Electroconvulsive Therapy Nursing Competencies and Training Training Objectives

Electroconvulsive Therapy Nursing Competencies and Training

Training Objectives • Provide a clinical overview of ECT • History • Indications • Informed Consent Process • Pre- ECT evaluation • Technique • Risks, Side Effects, Adverse Outcomes • Recovery Management • Role of Nursing: ECT RN, Recovery & Inpatient staff • Overview of Process, Review Forms and Documentation Expectations
History of ECT • ECT was first developed in the 1930’s after it was noted that some people with depression and schizophrenia, who also had epilepsy, reported an improved mood after suffering a seizure. • ECT was used widely in the 1950’s and 60’s. Many myths surrounding ECT are based on the early treatments where anesthetic and muscle relaxants were not given. • Since its initial introduction, the process for ECT treatment has been refined, and it is considered a very safe and effective treatment.
How does ECT work • ECT involves receiving conscious sedation and then having small electric currents pass through the brain to trigger a brief seizure (Mayo clinic, 2016) • Although the exact mechanism of action isn’t fully understood, the seizure brought on by the electric stimulus seems to cause changes in the brain that can quickly alleviate depressive symptoms (Mayo clinic, 2016) • ECT is particularly effective in treating depression that hasn’t responded to other types of treatment
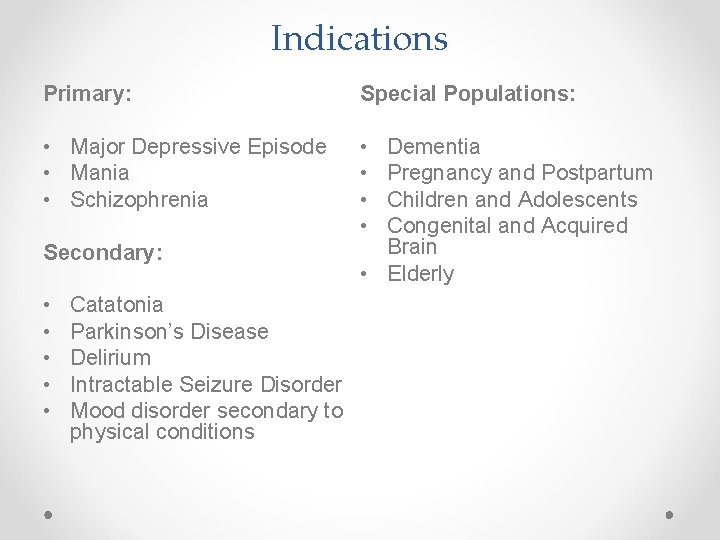
Indications Primary: Special Populations: • Major Depressive Episode • Mania • Schizophrenia • • Secondary: • • • Catatonia Parkinson’s Disease Delirium Intractable Seizure Disorder Mood disorder secondary to physical conditions Dementia Pregnancy and Postpartum Children and Adolescents Congenital and Acquired Brain • Elderly
Special Populations continued… ECT not indicated for: • Anxiety disorders, post-traumatic stress disorder, primary delusional disorder, • Caution when used to treat affective symptoms in chronic pain or personality disorders
Initiating a Course of ECT Psychiatrist: • Discusses proposed treatment • Obtains consent • Completes order set • Assessments: • Medical Clearance Form • Mo. Ca • Additional Consults • Diagnostic and Lab investigations See Appendix A, B, and C; Order Set, Medical Clearance Form, Mo. CA In learning package
Informed Consent Process • Consent a dynamic process that starts when treatment is recommended and ends when therapy is completed- much more than “signing a form” • Physician must obtain and document informed consent from the patient and/or SDM, (if patient is not capable) • When capacity is questioned, a second opinion from another psychiatrist is required • Information about ECT must be provided to the patient to assist them in making an informed decision- oral, written, visual media and/or internet resources • Consent may be withdrawn at anytime • Consent must be renewed every 6 months or 15 ECT treatments (which ever comes first)
Informed Consent continued…. Physician must discuss: • Why ECT is being recommended. • Describe alternative treatment options • Describe procedure, including type of treatment, expected course and frequency • Describe likelihood and severity of major risks and common adverse effects associated with the procedure. Including a discussion about appropriate emergency treatments in the event that it may be necessary • Discuss restrictions on patient behavior prior to and after procedure i. e. no benzo’s before, no driving 24 hrs after • Answer additional questions, providing information and education as needed.
