Emergency Medical Dispatch Current Research Implications for Clinical

- Slides: 22
Emergency Medical Dispatch: Current Research & Implications for Clinical Practice AMY GUTMAN MD EMS MEDICAL DIRECTOR PREHOSPITALMD@GMAIL. COM
Hettinger AZ. EMD Codes Association with ED Outcomes. PEC. Jan 2012 � Objective: Examined whether a subset of MPDS codes could predict patient outcomes � Results: 90% MPDS records matched to EMS records; 84% EMS records matched to ED data, resulting in 26, 846 subjects Average 46. 2 yrs; 54% female Of transported patients, 70% discharged from ED, with 9 dispatch codes demonstrating >90% predictive power 3 codes >60% predictive power for admission/death Subjects >65 yrs at increased risk for admission/death in 33 dispatch codes � Conclusions: 8% MPDS codes associated >90% predictive ability for ED discharge Older adults are at increased risk for admission/death suggesting that age criteria may be useful to identify higher-acuity patients within the MPDS code
Sporer KA. How Well Do EMD Codes Predict Prehospital Medication Administration In A Diverse Urban Community? JEM. Oct 2012 � OBJECTIVE: Evaluates ability of MPDS codes to predict prehospital use of medications � METHODS / RESULTS EMD records of transported patients in a diverse urban community queried for prehospital interventions and matched to their MPDS classifications 38, 005 patients; only MPDS subgroups with >10 calls included in the analysis Patients with CP, SOB, heart & diabetic problems received the most medications. Medications administered in 19% of calls MPDS with highest rate of med administration was breathing problems (76%) Higher rates of ALS in EMD categories: unconscious/fainting, breathing problems, abdominal pain; but not in: seizure, sick person, traumatic injury, hemorrhage/lacerations
Coventry LL. MI: Sex Differences in Symptoms Reported to Emergency Dispatch. PEC. Oct 2012 � Objective: Measure effect of sex on symptoms reported to dispatch & response times � Methods: Australia Emergency Department Information System (EDIS) used to identify patients with ED diagnoses of MI arriving by ambulance Their 911 calls transcribed to identify presenting symptoms Ambulance data were used to document ambulance times � Results 1, 681 emergency calls analyzed Women (n=621; 37%) older than men & less likely to report chest pain Ambulance times did not differ between male & female patients with chest pain Women with chest pain less likely than men with chest pain to be allocated a "priority 1" ambulance response (men 98% vs. women 95%)
Petrillo T. The use of a modified pediatric early warning score to assess stability of pediatric patients during transport. Pedi EC. Sept 2012 � OBJECTIVE: In an effort to consistently assess patient acuity and the impact of our team's interventions, we instituted a modified transport pediatric early warning scores (TPEWS). � METHODS / RESULTS: 100 consecutive children transported by Children's Transport PEWS given during triage by the dispatch center (TPEWStri), TPEWS calculated at referring facility by the team (TPEWSref), and final TPEWS at the accepting institution (TPEWSacc) were compared. 86 patients transported by ground Median age was 50 months 60% received some intervention from the transport team. Median TPEWSref was 3 (0 -9) upon initial assessment & TPEWSacc was 2 (0 -9) on arrival at the accepting facility 73% transported to the ED, 15% to general in-patient floor, 12% to the ICU � CONCLUSIONS: Transport PEWS may function as a tool for assessing severity of illness, optimizing transport dispatch & patient disposition
Scott G. Accuracy of EMD-assisted layperson-caller pulse check using medical priority dispatch system protocol. Prehosp Dis Med. Jan 2012 � HYPOTHESIS: when instructed by a trained emergency medical dispatcher (EMD) using the scripted Medical Priority Dispatch System (MPDS) protocol Pulse Check Diagnostic Tool (PCDx. T), a layperson-caller can detect a carotid pulse and accurately determine the pulse rate in a conscious person. � METHODS: � This non-randomized and non-controlled prospective study was conducted at three different � � public locations in the state of Utah (USA). A healthy, mock patient's pulse rate was obtained using an electrocardiogram (ECG) monitor. Layperson-callers, in turn, initiated a simulated 911 phone call to an EMD call-taker who provided instructions for determining the pulse rate of the patient. Layperson accuracy was assessed using correlations between the layperson-caller's finding and the ECG reading. RESULTS: Two hundred sixty-eight layperson-callers participated; 248 (92. 5%) found the pulse of the mock patient. There was a high correlation between pulse rates obtained using the ECG monitor and those found by the layperson-callers, overall (94. 6%, P <. 001), and by site, gender, and age. CONCLUSIONS: Layperson-callers, when provided with expert, scripted instructions by a trained 911 dispatcher over the phone, can accurately determine the pulse rate of a conscious and healthy person. Improvements to the 911 instructions may further increase layperson accuracy.
