DualConformant CCDA Recommendations and options to resolve inconsistencies
- Slides: 21
Dual-Conformant C-CDA Recommendations and options to resolve inconsistencies
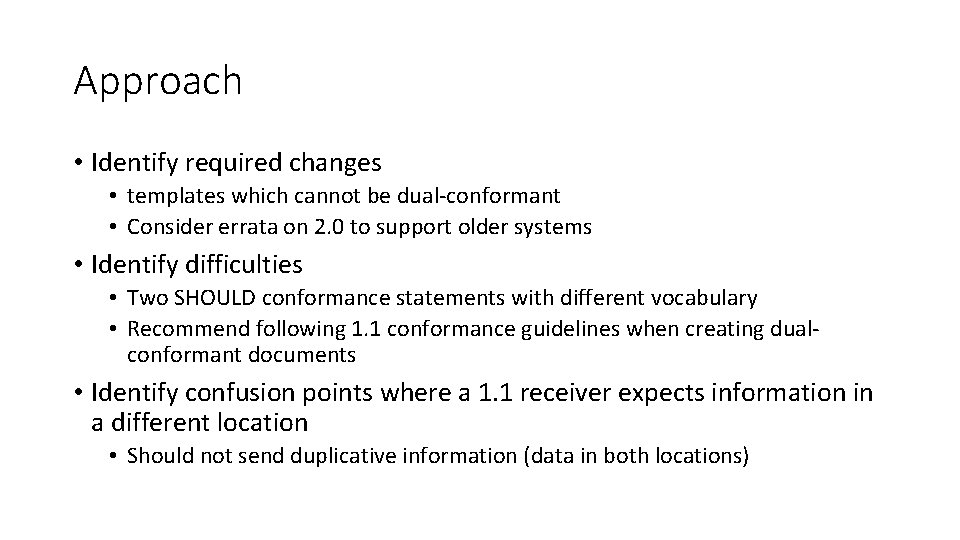
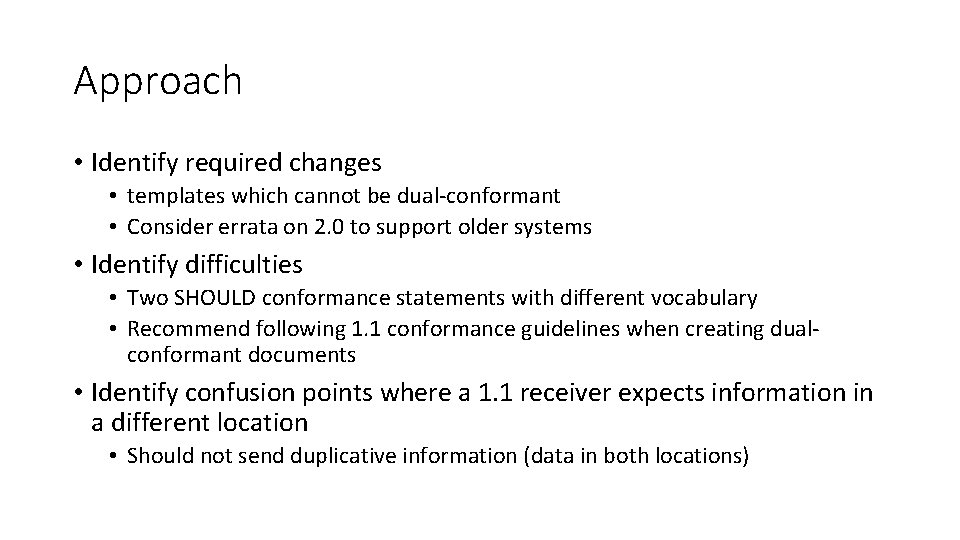
Approach • Identify required changes • templates which cannot be dual-conformant • Consider errata on 2. 0 to support older systems • Identify difficulties • Two SHOULD conformance statements with different vocabulary • Recommend following 1. 1 conformance guidelines when creating dualconformant documents • Identify confusion points where a 1. 1 receiver expects information in a different location • Should not send duplicative information (data in both locations)
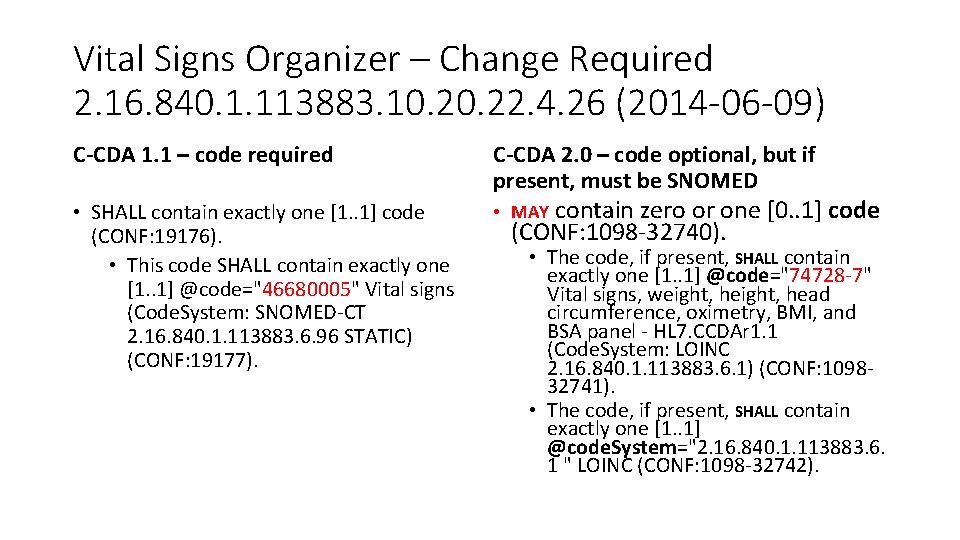
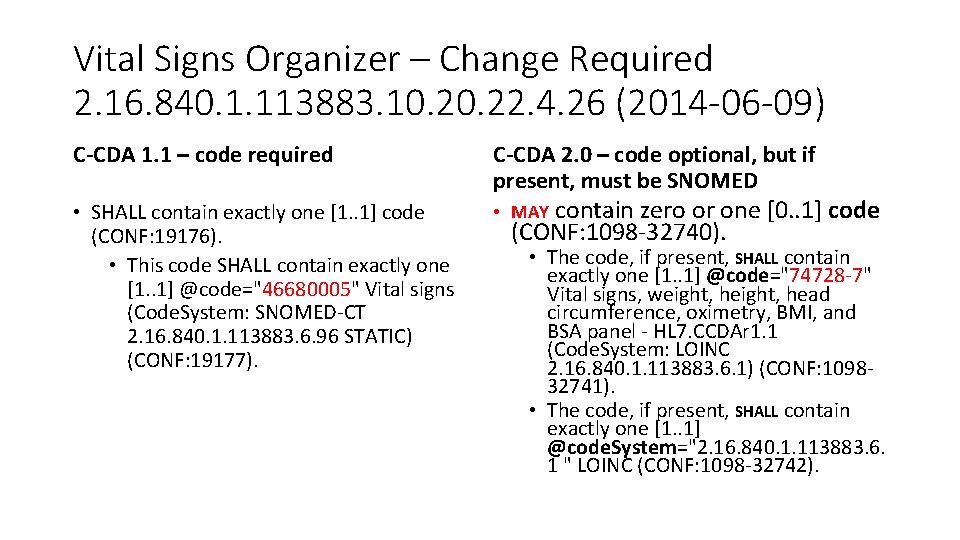
Vital Signs Organizer – Change Required 2. 16. 840. 1. 113883. 10. 22. 4. 26 (2014 -06 -09) C-CDA 1. 1 – code required C-CDA 2. 0 – code optional, but if present, must be SNOMED • SHALL contain exactly one [1. . 1] code (CONF: 19176). • This code SHALL contain exactly one [1. . 1] @code="46680005" Vital signs (Code. System: SNOMED-CT 2. 16. 840. 1. 113883. 6. 96 STATIC) (CONF: 19177). • MAY contain zero or one [0. . 1] code (CONF: 1098 -32740). • The code, if present, SHALL contain exactly one [1. . 1] @code="74728 -7" Vital signs, weight, head circumference, oximetry, BMI, and BSA panel - HL 7. CCDAr 1. 1 (Code. System: LOINC 2. 16. 840. 1. 113883. 6. 1) (CONF: 109832741). • The code, if present, SHALL contain exactly one [1. . 1] @code. System="2. 16. 840. 1. 113883. 6. 1 " LOINC (CONF: 1098 -32742).