Medical Evaluation • • Physical examination Baseline cognitive assessment (Mo. CA) ECG Routine Lab guided by patients history and physical- i. e. Hemoglobin, Electrolytes, renal function tests Chest x-ray Cervical spine x-ray (if indicated) Evaluation of dentition and temporal-mandibular joint problems Pertinent specialty consults- anesthesia, medicine, obstetrics, psychiatry
Physiological Effects of ECT • Large increases of cerebral blood flow and intercranial pressure • Initial parasympathetic discharge manifested by bradycardia, occasional asystole, premature atrial and ventricuar contraction, hypotension and salivation • Follows with a sympathetic discharge- tachycardia hypertension, premature ventricular contractions and rarely, ventricular tachycardia and ECG changes including ST segment depression and t-wave inversion significant morbidity in high risk patients • Glucose homeostasis is affected-hyperglycemia in insulin dependent patients
Contraindications ECT may be required even when relative contraindications exist. These include: • Unstable or severe cardiovascular conditions i. e. recent MI, unstable angina, poorly-compensated heart failure, severe valvular disease • Aneurysm or vascular malformations • Increased intracranial pressure, brain tumors, space-occupying lesions • Recent cerebral infarction • Pulmonary conditions-COPD, asthma, pneumonia • Patient status rated as ASA level 4 or 5 • Higher risk- retinal detachment acute narrow angle glaucoma Pheochromocytoma
Short Term Side Effects • Muscle and jaw aches – treat with mild analgesic • Confusion and disorientation in recovery phasereorientation • Tearfulness or frightened – support and reassurance • Short term memory- period immediately before and after treatment • Older patients typically present with more confusion/disorientation and require more time to recover
Long Term Side Effects • Memory loss is the most common long term side effect • Typically memory improves a few months after course of ECT is complete • Some report that memory is permanently altered, greater risk for memory impairment in older populations • Rare cases, people report changes to their personality and loss of skills and abilities
Adverse Effects • Small risk of damage to teeth, tongue, lips – mitigate with medication and “bite block” • Associated risks from general anesthetic Postictal Delirium: • Marked agitation, disorientation, poor response to commands and a sympathetic response (fight or flight) • May take 5 – 45 min to recover • Patient often amnesic for the episode • Manage supportively with reassurance and/or pharmalogically (benzodiazepines and/or haldol) •
