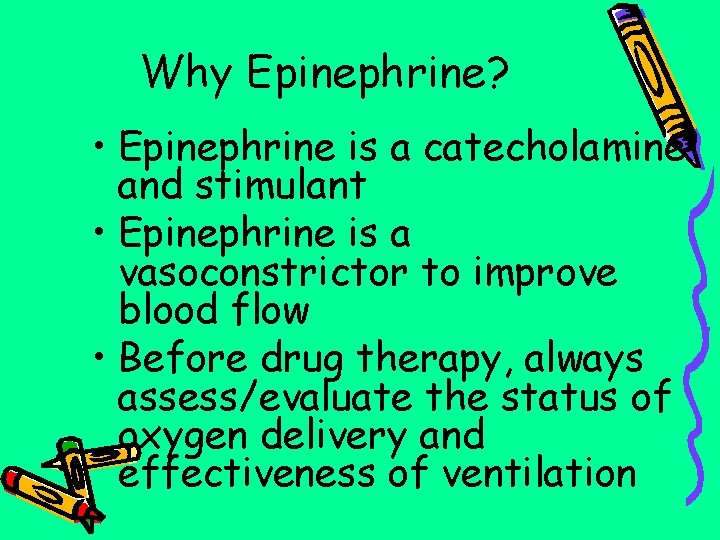
Why Epinephrine? • Epinephrine is a catecholamine and stimulant • Epinephrine is a vasoconstrictor to improve blood flow • Before drug therapy, always assess/evaluate the status of oxygen delivery and effectiveness of ventilation
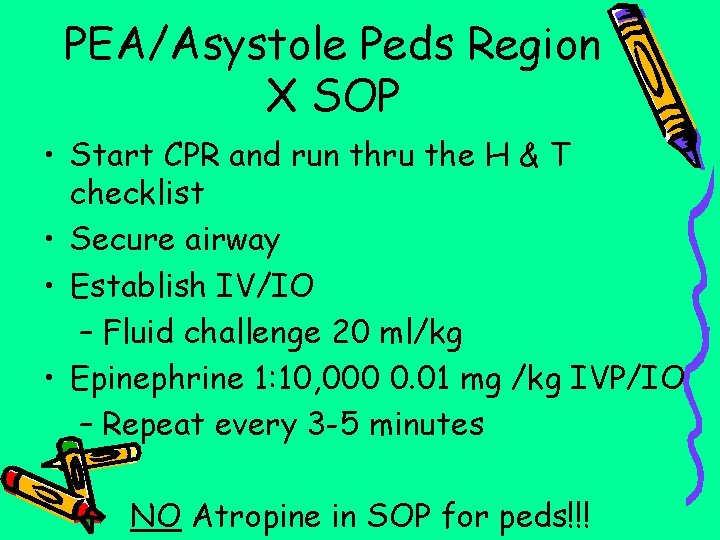
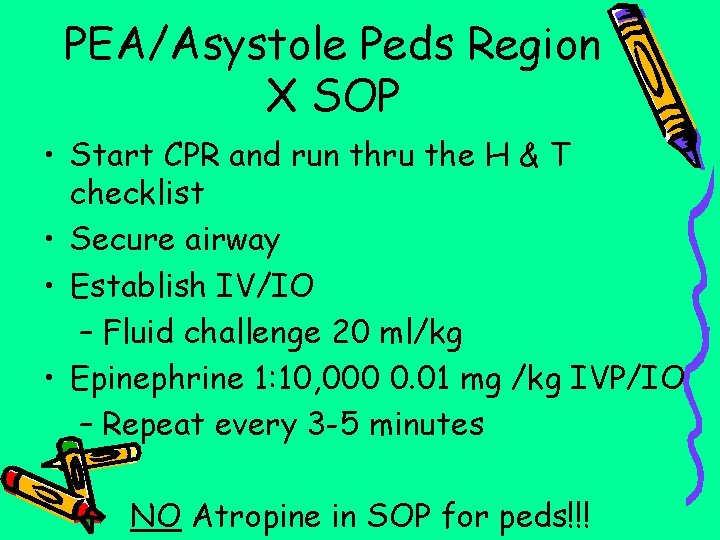
PEA/Asystole Peds Region X SOP • Start CPR and run thru the H & T checklist • Secure airway • Establish IV/IO – Fluid challenge 20 ml/kg • Epinephrine 1: 10, 000 0. 01 mg /kg IVP/IO – Repeat every 3 -5 minutes – NO Atropine in SOP for peds!!!
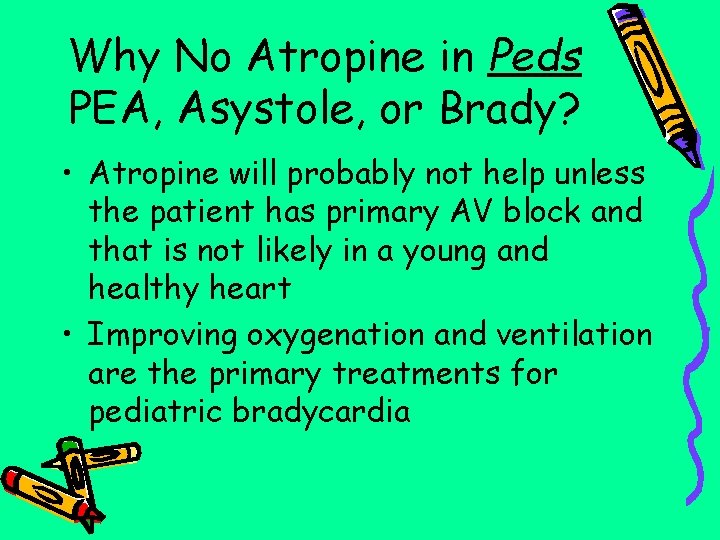
Why No Atropine in Peds PEA, Asystole, or Brady? • Atropine will probably not help unless the patient has primary AV block and that is not likely in a young and healthy heart • Improving oxygenation and ventilation are the primary treatments for pediatric bradycardia
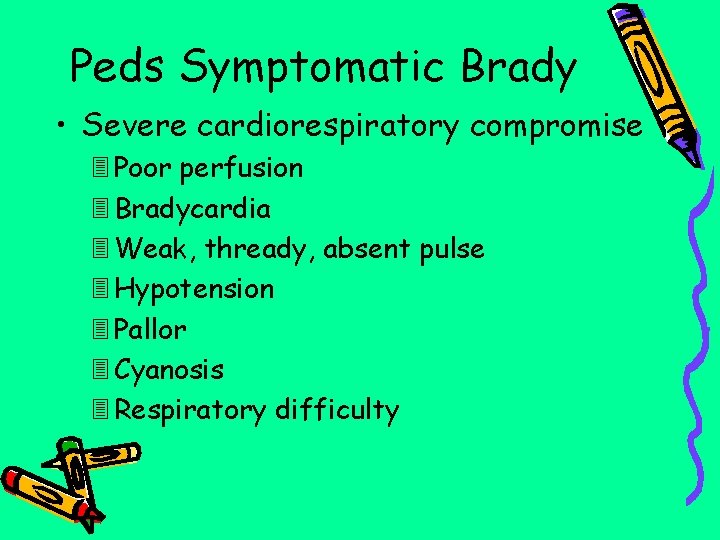
Peds Symptomatic Brady • Severe cardiorespiratory compromise Poor perfusion Bradycardia Weak, thready, absent pulse Hypotension Pallor Cyanosis Respiratory difficulty
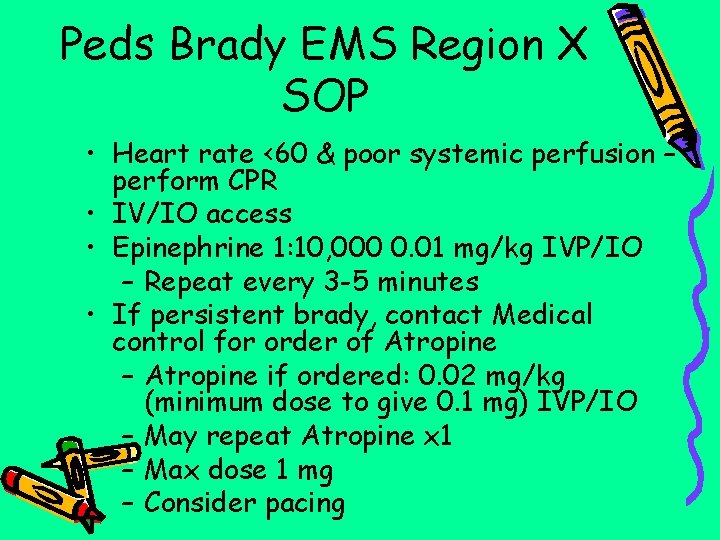
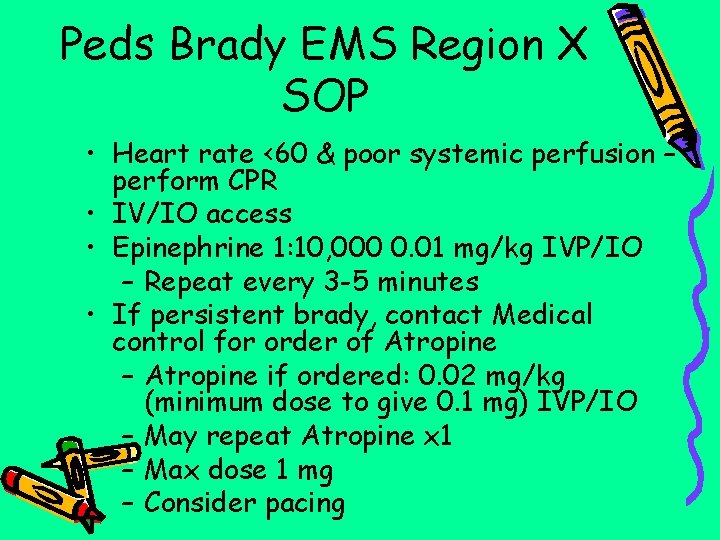
Peds Brady EMS Region X SOP • Heart rate <60 & poor systemic perfusion – perform CPR • IV/IO access • Epinephrine 1: 10, 000 0. 01 mg/kg IVP/IO – Repeat every 3 -5 minutes • If persistent brady, contact Medical control for order of Atropine – Atropine if ordered: 0. 02 mg/kg (minimum dose to give 0. 1 mg) IVP/IO – May repeat Atropine x 1 – Max dose 1 mg – Consider pacing
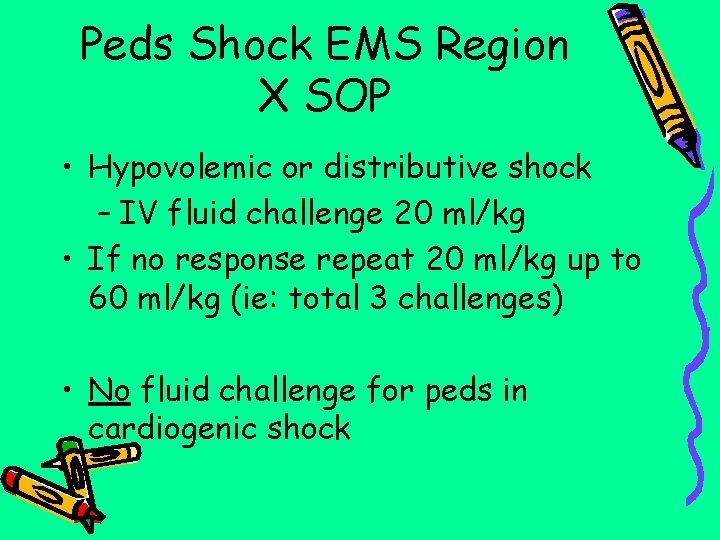
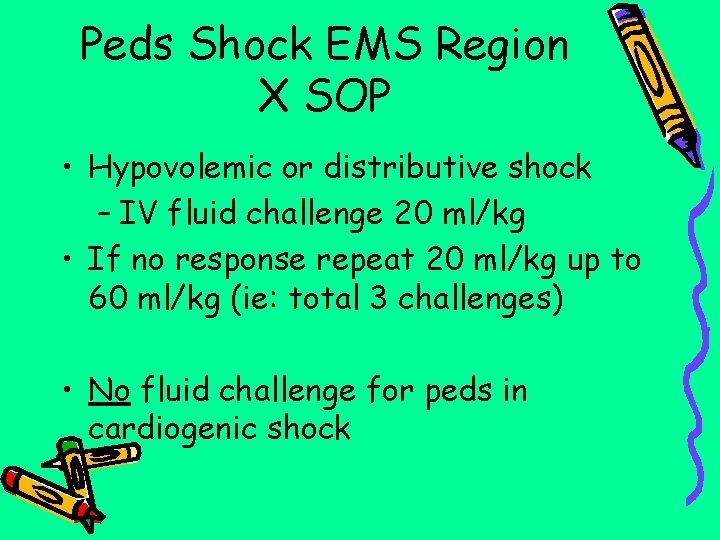
Peds Shock EMS Region X SOP • Hypovolemic or distributive shock – IV fluid challenge 20 ml/kg • If no response repeat 20 ml/kg up to 60 ml/kg (ie: total 3 challenges) • No fluid challenge for peds in cardiogenic shock