Barron T. Aspirin administration by EMD using a protocol-driven diagnostic & instruction tool. EMJ. July 2012 � BACKGROUND: � The American College of Cardiology and the American Heart Association recommend early aspirin � � � administration to patients with symptoms of acute coronary syndrome (ACS)/acute myocardial infarction (AMI). The primary objective of this study was to determine if Emergency Medical Dispatchers (EMD) can provide chest pain/heart attack patients with standardised instructions effectively, using an aspirin diagnostic and instruction tool (ADx. T) within the Medical Priority Dispatch System (MPDS) before arrival of an emergency response crew. METHODS: This retrospective study involved three dispatch centres in the UK and USA. We analysed 6 months of data involving chest pain/heart attack symptoms taken using the MPDS chest pain and heart problems/automated internal cardiac defibrillator protocols. RESULTS: The EMDs successfully completed the ADx. T on 69. 8% of the 44 141 cases analysed. The patient's mean age was higher when the ADx. T was completed, than when it was not (mean±SD: 53. 9± 19. 9 and 49. 9± 20. 2; p<0. 001, respectively). The ADx. T completion rate was higher for second-party than first-party calls (70. 3% and 69. 0%; p=0. 024, respectively). A higher percentage of male than female patients took aspirin (91. 3% and 88. 9%; p=0. 001, respectively). Patients who took aspirin were significantly younger than those who did not (mean±SD: 61. 8± 17. 5 and 64. 7± 17. 9, respectively). Unavailability of aspirin was the major reason (44. 4%) why eligible patients did not take aspirin when advised. CONCLUSIONS: EMDs, using a standardised protocol, can enable early aspirin therapy to treat potential ACS/AMI prior to responders' arrival. Further research is required to assess reasons for not using the protocol, and the significance of the various associations discovered.
Clawson J. Medical Priority Dispatch System breathing problems protocol key question combinations are associated with patient acuity. Prehosp Dis Med. Aug 2012 � INTRODUCTION: The Breathing Problems Chief Complaint is the MPDS’ most frequently used protocol. “Severe breathing problems" is a also a significant predictor of cardiac arrest (CA). The hypothesis in this study was that certain combinations of caller answers to the breathing problems protocol key questions (KQs) correlated with different but specific patient acuities. RESULTS: 42, 000 cases recorded; 52% female, median age 61 yrs. Overall patients with abnormal breathing and clammy conditions were the youngest. Difficulty speaking between breaths (DSBB) condition was the most prevalent (50. 