Emergence Delirium in Pediatric Patients Updated May 2019
- Slides: 34
Emergence Delirium in Pediatric Patients Updated May 2019 Valerie Au, M. D. Andrew Infosino, M. D. Department of Anesthesia and Perioperative Care University of California, San Francisco
Disclosures No relevant financial relationships
Learning Objectives • Recognize emergence delirium in pediatric patients in the recovery room and differentiate it from agitation due to pain. • Compare and contrast the PAED, Cravero and Watcha numerical scales for rating emergence delirium • Identify the risk factors for emergence delirium in pediatric patients • Describe approaches for reducing the incidence of emergence delirium • Develop an algorithm for treating emergence delirium in the recovery room
Emergence Delirium: What is it? Dissociated state of consciousness after anesthesia • Crying, thrashing, kicking, uncooperative • Incoherent, inconsolable and combative • No eye contact, no recognition familiar objects, parents or caregivers of
Emergence Delirium: What is it? • Occurs in 10 – 20% of children who have anesthetics 1 • Most common from age 2 – 5 years 1 • Emergence delirium usually lasts from 3 – 45 minutes with a mean duration of 14 minutes 2 • 90 – 95% of cases resolve by themselves in less than 30 minutes 3 1. Cote C, A Practice of Anesthesia for Infants and Children 6 e 2. Voepel-Lewis et al. , Anesth Analg 2003; 96: 1625 -30 3. Lee CJ et al. , Korean J Anesthesiol 2010; 59: 75 -81
Emergence Delirium: Why is it a problem? • Can harm parents or caregivers • Can harm themselves • Can pull out IVs, pull off monitors and remove dressings
Emergence Delirium: What is the impact? • Requires increased nursing resources • Additional medication administration • Longer recovery room stays and increased costs • Frightening to parents • Decreased parental satisfaction scores • Post-operative behavioral changes
Emergence Delirium: What is the impact? Post-operative behavioral changes • • • Increased general anxiety Problems with separation Sleep disturbances Bedwetting Temper tantrums Eating disturbances
Differentiating Emergence Delirium (ED) from post-operative pain • Both can be difficult to assess in preverbal children and preschoolers • Both present similarly with crying, thrashing and inconsolability • ED can occur after non-painful procedures such as MRIs
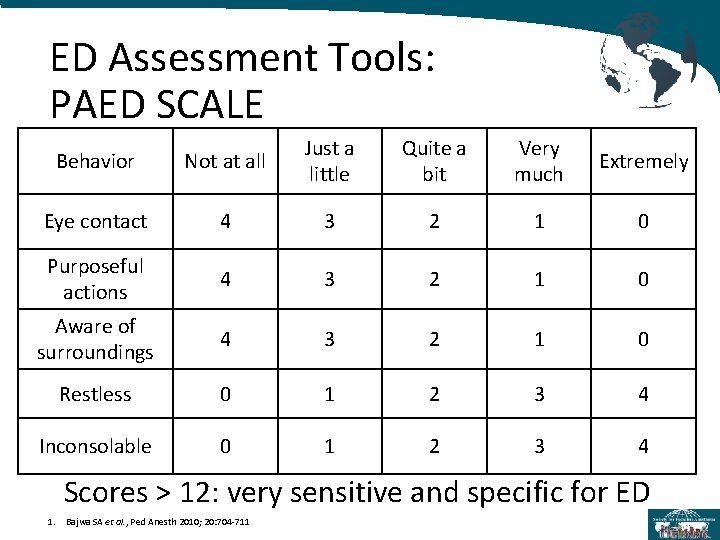