Peds Tachycardia ¤Bradydysrhythmias are more common in peds patients than tachycardias • Sinus Tachycardia – Heart rates in infants are under 220 and in children under 180 – No drug therapy indicated – Search for possible causes
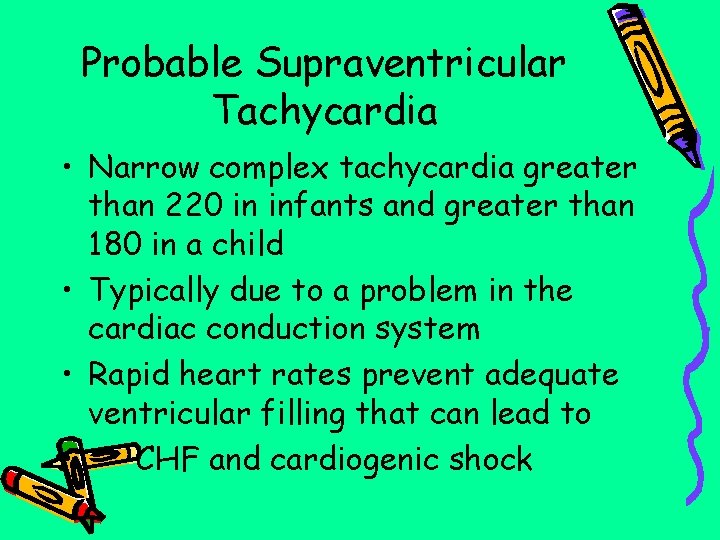
Probable Supraventricular Tachycardia • Narrow complex tachycardia greater than 220 in infants and greater than 180 in a child • Typically due to a problem in the cardiac conduction system • Rapid heart rates prevent adequate ventricular filling that can lead to • CHF and cardiogenic shock
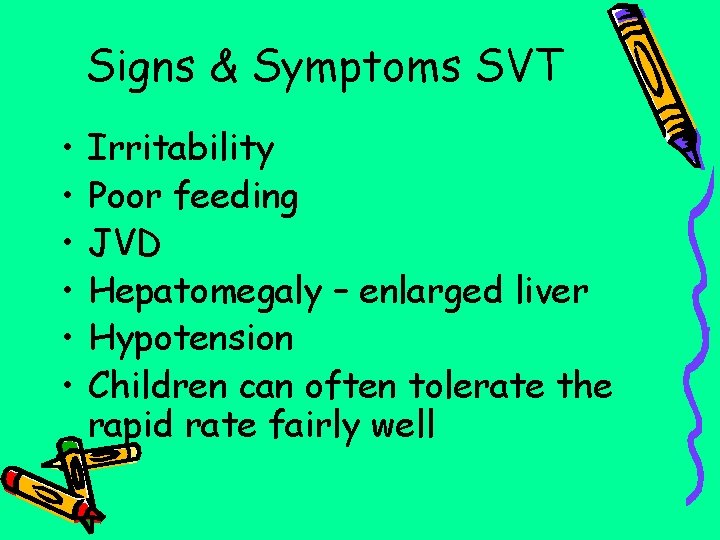
Signs & Symptoms SVT • • • Irritability Poor feeding JVD Hepatomegaly – enlarged liver Hypotension Children can often tolerate the rapid rate fairly well
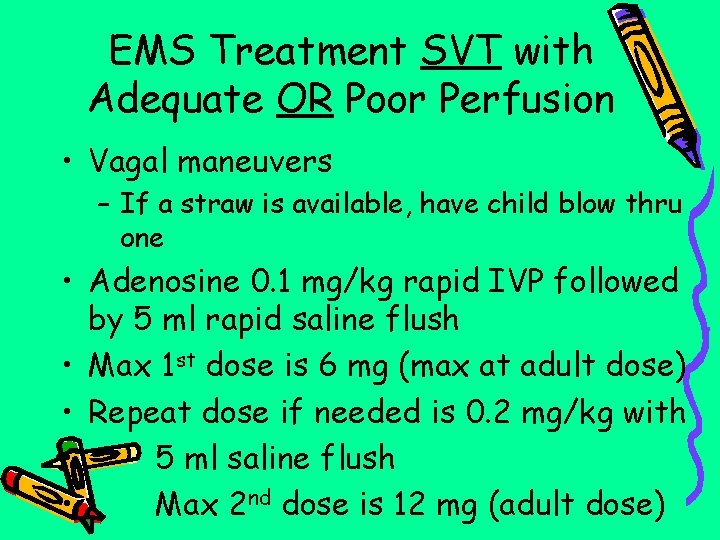
EMS Treatment SVT with Adequate OR Poor Perfusion • Vagal maneuvers – If a straw is available, have child blow thru one • Adenosine 0. 1 mg/kg rapid IVP followed by 5 ml rapid saline flush • Max 1 st dose is 6 mg (max at adult dose) • Repeat dose if needed is 0. 2 mg/kg with • 5 ml saline flush • Max 2 nd dose is 12 mg (adult dose)
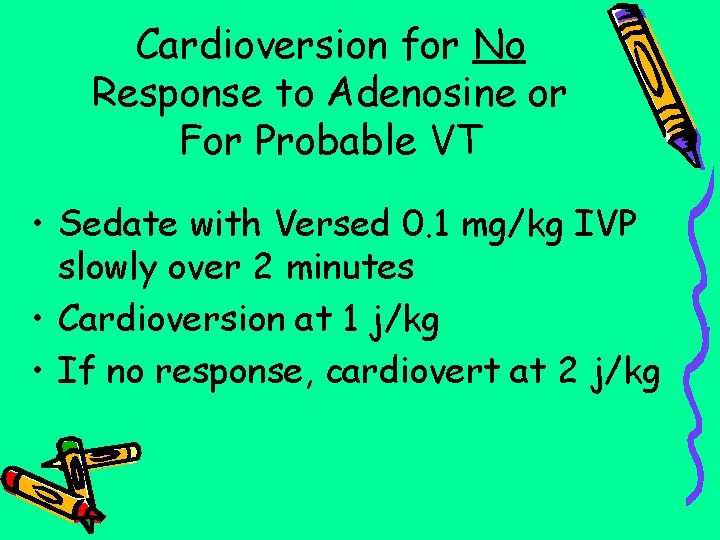
Cardioversion for No Response to Adenosine or For Probable VT • Sedate with Versed 0. 1 mg/kg IVP slowly over 2 minutes • Cardioversion at 1 j/kg • If no response, cardiovert at 2 j/kg
Why Versed? • • • Amnesic Relaxes patient Shorter acting than Valium Does NOT take away pain! Can cause respiratory depression – Have BVM reached & ready whenever Versed or Valium are given in case the patient needs ventilation support

Probable VT with Poor Perfusion • No time to allow drugs to work to slow or convert rhythm • Need to be more aggressive • Cardiovert the patient – 1 st attempt 1 j/kg – 2 nd attempt if needed 2 j/kg • If no response to cardioversion, contact Medical Control for possible • Amiodarone or Lidocaine order