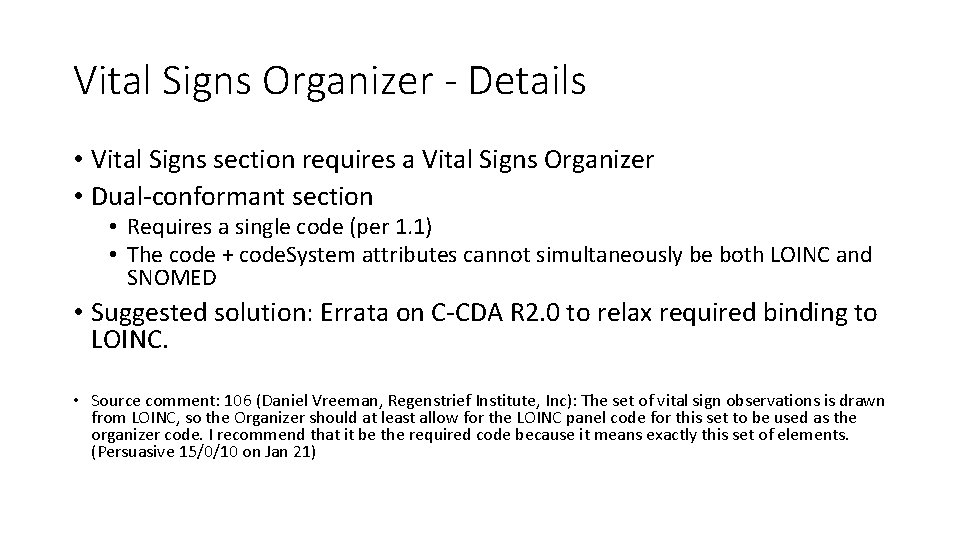
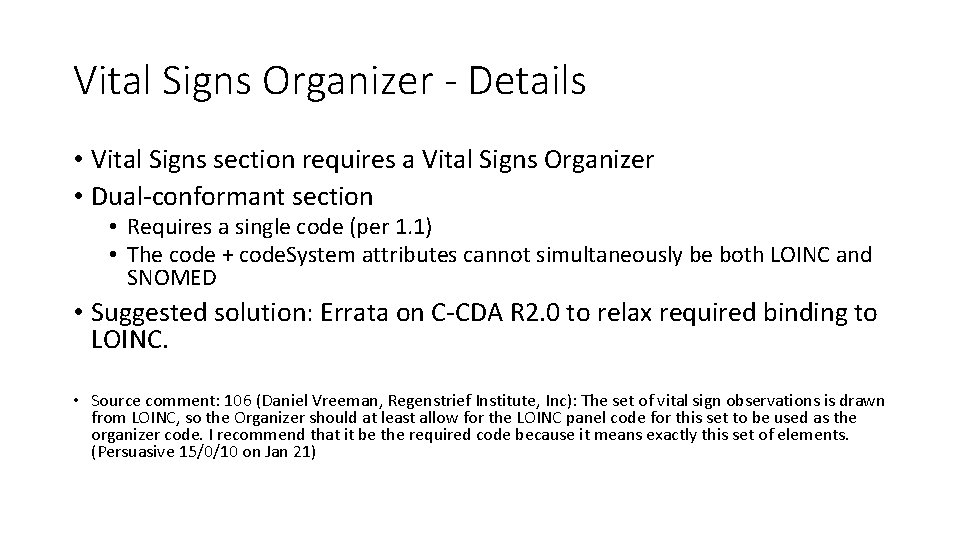
Vital Signs Organizer - Details • Vital Signs section requires a Vital Signs Organizer • Dual-conformant section • Requires a single code (per 1. 1) • The code + code. System attributes cannot simultaneously be both LOINC and SNOMED • Suggested solution: Errata on C-CDA R 2. 0 to relax required binding to LOINC. • Source comment: 106 (Daniel Vreeman, Regenstrief Institute, Inc): The set of vital sign observations is drawn from LOINC, so the Organizer should at least allow for the LOINC panel code for this set to be used as the organizer code. I recommend that it be the required code because it means exactly this set of elements. (Persuasive 15/0/10 on Jan 21)
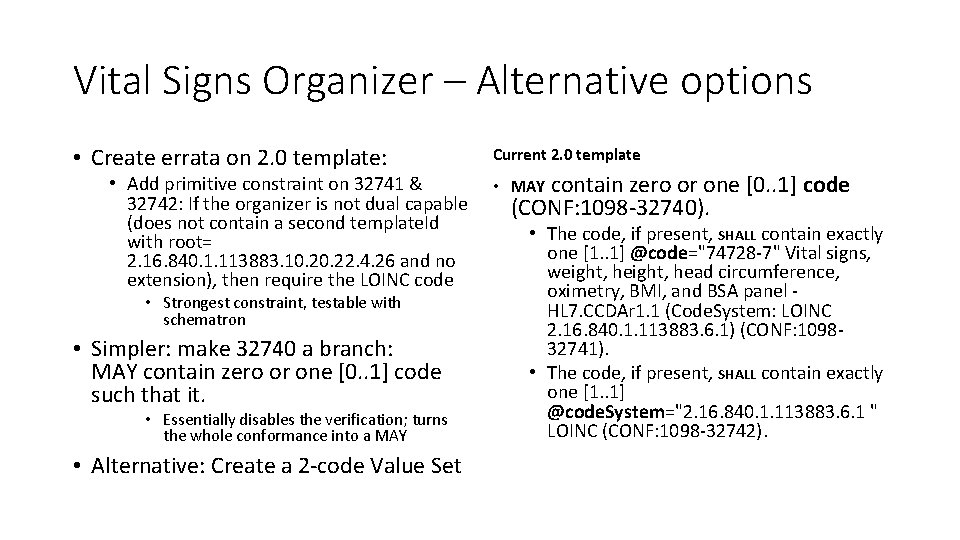
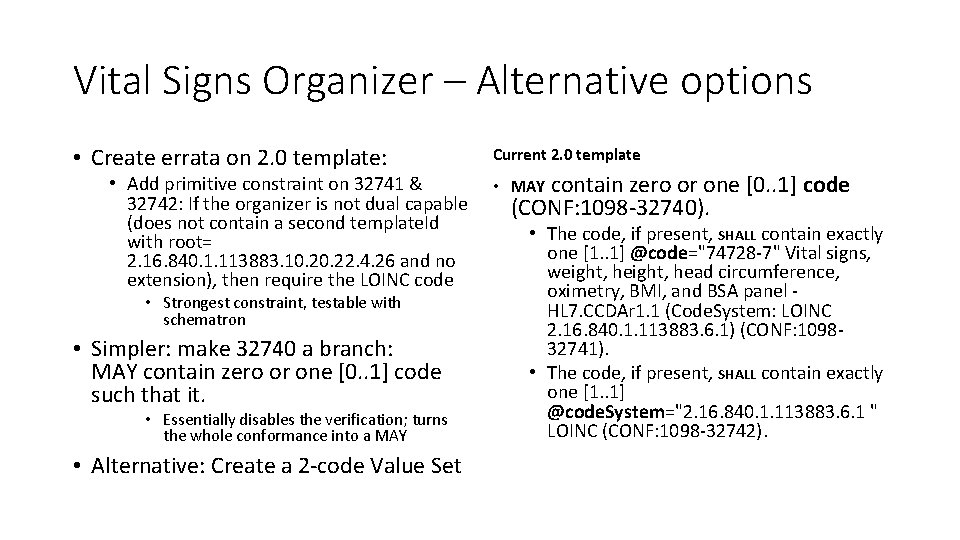
Vital Signs Organizer – Alternative options • Create errata on 2. 0 template: • Add primitive constraint on 32741 & 32742: If the organizer is not dual capable (does not contain a second template. Id with root= 2. 16. 840. 1. 113883. 10. 22. 4. 26 and no extension), then require the LOINC code • Strongest constraint, testable with schematron • Simpler: make 32740 a branch: MAY contain zero or one [0. . 1] code such that it. • Essentially disables the verification; turns the whole conformance into a MAY • Alternative: Create a 2 -code Value Set Current 2. 0 template contain zero or one [0. . 1] code (CONF: 1098 -32740). • MAY • The code, if present, SHALL contain exactly one [1. . 1] @code="74728 -7" Vital signs, weight, head circumference, oximetry, BMI, and BSA panel HL 7. CCDAr 1. 1 (Code. System: LOINC 2. 16. 840. 1. 113883. 6. 1) (CONF: 109832741). • The code, if present, SHALL contain exactly one [1. . 1] @code. System="2. 16. 840. 1. 113883. 6. 1 " LOINC (CONF: 1098 -32742).
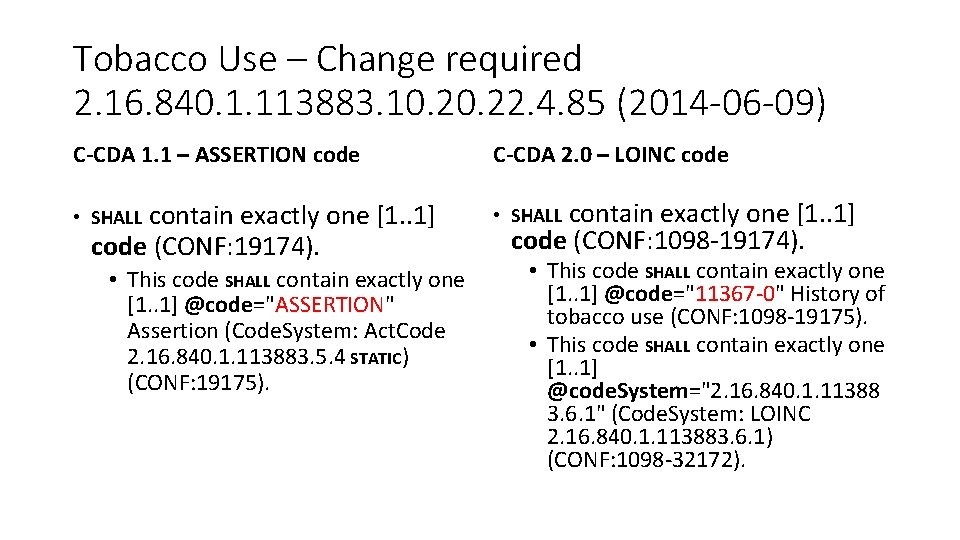
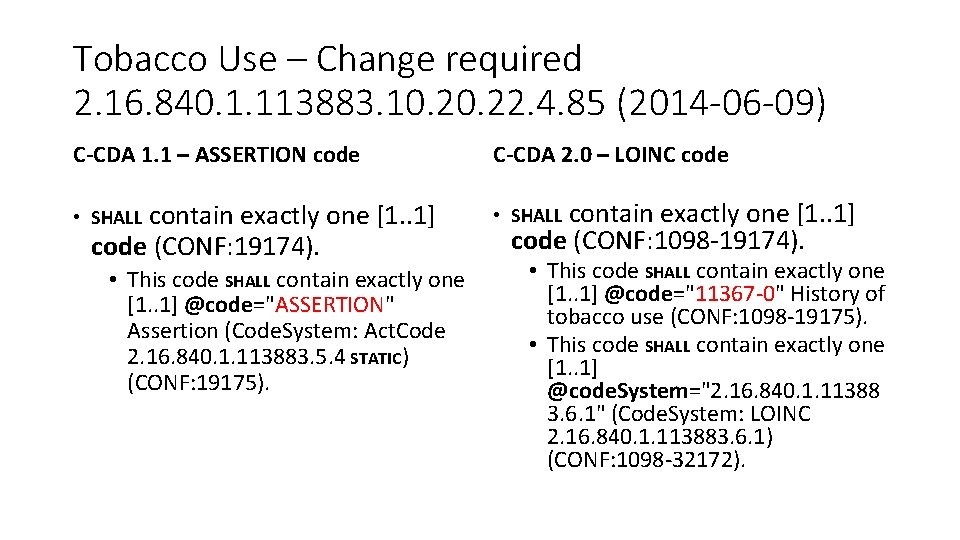
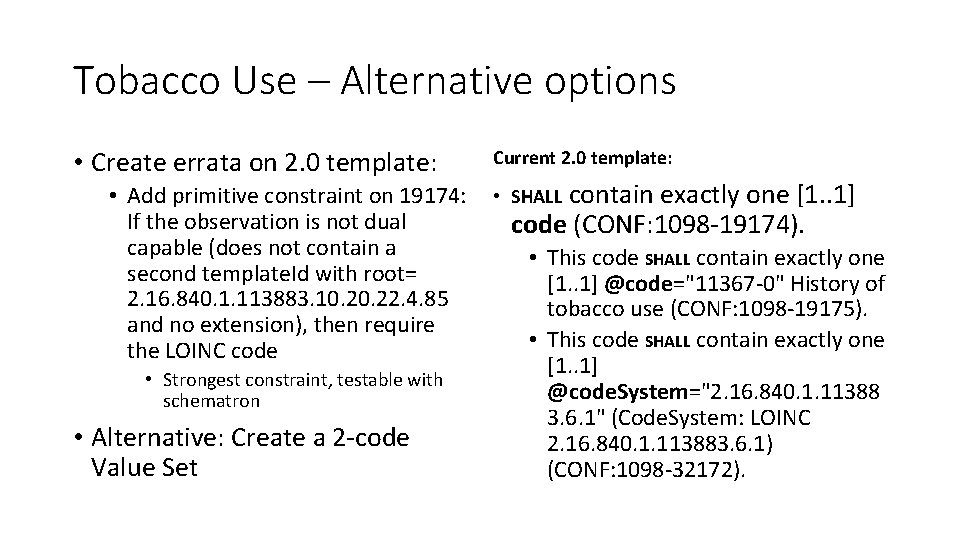
Tobacco Use – Change required 2. 16. 840. 1. 113883. 10. 22. 4. 85 (2014 -06 -09) C-CDA 1. 1 – ASSERTION code contain exactly one [1. . 1] code (CONF: 19174). • SHALL • This code SHALL contain exactly one [1. . 1] @code="ASSERTION" Assertion (Code. System: Act. Code 2. 16. 840. 1. 113883. 5. 4 STATIC) (CONF: 19175). C-CDA 2. 0 – LOINC code contain exactly one [1. . 1] code (CONF: 1098 -19174). • SHALL • This code SHALL contain exactly one [1. . 1] @code="11367 -0" History of tobacco use (CONF: 1098 -19175). • This code SHALL contain exactly one [1. . 1] @code. System="2. 16. 840. 1. 11388 3. 6. 1" (Code. System: LOINC 2. 16. 840. 1. 113883. 6. 1) (CONF: 1098 -32172).
