DVT and PE Pharamcotherapy TEACHING SLIDES Olavo Fernandes
- Slides: 24
DVT and PE Pharamcotherapy TEACHING SLIDES Olavo Fernandes Pharm. D. Pharmacy Practice Leader, University Health Network Assistant Professor, University of Toronto October 2002
UHN Residency Open House • Monday October 21 st, 2002 5: 30 pm to 8: 00 pm • Princess Margaret Hospital 610 University Ave 5 th Floor Cafeteria • The evening will include: • An information session on our residency program · A question and answer period · Tours of the department and the hospitals • Food will be provided • Please RSVP • to Tamar / Nancy at 416 -340 -3611 By October 18 th, 2002
DEFINTIONS DVT • thrombus material composed of cellular material (RBC, WBC, Plts) bound together with fibrin strands • forms in the venous portion of the vasculature PE • thrombus from systemic circulation lodges in pulmonary artery or branches causing complete or partial obstruction of pulmonary blood flow • 95% originate from DVT • Submassive – <50 % of pulmonary vascular bed occluded • VTE= DVT + PE • Massive – <50 % of pulmonary vascular bed occluded
EPIDEMIOLOGY DVT • 48 per 100, 000 PE • 69 per 100, 000 (with our without associated DVT) • 100, 000 deaths annually due to PE • Mortality (30% untreated; 8% with treatment )
PATHOPHYSIOLOGY • Virchow’s Triangle – abnormalities in blood blow • (bed rest, tumour obstruction) – abnormalities in clotting function • (malignancy, pregnancy, deficiencies in Anti-thrombin III, Ptn S or C) – abnormal vascular surfaces • (catheters, vascular injury, trauma) • To form a clot: imbalance in triangle; activation of intrinsic and extrinsic pathway and cascade • Venous Thrombi (red) • Arterial Thrombi (white)
RISK FACTORS for DVT • • surgery or trauma MI stroke increasing age prior VTE estrogen use Factor V leiden • • Anti-phospholipid syndrome pregnancy CHF Cancer obesity prolonged immobilization Smoking Ptn C or S or antithrombin deficiency • HIT
CLINICAL PRESENTATION DVT • • • symptoms present when – obstruction of venous flow – inflammation of vein wall or perivascular space – embolization to lung unilateral leg pain leg tenderness leg swelling redness/ discolouration palpable cord venous distention Homan sign (calf pain on dorsiflexion of the foot) SILENT presentation PE • • • *transient dyspnea (84%) tachypnea (RR > 20) 85% +pleuritic chest pain (74%) *apprehension (63%) tachycardia (HR > 100) (58%) cough (50%) +hemoptysis (28%) *syncope (13%) hypoxemia, hypotension, cardiogenic shock *more often assoc with massive PE +more often assoc with submassive PE SILENT presentation
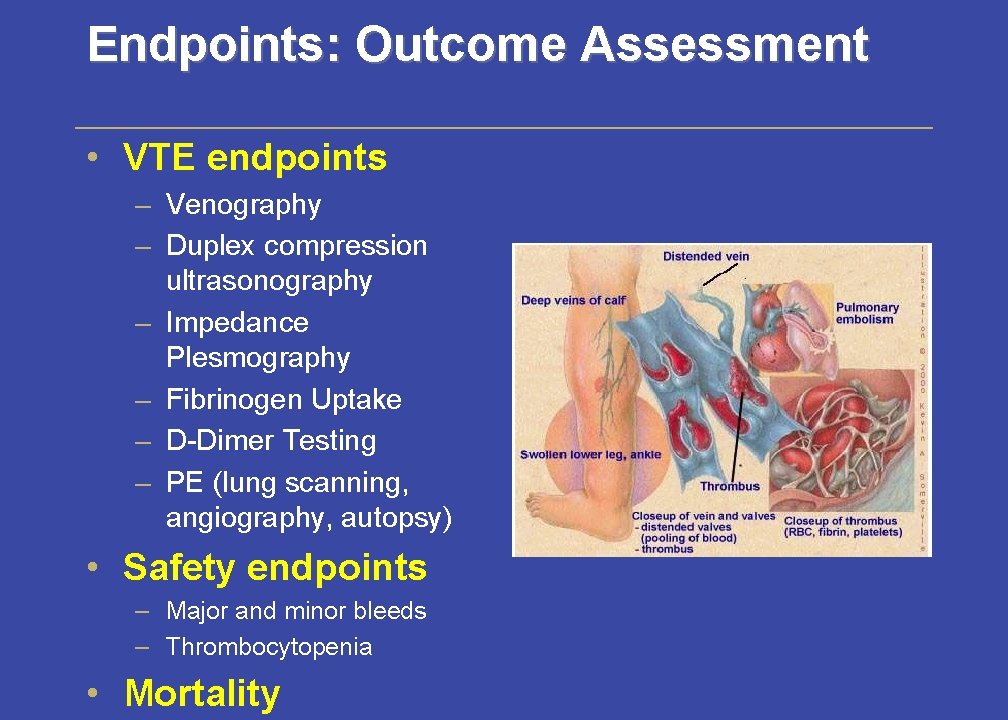
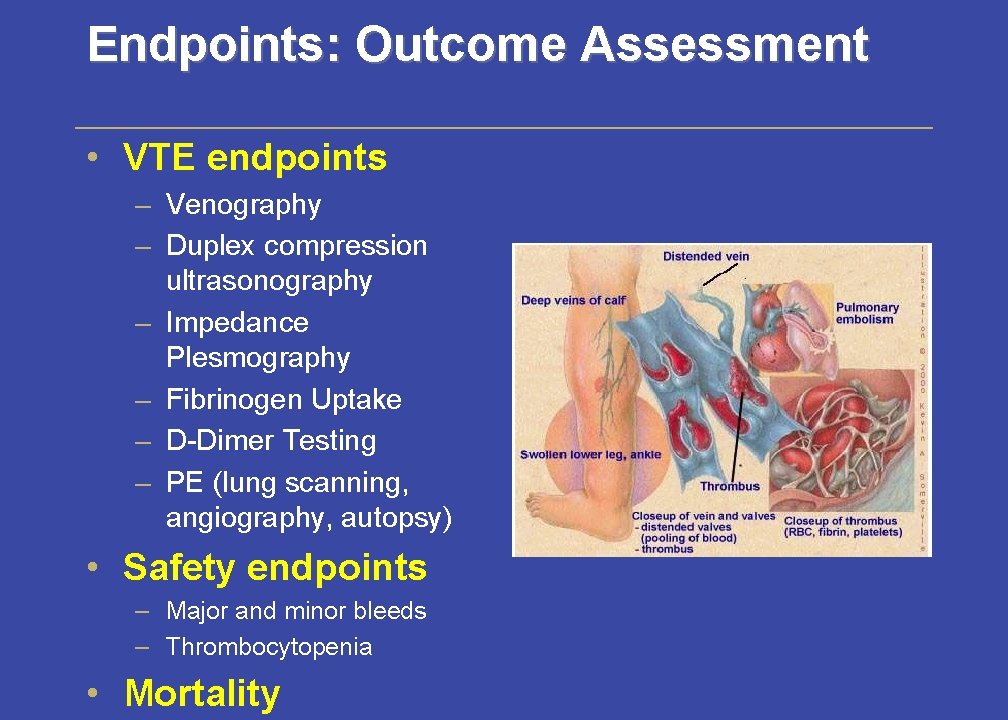
Endpoints: Outcome Assessment • VTE endpoints – Venography – Duplex compression ultrasonography – Impedance Plesmography – Fibrinogen Uptake – D-Dimer Testing – PE (lung scanning, angiography, autopsy) • Safety endpoints – Major and minor bleeds – Thrombocytopenia • Mortality
MANAGEMENT OPTIONS DVT • pharmacological agents • surgery (rarely indicated) PE • pharmacological agents • thrombolytics • surgery (endarterectomy, can be life saving, specialized centres) • Greenfield Filters (px)
THERAPEUTIC OPTIONS • • • Heparin LMWH Warfarin (oral) Danaparoid Hirudin/ Lepirudin Ancrod Thrombolytics (PE) Pentasacharide Injection (phase 3) Thrombin inhibitors (oral) (phase 3)
Pharmacologic Agents • • • MOA Place in Therapy Dosing Monitoring Adverse Effects/ Limitations Reversal Agents
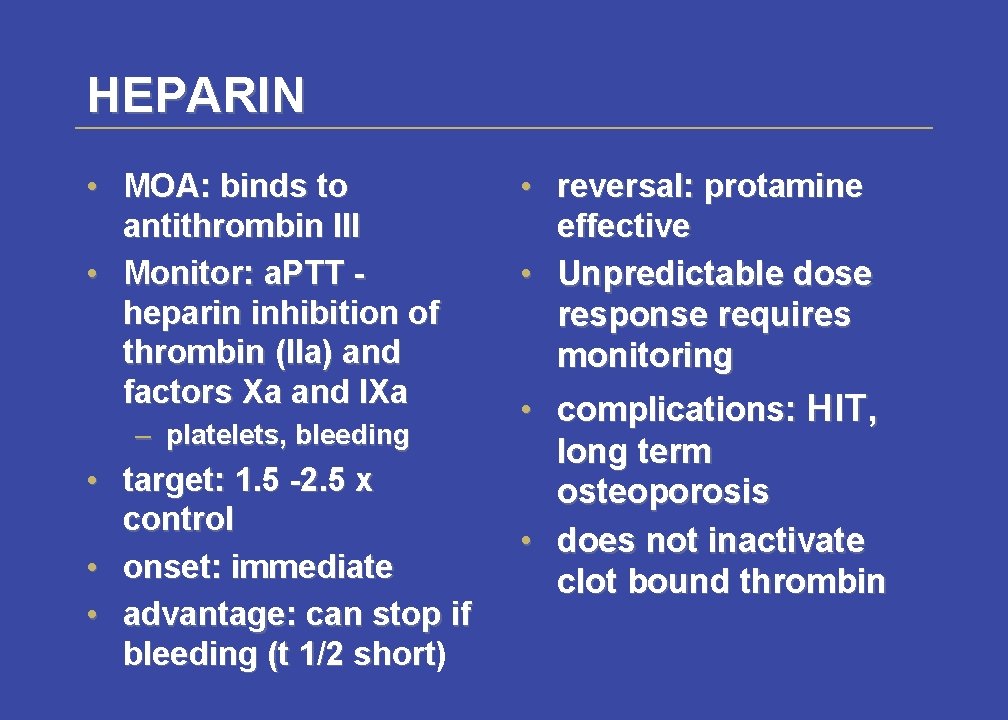
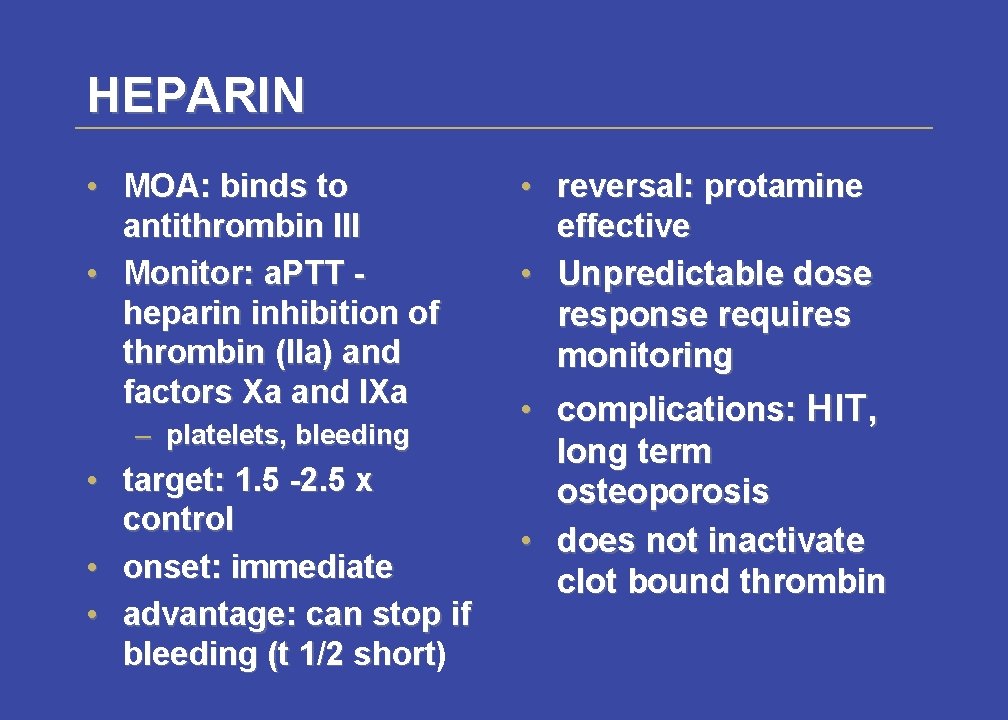
