Eating Disorders and Disordered Eating in Persons with
- Slides: 34
Eating Disorders and Disordered Eating in Persons with Type 1 Diabetes (T 1 DM): Identification, Treatment, and Prevention Barbara J. Anderson, Ph. D. Professor of Pediatrics Baylor College of Medicine Houston, TX
Overview Eating Disorders- definitions of psychiatric conditions n Disordered eating in the context of Type 1 Diabetes (T 1 DM) n Identifying, treating, and preventing disordered eating in pts. with T 1 DM n
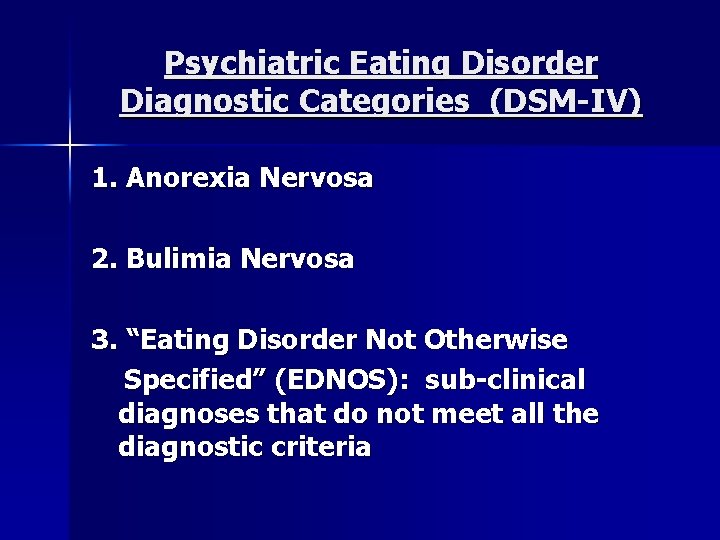
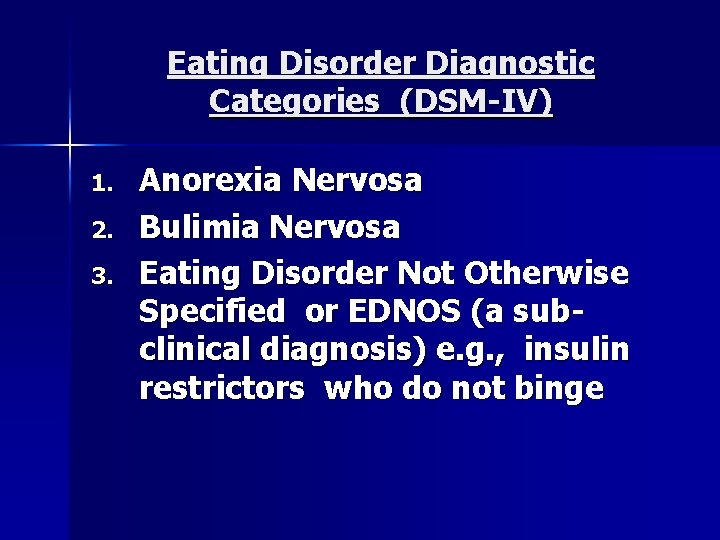
Psychiatric Eating Disorder Diagnostic Categories (DSM-IV) 1. Anorexia Nervosa 2. Bulimia Nervosa 3. “Eating Disorder Not Otherwise Specified” (EDNOS): sub-clinical diagnoses that do not meet all the diagnostic criteria
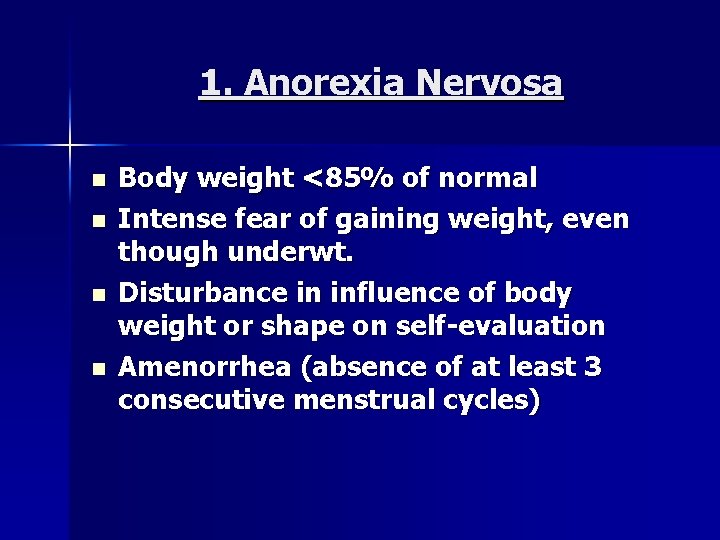
1. Anorexia Nervosa n n Body weight <85% of normal Intense fear of gaining weight, even though underwt. Disturbance in influence of body weight or shape on self-evaluation Amenorrhea (absence of at least 3 consecutive menstrual cycles)
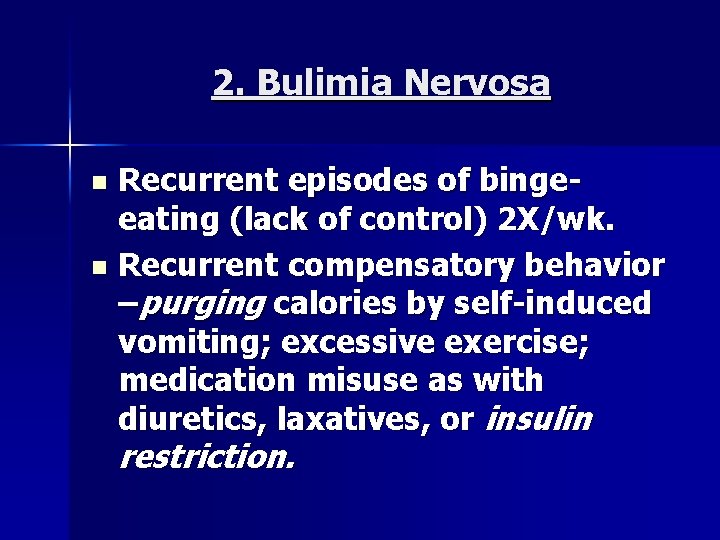
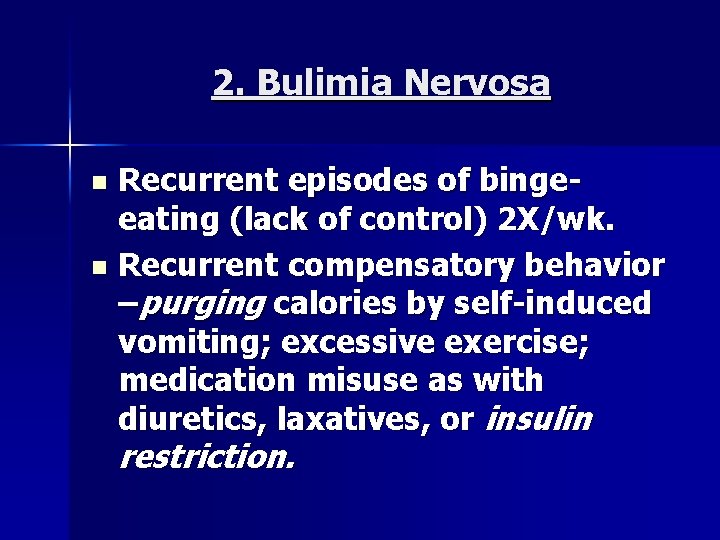
