Early Initiation of Insulin Basal Bolus versus Premixed
Early Initiation of Insulin: Basal Bolus versus Premixed
ADA Diabetes Management Algorithm 2015
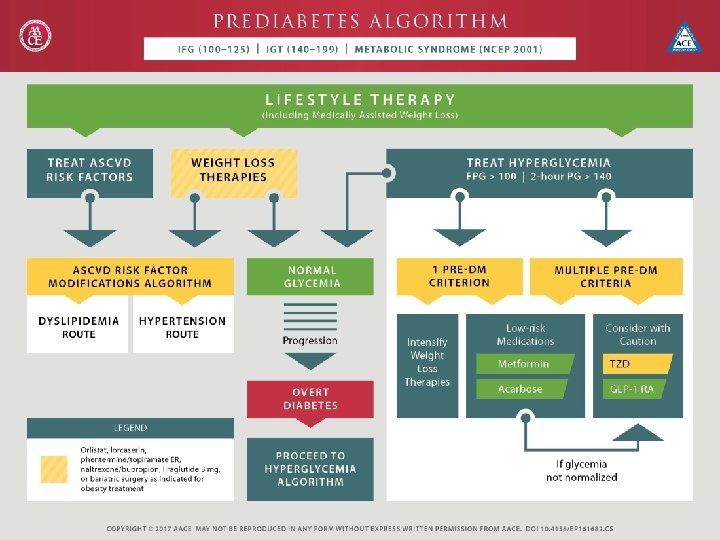
Need for Early and aggressive treatment
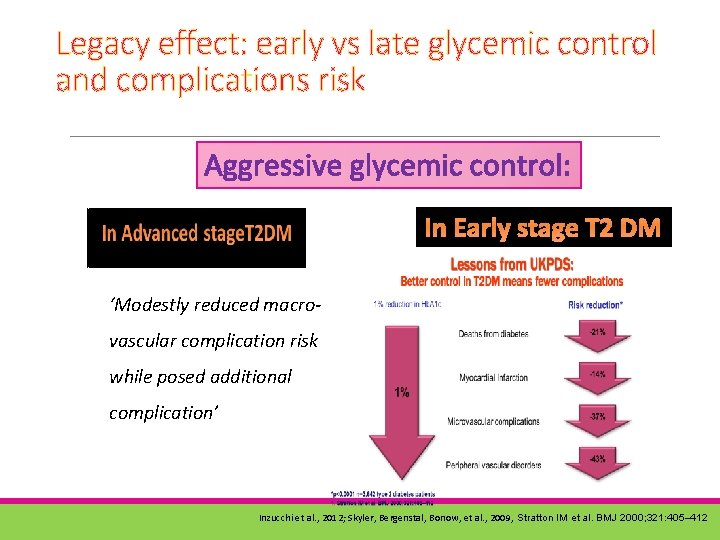
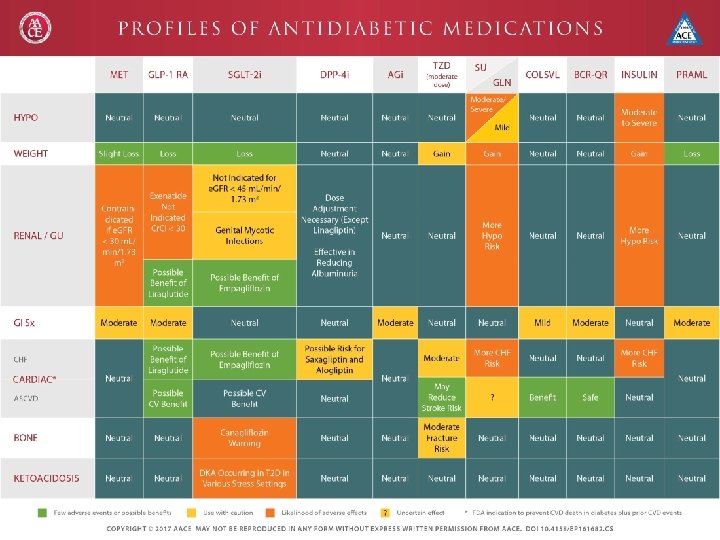
Legacy effect: early vs late glycemic control and complications risk Aggressive glycemic control: In Early stage T 2 DM ‘Modestly reduced macrovascular complication risk while posed additional complication’ Inzucchi et al. , 2012; Skyler, Bergenstal, Bonow, et al. , 2009, Stratton IM et al. BMJ 2000; 321: 405– 412
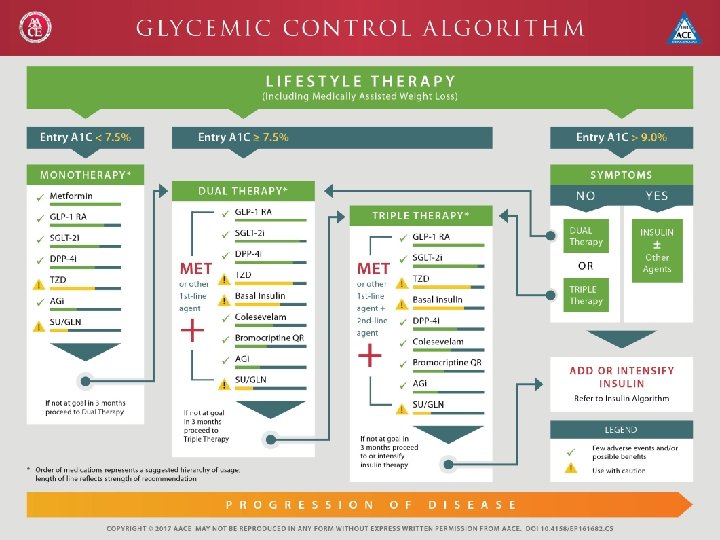
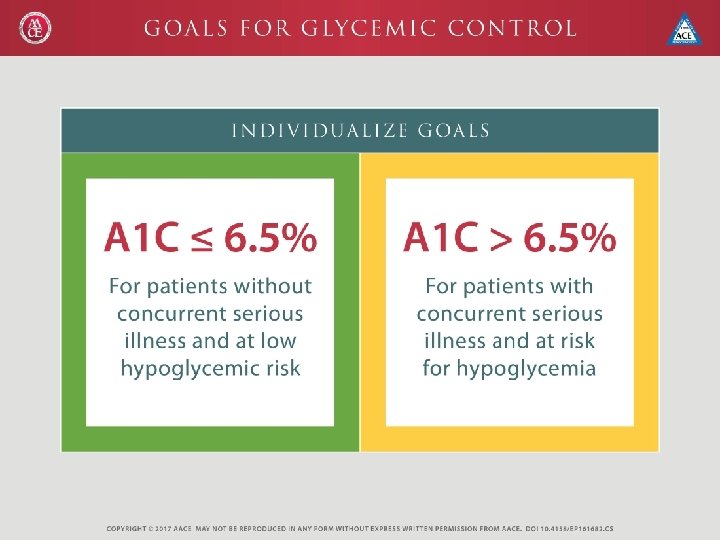
Insulin at Diagnosis AACE and the Canadian Diabetes Association suggest considering insulin treatment at the time of T 2 DM diagnosis if glycemic control is very poor (Hb. A 1 c levels >9%) ADA/EASD guidelines recommend insulin therapy be considered for patients who present for the first time with T 2 DM and an Hb. A 1 c level >10%. Handelsman, Y. et al. Endocr. Pract. 17 (Suppl. 2), 1– 53 (2011). Bhattacharyya, O. K. Can. Fam. Physician. 55, 39– 43 (2009).
