ECT Service RPIW Report Out Report Out Presentation

- Slides: 39
ECT Service RPIW Report Out
Report Out Presentation Current State and Problem identified Ideas and Key Improvements – Trust wide Service at multiple sites – Staffing – Transport and Booking Capacity of the service
What is the problem we are trying to solve? Electro Convulsive Therapy Are our ECT processes as high quality and efficient as they can be? Waiting within Clinics ‘Waiting lists’ Means that Service Users don’t get treatment immediately Service User experience- waiting, again!
What is the problem we are trying to solve? Maximise Service User experience by- 1. Maximise quality and efficiency across Southern Health to improve access 2. Reducing waiting times in the process 3. Eliminating waiting lists for treatment
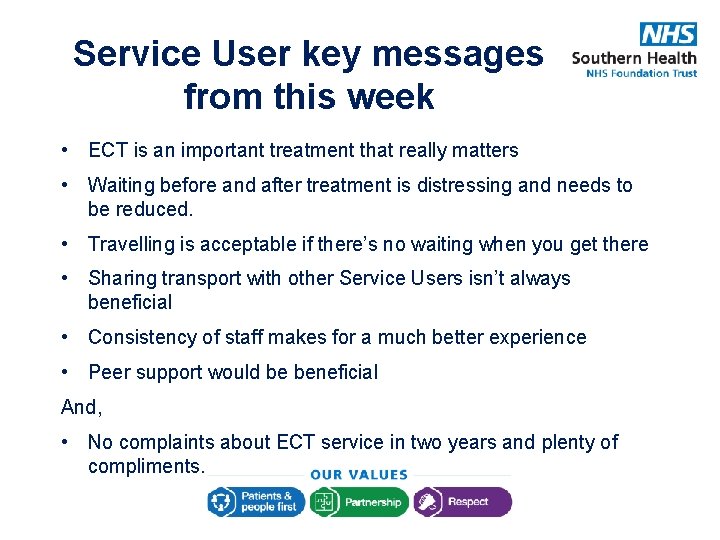
Service User key messages from this week • ECT is an important treatment that really matters • Waiting before and after treatment is distressing and needs to be reduced. • Travelling is acceptable if there’s no waiting when you get there • Sharing transport with other Service Users isn’t always beneficial • Consistency of staff makes for a much better experience • Peer support would be beneficial And, • No complaints about ECT service in two years and plenty of compliments.
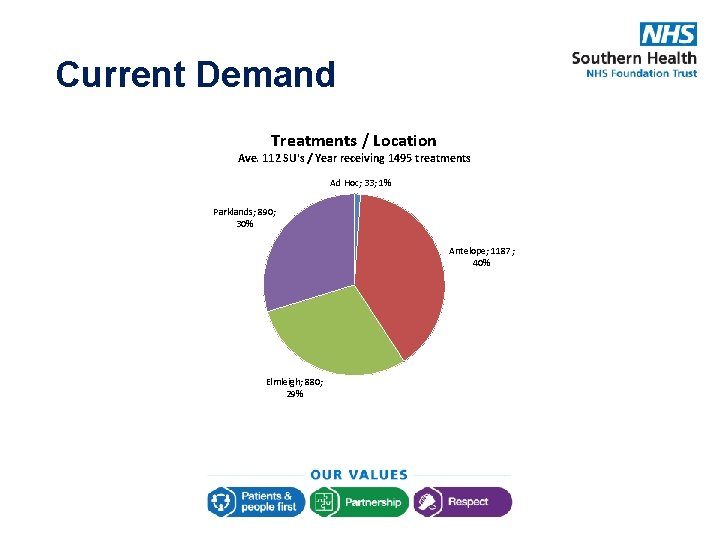
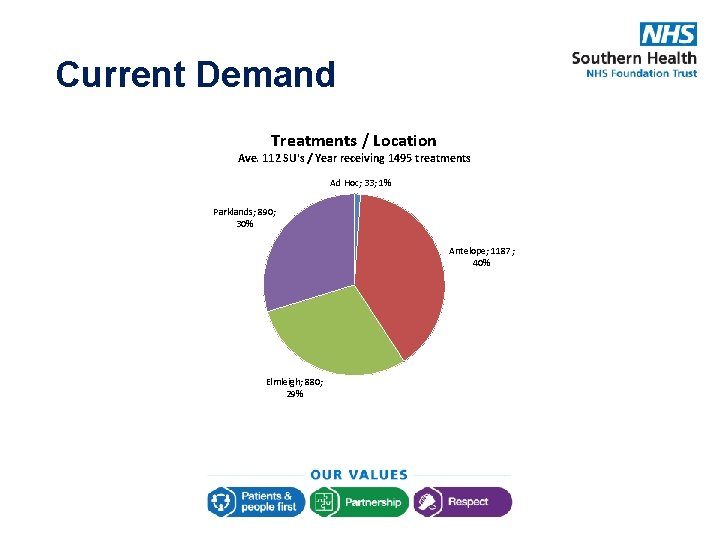