HEPARIN • MOA: binds to antithrombin III • Monitor: a. PTT heparin inhibition of thrombin (IIa) and factors Xa and IXa – platelets, bleeding • target: 1. 5 -2. 5 x control • onset: immediate • advantage: can stop if bleeding (t 1/2 short) short • reversal: protamine effective • Unpredictable dose response requires monitoring • complications: HIT, long term osteoporosis • does not inactivate clot bound thrombin
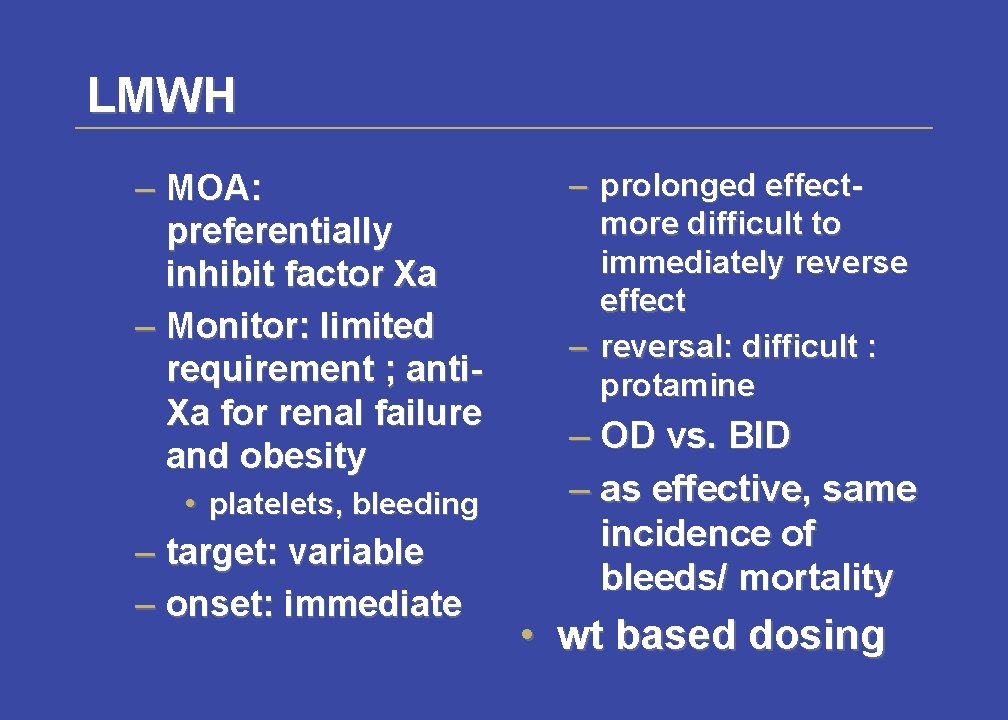
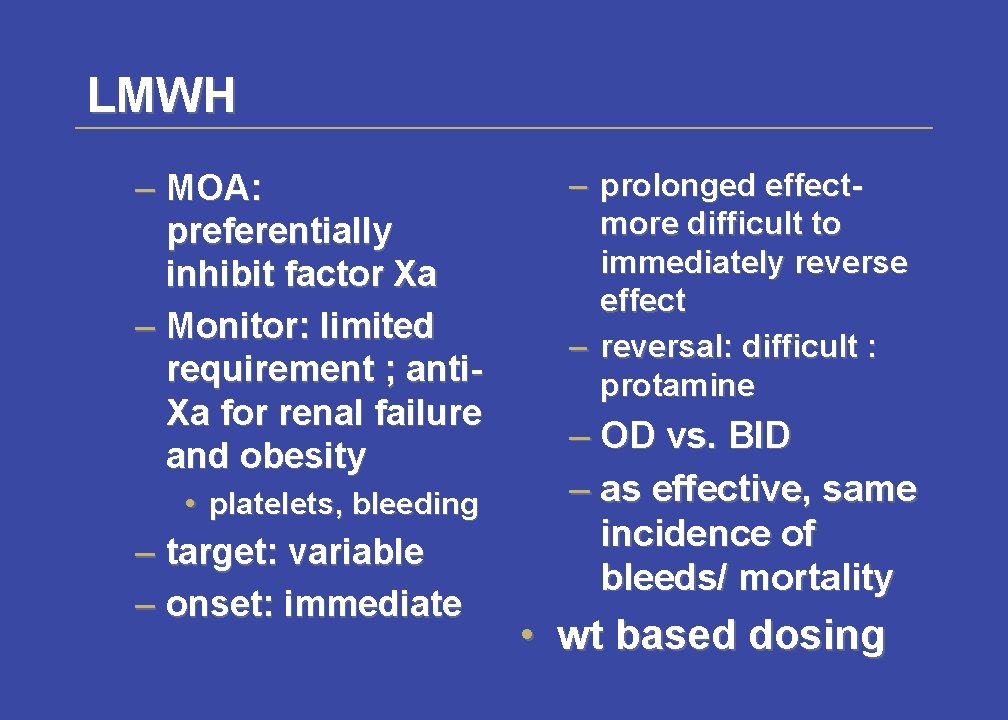
LMWH – MOA: preferentially inhibit factor Xa – Monitor: limited requirement ; anti. Xa for renal failure and obesity • platelets, bleeding – target: variable – onset: immediate – prolonged effectmore difficult to immediately reverse effect – reversal: difficult : protamine – OD vs. BID – as effective, same incidence of bleeds/ mortality • wt based dosing
UFH and LMWH • Continue therapy for at least 5 days (Grade 1 A) • longer duration of UFH or LMWH if massive PE • Should overlap with warfarin for at least 4 -5 days. – D/C after 2 consecutive days of therapeutic INR
