Electrophysiology of Conduction Block and Temporal Dispersion PGY3
Electrophysiology of Conduction Block and Temporal Dispersion PGY-3 Neuromuscular Lecture Series David C. Preston M. D.
Electrophysiology of Demyelination Markedly Prolonged Distal Latencies n (> 130% upper limit of normal) Markedly Slowed Conduction Velocities n (< 75% lower limit of normal) Absent or Markedly Prolonged Late Responses n (> 130% upper limit of normal) Conduction Block
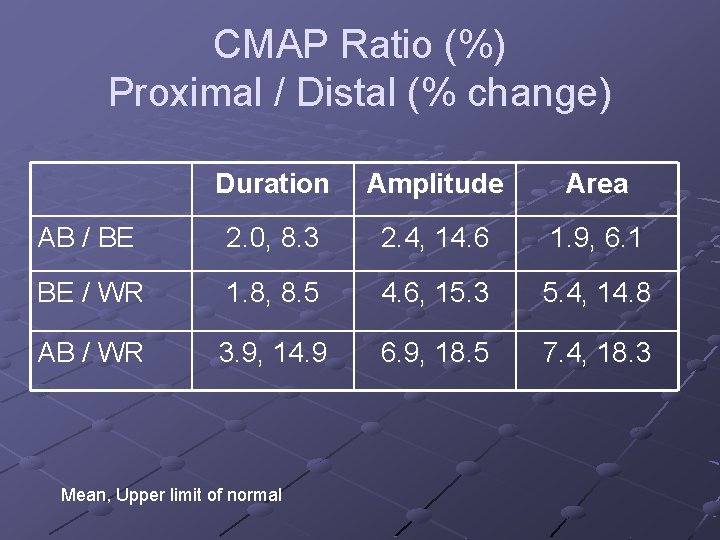
CMAP Ratio (%) Proximal / Distal (% change) Duration Amplitude Area AB / BE 2. 0, 8. 3 2. 4, 14. 6 1. 9, 6. 1 BE / WR 1. 8, 8. 5 4. 6, 15. 3 5. 4, 14. 8 AB / WR 3. 9, 14. 9 6. 9, 18. 5 7. 4, 18. 3 Mean, Upper limit of normal
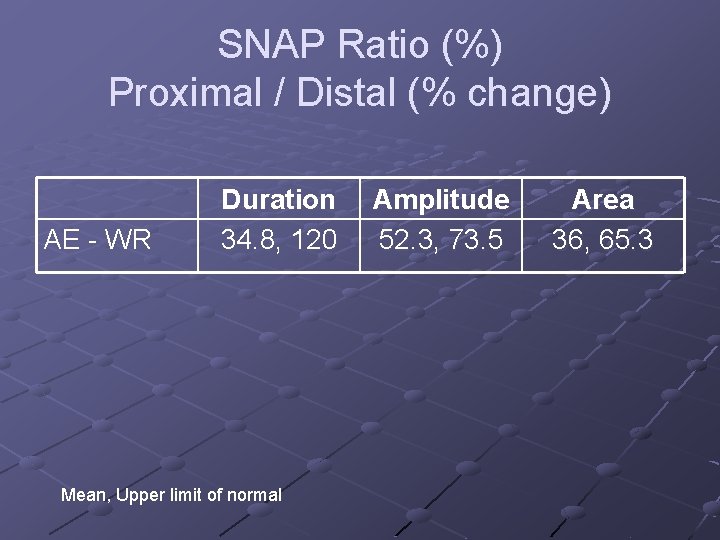
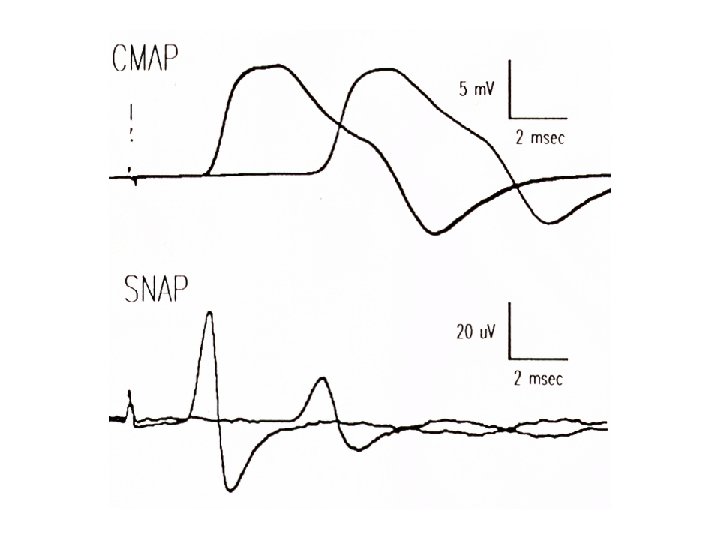
SNAP Ratio (%) Proximal / Distal (% change) AE - WR Duration 34. 8, 120 Mean, Upper limit of normal Amplitude 52. 3, 73. 5 Area 36, 65. 3

Summary: Normal Temporal Dispersion SNAP affected more than CMAP Amplitude affected more than area From Olney, Budingen, Miller. Muscle Nerve 1987
The Dilemma Does low amplitude = Axon loss? How much drop in amplitude between proximal and distal sites indicate conduction block?
The Normal Nerve
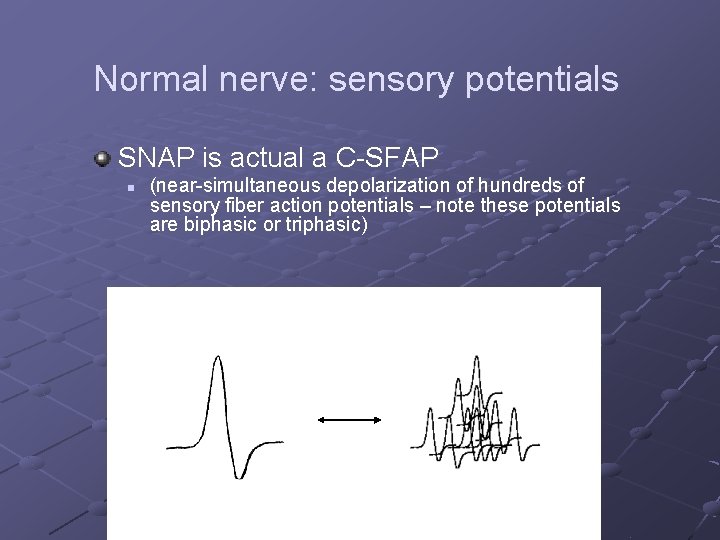
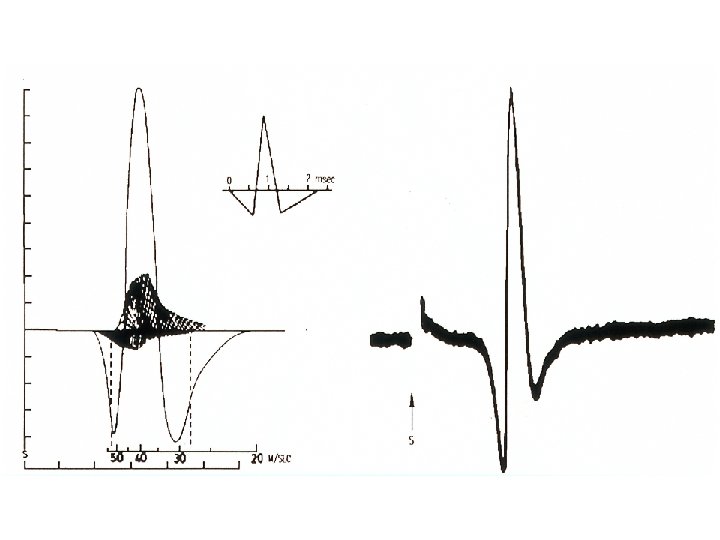
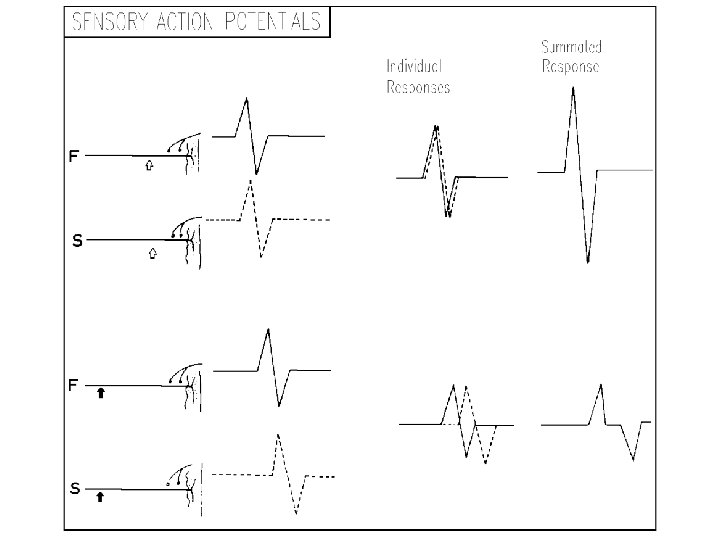
Normal nerve: sensory potentials SNAP is actual a C-SFAP n (near-simultaneous depolarization of hundreds of sensory fiber action potentials – note these potentials are biphasic or triphasic)
