Emphysematous urinary tract infections 2012 09 19 Introduction
![• • Tabaxin inj. 4. 5 g [Tazobactam/Piperacillin sodium] q 8 hr IV • • Tabaxin inj. 4. 5 g [Tazobactam/Piperacillin sodium] q 8 hr IV](https://slidetodoc.com/presentation_image/1a59690b1e83e1af708b6519df62d219/image-29.jpg)
- Slides: 29
Emphysematous urinary tract infections 2012. 09. 19 신장내과 유진영
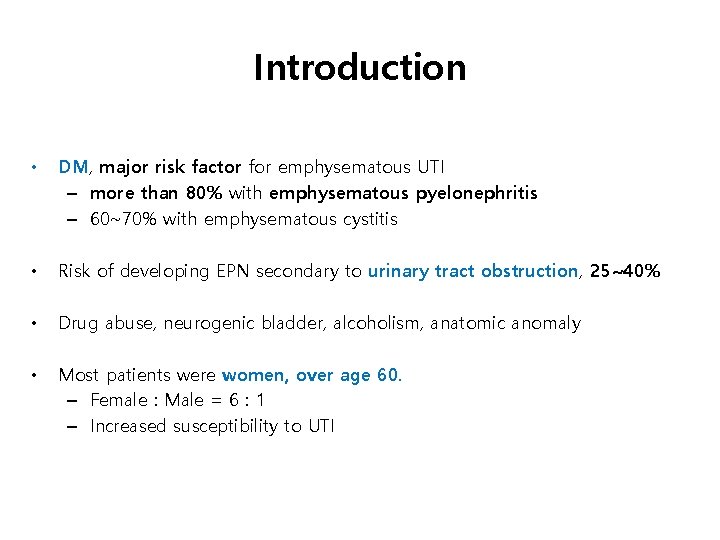
Introduction • Emphysematous urinary tract infections (UTIs) – infections of lower or upper urinary tract associated with gas formation – cystitis, pyelitis, or pyelonephritis • The first case was reported by Kelly and Mac. Cullum in 1898. • In 1962, Schultz and Klorfein, use of ‘emphysematous pyelonephritis’ term • Mortality rate of up to 78% until the late 1970 s but, over the last two decades, mortality rate 21%
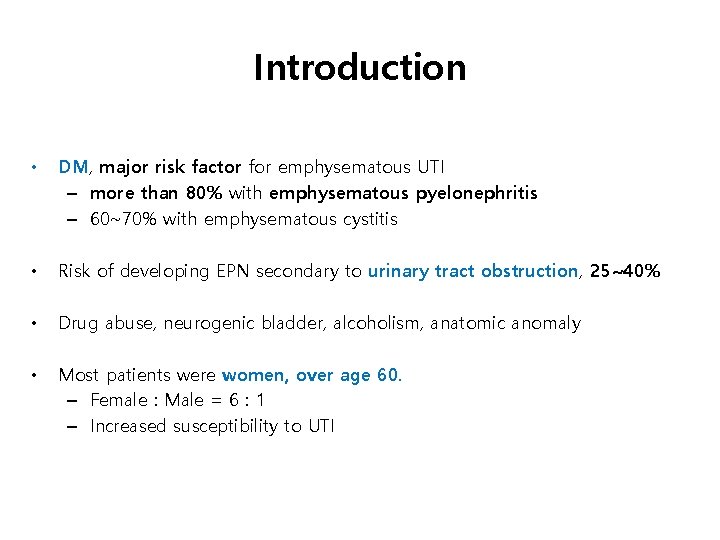
Introduction • DM, major risk factor for emphysematous UTI – more than 80% with emphysematous pyelonephritis – 60~70% with emphysematous cystitis • Risk of developing EPN secondary to urinary tract obstruction, 25~40% • Drug abuse, neurogenic bladder, alcoholism, anatomic anomaly • Most patients were women, over age 60. – Female : Male = 6 : 1 – Increased susceptibility to UTI
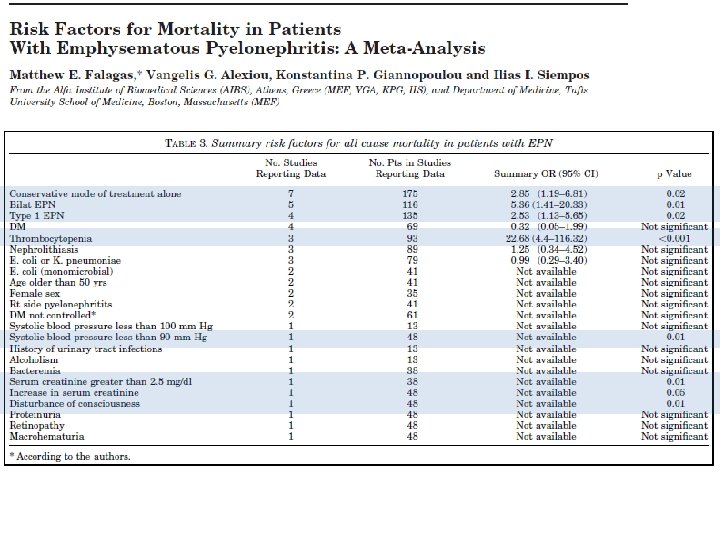
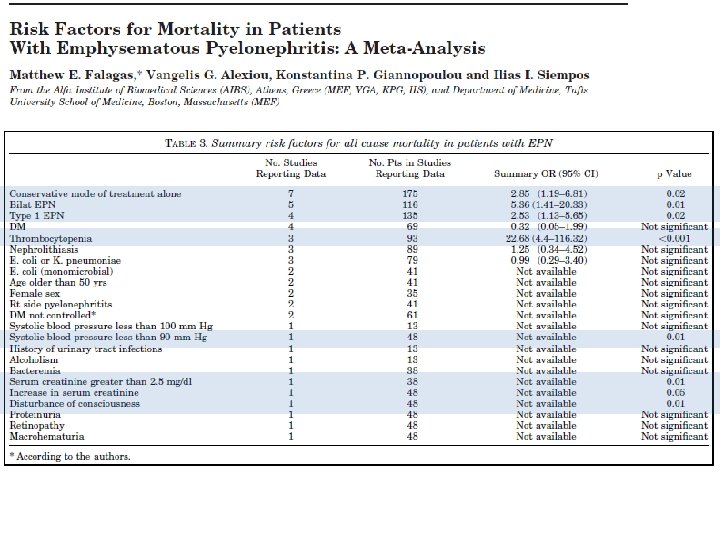
MEDLINE, Pub. Med, EMBASE, CINAHL and the Cochrane Library from 1966 to 2006.
