EHLERS DANLOS SYNDROMES DISORDERS OF THE PELVIC FLOOR
- Slides: 37
EHLERS DANLOS SYNDROMES & DISORDERS OF THE PELVIC FLOOR Dr. Colleen Mc. Dermott; MSc, MD, FRCSC FPMRS Nov. 5, 2017
OBJECTIVES • Review Evidence, Investigations, Treatment Options for EDS and: • Lower Urinary Tract Symptoms • Pelvic Organ Prolapse • Pelvic Pain
EDS - BACKGROUND • EDS group of connective tissue disorders, 13 subtypes, collagen defects • Classification based on symptoms, genetics, and biochemical markers • Common findings include: • • Hyperextensibility of skin Joint hypermobility Abnormal tissue fragility Easy bruising • Common gynecologic issues can include: • Urinary symptoms • Pelvic Organ Prolapse • Pelvic Pain
EDS – LOWER URINARY TRACT SYMPTOMS • THE EVIDENCE • Mc. Intosh et al 1 • 41 EDS female volunteers (type I/II/III; 1995) pelvic exam, urodynamics, physiotherapy consult • 60% reported urinary incontinence (UI), 80% of these had stress incontinence (SUI) • All urodynamic testing was normal • Carley et al 2 • 8 women with EDS (type not specified) • 4 patients had UI, 2 had surgery for UI, 3 had SUI, 1 had mixed UI 1. 2. J Soc Gynecol Invest 1995; 2: 559 -64. Am J Obstet Gynecol 2000; 182: 1021 -23.
EDS – LOWER URINARY TRACT SYMPTOMS • THE EVIDENCE • Jha et al 1 • 30 women with Benign Joint Hypermobility Syndrome (BJHS) and 30 Control women • Mail and telephone surveys • 60% BJHS group had UI versus 30% in control group 1. IUJ 2007; 18: 61 -64.
EDS – LOWER URINARY TRACT SYMPTOMS • WORK-UP • History • • Onset, frequency, severity, pattern of UI Frequency, dysuria, urgency, nocturia Pads/24 hrs? Obstructive urinary symptoms (incomplete voiding, hesitancy, straining, post-void dribbling, recurrent UTI) • POP symptoms
