Electrical Cardiometry for the measurement of cardiac output

- Slides: 75
Electrical Cardiometry for the measurement of cardiac output in pregnancy Tom Archer, MD, MBA Clinical Professor and Director of Obstetric Anesthesia University of California, San Diego Modified June 19, 2013
Our Research Team • Tom Archer, MD, MBA • Jerry Ballas, MD, MPH • Kristin Mantell, MD • Kristen Buono, MD • Thao Huyhn-Covey RDCS
Cardiac output in OB—why? Post-partum hemorrhage? Preeclampsia? Cardiomyopathy? Sepsis? Valvular heart disease? Anesthesia? Aortocaval compression? Obesity? Uterotonic titration? Study of normal events?
Cardiac output in OB—why not? Predominantly awake and healthy patients Happy, “normal” event (hopefully) Reduced tolerance for discomfort during personal, happy, normal event There has been no good technology to measure cardiac output comfortably, cheaply and continuously in awake patients!
But first, the bad news about Electrical Cardiometry… I am fascinated with this technology but it has several possibly insurmountable barriers to its being accepted…
“Problems” with electrical cardiometry (EC) • EC is too easy to use, both for operator and patient. • EC does not look impressive. • EC does not require bulky and intimidating equipment. • EC is not even slightly uncomfortable for the patient. • EC does not require advanced training.
“Problems” with electrical cardiometry (EC) • EC does not require assistants or technicians to obtain measurements and to clean and maintain the equipment. • EC does not required the placement of large tubes in large blood vessels.
“Problems” with electrical cardiometry (EC) • EC costs almost nothing on a per-use basis (four EKG patches). • EC does not require workshops in order to master it. • There is no American Society of Electrical Cardiometry (yet) for you to belong to and which will certify you so that you can have more cool letters behind your name such as “FASEC”. • EC is not fashionable (yet).
“Problems” with electrical cardiometry (EC) • But, the worst aspect of EC-- which probably makes it totally unacceptable to the medical community– is that: • EC involves mathematics and electricity.
All kidding aside… • Electrical cardiometry is a very promising technology which I believe may facilitate patient management not just in obstetrics, but in all of medicine…
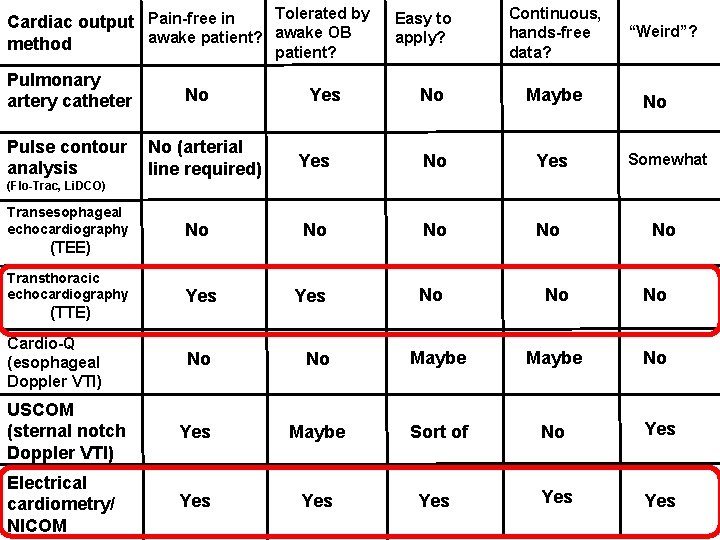
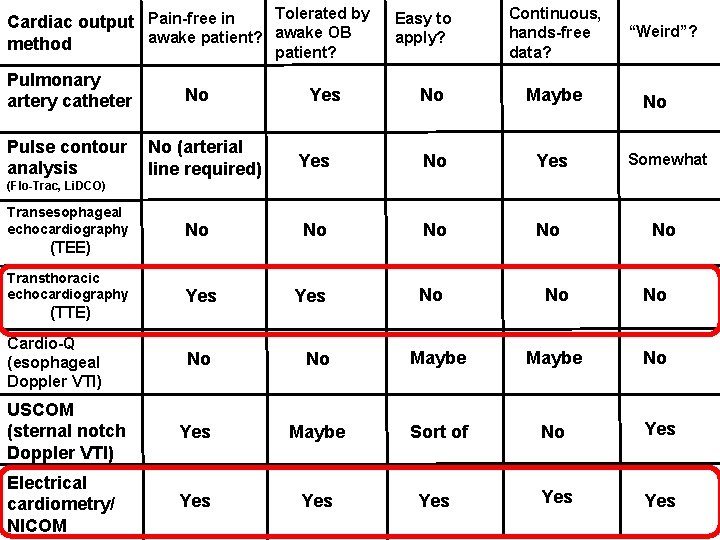
Tolerated by Cardiac output Pain-free in awake patient? awake OB method patient? Pulmonary artery catheter Pulse contour analysis No No (arterial line required) Yes Easy to apply? Continuous, hands-free data? “Weird”? No Maybe Yes No Yes Somewhat No No Yes No No (Flo-Trac, Li. DCO) Transesophageal echocardiography (TEE) Transthoracic echocardiography (TTE) Cardio-Q (esophageal Doppler VTI) No Yes No No Maybe No USCOM (sternal notch Doppler VTI) Yes Maybe Sort of No Yes Electrical cardiometry/ NICOM Yes Yes Yes
Background and Review
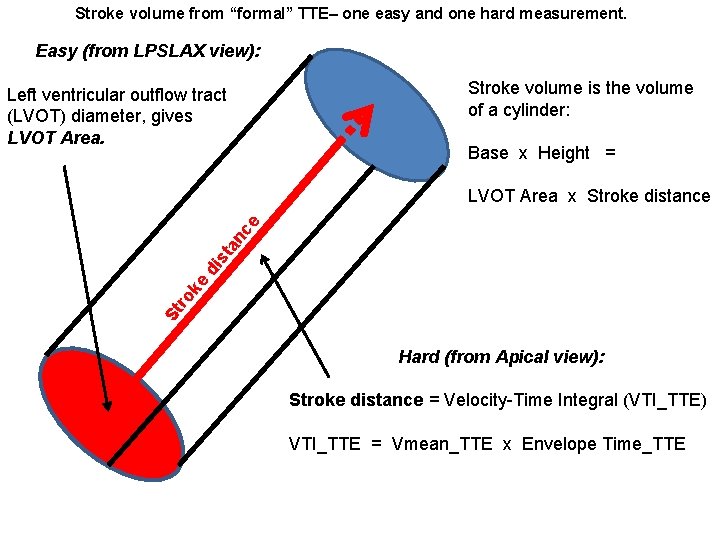
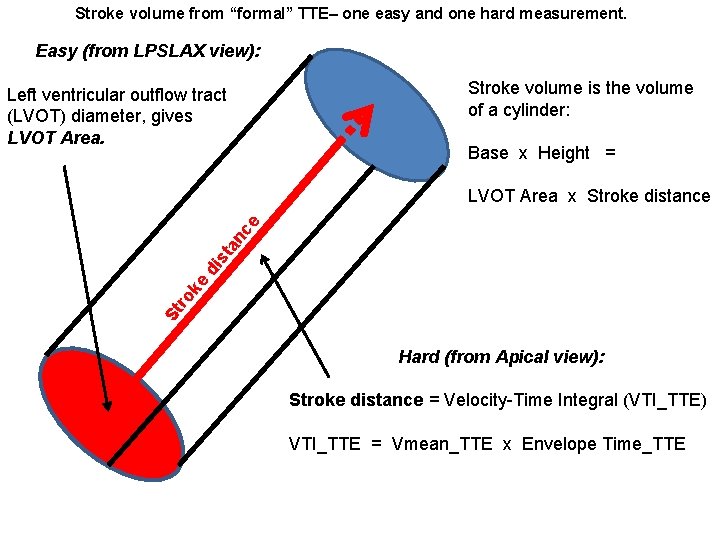
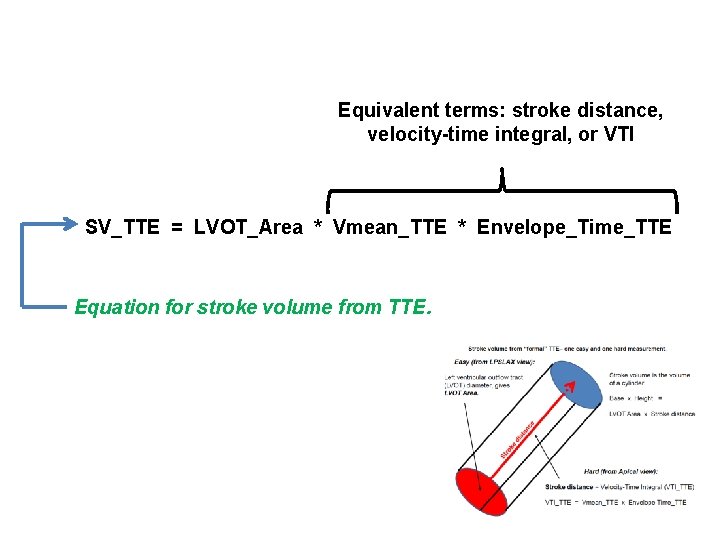
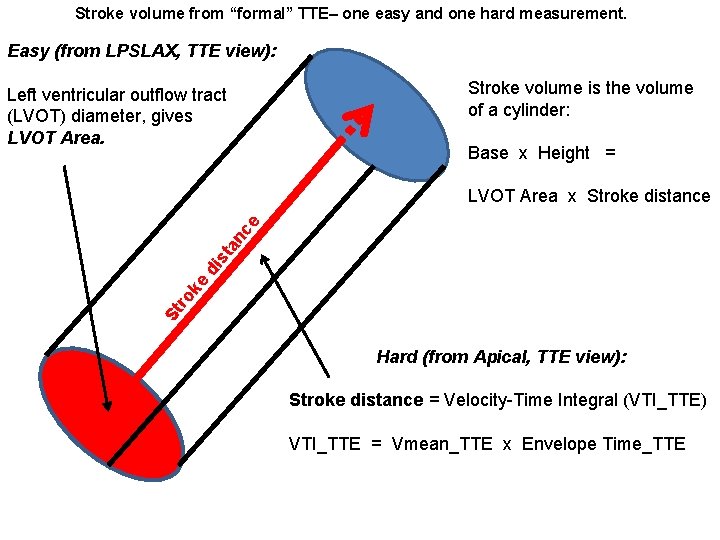
Stroke volume from “formal” TTE– one easy and one hard measurement. Easy (from LPSLAX view): Stroke volume is the volume of a cylinder: Left ventricular outflow tract (LVOT) diameter, gives LVOT Area. Base x Height = St ro ke di st a nc e LVOT Area x Stroke distance Hard (from Apical view): Stroke distance = Velocity-Time Integral (VTI_TTE) VTI_TTE = Vmean_TTE x Envelope Time_TTE
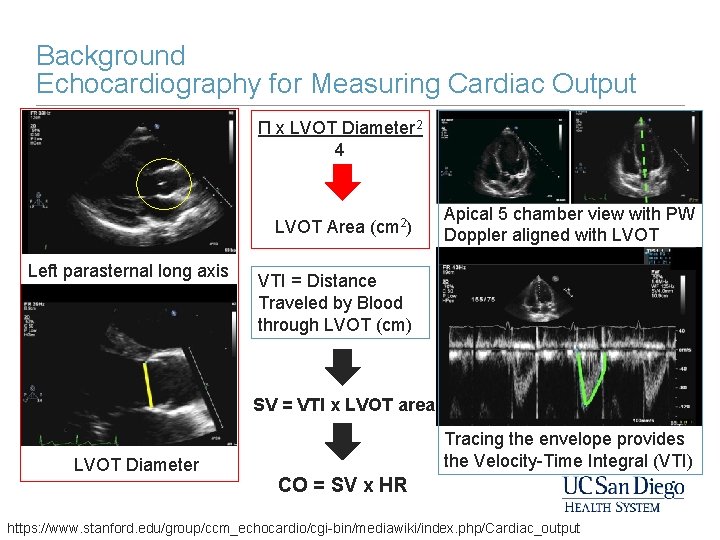
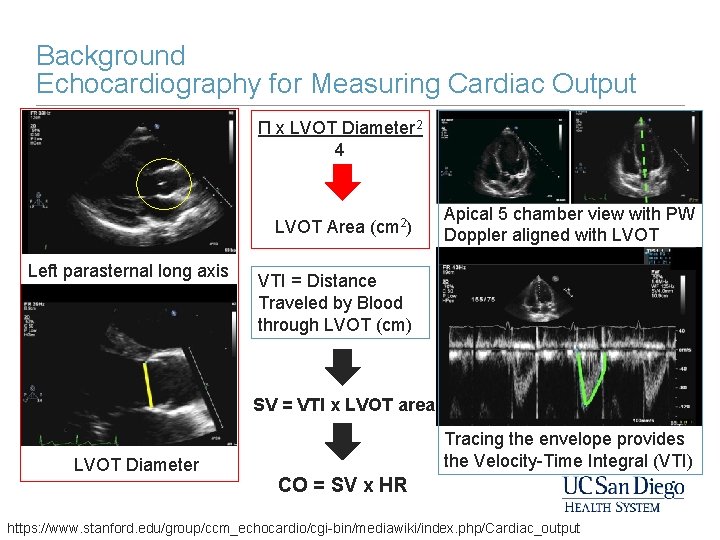
Background Echocardiography for Measuring Cardiac Output Π x LVOT Diameter 2 4 LVOT Area Left parasternal long axis (cm 2) Apical 5 chamber view with PW Doppler aligned with LVOT VTI = Distance Traveled by Blood through LVOT (cm) SV = VTI x LVOT area LVOT Diameter Tracing the envelope provides the Velocity-Time Integral (VTI) CO = SV x HR https: //www. stanford. edu/group/ccm_echocardio/cgi-bin/mediawiki/index. php/Cardiac_output
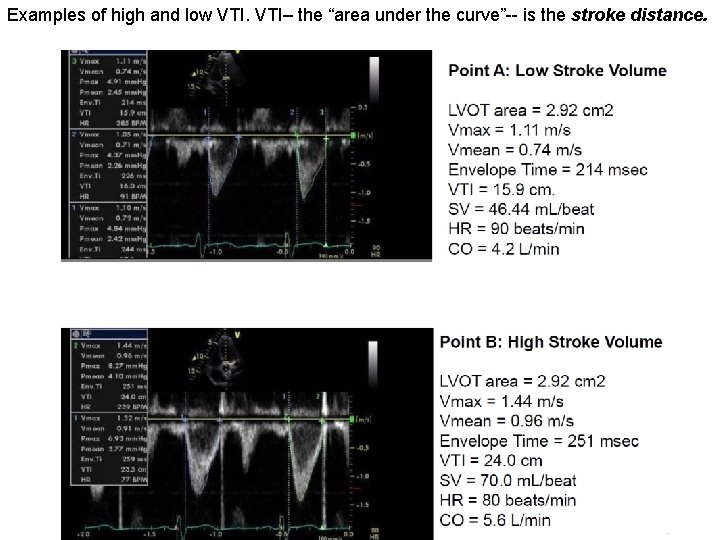
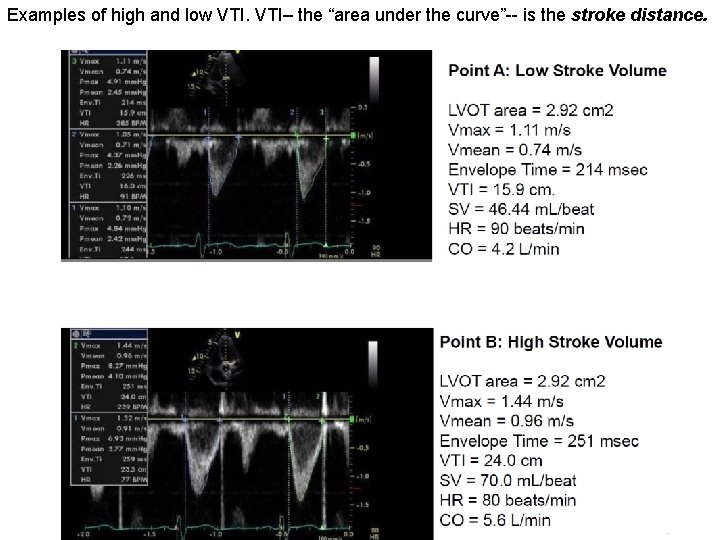
Examples of high and low VTI– the “area under the curve”-- is the stroke distance.
