ELDERLY FRACTURES TUDOLAKO LECTURE IV POPULATION AGEING Indonesian
- Slides: 35
ELDERLY FRACTURES TUDOLAKO LECTURE IV
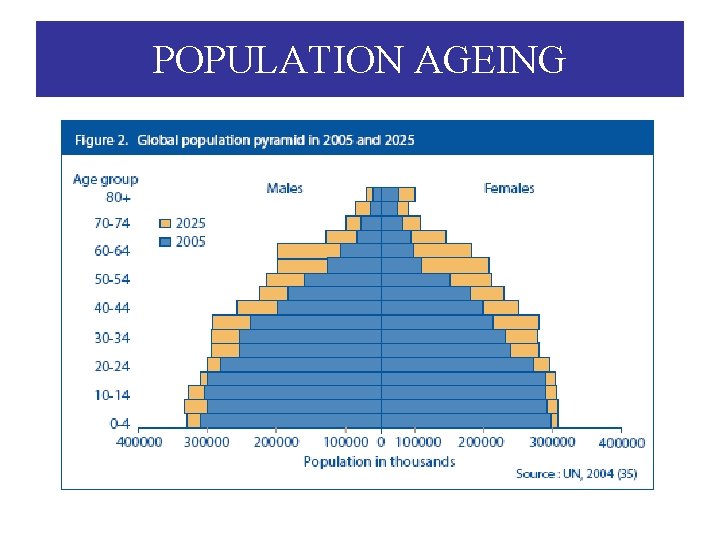
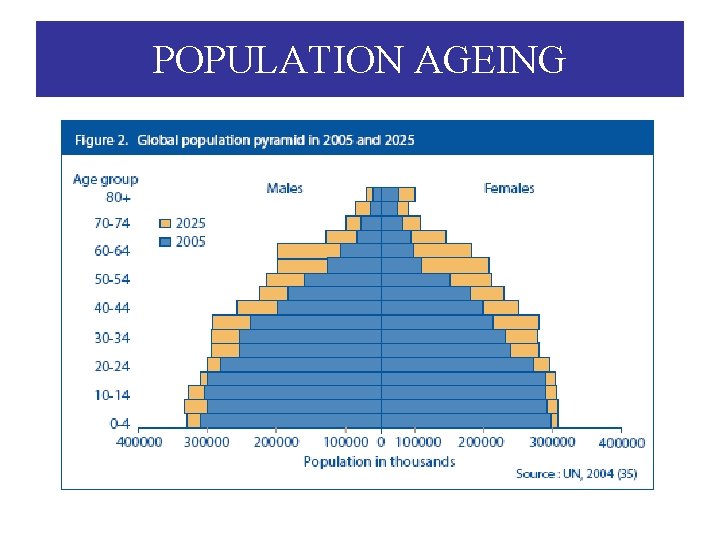
POPULATION AGEING
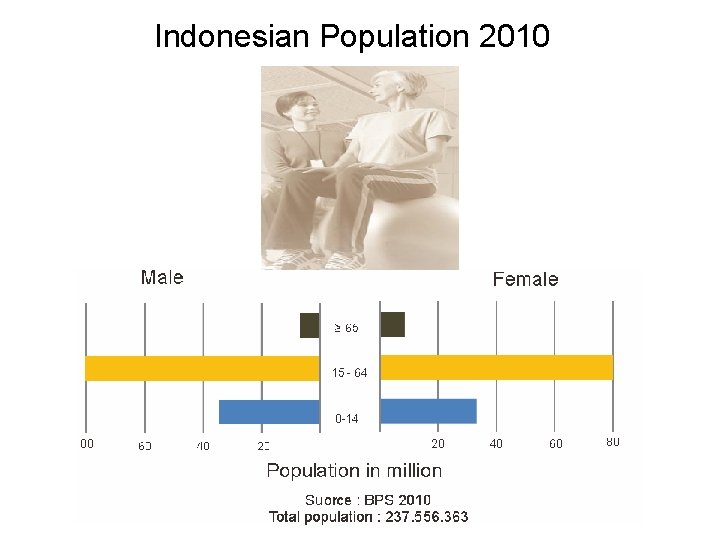
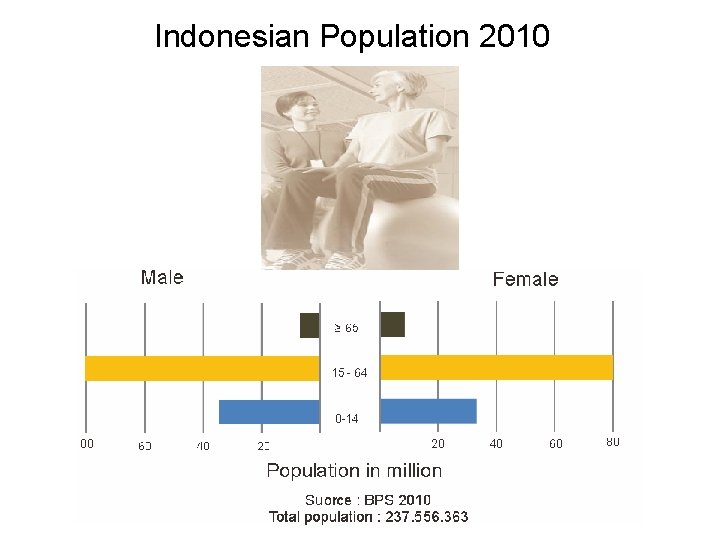
Indonesian Population 2010
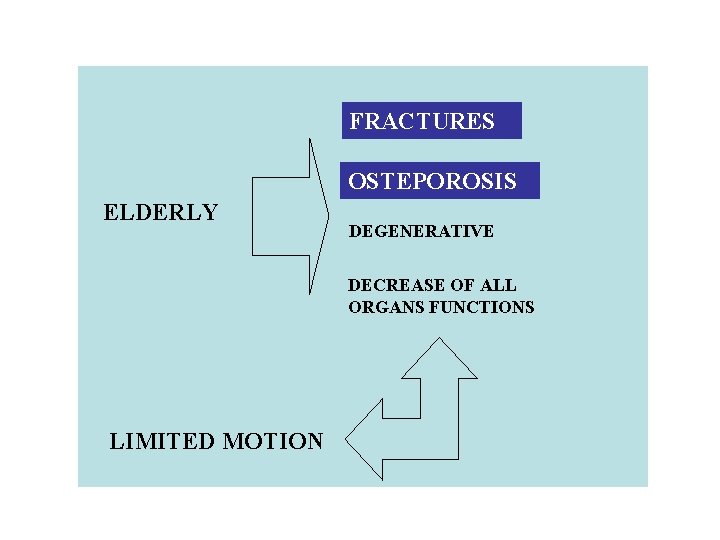
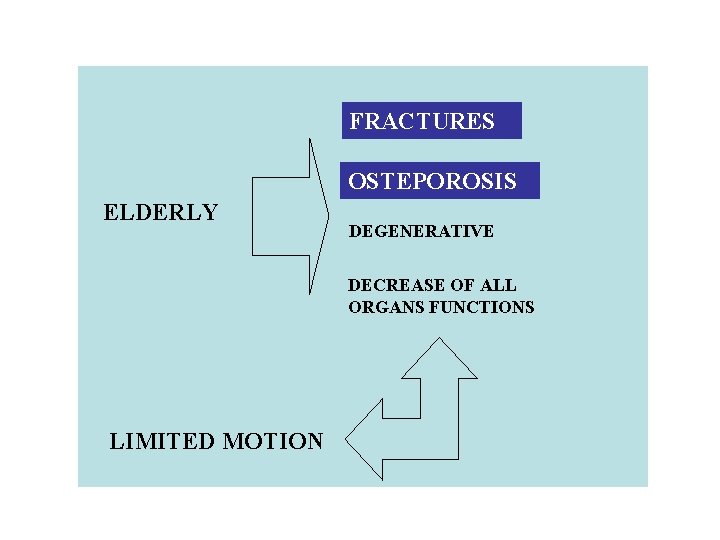
FRACTURES OSTEPOROSIS ELDERLY DEGENERATIVE DECREASE OF ALL ORGANS FUNCTIONS LIMITED MOTION
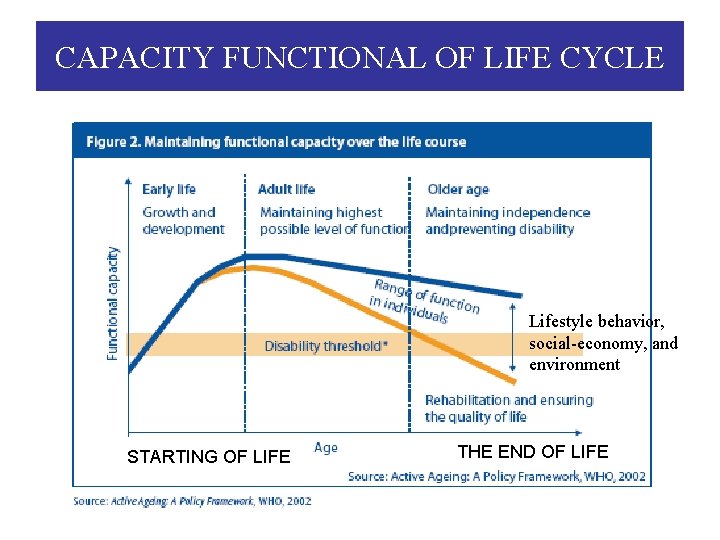
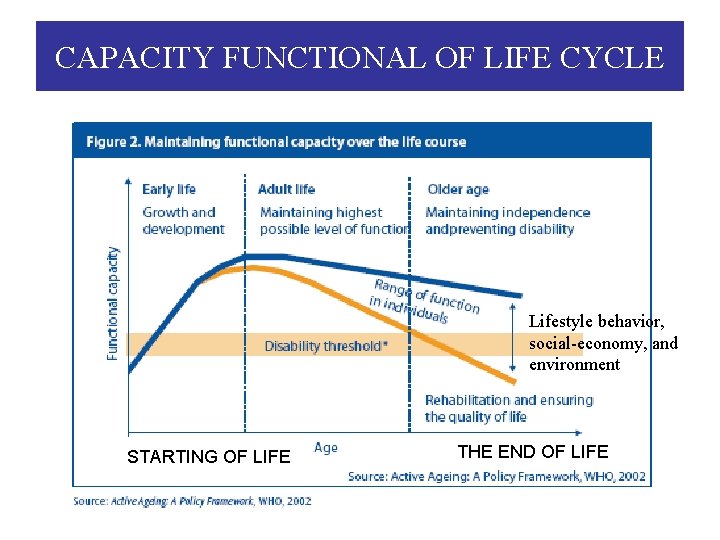
CAPACITY FUNCTIONAL OF LIFE CYCLE Lifestyle behavior, social-economy, and environment STARTING OF LIFE THE END OF LIFE
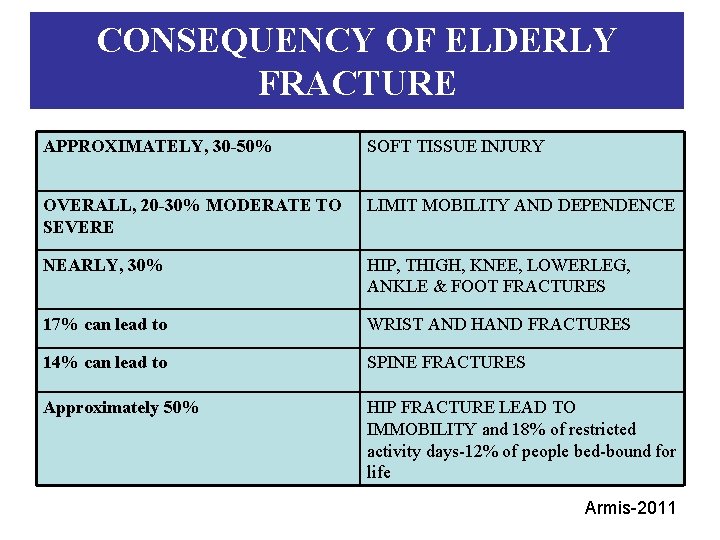
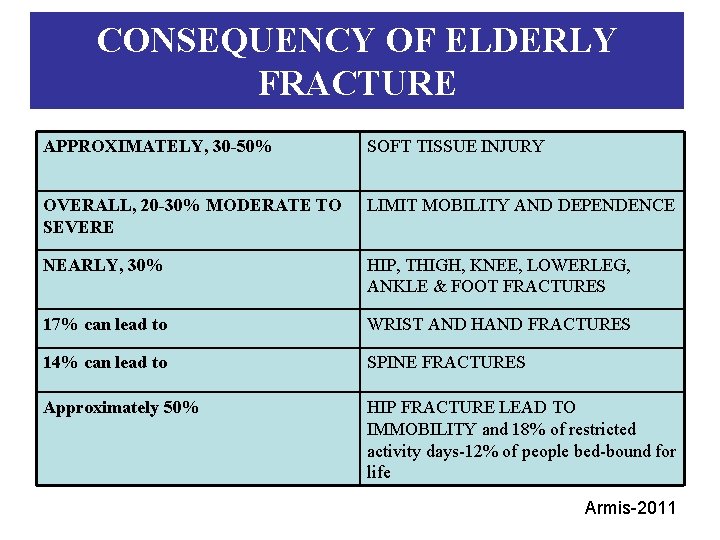
