Empowering SAS in Developing Service Pathways BILIARY SEPSIS
Empowering SAS in Developing Service Pathways BILIARY SEPSIS PATHWAY Dr Ahmed Shalaby SAS Tutor Wrightington Wigan & Leigh NHS F Trust ST 05_Mar 12 your hospitals, your health, our priority
Case Study • Mrs RH was 72 y/o pensioner who in the summer of 2015 experienced worsening RUQ pain and vomiting while attending to her garden. Her husband noticed her to be jaundiced. She soon developed fever and he took her to RAEI on a Thursday morning. She was diagnosed with biliary sepsis due to stones blocking her liver tubes and was told that her conditions needed an urgent camera procedure that extract them. your hospitals, your health, our priority
Case Study • On Friday morning there was a list, but no slots available. On the endoscopy planner, there were no lists dedicated for this procedure over the weekend, nor Monday, nor Tuesday. She was scheduled for Wednesday, but the list on that day was cancelled due to technical problems. On Thursday the consultant was on annual leave. An OP case had to be cancelled on the following Friday to accommodate her. • This was not an isolated case! your hospitals, your health, our priority
Case Study • What are the implications 1. Prolonged hospital admission 2. Increased risk of hospital acquired infections and other complications 3. Pt & family waiting in anxiety and pain 4. Another patient was cancelled and delayed 5. A complaint! your hospitals, your health, our priority
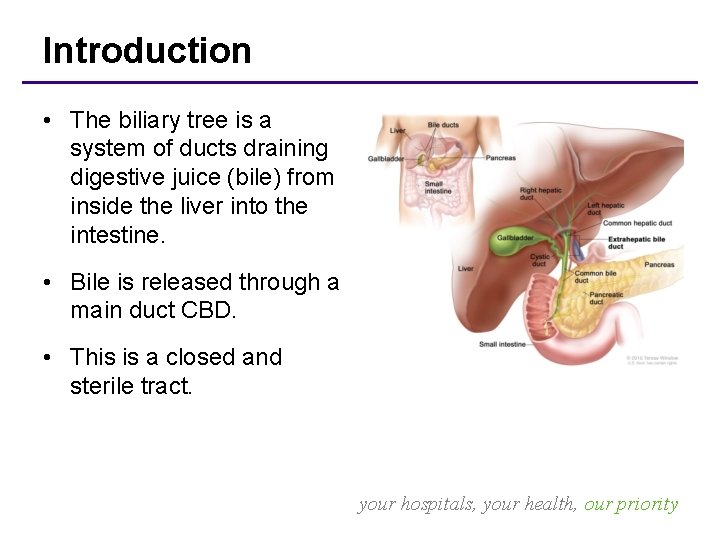
Introduction • The biliary tree is a system of ducts draining digestive juice (bile) from inside the liver into the intestine. • Bile is released through a main duct CBD. • This is a closed and sterile tract. your hospitals, your health, our priority