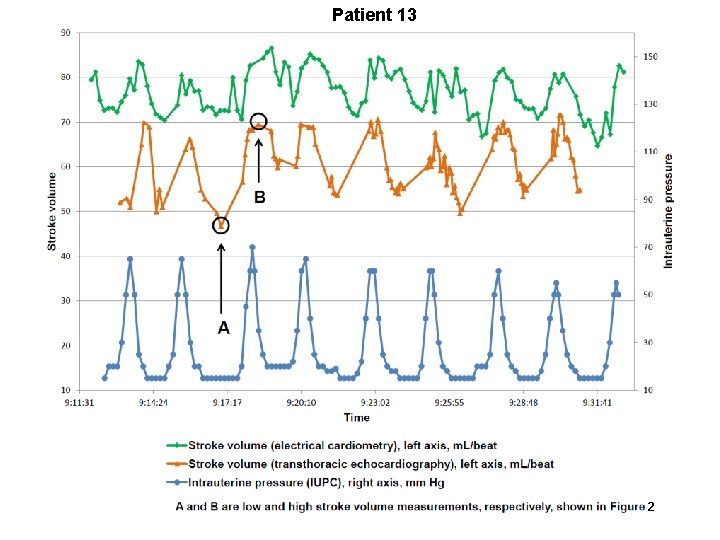
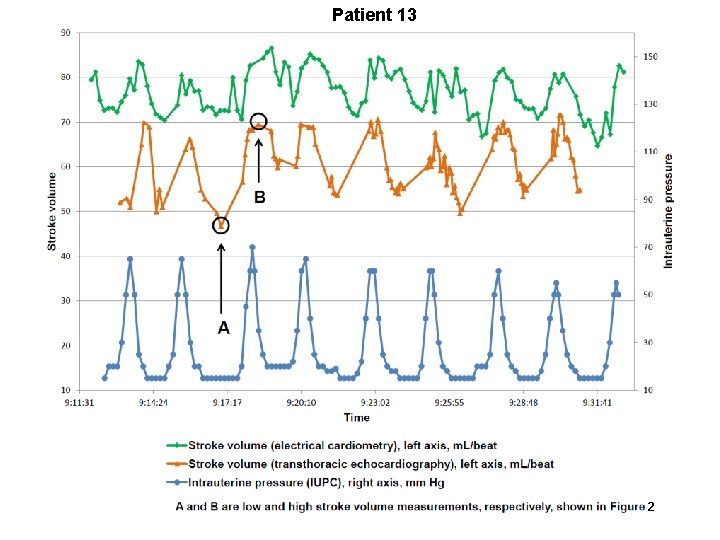
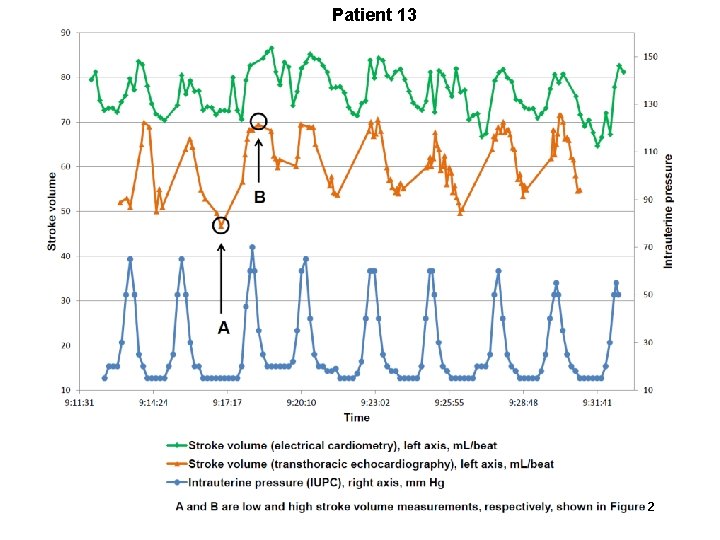
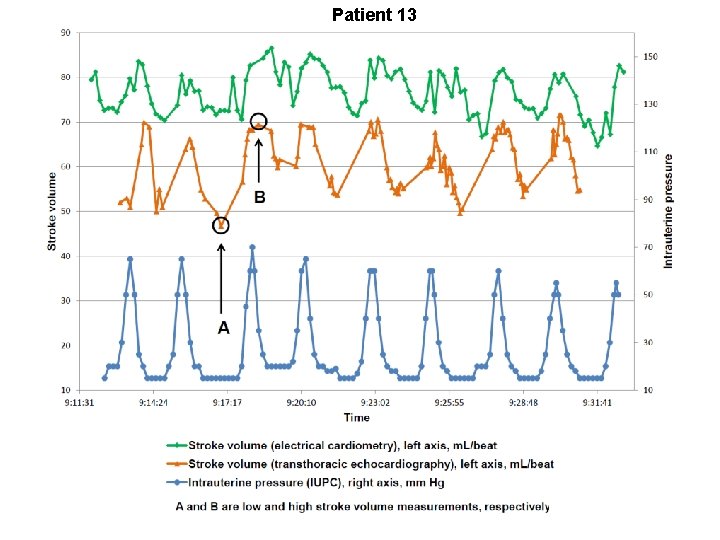
Patient 13 2
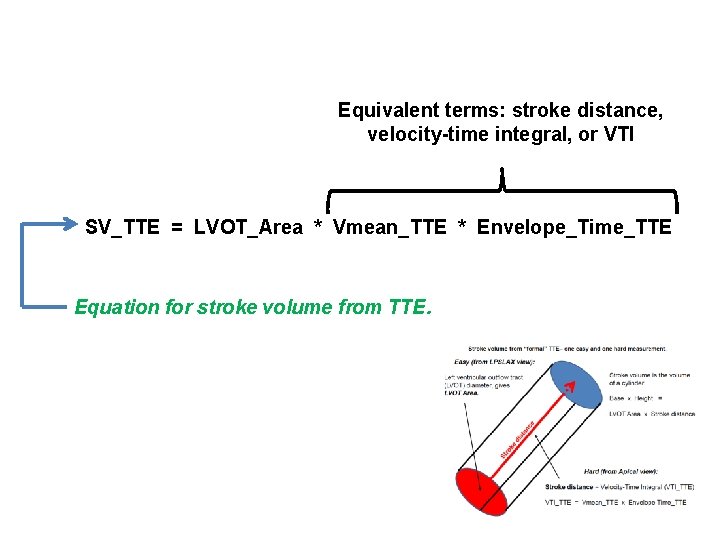
Equivalent terms: stroke distance, velocity-time integral, or VTI SV_TTE = LVOT_Area * Vmean_TTE * Envelope_Time_TTE Equation for stroke volume from TTE.
Summary of study results
Summary • Non-invasive, painless, continuous and inexpensive measurement of cardiac output might be useful in some pregnant patients (as well as in critical care in general). • Electrical cardiometry, without further modification, appears to identify trends in cardiac output in pregnant patients.
Summary • Electrical cardiometry, without further modification, appears not to give acceptably accurate absolute values of cardiac output in pregnant patients. • We propose modifications to electrical cardiometry in order to deliver absolute values of cardiac output with acceptable accuracy.
Summary • We propose two models for using left ventricular outflow tract diameter together with electrical cardiometry to acquire absolute values for stroke volume: • Model A • Model B
Summary • Model A uses left ventricular outflow tract diameter to “calibrate” the existing “off the shelf” measurement of stroke volume.
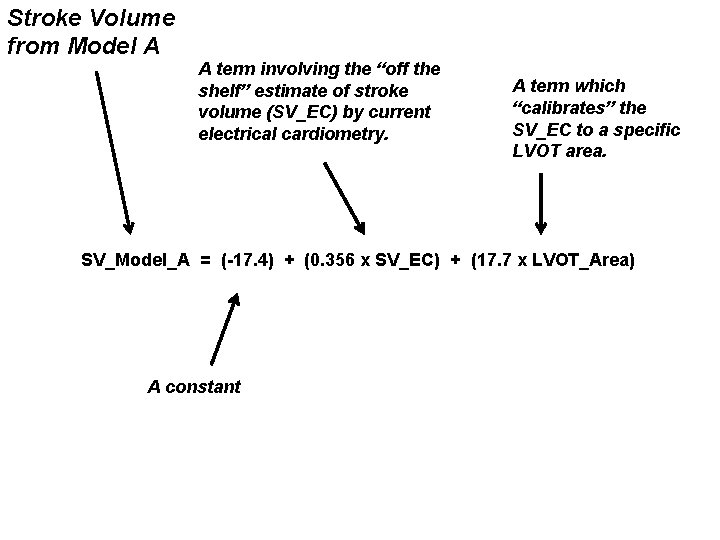
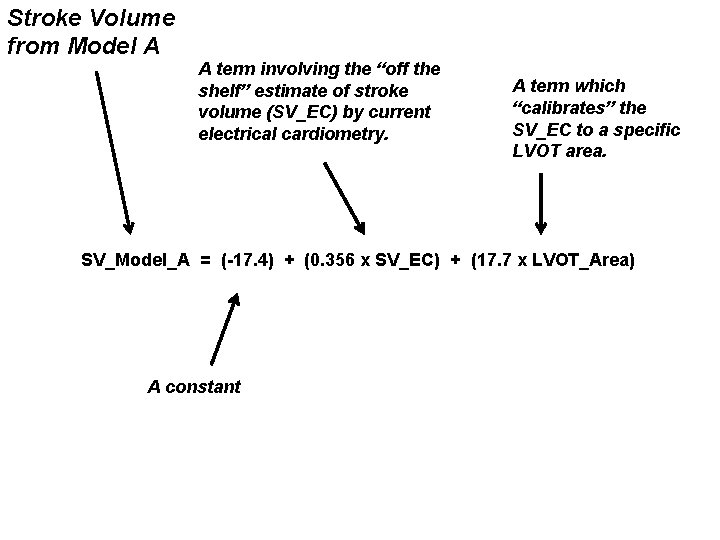
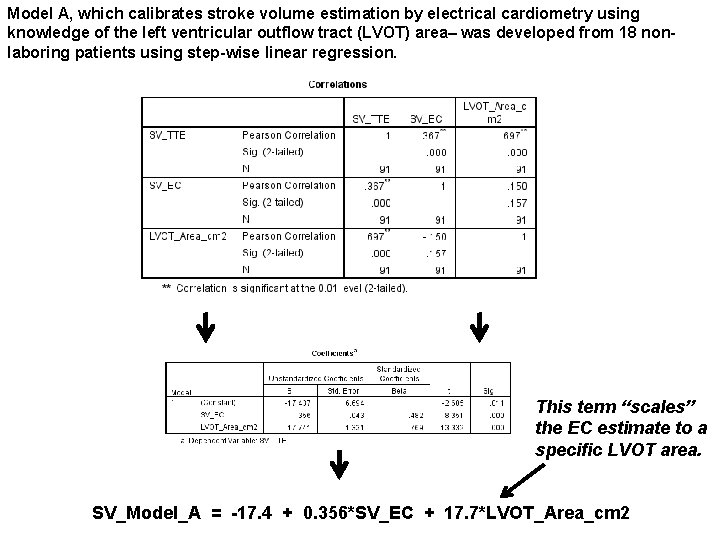
Stroke Volume from Model A A term involving the “off the shelf” estimate of stroke volume (SV_EC) by current electrical cardiometry. A term which “calibrates” the SV_EC to a specific LVOT area. SV_Model_A = (-17. 4) + (0. 356 x SV_EC) + (17. 7 x LVOT_Area) A constant
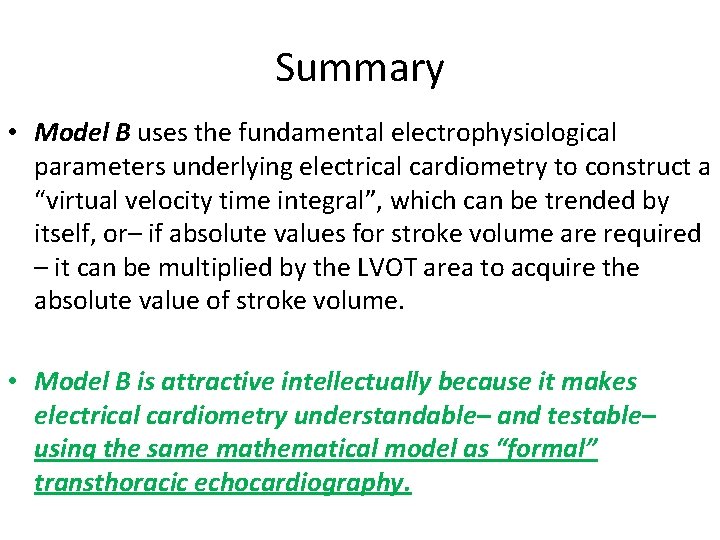
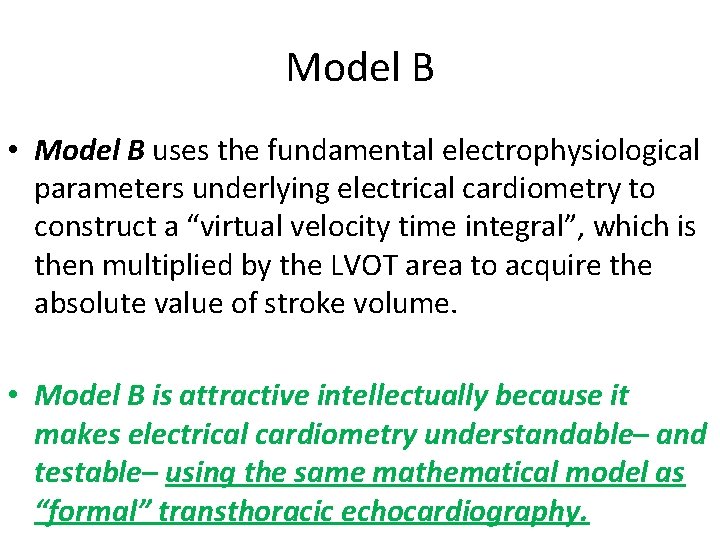
Summary • Model B uses the fundamental electrophysiological parameters underlying electrical cardiometry to construct a “virtual velocity time integral”, which can be trended by itself, or– if absolute values for stroke volume are required – it can be multiplied by the LVOT area to acquire the absolute value of stroke volume. • Model B is attractive intellectually because it makes electrical cardiometry understandable– and testable– using the same mathematical model as “formal” transthoracic echocardiography.
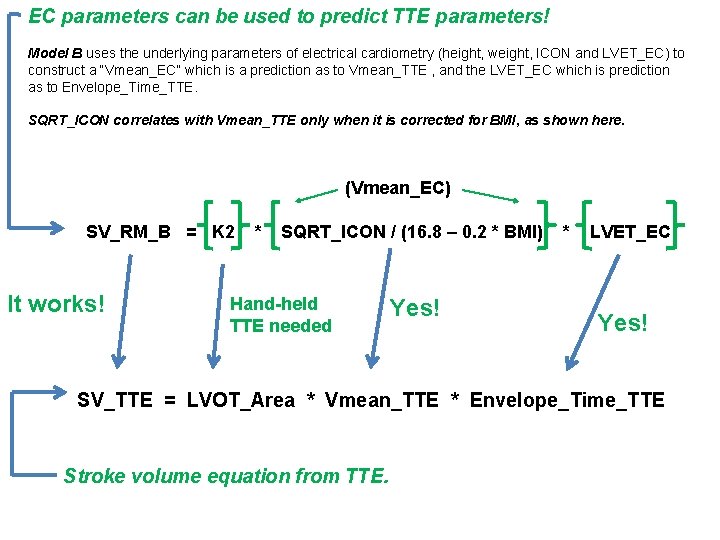
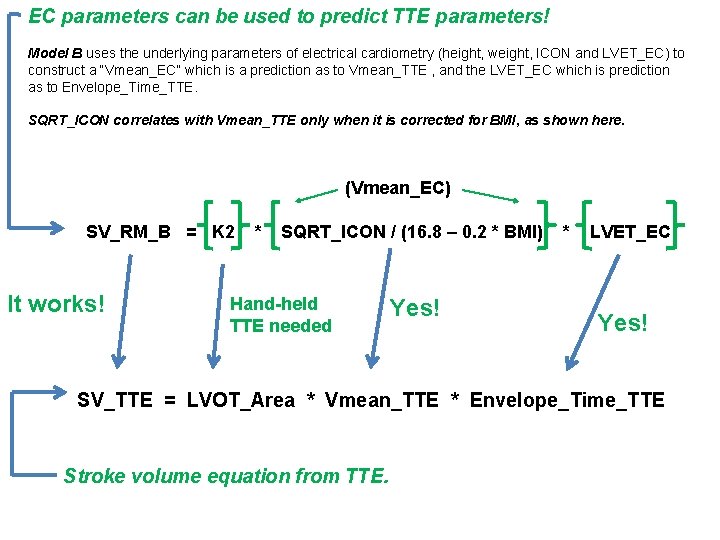
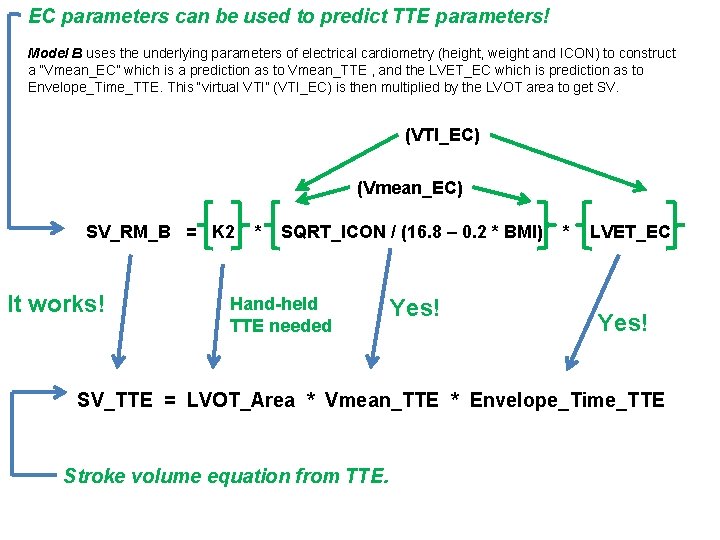
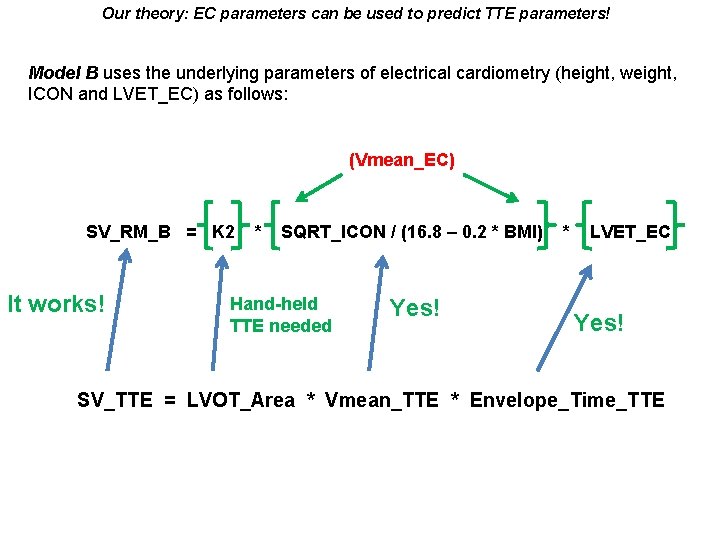
EC parameters can be used to predict TTE parameters! Model B uses the underlying parameters of electrical cardiometry (height, weight, ICON and LVET_EC) to construct a “Vmean_EC” which is a prediction as to Vmean_TTE , and the LVET_EC which is prediction as to Envelope_Time_TTE. SQRT_ICON correlates with Vmean_TTE only when it is corrected for BMI, as shown here. (Vmean_EC) SV_RM_B = K 2 It works! * SQRT_ICON / (16. 8 – 0. 2 * BMI) Hand-held TTE needed Yes! * LVET_EC Yes! SV_TTE = LVOT_Area * Vmean_TTE * Envelope_Time_TTE Stroke volume equation from TTE.
