Eliminating Emergency Department Ambulance to Cath Lab Transfer
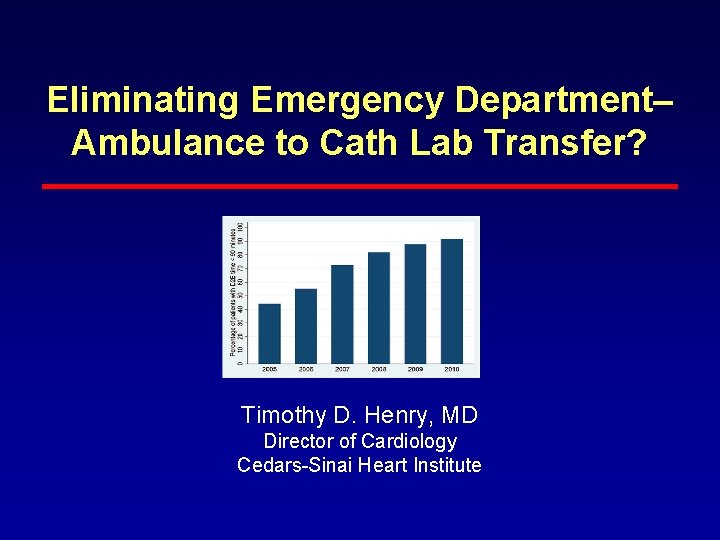
Eliminating Emergency Department– Ambulance to Cath Lab Transfer? Timothy D. Henry, MD Director of Cardiology Cedars-Sinai Heart Institute
Disclosure • No disclosure related to this presentation
Clinical Practice in 2016: Standard of Care • PCI centers should do PCI (in a timely manner <90 min) • Short distance transfer pts should have PCI (in a timely manner <120) • Long distance transfer or pts with expected delay remains an area of controversy!!
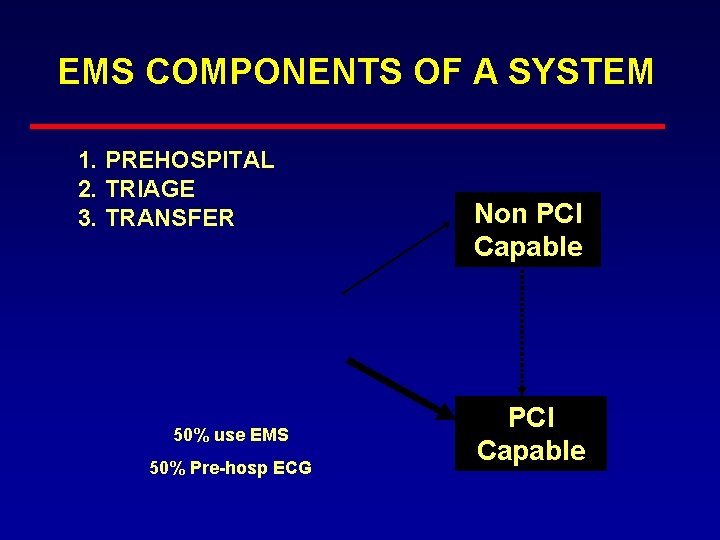
EMS COMPONENTS OF A SYSTEM 1. PREHOSPITAL 2. TRIAGE 3. TRANSFER 50% use EMS 50% Pre-hosp ECG Non PCI Capable
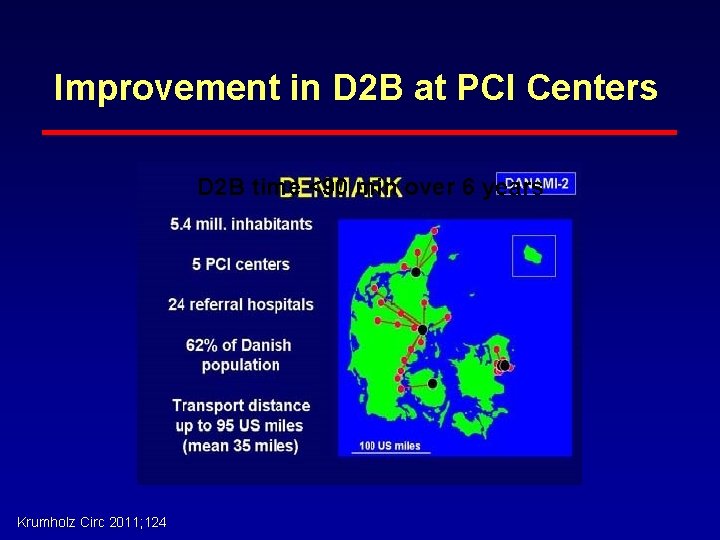
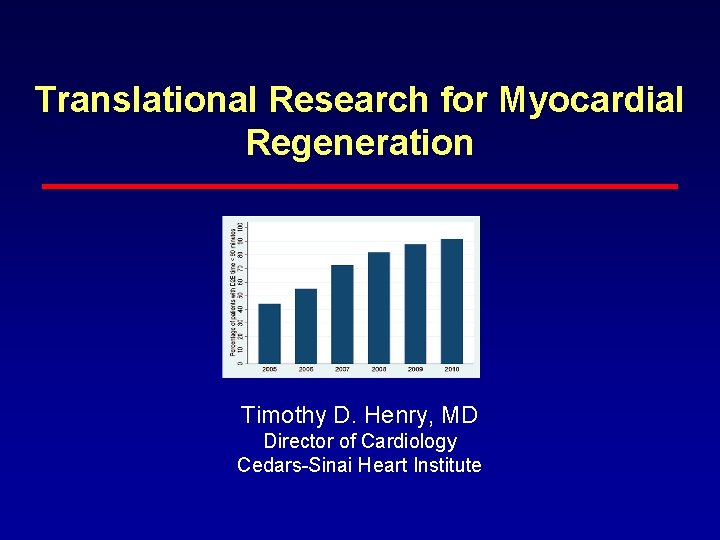
Improvement in D 2 B at PCI Centers D 2 B time <90 min over 6 years Krumholz Circ 2011; 124
STEMI – Door to Balloon and Door to Needle Times: Cumulative 12 Month Data High performing institutions are engaged in QI Monitoring ACTION Registry-GWTG DATA: January 1 – December 31, 2008 DTB = 1 st Door to Balloon for Primary PCI DTN = Door to Needle for Lytics
Even in Denmark! • “For field-triaged, transferred, and all EMS-transported patients, the proportion treated with a system delay <120 min was 72%, 35%, 48% respectively” Terkelsen et al, JAMA 304: 2010