EDS – LOWER URINARY TRACT SYMPTOMS • WORK-UP • History • • Neurologic conditions/symptoms Vaginal sx or incontinence sx OB history, current menopausal/HT status Medications (sedatives, diuretics, anticholinergic medications, OTCs) • Lifestyle risk factors: (caffeine, smoking, weight, exercise, occupation) • Urinary diary
EDS – LOWER URINARY TRACT SYMPTOMS • WORK-UP • Physical Examination • Height, weight, BMI • Abdominal exam: scars, abdominal mass, presence of a full bladder • Neurologic exam: S 2 -S 4 sacral nerves (motor, sensory, and reflexes)
EDS – LOWER URINARY TRACT SYMPTOMS • WORK-UP • Physical Examination • Pelvic exam: inspect vulva and urogenital epithelium, assess for signs of pelvic organ prolapse, DRE to assess for anal sphincter tone and perineal sensation • Standing stress test
EDS – LOWER URINARY TRACT SYMPTOMS • WORK-UP • Studies: • Urinalysis hematuria, pyuria, glucosuria, proteinuria • Hematuria/irritative voiding symptoms cytology • Pyuria/bacteriuria urine culture • PVR • Normal: <1/3 total volume • Abnormal: >1/3 total volume (poor bladder contractility or bladder outlet obstruction)
EDS – LOWER URINARY TRACT SYMPTOMS • WORK-UP • Studies: • Urodynamic testing: • Unclear diagnosis, mixed symptoms, prior LUT surgery, known or suspected neurogenic bladder, a negative SST, abnormal PVR or evidence of voiding dysfunction
EDS – LOWER URINARY TRACT SYMPTOMS • TREATMENT OPTIONS • OVERACTIVE BLADDER syndrome defined as "urgency, with or without urge incontinence (UUI), usually with frequency and nocturia” • BEHAVIOUR MODIFICATION • Lifestyle/Habit Changes • Bladder irritants caffeine, nicotine, alcohol, artificial sweeteners • Water consumption 40 -50 oz/day, stop fluid consumption 3 -4 hrs before bedtime, consume most of fluid in morning/afternoon • Weight management 5% weight reduction = >50% reduction in incontinence episodes • Effective cough management • Treat constipation/fecal impaction • Bladder training with Pelvic Physio
