Emergency Oxygen Administration 2012 EMS Safety Version A
- Slides: 80
Emergency Oxygen Administration © 2012 EMS Safety Version A
INTRODUCTION Emergency Oxygen Administration 2
What We Will Learn Today • Safe and effective administration of emergency oxygen • Definition of emergency oxygen • When & how to use it • Safe assembly and storage • Risks associated with oxygen delivery • Follow your local EMS authority or Medical Director’s guidelines • Always use standard or universal precautions according to your workplace and OSHA guidelines Emergency Oxygen Administration Introduction 3
Key Concepts • Every cell in the body needs oxygen (O 2) to live • In a medical emergency the body may inspire (inhale) or deliver lower levels of oxygen • Hypoxia (inadequate O 2) leads to organ and brain damage • Providing supplemental oxygen during an emergency may delay damage to vital organs Emergency Oxygen Administration Introduction 4
The Air We Breathe • Not made of 100% oxygen – – – Oxygen = 02 Made of several different gasses 21% oxygen 78% nitrogen 1% other elements • The body only uses about 5% of inhaled oxygen in atmosphere – 16% oxygen in our exhaled air – Enough to keep someone alive w/ rescue breaths for a short time O 2 Molecules! Emergency Oxygen Administration Introduction 5
Perfusion • Oxygen perfusion is when cells receive oxygen -rich blood • Depending on condition or emergency, the victim may be able to breathe but can’t perfuse oxygen • Emergency oxygen is a higher concentration of oxygen than the air we breathe • Emergency oxygen can increase oxygen concentrations in the lungs, which may allow more oxygen to be absorbed (perfused) into the bloodstream Emergency Oxygen Administration Introduction 6
COURSE OVERVIEW Emergency Oxygen Administration 7
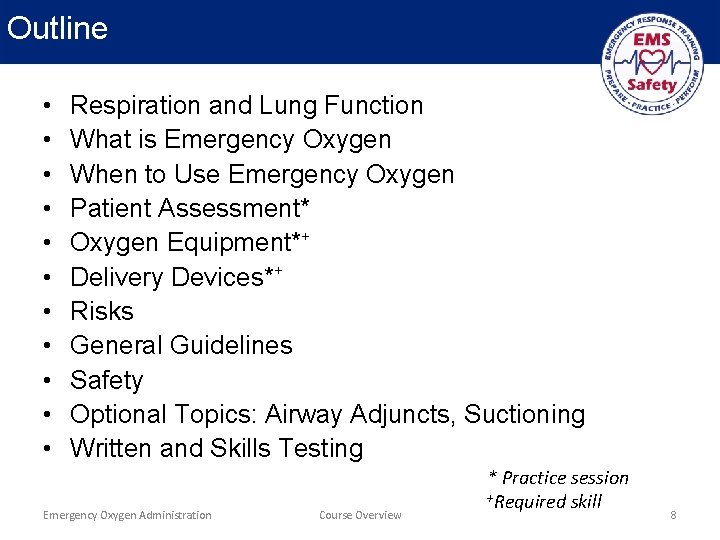
Outline • • • Respiration and Lung Function What is Emergency Oxygen When to Use Emergency Oxygen Patient Assessment* Oxygen Equipment*+ Delivery Devices*+ Risks General Guidelines Safety Optional Topics: Airway Adjuncts, Suctioning Written and Skills Testing Emergency Oxygen Administration Course Overview * Practice session +Required skill 8
Certification Requirements • Participate in entire course • Complete all practice sessions • Pass written exam with minimum score of 80% • Pass skills exam Emergency Oxygen Administration Course Overview 9
Respiration: The exchange of carbon dioxide for oxygen RESPIRATION & LUNG FUNCTION Emergency Oxygen Administration 10
Respiration & Ventilation • Respiration – Exchange of carbon dioxide (CO 2), the waste product from breathing, with fresh air from the atmosphere • Ventilation – Moving air in and out of the lungs for respiration • Alveoli – – – Where the exchange of O 2 and CO 2 is accomplished Small air sacs in the lower lobes of right and left lungs Shaped like miniature broccoli stems Intertwined with capillaries Exchange of O 2 and CO 2 occurs through fenestrations (tiny holes) along the alveoli and capillary beds Emergency Oxygen Administration Respiration & Lung Function 11
Blood Flow for Respiration • Deoxygenated blood – Pumped from right ventricle of heart to lungs – Down into alveoli – O 2/CO 2 exchanged • Newly-oxygenated blood – Pumped back to left side of heart – Out to the rest of the body Emergency Oxygen Administration Respiration and Lung Function 12
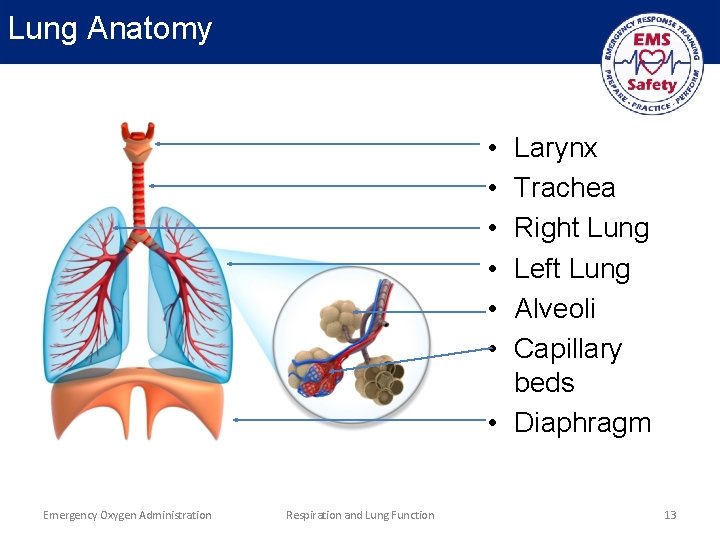
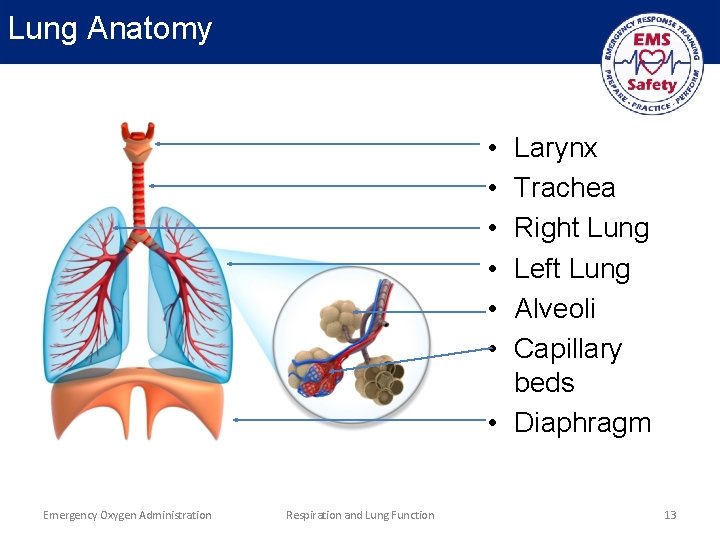
