Edward Evans MD FACC Desoto Heart Clinic Disclosures
- Slides: 32
Edward Evans MD FACC Desoto Heart Clinic Disclosures • Medtronic: • St. Jude Medical: speaker
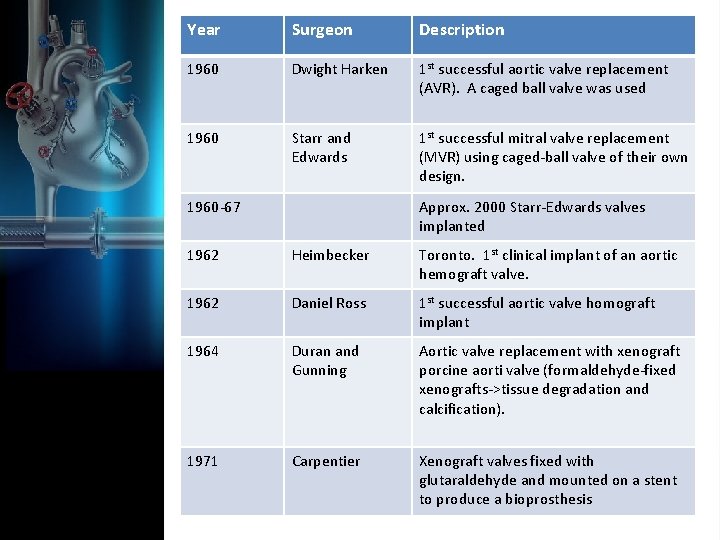
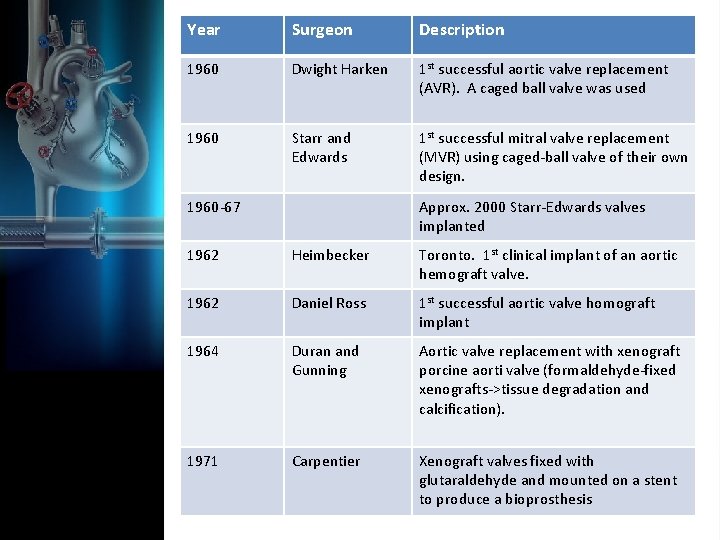
Year Surgeon Description 1960 Dwight Harken 1 st successful aortic valve replacement (AVR). A caged ball valve was used 1960 Starr and Edwards 1 st successful mitral valve replacement (MVR) using caged-ball valve of their own design. Valvular Surgery 1960 -67 Approx. 2000 Starr-Edwards valves implanted 1962 Heimbecker Toronto. 1 st clinical implant of an aortic hemograft valve. 1962 Daniel Ross 1 st successful aortic valve homograft implant 1964 Duran and Gunning Aortic valve replacement with xenograft porcine aorti valve (formaldehyde-fixed xenografts->tissue degradation and calcification). 1971 Carpentier Xenograft valves fixed with glutaraldehyde and mounted on a stent to produce a bioprosthesis
• 4 1858 - Improved bottle stopper conceptual impetus for the first successful ball and cage design
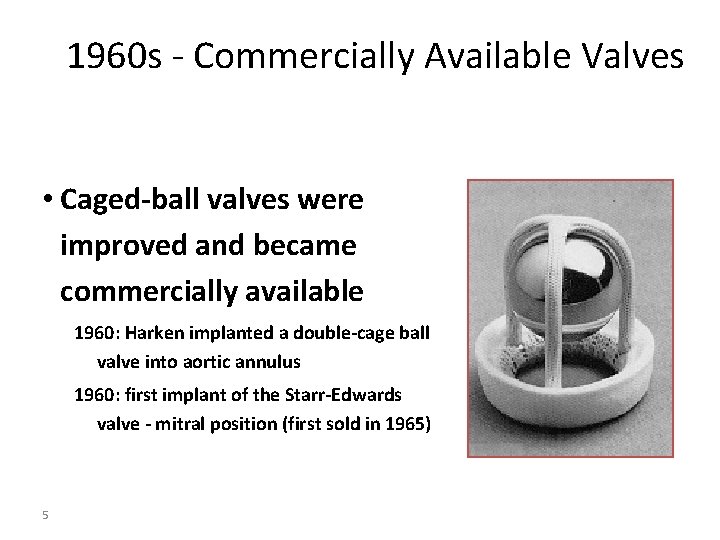
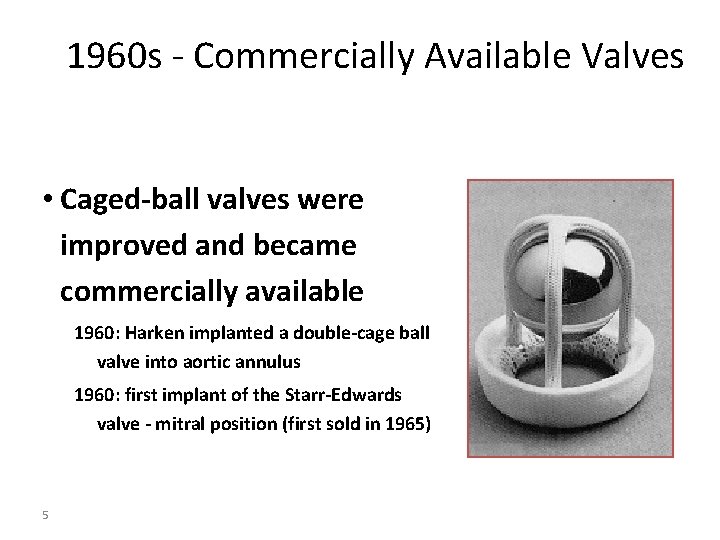
1960 s - Commercially Available Valves • Caged-ball valves were improved and became commercially available 1960: Harken implanted a double-cage ball valve into aortic annulus 1960: first implant of the Starr-Edwards valve - mitral position (first sold in 1965) 5
Prosthetic Heart Valve Management
Prosthetic Heart Valve Management • • Post-operative surveillance Prevention of infection Prevention of thrombosis Management of complications