2. Bulimia Nervosa Recurrent episodes of bingeeating (lack of control) 2 X/wk. n Recurrent compensatory behavior –purging calories by self-induced vomiting; excessive exercise; medication misuse as with diuretics, laxatives, or insulin n restriction.
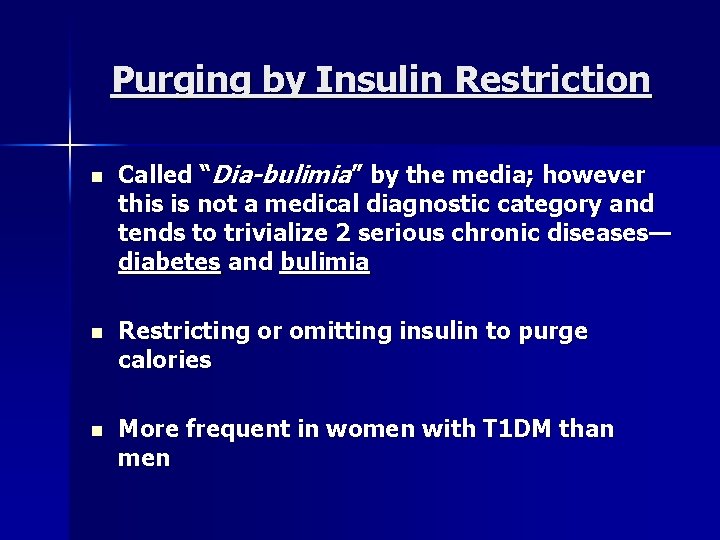
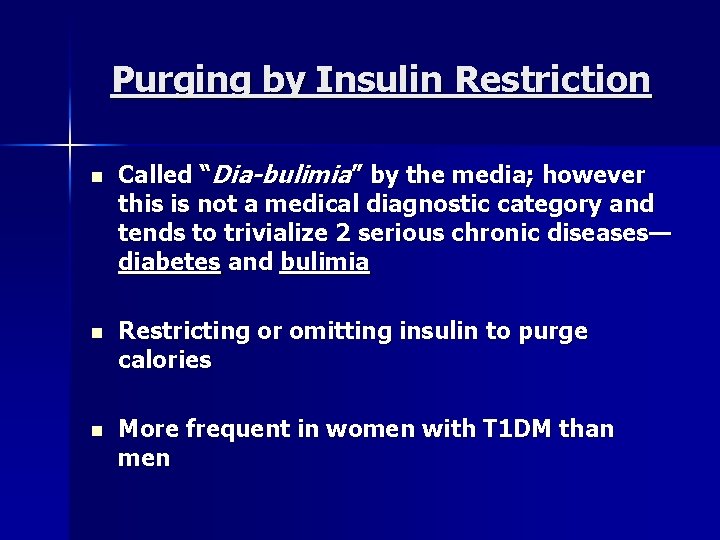
Purging by Insulin Restriction n Called “Dia-bulimia” by the media; however this is not a medical diagnostic category and tends to trivialize 2 serious chronic diseases— diabetes and bulimia n Restricting or omitting insulin to purge calories n More frequent in women with T 1 DM than men
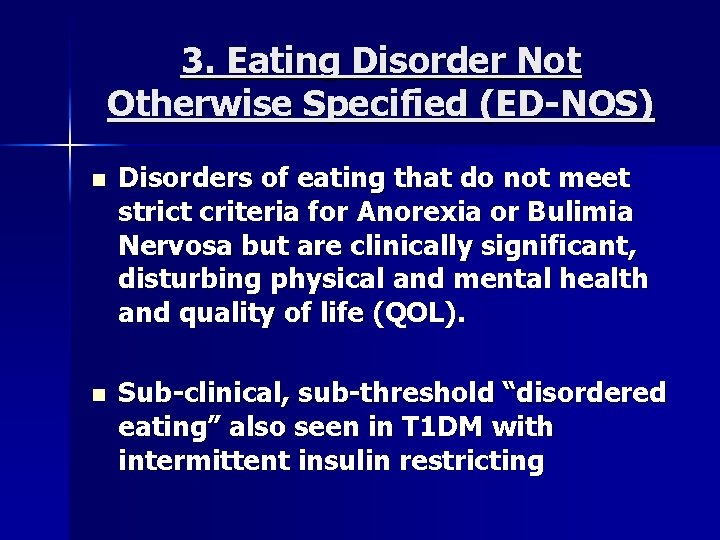
3. Eating Disorder Not Otherwise Specified (ED-NOS) n Disorders of eating that do not meet strict criteria for Anorexia or Bulimia Nervosa but are clinically significant, disturbing physical and mental health and quality of life (QOL). n Sub-clinical, sub-threshold “disordered eating” also seen in T 1 DM with intermittent insulin restricting
Eating Disorder Diagnostic Categories (DSM-IV) 1. 2. 3. Anorexia Nervosa Bulimia Nervosa Eating Disorder Not Otherwise Specified or EDNOS (a subclinical diagnosis) e. g. , insulin restrictors who do not binge