EDS – LOWER URINARY TRACT SYMPTOMS • TREATMENT OPTIONS • OVERACTIVE BLADDER syndrome defined as "urgency, with or without urge incontinence (UUI), usually with frequency and nocturia” • Medication: anticholinergics, β-adrenergic agonist • Botox into bladder • Sacral Neuromodulation
EDS – LOWER URINARY TRACT SYMPTOMS • TREATMENT OPTIONS • STRESS URINARY INCONTINENCE Involuntary leakage on effort/exertion or with sudden increase in abdominal pressure • • Pelvic Floor Training with Physio Incontinence Tampon Incontinence Pessary Procedure • Vaginal Laser • Urethral Bulking • Burch Urethropexy (abdominal surgery) • Midurethral Sling (MESH – CAUTION***)
EDS – LOWER URINARY TRACT SYMPTOMS • TREATMENT OPTIONS • VOIDING DYSFUNCTION unable to empty bladder, disorder of the bladder/bladder outlet/or both, neurogenic or non-neurogenic • • • Pelvic floor rehabilitation with Physio Intermittent self catheterization Medications to relax pelvic floor, urethra, and/or bladder Botox injection into the bladder and/or urethral sphincter Sacral neuromodulation Treat prolapse if contributing
EDS – PELVIC ORGAN PROLAPSE • THE EVIDENCE • Norton et al 1 • Cohort of 107 women, 39 with hypermobility • Hypermobile patients had significantly higher rates of cystocele, rectocele, uterine prolapse • Mc. Intosh et al 2 • 46 EDS patients • No correlation between joint hypermobility and vaginal prolapse 1. 2. Obstet Gynecol 1995; 85: 225 -228. Gynecol Obstet Invest 1996; 41: 135 -139.
EDS – PELVIC ORGAN PROLAPSE • THE EVIDENCE • Mastoroudes et al 1 • 60 patients with benign joint hypermobility and 60 controls • Significantly more prolapse in BJHS group • In BJHS group prolapse had a greater impact on sexual and defecatory function • Carley et al 2 • 8 women with EDS (type not specified) • 6 patients had symptoms of prolapse 1. 2. BJOG 2013; 120: 187 -192. Am J Obstet Gynecol 2000; 182: 1021 -23.
