E M CHART AUDITING Department of Neurology CORE





![Extent of ROS § Problem Focused: N/A [0] 99212 § Expanded Focused: Problem Pertinent Extent of ROS § Problem Focused: N/A [0] 99212 § Expanded Focused: Problem Pertinent](https://slidetodoc.com/presentation_image_h2/a688aa5a2986646b31deddab8627f8f3/image-24.jpg)
- Slides: 53
E & M CHART AUDITING Department of Neurology – CORE Presentation on E/M Documentation Neurology Residency/Fellow Program Presented by the MSU Health. Team Compliance Office September 2020
Documentation Timeliness § Per CMS and reiterated by our Medicare Administrative Contractor (MAC): Documentation should be completed within 24 to 48 hours and the general interpretation for this is 1 -2 business days. Additionally, it also describes that if documentation is not complete, services may not be billed. As well as if the signature is late, then do not just sign but enter a signed attestation. § Please see Health. Team Policy MRC-07 advising documentation must be completed within two business days of the visit: https: //www. healthteam. msu. edu/intranet/Policies/MRC%207%20 Monitoring%20 Timeliness%20 of%20 MR%20 Doc. pdf 2
Documentation Timeliness, cont… § Health. Team's policy on documentation is MRC-01 and mimics these guidelines (found at: https: //healthteam. msu. edu/intranet/Policies/MRC%2001%20 Medical%20 Record%20 Documentation. pdf), where third paragraph excerpt reads: § "Documentation must support the level of coding for billing purposes (see CPT E&M requirements) and shall be completed and electronically signed no later than two business days after the ambulatory encounter. Billing transactions must not be transmitted until documentation in the medical record is complete and permanently signed. " 3
Signature Attestations § If your signature isn’t completed within the two business days following each service, a signature attestation should be appended and should include, but is not limited to, the following information: § “I, _____[print full name of the physician/practitioner]___, hereby attest that the medical record entry for _____[date of service]___ accurately reflects signatures/notations that I made in my capacity as _____[insert provider credentials, e. g. , M. D. ]__when I treated/diagnosed the above listed Medicare beneficiary. I do hereby attest that this information is true, accurate and complete to the best of my knowledge and I understand that any falsification, omission, or concealment of material fact may subject me to administrative, civil, or criminal liability. ” § You’re allowed to change the format, but if you completely change the wording Compliance needs to review and approve 4
Signature Tips § The signature for each entry must be legible and should include the practitioner’s first and last name. § For clarification purposes, it is required by CMS to include applicable credentials, e. g. , M. D, D. O. , P. A, etc. (see MLN MM 6698) § Residents/Fellows must sign the document when performing any key components of HPI, exam, or MDM. 5

E/M Services 6
Why Document ? § Continuum of Care § Legal Liability § Reimbursement Not Documented = Not Done ! 7