Favourable properties of a LMWH – increased plasma half life- once daily/ bid dosing – reduced non-specific binding to plasma proteins (predictable anticoagulant response, predictable bioavialability) – reduced binding to platelets : (less HIT, potential for less bleeding) – less need for monitoring/ SC outpatient option – less daily injections – reduced binding to osteoblasts (less bone loss)
Favourable properties of a LMWH – less expensive – short acting- desirable in patients at high risk of bleeding - can quickly reverse anticoagulation
WARFARIN – MOA: inhibits vit K dep coagn factors (II, VII, IX, X) – Monitor: INR , bleeding – target: 2 -3 unless MVR – onset: delayed clotting factor half lives (factor II 72 hrs) – reversal: Vitamin K • Bleeding risk correlated to INR – inc with INR > 4 – major bleeds < 3% INR 2 -3 • Drug Interactions
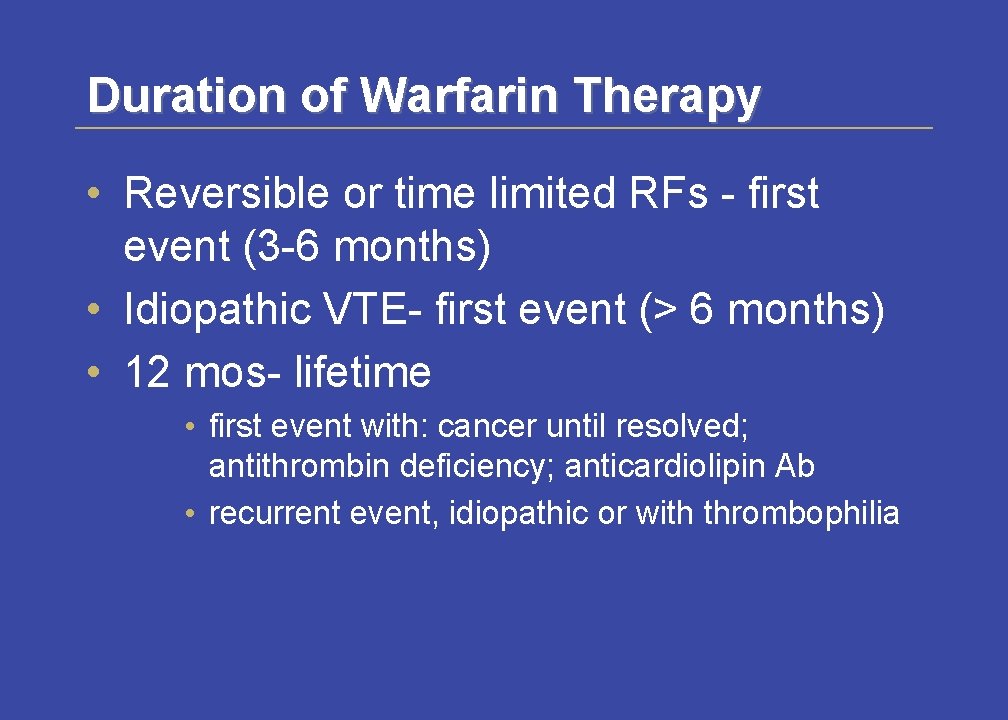
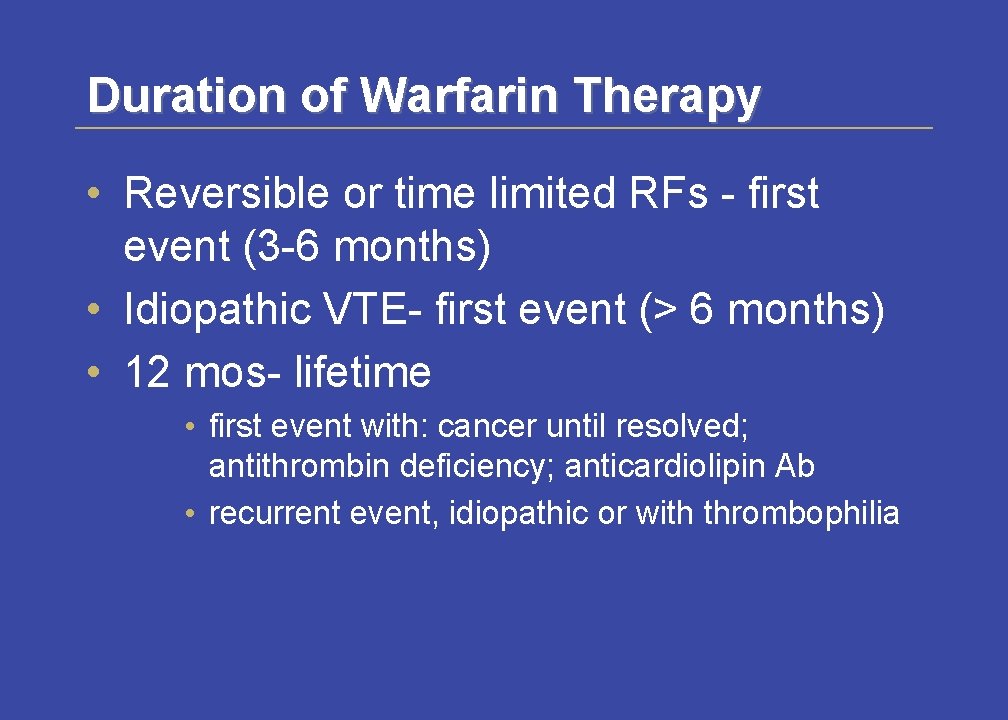
Duration of Warfarin Therapy • Reversible or time limited RFs - first event (3 -6 months) • Idiopathic VTE- first event (> 6 months) • 12 mos- lifetime • first event with: cancer until resolved; antithrombin deficiency; anticardiolipin Ab • recurrent event, idiopathic or with thrombophilia
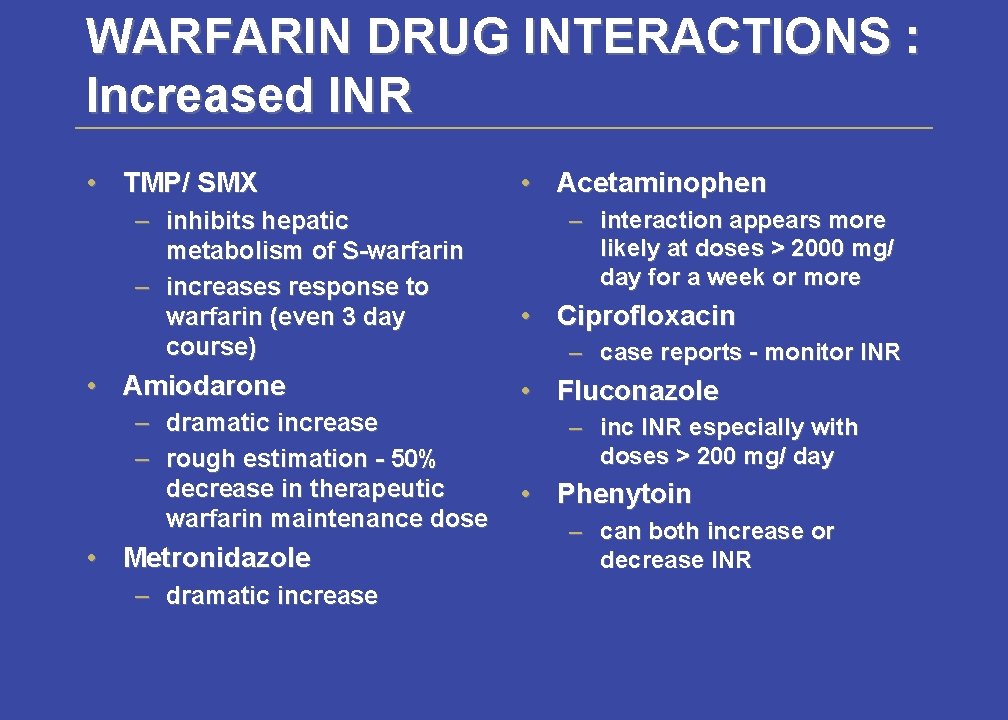
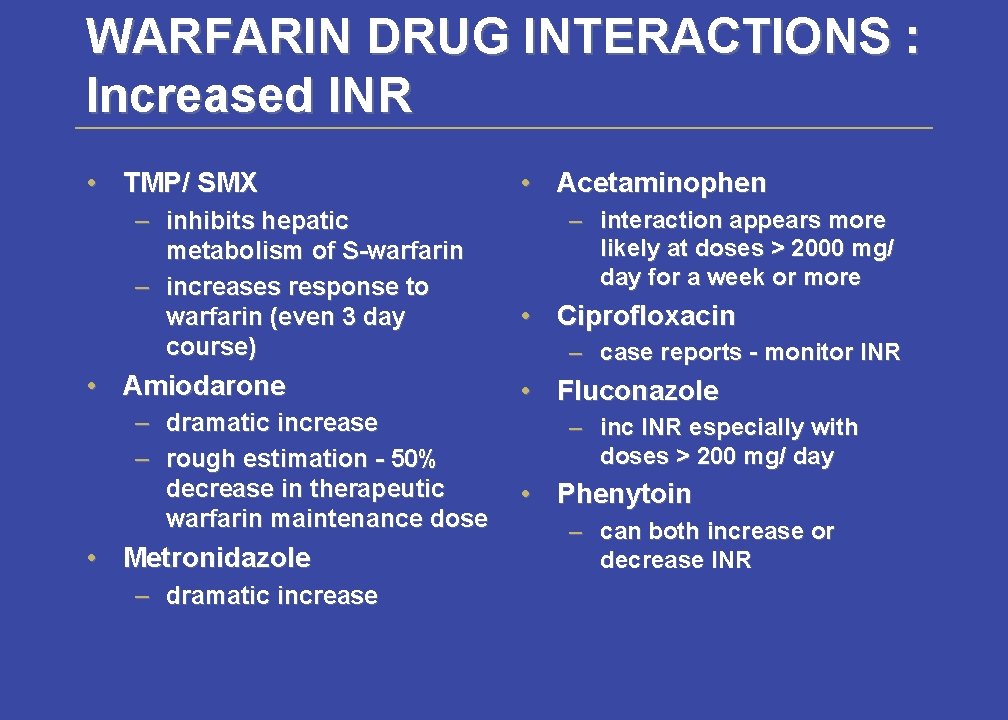
