Ear disorders 1 The most common disorder is



- Slides: 39
Ear disorders 1
§The most common disorder is called: Otitis media, which means an inflammation and infection of the middle ear. 2
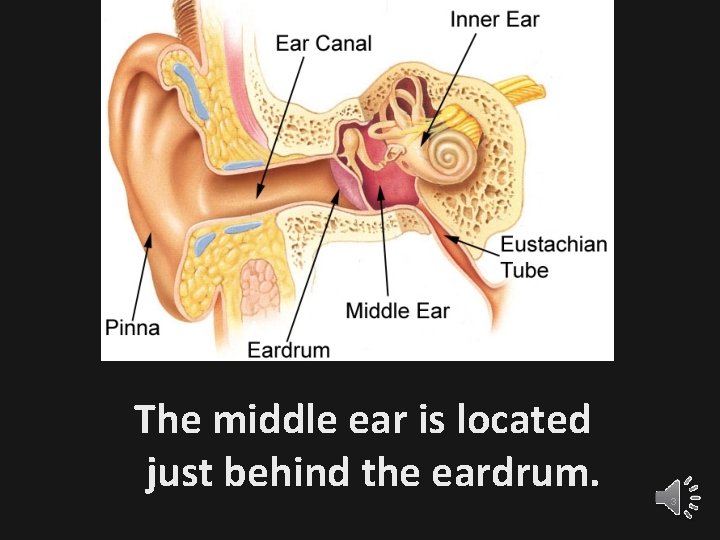
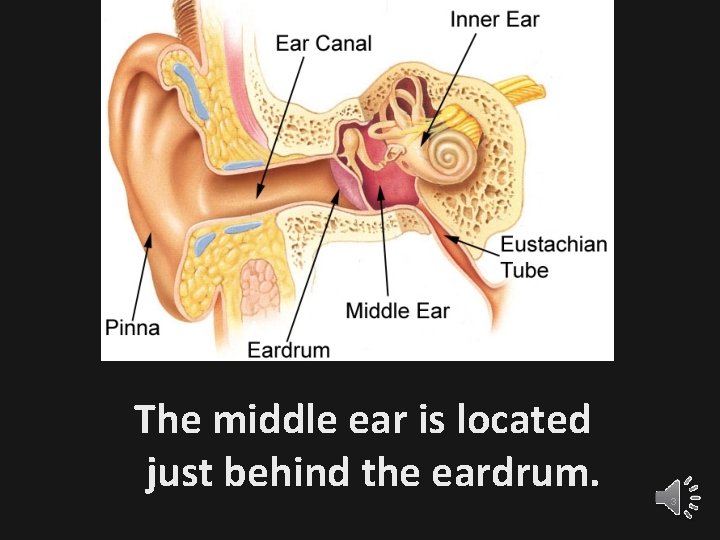
The middle ear is located just behind the eardrum. 3
§The term “Acute" refers to a short and painful episode. §An ear infection that lasts a long time or comes and goes is called Chronic Otitis Media 4
Causes Eustachian tubes to become swollen or blocked fluids to build up in the middle ear behind the eardrum. These causes include: 1 -Allergies. 2 -Colds and sinus infections 3 -Excess mucus and saliva produced during teething 4 -Infected or overgrown adenoids. 5 -Tobacco smoke or other 5
Risk factors § Cold climate (ear infections are more common in winter) § Exposure to smoke § Genetic factors (susceptibility to infection may run in families) § Ear infection § Recent illness of any type (lowers resistance of the body to infection) 6
Symptoms § In infants, the clearest sign is often irritability and inconsolable crying. - Many infants and children develop a fever or - have trouble sleeping. Symptoms in older children or adults include: § Ear pain or earache § Fullness in the ear § Feeling of general illness § Hearing loss in the affected ear 7
Exams and Tests 1 - Patient should be asked about ear infections in the past, and recent cold or allergy symptoms. 2 - Physical examination of the throat, sinuses, head, neck, lungs, and ears. 3 - The health care provider looks inside the ears using an instrument called an otoscope. 8