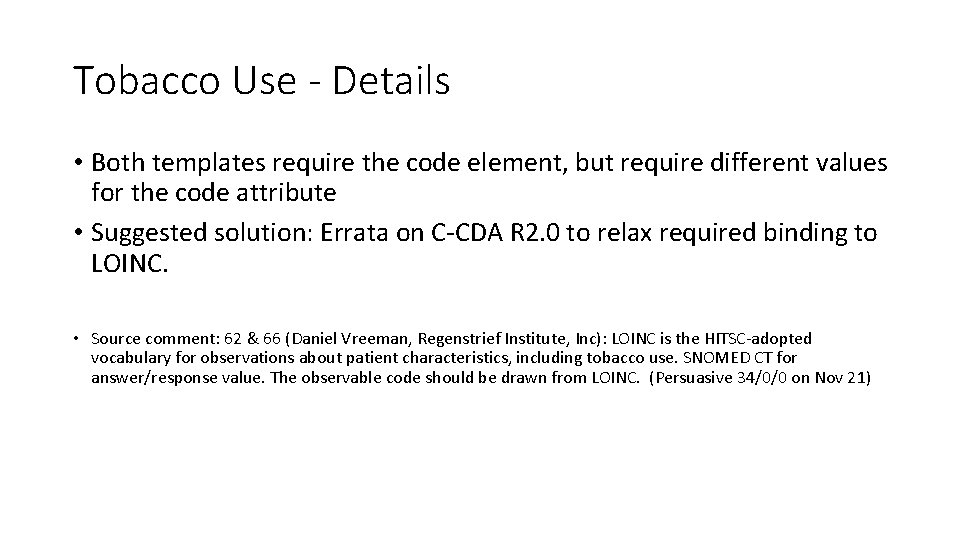
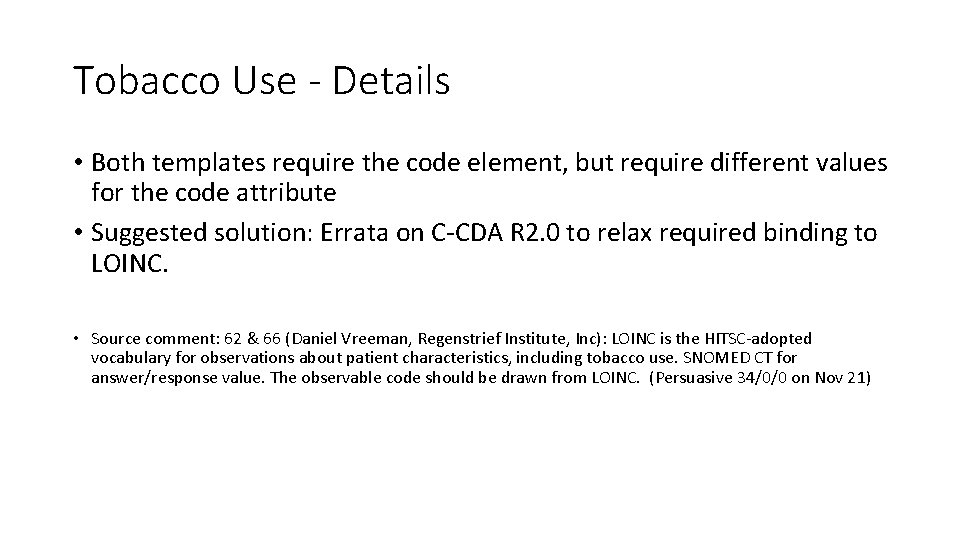
Tobacco Use - Details • Both templates require the code element, but require different values for the code attribute • Suggested solution: Errata on C-CDA R 2. 0 to relax required binding to LOINC. • Source comment: 62 & 66 (Daniel Vreeman, Regenstrief Institute, Inc): LOINC is the HITSC-adopted vocabulary for observations about patient characteristics, including tobacco use. SNOMED CT for answer/response value. The observable code should be drawn from LOINC. (Persuasive 34/0/0 on Nov 21)
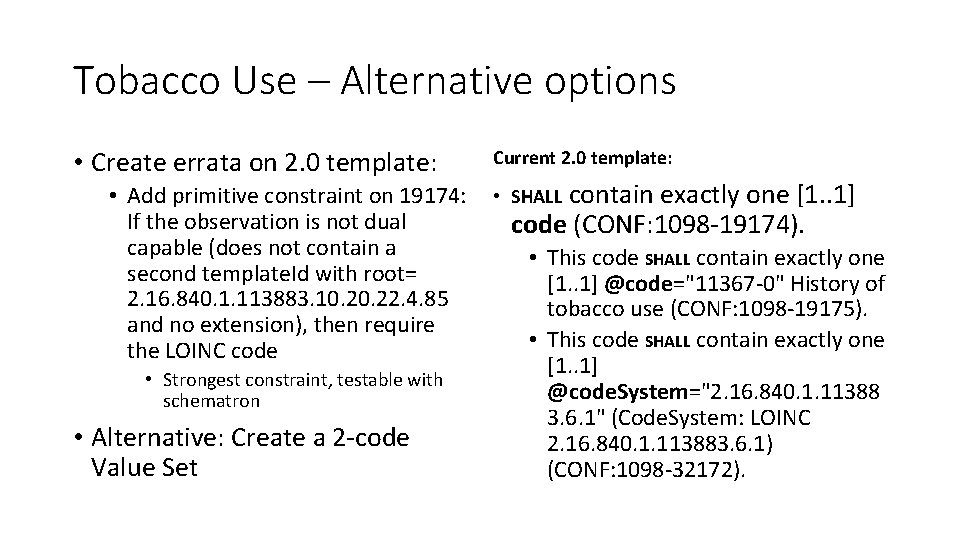
Tobacco Use – Alternative options • Create errata on 2. 0 template: • Add primitive constraint on 19174: If the observation is not dual capable (does not contain a second template. Id with root= 2. 16. 840. 1. 113883. 10. 22. 4. 85 and no extension), then require the LOINC code • Strongest constraint, testable with schematron • Alternative: Create a 2 -code Value Set Current 2. 0 template: contain exactly one [1. . 1] code (CONF: 1098 -19174). • SHALL • This code SHALL contain exactly one [1. . 1] @code="11367 -0" History of tobacco use (CONF: 1098 -19175). • This code SHALL contain exactly one [1. . 1] @code. System="2. 16. 840. 1. 11388 3. 6. 1" (Code. System: LOINC 2. 16. 840. 1. 113883. 6. 1) (CONF: 1098 -32172).