3%). Ineffective breathing and not alert conditions had the highest cardiac arrest quotient (CAQ). Based on the KQ combinations, the CA patients who also had the not alert condition were significantly older than other patients. The percentage of CA outcomes in asthmatic patients was significantly higher in DSBB plus not alert; DSBB plus not alert plus changing color; and DSBB plus not alert plus clammy conditions cases, compared to asthmatic abnormal breathing cases. � CONCLUSIONS: � The study findings demonstrated that MPDS KQ answer combinations relate to patient acuity. Cardiac arrest patients are significantly less likely to be asthmatic than those without CA, and vice versa. Using a prioritization scheme that accounts for the presence of either single or multiple signs and/or symptom combinations for the Breathing Problems CC protocol would be a more accurate method of assigning DELTA-level cases in the MPDS. � �
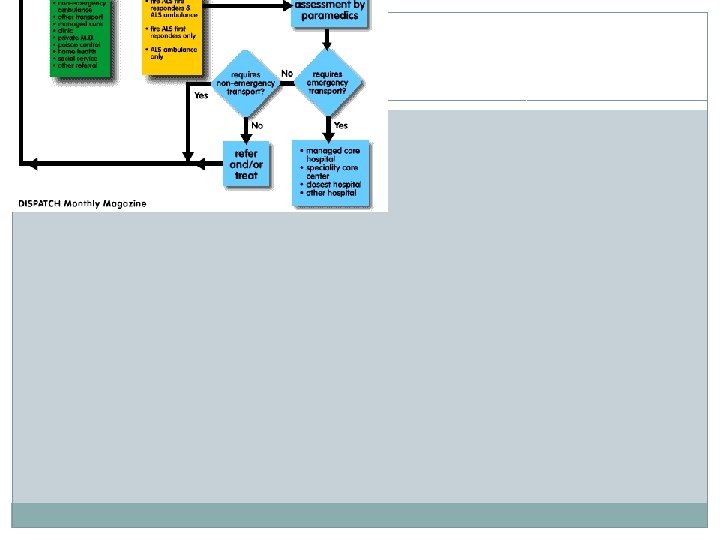
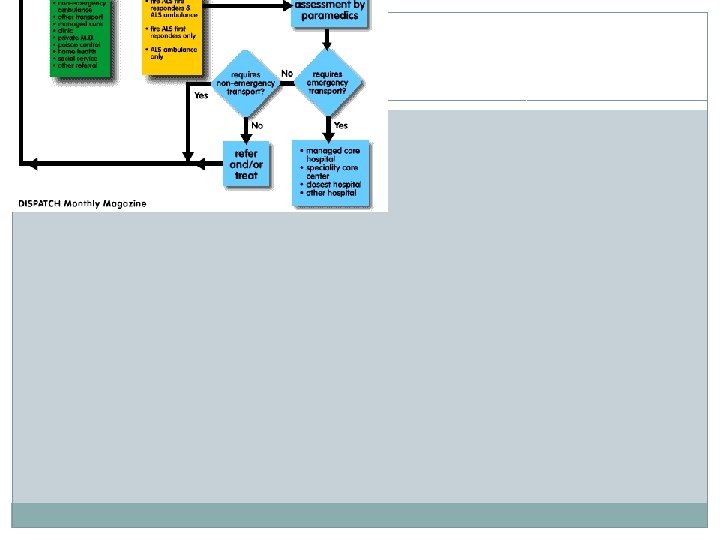
� � � � Prehosp Emerg Care. 2012 Apr-Jun; 16(2): 204 -9. Epub 2012 Jan 12. Utilization of prehospital dispatch protocols to identify low-acuity patients. Studnek JR, Thestrup L, Blackwell T, Bagwell B. Source Carolinas Medical Center, The Center for Prehospital Medicine and Mecklenburg EMS Agency, Charlotte, North Carolina 28232, USA. jonst@medic 911. com Abstract OBJECTIVES: To describe the experience of a U. S. emergency medical services (EMS) agency utilizing a dispatch algorithm to identify low-acuity patients and determine whether secondary telephone triage by a nurse was associated with subsequent hospital admission among those patients. METHODS: This was a retrospective study of all patients meeting the low-acuity Omega classification by the Medical Priority Dispatch System (MPDS) in a large urban EMS system, conducted in two phases. Patients were excluded from the study if a refusal for transport was obtained, the call was received from a third-party caller, the MPDS system was not used, the patient was being referred from a skilled nursing facility, school, or university nursing office or physician's office, or if the call was referred to the Carolina Poison Center. Patients were enrolled over two phases using two different versions of the MPDS protocol, and in phase 2 patients were offered the option of speaking with an advice-line nurse. The outcome of interest was emergency department disposition, classified as hospital admission or discharge home. Admission to an intensive care unit (ICU) bed was also collected as a subcategory of hospital admission. RESULTS: Of the 1, 862 patients in phase 1, 69. 3% were discharged home from the emergency department, whereas in phase 2, 73. 0% of the 1, 078 patients were discharged home. Individuals were most frequently admitted to the hospital across both phases if they had a dispatch determinant of pregnancy, psychiatric/behavioral, fall, sick person. Hospital admission was also associated with receiving an EMS or emergency department procedure. There were 530 patients in phase 2 who underwent secondary triage by an adviceline nurse. Among this cohort of patients, 134 (25. 3%) required subsequent hospital admission, with a further three (2. 2%) requiring an ICU admission. CONCLUSIONS: This study identified a method for classifying patients during the dispatch period as low-acuity while attempting to ensure that those individuals received the medical care that they needed.