Lung Anatomy • • • Larynx Trachea Right Lung Left Lung Alveoli Capillary beds • Diaphragm Emergency Oxygen Administration Respiration and Lung Function 13
WHAT IS EMERGENCY OXYGEN Emergency Oxygen Administration 14
Emergency Oxygen is a Compressed Gas • Classified as a drug • Regulated by the FDA • 100% pure oxygen stored in a cylinder • Categorized as either ‘Medical Oxygen’ or ‘Emergency Oxygen’ • Rescuers must be trained in use and storage of oxygen Emergency Oxygen Administration What is Emergency Oxygen 15
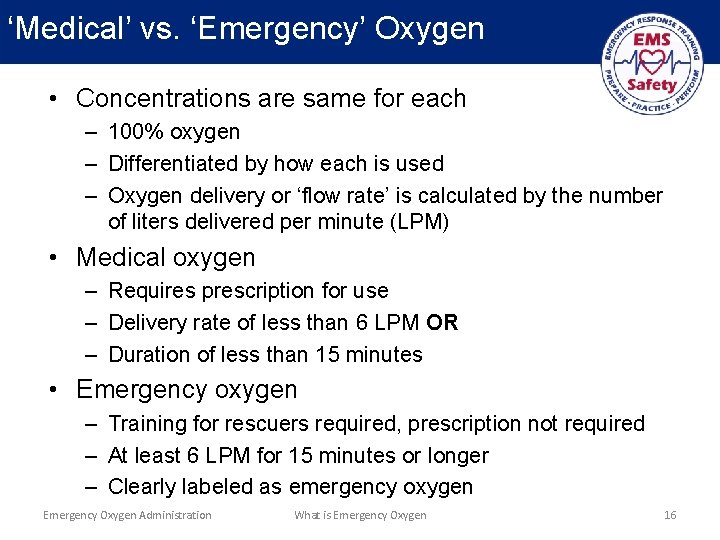
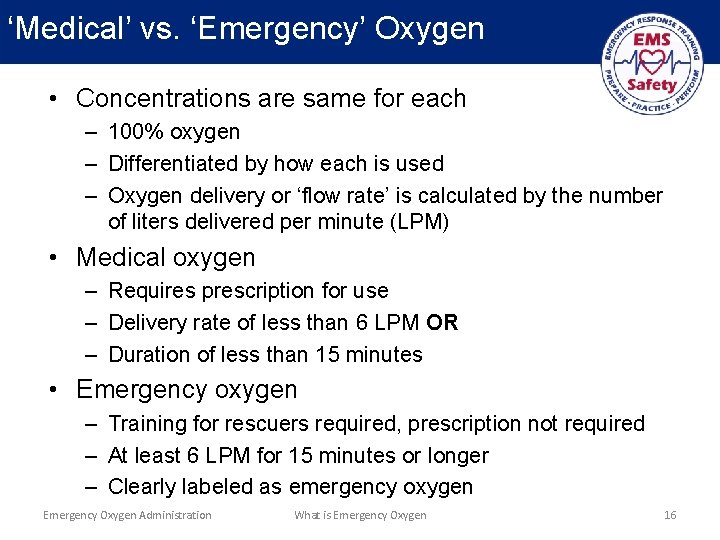
‘Medical’ vs. ‘Emergency’ Oxygen • Concentrations are same for each – 100% oxygen – Differentiated by how each is used – Oxygen delivery or ‘flow rate’ is calculated by the number of liters delivered per minute (LPM) • Medical oxygen – Requires prescription for use – Delivery rate of less than 6 LPM OR – Duration of less than 15 minutes • Emergency oxygen – Training for rescuers required, prescription not required – At least 6 LPM for 15 minutes or longer – Clearly labeled as emergency oxygen Emergency Oxygen Administration What is Emergency Oxygen 16
How and when emergency oxygen is used varies between Professional and Citizen rescuers. Always follow state and local protocols regarding when and how to use emergency oxygen. WHEN TO USE EMERGENCY OXYGEN Emergency Oxygen Administration 17
Why Use Emergency Oxygen? • Primary use: – Correct mild - moderate hypoxia (inadequate oxygen to organs and tissues) – Reduce the work of the heart • Use to treat breathing difficulty based on – Patient’s condition – Respiratory rates • Professional rescuers and healthcare providers may use emergency oxygen to treat signs and symptoms of certain suspected medical conditions. Emergency Oxygen Administration When to Use Emergency Oxygen 18
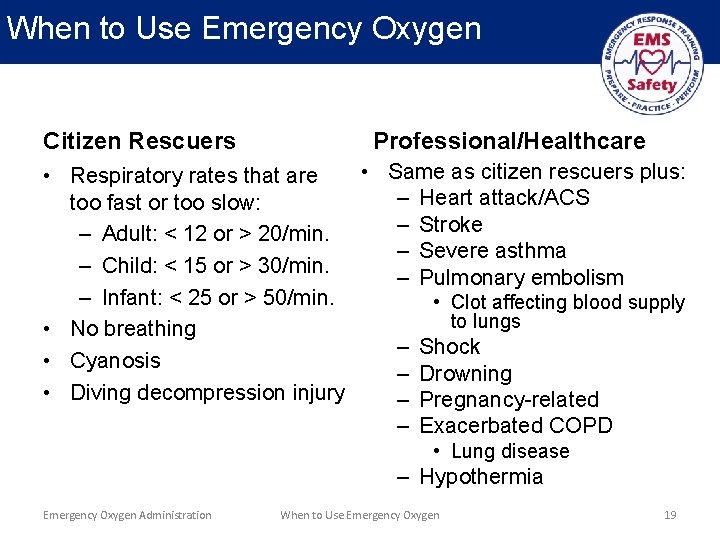
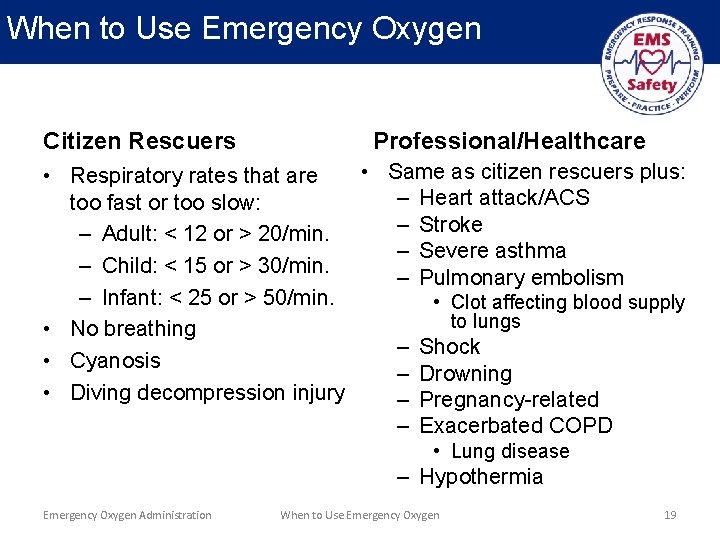
When to Use Emergency Oxygen Citizen Rescuers Professional/Healthcare • Same as citizen rescuers plus: • Respiratory rates that are – Heart attack/ACS too fast or too slow: – Stroke – Adult: < 12 or > 20/min. – Severe asthma – Child: < 15 or > 30/min. – Pulmonary embolism – Infant: < 25 or > 50/min. • Clot affecting blood supply to lungs • No breathing – Shock • Cyanosis – Drowning • Diving decompression injury – Pregnancy-related – Exacerbated COPD • Lung disease – Hypothermia Emergency Oxygen Administration When to Use Emergency Oxygen 19
Never Delay Critical Care! • The use of emergency oxygen should not delay life-saving treatments – Calling 9 -1 -1 – Applying direct pressure on a bleeding wound – Starting chest compressions • Only use emergency oxygen after – EMS (9 -1 -1) has been activated – Additional trained rescuers available to use emergency oxygen without interrupting life-saving activities Emergency Oxygen Administration When to Use Emergency Oxygen 20
PATIENT ASSESSMENT Emergency Oxygen Administration 21
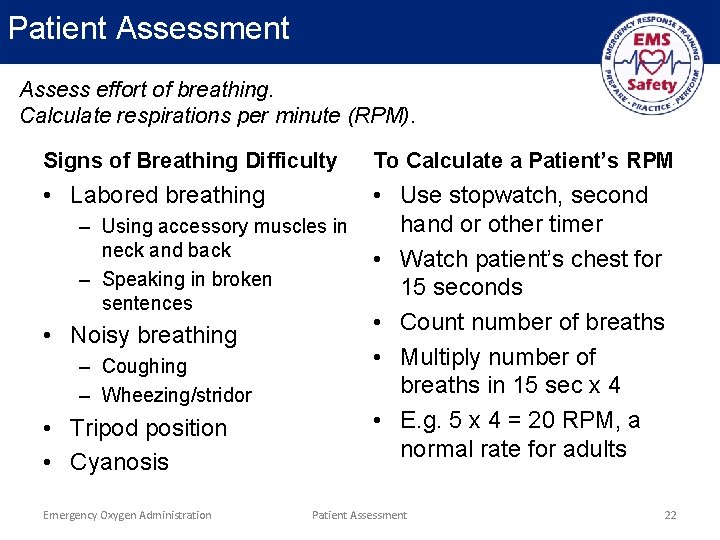
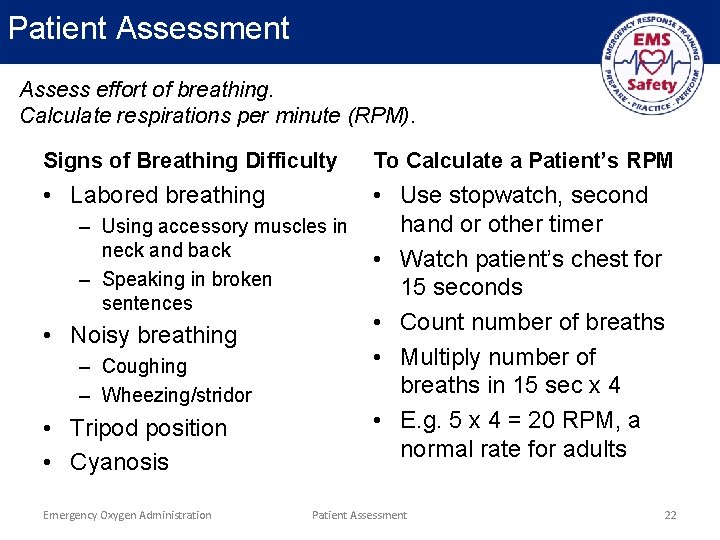
Patient Assessment Assess effort of breathing. Calculate respirations per minute (RPM). Signs of Breathing Difficulty To Calculate a Patient’s RPM • Labored breathing • Use stopwatch, second hand or other timer • Watch patient’s chest for 15 seconds • Count number of breaths • Multiply number of breaths in 15 sec x 4 • E. g. 5 x 4 = 20 RPM, a normal rate for adults – Using accessory muscles in neck and back – Speaking in broken sentences • Noisy breathing – Coughing – Wheezing/stridor • Tripod position • Cyanosis Emergency Oxygen Administration Patient Assessment 22