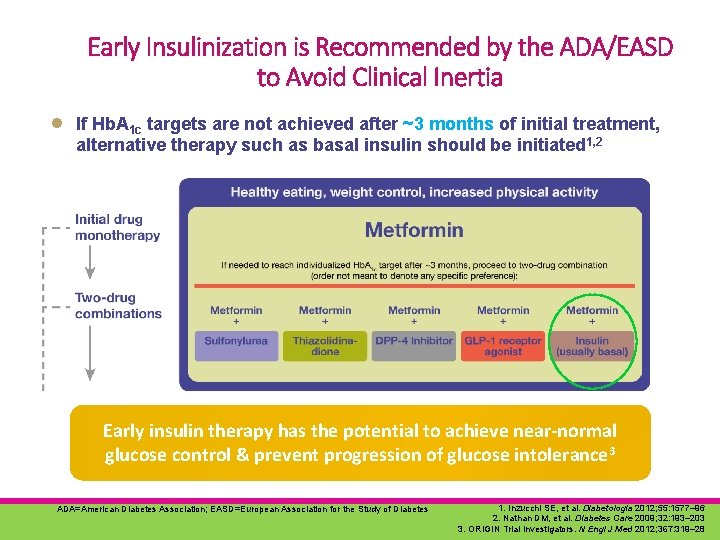
Early Insulinization is Recommended by the ADA/EASD to Avoid Clinical Inertia ● If Hb. A 1 c targets are not achieved after ~3 months of initial treatment, alternative therapy such as basal insulin should be initiated 1, 2 Early insulin therapy has the potential to achieve near-normal glucose control & prevent progression of glucose intolerance 3 ADA=American Diabetes Association; EASD=European Association for the Study of Diabetes 1. Inzucchi SE, et al. Diabetologia 2012; 55: 1577– 96 2. Nathan DM, et al. Diabetes Care 2009; 32: 193– 203 3. ORIGIN Trial Investigators. N Engl J Med 2012; 367: 319– 28
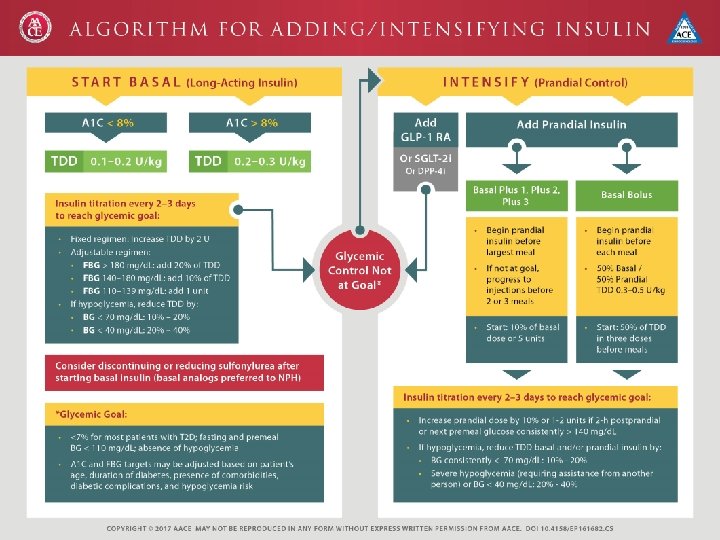
The legacy of basal insulin Treat-To-Target Concept has demonstrated the role of basal insulin analogs in facilitating early insulin replacement, lower risk of hypoglycemia and becoming foundation of therapy. 4 T study also showed that, over the longer term (3 years), a premixed insulin regimen was not as effective as basal insulin at attaining glycemic targets. Diabetes Care in 2012: Current Trends and Future Directions
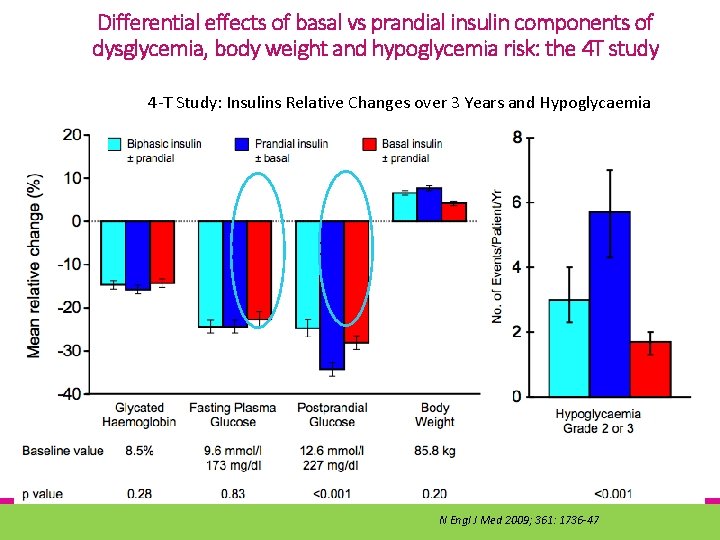
Differential effects of basal vs prandial insulin components of dysglycemia, body weight and hypoglycemia risk: the 4 T study 4 -T Study: Insulins Relative Changes over 3 Years and Hypoglycaemia N Engl J Med 2009; 361: 1736 -47
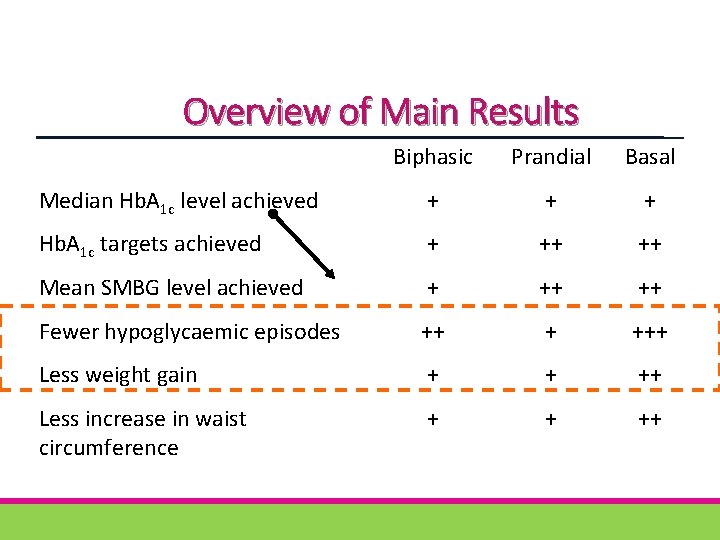
Overview of Main Results Biphasic Prandial Basal Median Hb. A 1 c level achieved + + + Hb. A 1 c targets achieved + ++ ++ Mean SMBG level achieved + ++ ++ Fewer hypoglycaemic episodes ++ + +++ Less weight gain + + ++ Less increase in waist circumference + + ++