CONSEQUENCY OF ELDERLY FRACTURE APPROXIMATELY, 30 -50% SOFT TISSUE INJURY OVERALL, 20 -30% MODERATE TO SEVERE LIMIT MOBILITY AND DEPENDENCE NEARLY, 30% HIP, THIGH, KNEE, LOWERLEG, ANKLE & FOOT FRACTURES 17% can lead to WRIST AND HAND FRACTURES 14% can lead to SPINE FRACTURES Approximately 50% HIP FRACTURE LEAD TO IMMOBILITY and 18% of restricted activity days-12% of people bed-bound for life Armis-2011
GOAL OF THE STUDY HOW THE ELDERLY PEOPLE ACHIEVE TO STAY ACTIVE, INDEPENDENCE, AND SAFE IN HEALTHY LIFESTYLE? Armis-2011
OBJETIVES The medical student should able: 1. To build awareness of community and government that elderly people to stay active, independent, and safe is an important 2. To achieve how elderly people feel better, active, and independent for life in the community 3. To identify fall risk factors in healthy lifestyle of elderly people 4. To implement fall prevention in healthy lifestyle of elderly people Armis-2011
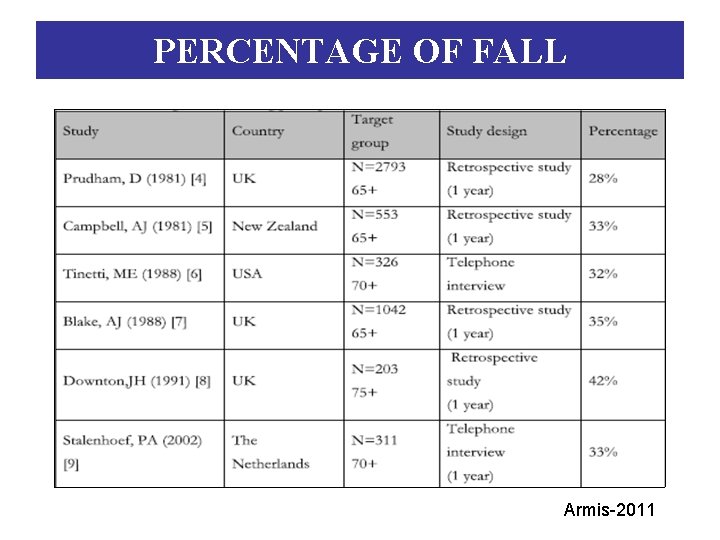
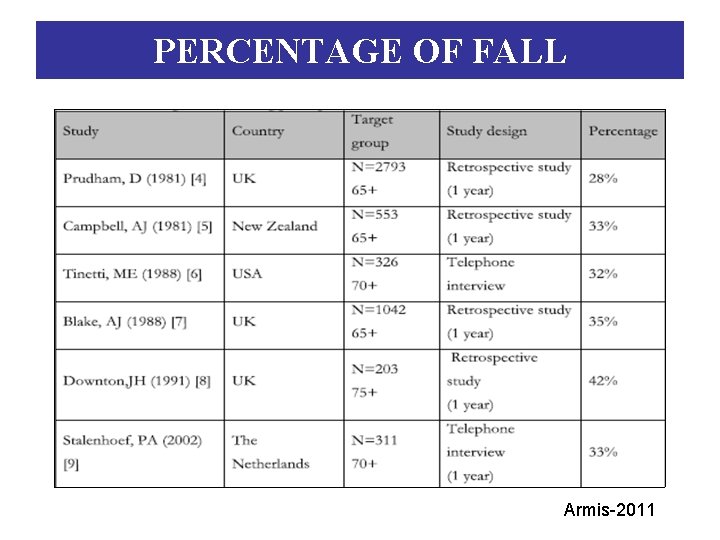
PERCENTAGE OF FALL Armis-2011