• Pathogenesis, poorly understood – Elevated tissue glucose levels in DM provide a more favorable microenvironment for gas-forming microbes – Impaired blood supply – Reduced host immunity – Obstruction within the urinary tract
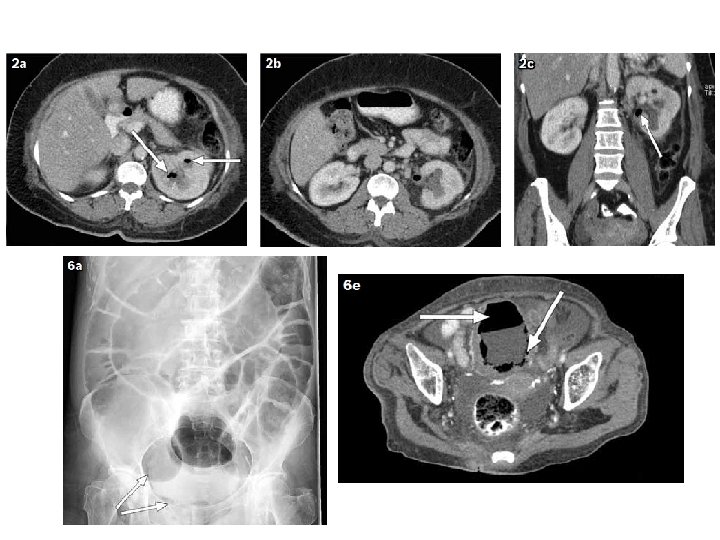
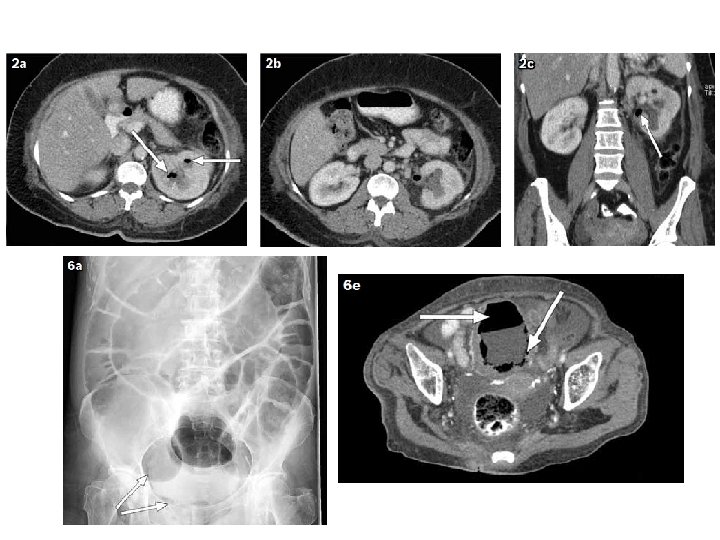
DIAGNOSIS • Plain film of abdomen / CT – air in the renal parenchyma, bladder, or surrounding tissue in 50 to 85% – CT scan, more sensitive than plain film extent of gas formation and any obstructing lesions in the urinary tract • Imaging, particularly CT scanning, classify emphysematous pyelonephritis to estimate prognosis & guide therapy
EMPHYSEMATOUS PYELONEPHRITIS AND PYELITIS
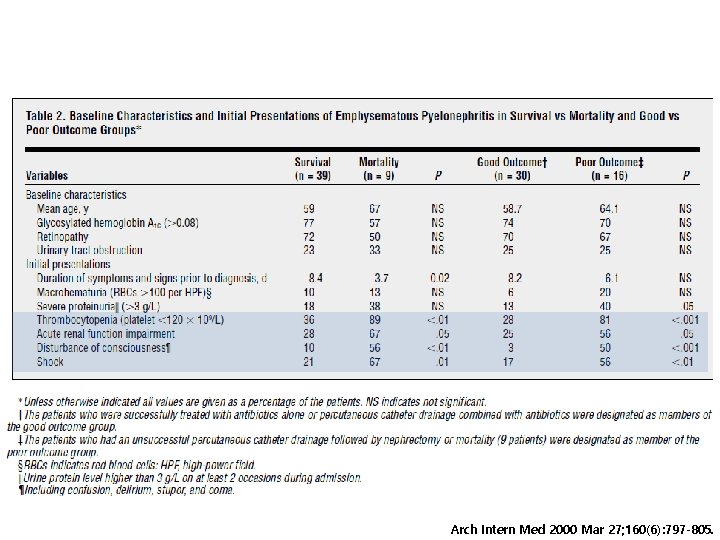
Clinical features • Indistinguishable from severe, acute pyelonephritis – fevers, chills, flank or abdominal pain, nausea, vomiting – onset of symptoms, abrupt or evolve slowly over two to three weeks • Laboratory testing – hyperglycemia, leukocytosis, elevated serum creatinine, pyuria – acute, anuric renal failure, uncommon complication in bilateral infection or unilateral disease in a solitary functioning kidney