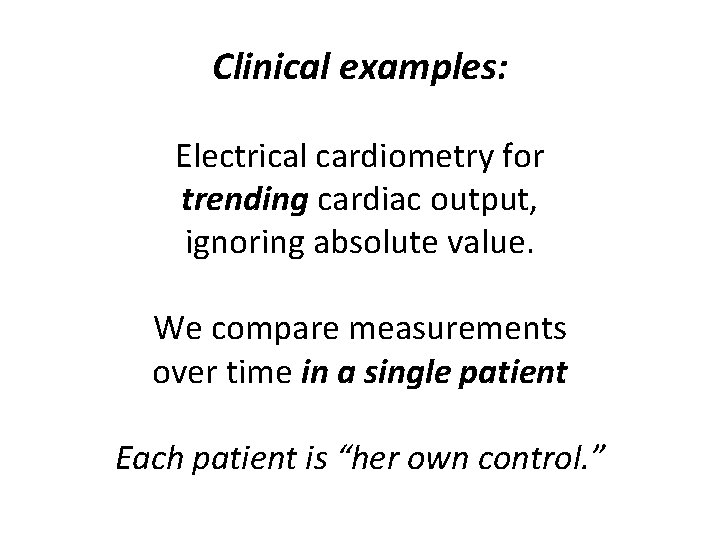
Clinical examples: Electrical cardiometry for trending cardiac output, ignoring absolute value. We compare measurements over time in a single patient Each patient is “her own control. ”
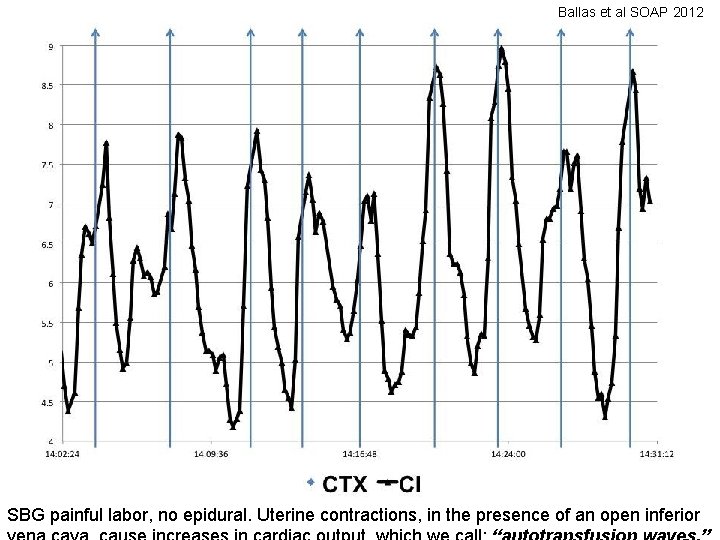
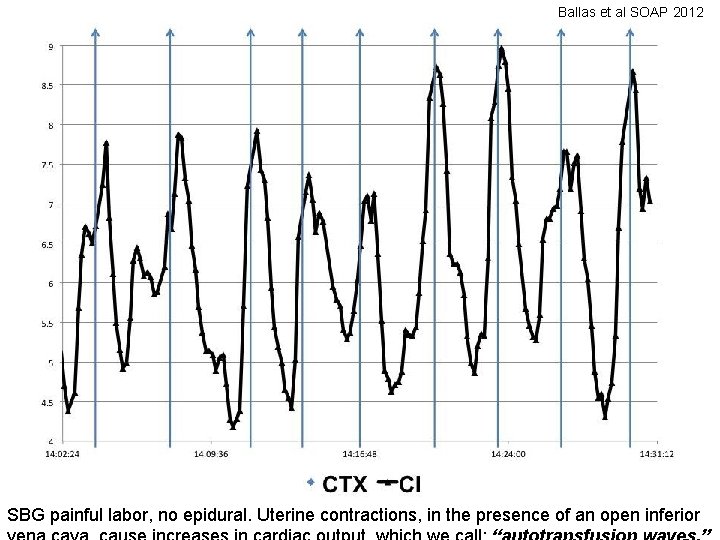
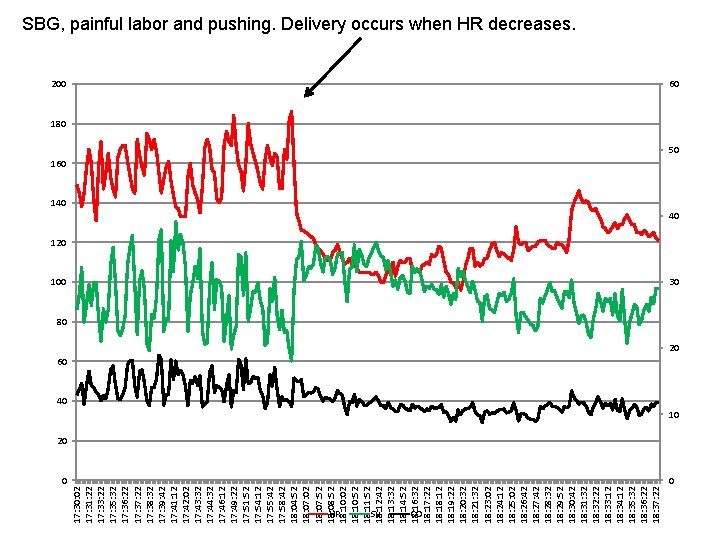
Ballas et al SOAP 2012 SBG painful labor, no epidural. Uterine contractions, in the presence of an open inferior
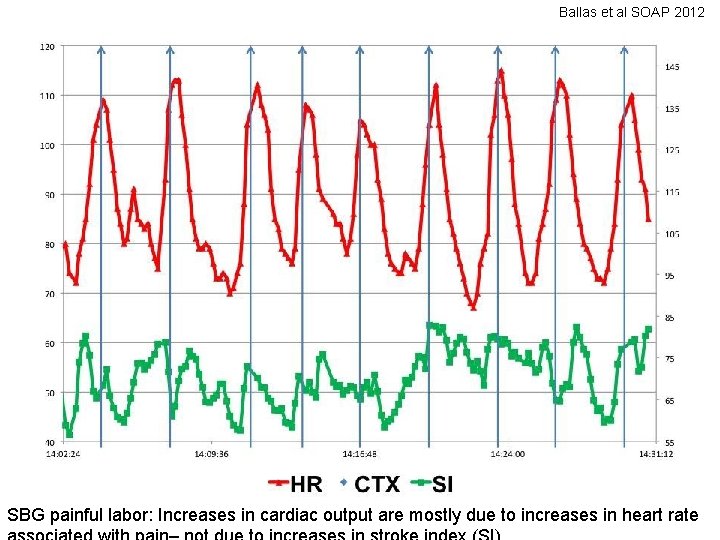
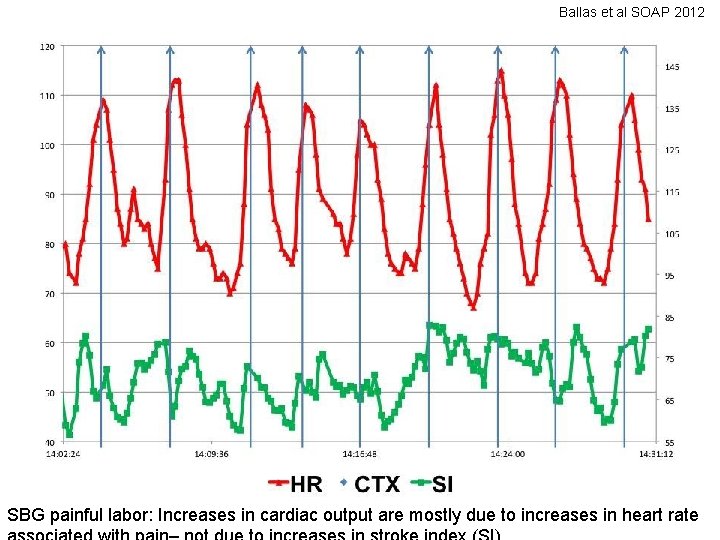
Ballas et al SOAP 2012 SBG painful labor: Increases in cardiac output are mostly due to increases in heart rate
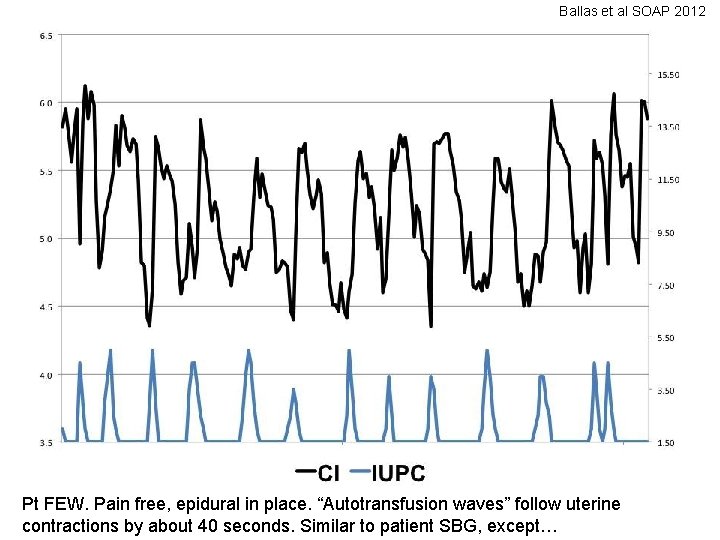
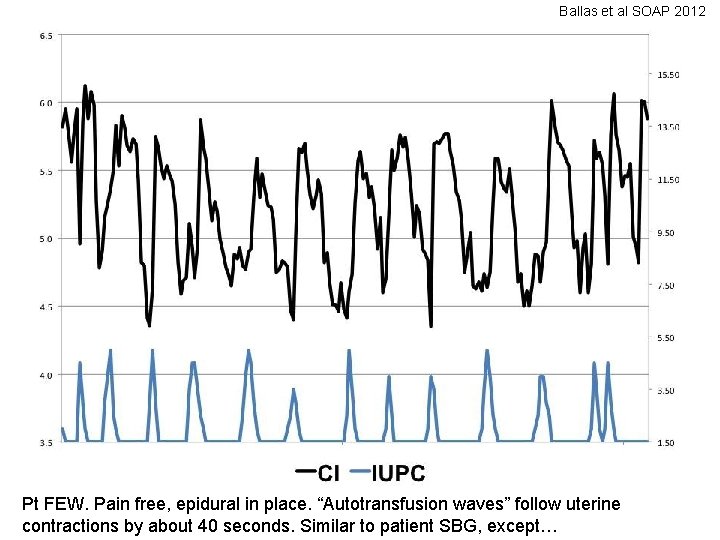
Ballas et al SOAP 2012 Pt FEW. Pain free, epidural in place. “Autotransfusion waves” follow uterine contractions by about 40 seconds. Similar to patient SBG, except…
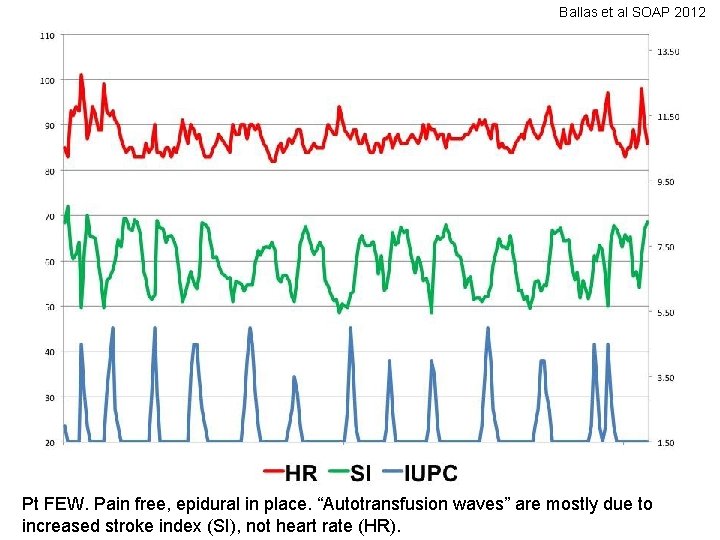
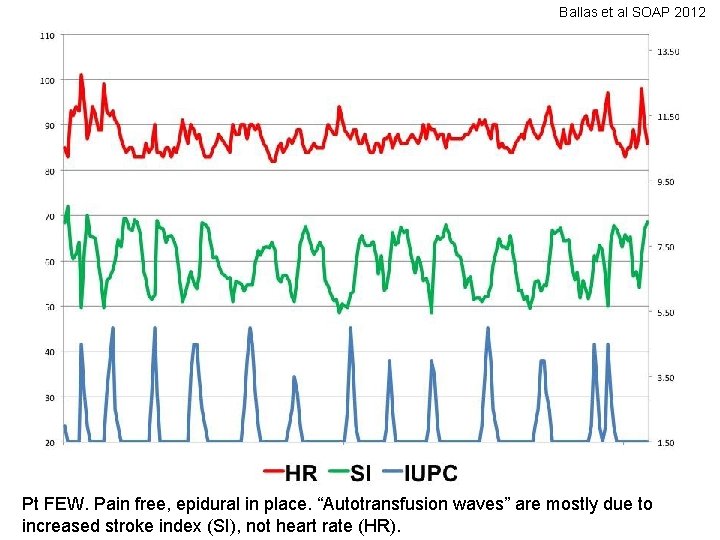
Ballas et al SOAP 2012 Pt FEW. Pain free, epidural in place. “Autotransfusion waves” are mostly due to increased stroke index (SI), not heart rate (HR).
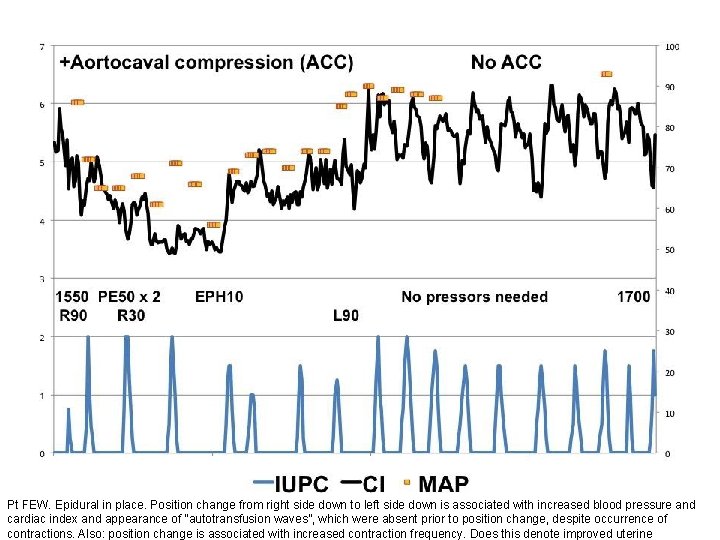
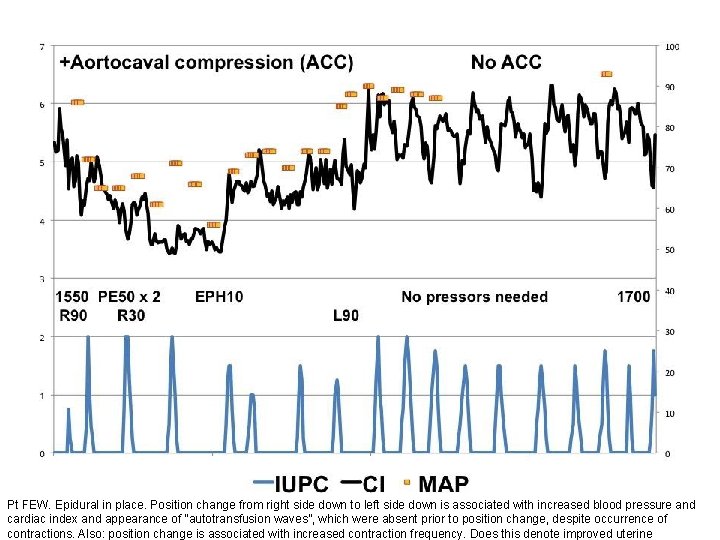
Pt FEW. Epidural in place. Position change from right side down to left side down is associated with increased blood pressure and cardiac index and appearance of “autotransfusion waves”, which were absent prior to position change, despite occurrence of contractions. Also: position change is associated with increased contraction frequency. Does this denote improved uterine
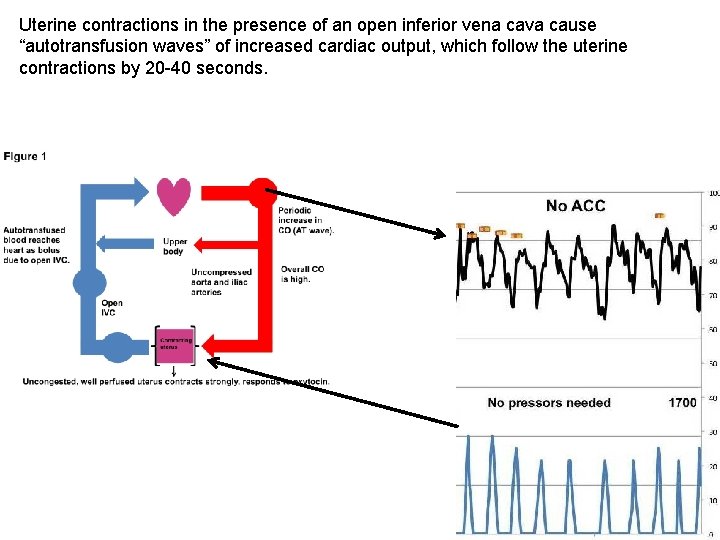
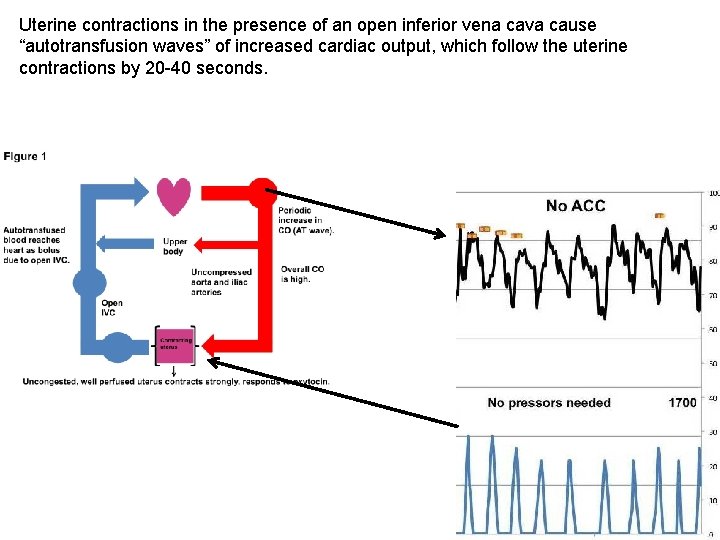
Uterine contractions in the presence of an open inferior vena cava cause “autotransfusion waves” of increased cardiac output, which follow the uterine contractions by 20 -40 seconds.
