Effective Perinatal Care EPC PARTOGRAM n At the

- Slides: 98
Effective Perinatal Care (EPC) PARTOGRAM
n At the end of this module, the participants will: Ø Know the history and the background of the partograph Ø Understand the effectiveness of the partograph for improving perinatal outcomes Ø Know how a partograph is used and how to complete one Ø Be able to interpret the partograph and use it to make decisions in managing labour Effective Perinatal Care (EPC) Learning objectives 3 MO-2
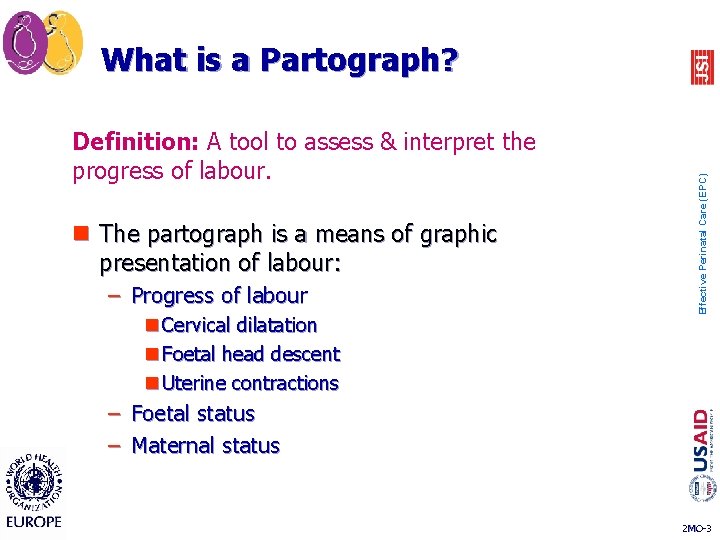
Definition: A tool to assess & interpret the progress of labour. n The partograph is a means of graphic presentation of labour: – Progress of labour n Cervical dilatation n Foetal head descent n Uterine contractions Effective Perinatal Care (EPC) What is a Partograph? – Foetal status – Maternal status 2 MO-3
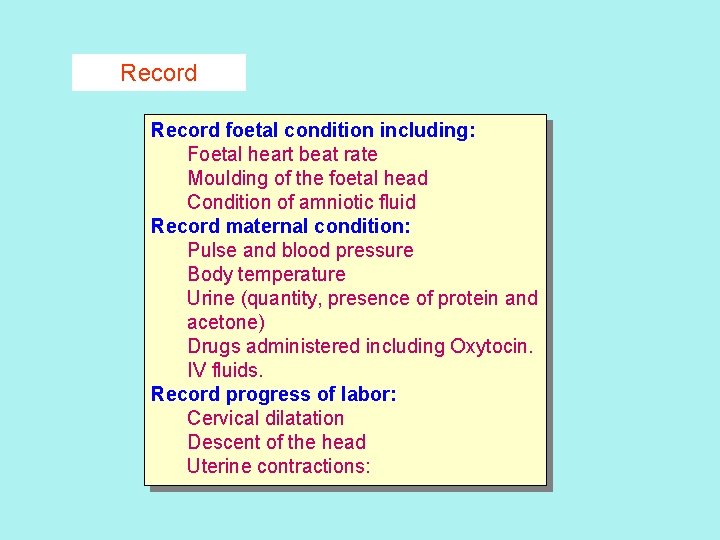
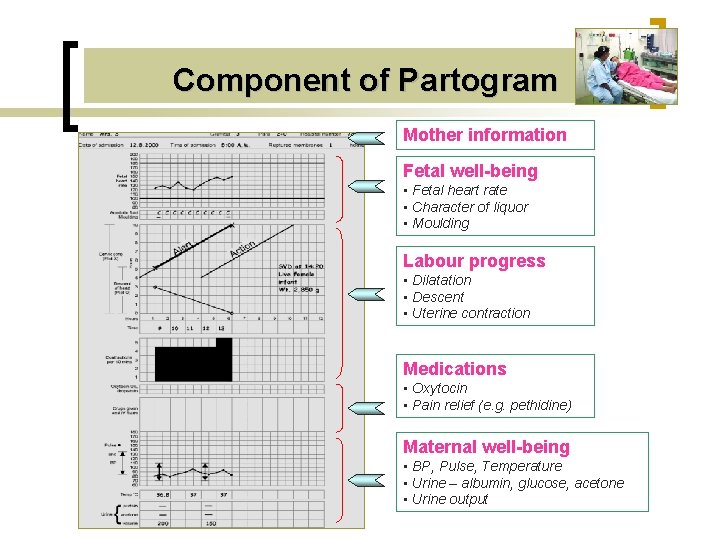
Record foetal condition including: Foetal heart beat rate Moulding of the foetal head Condition of amniotic fluid Record maternal condition: Pulse and blood pressure Body temperature Urine (quantity, presence of protein and acetone) Drugs administered including Oxytocin. IV fluids. Record progress of labor: Cervical dilatation Descent of the head Uterine contractions:
WHY IS IT IMPORTANT TO RECORD THE PROGRESS OF LABOUR Documentation is important n n n To provide continuity of care. To provide a basis of decision making. To facilitate research. To allow audit and review. To defend one’s actions – no documentation – no defense.
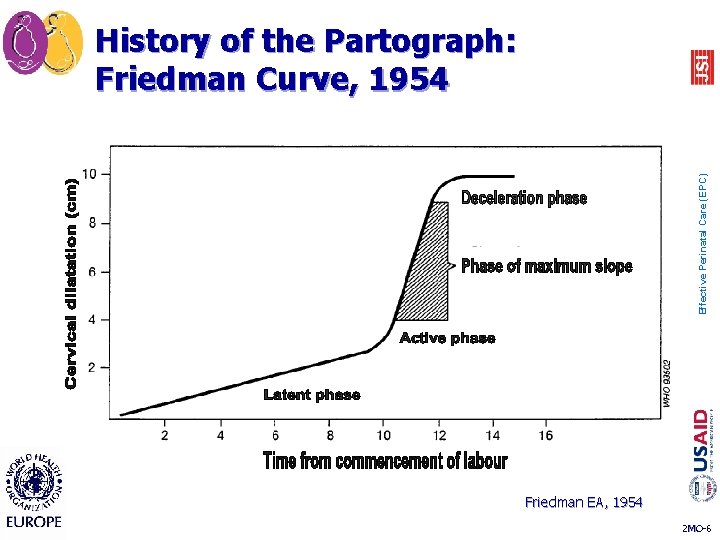
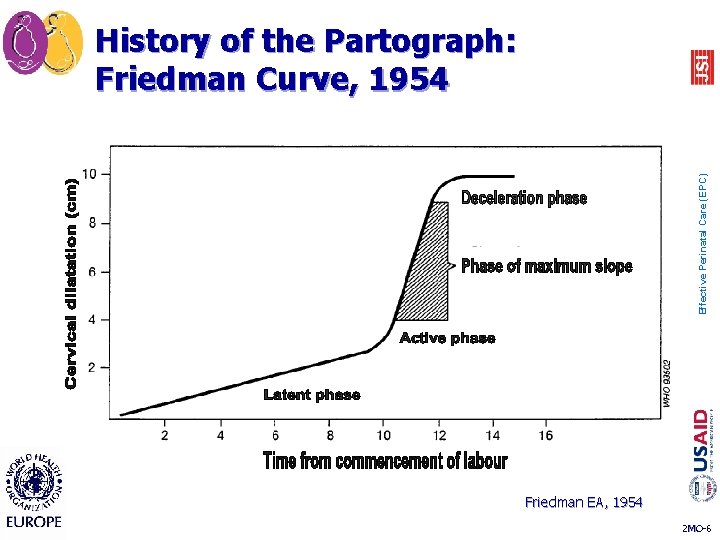
Effective Perinatal Care (EPC) History of the Partograph: Friedman Curve, 1954 Friedman EA, 1954 2 MO-6
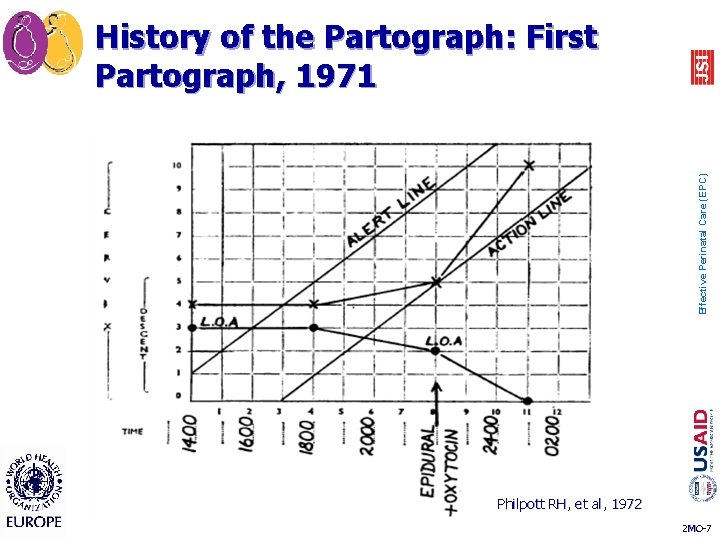
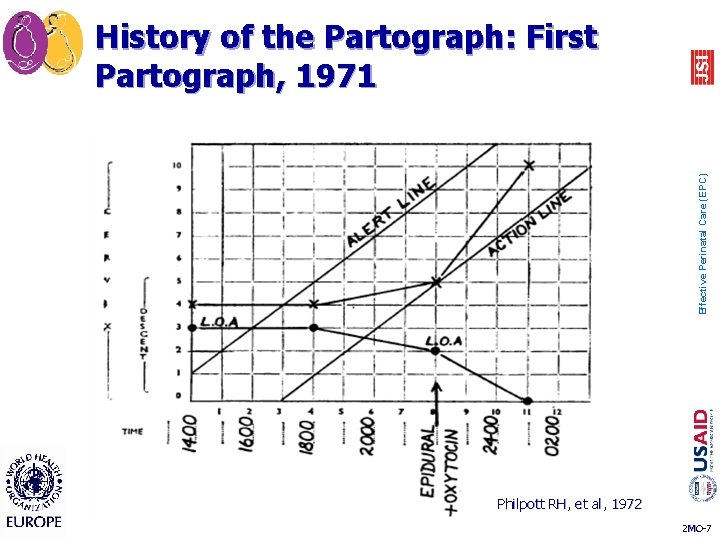
Effective Perinatal Care (EPC) History of the Partograph: First Partograph, 1971 Philpott RH, et al, 1972 2 MO-7
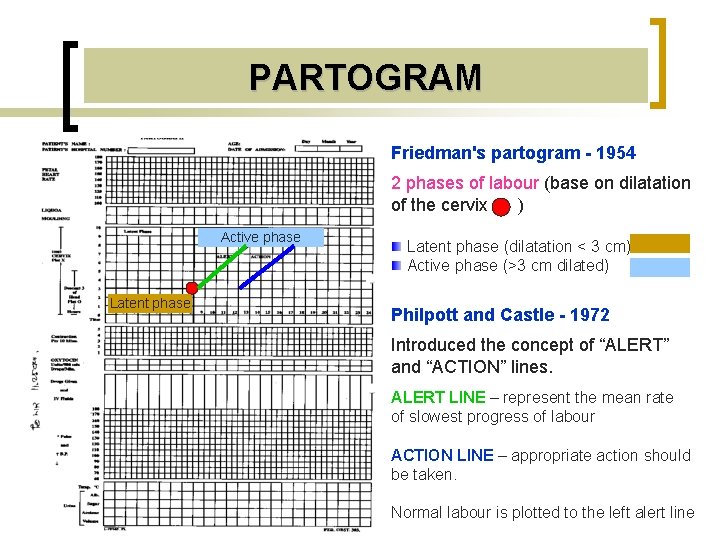
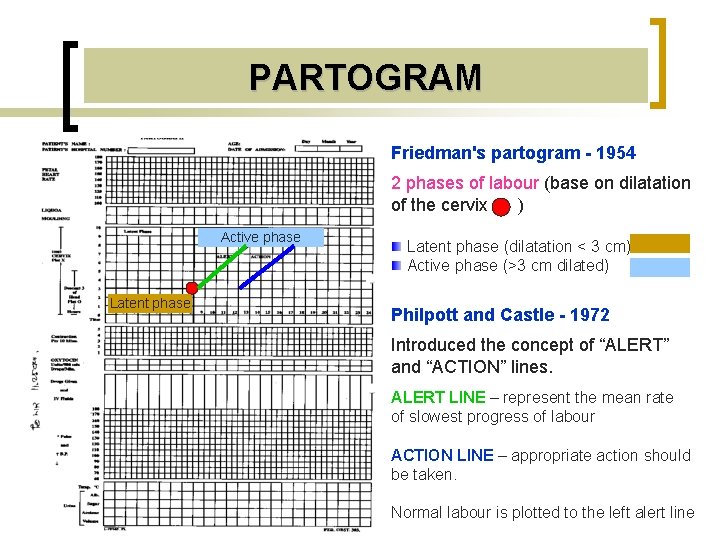
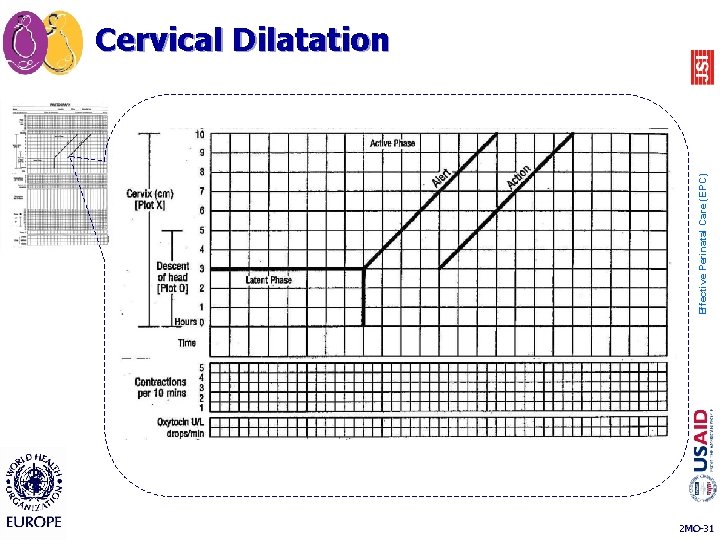
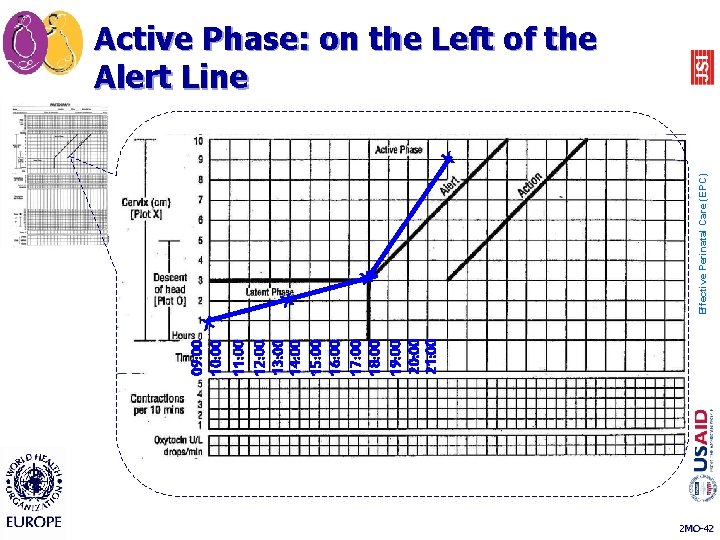
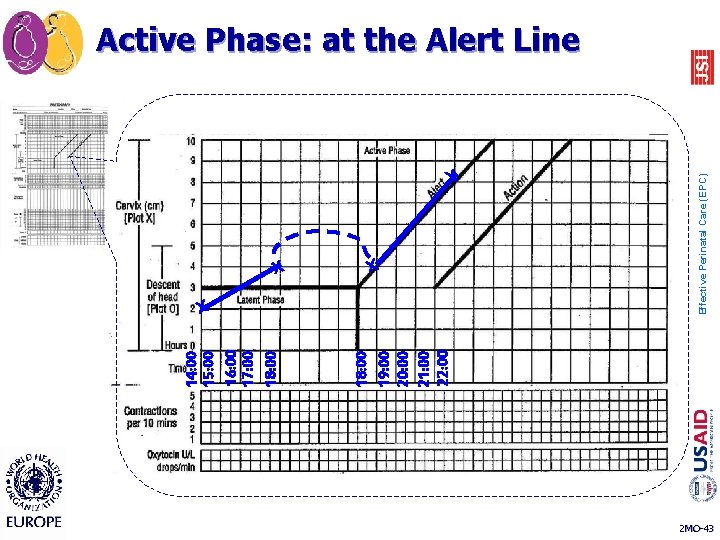
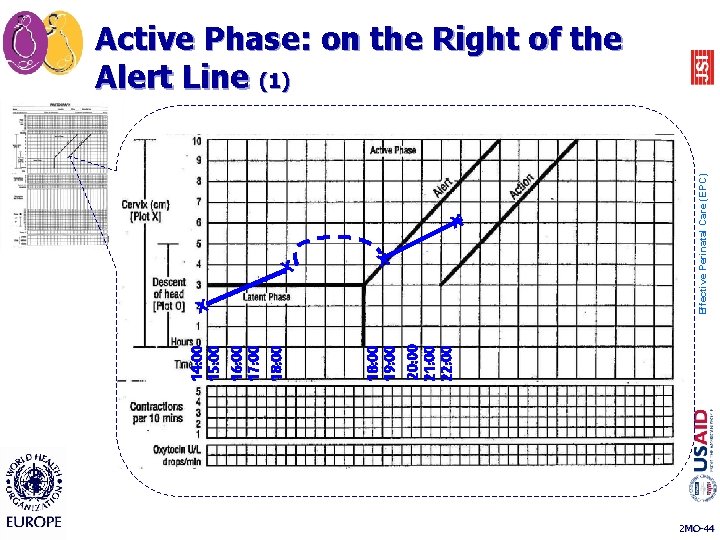
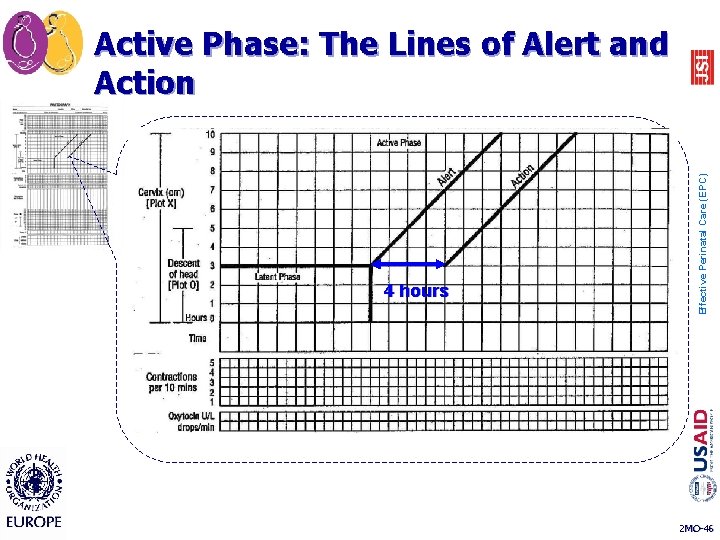
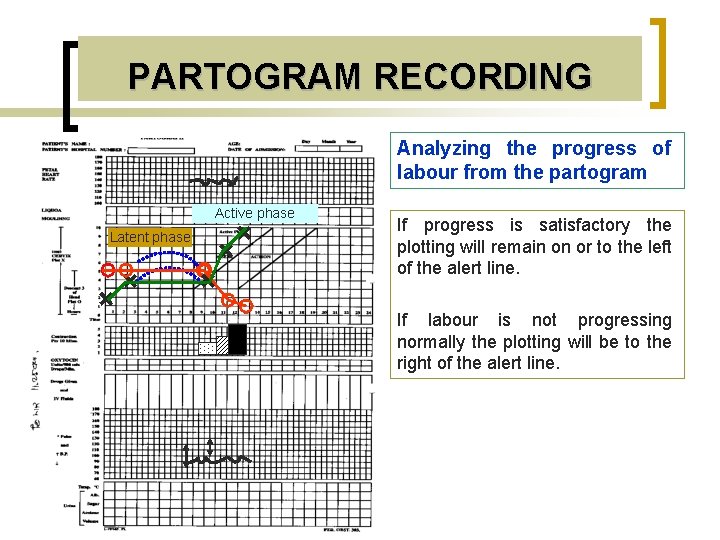
PARTOGRAM Friedman's partogram - 1954 2 phases of labour (base on dilatation of the cervix ) Active phase Latent phase (dilatation < 3 cm) Active phase (>3 cm dilated) Philpott and Castle - 1972 Introduced the concept of “ALERT” and “ACTION” lines. ALERT LINE – represent the mean rate of slowest progress of labour ACTION LINE – appropriate action should be taken. Normal labour is plotted to the left alert line
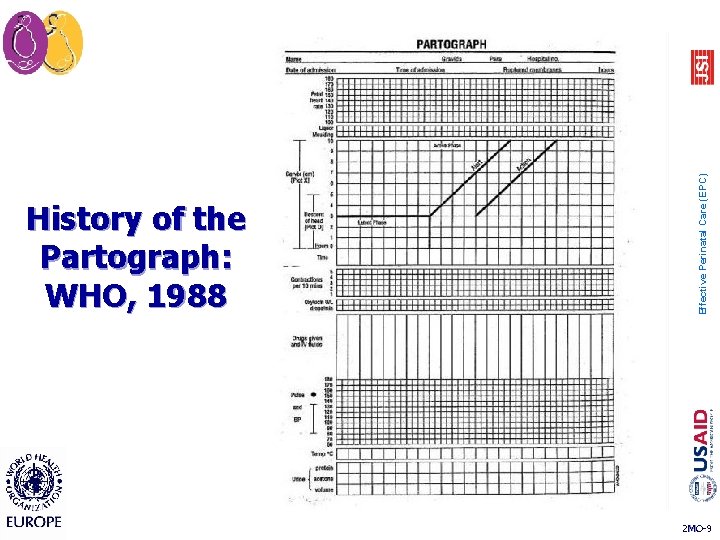
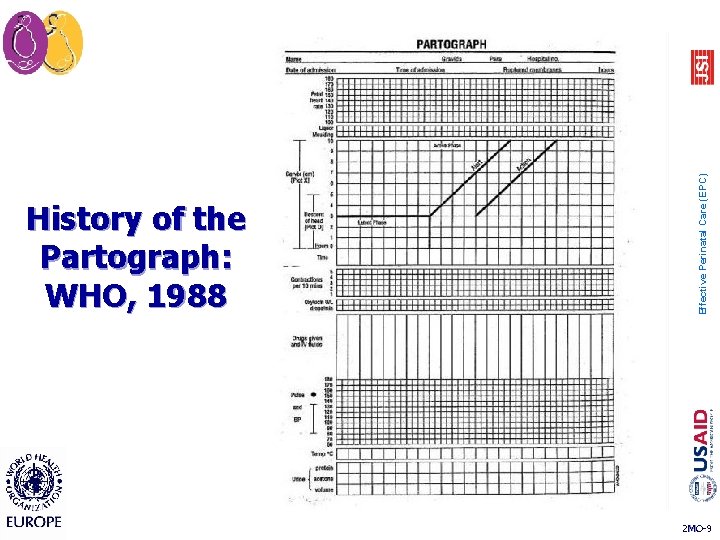
Effective Perinatal Care (EPC) History of the Partograph: WHO, 1988 2 MO-9
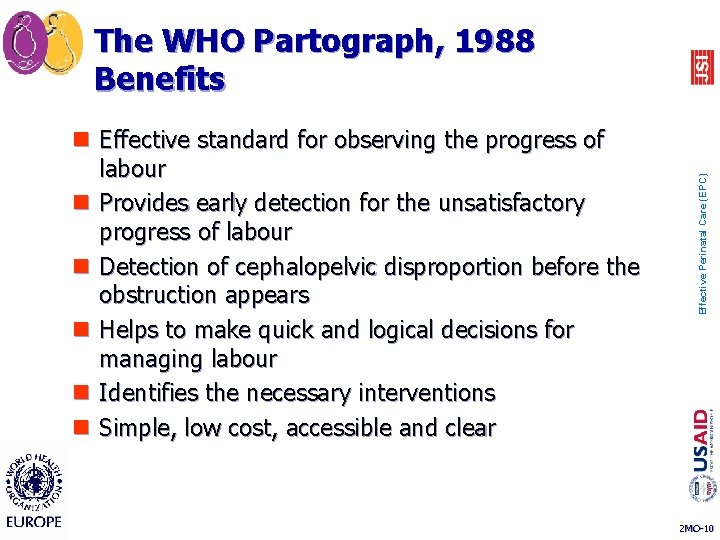