Demo/Practice Session 1 • Skill Demonstration: Patient Assessment • Skill Practice: Patient Assessment • Instructions – – Use Practice Sheet Demonstrate skill, answer questions Each student practices skill(s) Use skill sheet to review areas for improvement Emergency Oxygen Administration Patient Assessment 23
Emergency oxygen is delivered from a cylinder, through a pressure regulator and oxygen tubing, and into a delivery device such as a mask, cannula or bag mask… OXYGEN EQUIPMENT Emergency Oxygen Administration 24
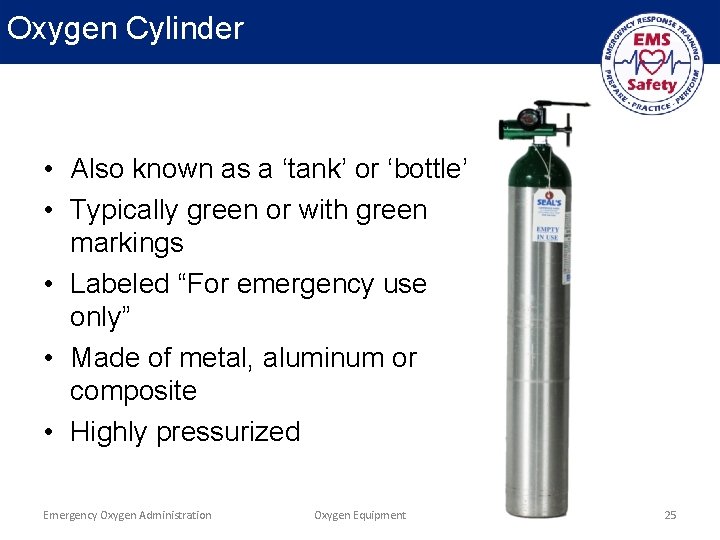
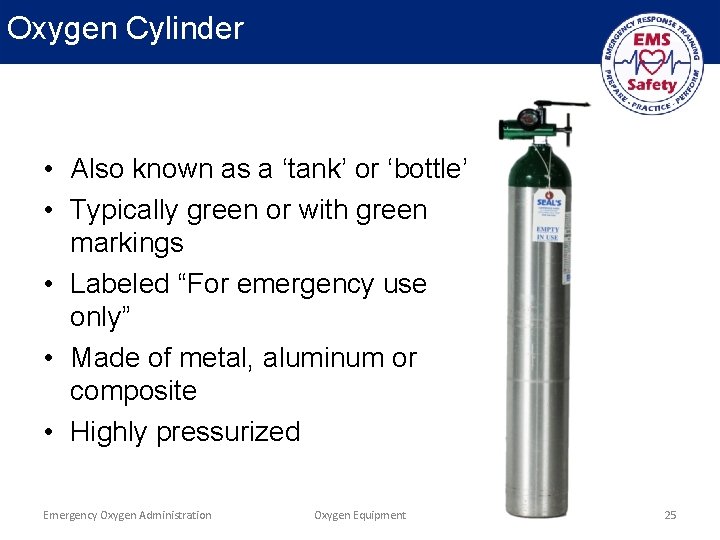
Oxygen Cylinder • Also known as a ‘tank’ or ‘bottle’ • Typically green or with green markings • Labeled “For emergency use only” • Made of metal, aluminum or composite • Highly pressurized Emergency Oxygen Administration Oxygen Equipment 25
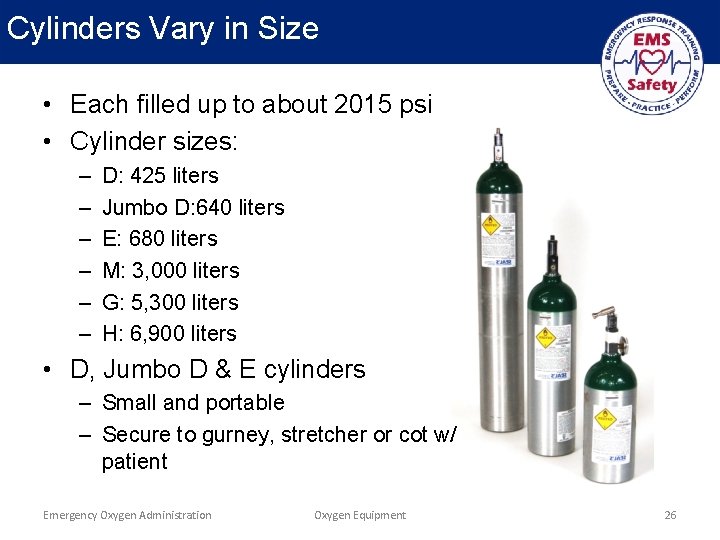
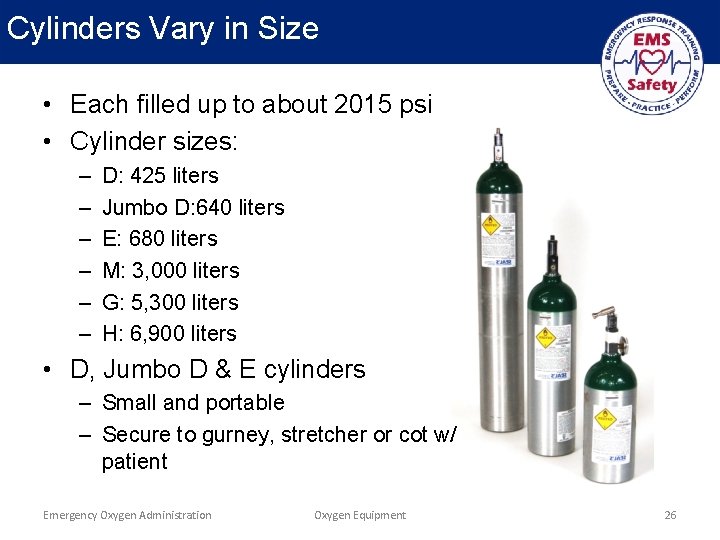
Cylinders Vary in Size • Each filled up to about 2015 psi • Cylinder sizes: – – – D: 425 liters Jumbo D: 640 liters E: 680 liters M: 3, 000 liters G: 5, 300 liters H: 6, 900 liters • D, Jumbo D & E cylinders – Small and portable – Secure to gurney, stretcher or cot w/ patient Emergency Oxygen Administration Oxygen Equipment 26
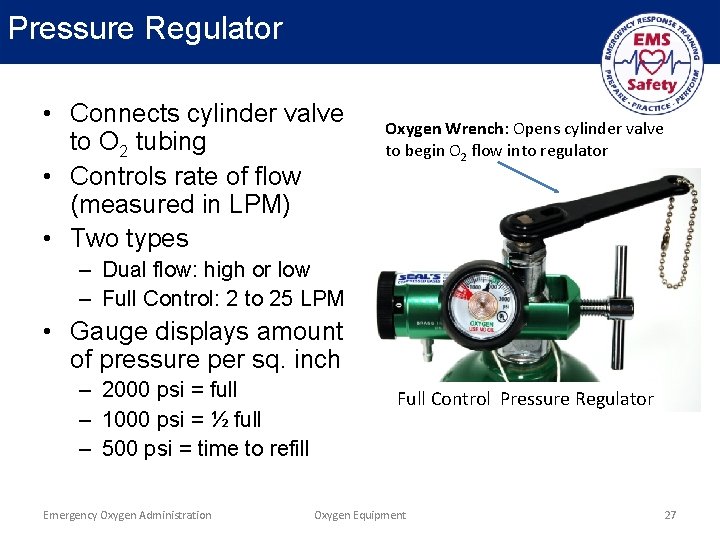
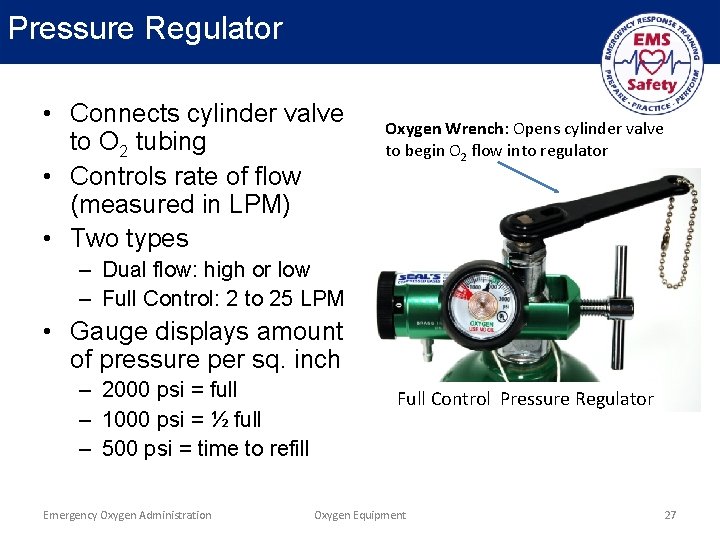
Pressure Regulator • Connects cylinder valve to O 2 tubing • Controls rate of flow (measured in LPM) • Two types Oxygen Wrench: Opens cylinder valve to begin O 2 flow into regulator – Dual flow: high or low – Full Control: 2 to 25 LPM • Gauge displays amount of pressure per sq. inch – 2000 psi = full – 1000 psi = ½ full – 500 psi = time to refill Emergency Oxygen Administration Full Control Pressure Regulator Oxygen Equipment 27
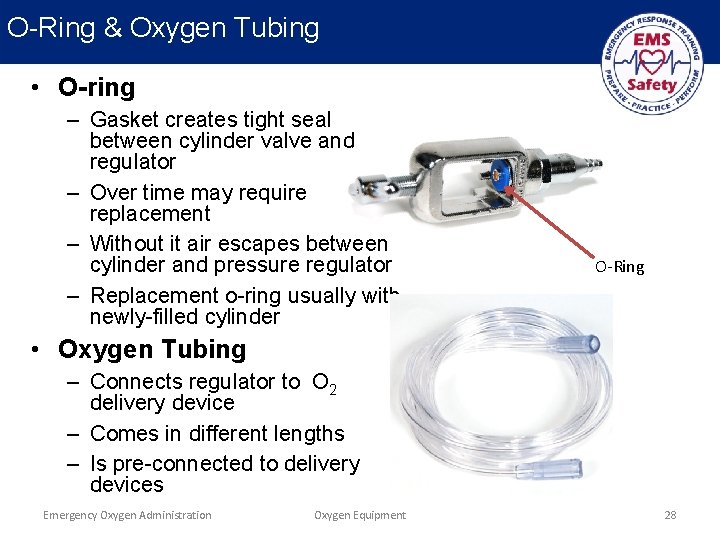
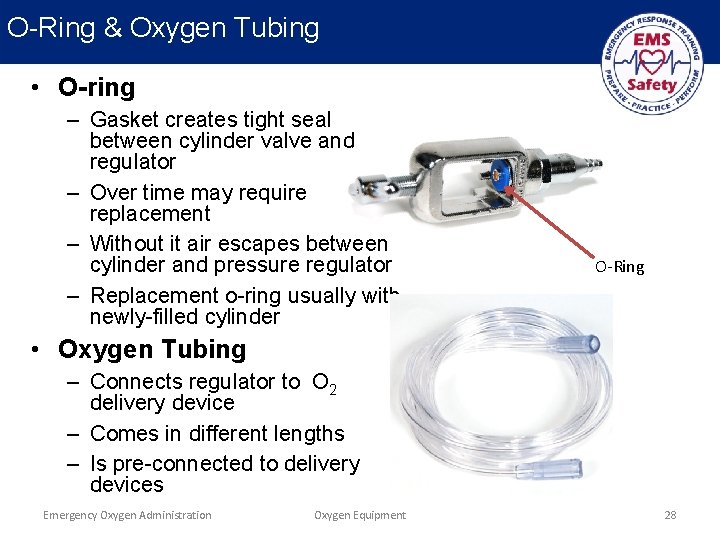
O-Ring & Oxygen Tubing • O-ring – Gasket creates tight seal between cylinder valve and regulator – Over time may require replacement – Without it air escapes between cylinder and pressure regulator – Replacement o-ring usually with newly-filled cylinder O-Ring • Oxygen Tubing – Connects regulator to O 2 delivery device – Comes in different lengths – Is pre-connected to delivery devices Emergency Oxygen Administration Oxygen Equipment 28
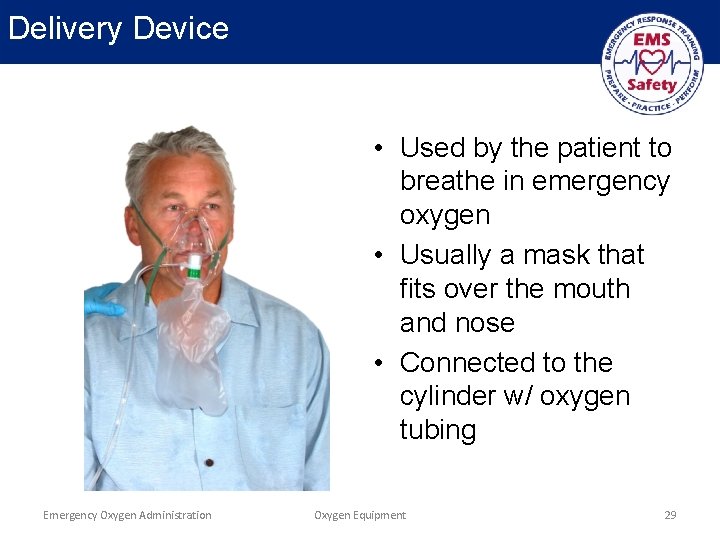
Delivery Device • Used by the patient to breathe in emergency oxygen • Usually a mask that fits over the mouth and nose • Connected to the cylinder w/ oxygen tubing Emergency Oxygen Administration Oxygen Equipment 29
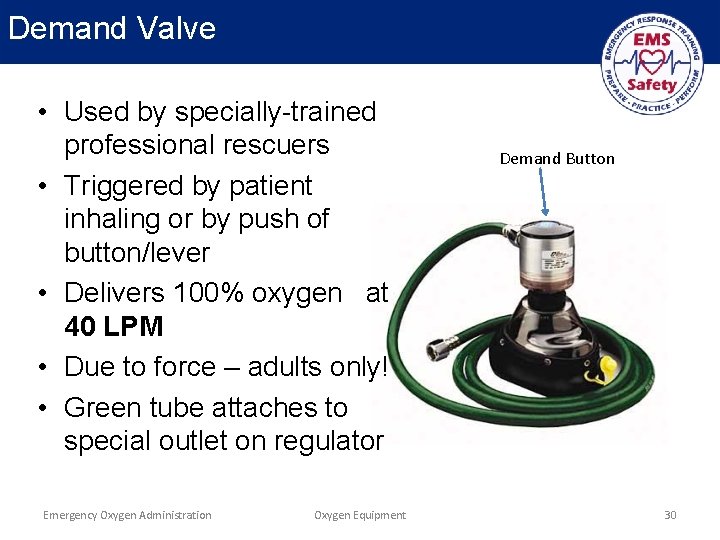
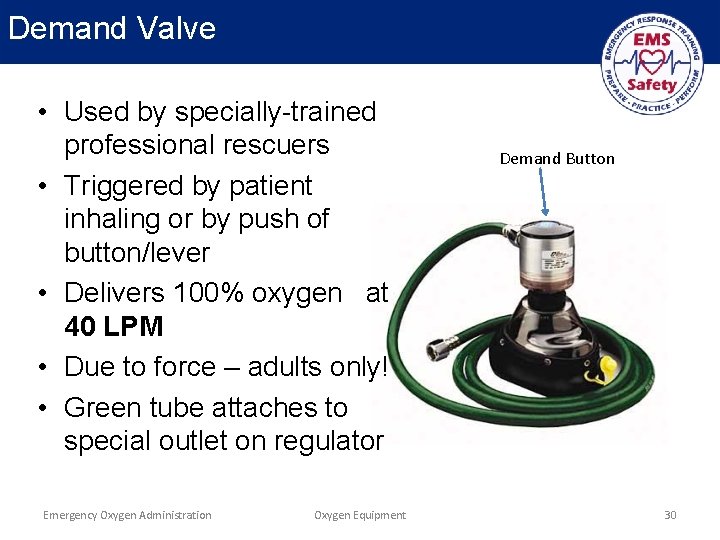
Demand Valve • Used by specially-trained professional rescuers • Triggered by patient inhaling or by push of button/lever • Delivers 100% oxygen at 40 LPM • Due to force – adults only! • Green tube attaches to special outlet on regulator Emergency Oxygen Administration Oxygen Equipment Demand Button 30
Oxygen Humidifier • Not typically used in emergency settings • Supplemental O 2 can dry out mucous membranes of the nose • Dryness causes irritation and possible nosebleed • Humidifier passes O 2 through sterile water • O 2 picks up tiny water molecules, reduces dryness & irritation Emergency Oxygen Administration Oxygen Equipment 31
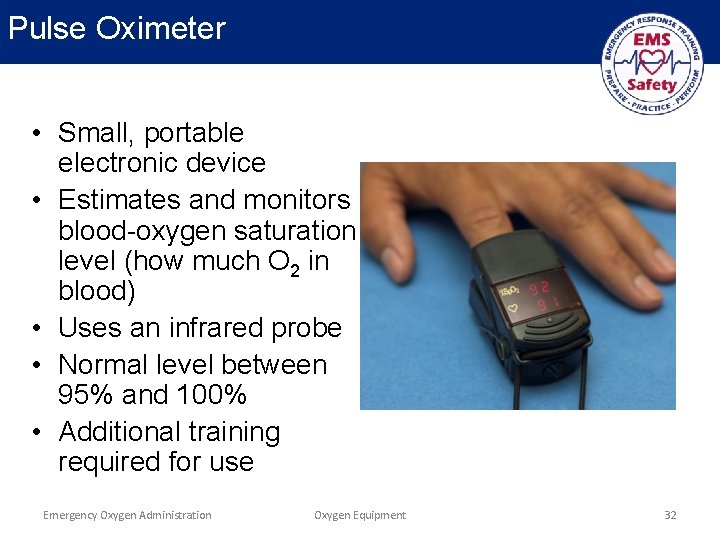
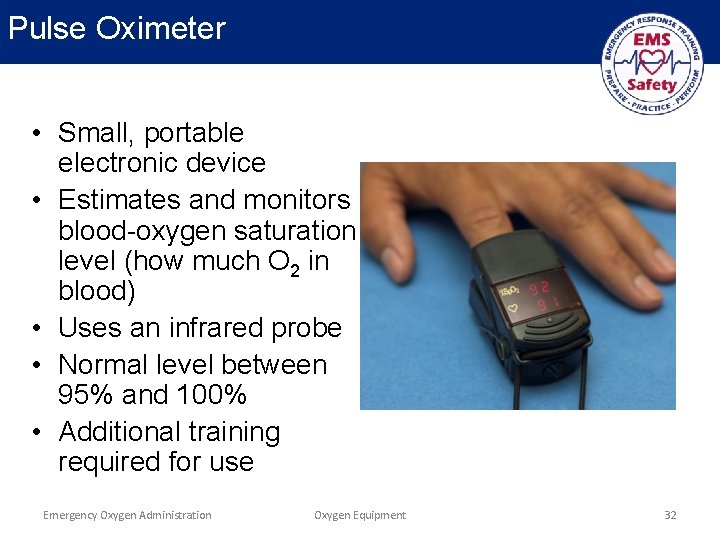
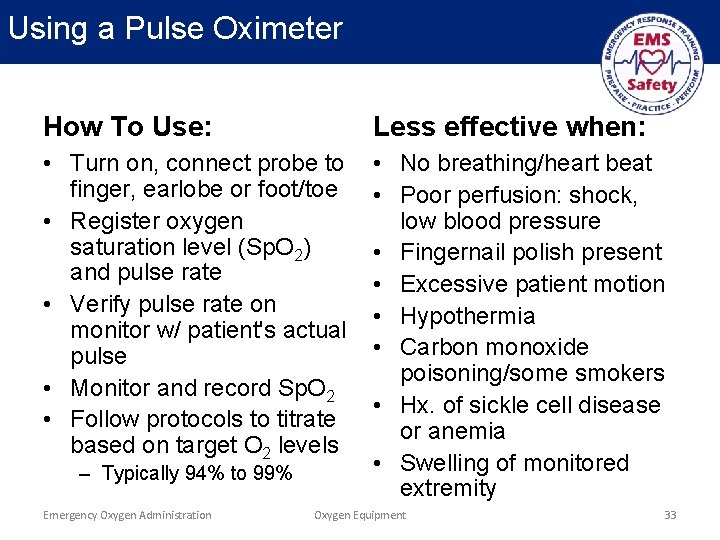