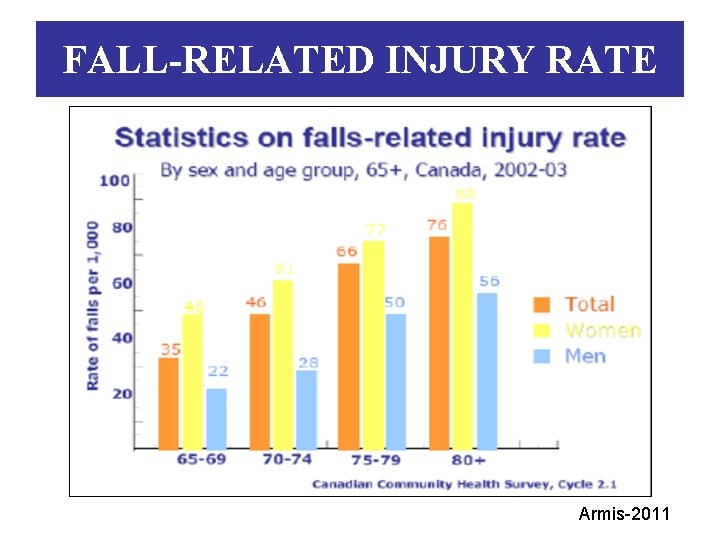
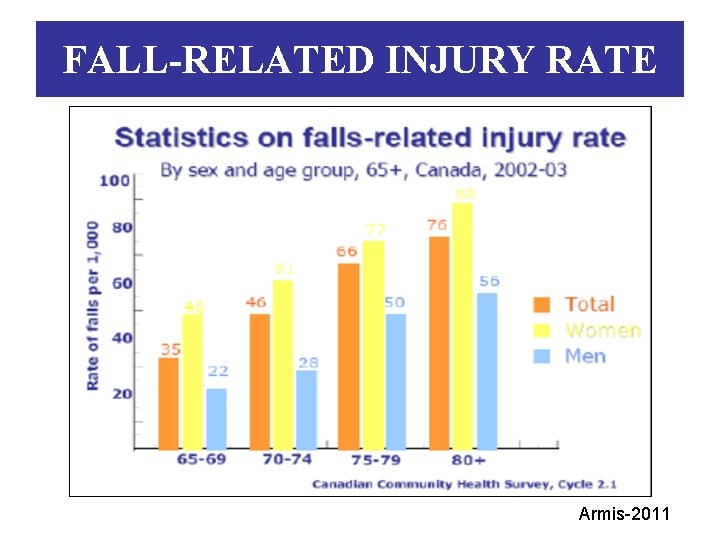
FALL-RELATED INJURY RATE Armis-2011
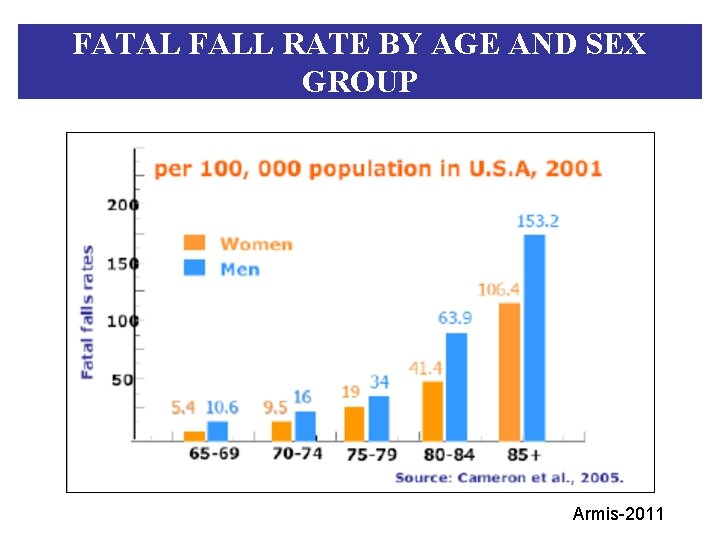
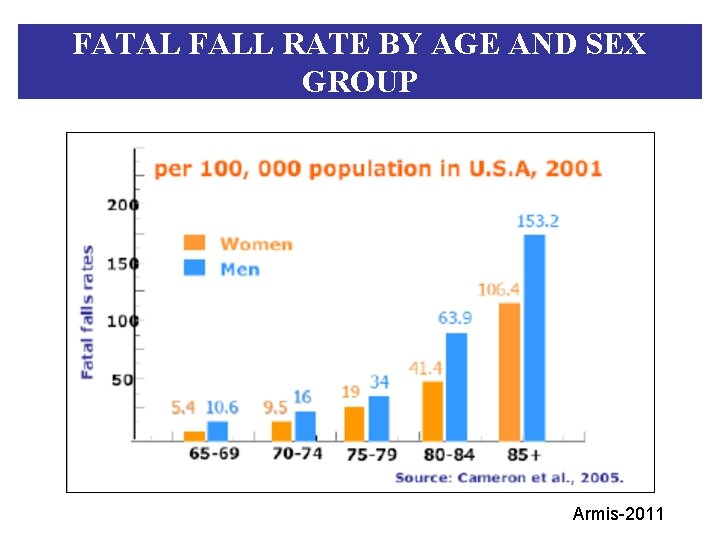
FATAL FALL RATE BY AGE AND SEX GROUP Armis-2011
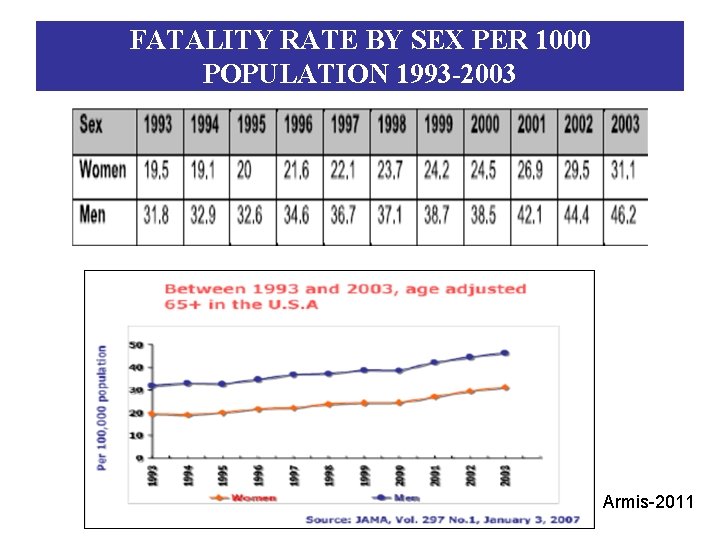
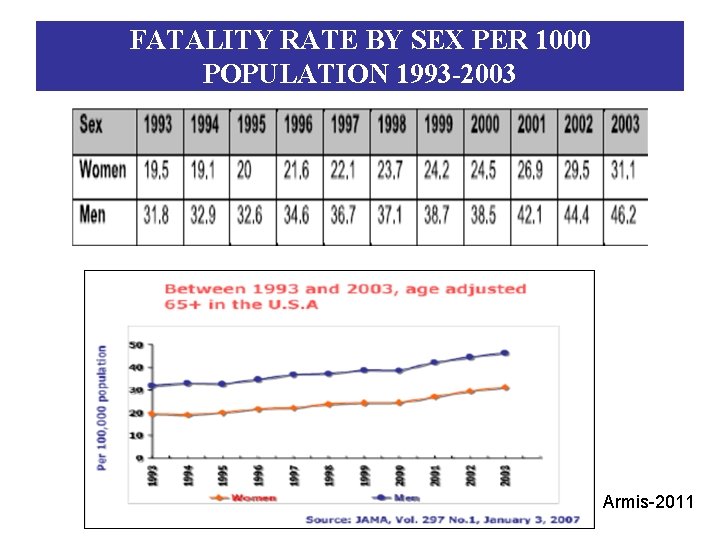
FATALITY RATE BY SEX PER 1000 POPULATION 1993 -2003 Armis-2011
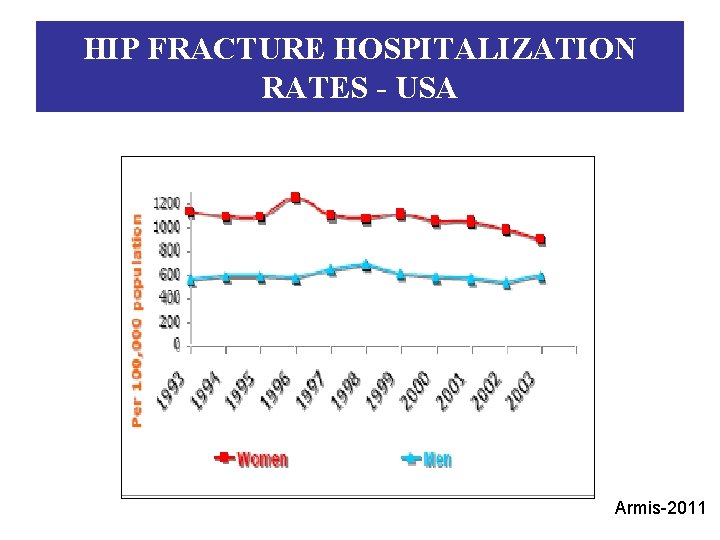
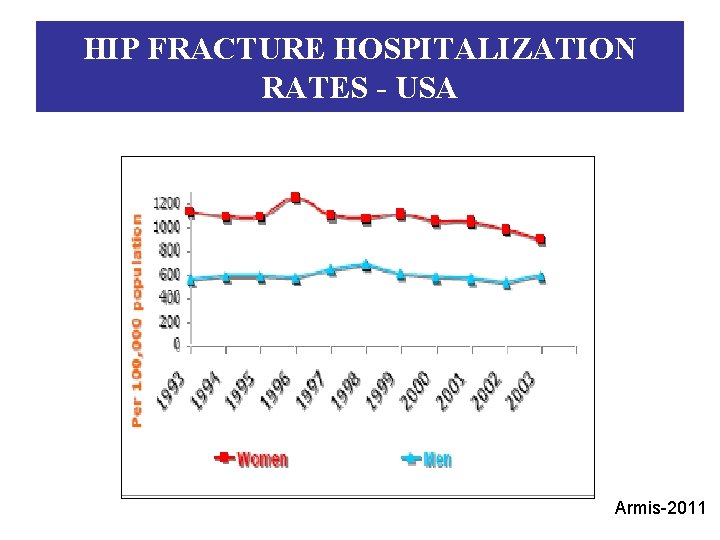
HIP FRACTURE HOSPITALIZATION RATES - USA Armis-2011
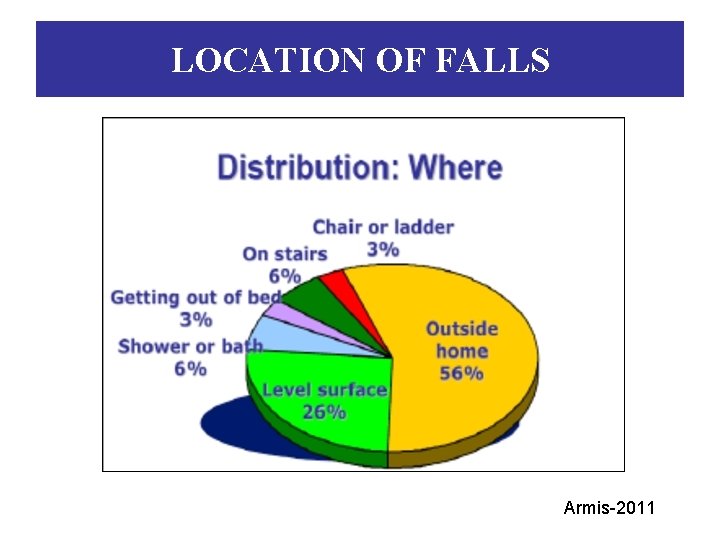
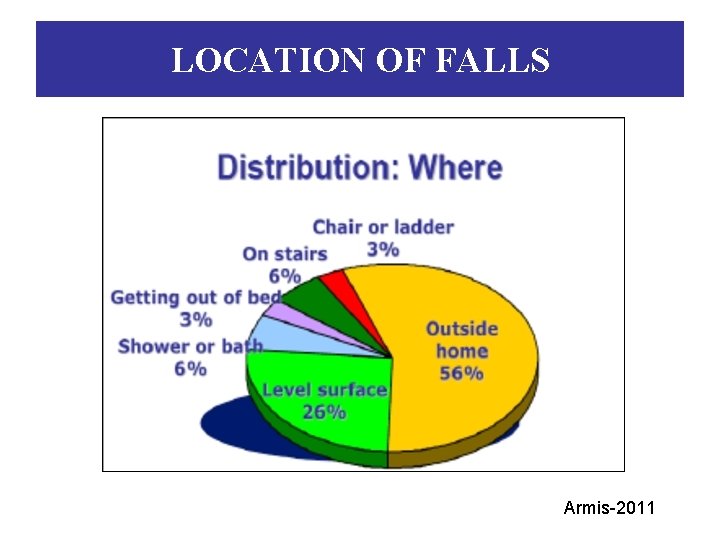
LOCATION OF FALLS Armis-2011
HIP ELDERLY FRACTURES PROBLEM: q. Increased mortality q. Longterm disability q. Loss independence
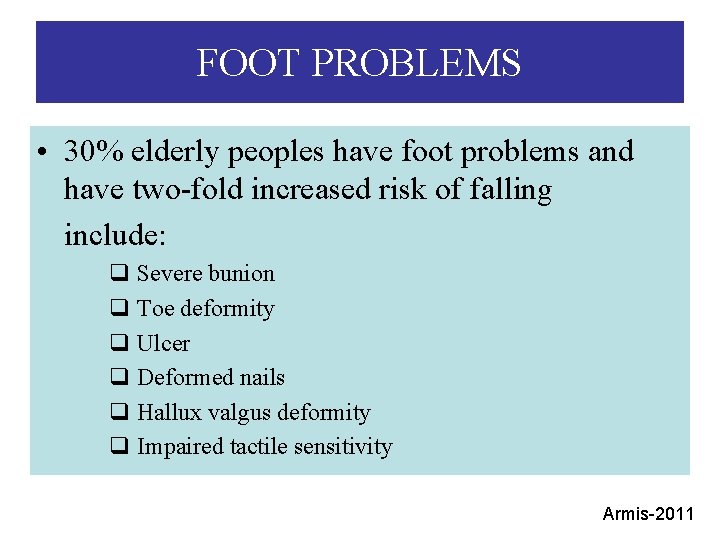
FOOT PROBLEMS • 30% elderly peoples have foot problems and have two-fold increased risk of falling include: q Severe bunion q Toe deformity q Ulcer q Deformed nails q Hallux valgus deformity q Impaired tactile sensitivity Armis-2011