Clinical features • Urine or pus culture (+), nearly 70% • Bacteremia, more than 50% • All organisms isolated from blood cultures were simultaneously found in cultures of the urine or renal pus. • Almost infections were due to E. coli (69%) or K. pneumoniae (29%). • In rare cases, anaerobic microorganisms including Clostridium septicum, Candida albicans, Cryptococcus neoformans and Pneumocystis jiroveci
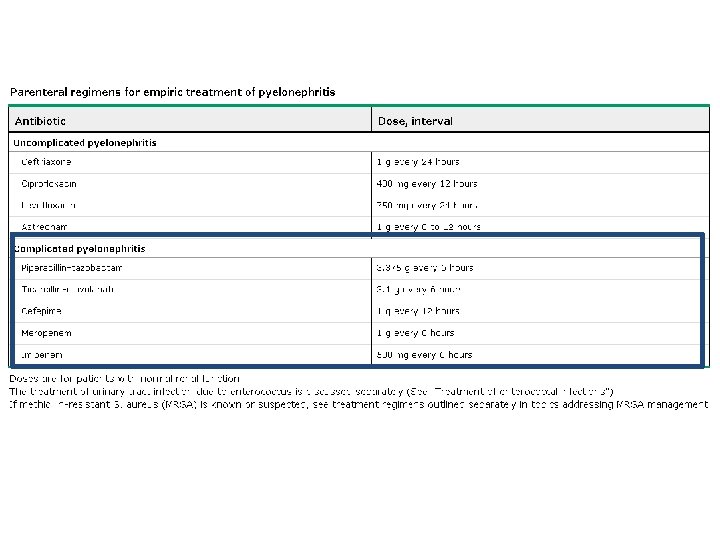
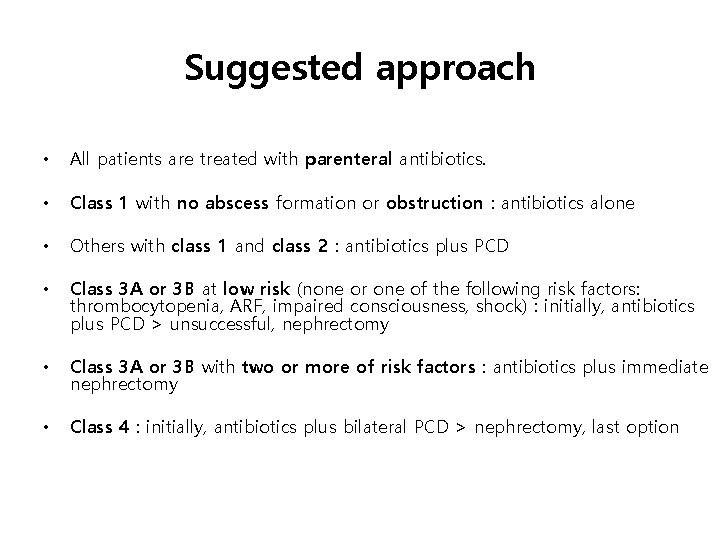
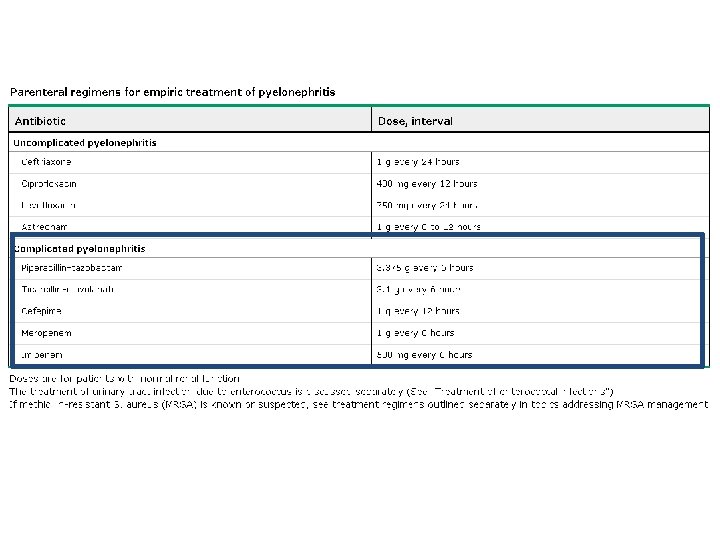
Treatment • In the past, usually nephrectomy or open drainage along with systemic antibiotics • However, selected patients can be managed successfully with antibiotics, percutaneous catheter drainage (PCD) of gas & purulent material • All patients are treated with parenteral antibiotics; antibiotics for the management of acute complicated pyelonephritis
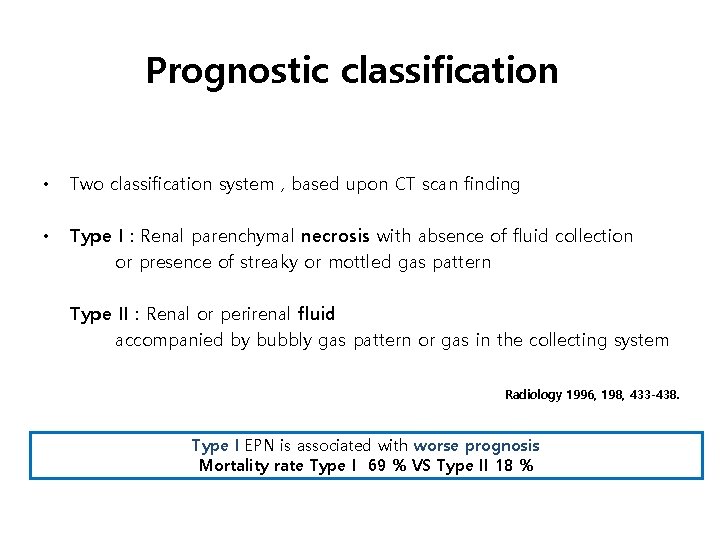
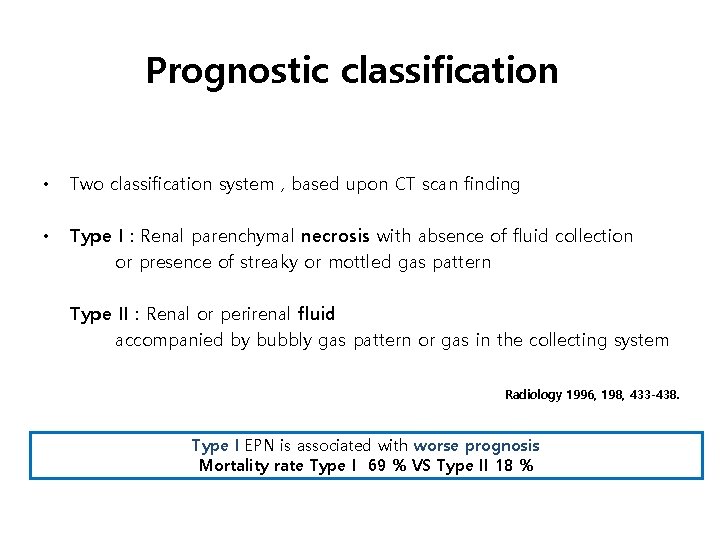