n Effective standard for observing the progress of labour n Provides early detection for the unsatisfactory progress of labour n Detection of cephalopelvic disproportion before the obstruction appears n Helps to make quick and logical decisions for managing labour n Identifies the necessary interventions n Simple, low cost, accessible and clear Effective Perinatal Care (EPC) The WHO Partograph, 1988 Benefits 2 MO-10
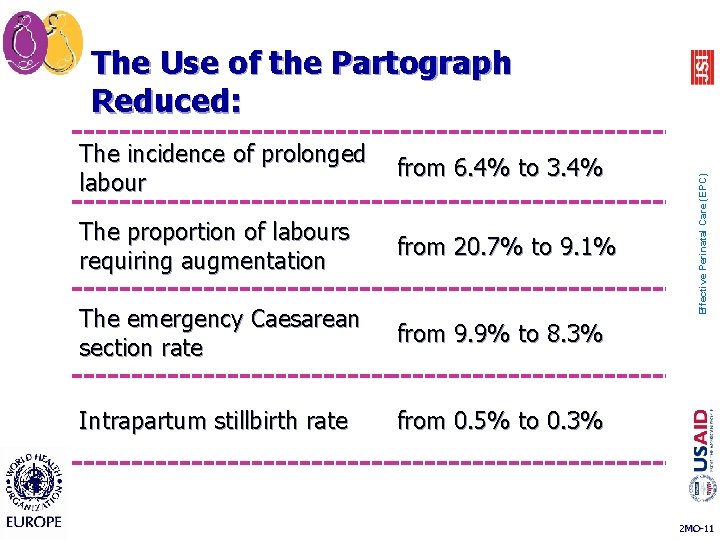
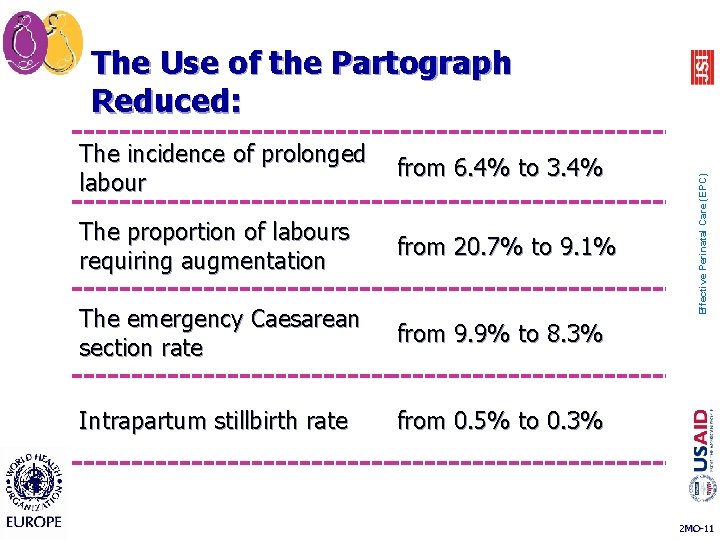
The incidence of prolonged from 6. 4% to 3. 4% labour The proportion of labours requiring augmentation from 20. 7% to 9. 1% The emergency Caesarean section rate from 9. 9% to 8. 3% Intrapartum stillbirth rate from 0. 5% to 0. 3% Effective Perinatal Care (EPC) The Use of the Partograph Reduced: 2 MO-11
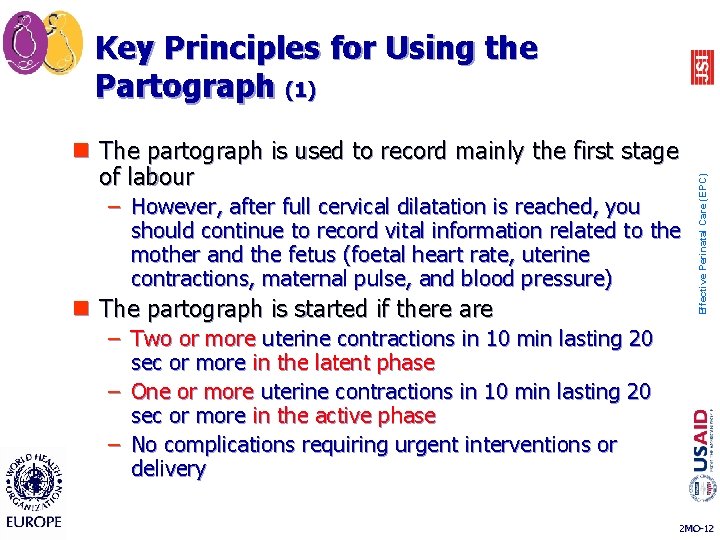
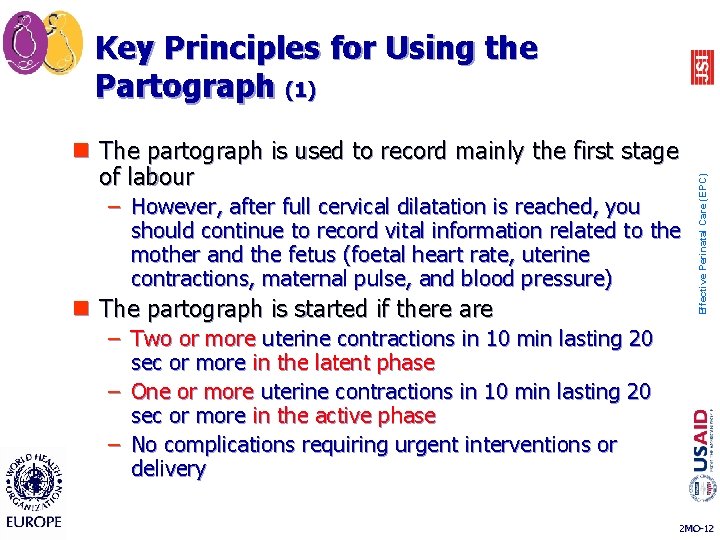
n The partograph is used to record mainly the first stage of labour – However, after full cervical dilatation is reached, you should continue to record vital information related to the mother and the fetus (foetal heart rate, uterine contractions, maternal pulse, and blood pressure) n The partograph is started if there are Effective Perinatal Care (EPC) Key Principles for Using the Partograph (1) – Two or more uterine contractions in 10 min lasting 20 sec or more in the latent phase – One or more uterine contractions in 10 min lasting 20 sec or more in the active phase – No complications requiring urgent interventions or delivery 2 MO-12
n The partograph is filled out during the labour not after birth n During labour, the partograph must be kept in the labour room n The partograph is filled in and interpreted by trained personnel (midwife or obstetrician) n Filling in the partograph should be stopped when Effective Perinatal Care (EPC) Key Principles for Using the Partograph (2) – Complications requiring urgent delivery arise 2 MO-13
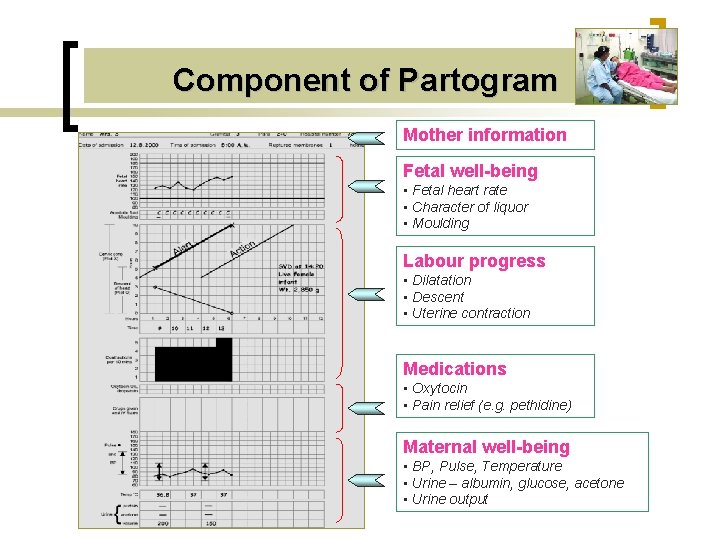
Component of Partogram Mother information Fetal well-being • Fetal heart rate • Character of liquor • Moulding Labour progress • Dilatation • Descent • Uterine contraction Medications • Oxytocin • Pain relief (e. g. pethidine) Maternal well-being • BP, Pulse, Temperature • Urine – albumin, glucose, acetone • Urine output
PARTOGRAM WHAT NEED TO BE RECORDED
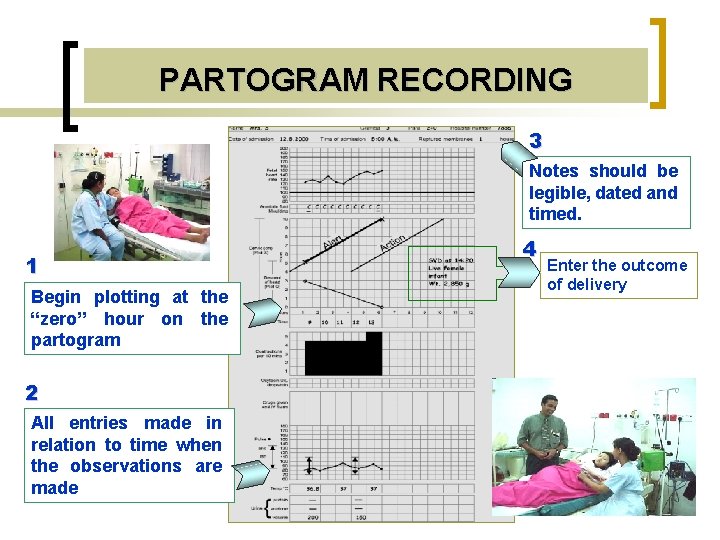
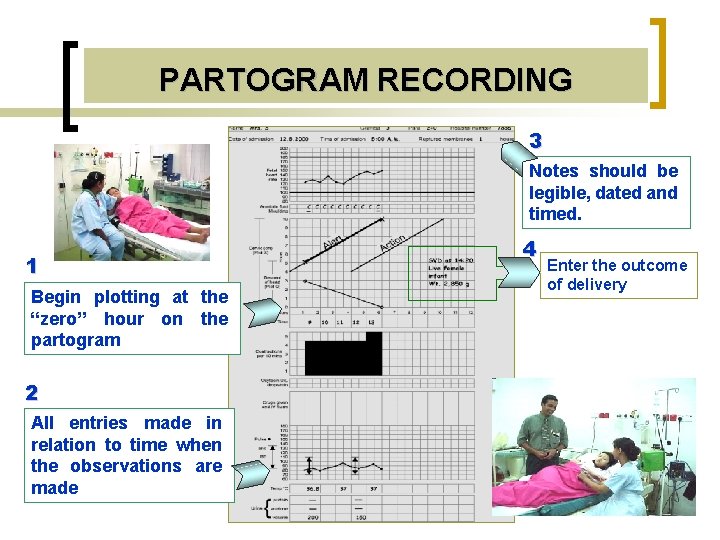
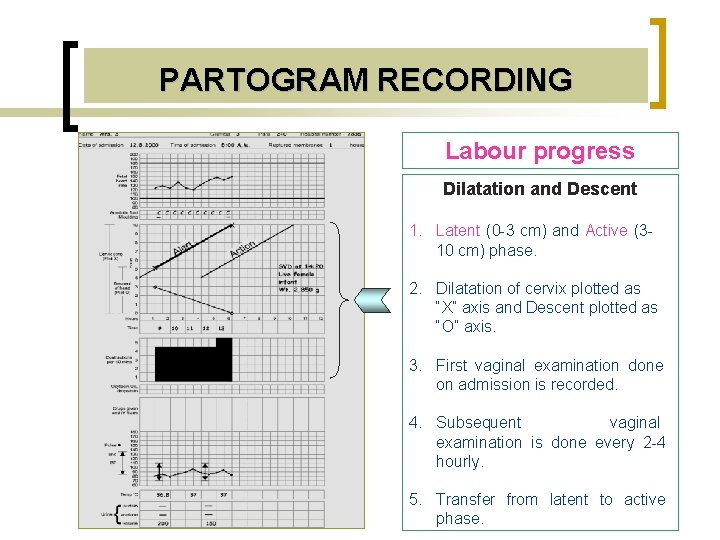
PARTOGRAM RECORDING 3 Notes should be legible, dated and timed. 1 Begin plotting at the “zero” hour on the partogram 2 All entries made in relation to time when the observations are made 4 Enter the outcome of delivery
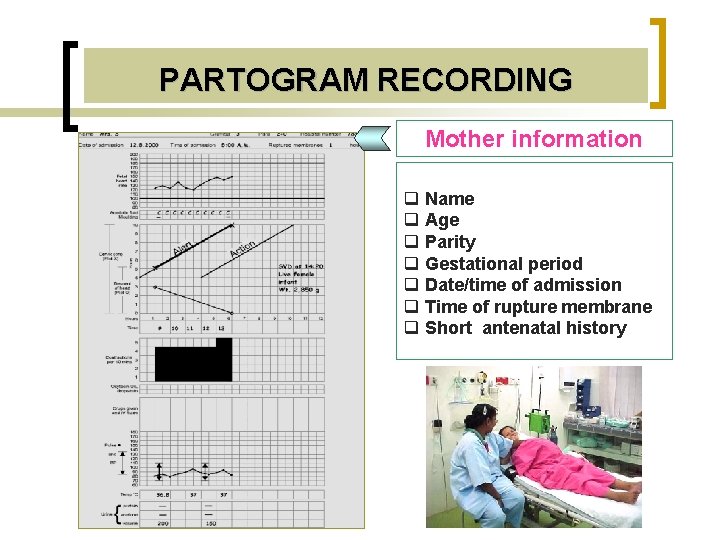
PARTOGRAM RECORDING Mother information q Name q Age q Parity q Gestational period q Date/time of admission q Time of rupture membrane q Short antenatal history
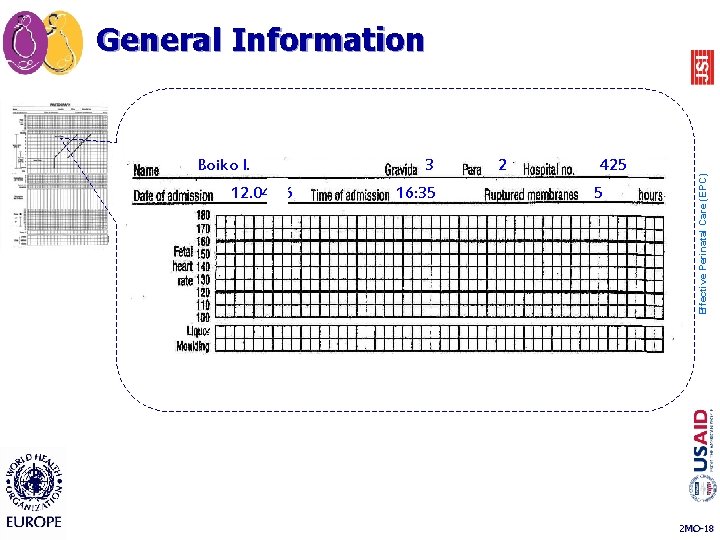
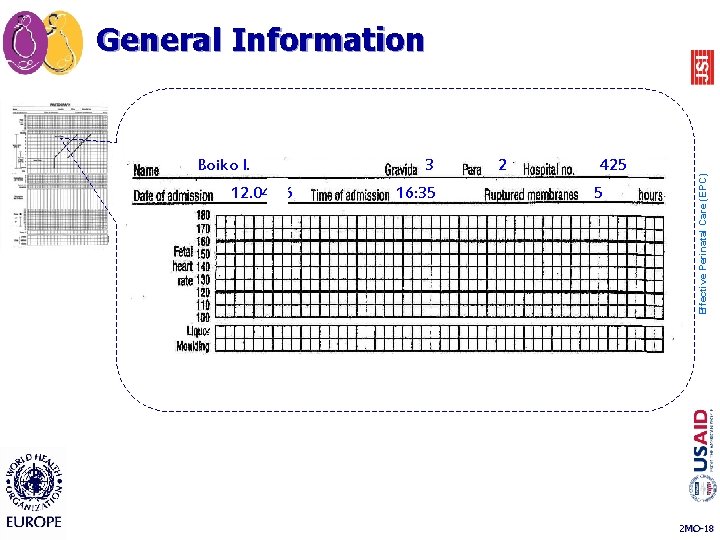
Boiko I. 12. 04. 06 3 16: 35 2 425 5 Effective Perinatal Care (EPC) General Information 2 MO-18
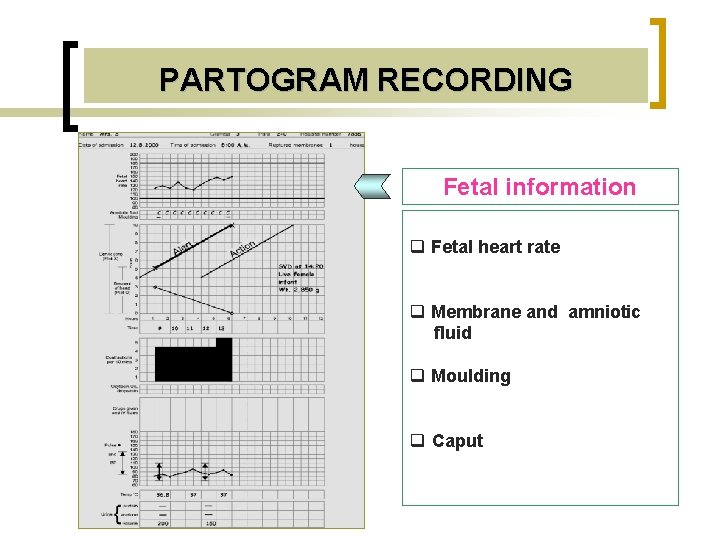
