EMS PATIENT REFUSALS Amy Gutman MD EMS Medical


- Slides: 27
EMS PATIENT REFUSALS Amy Gutman MD EMS Medical Director prehospitalmd@gmail. com
OVERVIEW Informed Consent Refusal of Care Transport Decisions Patient Restraint Non-Transport of Patients
INFORMED CONSENT Protects medical decision making autonomy Allows for legal information exchange between patient & provider If cannot make an informed choice, cannot refuse transport
INFORMED CONSENT Patient permission legally required prior to any evaluation Expressed Consent § Must be obtained from all physically or mentally able adult patients or emancipated minors § Expressed consent must be “informed” consent § Patients must understand risk: benefit ratio of refusing care vs consenting to care Implied Consent § Unconscious patient, minor or not competent § Consent “assumed” based upon idea that a rational person would consent to treatment if they were conscious
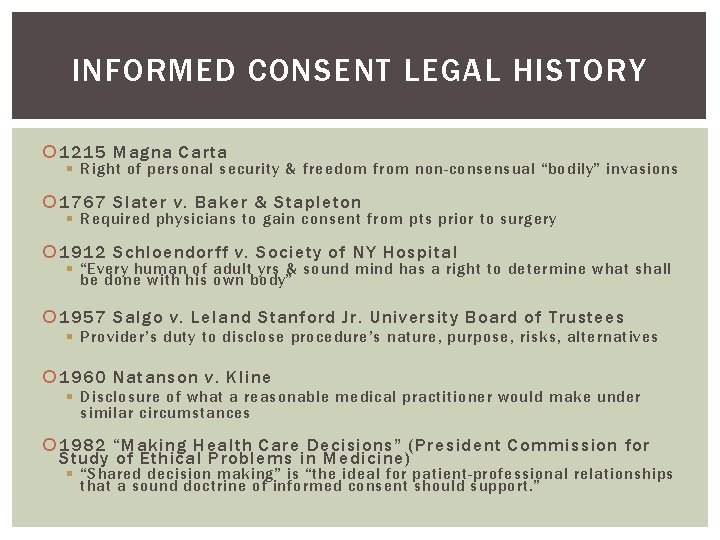
INFORMED CONSENT LEGAL HISTORY 1215 Magna Carta § Right of personal security & freedom from non-consensual “bodily” invasions 1767 Slater v. Baker & Stapleton § Required physicians to gain consent from pts prior to surgery 1912 Schloendorff v. Society of NY Hospital § “Every human of adult yrs & sound mind has a right to determine what shall be done with his own body” 1957 Salgo v. Leland Stanford Jr. University Board of Trustees § Provider’s duty to disclose procedure’s nature, purpose, risks, alternatives 1960 Natanson v. Kline § Disclosure of what a reasonable medical practitioner would make under similar circumstances 1982 “Making Health Care Decisions” (President Commission for Study of Ethical Problems in Medicine) § “Shared decision making” is “the ideal for patient-professional relationships that a sound doctrine of informed consent should support. ”