Adverse Effects continued… Cognitive Changes: • Psychiatrist to assess baseline Mo. CA , monitor for cognitive changes during treatment • Reassess Mo. CA frequently throughout the course of ECT - minimum q 6 months Mitigate cognitive changes by: • Adjusting medications • Changing electrode placement from bilateral to right unilateral • Decrease the stimulus dose • Change interval between treatments • Consider suspending a treatment course
Adverse Effects continued… Treatment emergent Hypomania or Mania: • Occurs more frequently with bipolar illness or family history of bipolar Treatment options/strategies to mitigate: • Same strategies used for cognitive changes • Stop ECT and treat with mood stabilizer/antipsychotic • Suspend and observe patient
Role of Nursing • Nurses play important role in the delivery of ECT • Emotional support and education for patients and families • Assist with coordinating care • Collaborate with Interprofessional team throughout the continuum of care: assisting with Pre-ECT preparation, assisting and monitoring during treatment procedure, recovery and assessment of treatment response Post. ECT
Emotional Support and Education • ECT patients are often anxious prior to their treatment; particularly if it’s earlier in their treatment course (Vera, 2012). • The client may be apprehensive or have been exposed to myths about ECT. Encourage them to express these feelings, offer re-assurance, clarify misconceptions and emphasis therapeutic value (Vera, 2012). • Patients and family may also have questions about the procedure or post-ECT care. Take the time to address these concerns and re-assure family members • Provide patients and families with written, oral and/or visual media information and resources See Appendix E Patient Handouts in Learning Package
Pre-ECT Preparation Pre-ECT preparation will be the responsibility of inpatient nursing and/or ECT RN (for outpatients only) • • Complete Pre-Anaesthetic Questionnaire Height and weight, baseline set of vitals, glucometer if diabetic Patient to remain NPO Benzodiazepines held 1700 hrs night before procedure. All other medications held the day of procedure, unless otherwise directed by the physician. Note: Lithium may be held or reduced prior to treatment Patients to be dressed in gown, remove metal objects, eyewear, hearing aids, dentures Please ensure patient has voided prior to ECT, offer incontinent pad if appropriate Establish peripheral IV if competent to do so Ensure patient’s ID and allergy bands are on • See Appendix E and F- Pre Anesthetic Questionnaire; Clinical Protocol • •