Pulse Oximeter • Small, portable electronic device • Estimates and monitors blood-oxygen saturation level (how much O 2 in blood) • Uses an infrared probe • Normal level between 95% and 100% • Additional training required for use Emergency Oxygen Administration Oxygen Equipment 32
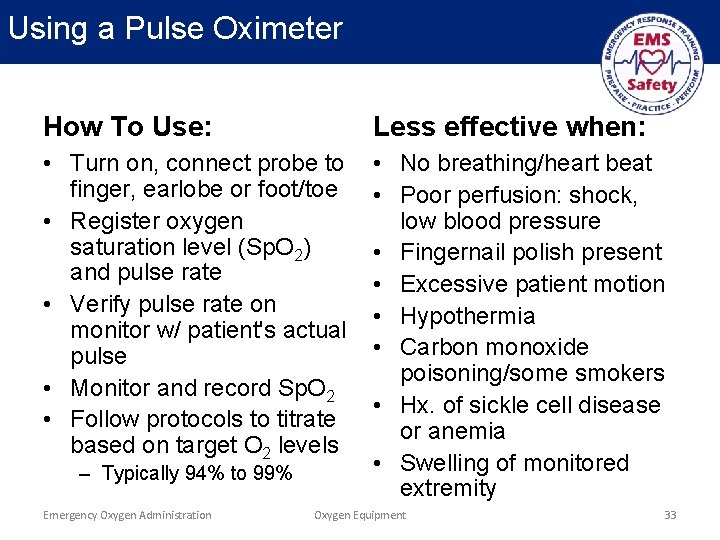
Using a Pulse Oximeter How To Use: Less effective when: • Turn on, connect probe to finger, earlobe or foot/toe • Register oxygen saturation level (Sp. O 2) and pulse rate • Verify pulse rate on monitor w/ patient's actual pulse • Monitor and record Sp. O 2 • Follow protocols to titrate based on target O 2 levels • No breathing/heart beat • Poor perfusion: shock, low blood pressure • Fingernail polish present • Excessive patient motion • Hypothermia • Carbon monoxide poisoning/some smokers • Hx. of sickle cell disease or anemia • Swelling of monitored extremity – Typically 94% to 99% Emergency Oxygen Administration Oxygen Equipment 33
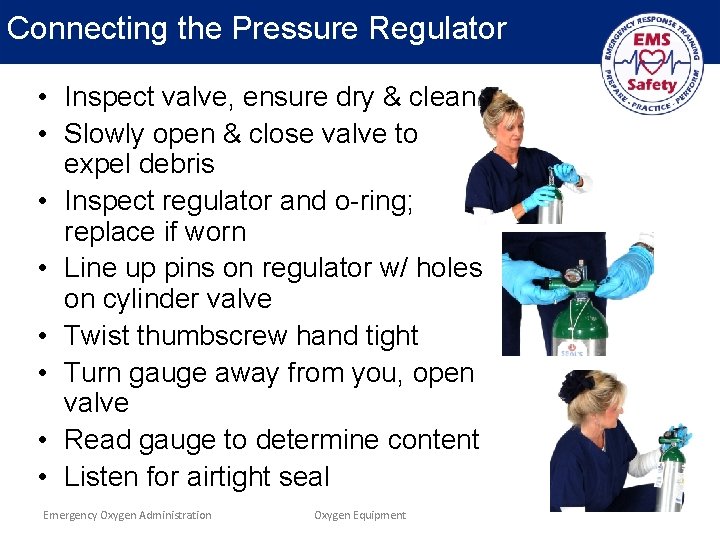
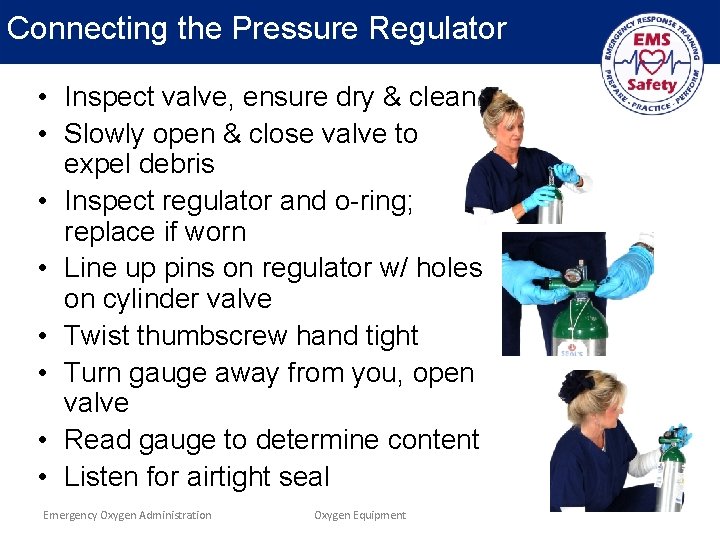
Connecting the Pressure Regulator • Inspect valve, ensure dry & clean • Slowly open & close valve to expel debris • Inspect regulator and o-ring; replace if worn • Line up pins on regulator w/ holes on cylinder valve • Twist thumbscrew hand tight • Turn gauge away from you, open valve • Read gauge to determine content • Listen for airtight seal Emergency Oxygen Administration Oxygen Equipment 34
Demo/Practice Session 2 • Skill Demonstration: Connect Pressure Regulator • Skill Practice: Connect Pressure Regulator • Instructions – – Use Practice Sheet Demonstrate skill, answer questions Each student practices skill(s) Use skill sheet to review areas for improvement Emergency Oxygen Administration Oxygen Equipment 35
The delivery device is connected to oxygen tubing, then attached to the nipple of the pressure regulator. DELIVERY DEVICES Emergency Oxygen Administration 36
Key Concepts • There are four basic types – – Non-rebreather mask Nasal cannula Bag mask CPR face mask w/ oxygen inlet • The non-rebreather and nasal cannula are for victims who are breathing on their own • Different sizes of delivery devices are available for adult, child and infant patients Emergency Oxygen Administration Delivery Devices 37
Non-Rebreather Mask • ‘High-flow’ device • Consists of mask, O 2 reservoir and tubing • Delivers oxygen concentrations between 90%-100% with each breath • Use 15 LPM Emergency Oxygen Administration Delivery Devices 38
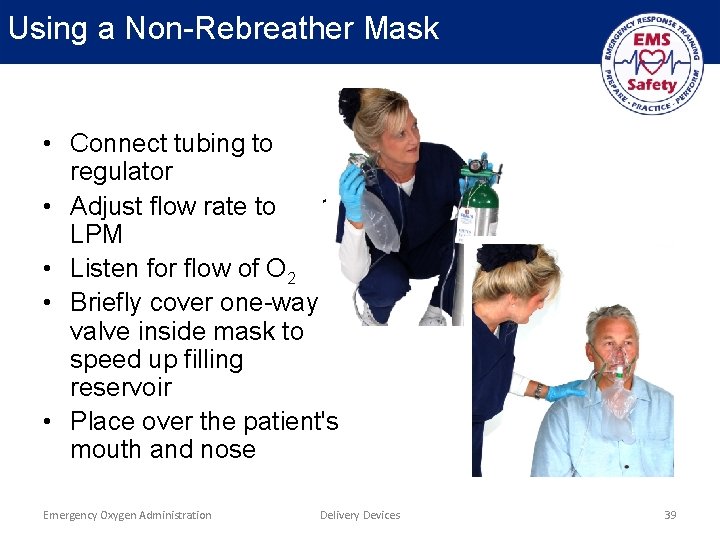
Using a Non-Rebreather Mask • Connect tubing to regulator • Adjust flow rate to 15 LPM • Listen for flow of O 2 • Briefly cover one-way valve inside mask to speed up filling reservoir • Place over the patient's mouth and nose Emergency Oxygen Administration Delivery Devices 39
Tolerating a Non-Rebreather Mask • The mask will completely cover the mouth & nose, which can make it intolerable for some • Patient may complain that flow of O 2 is restricted, even though they are getting more than 90% O 2 • Ensure flow rate is at least 15 LPM, oxygen is flowing and the reservoir is inflated • Rescuers may have to ‘coach’ a patient – Help get used to mask – Reassure they are getting more oxygen than normal Emergency Oxygen Administration Delivery Devices 40
Nasal Cannula • A low-flow device • Provides between 2 - 6 LPM • Max concentration delivered: 44% O 2 • Consists of loop of oxygen tubing, two prongs for the nostrils and an adjusting band Emergency Oxygen Administration Delivery Devices 41
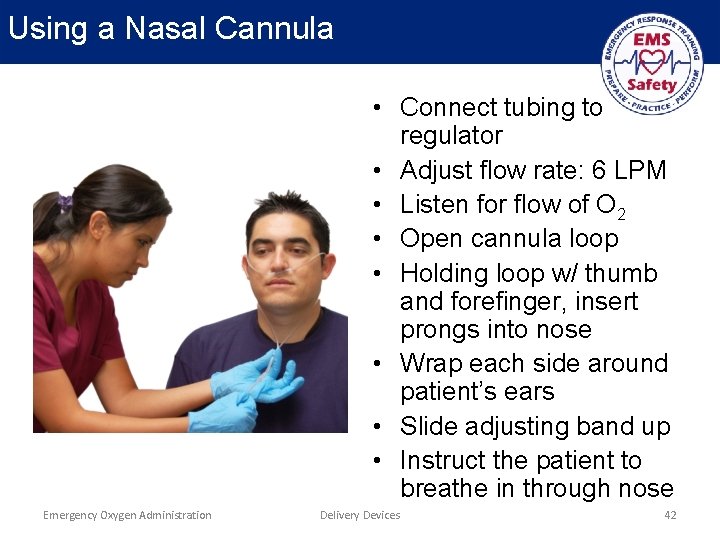