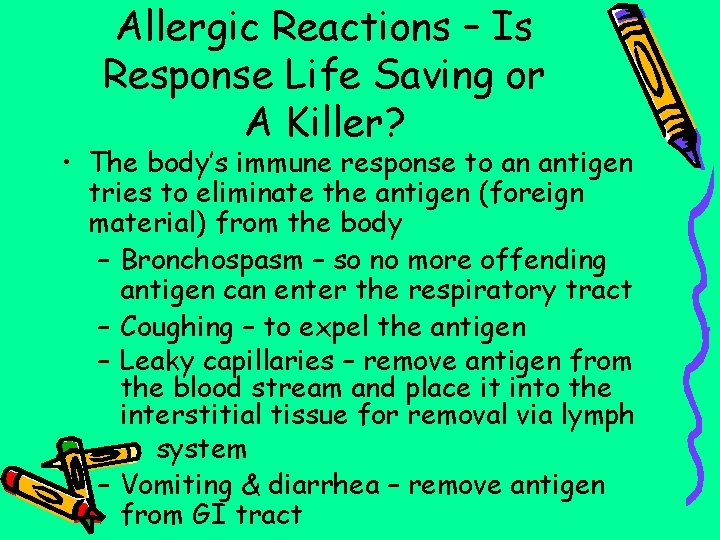
Allergic Reactions – Is Response Life Saving or A Killer? • The body’s immune response to an antigen tries to eliminate the antigen (foreign material) from the body – Bronchospasm – so no more offending antigen can enter the respiratory tract – Coughing – to expel the antigen – Leaky capillaries – remove antigen from the blood stream and place it into the interstitial tissue for removal via lymph system – Vomiting & diarrhea – remove antigen from GI tract
Antigen Exposure & Histamine Release • Increased capillary permeability – 3 rd spacing (intravascular fluid into interstitial space) • Edema • Relative hypovolemia • Peripheral vasodilation – ↓ peripheral vascular resistance (↓ B/P) • Smooth muscle constriction – Abdominal cramps, vomiting, diarrhea – Bronchoconstriction & laryngeal edema
Is it an Allergic Reaction or Anaphylaxis? • Anaphylaxis is the more severe response of the two – Usually occurs when a patient is exposed to a specific allergen, especially injected directly into the circulation • Anaphylaxis principally affects the cardiovascular, respiratory, GI systems and the skin • Faster the reaction, usually the more severe the reaction is • In anaphylaxis, the patient will be • hypotensive (ominous sign)
Why Epinephrine 1: 1000 For An Immune Response? • Stimulates certain receptors in the body (alpha & beta receptors) – Constricts blood vessels to help counter vasodilation effects of anaphylaxis (alpha affect) – Opens up airways by reversing bronchospasm of anaphylaxis (beta affect) – Max dose calculated at adult dose (0. 3 ml)!
What Does Epinephrine Do? • Primary drug used in reactions • Increases heart rate • Increases strength of cardiac contractions • Causes peripheral vasoconstriction • Can reverse bronchospasm • Can reverse capillary permeability • Effects short term