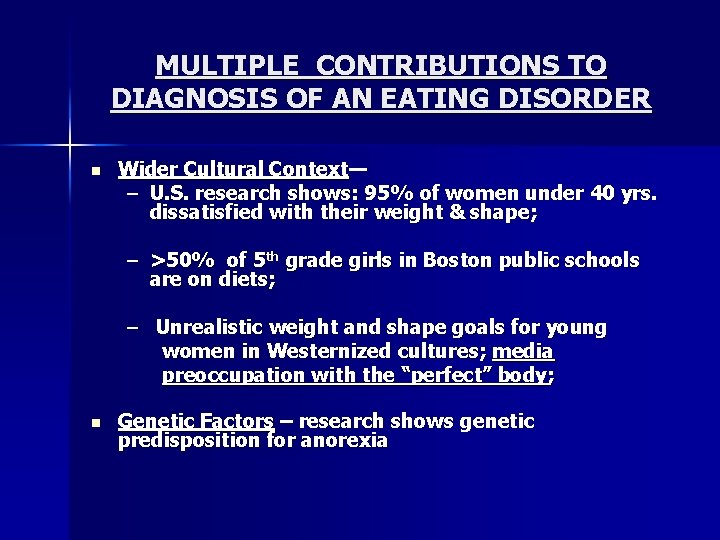
MULTIPLE CONTRIBUTIONS TO DIAGNOSIS OF AN EATING DISORDER n Wider Cultural Context— – U. S. research shows: 95% of women under 40 yrs. dissatisfied with their weight & shape; – >50% of 5 th grade girls in Boston public schools are on diets; – Unrealistic weight and shape goals for young women in Westernized cultures; media preoccupation with the “perfect” body; n Genetic Factors – research shows genetic predisposition for anorexia
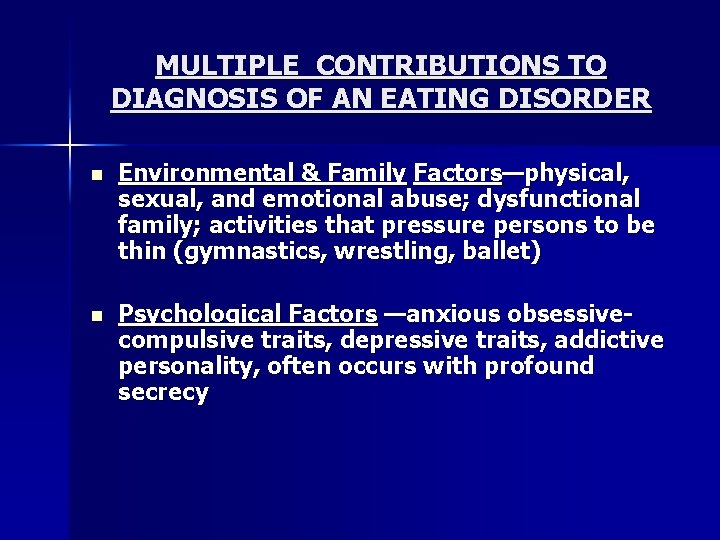
MULTIPLE CONTRIBUTIONS TO DIAGNOSIS OF AN EATING DISORDER n Environmental & Family Factors—physical, sexual, and emotional abuse; dysfunctional family; activities that pressure persons to be thin (gymnastics, wrestling, ballet) n Psychological Factors —anxious obsessivecompulsive traits, depressive traits, addictive personality, often occurs with profound secrecy
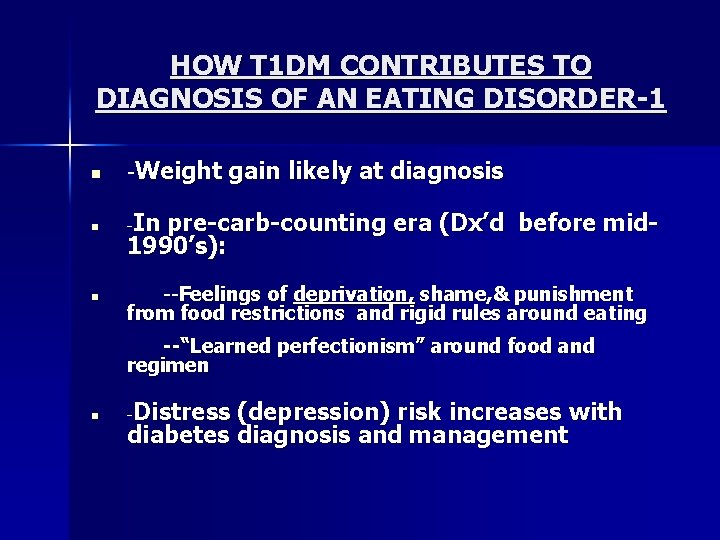
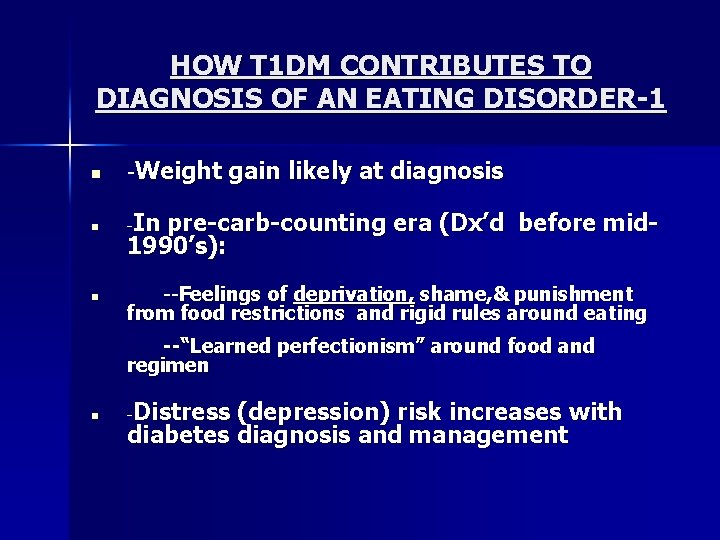
HOW T 1 DM CONTRIBUTES TO DIAGNOSIS OF AN EATING DISORDER-1 n -Weight n - n gain likely at diagnosis In pre-carb-counting era (Dx’d before mid 1990’s): --Feelings of deprivation, shame, & punishment from food restrictions and rigid rules around eating --“Learned perfectionism” around food and regimen n Distress (depression) risk increases with diabetes diagnosis and management -