CHILDREN & INCOMPETENT ADULTS Cannot provide consent or refuse medical care / transportation Legal authority to give consent: § Parent, Guardian, Power of Attorney, Next of Kin If life-threatening illness or injury when parent or guardian not present, care may be given based on implied consent If you believe parent / guardian denying care to a minor or incompetent adult, may involve police as well as medical control § i. e. suspected abuse

EMANCIPATED MINOR May give informed consent Person <18 years old who is: Married Pregnant or a parent A member of the armed forced Financially independent & living away from home May still be considered a “pediatric patient” even if emancipated

PATIENT REFUSAL There are many reasons for patient refusal, including denial, fear, failing to understand the seriousness of the situation, intoxication, etc. If you err on the side of providing patient care, your agency and medical director can justify your actions Criteria For Informed Consent & Refusal: § Patient given complete & accurate information about risks for refusal & benefit of treatment § Patient able to understand & communicate these risks & benefits § Patient able to make a decision consistent with their beliefs & life goals (cont. )
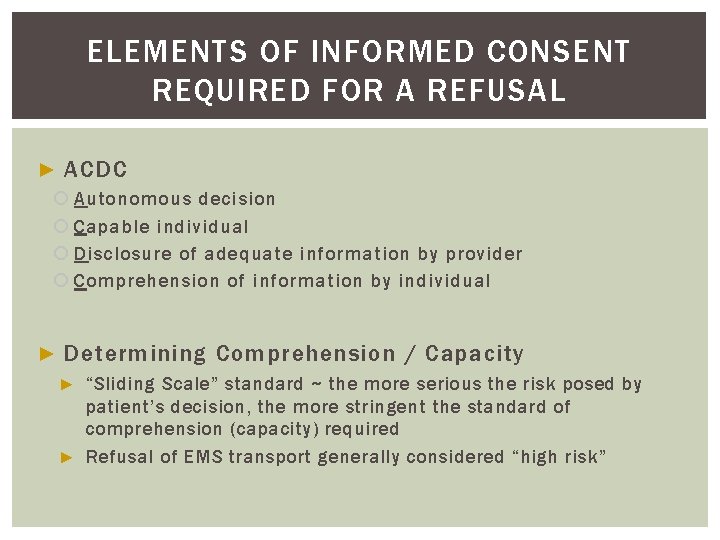
ELEMENTS OF INFORMED CONSENT REQUIRED FOR A REFUSAL ► ACDC Autonomous decision Capable individual Disclosure of adequate information by provider Comprehension of information by individual ► Determining Comprehension / Capacity “Sliding Scale” standard ~ the more serious the risk posed by patient’s decision, the more stringent the standard of comprehension (capacity) required ► Refusal of EMS transport generally considered “high risk” ►