EDS – PELVIC ORGAN PROLAPSE • WORK-UP • Pelvic Organ Prolapse (POP) a weakening in the structures of the pelvic floor resulting in descent of one or more of the pelvic structures (bladder/rectum/small intestine/uterus) into the vagina
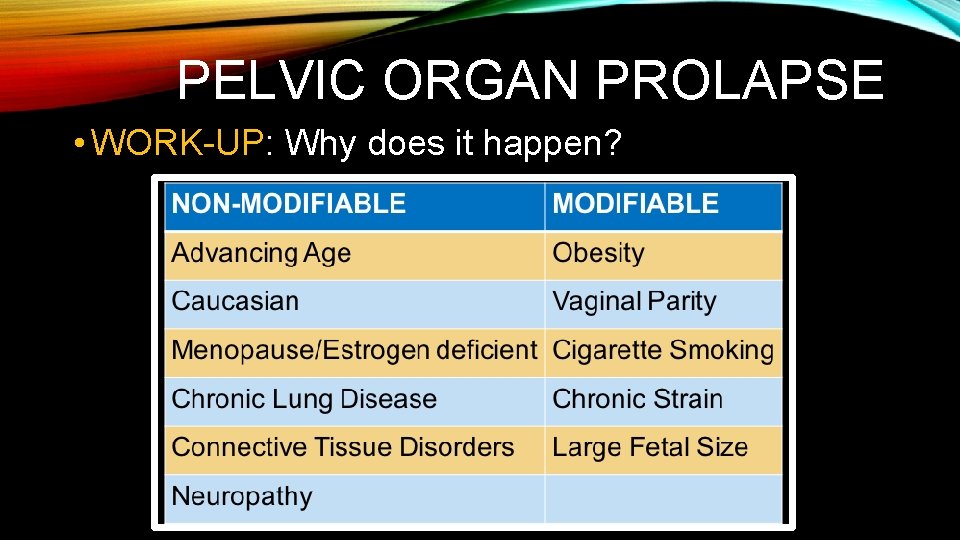
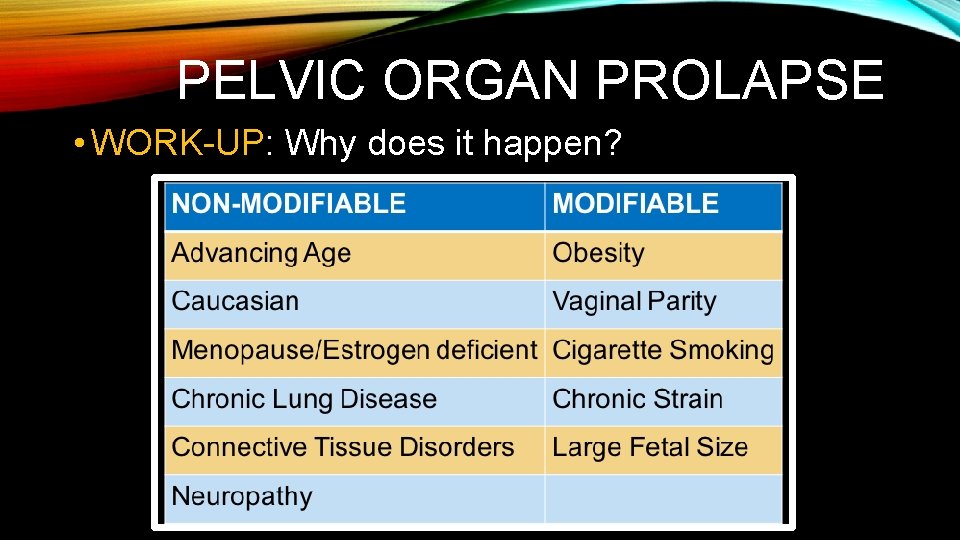
PELVIC ORGAN PROLAPSE • WORK-UP: Why does it happen?
EDS – PELVIC ORGAN PROLAPSE • WORK-UP • ON HISTORY …. . • Vaginal bulge • Pressure • Voiding symptoms: inability to empty, overactive bladder, recurrent UTI, vaginal splinting to empty • Defecatory symptoms: constipation, fecal incontinence (seepage), vaginal splinting to defecate • Sexual dysfunction: dyspareunia, embarrassment, decreased libido, decreased orgasm • OR NOTHING!
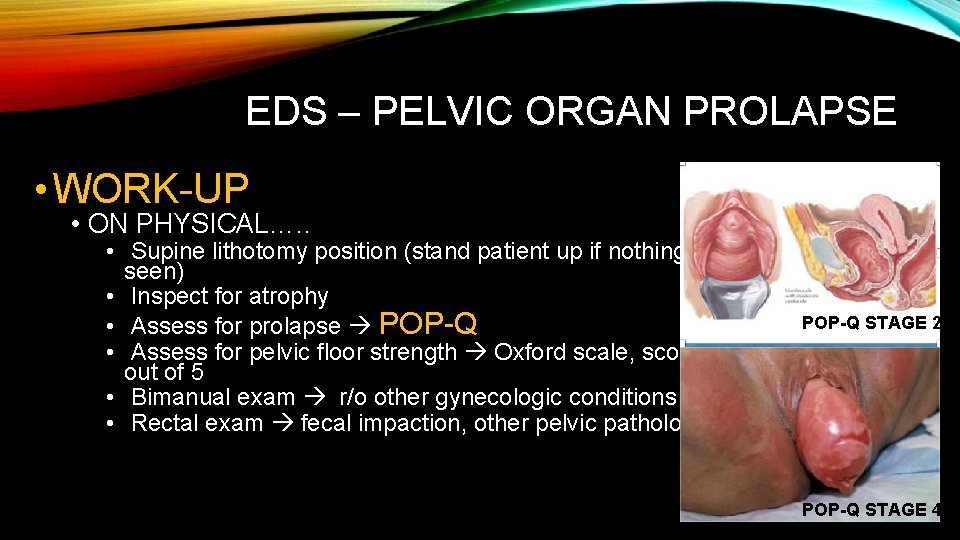
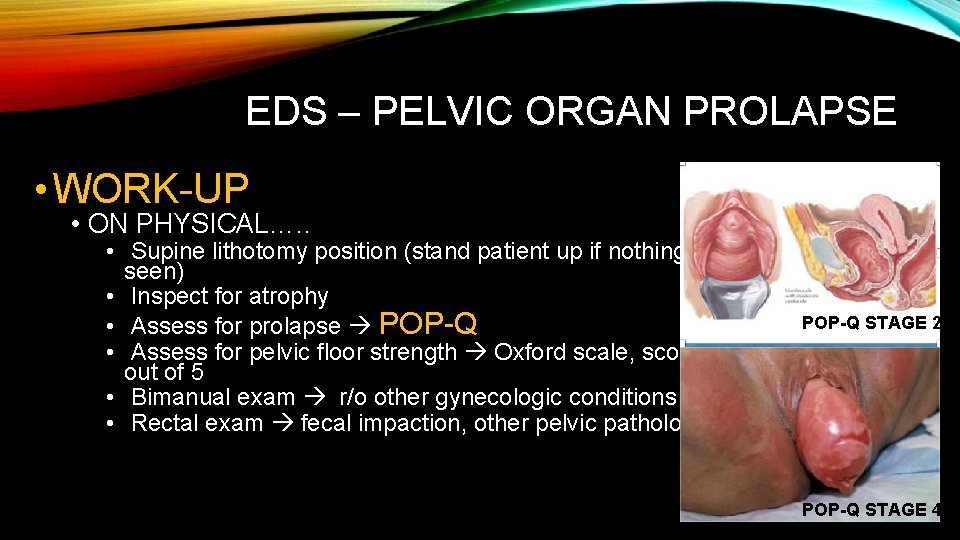
EDS – PELVIC ORGAN PROLAPSE • WORK-UP • ON PHYSICAL…. . • Supine lithotomy position (stand patient up if nothing seen) • Inspect for atrophy • Assess for prolapse POP-Q • Assess for pelvic floor strength Oxford scale, score out of 5 • Bimanual exam r/o other gynecologic conditions • Rectal exam fecal impaction, other pelvic pathology POP-Q STAGE 2 POP-Q STAGE 4
EDS – PELVIC ORGAN PROLAPSE • TREATMENT OPTIONS • Pelvic Floor Muscle Training (PFMT) • Pessary • Surgery • Native Tissue Repair* • Mesh Repair (CAUTION)
EDS – PELVIC PAIN • THE EVIDENCE • THERE IS NONE!!!
EDS – PELVIC PAIN • INVESTIGATIONS • Medical History • • Accidents (falls/back injuries), history of depression/mood disorder Medications have they tried for CPP and what was the response? What are current medications and who prescribed? What birth control are they currently using, tried in the past? • Surgical History • What surgeries have they had for CPP and what was response? • What other surgeries have they had? • Obstetrical History • Family History