General Principles of Documentation The documentation of each patient encounter should include: Reason for the encounter and relevant history, physical examination findings, and prior diagnostic test results Avoid phrases like “doing well” or “follow-up” without further elaboration. 8
General Principles of Documentation, cont… § Assessment, clinical impression or diagnosis § Clinical impressions or diagnoses should be documented for each visit § Plan of Care § Date and legible identity of the observer 9
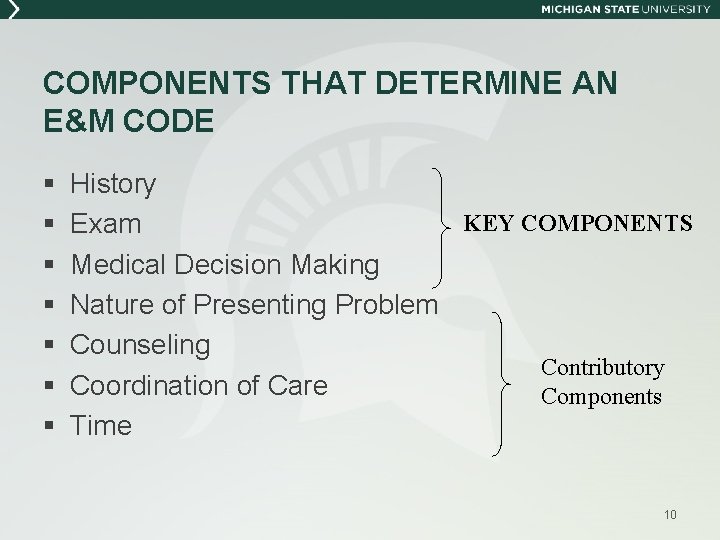
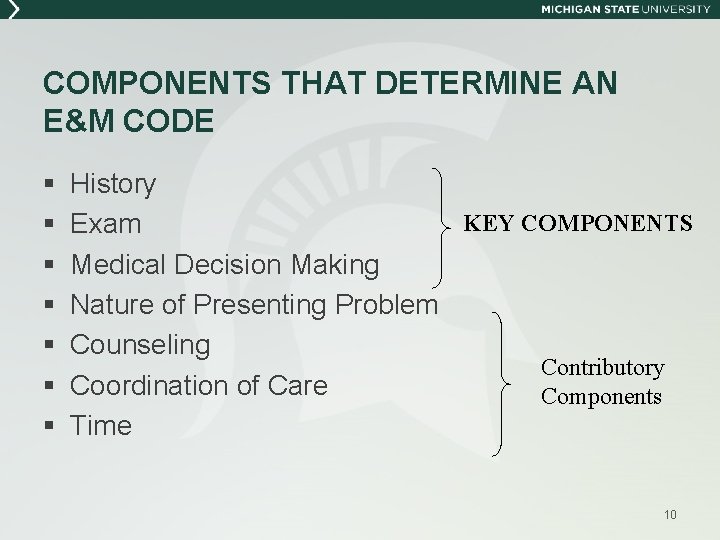
COMPONENTS THAT DETERMINE AN E&M CODE § § § § History KEY COMPONENTS Exam Medical Decision Making Nature of Presenting Problem Counseling Contributory Coordination of Care Components Time 10

NATURE OF PRESENTING PROBLEM § A presenting problem is a disease, condition, illness, injury, symptom, sign, finding, complaint, or other reason for an encounter with or without a diagnosis being established at the time of the encounter. § Medical necessity is an underlying requirement for all services billed and/or mortality and morbidity. 11
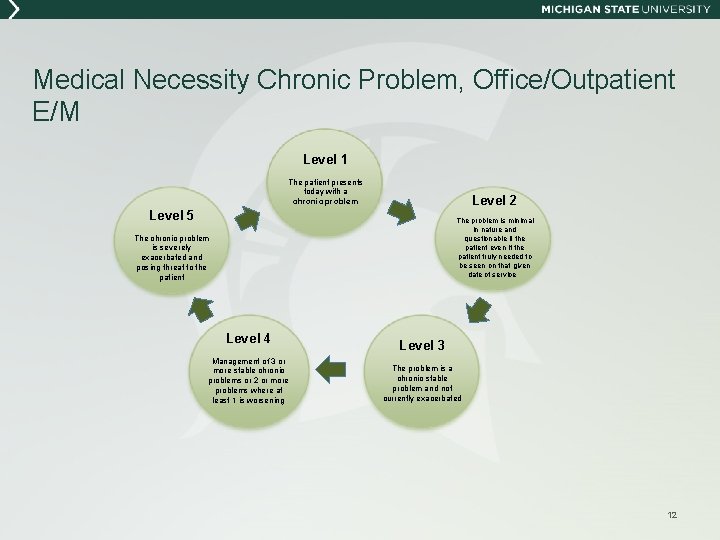
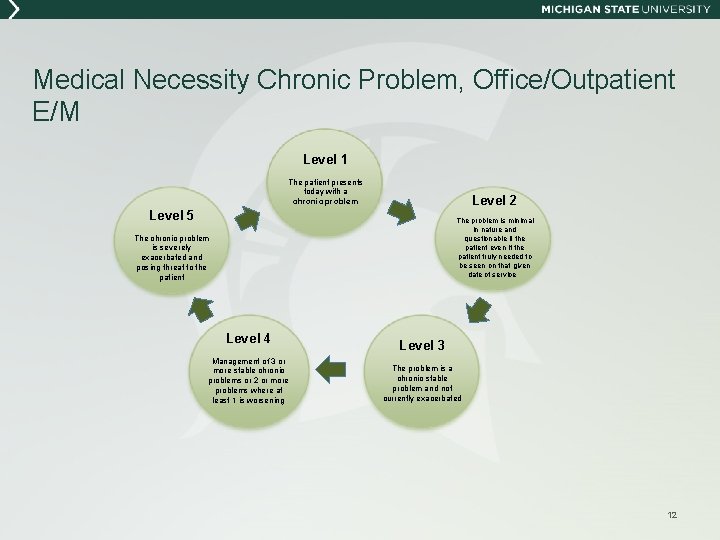
Medical Necessity Chronic Problem, Office/Outpatient E/M Level 1 The patient presents today with a chronic problem Level 2 Level 5 The problem is minimal in nature and questionable if the patient even if the patient truly needed to be seen on that given date of service The chronic problem is severely exacerbated and posing threat to the patient Level 4 Management of 3 or more stable chronic problems or 2 or more problems where at least 1 is worsening Level 3 The problem is a chronic stable problem and not currently exacerbated 12

Medical Necessity Acute Problem, Office/Outpatient E/M Level 1 The patient presents today with an Acute Presenting Problem Level 5 Level 2 The problem is minimal in nature and questionable if the patient even if the patient truly needed to be seen on that given date of service The acute problem poses a threat to life or bodily function during today’s encounter Level 4 The problem is acute with complicating factors contributing to the complexity of caring for the patient on this date of service Level 3 The problem is acute and uncomplicated in presentation to the provider 13
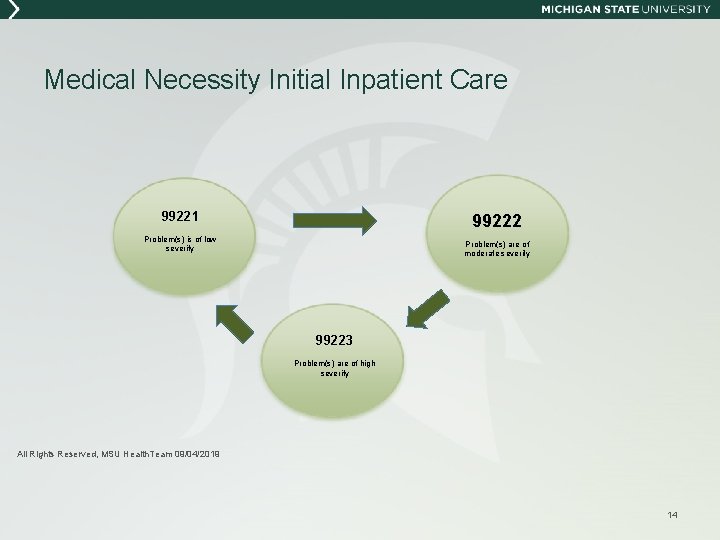
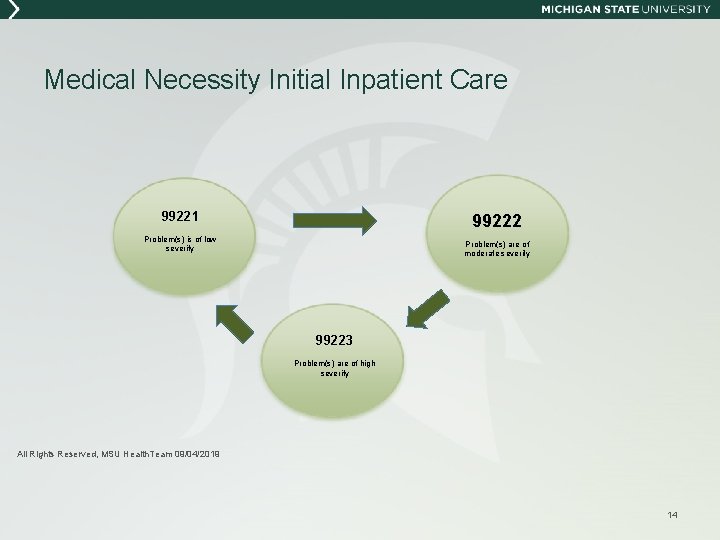
Medical Necessity Initial Inpatient Care 99221 99222 Problem(s) is of low severity Problem(s) are of moderate severity 99223 Problem(s) are of high severity All Rights Reserved, MSU Health. Team 09/04/2019 14
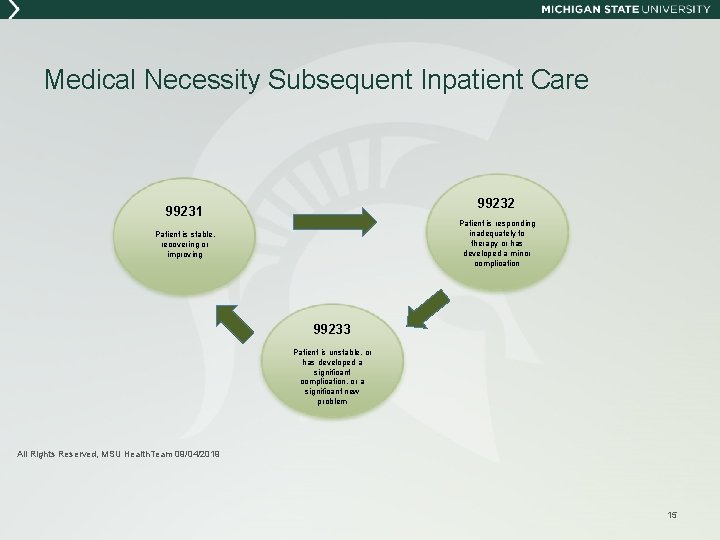
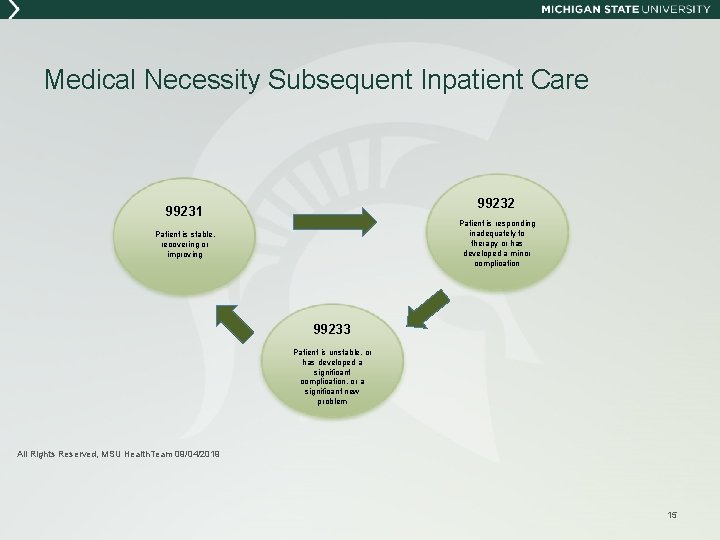
Medical Necessity Subsequent Inpatient Care 99232 99231 Patient is responding inadequately to therapy or has developed a minor complication Patient is stable, recovering or improving 99233 Patient is unstable, or has developed a significant complication, or a significant new problem All Rights Reserved, MSU Health. Team 09/04/2019 15
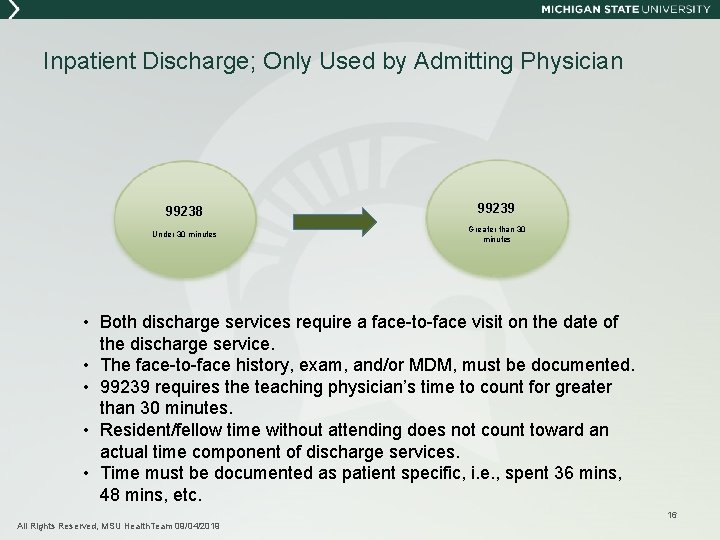