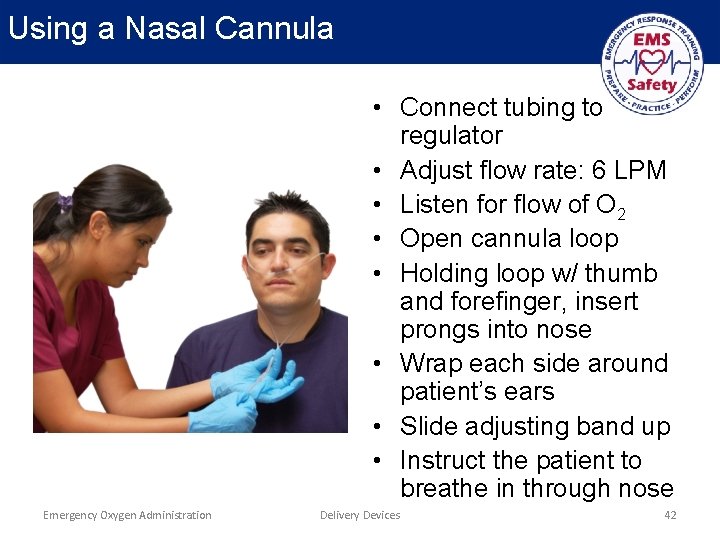
Using a Nasal Cannula • Connect tubing to regulator • Adjust flow rate: 6 LPM • Listen for flow of O 2 • Open cannula loop • Holding loop w/ thumb and forefinger, insert prongs into nose • Wrap each side around patient’s ears • Slide adjusting band up • Instruct the patient to breathe in through nose Emergency Oxygen Administration Delivery Devices 42
Bag Mask • Also known as Bag Valve Mask or BVM • Used for rescue breathing/CPR • Delivers nearly 100% oxygen • May reduce exposure to pathogens • Requires additional training to be used effectively Emergency Oxygen Administration Delivery Devices 43
Using a Bag Mask • May be used with or without oxygen • Science does not support or refute the use of oxygen during resuscitation • Risks related to over-exposure to oxygen are low; it is reasonable to use oxygen during resuscitation • Never delay resuscitation efforts in order to use emergency oxygen • The use of emergency oxygen does not change how rescue breaths are delivered with a bag mask Emergency Oxygen Administration Delivery Devices 44
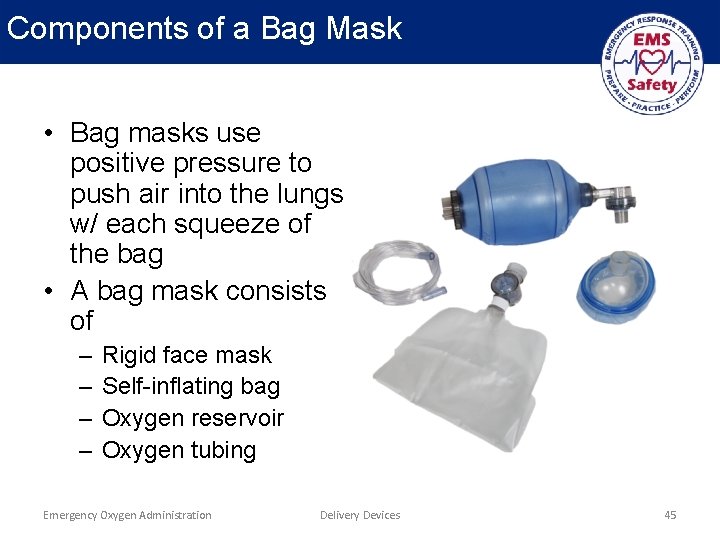
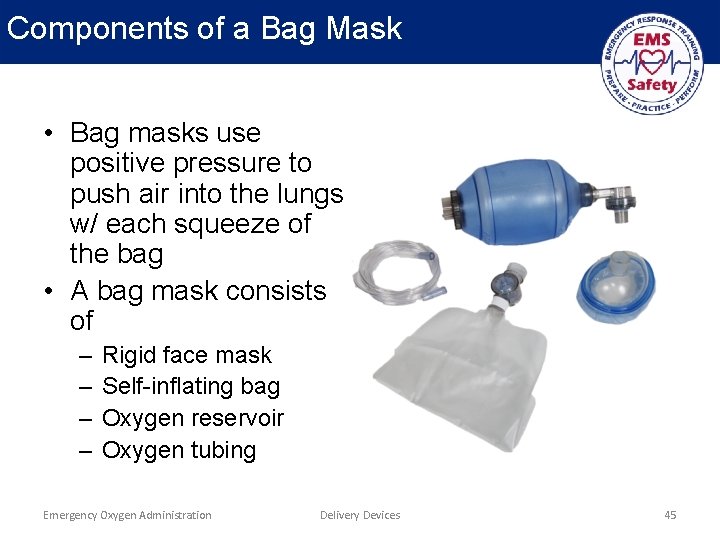
Components of a Bag Mask • Bag masks use positive pressure to push air into the lungs w/ each squeeze of the bag • A bag mask consists of – – Rigid face mask Self-inflating bag Oxygen reservoir Oxygen tubing Emergency Oxygen Administration Delivery Devices 45
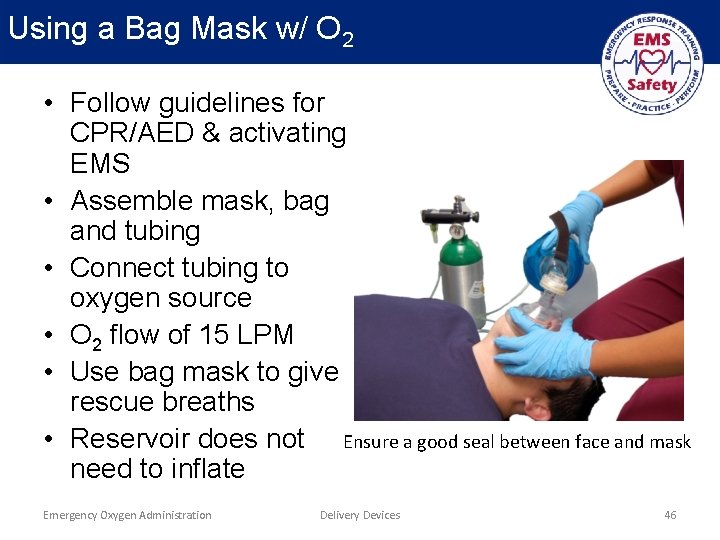
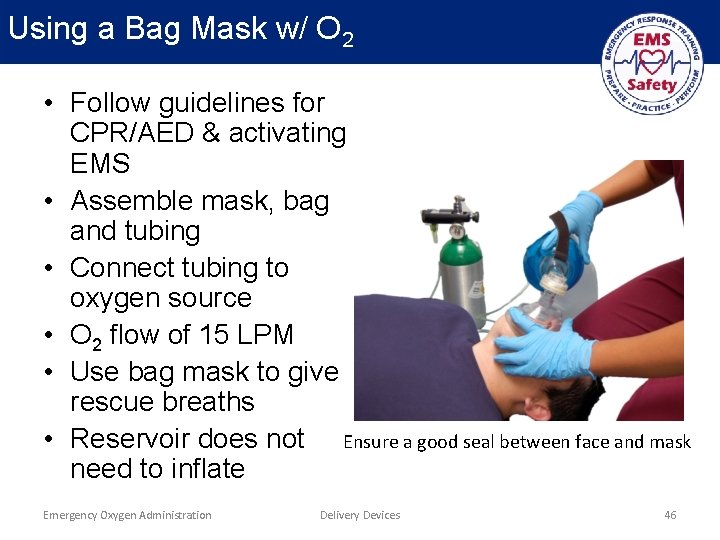
Using a Bag Mask w/ O 2 • Follow guidelines for CPR/AED & activating EMS • Assemble mask, bag and tubing • Connect tubing to oxygen source • O 2 flow of 15 LPM • Use bag mask to give rescue breaths • Reservoir does not Ensure a good seal between face and mask need to inflate Emergency Oxygen Administration Delivery Devices 46
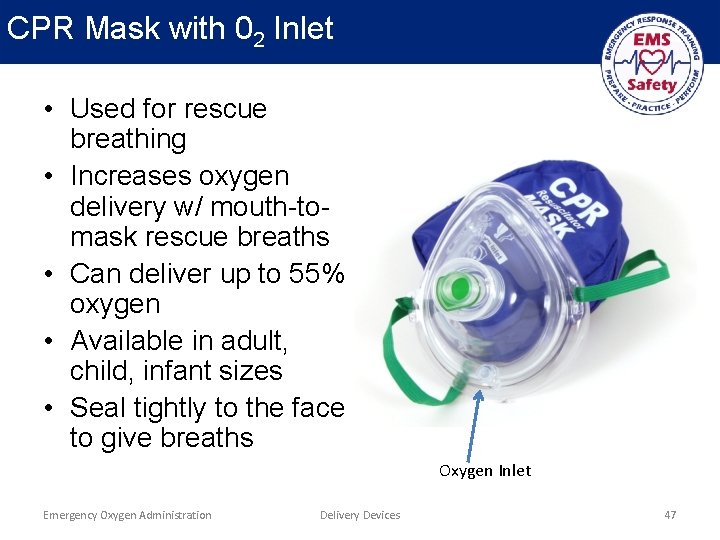
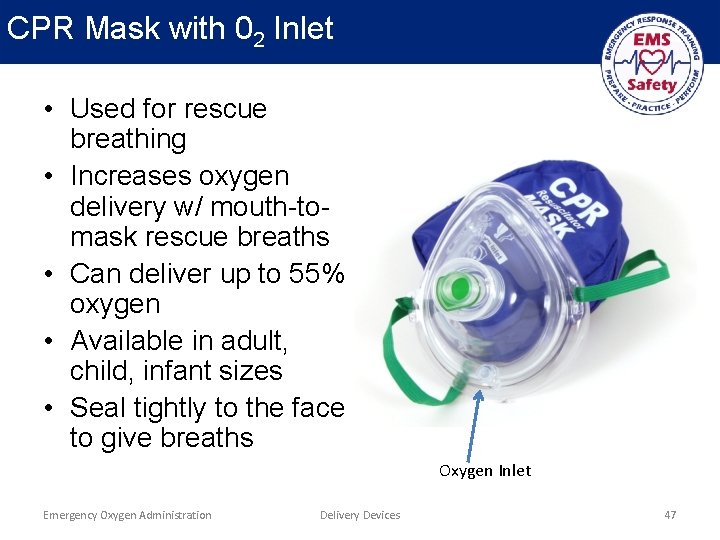
CPR Mask with 02 Inlet • Used for rescue breathing • Increases oxygen delivery w/ mouth-tomask rescue breaths • Can deliver up to 55% oxygen • Available in adult, child, infant sizes • Seal tightly to the face to give breaths Oxygen Inlet Emergency Oxygen Administration Delivery Devices 47
Using a CPR Face Mask w/ Oxygen • • Follow guidelines for CPR/AED & activating EMS Assemble mask Insert tubing into oxygen inlet on mask Connect tubing to oxygen source O 2 flow of 15 LPM Press mask firmly to the face and open airway Breathe into mask and watch for chest rise Emergency Oxygen Administration Delivery Devices 48
Bag Mask & CPR Face Mask • Can be used for resuscitation, or to provide emergency oxygen to a victim who is conscious or semi-conscious but breathing abnormally • Bag Mask – Maintain flow rate of 15 LPM – Have victim hold to his/her face if able – Assist abnormal rates as needed: • Less than 10 RPM: Squeeze bag between each breath • Greater than 30 RPM: Squeeze bag every second breath • CPR Face Mask – Use 6 -15 LPM – Have patient hold mask to his/her face Emergency Oxygen Administration Delivery Devices 49
Selecting a Delivery Device • Regulator Type Impacts Delivery Device • Full control regulator (2 -25 LPM) – Any type mask acceptable – Dial in proper LPM according to device • Dual flow: high or low – Low-flow setting • Nasal cannula • CPR face mask (for patient is who is breathing) – High-flow setting • Non-rebreather mask • Bag mask • CPR face mask (for breathing or non-breathing patient) Emergency Oxygen Administration Delivery Devices 50