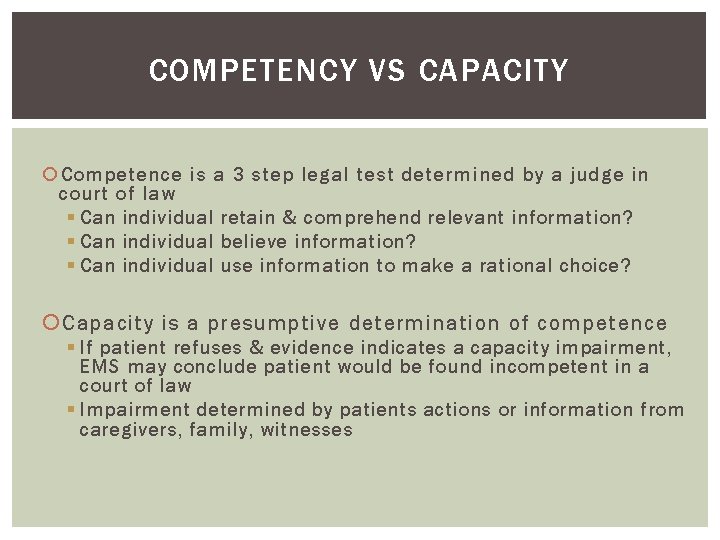
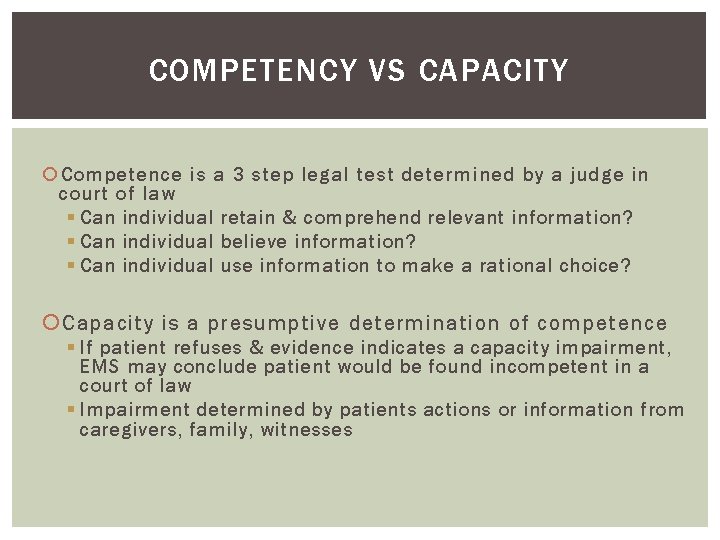
COMPETENCY VS CAPACITY Competence is a 3 step legal test determined by a judge in court of law § Can individual retain & comprehend relevant information? § Can individual believe information? § Can individual use information to make a rational choice? Capacity is a presumptive determination of competence § If patient refuses & evidence indicates a capacity impairment, EMS may conclude patient would be found incompetent in a court of law § Impairment determined by patients actions or information from caregivers, family, witnesses
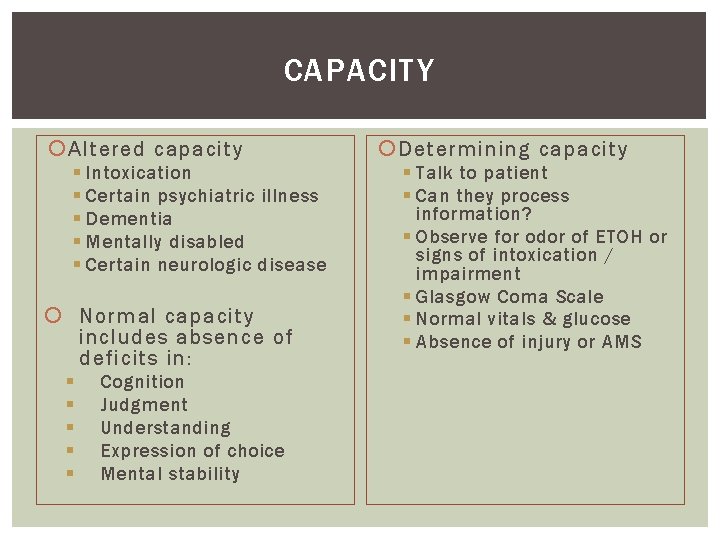
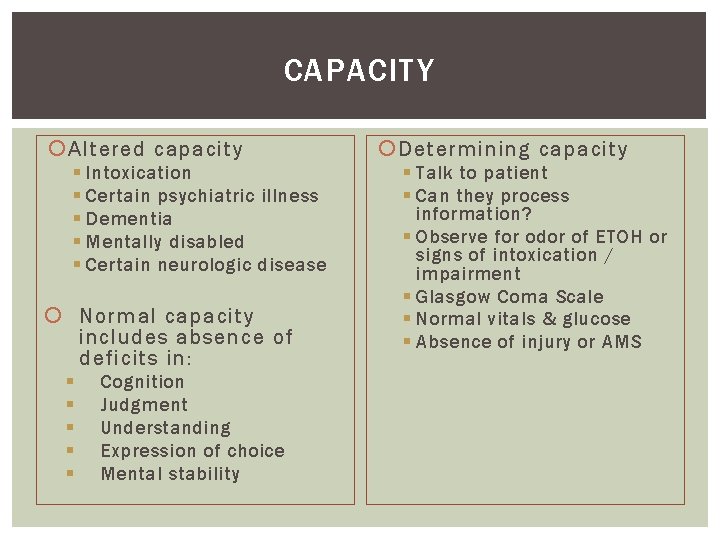
CAPACITY Altered capacity § Intoxication § Certain psychiatric illness § Dementia § Mentally disabled § Certain neurologic disease Normal capacity includes absence of deficits in: § § § Cognition Judgment Understanding Expression of choice Mental stability Determining capacity § Talk to patient § Can they process information? § Observe for odor of ETOH or signs of intoxication / impairment § Glasgow Coma Scale § Normal vitals & glucose § Absence of injury or AMS
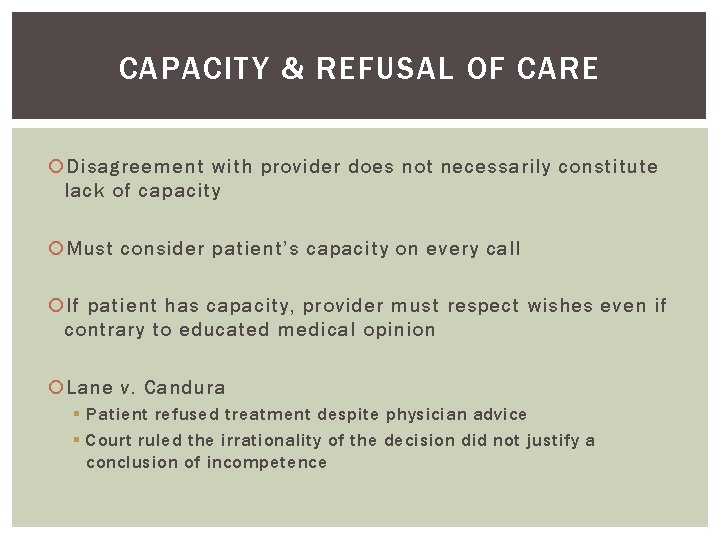
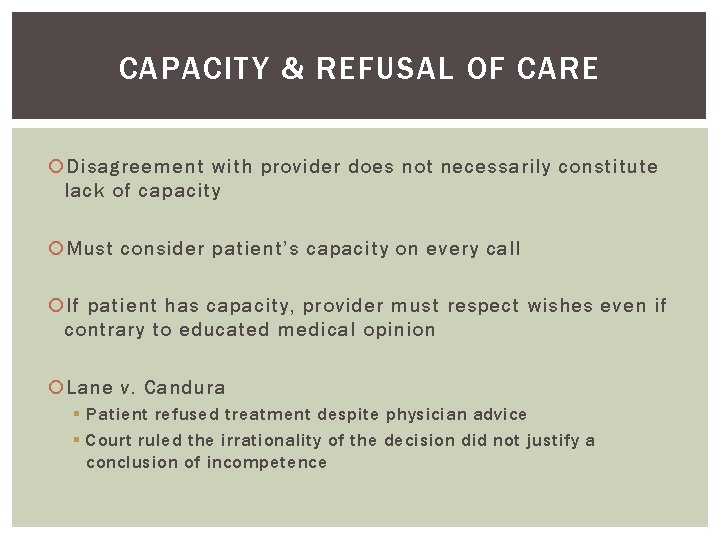
CAPACITY & REFUSAL OF CARE Disagreement with provider does not necessarily constitute lack of capacity Must consider patient’s capacity on every call If patient has capacity, provider must respect wishes even if contrary to educated medical opinion Lane v. Candura § Patient refused treatment despite physician advice § Court ruled the irrationality of the decision did not justify a conclusion of incompetence