Can we Bypass the ED? • For Transfer Pts- clearly yes • For ED Pts- Complicated – Data showing shorter D to B – Logistical issues – Call off rates – Probably no difference in outcomes – Certainly can and should be expedited!
“False Positive” Cath Lab Activation • While door-to-balloon times and clinical outcomes for STEMI have markedly improved, “false positive” activation of the cardiac catheterization laboratory (CCL) is an increasing problem • Definitions are a challenge!
What is the prevalence and etiology of “False Positive” Cath Lab Activation? STEMI Larson, DM et al JAMA 2007; 298(23): 2754 -2760
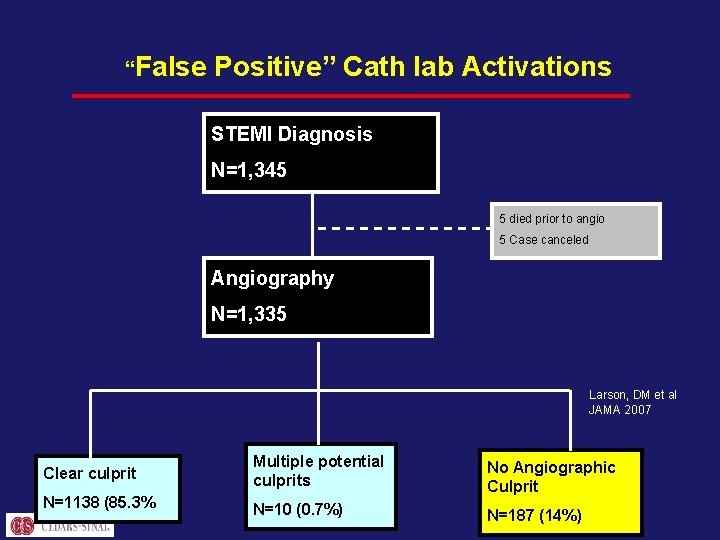
“False Positive” Cath lab Activations STEMI Diagnosis N=1, 345 5 died prior to angio 5 Case canceled Angiography N=1, 335 Larson, DM et al JAMA 2007 Clear culprit Multiple potential culprits N=1138 (85. 3% No Angiographic Culprit N=10 (0. 7%) N=187 (14%)
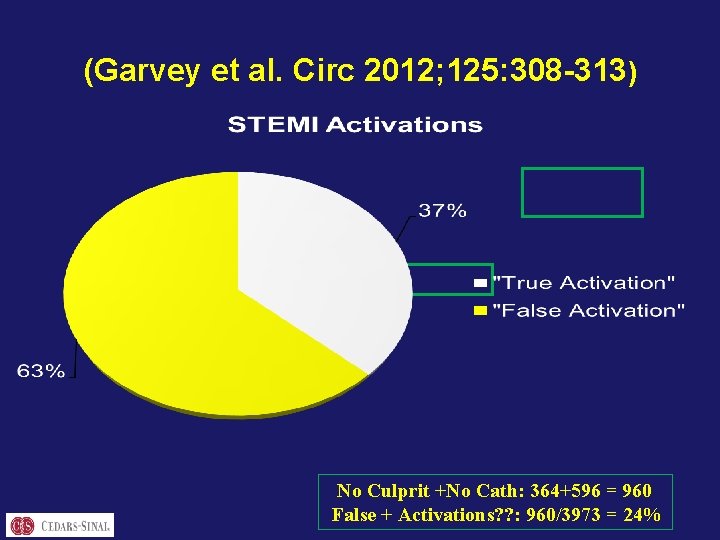
(Garvey et al. Circ 2012; 125: 308 -313) No Culprit +No Cath: 364+596 = 960 False + Activations? ? : 960/3973 = 24%
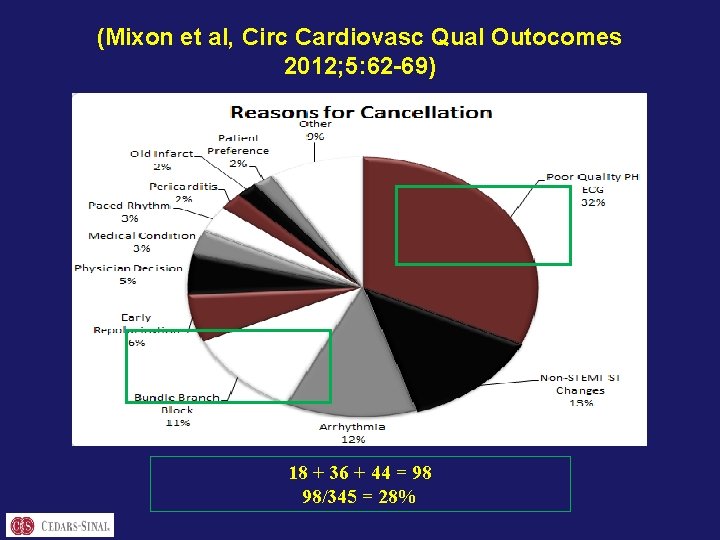
(Mixon et al, Circ Cardiovasc Qual Outocomes 2012; 5: 62 -69) 18 + 36 + 44 = 98 98/345 = 28%