4 - If infected, there may be: -Areas of dullness or redness -Air bubbles or fluid behind the eardrum. “The fluid may be bloody or filled with pus” 5 - Check for any signs of perforation (a hole) in the eardrum. 6 -A hearing test may be recommended if there is a history of persistent (chronic and recurrent) ear infections. 9
Treatment Often, treating the pain and allowing the body time to heal itself is all that is needed: 1 -Apply a warm cloth or warm water bottle to the affected ear. 2 -Use over-the-counter pain relief drops for ears, or ask the doctor about prescription ear drops to relieve pain. 3 -Take over-the-counter medications for pain or fever, such as ibuprofen or acetaminophen. 10
- DO NOT give aspirin to children - All children younger than 6 months with a fever or symptoms should see the doctor. -Children who are older than 6 months may be watched at home if they do not have: 1 - A fever higher than 39 ºC. 2 - More severe pain or other symptoms 3 - Other medical problems 4 - No improvement or symptoms get worse. 11
Antibiotics are often prescribed if: § Your child is under age 2 § Has a fever § Appears sick § Is not improving over 24 to 48 hours 12
§ Amoxicillin : commonly the first choice. -Other antibiotics that may be given are azithromycin or clarithromycin, cefuroxime, amoxicillin clavulanate (Augmentin), clindamycin, or ceftriaxone. § Side effects of antibiotics: -nausea, vomiting, and diarrhea. -Although rare, serious allergic reactions may also occur. . 13