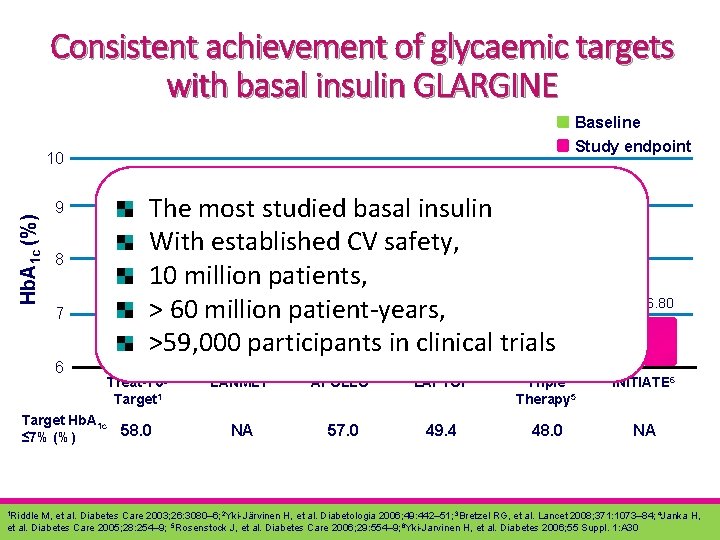
Consistent achievement of glycaemic targets with basal insulin GLARGINE Baseline Study endpoint Hb. A 1 c (%) 10 9 8 7 6 9. 5 8. 61 8. 85 8. 80 The most studied 8. 71 basal insulin With established CV safety, 10 million patients, 7. 15 7. 14 6. 96 > 60 million patient-years, >59, 000 participants in clinical trials Treat-To. Target 1 Target Hb. A 1 c 58. 0 ≤ 7% (%) 1 Riddle 8. 80 6. 80 LANMET 2 APOLLO 3 LAPTOP 4 Triple Therapy 5 INITIATE 6 NA 57. 0 49. 4 48. 0 NA M, et al. Diabetes Care 2003; 26: 3080– 6; 2 Yki-Järvinen H, et al. Diabetologia 2006; 49: 442– 51; 3 Bretzel RG, et al. Lancet 2008; 371: 1073– 84; 4 Janka H, et al. Diabetes Care 2005; 28: 254– 9; 5 Rosenstock J, et al. Diabetes Care 2006; 29: 554– 9; 6 Yki-Jarvinen H, et al. Diabetes 2006; 55 Suppl. 1: A 30
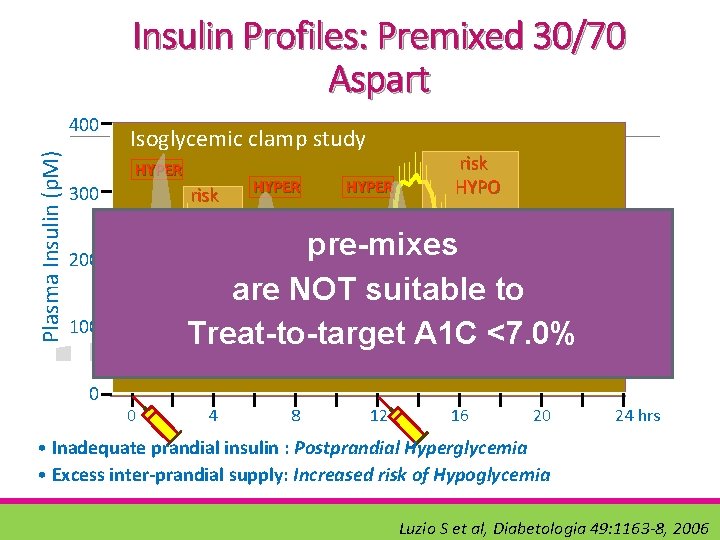
Insulin Profiles: Premixed 30/70 Aspart Plasma Insulin (p. M) 400 Isoglycemic clamp study HYPER 300 risk HYPO HYPER pre-mixes are NOT suitable to Treat-to-target A 1 C <7. 0% 200 100 0 HYPER risk HYPO 0 4 8 12 16 20 24 hrs • Inadequate prandial insulin : Postprandial Hyperglycemia • Excess inter-prandial supply: Increased risk of Hypoglycemia Luzio S et al, Diabetologia 49: 1163 -8, 2006
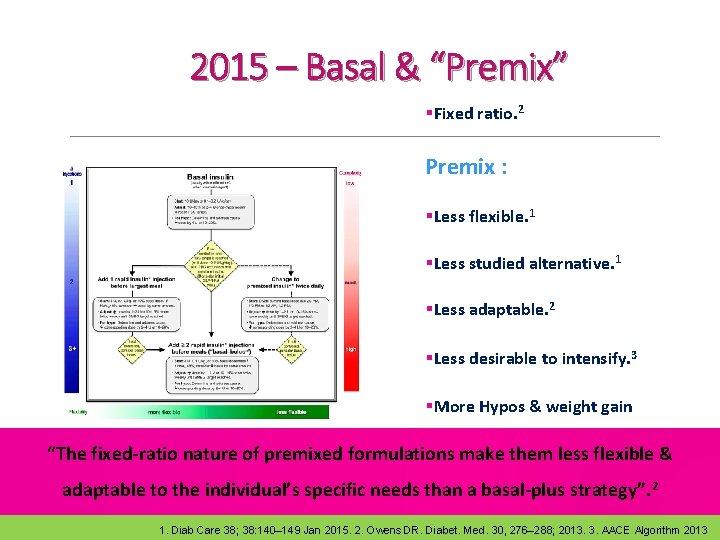
2015 – Basal & “Premix” §Fixed ratio. 2 Premix : §Less flexible. 1 §Less studied alternative. 1 §Less adaptable. 2 §Less desirable to intensify. 3 §More Hypos & weight gain §Unable to them titrateless individually “The fixed-ratio nature of premixed formulations make flexible & adaptable to the individual’s specific needs than a basal-plus strategy”. 2 1. Diab Care 38; 38: 140– 149 Jan 2015. 2. Owens DR. Diabet. Med. 30, 276– 288; 2013. 3. AACE Algorithm 2013