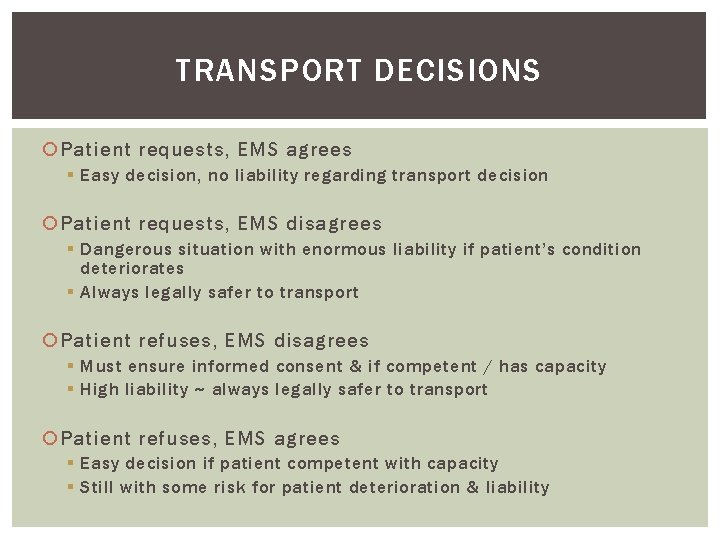
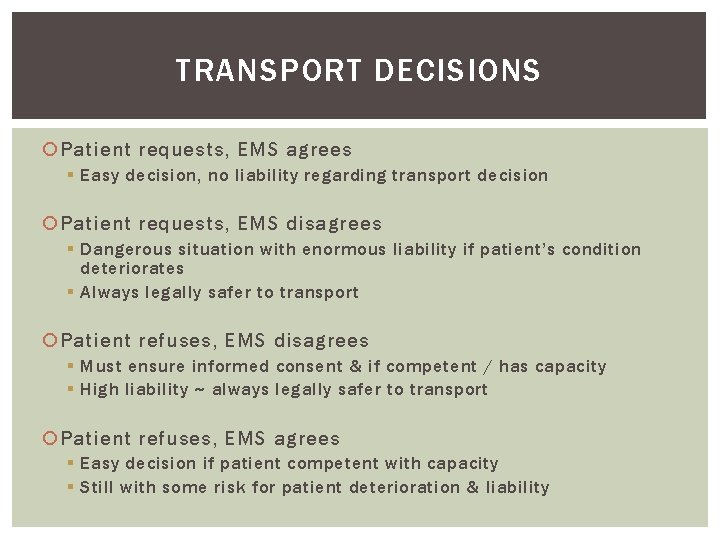
TRANSPORT DECISIONS Patient requests, EMS agrees § Easy decision, no liability regarding transport decision Patient requests, EMS disagrees § Dangerous situation with enormous liability if patient’s condition deteriorates § Always legally safer to transport Patient refuses, EMS disagrees § Must ensure informed consent & if competent / has capacity § High liability ~ always legally safer to transport Patient refuses, EMS agrees § Easy decision if patient competent with capacity § Still with some risk for patient deterioration & liability
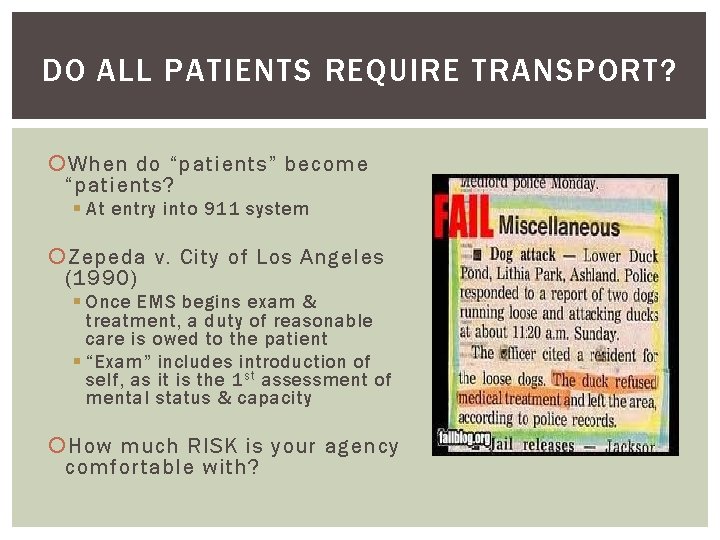
DO ALL PATIENTS REQUIRE TRANSPORT? When do “patients” become “patients? § At entry into 911 system Zepeda v. City of Los Angeles (1990) § Once EMS begins exam & treatment, a duty of reasonable care is owed to the patient § “Exam” includes introduction of self, as it is the 1 st assessment of mental status & capacity How much RISK is your agency comfortable with?
LAWSUITS & MALPRACTICE Negligence includes medical malpractice To prove negligence the plaintiff (patient) must prove that the defendant (provider) had a duty to the patient, breached that duty by not observing the required standard of care, & the failure of the defendant to comply with the standard of care was the cause of damage or injury to the patient If the plaintiff (patient) received no injury, negligence cannot be proved. EMS personnel have a duty to act, that is a duty to evaluate all patients requesting treatment because they present themselves as providing that service Protect yourself…if you don’t have personal malpractice YOU SHOULD!!!!