Prognostic classification • Two classification system , based upon CT scan finding • Type I : Renal parenchymal necrosis with absence of fluid collection or presence of streaky or mottled gas pattern Type II : Renal or perirenal fluid accompanied by bubbly gas pattern or gas in the collecting system Radiology 1996, 198, 433 -438. Type I EPN is associated with worse prognosis Mortality rate Type I 69 % VS Type II 18 %
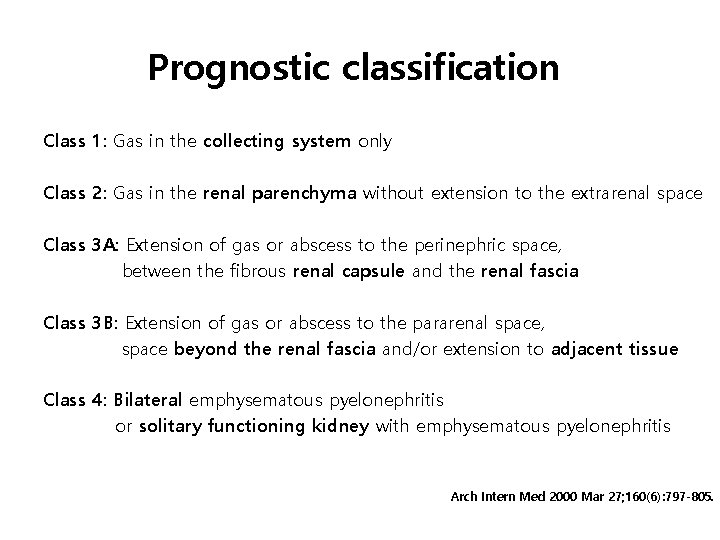
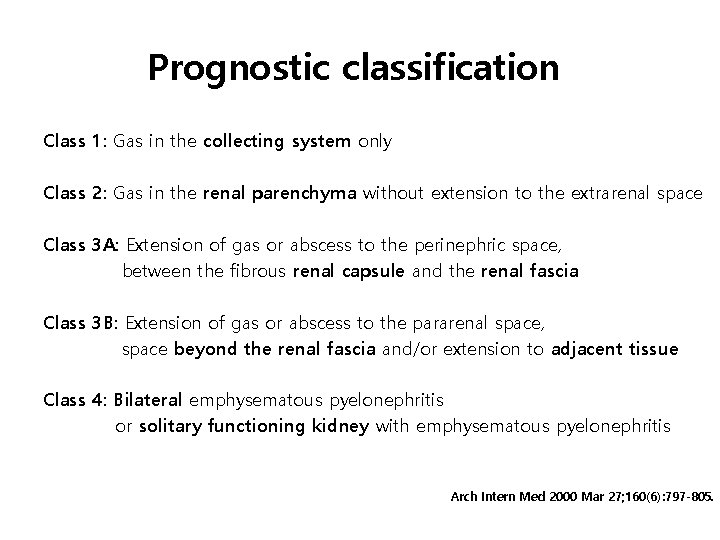
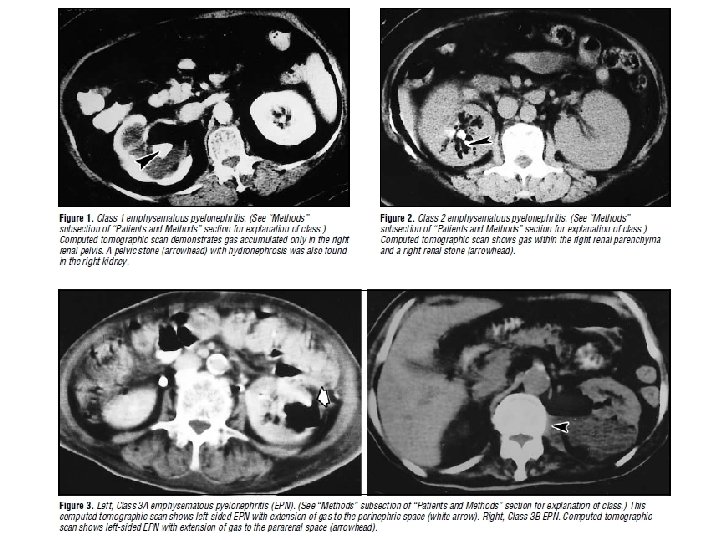
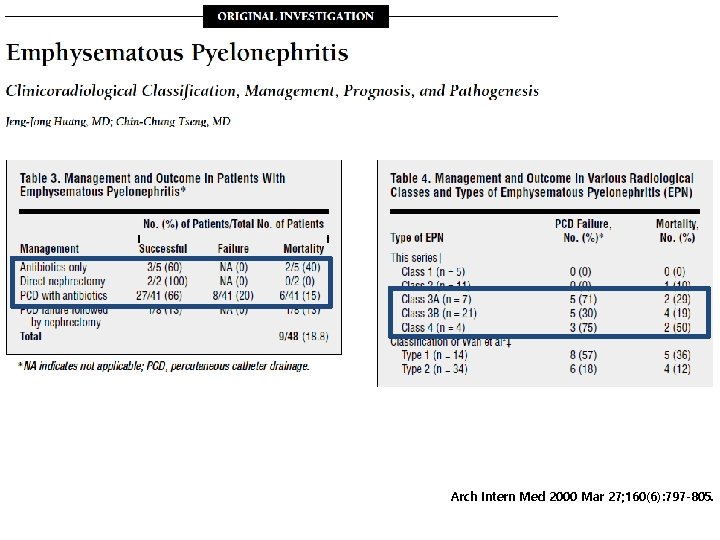
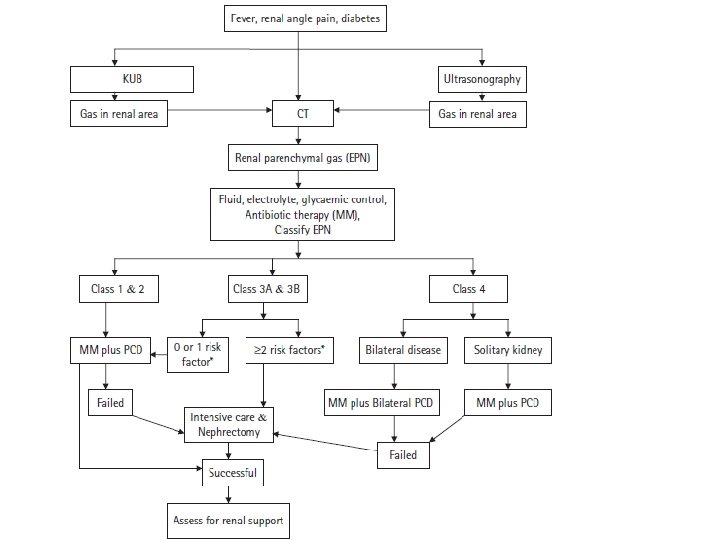
Prognostic classification Class 1: Gas in the collecting system only Class 2: Gas in the renal parenchyma without extension to the extrarenal space Class 3 A: Extension of gas or abscess to the perinephric space, between the fibrous renal capsule and the renal fascia Class 3 B: Extension of gas or abscess to the pararenal space, space beyond the renal fascia and/or extension to adjacent tissue Class 4: Bilateral emphysematous pyelonephritis or solitary functioning kidney with emphysematous pyelonephritis Arch Intern Med 2000 Mar 27; 160(6): 797 -805.