WARFARIN DRUG INTERACTIONS : Increased INR • TMP/ SMX – inhibits hepatic metabolism of S-warfarin – increases response to warfarin (even 3 day course) • Amiodarone – – dramatic increase rough estimation - 50% decrease in therapeutic warfarin maintenance dose • Metronidazole – dramatic increase • Acetaminophen – interaction appears more likely at doses > 2000 mg/ day for a week or more • Ciprofloxacin – case reports - monitor INR • Fluconazole – inc INR especially with doses > 200 mg/ day • Phenytoin – can both increase or decrease INR
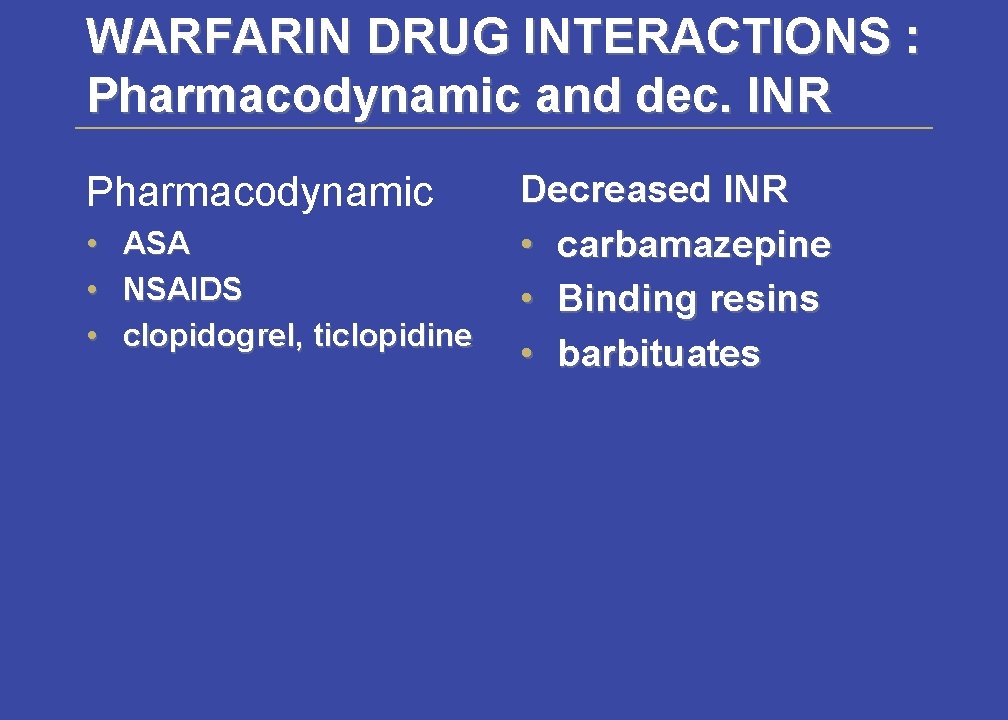
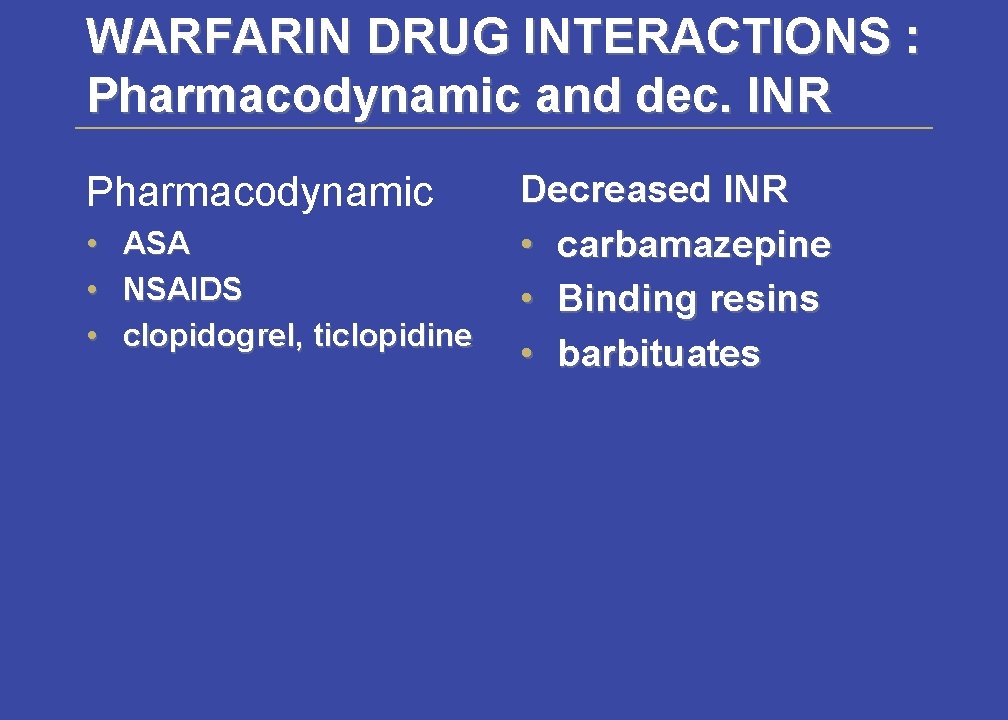
WARFARIN DRUG INTERACTIONS : Pharmacodynamic and dec. INR Pharmacodynamic • ASA • NSAIDS • clopidogrel, ticlopidine Decreased INR • carbamazepine • Binding resins • barbituates
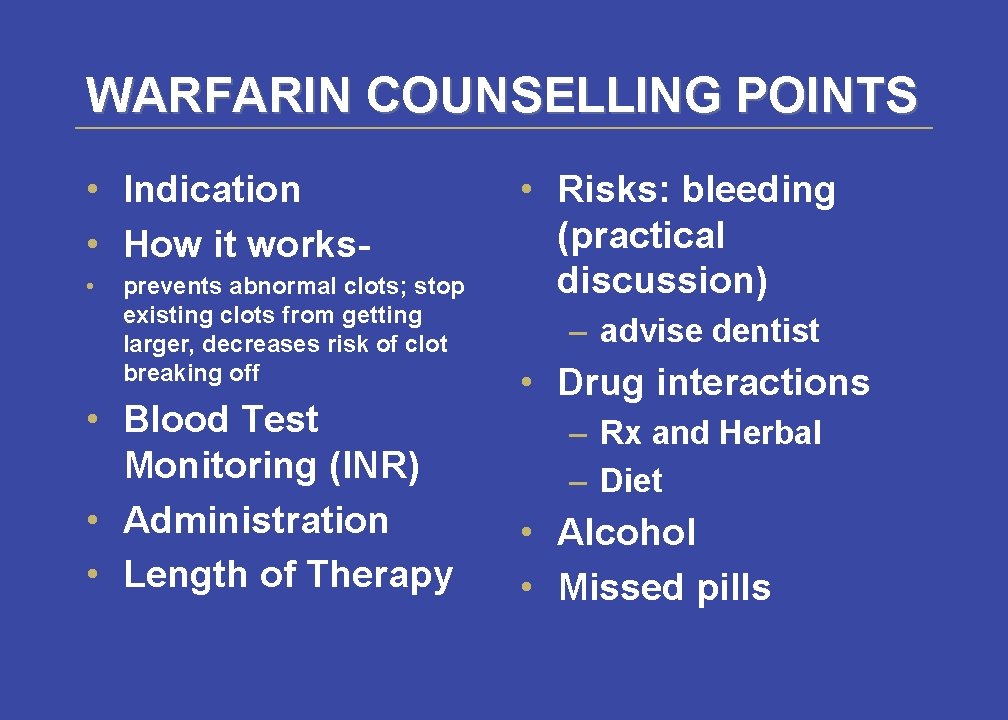
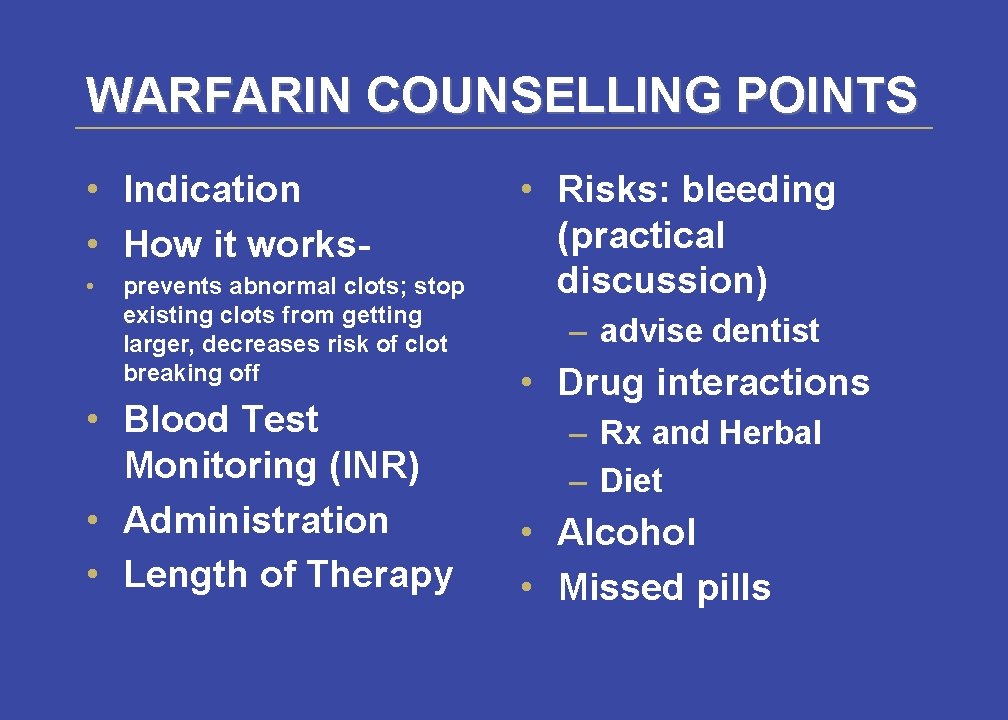
WARFARIN COUNSELLING POINTS • Indication • How it works • prevents abnormal clots; stop existing clots from getting larger, decreases risk of clot breaking off • Blood Test Monitoring (INR) • Administration • Length of Therapy • Risks: bleeding (practical discussion) – advise dentist • Drug interactions – Rx and Herbal – Diet • Alcohol • Missed pills