Inpatient Discharge; Only Used by Admitting Physician 99238 99239 Under 30 minutes Greater than 30 minutes • Both discharge services require a face-to-face visit on the date of the discharge service. • The face-to-face history, exam, and/or MDM, must be documented. • 99239 requires the teaching physician’s time to count for greater than 30 minutes. • Resident/fellow time without attending does not count toward an actual time component of discharge services. • Time must be documented as patient specific, i. e. , spent 36 mins, 48 mins, etc. 16 All Rights Reserved, MSU Health. Team 09/04/2019
HISTORY § § Chief Complaint History of Present Illness Review of Systems Past, Family, and Social History 17
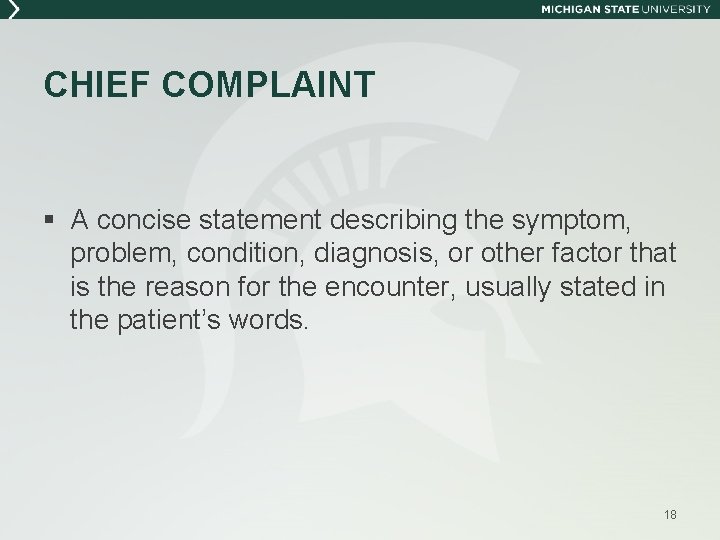
CHIEF COMPLAINT § A concise statement describing the symptom, problem, condition, diagnosis, or other factor that is the reason for the encounter, usually stated in the patient’s words. 18

HISTORY OF PRESENT ILLNESS A chronological description of the development of the patient’s present illness from the first sign and/or symptom to the present. This includes the following elements: § § § Location (Where? Low back pain) Quality (Sharp, dull, throbbing, etc…) Severity (Better/worse, mild, severe, 4/10, etc. . . ) Duration (Pain for two days, first started three years ago, etc…) Timing (Hurts in the morning, happening 3 x a week now, etc…) Context (Pain occurred after lifting bags, dropped weight on foot, etc…) § Modifying factors (Aspirin does not help, recent cerumen removal helped, etc…) § Associated signs and symptoms (i. e. vomiting, diarrhea, sweating, etc…) 19

STATUS OF CHRONIC CONDITIONS § For use with both the 1995 and 1997 Documentation Guidelines: 3 or more = Extended HPI Note: Document a brief comment about the status of the condition according to the patient, NOT the provider. This is part of the “history”, not the “assessment”. 20
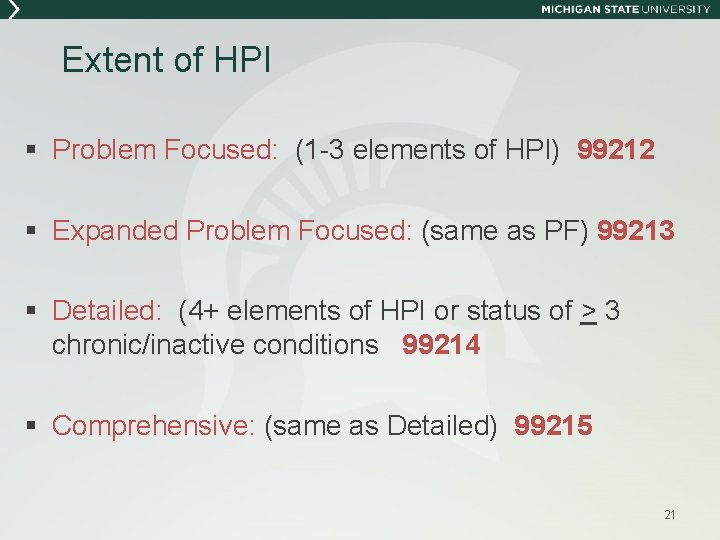
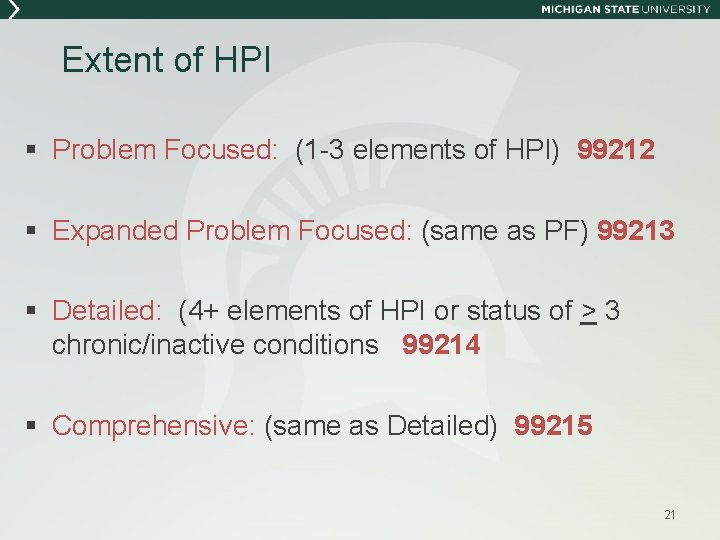
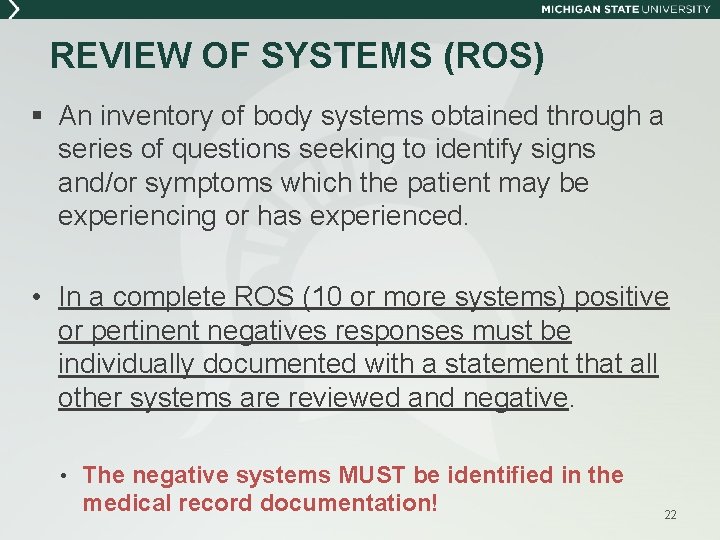
Extent of HPI § Problem Focused: (1 -3 elements of HPI) 99212 § Expanded Problem Focused: (same as PF) 99213 § Detailed: (4+ elements of HPI or status of > 3 chronic/inactive conditions 99214 § Comprehensive: (same as Detailed) 99215 21
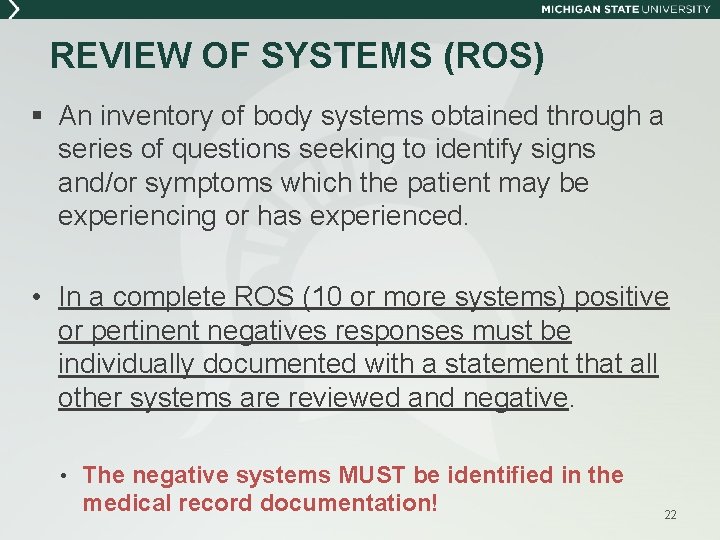
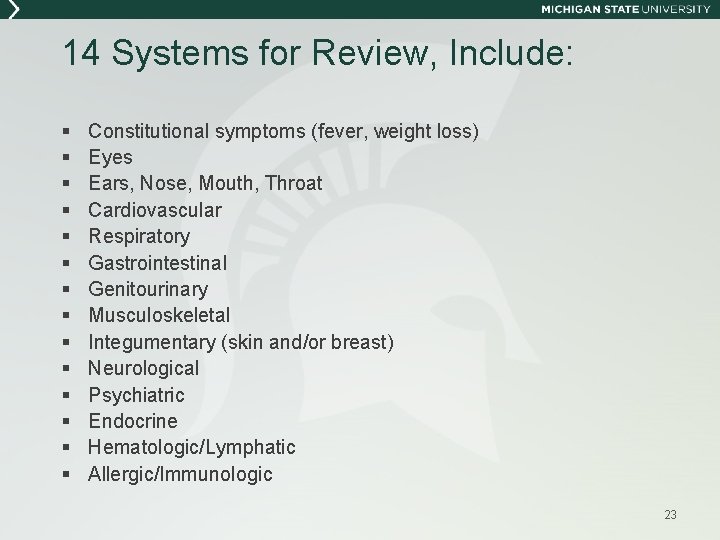
REVIEW OF SYSTEMS (ROS) § An inventory of body systems obtained through a series of questions seeking to identify signs and/or symptoms which the patient may be experiencing or has experienced. • In a complete ROS (10 or more systems) positive or pertinent negatives responses must be individually documented with a statement that all other systems are reviewed and negative. • The negative systems MUST be identified in the medical record documentation! 22
14 Systems for Review, Include: § § § § Constitutional symptoms (fever, weight loss) Eyes Ears, Nose, Mouth, Throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Integumentary (skin and/or breast) Neurological Psychiatric Endocrine Hematologic/Lymphatic Allergic/Immunologic 23