Surveillance • Initial post-op visit: – H&P, CXR, EKG –class 1 – 2 D echo – class 1 if unsatisfactory…other studies – Labs: CBC, INR
Surveillance • Later visits: (patients without complications) – Routine follow-up yearly. Earlier if clinical change—Class I – Routine serial echo—Class IIb • Echo if change in exam • New regurgitation—echo every 3 -6 months.
Prevention of Infection • Class I – 2% risk of infection at 14 days with no prophylaxis. • Dental procedures • Invasive Respiratory procedures with incision or biopsy • Surgery involving infected skin or musculoskeletal tissue
Prevention of Infection 30 -60 min before procedure • Amoxicillin 2 g PO/Ampicillin 2 g IV/IM • Cephalexin 2 g PO • Azithromycin 500 mg PO • Clindamycin 600 mg PO or IV • Cefaxolin or Ceftriaxone 1 g IV/IM
Anticoagulation • Mechanical valves: – Risk of thromboembolic event • Untreated: up to 8% per year • Treated: less than 2% per year – Mitral greater risk than aortic – Higher risk early post-operatively • Bioprosthetic valves: – 0. 7% per year risk
Anticoagulation • All valves require anticoagulation – Duration – Agent(s) • Valve type and position • Patient risk factors – Atrial fibrillation – Previous thromboembolic event – Hypercoagulable state – Low EF < 30% • Contraindications
Anticoagulatioin • Aspirin 75 -100 mg daily – All patients – class 1 – Use alone with bioprosthetic AVR and MVR with no risk factors • Coumadin (INR 2. 0 -3. 0) – Mechanical AVR bileaflet, no risk factors – Bioprosthetic • First 3 months – class 2 a • Long term with risk factors.