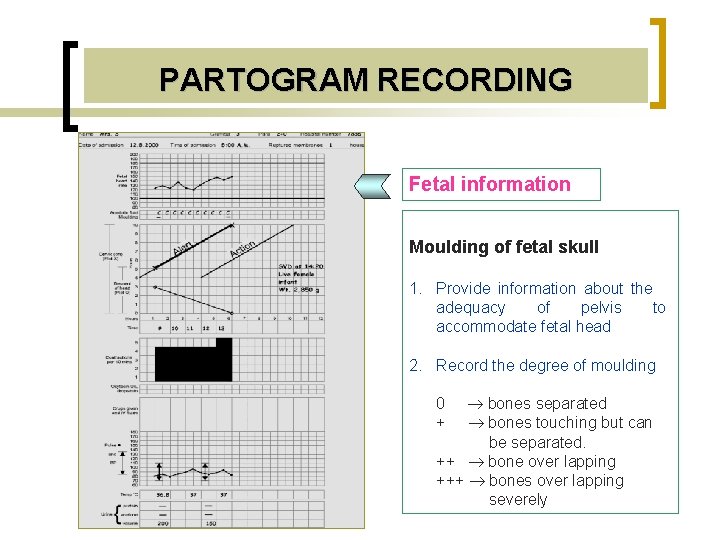
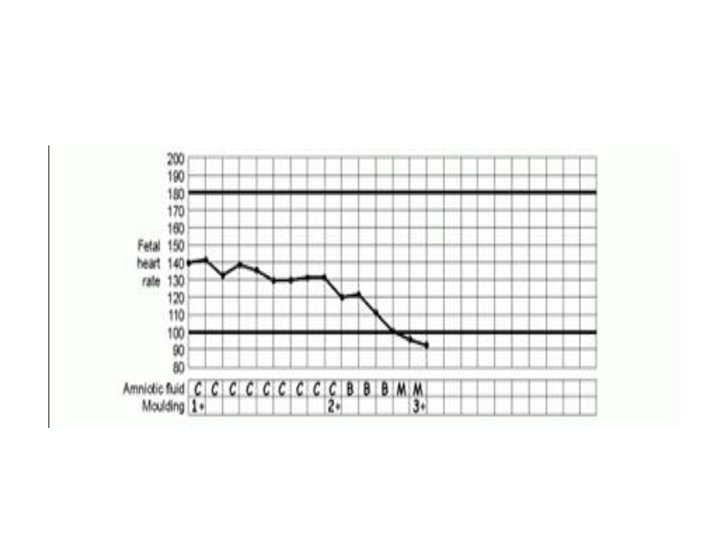
PARTOGRAM RECORDING Fetal information q Fetal heart rate q Membrane and amniotic fluid q Moulding q Caput
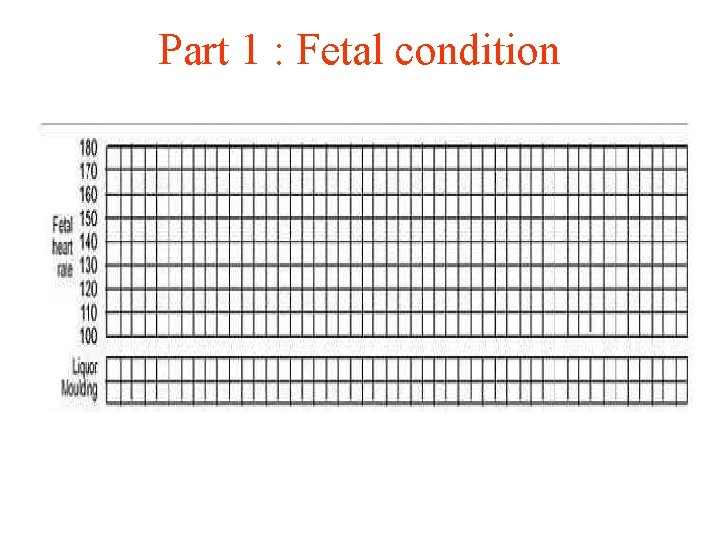
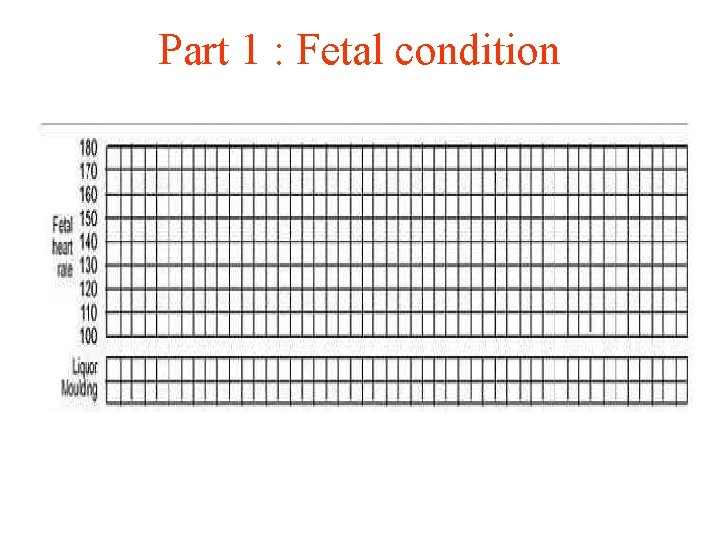
Part 1 : Fetal condition
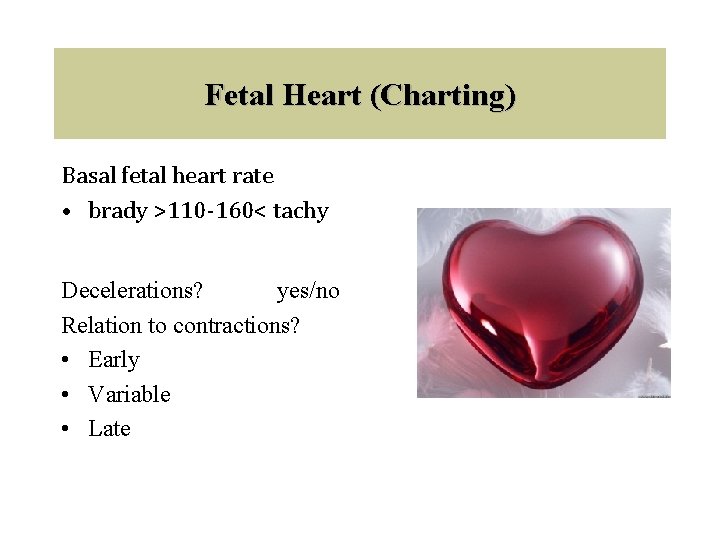
Fetal Heart (Charting) Basal fetal heart rate • brady >110 -160< tachy Decelerations? yes/no Relation to contractions? • Early • Variable • Late
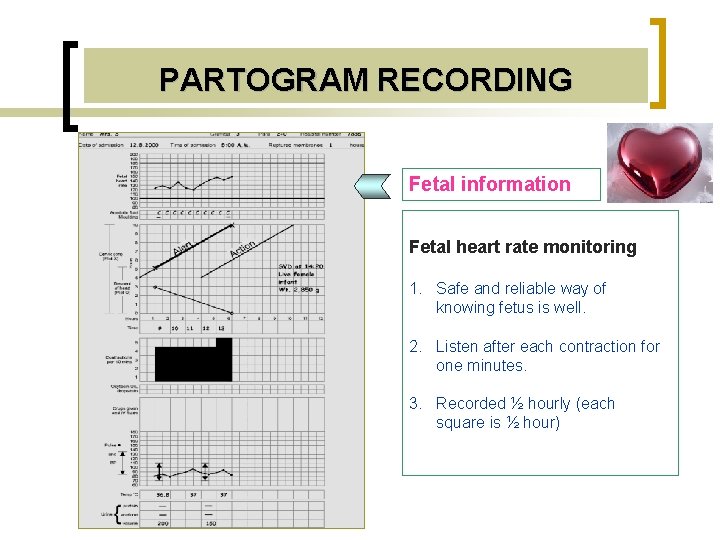
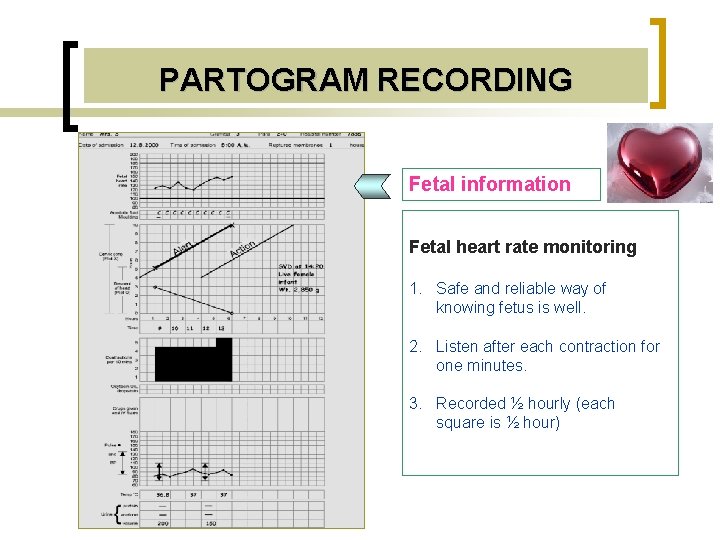
PARTOGRAM RECORDING Fetal information Fetal heart rate monitoring 1. Safe and reliable way of knowing fetus is well. 2. Listen after each contraction for one minutes. 3. Recorded ½ hourly (each square is ½ hour)
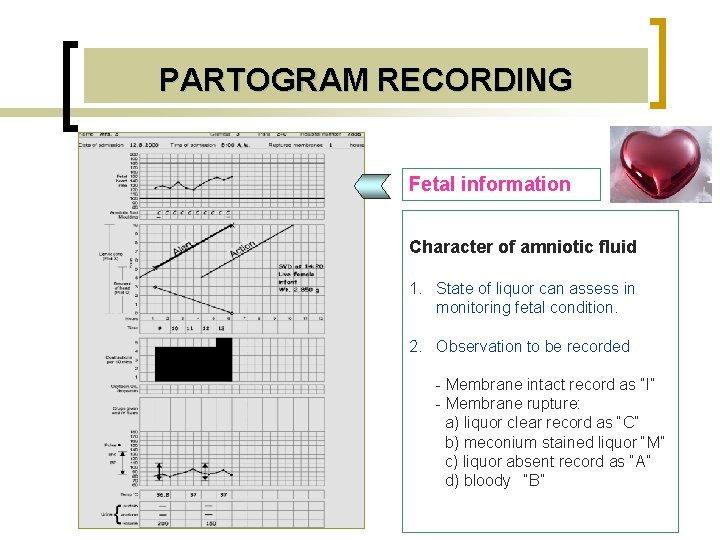
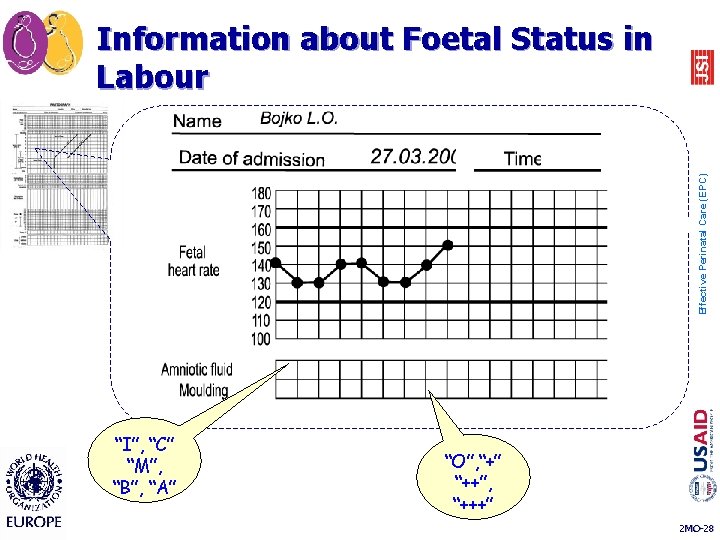
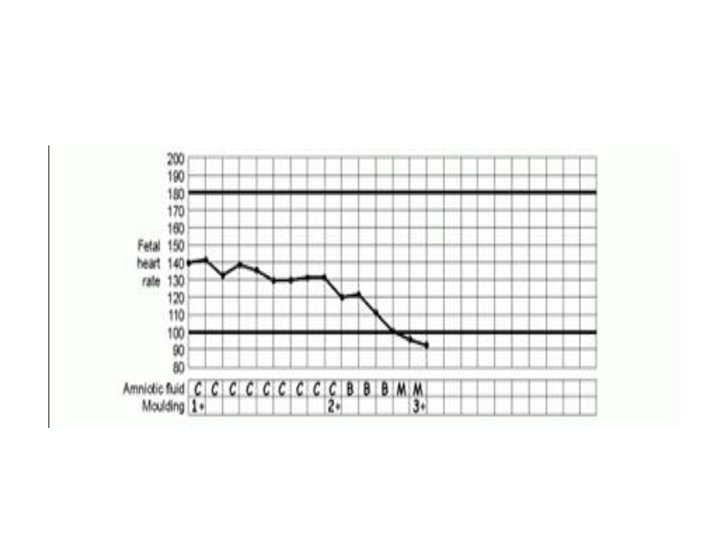
PARTOGRAM RECORDING Fetal information Character of amniotic fluid 1. State of liquor can assess in monitoring fetal condition. 2. Observation to be recorded - Membrane intact record as “I” - Membrane rupture: a) liquor clear record as “C” b) meconium stained liquor “M” c) liquor absent record as “A” d) bloody “B”
n I – the membranes intact n C – clear amniotic fluid n В – blood-stained amniotic fluid Effective Perinatal Care (EPC) Amniotic Fluid n M – meconium-stained amniotic fluid n A – absent amniotic fluid 2 MO-24
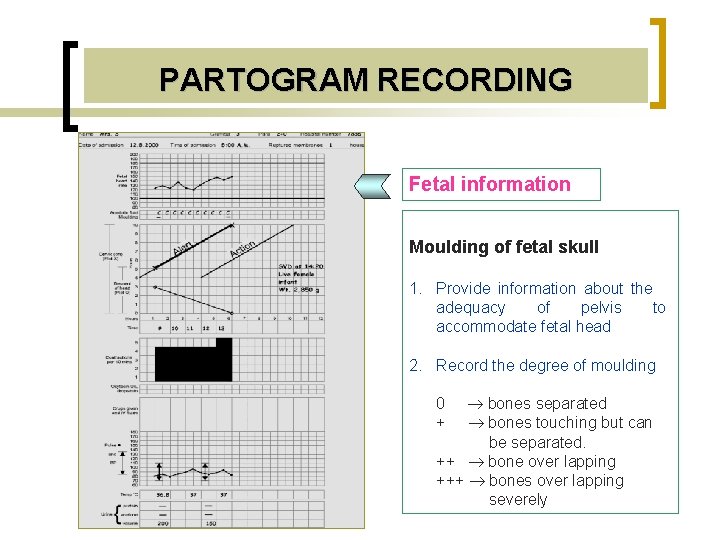
PARTOGRAM RECORDING Fetal information Moulding of fetal skull 1. Provide information about the adequacy of pelvis to accommodate fetal head 2. Record the degree of moulding bones separated bones touching but can be separated. ++ bone over lapping +++ bones over lapping severely 0 +
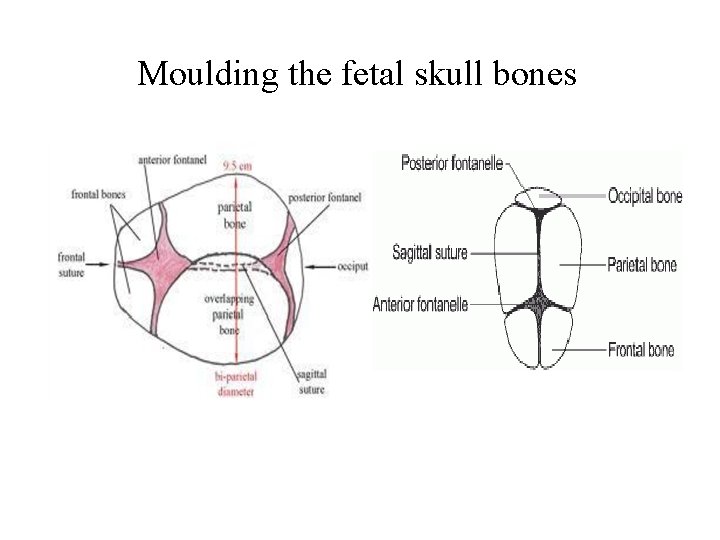
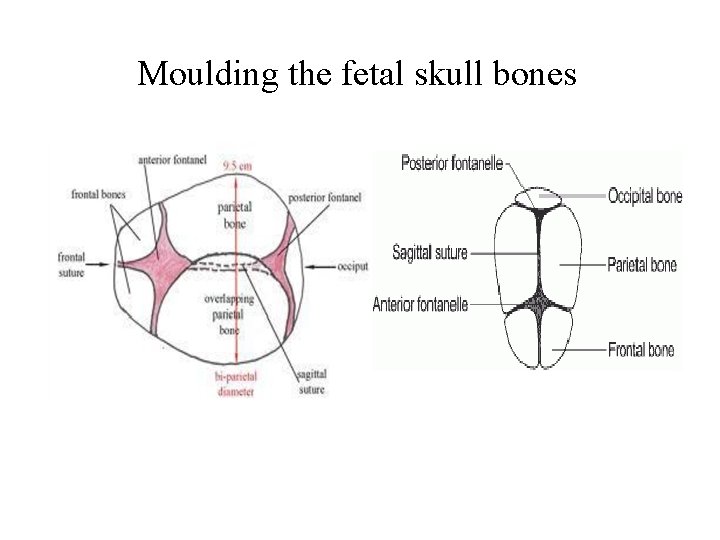
Moulding the fetal skull bones
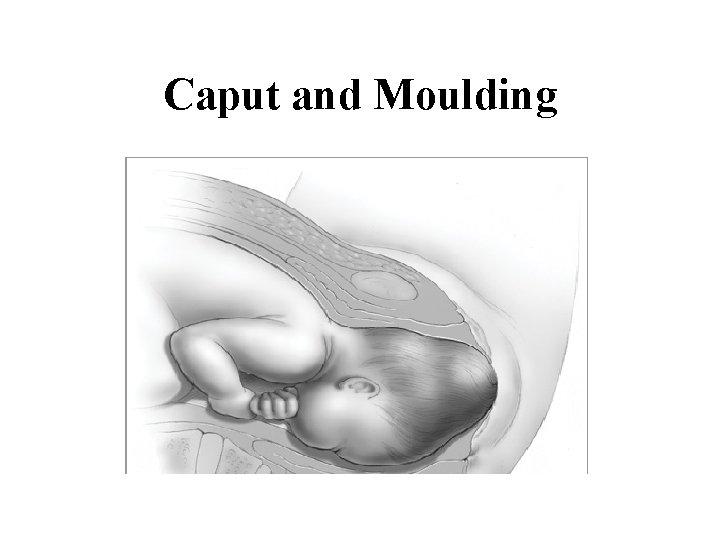
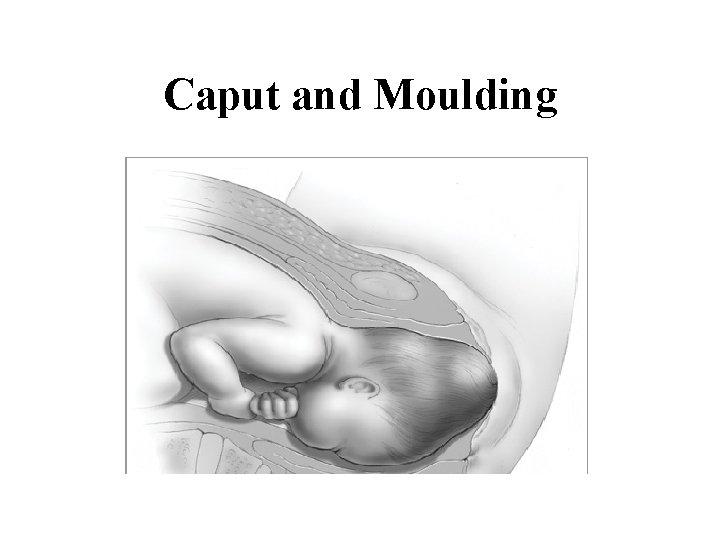
Caput and Moulding
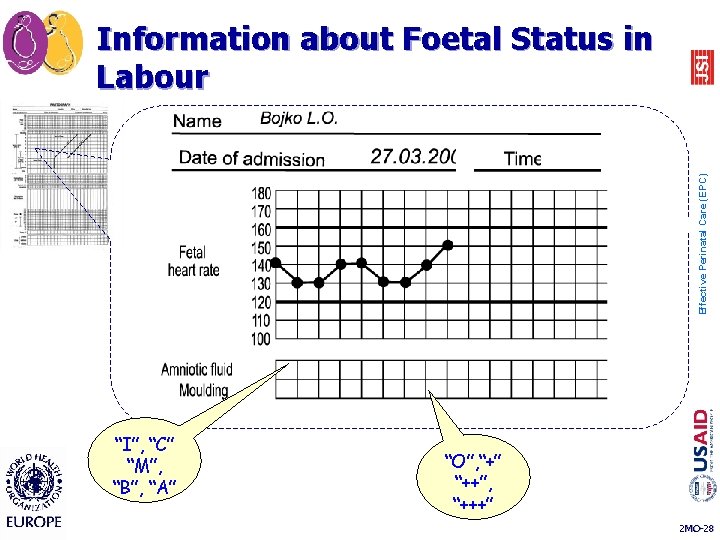
Effective Perinatal Care (EPC) Information about Foetal Status in Labour “I”, “C” “M”, “B”, “A” “O”, “+” “++”, “+++” 2 MO-28
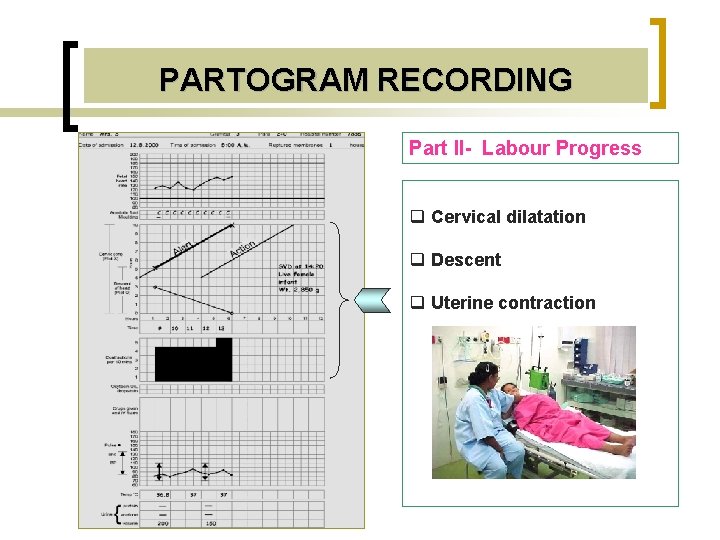
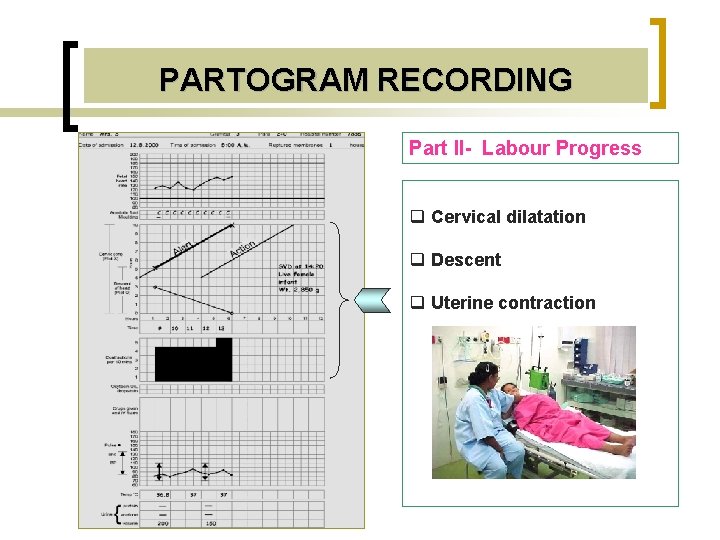
PARTOGRAM RECORDING Part II- Labour Progress q Cervical dilatation q Descent q Uterine contraction
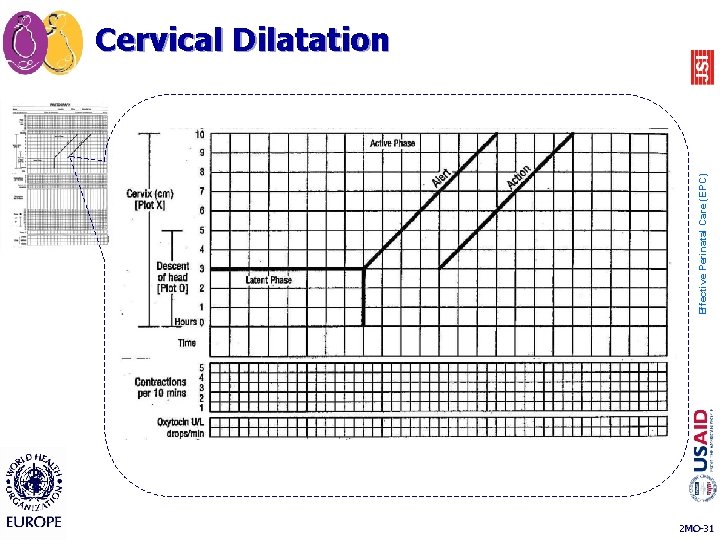
Effective Perinatal Care (EPC) Cervical Dilatation 2 MO-31
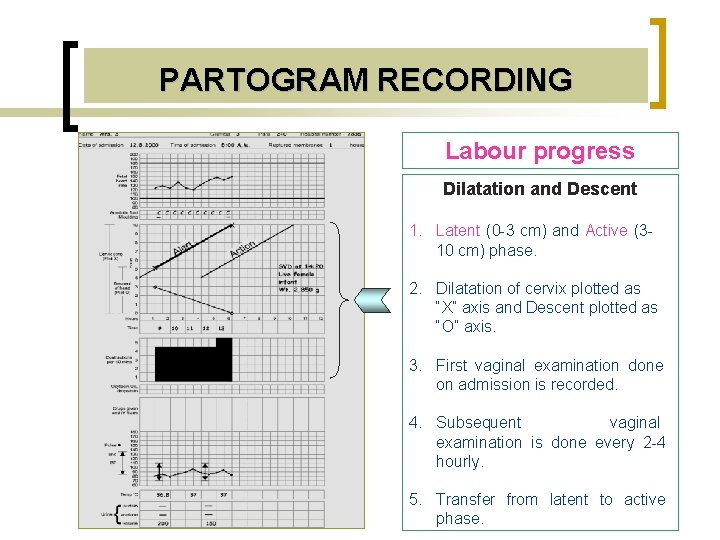
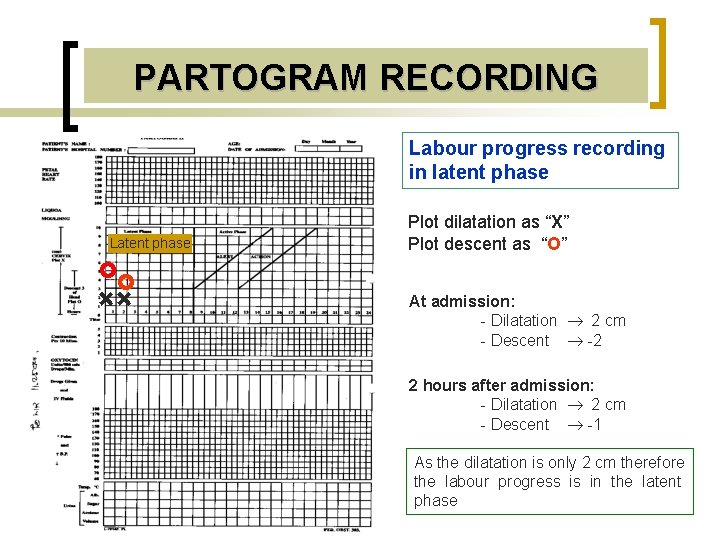
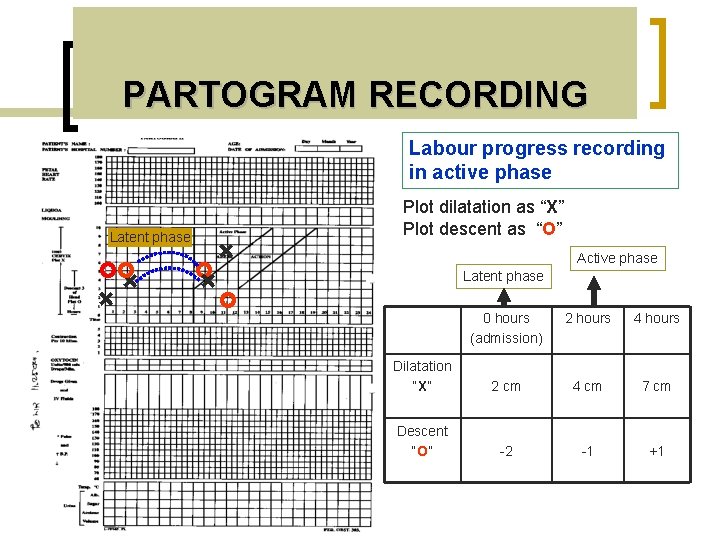
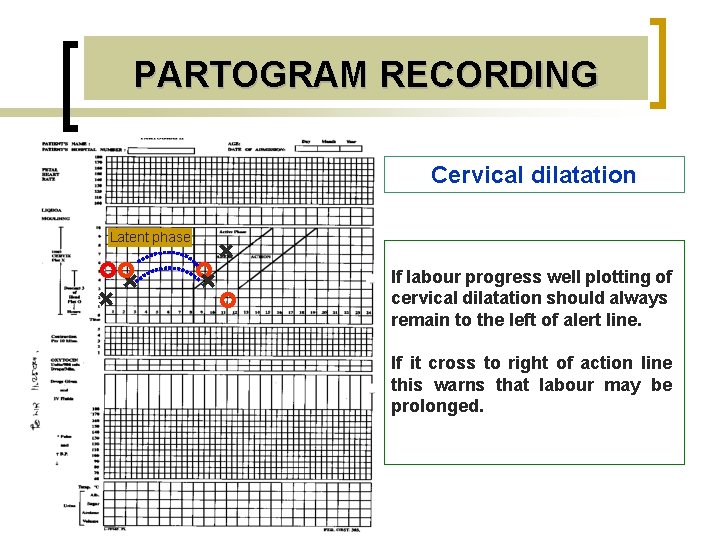
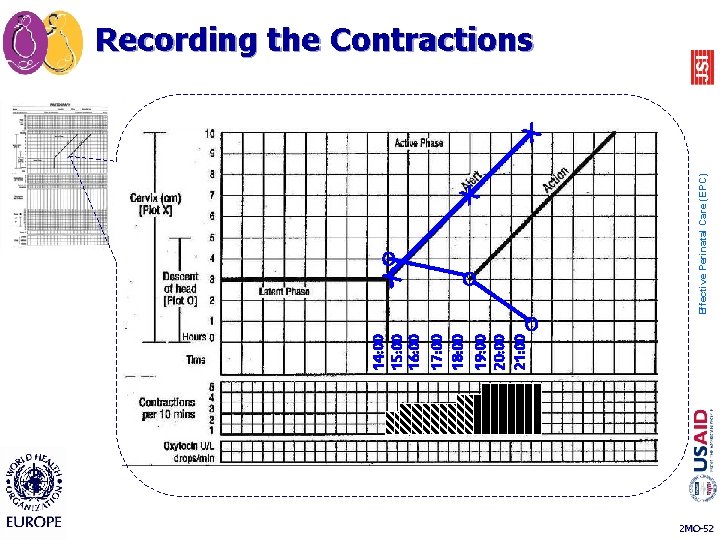
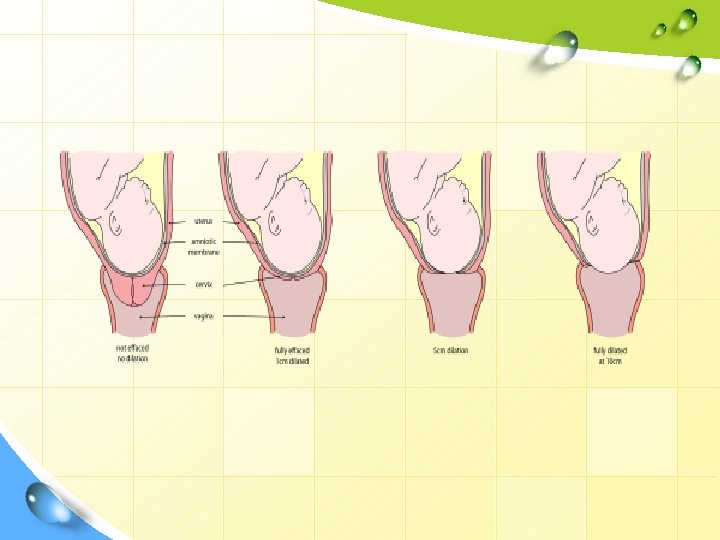
PARTOGRAM RECORDING Labour progress Dilatation and Descent 1. Latent (0 -3 cm) and Active (310 cm) phase. 2. Dilatation of cervix plotted as “X” axis and Descent plotted as “O” axis. 3. First vaginal examination done on admission is recorded. 4. Subsequent vaginal examination is done every 2 -4 hourly. 5. Transfer from latent to active phase.