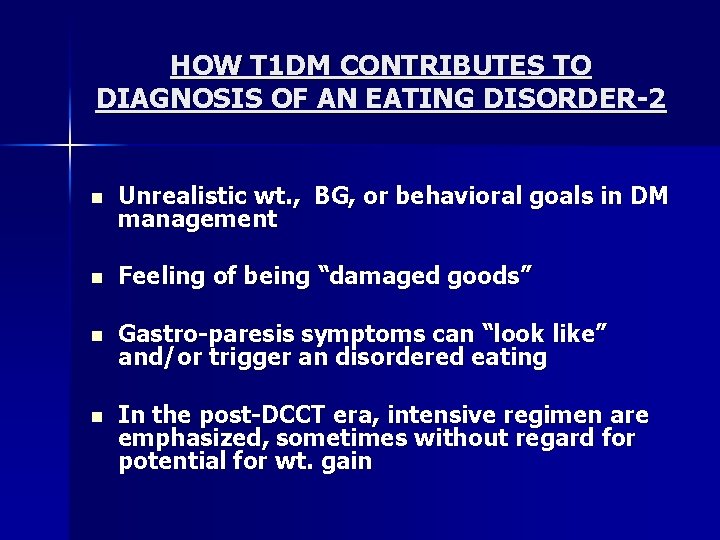
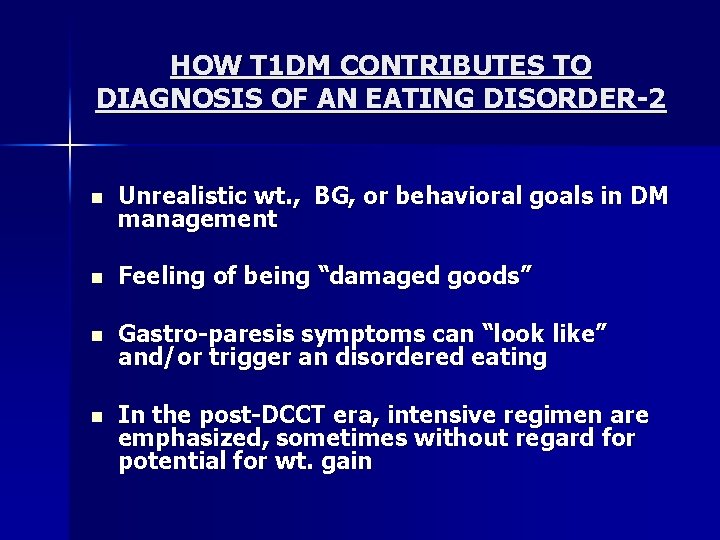
HOW T 1 DM CONTRIBUTES TO DIAGNOSIS OF AN EATING DISORDER-2 n Unrealistic wt. , BG, or behavioral goals in DM management n Feeling of being “damaged goods” n Gastro-paresis symptoms can “look like” and/or trigger an disordered eating n In the post-DCCT era, intensive regimen are emphasized, sometimes without regard for potential for wt. gain
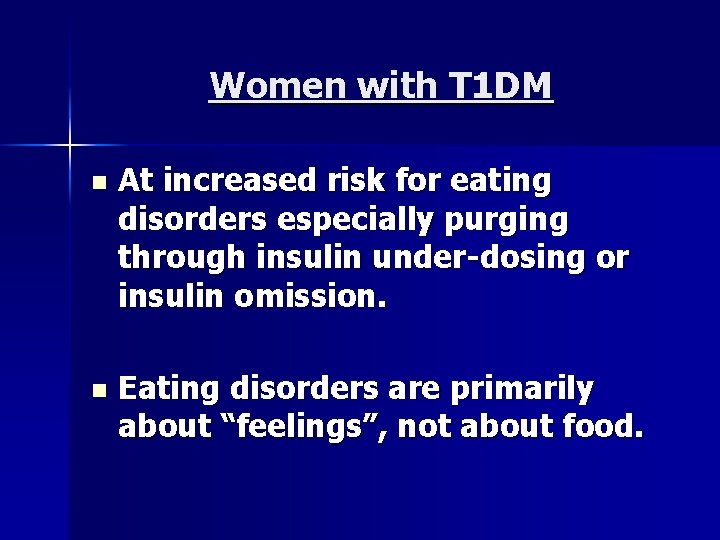
Women with T 1 DM n At increased risk for eating disorders especially purging through insulin under-dosing or insulin omission. n Eating disorders are primarily about “feelings”, not about food.
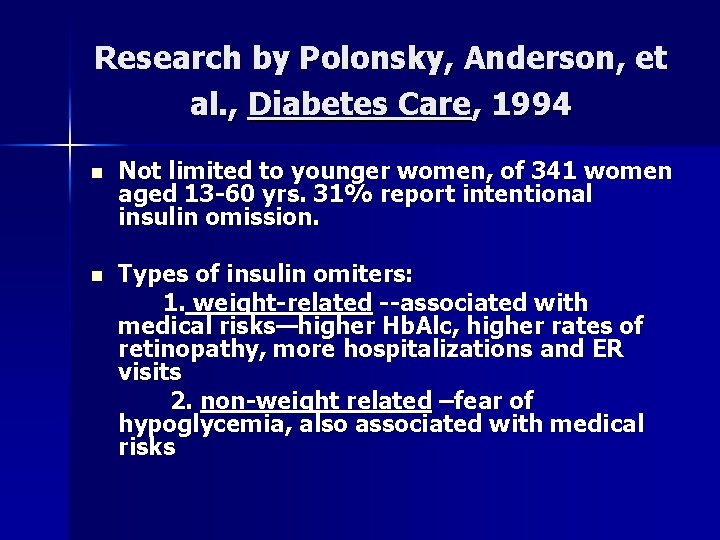
Research by Polonsky, Anderson, et al. , Diabetes Care, 1994 n Not limited to younger women, of 341 women aged 13 -60 yrs. 31% report intentional insulin omission. n Types of insulin omiters: 1. weight-related --associated with medical risks—higher Hb. Alc, higher rates of retinopathy, more hospitalizations and ER visits 2. non-weight related –fear of hypoglycemia, also associated with medical risks