Anticoagulation • Coumadin (INR 2. 5 -3. 5) – All others • Starr-Edwards run higher >3. 0
Anticoagulation • Events while at target: – INR 2 -3: increase to 2. 5 to 3. 5 – INR 2. 5 -3. 5: increase to 3. 5 to 4. 5 • Short term interruption: – Bileaflet AVR no risk factors: No bridge – Bridge all others with UFH – LMWH is class 2 b – FFP in emergencies – No vitamin K
Complications • • • Structural valve deterioration Non-structural Valve Dysfunction Thrombosis and Embolism Valvular endocarditis Hemolysis
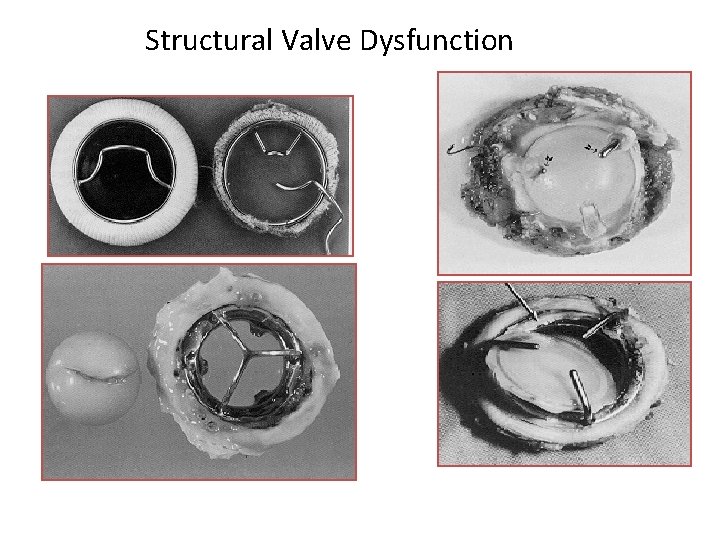
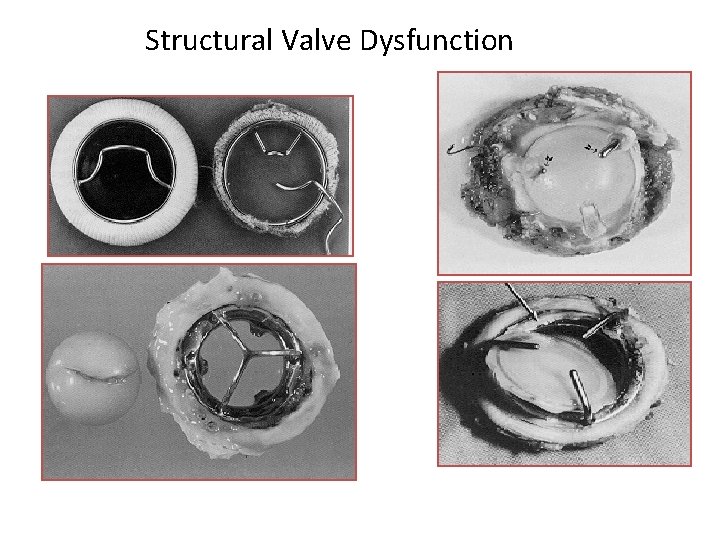
Structural Valve Dysfunction
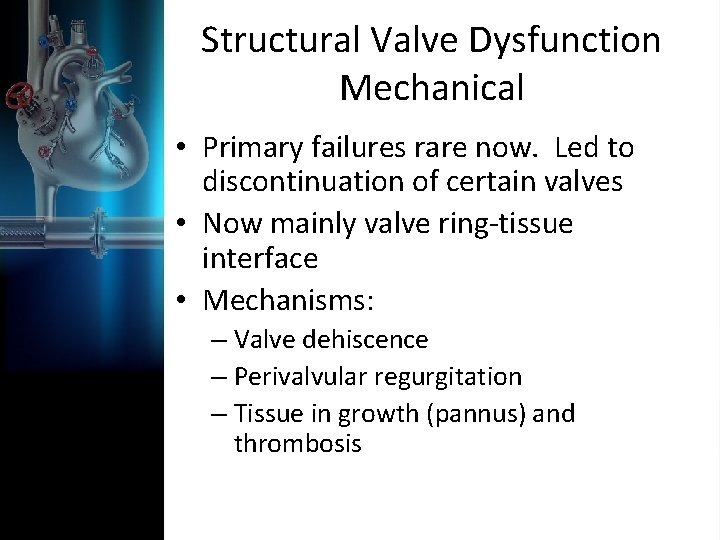