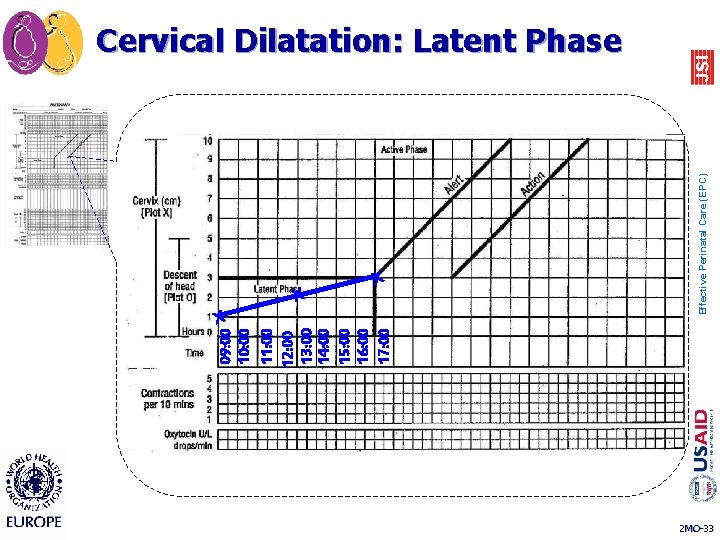
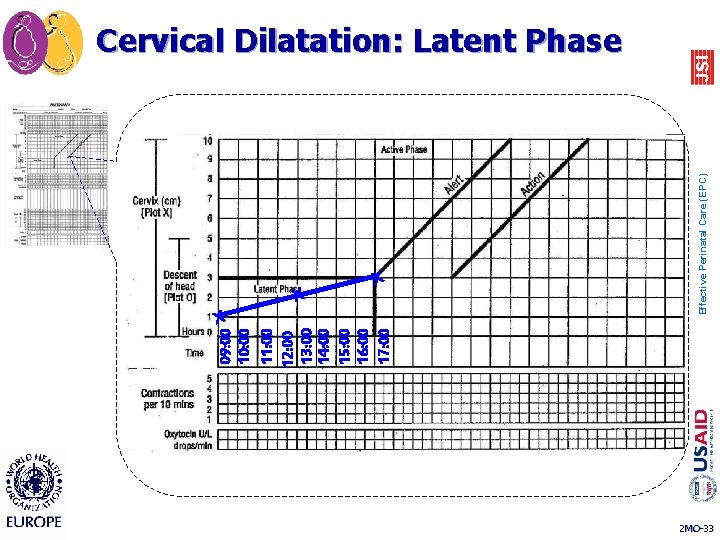
X X Effective Perinatal Care (EPC) X 09: 00 10: 00 11: 00 12: 00 13: 00 14: 00 15: 00 16: 00 17: 00 Cervical Dilatation: Latent Phase 2 MO-33
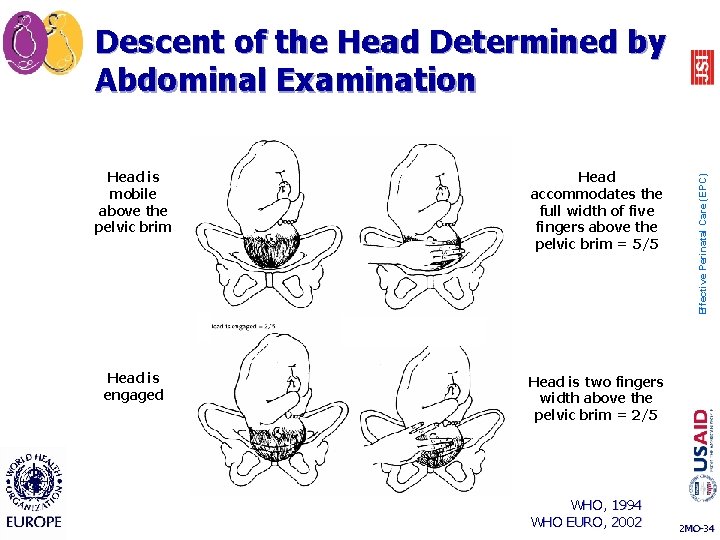
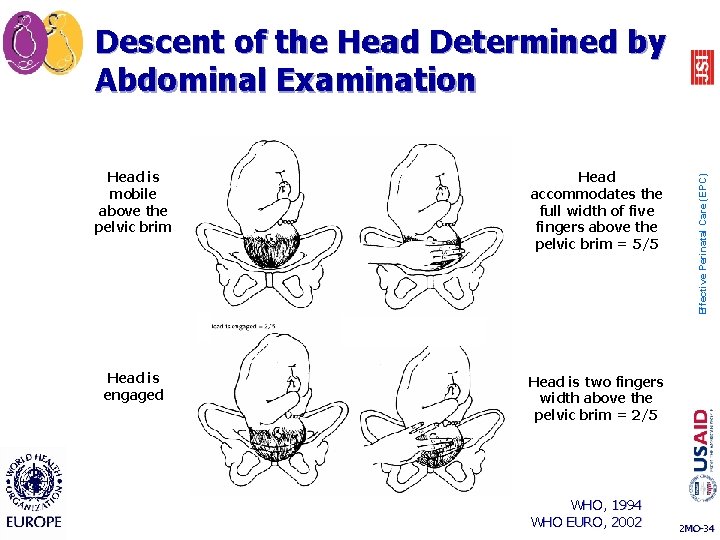
Head is mobile above the pelvic brim Head accommodates the full width of five fingers above the pelvic brim = 5/5 Head is engaged Head is two fingers width above the pelvic brim = 2/5 WHO, 1994 WHO EURO, 2002 Effective Perinatal Care (EPC) Descent of the Head Determined by Abdominal Examination 2 MO-34
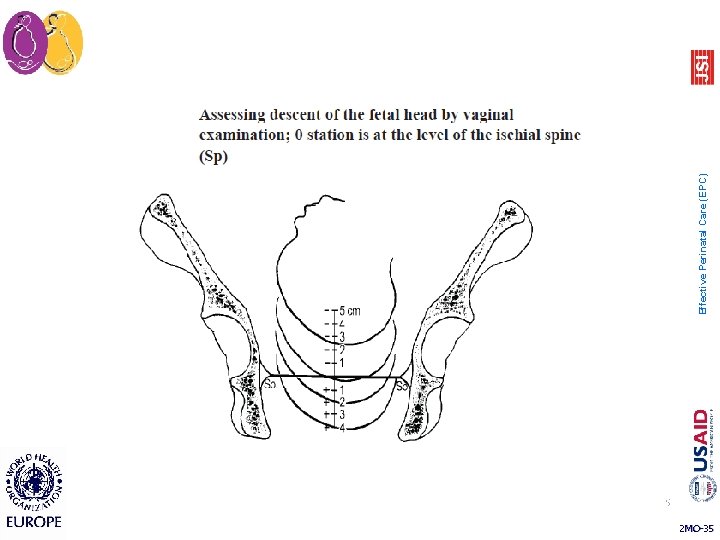
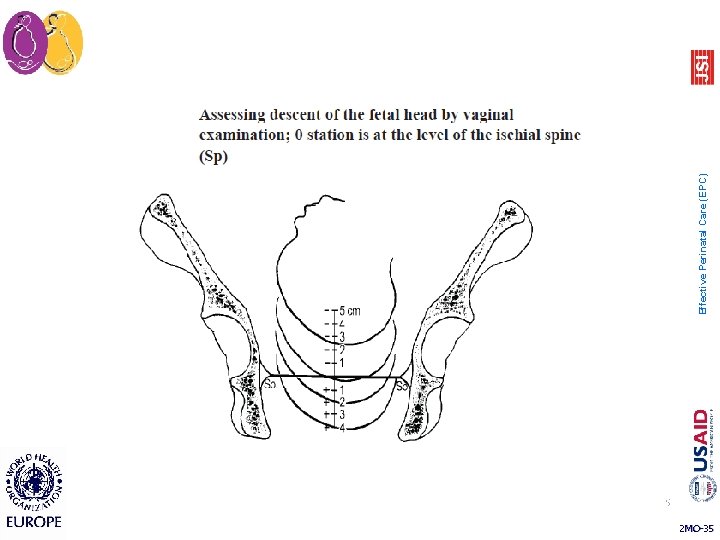
35 2 MO-35 Effective Perinatal Care (EPC)
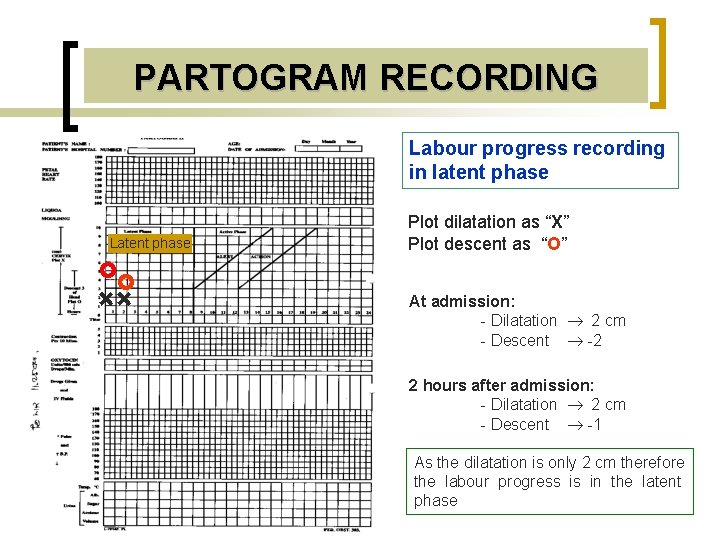
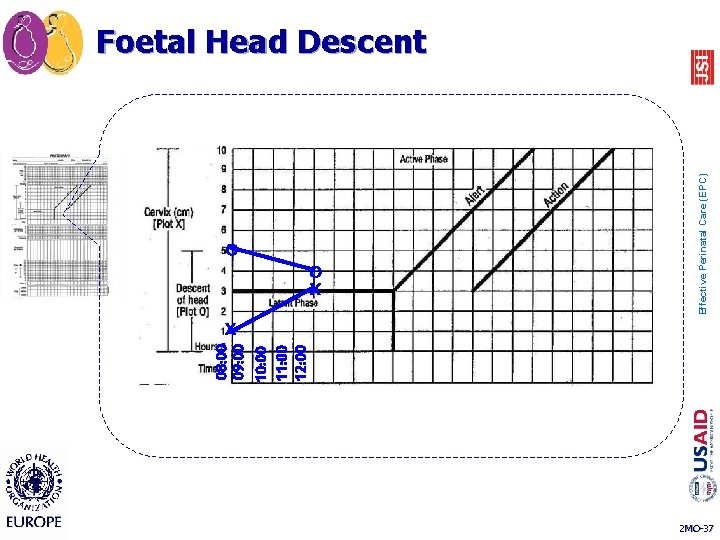
PARTOGRAM RECORDING Labour progress recording in latent phase Latent phase Plot dilatation as “X” Plot descent as “O” + + At admission: - Dilatation 2 cm - Descent -2 2 hours after admission: - Dilatation 2 cm - Descent -1 As the dilatation is only 2 cm therefore the labour progress is in the latent phase
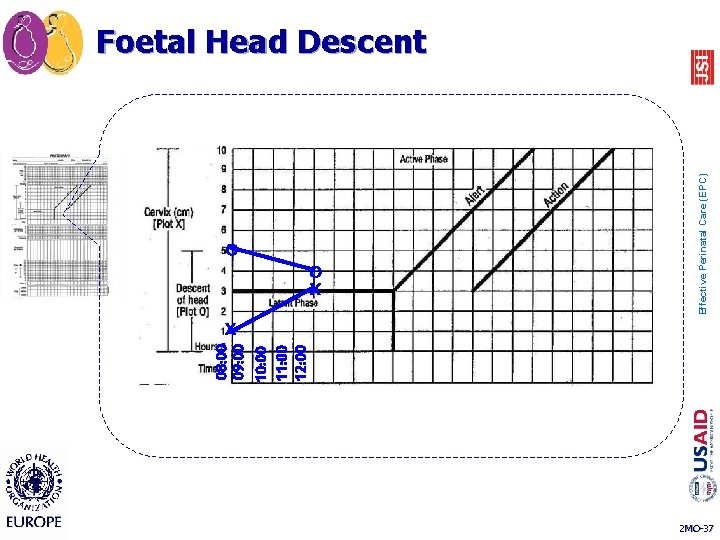
08: 00 09: 00 10: 00 11: 00 12: 00 O O X Effective Perinatal Care (EPC) Foetal Head Descent X 2 MO-37
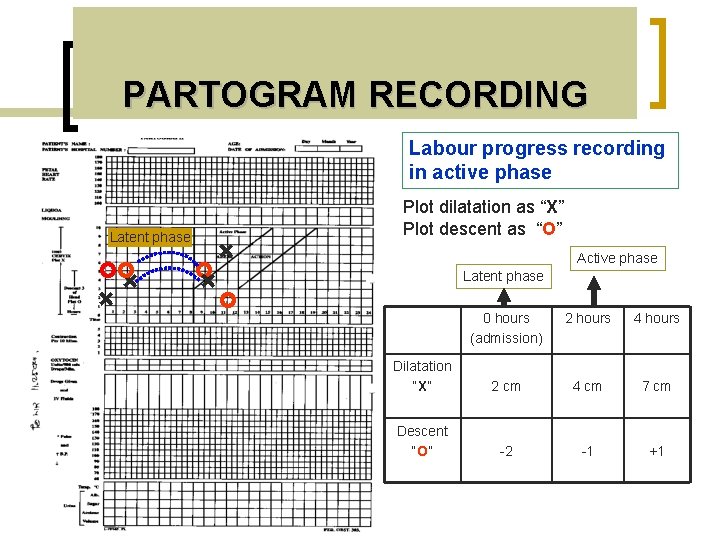
PARTOGRAM RECORDING Labour progress recording in active phase Plot dilatation as “X” Plot descent as “O” Latent phase + Active phase + + Latent phase + 0 hours (admission) 2 hours 4 hours Dilatation “X” 2 cm 4 cm 7 cm Descent “O” -2 -1 +1
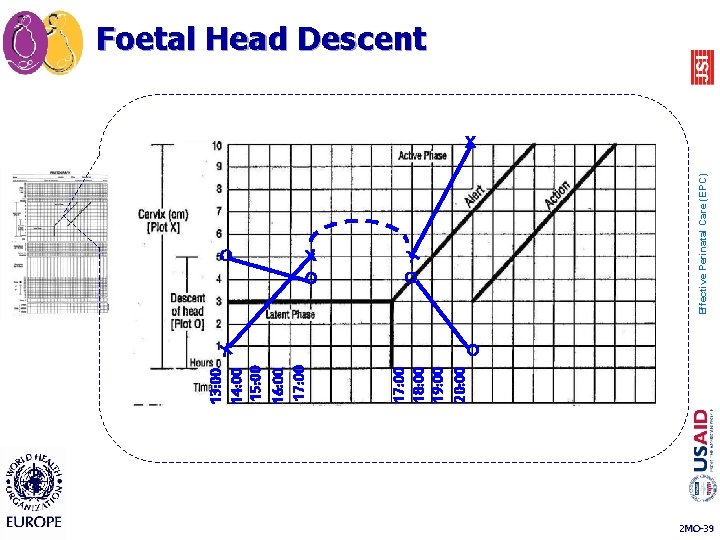
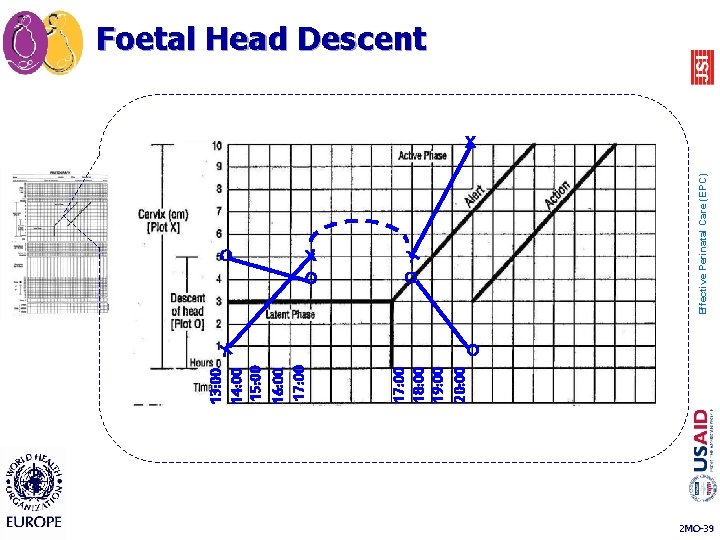
O X 17: 00 18: 00 19: 00 20: 00 13: 00 14: 00 15: 00 16: 00 17: 00 X O Effective Perinatal Care (EPC) Foetal Head Descent X O 2 MO-39
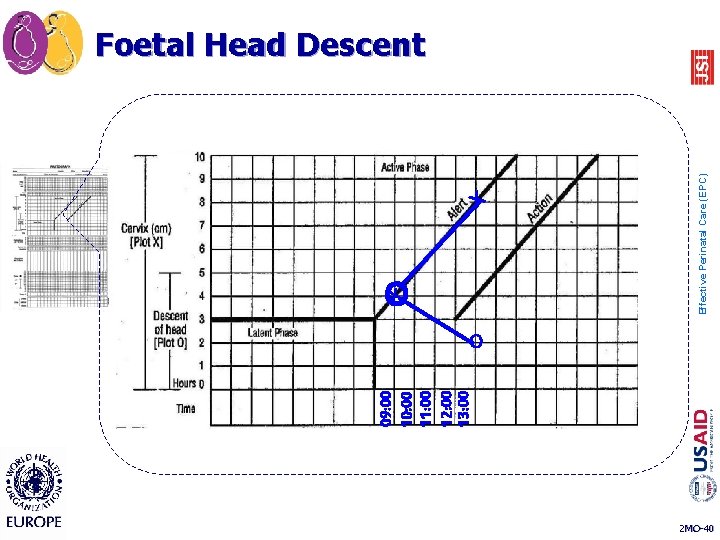
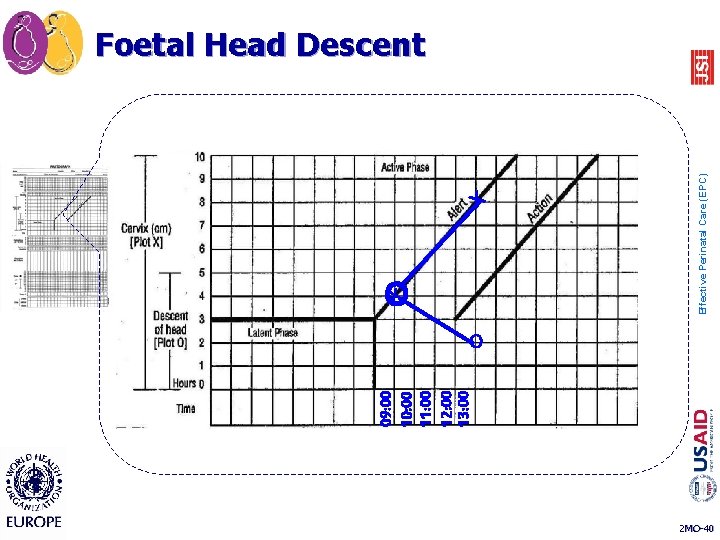
09: 00 10: 00 11: 00 12: 00 13: 00 X OX Effective Perinatal Care (EPC) Foetal Head Descent O 2 MO-40
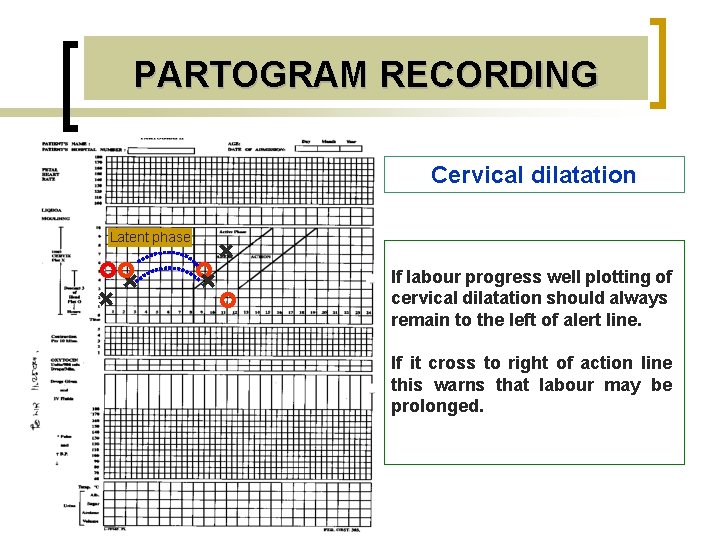
PARTOGRAM RECORDING Cervical dilatation Latent phase + + If labour progress well plotting of cervical dilatation should always remain to the left of alert line. If it cross to right of action line this warns that labour may be prolonged.