CLINICAL EVIDENCES for basal/basalplus/basal-bolus strategy versus premixed
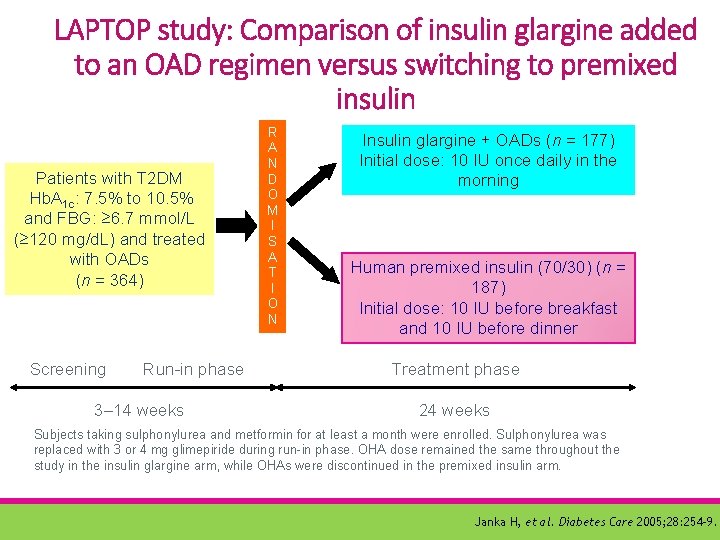
LAPTOP study: Comparison of insulin glargine added to an OAD regimen versus switching to premixed insulin Patients with T 2 DM Hb. A 1 c: 7. 5% to 10. 5% and FBG: ≥ 6. 7 mmol/L (≥ 120 mg/d. L) and treated with OADs (n = 364) Screening Run-in phase 3– 14 weeks R A N D O M I S A T I O N Insulin glargine + OADs (n = 177) Initial dose: 10 IU once daily in the morning Human premixed insulin (70/30) (n = 187) Initial dose: 10 IU before breakfast and 10 IU before dinner Treatment phase 24 weeks Subjects taking sulphonylurea and metformin for at least a month were enrolled. Sulphonylurea was replaced with 3 or 4 mg glimepiride during run-in phase. OHA dose remained the same throughout the study in the insulin glargine arm, while OHAs were discontinued in the premixed insulin arm. Janka H, et al. Diabetes Care 2005; 28: 254– 9.
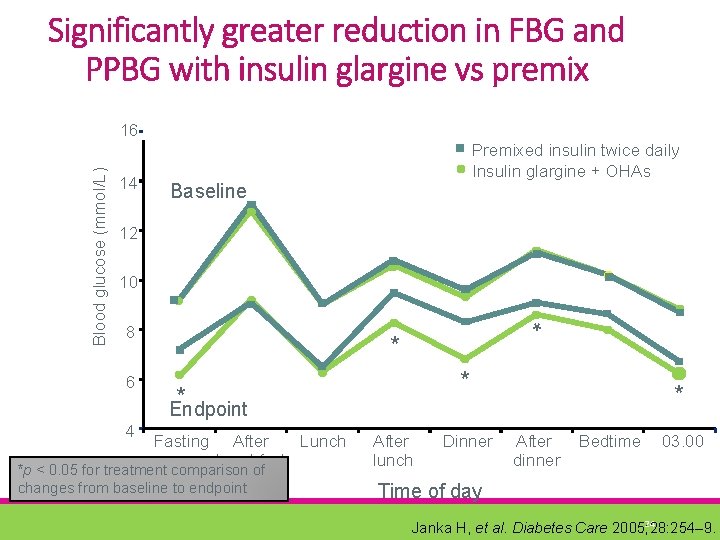
Significantly greater reduction in FBG and PPBG with insulin glargine vs premix 14 Premixed insulin twice daily Insulin glargine + OHAs Baseline 12 10 8 6 4 * Blood glucose (mmol/L) 16 * * * Endpoint Fasting Lunch After breakfast *p < 0. 05 for treatment comparison of changes from baseline to endpoint After lunch Dinner * After dinner Bedtime 03. 00 Time of day 24 Janka H, et al. Diabetes Care 2005; 28: 254– 9.