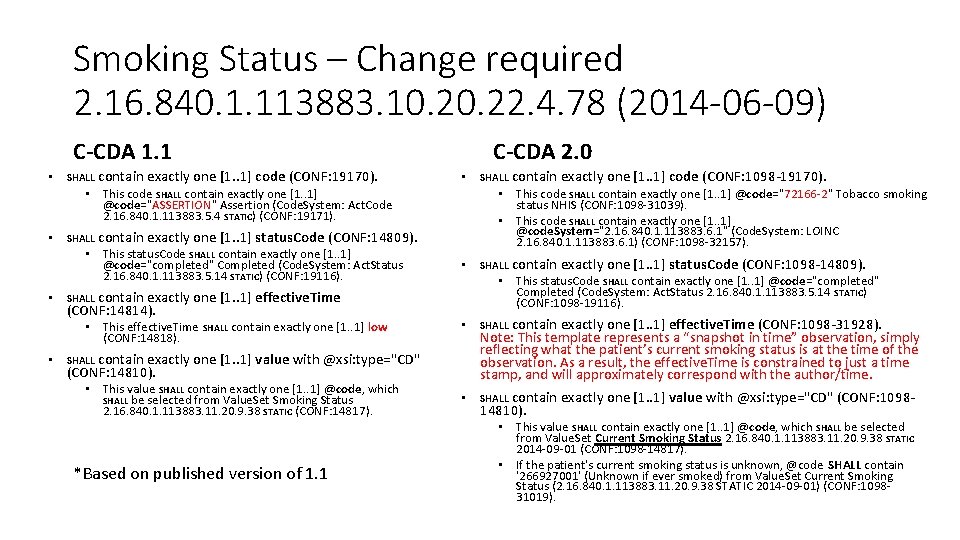
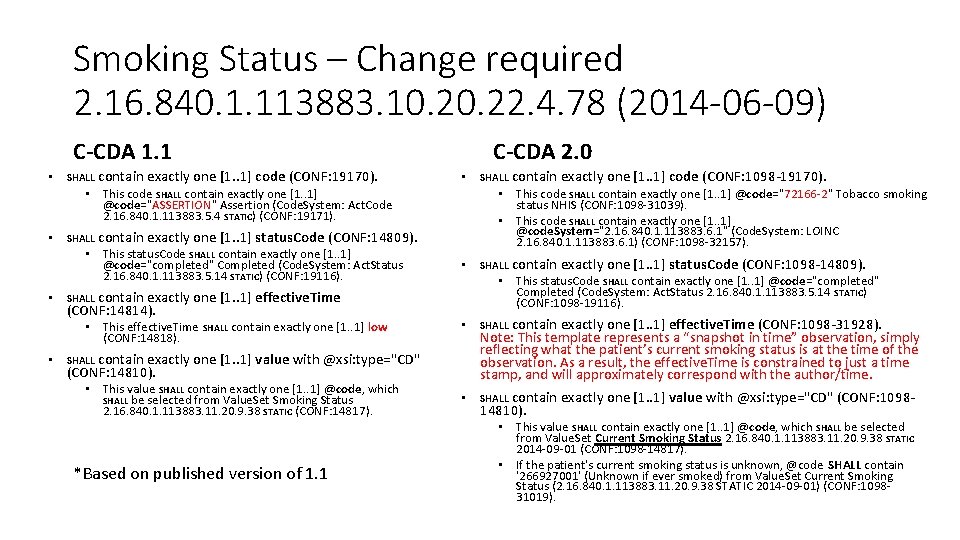
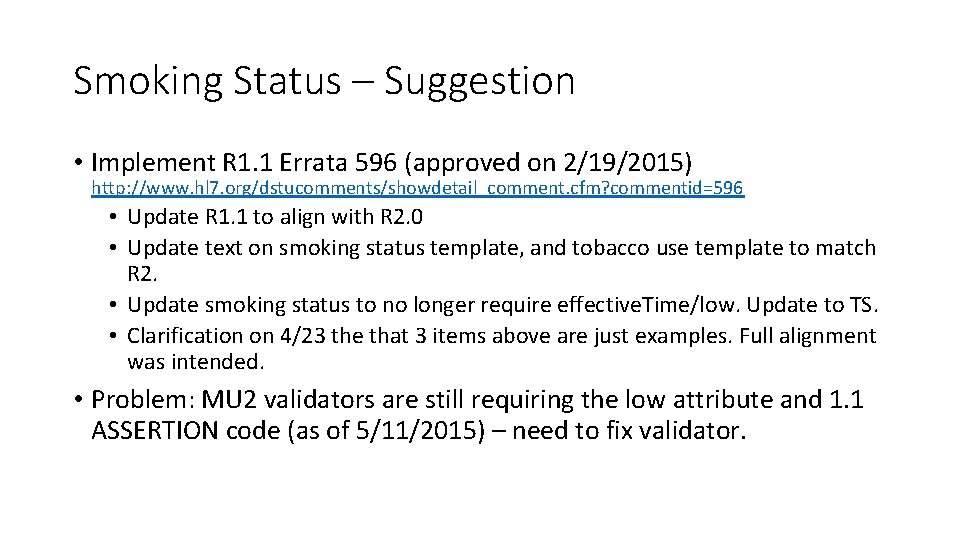
Smoking Status – Change required 2. 16. 840. 1. 113883. 10. 22. 4. 78 (2014 -06 -09) C-CDA 1. 1 • SHALL contain exactly one [1. . 1] code (CONF: 19170). C-CDA 2. 0 • • This code SHALL contain exactly one [1. . 1] @code="ASSERTION" Assertion (Code. System: Act. Code 2. 16. 840. 1. 113883. 5. 4 STATIC) (CONF: 19171). • SHALL • contain exactly one [1. . 1] effective. Time (CONF: 14814). • • SHALL contain exactly one [1. . 1] value with @xsi: type="CD" (CONF: 14810). *Based on published version of 1. 1 contain exactly one [1. . 1] status. Code (CONF: 1098 -14809). contain exactly one [1. . 1] effective. Time (CONF: 1098 -31928). Note: This template represents a “snapshot in time” observation, simply reflecting what the patient’s current smoking status is at the time of the observation. As a result, the effective. Time is constrained to just a time stamp, and will approximately correspond with the author/time. • SHALL • This value SHALL contain exactly one [1. . 1] @code, which SHALL be selected from Value. Set Smoking Status 2. 16. 840. 1. 113883. 11. 20. 9. 38 STATIC (CONF: 14817). SHALL • This status. Code SHALL contain exactly one [1. . 1] @code="completed" Completed (Code. System: Act. Status 2. 16. 840. 1. 113883. 5. 14 STATIC) (CONF: 1098 -19116). SHALL • This effective. Time SHALL contain exactly one [1. . 1] low (CONF: 14818). contain exactly one [1. . 1] code (CONF: 1098 -19170). • This code SHALL contain exactly one [1. . 1] @code="72166 -2" Tobacco smoking status NHIS (CONF: 1098 -31039). • This code SHALL contain exactly one [1. . 1] @code. System="2. 16. 840. 1. 113883. 6. 1" (Code. System: LOINC 2. 16. 840. 1. 113883. 6. 1) (CONF: 1098 -32157). contain exactly one [1. . 1] status. Code (CONF: 14809). • This status. Code SHALL contain exactly one [1. . 1] @code="completed" Completed (Code. System: Act. Status 2. 16. 840. 1. 113883. 5. 14 STATIC) (CONF: 19116). SHALL contain exactly one [1. . 1] value with @xsi: type="CD" (CONF: 109814810). • This value SHALL contain exactly one [1. . 1] @code, which SHALL be selected from Value. Set Current Smoking Status 2. 16. 840. 1. 113883. 11. 20. 9. 38 STATIC 2014 -09 -01 (CONF: 1098 -14817). • If the patient's current smoking status is unknown, @code SHALL contain '266927001' (Unknown if ever smoked) from Value. Set Current Smoking Status (2. 16. 840. 1. 113883. 11. 20. 9. 38 STATIC 2014 -09 -01) (CONF: 109831019).