Possible complications § Most children will have minor, temporary hearing loss during and right after an ear infection. (This is due to fluid lingering in the ear) 14
Other potential complications from otitis media include § Ruptured or perforated eardrum. § Chronic, recurrent ear infections. § Enlarged adenoids or tonsils. § Mastoiditis (an infection of the bones around the skull). 15
§ Meningitis (an infection of the brain). § Formation of an abscess or a cyst (called cholesteatoma). § Speech or language delay in a child who suffers lasting hearing loss from multiple, recurrent ear infections. 16
Prevention To reduce your child's risk of ear infections : § Wash hands and toys frequently. § Breastfeed -- this makes a child much less prone to ear infections. § Do not expose your child to secondhand smoke. 17
§ Make sure your child's immunizations are up-to-date. The pneumococcal vaccine prevents infections from the bacteria that most commonly causes acute ear infections. § Avoid overusing antibiotics (Resistance) 18

Eye disorders 19
: A- External ocular conditions § The most important is conjunctivitis § Conjunctivitis is an acute inflammation of the conjunctiva, most commonly due to: - an allergic reaction or - an infection (usually viral, but sometimes bacterial) 20
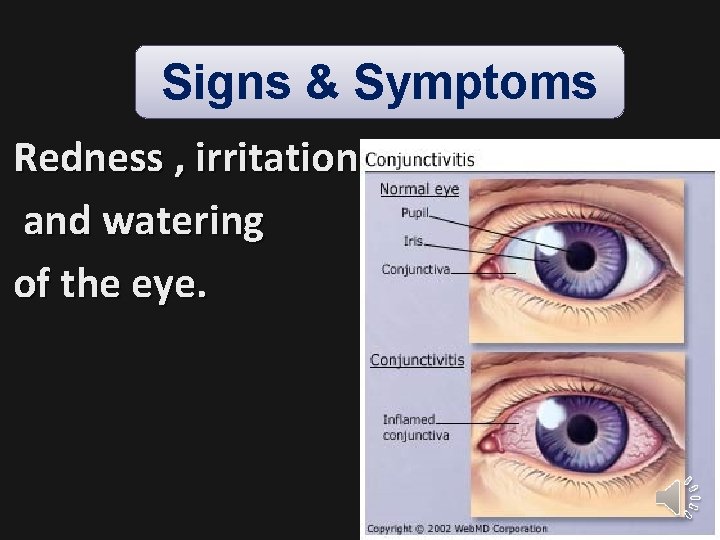
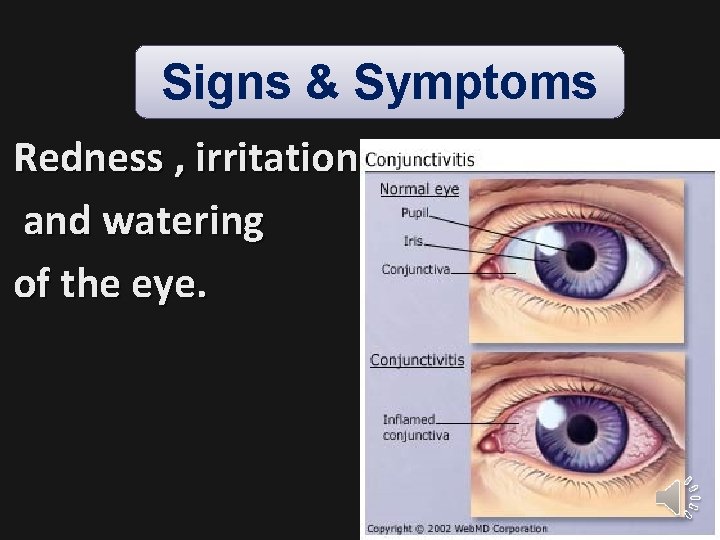
Signs & Symptoms Redness , irritation and watering of the eye. 21
Acute Conjunctivitis It has the following causes: 1 -Allergic § Typically itchy, and often involves some eye swelling. § Pale watery swelling or edema of the conjunctiva often with non-purulent mucoid discharge. Itching must be a primary symptom to make this diagnosis. 22