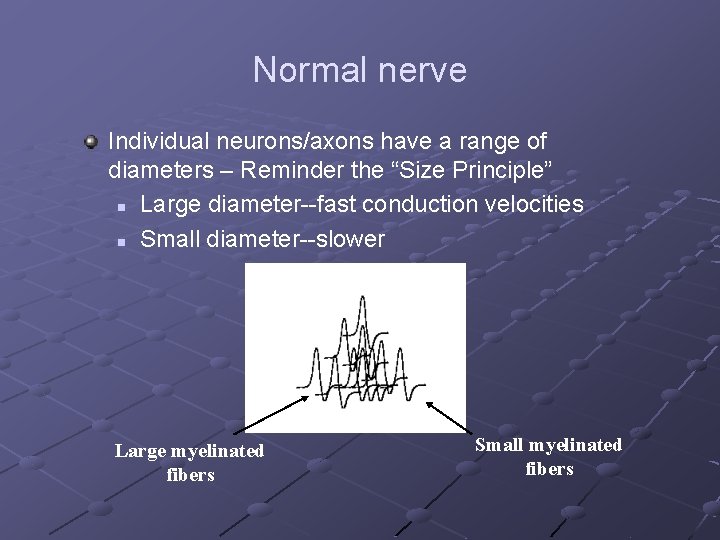
Normal nerve Individual neurons/axons have a range of diameters – Reminder the “Size Principle” n Large diameter--fast conduction velocities n Small diameter--slower Large myelinated fibers Small myelinated fibers
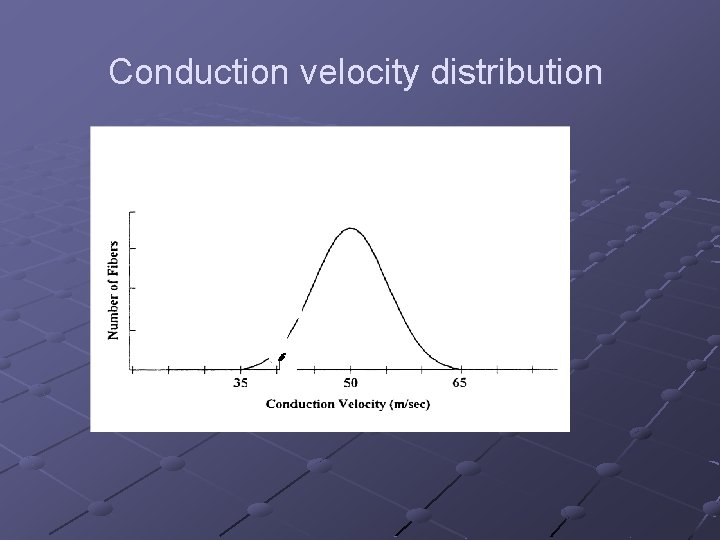
Conduction velocity distribution

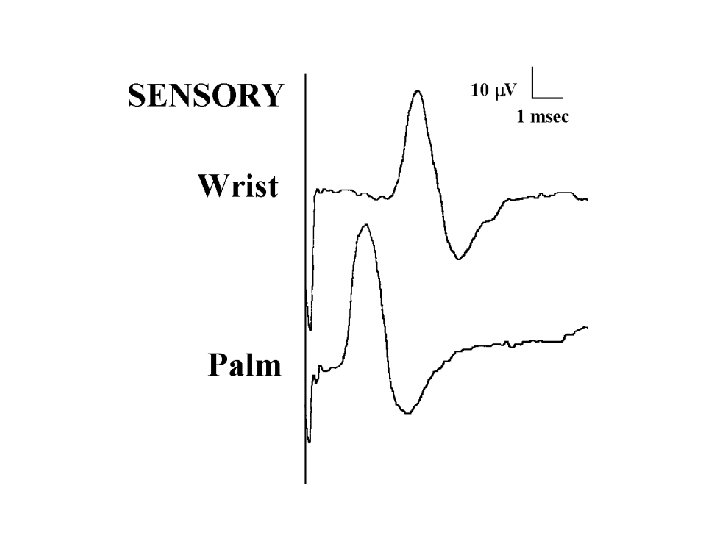
Normal nerve: temporal dispersion To simplify, imagine a sensory nerve with only two fibers n n One is thickly myelinated with a conduction velocity of 60 m/s One is a little smaller, with a conduction velocity of 50 m/s Over a short distance, the two action potentials are close together and relatively in-phase
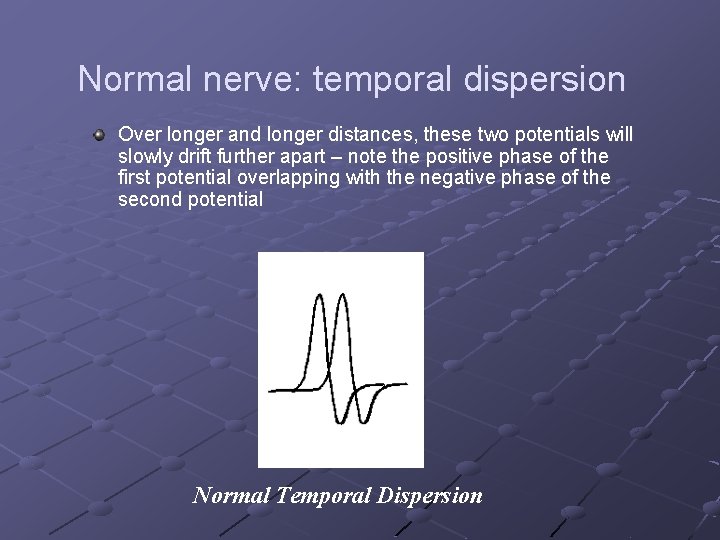
Normal nerve: temporal dispersion Over longer and longer distances, these two potentials will slowly drift further apart – note the positive phase of the first potential overlapping with the negative phase of the second potential Normal Temporal Dispersion

Normal nerve: temporal dispersion Similar to two runners, one slightly faster than the other. n n Over a short distance, they will still be close together Over long distances, further apart
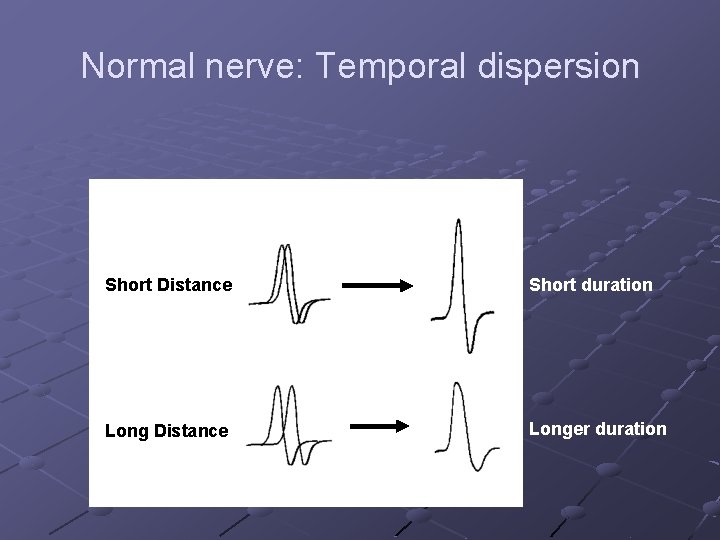
Normal nerve: Temporal dispersion Short Distance Short duration Long Distance Longer duration
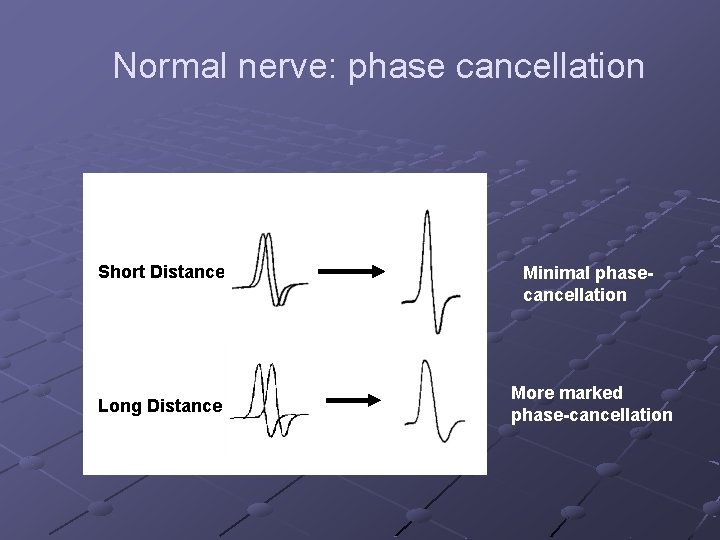
Normal nerve: phase cancellation Short Distance Long Distance Minimal phasecancellation More marked phase-cancellation
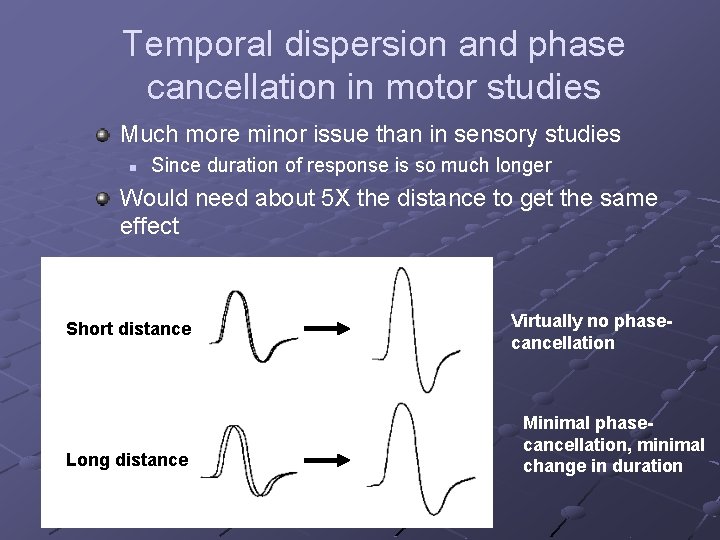