Current Demand Treatments / Location Ave. 112 SU's / Year receiving 1495 treatments Ad Hoc; 33; 1% Parklands; 890; 30% Antelope; 1187; 40% Elmleigh; 880; 29%
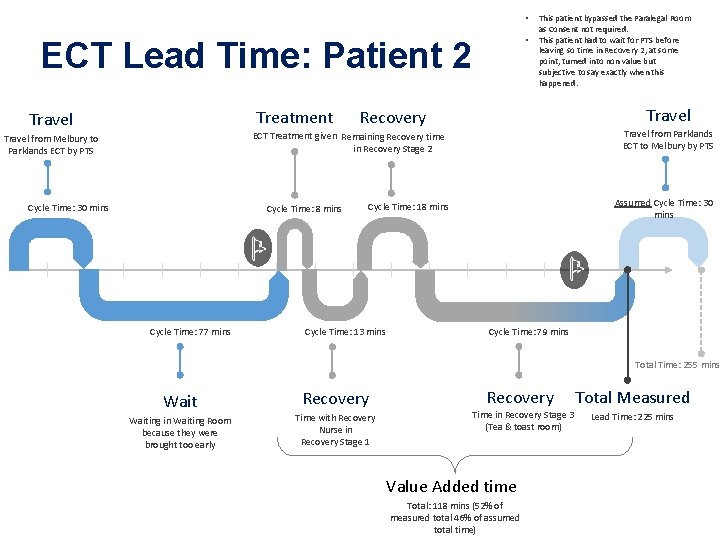
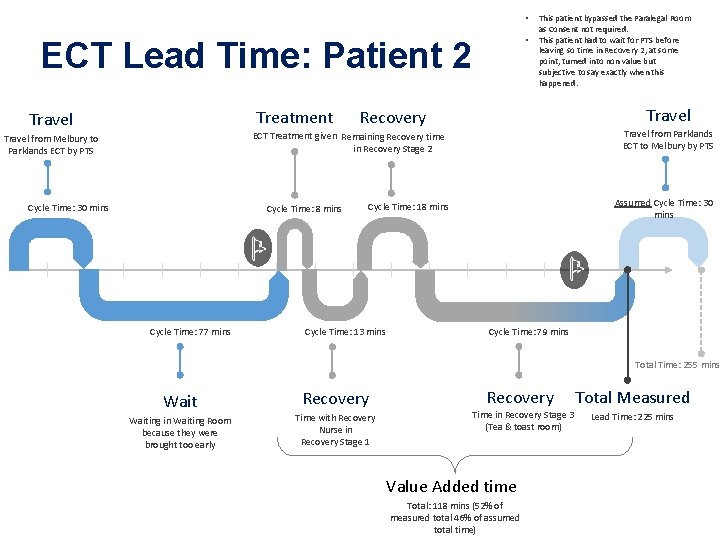
• • ECT Lead Time: Patient 2 Treatment Travel This patient bypassed the Paralegal Room as Consent not required. This patient had to wait for PTS before leaving so time in Recovery 2, at some point, turned into non value but subjective to say exactly when this happened. Travel Recovery Travel from Parklands ECT to Melbury by PTS ECT Treatment given Remaining Recovery time in Recovery Stage 2 Travel from Melbury to Parklands ECT by PTS Cycle Time: 30 mins Cycle Time: 8 mins Cycle Time: 77 mins Assumed Cycle Time: 30 mins Cycle Time: 18 mins Cycle Time: 13 mins Cycle Time: 79 mins Total Time: 255 mins Waiting in Waiting Room because they were brought too early Recovery Time with Recovery Nurse in Recovery Stage 1 Recovery Time in Recovery Stage 3 (Tea & toast room) Value Added time Total: 118 mins (52% of measured total 46% of assumed total time) Total Measured Lead Time: 225 mins
Ideas and Key Improvements 63 unique ideas generated Key themes • Improving booking and transport process • Trust wide service • Staffing and standardising staffing model
Trust wide Service on multiple sites