PATIENT RESTRAINT False Imprisonment § Restraint without proper justification or authority § Intentional & unjustifiable detention of a person without consent Assault § Unlawfully placing a person in apprehension of immediate body harm without consent Battery § Unlawfully touching an individual without consent Abandonment § Premature termination of provider: -patient relationship or failure to follow steps to ensure definitive care Reasonable Force § Dependent on force required to ensure patient does not cause injury to himself or others § Excessive force is a high liability area
ASSAULT & BATTERY If patient competent & refuses assessment, treatment or transport, you must respect their wishes Transporting competent patient against their will is false imprisonment § Unlawfully touching competent patient without their consent is battery § Treating a competent patient without their consent is battery A form of assault is in information released to the public in written or spoken format construed to be damaging to that person’s character, reputation or standing within the community § Defamation of character is “assault” § The spoken form of defamation is slander, the written form is “libel” § False information found to be slanderous or libelous is highly litigious; rarely do courts rule in the offending person’s behalf § Remember this when vocalizing your “opinions” about patients or peers on a chart or in correspondence (i. e. Facebook) especially if based upon rumor & not fact
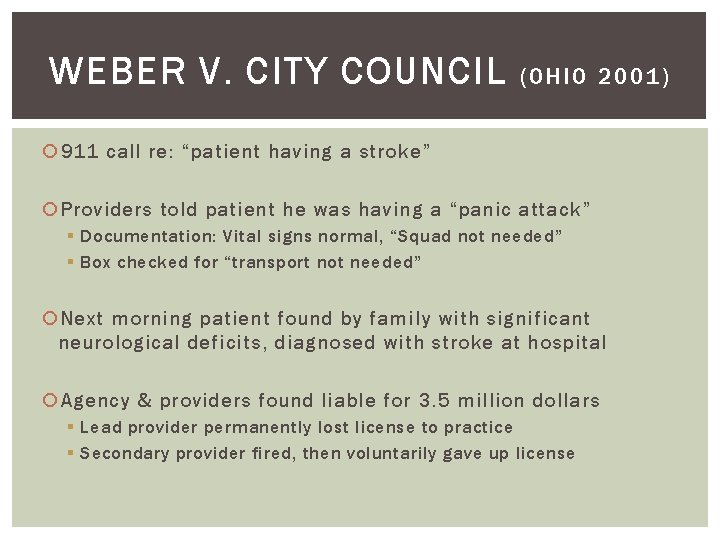
WEBER V. CITY COUNCIL (OHIO 2001) 911 call re: “patient having a stroke” Providers told patient he was having a “panic attack” § Documentation: Vital signs normal, “Squad not needed” § Box checked for “transport not needed” Next morning patient found by family with significant neurological deficits, diagnosed with stroke at hospital Agency & providers found liable for 3. 5 million dollars § Lead provider permanently lost license to practice § Secondary provider fired, then voluntarily gave up license