“Blow By” Oxygen Delivery • For infants and small children who can’t tolerate a mask or cannula • Use an oxygen mask and a high flow rate (at least 15 LPM) • Keep mask about 2 inches from patient's face • Wave mask slowly from side-to-side • Allows oxygen to pass over patient's mouth and nose to be inhaled Emergency Oxygen Administration Delivery Devices 51
Demo/Practice Session 3 • Skill Demonstration: Delivery Devices • Skill Practice: Delivery Devices • Instructions – – Use Practice Sheet Demonstrate skill, answer questions Each student practices skill(s) Use skill sheet to review areas for improvement Emergency Oxygen Administration Delivery Devices 52
RISKS ASSOCIATED W/ OXYGEN DELIVERY Emergency Oxygen Administration 53
Risks of Oxygen Delivery • Potential risks related to oxygen delivery – – Oxygen Toxicity Retinopathy of Prematurity Denitrogenation COPD and the Hypoxic Drive Emergency Oxygen Administration Oxygen Risks 54
Oxygen Toxicity • Occurs when there is too much oxygen in the blood • Caused by prolonged exposure to high concentrations of oxygen • Usually after 24 hours or more • Emergency oxygen is usually not administered long enough to cause oxygen toxicity, and is generally not a concern in the field • Signs/symptoms: visual changes, ringing in ears, twitching, irritability, dizziness, seizure Emergency Oxygen Administration Oxygen Risks 55
Retinopathy of Prematurity • Retinopathy of prematurity only occurs in premature infants • The retinas are immature before 34 weeks gestation, and can be damaged by high concentrations of oxygen • It is not a problem associated with the normal use of emergency oxygen Emergency Oxygen Administration Oxygen Risks 56
Denitrogenation • Also known as Absorption Atelectasis • Occurs when naturally-occurring nitrogen in the lungs is replaced with oxygen from over-saturation • Oxygen shares alveolar space with nitrogen • If the nitrogen is ‘washed out’ by too much O 2, the alveoli collapse • Can severely impair lung function (process known as atelectasis) • Not usually associated with emergency oxygen delivery because exposure to high concentrations of oxygen is limited to a relatively short period Emergency Oxygen Administration Oxygen Risks 57
COPD and Hypoxic Drive • ‘Hypoxic drive’ is condition associated w/ COPD – Normally, body stimulated to breathe when too much carbon dioxide is detected – COPD patients stimulated to breathe by lower O 2 levels and to NOT breathe with higher O 2 levels – Concern that emergency oxygen can eliminate the hypoxic drive of a COPD patient, causing person to stop breathing • General rule: – Always give emergency O 2 if indicated (even if history of COPD) – Difficulty breathing may be related to a condition other than COPD • Hypoxic drive is rare; do not withhold emergency O 2 Emergency Oxygen Administration Oxygen Risks 58
GENERAL GUIDELINES FOR EMERGENCY OXYGEN DELIVERY Emergency Oxygen Administration 59
General Guidelines • Guidelines for the delivery of emergency O 2 include the following: – – Monitor delivery Understand the use of oxygen in resuscitation Train emergency responders Follow federal, state and local regulations Emergency Oxygen Administration Guidelines for Oxygen Delivery 60
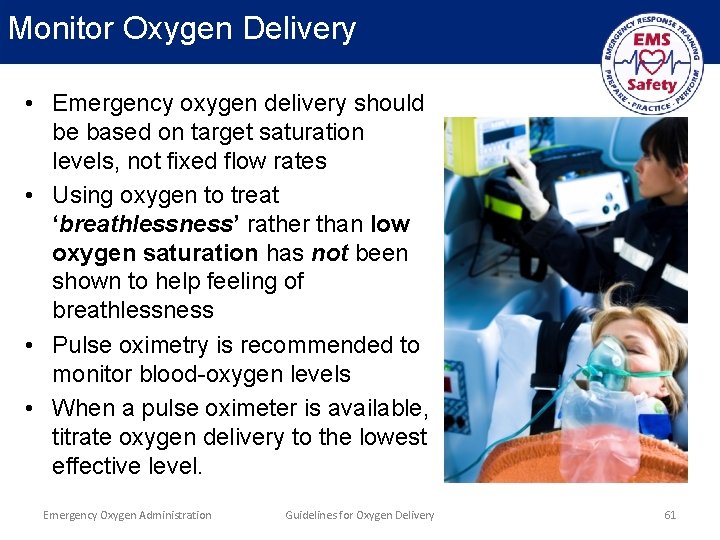
Monitor Oxygen Delivery • Emergency oxygen delivery should be based on target saturation levels, not fixed flow rates • Using oxygen to treat ‘breathlessness’ rather than low oxygen saturation has not been shown to help feeling of breathlessness • Pulse oximetry is recommended to monitor blood-oxygen levels • When a pulse oximeter is available, titrate oxygen delivery to the lowest effective level. Emergency Oxygen Administration Guidelines for Oxygen Delivery 61