Why Benadryl For Immune Response? • Antihistamines are the 2 nd line agents to give in reactions • Antihistamines block the effects of histamine released in the body by blocking histamine receptors • Duration of action is 6 -12 hours so anticipate rebound if the patient has not filled a prescription to continue taking the antihistamine • Max dose given is at adult dosing

EMS Benadryl Dosing • Epinephrine is 1 st line drug if applicable • Stable allergic reaction no airway involvement – Benadryl 1 mg/kg slow IVP or IM – Max 25 mg (adult dose) • Stable allergic reaction with airway involvement – Benadryl 1 mg/kg slow IVP – Max 50 mg (adult dose) • Anaphylactic shock - Benadryl 1 mg/kg slow IVP - Max 50 mg (adult dose)
Practice Calculating the GCS • Remember to use the “PEDS” alternative values when the patient is non-verbal • If the patient is old enough to talk, follow the adult prompts to calculate the GCS

GCS Calculation #1 • Patient is 7 months old • Eyes are open but do not focus or follow activities • The infant has an irritable cry • The infant pulls their arms in when the IV stick is attempted

GCS Calculation #2 • Patient is 3 years-old • Eyes flutter open when the patient is yelled at • The toddler cries after the injured extremity is manipulated • The toddler pulls back when the injured extremity is manipulated
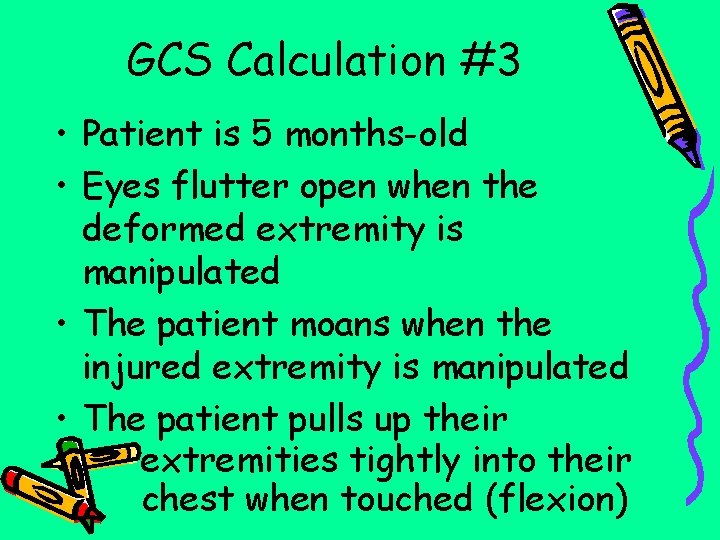
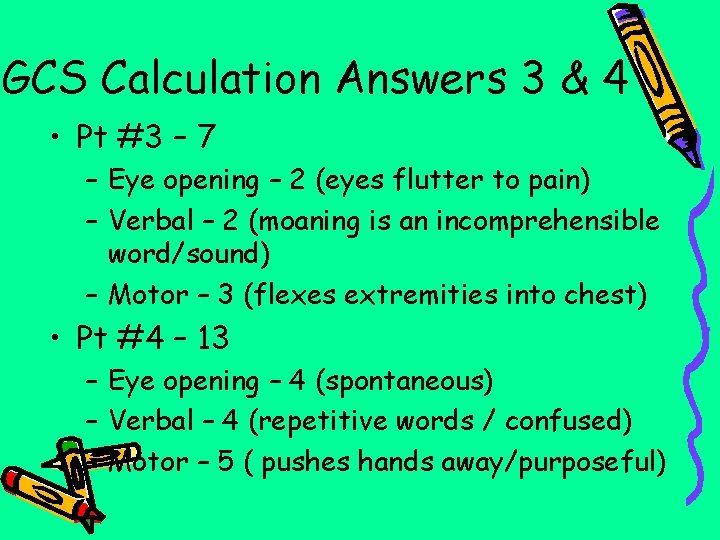
GCS Calculation #3 • Patient is 5 months-old • Eyes flutter open when the deformed extremity is manipulated • The patient moans when the injured extremity is manipulated • The patient pulls up their extremities tightly into their chest when touched (flexion)
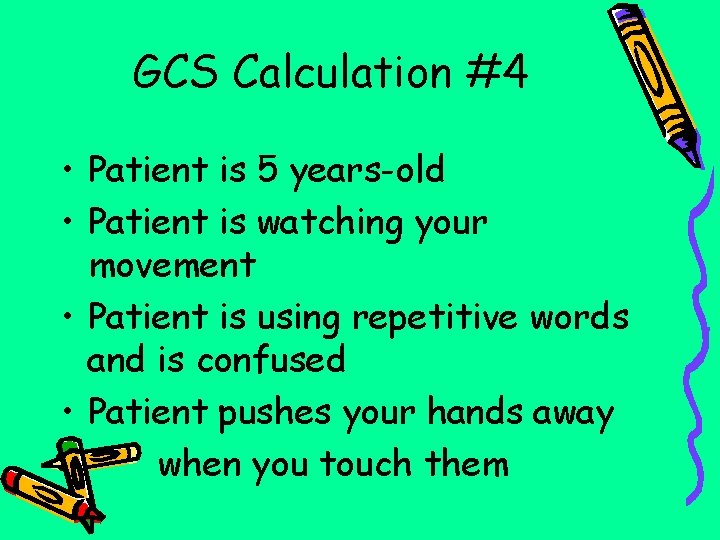