How Do You Measure Emergence Delirium? • Simple screening tools for PACU nursing, but with low specificity for distinguishing delirium from agitation/pain • Watcha Scale • Cravero Scale • More complex validated scale with higher specificity for delirium • PAED Scale
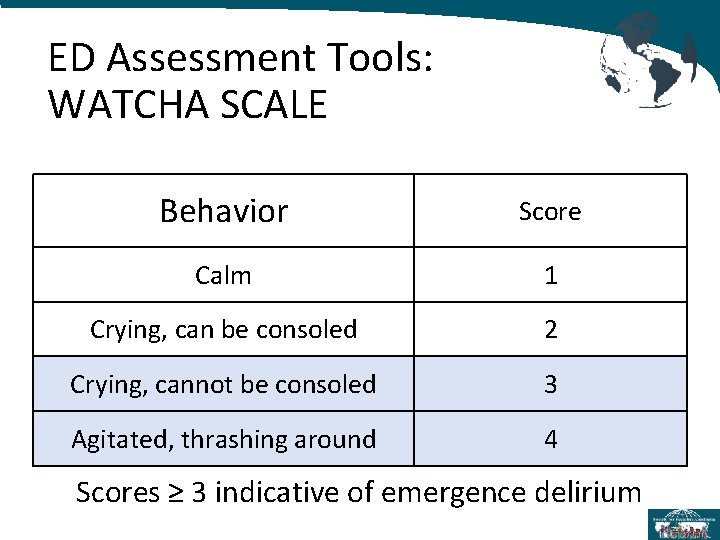
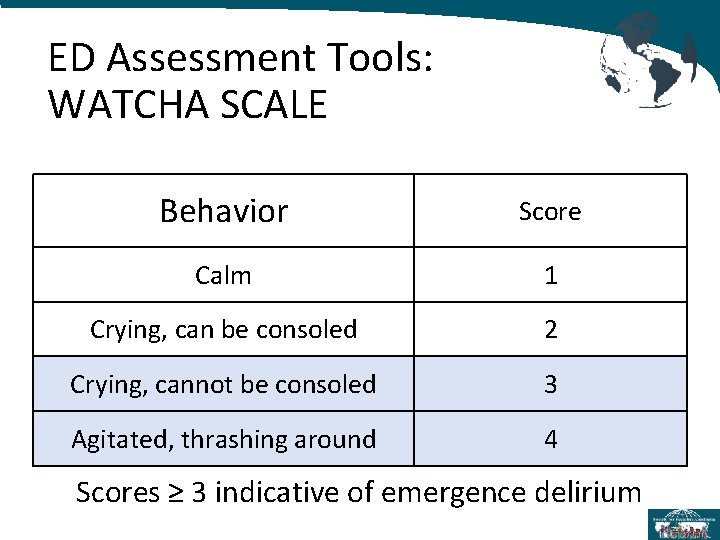
ED Assessment Tools: WATCHA SCALE Behavior Score Calm 1 Crying, can be consoled 2 Crying, cannot be consoled 3 Agitated, thrashing around 4 Scores ≥ 3 indicative of emergence delirium
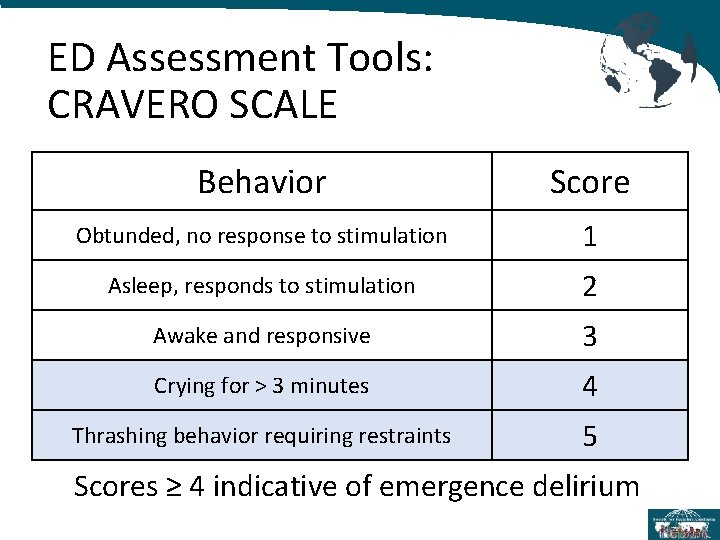
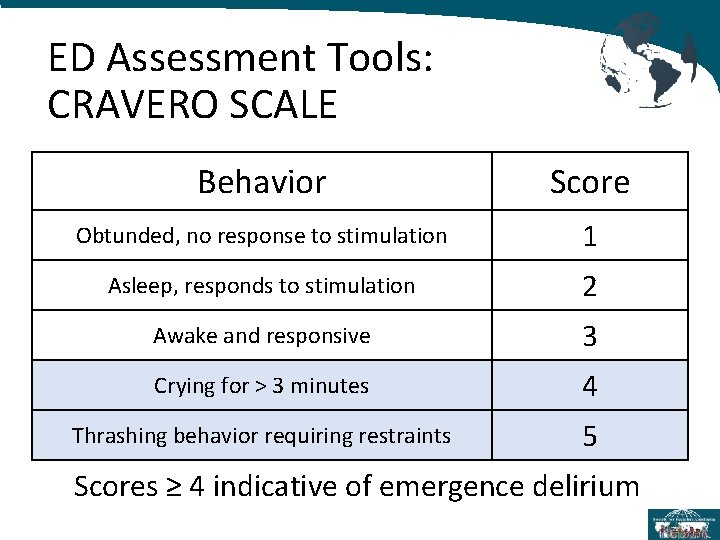
ED Assessment Tools: CRAVERO SCALE Behavior Score Obtunded, no response to stimulation 1 Asleep, responds to stimulation 2 Awake and responsive 3 Crying for > 3 minutes 4 Thrashing behavior requiring restraints 5 Scores ≥ 4 indicative of emergence delirium
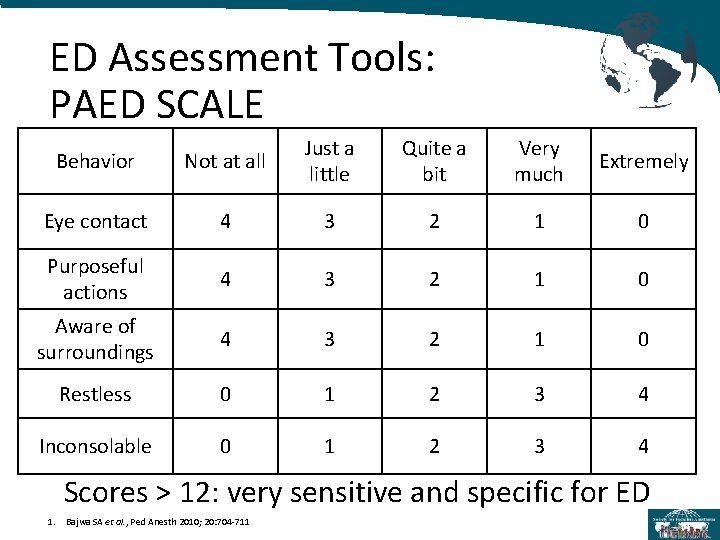
ED Assessment Tools: PAED SCALE Behavior Not at all Just a little Quite a bit Very much Extremely Eye contact 4 3 2 1 0 Purposeful actions 4 3 2 1 0 Aware of surroundings 4 3 2 1 0 Restless 0 1 2 3 4 Inconsolable 0 1 2 3 4 Scores > 12: very sensitive and specific for ED 1. Bajwa SA et al. , Ped Anesth 2010; 20: 704 -711
Question: What can we do as anesthesiologists to reduce the incidence of emergence delirium?