Temporal dispersion and phase cancellation in motor studies Much more minor issue than in sensory studies n Since duration of response is so much longer Would need about 5 X the distance to get the same effect Short distance Long distance Virtually no phasecancellation Minimal phasecancellation, minimal change in duration
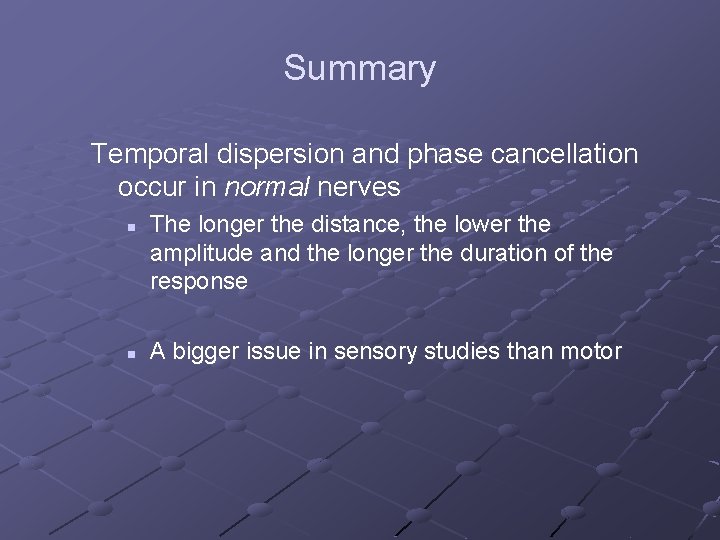
Summary Temporal dispersion and phase cancellation occur in normal nerves n n The longer the distance, the lower the amplitude and the longer the duration of the response A bigger issue in sensory studies than motor
Nerve function: Diseased States
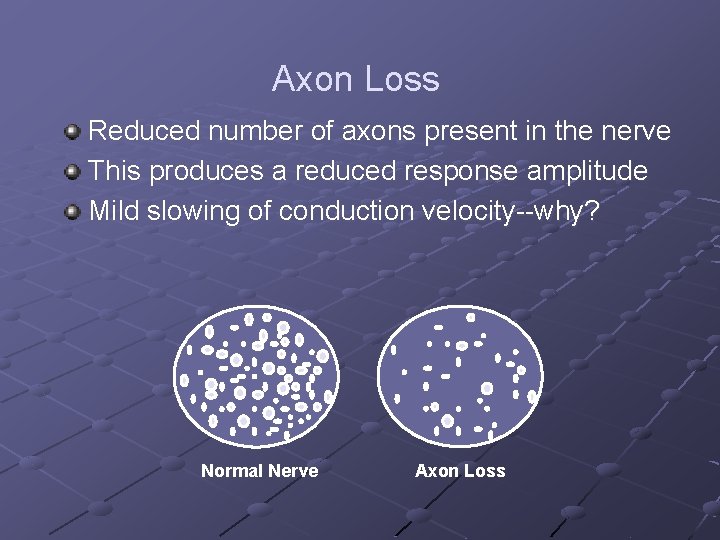
Axon Loss Reduced number of axons present in the nerve This produces a reduced response amplitude Mild slowing of conduction velocity--why? Normal Nerve Axon Loss
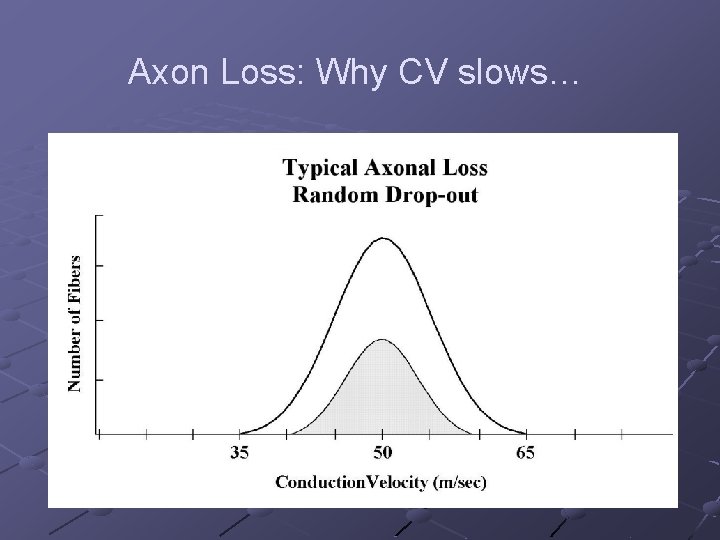
Axon Loss: Why CV slows…
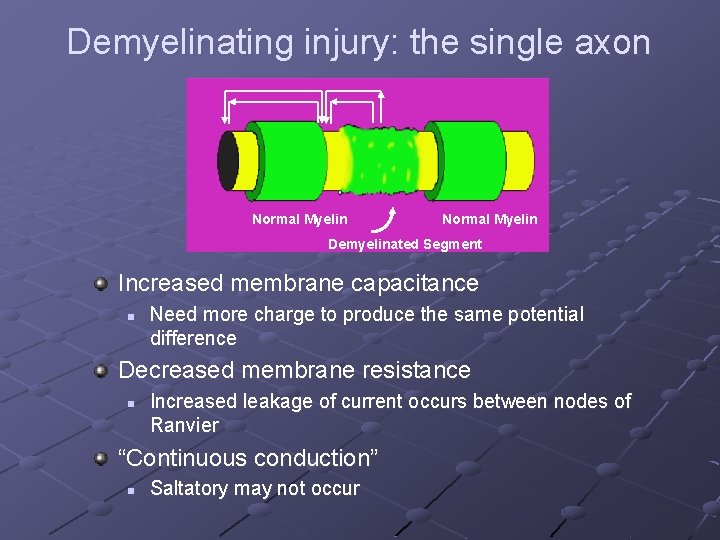
Demyelinating injury: the single axon Normal Myelin Demyelinated Segment Increased membrane capacitance n Need more charge to produce the same potential difference Decreased membrane resistance n Increased leakage of current occurs between nodes of Ranvier “Continuous conduction” n Saltatory may not occur
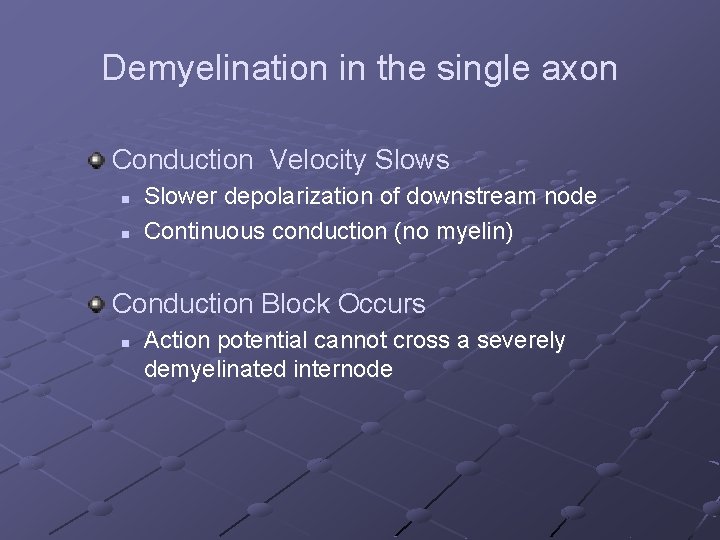
Demyelination in the single axon Conduction Velocity Slows n n Slower depolarization of downstream node Continuous conduction (no myelin) Conduction Block Occurs n Action potential cannot cross a severely demyelinated internode