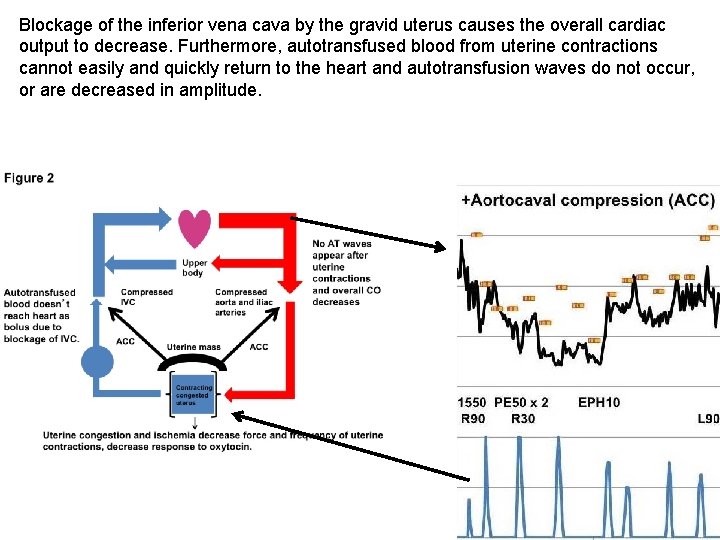
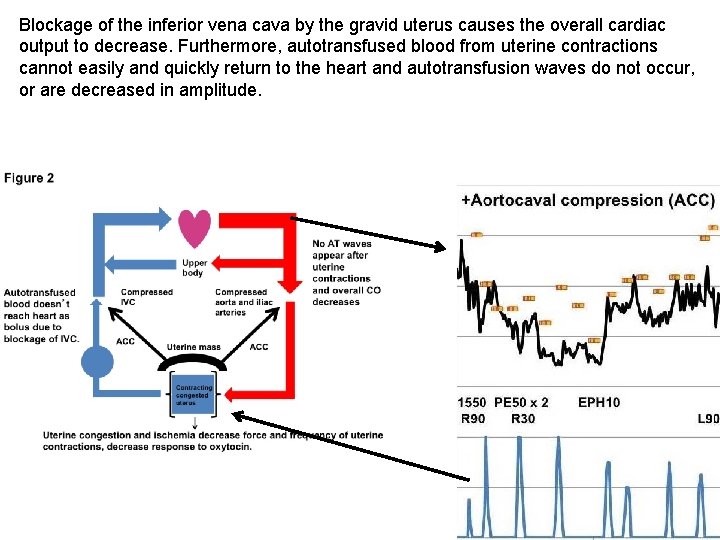
Blockage of the inferior vena cava by the gravid uterus causes the overall cardiac output to decrease. Furthermore, autotransfused blood from uterine contractions cannot easily and quickly return to the heart and autotransfusion waves do not occur, or are decreased in amplitude.
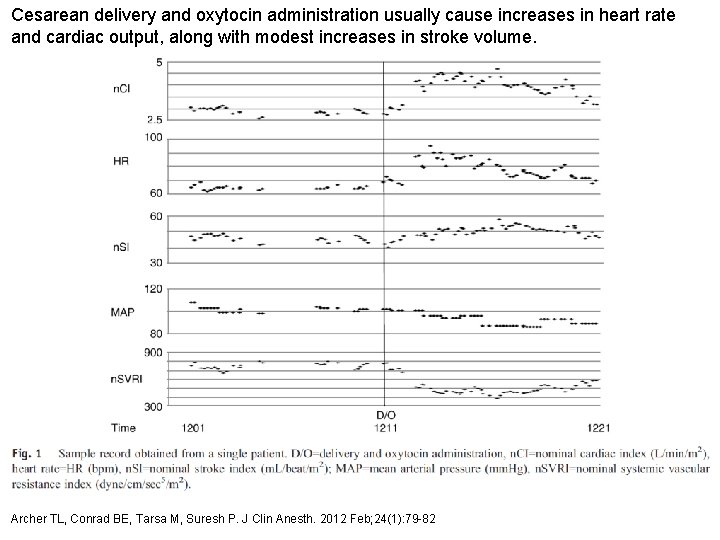
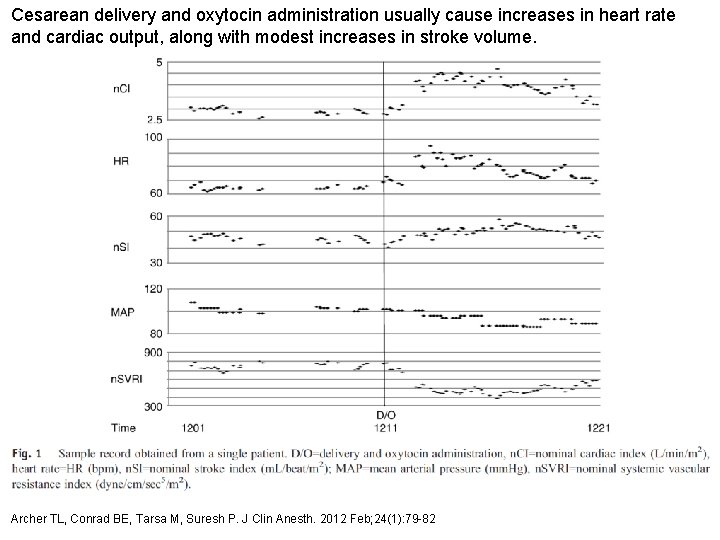
Cesarean delivery and oxytocin administration usually cause increases in heart rate and cardiac output, along with modest increases in stroke volume. Archer TL, Conrad BE, Tarsa M, Suresh P. J Clin Anesth. 2012 Feb; 24(1): 79 -82
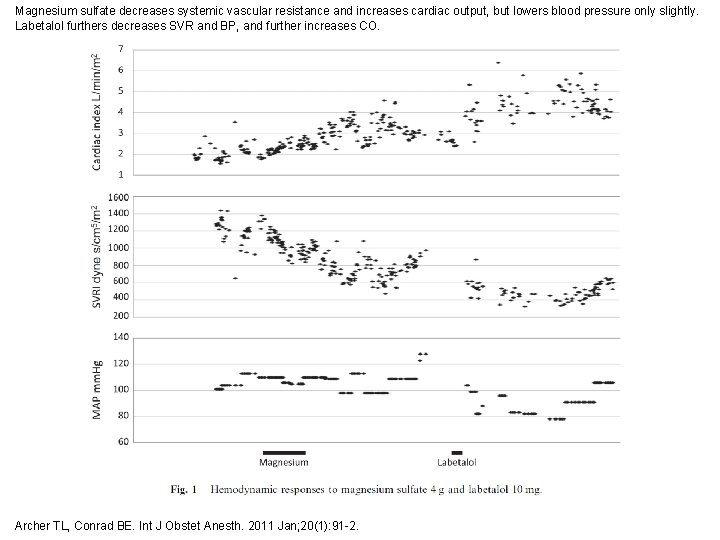
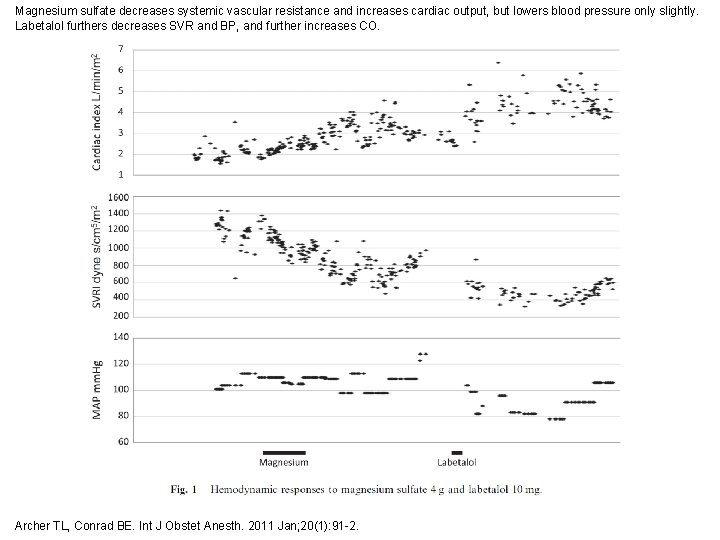
Magnesium sulfate decreases systemic vascular resistance and increases cardiac output, but lowers blood pressure only slightly. Labetalol furthers decreases SVR and BP, and further increases CO. Archer TL, Conrad BE. Int J Obstet Anesth. 2011 Jan; 20(1): 91 -2.
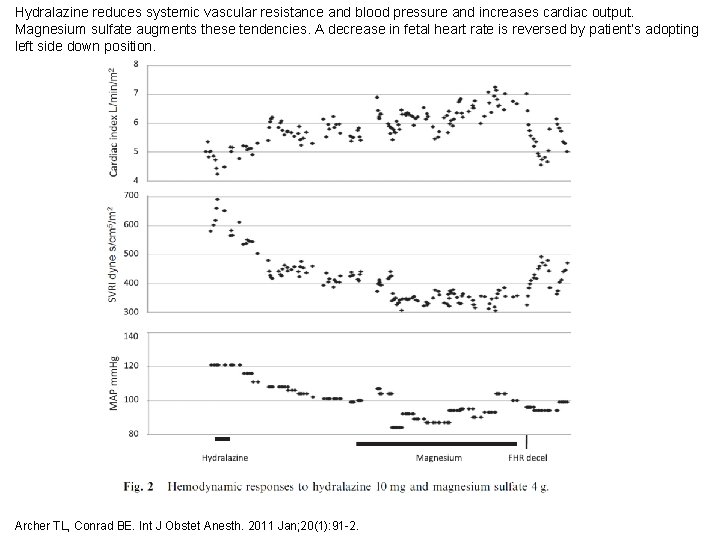
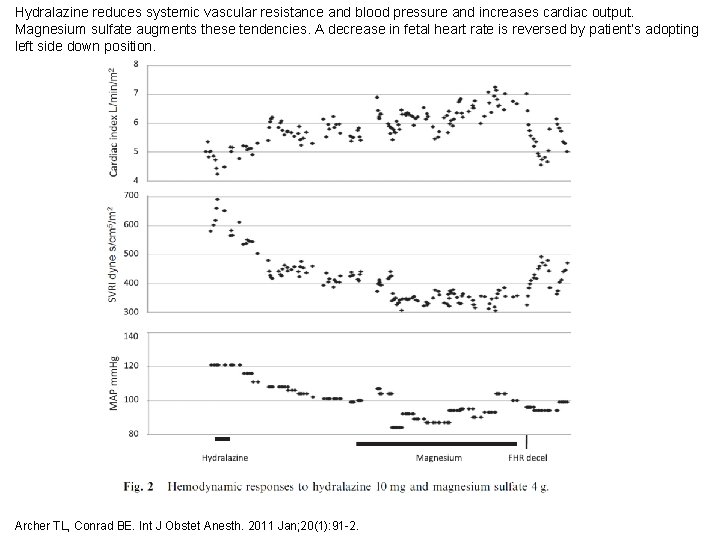
Hydralazine reduces systemic vascular resistance and blood pressure and increases cardiac output. Magnesium sulfate augments these tendencies. A decrease in fetal heart rate is reversed by patient’s adopting left side down position. Archer TL, Conrad BE. Int J Obstet Anesth. 2011 Jan; 20(1): 91 -2.
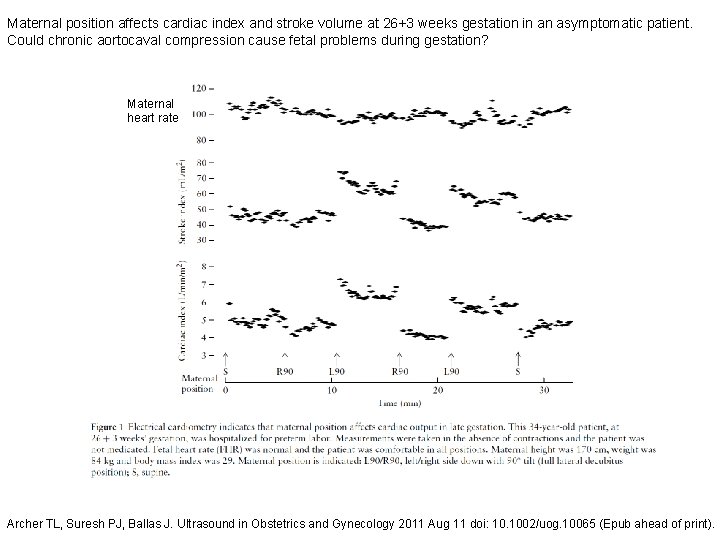
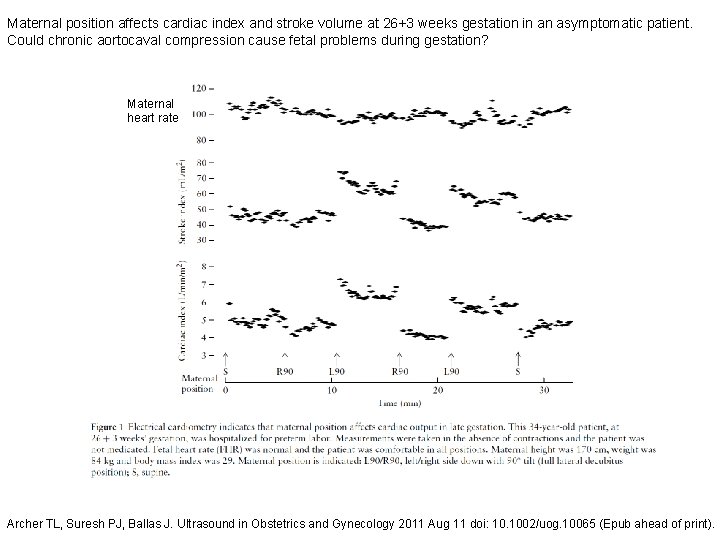
Maternal position affects cardiac index and stroke volume at 26+3 weeks gestation in an asymptomatic patient. Could chronic aortocaval compression cause fetal problems during gestation? Maternal heart rate Archer TL, Suresh PJ, Ballas J. Ultrasound in Obstetrics and Gynecology 2011 Aug 11 doi: 10. 1002/uog. 10065 (Epub ahead of print).
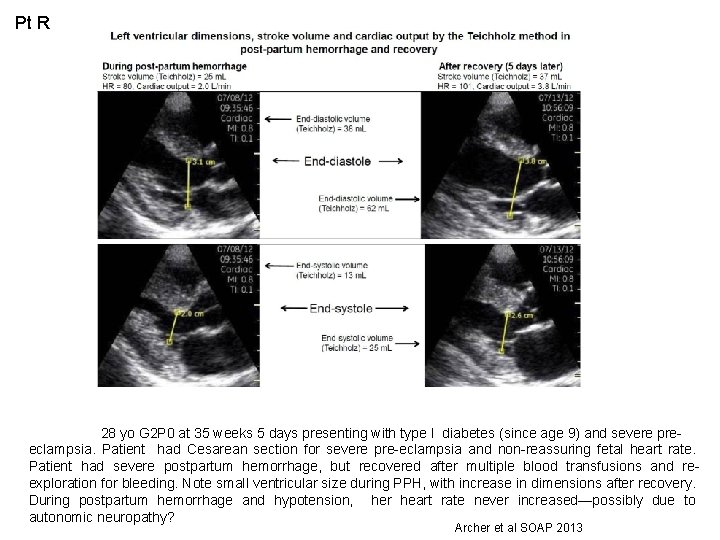
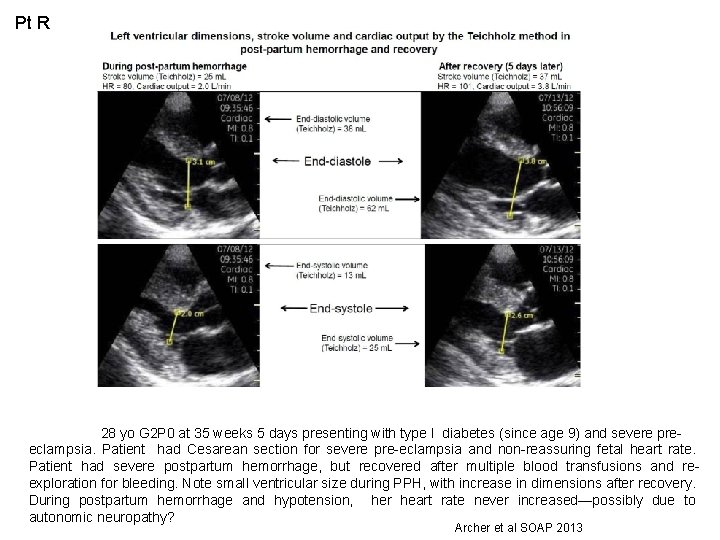
Pt R 28 yo G 2 P 0 at 35 weeks 5 days presenting with type I diabetes (since age 9) and severe preeclampsia. Patient had Cesarean section for severe pre-eclampsia and non-reassuring fetal heart rate. Patient had severe postpartum hemorrhage, but recovered after multiple blood transfusions and reexploration for bleeding. Note small ventricular size during PPH, with increase in dimensions after recovery. During postpartum hemorrhage and hypotension, her heart rate never increased—possibly due to autonomic neuropathy? Archer et al SOAP 2013
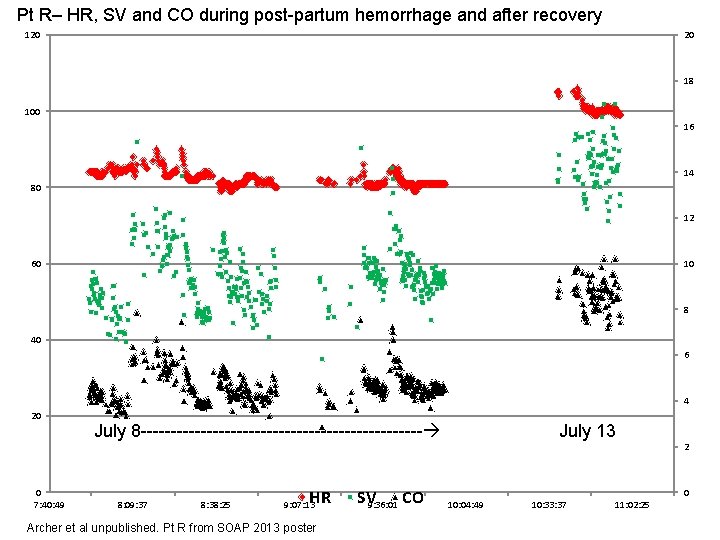
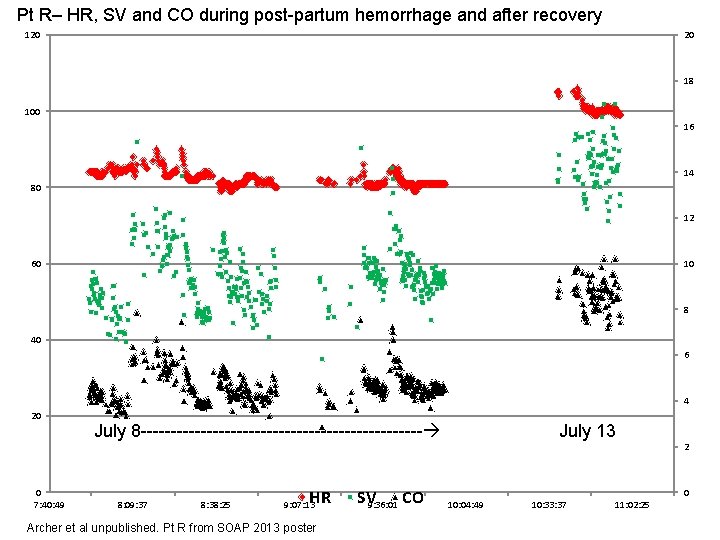
Pt R– HR, SV and CO during post-partum hemorrhage and after recovery 120 20 18 100 16 14 80 12 60 10 8 40 6 4 20 0 7: 40: 49 July 8 ------------------------ 8: 09: 37 8: 38: 25 HR 9: 07: 13 Archer et al unpublished. Pt R from SOAP 2013 poster SV 9: 36: 01 CO July 13 2 0 10: 04: 49 10: 33: 37 11: 02: 25
Electrical cardiometry for absolute value of cardiac output. Except for two slides which are noted, all measurements are from 23 laboring and non-laboring patients with their left side down and with time difference between TTE and EC measurements = or < 10 sec.