� � � � Prehosp Emerg Care. 2012 Apr-Jun; 16(2): 242 -50. Epub 2011 Dec 12. Time to first compression using Medical Priority Dispatch System compression-first dispatcher-assisted cardiopulmonary resuscitation protocols. Van Vleet LM, Hubble MW. Source Wake County EMS, Raleigh, North Carolina 27601, USA. lee. vanvleet@co. wake. nc. us Abstract INTRODUCTION: Without bystander cardiopulmonary resuscitation (CPR), cardiac arrest survival decreases 7%-10% for every minute of delay until defibrillation. Dispatcherassisted CPR (D-CPR) has been shown to increase the rates of bystander CPR and cardiac arrest survival. Other reports suggest that the most critical component of bystander CPR is chest compressions with minimal interruption. Beginning with version 11. 2 of the Medical Priority Dispatch System (MPDS) protocols, instructions for mouth-to-mouth ventilation (MTMV) and pulse check were removed and a compression-first pathway was introduced to facilitate rapid delivery of compressions. Additionally, unconscious choking and third-trimester pregnancy decision-making criteria were added in versions 11. 3 and 12. 0, respectively. However, the effects of these changes on time to first compression (TTFC) have not been evaluated. OBJECTIVE: We sought to quantify the TTFC of MPDS versions 11. 2, 11. 3, and 12. 0 for all calls identified as cardiac arrest on call intake that did not require MTMV instruction. METHODS: Audio recordings of all D-CPR events for October 2005 through May 2010 were analyzed for TTFC. Differences in TTFC across versions were compared using the Kruskal-Wallis test. RESULTS: A total of 778 cases received D-CPR. Of these, 259 were excluded because they met criteria for MTMV (pediatric patients, allergic reaction, etc. ), were missing data, or were not initially identified as cardiac arrest. Of the remaining 519 calls, the mean TTFC was 240 seconds, with no significant variation across the MPDS versions (p = 0. 08). CONCLUSIONS: Following the removal of instructions for pulse check and MTMV, as well as other minor changes in the MPDS protocols, we found the overall TTFC to be 240 seconds with little variation across the three versions evaluated. This represents an improvement in TTFC compared with reports of an earlier version of MPDS that included pulse checks and MTMV instructions (315 seconds). However, the MPDS TTFC does not compare favorably with reports of older, non-MPDS protocols that included pulse checks and MTMV. Efforts should continue to focus on improving this key, and modifiable, determinant of cardiac arrest survival.
