EMERGENCY CARDIAC PACING PACE MAKER INSERTION Majid Shojaee













- Slides: 60
EMERGENCY CARDIAC PACING PACE MAKER INSERTION Majid Shojaee MD Associate professor of EM EHMC SBMU 1
PACEMAKER • External (transcutaneous) • Internal (transvenous): • Temporary: • Blind: balloon tipped, • Guided: fluoroscopy, U. S, ECG • Permanent 2
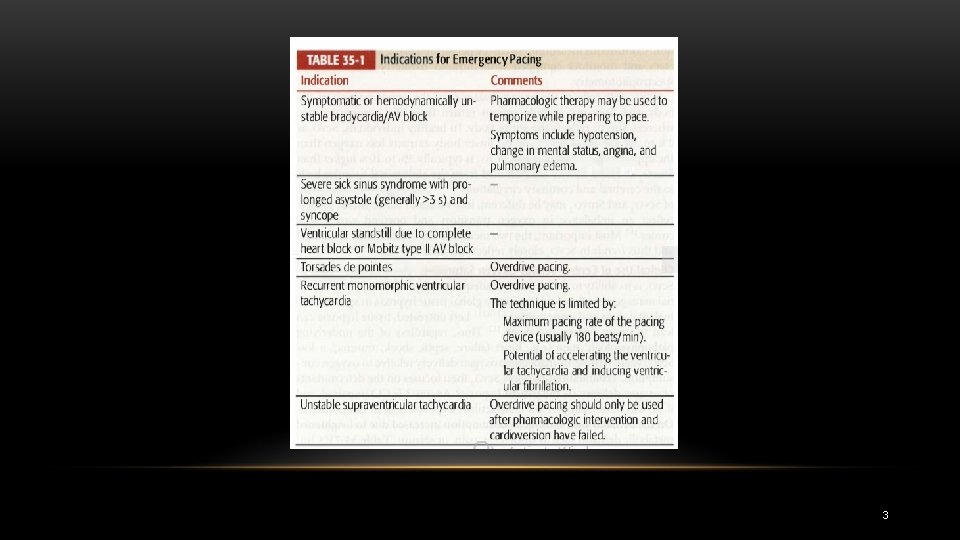
3
TRANSCUTANEOUS PACING • Because it can be instituted quickly and noninvasively, transcutaneous pacing is the technique of choice in the ED when time is of the essence 4
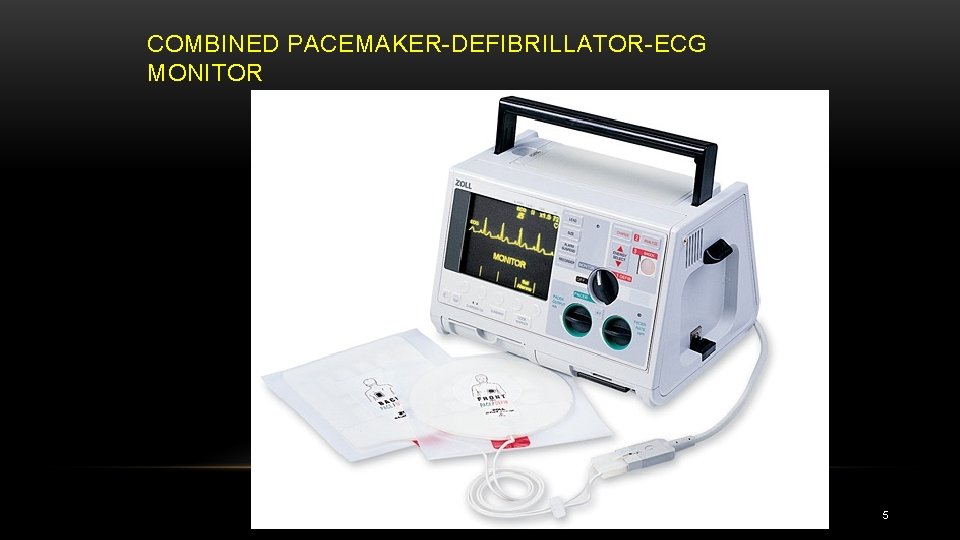
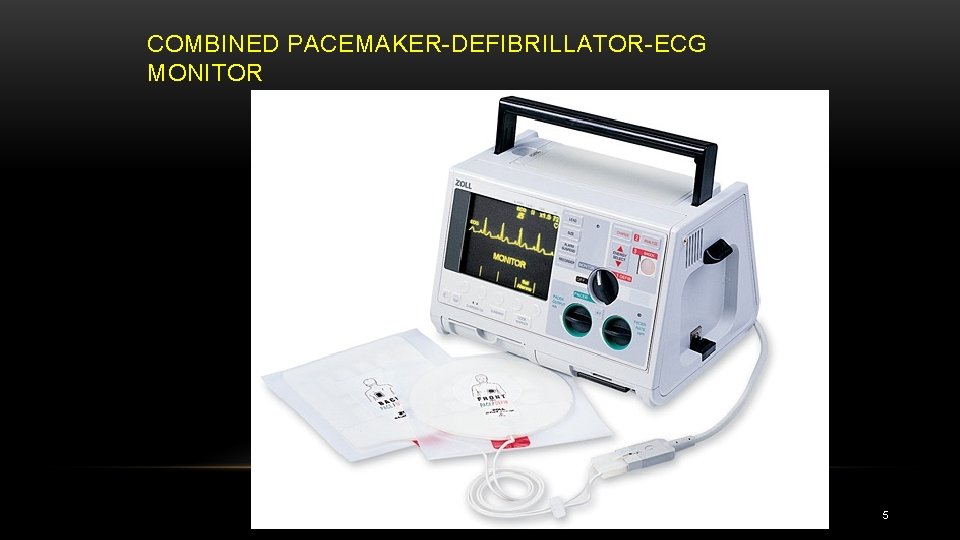
COMBINED PACEMAKER DEFIBRILLATOR ECG MONITOR 5
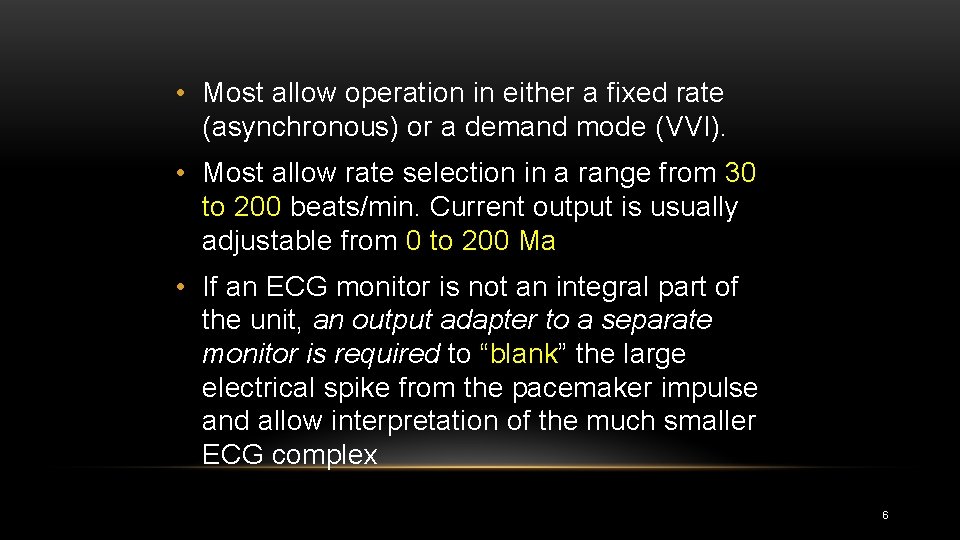
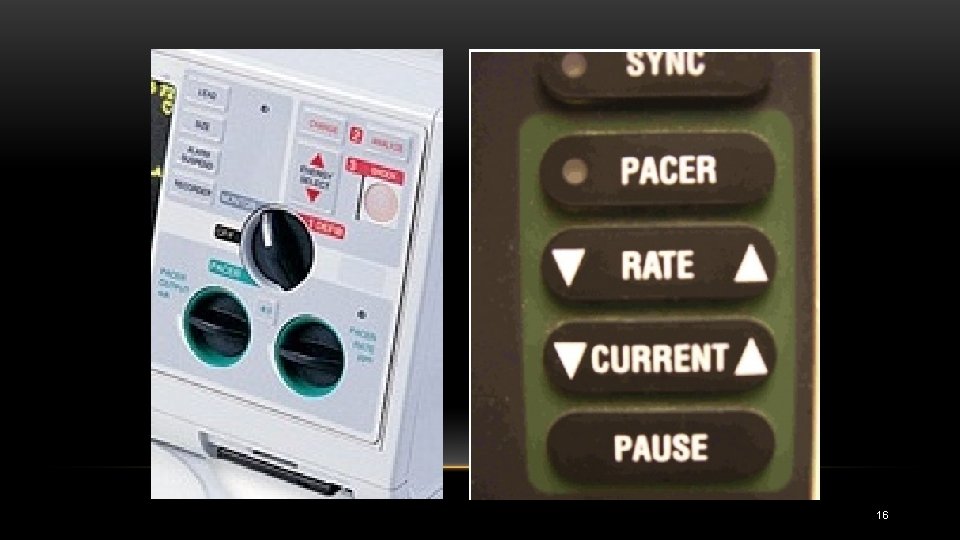
• Most allow operation in either a fixed rate (asynchronous) or a demand mode (VVI). • Most allow rate selection in a range from 30 to 200 beats/min. Current output is usually adjustable from 0 to 200 Ma • If an ECG monitor is not an integral part of the unit, an output adapter to a separate monitor is required to “blank” the large electrical spike from the pacemaker impulse and allow interpretation of the much smaller ECG complex 6
• Without blanking protection, the standard ECG machine is swamped by the pacemaker spike and is uninterpretable. • This could be disastrous because the large pacing artifacts can mask treatable ventricular fibrillation. 7
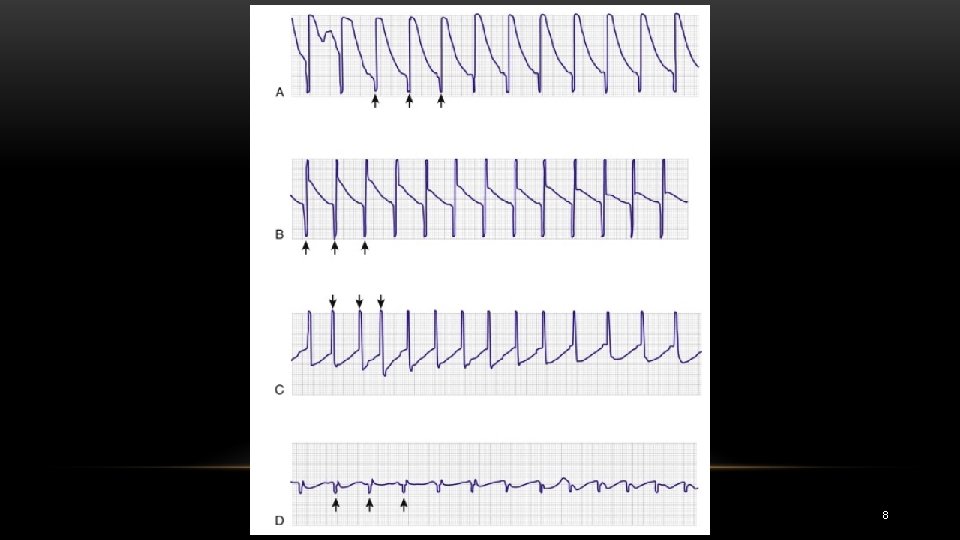