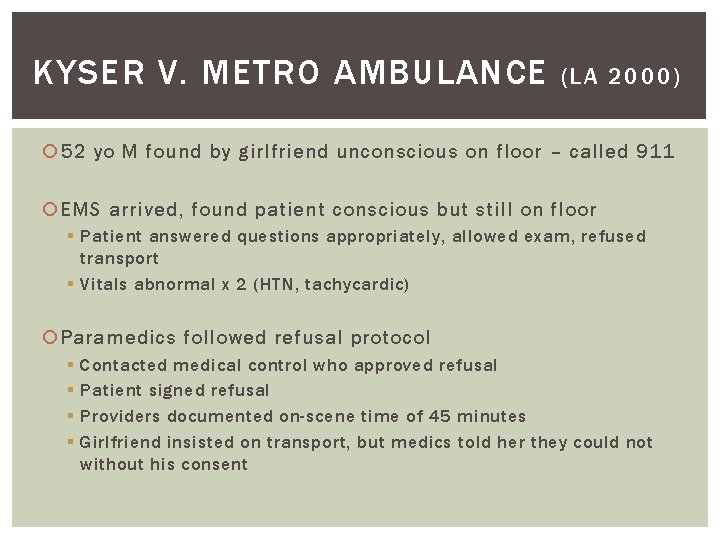
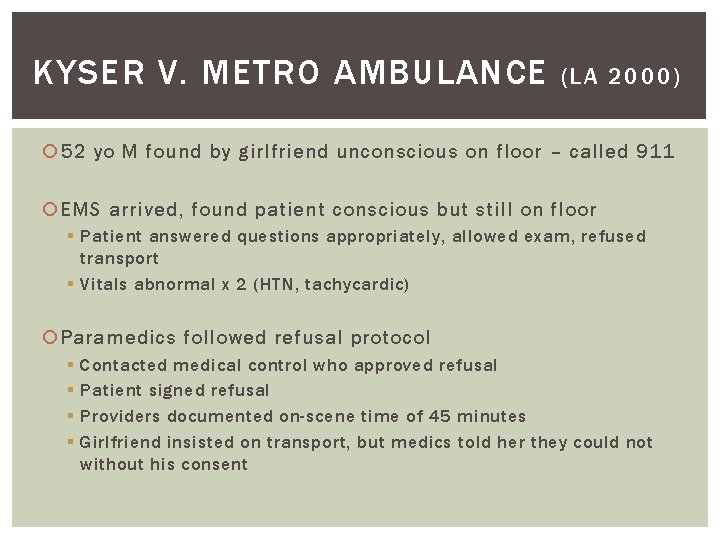
KYSER V. METRO AMBULANCE (LA 2000) 52 yo M found by girlfriend unconscious on floor – called 911 EMS arrived, found patient conscious but still on floor § Patient answered questions appropriately, allowed exam, refused transport § Vitals abnormal x 2 (HTN, tachycardic) Paramedics followed refusal protocol § § Contacted medical control who approved refusal Patient signed refusal Providers documented on-scene time of 45 minutes Girlfriend insisted on transport, but medics told her they could not without his consent
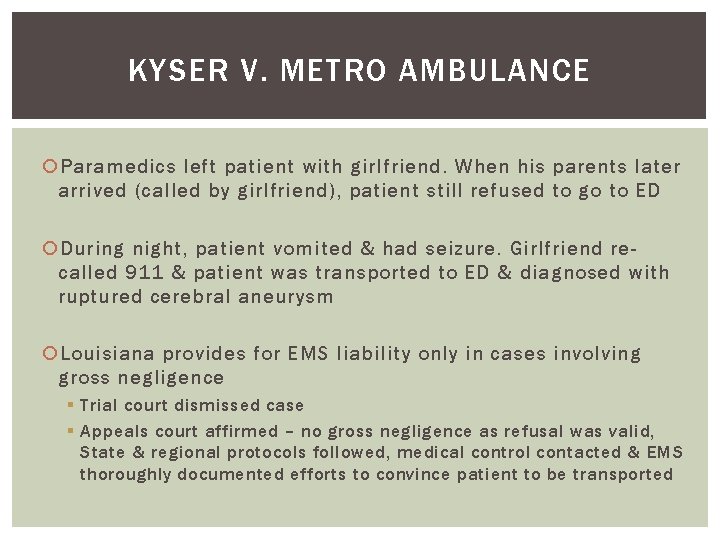
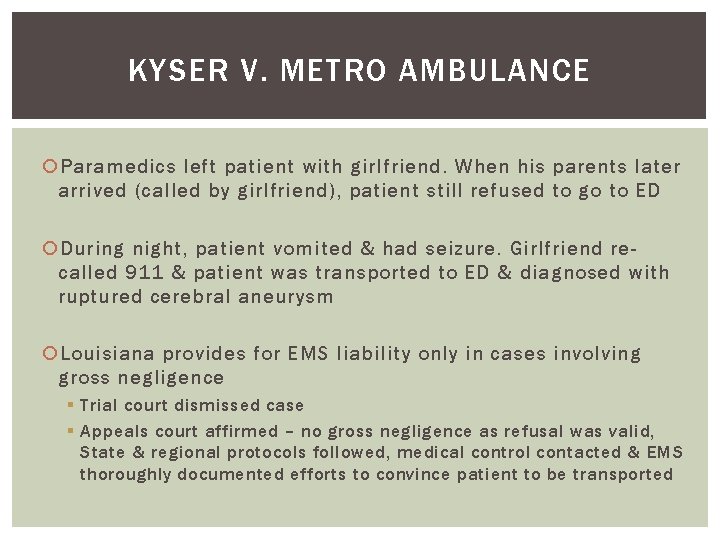
KYSER V. METRO AMBULANCE Paramedics left patient with girlfriend. When his parents later arrived (called by girlfriend), patient still refused to go to ED During night, patient vomited & had seizure. Girlfriend recalled 911 & patient was transported to ED & diagnosed with ruptured cerebral aneurysm Louisiana provides for EMS liability only in cases involving gross negligence § Trial court dismissed case § Appeals court affirmed – no gross negligence as refusal was valid, State & regional protocols followed, medical control contacted & EMS thoroughly documented efforts to convince patient to be transported
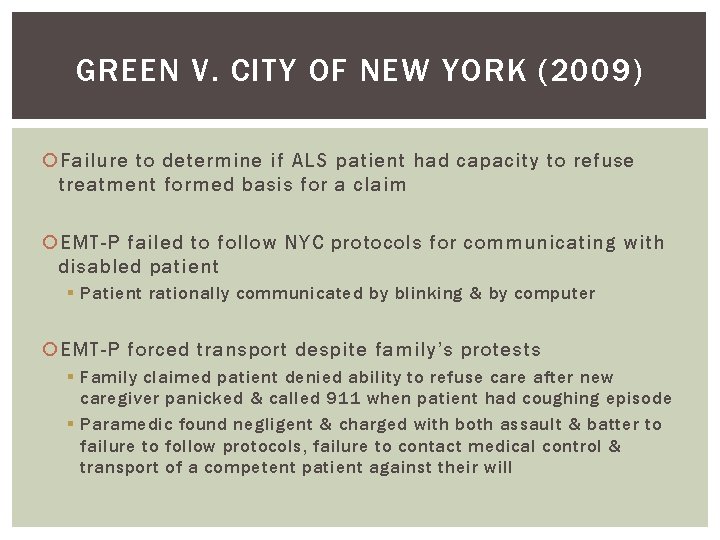
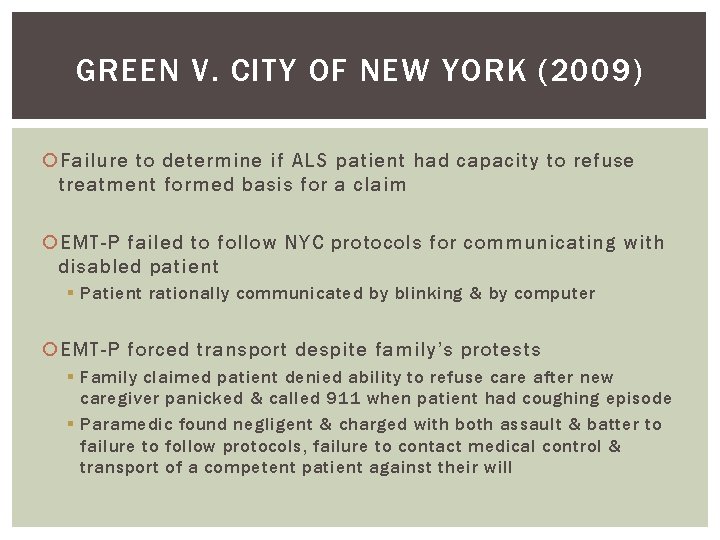
