Emotional Aspects of Pregnancy Nutritional Needs in Pregnancy









- Slides: 44
Emotional Aspects of Pregnancy Nutritional Needs in Pregnancy Educational Needs in Pregnancy
Psychological Responses • • • Ambivalence Acceptance Introversion Mood swings Changes in body image

Reva Rubin’s Maternal Tasks • • Safe passage Seeking acceptance Binding in to the child Giving of oneself
Expectant Father • First trimester- confused, baby seems “unreal” • Second trimester- Proud, acceptance and attachment, financial concerns • Third trimester- anticipating the birth, some fears about labor process, baby’s health • Couvade- unintentional development of physical sx: nausea, aches and pains, etc
Fathering steps • • Accepting the pregnancy Identifying with father role Reordering personal relationships Establishing relationship with fetus
Extended Family Preparation • • Siblings • Preparation: • Inclusion: Grandparents • Preparation: • Inclusion
Nursing Care in Pregnancy What happens throughout the pregnancy

Initial Prenatal Visit • • Generally recommended after 2 nd missed period Begin with thorough history • • • Chronic illnesses Social history Psychological needs Determine Estimated Due Date (EDD) or Estimated Date of Confinement (EDC) Present pregnancy~ LMP, presumptive signs, GTPAL

• Complete physical examination • • • Assess pelvis for diagonal conjugate, and adequacy of pelvis for vaginal delivery of average-sized baby Draw all prenatal labs Begin all the prenatal education: books, videos, etc.
Nagele’s Rule for EDC • • • Begin with LMP Subtract 3 months Add 7 days

Let’s try it!!! • • • EDC EDC • • • LMP 1 -05 -16 LMP 3 -25 -16 LMP 10 -10 -15

GTPAL vs Gravida - Para • • • Gravida= # of pregnancies Term deliveries= > 37 weeks-42 weeks Preterm deliveries= < 37 weeks(also Pt) Abortions= < 20 weeks Living children Gravida/Para = Pregnancy/Delivery
Gravida and Para vs GTPAL • • • Gravida= any pregnancy regardless of duration Para= Birth after 20 weeks’ gestation, regardless of whether the infant is born alive or dead “When using the detailed system, GTPAL, GRAVIDA keeps the same meaning, but the meaning of PARA changes because the detailed system counts each infant born rather than the number of pregnancies carried to viability” (Davidson et al, p. 318, 2012). • Can view 10 th edition on page 244
Lab Tests • • UA and culture Blood: CBC, Type/Rh VDRL/RPR/Serology Toxoplasmosis Rubella Hepatitis B HIV Antibody Screening
• • 10 -12 wks: Chorionic Villi Sampling 14 -16 wks: Amniocentesis 15 -20 wks: MSAFP (see Fetal Assessment Wksht) 24 -28 wks: Blood sugar 3 hr GTT 36 wks + : Beta strep vaginal culture Website for Group B Beta Strep~ CDC pamphlet Hgb & Hct repeated prn throughout pg. Urine: glucose and protein at every prenatal visit. Should be 1 st morning specimen collected and refrigerated, but can also be fresh sample upon arrival at office.
Other diagnostic testing. . . • • Pap test (hold her over until postpartum) Ultrasound for dates/anomalies
Educational Needs~begins at 1 st prenatal visit but continues throughout pregnancy • • • rest and sleep exercise employment recreation travel use of drugs & alcohol • • • immunizations skin and breast care clothing Dental health nutrition
Prenatal Exercises & Sexual Activity during Pregnancy • • • Website on prenatal exercises Refer to pp. 293 -295 (10 th ed) for suggested exercises Be open to discussion during prenatal visits re: sexual activity. See Teaching Plan p. 296; 10 th ed. • u u Changes in desire r/t nausea, fatigue in 1 st trimester, desire in 2 nd trimester, desire in 3 rd trimester r/t backache, size of baby Suggest alternative methods to express intimacy Stress importance of open communication between partners
WARNING SIGNS~assessed at each prenatal visit • • vaginal bleeding edema of face and in fingers severe continuous headache dim or blurred vision/spots/flashes abdominal pain/persistant vomiting fever and chills gush of fluid from vagina dysuria, backache, flank pain
Subsequent prenatal visits • Generally recommend monthly visits for low-risk mothers through 32 weeks gestation • • • Assess weight, BP, urine, sx of complications, FHR, Mc. Donald’s Rule 32 -36 weeks~ bi-monthly 36 weeks-delivery~ weekly
Maternal and Fetal Nutrition
• Why Pregnancy= more need for nutrients? Uterine-placental-fetal unit • Maternal blood volume • Mammary changes • RDA = 300 kcal more / day than prepregnant dietary needs • Look at Teaching plan on p. 296 (10 th ed)
Choose My Plate http: //www. choosemyplate. gov