Answers: 1) Identify risk factors 2) Determine best anesthetic approach to decrease the incidence of ED in high risk cases
Emergence Delirium: Risk Factors • Age – highest incidence in 2 -5 year-olds 1 • Anxiety – higher incidence in preexisting anxiety of patients and/or parents 2 • Surgical factors – associated with ENT/ophthalmological procedures 3 • Volatile anesthetics 3 • Prior history of emergence delirium 1. Cote, A Practice of Anesthesia for Infants and Children 6 e 2. Kain et al. Anesth Analg 2004; 99: 1648– 1654 3. Voepel-Lewis et al. , Anesth Analg 2003; 96: 1625 -30
Treating Preoperative Anxiety • Preoperative counseling and education • Child Life services • Parental presence during induction • Distraction techniques: videos, music, video games, virtual reality headsets • Allowing the child to bring a favorite stuffed animal or blanket into the operating room • Pharmacologic preoperative anxiolysis
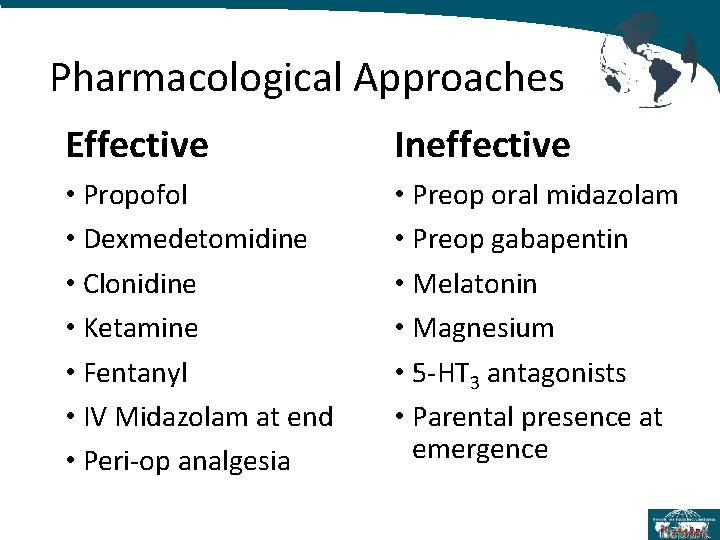
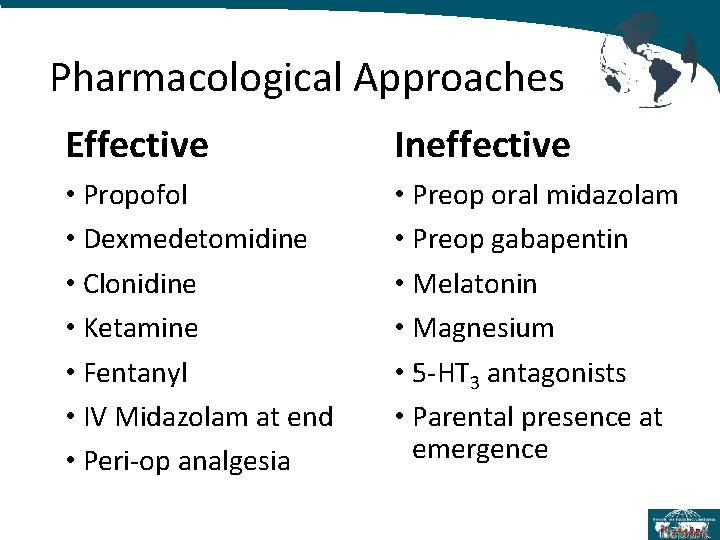
Pharmacological Approaches Effective Ineffective • Propofol • Dexmedetomidine • Clonidine • Ketamine • Fentanyl • IV Midazolam at end • Peri-op analgesia • Preop oral midazolam • Preop gabapentin • Melatonin • Magnesium • 5 -HT 3 antagonists • Parental presence at emergence
Reducing ED: Propofol • Propofol based anesthetic (induction and maintenance infusion) decreases the incidence of ED compared to either desflurane or sevoflurane 1, 2 • Propofol bolus at induction alone does not decrease the incidence of ED 1 • Propofol bolus (1 mg/kg) at the end of a sevoflurane based anesthetic decreases the incidence of ED vs placebo without lengthening recovery time 3 1. Dahmani et al, BJA, 2010; 104: 216 -23 2. Kanaya et al, J Anesth 2014; 28: 4 -11 3. Van Hoff et al, Pediatric Anesthesia, 2015; 25: 668 -76
Reducing ED: Alpha-2 Agonists • Dexmedetomidine IV bolus prior to end of a sevoflurane based anesthetic decreases the incidence of ED 1, 2, 3, 4 • Both IV bolus and infusions are effective 1 • May increase emergence, extubation and PACU times 3, 4 • Clonidine also decreases the incidence of ED 2 1. 2. 3. 4. Pickard et al, BJA, 2014; 112: 982 -90 Dahmani et al, BJA, 2010; 104: 216 -23 Zhu et al, PLo. S ONE 2015; 10(4): e 0123728 Zhang et al. , PLo. S ONE 2014; 16: e 99718
Reducing ED: Ketamine • Ketamine 6 mg/kg PO preoperatively decreases the incidence of ED 1 • Ketamine 0. 25 mg/kg IV 10 minutes prior to the end of surgery decreases the incidence of ED 2 • Does not lengthen recovery time 2 1. Kararmaz A et al. , Paediatr Anesth 2004; 14: 477 -482 2. Abu-Shawan I and Chowdary K. Pediatric Anesthesia 2007; 14: 846 -50
Reducing ED: Fentanyl prior to end of surgery decreases the incidence of ED 1, 2, 3 • Fentanyl 1 mcg/kg bolus at end of surgery effective 1 • IV and intranasal found to be effective 3 • Increase in PONV 1, 3 • Can increase in emergence time and recovery time 1, 3 1. Kim et al. , Ped Anesth 2017; 27: 885 -892 2. Dahmani et al. , BJA 2010; 104: 216 -223 3. Shi et al. , Plos One 2015 10: e 0135244