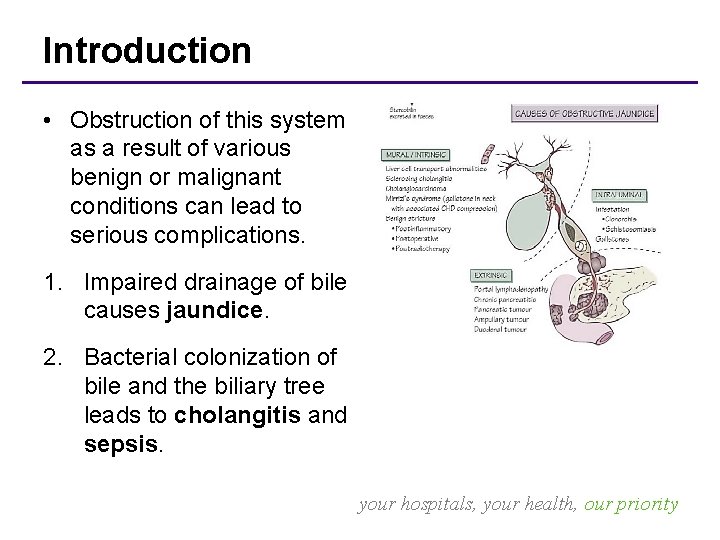
Introduction • Obstruction of this system as a result of various benign or malignant conditions can lead to serious complications. 1. Impaired drainage of bile causes jaundice. 2. Bacterial colonization of bile and the biliary tree leads to cholangitis and sepsis. your hospitals, your health, our priority
Biliary Sepsis • Infection of the biliary tract can potentially become acute, septic, and life-threatening. • It requires rapid evaluation and treatment due to its aggressive course. • If untreated, sepsis with shock, vascular collapse, multiorgan failure, and potentially death. your hospitals, your health, our priority
Biliary Sepsis • Antibiotics alone do not provide sufficient treatment in majority of patients. • Drainage of the biliary tree is the most critical step in management. • Endoscopic drainage (ERCP) in current practice is the best treatment line. your hospitals, your health, our priority
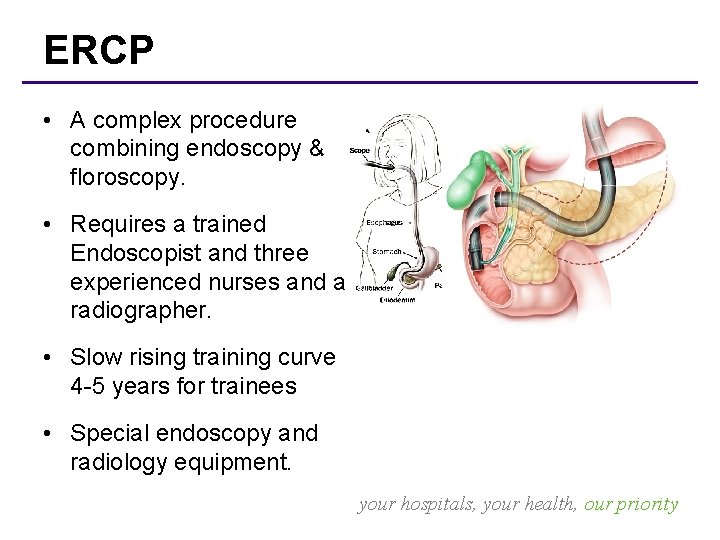
ERCP • A complex procedure combining endoscopy & floroscopy. • Requires a trained Endoscopist and three experienced nurses and a radiographer. • Slow rising training curve 4 -5 years for trainees • Special endoscopy and radiology equipment. your hospitals, your health, our priority
Plan • Goals: – Reduce length of hospital admission from (8. 5 days) – Decrease number of biliary sepsis. – Decrease the backlog for OP ERCP (250 cases) – Improve pt satisfaction • Identifying Problems: – Limited number of operators & staff – Limited resources available (rooms, equipment, etc) – Slow process of selection, referral & prioritizing cases your hospitals, your health, our priority
