DYSFUNCTIONAL UTERINE BLEEDING Definition Nomenclature DUB Bleeding from
DYSFUNCTIONAL UTERINE BLEEDING
Definition & Nomenclature • DUB: - Bleeding from the uterine endometrium with no demonstratable organic cause. • Abnormal uterine bleeding, Irregular uterine bleeding, Anovularoty uterine bleeding.
Ovulatory cycle • Proliferative Phase • Secretory Phase • Menstruation • Cyclic, predictable and relatively consistent menstrual blood loss.
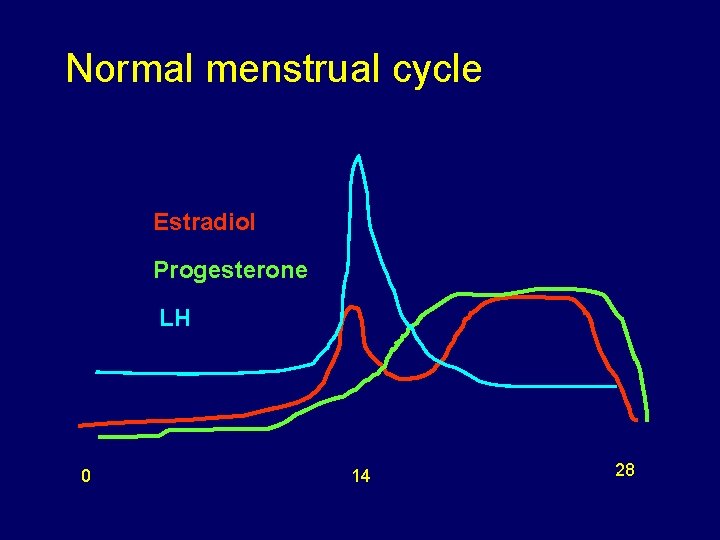
Normal menstrual cycle Estradiol Progesterone LH 0 14 28
Normal Menses • Intervals of 24 to 35 days. • Duration of 4 to 6 days. • Average volume of 35 ml.
Normal Menses Hemostasis: - • Vasoconstriction. • Platelet plugs. • Myometrial contraction.
Menstrual Abnormalities Menorrhagia ( hypermenorrhea ): • Duration > 7 days • Volume > 80 ml • Occurring at regular intervals
Menstrual Abnormalities Metrorrhagia: • Bleeding occurring at irregular but frequent intervals. • Volume is variable.
Menstrual Abnormalities Menometrorrhagia: - • Prolonged uterine bleeding at irregular intervals.
Menstrual Abnormalities Polymenorrhea: - • Bleeding at regular intervals of less than 24 days.
Menstrual Abnormalities • Oligomenorrhea: Intervals greater than 35 days.
Menstrual Abnormalities Intermanstrual Bleeding: - • Bleeding of variable amounts occurring between regular menstrual periods.
Causes of abnormal vaginal bleeding • • • Bleeding associated with pregnancy. Anovulation. Uterine leiomyoma. Endometrial polyp. Endometrial hyperplasia or carcinoma. Cervical or vaginal neoplasia. Infection. Adenomyosis. Coagulopathies. Iatrogenic & medications. Systemic diseases.
DUB • Anovulatory 90% , commonest at the extremes of the reproductive age. • Ovulatory 10%
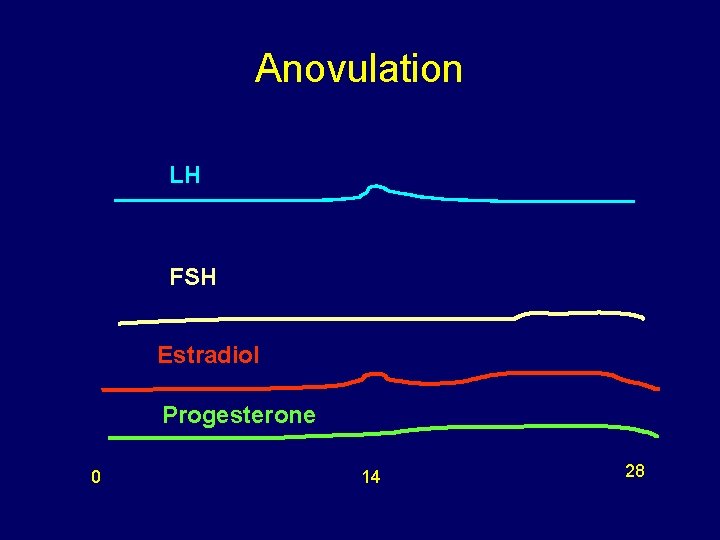
Anovulation LH FSH Estradiol Progesterone 0 14 28
Gynaecological bleeding • Estrogen withdrawal • Estrogen breakthrough • Progesterone withdrawal • Progesterone breakthrough
Pathophysiology • Anovulation. • No Corpus Luteum. • No progesterone. • Unopposed estrogen activity. • Unsustainable endometrial growth. • Irregular endometrial loss. ( non cyclic, unpredictable bleeding with inconsistent volume)
Causes of Anovulation Physiologic: • • Pregnancy Adolescence Perimenopause Lactation
Causes of Anovulation Pathologic: • Hyperandrogenic anovulation (PCO, CAH, Tumors) • Hypothalamic dysfunction (anorexia nervosa) • Hyperprolactinemia • Hypothyroidism • Primary pituitary disease • Premature ovarian failure • Iatrogenic
Establishing the diagnosis It is a diagnosis of exclusion • History. • Physical examination. • Investigations.
Age Considerations Adolescents (13 -18 Years) • Anovulation is physiologic. • Blood dyscrasias.
Age Considerations Reproductive age (19 -39 Years) • Between 6% to 10% have Hyperandrogenic chronic anovulation. • Hypothalamic dysfunction (stress, exercise, weight loss)
Age Considerations Later Reproductive Age (40 Years to Menopause) • Incidence of anovulatory uterine bleeding increases. • Represents a continuation of declining ovarian function.
Endometrial Evaluation Incidence: • Age 15 -19 is 0. 1 per 100, 000 • Age 19 -39 is 9. 5 per 100, 000 (however Age 35 -39 is 6. 1/100, 000) • Age 40 to Menopause is 36. 2/100, 000
Endometrial Evaluation • 2 -3 years of anovulatory bleeding, obese. • No response to medical therapy or prolonged periods of unopposed estrogen stimulation. • >40
management Goals: • Alleviate acute bleeding. • Prevent future episodes of non-cyclic bleeding. • Decrease the risk of long term complications of anovulation. • Improve the quality of life.
management • No single approach is appropriate for all. Approach depends on: • Amount of bleeding. • Age. • Medical status. • Desire to become pregnant.
Armamentarium • • Progestin Oral contraceptive pills Estrogen Nonsteroidal Anti-inflammatory Drugs Anti-fibrinolytic Agents Androgenic Steroids Gn. RH agonists
Armamentarium Surgical: • D&C • Endometrial ablation • Hysterectomy
Endometrial ablation • Satisfaction 80 -90 % • 34% of patients in 5 years had a hysterectomy.
Recommendations • Treatment of choice for anovulatory uterine bleeding is medical thearapy, OCP or Progestins. • Women who have failed medical therapy and no longer desire future childbearing are candidates for endometrial ablation or hysterectomy.
QUESTIONS
- Slides: 34