Emergency Oxygen & Resuscitation • Science is inconclusive about the use of emergency oxygen during resuscitation • Studies show emergency oxygen during resuscitation: – Increases amount of oxygen in the blood – Has little risk of complications • Ensure resuscitation efforts are NEVER DELAYED in order to use emergency oxygen • After a return of spontaneous circulation (ROSC) – Titrate delivery to the lowest level possible – Maintain an Sp. O 2 of 94%-99% Emergency Oxygen Administration Guidelines for Oxygen Delivery 62
Training for Emergency O 2 Use • The Organization’s medical authority should review and approve use and training methods before equipping staff • Train at least one staff member in use of emergency oxygen at all times during business hours • Training should be ‘certification’ level from a nationally-recognized organization • Training should incorporate any local guidelines that may differ from this training Emergency Oxygen Administration Guidelines for Oxygen Delivery 63
OXYGEN SAFETY Emergency Oxygen Administration 64
Key Concepts • Oxygen is very reactive and can create a dangerous situation by making items more flammable • When the oxygen level is increased, it is easier to start a fire and very difficult to put it out • Take precautions when – Using emergency oxygen w/ defibrillator – Storing and handling cylinders Emergency Oxygen Administration Oxygen Safety 65
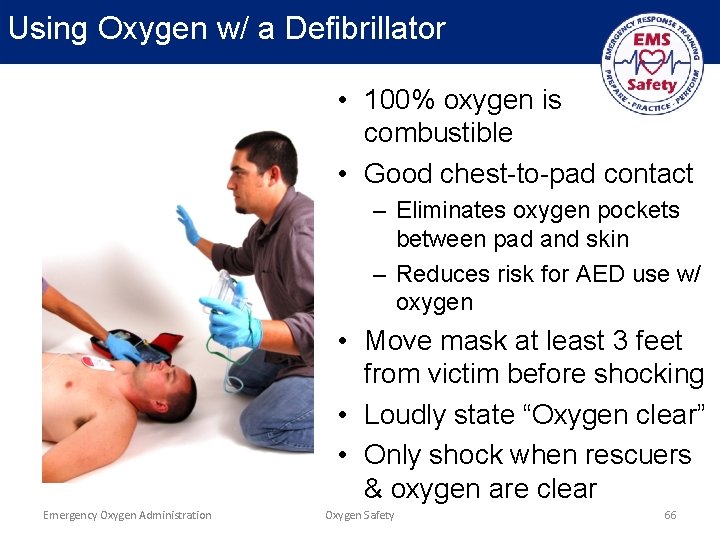
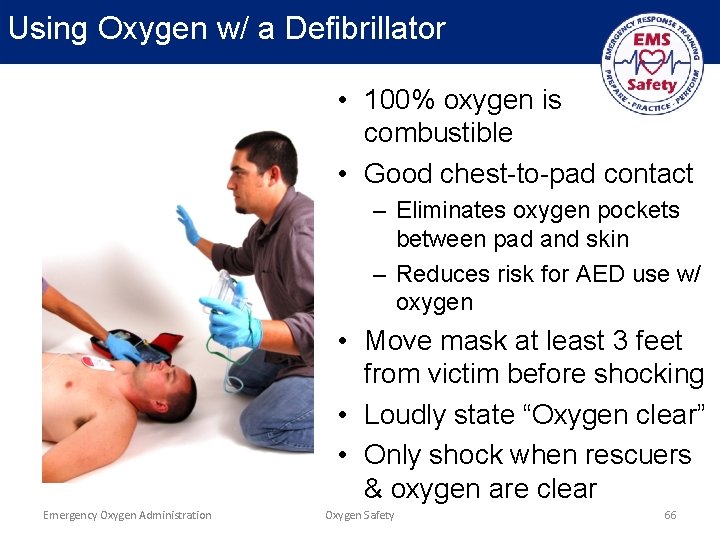
Using Oxygen w/ a Defibrillator • 100% oxygen is combustible • Good chest-to-pad contact – Eliminates oxygen pockets between pad and skin – Reduces risk for AED use w/ oxygen • Move mask at least 3 feet from victim before shocking • Loudly state “Oxygen clear” • Only shock when rescuers & oxygen are clear Emergency Oxygen Administration Oxygen Safety 66
Cylinder Storage • Store cylinders – Upright – Secured to prevent falling • Avoid storing different types of compressed gasses in the same area • Store in a well-ventilated area • Do not subject cylinders to temperatures greater than 125 o. F, prolonged exposure to direct sunlight, or exposure to other heat sources (e. g. radiator, space heater) Emergency Oxygen Administration Oxygen Safety 67
Cylinder Maintenance • Regularly inspect equipment and document inspections according to national and local guidelines and manufacturer specifications • Ensure labels and signs are in compliance w/ federal OSHA, state and local regulations • Do not use a cylinder that appears damaged • Keep oxygen equipment clean. Dirt and debris can be a fire hazard • Use a pressure gauge to check contents; do not rely solely on a tagging system (Full, In-Use, Empty) Emergency Oxygen Administration Oxygen Safety 68
Cylinder Handling • Do not slide, drag or roll cylinders • Do not use oil or grease on oxygen equipment • When on scene, lay the oxygen cylinder on the floor so it does not get knocked over accidentally • If transporting the cylinder with the patient, secure it to the cot, stretcher or gurney so that it does not slip or get knocked off Emergency Oxygen Administration Oxygen Safety 69
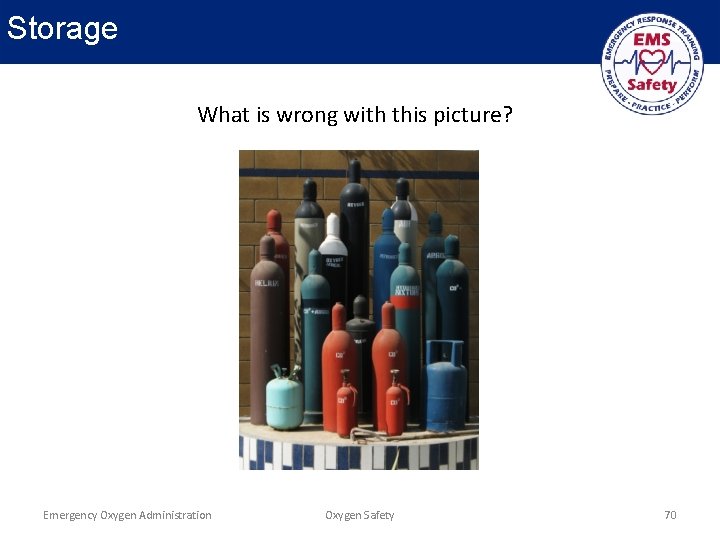
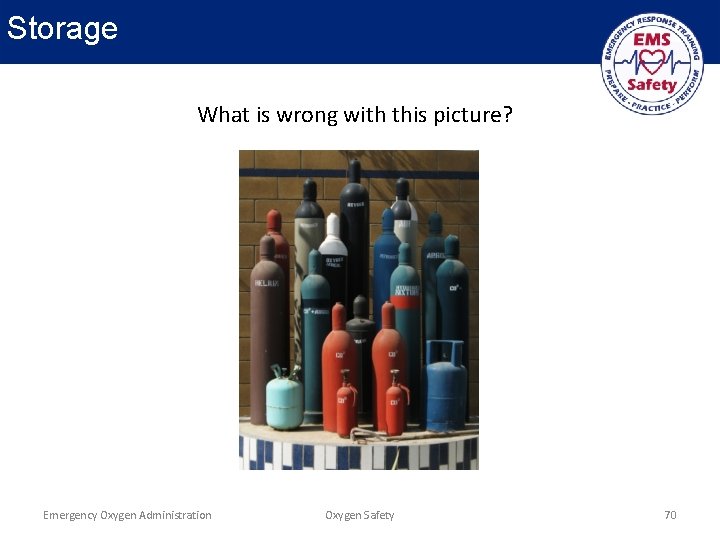
Storage What is wrong with this picture? Emergency Oxygen Administration Oxygen Safety 70