EDS – PELVIC PAIN • INVESTIGATIONS • Menstrual History • Frequency, length, flow, pain • Urinary Issues • Gastrointestinal Issues • Sexual Intercourse • Current activity, type, pain during/after intercourse, superficial/deep, pain with orgasm
EDS – PELVIC PAIN • INVESTIGATIONS • Health Habits • Exercise, smoking, alcohol, caffeine, recreational drugs • Coping Mechanisms • Who does patient talk to about pain, what is partner’s attitude towards pain • Social History • Relationship status, living with, education, type of work (current/past) • Short Form Mc. Gill Pain Questionnaire
EDS – PELVIC PAIN • INVESTIGATIONS • Talk to patient throughout exam, elicit feedback on if pain is being reproduced • Observe general demeanour, mobility, positioning, guarding • Back scoliosis, point tenderness (sacroiliac, piriformis, coccyx) • Abdomen look for scars, assess for trigger points in all four quadrants using light tough and deeper palpation, head raise test, pubic bone/symphysis pubis
EDS – PELVIC PAIN • INVESTIGATIONS • Pelvis may be done with a mirror • Vulva: inspect for vulvar skin dystrophy, Q-tip test, clitoroanal reflex • Single Digit Exam • Speculum: atrophy, prolapse, STI swabs • Psychosocial Assessment • Referral to Social Worker, Psychotherapist, Psychiatrist
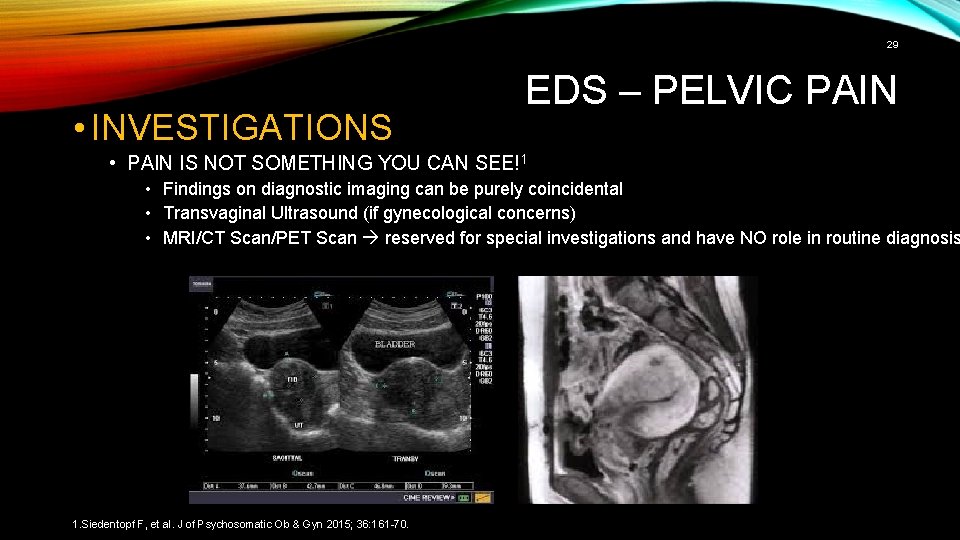
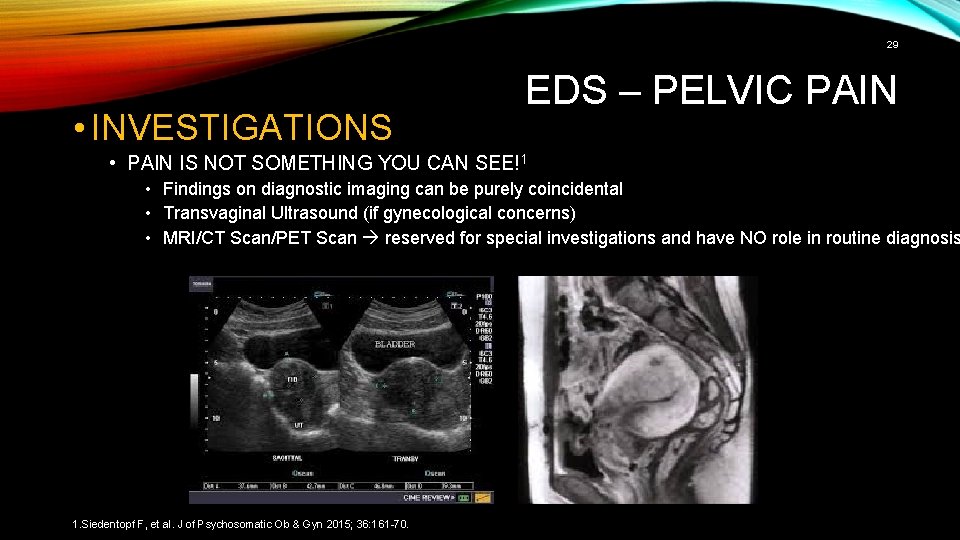
29 • INVESTIGATIONS EDS – PELVIC PAIN • PAIN IS NOT SOMETHING YOU CAN SEE!1 • Findings on diagnostic imaging can be purely coincidental • Transvaginal Ultrasound (if gynecological concerns) • MRI/CT Scan/PET Scan reserved for special investigations and have NO role in routine diagnosis 1. Siedentopf F, et al. J of Psychosomatic Ob & Gyn 2015; 36: 161 -70.