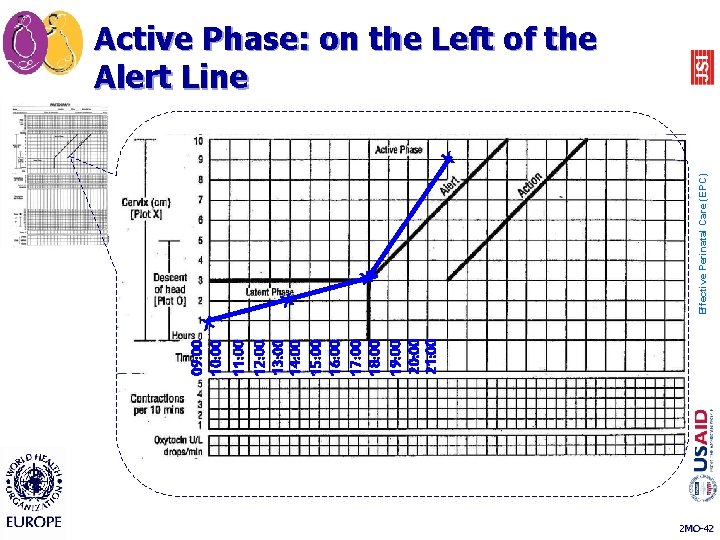
09: 00 10: 00 11: 00 12: 00 13: 00 14: 00 15: 00 16: 00 17: 00 18: 00 19: 00 20: 00 21: 00 X X Effective Perinatal Care (EPC) Active Phase: on the Left of the Alert Line X X 2 MO-42
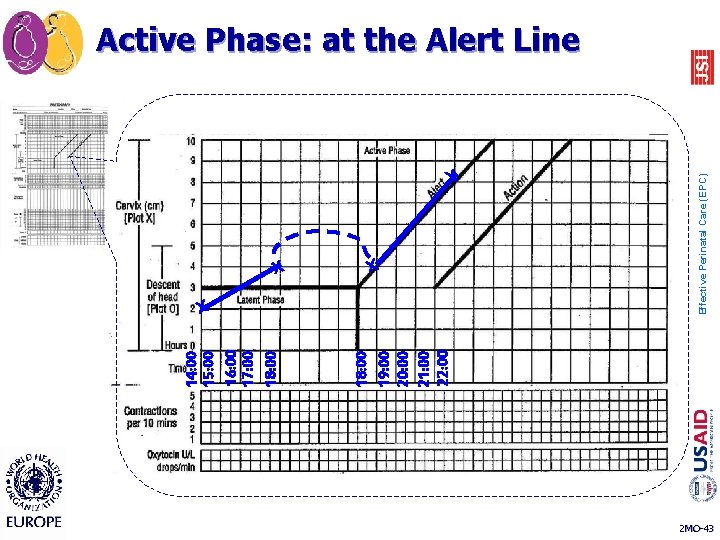
X 18: 00 19: 00 20: 00 21: 00 22: 00 14: 00 15: 00 16: 00 17: 00 18: 00 X X X Effective Perinatal Care (EPC) Active Phase: at the Alert Line 2 MO-43
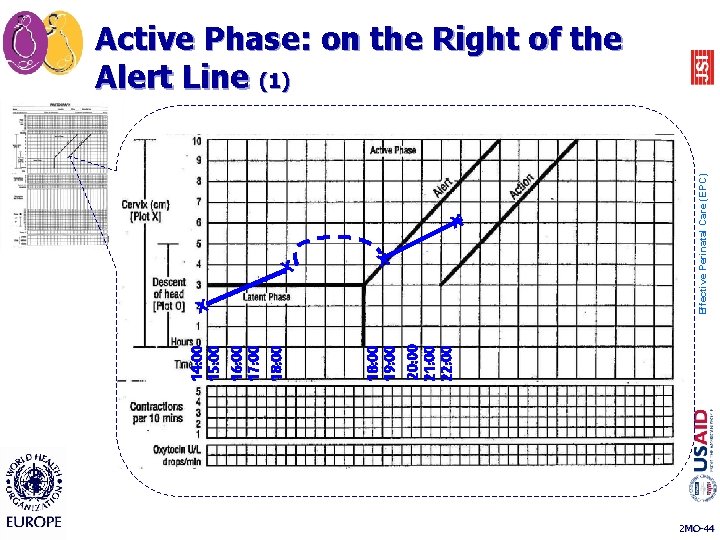
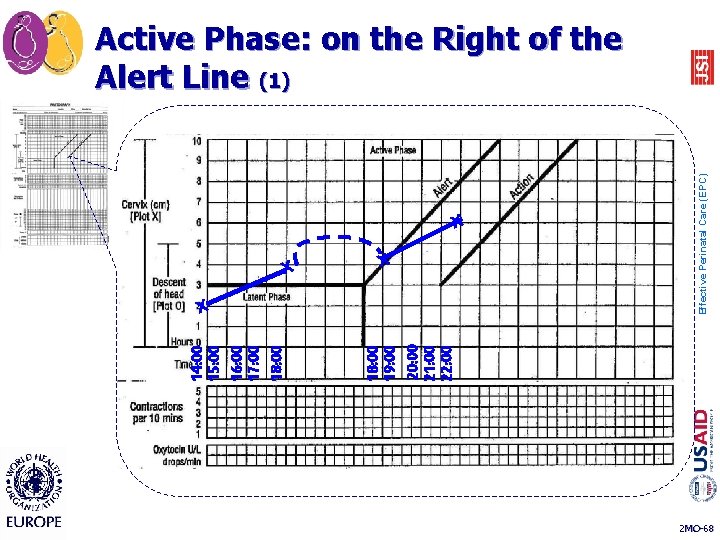
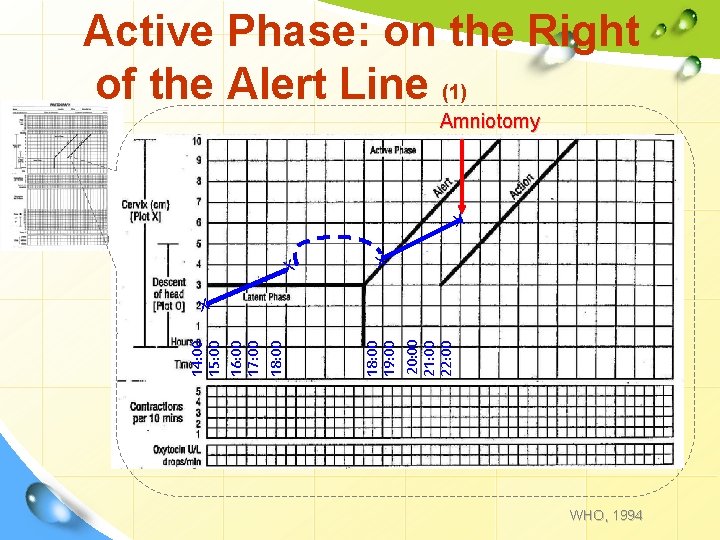
X 18: 00 19: 00 20: 00 21: 00 22: 00 14: 00 15: 00 16: 00 17: 00 18: 00 X X X Effective Perinatal Care (EPC) Active Phase: on the Right of the Alert Line (1) 2 MO-44
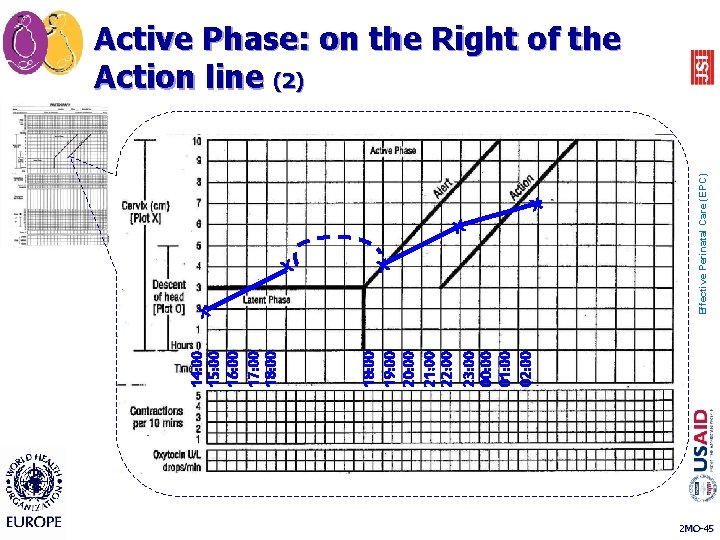
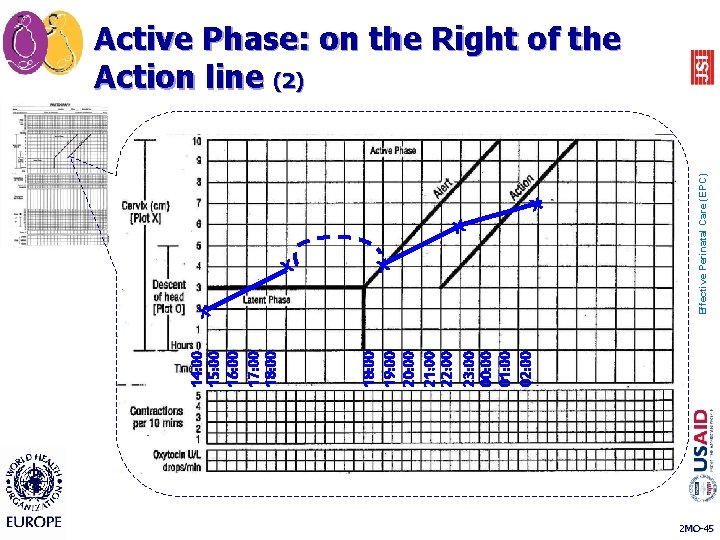
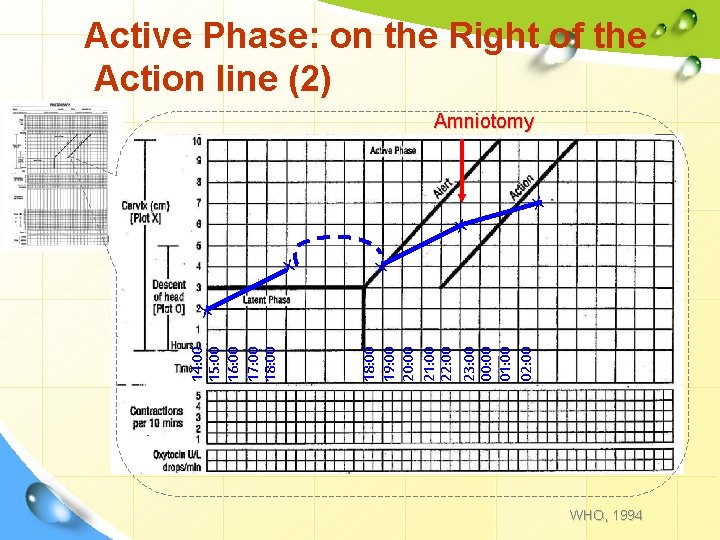
X 18: 00 19: 00 20: 00 21: 00 22: 00 23: 00 00: 00 01: 00 02: 00 14: 00 15: 00 16: 00 17: 00 18: 00 X X Effective Perinatal Care (EPC) Active Phase: on the Right of the Action line (2) 2 MO-45
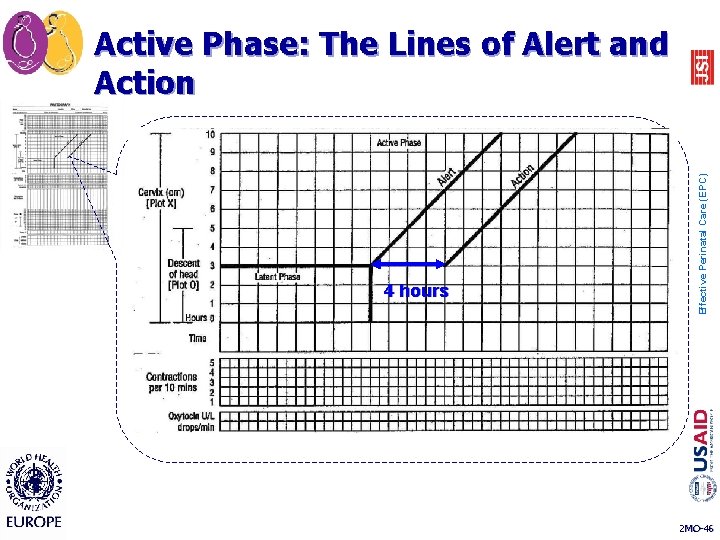
4 hours Effective Perinatal Care (EPC) Active Phase: The Lines of Alert and Action 2 MO-46
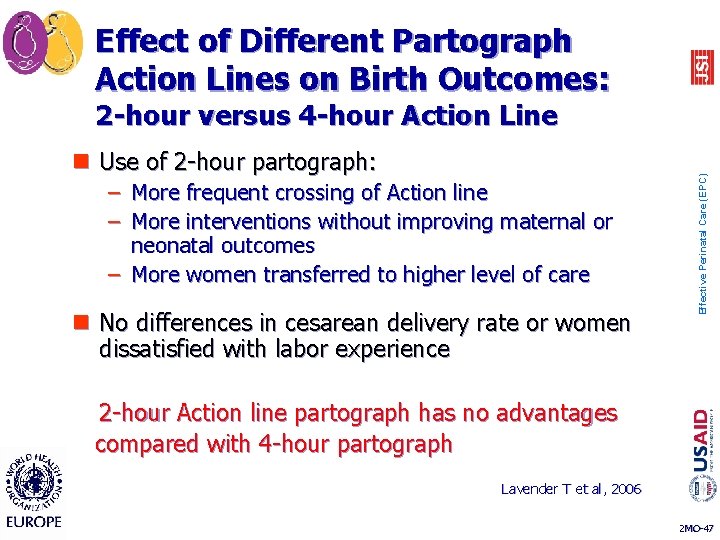
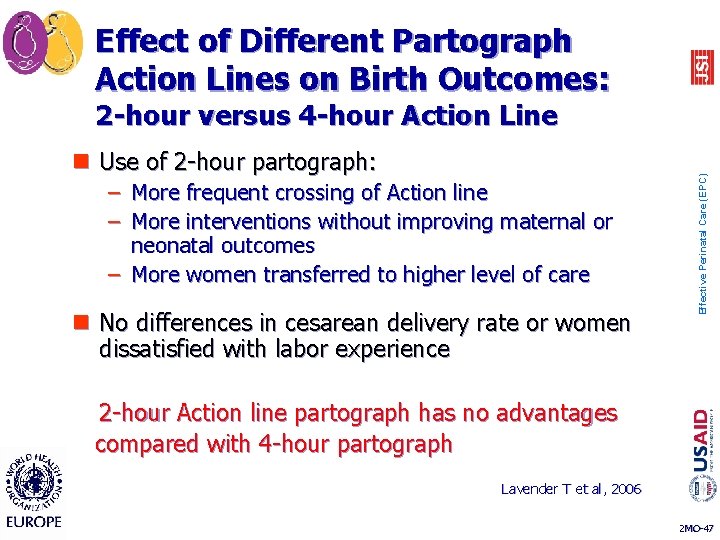
Effect of Different Partograph Action Lines on Birth Outcomes: n Use of 2 -hour partograph: – More frequent crossing of Action line – More interventions without improving maternal or neonatal outcomes – More women transferred to higher level of care n No differences in cesarean delivery rate or women dissatisfied with labor experience 2 -hour Action line partograph has no advantages compared with 4 -hour partograph Effective Perinatal Care (EPC) 2 -hour versus 4 -hour Action Line Lavender T et al, 2006 2 MO-47
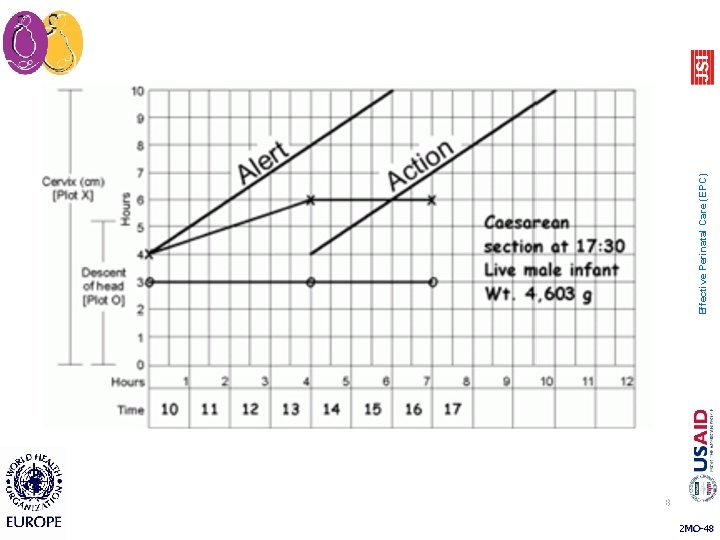
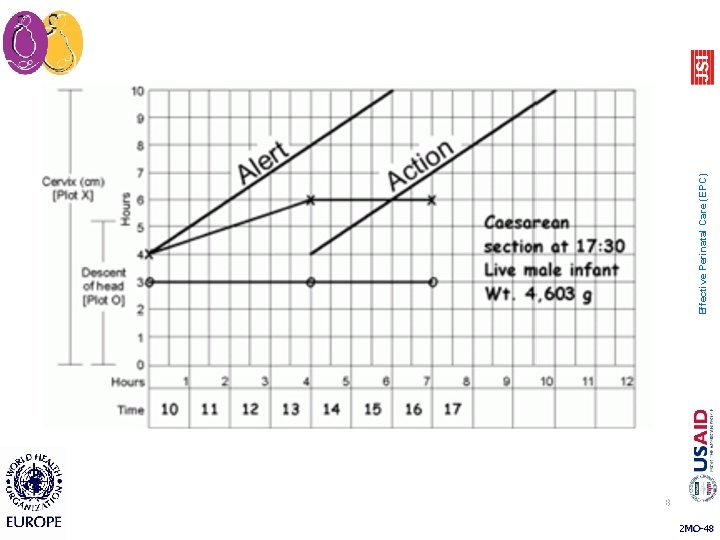
48 2 MO-48 Effective Perinatal Care (EPC)
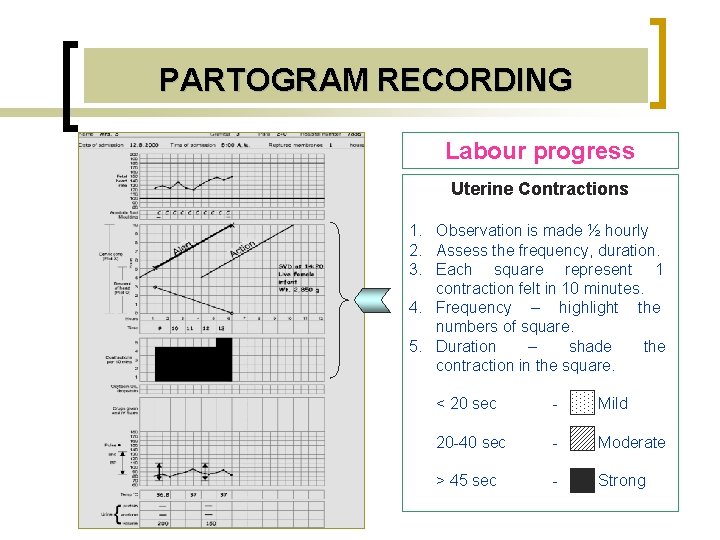
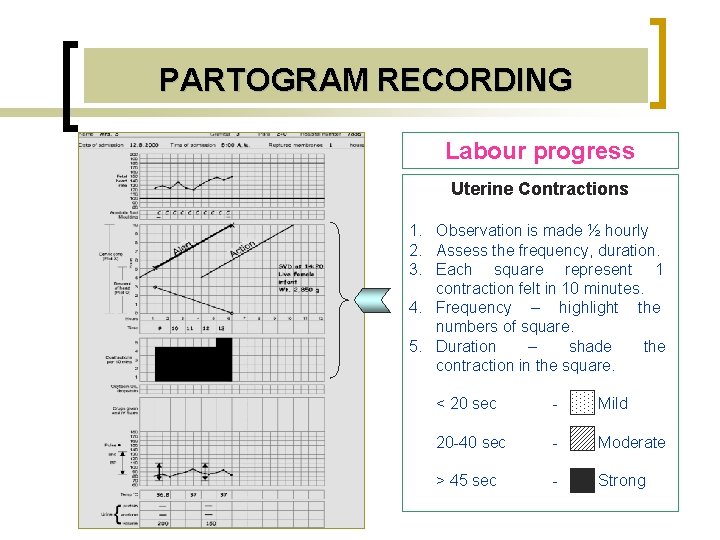
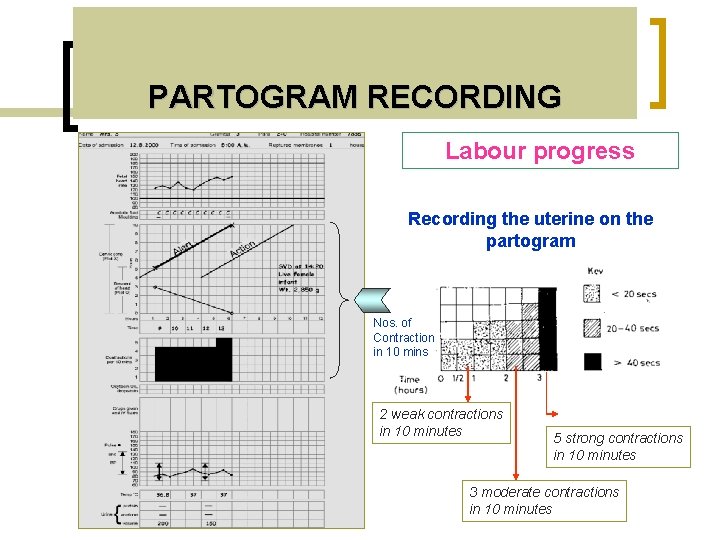
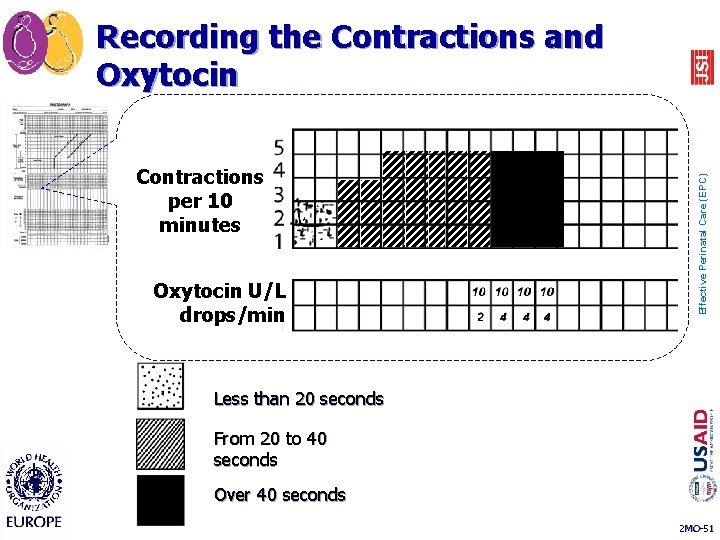
PARTOGRAM RECORDING Labour progress Uterine Contractions 1. Observation is made ½ hourly 2. Assess the frequency, duration. 3. Each square represent 1 contraction felt in 10 minutes. 4. Frequency – highlight the numbers of square. 5. Duration – shade the contraction in the square. < 20 sec - Mild 20 -40 sec - Moderate > 45 sec - Strong
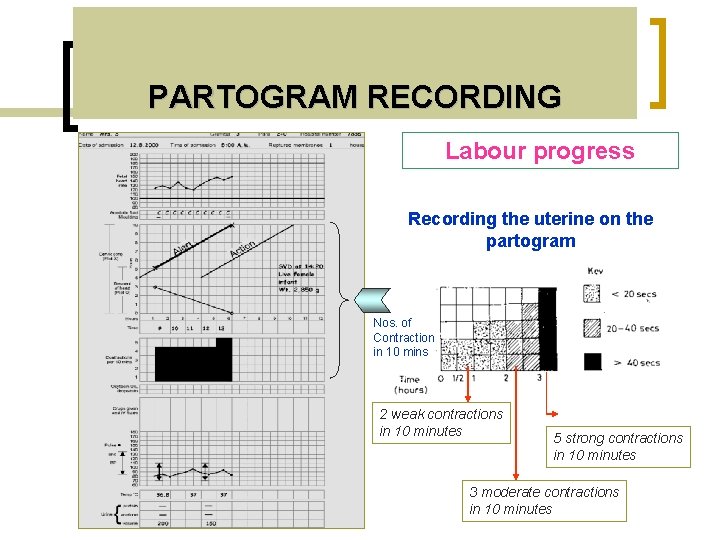
PARTOGRAM RECORDING Labour progress Recording the uterine on the partogram Nos. of Contraction in 10 mins 2 weak contractions in 10 minutes 5 strong contractions in 10 minutes 3 moderate contractions in 10 minutes
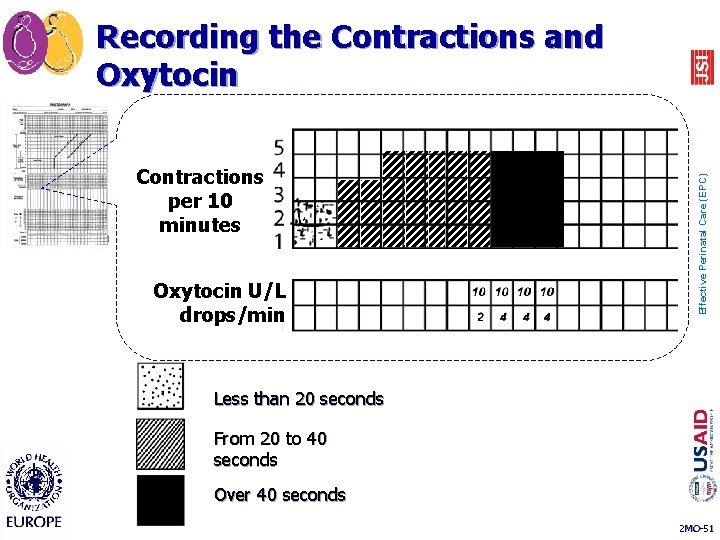
Contractions per 10 minutes Oxytocin U/L drops/min Effective Perinatal Care (EPC) Recording the Contractions and Oxytocin Less than 20 seconds From 20 to 40 seconds Over 40 seconds 2 MO-51
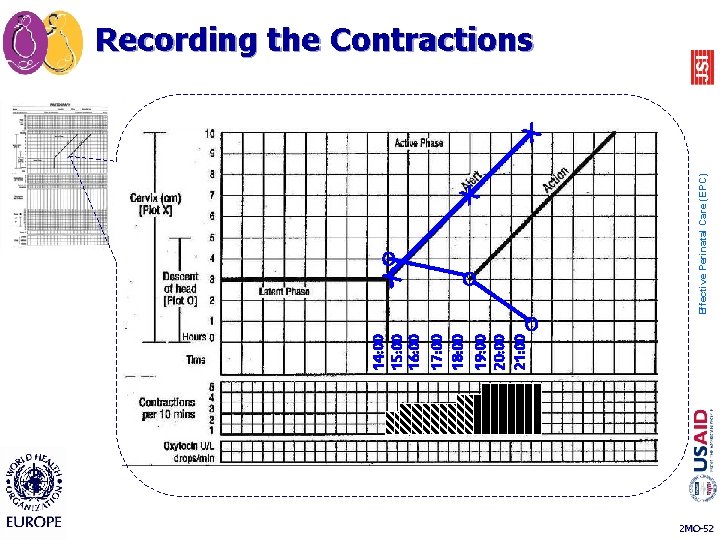
14: 00 15: 00 16: 00 17: 00 18: 00 19: 00 20: 00 21: 00 X O O Effective Perinatal Care (EPC) Recording the Contractions X 2 MO-52
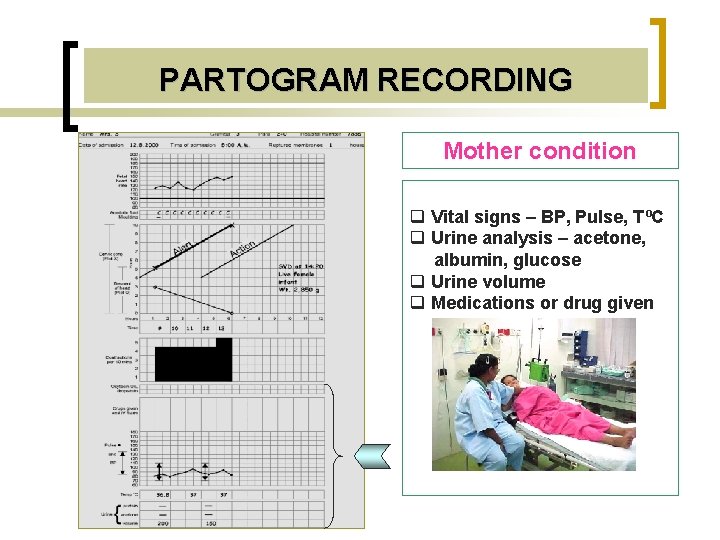
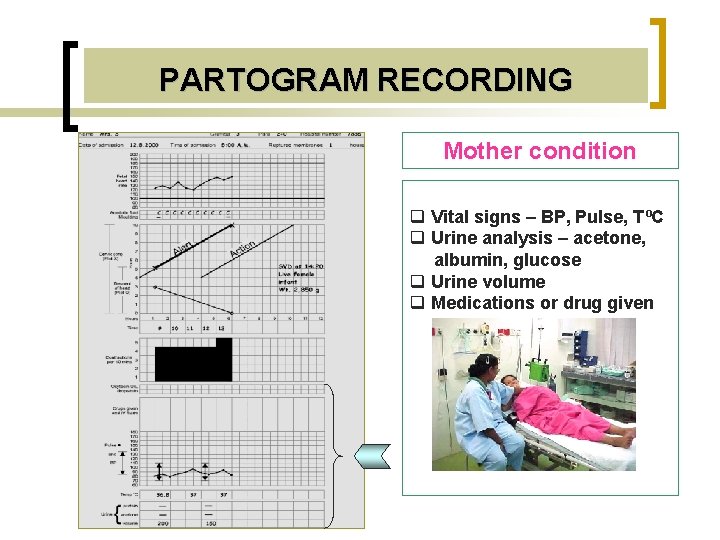
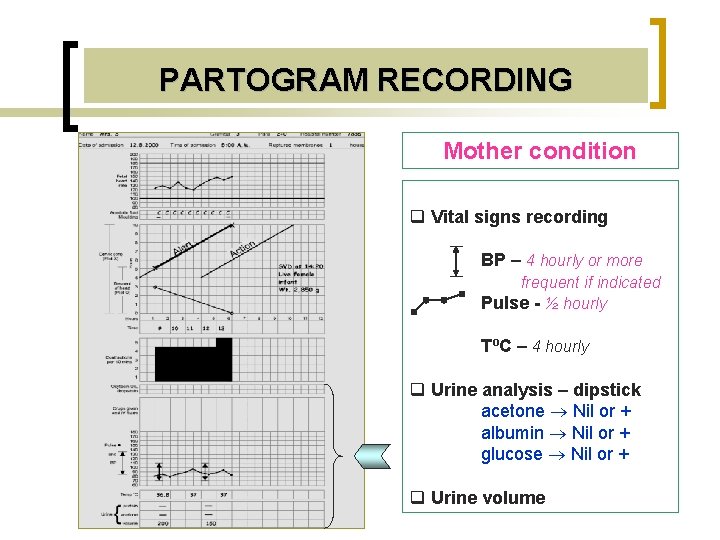
PARTOGRAM RECORDING Mother condition q Vital signs – BP, Pulse, TºC q Urine analysis – acetone, albumin, glucose q Urine volume q Medications or drug given
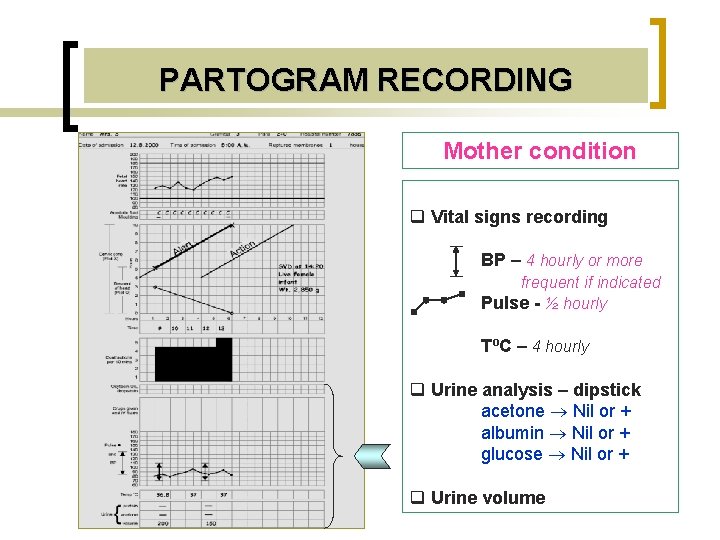
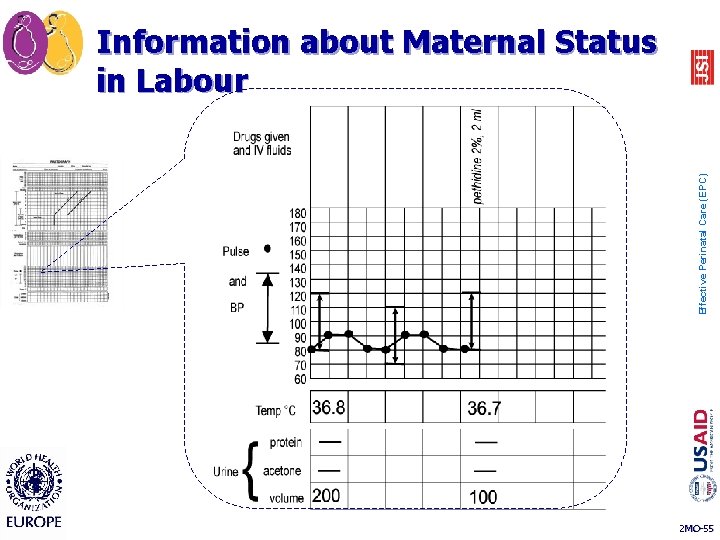
PARTOGRAM RECORDING Mother condition q Vital signs recording BP – 4 hourly or more frequent if indicated Pulse - ½ hourly TºC – 4 hourly q Urine analysis – dipstick acetone Nil or + albumin Nil or + glucose Nil or + q Urine volume
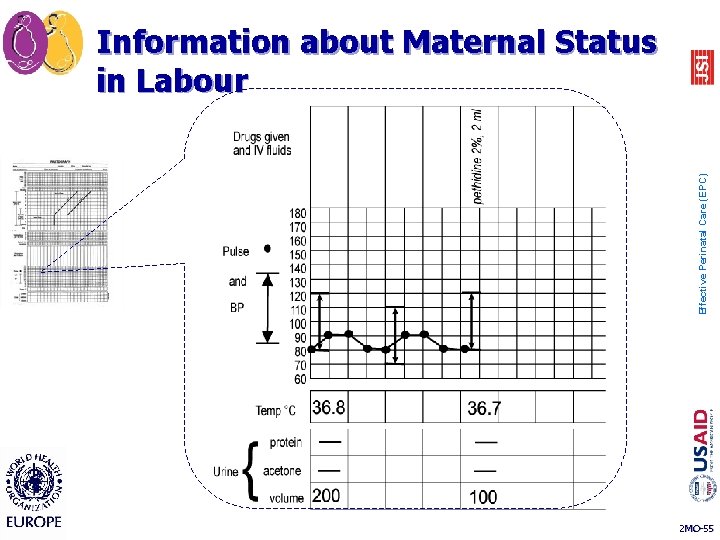
Effective Perinatal Care (EPC) Information about Maternal Status in Labour 2 MO-55
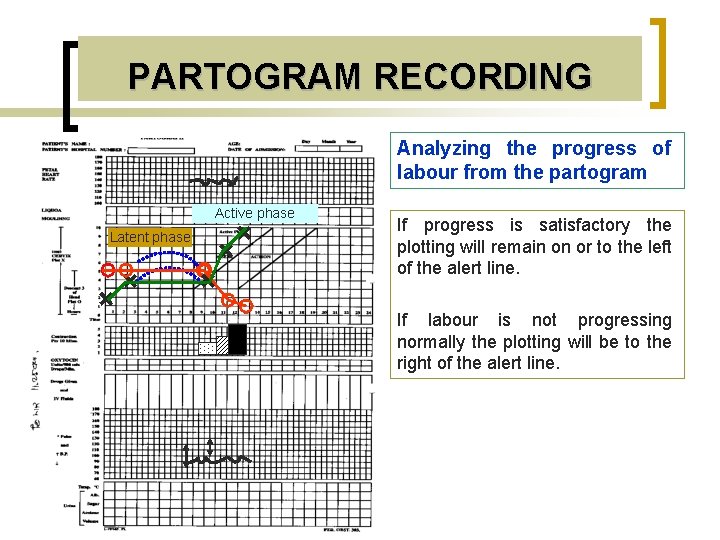
PARTOGRAM RECORDING Analyzing the progress of labour from the partogram Active phase + Latent phase + If progress is satisfactory the plotting will remain on or to the left of the alert line. + + + If labour is not progressing normally the plotting will be to the right of the alert line.