Pre-ECT Preparation continued… Checklist in Learning Package Using Nursing Pre-procedure Checklist, ensure all required documentation and paperwork is complete and filed in ECT section of the patients chart Documents include: • Order Set and Clinical protocol • Consent Form • Medical Clearance Form • ECG • Chest X ray • Blood work See Appendix F Nursing Pre-Procedure • • • Mo. CA Anaesthetic Consult Internal Medicine Consult Psychiatry Consult Current CMAR

Treatment Room Pre-ECT Preparation
Chart Review and Documentation • Verify that Clinical Protocol has been followed • Ensure all documents and assessments are complete • Review allergies • Verify patient identification and allergy band • Review medications: communicate any medications administered the morning of procedure to physicians • ;
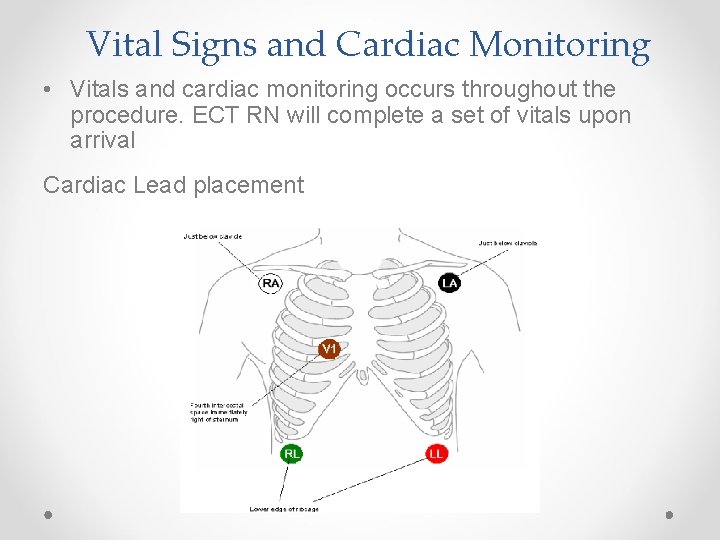
Vital Signs and Cardiac Monitoring • Vitals and cardiac monitoring occurs throughout the procedure. ECT RN will complete a set of vitals upon arrival Cardiac Lead placement

Skin Preparation Abrasive paste Conductive Gel
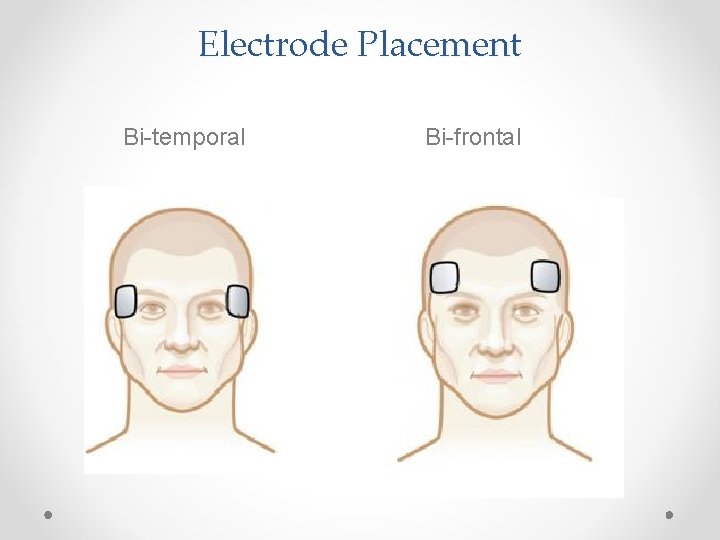
Electrode Placement Bi-temporal Bi-frontal
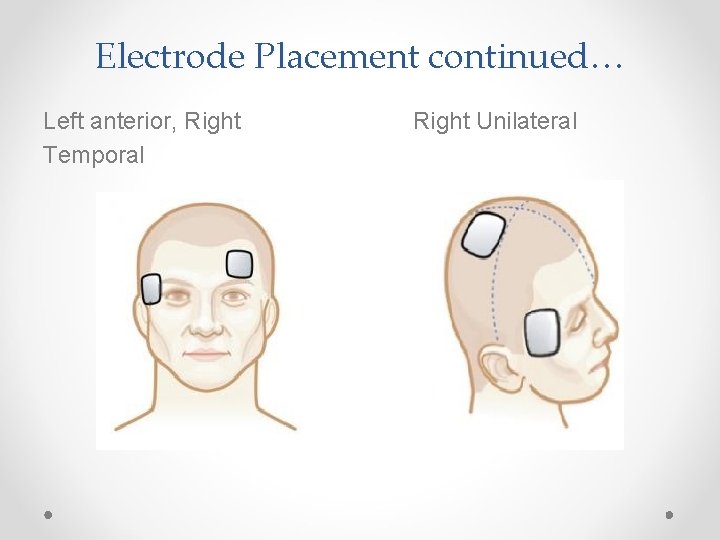
Electrode Placement continued… Left anterior, Right Temporal Right Unilateral
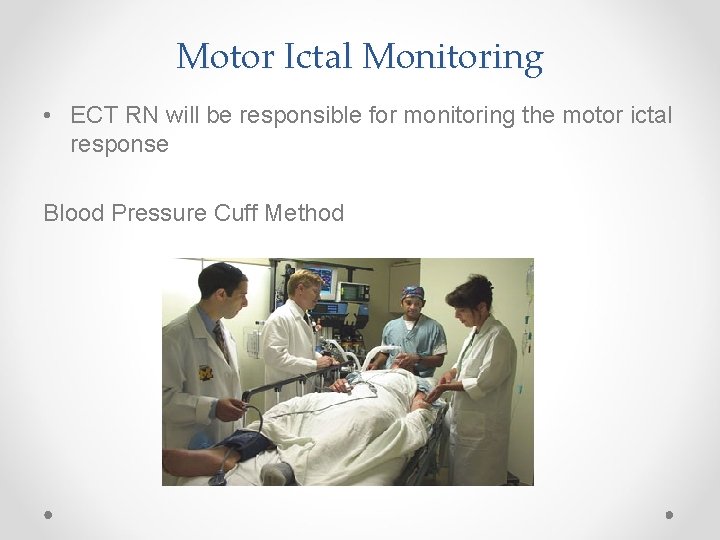
Motor Ictal Monitoring • ECT RN will be responsible for monitoring the motor ictal response Blood Pressure Cuff Method
Drugs Infused prior to ECT Muscle Relaxant Opioid Analgesic Sleep Induction The following drugs are given IV push by the anesthetist prior to ECT: • Succinylcholine (muscle relaxant)- be wary of Malignant Hyerthermia • Remifentanil (. 5 -1. 0 mcg/KG)-reduces amount of propofol required • Propofol (titrated to effective dose to induce sleep)
Supporting Client Ventilation • Anesthetist will support patient airway
Insertion of Bite Block Anesthetist inserts the bite block Autoclavable Single per patient use (throughout the series)
ECT Stimulus • Psychiatrist delivers ECT stimulus. Usually 1 -2 minutes after succinylcholine given. • Psychiatrist primarily monitors the EEG readings • A good seizure will have a gradual onset and last at least 20 seconds. Any seizure lasting longer that 3 minutes is terminated pharmalogically • It is possible the first ECT stimulus will have no effectand will need to be delivered a second time. The anesthetist must approve of this second stimulus.