Reducing ED: Midazolam • Meta-analysis by Dahmani et al. of 4 studies demonstrated that oral midazolam does NOT decrease the incidence of ED 1 • Study by Cho et al 2 and a study by Kim et al 3 both demonstrated that IV midazolam given prior to emergence DOES decrease the incidence of ED 1. Dahmani et al. , BJA 2010; 104: 216 -223 2. Cho et al. , Anesthesiology 2014; 2010: 1354 -61 3. Kim et al. , Ped Anesth 2017; 27: 885 -892
Reducing ED: What Doesn’t Work? • • • Gabapentin Magnesium Melatonin 5 -HT 3 Antagonists Acupuncture Ketorolac 1. Dahmani et al. , BJA 2010; 104: 216 -223
A Case… A 4 year old with history of emergence delirium after a previous anesthetic presents for T & A. What should I do to decrease this patient’s risk of emergence delirium?
Recommendations For High Risk Cases • Minimize preoperative anxiety in parents and patient including nonpharmacologic techniques • Propofol based anesthetic, rather than sevoflurane • Dexmedetomidine 0. 3 – 0. 5 mcg/kg IV prior to emergence
Question: What can we do as anesthesiologists to treat emergence delirium in the recovery room?
Answers: 1. Rule out other causes of agitation in the recovery room 2. Reassure parents 3. Educate PACU nurses 4. Pharmacologic treatment
Ruling Out Other Causes • Hypoxemia – check O 2 Sat • Urinary retention – evaluate IVFs given and last void • Irritation from foley catheter • Hypoglycemia – check blood glucose in at risk patients • Pain – evaluate for pain and treat with appropriate medication (e. g. fentanyl) 29
Emergence Delirium: Treatment Tincture of Time: Remember that the vast majority of cases of of emergence delirium resolve by themselves in less than 30 minutes • Reassure parents • Educate PACU nurses and parents 30
Emergence Delirium: Treatment If emergence delirium persists in the PACU consider IV bolus of either: • • Dexmedetomidine (0. 2 -0. 4 mcg/kg) Propofol (1 -2 mg/kg) Remember to have emergency airway equipment available at the bedside 31
Conclusions • ED is a complex behavioral state that is poorly understood • ED is difficult to distinguish from agitation/pain • PAED is best current assessment tool for ED • Propofol based anesthetic with Dexmedetomidine is best approach to decrease the incidence of ED in high risk cases • Consider Dexmedetomidine or Propofol IV bolus to manage ED in PACU
References: 1. Abu-Shahwan MD, Chowdary K. Ketamine is effective in decreasing the incidence of emergence agitation in children undergoing dental repair under sevoflurane general anesthesia. Pediatric Anesthesia 2007 17: 846– 850 2. Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anesthesia in children. Pediatric Anesthesia 2010; 20: 704 -711 3. Cho EJ, Yoo SZ, Cho JE, Lee HW. Comparison of effects of 0. 03 and 0. 