GREEN V. CITY OF NEW YORK (2009) Failure to determine if ALS patient had capacity to refuse treatment formed basis for a claim EMT-P failed to follow NYC protocols for communicating with disabled patient § Patient rationally communicated by blinking & by computer EMT-P forced transport despite family’s protests § Family claimed patient denied ability to refuse care after new caregiver panicked & called 911 when patient had coughing episode § Paramedic found negligent & charged with both assault & batter to failure to follow protocols, failure to contact medical control & transport of a competent patient against their will
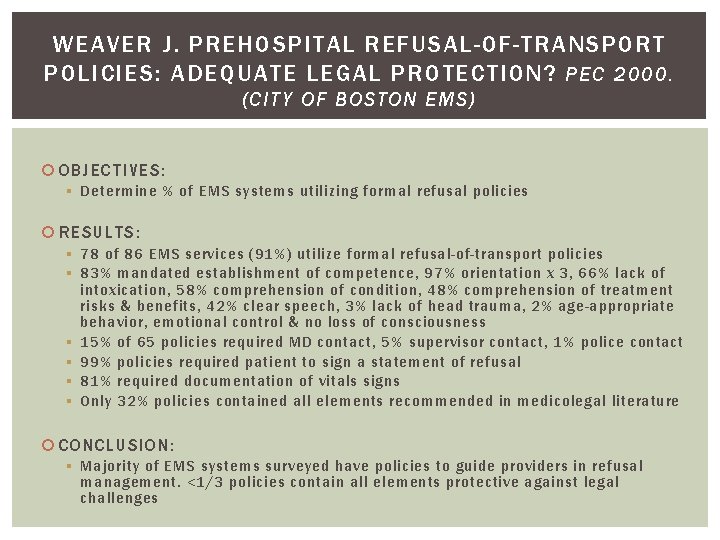
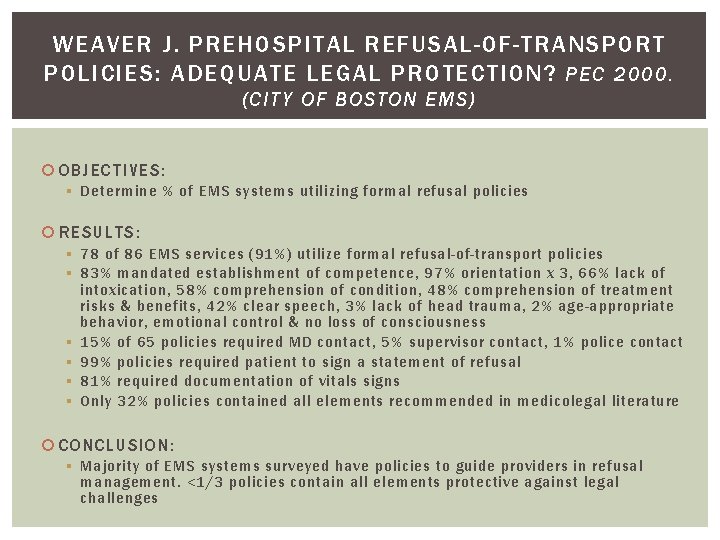
WEAVER J. PREHOSPITAL REFUSAL-OF-TRANSPORT POLICIES: ADEQUATE LEGAL PROTECTION? PEC 2000. (CITY OF BOSTON EMS) OBJECTIVES: § Determine % of EMS systems utilizing formal refusal policies RESULTS: § 78 of 86 EMS services (91%) utilize formal refusal-of-transport policies § 83% mandated establishment of competence, 97% orientation x 3, 66% lack of intoxication, 58% comprehension of condition, 48% comprehension of treatment risks & benefits, 42% clear speech, 3% lack of head trauma, 2% age-appropriate behavior, emotional control & no loss of consciousness § 15% of 65 policies required MD contact, 5% supervisor contact, 1% police contact § 99% policies required patient to sign a statement of refusal § 81% required documentation of vitals signs § Only 32% policies contained all elements recommended in medicolegal literature CONCLUSION: § Majority of EMS systems surveyed have policies to guide providers in refusal management. <1/3 policies contain all elements protective against legal challenges
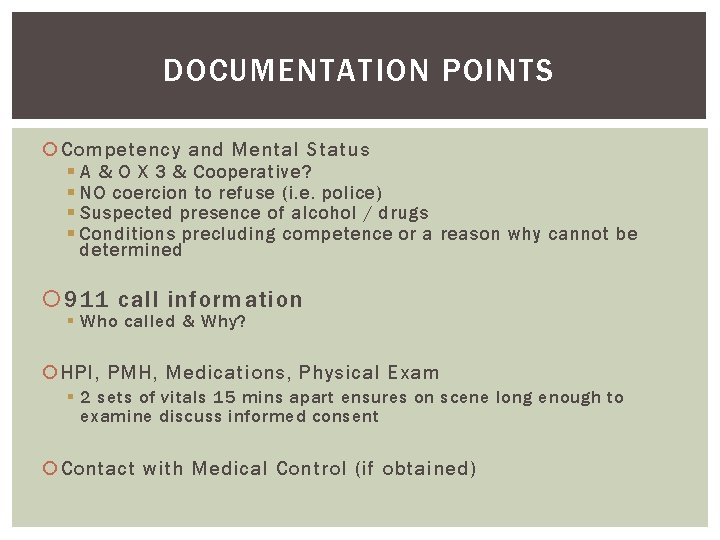
DOCUMENTATION POINTS Competency and Mental Status § A & O X 3 & Cooperative? § NO coercion to refuse (i. e. police) § Suspected presence of alcohol / drugs § Conditions precluding competence or a reason why cannot be determined 911 call information § Who called & Why? HPI, PMH, Medications, Physical Exam § 2 sets of vitals 15 mins apart ensures on scene long enough to examine discuss informed consent Contact with Medical Control (if obtained)
