Ectopic pregnancy Dr F Mostajeran MD Ectopic pregnancy






- Slides: 27
Ectopic pregnancy Dr. F Mostajeran MD

§ Ectopic pregnancy remains § Leading cause life/hreatening F- Trimester (morbidity) § Medical therapy method terexate as standard first line therop. Surgery § Hemorrhage? § Medical failures § Neglected cases § Medical contraindicated

Incidence E. P o Unprecedented sexual liberties. o ↑Ascertainment E. P o ↑ART o Leading cause maternal death U. S 5 -6% all M. death
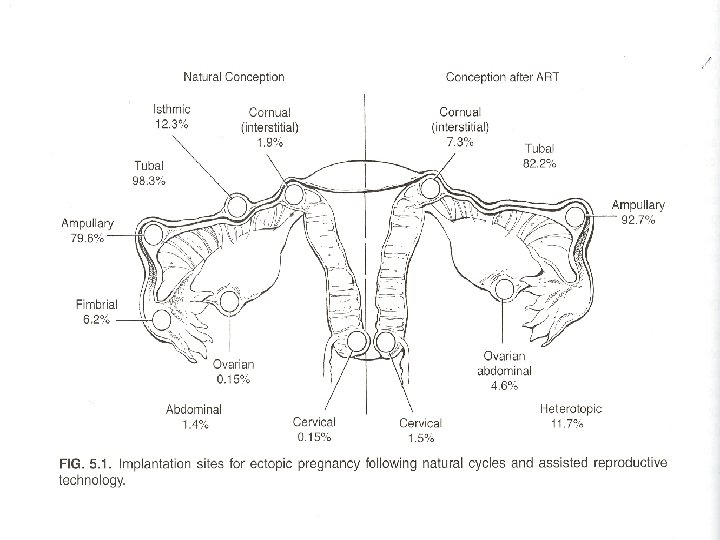
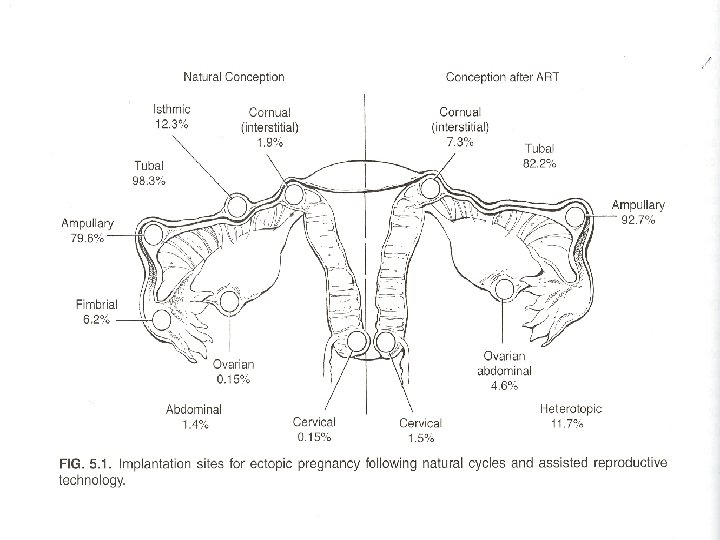
Pathogenesis • Ability tube transport gametes embryos • Clinical picture • Most common site Tub 98 -3% • Ampoule – isthmus – fimbrial cornual. • Rarely abdominal – ovarian – cervical. site E. P

• Proliferating trophoblast • Tubale wall • Growth may extend luminal mucosa. • Muscularis- serosa full thickness blood vessels • Distorts tube stretches serosa → pain bleeding takes phase. • 80% embryo degenerates. • 50% often clinically silent. • Tubal abortion self limited.
Risk factors o Needs aggressive monitoring pregnancy immediately after first missed menses Ø High risk • Tubal surgery (21) • Risk factors • Tubal ligation • Tubal Epithelial damage. • Previous E. P (6 -8) • I U D , Morning after pill • ART
• Moderate risk • Infertility • PID • Multiple sexual partners • Salpingitis ü Low risk • Cigarette • Vaginal douching first intercourse <18
• Signs and symptoms • Many E. P never produce symptoms rather • Timely diagnosed and treated (H. R) • If diagnosis → delayed → classic triad. • Amenorrhea , irregular V. B , lower ab- pain. • Sudden sever ab pain 90 -100% symptomatic patient. • Pain radiating shoulder. • Syncope shock → hemoperitaneum. ( up to 20%)

• Most common signs ab EX • 90% tenderness , rebound tenderness in 70%. • P. EX nonspecific. • 2⁄3 C-motion tenderness. • Adnexal mass 50%.