GCS Calculation #4 • Patient is 5 years-old • Patient is watching your movement • Patient is using repetitive words and is confused • Patient pushes your hands away when you touch them

GCS Calculation Answers 1 & 2 • Pt #1 – GCS 12 Eye opening – 4 (spontaneous) Verbal – 4 (irritable cry) Motor 4 – (withdraws to pain) • Pt #2 – GCS 10 Eye opening -3 (eyes open to voice) – Verbal – 3 (cries to pain) – Motor – 4 (withdraws to pain)
GCS Calculation Answers 3 & 4 • Pt #3 – 7 – Eye opening – 2 (eyes flutter to pain) – Verbal – 2 (moaning is an incomprehensible word/sound) – Motor – 3 (flexes extremities into chest) • Pt #4 – 13 – Eye opening – 4 (spontaneous) – Verbal – 4 (repetitive words / confused) – Motor – 5 ( pushes hands away/purposeful)
Scenarios • Read the following case studies • Determine your general impression based on the pediatric assessment triangle (PAT) • Determine interventions appropriate to the situation

Case Study #1 • EMS is at a local high school track meet when a 12 year-old boy collapses while running the 100 -yard dash. Initial assessment reveals the child is apneic and pulseless. CPR is started immediately • What are the next appropriate steps to take? • Can an AED be used on a 12 year-old?
Case Study #1 • AED’s can be used in patients over 1 years-old – Use the child pads for 1 – 8 year olds – If no child pads available, use adult pads – Cannot use child pads though on the adult • CPR for 12 year-old is adult standards • CPR 1 person infant & child (1 -8 years-old per AHA) is 30: 2; 2 person is 15: 2; once intubated ventilations are delivered once every 6 -8 seconds
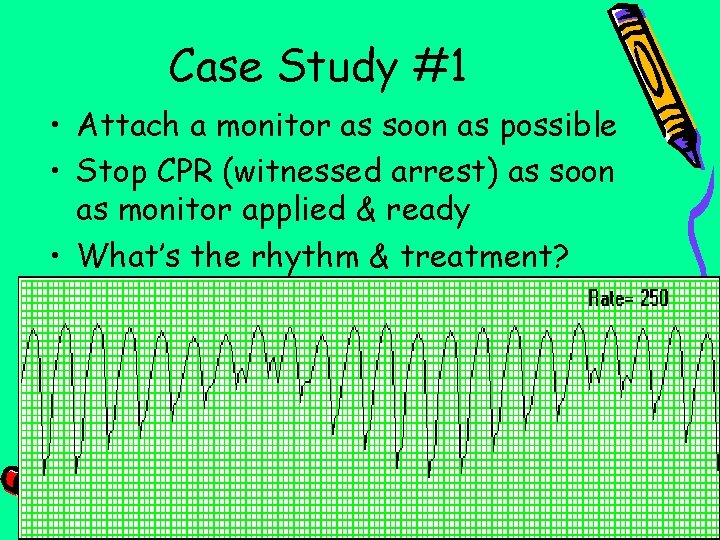
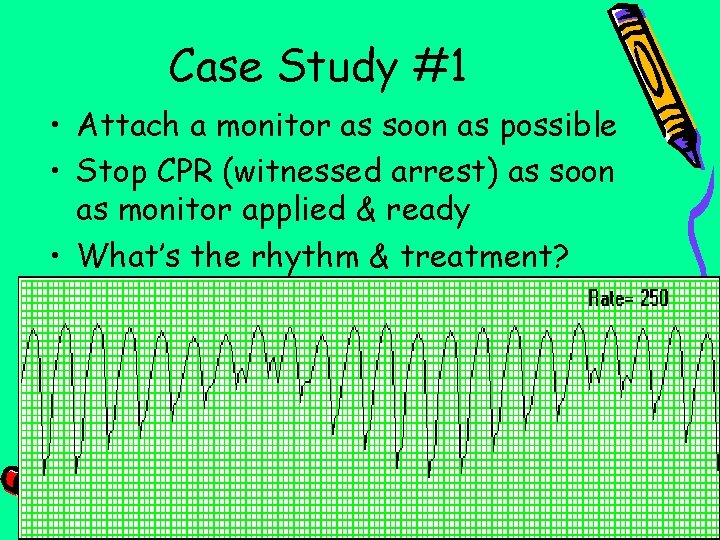
Case Study #1 • Attach a monitor as soon as possible • Stop CPR (witnessed arrest) as soon as monitor applied & ready • What’s the rhythm & treatment?