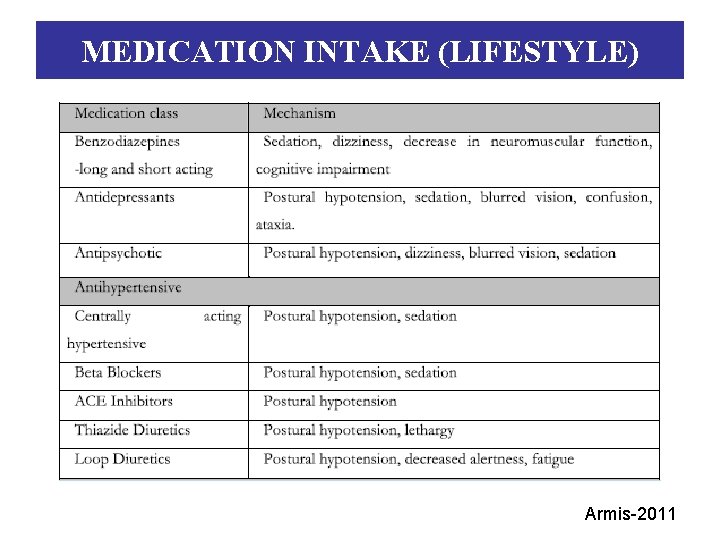
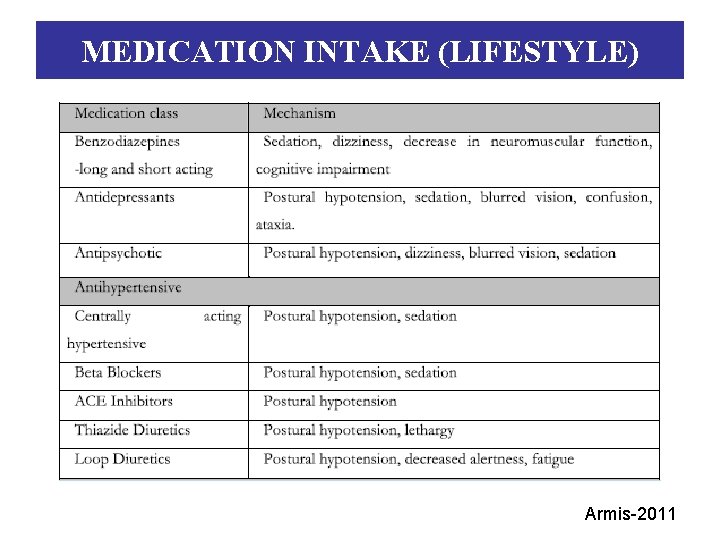
MEDICATION INTAKE (LIFESTYLE) Armis-2011
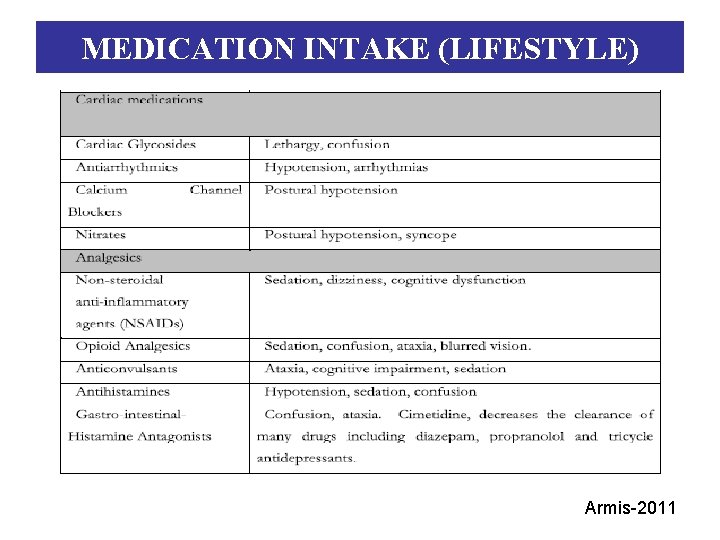
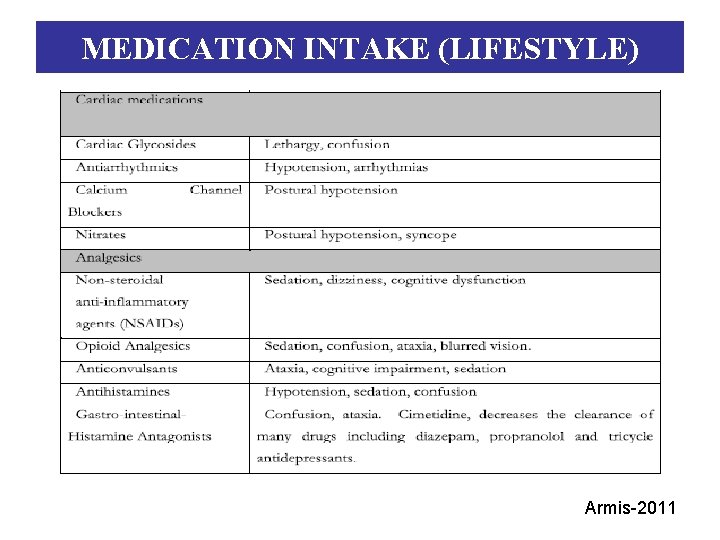
MEDICATION INTAKE (LIFESTYLE) Armis-2011
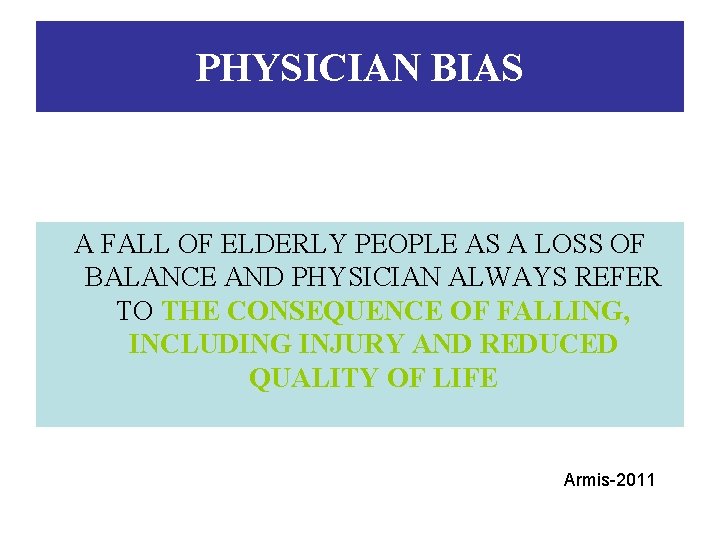
PHYSICIAN BIAS A FALL OF ELDERLY PEOPLE AS A LOSS OF BALANCE AND PHYSICIAN ALWAYS REFER TO THE CONSEQUENCE OF FALLING, INCLUDING INJURY AND REDUCED QUALITY OF LIFE Armis-2011
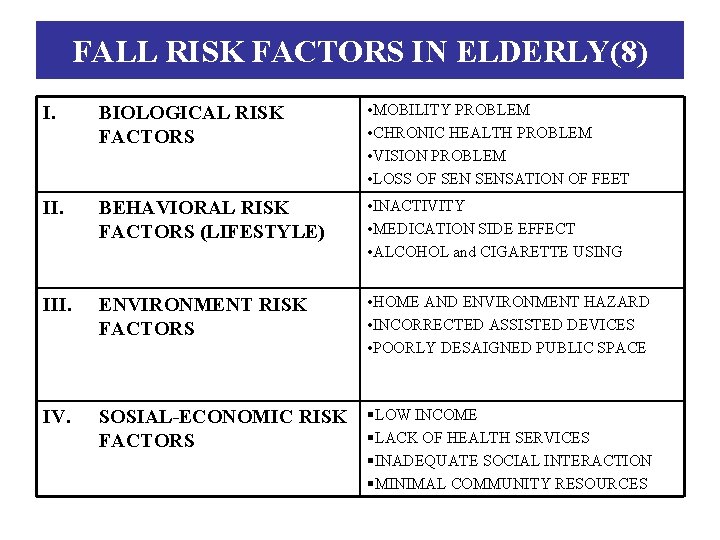
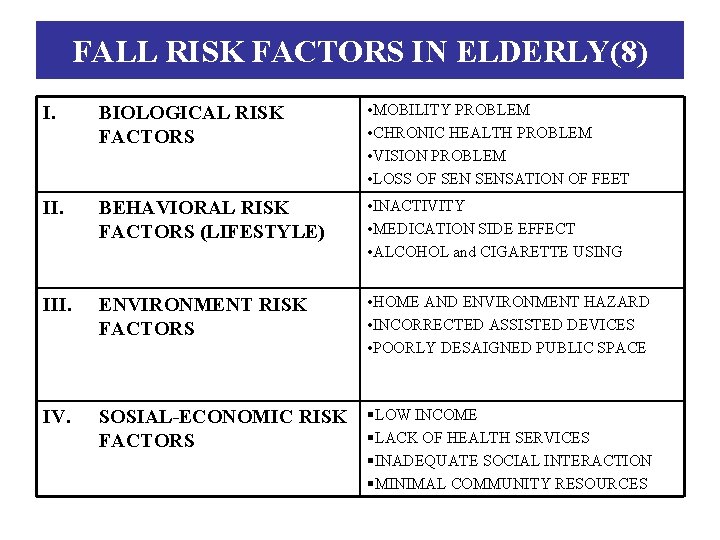
FALL RISK FACTORS IN ELDERLY(8) I. BIOLOGICAL RISK FACTORS • MOBILITY PROBLEM • CHRONIC HEALTH PROBLEM • VISION PROBLEM • LOSS OF SENSATION OF FEET II. BEHAVIORAL RISK FACTORS (LIFESTYLE) • INACTIVITY • MEDICATION SIDE EFFECT • ALCOHOL and CIGARETTE USING III. ENVIRONMENT RISK