05 mg/kg midazolam with placebo on prevention of emergence agitation in children having strabismus surgery. Anesthesiology 2014; 210: 1354 -61 4. Cote, C, Jerrold L, Anderson Brian (2013) A Practice of Anesthesia for Infants and Children 6 e. Philadelphia, PA. Saunders 5. Dahmani S, Stany I, Brasher C, et al. Pharmacological prevention of sevoflurane and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth 2010; 104: 216– 23 6. Dahmani S, Delivet H, Hilly J. Emergence delirium in children: an update. Curr Opin Anesthesiol 2014; 27: 309– 315. 7. Kararmaz A, Kaya S, Turhanoglu S, Ozyilmaz MA. Oral ketamine premedication can prevent emergence agitation in children after desflurane anaesthesia. Paediatr Anesth 2004; 14: 477 -482 8. Kain ZN, Caldwell-Andrews AA, Maranets I, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviours. Anesth Analg 2004; 99: 1648– 1654 9. Kanaya A, Kuratani N, Satoh. D, Kurosawa S. Lower incidence of emergence agitation in children after propofol anesthesia compared with sevoflurane: a meta-analysis of randomized controlled trials. J Anesth 2014; 28: 4– 11 10. Kim KM, Lee KH, Kim YH, Ko MJ, Jun J, Kang E. Comparison of effects of intravenous midazolam and ketamine on emergence agitation in children: randomized controlled trial. J International Med Res. 2016; 44: 258– 266 11. Kim N, Park JH, Lee JS, Choi T, Kim M. Effects of intravenous fentanyl around the end of surgery on emergence agitation in children: systematic review and meta-analysis. Ped Anesth 2017; 27: 885– 892
References (cont. ): 12. Lee CJ et al. The effect of Propofol on emergence agitation in children receiving sevoflurane for adenotonsillectomy. Korean J Anesthesiol 2010: 59: 75 -81 13. Pickard A, Davies P, Birnie K, Beringer R. Systematic review and meta-analysis of the effect of intraoperative a 2 -adrenergic agonists on postoperative behavior in children. . Br J Anaesth 2014; 14. Shi F, Xiao Y, Xiong W, Zhou Q, Yang P, Huang X. Effects of fentanyl on emergence agitation in children under sevoflurane anesthesia: Meta-analysis of Randomized Controlled Trials. Plos One 2015 10: e 0135244 15. Van Hoff SL, O’Neill ES, Cohen LC, Collins BA. Does a prophylactic dose of Propofol reduce emergence agitation in children receiving anesthesia? A systematic review and meta-analysis. Paediatr Anaesth 2015; 25: 668 -76 16. Vlajkovic G, Sindjelic R. Emergence delirium in children: many questions, few answers. Anesthesia & Analgesia 2007; 104: 84 -91 17. Voepel-Lewis T, Malviya S, Tait AR. A Prospective Cohort Study of Emergence Agitation in the Pediatric Postanesthesia Care Unit. Anesth Analg 2003; 96: 1625 -30 18. Zhang C, Hu J, Liu X, Yan J. effects of intravenous dexmedetomidine on emergence agitation in children under sevoflurane anesthesia: a meta-analysis of randomized controlled trials. PLo. S ONE 2014; 16: e 99718 19. Zhu M, Wang H, Zhu A, Niu K, Wang G. Meta-Analysis of Dexmdetomidine on Emergence Agitation and Recovery Profiles in Children after Sevoflurane Anesthesia: Different Administration and Different Dosage. PLo. S ONE 2015; 10(4): e 0123728 34