8
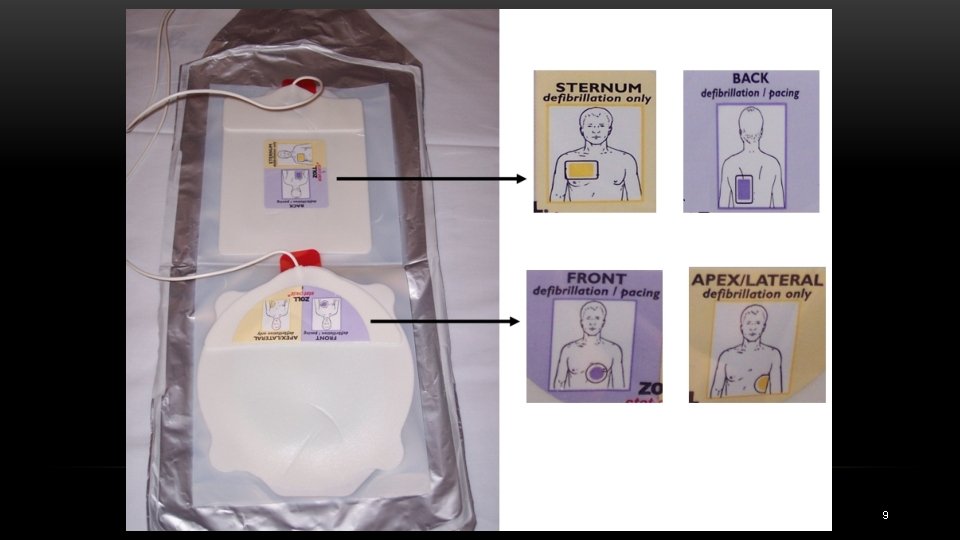
9
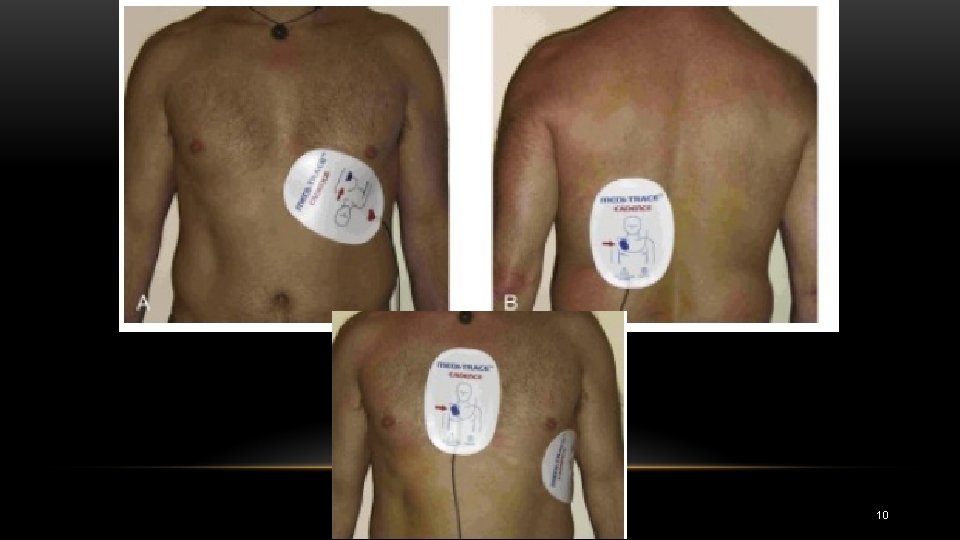
10
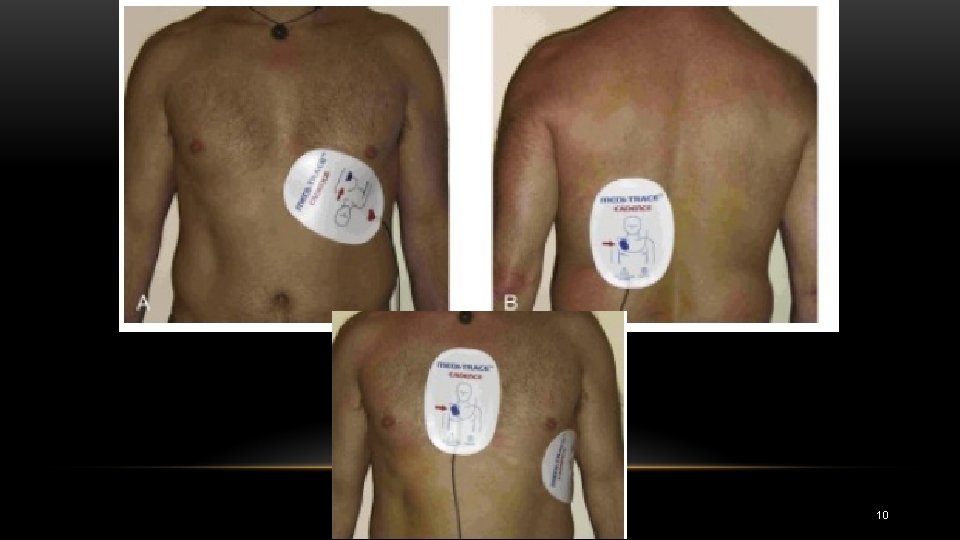
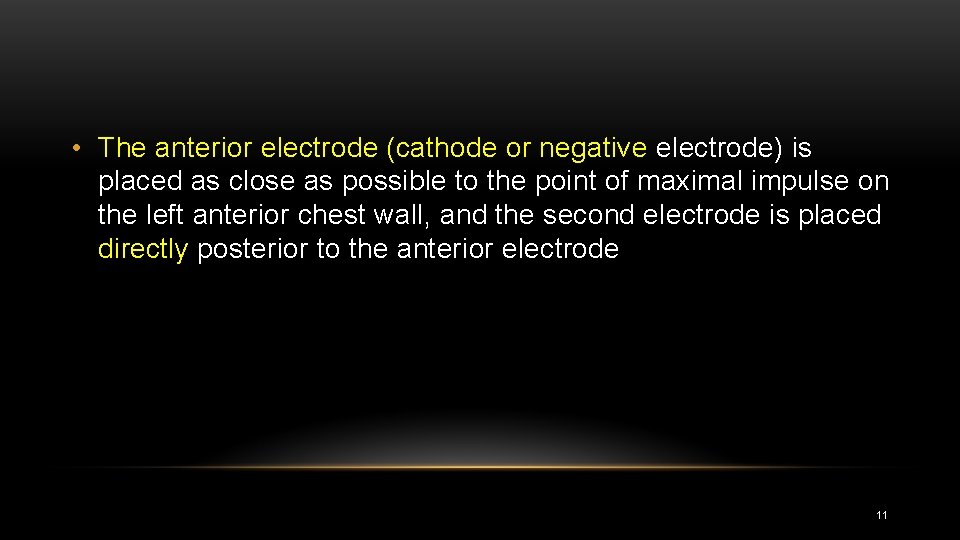
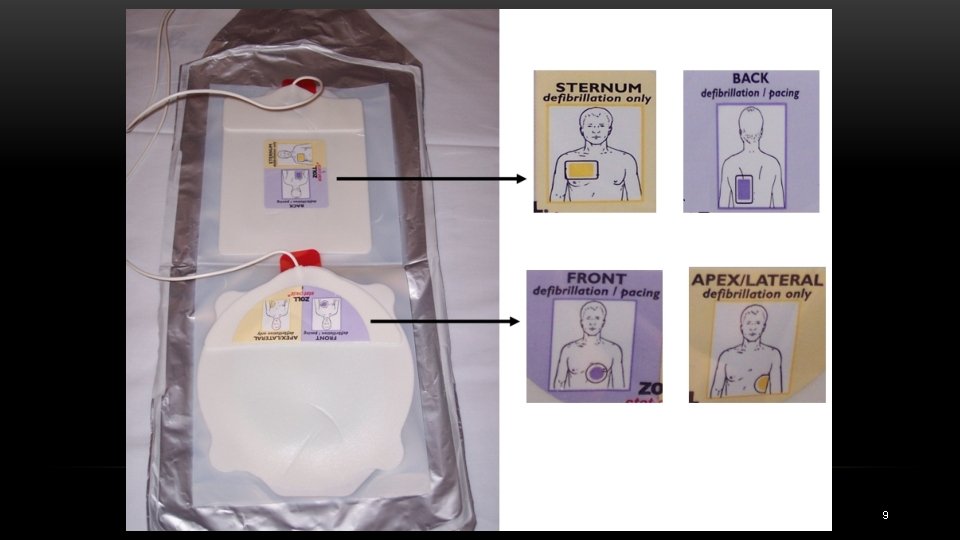
• The anterior electrode (cathode or negative electrode) is placed as close as possible to the point of maximal impulse on the left anterior chest wall, and the second electrode is placed directly posterior to the anterior electrode 11

• Although the polarity of the electrodes does not appear to be important for defibrillation, at least one study indicated that it might be for pacing. • The electrodes are labeled by the manufacturer to indicate which should be placed over the precordium; • it is prudent to observe this recommendation • If separate defibrillator pads or paddles are used, place them at least 2 to 3 cm from the pacing pads. 12
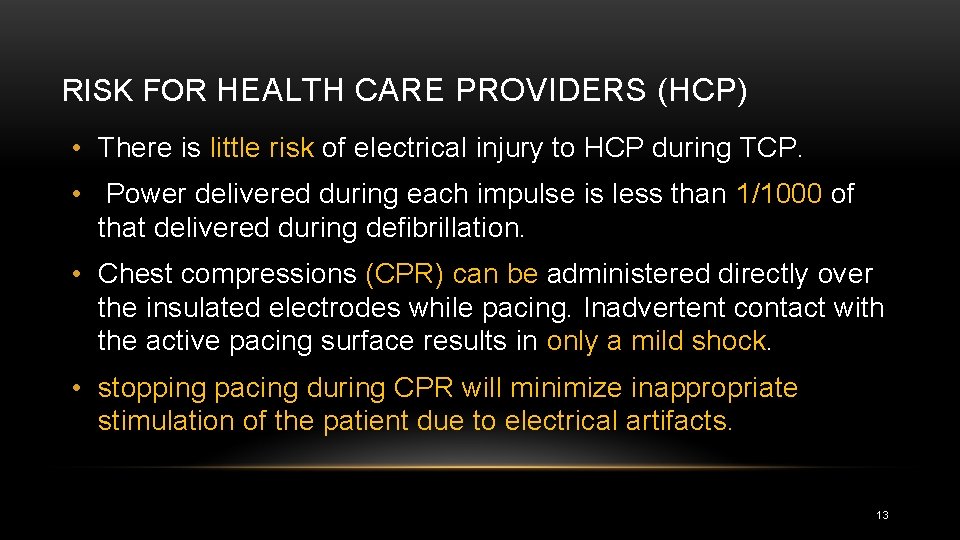
RISK FOR HEALTH CARE PROVIDERS (HCP) • There is little risk of electrical injury to HCP during TCP. • Power delivered during each impulse is less than 1/1000 of that delivered during defibrillation. • Chest compressions (CPR) can be administered directly over the insulated electrodes while pacing. Inadvertent contact with the active pacing surface results in only a mild shock. • stopping pacing during CPR will minimize inappropriate stimulation of the patient due to electrical artifacts. 13
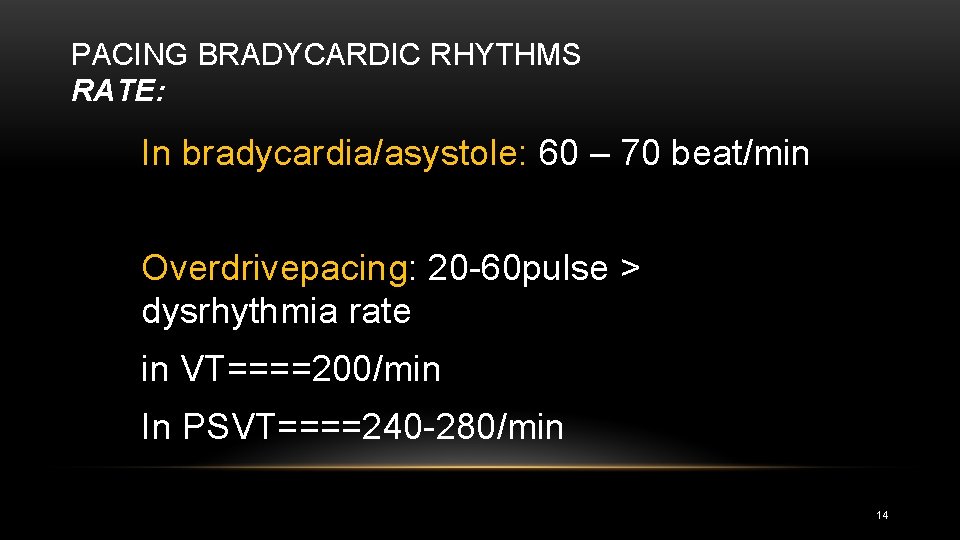