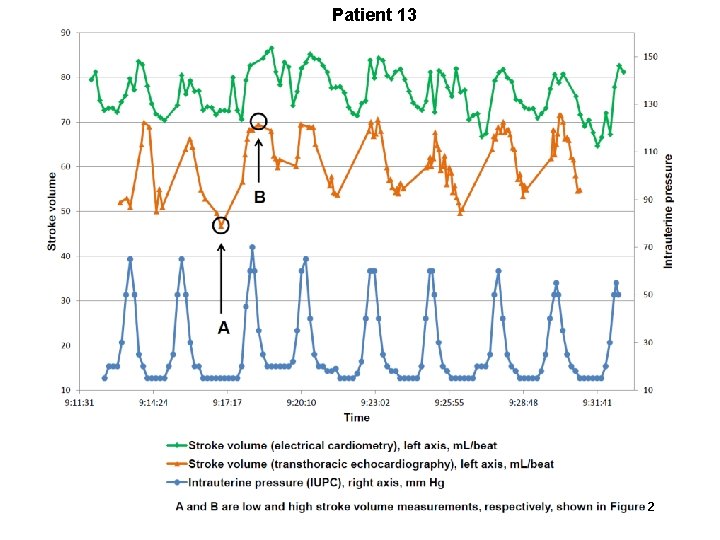
Patient 13 2
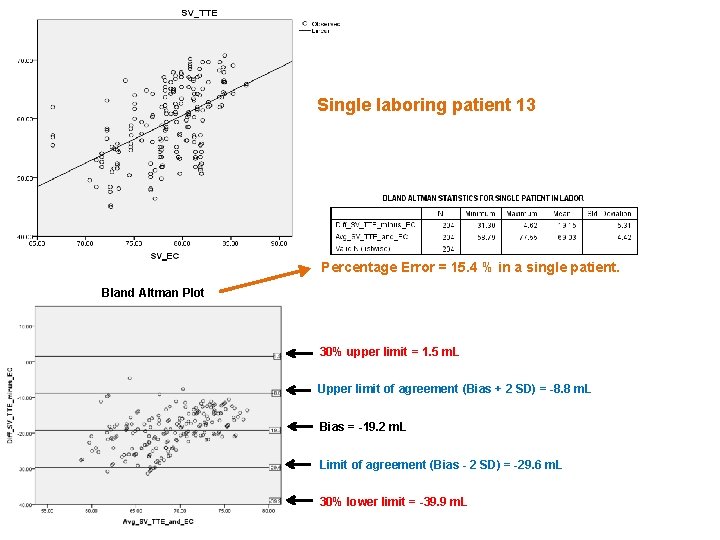
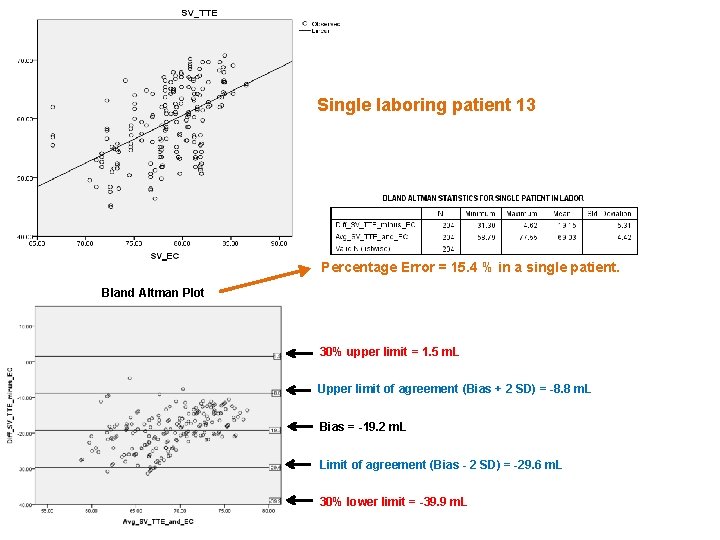
Single laboring patient 13 Percentage Error = 15. 4 % in a single patient. Bland Altman Plot 30% upper limit = 1. 5 m. L Upper limit of agreement (Bias + 2 SD) = -8. 8 m. L Bias = -19. 2 m. L Limit of agreement (Bias - 2 SD) = -29. 6 m. L 30% lower limit = -39. 9 m. L
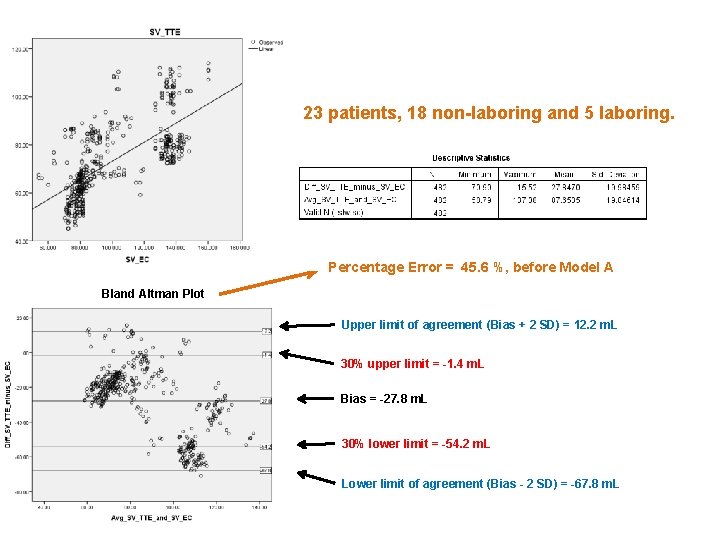
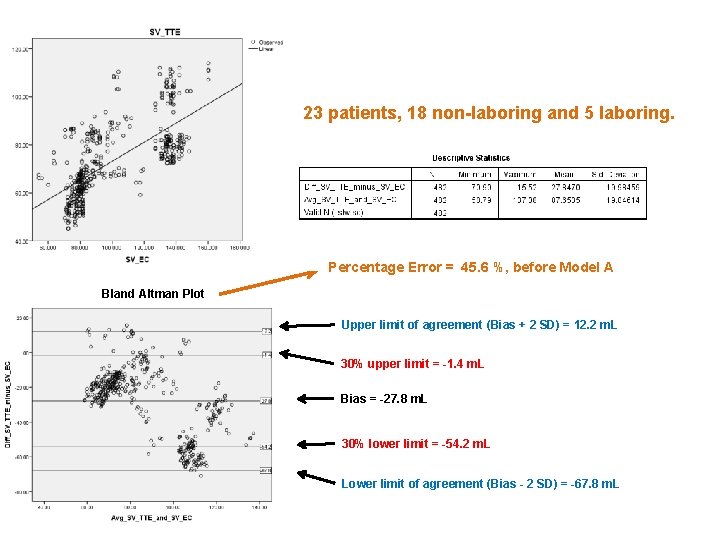
23 patients, 18 non-laboring and 5 laboring. Percentage Error = 45. 6 %, before Model A Bland Altman Plot Upper limit of agreement (Bias + 2 SD) = 12. 2 m. L 30% upper limit = -1. 4 m. L Bias = -27. 8 m. L 30% lower limit = -54. 2 m. L Lower limit of agreement (Bias - 2 SD) = -67. 8 m. L
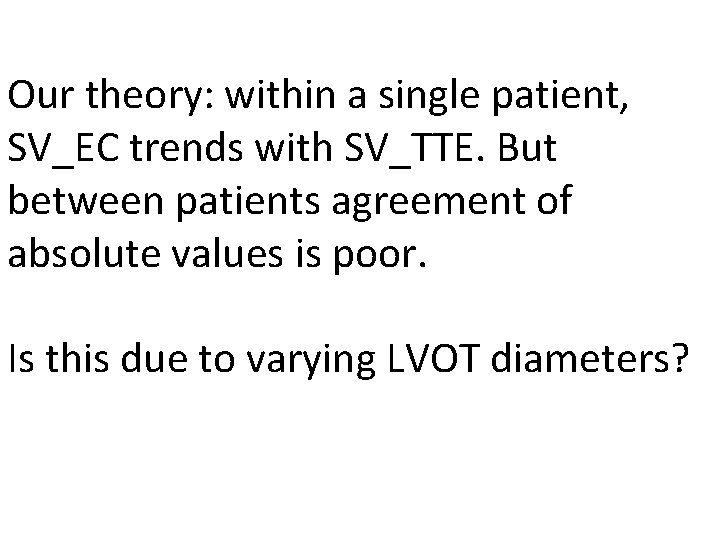
Our theory: within a single patient, SV_EC trends with SV_TTE. But between patients agreement of absolute values is poor. Is this due to varying LVOT diameters?
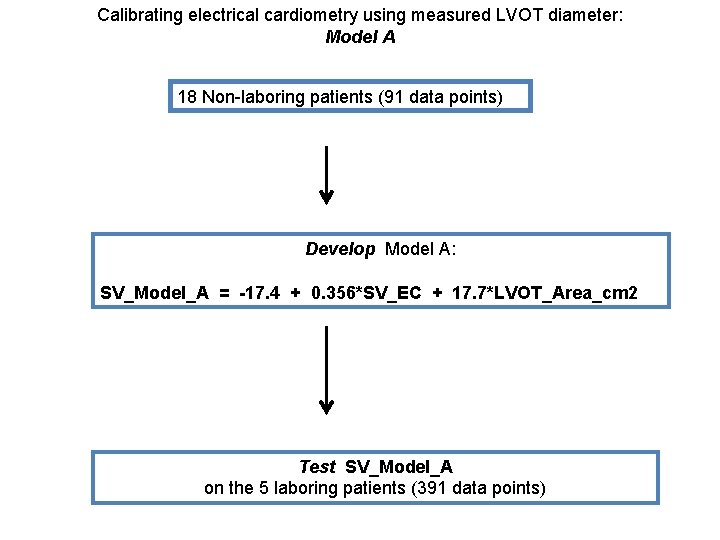
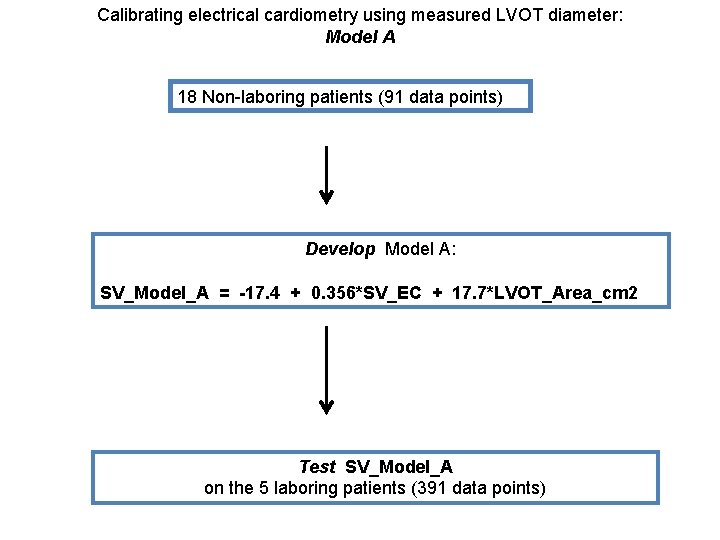
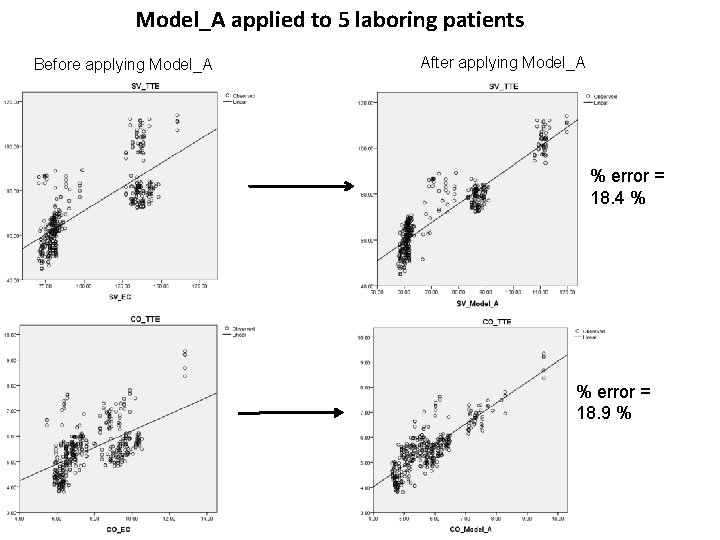
Calibrating electrical cardiometry using measured LVOT diameter: Model A 18 Non-laboring patients (91 data points) Develop Model A: SV_Model_A = -17. 4 + 0. 356*SV_EC + 17. 7*LVOT_Area_cm 2 Test SV_Model_A on the 5 laboring patients (391 data points)
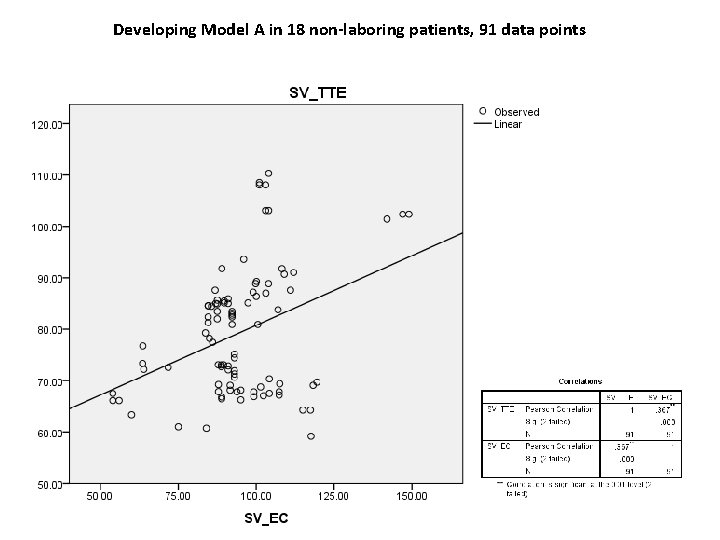
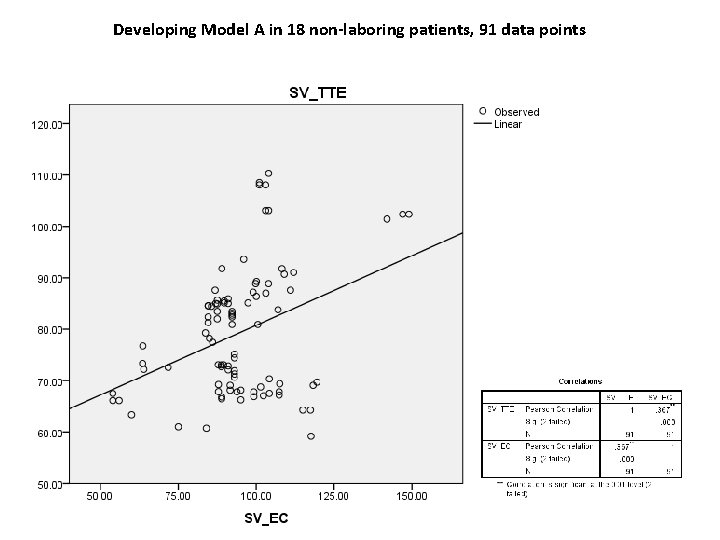
Developing Model A in 18 non-laboring patients, 91 data points
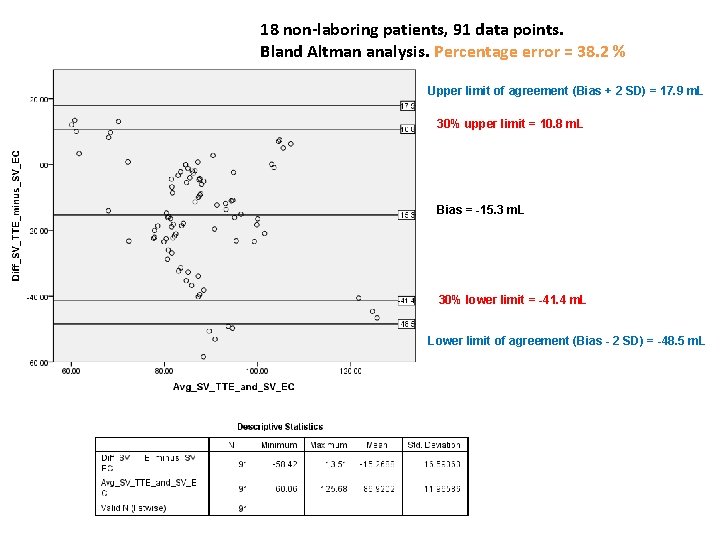
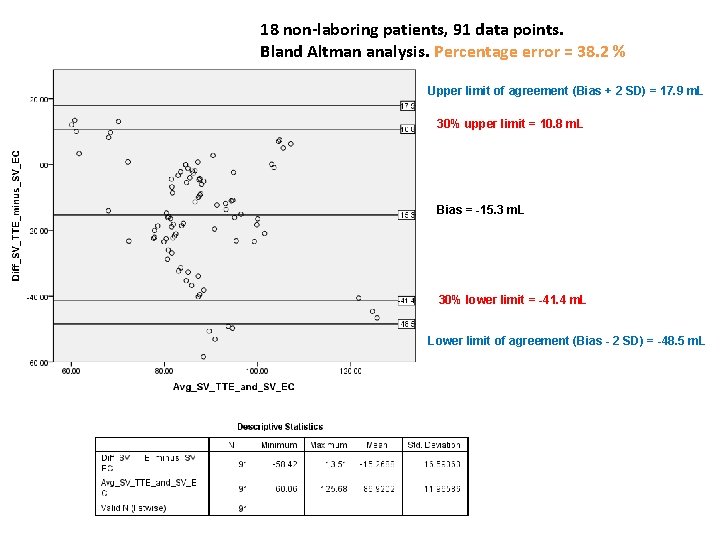
18 non-laboring patients, 91 data points. Bland Altman analysis. Percentage error = 38. 2 % Upper limit of agreement (Bias + 2 SD) = 17. 9 m. L 30% upper limit = 10. 8 m. L Bias = -15. 3 m. L 30% lower limit = -41. 4 m. L Lower limit of agreement (Bias - 2 SD) = -48. 5 m. L
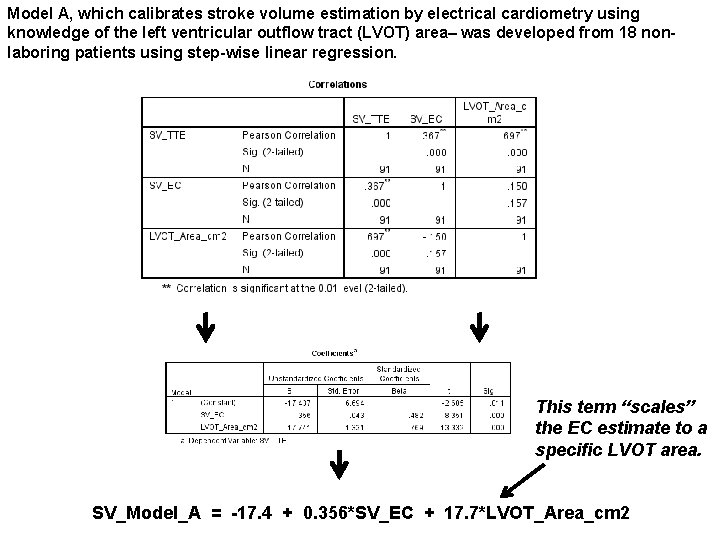
Model A, which calibrates stroke volume estimation by electrical cardiometry using knowledge of the left ventricular outflow tract (LVOT) area– was developed from 18 nonlaboring patients using step-wise linear regression. This term “scales” the EC estimate to a specific LVOT area. SV_Model_A = -17. 4 + 0. 356*SV_EC + 17. 7*LVOT_Area_cm 2
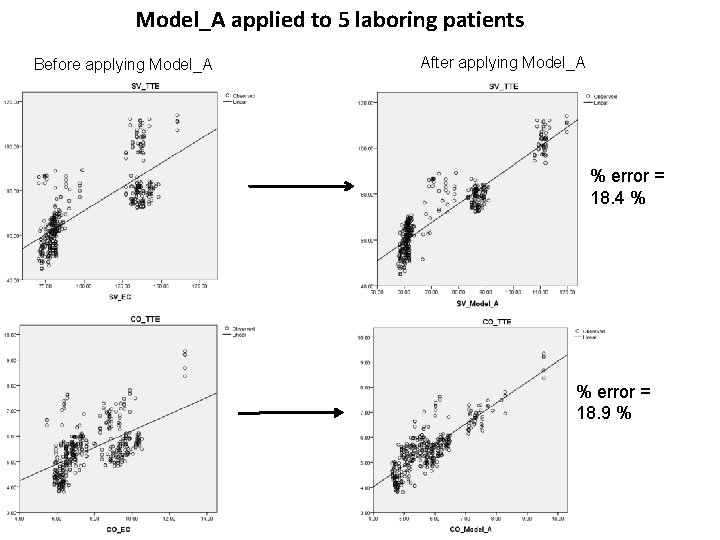
Model_A applied to 5 laboring patients Before applying Model_A After applying Model_A % error = 18. 4 % % error = 18. 9 %
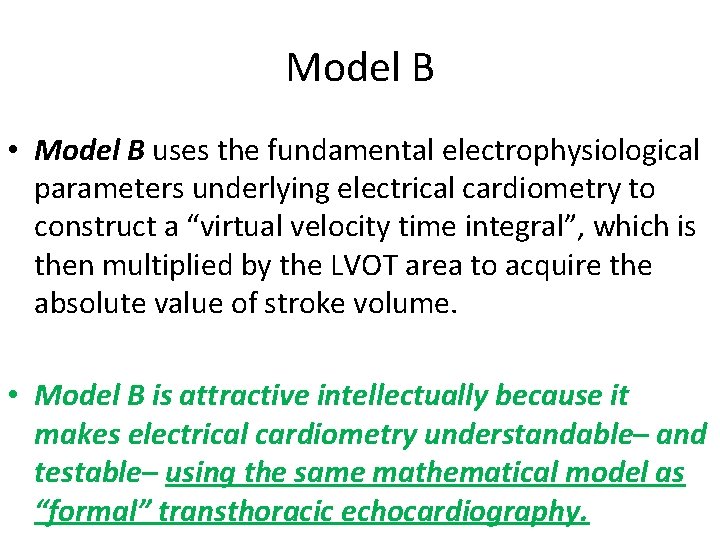
Model B • Model B uses the fundamental electrophysiological parameters underlying electrical cardiometry to construct a “virtual velocity time integral”, which is then multiplied by the LVOT area to acquire the absolute value of stroke volume. • Model B is attractive intellectually because it makes electrical cardiometry understandable– and testable– using the same mathematical model as “formal” transthoracic echocardiography.