Blanchard IE. EMS response time and mortality in an urban setting. PEC. Jan 2012. � � � � � BACKGROUND: A common tenet in emergency medical services (EMS) is that faster response equates to better patient outcome, translated by some EMS operations into a goal of a response time of 8 minutes or less for advanced life support (ALS) units responding to lifethreatening events. OBJECTIVE: To explore whether an 8 -minute EMS response time was associated with mortality. METHODS: This was a one-year retrospective cohort study of adults with a life-threatening event as assessed at the time of the 9 -1 -1 call (Medical Priority Dispatch System Echo- or Delta-level event). The study setting was an urban all-ALS EMS system serving a population of approximately 1 million. Response time was defined as 9 -1 -1 call receipt to ALS unit arrival on scene, and outcome was defined as all-cause mortality at hospital discharge. Potential covariates included patient acuity, age, gender, and combined scene and transport interval time. Stratified analysis and logistic regression were used to assess the response time-mortality association. RESULTS: There were 7, 760 unit responses that met the inclusion criteria; 1, 865 (24%) were ≥ 8 minutes. The average patient age was 56. 7 years (standard deviation = 21. 5). For patients with a response time ≥ 8 minutes, 7. 1% died, compared with 6. 4% for patients with a response time ≤ 7 minutes 59 seconds (risk difference 0. 7%; 95% confidence interval [CI]: -0. 5%, 2. 0%). The adjusted odds ratio of mortality for ≥ 8 minutes was 1. 19 (95% CI: 0. 97, 1. 47). An exploratory analysis suggested there may be a small beneficial effect of response ≤ 7 minutes 59 seconds for those who survived to become an inpatient (adjusted odds ratio = 1. 30; 95% CI: 1. 00, 1. 69). CONCLUSIONS: These results call into question the clinical effectiveness of a dichotomous 8 -minute ALS response time on decreasing mortality for the majority of adult patients identified as having a life-threatening event at the time of the 9 -1 -1 call. However, this study does not suggest that rapid EMS response is undesirable or unimportant for certain patients. This analysis highlights the need for further research on who may benefit from rapid EMS response, whether these individuals can be identified at the time of the 9 -1 -1 call, and what the optimum response time is.
Sporer KA. Detailed analysis of prehospital interventions in medical priority dispatch system determinants. West JEM. Feb 2011. � � � � � BACKGROUND: Medical Priority Dispatch System (MPDS) is a type of Emergency Medical Dispatch (EMD) system used to prioritize 9 -1 -1 calls and optimize resource allocation. Dispatchers use a series of scripted questions to assign determinants to calls based on chief complaint and acuity. OBJECTIVE: We analyzed the prehospital interventions performed on patients with MPDS determinants for breathing problems, chest pain, unknown problem (man down), seizures, fainting (unconscious) and falls for transport status and interventions. METHODS: We matched all prehospital patients in complaint-based categories for breathing problems, chest pain, unknown problem (man down), seizures, fainting (unconscious) and falls from January 1, 2004, to December 31, 2006, with their prehospital record. Calls were queried for the following prehospital interventions: Basic Life Support care only, intravenous line placement only, medication given, procedures or non-transport. We defined Advanced Life Support (ALS) interventions as the administration of a medication or a procedure. RESULTS: Of the 77, 394 MPDS calls during this period, 318 (40%) patients met inclusion criteria. Breathing problems made up 12. 2%, chest pain 6%, unknown problem 1. 4%, seizures 3%, falls 9% and unconscious/fainting 9% of the total number of MPDS calls. Patients with breathing problem had a low rate of procedures (0. 7%) and cardiac arrest medications (1. 6%) with 38% receiving some medication. Chest pain patients had a similar distribution; procedures (0. 5%), cardiac arrest medication (1. 5%) and any medication (64%). Unknown problem: procedures (1%), cardiac arrest medication (1. 3%), any medication (18%). Patients with Seizures had a low rate of procedures (1. 1%) and cardiac arrest medications (0. 6%) with 20% receiving some medication. Fall patients had a lower rate of severe illness with more medication, mostly morphine: procedures (0. 2%), cardiac arrest medication (0. 2%), all medications (28%). Unconscious/fainting patients received the following interventions: procedures (0. 3%), cardiac arrest medication (1. 9%), all medications (32%). Few stepwise increases in the rate of procedures or medications were seen as determinants increased in acuity. CONCLUSION: Among these common MPDS complaint-based categories, the rates of advanced procedures and cardiac arrest medications were low. ALS medications were common in all categories and most determinants. Multiple determinants were rarely used and did not show higher rates of interventions with increasing acuity. Many MPDS determinants are of modest use to predict ALS intervention.
