Emergency Oxygen Therapy Is there a problem Tom
Emergency Oxygen Therapy Is there a problem? Tom Heaps CONSULTANT ACUTE PHYSICIAN
Clinical Case No. 1 • • 79 -year-old female, diabetic, morbidly obese Admitted with ‘LVF’ Overnight ‘Reduced GCS ? cause’ 15 L oxygen via non-rebreathe in situ ABG showed p. H 6. 9, p. CO 2 15. 9 k. Pa normal range 4. 5 -6. 0 k. Pa Woke up when oxygen removed! Oxygen prescribed with target Sp. O 2 88 -92%, documented in notes • Following morning on AMU GCS 3/15 and 15 L NRB back in situ! • Not a candidate for NIV → RIP
Clinical Case No. 2 • 75 -year-old male, cervical myelopathy (cord compression due to OA) • • Admitted with reduced GCS (9/15) p. H 7. 1, p. CO 2 9. 6 k. Pa (respiratory acidosis) Improved with controlled O 2 24 -28% Treated for pneumonia Became drowsy again with rising p. CO 2 and low RR Miotic (small) pupils Covered in fentanyl patches Improved once patches removed and naloxone given!
Clinical Case No. 3 • 86 -year-old female from RH, osteoporosis • Admitted with pneumonia • Asked to see on AMU because of ‘fitting’ • Hypotensive, myoclonic jerks, bounding pulse • On 10 L O 2 via NRB since admission • ABG showed p. H 7. 23, p. CO 2 12. 9 k. Pa • Minimal improvement with reduced Fi. O 2 • Not a candidate for HDU or NIV on the respiratory ward → RIP
Oxygen —there is a problem! Published national audits have shown; • Doctors and nurses have a poor understanding of how oxygen should be used • Oxygen is often given without any prescription • If there is a prescription, it is unusual for the patient to receive what is specified on the prescription • Monitoring of oxygen administration is often poor →OXYGEN IS DANGEROUS NPSA alert 2009

Emergency Oxygen Use in Adult Patients BTS Guideline 2009 • Prescribing by target oxygen saturation • Keeping Sp. O 2 within normal limits • Target Sp. O 2 94 -98% for most patients 92 -98% if >70 • Target Sp. O 2 88 -92% (p. O 2 6. 7 -10 k. Pa) for those with or at risk of hypercapnic (high CO 2) respiratory failure
Aims of Emergency Oxygen Therapy 1. To correct or prevent potentially harmful hypoxaemia 2. To alleviate breathlessness only if hypoxaemic Increasing Fi. O 2 (inspired oxygen concentration) is only one way of increasing overall O 2 carrying capacity of blood: – Protect airway – Enhance circulating volume and cardiac output – Correct severe anaemia – Avoid or reverse respiratory depressants e. g. morphine – Treat underlying cause e. g. LVF, asthma