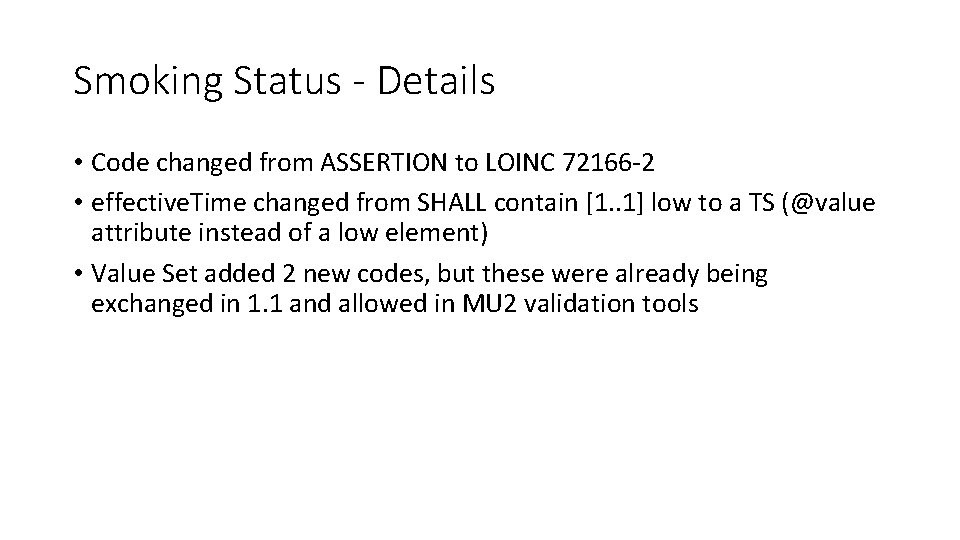
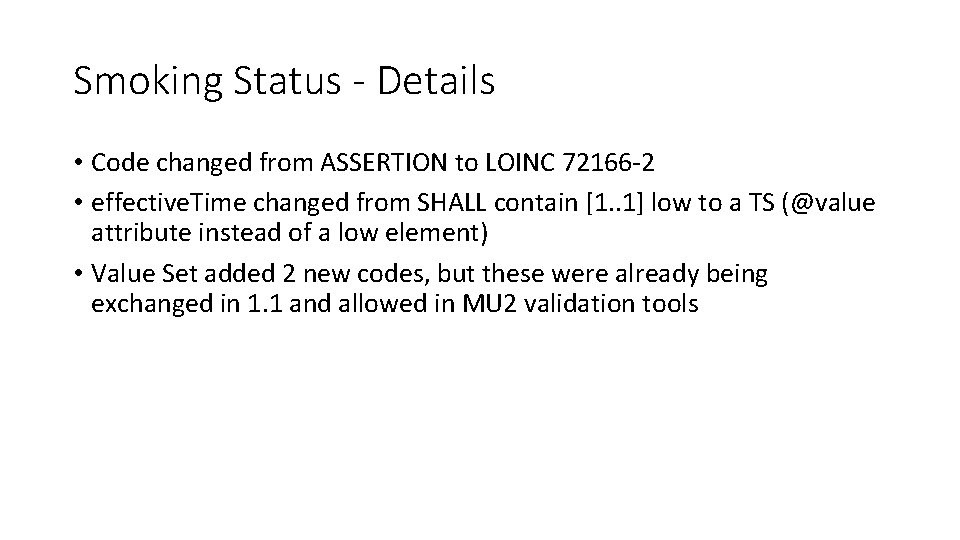
Smoking Status - Details • Code changed from ASSERTION to LOINC 72166 -2 • effective. Time changed from SHALL contain [1. . 1] low to a TS (@value attribute instead of a low element) • Value Set added 2 new codes, but these were already being exchanged in 1. 1 and allowed in MU 2 validation tools
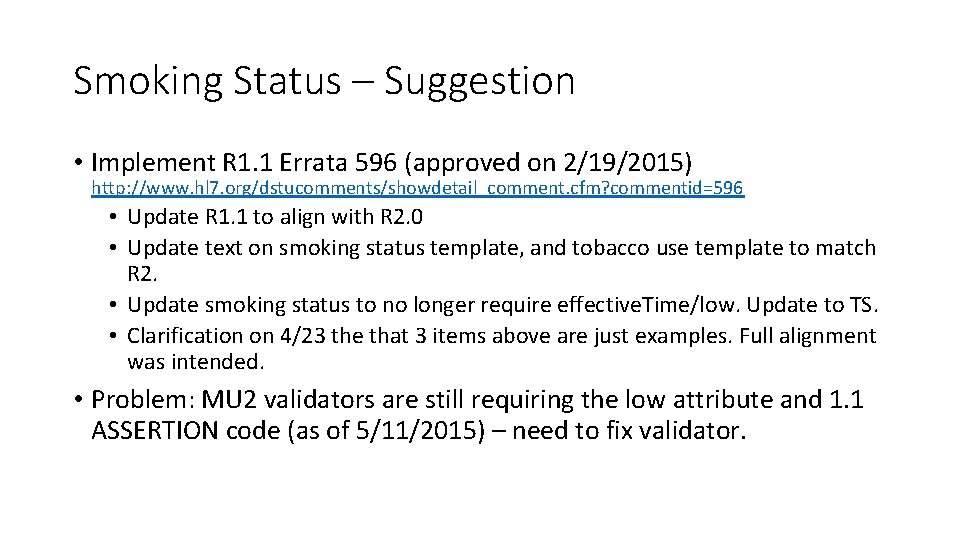
Smoking Status – Suggestion • Implement R 1. 1 Errata 596 (approved on 2/19/2015) http: //www. hl 7. org/dstucomments/showdetail_comment. cfm? commentid=596 • Update R 1. 1 to align with R 2. 0 • Update text on smoking status template, and tobacco use template to match R 2. • Update smoking status to no longer require effective. Time/low. Update to TS. • Clarification on 4/23 the that 3 items above are just examples. Full alignment was intended. • Problem: MU 2 validators are still requiring the low attribute and 1. 1 ASSERTION code (as of 5/11/2015) – need to fix validator.
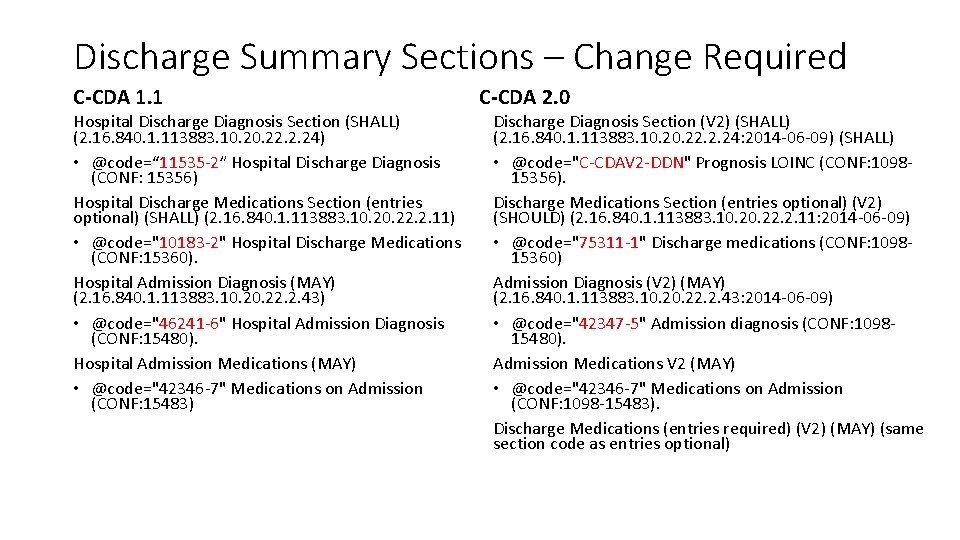
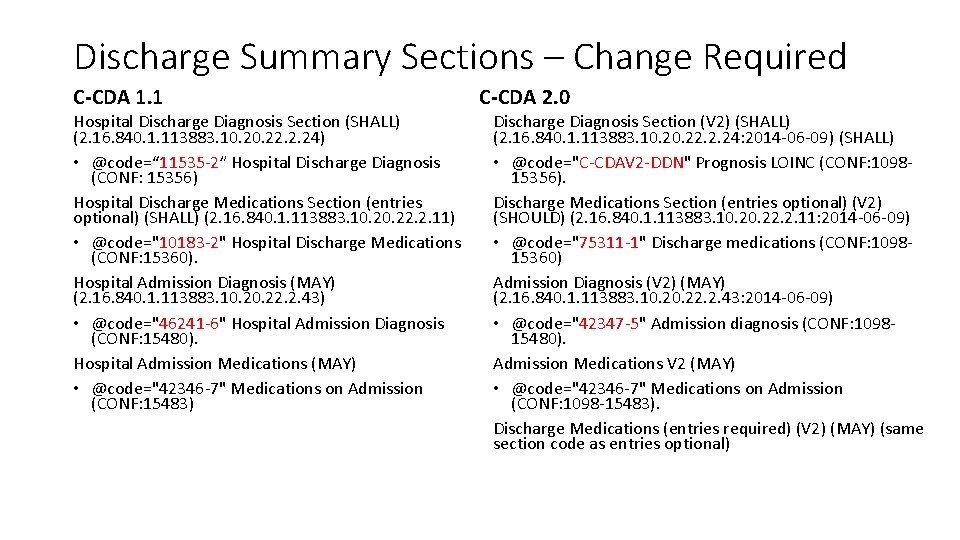
Discharge Summary Sections – Change Required C-CDA 1. 1 Hospital Discharge Diagnosis Section (SHALL) (2. 16. 840. 1. 113883. 10. 22. 2. 24) • @code=“ 11535 -2” Hospital Discharge Diagnosis (CONF: 15356) Hospital Discharge Medications Section (entries optional) (SHALL) (2. 16. 840. 1. 113883. 10. 22. 2. 11) • @code="10183 -2" Hospital Discharge Medications (CONF: 15360). Hospital Admission Diagnosis (MAY) (2. 16. 840. 1. 113883. 10. 22. 2. 43) • @code="46241 -6" Hospital Admission Diagnosis (CONF: 15480). Hospital Admission Medications (MAY) • @code="42346 -7" Medications on Admission (CONF: 15483) C-CDA 2. 0 Discharge Diagnosis Section (V 2) (SHALL) (2. 16. 840. 1. 113883. 10. 22. 2. 24: 2014 -06 -09) (SHALL) • @code="C-CDAV 2 -DDN" Prognosis LOINC (CONF: 109815356). Discharge Medications Section (entries optional) (V 2) (SHOULD) (2. 16. 840. 1. 113883. 10. 22. 2. 11: 2014 -06 -09) • @code="75311 -1" Discharge medications (CONF: 109815360) Admission Diagnosis (V 2) (MAY) (2. 16. 840. 1. 113883. 10. 22. 2. 43: 2014 -06 -09) • @code="42347 -5" Admission diagnosis (CONF: 109815480). Admission Medications V 2 (MAY) • @code="42346 -7" Medications on Admission (CONF: 1098 -15483). Discharge Medications (entries required) (V 2) (MAY) (same section code as entries optional)
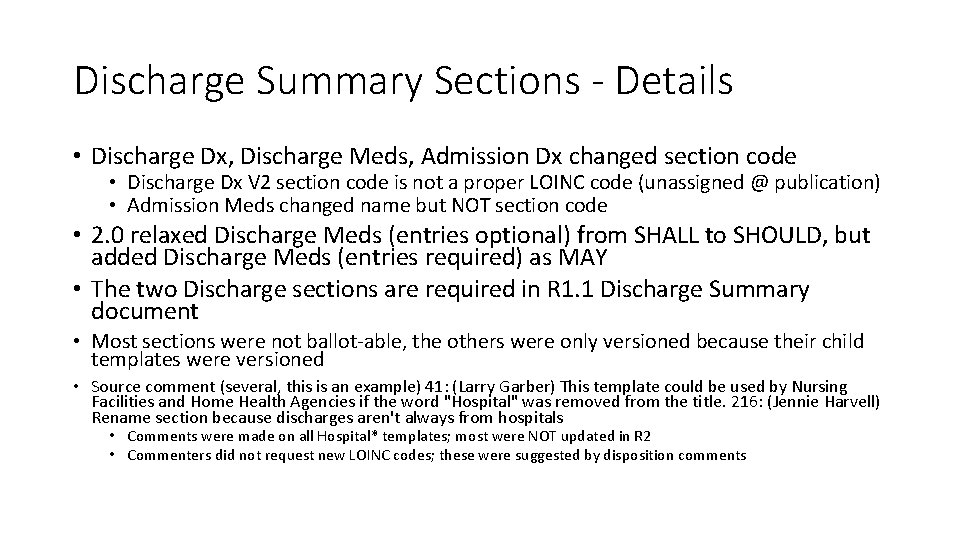