Oxygen is Combustible • 100% oxygen is highly reactive, and can cause other materials to catch on fire • Keep away from heat sources and flammable items • Avoid alcohol, aerosol sprays, solvents, perfumes and petroleum products • Never combine oxygen with an ignition source (e. g. cigarette) Emergency Oxygen Administration Oxygen Safety 71
Suction Devices and Airway Adjuncts… OPTIONAL TOPICS Emergency Oxygen Administration 72
Suctioning & Airway Adjuncts • Objectives – Identify equipment associated w/ the use of emergency oxygen and airway management • Key Concepts – It’s important to be familiar w/ the equipment that may be used by all levels of rescuers – Oxygen delivery may also be associated with • Advanced airway adjuncts • Suction devices Emergency Oxygen Administration Suction Devices & Airway Adjuncts 73
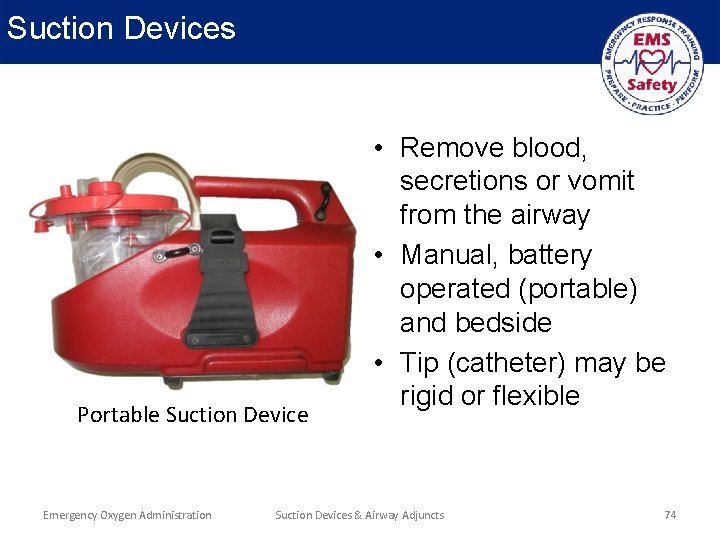
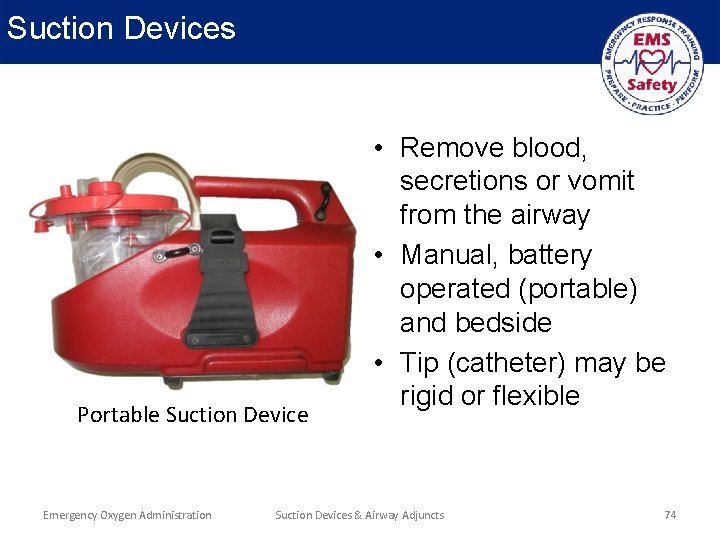
Suction Devices Portable Suction Device Emergency Oxygen Administration • Remove blood, secretions or vomit from the airway • Manual, battery operated (portable) and bedside • Tip (catheter) may be rigid or flexible Suction Devices & Airway Adjuncts 74
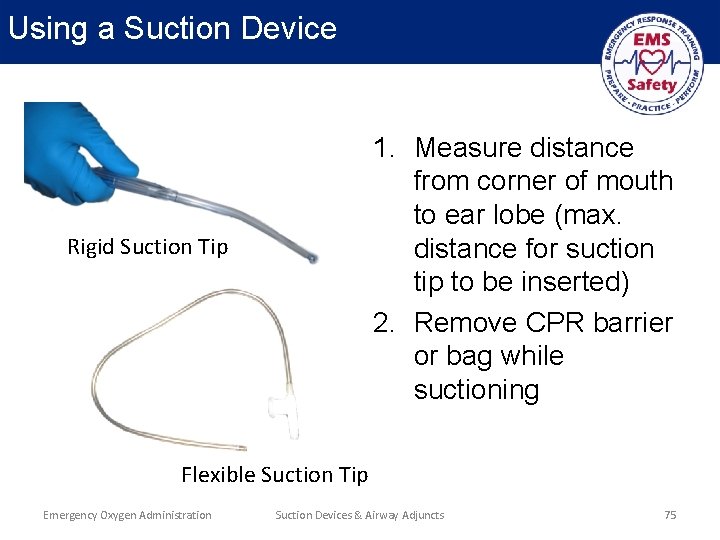
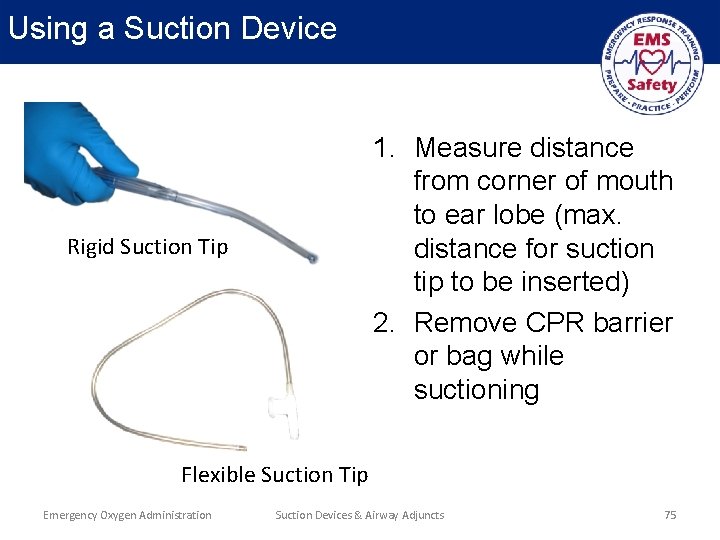
Using a Suction Device 1. Measure distance from corner of mouth to ear lobe (max. distance for suction tip to be inserted) 2. Remove CPR barrier or bag while suctioning Rigid Suction Tip Flexible Suction Tip Emergency Oxygen Administration Suction Devices & Airway Adjuncts 75
Airway Adjuncts • Used for patient in severe distress – Unresponsive or semiconscious – Rescue breathing – Cardiac arrest • Airway adjuncts establish and maintain an open airway • Simple airways can be used w/ no change to CPR sequence – Oral airway – Nasal airway • Advanced airways require change in delivery of compressions & ventilations Emergency Oxygen Administration Suction Devices & Airway Adjuncts 76
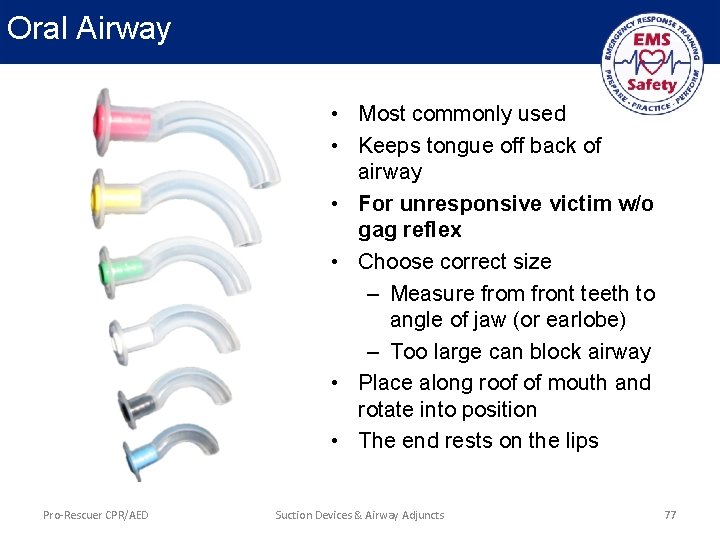
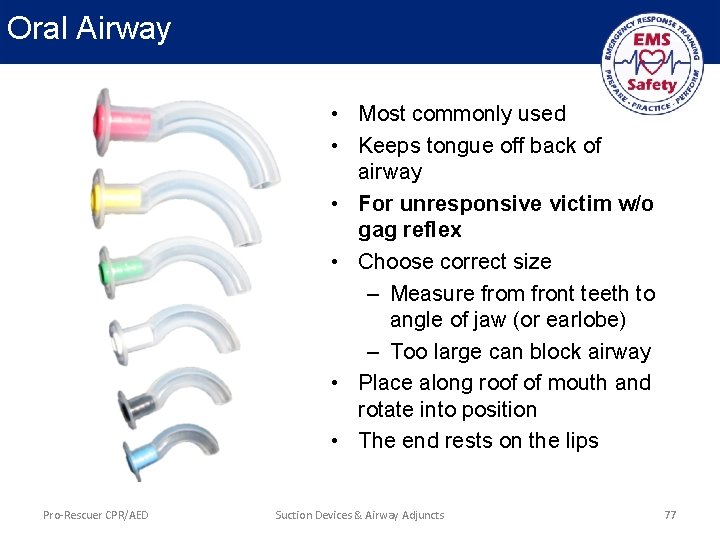
Oral Airway • Most commonly used • Keeps tongue off back of airway • For unresponsive victim w/o gag reflex • Choose correct size – Measure from front teeth to angle of jaw (or earlobe) – Too large can block airway • Place along roof of mouth and rotate into position • The end rests on the lips Pro-Rescuer CPR/AED Suction Devices & Airway Adjuncts 77
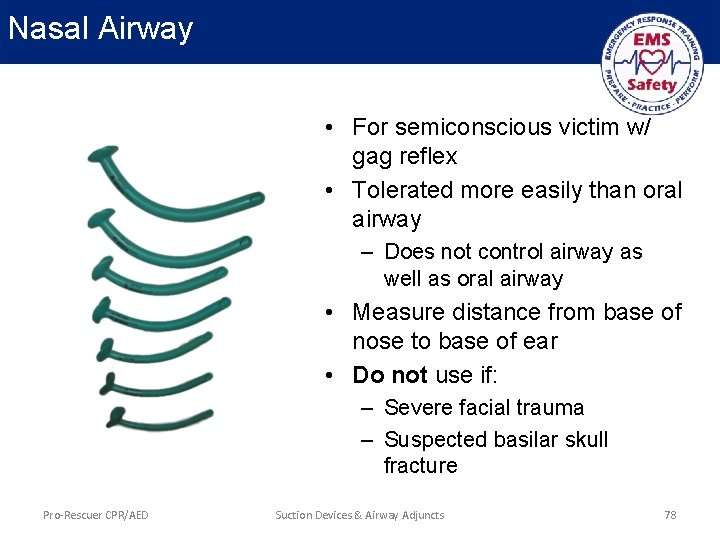
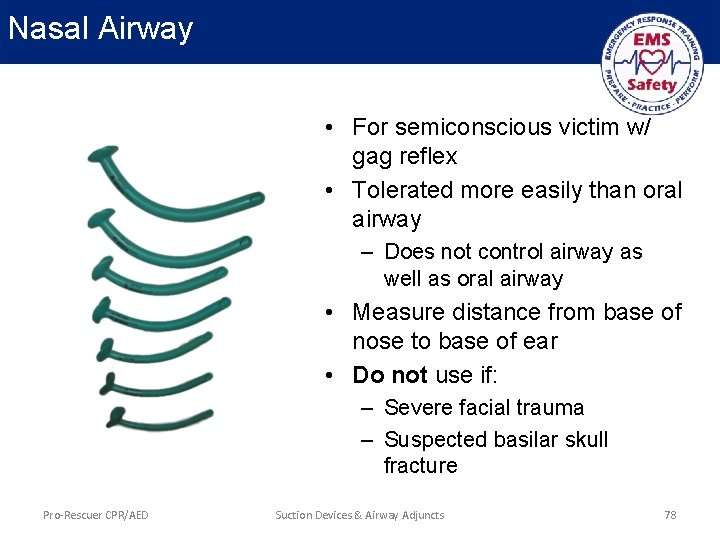
Nasal Airway • For semiconscious victim w/ gag reflex • Tolerated more easily than oral airway – Does not control airway as well as oral airway • Measure distance from base of nose to base of ear • Do not use if: – Severe facial trauma – Suspected basilar skull fracture Pro-Rescuer CPR/AED Suction Devices & Airway Adjuncts 78
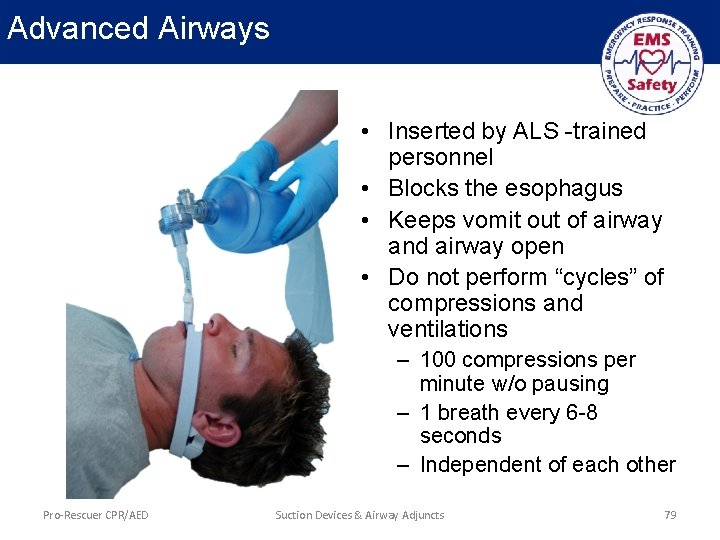
Advanced Airways • Inserted by ALS -trained personnel • Blocks the esophagus • Keeps vomit out of airway and airway open • Do not perform “cycles” of compressions and ventilations – 100 compressions per minute w/o pausing – 1 breath every 6 -8 seconds – Independent of each other Pro-Rescuer CPR/AED Suction Devices & Airway Adjuncts 79
Conclusion • Never delay critical care to provide emergency oxygen • Follow federal, state and local protocols • Only provide oxygen when indicated by patient assessment • At the earliest opportunity, titrate oxygen LPM and delivery device to the lowest level possible to maintain Sp. O 2 94 -99% Emergency Oxygen Administration Conclusion 80