FACTORS • HOME AND ENVIRONMENT HAZARD • INCORRECTED ASSISTED DEVICES • POORLY DESAIGNED PUBLIC SPACE IV. SOSIAL-ECONOMIC RISK §LOW INCOME §LACK OF HEALTH SERVICES FACTORS §INADEQUATE SOCIAL INTERACTION §MINIMAL COMMUNITY RESOURCES
CONCLUSION “ FALL PREVENTION IS THE BEST STRATEGY IN HEALTHY LIFE OF ELDERLY PEOPLE” §COSTLY §FATALITY RATE §PREVENTABLE Armis-2011
FALL PREVENTION PROGRAM PLANNING 1. To define the effective program 2. To provide information to elderly peoples Armis-2011
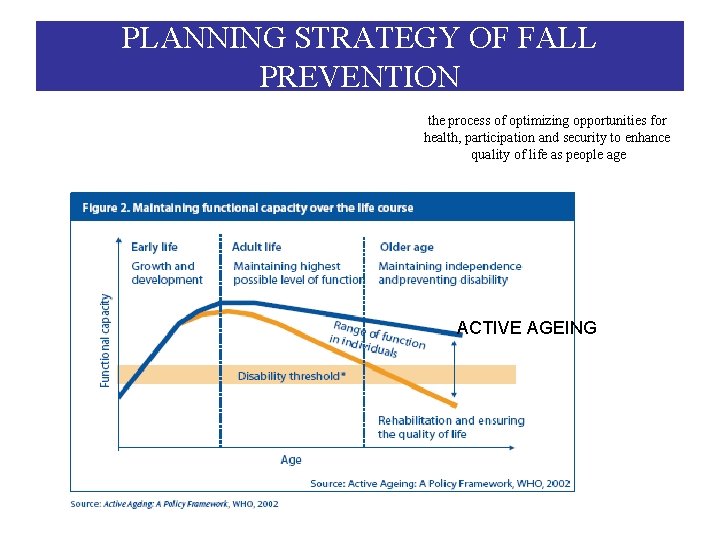
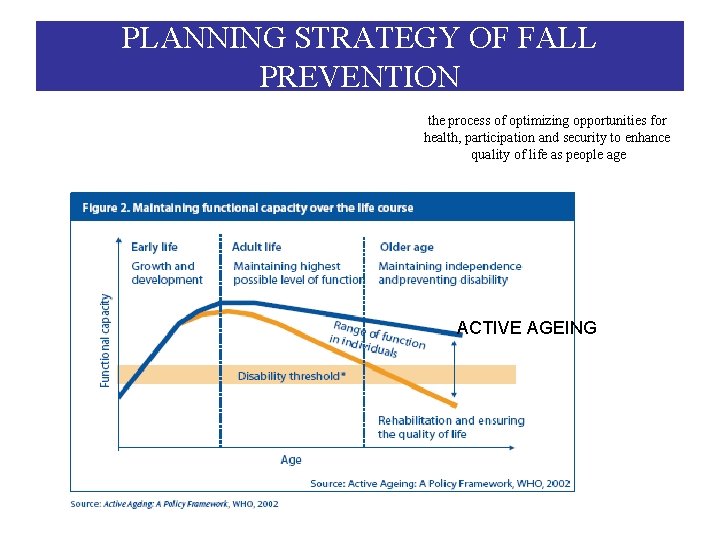
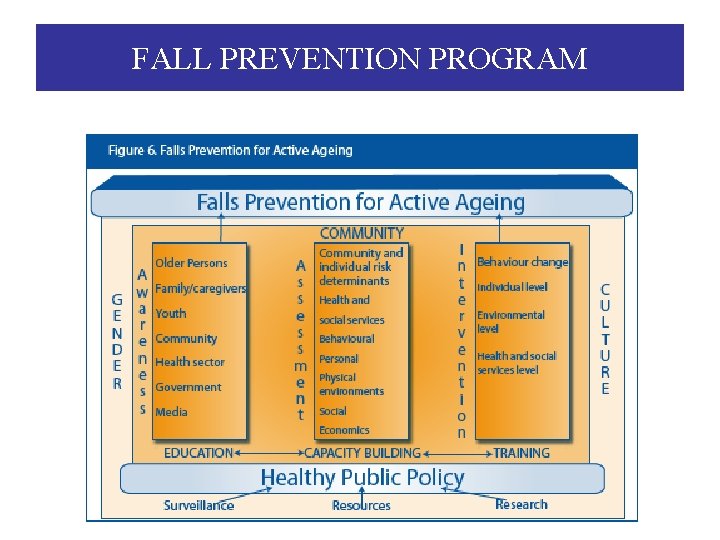
PLANNING STRATEGY OF FALL PREVENTION the process of optimizing opportunities for health, participation and security to enhance quality of life as people age ACTIVE AGEING
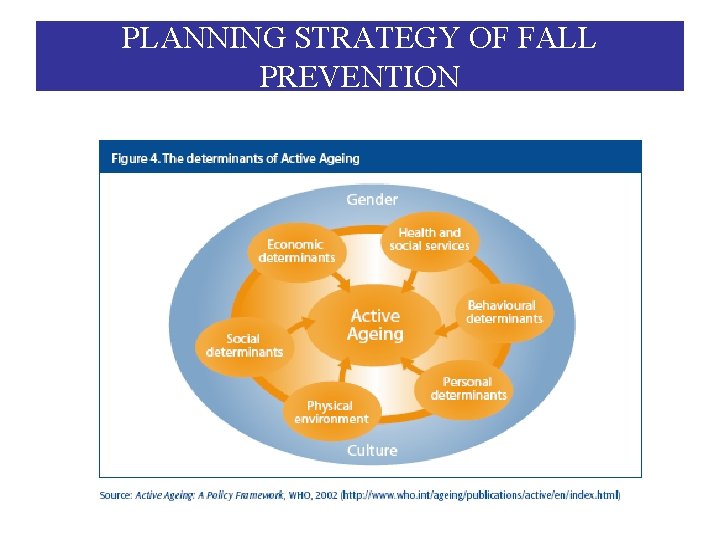
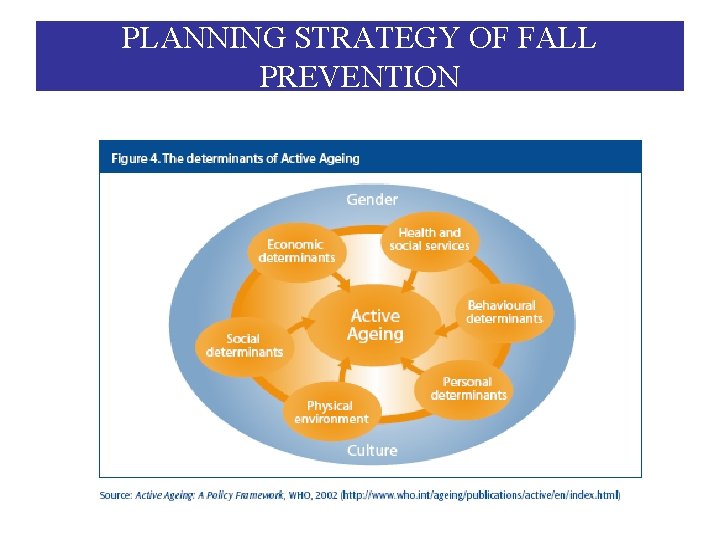
PLANNING STRATEGY OF FALL PREVENTION