• Diagnosis • Diag as early as 4. 5 WK. • Visualization is frequently not possible. • Traditional laparoscopic visualization rarely necessary. • Routine diagnostic Tests. • Serial 3 HCG. • U. S • Progesterone levels. • U - curettage.
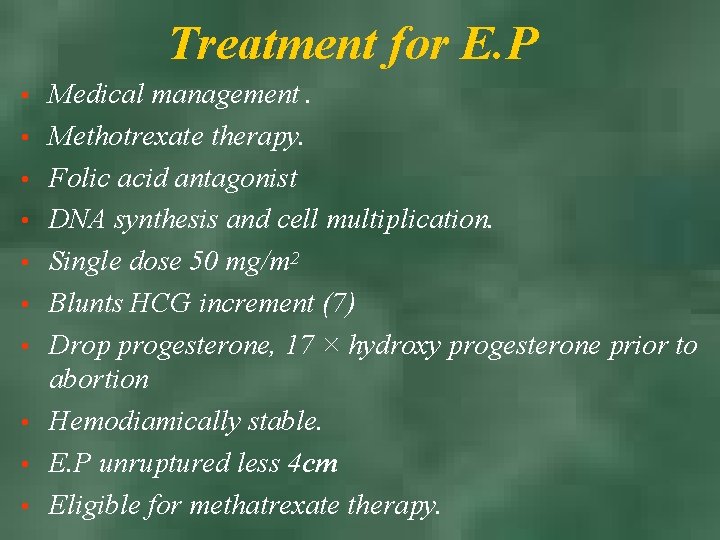
Treatment for E. P • • • Medical management. Methotrexate therapy. Folic acid antagonist DNA synthesis and cell multiplication. Single dose 50 mg/m 2 Blunts HCG increment (7) Drop progesterone, 17 × hydroxy progesterone prior to abortion Hemodiamically stable. E. P unruptured less 4 cm Eligible for methatrexate therapy.
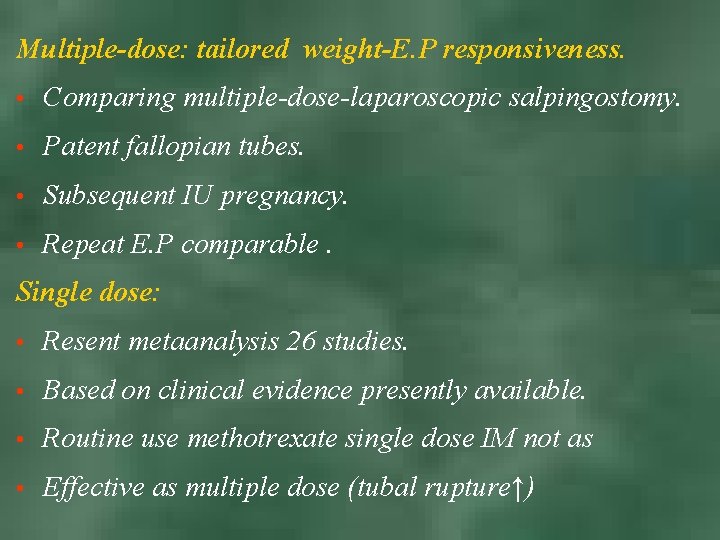
Multiple-dose: tailored weight-E. P responsiveness. • Comparing multiple-dose-laparoscopic salpingostomy. • Patent fallopian tubes. • Subsequent IU pregnancy. • Repeat E. P comparable. Single dose: • Resent metaanalysis 26 studies. • Based on clinical evidence presently available. • Routine use methotrexate single dose IM not as • Effective as multiple dose (tubal rupture↑)