Case Study #1 • Rhythm: Torsades – Most likely this young athlete has long QT syndrome (conduction defect) that makes them prone to arrest during physical exertion • Treat like VF (follow Region x SOP for EMS) – Defibrillate 1 st at 2 j/kg (peds pt <15) – Repeat defibrillations at 4 j/kg – Epinephrine 1: 10, 000 0. 01 mg/kg IV/IO • Repeat every 3 -5 minutes • Choose one antidysrhythmic (Amiodarone or Lidocaine; one dose)

Case Study #2 • A 2 year-old at preschool fell from a sitting position and the teacher witnessed jerking of the arms and legs that lasted for 1 -2 minutes. Parent told teacher the child was not feeling well during the night. • On arrival, the child is drowsy, will open their eyes to voice but does not answer questions, moans & withdraws when touched. • VS: B/P 110/58; HR 100; RR 30; skin warm to the touch • What is your impression based on the assessment triangle? • What is the GCS?
Case Study #2 • Patient appears physiologically stable – Drowsy, no extra effort or noise for breathing, skin pink and warm – GCS 10 (3, 2, 5) (currently post-ictal) • Initial impression is febrile seizure (no history trauma, history of being ill last night, feels warms to touch) • Field treatment limited to cooling measures – Remove extra clothing, cool cloths on forehead • Reevaluate GCS watching for improvement as level of consciousness improves
Case Study #2 Is Valium Indicated Now? • No active seizure currently, so no drug • Valium stops the current seizure but does not prevent future seizures • Valium indicated if multiple seizures occur or seizure lasts longer than a few minutes • Long lasting seizure can cause hypoxia • Side effects of valium are respiratory depression
Case Study #3 • You are on the scene for an 18 month-old child who is having difficult breathing • The mother states a 2 day hx of slight fever and wheezing esp when crying • Pt suddenly woke tonight short of breath with loud noises on inhalation • Child sitting on mother’s lap, anxious, watches you and cries weakly when you approach
Case Study #3 • Color pink, has retractions with nasal flaring • HR 180; RR 42 • Strong pulses, cap refill 2 seconds • Loud, harsh breath sounds bilaterally
Case Study #3 • How sick is this child? – PAT (pediatric assessment triangle) • Evaluate appearance, work of breathing, & circulation to skin • What is your general impression? – Do you think this is an upper or lower airway problem? • • How should you care for this child in the field?
Case Study #3 • PAT: makes eye contact & cries when EMS approaches; exhibiting stridor & increased work of breathing; skin pink & warm • This child is in respiratory distress, not failure, with an upper airway problem – Stridor indicates upper airway obstruction and history of a few days of respiratory infection is consistent with croup
Case Study #3 • Management upper airway obstruction based on severity of symptoms – Position of comfort – usually best to leave child sitting upright – O 2 – best if humidified • Can humidified O 2 be given in the field? Yes!
Humidified Oxygenation in the Field • Place 6 ml normal saline into the nebulizer • Finish assembling the nebulizer • Connect tubing to the O 2 source • Turn up the liter flow to generate a flow of mist • Aim the mist near the child’s face • Helpful for croup & epiglottitis
Case Study #3 • If wheezing, EMS gives Albuterol 2. 5 mg – Used as bronchodilator – FYI: Research indicates Albuterol does not have much affect in croup • Place Albuterol into nebulizer • Place nebulizer mask over patient’s face if child too small to place lips around mouthpiece or direct mist near child’s face
Case Study #4 • 911 called to the scene for a 3 -month old who has had 3 days of cough, runny nose & low-grade fever. • Caregiver concerned because the child is working harder to breathe and having hard time feeding • Child is in caregiver’s lap • Child is sleepy, no eye contact or response to the exam

Case Study #4 • Child limp, audible wheezing, deep retractions, nasal flaring, skin mottled, diaphoretic • VS: HR 180; RR 70; Sa. O 2 on room air 74% • Breath sounds: tight with only fair movement with high-pitched inspiratory & expiratory wheezes
Case Study #4 • Is this child in respiratory distress or respiratory failure? • What is your general impression? • What do you need to do to manage this patient?