PACING BRADYCARDIC RHYTHMS RATE: In bradycardia/asystole: 60 – 70 beat/min Overdrivepacing: 20 60 pulse > dysrhythmia rate in VT====200/min In PSVT====240 280/min 14

PACING BRADYCARDIC RHYTHMS OUTPUT(CURRENT): • In the setting of bradyasystolic arrest, it is reasonable to turn the stimulating current to maximal output and then decrease the output as appropriate after capture is achieved • Clinicians should slowly increase the output from minimal settings until capture is achieved in patients with a hemodynamically compromising bradycardia who are not in cardiac arrest 15
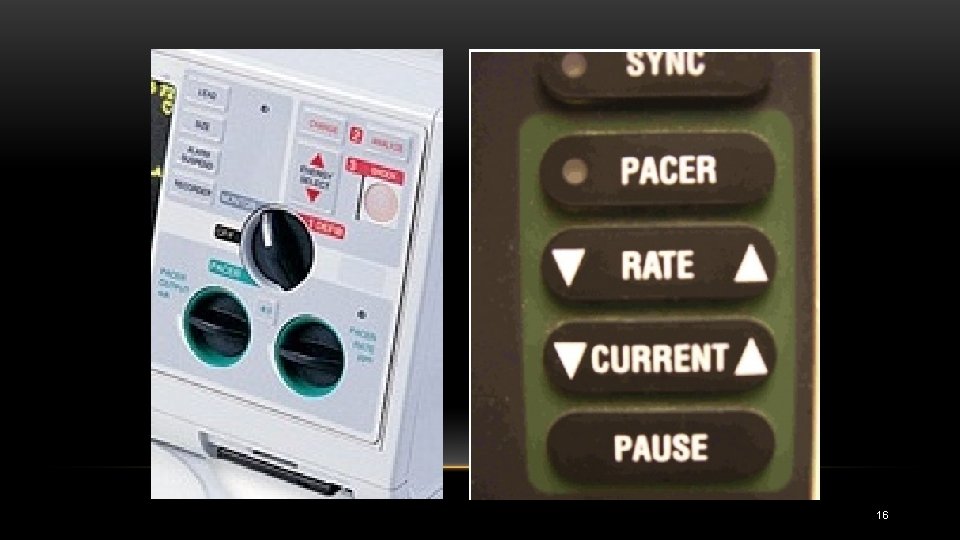
16

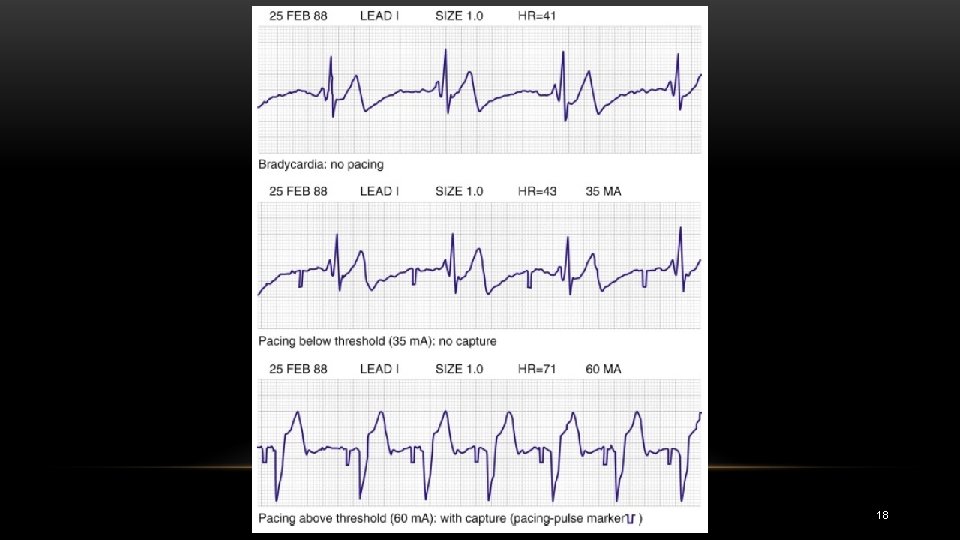
CAPTURE • Electrical capture can be made by monitoring the electrocardiogram on the filtered monitor of the pacing unit • Mechanical capture is assessed by palpating the pulse. • palpating the femoral pulse may be easier 17
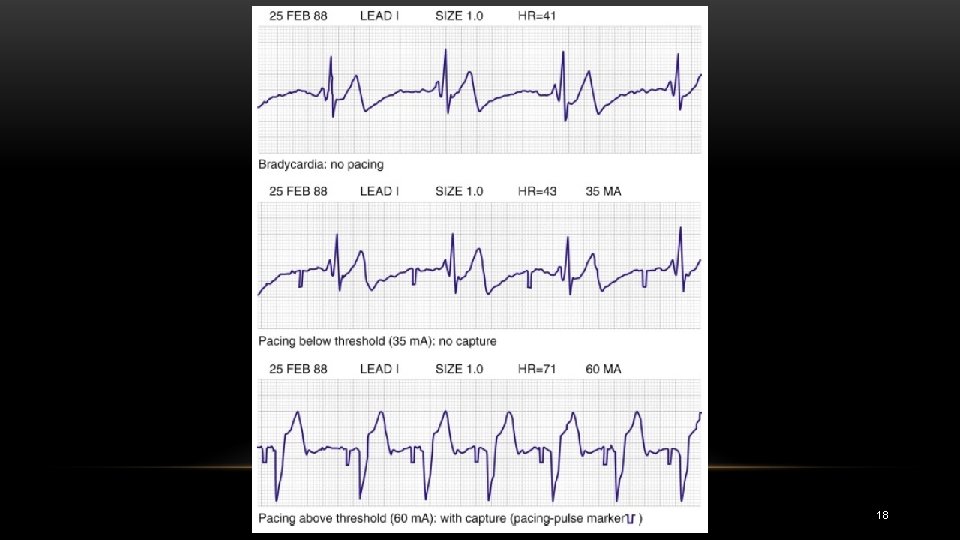
18
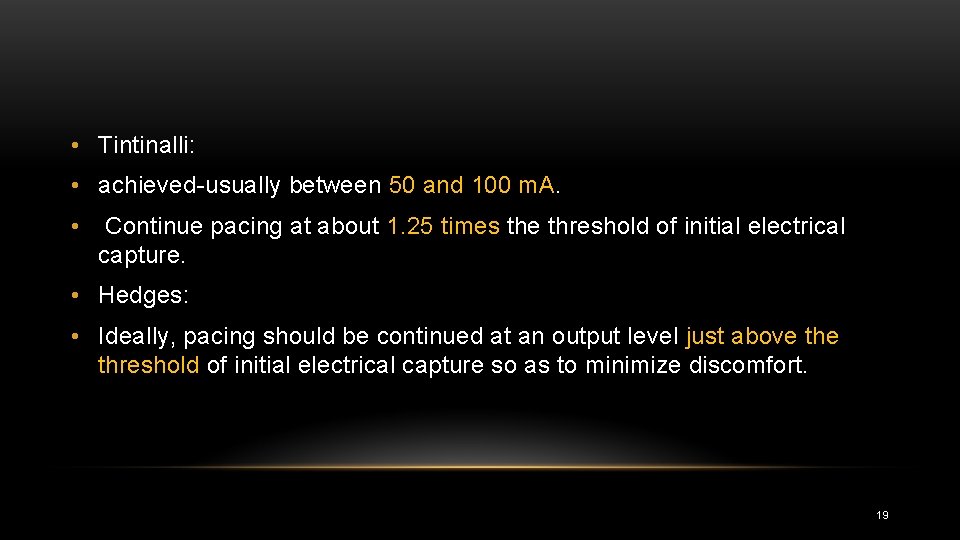
• Tintinalli: • achieved usually between 50 and 100 m. A. • Continue pacing at about 1. 25 times the threshold of initial electrical capture. • Hedges: • Ideally, pacing should be continued at an output level just above threshold of initial electrical capture so as to minimize discomfort. 19

• Transcutaneous pacing may be fixed rate (asynchronous) or demand (synchronous). • Asynchronous pacing delivers an electrical impulse at a regular interval without regard to intrinsic cardiac pacemaker activity. • This creates the risk of precipitating a dysrhythmia… 20