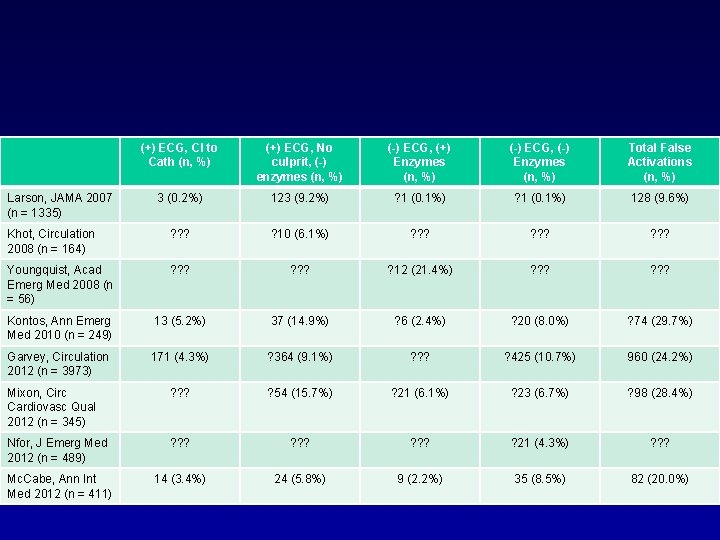
(+) ECG, CI to Cath (n, %) (+) ECG, No culprit, (-) enzymes (n, %) (-) ECG, (+) Enzymes (n, %) (-) ECG, (-) Enzymes (n, %) Total False Activations (n, %) 3 (0. 2%) 123 (9. 2%) ? 1 (0. 1%) 128 (9. 6%) Khot, Circulation 2008 (n = 164) ? ? ? ? 10 (6. 1%) ? ? ? Youngquist, Acad Emerg Med 2008 (n = 56) ? ? ? ? 12 (21. 4%) ? ? ? Kontos, Ann Emerg Med 2010 (n = 249) 13 (5. 2%) 37 (14. 9%) ? 6 (2. 4%) ? 20 (8. 0%) ? 74 (29. 7%) Garvey, Circulation 2012 (n = 3973) 171 (4. 3%) ? 364 (9. 1%) ? ? ? ? 425 (10. 7%) 960 (24. 2%) Mixon, Circ Cardiovasc Qual 2012 (n = 345) ? ? ? ? 54 (15. 7%) ? 21 (6. 1%) ? 23 (6. 7%) ? 98 (28. 4%) Nfor, J Emerg Med 2012 (n = 489) ? ? ? ? 21 (4. 3%) ? ? ? Mc. Cabe, Ann Int Med 2012 (n = 411) 14 (3. 4%) 24 (5. 8%) 9 (2. 2%) 35 (8. 5%) 82 (20. 0%) Larson, JAMA 2007 (n = 1335)
• “False” activations are costly to the medical system for a variety of reasons: – Patient satisfaction and trust; – CCL-staff morale, fatigue and economics – Health care resource utilization
• Universal definitions for “false” activations are necessary to define the scope of the problem • False activation: any patient who does not require emergent coronary angiography for STEMI – – Contraindications to Cath Goals of care ECG findings Clinical scenario