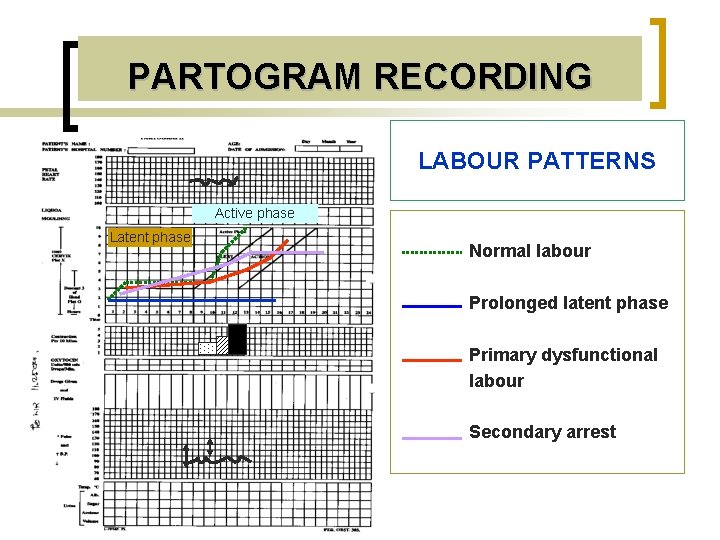
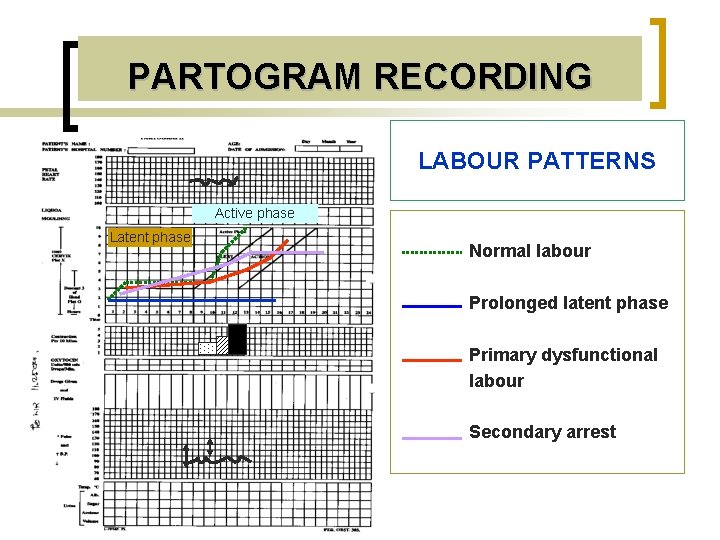
PARTOGRAM RECORDING LABOUR PATTERNS Active phase Latent phase Normal labour Prolonged latent phase Primary dysfunctional labour Secondary arrest
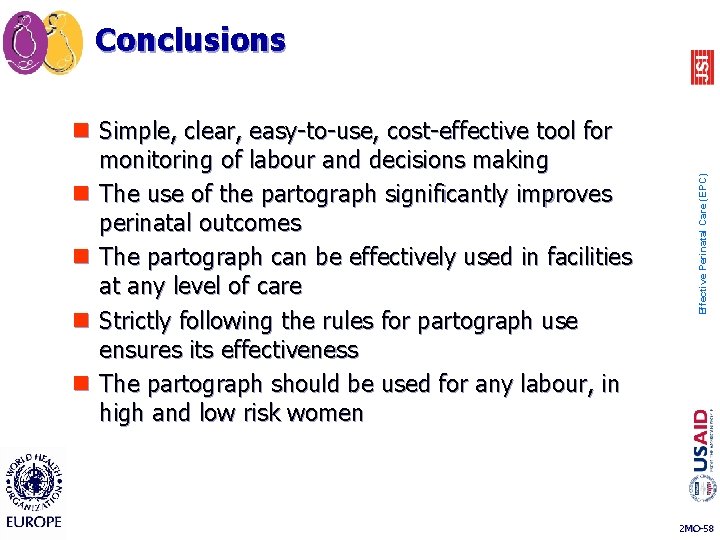
n Simple, clear, easy-to-use, cost-effective tool for monitoring of labour and decisions making n The use of the partograph significantly improves perinatal outcomes n The partograph can be effectively used in facilities at any level of care n Strictly following the rules for partograph use ensures its effectiveness n The partograph should be used for any labour, in high and low risk women Effective Perinatal Care (EPC) Conclusions 2 MO-58
Effective Perinatal Care (EPC) Interpretation of labor using the Partograph
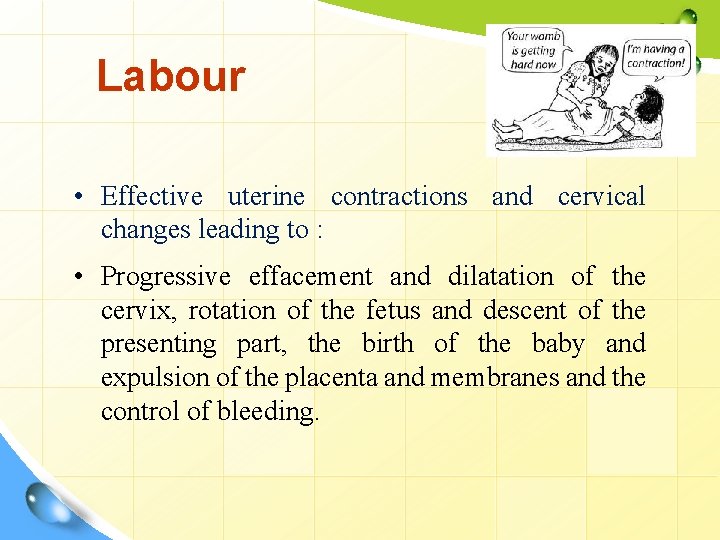
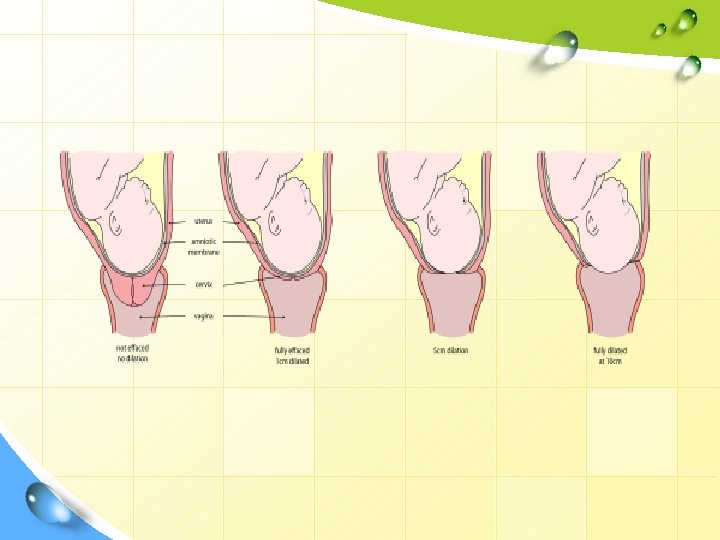
Labour • Effective uterine contractions and cervical changes leading to : • Progressive effacement and dilatation of the cervix, rotation of the fetus and descent of the presenting part, the birth of the baby and expulsion of the placenta and membranes and the control of bleeding.
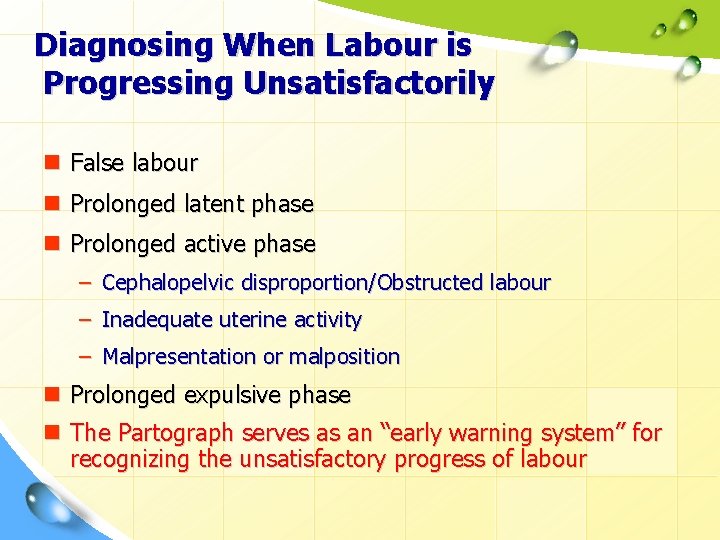
Diagnosing When Labour is Progressing Unsatisfactorily n False labour n Prolonged latent phase n Prolonged active phase – Cephalopelvic disproportion/Obstructed labour – Inadequate uterine activity – Malpresentation or malposition n Prolonged expulsive phase n The Partograph serves as an “early warning system” for recognizing the unsatisfactory progress of labour
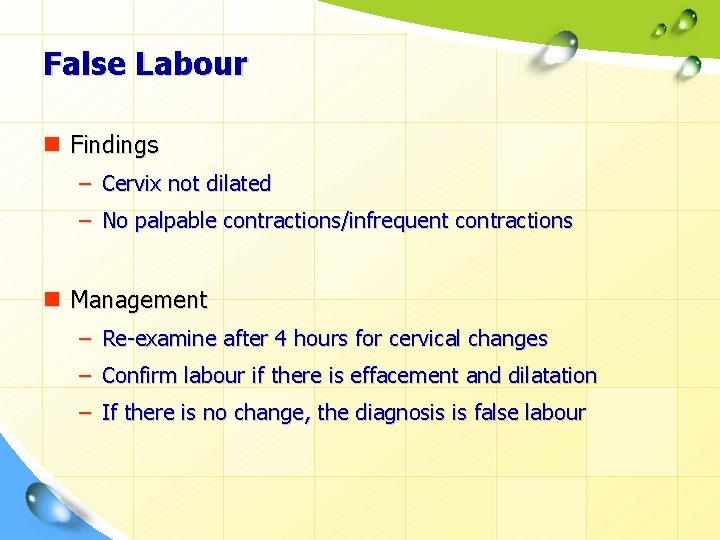
False Labour n Findings – Cervix not dilated – No palpable contractions/infrequent contractions n Management – Re-examine after 4 hours for cervical changes – Confirm labour if there is effacement and dilatation – If there is no change, the diagnosis is false labour
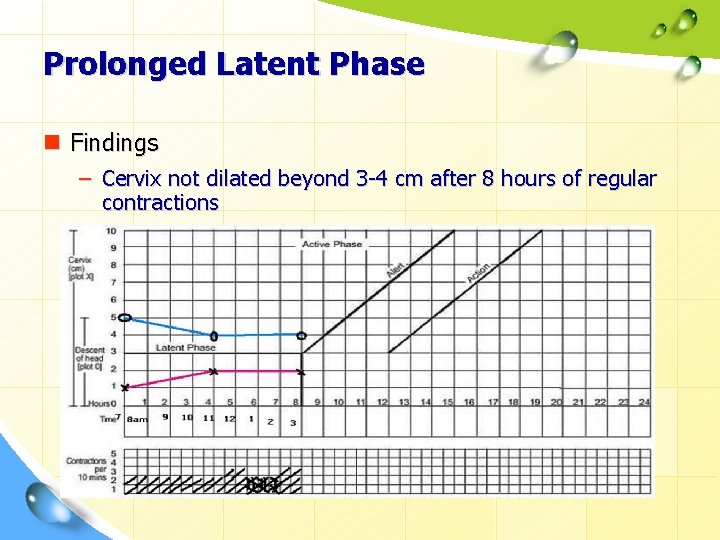
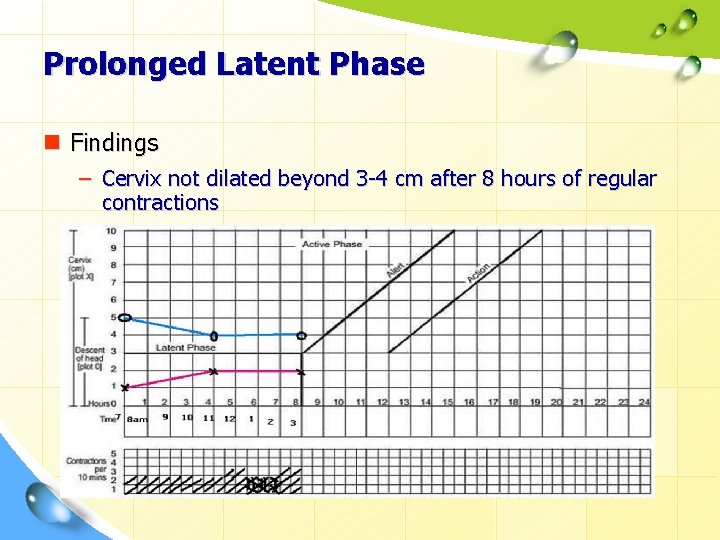
Prolonged Latent Phase n Findings – Cervix not dilated beyond 3 -4 cm after 8 hours of regular contractions
Prolonged Latent Phase n Management – Reassess the cervix – If no change, the woman may not be in labour n Midwifery care Ø The woman needs support and encouragement Ø Adequate food and fluid intake Ø Back massage, Ø Changes of position, upright position Ø Maintain hydration Ø Warm bath or some simple analgesia.