FAILURE TO CAPTURE WITH TRANSCUTANEOUS PACING: • Faulty electrical contact, • Electrode placement, • Patient size, • Underlying path ology. • Recheck lead connections, skin electrode contact, and electrode placement. • Rule out pneumothorax, pericardial effusion or tamponade, severe myocardial ischemia, and metabolic derangements. 21
FAILURE TO CAPTURE WITH TCP • may be related to electrode placement or patient size. • barrel shaped chests • large amounts of intrathoracic air conduct electricity poorly… • the scarring associated with thoracotomy • A large pericardial effusion • Failure to electrically capture with a transcutaneous device in these settings is an indication to consider immediate transvenous pacer placement 22
CONSCIOUS PATIENTS • Analgesia : Fentanyl • Sedation: BZD 23
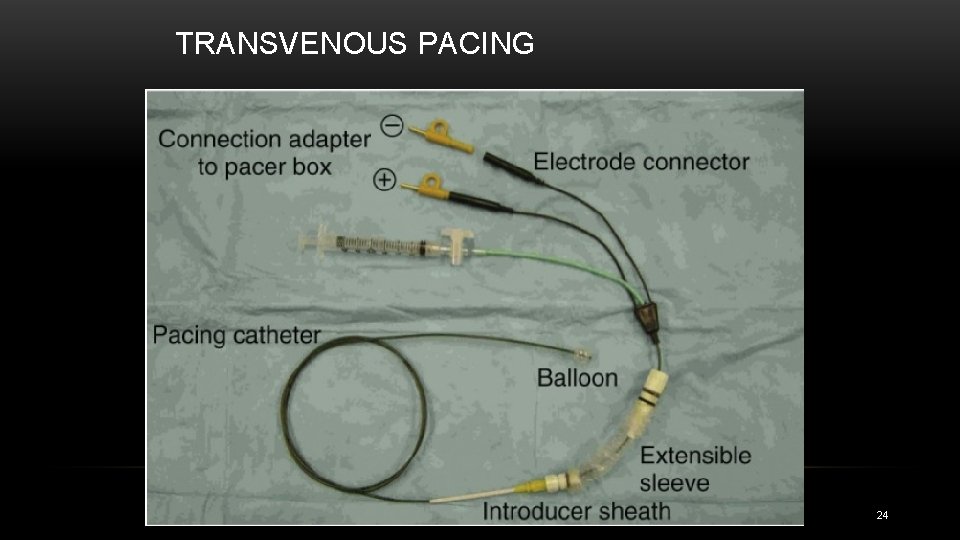
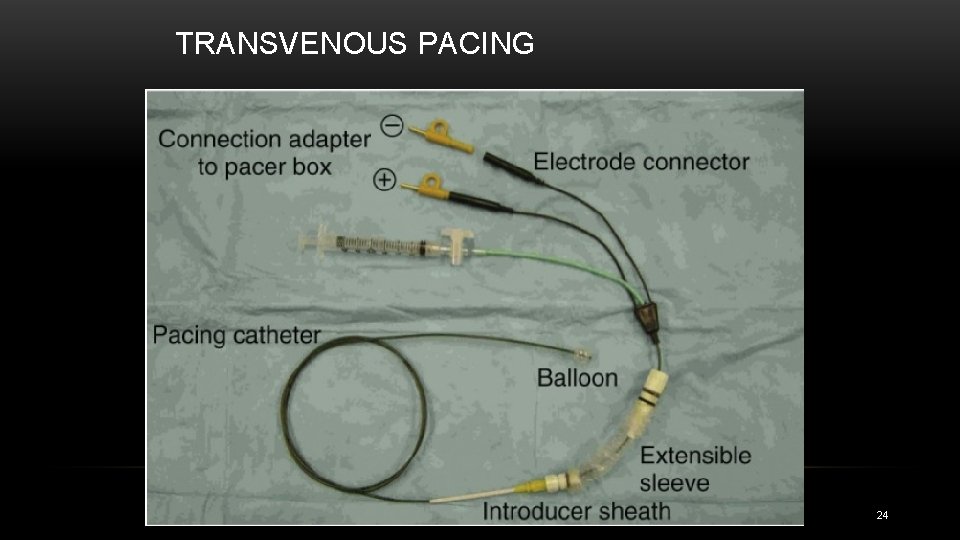
TRANSVENOUS PACING 24
25
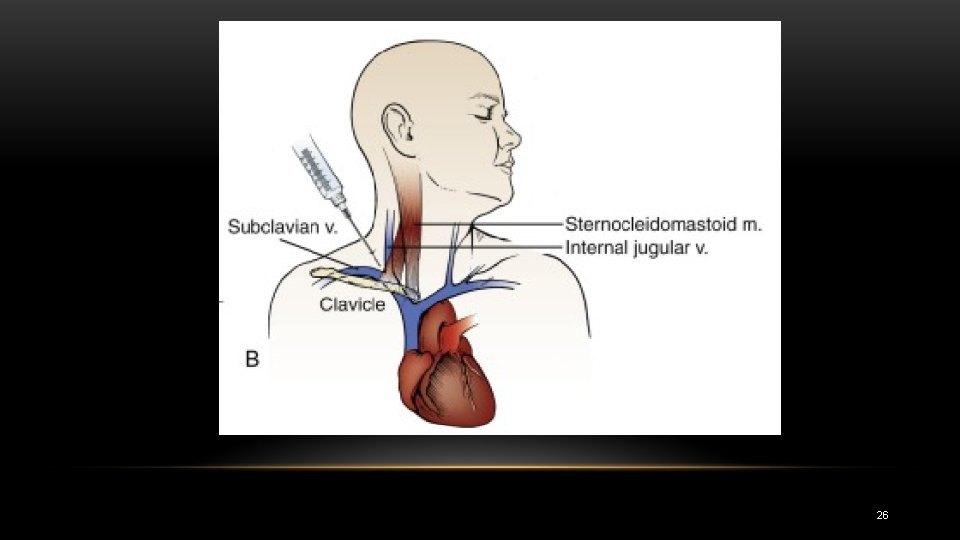
26

27
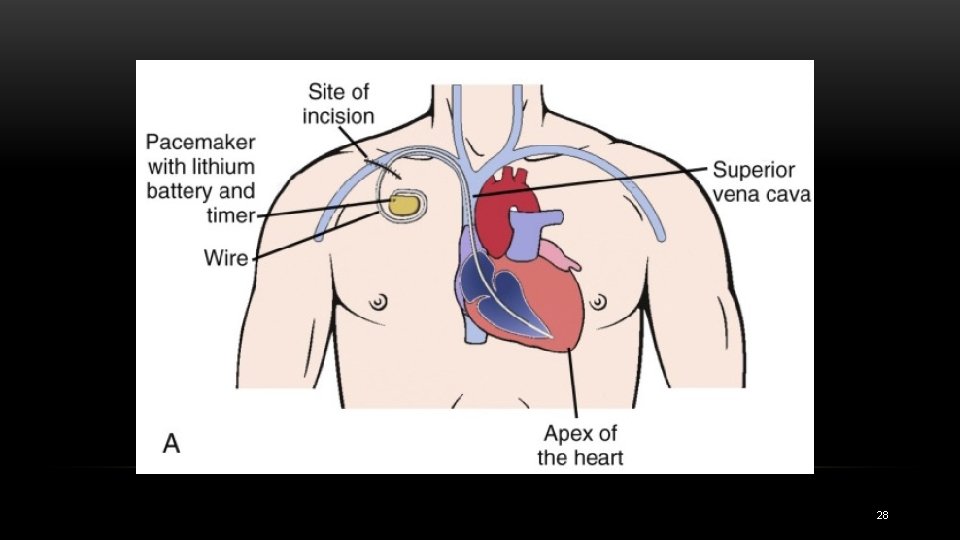
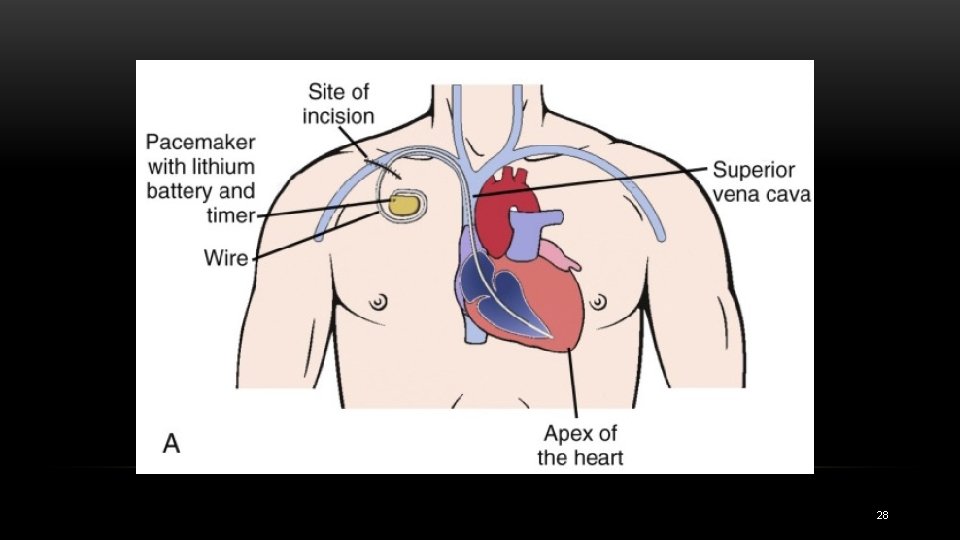
28

CONTRAINDICATIONS • Prosthetic tricuspid valve is generally considered to be an absolute contraindication to transvenous cardiac pacing. • Severe hypothermia IS RELATIVE 29
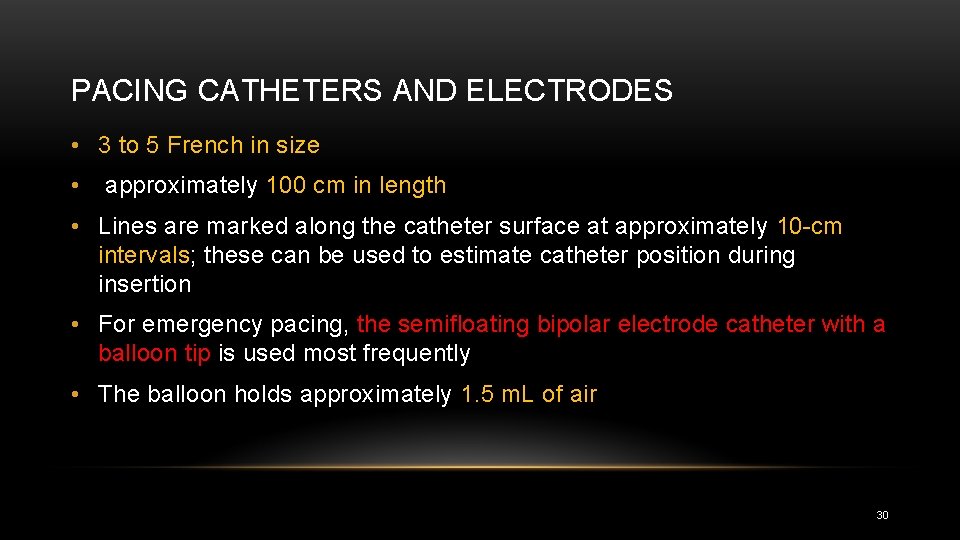
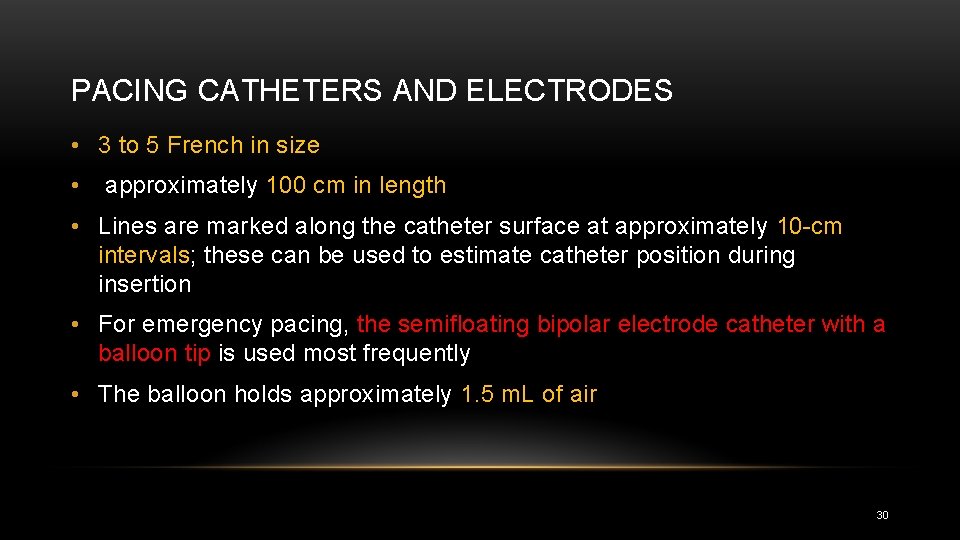
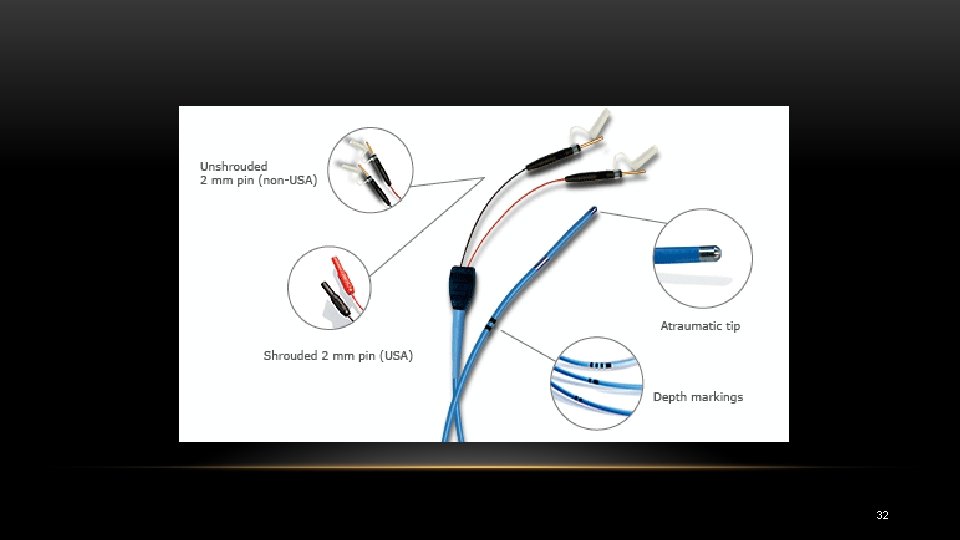
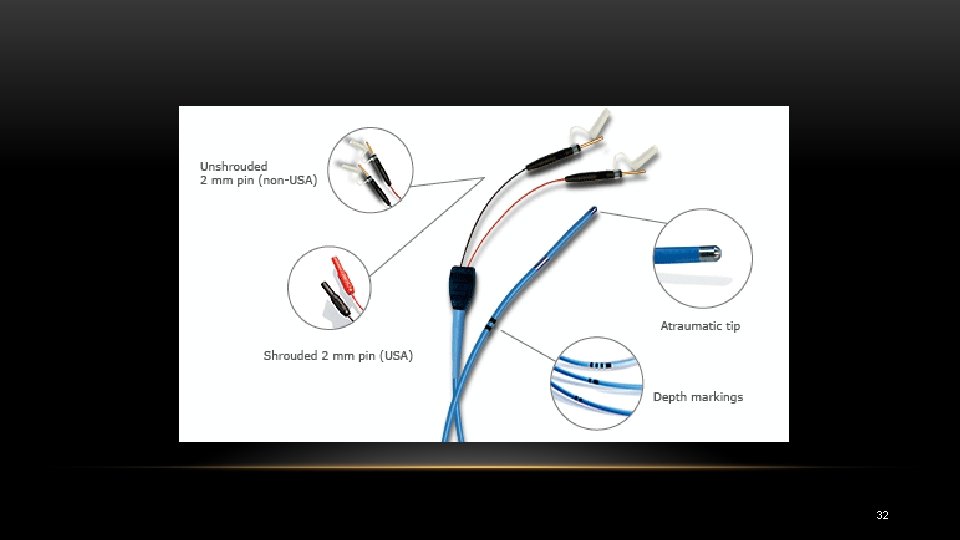