Discharge Summary Sections - Details • Discharge Dx, Discharge Meds, Admission Dx changed section code • Discharge Dx V 2 section code is not a proper LOINC code (unassigned @ publication) • Admission Meds changed name but NOT section code • 2. 0 relaxed Discharge Meds (entries optional) from SHALL to SHOULD, but added Discharge Meds (entries required) as MAY • The two Discharge sections are required in R 1. 1 Discharge Summary document • Most sections were not ballot-able, the others were only versioned because their child templates were versioned • Source comment (several, this is an example) 41: (Larry Garber) This template could be used by Nursing Facilities and Home Health Agencies if the word "Hospital" was removed from the title. 216: (Jennie Harvell) Rename section because discharges aren't always from hospitals • Comments were made on all Hospital* templates; most were NOT updated in R 2 • Commenters did not request new LOINC codes; these were suggested by disposition comments
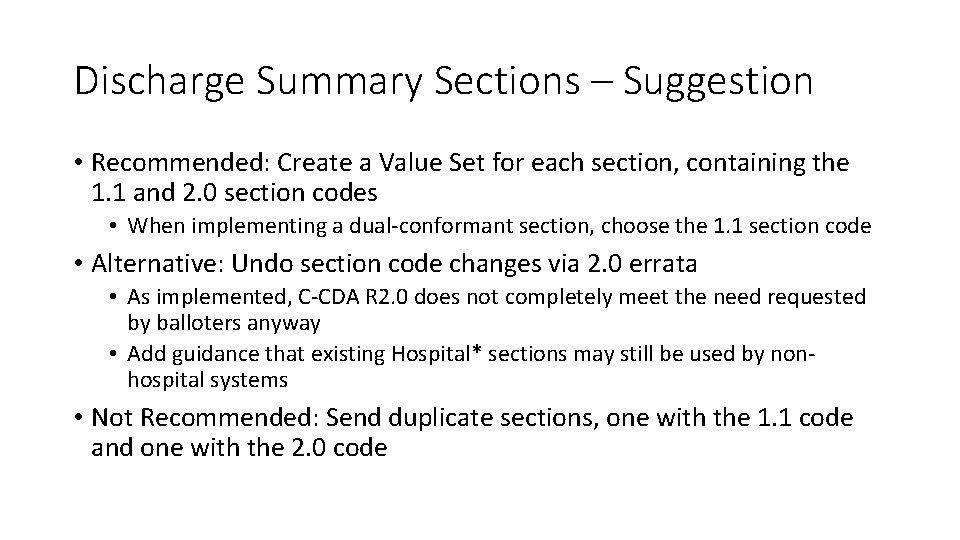
Discharge Summary Sections – Suggestion • Recommended: Create a Value Set for each section, containing the 1. 1 and 2. 0 section codes • When implementing a dual-conformant section, choose the 1. 1 section code • Alternative: Undo section code changes via 2. 0 errata • As implemented, C-CDA R 2. 0 does not completely meet the need requested by balloters anyway • Add guidance that existing Hospital* sections may still be used by nonhospital systems • Not Recommended: Send duplicate sections, one with the 1. 1 code and one with the 2. 0 code
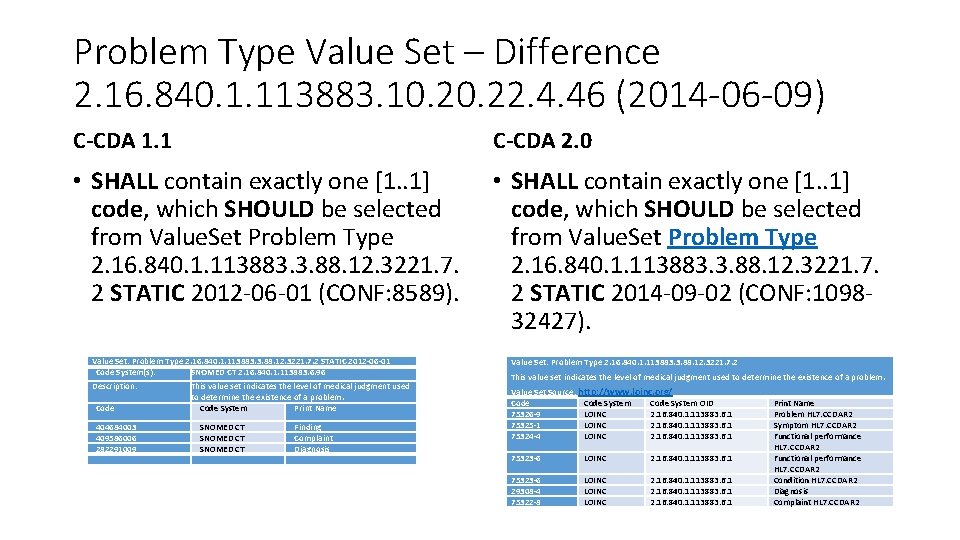
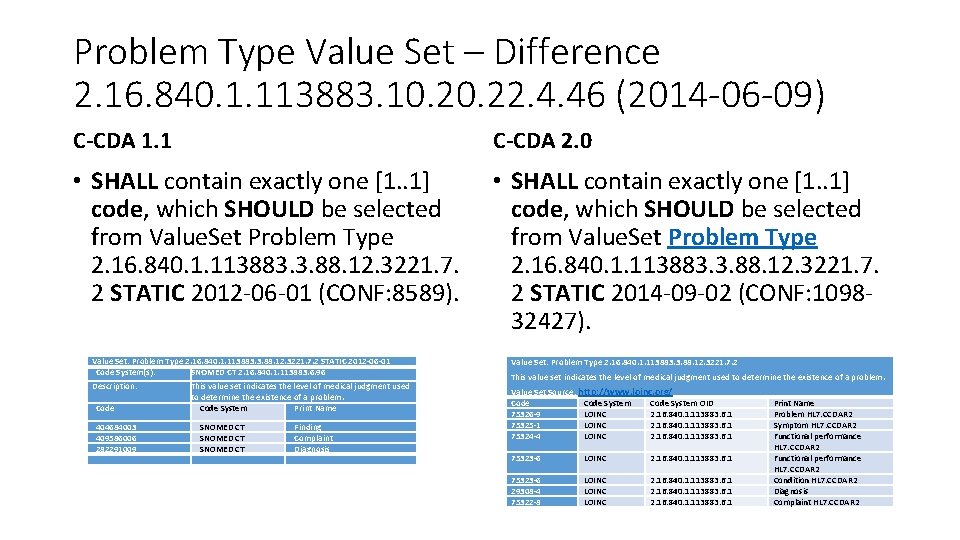
Problem Type Value Set – Difference 2. 16. 840. 1. 113883. 10. 22. 4. 46 (2014 -06 -09) C-CDA 1. 1 C-CDA 2. 0 • SHALL contain exactly one [1. . 1] code, which SHOULD be selected from Value. Set Problem Type 2. 16. 840. 1. 113883. 3. 88. 12. 3221. 7. 2 STATIC 2012 -06 -01 (CONF: 8589). • SHALL contain exactly one [1. . 1] code, which SHOULD be selected from Value. Set Problem Type 2. 16. 840. 1. 113883. 3. 88. 12. 3221. 7. 2 STATIC 2014 -09 -02 (CONF: 109832427). Value Set: Problem Type 2. 16. 840. 1. 113883. 3. 88. 12. 3221. 7. 2 STATIC 2012 -06 -01 Code System(s): SNOMED CT 2. 16. 840. 1. 113883. 6. 96 Value Set: Problem Type 2. 16. 840. 1. 113883. 3. 88. 12. 3221. 7. 2 Description: Value Set Source: http: //www. loinc. org/ Code System OID 75326 -9 LOINC 2. 16. 840. 1. 113883. 6. 1 75325 -1 LOINC 2. 16. 840. 1. 113883. 6. 1 75324 -4 LOINC 2. 16. 840. 1. 113883. 