Weight Gain over entire pregnancy • • Underweight 28 – 40 lbs. Normal weight 25 – 35 lbs. Overweight 15 – 25 lbs. Obese 15 lbs. Adolescents - high end of range Short women – low end of range Twins ~44 lbs. Has best outcome

Recommended Weight Gain Throughout Pregnancy~ know this! • 1 st Trimester~ 3. 5 -5 lbs (1. 6 -2. 3 kg) • 2 nd & 3 rd trimesters~1 lb/week (0. 5 kg/wk)
PROTEIN~60 g/day • • • Fetal growth Placental growth Amniotic fluid production Uterine muscle growth Blood production
IRON (27 mg/day) • • • Facilitates blood cell production If mom is anemic, there is risk of lethargy in mom, preterm births, intolerance to blood loss at delivery Guidelines for taking Iron (e. g. . Ferrous Sulfate Fe. SO 4 , Ferro. Sequels, Ferrous Fumarate) -- Take on an empty stomach with OJ -- Do NOT take with milk, coffee, tea -- Keep away from CHILDREN-- risk of toxic ingestion -- Instruct mom on possible stool changes: black and tarry, risk of constipation
WATER • Necessary for expansion of blood volume & to risk of constipation • Need to drink 6 – 8 glasses/day • Limit caffeine intake • Avoid artificial sweeteners in beverages
SODIUM • • Needed due to expanding circulating fluid volume Need to balance ECF concentration due to GFR Don’t restrict because Sodium is essential to fluid & electrolyte balance Don’t overdue as it may lead to excessive fluid retention (edema of face & hands)
CALCIUM(1000 mg) • • • Fosters fetal calcification of bones If intake not adequate, demineralization of maternal bones occurs 4 cups of milk or its equivalent Assess cultural diet as some cultures do not advocate milk & dairy products Review alternative resources of Calcium as green leafy vegetables, and Ca+++ fortified foods
FAT-SOLUBLE VITAMINS • • • ADEK In excess amounts, they are toxic Necessary for tooth budding and bone growth Excellent source of Vitamin D: fortified milk & sunlight which produces D on our skin May be taken in water-miscible form if not able to metabolize properly
ZINC • • • Contained in enzymes of metabolic pathways Best resources~ meats, shellfish, poultry, OR whole grains and legumes Iron and folic acid inhibit absorption
LACTATION • • • RDA: 500 kcal more than non-pregnant woman Minimum of 1800 kcal/day Calcium and Iron intake Smoking: impairs milk production Alcohol in excess impairs milk ejection reflex Caffeine: accumulated in infant through breastmilk will be manifested as a wakeful and active baby!
FOLIC ACID • • Low levels correlate with neural tube defects. Critical to begin increasing Folic Acid intake at least 3 months before conception! Supplemental Folic Acid only begun in 1992, Now a big March of Dimes initiative Acceptable Folic Acid levels are most critical in the 1 st 6 wks of pregnancy and should be continued throughout pregnancy.
Factors affecting nutrition • Eating disorders • Lactase deficiency (lactose intolerance) • Pica~Pica is the practice of eating non-edible substances(clay, dirt, laundry starch, etc. ). • It is especially important for the nurse to assess the pregnant patient who has lower hemoglobin levels as she may be replacing low-nutrient products for nutritious foods.
Cultural Spiritual influences • • MANY cultures have “hot/cold” theories on nutrition and pregnancy is often viewed as a “hot” time that requires foods that fall under the “cold” categories. These foods generally include dairy foods. Be sure to assess carefully. Vegetarians still need adequate proteins and need to be taught of good resources.
Vegetarians~ website Types • Lacto-ovovegetarians~mild, dairy products, & eggs • Lactovegetarians~ include dairy, but no eggs • Vegans~strict vegetarians who eat no food from any animal sources. These persons need to plan how to get adequate complete proteins and sufficient calories. u Examples of complete proteins: beans & rice, or peanut butter on whole grain bread, whole grain cereal with soy milk.
Psychosocial factors~role of food and serving food as a maternal role • Socioeconomic factors (see slide on WIC) • Education~ it is essential for nurses to integrate teaching on healthy eating in pregnancy from the first prenatal visit. • Psychological Factors~ food may be used as a substitute for emotions OR may be avoided if patient is depressed.
Common Discomforts of Pregnancy • • Refer to pp. 282 -288 (10 th ed) in Davidson et al for discussion of many general discomforts of pregnancy and how to alleviate them. The following discussion focuses on those related to nutrition in pregnancy and discomforts associated with it.