Case Study #4 • You note increased work of breathing, abnormal appearance, and poor circulation • This patient is in respiratory failure • With the wheezing, the problem is most likely a lower airway obstruction – Most likely bronchiolitis (inflammation of the bronchioles often caused by RSV – a viral infection)
Case Study #4 • Rapid and urgent transport • This patient most likely does not have an easily reversible respiratory problem and is likely to deteriorate further • Enroute EMS to administer a bronchodilator (Albuterol) via nebulizer via mask (won’t be able to put mouth around mouthpiece)
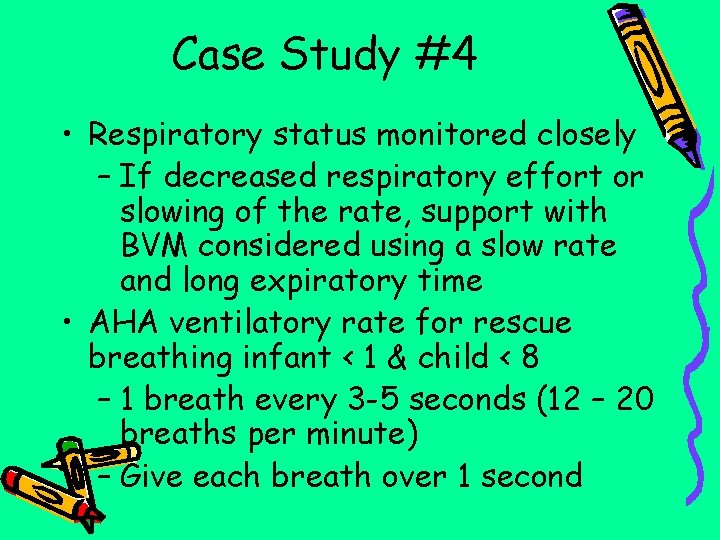
Case Study #4 • Respiratory status monitored closely – If decreased respiratory effort or slowing of the rate, support with BVM considered using a slow rate and long expiratory time • AHA ventilatory rate for rescue breathing infant < 1 & child < 8 – 1 breath every 3 -5 seconds (12 – 20 breaths per minute) – Give each breath over 1 second
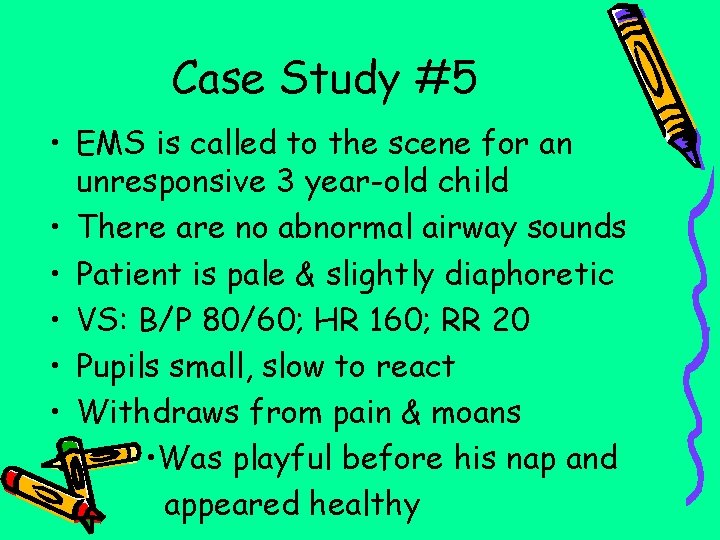
Case Study #5 • EMS is called to the scene for an unresponsive 3 year-old child • There are no abnormal airway sounds • Patient is pale & slightly diaphoretic • VS: B/P 80/60; HR 160; RR 20 • Pupils small, slow to react • Withdraws from pain & moans • Was playful before his nap and appeared healthy
Case Study #5 • What is your general assessment? • What is the GCS? • What other assessments need to be done? • What interventions are needed?
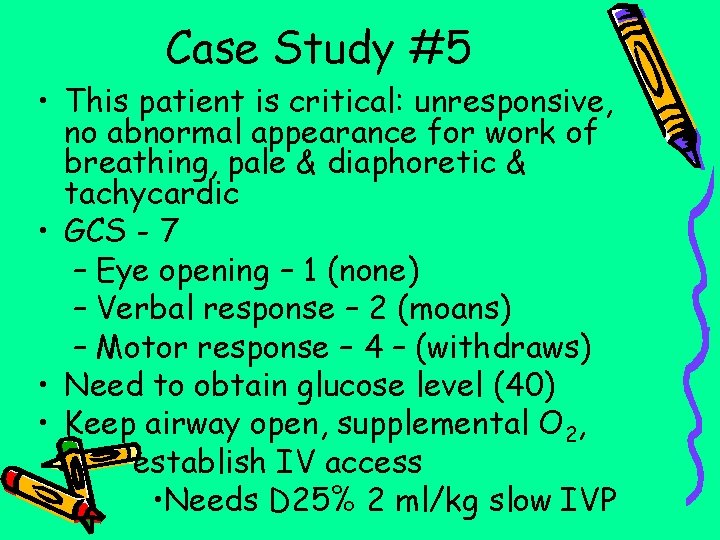
Case Study #5 • This patient is critical: unresponsive, no abnormal appearance for work of breathing, pale & diaphoretic & tachycardic • GCS - 7 – Eye opening – 1 (none) – Verbal response – 2 (moans) – Motor response – 4 – (withdraws) • Need to obtain glucose level (40) • Keep airway open, supplemental O 2, establish IV access • Needs D 25% 2 ml/kg slow IVP
Case Study #5 • Calculating & administrating Dextrose – D 25% ages 1 – 15 is 2 ml/kg – This 3 year-old weighs 29 pounds – How much D 25% do you administer? – Where are your resources to – find the information?
Case Study #5 • Check the back of the SOP’s • Check the Broselow tape • Divide pounds by 2. 2 to determine kg – 29 2. 2 = 13 kg • Multiply kg by the formula (2 ml/kg) – 13 kg x 2 ml/kg = 26 ml D 25% • D 25% is packaged in 10 ml prefilled syringe • Administer IV dose slowly to • minimize vein irritation from the med
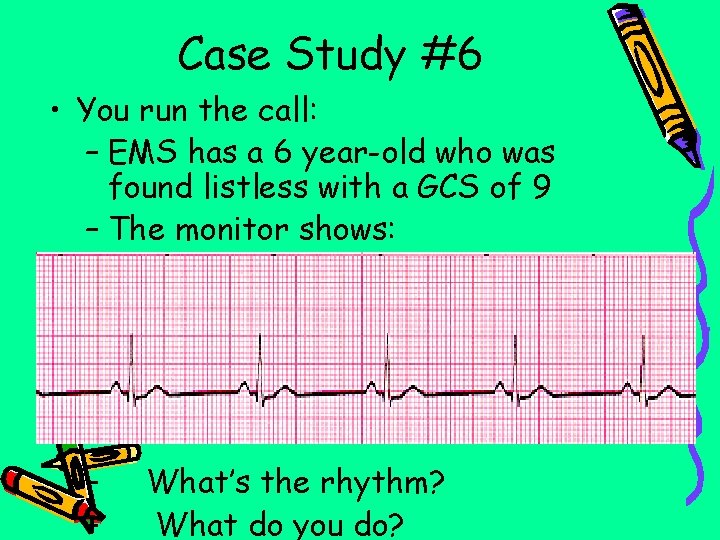
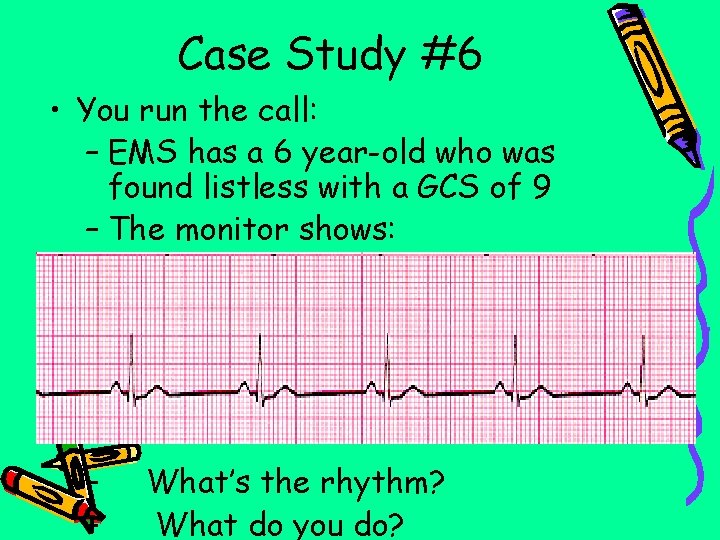
Case Study #6 • You run the call: – EMS has a 6 year-old who was found listless with a GCS of 9 – The monitor shows: – – What’s the rhythm? What do you do?