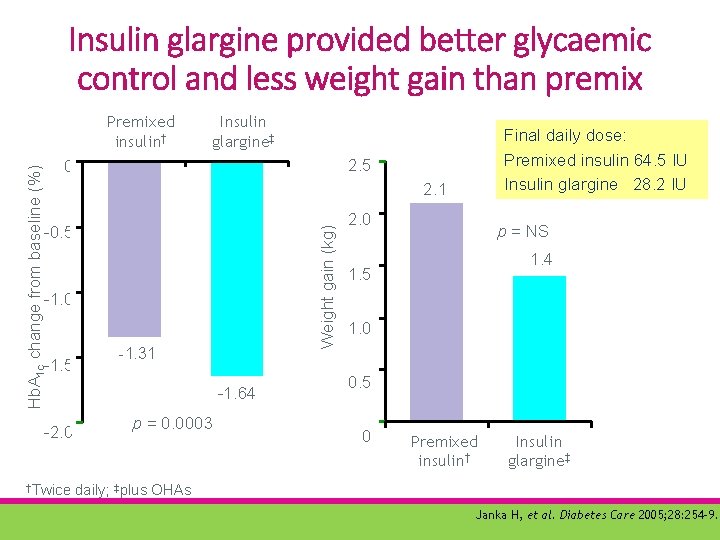
Insulin glargine provided better glycaemic control and less weight gain than premix Hb. A 1 c change from baseline (%) Premixed insulin† Insulin glargine‡ 2. 5 0 2. 1 Weight gain (kg) -0. 5 -1. 0 -1. 5 -2. 0 †Twice Final daily dose: Premixed insulin 64. 5 IU Insulin glargine 28. 2 IU -1. 31 -1. 64 p = 0. 0003 2. 0 p = NS 1. 4 1. 5 1. 0 0. 5 0 Premixed insulin† Insulin glargine‡ daily; ‡plus OHAs Janka H, et al. Diabetes Care 2005; 28: 254– 9.
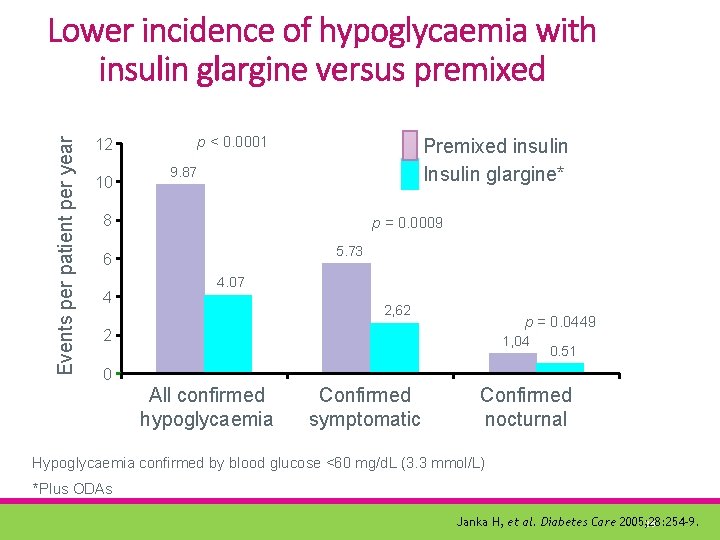
Events per patient per year Lower incidence of hypoglycaemia with insulin glargine versus premixed p < 0. 0001 12 10 Premixed insulin Insulin glargine* 9. 87 8 p = 0. 0009 5. 73 6 4 4. 07 2, 62 p = 0. 0449 2 1, 04 0. 51 0 All confirmed hypoglycaemia Confirmed symptomatic Confirmed nocturnal Hypoglycaemia confirmed by blood glucose <60 mg/d. L (3. 3 mmol/L) *Plus ODAs Janka H, et al. Diabetes Care 2005; 28: 254– 9. 26
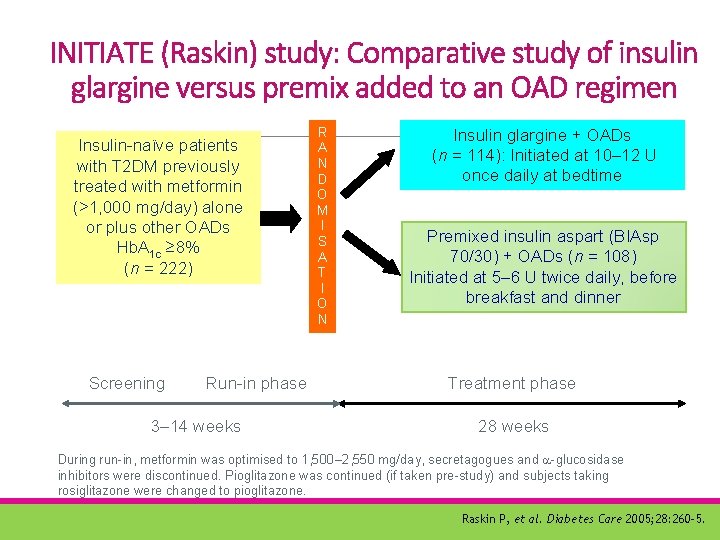
INITIATE (Raskin) study: Comparative study of insulin glargine versus premix added to an OAD regimen Insulin-naïve patients with T 2 DM previously treated with metformin (>1, 000 mg/day) alone or plus other OADs Hb. A 1 c ≥ 8% (n = 222) Screening Run-in phase 3– 14 weeks R A N D O M I S A T I O N Insulin glargine + OADs (n = 114): Initiated at 10– 12 U once daily at bedtime Premixed insulin aspart (BIAsp 70/30) + OADs (n = 108) Initiated at 5– 6 U twice daily, before breakfast and dinner Treatment phase 28 weeks During run-in, metformin was optimised to 1, 500– 2, 550 mg/day, secretagogues and -glucosidase inhibitors were discontinued. Pioglitazone was continued (if taken pre-study) and subjects taking rosiglitazone were changed to pioglitazone. Raskin P, et al. Diabetes Care 2005; 28: 260– 5.