STE with + biomarkers but no clear culprit/no PCI is NOT a False Activation!!!!!
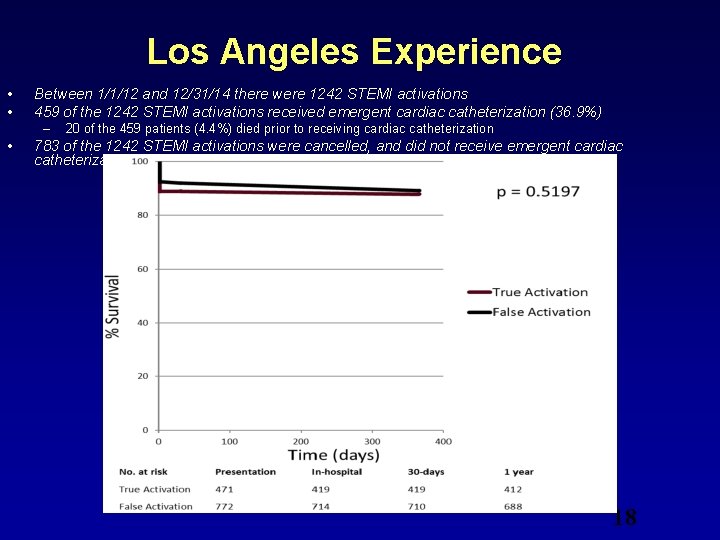
Los Angeles Experience • • Between 1/1/12 and 12/31/14 there were 1242 STEMI activations 459 of the 1242 STEMI activations received emergent cardiac catheterization (36. 9%) – • 20 of the 459 patients (4. 4%) died prior to receiving cardiac catheterization 783 of the 1242 STEMI activations were cancelled, and did not receive emergent cardiac catheterization (63. 0%) 18
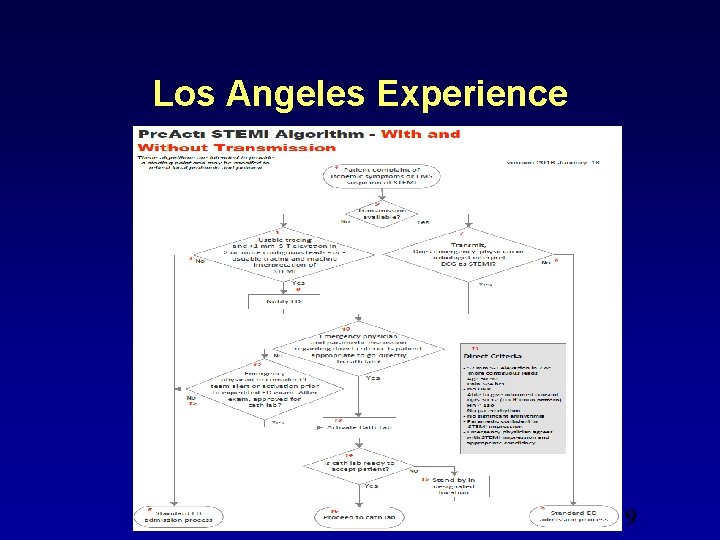
Los Angeles Experience 19
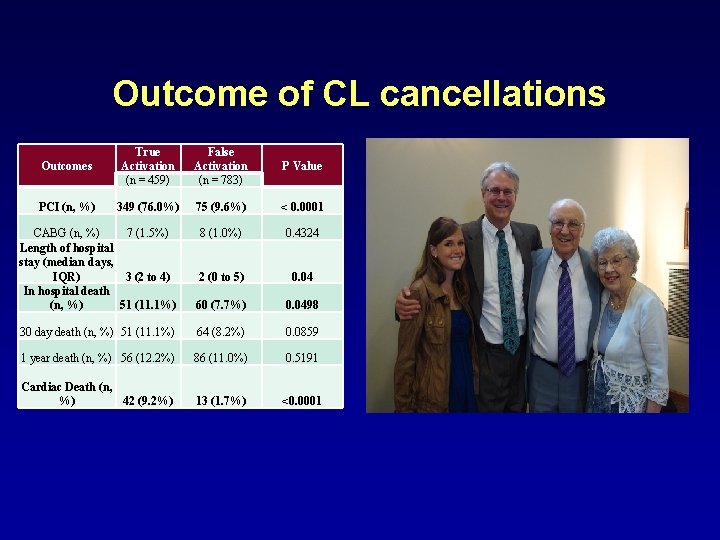
Outcome of CL cancellations Outcomes True Activation (n = 459) False Activation (n = 783) P Value PCI (n, %) 349 (76. 0%) 75 (9. 6%) < 0. 0001 8 (1. 0%) 0. 4324 CABG (n, %) 7 (1. 5%) Length of hospital stay (median days, IQR) 3 (2 to 4) In hospital death (n, %) 51 (11. 1%) 2 (0 to 5) 0. 04 60 (7. 7%) 0. 0498 30 day death (n, %) 51 (11. 1%) 64 (8. 2%) 0. 0859 1 year death (n, %) 56 (12. 2%) 86 (11. 0%) 0. 5191 Cardiac Death (n, %) 42 (9. 2%) 13 (1. 7%) <0. 0001
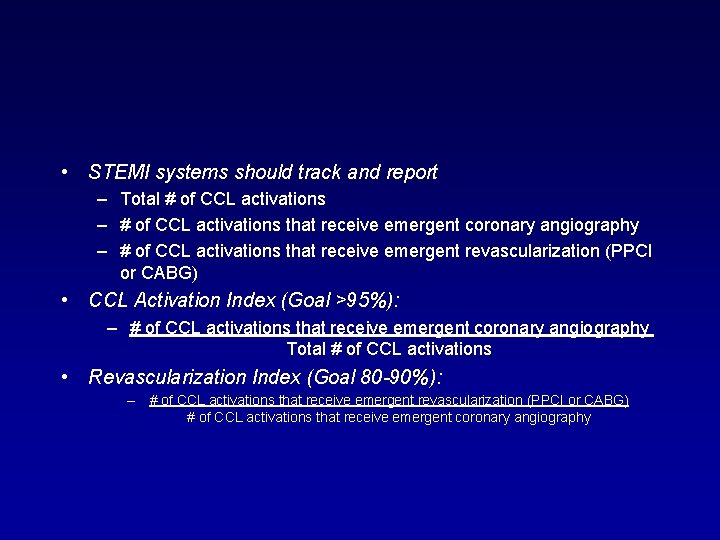
• STEMI systems should track and report – Total # of CCL activations – # of CCL activations that receive emergent coronary angiography – # of CCL activations that receive emergent revascularization (PPCI or CABG) • CCL Activation Index (Goal >95%): – # of CCL activations that receive emergent coronary angiography Total # of CCL activations • Revascularization Index (Goal 80 -90%): – # of CCL activations that receive emergent revascularization (PPCI or CABG) # of CCL activations that receive emergent coronary angiography
• Efforts to reduce “false” activation rates must be geared toward process improvement, but CANNOT lead to increased rates of “missed” STEMIs. Specificity of CCL activation for STEMI must be optimized without sacrificing the sensitivity.

Summary • False Activation of the Cath Lab: – Varies significantly from system to system – No agreed upon standard definitions – Costly to the system on many levels – Every system should track their numbers – Transmission may or may not help! – Need innovative ways to solve the problem!
When complimented for thinking outside the box: “I didn’t know there was a box. ” A very special man, Ed Lother 1925 -2013

Translational Research for Myocardial Regeneration Timothy D. Henry, MD Director of Cardiology Cedars-Sinai Heart Institute
- Slides: 27