Prolonged Latent Phase n Management – Reassess the cervix – If no change, the woman may not be in labour – If changes in cervical effacement or dilatation, rupture membranes and induce labour: n Reassess every 4 hours n If the woman has not entered the active phase after 8 hours of oxytocin infusion, deliver by caesarean section n Intervention such as an ARM at this stage can interfere with the action of amniotic prostaglandin on the cervix and be counterproductive
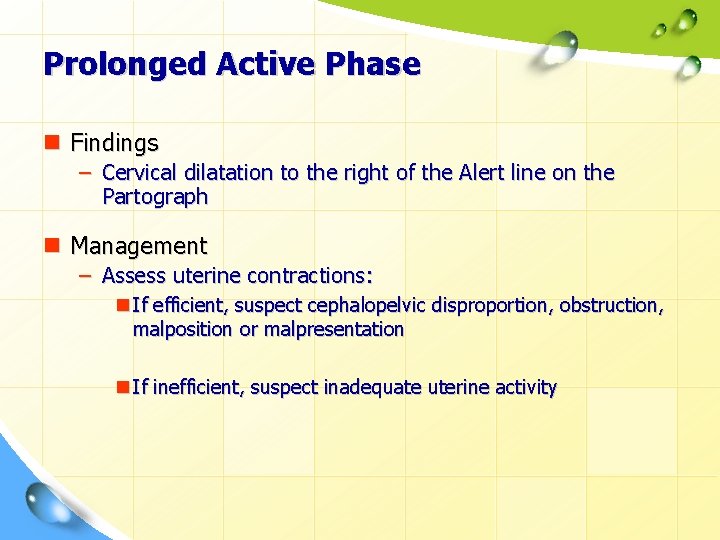
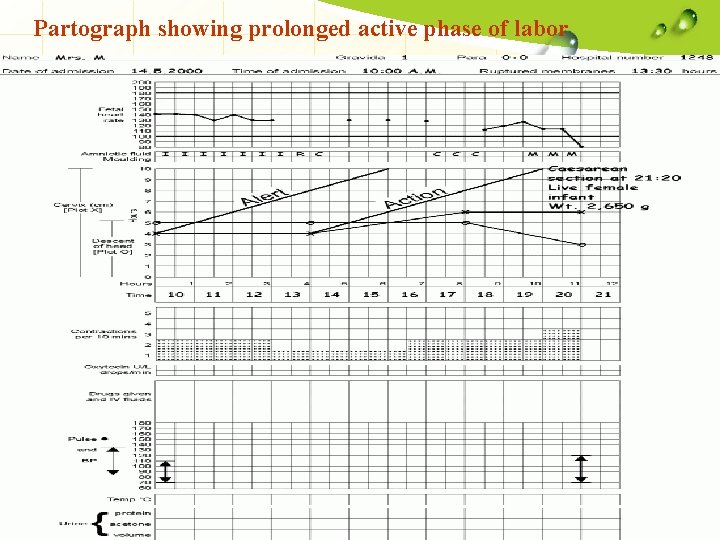
Prolonged Active Phase n Findings – Cervical dilatation to the right of the Alert line on the Partograph n Management – Assess uterine contractions: n If efficient, suspect cephalopelvic disproportion, obstruction, malposition or malpresentation n If inefficient, suspect inadequate uterine activity
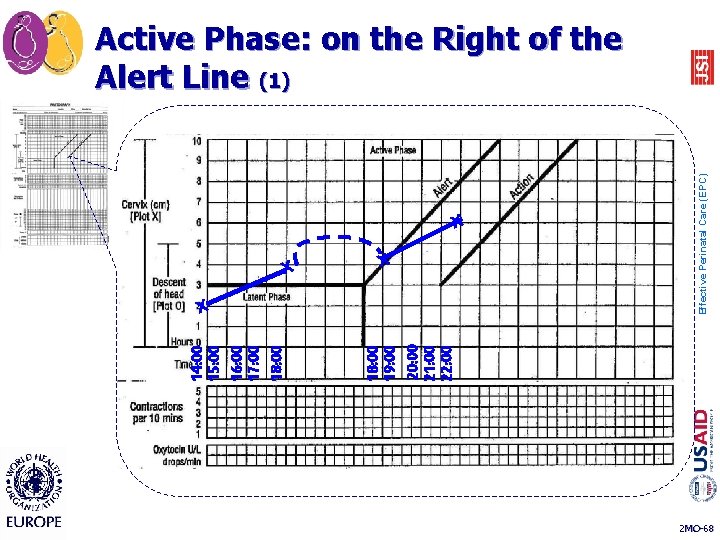
X 18: 00 19: 00 20: 00 21: 00 22: 00 14: 00 15: 00 16: 00 17: 00 18: 00 X X X Effective Perinatal Care (EPC) Active Phase: on the Right of the Alert Line (1) 2 MO-68
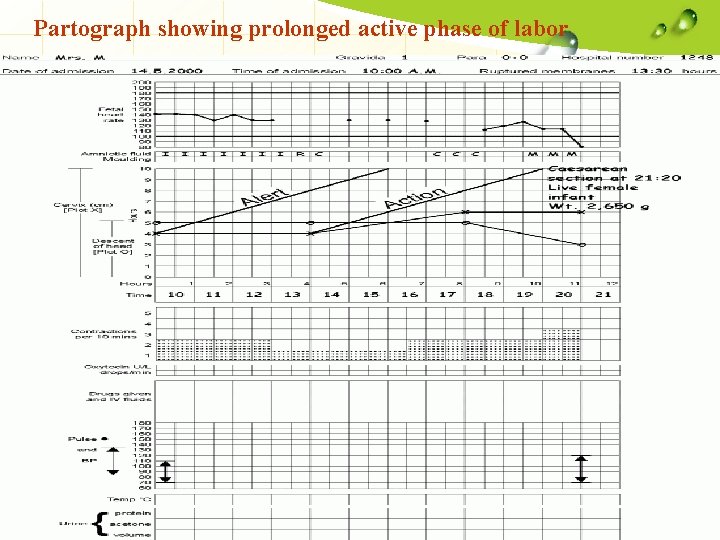
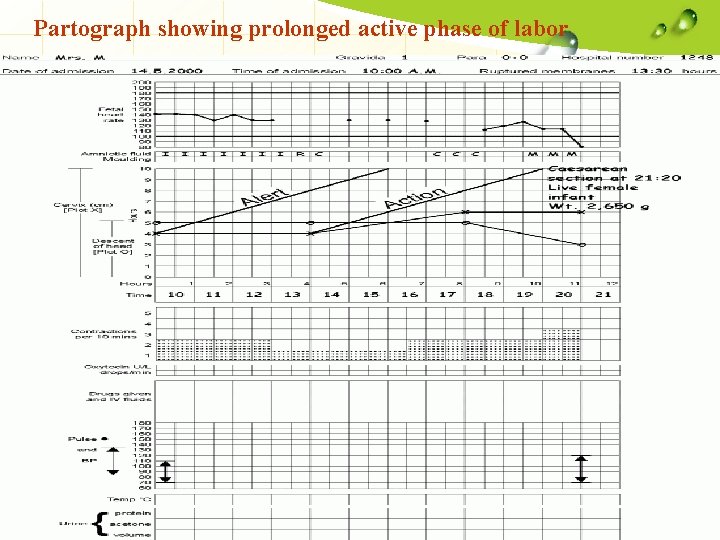
Partograph showing prolonged active phase of labor
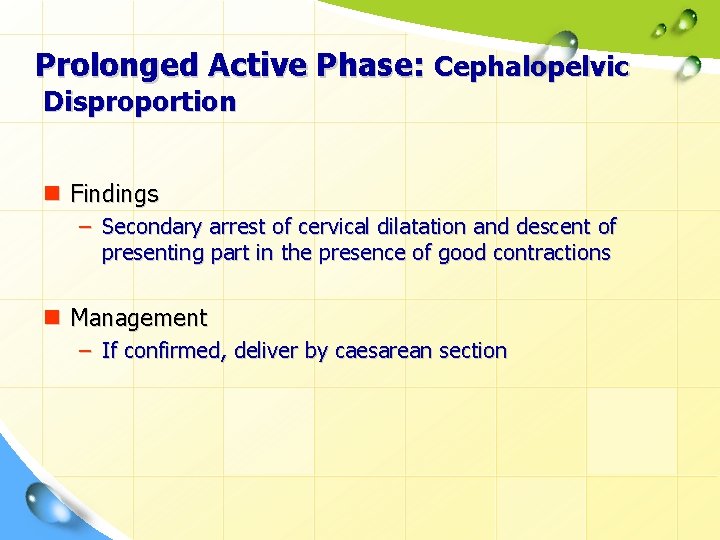
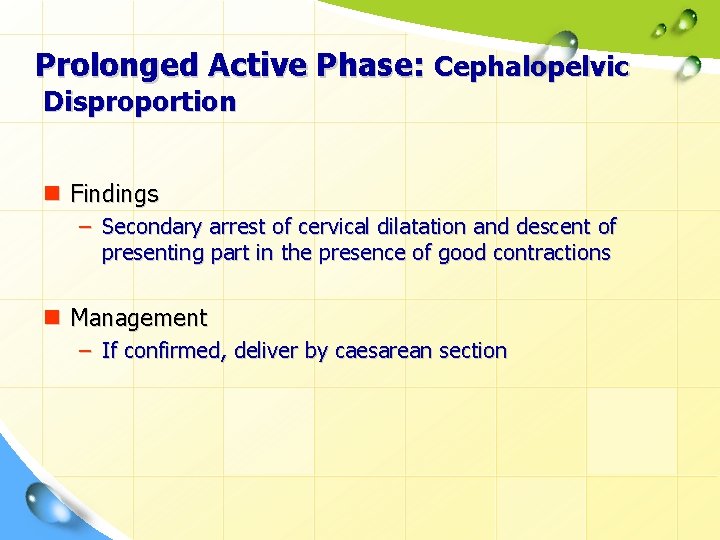
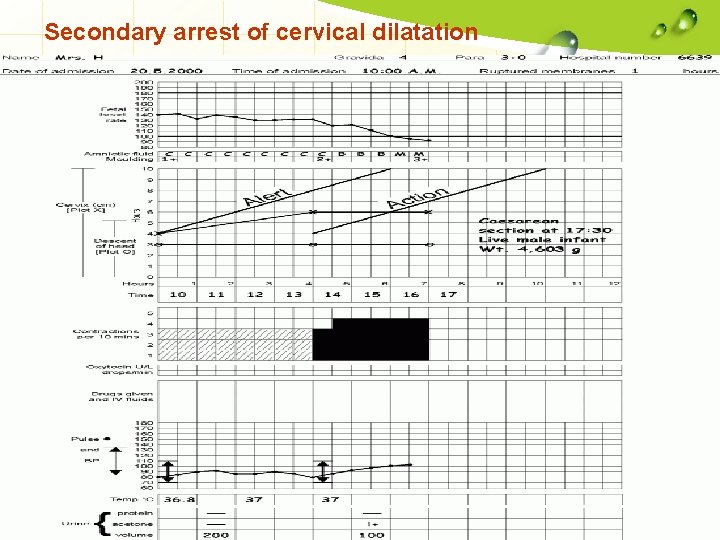
Prolonged Active Phase: Cephalopelvic Disproportion n Findings – Secondary arrest of cervical dilatation and descent of presenting part in the presence of good contractions n Management – If confirmed, deliver by caesarean section
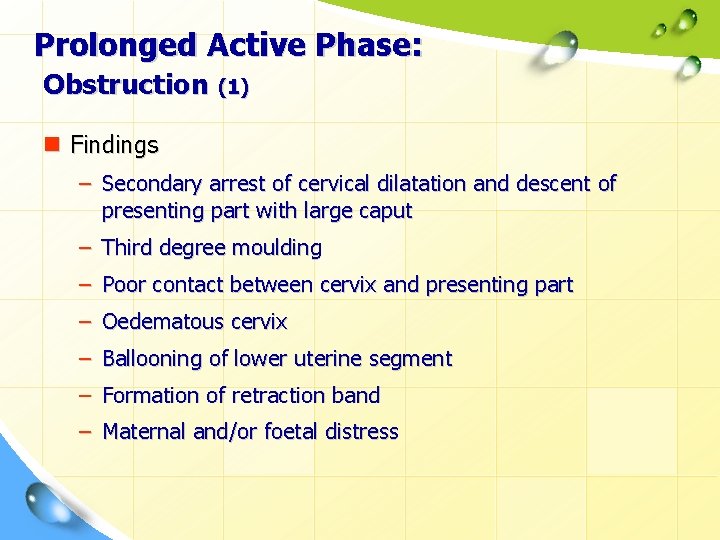
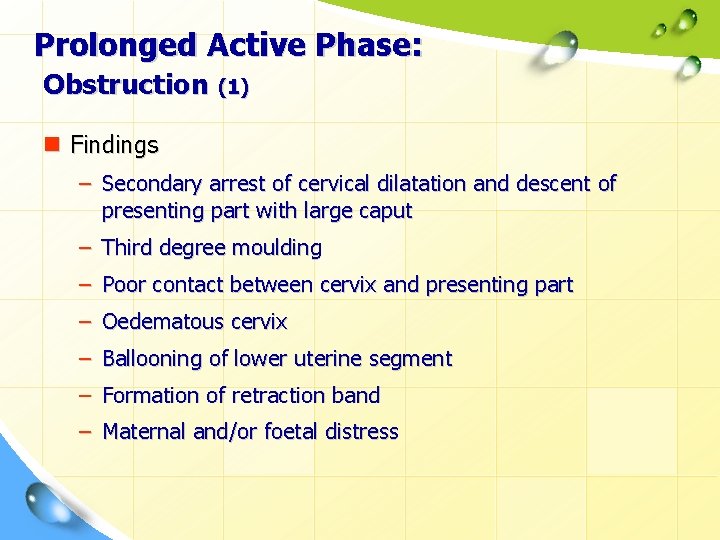
Prolonged Active Phase: Obstruction (1) n Findings – Secondary arrest of cervical dilatation and descent of presenting part with large caput – Third degree moulding – Poor contact between cervix and presenting part – Oedematous cervix – Ballooning of lower uterine segment – Formation of retraction band – Maternal and/or foetal distress
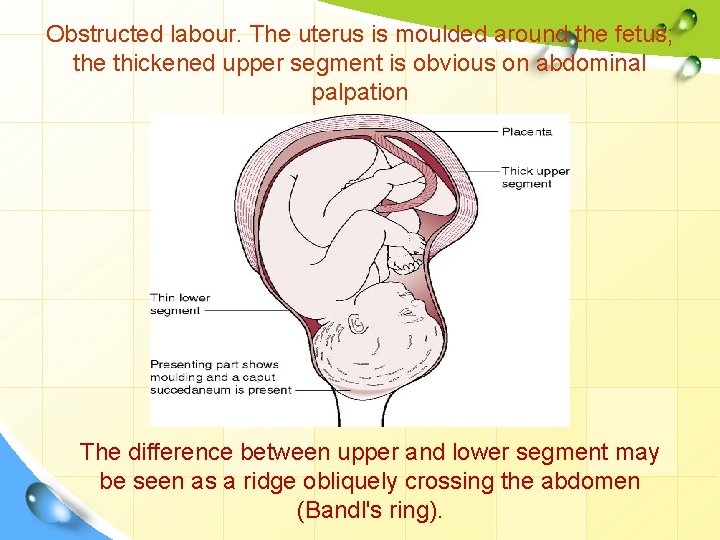
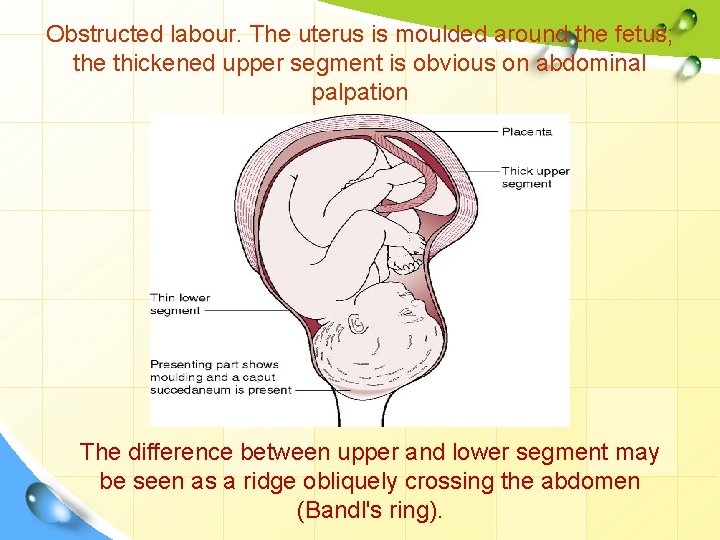
Obstructed labour. The uterus is moulded around the fetus; the thickened upper segment is obvious on abdominal palpation The difference between upper and lower segment may be seen as a ridge obliquely crossing the abdomen (Bandl's ring).
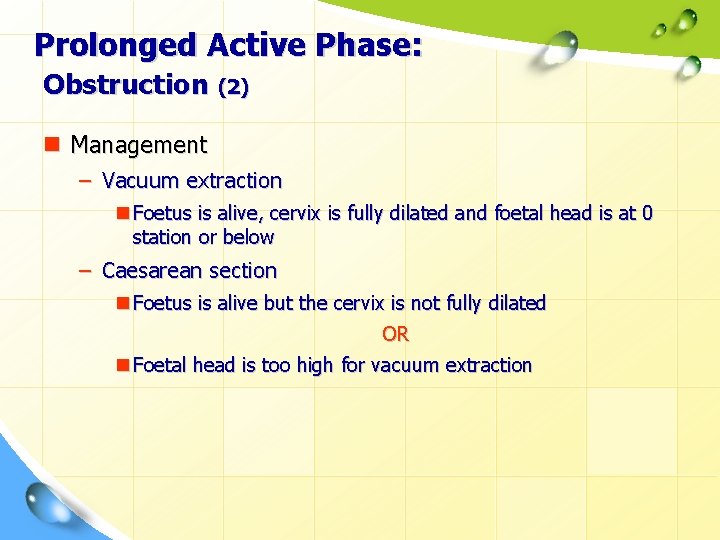
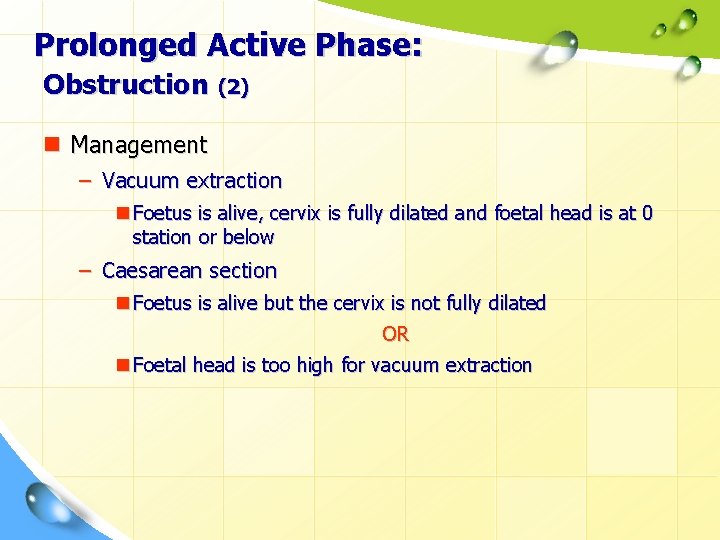
Prolonged Active Phase: Obstruction (2) n Management – Vacuum extraction n Foetus is alive, cervix is fully dilated and foetal head is at 0 station or below – Caesarean section n Foetus is alive but the cervix is not fully dilated OR n Foetal head is too high for vacuum extraction
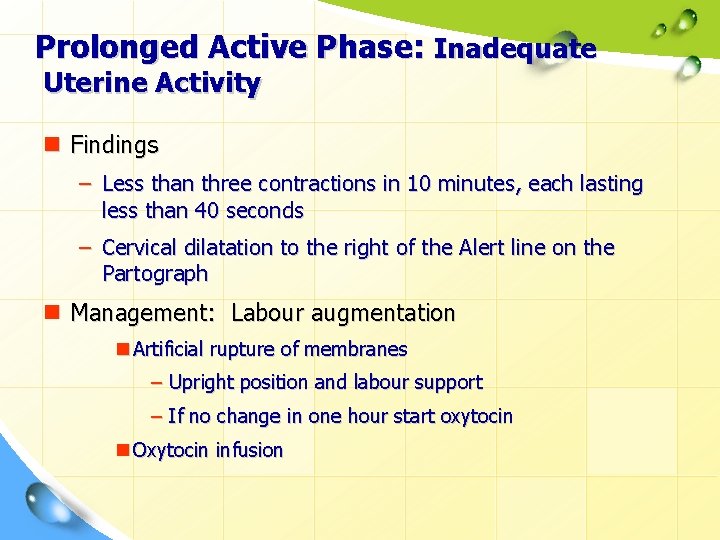
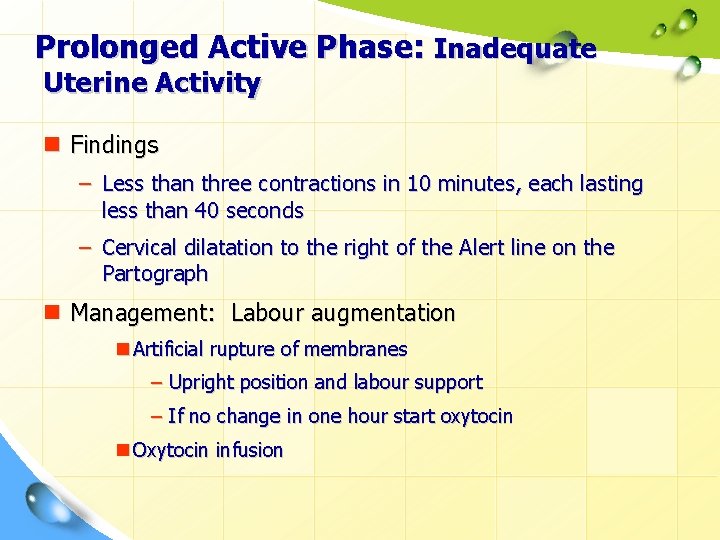
Prolonged Active Phase: Inadequate Uterine Activity n Findings – Less than three contractions in 10 minutes, each lasting less than 40 seconds – Cervical dilatation to the right of the Alert line on the Partograph n Management: Labour augmentation n Artificial rupture of membranes – Upright position and labour support – If no change in one hour start oxytocin n Oxytocin infusion
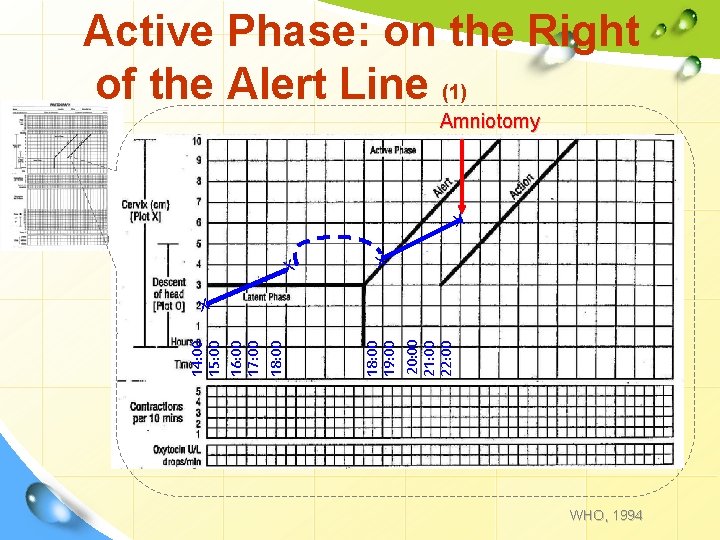
Active Phase: on the Right of the Alert Line (1) Amniotomy X X X 18: 00 19: 00 20: 00 21: 00 22: 00 14: 00 15: 00 16: 00 17: 00 18: 00 X WHO, 1994
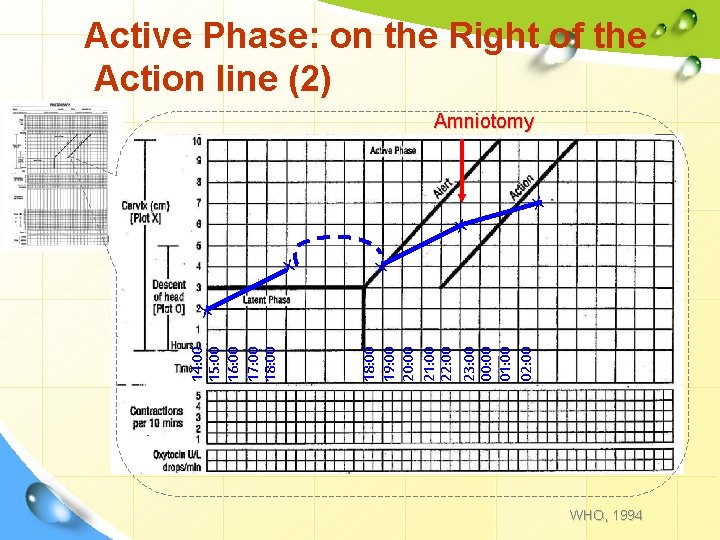
Active Phase: on the Right of the Action line (2) Amniotomy X X 18: 00 19: 00 20: 00 21: 00 22: 00 23: 00 00: 00 01: 00 02: 00 14: 00 15: 00 16: 00 17: 00 18: 00 X WHO, 1994
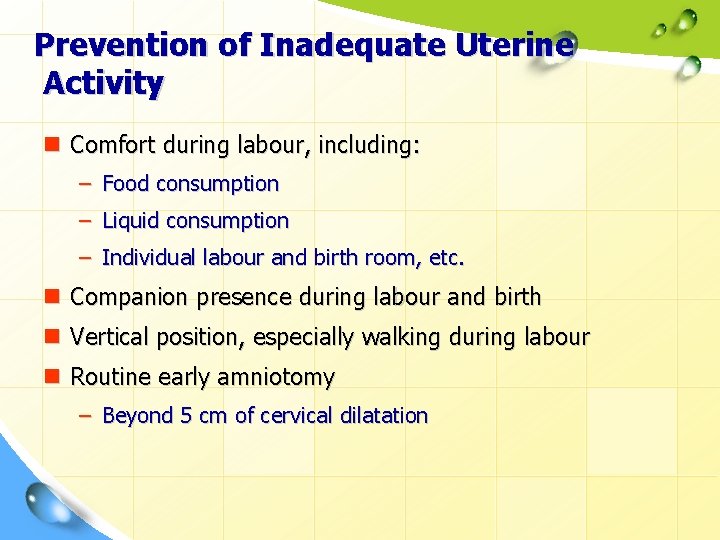
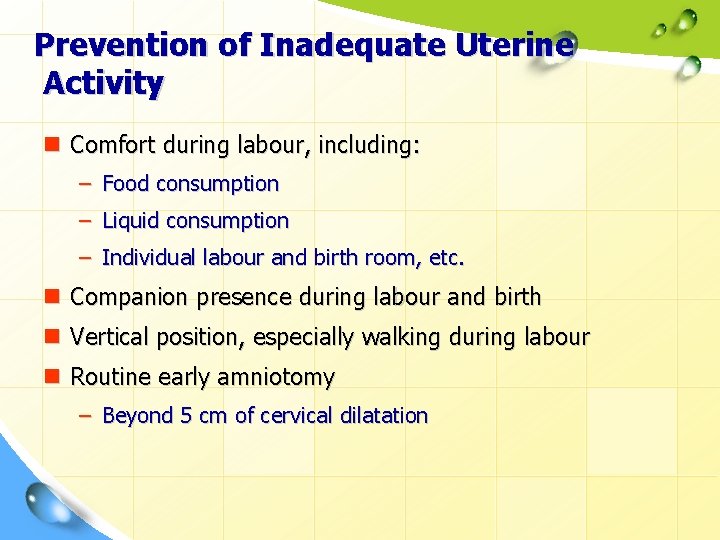
Prevention of Inadequate Uterine Activity n Comfort during labour, including: – Food consumption – Liquid consumption – Individual labour and birth room, etc. n Companion presence during labour and birth n Vertical position, especially walking during labour n Routine early amniotomy – Beyond 5 cm of cervical dilatation
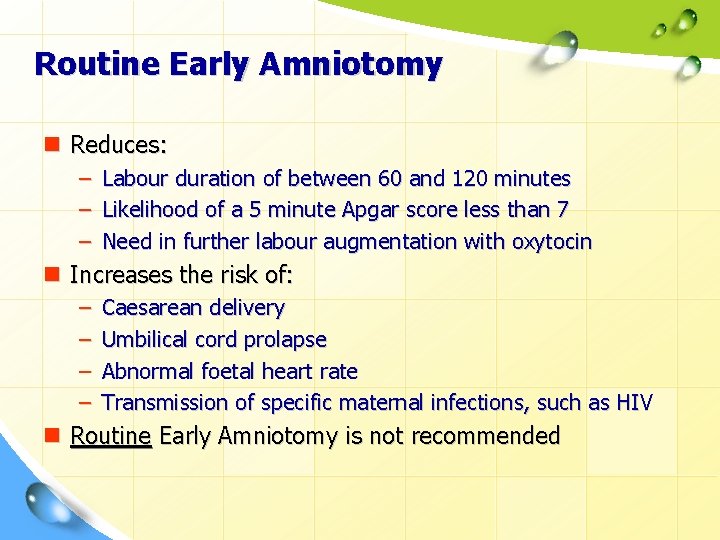
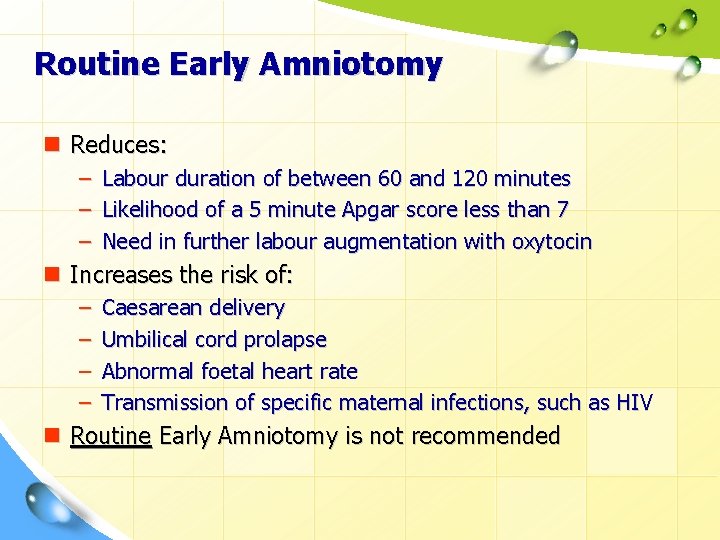
Routine Early Amniotomy n Reduces: – Labour duration of between 60 and 120 minutes – Likelihood of a 5 minute Apgar score less than 7 – Need in further labour augmentation with oxytocin n Increases the risk of: – – Caesarean delivery Umbilical cord prolapse Abnormal foetal heart rate Transmission of specific maternal infections, such as HIV n Routine Early Amniotomy is not recommended
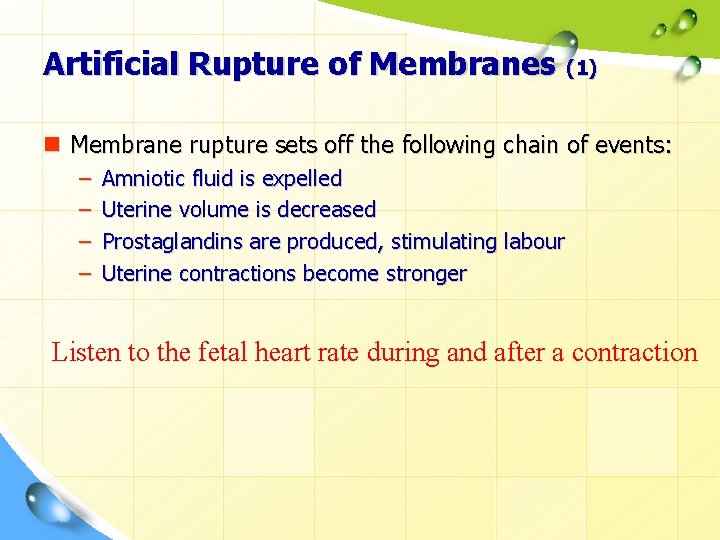
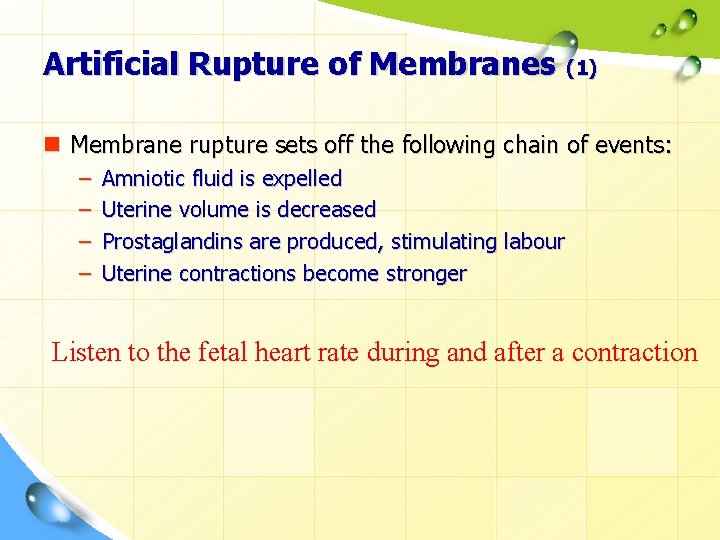
Artificial Rupture of Membranes (1) n Membrane rupture sets off the following chain of events: – – Amniotic fluid is expelled Uterine volume is decreased Prostaglandins are produced, stimulating labour Uterine contractions become stronger Listen to the fetal heart rate during and after a contraction
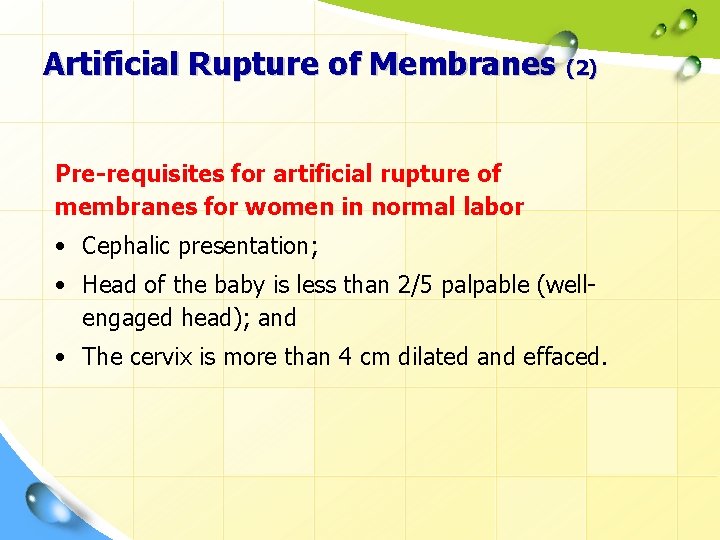
Artificial Rupture of Membranes (2) Pre-requisites for artificial rupture of membranes for women in normal labor • Cephalic presentation; • Head of the baby is less than 2/5 palpable (wellengaged head); and • The cervix is more than 4 cm dilated and effaced.