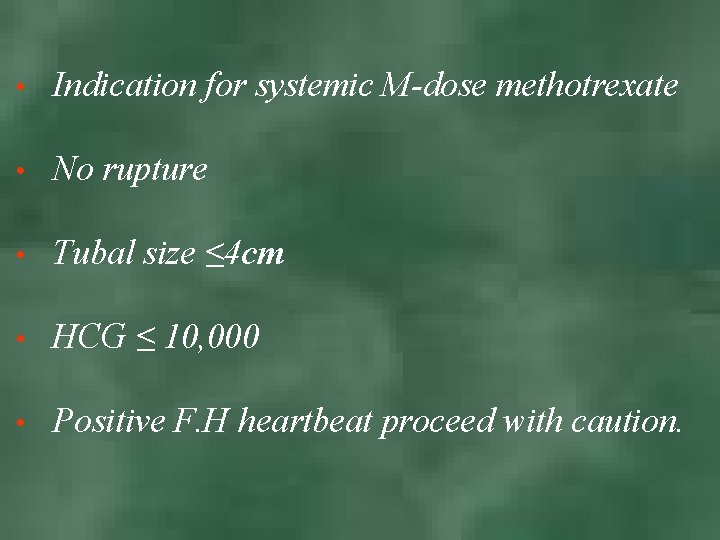
• Indication for systemic M-dose methotrexate • No rupture • Tubal size ≤ 4 cm • HCG ≤ 10, 000 • Positive F. H heartbeat proceed with caution.
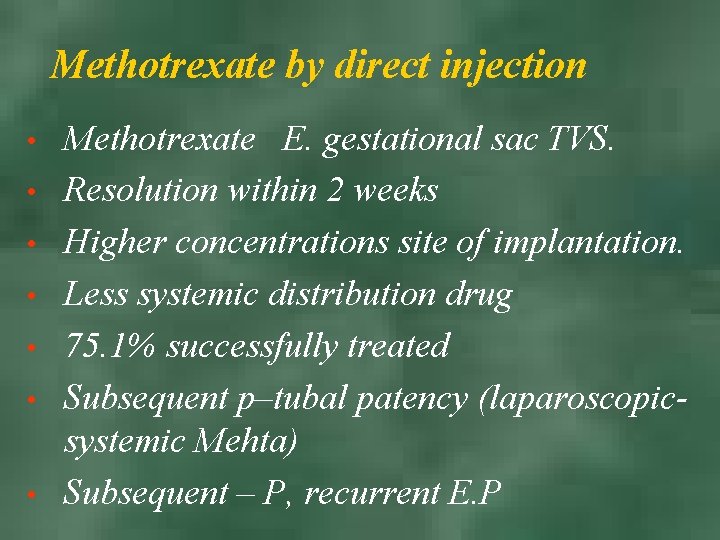
Methotrexate by direct injection • • Methotrexate E. gestational sac TVS. Resolution within 2 weeks Higher concentrations site of implantation. Less systemic distribution drug 75. 1% successfully treated Subsequent p–tubal patency (laparoscopicsystemic Mehta) Subsequent – P, recurrent E. P
Methotrexate failure o Pain is sever and persistent (>12 h 4 -12 3 -7 after start therapy) o Falling HCT o Orthostatic hypotension.
Side effects • High dose • Bone marrow supp • Hepatotoxicity • Stomatitis • Pulmonary fibrosis • Alopecia • Photosensitivity • Infrequent in E. P therapy