6. 1 Code 404684003 409586006 282291009 This value set indicates the level of medical judgment used to determine the existence of a problem. Code System Print Name SNOMED CT Finding Complaint Diagnosis This value set indicates the level of medical judgment used to determine the existence of a problem. 75323 -6 LOINC 2. 16. 840. 1. 113883. 6. 1 75323 -6 29308 -4 75322 -8 LOINC 2. 16. 840. 1. 113883. 6. 1 Print Name Problem HL 7. CCDAR 2 Symptom HL 7. CCDAR 2 Functional performance HL 7. CCDAR 2 Condition HL 7. CCDAR 2 Diagnosis Complaint HL 7. CCDAR 2
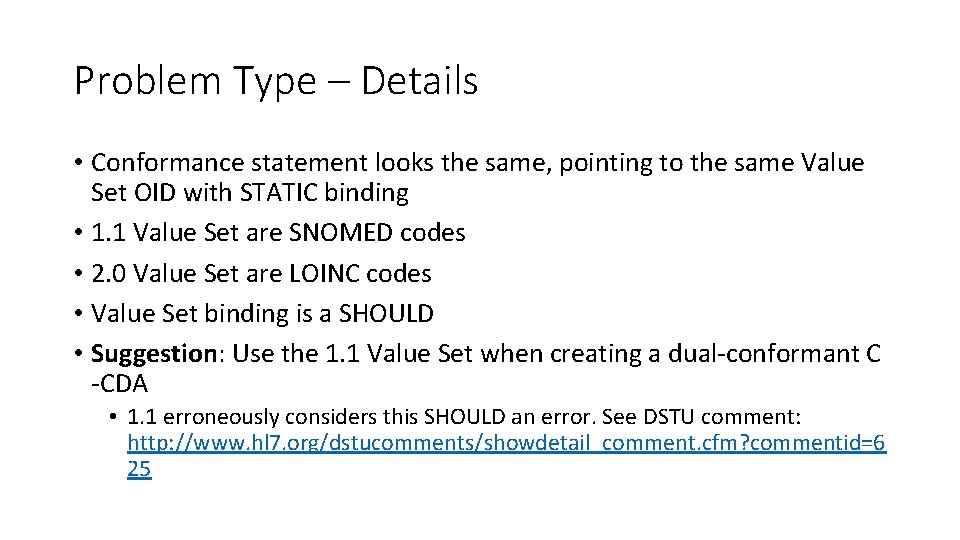
Problem Type – Details • Conformance statement looks the same, pointing to the same Value Set OID with STATIC binding • 1. 1 Value Set are SNOMED codes • 2. 0 Value Set are LOINC codes • Value Set binding is a SHOULD • Suggestion: Use the 1. 1 Value Set when creating a dual-conformant C -CDA • 1. 1 erroneously considers this SHOULD an error. See DSTU comment: http: //www. hl 7. org/dstucomments/showdetail_comment. cfm? commentid=6 25
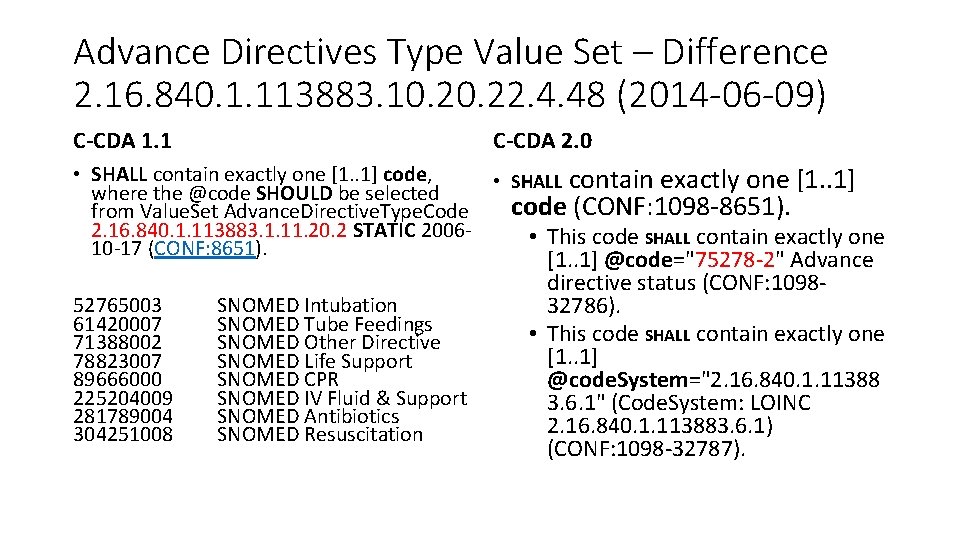
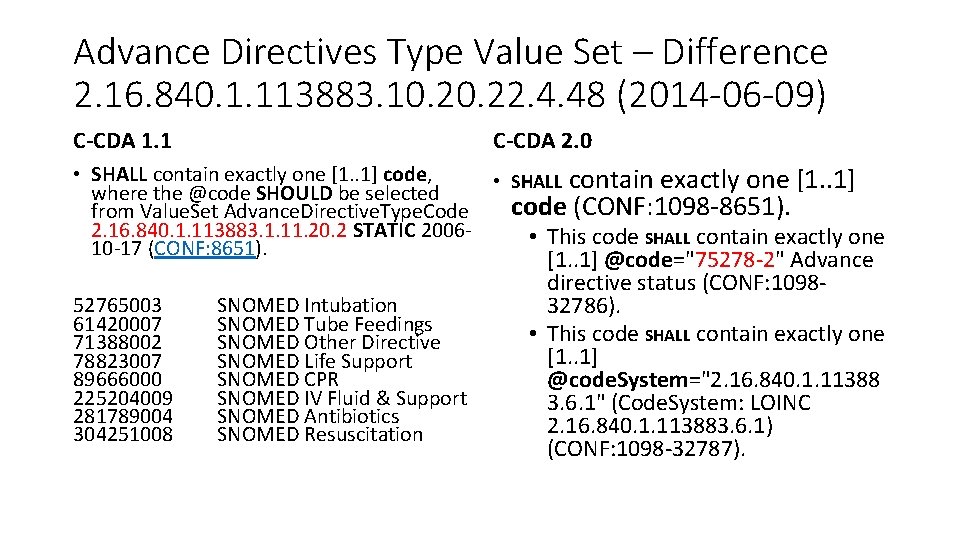
Advance Directives Type Value Set – Difference 2. 16. 840. 1. 113883. 10. 22. 4. 48 (2014 -06 -09) C-CDA 1. 1 C-CDA 2. 0 • SHALL contain exactly one [1. . 1] code, • SHALL contain exactly one [1. . 1] where the @code SHOULD be selected code (CONF: 1098 -8651). from Value. Set Advance. Directive. Type. Code 2. 16. 840. 1. 113883. 1. 11. 20. 2 STATIC 2006 • This code SHALL contain exactly one 10 -17 (CONF: 8651). 52765003 61420007 71388002 78823007 89666000 225204009 281789004 304251008 SNOMED Intubation SNOMED Tube Feedings SNOMED Other Directive SNOMED Life Support SNOMED CPR SNOMED IV Fluid & Support SNOMED Antibiotics SNOMED Resuscitation [1. . 1] @code="75278 -2" Advance directive status (CONF: 109832786). • This code SHALL contain exactly one [1. . 1] @code. System="2. 16. 840. 1. 11388 3. 6. 1" (Code. System: LOINC 2. 16. 840. 1. 113883. 6. 1) (CONF: 1098 -32787).
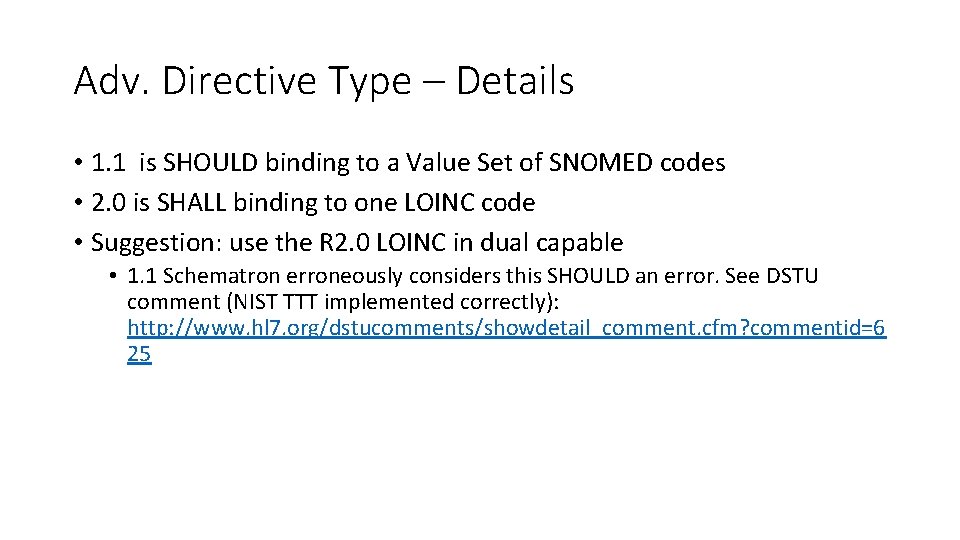
Adv. Directive Type – Details • 1. 1 is SHOULD binding to a Value Set of SNOMED codes • 2. 0 is SHALL binding to one LOINC code • Suggestion: use the R 2. 0 LOINC in dual capable • 1. 1 Schematron erroneously considers this SHOULD an error. See DSTU comment (NIST TTT implemented correctly): http: //www. hl 7. org/dstucomments/showdetail_comment. cfm? commentid=6 25
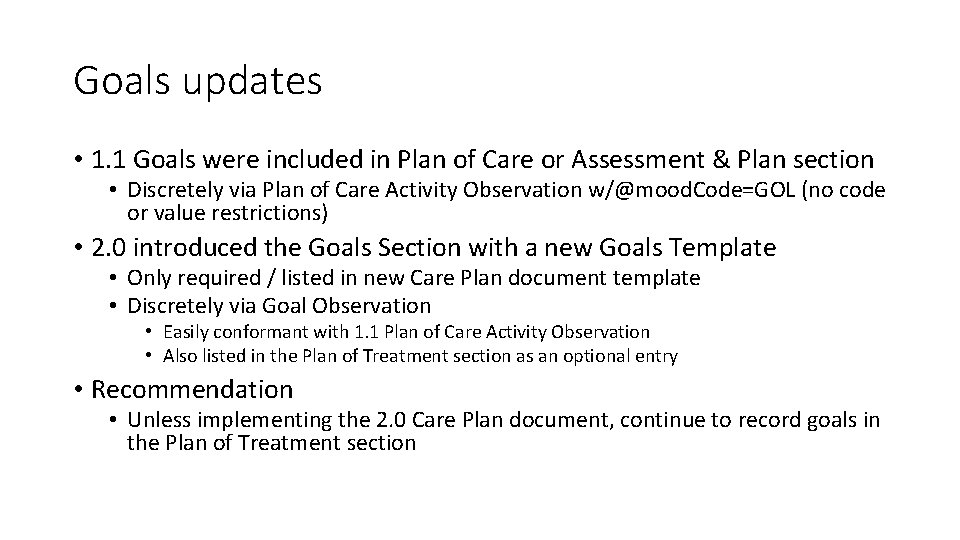
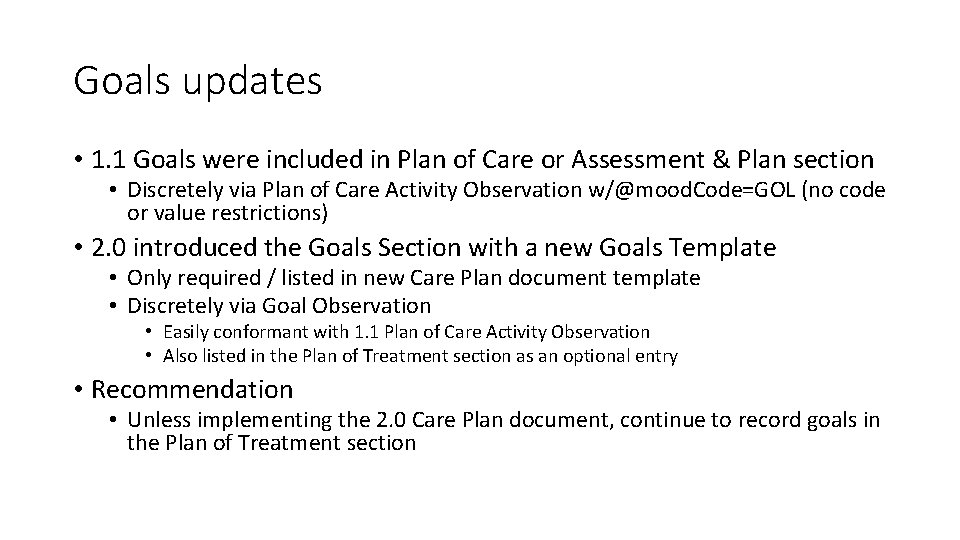