Demyelination: multiple fibers Demyelination in multiple fibers is complex n Effects due to conduction velocity slowing n Effects due to conduction block
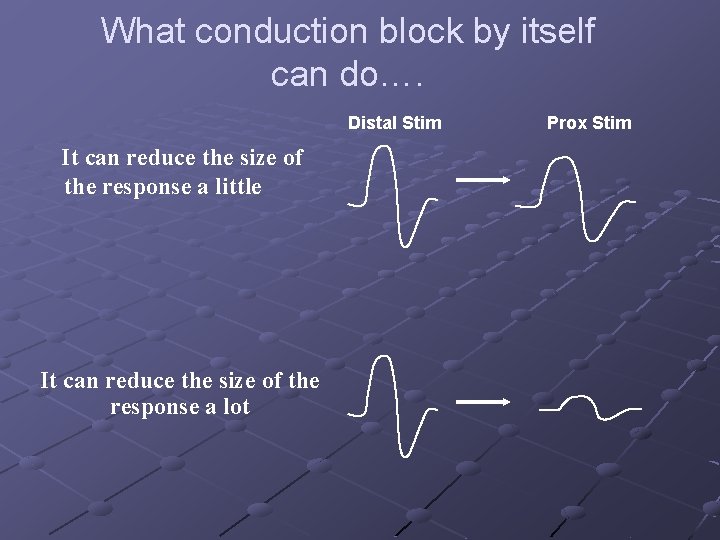
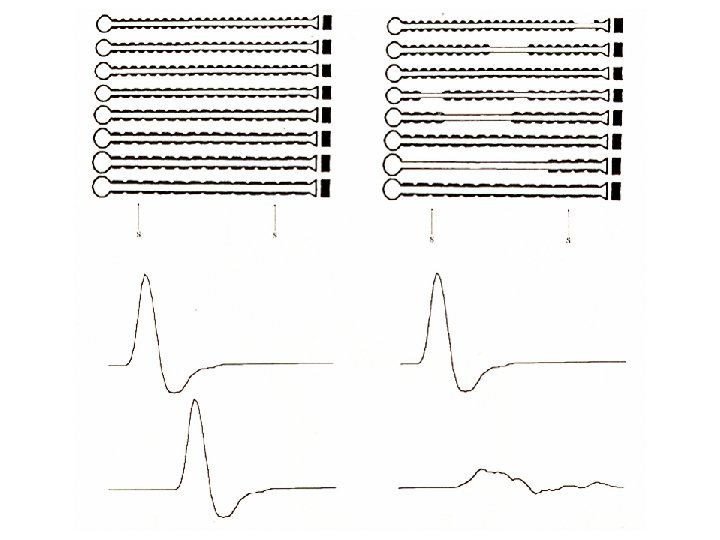
What conduction block by itself can do…. Distal Stim It can reduce the size of the response a little It can reduce the size of the response a lot Prox Stim
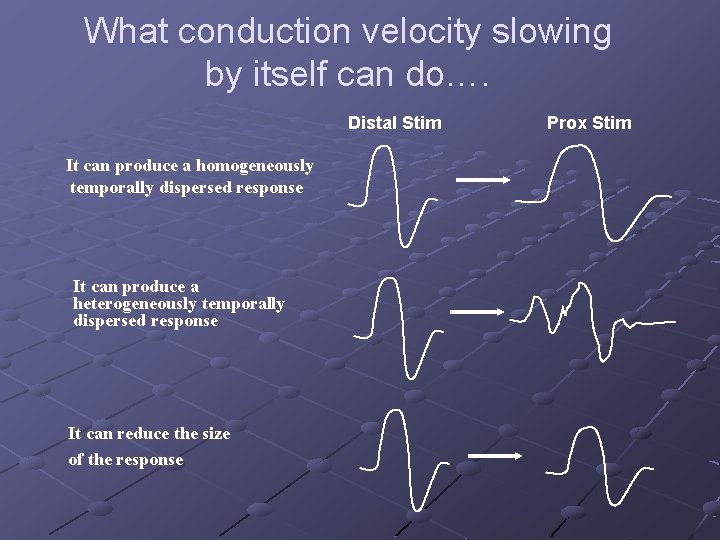
What conduction velocity slowing by itself can do…. Distal Stim It can produce a homogeneously temporally dispersed response It can produce a heterogeneously temporally dispersed response It can reduce the size of the response Prox Stim
How can reduced CV, by itself, reduce response size?
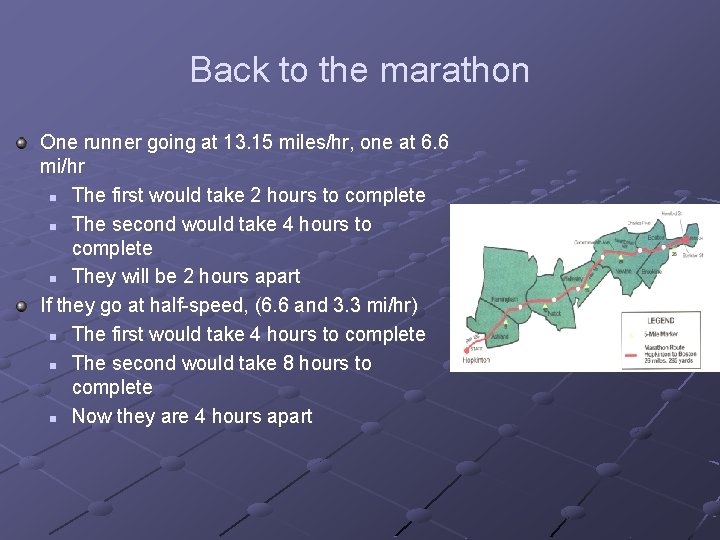
Back to the marathon One runner going at 13. 15 miles/hr, one at 6. 6 mi/hr n The first would take 2 hours to complete n The second would take 4 hours to complete n They will be 2 hours apart If they go at half-speed, (6. 6 and 3. 3 mi/hr) n The first would take 4 hours to complete n The second would take 8 hours to complete n Now they are 4 hours apart
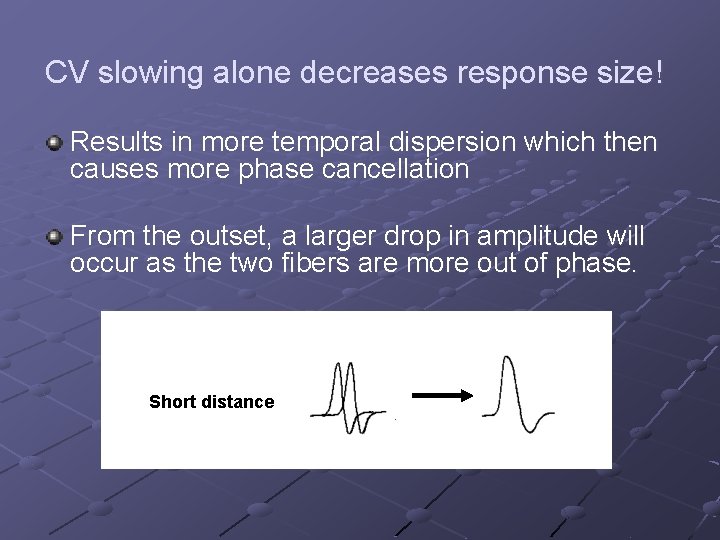
CV slowing alone decreases response size! Results in more temporal dispersion which then causes more phase cancellation From the outset, a larger drop in amplitude will occur as the two fibers are more out of phase. Short distance
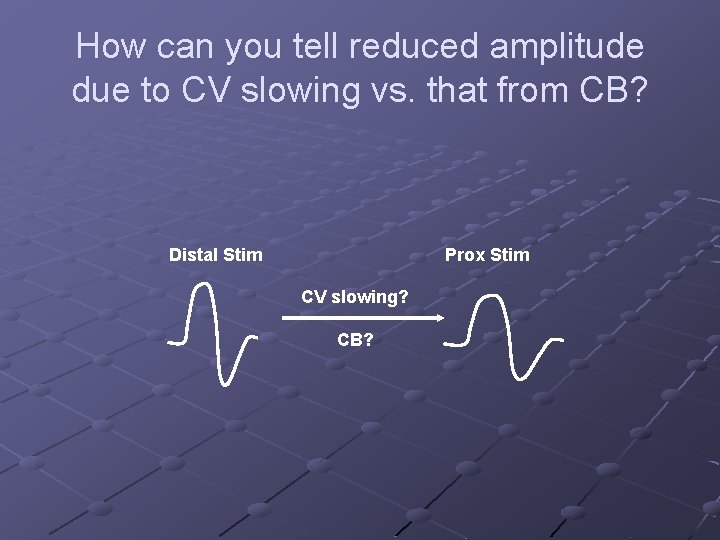
How can you tell reduced amplitude due to CV slowing vs. that from CB? Distal Stim Prox Stim CV slowing? CB?