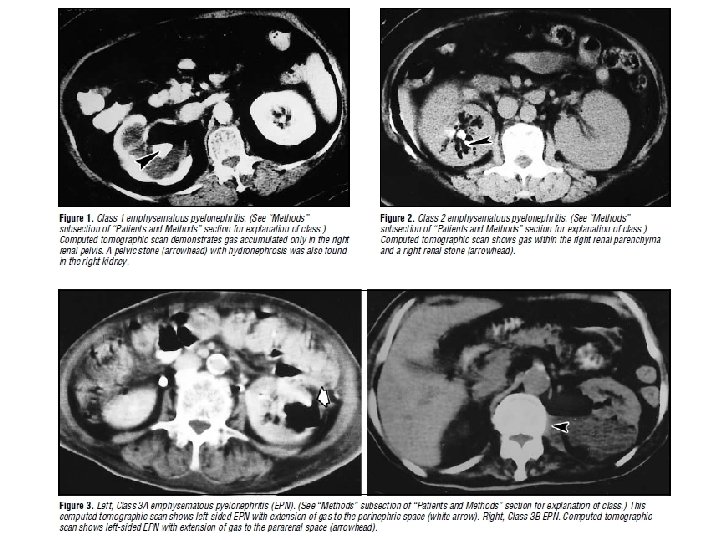
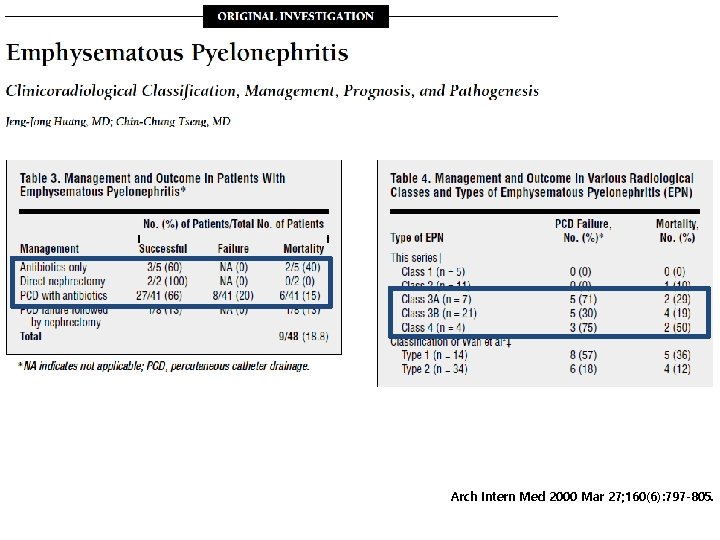
Arch Intern Med 2000 Mar 27; 160(6): 797 -805.
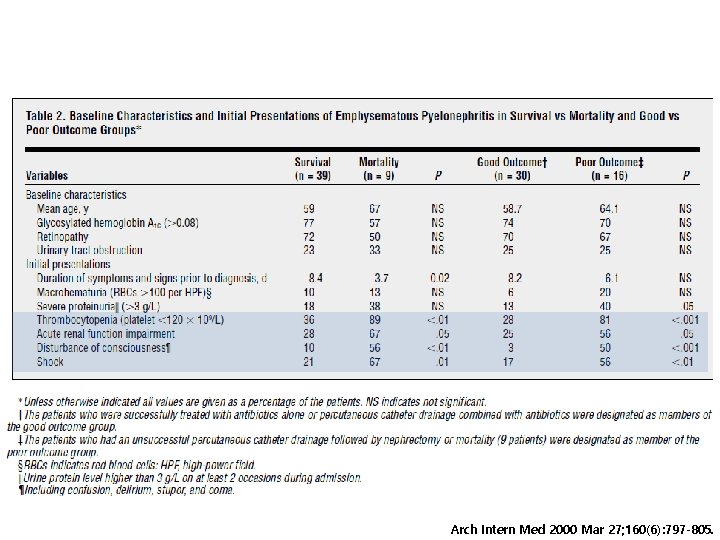
Arch Intern Med 2000 Mar 27; 160(6): 797 -805.