WARFARIN COUNSELLING POINTS • When to contact MD: blood in urine, stool, persistent nose bleed, increased swelling in extremity • When to go to ER: – SOB, Chest pain, coughing up blood, black tarry stools, severe HA of sudden onset, slurred speech
Thrombolytics for PE • Indicated only if massive PE, submassive with hemodynamic compromise (or failure of heparin tx) • can start 7 -14 days after PE dx • only when dx certain (V/Q scan, angiography) • only if no contraindications – absolute (active bleed; CVA or neurosurg in last 10 days) – relative (sx in last 10 days; severe HTN, pregnancy, GI bleed in last 3 months), arotic aneurysm, diabetic retinopathy, serious recent trauma • bleeding risks • expensive
Indications for Exoxaparin • Non-ST segment elevation ACS – angina at rest lasting at least 10 min – evidence of underlying IHD - specific ECG changes – inpatients • Exclude: – chest pain NYD, persistent ST segment elevation; emergency intervention within 24 hrs
 Dr olavo fernandes
Dr olavo fernandes Escola olavo pezzotti
Escola olavo pezzotti Exemplos de haicai
Exemplos de haicai Parnasianismo o que foi
Parnasianismo o que foi Um beijo olavo bilac
Um beijo olavo bilac A small child slides down the four frictionless slides
A small child slides down the four frictionless slides A crane lowers a girder into place at constant speed
A crane lowers a girder into place at constant speed Culturally responsive teaching and the brain slides
Culturally responsive teaching and the brain slides Dr ryan fernandes
Dr ryan fernandes Ana lucia fernandes pack
Ana lucia fernandes pack Fundamentos de filosofia gilberto cotrim
Fundamentos de filosofia gilberto cotrim Althea fernandes
Althea fernandes Walnei fernandes barbosa
Walnei fernandes barbosa Adriano yacubian fernandes
Adriano yacubian fernandes Dr ryan fernandes
Dr ryan fernandes Nissologia
Nissologia Dr ryan fernandes
Dr ryan fernandes Dr ryan fernandes
Dr ryan fernandes Ana paula morais fernandes
Ana paula morais fernandes Pnld 2021
Pnld 2021 Aires fernandes tabela preços
Aires fernandes tabela preços Dr regis fernandes
Dr regis fernandes Florestan fernandes mapa mental
Florestan fernandes mapa mental Dr frederico fernandes pneumologista
Dr frederico fernandes pneumologista Dr renato fernandes
Dr renato fernandes