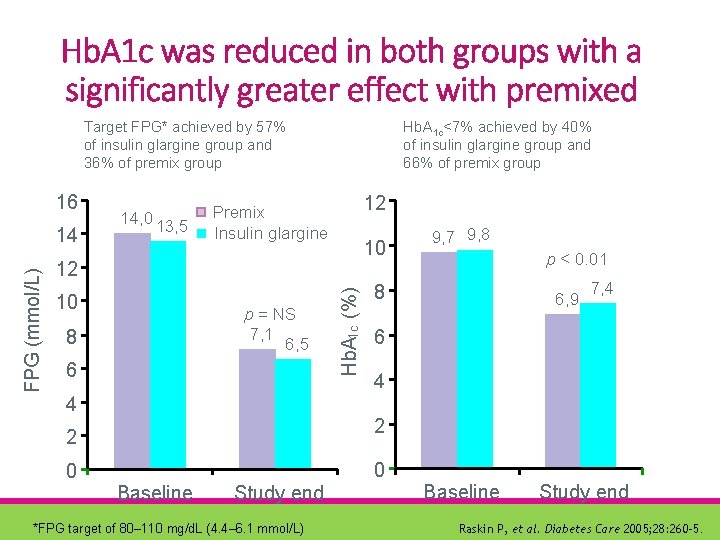
Hb. A 1 c was reduced in both groups with a significantly greater effect with premixed Target FPG* achieved by 57% of insulin glargine group and 36% of premix group 16 12 Premix Insulin glargine 10 12 10 p = NS 7, 1 6, 5 8 6 4 9, 7 9, 8 p < 0. 01 8 6, 9 7, 4 6 4 2 2 0 Hb. A 1 c (%) FPG (mmol/L) 14 14, 0 13, 5 Hb. A 1 c<7% achieved by 40% of insulin glargine group and 66% of premix group 0 Baseline Study end *FPG target of 80– 110 mg/d. L (4. 4– 6. 1 mmol/L) Baseline Study end Raskin P, et al. Diabetes Care 2005; 28: 260– 5.
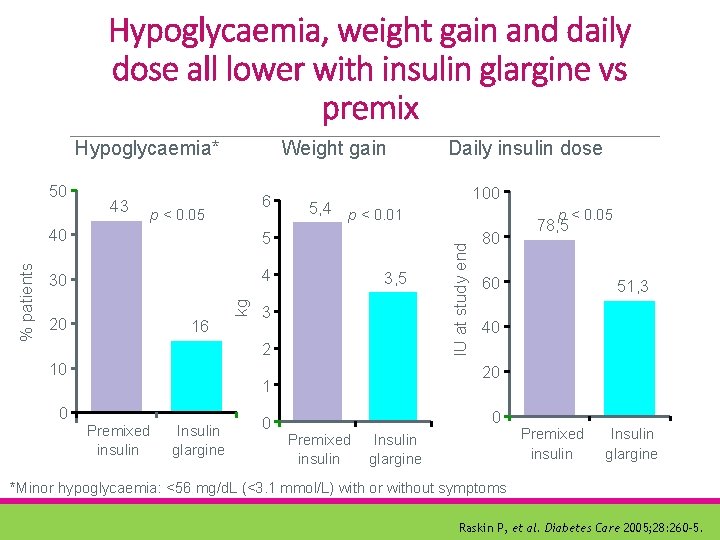
Hypoglycaemia, weight gain and daily dose all lower with insulin glargine vs premix 43 6 p < 0. 05 40 5 30 4 20 16 kg % patients 50 Weight gain 0 3, 5 3 Insulin glargine 0 p < 0. 05 80 78, 5 60 51, 3 40 20 1 Premixed insulin 100 5, 4 p < 0. 01 2 10 Daily insulin dose IU at study end Hypoglycaemia* 0 Premixed insulin Insulin glargine *Minor hypoglycaemia: <56 mg/d. L (<3. 1 mmol/L) with or without symptoms Raskin P, et al. Diabetes Care 2005; 28: 260– 5.
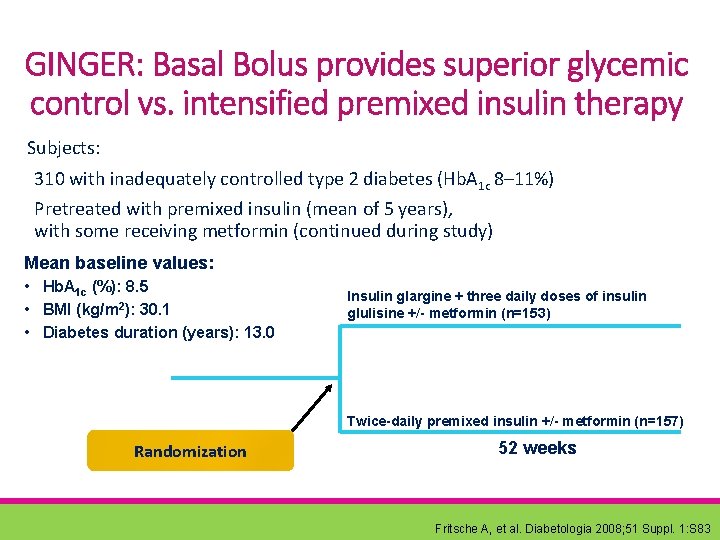
GINGER: Basal Bolus provides superior glycemic control vs. intensified premixed insulin therapy Subjects: 310 with inadequately controlled type 2 diabetes (Hb. A 1 c 8– 11%) Pretreated with premixed insulin (mean of 5 years), with some receiving metformin (continued during study) Mean baseline values: • Hb. A 1 c (%): 8. 5 • BMI (kg/m 2): 30. 1 • Diabetes duration (years): 13. 0 Insulin glargine + three daily doses of insulin glulisine +/- metformin (n=153) Twice-daily premixed insulin +/- metformin (n=157) Randomization 52 weeks Fritsche A, et al. Diabetologia 2008; 51 Suppl. 1: S 83