Structural Valve Dysfunction Mechanical • Primary failures rare now. Led to discontinuation of certain valves • Now mainly valve ring-tissue interface • Mechanisms: – Valve dehiscence – Perivalvular regurgitation – Tissue in growth (pannus) and thrombosis
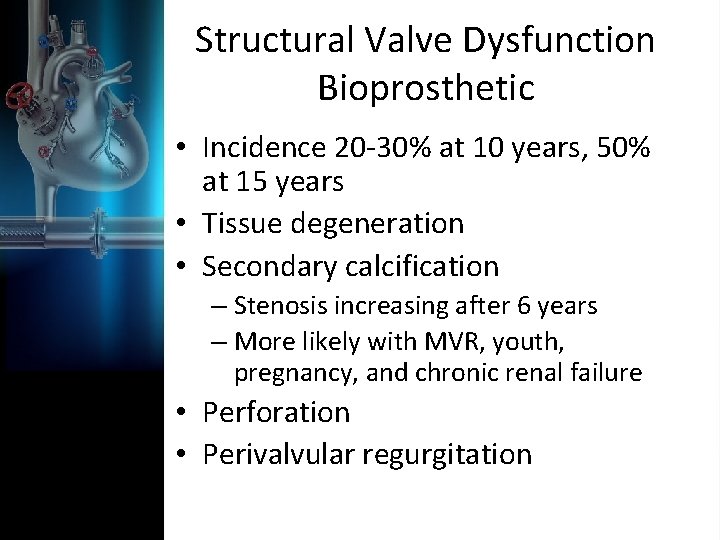
Structural Valve Dysfunction Bioprosthetic • Incidence 20 -30% at 10 years, 50% at 15 years • Tissue degeneration • Secondary calcification – Stenosis increasing after 6 years – More likely with MVR, youth, pregnancy, and chronic renal failure • Perforation • Perivalvular regurgitation
Nonstructural Valve Dysfunction • Clinically significant obstruction in the setting of normal prosthetic function • Patient prosthetic mismatch • Occurs mostly in older women • Thrombus and Pannus
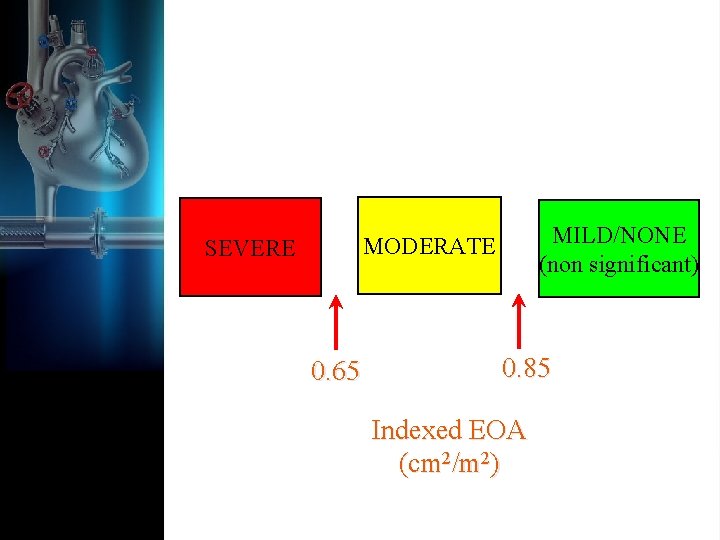
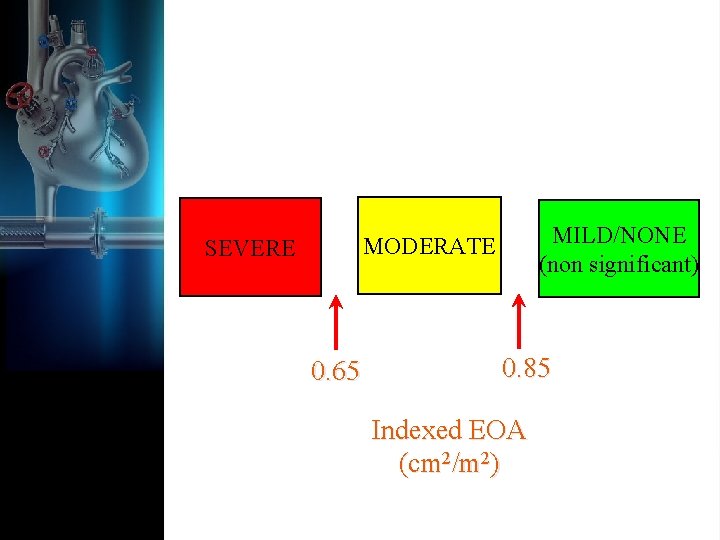