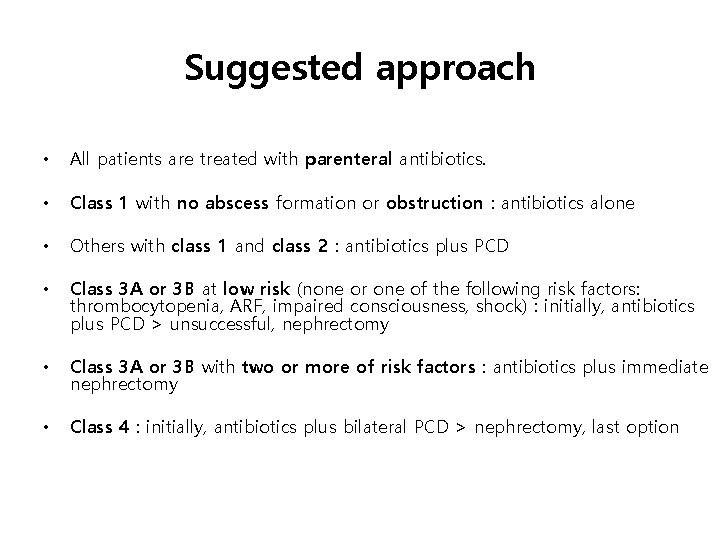
Suggested approach • All patients are treated with parenteral antibiotics. • Class 1 with no abscess formation or obstruction : antibiotics alone • Others with class 1 and class 2 : antibiotics plus PCD • Class 3 A or 3 B at low risk (none or one of the following risk factors: thrombocytopenia, ARF, impaired consciousness, shock) : initially, antibiotics plus PCD > unsuccessful, nephrectomy • Class 3 A or 3 B with two or more of risk factors : antibiotics plus immediate nephrectomy • Class 4 : initially, antibiotics plus bilateral PCD > nephrectomy, last option
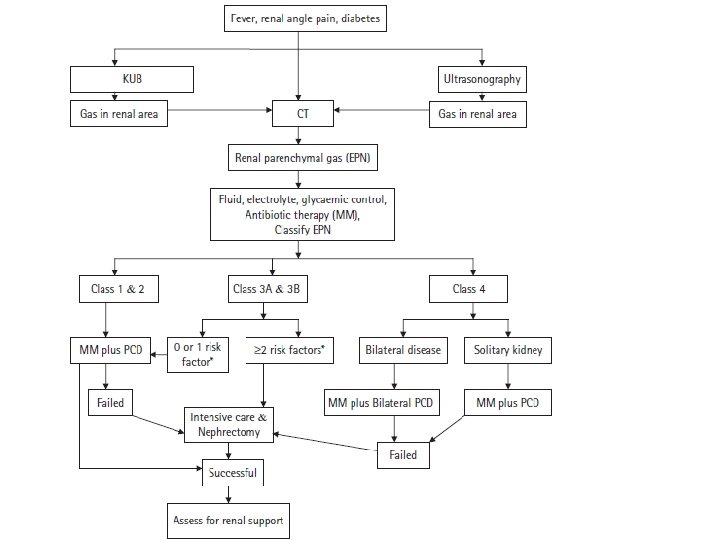
• PCD, drainage time varies from 5 days to 12. 6 weeks • Commonly irrigate & aspirate PCD tube to ensure maximum drainage • Chen et al, recommend a repeat CT after 4 to 7 days to look for other noncommunicating air/fluid collections, to plan nephrectomy for non-responders to PCD. J Urol 1997; 157: 1569 -73 • Elective nephrectomy for prolonged fever and sepsis
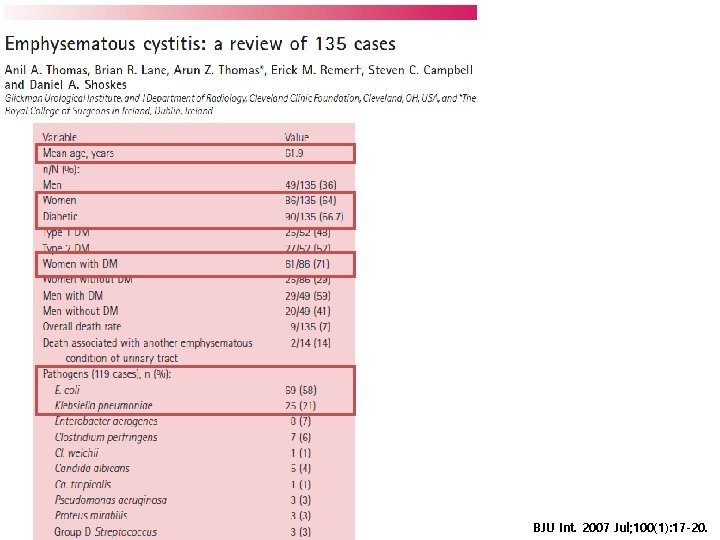
EMPHYSEMATOUS CYSTITIS
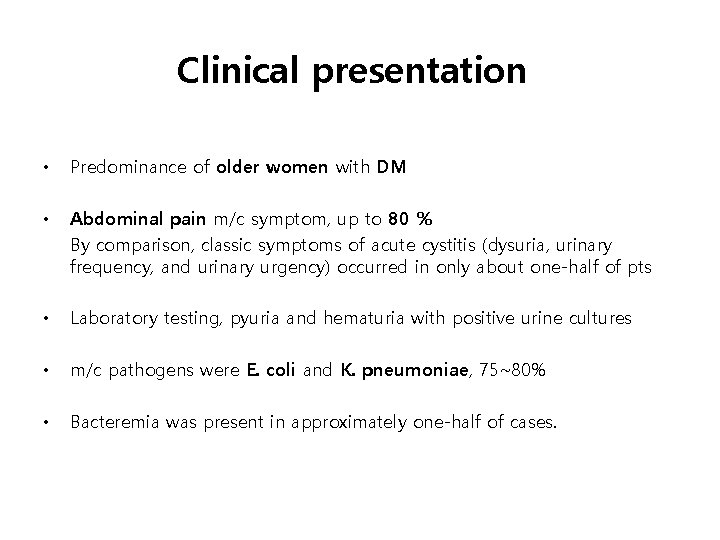
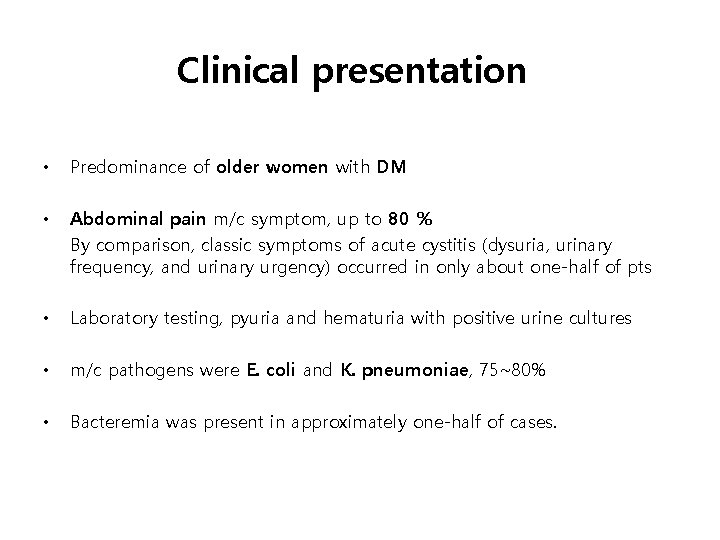
Clinical presentation • Predominance of older women with DM • Abdominal pain m/c symptom, up to 80 % By comparison, classic symptoms of acute cystitis (dysuria, urinary frequency, and urinary urgency) occurred in only about one-half of pts • Laboratory testing, pyuria and hematuria with positive urine cultures • m/c pathogens were E. coli and K. pneumoniae, 75~80% • Bacteremia was present in approximately one-half of cases.