Post-Stimulus • 2 sets of post-ECT vitals are taken approx. 3 min apart • The patient remains in the ECT suite until they are awake and then are transferred to the recovery area • ECT RN will prepare for next patient
Recovery Phase
Recovery • Patients 65 and over remain in recovery for approx. 1 hour; under 65 for approx. 40 minutes • Vital signs are taken Q 10 minutes in recovery • Temperature is taken upon arrival to the unit ( to check for MH) • Nurse orientates patient to their environment; lets them know they have had their treatment. • Patient cognition is monitored at all checks
Recovery • After approx. 15 -20 minutes in recovery, the nurse will ask patient the date, day, year etc. • Post Anaesthesis Discharge Scoring System (PADSS) in order to be D/C’d from recovery, back to their inpatient room or home • Prior to discharge from recovery, the psychiatrist will meet with the patient and discuss the efficacy of treatment and write the next order
Discharge from Recovery • The IV is removed by the nurse prior to patient Inpatient’s: • Patient’s will be transported via wheelchair by a porter when the discharge criteria has been met • Ensure inpatient staff are notified and report is complete prior to transfer.
Discharge from recovery continued… Outpatient Considerations: • Ensure patient is accompanied by a responsible adult when leaving-they cannot drive after the procedure, nor should they drive throughout the course of an acute series. • Instruct patient and accompanying adult about possible side effects from anesthesia and whom to contact regarding untoward reactions • Alert family to assess need for supervision 24 hours after procedure
Return Transfer to Inpatient Unit • Assess patients physical and mental status • Vitals completed upon return to unit. • Offer nutrition • Assess frequency of observation based on patients vital signs and level of consciousness – includes readiness to go out on pass
References Acton, M. , RN, Burgi, P. , MD, Donnelly, M. , MD, Gosselin, C. , MD, Isomura, T. , MD, & Kang, N. , MD. (n. d. ). Electroconvulsive Therapy Guidelines for Health Authorities in British Columbia (pp. 1 -148) (Canada, Mental Health Evaluation & Community Consultation Unit, British Columbia Ministry of Health Service). Chan, P. , Graf, P. , Enns, M. , Delva, N. , Gilron, I. , Lawson, J. S. , . . . Martin, B. (2012). Canadian Survey of Standards of Electroconvulsive Therapy: A call for accreditation. The Canadian Journal of Psychiatry, 57(10), 634 -642. Kellner CH, Knapp R, Husain MM, et al. Bifrontal, bitemporal and right unilateral electrode placement in ECT: randomised trial. The British Journal of Psychiatry. 2010; 196(3): 226 -234. doi: 10. 1192/bjp. bp. 109. 066183. Merchant, R. , MD, Chartrand, D. , MD, Dain, S. , MD, Dobson, G. , MD, Kurreck, M. M. , MD, Lagace, A. , MD, . . . Sullivan, P. , MD. (n. d. ). Guidelines to the Practice of Anesthesia – Revised Edition 2016. Canadian Journal of Anesthesia, 63, 86 -112. Petrides, G. , Tobias, K. G. , Kellner, C. H. , & Rudorfer, M. V. (2011, July). Continuation and Maintenance Electroconvulsive Therapy for Mood Disorders: Review of the Literature. Neuropsychobiology, 64(3), 129 -140. Merchant, R. , MD, Chartrand, D. , MD, Dain, S. , MD, Dobson, G. , MD, Kurreck, M. M. , MD, Lagace, A. , MD, . . . Sullivan, P. , MD. (n. d. ). Guidelines to the Practice of Anesthesia – Revised Edition 2016. Canadian Journal of Anesthesia, 63, 86 -112. Royal College of Psychiatrists ECT Accreditation Service (ECTAS) (2016) Standards for Administration of ECT. Hodge, S. & Buley, N. •
- Slides: 41