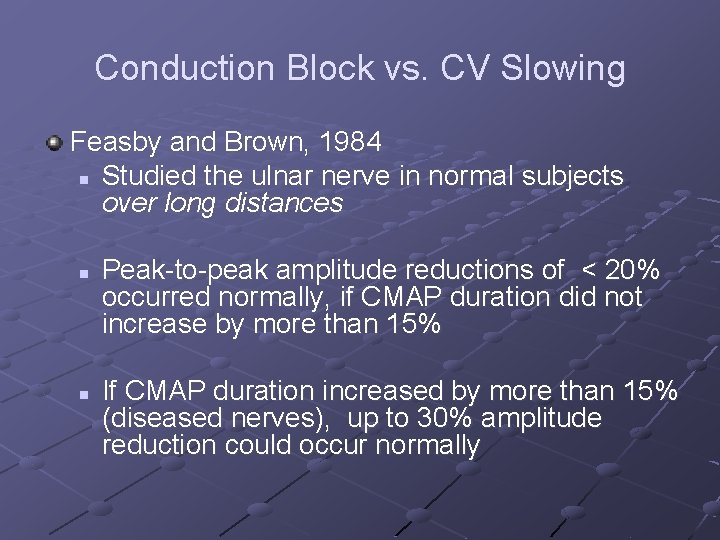
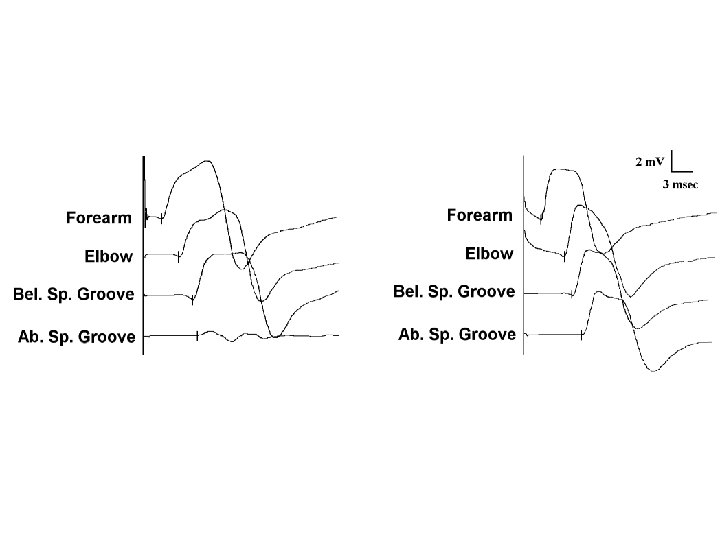
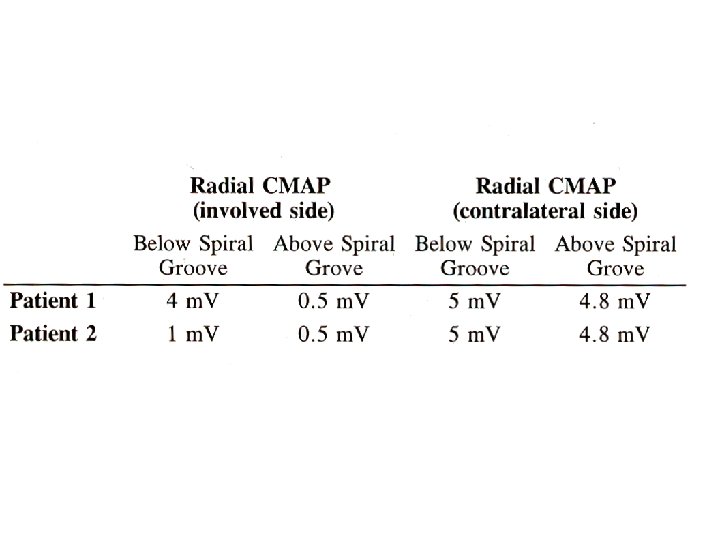
Conduction Block vs. CV Slowing Feasby and Brown, 1984 n Studied the ulnar nerve in normal subjects over long distances n n Peak-to-peak amplitude reductions of < 20% occurred normally, if CMAP duration did not increase by more than 15% If CMAP duration increased by more than 15% (diseased nerves), up to 30% amplitude reduction could occur normally
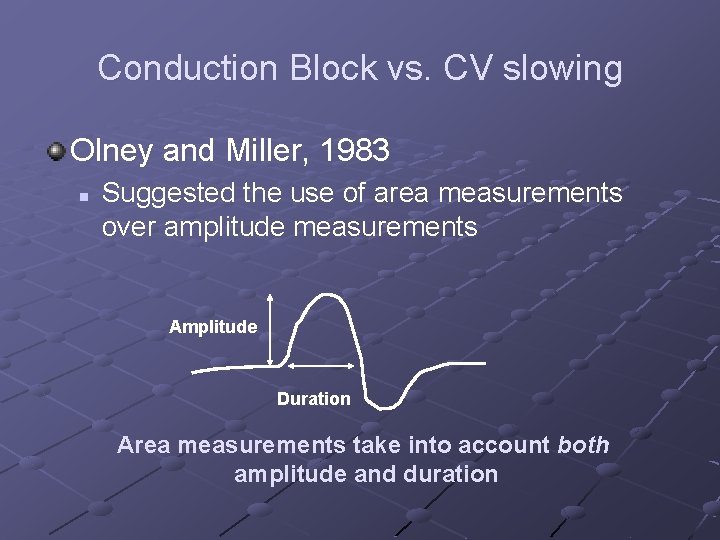
Conduction Block vs. CV slowing Olney and Miller, 1983 n Suggested the use of area measurements over amplitude measurements Amplitude Duration Area measurements take into account both amplitude and duration
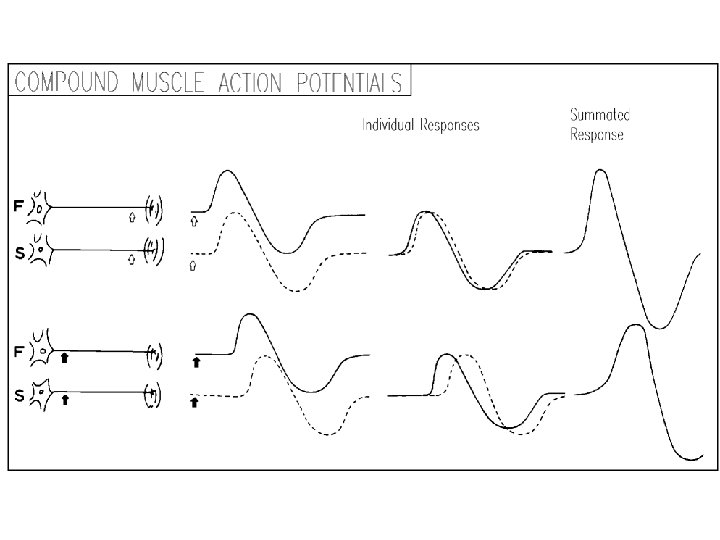
Conduction Block vs. CV slowing Rhee, England, and Sumner, 1990 An in vivo study of motor units in mice Computer simulations to determine how 60 of these motor units might summate to produce CMAPs. How does amplitude/area change when you block different subsets of fibers? How does amplitude/area change when you slow different subsets of fibers?