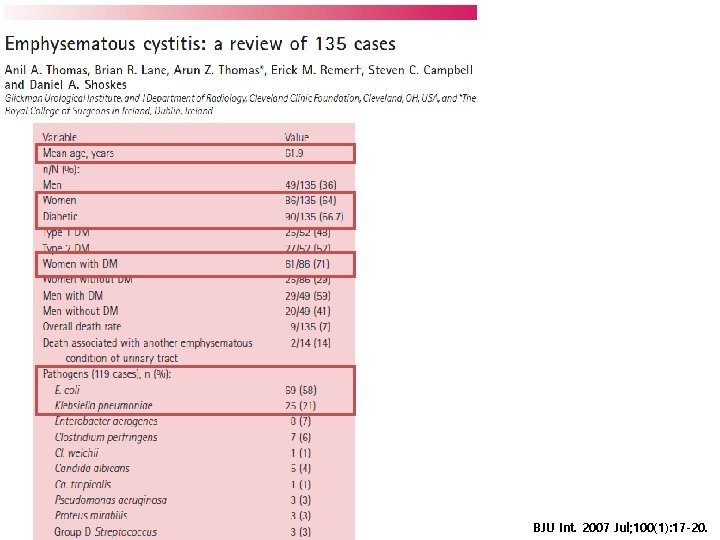
BJU Int. 2007 Jul; 100(1): 17 -20.
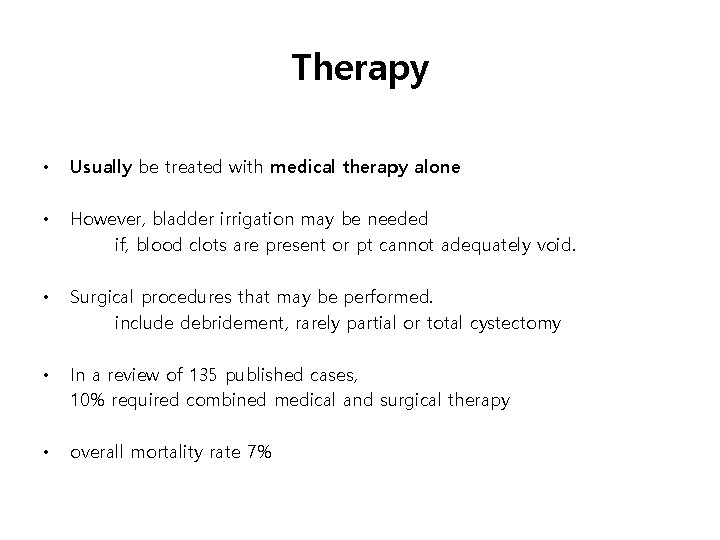
Therapy • Usually be treated with medical therapy alone • However, bladder irrigation may be needed if, blood clots are present or pt cannot adequately void. • Surgical procedures that may be performed. include debridement, rarely partial or total cystectomy • In a review of 135 published cases, 10% required combined medical and surgical therapy • overall mortality rate 7%
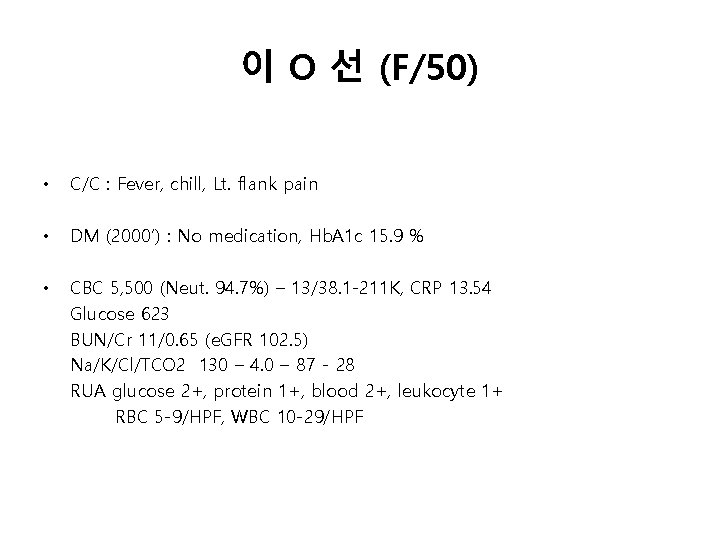
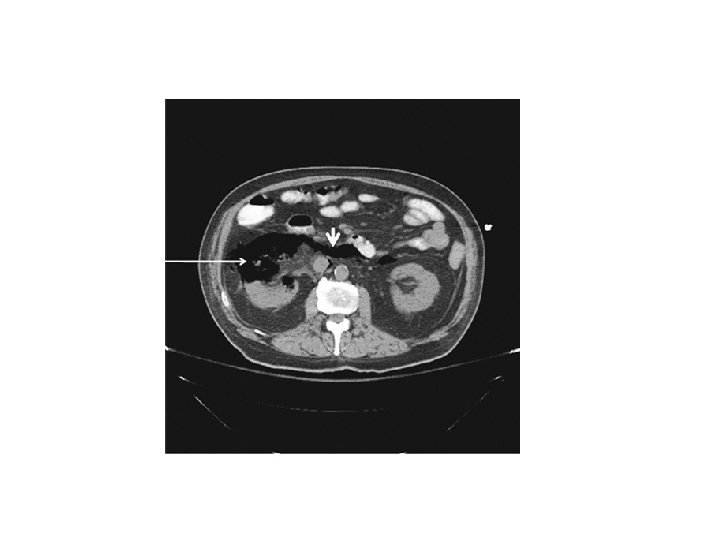
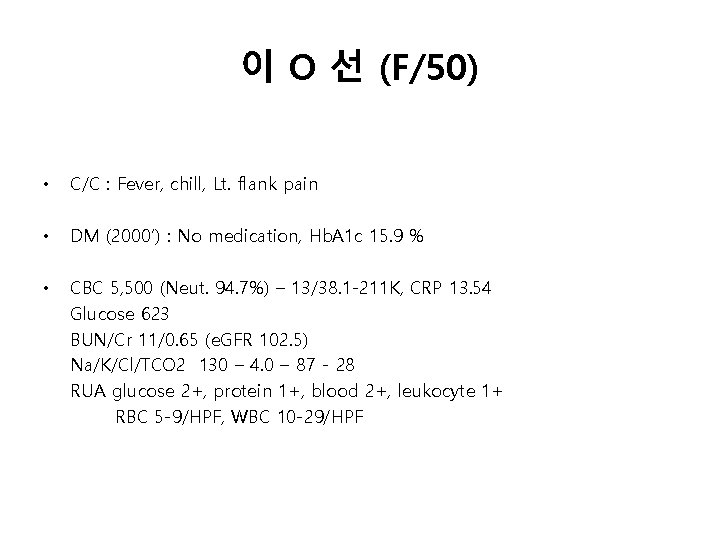
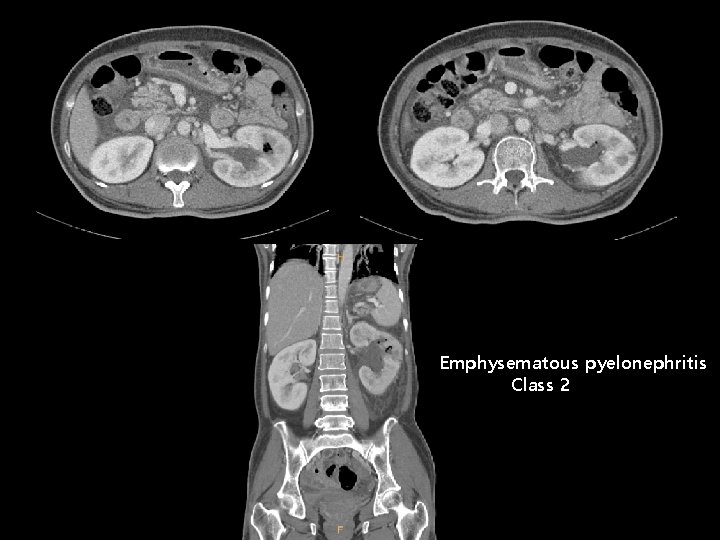
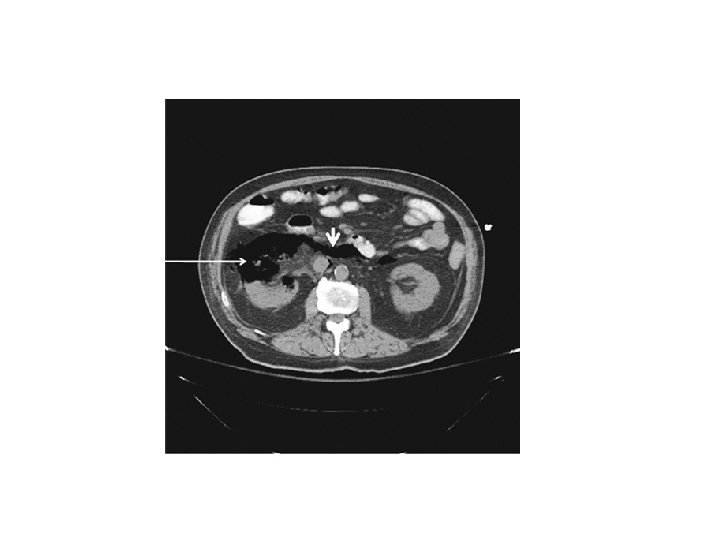