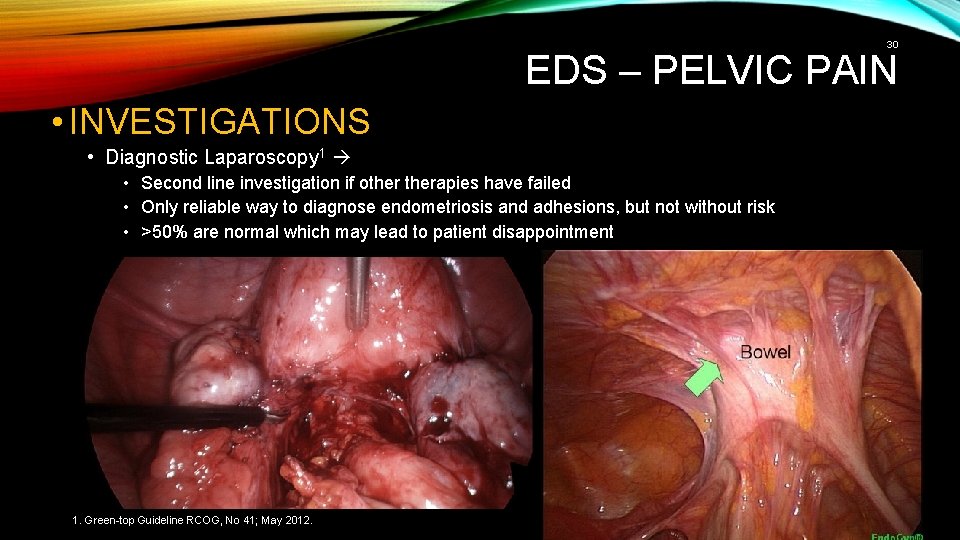
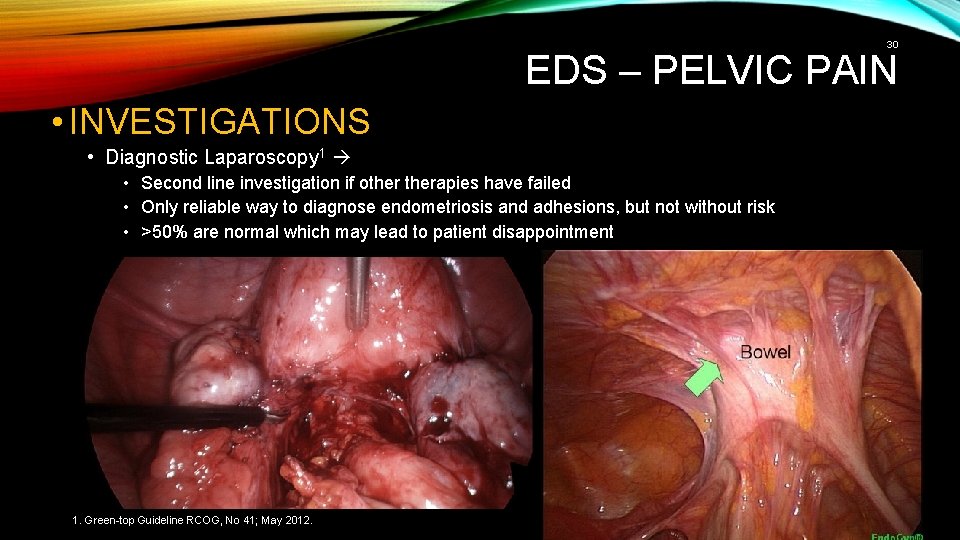
30 EDS – PELVIC PAIN • INVESTIGATIONS • Diagnostic Laparoscopy 1 • Second line investigation if otherapies have failed • Only reliable way to diagnose endometriosis and adhesions, but not without risk • >50% are normal which may lead to patient disappointment 1. Green-top Guideline RCOG, No 41; May 2012.
EDS – PELVIC PAIN • DIFFERENTIAL DIAGNOSES • Bladder Pain Syndrome • Gynecological conditions: vulvodynia, endometriosis • Myofascial Pelvic Pain • Gastrointestinal conditions: IBS, chronic anal pain
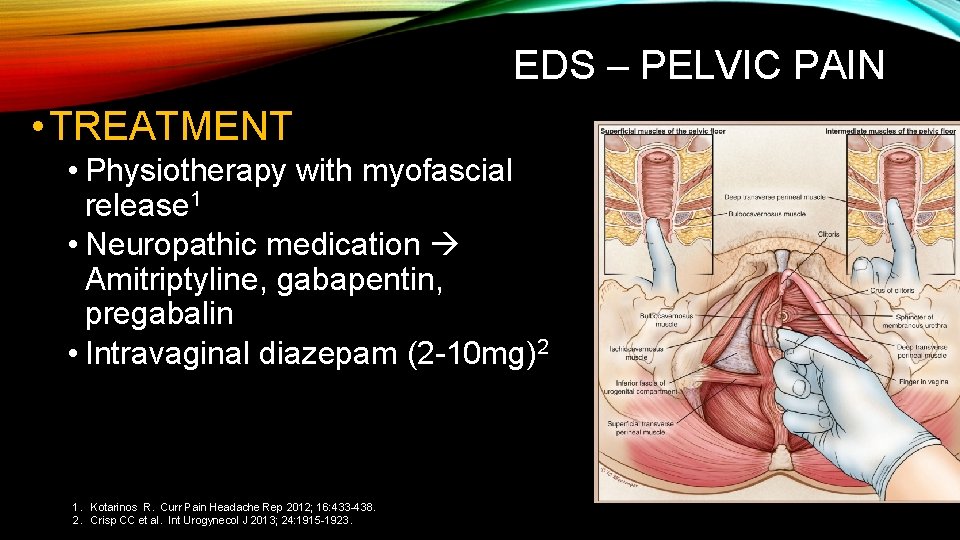
EDS – PELVIC PAIN • Often described as pelvic, groin, low back, or gluteal pain • Radiation to hip and sacrum • Involves pubococcygeus, puborectalis, iliococcygeus, and coccygeus muscles (levator ani) • Also ischiocavernosus, bulbocavernosus, and transverse perinei (superficial urogenital diaphragm) • Translate to nearby organs (bladder, bowel, vagina) dysuria/urinary retention, dyspareunia, dyschezia 1. Gyang A et al. Obstet Gynecol 2013; 121: 645 -650.