![Extent of ROS Problem Focused NA 0 99212 Expanded Focused Problem Pertinent Extent of ROS § Problem Focused: N/A [0] 99212 § Expanded Focused: Problem Pertinent](https://slidetodoc.com/presentation_image_h2/a688aa5a2986646b31deddab8627f8f3/image-24.jpg)
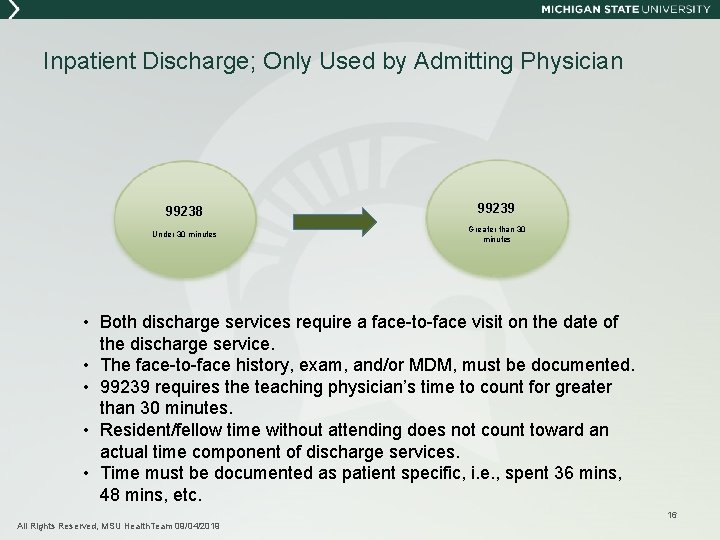
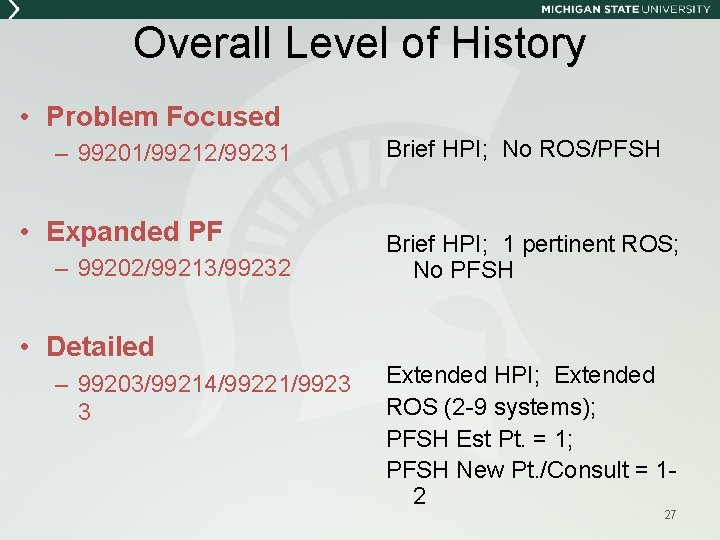
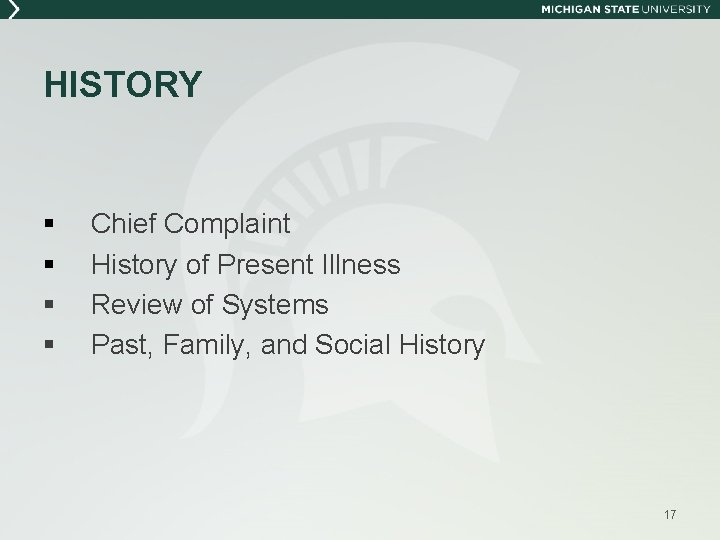
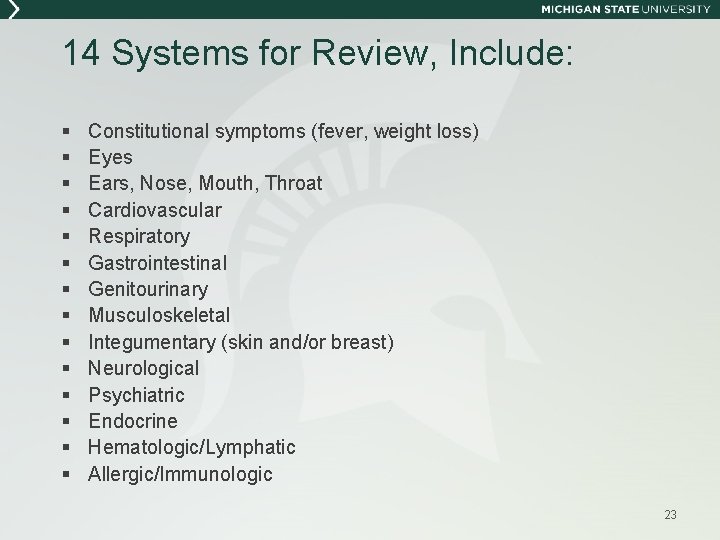
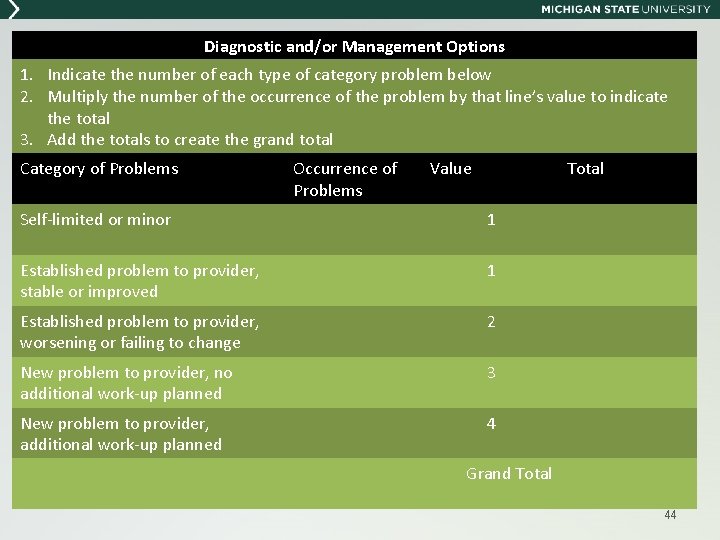
Extent of ROS § Problem Focused: N/A [0] 99212 § Expanded Focused: Problem Pertinent [1] 99213 § Detailed: Extended [2 -9] 99214 § Comprehensive: Complete [10+] 99215 § or pertinent positive and pertinent negative responses with notation that “all other systems reviewed and negative* • The “all other systems” MUST have each system identified in the medical record documentation! 24
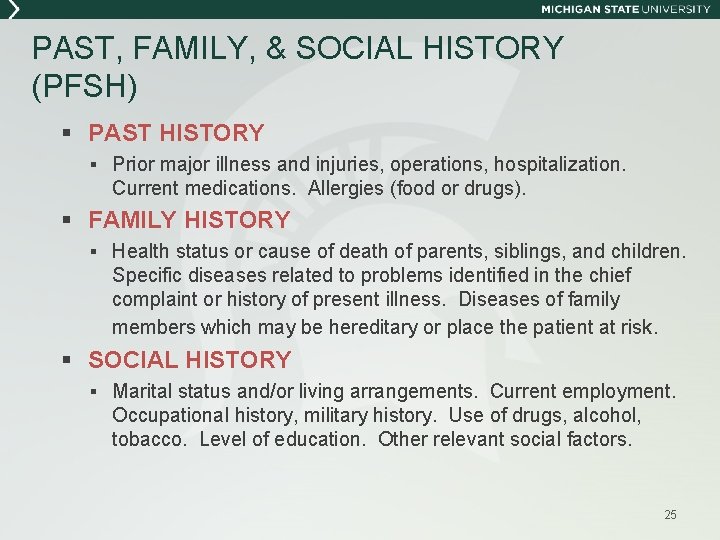
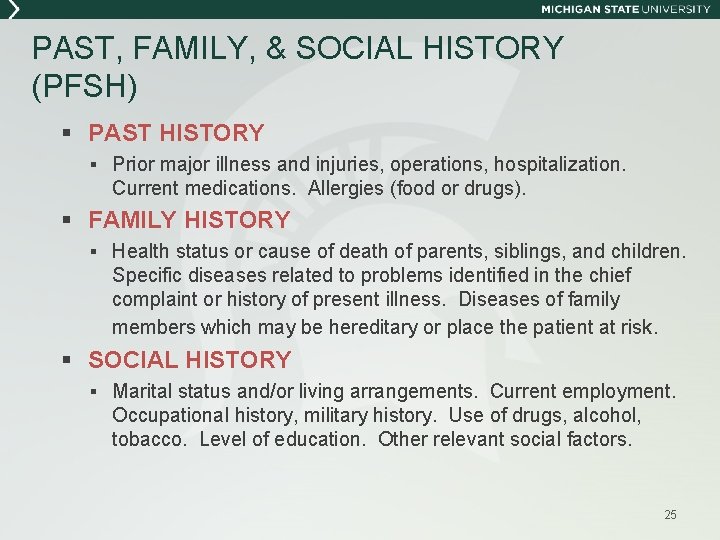
PAST, FAMILY, & SOCIAL HISTORY (PFSH) § PAST HISTORY § Prior major illness and injuries, operations, hospitalization. Current medications. Allergies (food or drugs). § FAMILY HISTORY § Health status or cause of death of parents, siblings, and children. Specific diseases related to problems identified in the chief complaint or history of present illness. Diseases of family members which may be hereditary or place the patient at risk. § SOCIAL HISTORY § Marital status and/or living arrangements. Current employment. Occupational history, military history. Use of drugs, alcohol, tobacco. Level of education. Other relevant social factors. 25
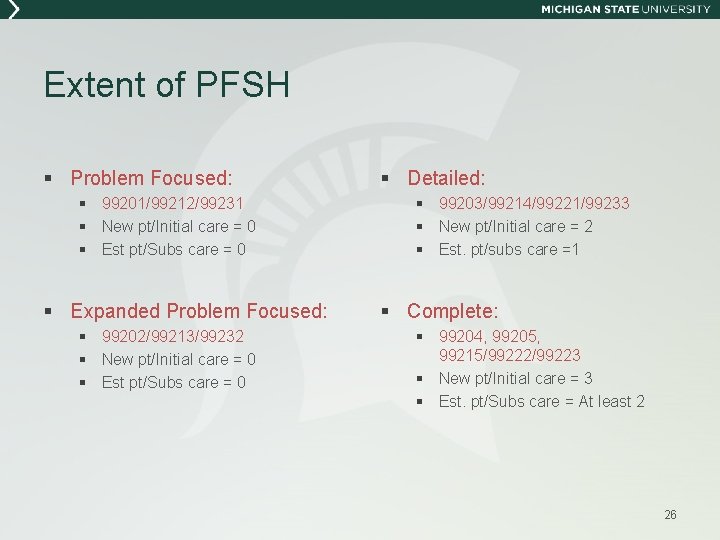
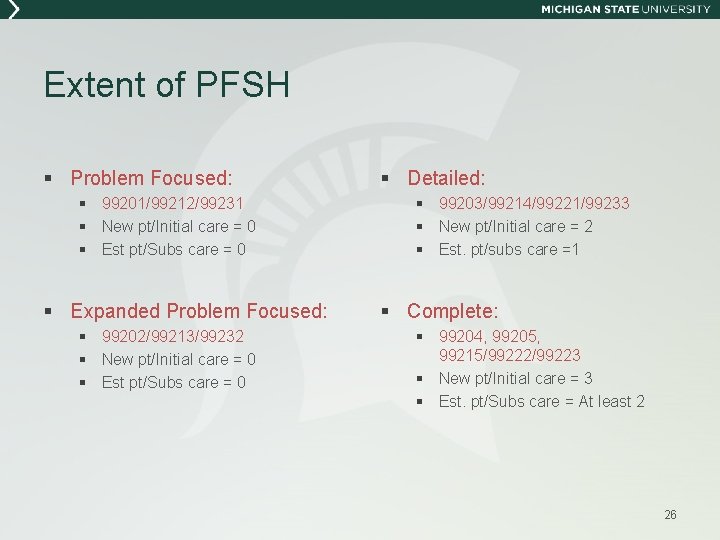
Extent of PFSH § Problem Focused: § 99201/99212/99231 § New pt/Initial care = 0 § Est pt/Subs care = 0 § Expanded Problem Focused: § 99202/99213/99232 § New pt/Initial care = 0 § Est pt/Subs care = 0 § Detailed: § 99203/99214/99221/99233 § New pt/Initial care = 2 § Est. pt/subs care =1 § Complete: § 99204, 99205, 99215/99222/99223 § New pt/Initial care = 3 § Est. pt/Subs care = At least 2 26
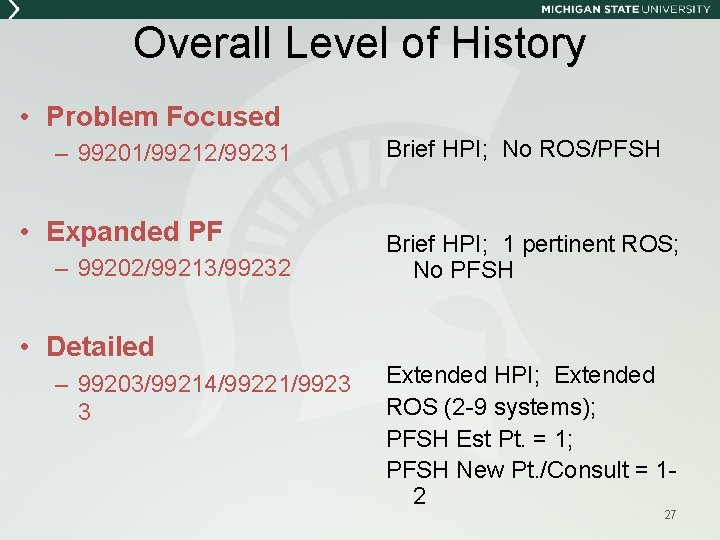
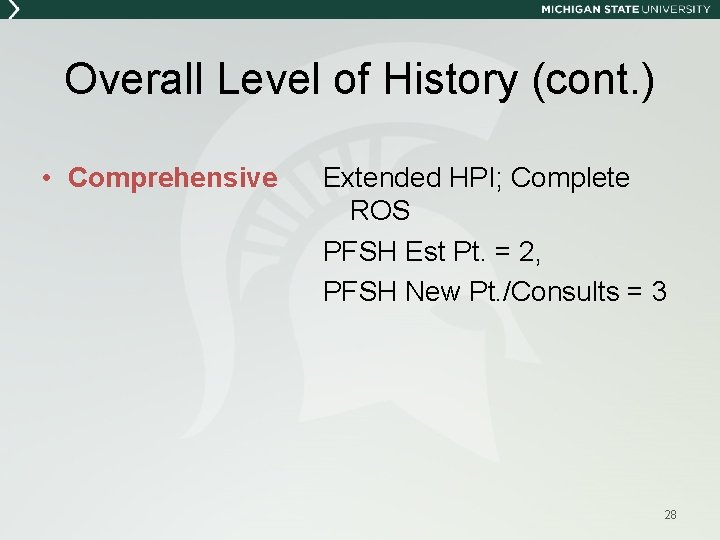
Overall Level of History • Problem Focused – 99201/99212/99231 • Expanded PF – 99202/99213/99232 • Detailed – 99203/99214/99221/9923 3 Brief HPI; No ROS/PFSH Brief HPI; 1 pertinent ROS; No PFSH Extended HPI; Extended ROS (2 -9 systems); PFSH Est Pt. = 1; PFSH New Pt. /Consult = 12 27
Overall Level of History (cont. ) • Comprehensive Extended HPI; Complete ROS PFSH Est Pt. = 2, PFSH New Pt. /Consults = 3 28
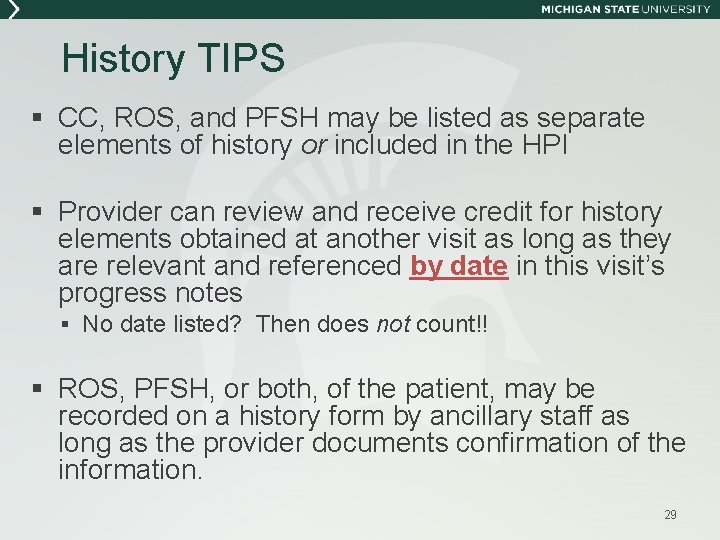
History TIPS § CC, ROS, and PFSH may be listed as separate elements of history or included in the HPI § Provider can review and receive credit for history elements obtained at another visit as long as they are relevant and referenced by date in this visit’s progress notes § No date listed? Then does not count!! § ROS, PFSH, or both, of the patient, may be recorded on a history form by ancillary staff as long as the provider documents confirmation of the information. 29
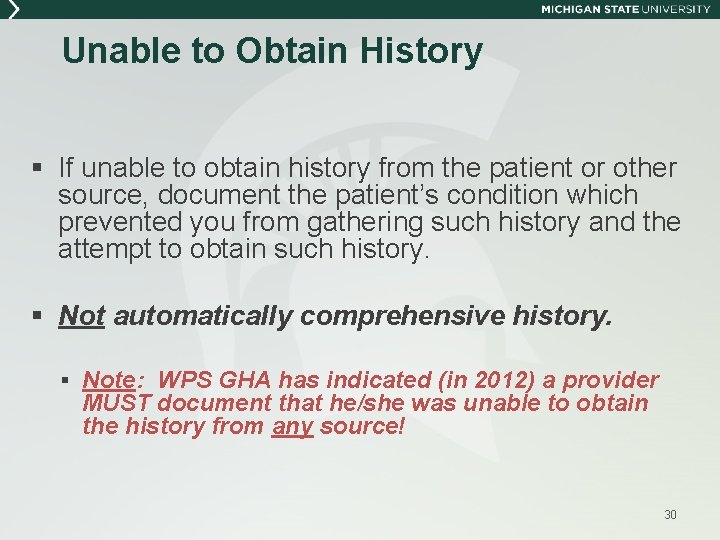