Vilensky D. Communication errors in dispatch of air medical transport PEC. Jan 2011. � � � � � BACKGROUND: Communication errors are a source of preventable medical errors. In high-risk health care settings, identifying the source and addressing root causes can reduce error and improve patient safety. While air medical transport is a high-risk setting, its sources and rates of error have been investigated only within the last several years. OBJECTIVES: This investigation examined the rate and types of communication errors during call booking of interfacility air medical transports. The primary objective was to determine the incidence and type of errors when the initial requests for transfer took place between the sending facility and transport medicine communication center. The secondary objective was to identify potential underlying causes of these errors. METHODS: Requests for urgent and emergent interfacility air medical transfers were examined prospectively during a consecutive two-week period. As the first step in call booking, sending facility staff speak directly to communication center staff and are asked for administrative, demographic, and medical details to determine patient acuity and call priority. After this information was captured, investigators contacted the sending facility to verify the information and identify any communication errors. Errors were classified as major (potentially impacting care) or minor (unlikely to impact care) and as errors of omission or commission. Common error types were presented to a management focus group to identify potential contributing causes for these errors. RESULTS: One hundred twelve calls were randomly selected during the study period, with 98 meeting study criteria. Of those, 41 (42%) calls contained a total of 65 errors. Eleven were classified as major, including five errors of omission and six errors of commission. The most common major errors were recording "no drug allergies" when a drug allergy was present (n = 4), incorrect diagnosis (n = 2), and failure to record that patients were intubated or required mechanical ventilation (n = 2 each). There were 54 minor errors, including 41 omission errors and 13 commission errors. Nearly half the errors were attributed to procedures and software. No identified error resulted in patient harm or an adverse outcome. CONCLUSIONS: Communication-based errors are common in the initial phases of call booking in air medical transport. Human and process-driven errors contribute equally to these errors.
� � � � Prehosp Emerg Care. 2007 Apr-Jun; 11(2): 192 -8. The ability of emergency medical dispatch codes of medical complaints to predict ALS prehospital interventions. Sporer KA, Youngblood GM, Rodriguez RM. Source Department of Medicine, University of California, San Francisco, USA. ksporer@sfghed. ucsf. edu Abstract OBJECTIVE: The Medical Priority Dispatch System (MPDS) is an emergency medical dispatch (EMD) system that is commonly used to triage 91 -1 calls and optimize paramedic and EMT dispatch. The objective of this study was to determine the sensitivity, specificity, and positive and negative predictive values of selected MPDS dispatch codes to predict the need for ALS medication or procedures. METHODS: Patients with selected MPDS codes between November 1, 2003, and October 31, 2005, from a suburban California county were matched with their electronic patient care record. The records of all transported patients were queried for prehospital interventions and matched to their MPDS classification [Basic Life Support (BLS) versus Advanced Life Support (ALS)]. Patients who received prehospital interventions or medications were considered ALS Intervention. With true positive = ALS by MPDS + ALS Intervention, true negative = BLS by MPDS + BLS Interventions, false positive = ALS by MPDS + BLS Interventions, and false negative = BLS by MPDS + ALS Interventions, the screening performance of the San Mateo County EMD system was determined for selected complaint categories (abdominal pain, breathing problems chest pain, sick person, seizures, and unconscious/fainting). RESULTS: There were a total of 64, 647 medical calls, and 42, 651 went through the EMD process; 31, 187 went through the EMD process and were transported; 22, 243 of these were matched to a patient care record. The sensitivity and specificity with 95% confidence intervals in () were as follows: all EMD calls 84 (83 -85), 36 (35 -36); abdominal pain, 53 (41 -65), 47 (43 -51); chest pain 99 (99100), 2 (1 -3); seizure 83 (77 -88), 20 (17 -23), sick 59 (53 -64), 51 (49 -54), and unconscious/fainting 99 (98 -100), 2 (2 -3). CONCLUSION: In our EMS system, MPDS coding for all medical calls had high sensitivity and low specificity for the prediction of calls that required ALS intervention. Chest pain and unconscious/fainting calls were screened with very high sensitivity but very low specificity.