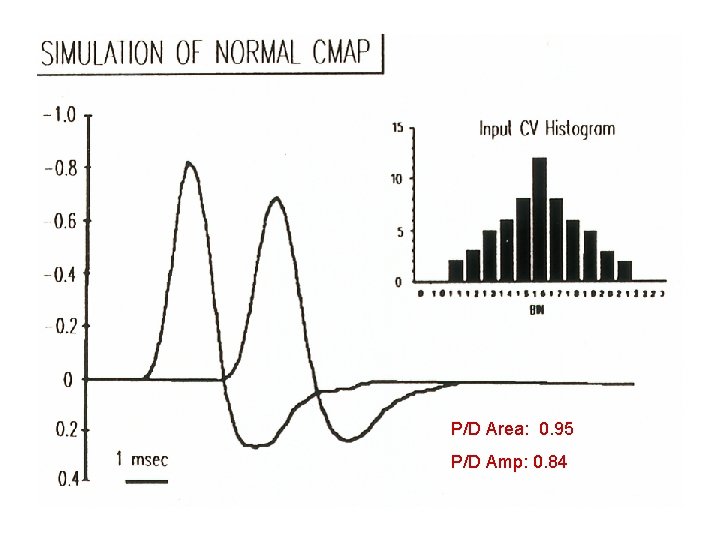
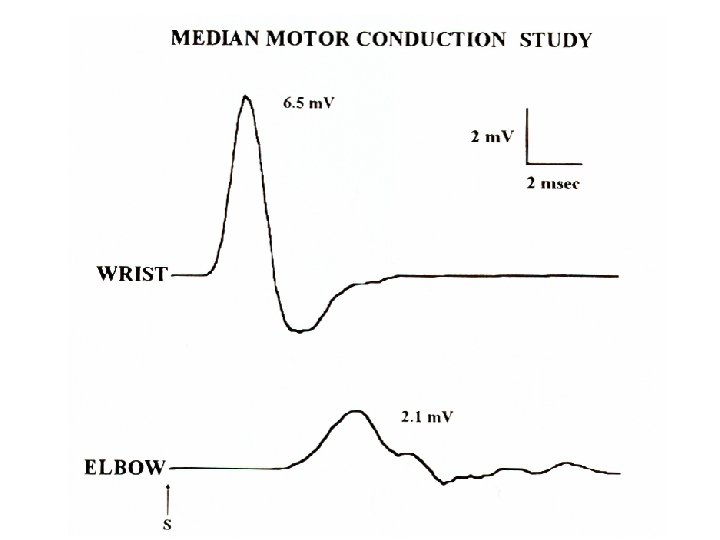
P/D Area: 0. 95 P/D Amp: 0. 84
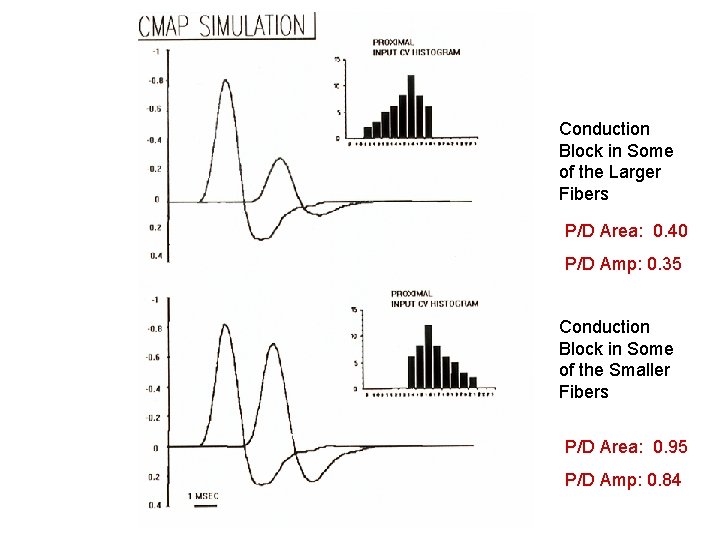
Conduction Block in Some of the Larger Fibers P/D Area: 0. 40 P/D Amp: 0. 35 Conduction Block in Some of the Smaller Fibers P/D Area: 0. 95 P/D Amp: 0. 84
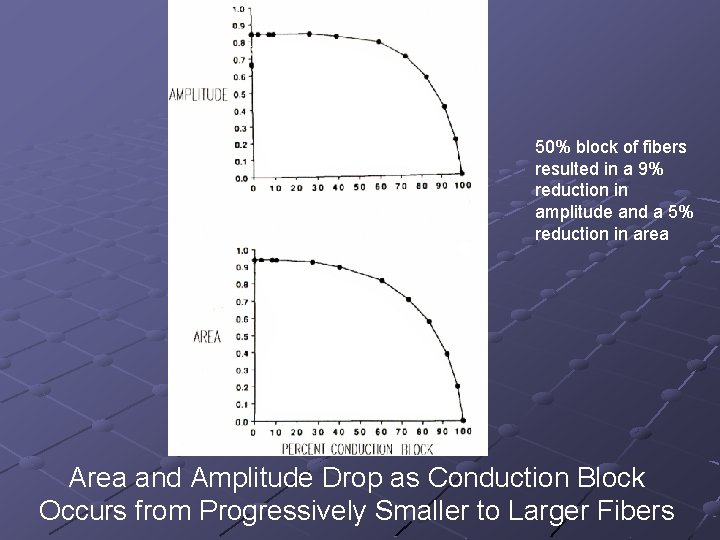
50% block of fibers resulted in a 9% reduction in amplitude and a 5% reduction in area Area and Amplitude Drop as Conduction Block Occurs from Progressively Smaller to Larger Fibers
How much can the size of a response decrease based only on temporal dispersion and phase cancellation from conduction velocity abnormalities alone (no block)?