Surgical Treatment • 1884 E. P laparotomy salpingectom. • 1953 salpingostomy • Manual fimbrial expression • Segmental resection.
• Ruptured E. P • Laparoscopy – laparotomy – salpingectomy. • Inpatients hypovolemic shock. • Surgery is choice.
Stable E. P • If methotrexate contraindicated. • Laparoscopic salpigostomy first surgical choice. • Salpingectomy v Laparoscopy v Laparotomy
Expectant management • E. P may resolve spontaneously • 67. 2% E. P resolved without surgery (over treats) • Falling 3 HCC under 1000 fallowed with conservative expectant management • With low initial and falling HCG
Rare types of E. P • Abdominal pregnancy • 1⁄8000 birth • M. M 5. 1⁄1000 7. 7 higher than other E. P • (Higher due to delay in diagnosis) prognosis poor
Primary - Secondary • • Symptoms → normal for pregnancy to sever if time permits Abdominal pain intra abdominal hemorrhage shock Primary rare usually abort Secondary (reimplantation → abortion , rupture) U. S choice empty uterus If fetus near viability → hospitalization Adequate blood, bowel preparation Placenta removed unless major vessels, vital organ methotrexate
Ovarian pregnancy • • Most common form abdominal pregnancy less than 3% of E. P Clinical finding similar tubal E. P ab-pain , V. B Amenorrhea 30% hemodynamic instability → rupture Usually young multiparous cause Treatment → systectomy, wedge resection or oophorectomy
Cornual pregnancy or interstitial pregnancy • 4. 7% E. P 2. 2% M. mortality • Most frequent symptom menstrual aberration • Abdominal pain V. B, shock → rapture uterine(9 -12 nk) • Risk factor previous salpingectomy • Repeat U. S with Doppler flow studies → early diagnosis • Cornual resection lapa - resection systemic methatraxate local
Cervical pregnancy 1⁄12000 Most common risk factor o D. C o Previous CS o IVF • Symptom most common V. B painless • C. EP usually diagnosis incidentally during routine U. S or at time surgery for abortion • Cervix enlarged- globular, distended it appears cyanotic hyperemic soft • Diagnosis – US, MRI , GSOC below C. OS, • Metha, U. Artery embolization, hysterectomy
Heterotopic pregnancy • E. P + intrauterine pregnancy 1⁄6778 • Most causes diagnosed after sign symptoms develop admitted for emergency surgery • Lower abdominal pain serial 3 HCG not helpful
 Icd 10 code for ectopic pregnancy
Icd 10 code for ectopic pregnancy Implantation bleeding pictures
Implantation bleeding pictures Hydrocolpus
Hydrocolpus Horseshoe kidney
Horseshoe kidney Ectopic fat definition
Ectopic fat definition Ectopic mulberry molars
Ectopic mulberry molars Re entry
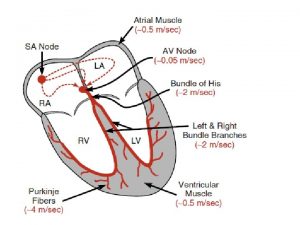
Re entry For teenage pregnancy
For teenage pregnancy Taxonomy of goat
Taxonomy of goat How to calculate insulin dose in pregnancy
How to calculate insulin dose in pregnancy Implantation steps
Implantation steps Nursing theories related to teenage pregnancy
Nursing theories related to teenage pregnancy Partial molar pregnancy
Partial molar pregnancy Hormones during pregnancy
Hormones during pregnancy Pregnancy gestational diabetes mellitus
Pregnancy gestational diabetes mellitus Pregnancy declaration
Pregnancy declaration For teenage pregnancy
For teenage pregnancy Rapiprazole
Rapiprazole High levels of fibrinogen in pregnancy
High levels of fibrinogen in pregnancy Lack of knowledge in teenage pregnancy
Lack of knowledge in teenage pregnancy Role of nurse in reproductive health ppt
Role of nurse in reproductive health ppt Endoscopy in pregnancy guidelines
Endoscopy in pregnancy guidelines Afe pregnancy
Afe pregnancy The standard days method
The standard days method Haemaccel drip uses in pregnancy
Haemaccel drip uses in pregnancy Malaria in pregnancy definition
Malaria in pregnancy definition Chapter 4 prenatal care and adaptations to pregnancy
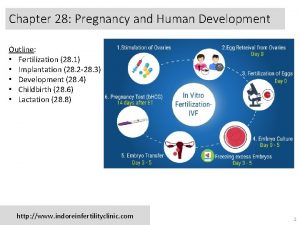
Chapter 4 prenatal care and adaptations to pregnancy Pregnancy category a
Pregnancy category a