Our aim is to improve quality and efficiency of ECT services That is made difficult by how we are currently organised…. • • • 3 different services and teams 3 different budgets 3 different management chains 3 different ways of working 3 different contracts / SLAs for staff supporting the service (e. g. anaesthetist) Limited sharing across sites in terms of issues, safety concerns, improvement opportunities • Inequitable demand, resources and activity across the 3 services • Difficulty in understanding peaks and troughs in individual sites and re-allocating demand across sites • Inconsistent roles / skills, difficulty recruiting staff, worries about succession planning, few development opportunities and little or no cross-cover to support routine gaps in resource Creating variable service user access to ECT and experience of the service
Our idea: One Trust-wide ECT Service operating across multiple sites “ 1” Delivering high quality and efficient services for ALL service users and staff
Benefits: One Trust-wide ECT Service operating across multiple sites • Equitable access and experience for service users • Sustainable staffing and improved workforce / succession planning • Standard systems, equipment and ways of working – both clinical and logistic • One line of accountability and speedy resolution of issues across sites • One system of governance and one set of data and information supporting it, promoting learning and improvement across all sites • Best use of resources and budget, balancing capacity with future demand, and able to flex resources across sites to manage peaks and troughs in demand operational issues
Benefits: One Trust-wide ECT Service operating across multiple sites • Equitable access and experience for service users • Sustainable staffing and improved workforce / succession planning simply… • Put Standard systems, equipment and ways of working – both and logistic • clinical We have the right people, with the right skills, working in the • One best line way. of accountability and speedy resolution of issues across • sites We can see what is happening and put things right quickly • One systemif of governance and one set of data and information and safely there’s a problem. it, promoting andquality improvement all • supporting We continue to deliver alearning safe, high service, across confident sites it’s the best it can be. • Best use of resources and budget, balancing capacity with future demand, and able to flex resources across sites to manage peaks and troughs in demand operational issues
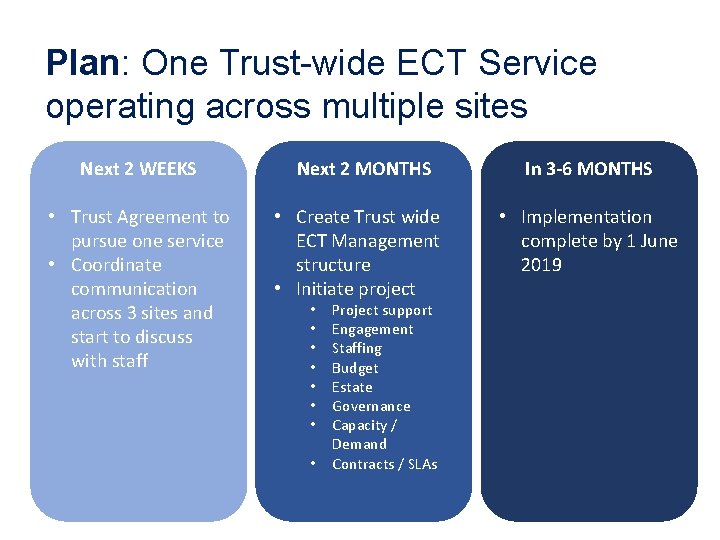
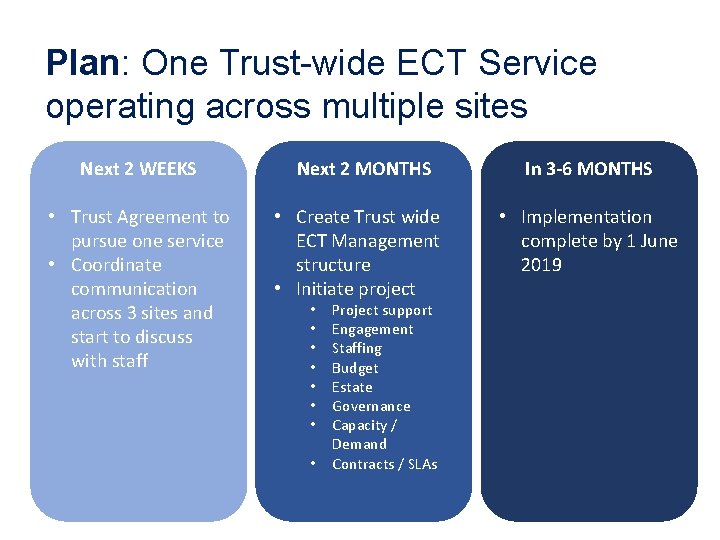