Active Steps • Drivers: (Feb 2017) – In-house training of gastro SAS in DGH (12 months) – Two ERCP training courses funded by the bursary – Improve the biliary referral scheme by surgical SAS • dedicated biliary ward rounds on Mondays • ad hoc extra ERCP on Monday PM – Negotiating a new job plan with clinical lead & clinical director to make ERCP sessions and HPB ward rounds available most week-days – Vacating a C-arm room on Monday for urgent ERCPs your hospitals, your health, our priority
Active Steps • Balancing workload for all staff while avoiding to neglect other commitments your hospitals, your health, our priority
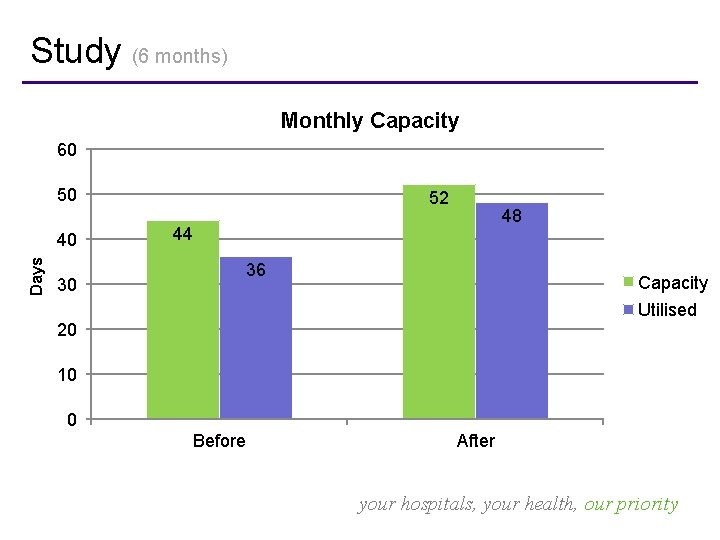
Study (6 months) Monthly Capacity 60 50 Days 40 52 48 44 36 30 Capacity Utilised 20 10 0 Before After your hospitals, your health, our priority
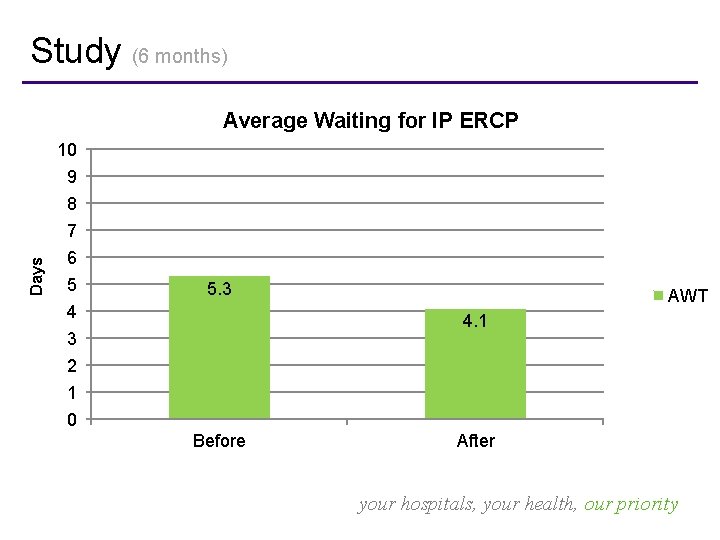
Study (6 months) Average Waiting for IP ERCP 10 9 8 Days 7 6 5 5. 3 4 AWT 4. 1 3 2 1 0 Before After your hospitals, your health, our priority
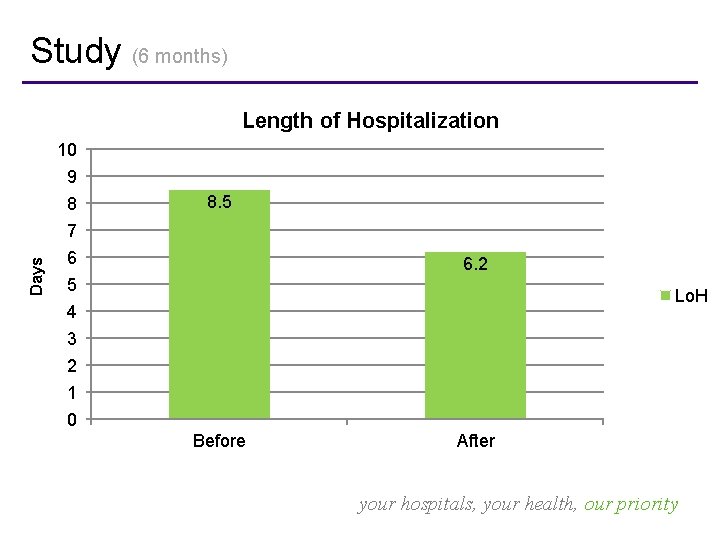
Study (6 months) Length of Hospitalization 10 9 8 8. 5 Days 7 6 6. 2 5 Lo. H 4 3 2 1 0 Before After your hospitals, your health, our priority
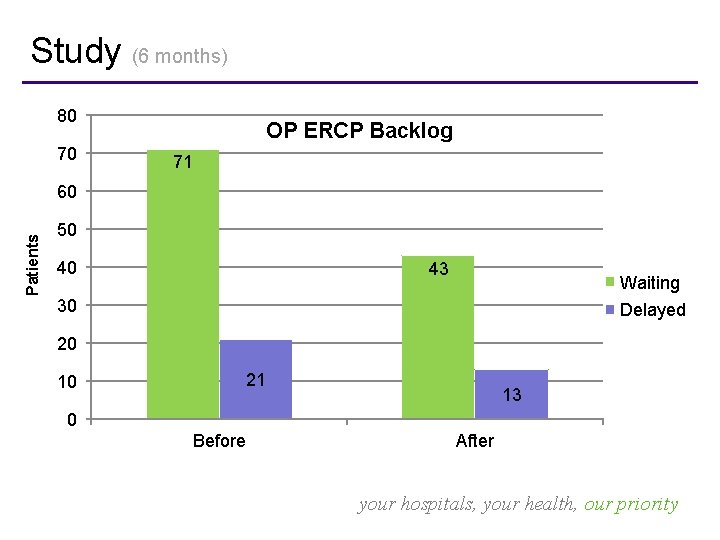
Study (6 months) 80 70 OP ERCP Backlog 71 Patients 60 50 40 43 Waiting 30 Delayed 20 21 10 13 0 Before After your hospitals, your health, our priority
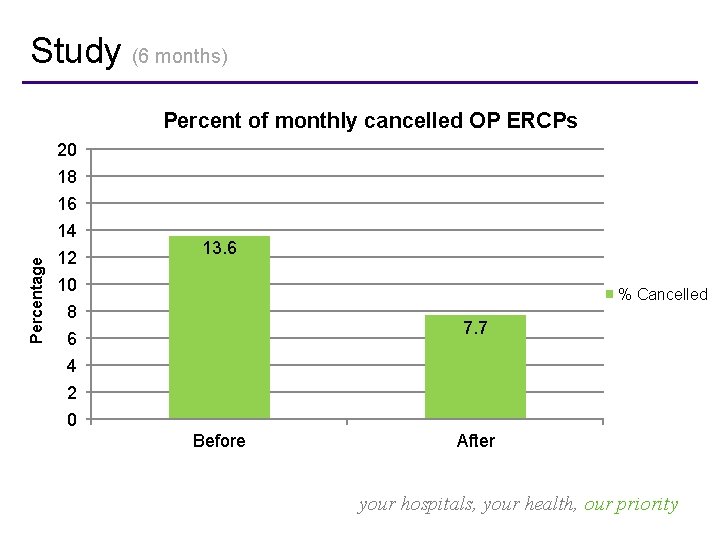
Study (6 months) Percent of monthly cancelled OP ERCPs 20 18 16 Percentage 14 12 13. 6 10 % Cancelled 8 7. 7 6 4 2 0 Before After your hospitals, your health, our priority
Study (12 months) • Positives – Increased average ERCP procedures from 44 to 52 monthly – Reduced average waiting time for IP ERCP from 5. 3 to 4. 1 days – Reduced LOS from 8. 5 to 6. 2 days – Decreased waiting backlog for OP ERCP from 71 to 43 pts – Less monthly number of cancelled OP ERCP cases (4, 7. 7% vs 6, 13. 6%) – Number of cases admitted with obstructive jaundice or cholecystitis progressing to biliary sepsis 21% v 13%. your hospitals, your health, our priority