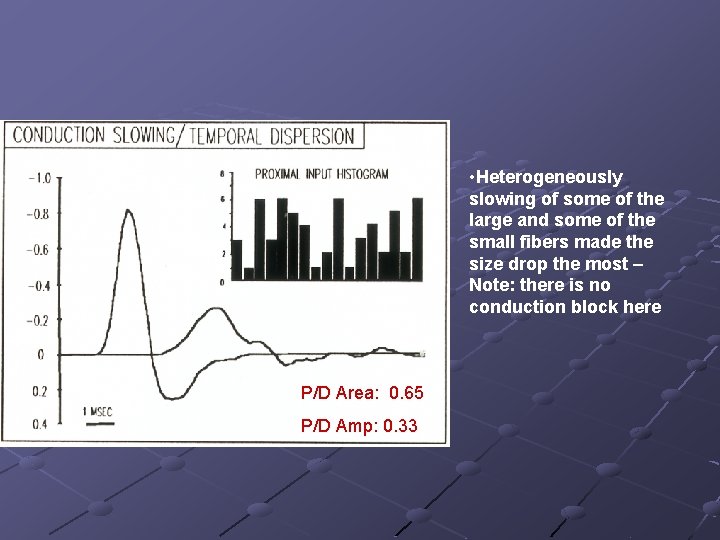
• Heterogeneously slowing of some of the large and some of the small fibers made the size drop the most – Note: there is no conduction block here P/D Area: 0. 65 P/D Amp: 0. 33
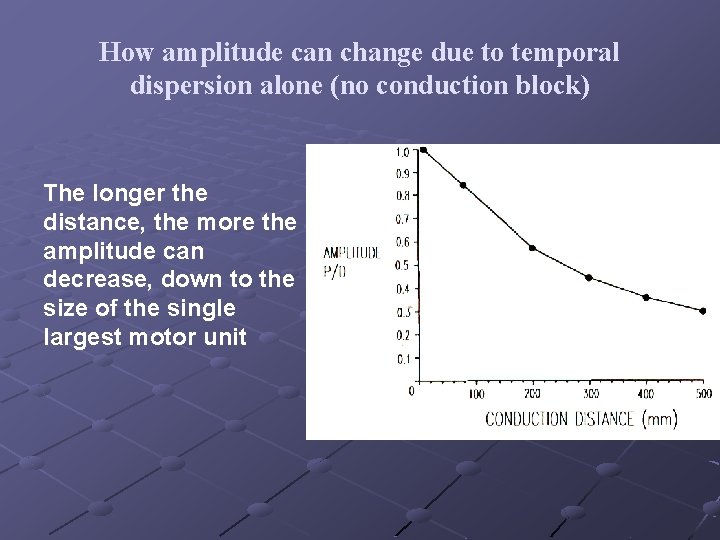
How amplitude can change due to temporal dispersion alone (no conduction block) The longer the distance, the more the amplitude can decrease, down to the size of the single largest motor unit
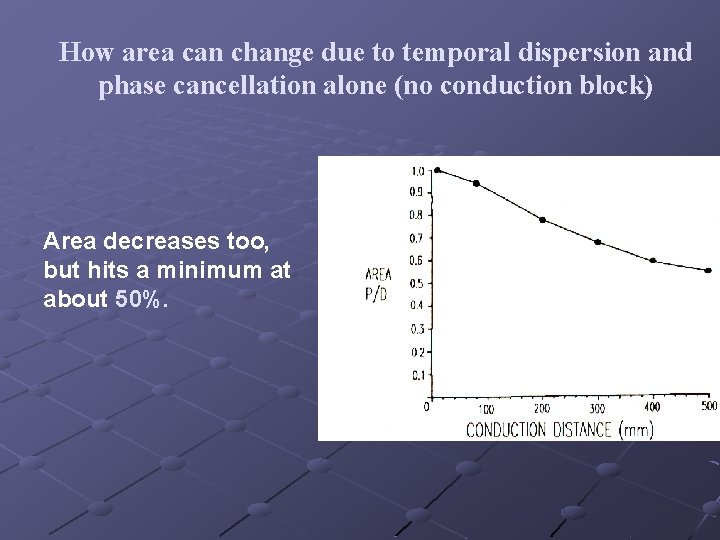
How area can change due to temporal dispersion and phase cancellation alone (no conduction block) Area decreases too, but hits a minimum at about 50%.
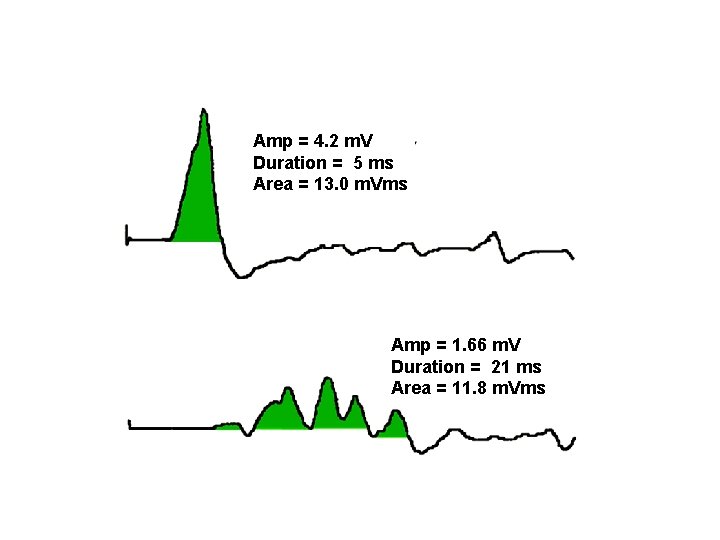
Amp = 4. 2 m. V Duration = 5 ms Area = 13. 0 m. Vms Amp = 1. 66 m. V Duration = 21 ms Area = 11. 8 m. Vms
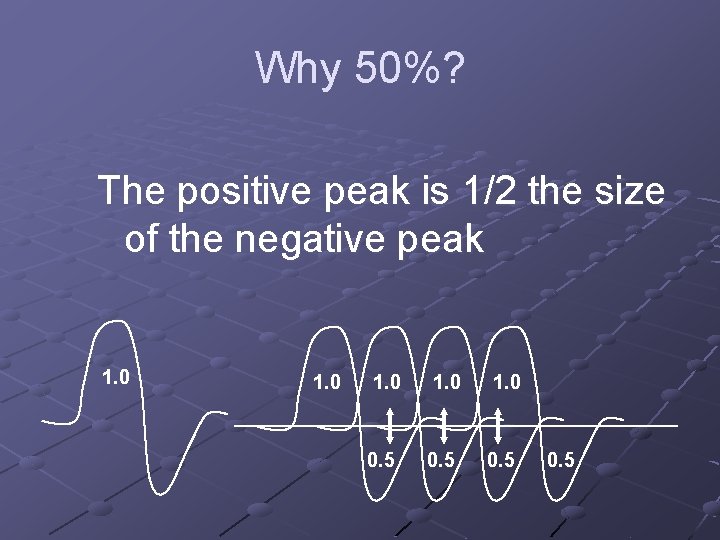
Why 50%? The positive peak is 1/2 the size of the negative peak 1. 0 1. 0 0. 5
Summary Fastest fibers make up a disproportionate contribution of the CMAP configuration CB can be hidden if only small fibers are blocked The effects of temporal dispersion are most marked when they occur among the fastest fibers Temporal dispersion without block can cause an area decrement up to 50% and an amplitude decrement down to the size of the largest individual MUAP
Summary - 2 Assessing the degree of conduction block by the CMAP amplitude and area can be very inaccurate without knowing the subpopulation of the axons affected CV slowing alone can make the amplitude drop up to 80% (i. e. , down to the size of the single largest motor unit)

Summary - 3 For definite conduction block: n Area drop greater than 50% between stimulation sites, regardless of length of distance However, from studies on normals: n n n Over typical wrist-elbow and ankle-knee segments, a drop > 20% of amplitude is abnormal, especially if temporal dispersion is not marked (<115%) These numbers must be liberalized if conducting from axilla or Erb’s point Over very short distances (e. g. , inching) smaller drops are likely significant

Don’t Forget: Conduction Block and Temporal Dispersion/Phase Cancellation Both Signify Demyelination
Conduction Block Electrophysiologic Definition Physiologic Definition? n n What is the clinical correlate of CB? What is the Needle EMG correlate of CB?