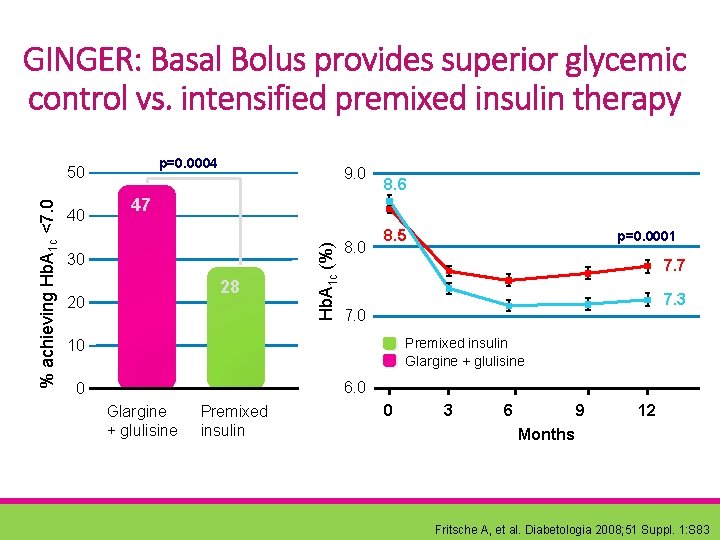
GINGER: Basal Bolus provides superior glycemic control vs. intensified premixed insulin therapy p=0. 0004 40 9. 0 8. 6 47 30 28 20 Hb. A 1 c (%) % achieving Hb. A 1 c <7. 0 50 8. 5 p=0. 0001 7. 7 7. 3 7. 0 Premixed insulin Glargine + glulisine 10 6. 0 0 Glargine + glulisine Premixed insulin 0 3 6 9 12 Months Fritsche A, et al. Diabetologia 2008; 51 Suppl. 1: S 83
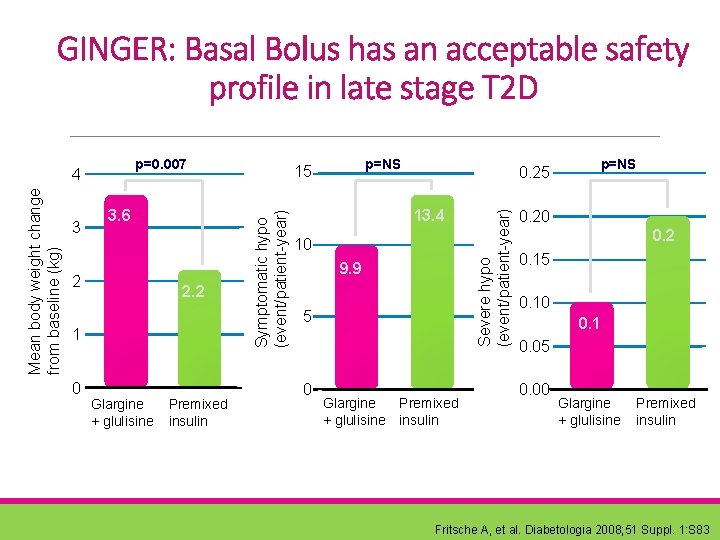
GINGER: Basal Bolus has an acceptable safety profile in late stage T 2 D 3. 6 2 2. 2 1 0 Glargine + glulisine Premixed insulin Symptomatic hypo (event/patient-year) Mean body weight change from baseline (kg) 3 p=NS 15 0. 25 13. 4 10 9. 9 5 0 Glargine + glulisine Premixed insulin Severe hypo (event/patient-year) p=0. 007 4 p=NS 0. 20 0. 2 0. 15 0. 10 0. 1 0. 05 0. 00 Glargine + glulisine Premixed insulin Fritsche A, et al. Diabetologia 2008; 51 Suppl. 1: S 83
Treatment satisfaction with insulin glargine vs premixed insulin analogues
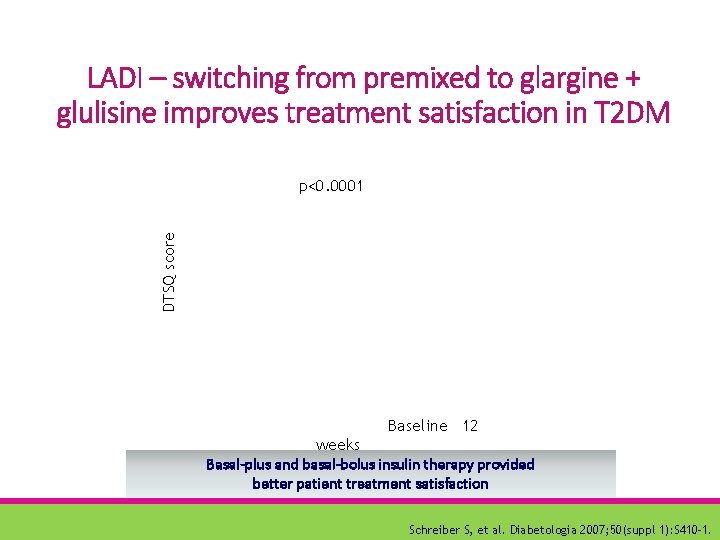
LADI – switching from premixed to glargine + glulisine improves treatment satisfaction in T 2 DM DTSQ score p<0. 0001 Baseline 12 weeks Basal-plus and basal-bolus insulin therapy provided better patient treatment satisfaction Schreiber S, et al. Diabetologia 2007; 50(suppl 1): S 410– 1.
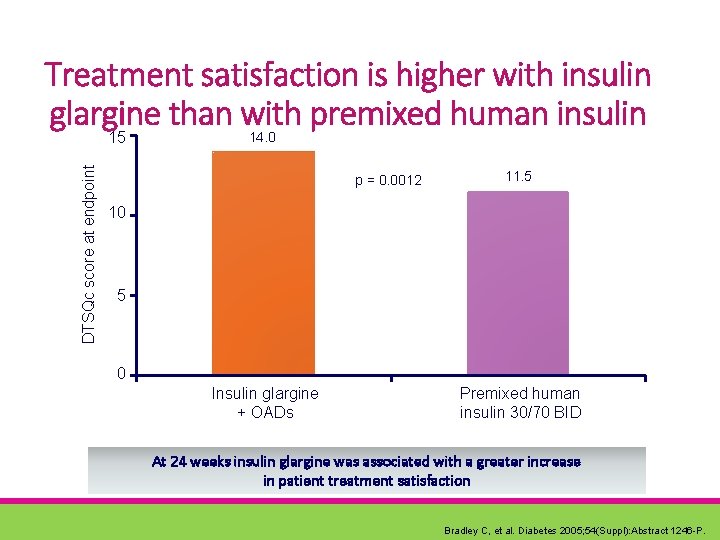
Treatment satisfaction is higher with insulin glargine than with premixed human insulin DTSQc score at endpoint 15 14. 0 p = 0. 0012 11. 5 10 5 0 Insulin glargine + OADs Premixed human insulin 30/70 BID At 24 weeks insulin glargine was associated with a greater increase in patient treatment satisfaction Bradley C, et al. Diabetes 2005; 54(Suppl): Abstract 1246 -P.