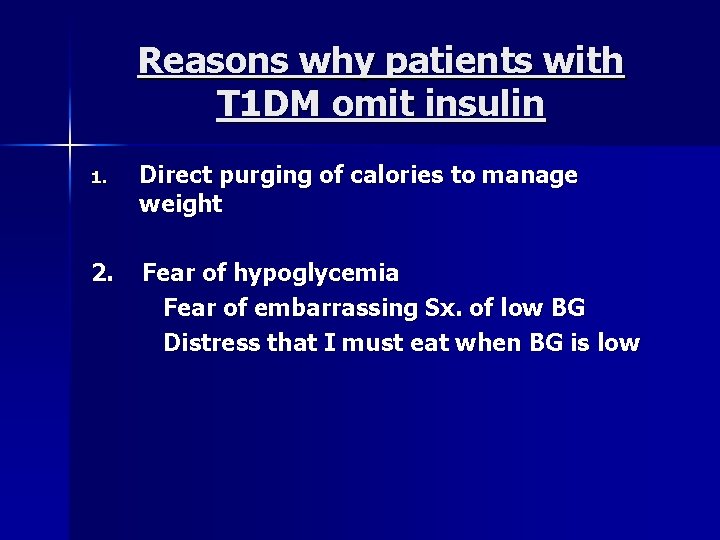
Reasons why patients with T 1 DM omit insulin 1. Direct purging of calories to manage weight 2. Fear of hypoglycemia Fear of embarrassing Sx. of low BG Distress that I must eat when BG is low
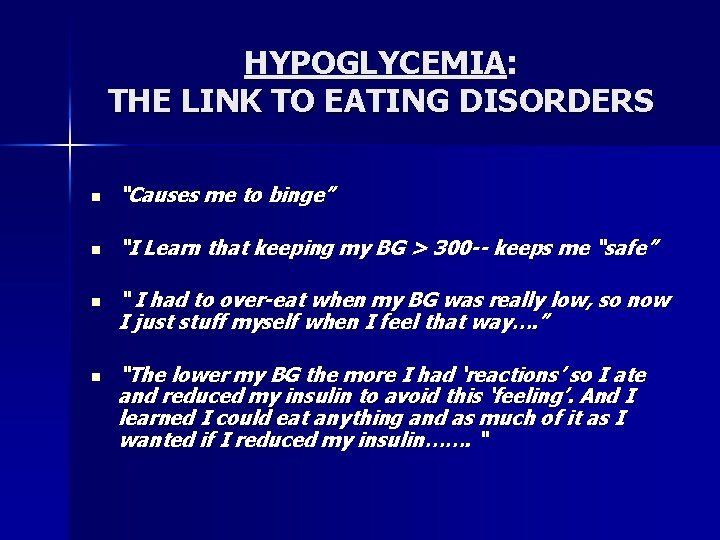
HYPOGLYCEMIA: THE LINK TO EATING DISORDERS n “Causes me to binge” n “I Learn that keeping my BG > 300 -- keeps me “safe” n n “ I had to over-eat when my BG was really low, so now I just stuff myself when I feel that way…. ” “The lower my BG the more I had ‘reactions’ so I ate and reduced my insulin to avoid this ‘feeling’. And I learned I could eat anything and as much of it as I wanted if I reduced my insulin……. “
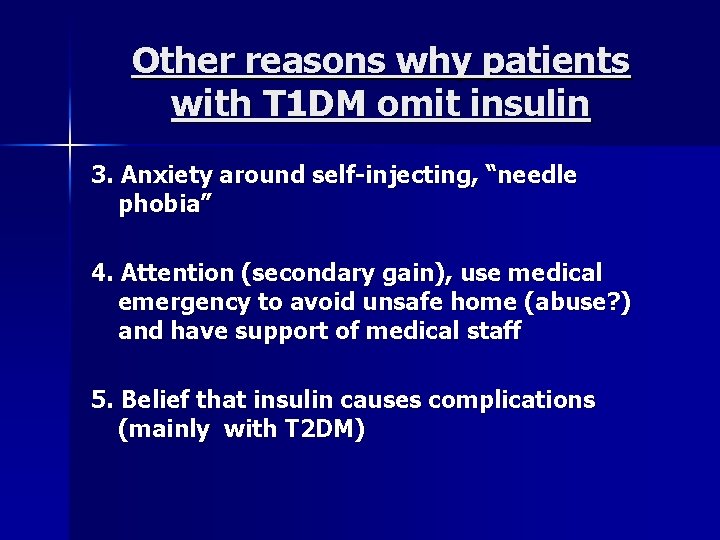
Other reasons why patients with T 1 DM omit insulin 3. Anxiety around self-injecting, “needle phobia” 4. Attention (secondary gain), use medical emergency to avoid unsafe home (abuse? ) and have support of medical staff 5. Belief that insulin causes complications (mainly with T 2 DM)
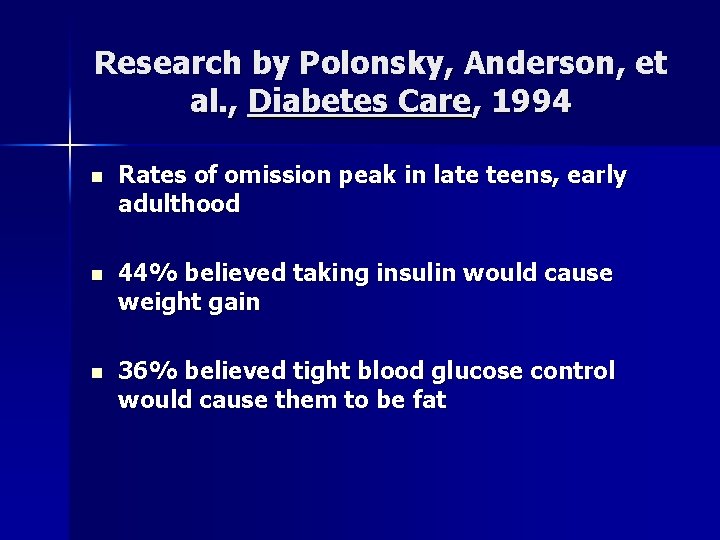
Research by Polonsky, Anderson, et al. , Diabetes Care, 1994 n Rates of omission peak in late teens, early adulthood n 44% believed taking insulin would cause weight gain n 36% believed tight blood glucose control would cause them to be fat
10 -year-Follow-Up Study (Goebel-Fabbri et al, 2008) n Significantly greater risk of diabetes complications in women who restricted insulin 10 years earlier vs. those who did not n Significantly greater risk of death in women who restricted insulin 10 years earlier vs. those who did not
T 1 DM Considerations n Weight loss at diagnosis is typical, followed by weight gain when insulin is started. n Fears that “insulin makes me fat” reinforced at diagnosis as well as when edema and weight gain follow periods of insulin omission. n Patients in intensive treatment arm of DCCT gained, on average, 10 lbs. Results of 9 yr. follow-up of these pts. “hard to lose wt. ”
T 1 DM Considerations-2 n Insulin dose increases during puberty, often not decreased after puberty. n Before “carbohydrate counting was recognized as a therapeutic tool for management of T 1 DM in 1994, restricted eating was the traditional medical treatment. There were “good foods” and “bad foods”. n Feelings of deprivation and punishment from food restrictions.