Indications for Emergency Oxygen 1. Sp. O 2 <94% <88% if risk of hypercapnia 2. Critical illness e. g. septic shock, major trauma, anaphylaxis, acute LVF during initial ABCDE 3. Carbon monoxide poisoning irrespective of Sp. O 2
Too much O 2 can be harmful… • Risk of hypercapnia (high CO 2) in selected patients – some patients with chronic hypercapnia are dependent on hypoxaemia to maintain respiratory drive • Constriction of coronary arteries – high O 2 levels INCREASED mortality in survivors of cardiac arrest • Constriction of cerebral arteries – high O 2 levels INCREASED mortality in non-hypoxic patients with mild-moderate stroke
Patients at risk of hypercapnia? • COPD not all patients with COPD —elevated HCO 3 - on ABG is a useful clue to chronic CO 2 retention • Morbid obesity OHS and OSA • Neuromuscular weakness MND, myasthenia, GBS • Chest wall deformity kyphoscoliosis • Reduced conscious level • Morphine and other respiratory sedatives
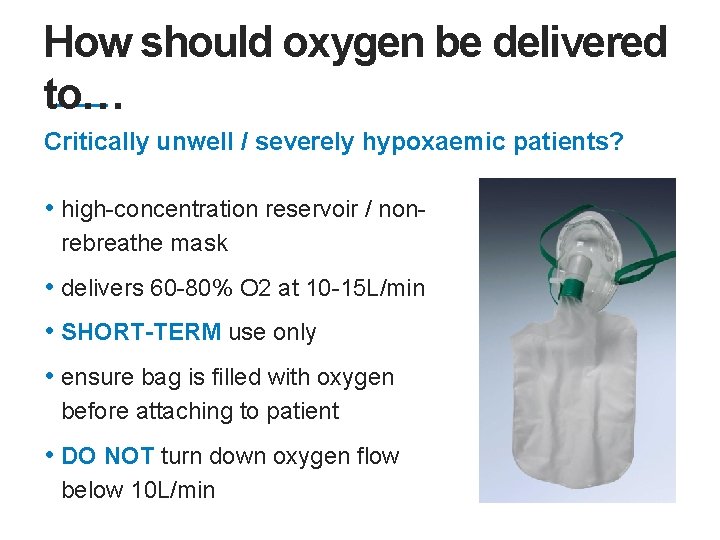
How should oxygen be delivered to… Critically unwell / severely hypoxaemic patients? • high-concentration reservoir / nonrebreathe mask • delivers 60 -80% O 2 at 10 -15 L/min • SHORT-TERM use only • ensure bag is filled with oxygen before attaching to patient • DO NOT turn down oxygen flow below 10 L/min
How should oxygen be delivered to… Most other patients? • nasal cannulae / specs • comfortable, well-tolerated, low -cost and no risk of rebreathing • 2 -6 L/min gives ~24 -50% oxygen • concentration actually delivered also depends on patient’s: patients with COPD tend to breath disproportionately more oxygen than air with every breath → risk of hypercapnia
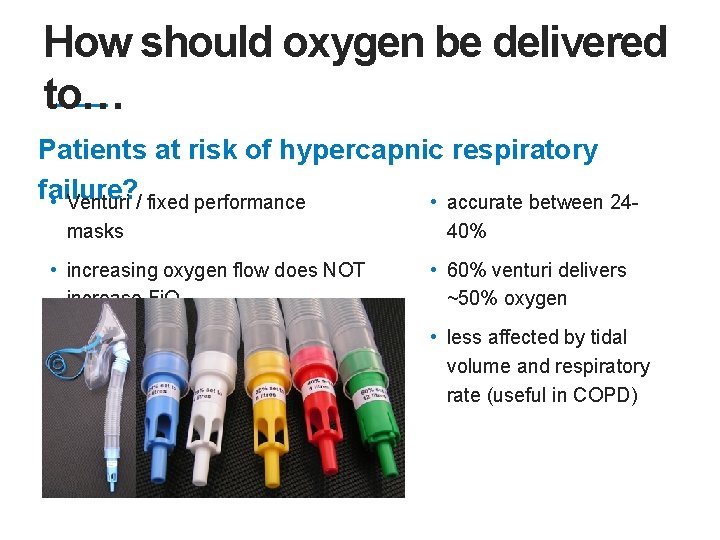
How should oxygen be delivered to… Patients at risk of hypercapnic respiratory failure? • Venturi / fixed performance • accurate between 24 masks • increasing oxygen flow does NOT increase Fi. O 2 40% • 60% venturi delivers ~50% oxygen • less affected by tidal volume and respiratory rate (useful in COPD)
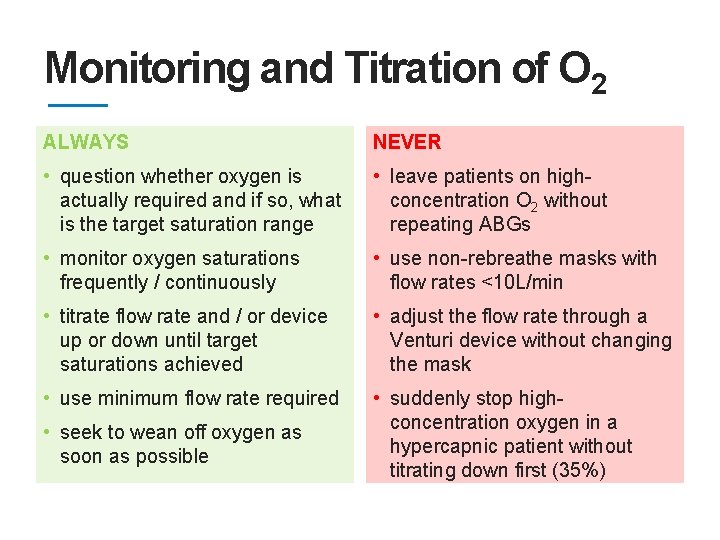