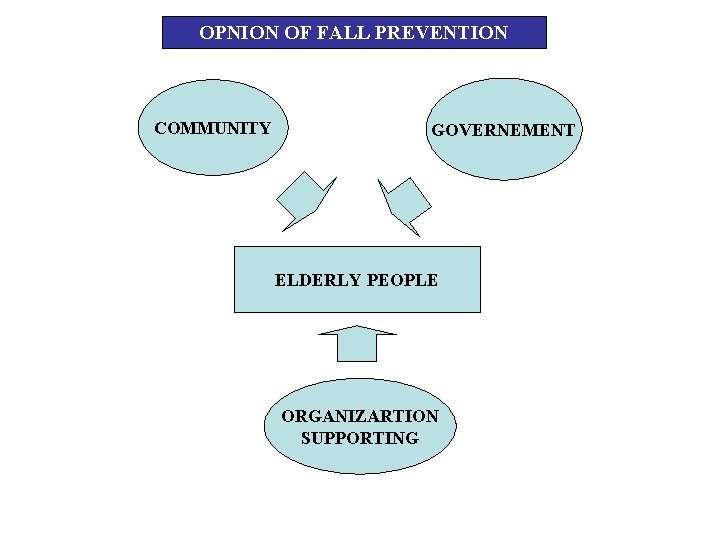
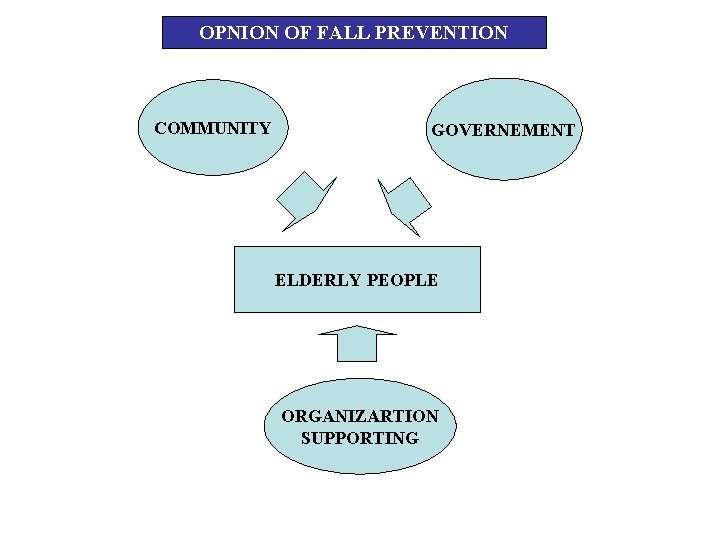
OPNION OF FALL PREVENTION COMMUNITY GOVERNEMENT ELDERLY PEOPLE ORGANIZARTION SUPPORTING
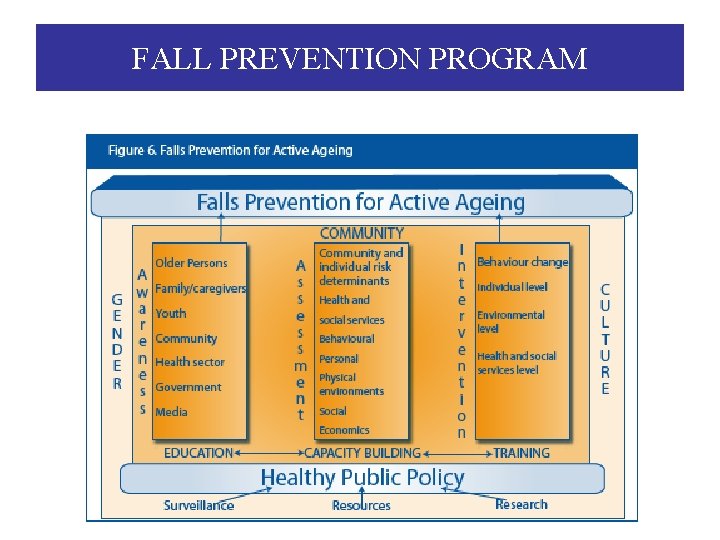
FALL PREVENTION PROGRAM
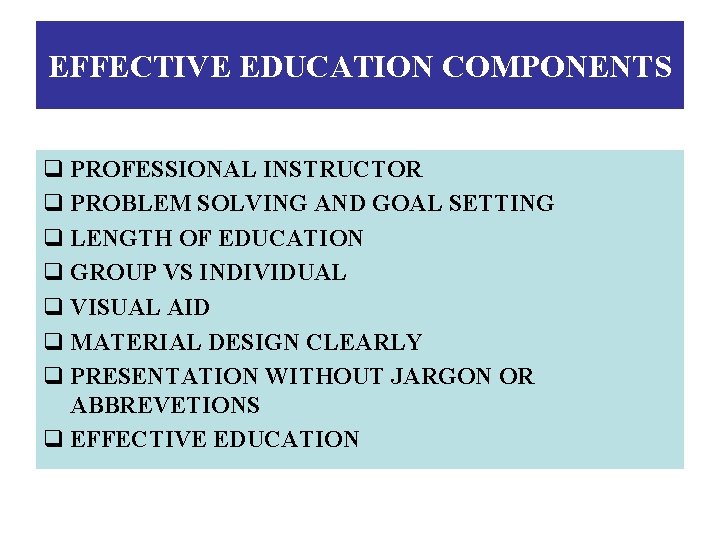
EFFECTIVE EDUCATION COMPONENTS q PROFESSIONAL INSTRUCTOR q PROBLEM SOLVING AND GOAL SETTING q LENGTH OF EDUCATION q GROUP VS INDIVIDUAL q VISUAL AID q MATERIAL DESIGN CLEARLY q PRESENTATION WITHOUT JARGON OR ABBREVETIONS q EFFECTIVE EDUCATION
EFFECTIVE EDUCATION PROGRAM OF FALL PREVENTION (2001) 1. Education falls risk factors and prevention strategies for elderly people 2. Exercise program: Tai Chi, Strengthening exercises, Balance exercises 3. Reduced medication 4. Vision correction 5. Home safety Armis-2011
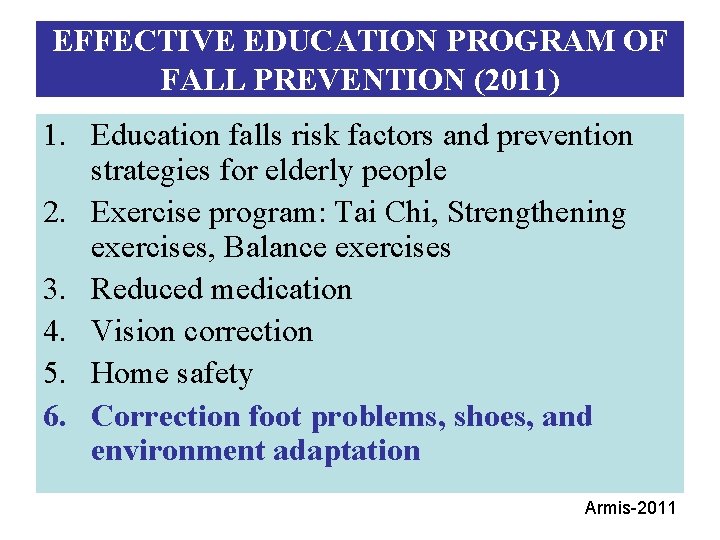
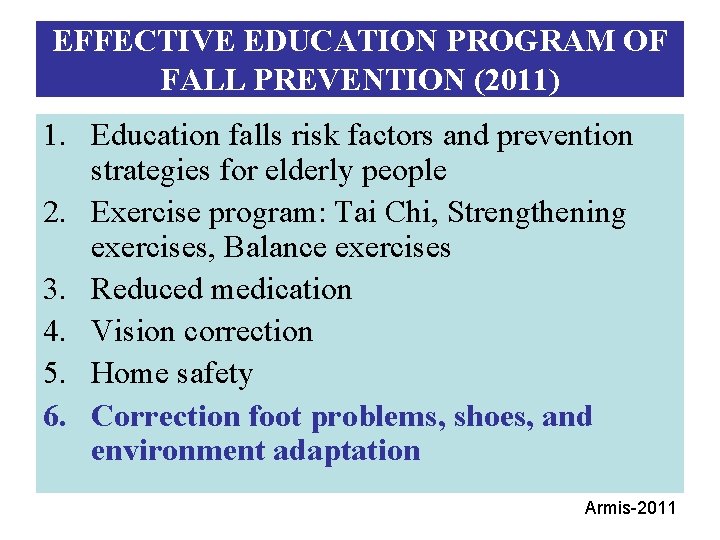