2 - Viral § Often associated with an infection of the upper respiratory tract, a common cold, and/or a sore throat. § Its Symptoms : Watery discharge and variable itch. Usually begins with one eye, but may spread easily to the other. § Causes: Commonly adenoviruses & herpes simplex viruses) can be serious and requires treatment with acyclovir 23
3 -Bacterial § By the common pyogenic bacteria § Causes: -Marked irritation -Opaque, grey or yellowish mucopurulent discharge may cause the lids to stick together (matting), especially after sleeping. -Also, severe crusting of the infected eye and the surrounding skin. 24
N. B. § Chlamydia trachomatis can cause a non-exudative but persistent conjunctivitis without much redness. § Like viral conjunctivitis, it usually affects only one eye but may spread easily to the other eye 25
4 -Chemical Irritant or toxic conjunctivitis is: irritable or painful when the infected eye is pointed far down or far up. § Discharge and itch are usually absent. § This is the only group in which severe pain and uncomfort may occur. § Primarily marked redness. § With some chemicals (specially with caustic alkalis such as sodium hydroxide)—necrosis may occur 26
Differential diagnosis § Symptoms and signs are (relatively non-specific) § Even after bio microscopy, laboratory tests are often necessary § Itching (rubbing eyes) hallmark symptom of Allergic conjunctivitis. § A diffuse conjunctivitis (looking pink rather than red) a Viral cause, § Scarring of the tarsal conjunctiva Trachoma. (Swabs for bacterial culture are necessary if the history and signs suggest bacterial conjunctivitis, but no response to topical antibiotics) 27