Plan: One Trust-wide ECT Service operating across multiple sites Next 2 WEEKS • Trust Agreement to pursue one service • Coordinate communication across 3 sites and start to discuss with staff Next 2 MONTHS • Create Trust wide ECT Management structure • Initiate project • • Project support Engagement Staffing Budget Estate Governance Capacity / Demand Contracts / SLAs In 3 -6 MONTHS • Implementation complete by 1 June 2019

Capacity generated by new approach
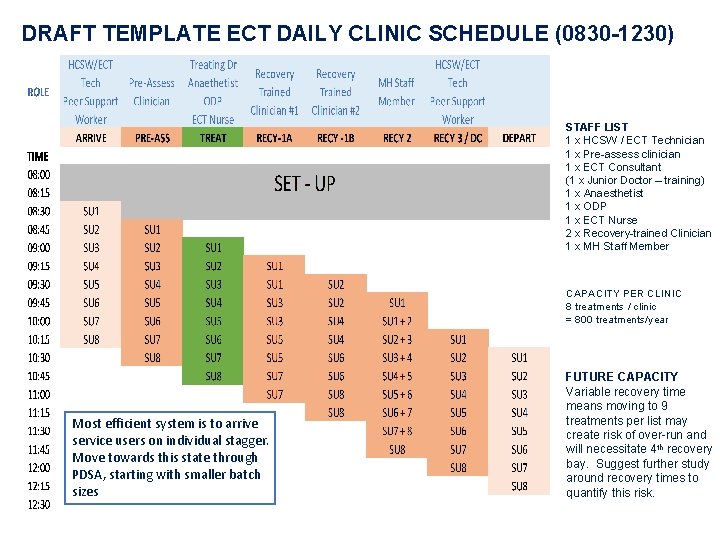
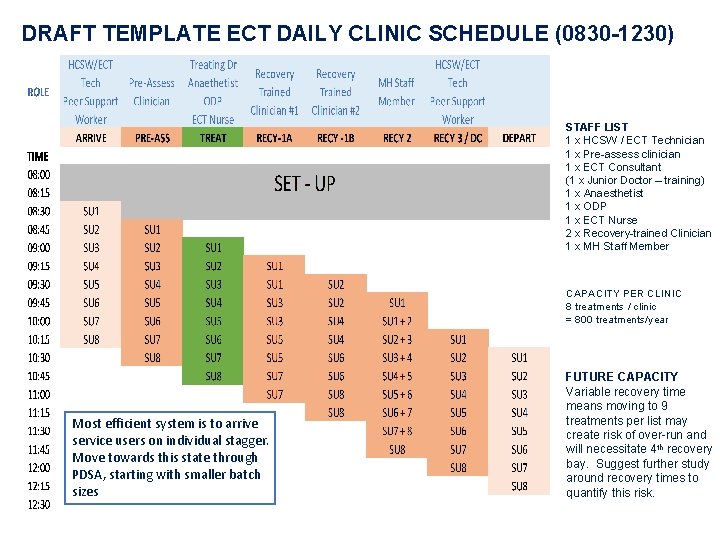
DRAFT TEMPLATE ECT DAILY CLINIC SCHEDULE (0830 -1230) STAFF LIST 1 x HCSW / ECT Technician 1 x Pre-assess clinician 1 x ECT Consultant (1 x Junior Doctor – training) 1 x Anaesthetist 1 x ODP 1 x ECT Nurse 2 x Recovery-trained Clinician 1 x MH Staff Member CAPACITY PER CLINIC 8 treatments / clinic = 800 treatments/year Most efficient system is to arrive service users on individual stagger. Move towards this state through PDSA, starting with smaller batch sizes FUTURE CAPACITY Variable recovery time means moving to 9 treatments per list may create risk of over-run and will necessitate 4 th recovery bay. Suggest further study around recovery times to quantify this risk.
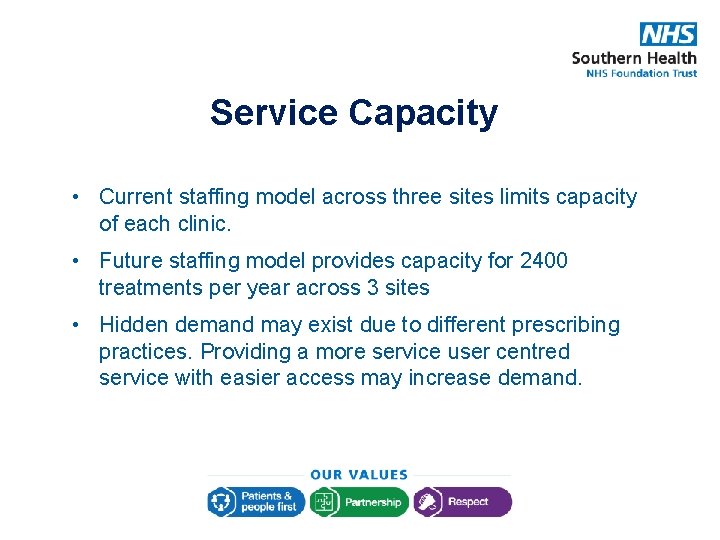
Service Capacity • Current staffing model across three sites limits capacity of each clinic. • Future staffing model provides capacity for 2400 treatments per year across 3 sites • Hidden demand may exist due to different prescribing practices. Providing a more service user centred service with easier access may increase demand.