EFFECTIVE EDUCATION PROGRAM OF FALL PREVENTION (2011) 1. Education falls risk factors and prevention strategies for elderly people 2. Exercise program: Tai Chi, Strengthening exercises, Balance exercises 3. Reduced medication 4. Vision correction 5. Home safety 6. Correction foot problems, shoes, and environment adaptation Armis-2011
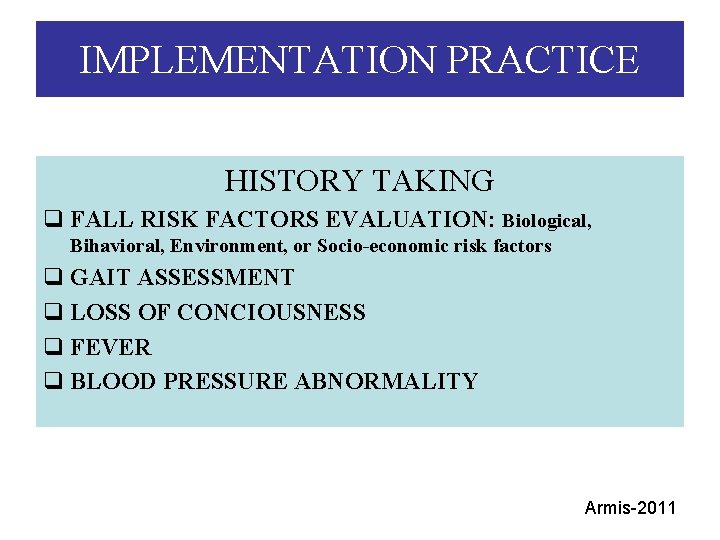
IMPLEMENTATION PRACTICE HISTORY TAKING q FALL RISK FACTORS EVALUATION: Biological, Bihavioral, Environment, or Socio-economic risk factors q GAIT ASSESSMENT q LOSS OF CONCIOUSNESS q FEVER q BLOOD PRESSURE ABNORMALITY Armis-2011
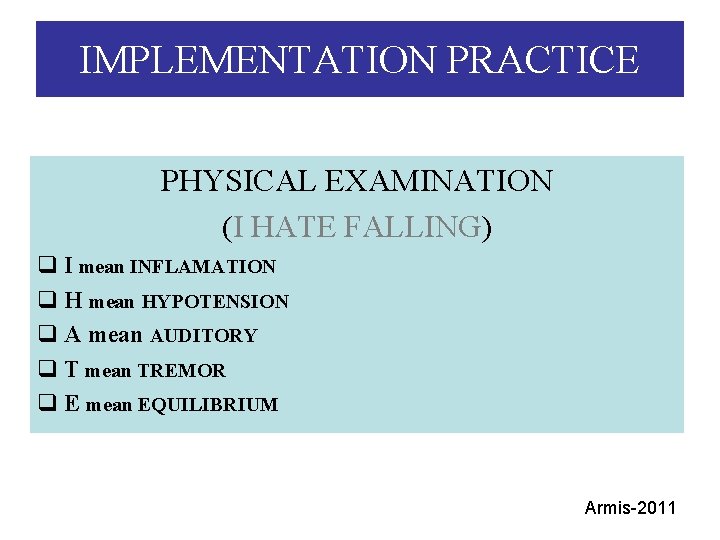
IMPLEMENTATION PRACTICE PHYSICAL EXAMINATION (I HATE FALLING) q I mean INFLAMATION q H mean HYPOTENSION q A mean AUDITORY q T mean TREMOR q E mean EQUILIBRIUM Armis-2011
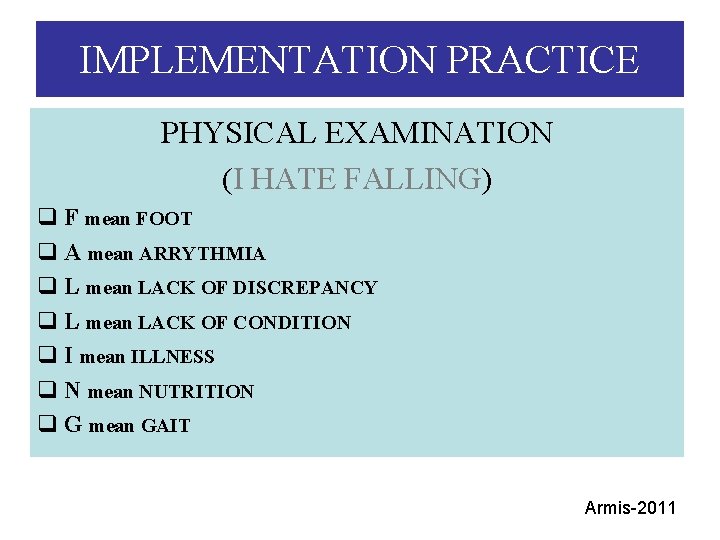
IMPLEMENTATION PRACTICE PHYSICAL EXAMINATION (I HATE FALLING) q F mean FOOT q A mean ARRYTHMIA q L mean LACK OF DISCREPANCY q L mean LACK OF CONDITION q I mean ILLNESS q N mean NUTRITION q G mean GAIT Armis-2011