Unable to Obtain History § If unable to obtain history from the patient or other source, document the patient’s condition which prevented you from gathering such history and the attempt to obtain such history. § Not automatically comprehensive history. § Note: WPS GHA has indicated (in 2012) a provider MUST document that he/she was unable to obtain the history from any source! 30
HISTORY QUESTIONS 31
1995 PHYSICAL EXAMINATION
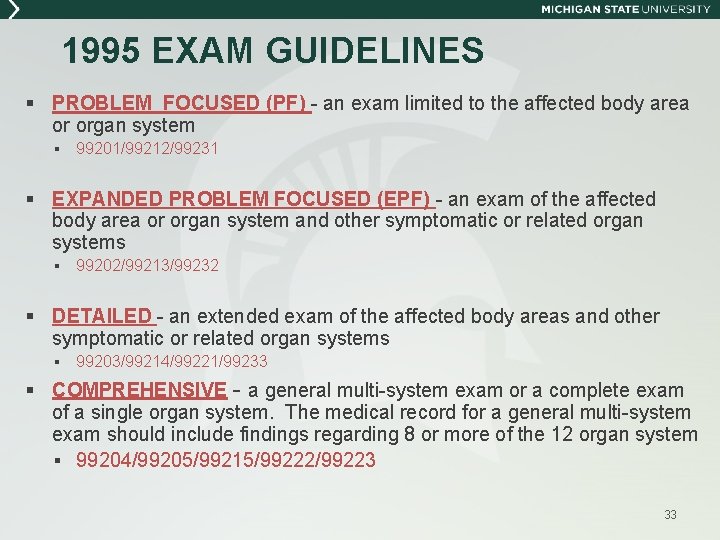
1995 EXAM GUIDELINES § PROBLEM FOCUSED (PF) - an exam limited to the affected body area or organ system § 99201/99212/99231 § EXPANDED PROBLEM FOCUSED (EPF) - an exam of the affected body area or organ system and other symptomatic or related organ systems § 99202/99213/99232 § DETAILED - an extended exam of the affected body areas and other symptomatic or related organ systems § 99203/99214/99221/99233 § COMPREHENSIVE - a general multi-system exam or a complete exam of a single organ system. The medical record for a general multi-system exam should include findings regarding 8 or more of the 12 organ system § 99204/99205/99215/99222/99223 33
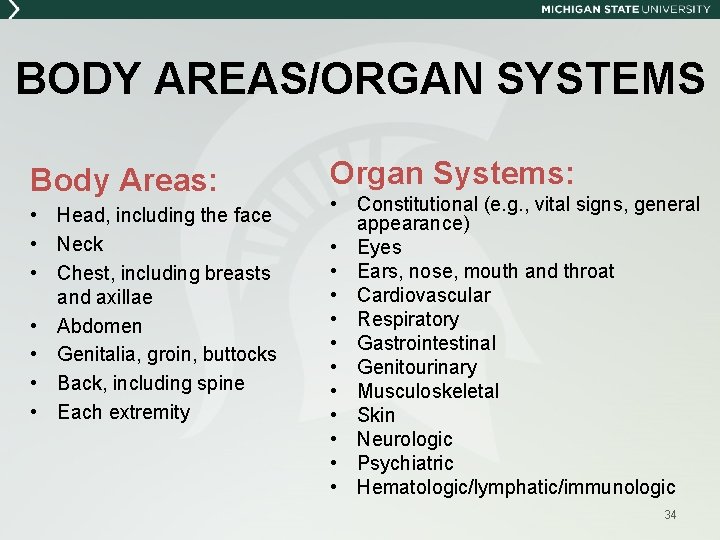
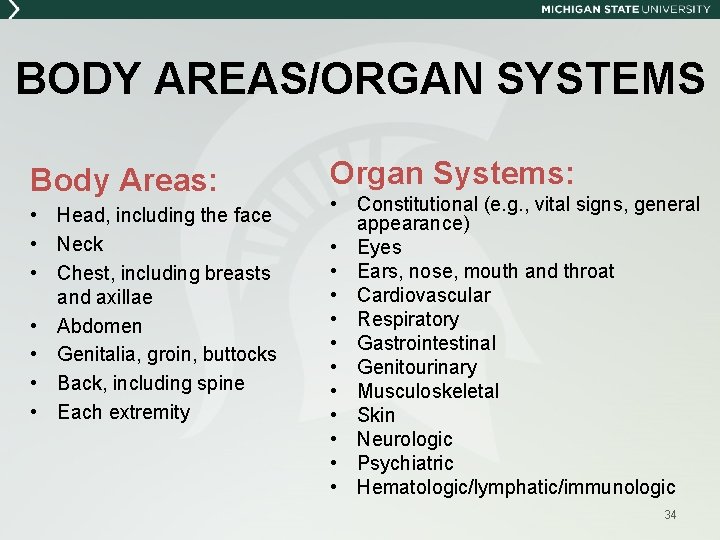
BODY AREAS/ORGAN SYSTEMS Body Areas: • Head, including the face • Neck • Chest, including breasts and axillae • Abdomen • Genitalia, groin, buttocks • Back, including spine • Each extremity Organ Systems: • Constitutional (e. g. , vital signs, general appearance) • Eyes • Ears, nose, mouth and throat • Cardiovascular • Respiratory • Gastrointestinal • Genitourinary • Musculoskeletal • Skin • Neurologic • Psychiatric • Hematologic/lymphatic/immunologic 34
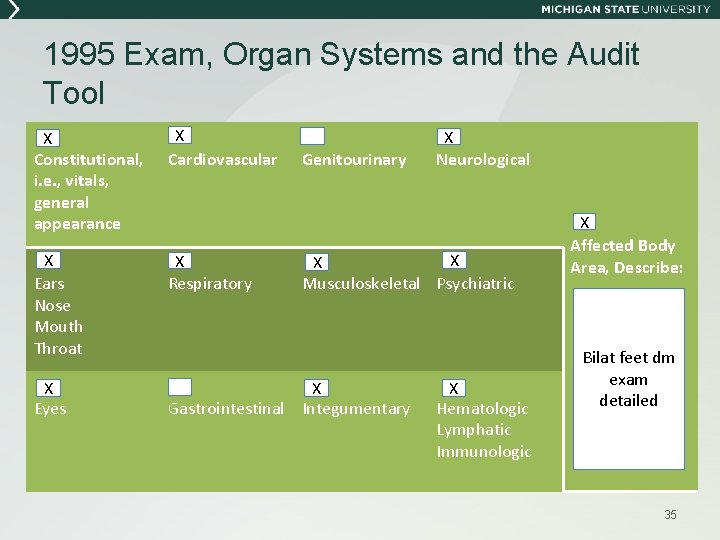
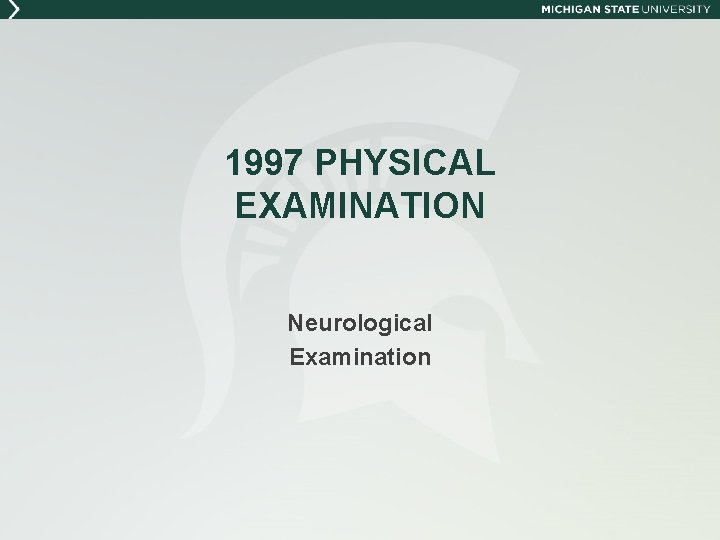
1995 Exam, Organ Systems and the Audit Tool X Constitutional, i. e. , vitals, general appearance X Cardiovascular X Ears Nose Mouth Throat X Respiratory X Eyes X Gastrointestinal Integumentary Genitourinary X Neurological X X Musculoskeletal Psychiatric X Hematologic Lymphatic Immunologic X Affected Body Area, Describe: Bilat feet dm exam detailed 35
1997 PHYSICAL EXAMINATION Neurological Examination
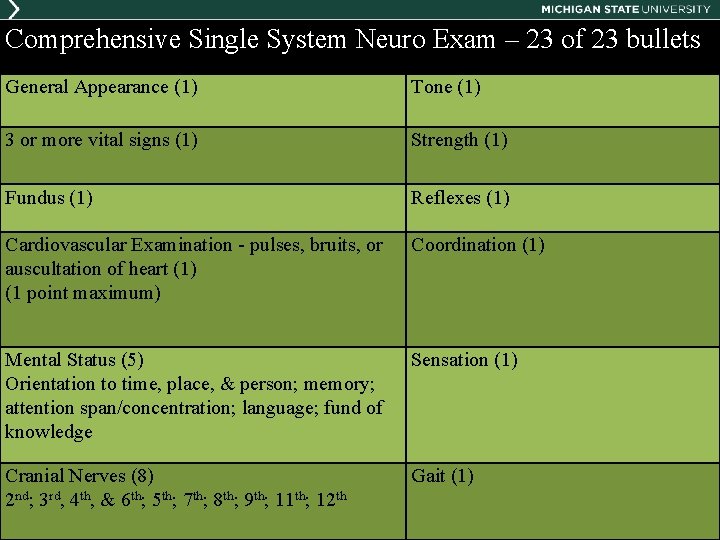
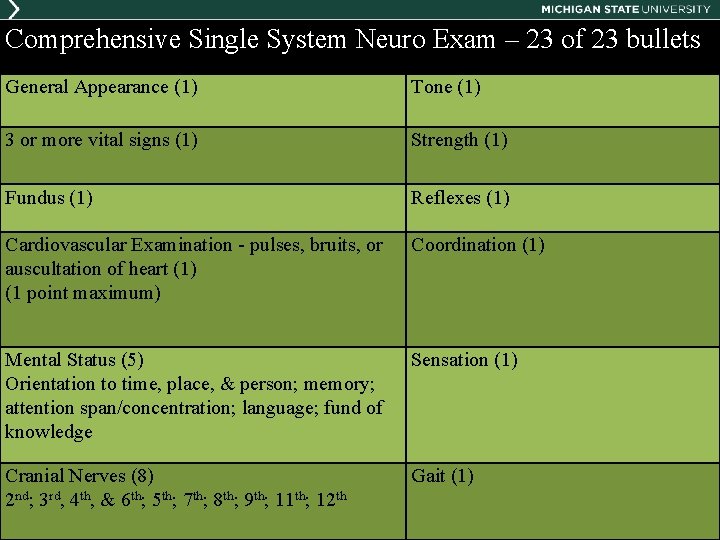
Comprehensive Single System Neuro Exam – 23 of 23 bullets General Appearance (1) Tone (1) 3 or more vital signs (1) Strength (1) Fundus (1) Reflexes (1) Cardiovascular Examination - pulses, bruits, or auscultation of heart (1) (1 point maximum) Coordination (1) Mental Status (5) Orientation to time, place, & person; memory; attention span/concentration; language; fund of knowledge Sensation (1) Cranial Nerves (8) 2 nd; 3 rd, 4 th, & 6 th; 5 th; 7 th; 8 th; 9 th; 11 th; 12 th Gait (1) 37
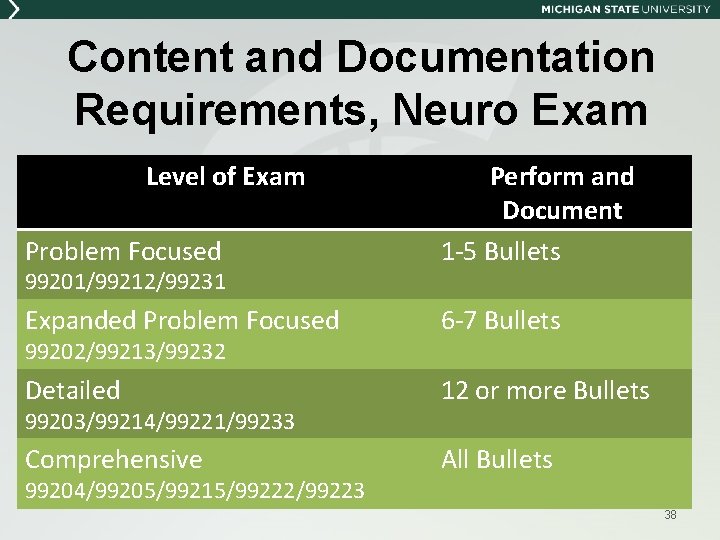
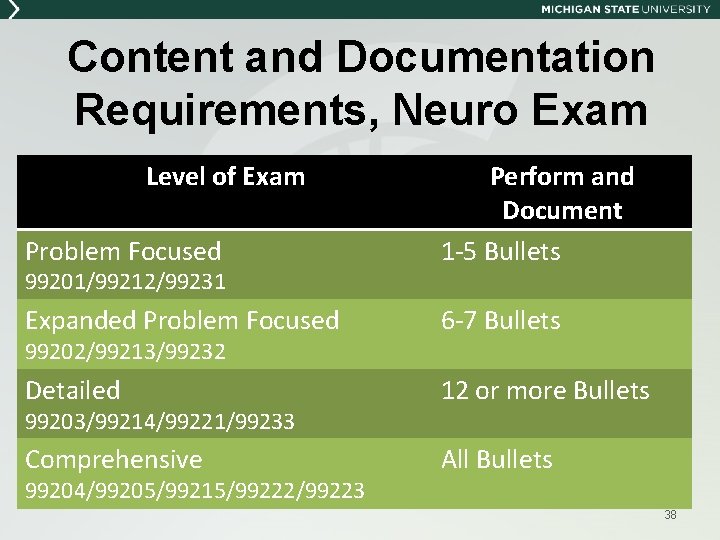
Content and Documentation Requirements, Neuro Exam Level of Exam Problem Focused Perform and Document 1 -5 Bullets Expanded Problem Focused 6 -7 Bullets Detailed 12 or more Bullets Comprehensive All Bullets 99201/99212/99231 99202/99213/99232 99203/99214/99221/99233 99204/99205/99215/99222/99223 38
EXAMINATION QUESTIONS 39