Staffing
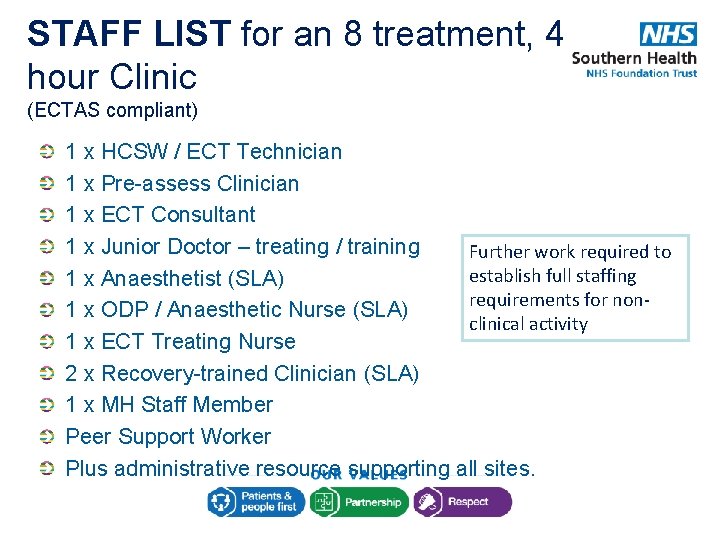
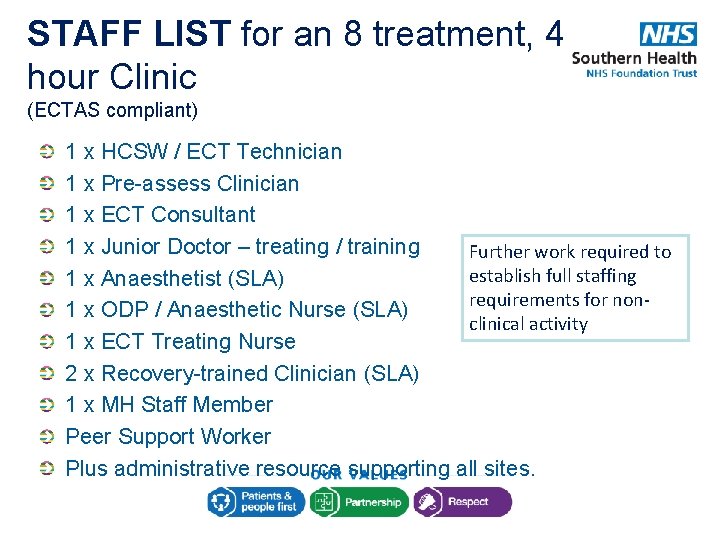
STAFF LIST for an 8 treatment, 4 hour Clinic (ECTAS compliant) 1 x HCSW / ECT Technician 1 x Pre-assess Clinician 1 x ECT Consultant 1 x Junior Doctor – treating / training Further work required to establish full staffing 1 x Anaesthetist (SLA) requirements for non 1 x ODP / Anaesthetic Nurse (SLA) clinical activity 1 x ECT Treating Nurse 2 x Recovery-trained Clinician (SLA) 1 x MH Staff Member Peer Support Worker Plus administrative resource supporting all sites.
Challenges Sufficient recovery trained staff Training of Junior Doctors Retention of skilled but unqualified staff Succession planning for all staff, particularly lead nurses and psychiatrists
Solutions Consistent and robust SLAs to provide Recovery Trained Staff: ODP, recovery nurse, anaesthetic nurse. Develop a peer support worker role Complete competencies for RMNs to support recovery. Develop a B 4 ECT technician role to provide Career Progression. Involve Junior Doctors in pre-assessment
Promote understanding of ECT Expand lead nurse to increase promotion Create a video about ECT to provide information for staff and service users Plan story board within 30 days Film within 60 days Release within 90 days
Peer Support in ECT Support patients in waiting areas before and/or after treatment Show patients around ECT suites prior to treatment starting Design/contribute to ECT literature Contribute to ECT education sessions Contribute to ECT forums Improve patient experience!
Benefits for Service Users and Carers Building up relationships – a familiar face Support in waiting areas, answering questions Advocacy – bridging the gap between Service User / Carer and clinic staff Shared experience – listening to Service User’s experience Signpost to other resources/literature Improve overall treatment outcome – more likely to complete treatment? Hope! Recovery is possible!