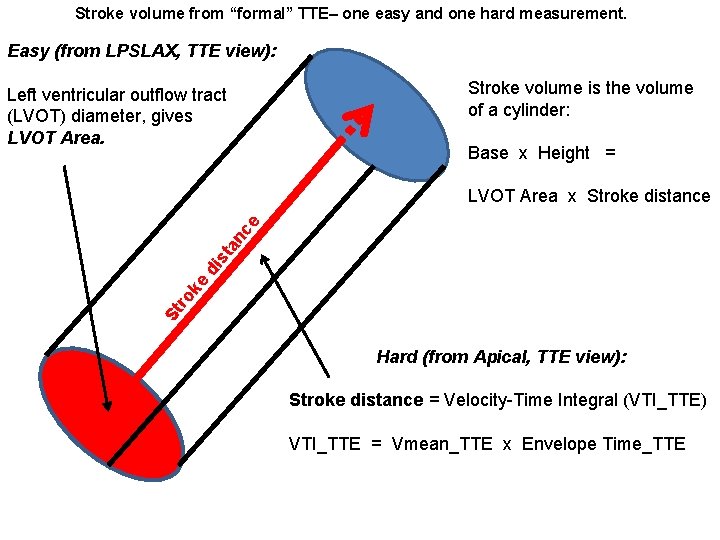
Stroke volume from “formal” TTE– one easy and one hard measurement. Easy (from LPSLAX, TTE view): Stroke volume is the volume of a cylinder: Left ventricular outflow tract (LVOT) diameter, gives LVOT Area. Base x Height = St ro ke di st a nc e LVOT Area x Stroke distance Hard (from Apical, TTE view): Stroke distance = Velocity-Time Integral (VTI_TTE) VTI_TTE = Vmean_TTE x Envelope Time_TTE
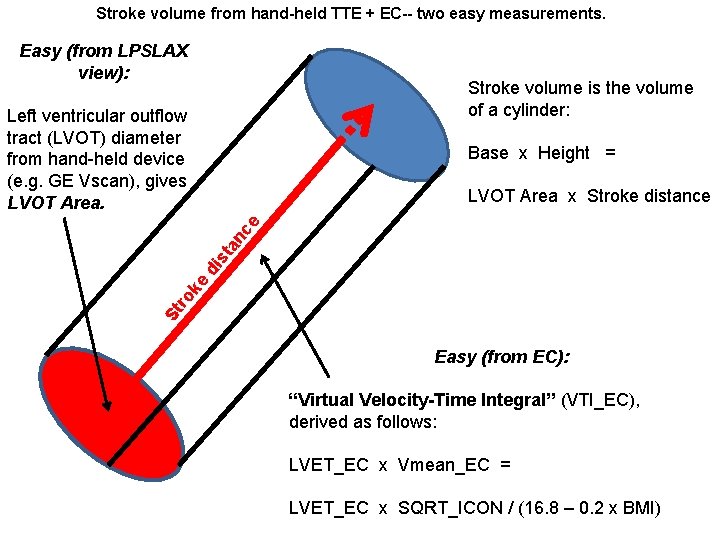
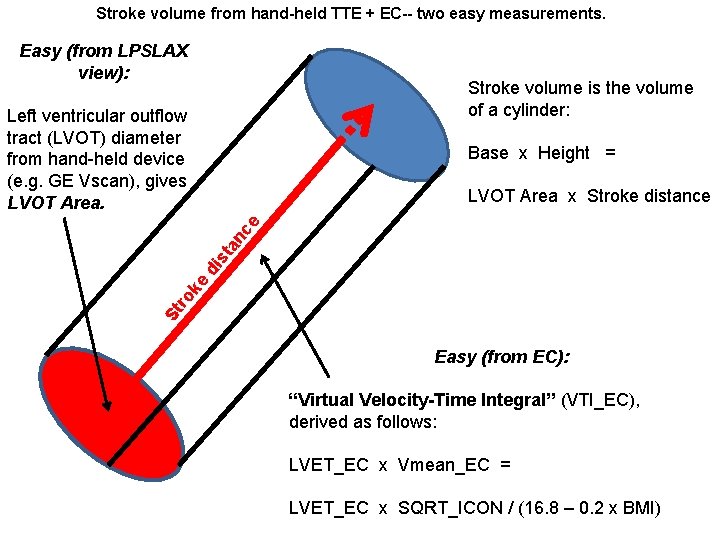
Stroke volume from hand-held TTE + EC-- two easy measurements. Easy (from LPSLAX view): Stroke volume is the volume of a cylinder: Left ventricular outflow tract (LVOT) diameter from hand-held device (e. g. GE Vscan), gives LVOT Area. Base x Height = St ro ke di st a nc e LVOT Area x Stroke distance Easy (from EC): “Virtual Velocity-Time Integral” (VTI_EC), derived as follows: LVET_EC x Vmean_EC = LVET_EC x SQRT_ICON / (16. 8 – 0. 2 x BMI)
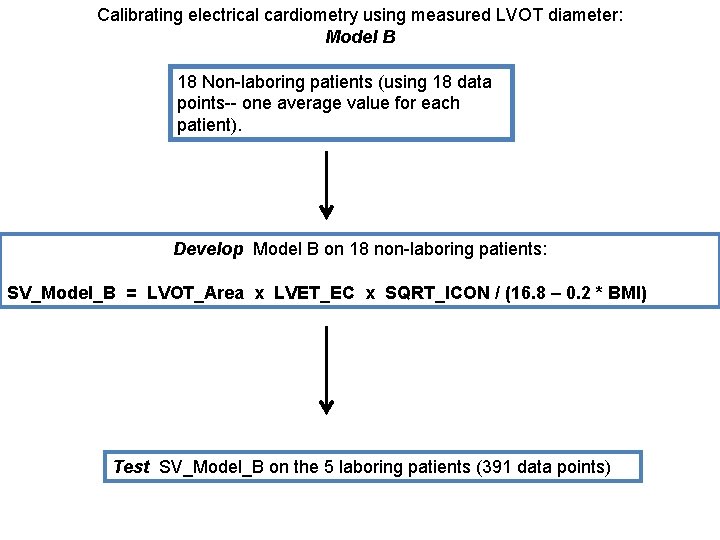
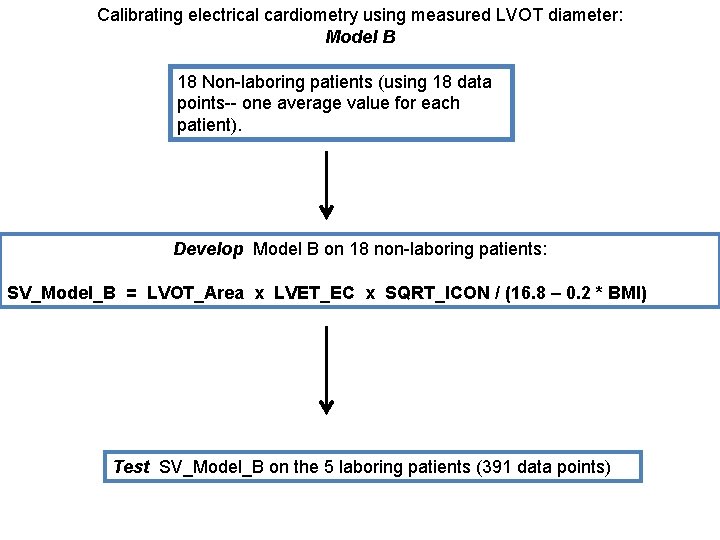
Calibrating electrical cardiometry using measured LVOT diameter: Model B 18 Non-laboring patients (using 18 data points-- one average value for each patient). Develop Model B on 18 non-laboring patients: SV_Model_B = LVOT_Area x LVET_EC x SQRT_ICON / (16. 8 – 0. 2 * BMI) Test SV_Model_B on the 5 laboring patients (391 data points)
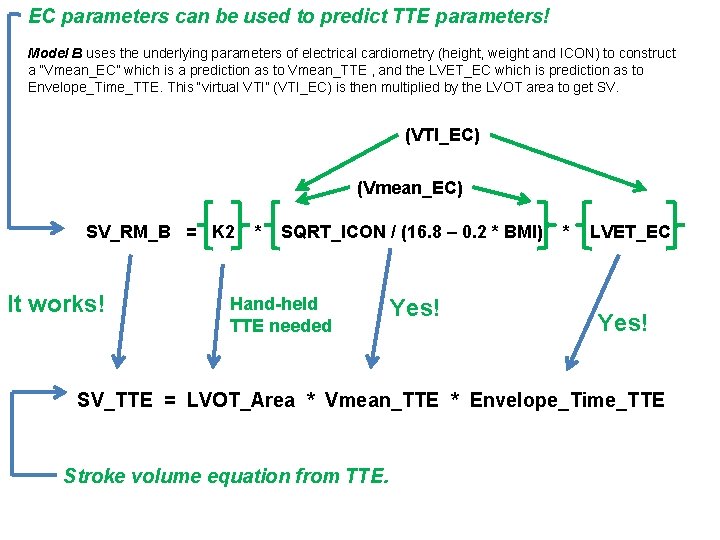
EC parameters can be used to predict TTE parameters! Model B uses the underlying parameters of electrical cardiometry (height, weight and ICON) to construct a “Vmean_EC” which is a prediction as to Vmean_TTE , and the LVET_EC which is prediction as to Envelope_Time_TTE. This “virtual VTI” (VTI_EC) is then multiplied by the LVOT area to get SV. (VTI_EC) (Vmean_EC) SV_RM_B = K 2 It works! * SQRT_ICON / (16. 8 – 0. 2 * BMI) Hand-held TTE needed Yes! * LVET_EC Yes! SV_TTE = LVOT_Area * Vmean_TTE * Envelope_Time_TTE Stroke volume equation from TTE.