MEDICAL DECISION MAKING INCLUDES: § Part A - Number of Diagnoses or Treatment Options § Part B - Amount and Complexity of Data § Part C - Risk of Significant Complications, Morbidity, and Mortality 40
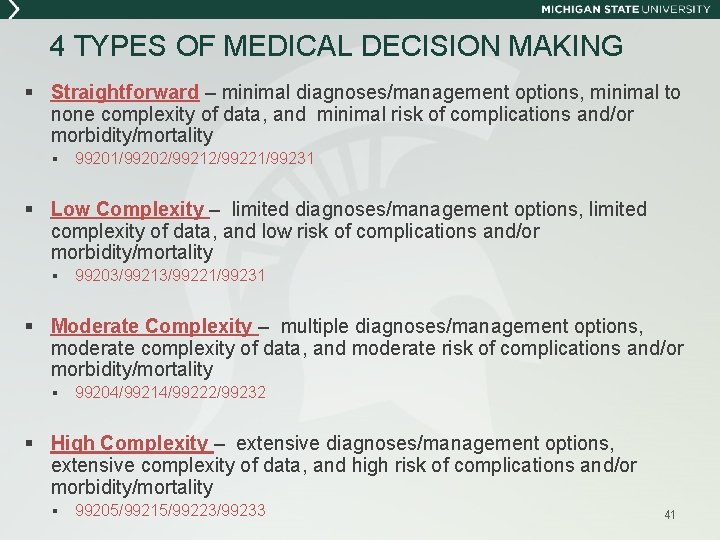
4 TYPES OF MEDICAL DECISION MAKING § Straightforward – minimal diagnoses/management options, minimal to none complexity of data, and minimal risk of complications and/or morbidity/mortality § 99201/99202/99212/99221/99231 § Low Complexity – limited diagnoses/management options, limited complexity of data, and low risk of complications and/or morbidity/mortality § 99203/99213/99221/99231 § Moderate Complexity – multiple diagnoses/management options, moderate complexity of data, and moderate risk of complications and/or morbidity/mortality § 99204/99214/99222/99232 § High Complexity – extensive diagnoses/management options, extensive complexity of data, and high risk of complications and/or morbidity/mortality § 99205/99215/99223/99233 41
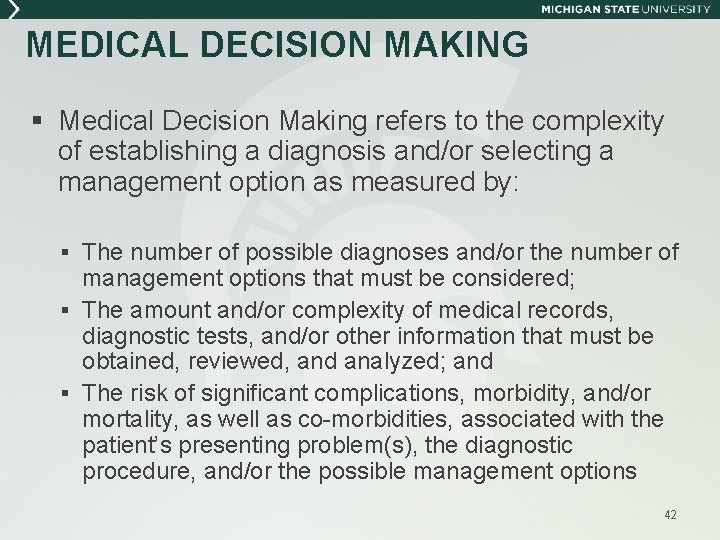
MEDICAL DECISION MAKING § Medical Decision Making refers to the complexity of establishing a diagnosis and/or selecting a management option as measured by: § The number of possible diagnoses and/or the number of management options that must be considered; § The amount and/or complexity of medical records, diagnostic tests, and/or other information that must be obtained, reviewed, and analyzed; and § The risk of significant complications, morbidity, and/or mortality, as well as co-morbidities, associated with the patient’s presenting problem(s), the diagnostic procedure, and/or the possible management options 42
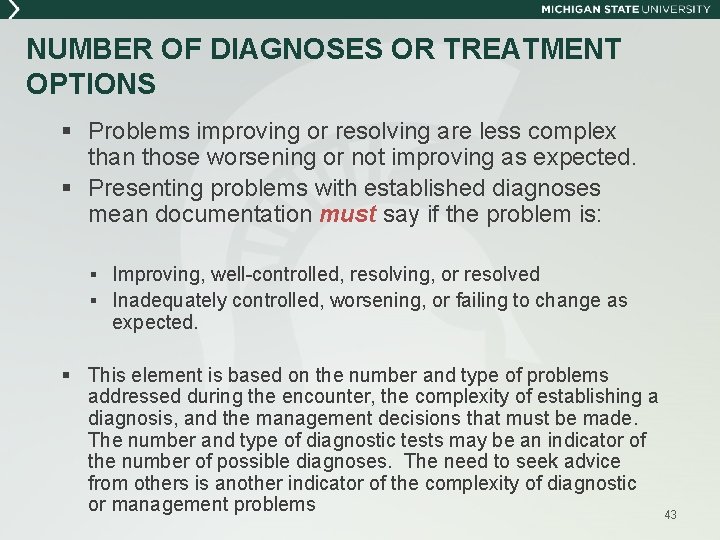
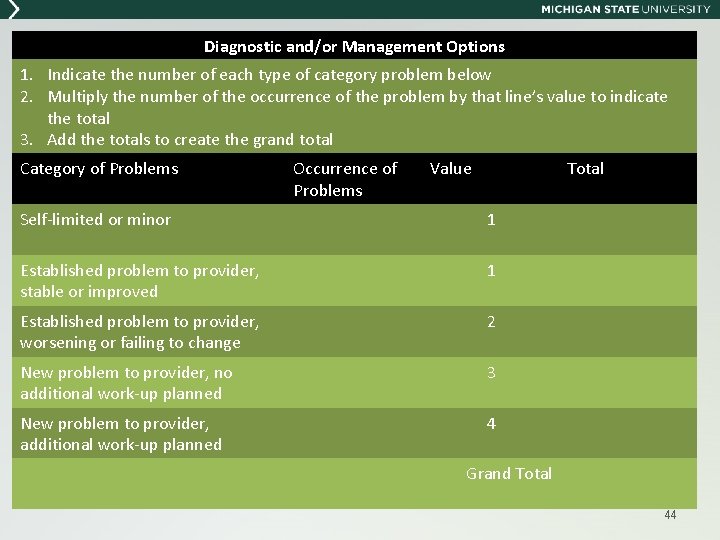
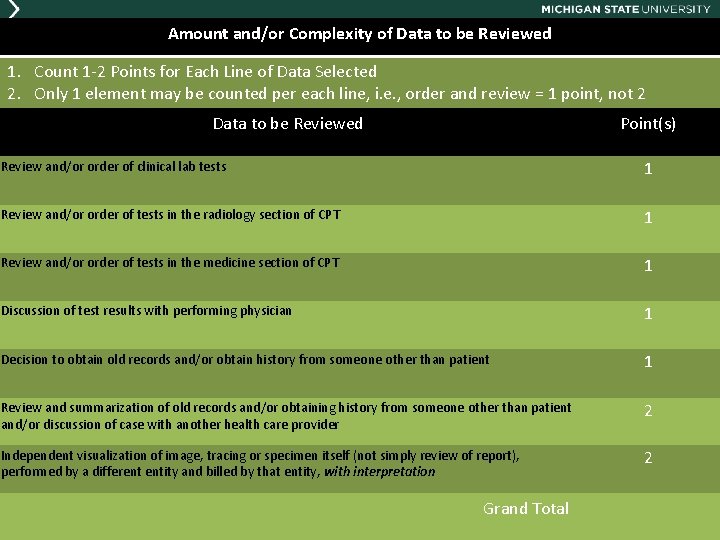
NUMBER OF DIAGNOSES OR TREATMENT OPTIONS § Problems improving or resolving are less complex than those worsening or not improving as expected. § Presenting problems with established diagnoses mean documentation must say if the problem is: § Improving, well-controlled, resolving, or resolved § Inadequately controlled, worsening, or failing to change as expected. § This element is based on the number and type of problems addressed during the encounter, the complexity of establishing a diagnosis, and the management decisions that must be made. The number and type of diagnostic tests may be an indicator of the number of possible diagnoses. The need to seek advice from others is another indicator of the complexity of diagnostic or management problems 43
Diagnostic and/or Management Options 1. Indicate the number of each type of category problem below 2. Multiply the number of the occurrence of the problem by that line’s value to indicate the total 3. Add the totals to create the grand total Category of Problems Occurrence of Problems Value Total Self-limited or minor 1 Established problem to provider, stable or improved 1 Established problem to provider, worsening or failing to change 2 New problem to provider, no additional work-up planned 3 New problem to provider, additional work-up planned 4 Grand Total 44
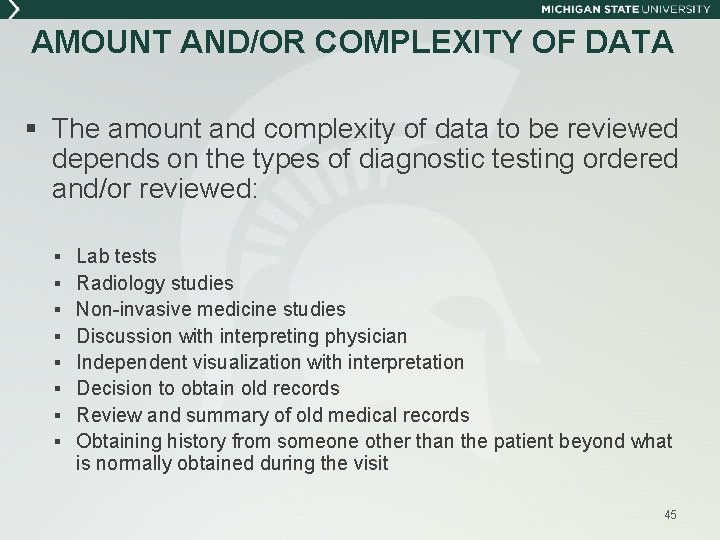
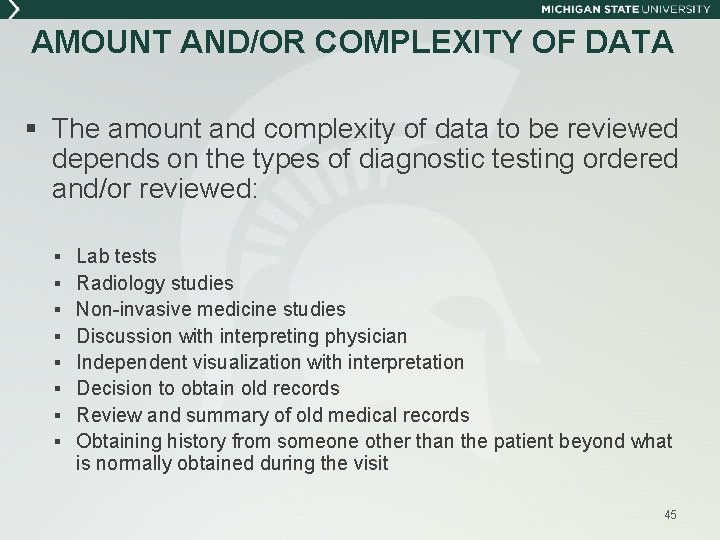