Study (12 months) • Positives – SAS doctors proof they are of extremely important value in providing health care – Enhanced SAS doctors communication and collaboration across different specialties and with other nonmedical staff (nursing, radiographers, theatre staff) – Joining or even leading the HPB MDT (management and leadership roles) your hospitals, your health, our priority
Study (12 months) • Challenges: – SAS having to skip ward rounds or dropping other clinical commitments to review referrals – Subspecialisation limits chances for CESR – More responsibilities comes with more stress – Increased complications related to ERCP – Increased workload on wards resulting in some mistakes preparing cases for ERCP your hospitals, your health, our priority
Study (beyond 12 months) • Improvements – Reduced LOS from to 4. 7 days – Maintained low average waiting time for IP ERCP at 4. 3 days – Decreased waiting backlog for OP ERCP to 31 pts – Monthly n° of cancelled OP for IP ERCP dropped to 3 – Number of IP developing biliary sepsis 9%. – Post ERCP / discharge questionnaire showed patient satisfaction of 85. 7% your hospitals, your health, our priority
Conclusion • SAS doctors should be assertive in taking initiative to improve quality of service. • Career development and progression benefits the individual and the employer your hospitals, your health, our priority
Acknowledgements • • • Dr R Keld, Dr CS Lee Dr N Prasad, Dr P Bliss S Lynch S Ackers S Walsh, C Reddington, V Stevenson-Hornby your hospitals, your health, our priority
THANK YOU your hospitals, your health, our priority
- Slides: 24