Artificial Rupture of Membranes (3) n Sterile gloves and instruments should be used to perform the amniotomy n Listen to and note the foetal heart rate before and after amniotomy n Note the colour of the fluid (clear, greenish, bloody, thick meconium) n Monitor uterine contractions – If good labour is not established 1 hour after amniotomy, begin oxytocin infusion n Record on the Partograph
Oxytocin Infusion (1) n Should be administered only by IV infusion n The effective dose of oxytocin varies greatly between women n Use oxytocin with caution because of the risk of: – Foetal distress – Hyperstimulation – Uterine rupture (rarely) n Multiparous women are at higher risk for uterine rupture
Oxytocin Infusion (2) n Carefully observe women receiving oxytocin – – Pulse and blood pressure Contractions Foetal heart rate Rate of oxytocin infusion n Record findings on Partograph n Electronic foetal monitoring is recommended if oxytocin is used
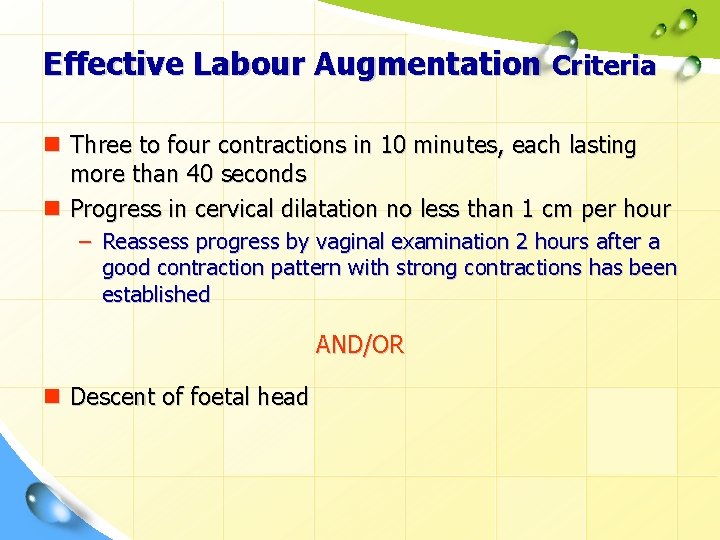
Effective Labour Augmentation Criteria n Three to four contractions in 10 minutes, each lasting more than 40 seconds n Progress in cervical dilatation no less than 1 cm per hour – Reassess progress by vaginal examination 2 hours after a good contraction pattern with strong contractions has been established AND/OR n Descent of foetal head
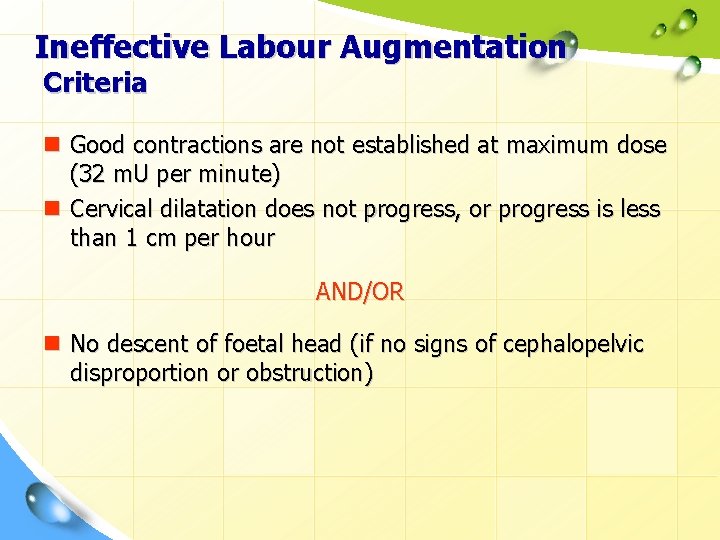
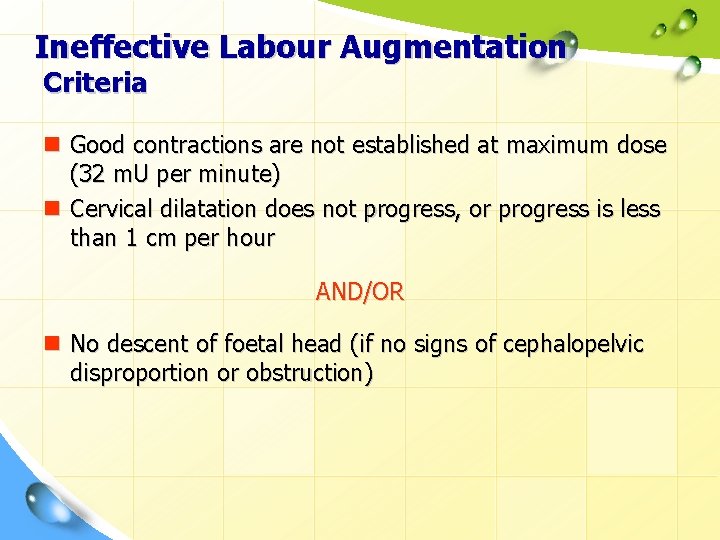
Ineffective Labour Augmentation Criteria n Good contractions are not established at maximum dose (32 m. U per minute) n Cervical dilatation does not progress, or progress is less than 1 cm per hour AND/OR n No descent of foetal head (if no signs of cephalopelvic disproportion or obstruction)
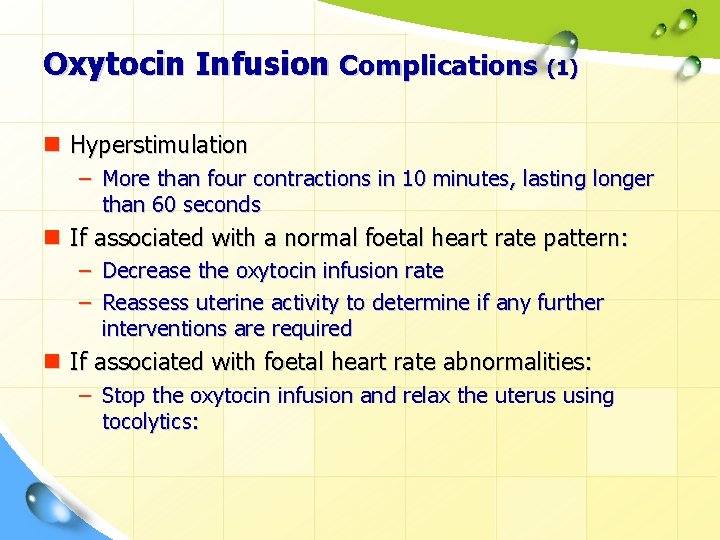
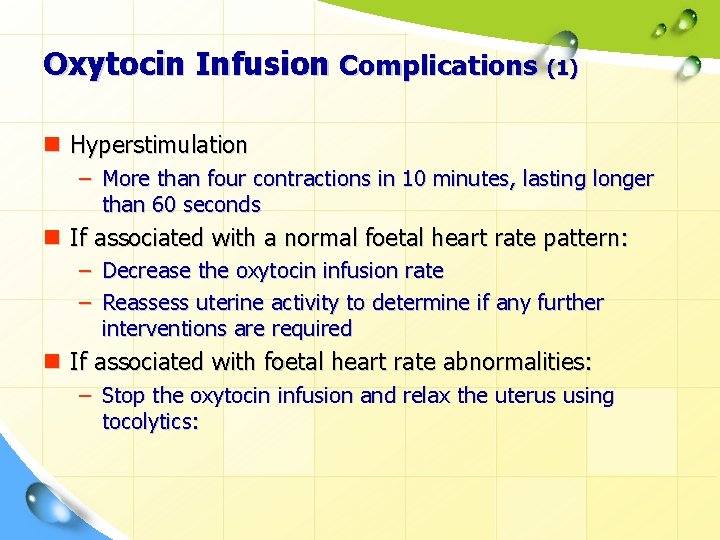
Oxytocin Infusion Complications (1) n Hyperstimulation – More than four contractions in 10 minutes, lasting longer than 60 seconds n If associated with a normal foetal heart rate pattern: – Decrease the oxytocin infusion rate – Reassess uterine activity to determine if any further interventions are required n If associated with foetal heart rate abnormalities: – Stop the oxytocin infusion and relax the uterus using tocolytics:
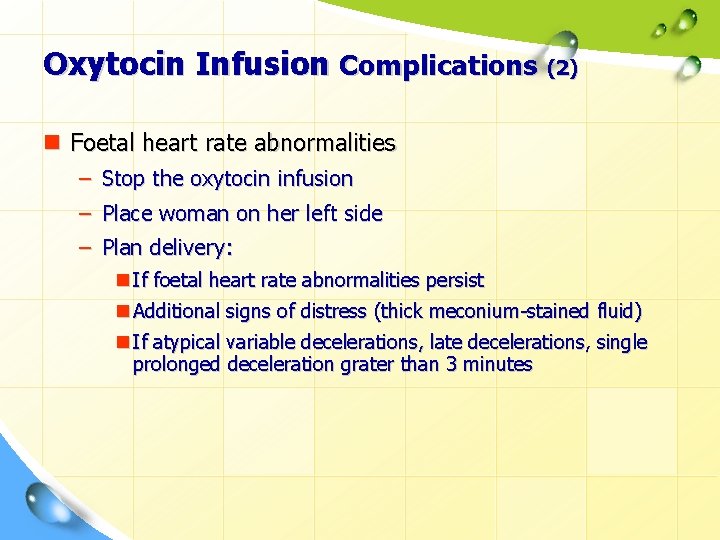
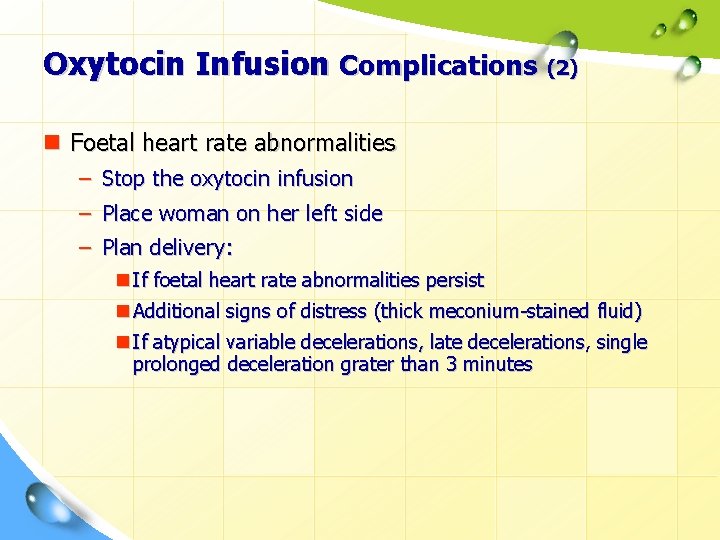
Oxytocin Infusion Complications (2) n Foetal heart rate abnormalities – Stop the oxytocin infusion – Place woman on her left side – Plan delivery: n If foetal heart rate abnormalities persist n Additional signs of distress (thick meconium-stained fluid) n If atypical variable decelerations, late decelerations, single prolonged deceleration grater than 3 minutes
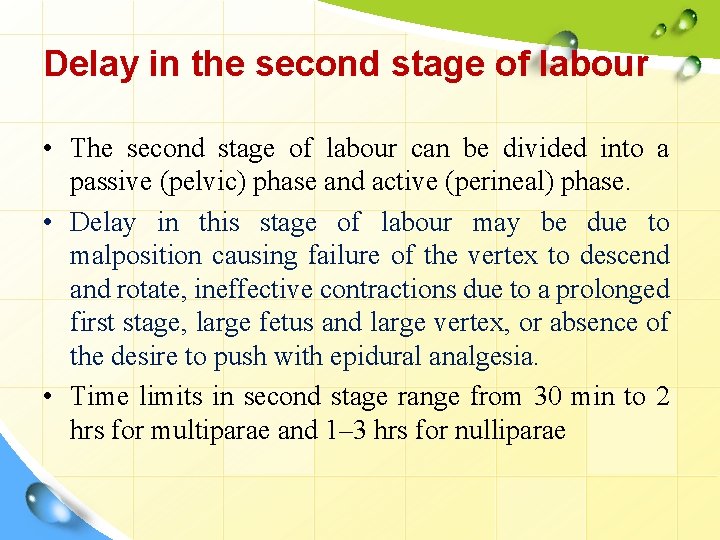
Delay in the second stage of labour • The second stage of labour can be divided into a passive (pelvic) phase and active (perineal) phase. • Delay in this stage of labour may be due to malposition causing failure of the vertex to descend and rotate, ineffective contractions due to a prolonged first stage, large fetus and large vertex, or absence of the desire to push with epidural analgesia. • Time limits in second stage range from 30 min to 2 hrs for multiparae and 1– 3 hrs for nulliparae
Management • When a diagnosis of delay in the second stage has been made the case is referred to the obstetrician for review and assessment. • The risk to both mother and fetus if the second stage is allowed to exceed normal time limits must be weighed against the risks of intervening with an instrumental or operative delivery. • Where there is any indication that the mother or the fetus is compromised the birth must be expedited as soon as possible
Precipitate labour • In some women, the uterus is over-efficient and the onset of labour to birth is an hour or less. • Much or all of the first stage is not recognized because contractions are not painful and the realization of the birth of the head may be the first indication that labour has actually started.
Risk • • • Soft tissue trauma of the maternal genital tract Fetal Hypoxia Fetal Intracranial haemorrhage Fetal head and body injury Retained placenta and/or postpartum haemorrhage • The psychological impact of such a rapid birth must not be underestimated
Management • Precipitate labour will often recur in subsequent pregnancies and the obstetrician may advise induction of labour once term (37 completed weeks) is reached. • Working together as a team can only help to contribute to that positive birth experience.
Conclusions n Labour abnormalities can be revealed in a timely manner by using the WHO Partograph n Create a warm and friendly atmosphere in the maternity, have a companion present during labour and birth, encourage food and fluid consumption and upright position to reduce the rate of prolonged labour n Early amniotomy should not be routinely used n Amniotomy should be reserved for women when labour progresses abnormally n Oxytocin should be used with caution, followed by closely monitoring the progress of labour, and the condition of mother and baby
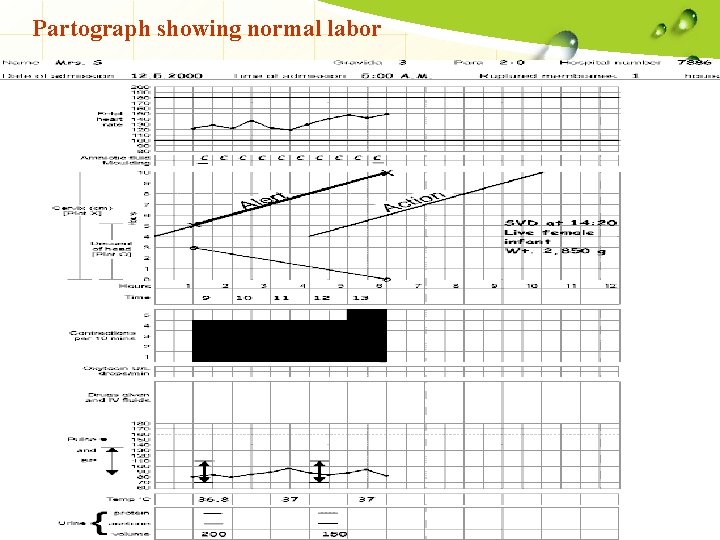
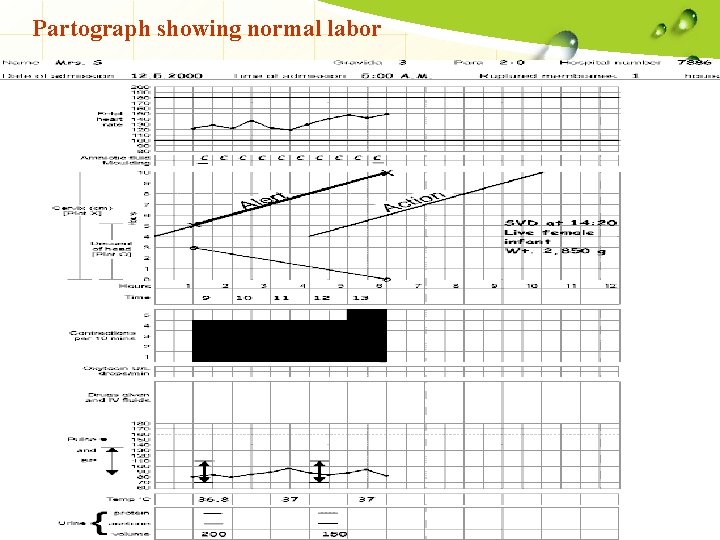
Partograph showing normal labor
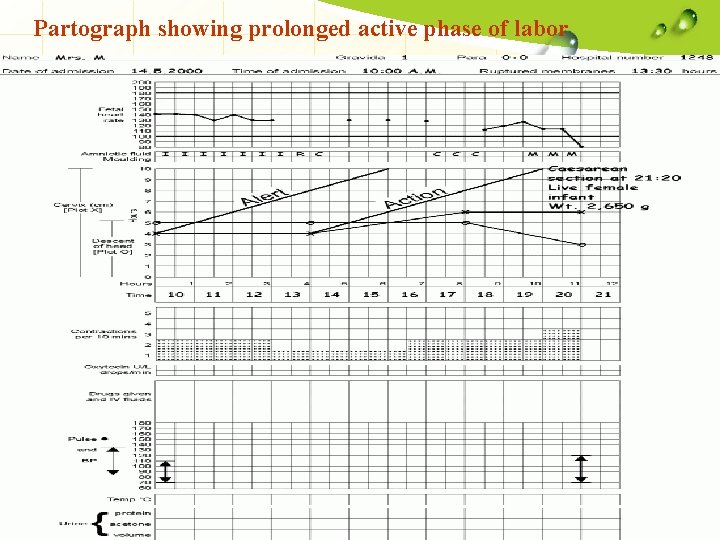
Partograph showing prolonged active phase of labor
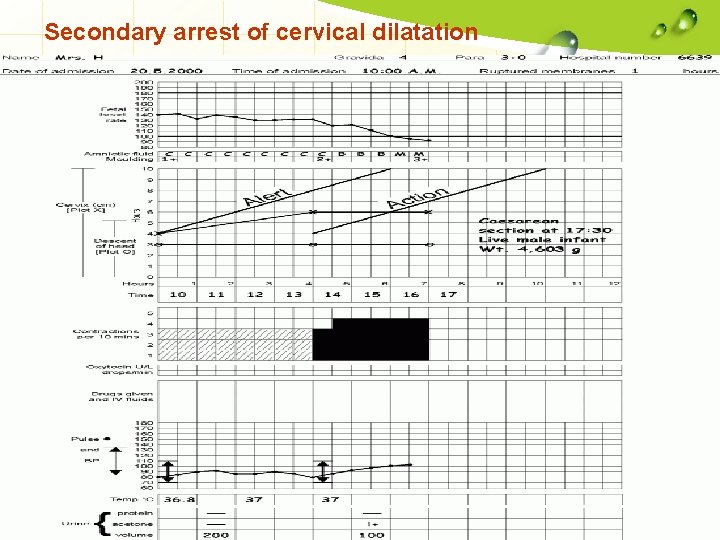
Secondary arrest of cervical dilatation
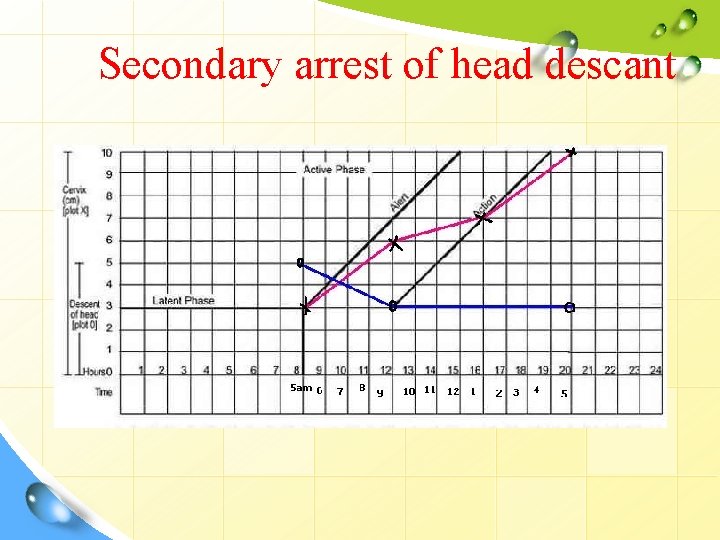
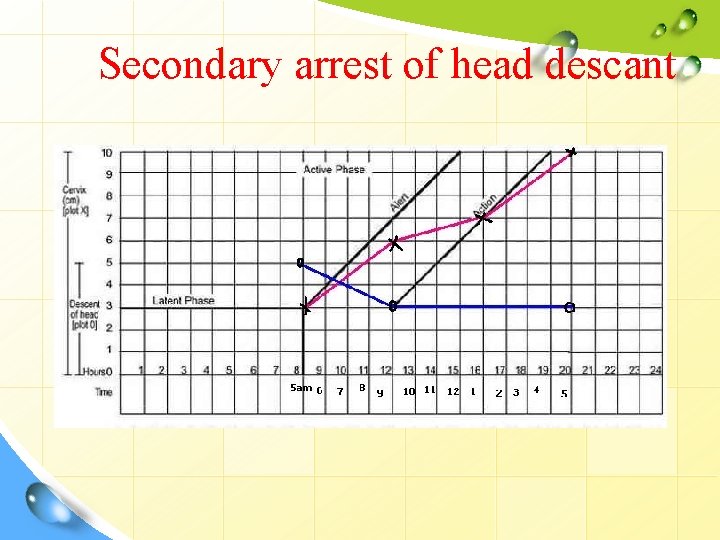
Secondary arrest of head descant

Thank You! L/O/G/O With best wishes , RN. laila M. Elmasharfa