Value of Conduction Block Entrapment Neuropathy n n n Lesion Localization Assess Axonal Loss vs. Demyelination Prognosis Inherited vs. Acquired Demyelinating Neuropathy Motor Neuron Disease vs. Motor Neuropathy
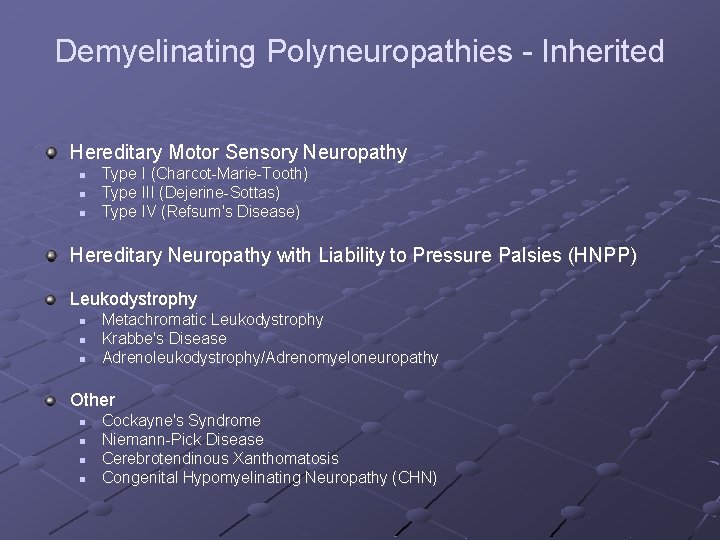
Demyelinating Polyneuropathies - Inherited Hereditary Motor Sensory Neuropathy n n n Type I (Charcot-Marie-Tooth) Type III (Dejerine-Sottas) Type IV (Refsum's Disease) Hereditary Neuropathy with Liability to Pressure Palsies (HNPP) Leukodystrophy n n n Metachromatic Leukodystrophy Krabbe's Disease Adrenoleukodystrophy/Adrenomyeloneuropathy Other n n Cockayne's Syndrome Niemann-Pick Disease Cerebrotendinous Xanthomatosis Congenital Hypomyelinating Neuropathy (CHN)
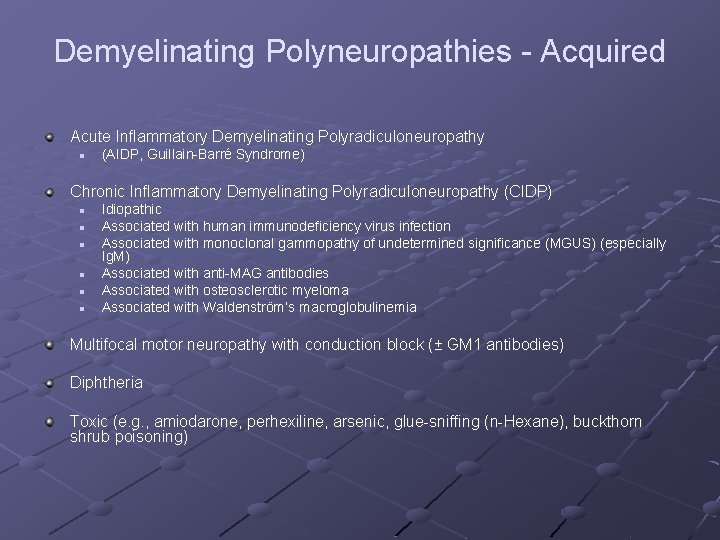
Demyelinating Polyneuropathies - Acquired Acute Inflammatory Demyelinating Polyradiculoneuropathy n (AIDP, Guillain-Barré Syndrome) Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) n n n Idiopathic Associated with human immunodeficiency virus infection Associated with monoclonal gammopathy of undetermined significance (MGUS) (especially Ig. M) Associated with anti-MAG antibodies Associated with osteosclerotic myeloma Associated with Waldenström’s macroglobulinemia Multifocal motor neuropathy with conduction block (± GM 1 antibodies) Diphtheria Toxic (e. g. , amiodarone, perhexiline, arsenic, glue-sniffing (n-Hexane), buckthorn shrub poisoning)
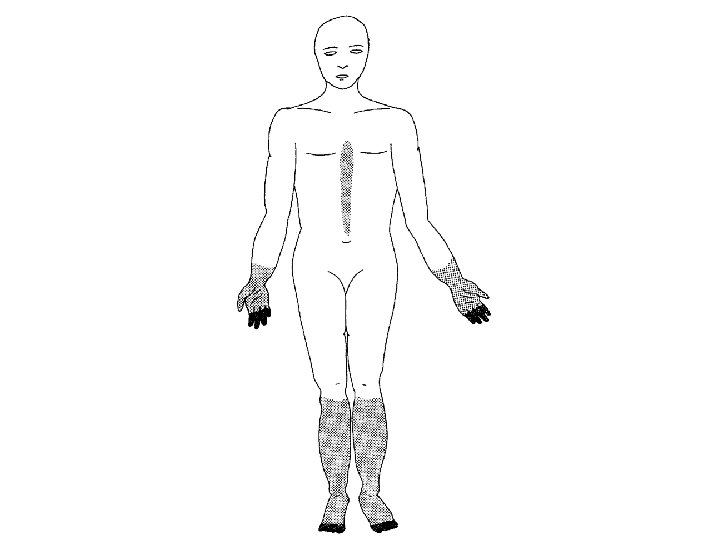
Demyelinating Polyneuropathies Hereditary Motor Sensory Neuropathy, Type I (Charcot-Marie-Tooth) Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP)
Differentiation between Inherited and Acquired Demyelinating Neuropathy Symmetry Conduction Block n Generally signifies an acquired and potentially treatable conduction. Patients with hereditary neuropathy typically do not display CB
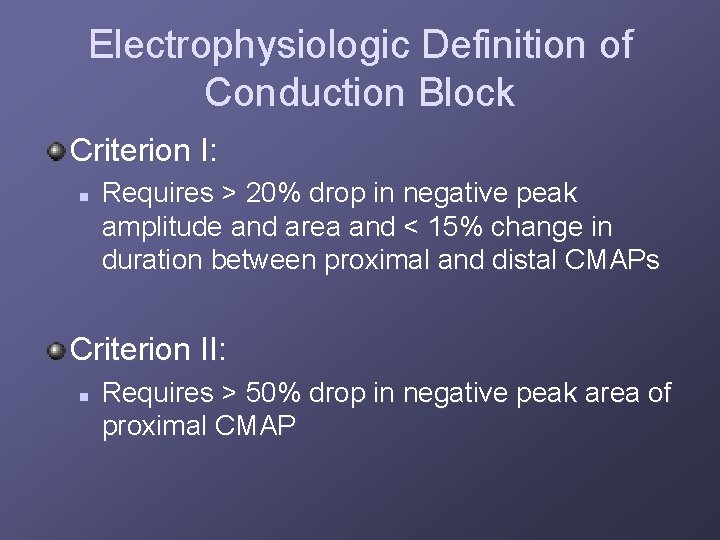
Electrophysiologic Definition of Conduction Block Criterion I: n Requires > 20% drop in negative peak amplitude and area and < 15% change in duration between proximal and distal CMAPs Criterion II: n Requires > 50% drop in negative peak area of proximal CMAP
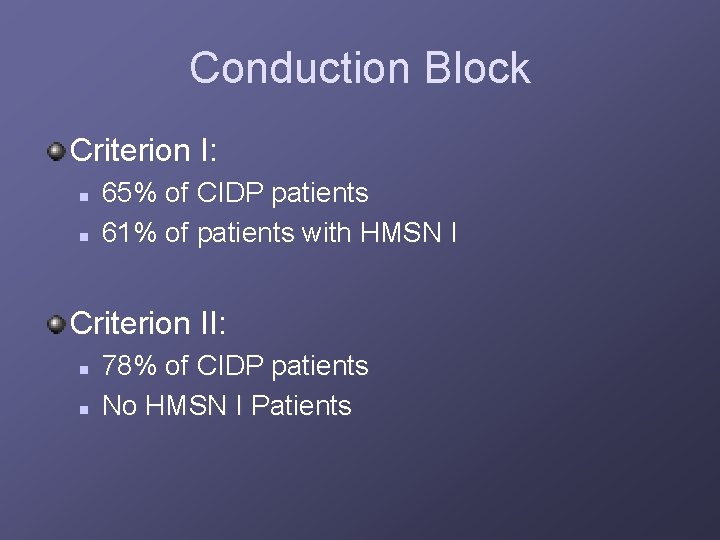
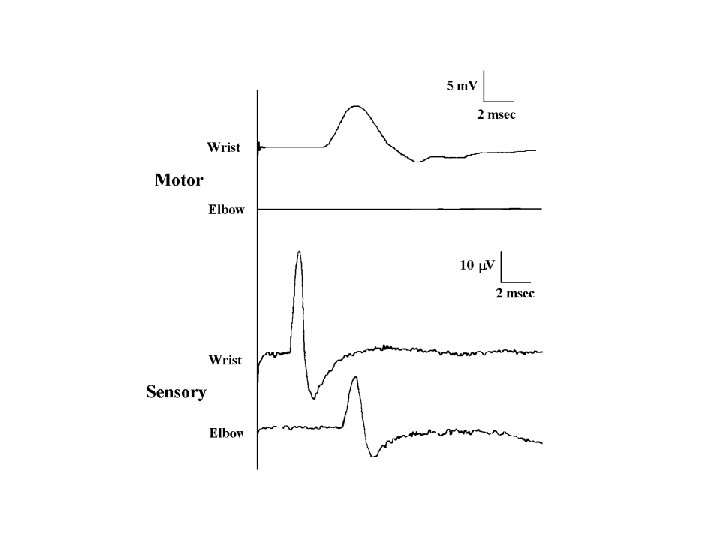
Conduction Block Criterion I: n n 65% of CIDP patients 61% of patients with HMSN I Criterion II: n n 78% of CIDP patients No HMSN I Patients
Pure Motor Disorder Motor Neuron Disease (especially PMA) Multifocal Motor Neuropathy with Conduction Block

Thanks to Seward Rutkove, MD, Beth Israel Hospital, Boston, MA for use for several of the his powerpoint slides in this presentation.
- Slides: 67