Monitoring and Titration of O 2 ALWAYS NEVER • question whether oxygen is • leave patients on high- actually required and if so, what is the target saturation range • monitor oxygen saturations frequently / continuously • titrate flow rate and / or device up or down until target saturations achieved • use minimum flow rate required • seek to wean off oxygen as soon as possible concentration O 2 without repeating ABGs • use non-rebreathe masks with flow rates <10 L/min • adjust the flow rate through a Venturi device without changing the mask • suddenly stop highconcentration oxygen in a hypercapnic patient without titrating down first (35%)
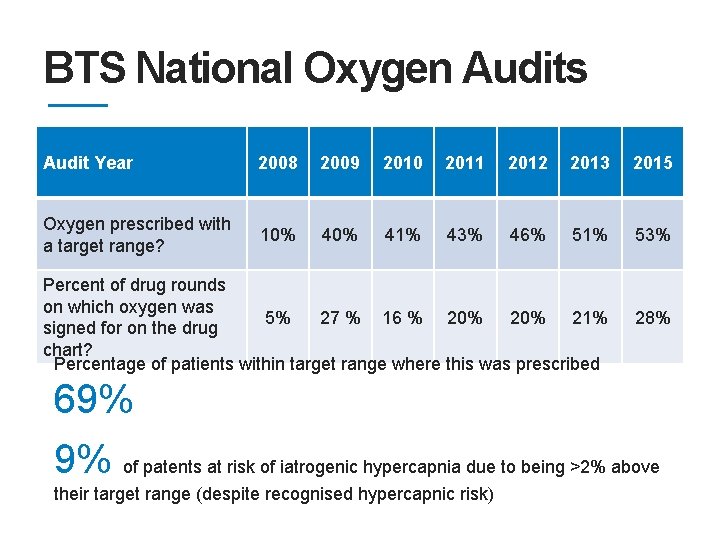
BTS National Oxygen Audits Audit Year 2008 2009 2010 2011 2012 2013 2015 Oxygen prescribed with a target range? 10% 41% 43% 46% 51% 53% Percent of drug rounds on which oxygen was 5% 27 % 16 % 20% 21% signed for on the drug chart? Percentage of patients within target range where this was prescribed 28% 69% 9% of patents at risk of iatrogenic hypercapnia due to being >2% above their target range (despite recognised hypercapnic risk)
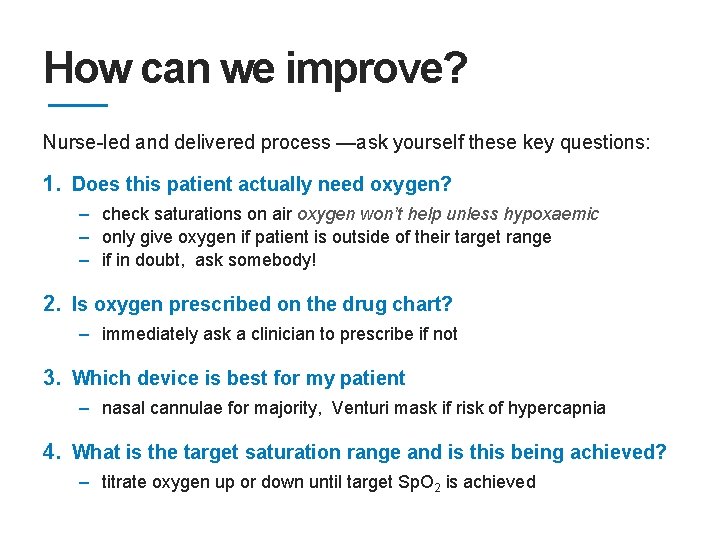
How can we improve? Nurse-led and delivered process —ask yourself these key questions: 1. Does this patient actually need oxygen? – check saturations on air oxygen won’t help unless hypoxaemic – only give oxygen if patient is outside of their target range – if in doubt, ask somebody! 2. Is oxygen prescribed on the drug chart? – immediately ask a clinician to prescribe if not 3. Which device is best for my patient – nasal cannulae for majority, Venturi mask if risk of hypercapnia 4. What is the target saturation range and is this being achieved? – titrate oxygen up or down until target Sp. O 2 is achieved
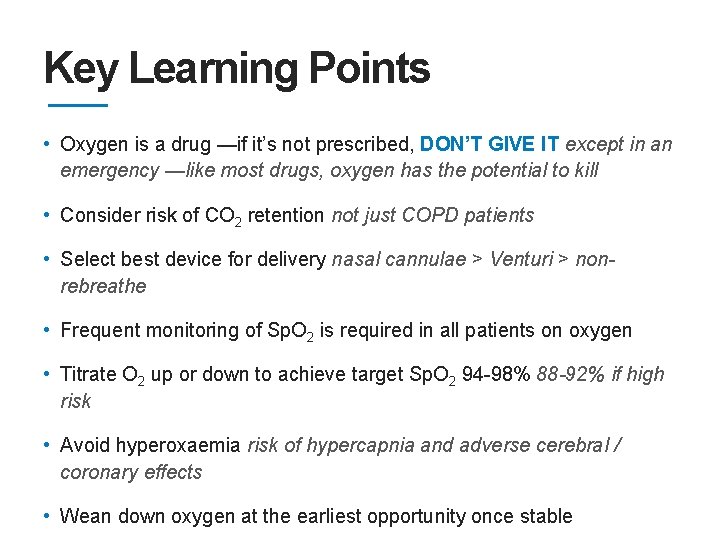
Key Learning Points • Oxygen is a drug —if it’s not prescribed, DON’T GIVE IT except in an emergency —like most drugs, oxygen has the potential to kill • Consider risk of CO 2 retention not just COPD patients • Select best device for delivery nasal cannulae > Venturi > nonrebreathe • Frequent monitoring of Sp. O 2 is required in all patients on oxygen • Titrate O 2 up or down to achieve target Sp. O 2 94 -98% 88 -92% if high risk • Avoid hyperoxaemia risk of hypercapnia and adverse cerebral / coronary effects • Wean down oxygen at the earliest opportunity once stable
- Slides: 17