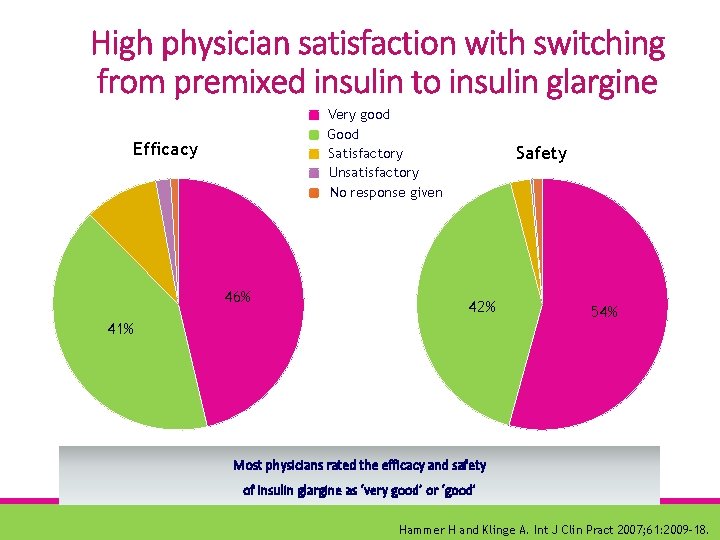
High physician satisfaction with switching from premixed insulin to insulin glargine Very good Good Satisfactory Unsatisfactory No response given Efficacy 46% Safety 42% 41% 54% Most physicians rated the efficacy and safety of insulin glargine as ‘very good’ or ‘good’ Hammer H and Klinge A. Int J Clin Pract 2007; 61: 2009– 18.
Markers of glycemic variability were better in patients treated with BB than in those treated with MIX in better control group. Conclusion: These results suggest that BB therapy achieves better glucose profiles than MIX therapy.
Subcontinental Data
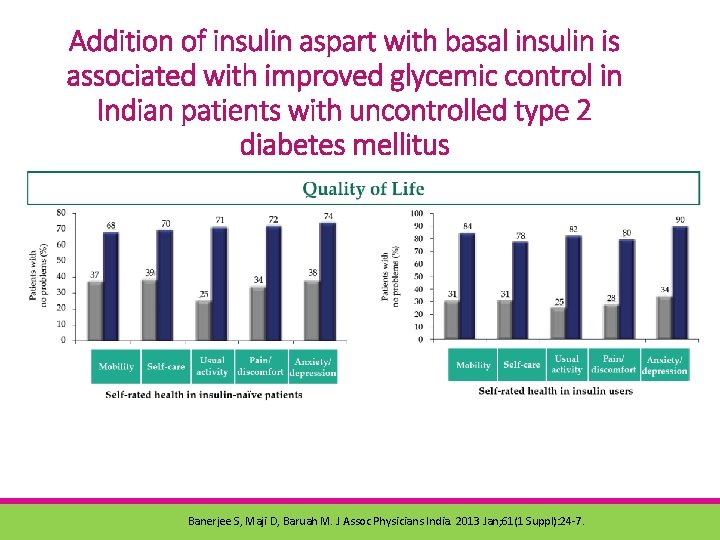
Addition of insulin aspart with basal insulin is associated with improved glycemic control in Indian patients with uncontrolled type 2 diabetes mellitus Banerjee S, Maji D, Baruah M. J Assoc Physicians India. 2013 Jan; 61(1 Suppl): 24 -7.
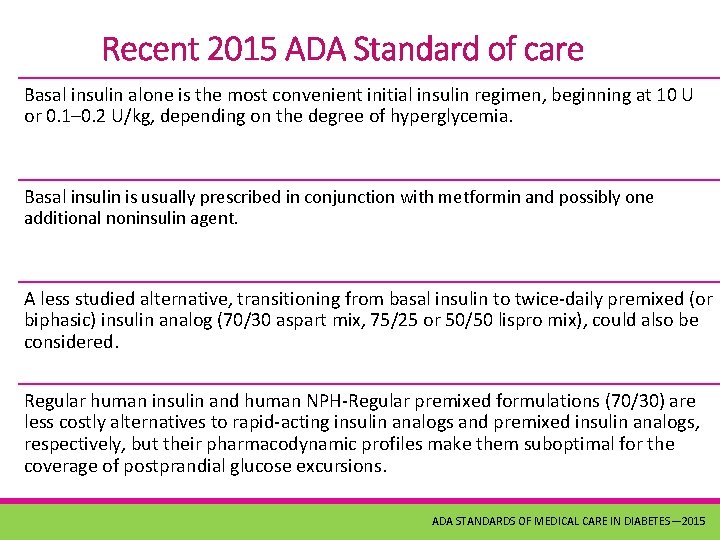
Recent 2015 ADA Standard of care Basal insulin alone is the most convenient initial insulin regimen, beginning at 10 U or 0. 1– 0. 2 U/kg, depending on the degree of hyperglycemia. Basal insulin is usually prescribed in conjunction with metformin and possibly one additional noninsulin agent. A less studied alternative, transitioning from basal insulin to twice-daily premixed (or biphasic) insulin analog (70/30 aspart mix, 75/25 or 50/50 lispro mix), could also be considered. Regular human insulin and human NPH-Regular premixed formulations (70/30) are less costly alternatives to rapid-acting insulin analogs and premixed insulin analogs, respectively, but their pharmacodynamic profiles make them suboptimal for the coverage of postprandial glucose excursions. ADA STANDARDS OF MEDICAL CARE IN DIABETES— 2015
Conclusion Basal Insulin strategy: • Simple, flexible approach to intensifying a basal insulin regimen. • Easily progressed to a basal-bolus regimen, if required. • Premixed insulin regimens are less flexible & must be switched to a more physiological basal-bolus regimen if further intensification is required. • Switching from premixed insulin regimens to basal ± boluses improves patient satisfaction. • The basal-bolus regimen offers patients flexible treatment that responds to different needs and lifestyles and reduces glucose variability
. . . Initiate Study 2 Laptop Study 1 AT-LANTUS Study 5 Hammer & Kingler 3 Thank you DURABLE Study 5 Janka H, et al. Diabetes Care 2005; 28: 254– 9. 2. Raskin P, et al. Diabetes Care 2005; 28: 260– 5. 3. Davies M, et al. Diabetes Res Clin Pract 2008; 79: 368– 75. 4. Hammer H and Klinge A. Int J Clin Pract 2007; 61: 2009– 18 5. Diabetes Care 34: 249– 255, 2011.
- Slides: 42