MILD/NONE (non significant) MODERATE SEVERE 0. 65 0. 85 Indexed EOA (cm 2/m 2)
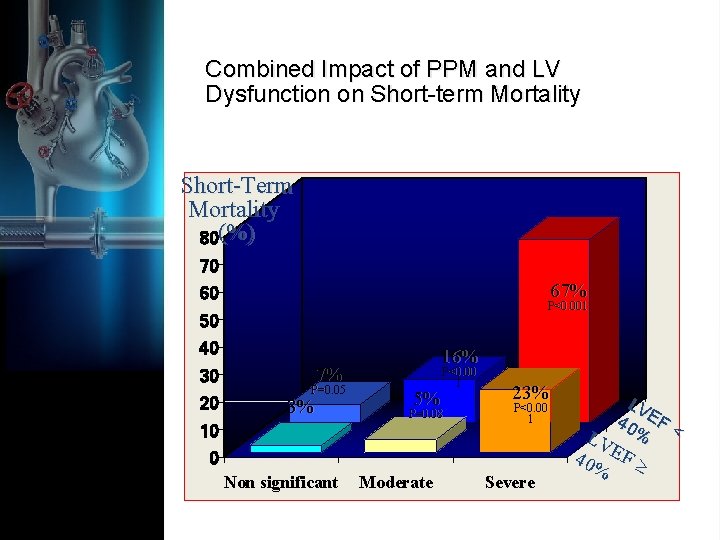
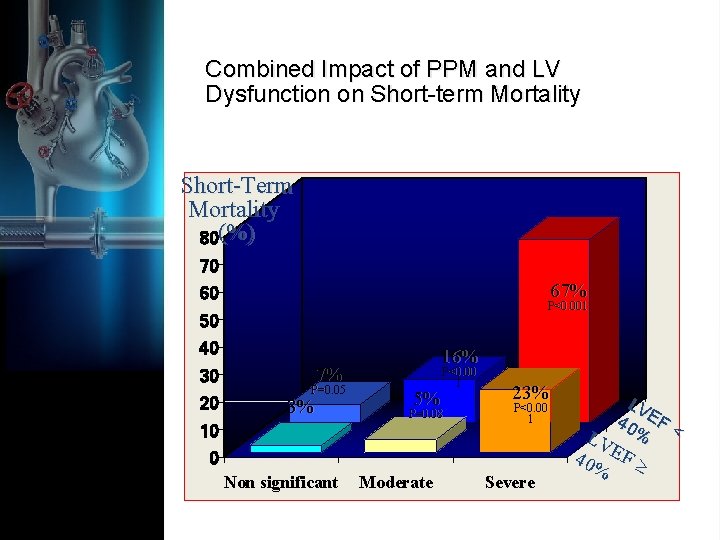
Combined Impact of PPM and LV Dysfunction on Short-term Mortality Short-Term Mortality 80(%) 70 67% 60 P<0. 001 50 40 30 20 16% 7% P=0. 05 3% 5% P<0. 00 1 P=0. 08 10 23% P<0. 00 1 0 Non significant Moderate Severe LV 40 EF < % LV 40% EF
Thrombosis and Embolism • Incidence 0. 6% to 2. 3% per patient year – Anticoagulated mechanical rate same as unanticoagulated bioprosthetic – Mitral position greater risk than aortic – Tricuspid greatest risk • Intrinsic thrombogenicity of valve materials, flow turbulence and stagnation, shear stresses, risk factors