T 1 DM Considerations-3 n Perfectionism around food and regimen behavior. n Distress with diet and regimen can lead to depression. n Unrealistic goals for weight and blood sugars and for self-care behavior. n Complex emotional consequences of T 1 DM – “Shame & blame syndrome” “damaged goods”, etc.
Pt. Who Omits Insulin for Weight Control: The Medical Picture n Increasing Hb. Alc despite insulin adjustments, multiple daily injections prescribed. n Illogical blood sugar patterns n Erratic outpatient follow-up. n Weight loss in the context of non-dieting.
Pt. Who Omits Insulin for Weight Control: The Medical Picture-2 n Repeated, unexplained hospitalizations/ER. n Patient refuses to share insulin injection responsibilities. Lots of secrecy. n Patient denies “missing shots”.
Pt. Who Omits Insulin for Weight Control: The Psychosocial Picture n Dissatisfaction with body & unrealistic weight goals present but not sufficient n Relationship problems: Attachments problems in family of origin Lack of peer network and problems in intimate relationships
Pt. Who Omits Insulin for Weight Control: The Psychosocial Picture-2 n Overwhelmed and stressed about dm mgt. n Symptoms of chronic high BG (which mimic Sx of clinical depression): fatigue, loss of energy & interests, flat affect. n Secretive about eating habits and regimenrelated behaviors (shots, BGM)
Treatment of eating disorders in T 1 DM n n n Focus on this as a common “struggle” avoid blame/shame of pt. Multidisciplinary team needed Mental and physical health assessments for level of treatment needed
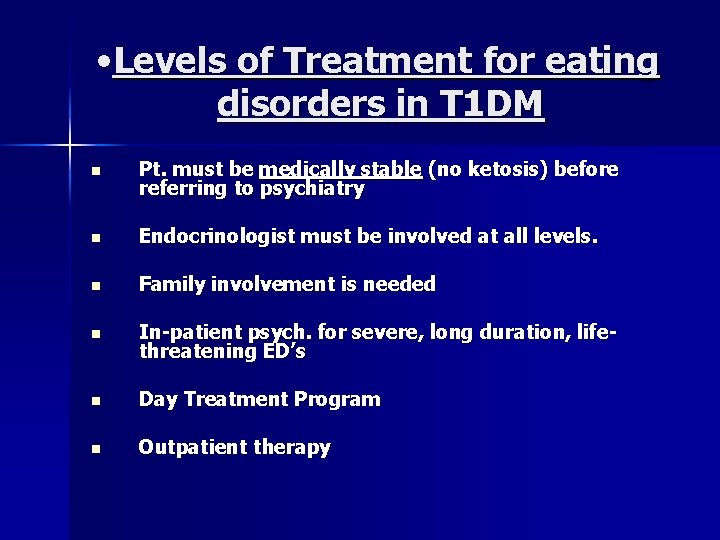
• Levels of Treatment for eating disorders in T 1 DM n Pt. must be medically stable (no ketosis) before referring to psychiatry n Endocrinologist must be involved at all levels. n Family involvement is needed n In-patient psych. for severe, long duration, lifethreatening ED’s n Day Treatment Program n Outpatient therapy
Treatment of eating disorders in T 1 DM n Higher mortality associated ED Dx’s than any other psychiatric condition. n For women with ED and DM, risk of complications is significant (Rydall et al, New Engl Journ Med, 1997).
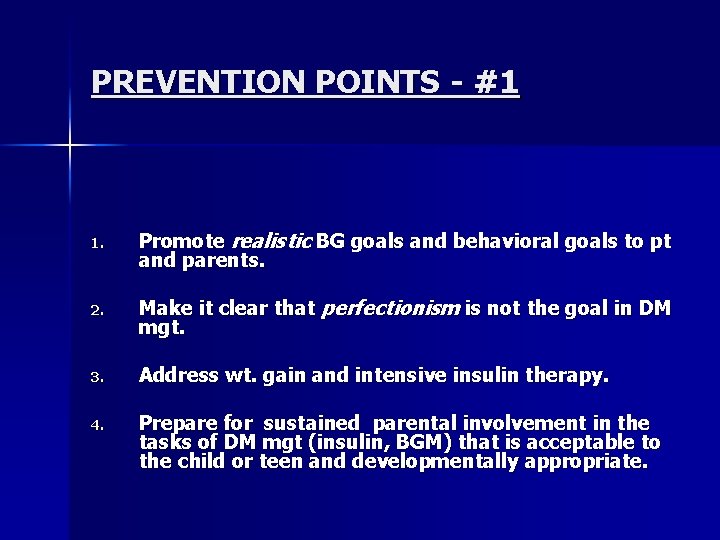
PREVENTION POINTS - #1 1. Promote realistic BG goals and behavioral goals to pt and parents. 2. Make it clear that perfectionism is not the goal in DM mgt. 3. Address wt. gain and intensive insulin therapy. 4. Prepare for sustained parental involvement in the tasks of DM mgt (insulin, BGM) that is acceptable to the child or teen and developmentally appropriate.