Bailey ED. Use of EMD protocols to reduce the number of inappropriate scene responses by ALS personnel NAEMSP. July 1997 � Objectives. To determine whether implementation of an emergency medical dispatch (EMD) system would reduce the rate of inappropriate advanced life support (ALS) utilization, and enable more accurate identification of those patients requiring ALS care. Methods. An emergency medical services (EMS) site providing basic life support (BLS) and ALS care to a population of 200, 000 served as the study site for calendar year 1996. This study compared the prospective identification of patients as ALS or BLS using EMD with that using chief complaintbased dispatch criteria. Each patient served as his or her own control. The ALS or BLS priority was assigned using both chief complaint and EMD criteria. Chief complaint-based dispatching meant that all patients with preestablished chief complaints received ALS without further triage questions, while EMD allowed the dispatchers to question callers using a scripted set of questions. The outcome measures included the number of calls categorized as ALS or BLS, the number of calls cancelled by BLS, and the number of ALS calls released to BLS care. Yatescorrected chi-square was used for statistical analysis. Results. There were 11, 174 patients enrolled. The use of EMD was associated with a significant decrease in the proportion of calls designated as ALS (44. 7% vs 55. 8%, p < 0. 0001), as well as a significant decrease in the number of ALS responses cancelled by BLS (9. 2% vs 23. 8%, p < 0. 0001) and patients released to BLS by medical control (4. 7% vs 7. 3%, p < 0. 0001). Conclusions. Implementation of an EMD system significantly decreased inappropriate ALS dispatching, as defined by decreased rate of ALS cancellations and BLS releases. Further study is needed to see whether other EMD dispatch models may further refine ALS dispatch. PREHOSPITAL EMERGENCY CARE 2000; 4: 186 -189
www. naedjoural. org � � � � Medical eye problems Brett: Our agency had a call with a Chief Complaint of “I can’t see” and when asked for clarification (“Tell me exactly what happened. ”) the dispatcher was told that the individual had liposuction that day. The EMD coded it as a 16 -A-3 (Medical eye problems). Thoughts? Joe Tassitano Captain Alpharetta Department of Public Safety Alpharetta, Georgia, USA Joe: A SUDDEN change in eyesight is very commonly associated with a stroke, and should be handled as such. This Chief Complaint selection principle is covered in the STROKE Symptoms list in the AI section of Protocol 28: “Sudden trouble seeing in one or both eyes. ” This list, which is relatively new to the Protocol, should be very familiar to EMDs, exactly like the HEART ATTACK Symptoms list accompanying Protocol 10. Just as some patients may not use the exact words “chest pain” when describing the symptoms of acute coronary syndrome, stroke patients sometimes only describe the symptoms of stroke without actually complaining of a stroke. This is especially true with symptoms such as a sudden loss of vision, which is not as commonly associated with stroke as a sudden loss of motor function on one side of the body. Please educate your EMDs about this important section of the Protocol with emphasis on the word SUDDEN, as the symptoms listed are nearly always associated with STROKE. The particular complaint you describe is almost certainly associated with a thrombus, which was caused by the recent liposuction procedure, that likely entered the bloodstream and became lodged in an ophthalmic artery, or in an area of the brain that controls vision. Brett A. Patterson IAED Academics & Standards Associate Research Council Chair

References �www. 911 dispatchers. com �www. neci 911. com �Emergency Medical Dispatch Protocol Reference System �National Highway Transportation Safety Administration (NHTSA)