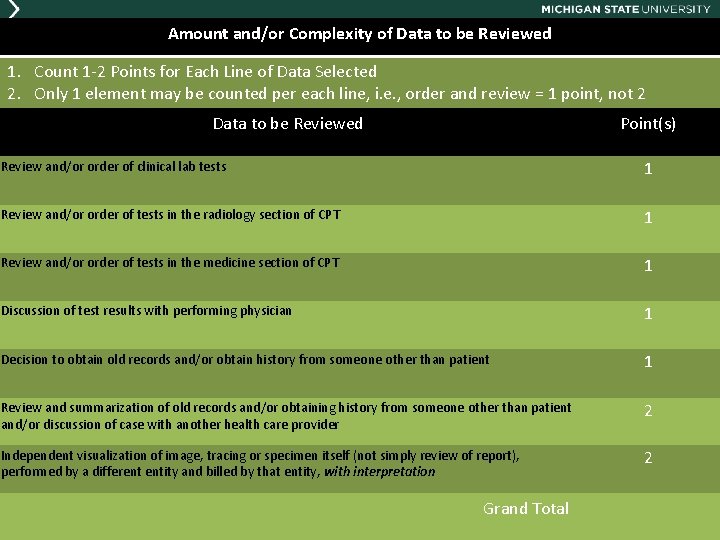
AMOUNT AND/OR COMPLEXITY OF DATA § The amount and complexity of data to be reviewed depends on the types of diagnostic testing ordered and/or reviewed: § Lab tests § Radiology studies § Non-invasive medicine studies § Discussion with interpreting physician § Independent visualization with interpretation § Decision to obtain old records § Review and summary of old medical records § Obtaining history from someone other than the patient beyond what is normally obtained during the visit 45
Amount and/or Complexity of Data to be Reviewed 1. Count 1 -2 Points for Each Line of Data Selected 2. Only 1 element may be counted per each line, i. e. , order and review = 1 point, not 2 Data to be Reviewed Point(s) Review and/or order of clinical lab tests 1 Review and/or order of tests in the radiology section of CPT 1 Review and/or order of tests in the medicine section of CPT 1 Discussion of test results with performing physician 1 Decision to obtain old records and/or obtain history from someone other than patient 1 Review and summarization of old records and/or obtaining history from someone other than patient and/or discussion of case with another health care provider 2 Independent visualization of image, tracing or specimen itself (not simply review of report), performed by a different entity and billed by that entity, with interpretation 2 Grand Total 46
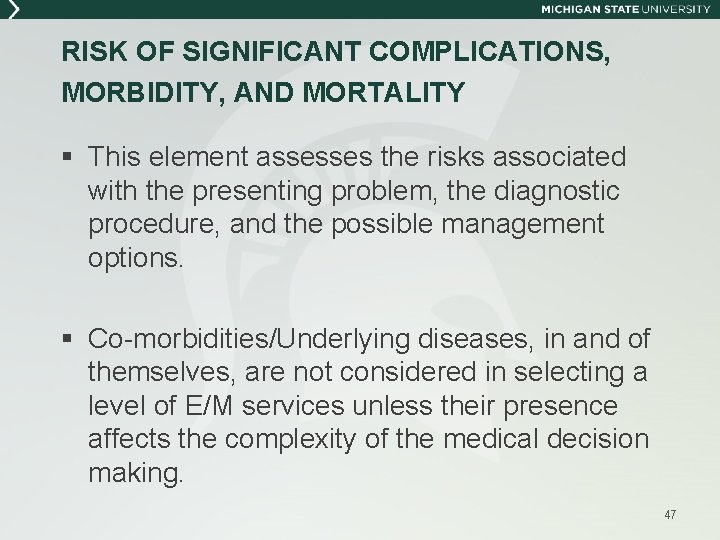
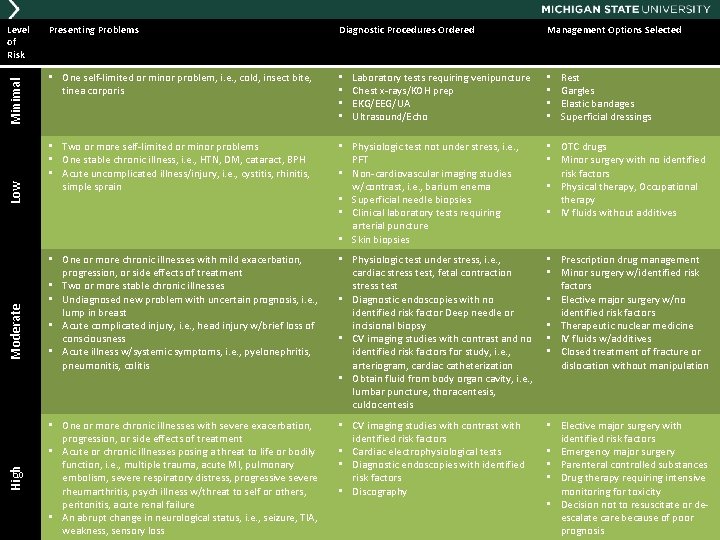
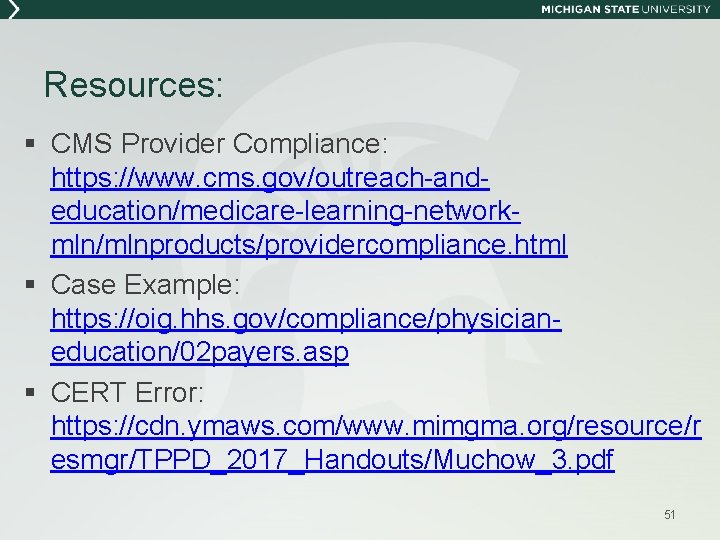
RISK OF SIGNIFICANT COMPLICATIONS, MORBIDITY, AND MORTALITY § This element assesses the risks associated with the presenting problem, the diagnostic procedure, and the possible management options. § Co-morbidities/Underlying diseases, in and of themselves, are not considered in selecting a level of E/M services unless their presence affects the complexity of the medical decision making. 47
High Moderate Low Minimal Level of Risk Presenting Problems Diagnostic Procedures Ordered • One self-limited or minor problem, i. e. , cold, insect bite, tinea corporis • • • Two or more self-limited or minor problems • One stable chronic illness, i. e. , HTN, DM, cataract, BPH • Acute uncomplicated illness/injury, i. e. , cystitis, rhinitis, simple sprain • Physiologic test not under stress, i. e. , PFT • Non-cardiovascular imaging studies w/contrast, i. e. , barium enema • Superficial needle biopsies • Clinical laboratory tests requiring arterial puncture • Skin biopsies • OTC drugs • Minor surgery with no identified risk factors • Physical therapy, Occupational therapy • IV fluids without additives • One or more chronic illnesses with mild exacerbation, progression, or side effects of treatment • Two or more stable chronic illnesses • Undiagnosed new problem with uncertain prognosis, i. e. , lump in breast • Acute complicated injury, i. e. , head injury w/brief loss of consciousness • Acute illness w/systemic symptoms, i. e. , pyelonephritis, pneumonitis, colitis • Physiologic test under stress, i. e. , cardiac stress test, fetal contraction stress test • Diagnostic endoscopies with no identified risk factor Deep needle or incisional biopsy • CV imaging studies with contrast and no identified risk factors for study, i. e. , arteriogram, cardiac catheterization • Obtain fluid from body organ cavity, i. e. , lumbar puncture, thoracentesis, culdocentesis • Prescription drug management • Minor surgery w/identified risk factors • Elective major surgery w/no identified risk factors • Therapeutic nuclear medicine • IV fluids w/additives • Closed treatment of fracture or dislocation without manipulation • One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment • Acute or chronic illnesses posing a threat to life or bodily function, i. e. , multiple trauma, acute MI, pulmonary embolism, severe respiratory distress, progressive severe rheumarthritis, psych illness w/threat to self or others, peritonitis, acute renal failure • An abrupt change in neurological status, i. e. , seizure, TIA, weakness, sensory loss • CV imaging studies with contrast with identified risk factors • Cardiac electrophysiological tests • Diagnostic endoscopies with identified risk factors • Discography • Elective major surgery with identified risk factors • Emergency major surgery • Parenteral controlled substances • Drug therapy requiring intensive monitoring for toxicity • Decision not to resuscitate or de 48 poor escalate care because of prognosis Laboratory tests requiring venipuncture Chest x-rays/KOH prep EKG/EEG/UA Ultrasound/Echo Management Options Selected • • Rest Gargles Elastic bandages Superficial dressings
MEDICAL DECISION MAKING QUESTIONS 49
Resources § CMS 1995 DG: https: //www. cms. gov/outreach-andeducation/medicare-learning-networkmln/mlnedwebguide/downloads/95 docguidelines. pdf § CMS 1997 DG: https: //www. cms. gov/outreach-andeducation/medicare-learning-networkmln/mlnedwebguide/downloads/97 docguidelines. pdf § CMS Complying with Medical Record Documentation Requirements: https: //www. cms. gov/Outreach-and. Education/Medicare-Learning-Network. MLN/MLNProducts/Downloads/CERTMed. Rec. Doc-Fact. Sheet. ICN 909160. pdf § CMS Fraud, Waste, and Abuse Toolkit: https: //www. cms. gov/outreach-andeducation/outreach/partnerships/fraudpreventiontoolkit. html 50
Resources: § CMS Provider Compliance: https: //www. cms. gov/outreach-andeducation/medicare-learning-networkmln/mlnproducts/providercompliance. html § Case Example: https: //oig. hhs. gov/compliance/physicianeducation/02 payers. asp § CERT Error: https: //cdn. ymaws. com/www. mimgma. org/resource/r esmgr/TPPD_2017_Handouts/Muchow_3. pdf 51
Resources: § CMS E/M Documentation by Students: https: //www. cms. gov/Outreach-and. Education/Medicare-Learning-Network. MLN/MLNMatters. Articles/Downloads/MM 10412. pdf § Health. Team Policies: https: //www. healthteam. msu. edu/intranet/policie s. asp 52
MSU HEALTHTEAM COMPLIANCE OFFICE Kristine Cuddy-Cummings - Compliance Analyst 355 -4547 Laticia Wing – Compliance Analyst 432 -8681 Michelle Campbell - Compliance Analyst in Training 353 -5733 Kris Fortin – Operations Coordinator I 432 -8680 John Hazewinkel – Compliance Officer 355 -1822