Valve thrombosis • Echo, TEE, Fluoroscopy, MRI/CT • Thrombolysis – 70 -90% effective – Mortality 4 -12% acutely – Better for right sided valves – Duration < 24 hours • Surgery – Class 2 a for large clot, NYHA 3 -4 – Class 1 small clot, failure or contraindications to lysis
Embolism • Mechanical valves – No anticoagulation: 4% per year – Aspirin: 2% per year – Coumadin (therapeutic) 1% per year – Mitral valves twice the risk of aortic valves
Prosthetic valve endocarditis • Yearly risk 0. 5% despite prophylaxis • Highest risk MVR • No difference mechanical and bioprosthetic • Risk greatest in first 6 months • Usually involves the valve ring • Substantial mortality
Prosthetic Valve Endocarditis • Medical – Hospitalize at CV surgery center – Delay antibiotics until organism identified – TEE – Prolonged antibiotics with ID guidance • Surgery – Heart failure, abscess, dehiscence, relapsing infection, failed antibiotic
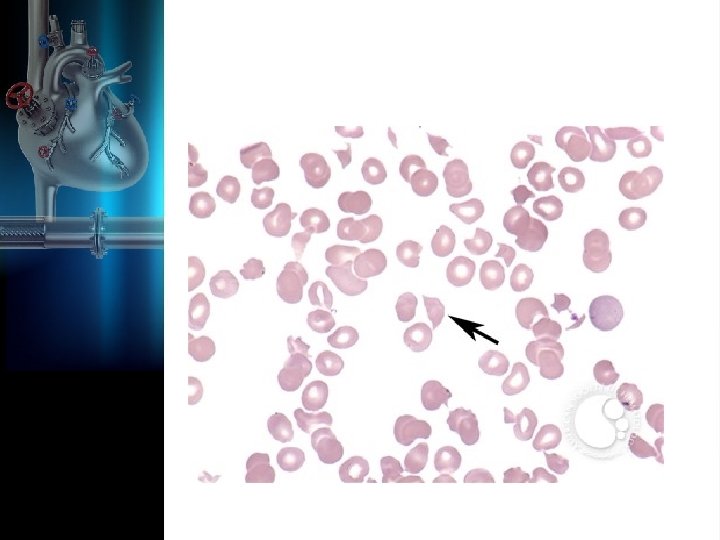
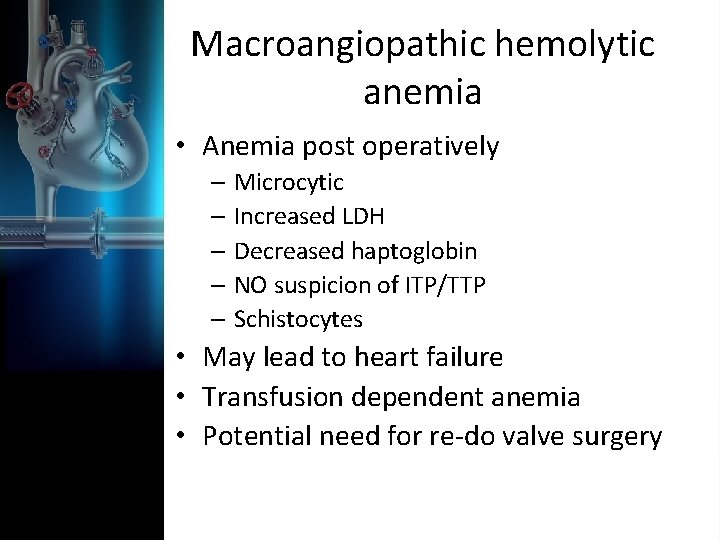
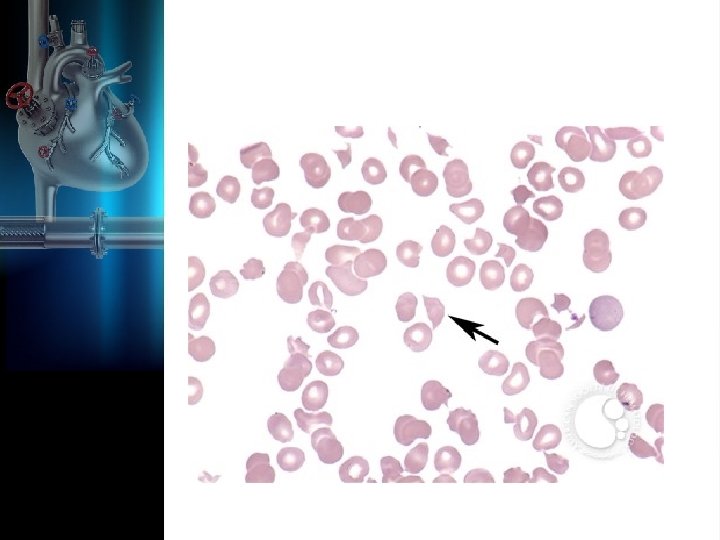
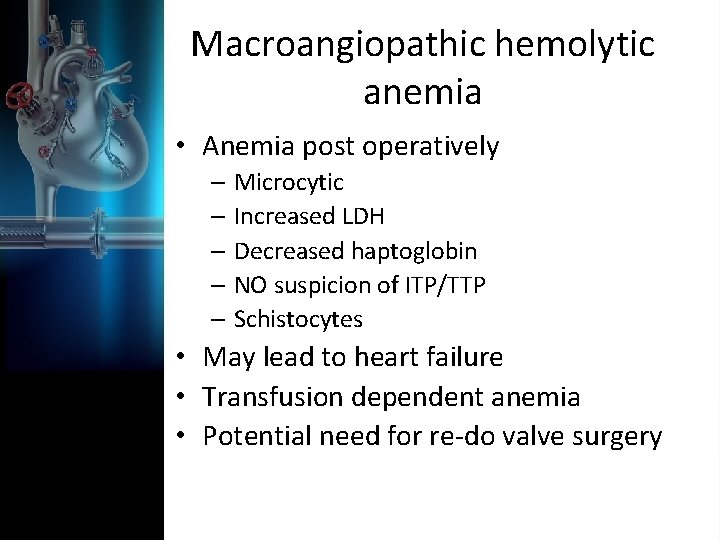
Macroangiopathic hemolytic anemia • Anemia post operatively – Microcytic – Increased LDH – Decreased haptoglobin – NO suspicion of ITP/TTP – Schistocytes • May lead to heart failure • Transfusion dependent anemia • Potential need for re-do valve surgery
Summary • Prosthetic valves are not a cure for valvular disease • Associated with large number of potential medical management issues • Careful post-operative valvular surveillance is important
Questions?