PACING CATHETERS AND ELECTRODES • 3 to 5 French in size • approximately 100 cm in length • Lines are marked along the catheter surface at approximately 10 cm intervals; these can be used to estimate catheter position during insertion • For emergency pacing, the semifloating bipolar electrode catheter with a balloon tip is used most frequently • The balloon holds approximately 1. 5 m. L of air 30
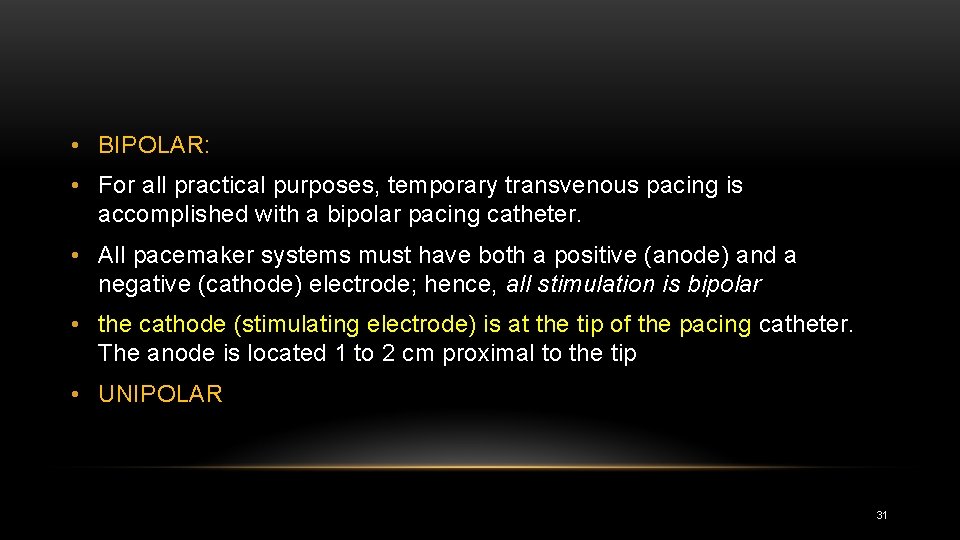
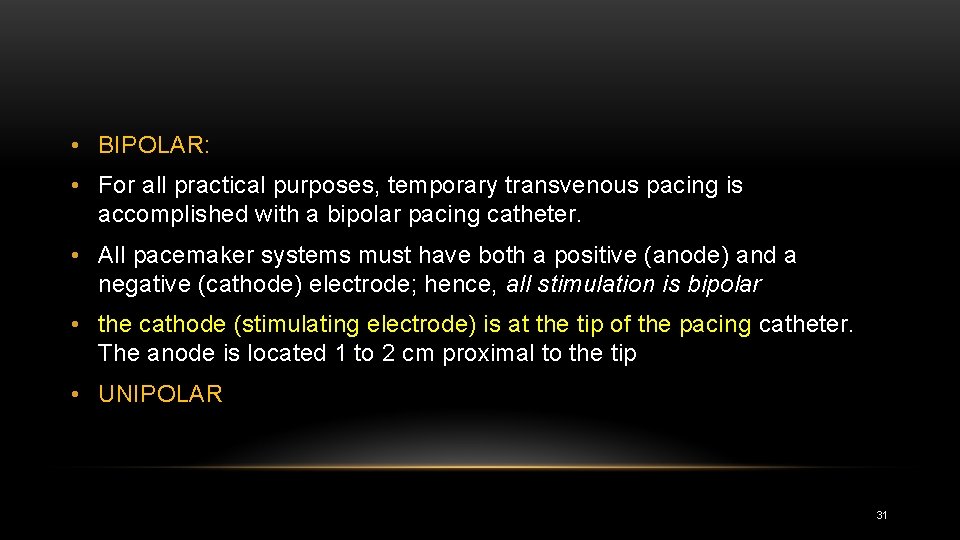
• BIPOLAR: • For all practical purposes, temporary transvenous pacing is accomplished with a bipolar pacing catheter. • All pacemaker systems must have both a positive (anode) and a negative (cathode) electrode; hence, all stimulation is bipolar • the cathode (stimulating electrode) is at the tip of the pacing catheter. The anode is located 1 to 2 cm proximal to the tip • UNIPOLAR 31
32
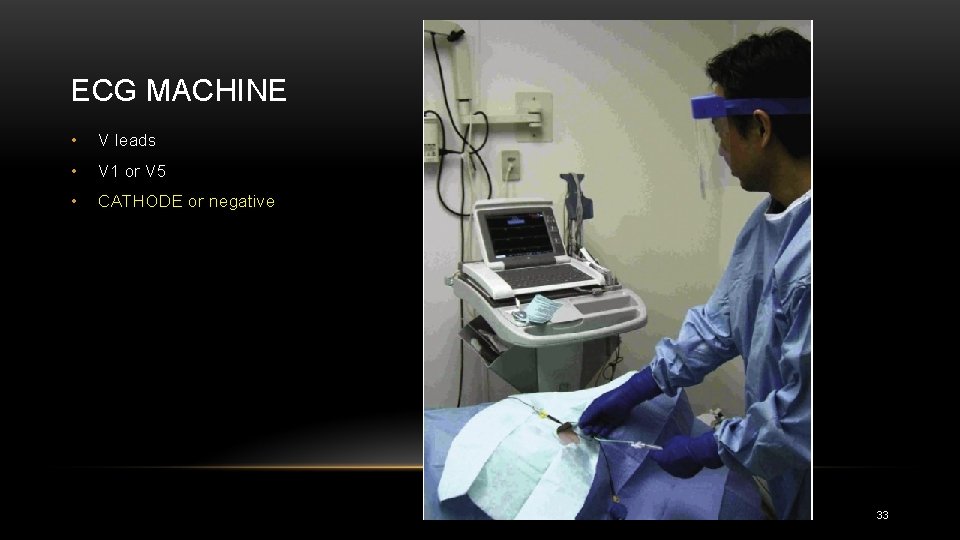
ECG MACHINE • V leads • V 1 or V 5 • CATHODE or negative 33
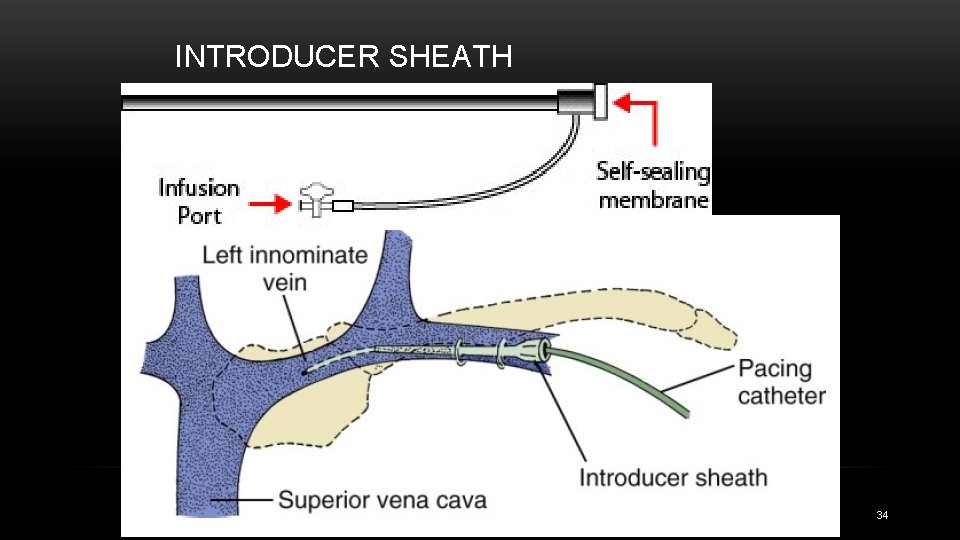
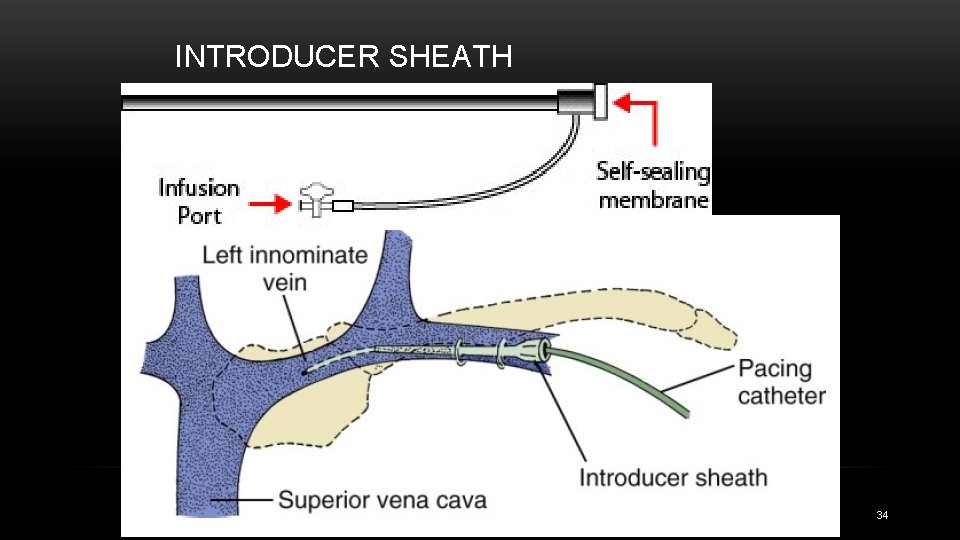
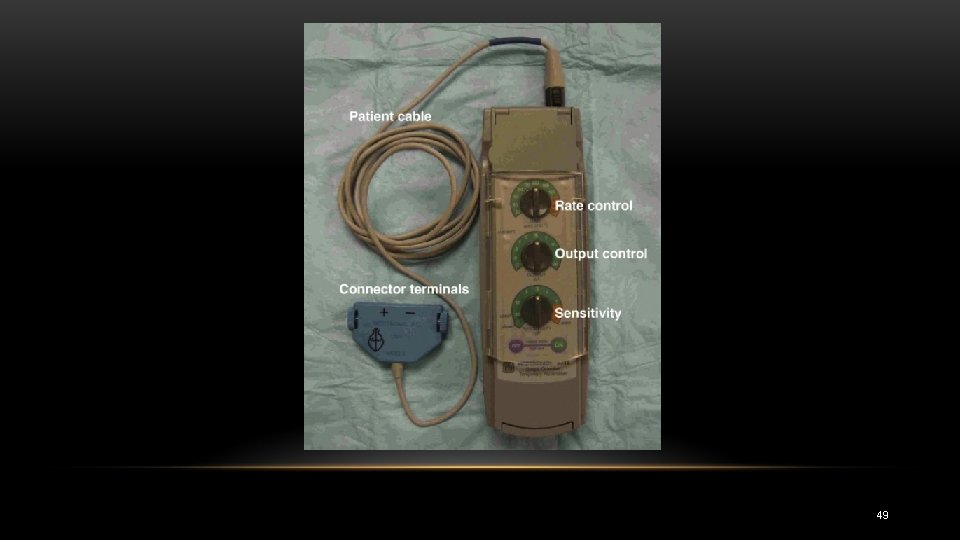
INTRODUCER SHEATH 34
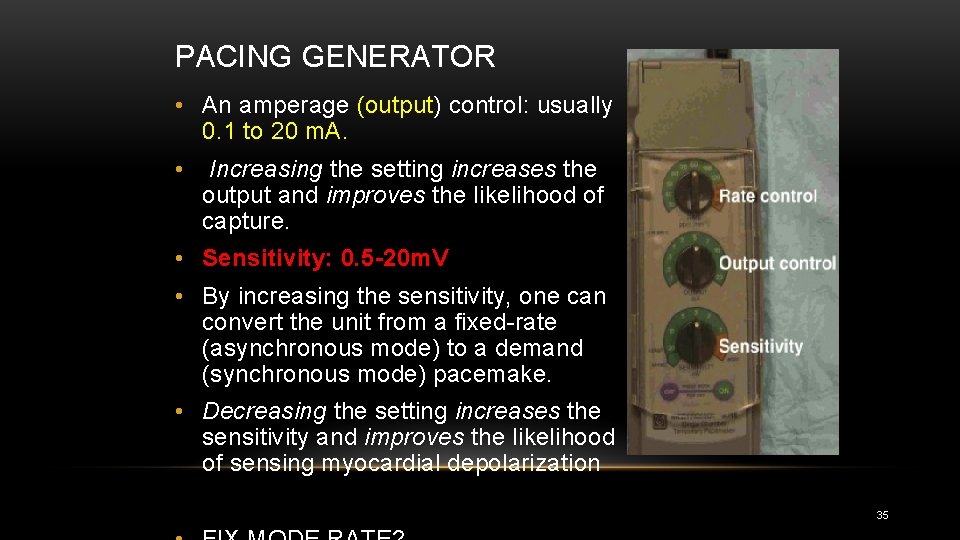
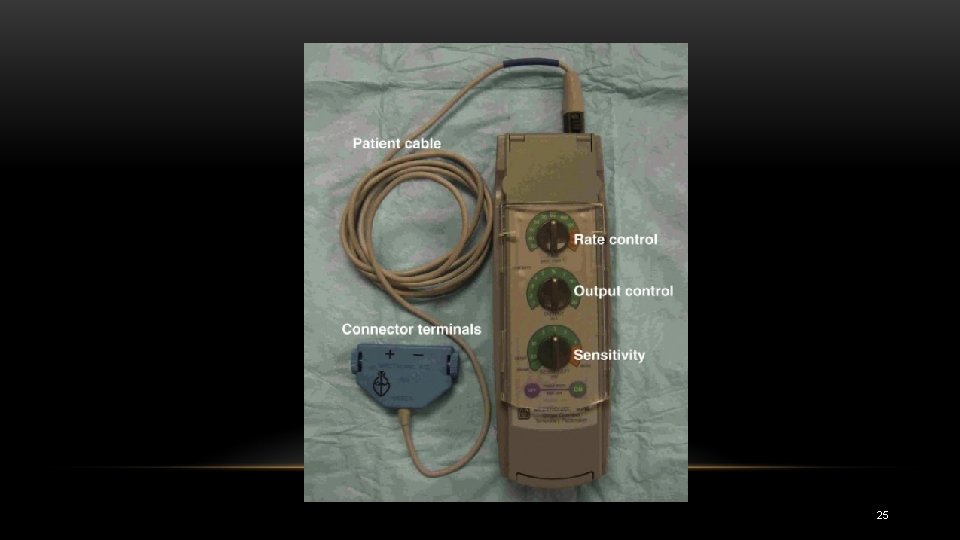
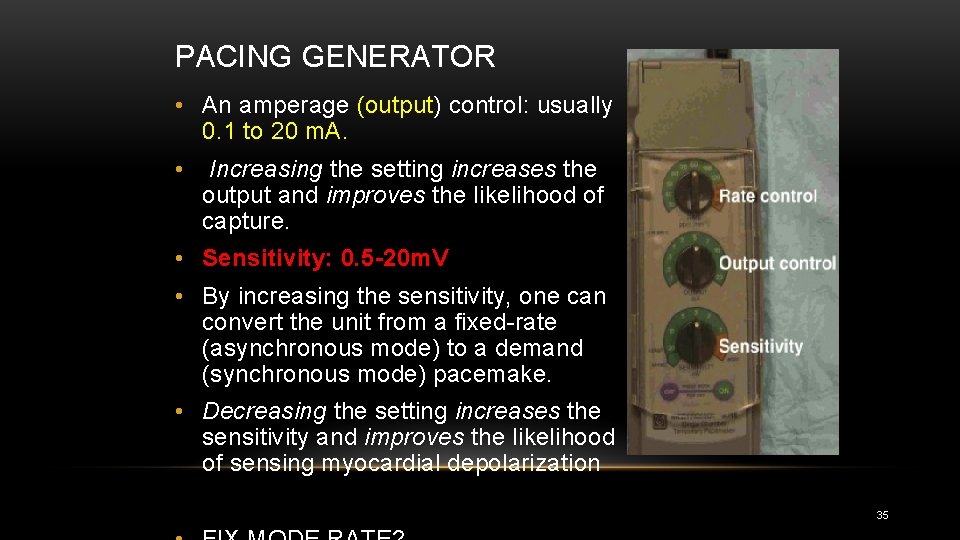
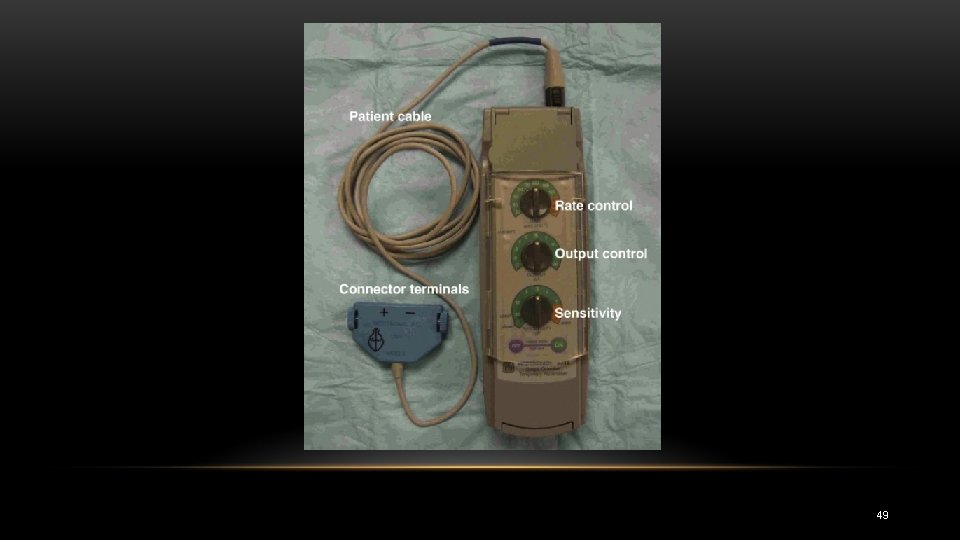
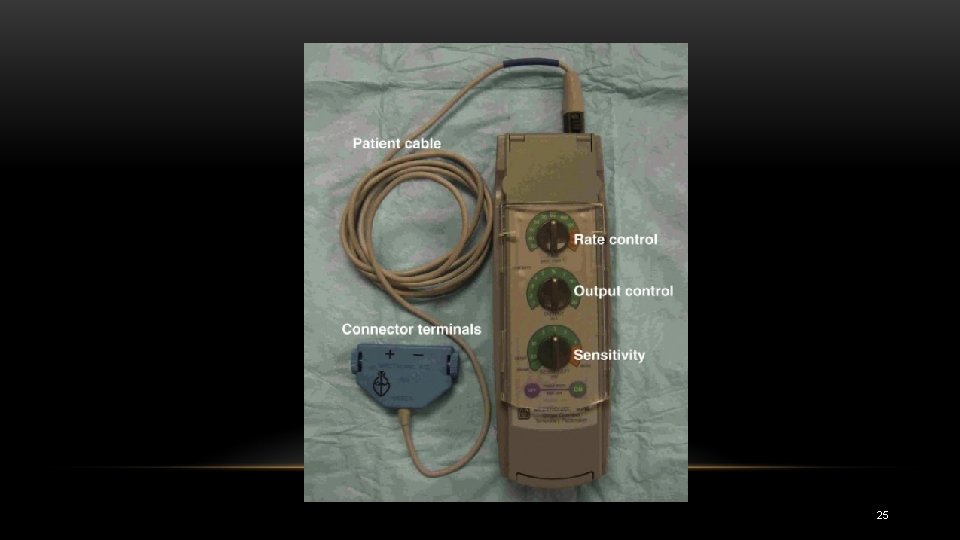