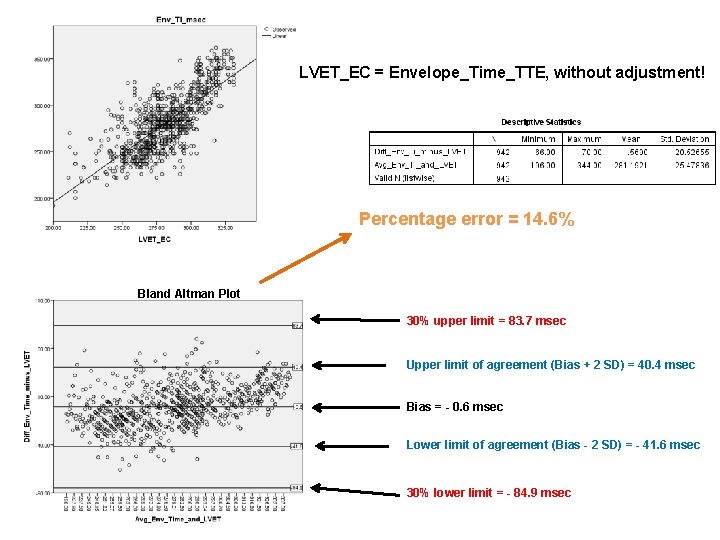
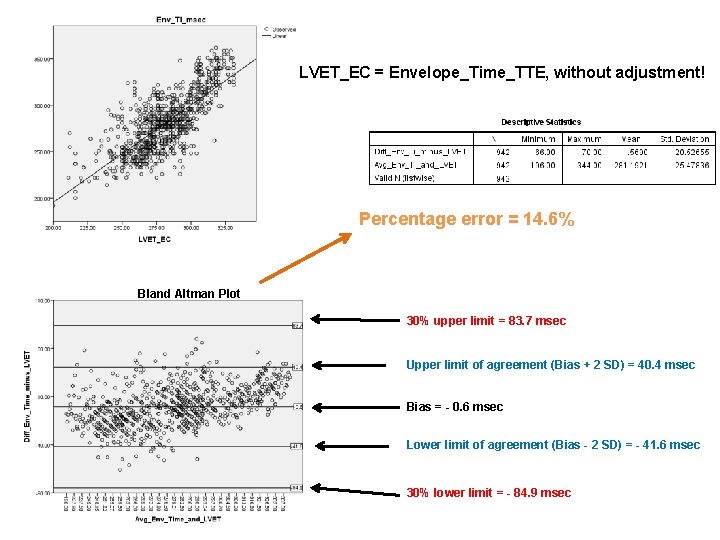
LVET_EC = Envelope_Time_TTE, without adjustment! Percentage error = 14. 6% Bland Altman Plot 30% upper limit = 83. 7 msec Upper limit of agreement (Bias + 2 SD) = 40. 4 msec Bias = - 0. 6 msec Lower limit of agreement (Bias - 2 SD) = - 41. 6 msec 30% lower limit = - 84. 9 msec
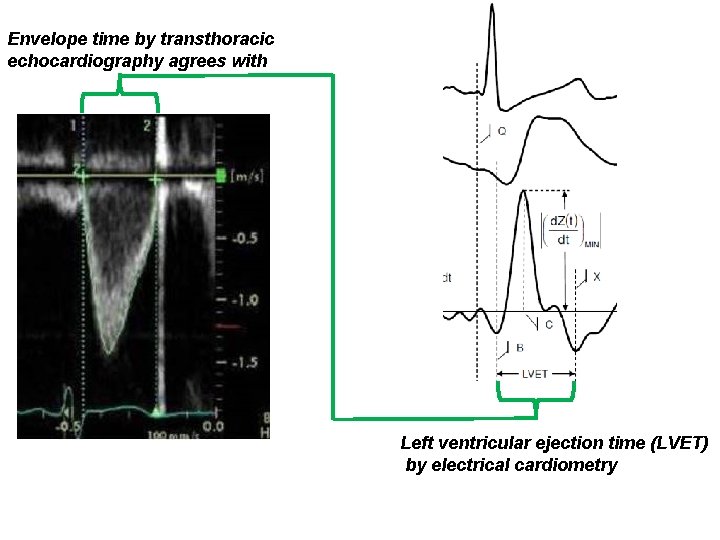
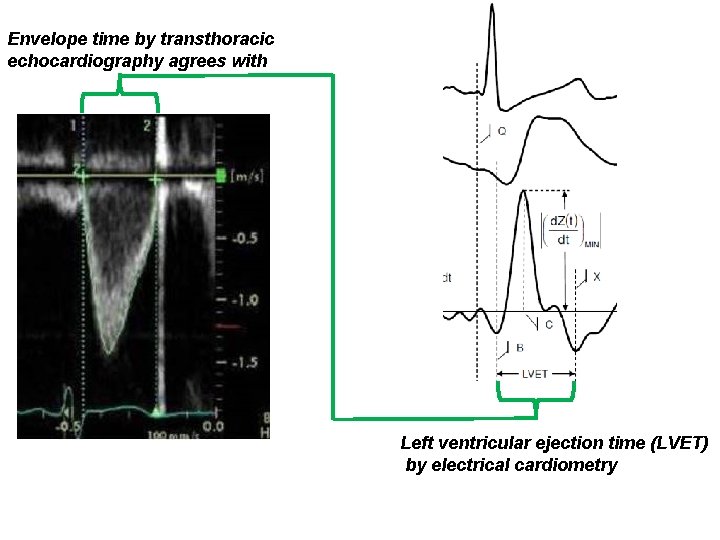
Envelope time by transthoracic echocardiography agrees with Left ventricular ejection time (LVET) by electrical cardiometry
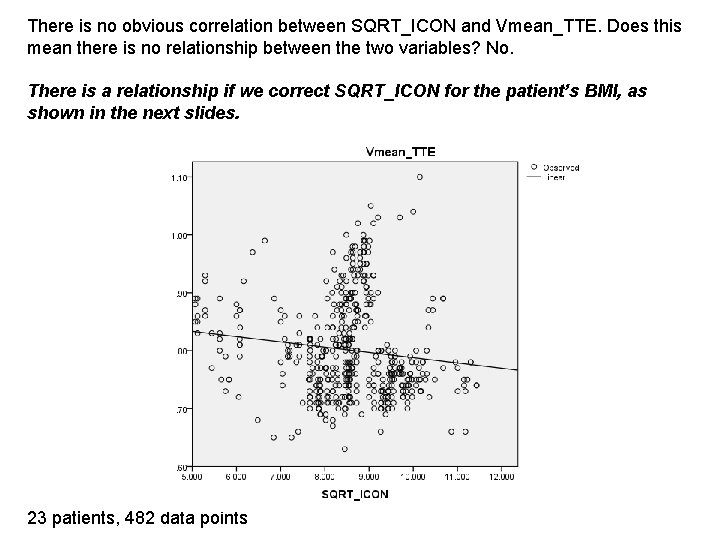
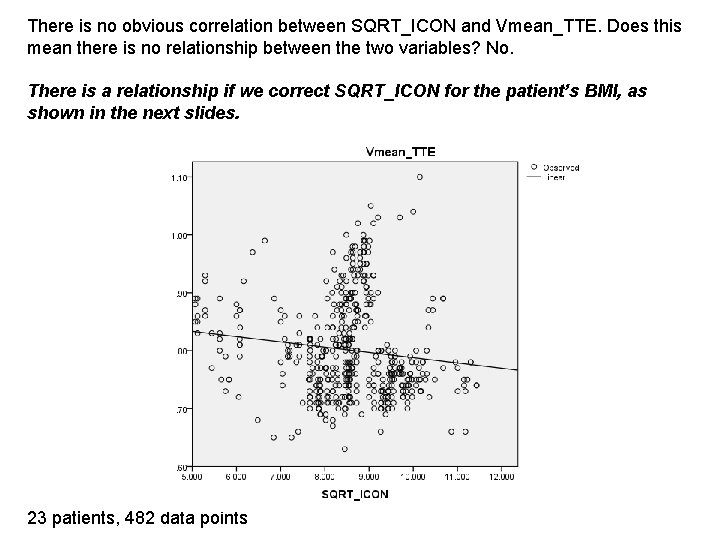
There is no obvious correlation between SQRT_ICON and Vmean_TTE. Does this mean there is no relationship between the two variables? No. There is a relationship if we correct SQRT_ICON for the patient’s BMI, as shown in the next slides. 23 patients, 482 data points
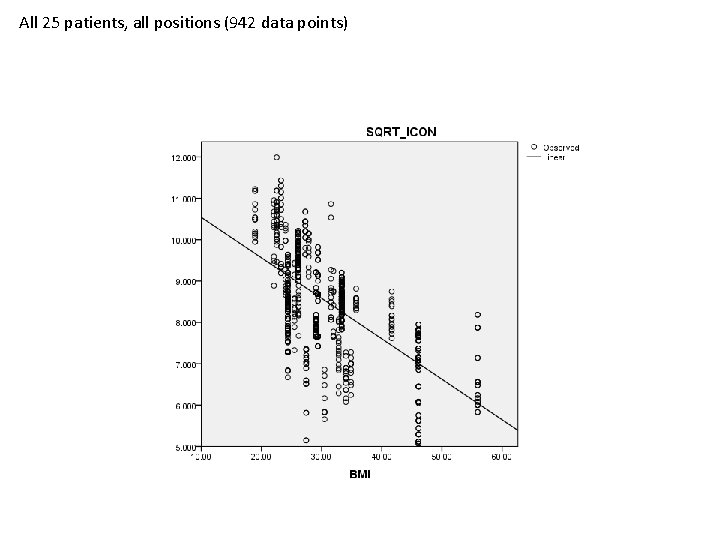
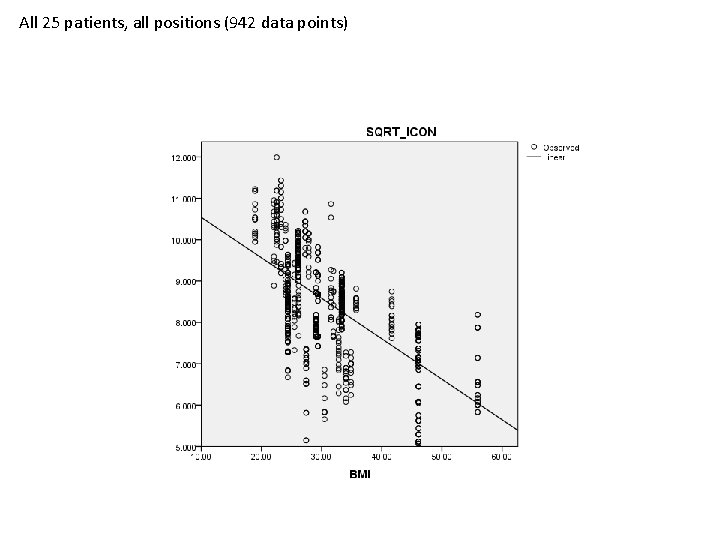
All 25 patients, all positions (942 data points)
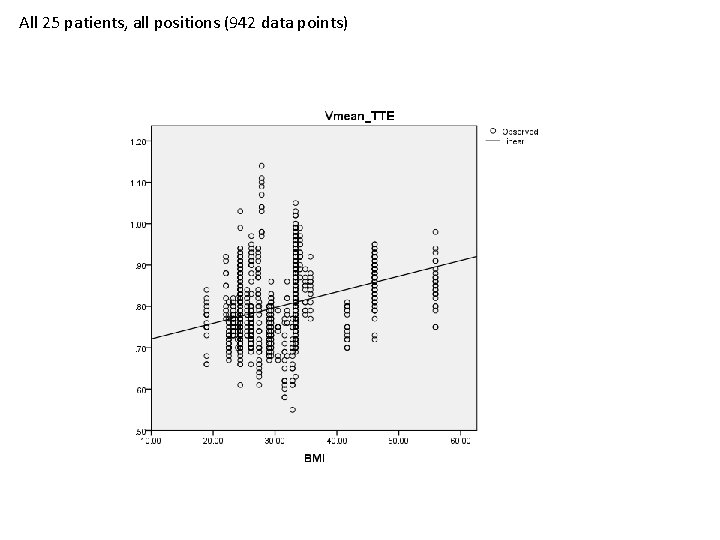
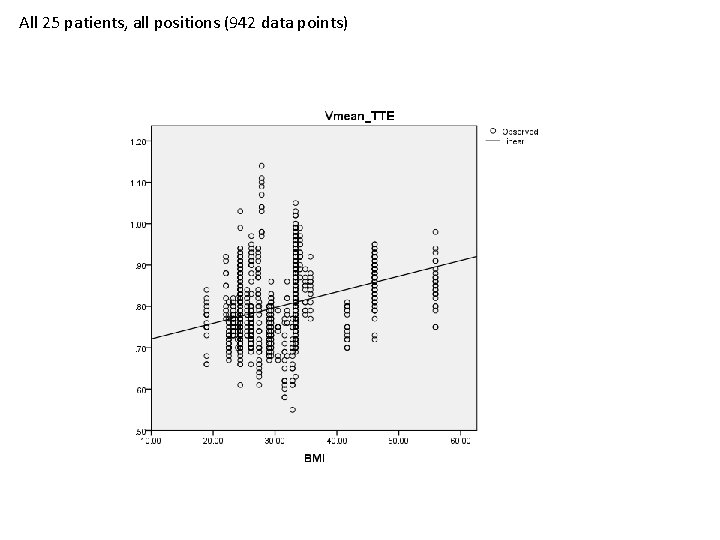
All 25 patients, all positions (942 data points)
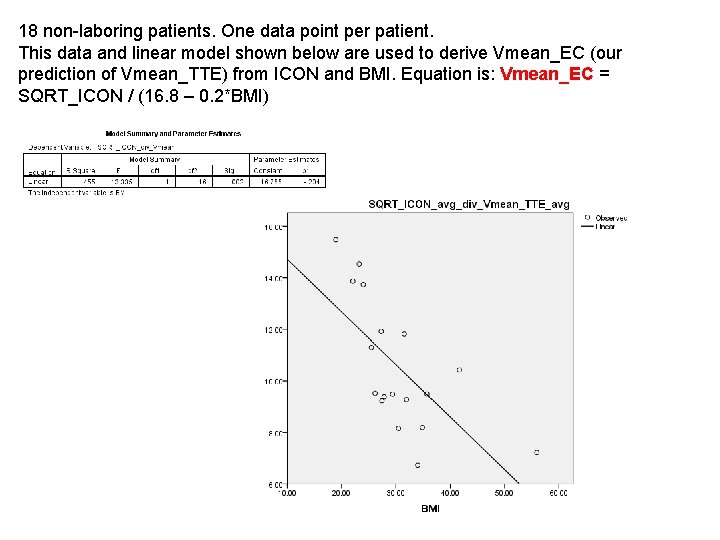
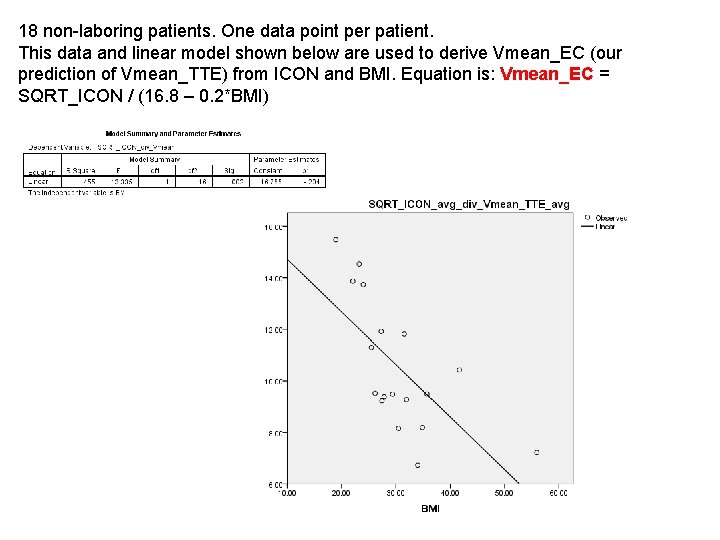
18 non-laboring patients. One data point per patient. This data and linear model shown below are used to derive Vmean_EC (our prediction of Vmean_TTE) from ICON and BMI. Equation is: Vmean_EC = SQRT_ICON / (16. 8 – 0. 2*BMI)
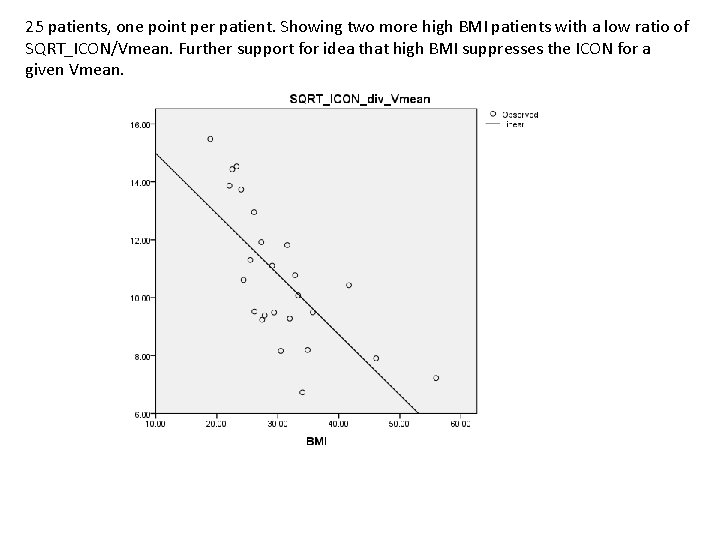
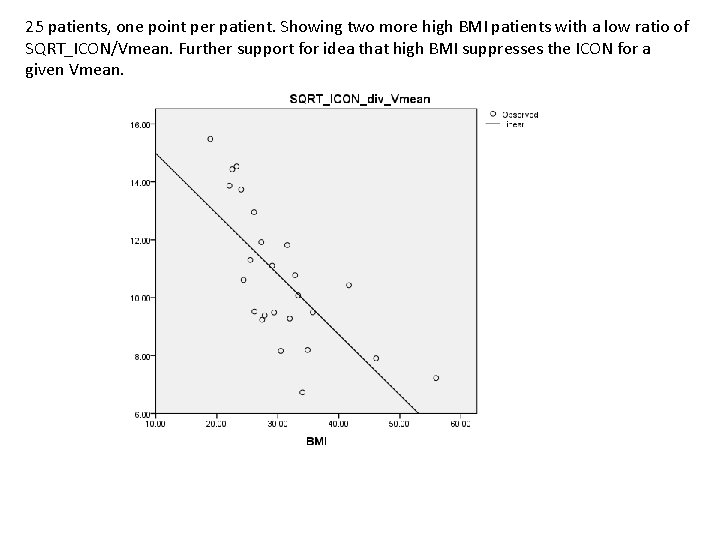
25 patients, one point per patient. Showing two more high BMI patients with a low ratio of SQRT_ICON/Vmean. Further support for idea that high BMI suppresses the ICON for a given Vmean.