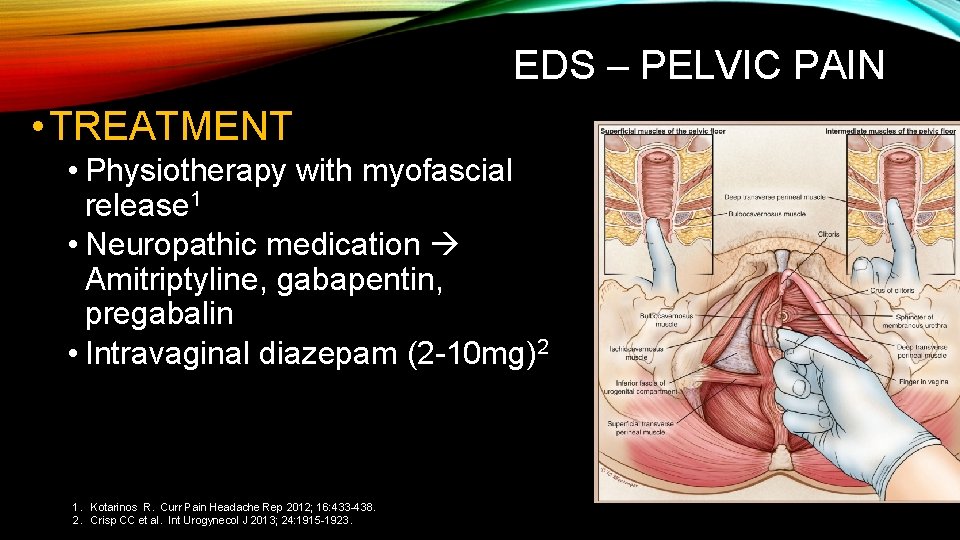
EDS – PELVIC PAIN • TREATMENT • Physiotherapy with myofascial release 1 • Neuropathic medication Amitriptyline, gabapentin, pregabalin • Intravaginal diazepam (2 -10 mg)2 1. Kotarinos R. Curr Pain Headache Rep 2012; 16: 433 -438. 2. Crisp CC et al. Int Urogynecol J 2013; 24: 1915 -1923.
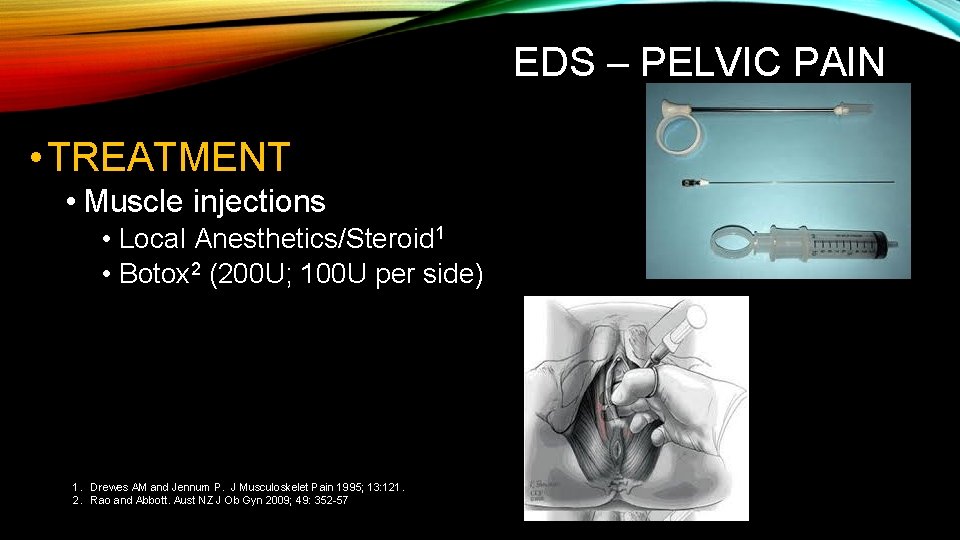
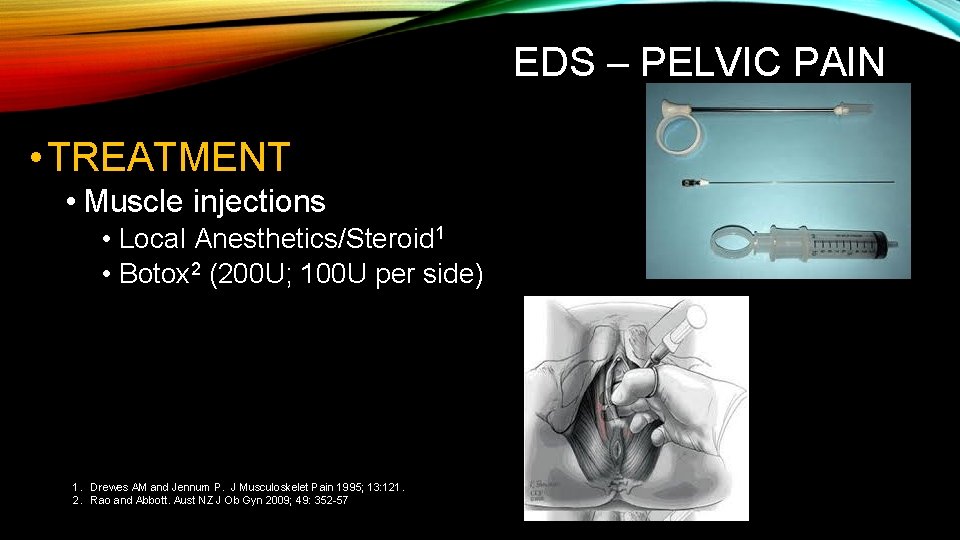
EDS – PELVIC PAIN • TREATMENT • Muscle injections • Local Anesthetics/Steroid 1 • Botox 2 (200 U; 100 U per side) 1. Drewes AM and Jennum P. J Musculoskelet Pain 1995; 13: 121. 2. Rao and Abbott. Aust NZ J Ob Gyn 2009; 49: 352 -57