Case Study #7 • Pediatric bradycardia is a hypoxia problem until proven otherwise • CPR started with attention to ventilation • IV or IO access established • What drug therapy is necessary for the pediatric symptomatic bradycardia?
Case Study #7 • EZ IO landmarks – 2 fingerbreadths down from patella over tibial tuberosity – 1 fingerbreadth toward medial surface away from tibial tuberosity • Peds bradycardia treatment – Epinephrine 1: 10, 000 0. 01 mg/kg IV/IO – Repeated every 3 -5 minutes – Persistent , Medical Control would need to order Atropine
Bibliography • Aehlert, B. PALS Study Guide. Elsevier. 2007. • American Academy of Pediatrics. Pediatric Education for Prehospital Professionals. 2 nd edition. Jones & Bartlett. 2006. • Rahm, S. Pediatric Case Studies for the Paramedic. AAOS. 2006. • Region X SOP’s. Amended 1/08. • www. peds. umn. edu/. . . /teaching/lung/ stridor. jpg
 Encountering jesus in the new testament
Encountering jesus in the new testament Encountering jesus in the new testament
Encountering jesus in the new testament Encountering jesus in the new testament
Encountering jesus in the new testament Encountering the mongols comparing three cases
Encountering the mongols comparing three cases Information encountering
Information encountering Joan condell
Joan condell Gbmc medical records
Gbmc medical records Torrance memorial map
Torrance memorial map Cartersville medical center medical records
Cartersville medical center medical records Patient 2 patient
Patient 2 patient Patient centered medical home conference
Patient centered medical home conference Patient centered medical home
Patient centered medical home Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Heaton moor medical centre doctors
Heaton moor medical centre doctors Chafford hundred medical centre email address
Chafford hundred medical centre email address Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worm breton
Tư thế worm breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V. c c
V. c c Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Các số nguyên tố
Các số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Ptal california medical board
Ptal california medical board Difference between medical report and medical certificate
Difference between medical report and medical certificate Wyndham hotel medical center
Wyndham hotel medical center Umass neurology residency
Umass neurology residency Makati medical center charity program
Makati medical center charity program Nipt test kuwait
Nipt test kuwait Jacobi hospital building 6
Jacobi hospital building 6 New innov nyu
New innov nyu Berkshire medical center program
Berkshire medical center program Valor program pharmacy
Valor program pharmacy Vanderbilt neurology residents
Vanderbilt neurology residents Empp university medical center
Empp university medical center Duke medical library
Duke medical library Ospital ng maynila directory
Ospital ng maynila directory Chinle indian health service
Chinle indian health service Slowenien university medical center
Slowenien university medical center Va hospital fairbanks alaska
Va hospital fairbanks alaska Ku medical center histology slides
Ku medical center histology slides Outpatient medical center tallulah la
Outpatient medical center tallulah la Columbia university medical center
Columbia university medical center Mercy regional medical center lorain
Mercy regional medical center lorain Dr suhail allaqaband
Dr suhail allaqaband Columbia university medical center
Columbia university medical center Suny downstate medical center
Suny downstate medical center Sinai samaritan
Sinai samaritan Global east asia medical center
Global east asia medical center Arden medical centre
Arden medical centre Tufts medical center anesthesiology residency
Tufts medical center anesthesiology residency Islamic medical center kuwait
Islamic medical center kuwait Joint special operations medical training center
Joint special operations medical training center Dr steven shapiro
Dr steven shapiro Meritus health family medicine residency
Meritus health family medicine residency Iakentro thessaloniki
Iakentro thessaloniki Unm sandoval regional medical center billing
Unm sandoval regional medical center billing Central washington medical center
Central washington medical center Wi dhs ems
Wi dhs ems Deferred payment plan uc merced
Deferred payment plan uc merced Ems felvételre kijelölt posták
Ems felvételre kijelölt posták Verdant thermostat occupancy sensor
Verdant thermostat occupancy sensor Ssv ems protocols
Ssv ems protocols Ems equipment repair
Ems equipment repair Southwest virginia ems council
Southwest virginia ems council Ems latlit
Ems latlit Fire report writing
Fire report writing Nbitrex
Nbitrex Nevada ems soap
Nevada ems soap Iso 9001 environmental management system
Iso 9001 environmental management system Eduphoria login emsisd
Eduphoria login emsisd Pww ems law
Pww ems law Ems98
Ems98 For adult
For adult Factors of production ems grade 8
Factors of production ems grade 8 Hotmail
Hotmail Dhec ems
Dhec ems Ems soap narrative examples
Ems soap narrative examples Ems lifting devices
Ems lifting devices Chapter 1 ems systems
Chapter 1 ems systems National ems education standards
National ems education standards Bcts ems
Bcts ems Ems system design
Ems system design Gems diamond ems
Gems diamond ems Grade 9 ems assignments term 3 business plan
Grade 9 ems assignments term 3 business plan Central shenandoah ems
Central shenandoah ems Ems cortal
Ems cortal