PACING GENERATOR • An amperage (output) control: usually 0. 1 to 20 m. A. • Increasing the setting increases the output and improves the likelihood of capture. • Sensitivity: 0. 5 -20 m. V • By increasing the sensitivity, one can convert the unit from a fixed rate (asynchronous mode) to a demand (synchronous mode) pacemake. • Decreasing the setting increases the sensitivity and improves the likelihood of sensing myocardial depolarization 35
PATIENT PREPARATION • Patient instruction is an extremely important aspect of any procedure • sufficient information should be provided so that the patient feels at ease • Patients should be assured that they will feel no discomfort after the venipuncture site has been anesthetized and that they will feel better when the catheter is in place and is functional. • Continued reassurance is required during the procedure • Sedation and analgesia should be considered when appropriate 36
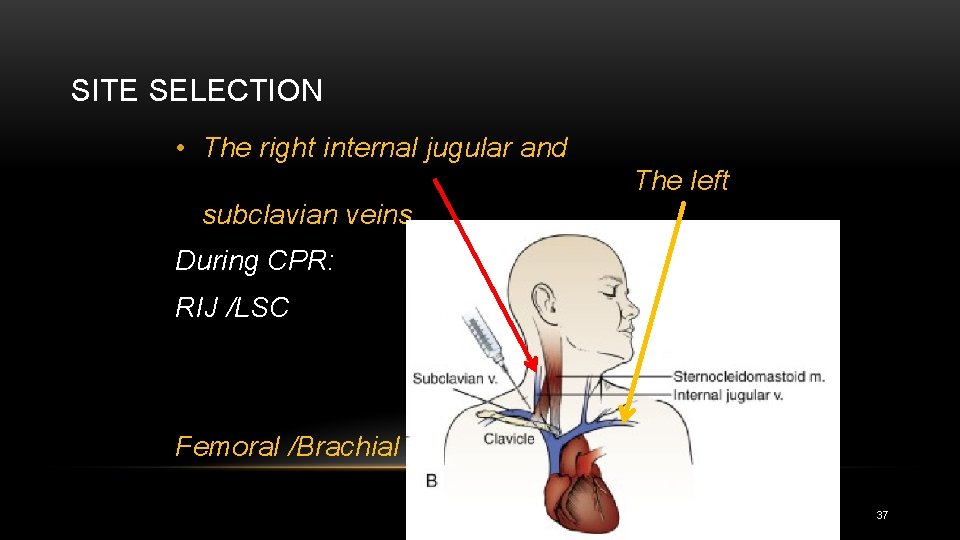
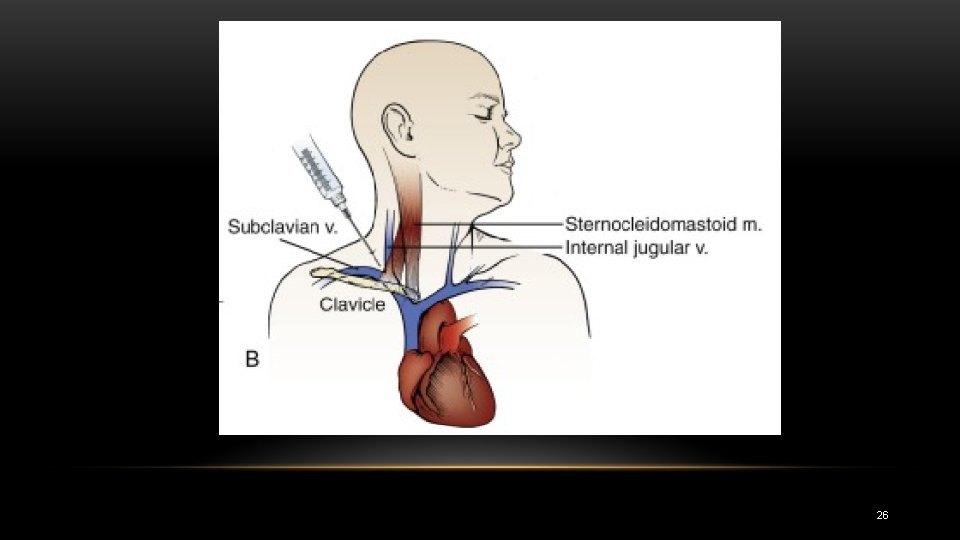
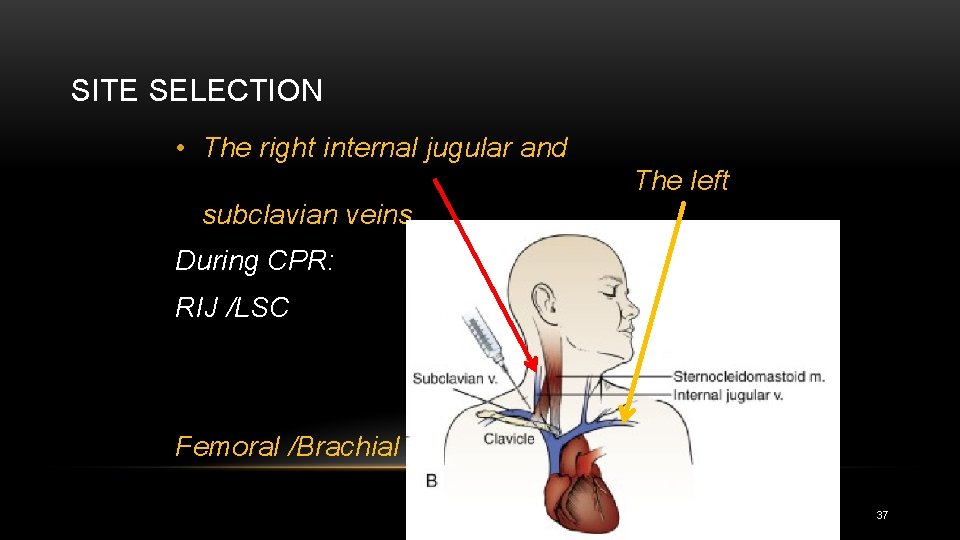
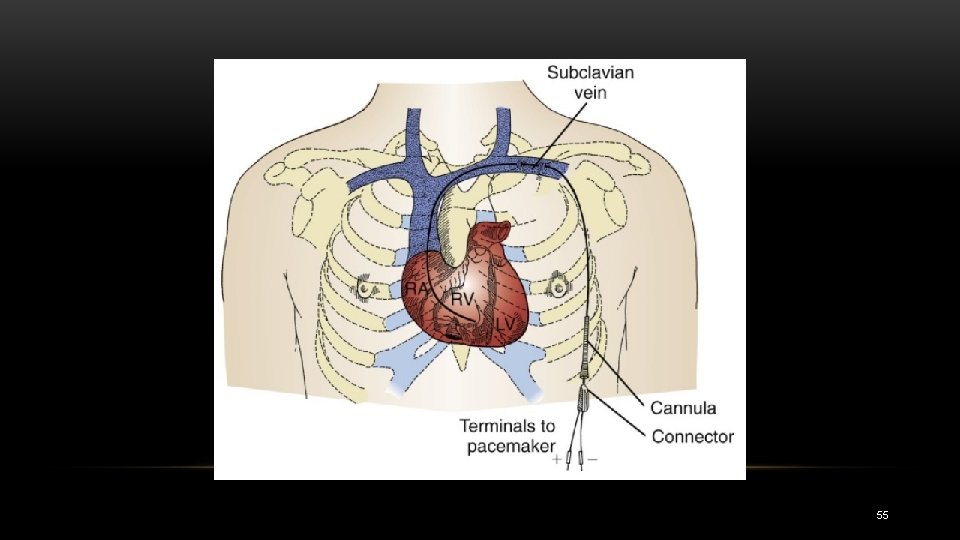
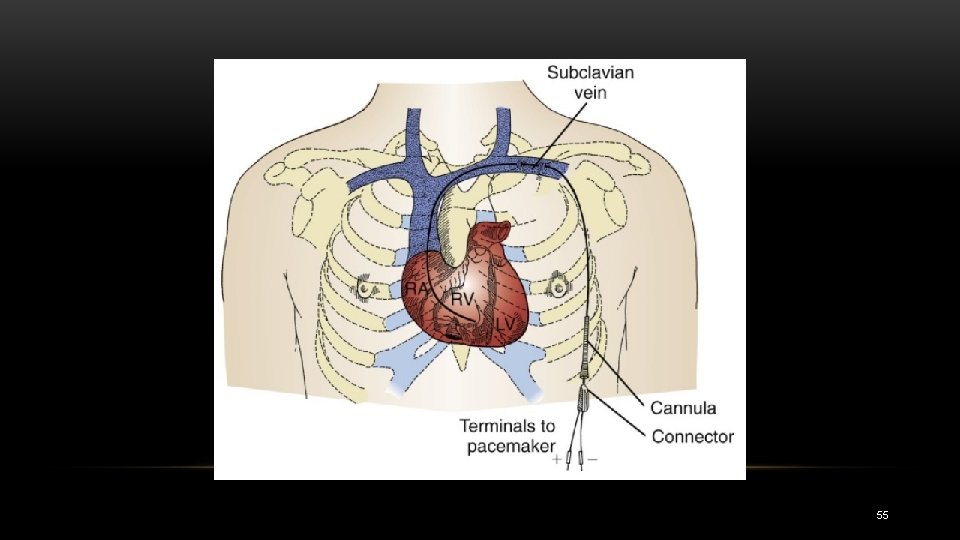
SITE SELECTION • The right internal jugular and The left subclavian veins During CPR: RIJ /LSC Femoral /Brachial 37
SITE …. • In some centers, a particular site is preferred for permanent transvenous pacemaker placement, and if possible, this site should be avoided for temporary placement 38

PACEMAKER PLACEMENT • Venous access • ECG guidance? 39

40
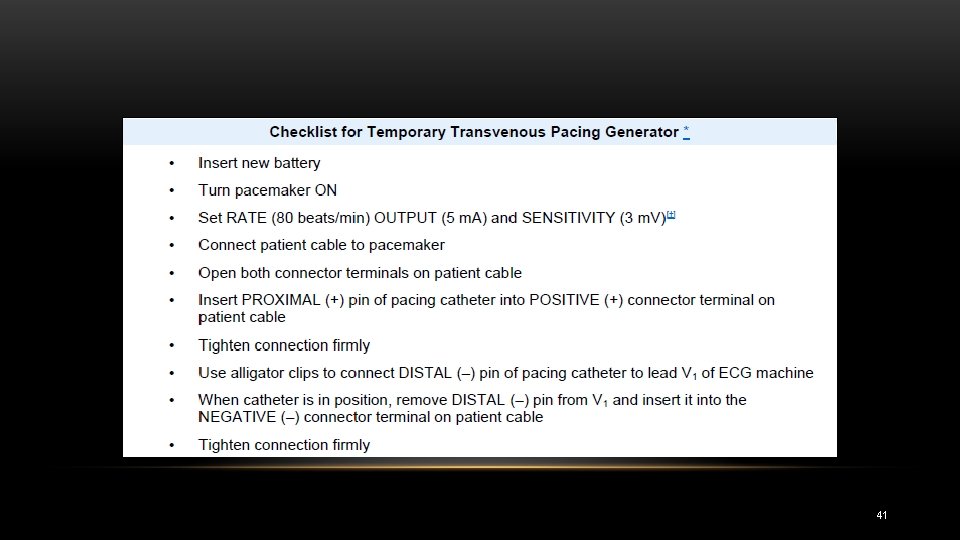
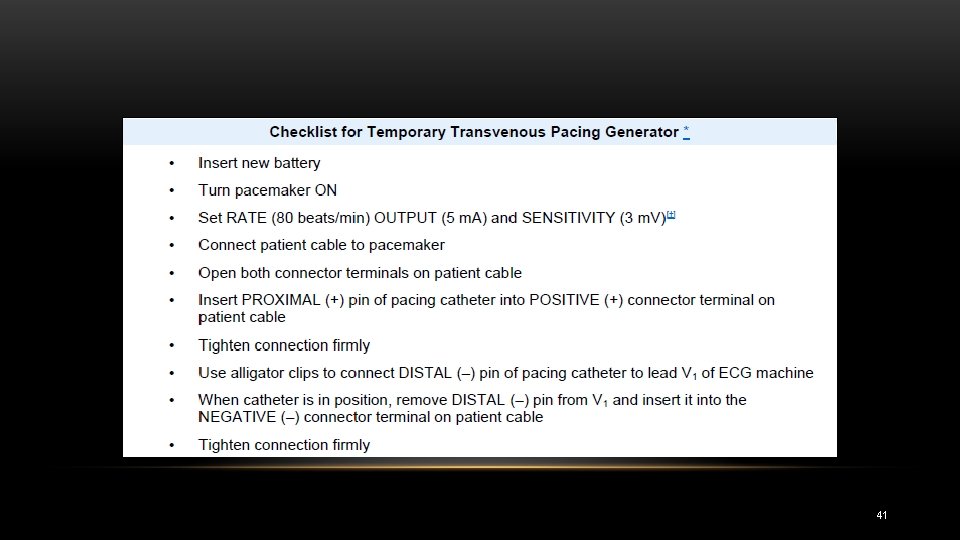
41
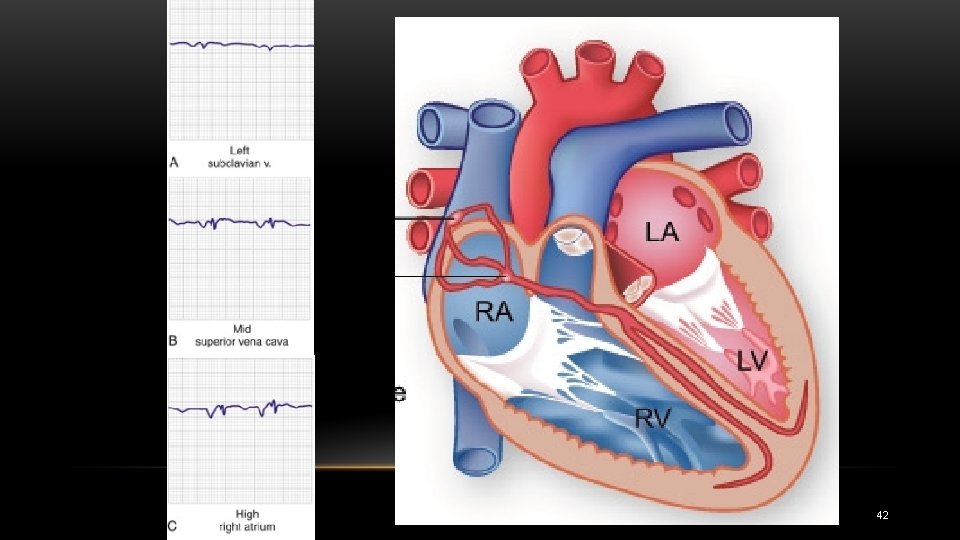