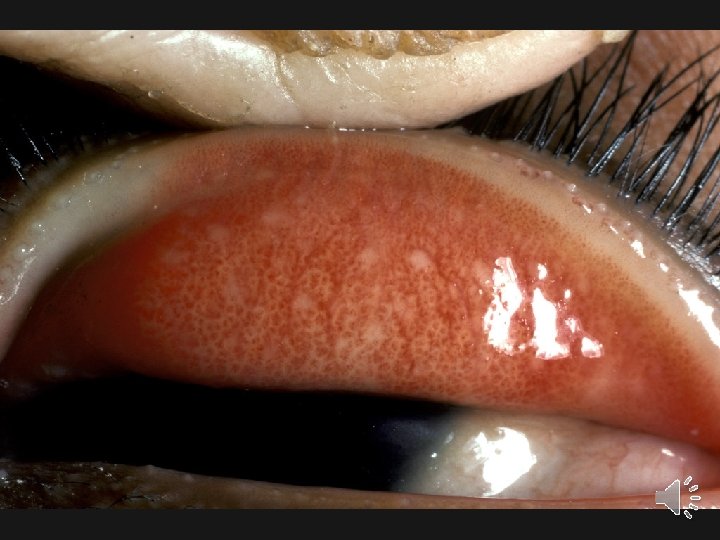
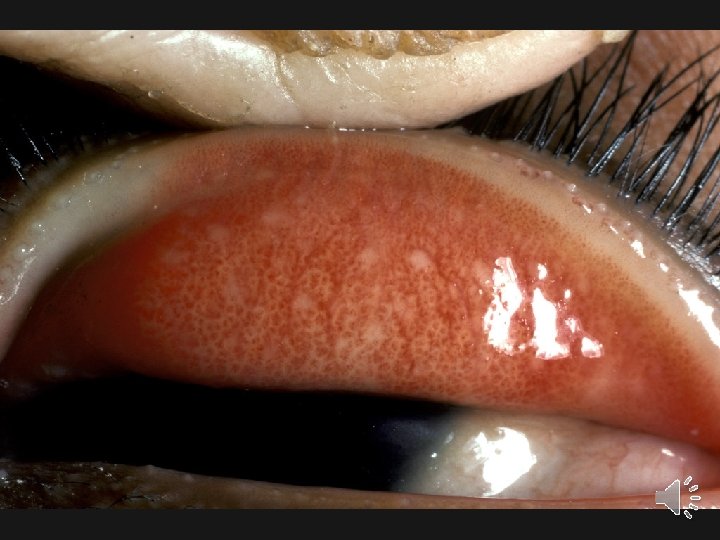
28

29
Management - 65% of cases Resolves without treatment, within 2 – 5 days. - The prescribing of antibiotics to most cases is not necessary 30
1 -Allergic § Cool water poured over the face constricts capillaries, § Severe cases: NSAIDs and antihistamines may be prescribed. Persistent allergic conjunctivitis may also require topical steroid drops. 2 -Bacterial § Resolves without treatment. § No improvement after 3 days Antibiotics, eye drops, or ointment. 31
3 -Viral § No specific treatment. § Symptomatic relief with cold compresses. § Avoid touching eyes or sharing towels and washcloths. 4 - Chemical § Irrigation with Ringer's lactate or saline solution. § Chemical injuries (particularly alkali burns) medical emergencies : can lead to severe scarring, and intraocular damage. 32
A- Internal ocular conditions § The most important is Glaucoma in which: Fluid pressure inside the eye increases causing the optic nerve to be damaged, leading to progressive, irreversible loss of vision. § It is often, but not always, associated with I. O. P. § Divided into: “Open angle" and “Closed angle" 33
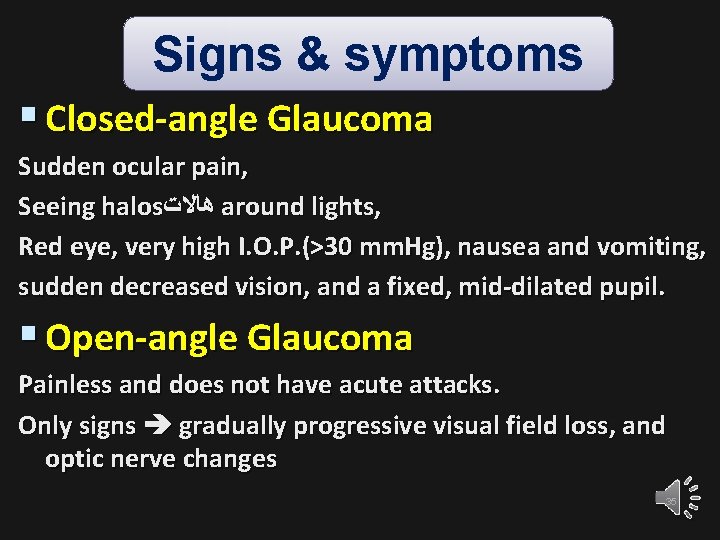
§ Closed angle glaucoma: -can appear suddenly -often painful -visual loss can progress quickly but the discomfort often leads patients to seek medical attention before permanent damage occurs. § Open angle, -chronic glaucoma -progress at a slower rate the patient may notice that they have lost vision until the disease has progressed significantly 34