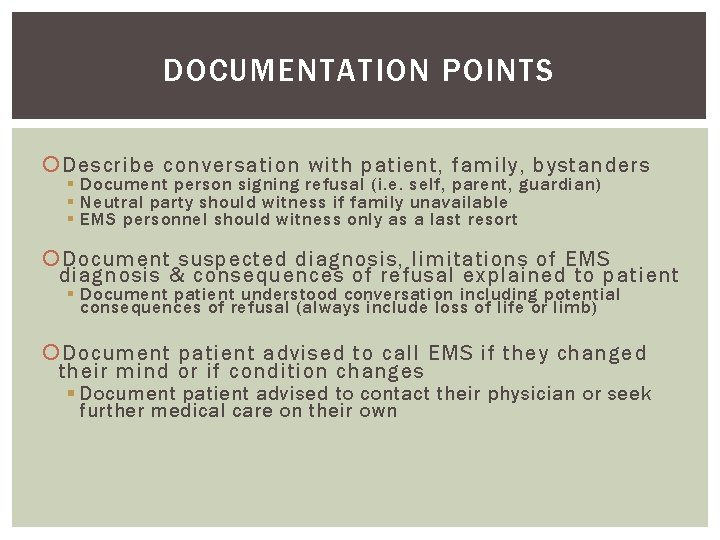
DOCUMENTATION POINTS Describe conversation with patient, family, bystanders § Document person signing refusal (i. e. self, parent, guardian) § Neutral party should witness if family unavailable § EMS personnel should witness only as a last resort Document suspected diagnosis, limitations of EMS diagnosis & consequences of refusal explained to patient § Document patient understood conversation including potential consequences of refusal (always include loss of life or limb) Document patient advised to call EMS if they changed their mind or if condition changes § Document patient advised to contact their physician or seek further medical care on their own
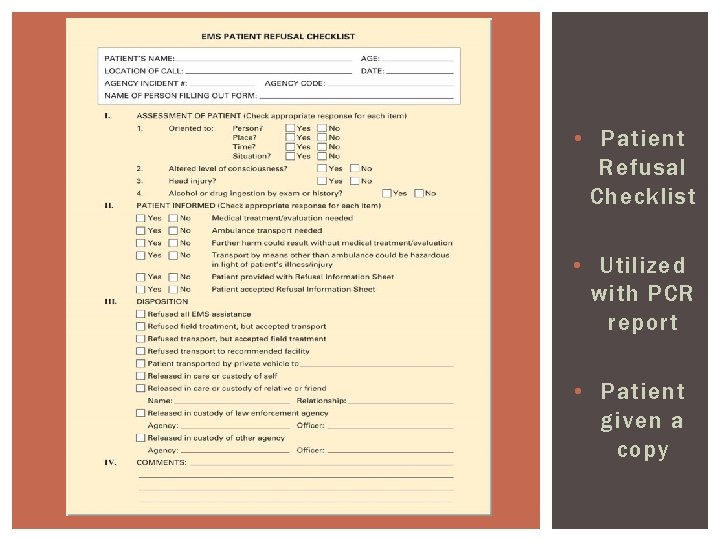
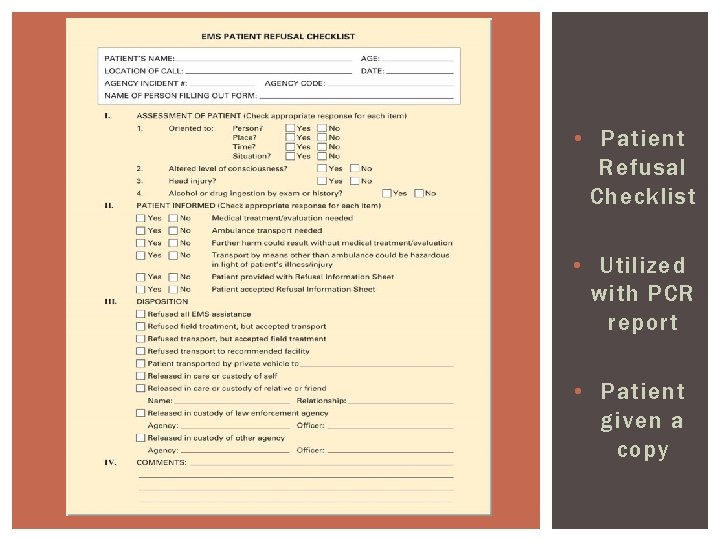
• Patient Refusal Checklist • Utilized with PCR report • Patient given a copy
REFERENCES Caroline’s Emergency Care in the Street. Jones & Bartlett. 2012 Limmer et al. Emergency Care 11 t h ED. Brady. 2009. Page, Wolfberg & White Website (www. pwwemslaw. com) www. NAEMT. org www. NAEMSE. org www. iaff. org
SUMMARY PREHOSPITALMD@GMAIL. COM Patient refusals among the highest liability cases & as such require the most through documentation Generally the only way the CQI officer or Medical Director knows about these cases is if patient ends up in the ED with a bad outcome § “Hiding” calls a great way to lose your license § No documentation…no defense in court Understand concepts of informed consent Competent, adult patients have the right to refuse care even if you disagree § Make sure you document thoroughly including involvement of the medical director