Benefits for Staff Free up clinical staff for clinical activities, for example, ’meet and greet' Support staff An example for other Trusts – demonstrate the benefits
New roles Develop business case for peer support worker and ECT technician roles – – – Job descriptions Link to wider Peer Support Programme Defining benefits 45 days to deliver business case 60 days to get a decision on business case 120 days to complete recruitment
Consistent Service Level Agreements (SLAs) Engage support from Contracts Department / expertise (30 days) Review current state with Contracts Department Define service requirements (60 days) Agree SLAs with Acute Trusts / Private Hospitals (by April 2019)
Transport and Booking
Transport What we’ve done this week Current state • Unreliable transport; service Met with transport and users arriving early/late developed collaborative • Service Users are generally working relationship given the same arrival time due Developed a joint to concerns about transport understanding of KPIs and • No perceived flexibility in processes Transport • Waiting areas become congested • Wait for transport particularly hard when service users are ready to go home
Transport Plan • Work towards standard and staggered booking system to be implemented • Develop appointment cards for service users • Develop patient centred survey to provide monitoring for review • Transport tracking system to be implemented in ECT suites • Review and track compliance with transport contract • Transport will be informed if service users are ready to go home earlier than time transport booked • Taxi will be booked if transport has not arrived by end of clinic time. • SCAS escalation and complaints processes to be shared and used when contract expectations are not met to enable meaningful feedback
Transport Plan - Timescales 30 days – All systems will be in place to be able to start giving timed appointments – includes: tracking system on ECT computers, training delivered to transport planners, review of previous booking processes, dissemination of complaints procedure, update of job description & competencies, appointment cards developed, escort survey & service user survey developed, baseline data collection completed, communication to referrers of new system for booking 60 days – Review of transportation timescale commitments, review of initial action plan, timed appointments started, survey launched, data collection in underway (march/april) 90 days – Present findings from transport survey & data collection to ECT forum including transport representatives: Review of success of appointment card system & transportation. Adaptations made, if required, and future review planned. Continued… ECT forum will continue to review transport & booking situation as a standard agenda item and report back to Quality & Governance Annually
Current Booking System Current State: • Service users are put on Ri. O who are not ready to have their first treatment • Pressure on staff to allocate service users a clinic slot before care pathway is fully complete • Reluctance to transport staff & service users to other ECT sites when local site does not have capacity • Communication between ECT area teams are sometimes not as robust as it should be
Proposed Standard Booking The Plan • Create generic email (within 30 days) • Create a single point of contact for referrals (within 30 days) which will incorporate: • People being considered for ECT will be put on a holding list until ready for treatment to commence • People will be added to Ri. O and assigned a clinic appointment only when care pathway is correctly completed • When preferred site has reached capacity an alternative site will be allocated
Booking Considerations The Plan • Conversation in advance of referral to determine which inpatient unit best meets needs, not necessarily local • Within the booking, determine priority and allocate based on criteria such as frailty, anxiety, physical health, dehydration status, etc.
Other ideas
24 hour Appropriate Adult Community service users undergoing ECT must be accompanied by an ‘appropriate adult’ for 24 hours following treatment. Where service users do not have someone to fulfil this role they end up being admitted into an inpatient bed. Efforts to try and avoid this are usually met with discussions about budget. We would like access to spot purchase of 24 hour ‘sit-in cover’ to avoid unnecessary admissions and the cost associated with this (e. g. out of area beds)
Other ideas continued • Explore Pre-clerking days for community patients with no access to physical health monitoring equipment. • Single stores to reduce issues with re-ordering essential equipment • Separate Clinic for Maintenance service users • Placements for students • Review Ri. O data capture to remove need for additional reporting mechanisms • Engagement with Solent Consultants to improve access for Solent service users • Unpick why some areas refer more than others • Nurse Administered ECT
Lessons Learnt • Service user involvement is essential • Ensure early engagement with Process Owner • Preparation is key – ensure problem to be solved is the problem • Early planning and support for securing Clinicians’ time • Potentially involve staff and Service Users who have previously been through RPIW in Day 1 • ‘Connect’ day 1 to the rest of the week • Ensure team involved know that they own the ‘solution/s’ from the start and what Report Out for Day 5 entails
Service User Reflection