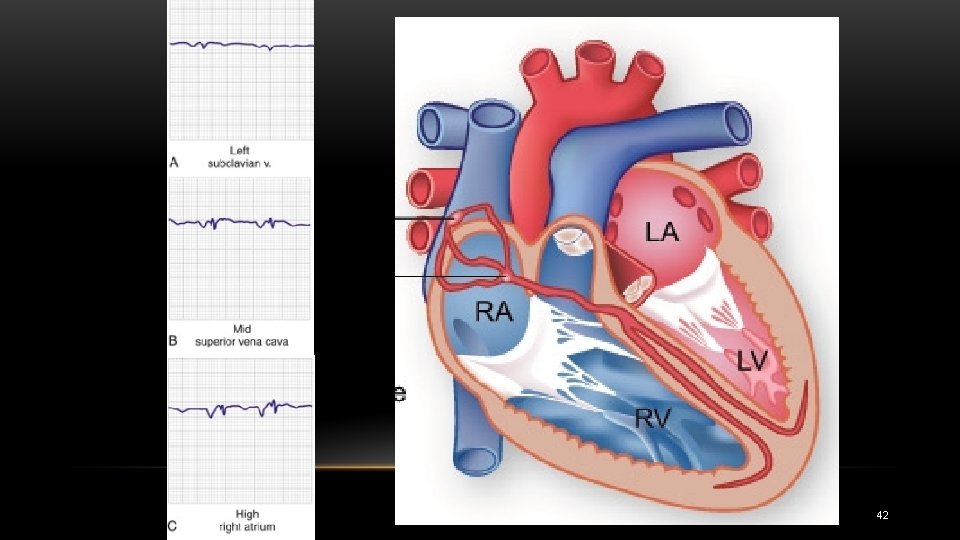
42
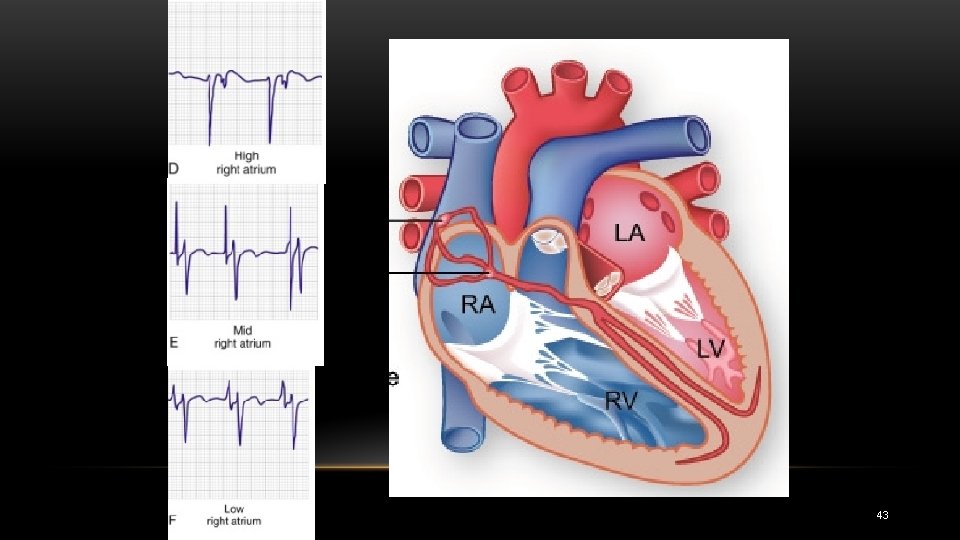
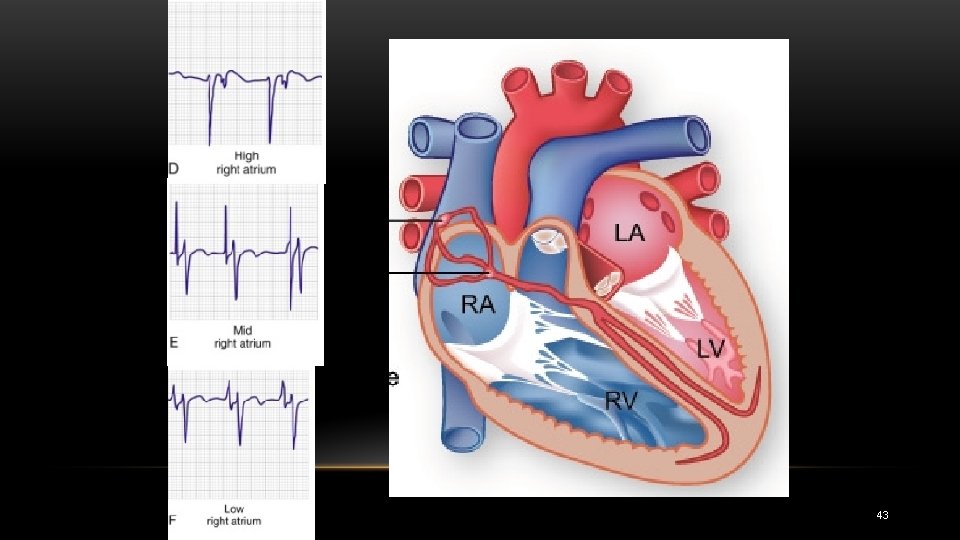
43

44

45
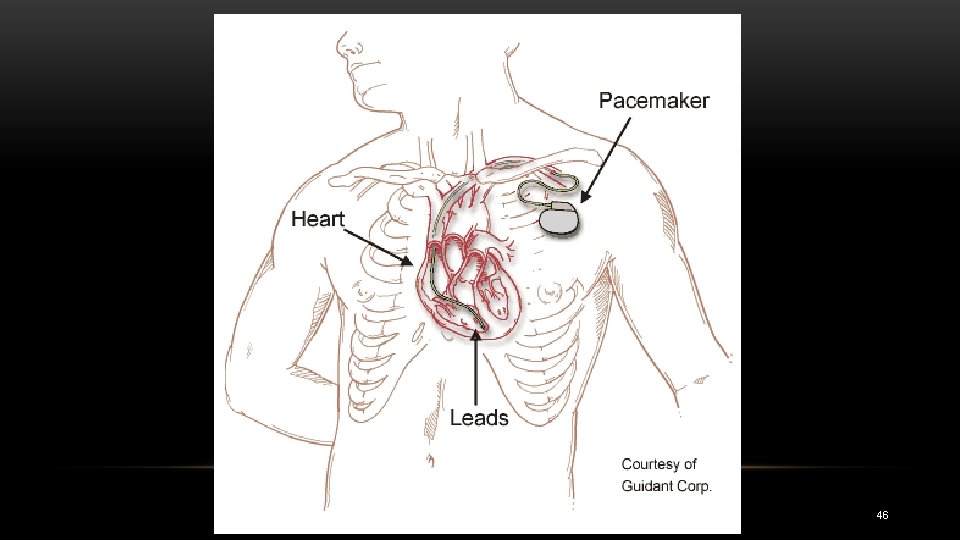
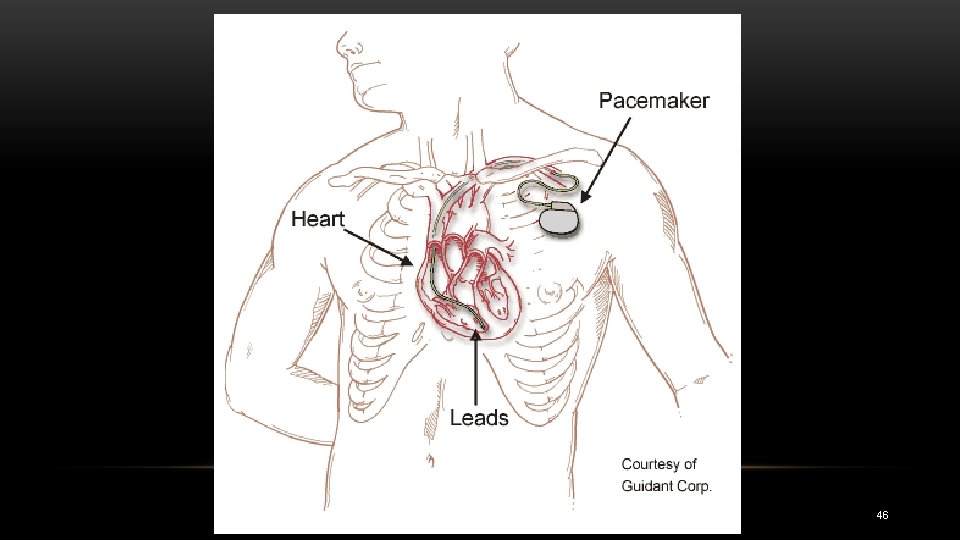
46
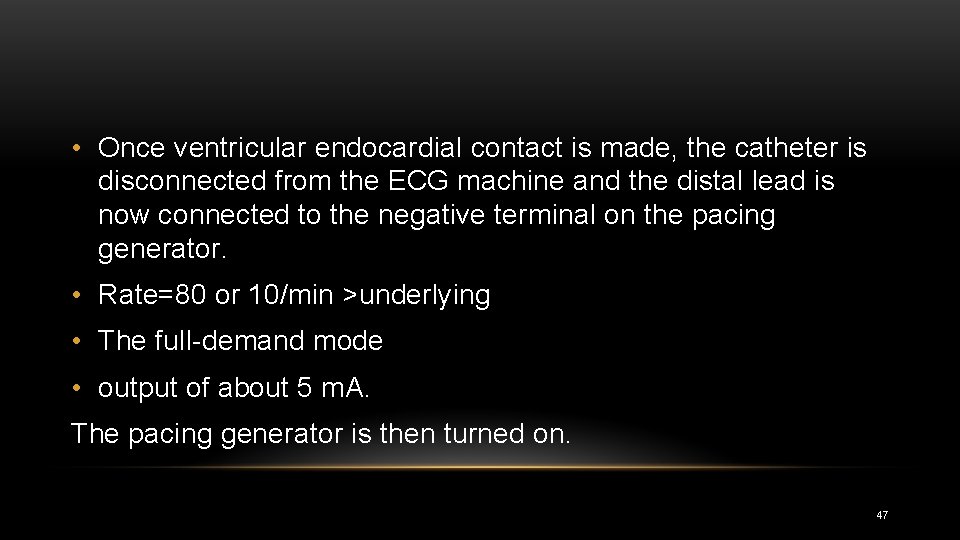
• Once ventricular endocardial contact is made, the catheter is disconnected from the ECG machine and the distal lead is now connected to the negative terminal on the pacing generator. • Rate=80 or 10/min >underlying • The full demand mode • output of about 5 m. A. The pacing generator is then turned on. 47
• MOVIES 1, 2 48
49
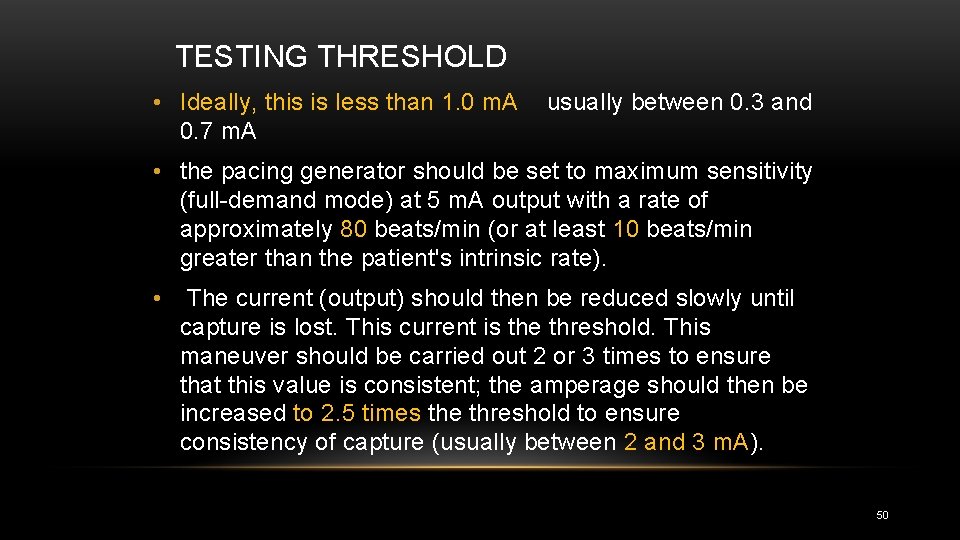
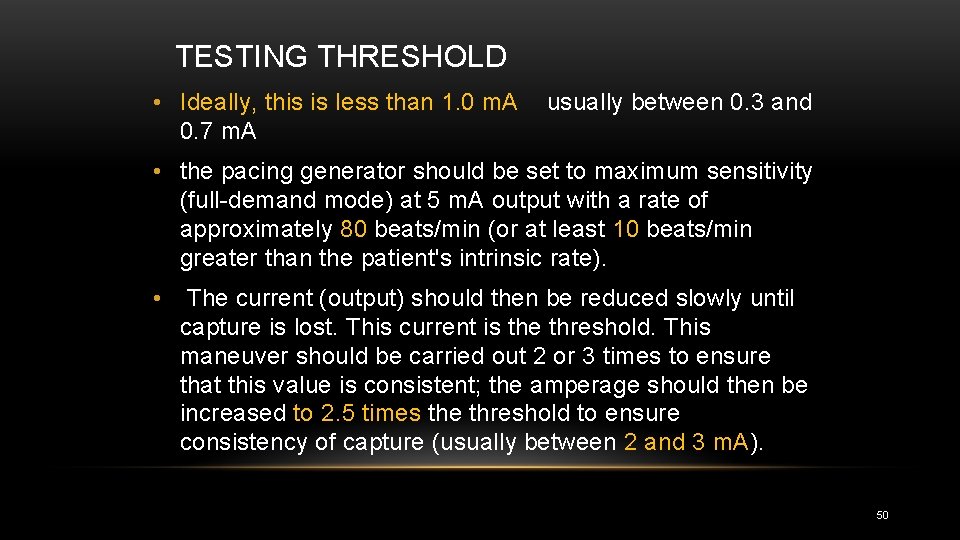
TESTING THRESHOLD • Ideally, this is less than 1. 0 m. A 0. 7 m. A usually between 0. 3 and • the pacing generator should be set to maximum sensitivity (full demand mode) at 5 m. A output with a rate of approximately 80 beats/min (or at least 10 beats/min greater than the patient's intrinsic rate). • The current (output) should then be reduced slowly until capture is lost. This current is the threshold. This maneuver should be carried out 2 or 3 times to ensure that this value is consistent; the amperage should then be increased to 2. 5 times the threshold to ensure consistency of capture (usually between 2 and 3 m. A). 50
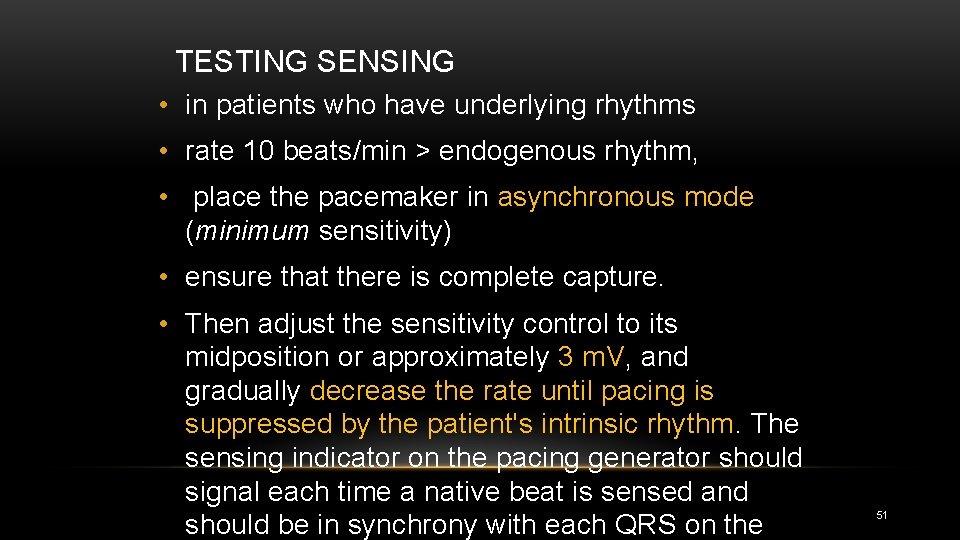