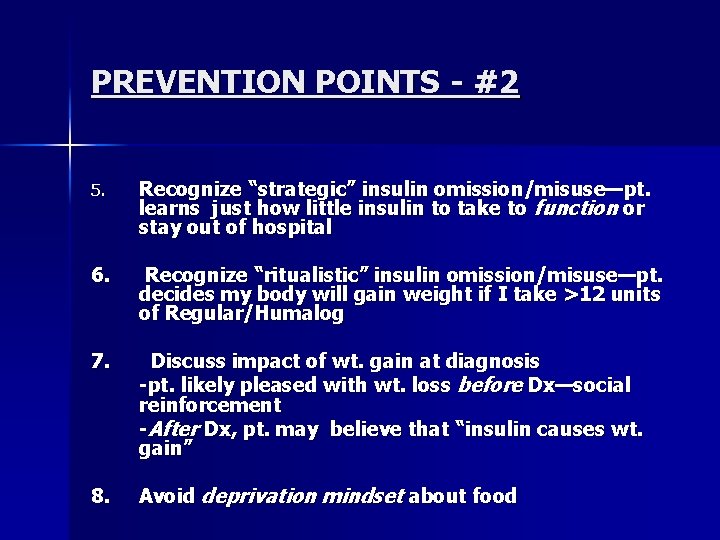
PREVENTION POINTS - #2 5. Recognize “strategic” insulin omission/misuse—pt. learns just how little insulin to take to function or stay out of hospital 6. Recognize “ritualistic” insulin omission/misuse—pt. decides my body will gain weight if I take >12 units of Regular/Humalog 7. Discuss impact of wt. gain at diagnosis -pt. likely pleased with wt. loss before Dx—social reinforcement -After Dx, pt. may believe that “insulin causes wt. gain” 8. Avoid deprivation mindset about food
Summary n Clinicians must have a high “index of suspicion” when classic medical picture of an eating disorder appears in young female with T 1 DM. Remember: Secrecy is common in eating disorders. n Pts. with T 1 DM and disordered eating are at high risk for complications and mortality.
Summary-2 n Demands multidisciplinary treatment, collaborate with mental health expert in eating disorders n Prevention is key!
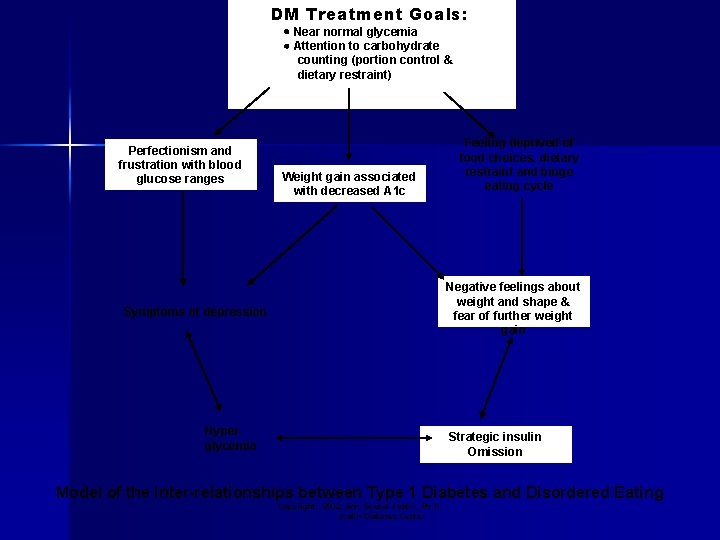
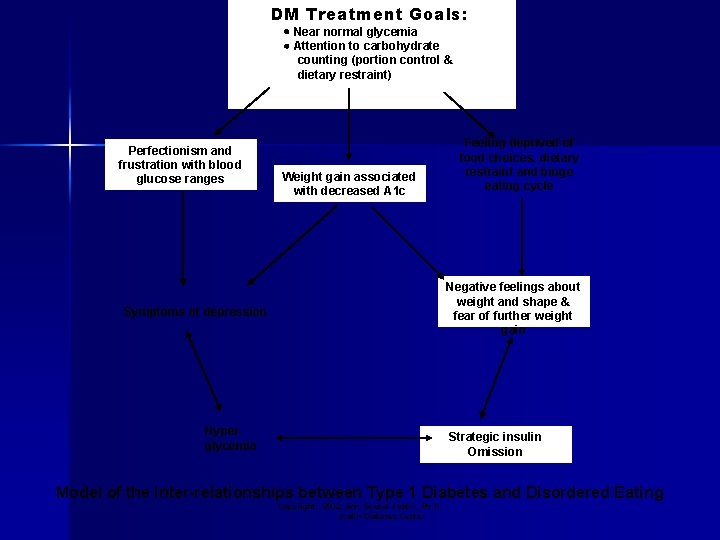
DM Treatment Goals: Near normal glycemia Attention to carbohydrate counting (portion control & dietary restraint) Perfectionism and frustration with blood glucose ranges Weight gain associated with decreased A 1 c Feeling deprived of food choices, dietary restraint and binge eating cycle Negative feelings about weight and shape & fear of further weight gain Symptoms of depression Hyperglycemia Strategic insulin Omission Model of the Inter-relationships between Type 1 Diabetes and Disordered Eating Copyright: 2002, Ann Goebel-Fabbri, Ph. D. Joslin Diabetes Center