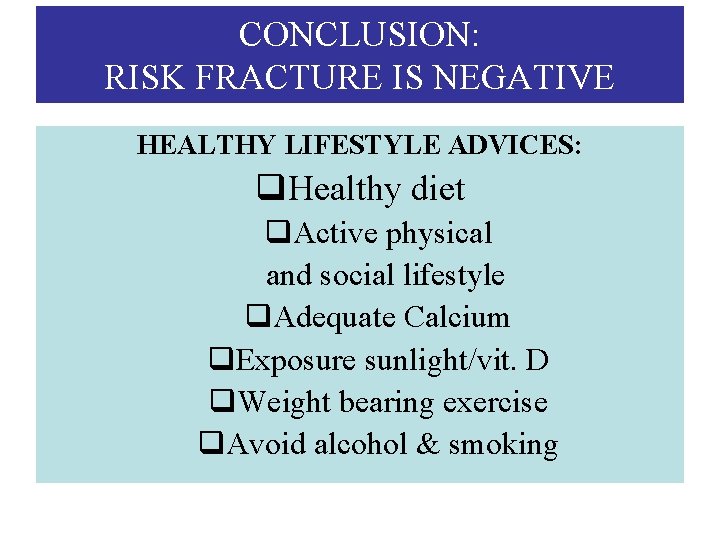
CONCLUSION: RISK FRACTURE IS NEGATIVE HEALTHY LIFESTYLE ADVICES: q. Healthy diet q. Active physical and social lifestyle q. Adequate Calcium q. Exposure sunlight/vit. D q. Weight bearing exercise q. Avoid alcohol & smoking
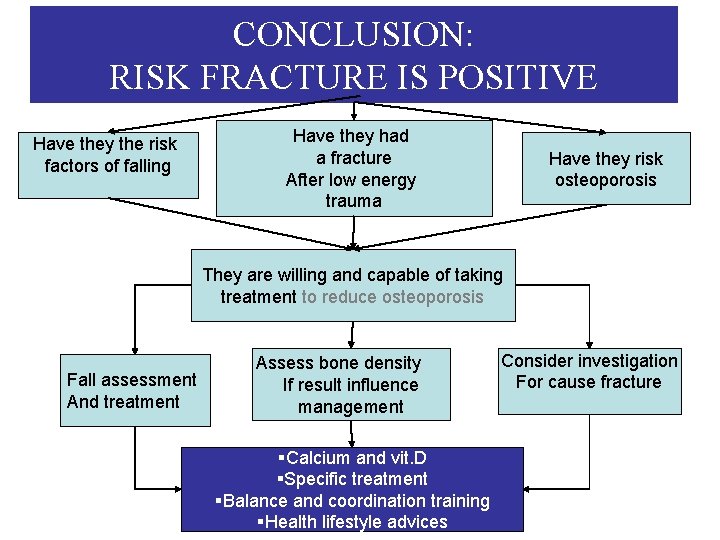
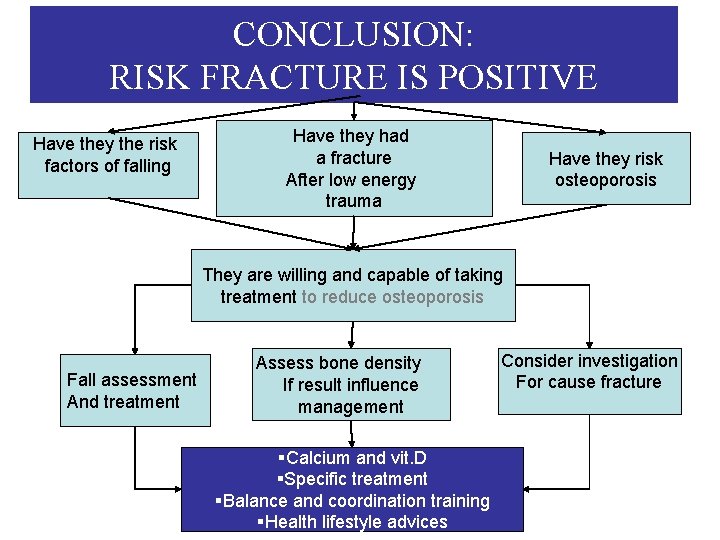
CONCLUSION: RISK FRACTURE IS POSITIVE Have they the risk factors of falling Have they had a fracture After low energy trauma Have they risk osteoporosis They are willing and capable of taking treatment to reduce osteoporosis Fall assessment And treatment Assess bone density If result influence management §Calcium and vit. D §Specific treatment §Balance and coordination training §Health lifestyle advices Consider investigation For cause fracture
ANY QUESTIONS? ? Armis-2011 35