Feeling GREEN(nauseated)? GREEN(nauseated) • • • eat dry foods(CHO’s) small amts frequently don’t get hungry! fresh air helps limit fried/fatty foods • • • eat cold foods with little or no smell don’t brush teeth right after eating
Feeling STUCK(constipated)? !? STUCK(constipated)? • • eat high fiber increase fluids exercise to increase bowel motility Avoid laxatives
PLOP FIZZ(heartburn) • • • small frequent meals avoid spicy foods no tight clothes across tummy don’t lie down after meals may need to sleep in recliner in last weeks
WIC • • Women Infants & Children (federally funded program provided by Health Dept. ) Supplemental nutrition program for moms & babies Income eligible Food coupons for pregnant & lactating women Formula available for bottlefed babies Must go to nutrition class taught by dietician Children have regular developmental assessments by nurses

There you have it!!
 Purpose of malnutrition
Purpose of malnutrition Nutritional needs throughout the life cycle
Nutritional needs throughout the life cycle Chapter 2 nutritional needs
Chapter 2 nutritional needs Medicolegal importance of lochia
Medicolegal importance of lochia Early pregnancy pictures of spotting during pregnancy
Early pregnancy pictures of spotting during pregnancy Social emotional needs of ell students
Social emotional needs of ell students Simple claustral complex
Simple claustral complex Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Primary needs and secondary needs
Primary needs and secondary needs Target needs and learning needs in esp
Target needs and learning needs in esp Satisfaction
Satisfaction Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Nutritional epidemiology definition
Nutritional epidemiology definition Nutritional requirements of microorganisms
Nutritional requirements of microorganisms Quick breads definition
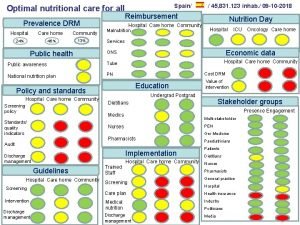
Quick breads definition Optimal nutritional care for all
Optimal nutritional care for all What is nutritional quackery
What is nutritional quackery Abcd of nutritional assessment
Abcd of nutritional assessment Malabsorption causes
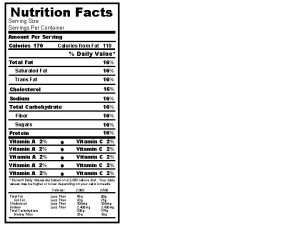
Malabsorption causes Servings per container
Servings per container Diet chart for diabetic patient
Diet chart for diabetic patient Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Nutritional diseases
Nutritional diseases Tallund man
Tallund man Abcd of nutritional assessment
Abcd of nutritional assessment Chapter 11 nutrition and diets
Chapter 11 nutrition and diets Malnutrition conclusion
Malnutrition conclusion Ada 411
Ada 411 How can we crack nature’s secret nutritional code
How can we crack nature’s secret nutritional code Chapter 27 nutritional therapy and assisted feeding
Chapter 27 nutritional therapy and assisted feeding Abcd assessment nutrition
Abcd assessment nutrition Chapter 24 nutritional care and support
Chapter 24 nutritional care and support Elastin culinary definition
Elastin culinary definition Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Mini nutritional assessment
Mini nutritional assessment What ecological role best describes grizzly bears?
What ecological role best describes grizzly bears? Nutritional diseases
Nutritional diseases Nutritional recovery syndrome
Nutritional recovery syndrome Foodafactoflife nutritional analysis
Foodafactoflife nutritional analysis Types of nutritional survey
Types of nutritional survey What is nutritional health
What is nutritional health Nutritional requirements of plants
Nutritional requirements of plants Nutritional intervention
Nutritional intervention Specialized nutrition support
Specialized nutrition support Abcd of nutritional assessment
Abcd of nutritional assessment