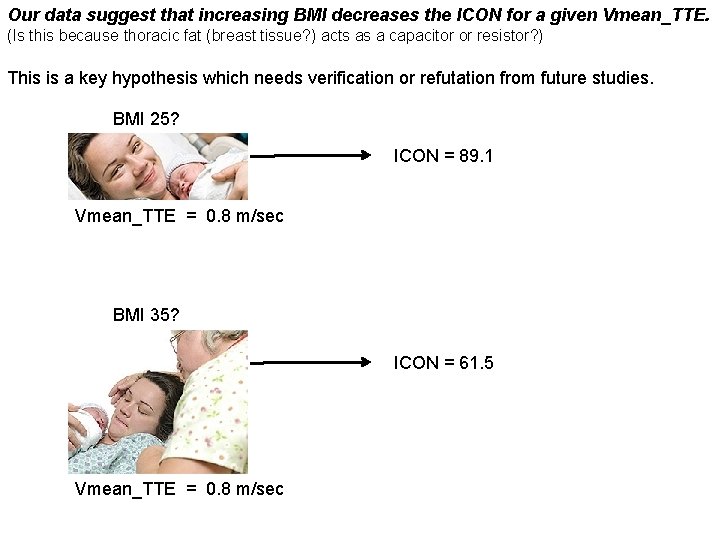
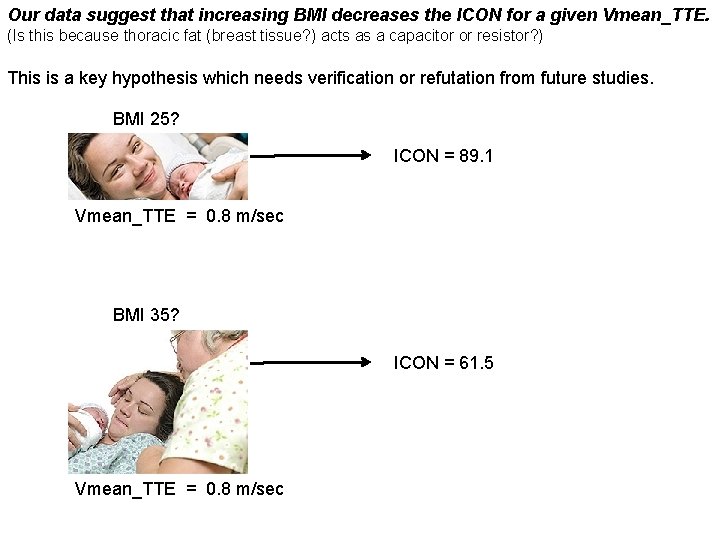
Our data suggest that increasing BMI decreases the ICON for a given Vmean_TTE. (Is this because thoracic fat (breast tissue? ) acts as a capacitor or resistor? ) This is a key hypothesis which needs verification or refutation from future studies. BMI 25? ICON = 89. 1 Vmean_TTE = 0. 8 m/sec BMI 35? ICON = 61. 5 Vmean_TTE = 0. 8 m/sec
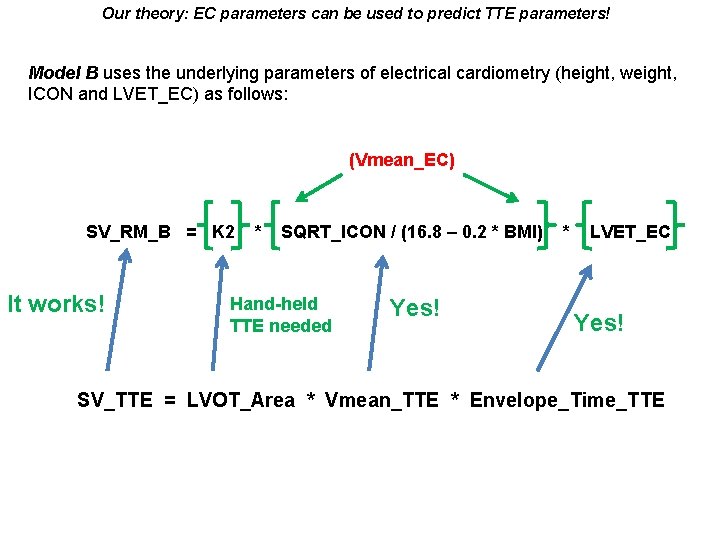
Our theory: EC parameters can be used to predict TTE parameters! Model B uses the underlying parameters of electrical cardiometry (height, weight, ICON and LVET_EC) as follows: (Vmean_EC) SV_RM_B = K 2 It works! * SQRT_ICON / (16. 8 – 0. 2 * BMI) Hand-held TTE needed Yes! * LVET_EC Yes! SV_TTE = LVOT_Area * Vmean_TTE * Envelope_Time_TTE
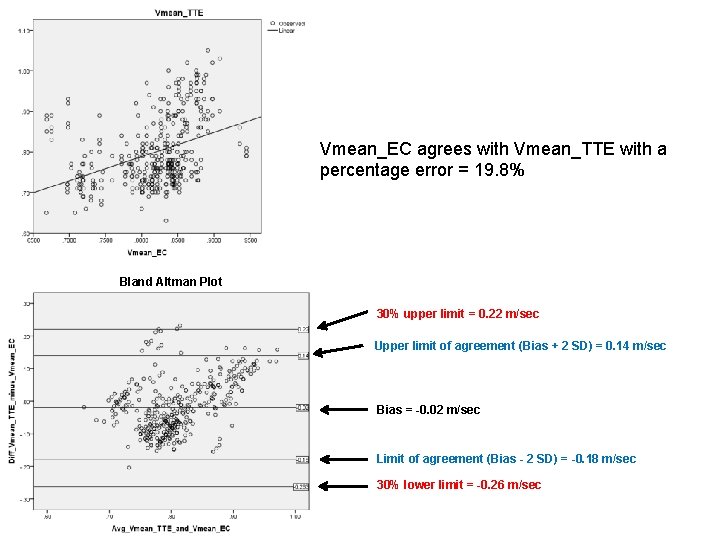
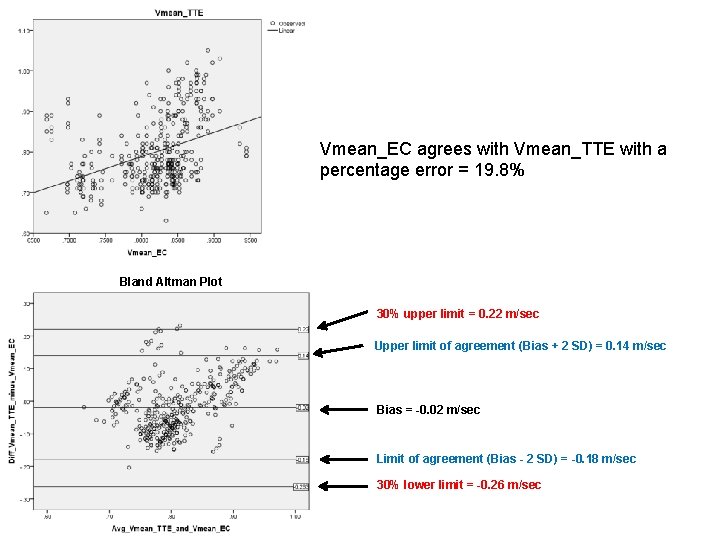
Vmean_EC agrees with Vmean_TTE with a percentage error = 19. 8% Bland Altman Plot 30% upper limit = 0. 22 m/sec Upper limit of agreement (Bias + 2 SD) = 0. 14 m/sec Bias = -0. 02 m/sec Limit of agreement (Bias - 2 SD) = -0. 18 m/sec 30% lower limit = -0. 26 m/sec
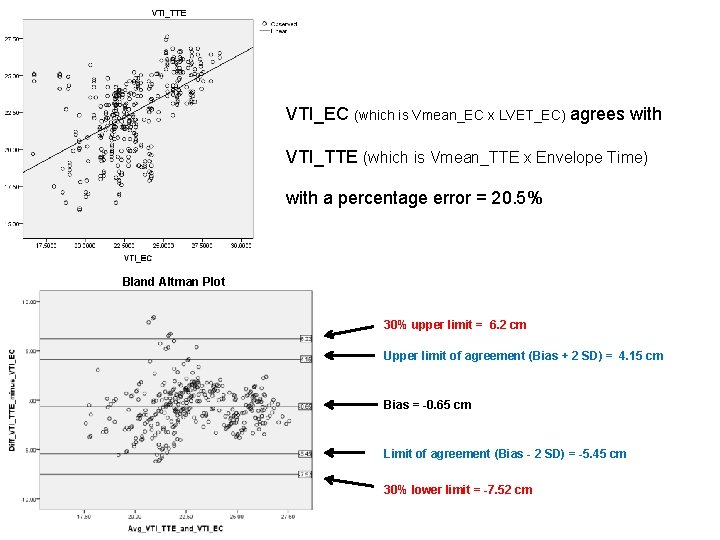
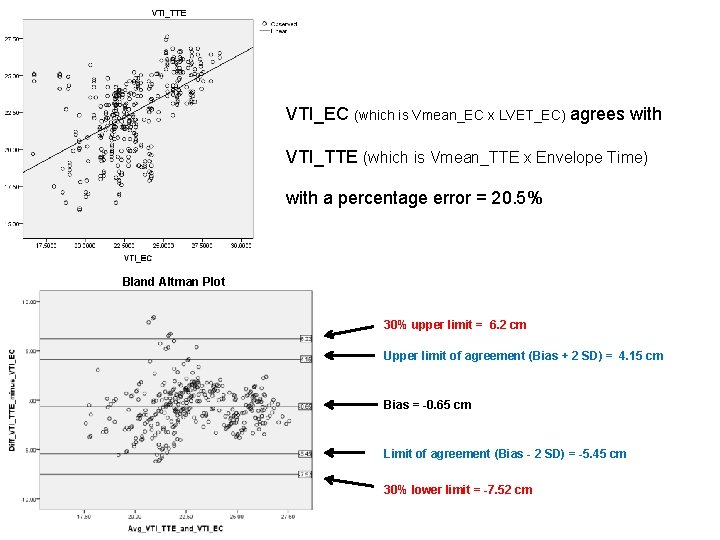
VTI_EC (which is Vmean_EC x LVET_EC) agrees with VTI_TTE (which is Vmean_TTE x Envelope Time) with a percentage error = 20. 5% Bland Altman Plot 30% upper limit = 6. 2 cm Upper limit of agreement (Bias + 2 SD) = 4. 15 cm Bias = -0. 65 cm Limit of agreement (Bias - 2 SD) = -5. 45 cm 30% lower limit = -7. 52 cm

Model_B applied to 5 laboring patients Before applying Model_B After applying Model_B % error = 20. 8 % error = 21. 4
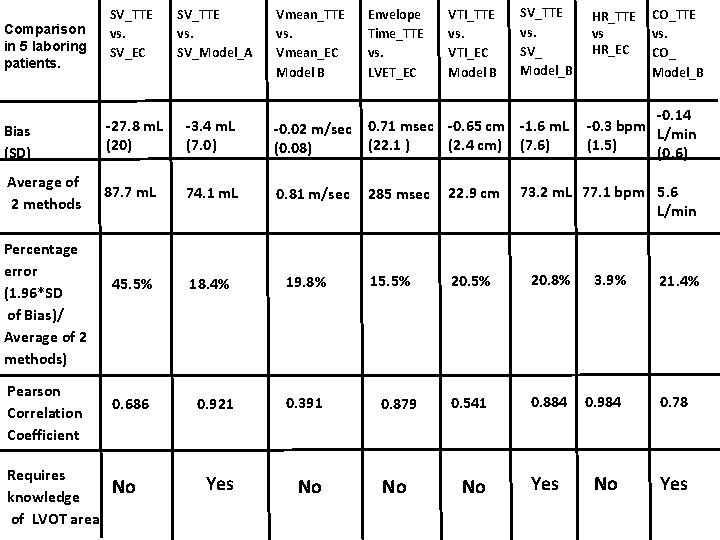
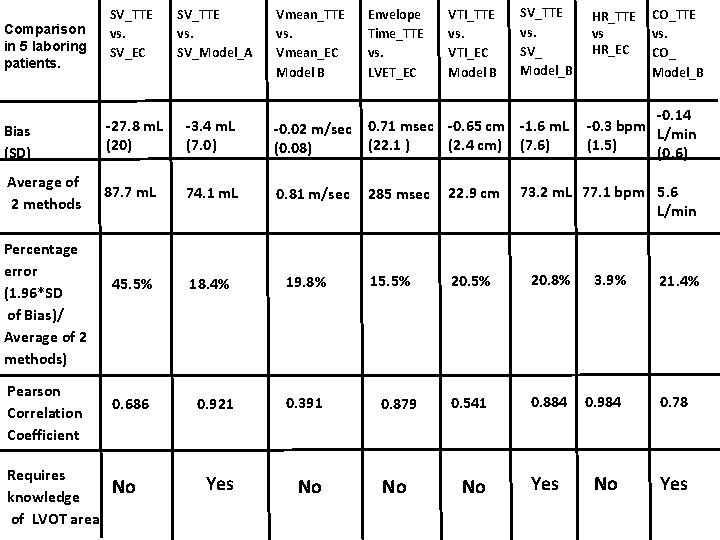
Comparison in 5 laboring patients. SV_TTE vs. SV_EC SV_TTE vs. SV_Model_A Vmean_TTE vs. Vmean_EC Model B Envelope Time_TTE vs. LVET_EC VTI_TTE vs. VTI_EC Model B SV_TTE vs. SV_ Model_B Bias (SD) -27. 8 m. L (20) -3. 4 m. L (7. 0) -0. 02 m/sec 0. 71 msec -0. 65 cm -1. 6 m. L (22. 1 ) (2. 4 cm) (7. 6) (0. 08) Average of 2 methods 87. 7 m. L 74. 1 m. L 0. 81 m/sec 45. 5% 18. 4% 19. 8% 0. 686 0. 921 0. 391 Yes No Percentage error (1. 96*SD of Bias)/ Average of 2 methods) Pearson Correlation Coefficient Requires knowledge of LVOT area No HR_TTE vs HR_EC CO_TTE vs. CO_ Model_B -0. 14 -0. 3 bpm L/min (1. 5) (0. 6) 73. 2 m. L 77. 1 bpm 5. 6 L/min 285 msec 22. 9 cm 15. 5% 20. 8% 0. 879 0. 541 0. 884 0. 984 0. 78 No No Yes 3. 9% 21. 4%
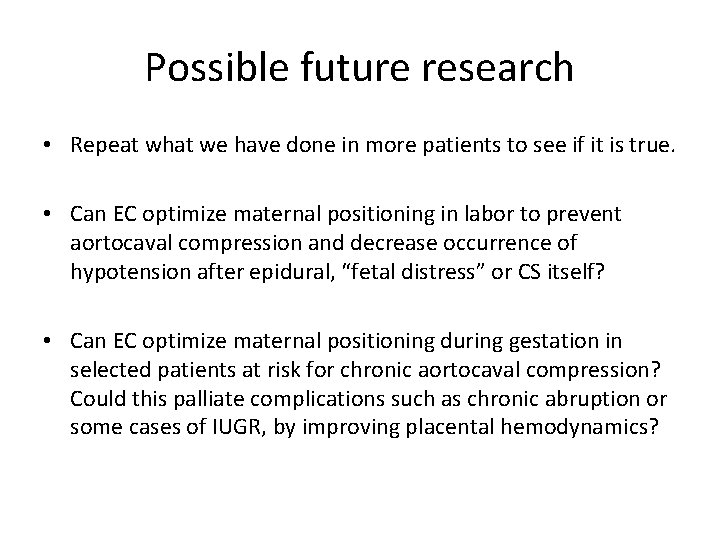
Possible future research • Repeat what we have done in more patients to see if it is true. • Can EC optimize maternal positioning in labor to prevent aortocaval compression and decrease occurrence of hypotension after epidural, “fetal distress” or CS itself? • Can EC optimize maternal positioning during gestation in selected patients at risk for chronic aortocaval compression? Could this palliate complications such as chronic abruption or some cases of IUGR, by improving placental hemodynamics?
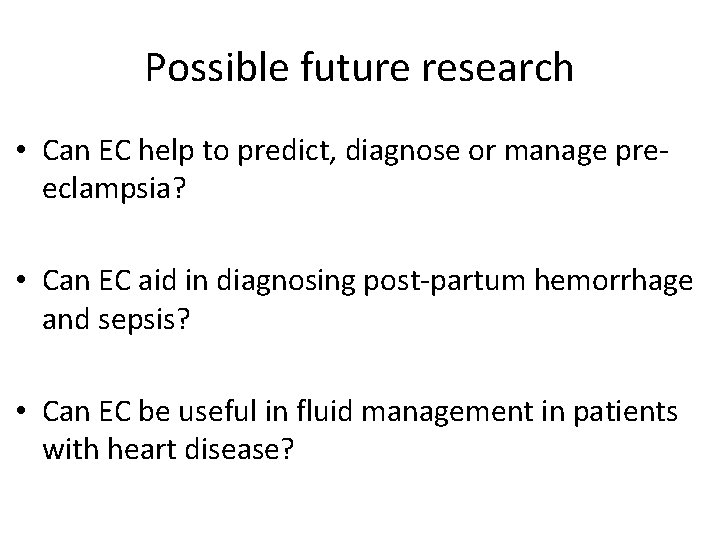
Possible future research • Can EC help to predict, diagnose or manage preeclampsia? • Can EC aid in diagnosing post-partum hemorrhage and sepsis? • Can EC be useful in fluid management in patients with heart disease?
Possible future research • Can EC help us to understand autotransfusion and other normal events of labor? • Can EC be useful in general Critical Care (outside of obstetrics)?
The End
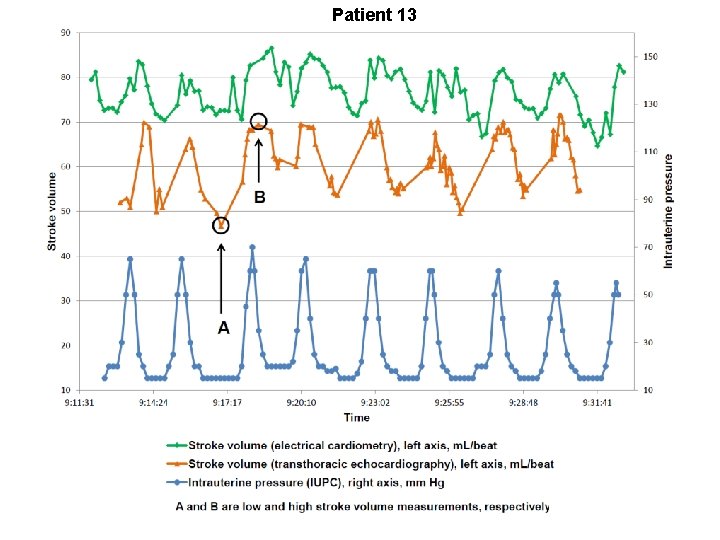
Patient 13 2
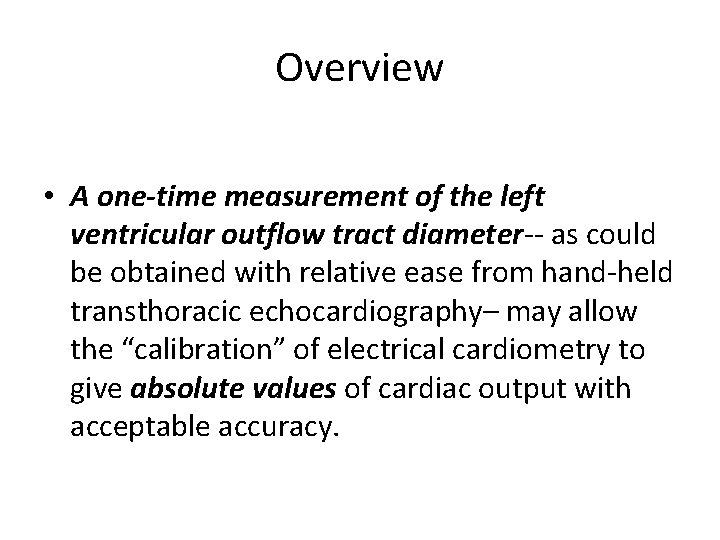
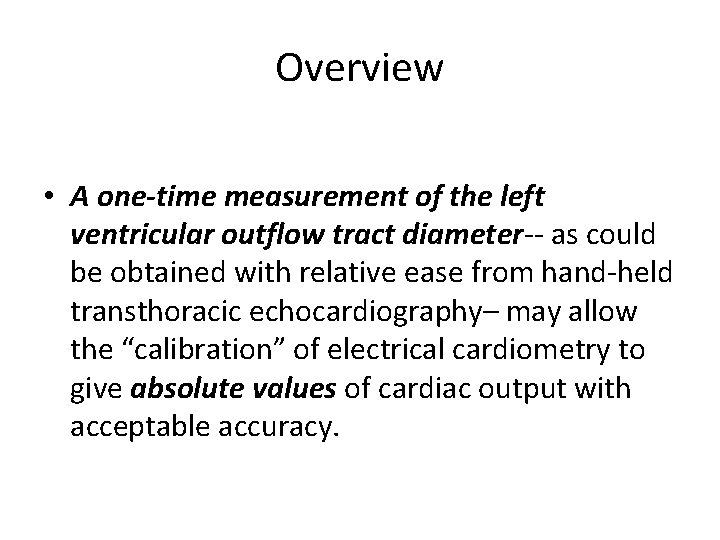
Overview • A one-time measurement of the left ventricular outflow tract diameter-- as could be obtained with relative ease from hand-held transthoracic echocardiography– may allow the “calibration” of electrical cardiometry to give absolute values of cardiac output with acceptable accuracy.
A question and a challenge: • If you could effortlessly, continuously and noninvasively measure cardiac output after a 5 minute, pain free set up time– would this be useful? • We believe we can do this. • I challenge you to prove us right or wrong.
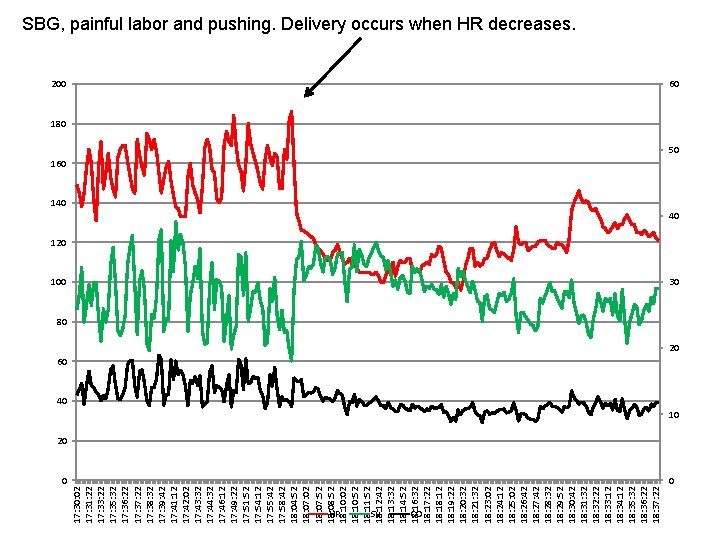
17: 30: 02 17: 31: 22 17: 33: 22 17: 35: 32 17: 36: 22 17: 37: 22 17: 38: 32 17: 39: 42 17: 41: 12 17: 42: 02 17: 43: 32 17: 44: 32 17: 46: 12 17: 49: 22 17: 51: 52 17: 54: 12 17: 55: 42 17: 58: 42 18: 04: 52 18: 07: 02 18: 07: 52 18: 08: 52 18: 10: 02 18: 10: 52 18: 11: 52 18: 12: 42 18: 13: 32 18: 14: 52 18: 16: 32 18: 17: 22 18: 12 18: 19: 22 18: 20: 32 18: 21: 32 18: 23: 02 18: 24: 12 18: 25: 02 18: 26: 42 18: 27: 42 18: 28: 32 18: 29: 52 18: 30: 42 18: 31: 32 18: 32: 22 18: 33: 12 18: 34: 12 18: 35: 32 18: 36: 22 18: 37: 22 SBG, painful labor and pushing. Delivery occurs when HR decreases. 200 60 180 160 50 140 40 120 100 30 80 20 60 40 10 20 0 0 HR SV CO