TESTING SENSING • in patients who have underlying rhythms • rate 10 beats/min > endogenous rhythm, • place the pacemaker in asynchronous mode (minimum sensitivity) • ensure that there is complete capture. • Then adjust the sensitivity control to its midposition or approximately 3 m. V, and gradually decrease the rate until pacing is suppressed by the patient's intrinsic rhythm. The sensing indicator on the pacing generator should signal each time a native beat is sensed and should be in synchrony with each QRS on the 51

• If the pacer fails to sense the intrinsic rhythm, increase the sensitivity (decrease the millivolts) until the pacer is suppressed. • Conversely, if the sensing indicator is triggered by P or T waves or by artifact, decrease the sensitivity until only the QRS is sensed. Once the sensitivity threshold is determined, • set the millivoltage to about half of that value. 52
• The patient should be assessed for electrical and mechanical capture • THEN ECG, and chest radiographs 53
• If catheter induced ectopy develops, the catheter should be slightly withdrawn until the ectopy stops; then it should be readvanced. • Occasionally, an antidysrhythmic drug such as lidocaine may need to be given to desensitize the myocardium. 54
55

FLUOROSCOPY GUIDED PACE INSERTION 56

57
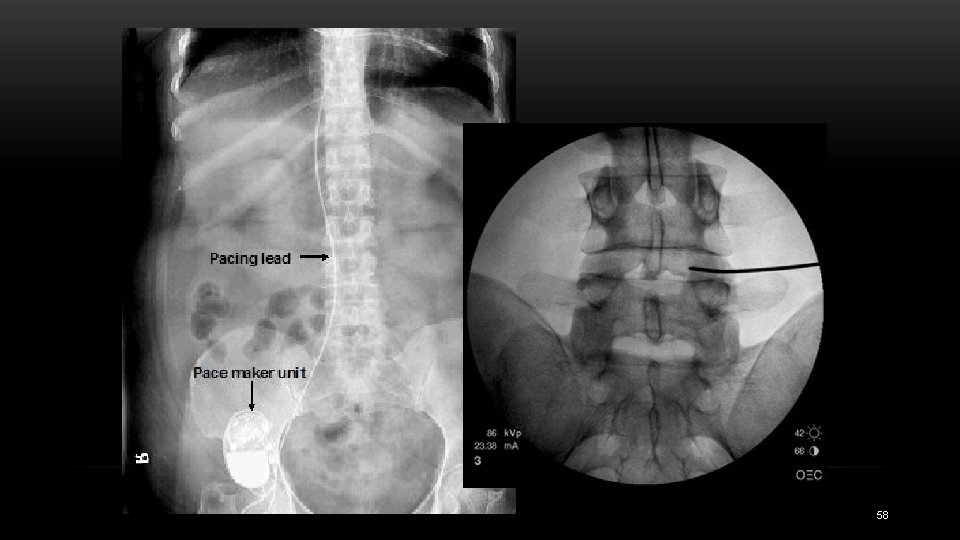
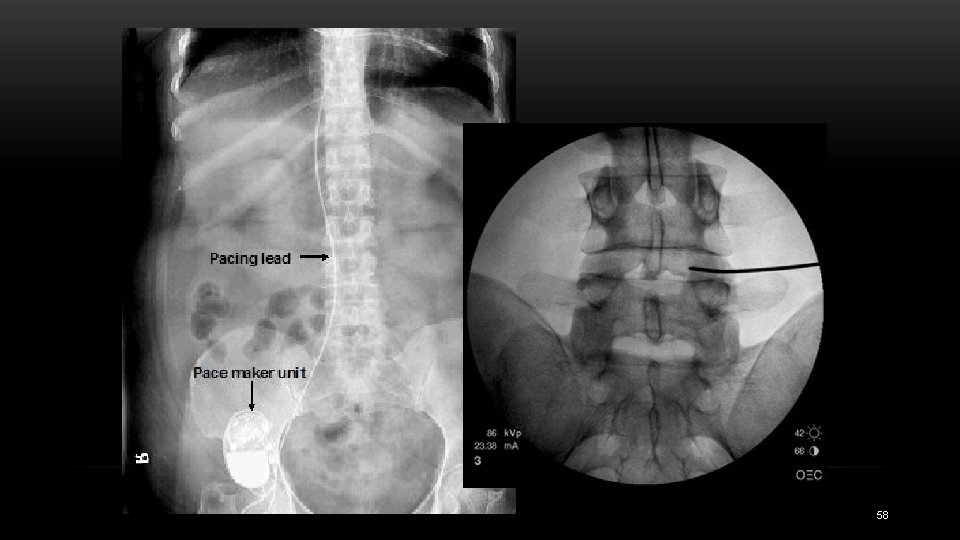
58
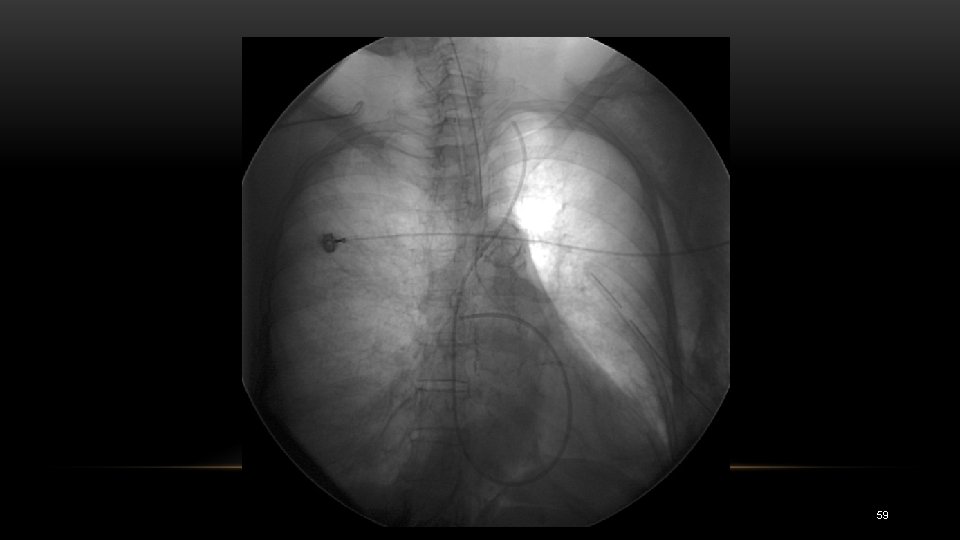
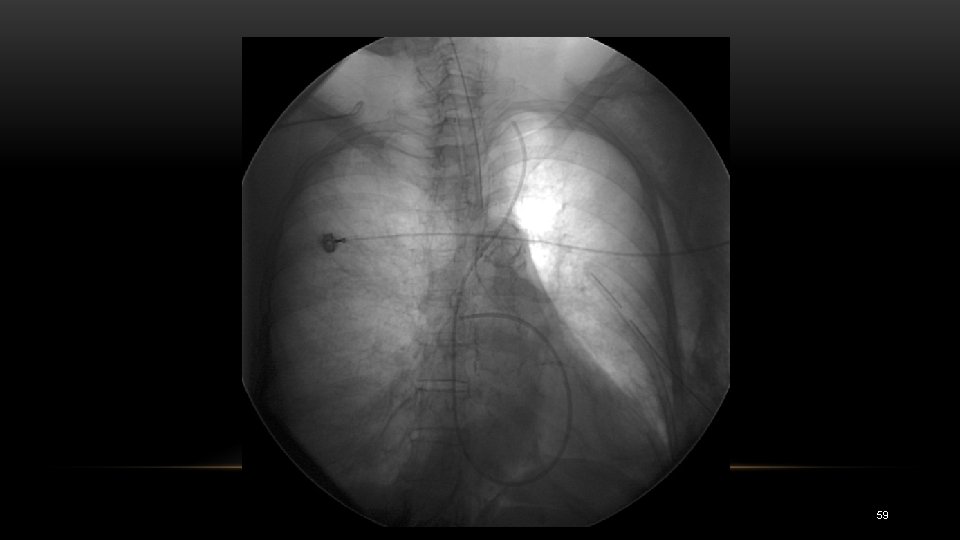
59
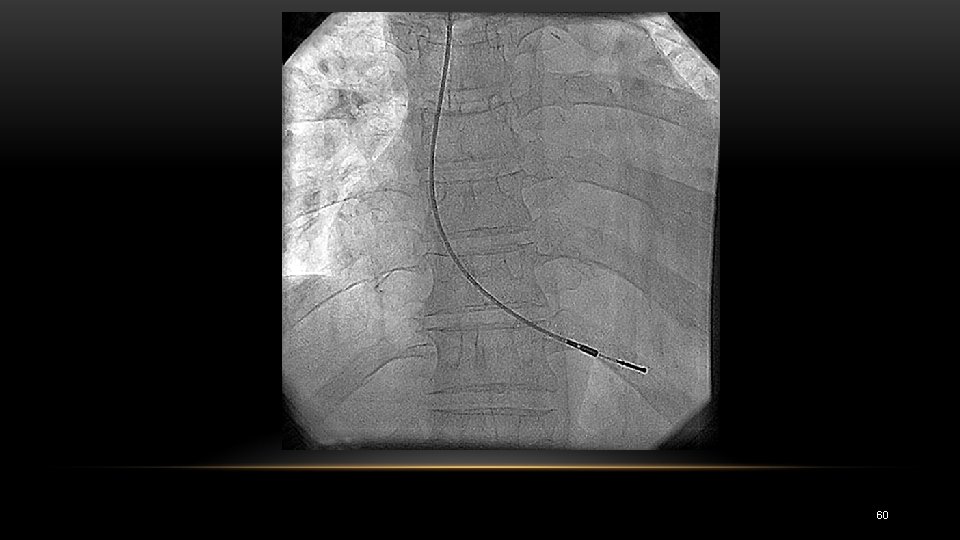
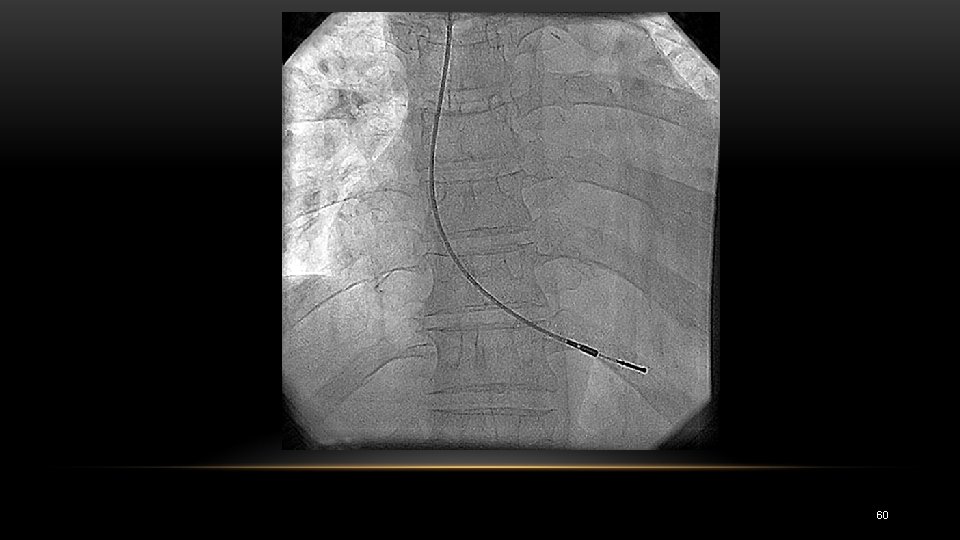
60