SUMMARY • EDS and LUTS • • • Discuss options with urogynecologist or urologist Lifestyle Modifications PELVIC PHYSIO Consider medications Non-surgical options Beware of implants! • EDS and PROLAPSE • • • Discuss options with urogynecologist Lifestyle Modifications PELVIC PHYSIO Non-surgical options Beware of implants!!!
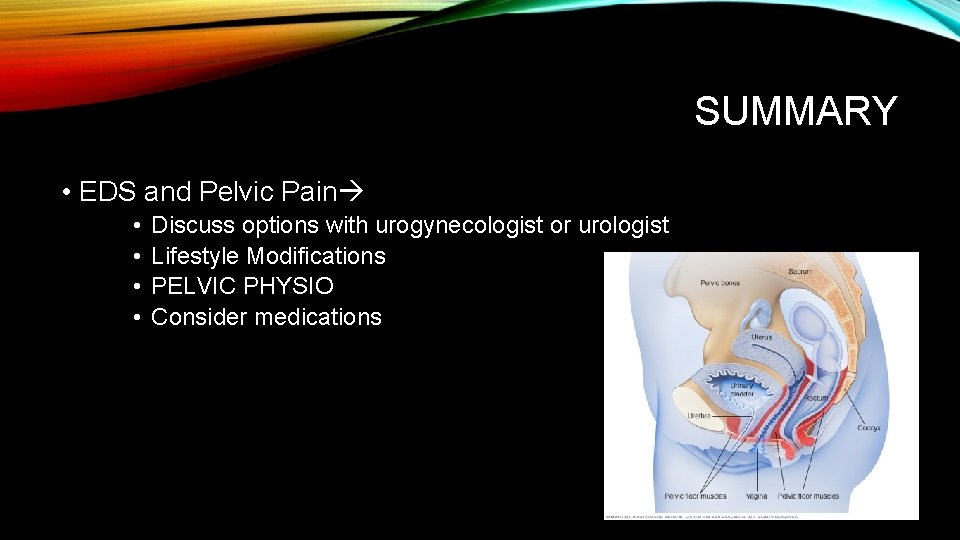
SUMMARY • EDS and Pelvic Pain • • Discuss options with urogynecologist or urologist Lifestyle Modifications PELVIC PHYSIO Consider medications
THANK YOU!