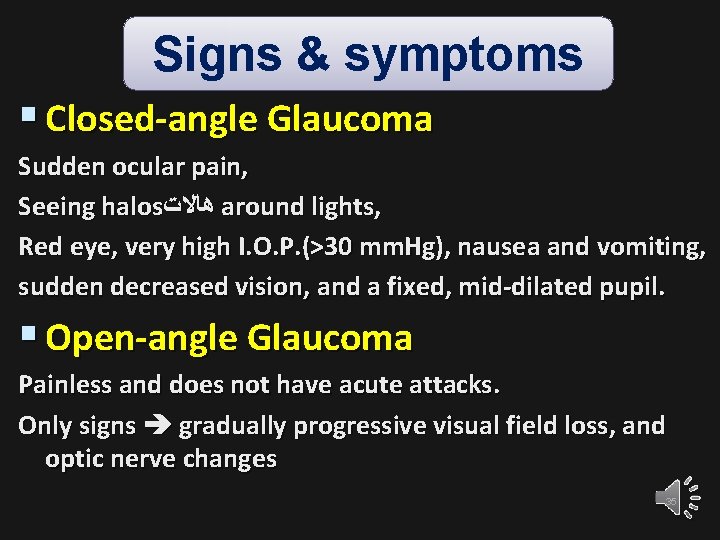
Signs & symptoms § Closed-angle Glaucoma Sudden ocular pain, Seeing halos ﻫﺎﻻﺕ around lights, Red eye, very high I. O. P. (>30 mm. Hg), nausea and vomiting, sudden decreased vision, and a fixed, mid-dilated pupil. § Open-angle Glaucoma Painless and does not have acute attacks. Only signs gradually progressive visual field loss, and optic nerve changes 35
Management § via various pharmaceuticals and/or surgical techniques is currently the mainstay of glaucoma treatment 36
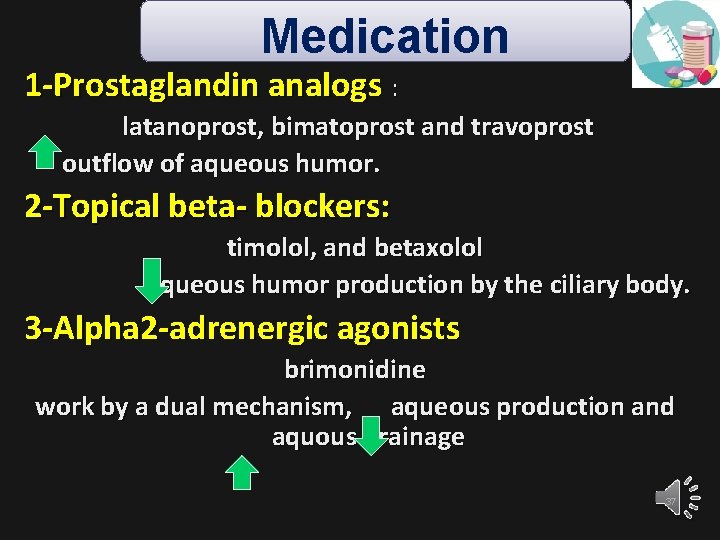
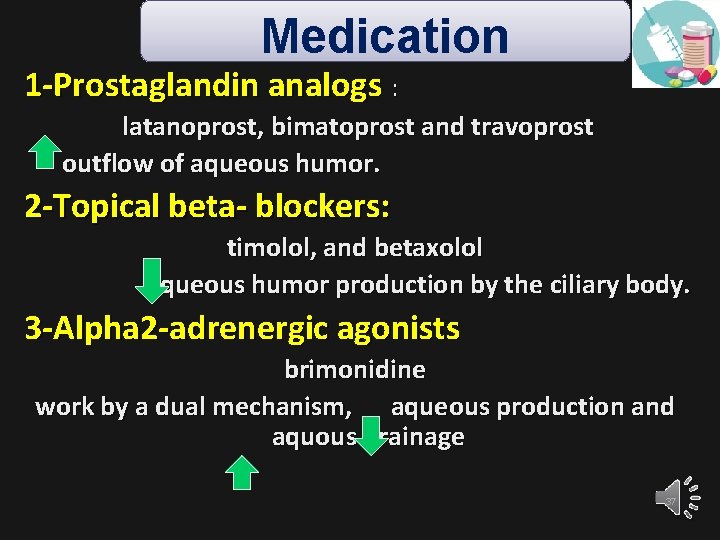
Medication 1 -Prostaglandin analogs : latanoprost, bimatoprost and travoprost outflow of aqueous humor. 2 -Topical beta- blockers: timolol, and betaxolol aqueous humor production by the ciliary body. 3 -Alpha 2 -adrenergic agonists brimonidine work by a dual mechanism, aqueous production and aquous drainage 37
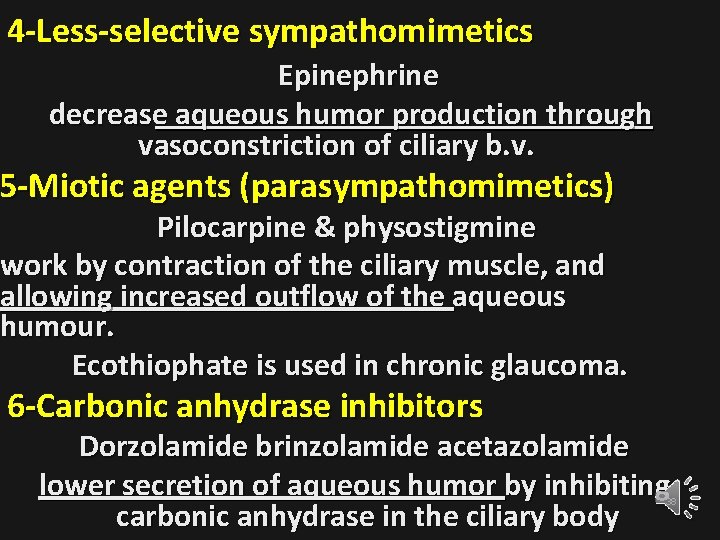
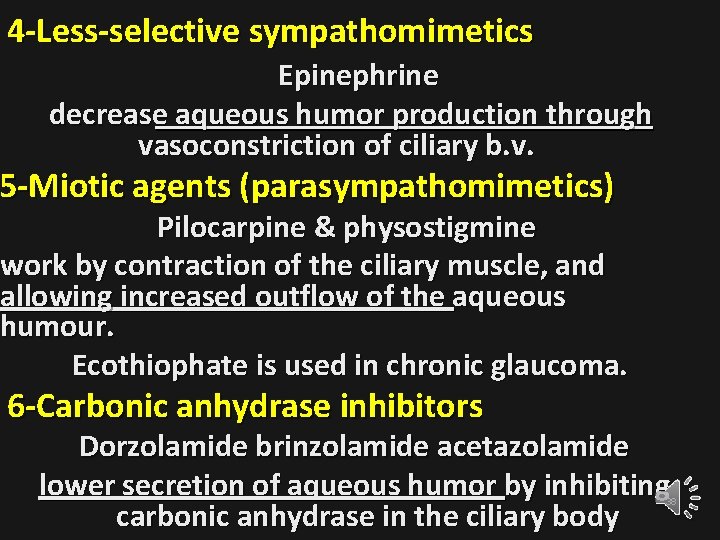
4 -Less-selective sympathomimetics Epinephrine decrease aqueous humor production through vasoconstriction of ciliary b. v. 5 -Miotic agents (parasympathomimetics) Pilocarpine & physostigmine work by contraction of the ciliary muscle, and allowing increased outflow of the aqueous humour. Ecothiophate is used in chronic glaucoma. 6 -Carbonic anhydrase inhibitors Dorzolamide brinzolamide acetazolamide lower secretion of aqueous humor by inhibiting carbonic anhydrase in the ciliary body 38

THANKS 39