이 O 선 (F/50) • C/C : Fever, chill, Lt. flank pain • DM (2000’) : No medication, Hb. A 1 c 15. 9 % • CBC 5, 500 (Neut. 94. 7%) – 13/38. 1 -211 K, CRP 13. 54 Glucose 623 BUN/Cr 11/0. 65 (e. GFR 102. 5) Na/K/Cl/TCO 2 130 – 4. 0 – 87 - 28 RUA glucose 2+, protein 1+, blood 2+, leukocyte 1+ RBC 5 -9/HPF, WBC 10 -29/HPF
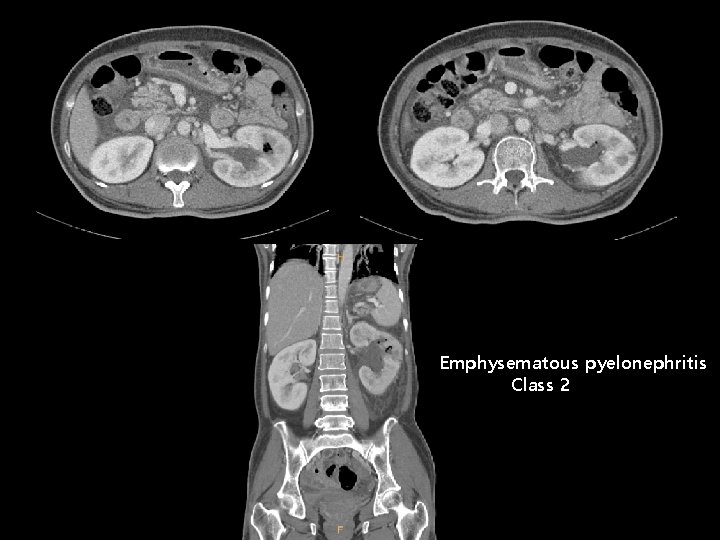
Emphysematous pyelonephritis Class 2
![Tabaxin inj 4 5 g TazobactamPiperacillin sodium q 8 hr IV • • Tabaxin inj. 4. 5 g [Tazobactam/Piperacillin sodium] q 8 hr IV](https://slidetodoc.com/presentation_image/1a59690b1e83e1af708b6519df62d219/image-29.jpg)
• • Tabaxin inj. 4. 5 g [Tazobactam/Piperacillin sodium] q 8 hr IV PCD insertion