Goals updates • 1. 1 Goals were included in Plan of Care or Assessment & Plan section • Discretely via Plan of Care Activity Observation w/@mood. Code=GOL (no code or value restrictions) • 2. 0 introduced the Goals Section with a new Goals Template • Only required / listed in new Care Plan document template • Discretely via Goal Observation • Easily conformant with 1. 1 Plan of Care Activity Observation • Also listed in the Plan of Treatment section as an optional entry • Recommendation • Unless implementing the 2. 0 Care Plan document, continue to record goals in the Plan of Treatment section
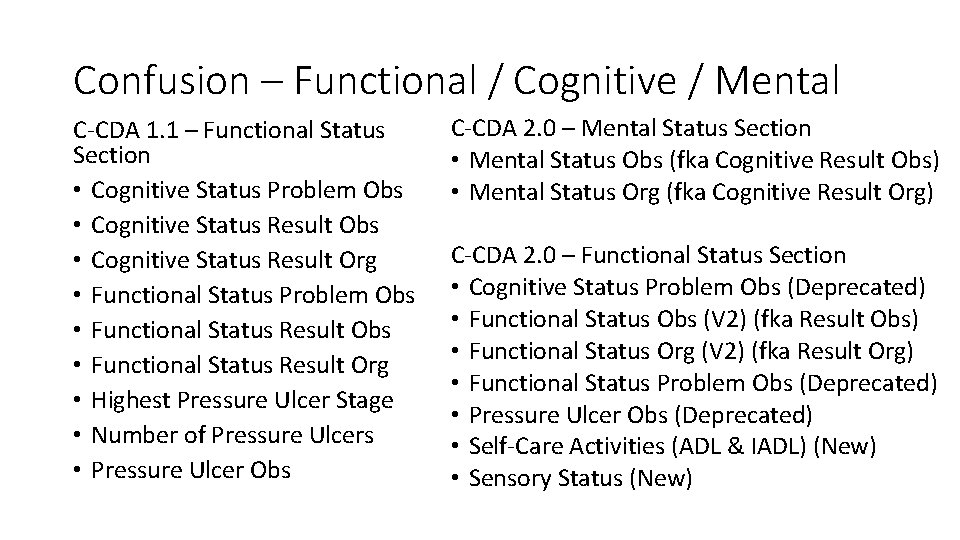
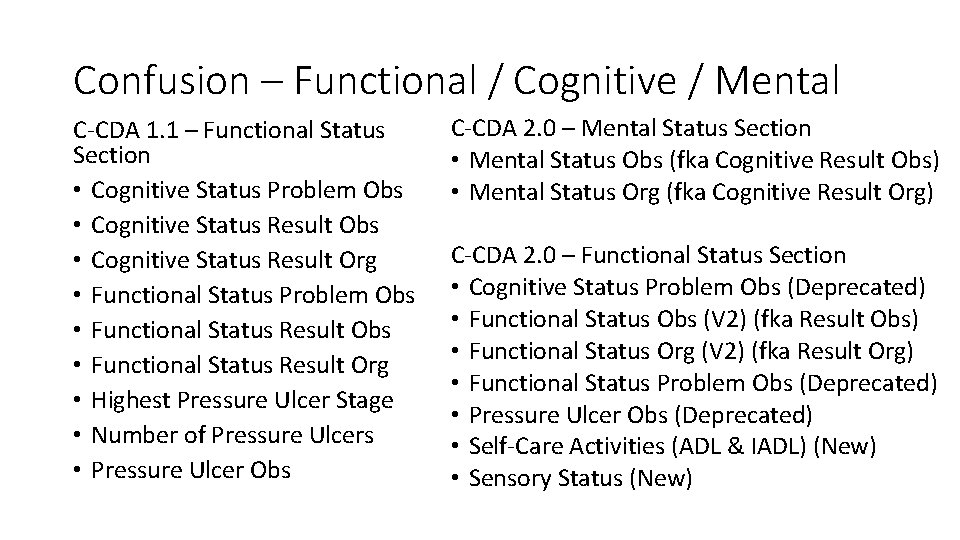
Confusion – Functional / Cognitive / Mental C-CDA 1. 1 – Functional Status Section • Cognitive Status Problem Obs • Cognitive Status Result Org • Functional Status Problem Obs • Functional Status Result Org • Highest Pressure Ulcer Stage • Number of Pressure Ulcers • Pressure Ulcer Obs C-CDA 2. 0 – Mental Status Section • Mental Status Obs (fka Cognitive Result Obs) • Mental Status Org (fka Cognitive Result Org) C-CDA 2. 0 – Functional Status Section • Cognitive Status Problem Obs (Deprecated) • Functional Status Obs (V 2) (fka Result Obs) • Functional Status Org (V 2) (fka Result Org) • Functional Status Problem Obs (Deprecated) • Pressure Ulcer Obs (Deprecated) • Self-Care Activities (ADL & IADL) (New) • Sensory Status (New)
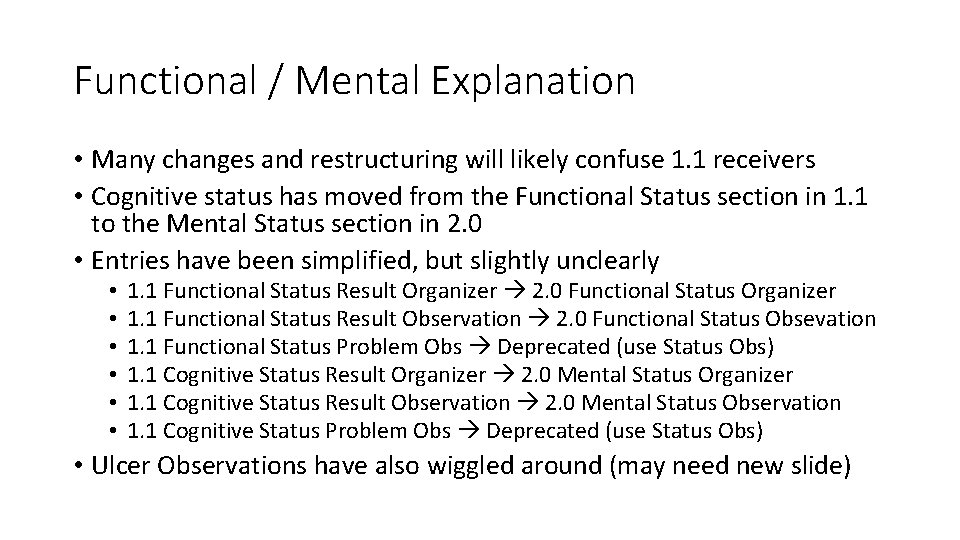
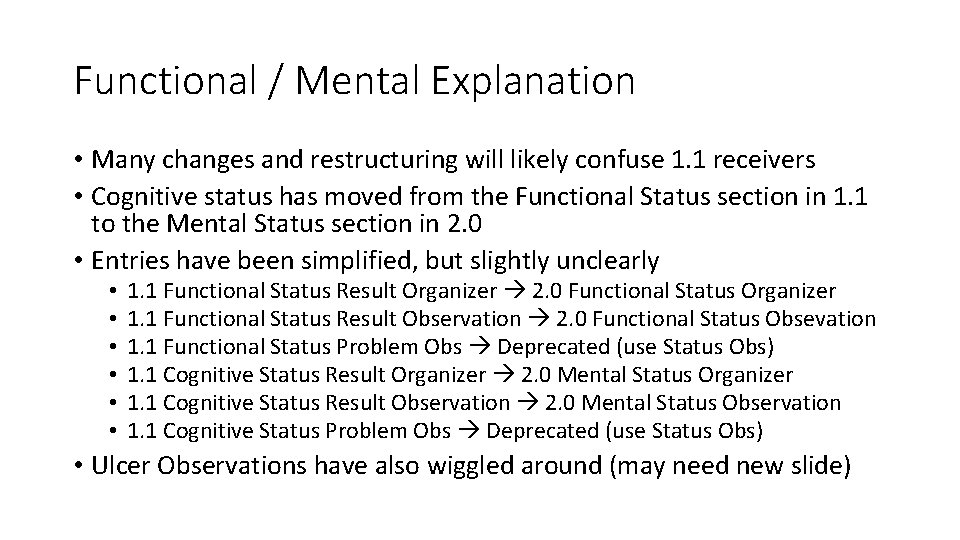
Functional / Mental Explanation • Many changes and restructuring will likely confuse 1. 1 receivers • Cognitive status has moved from the Functional Status section in 1. 1 to the Mental Status section in 2. 0 • Entries have been simplified, but slightly unclearly • • • 1. 1 Functional Status Result Organizer 2. 0 Functional Status Organizer 1. 1 Functional Status Result Observation 2. 0 Functional Status Obsevation 1. 1 Functional Status Problem Obs Deprecated (use Status Obs) 1. 1 Cognitive Status Result Organizer 2. 0 Mental Status Organizer 1. 1 Cognitive Status Result Observation 2. 0 Mental Status Observation 1. 1 Cognitive Status Problem Obs Deprecated (use Status Obs) • Ulcer Observations have also wiggled around (may need new slide)
 Ccda healthcare
Ccda healthcare Resolve complaint
Resolve complaint Define the short story
Define the short story Get up and bar the door translation
Get up and bar the door translation Aspects of the setting
Aspects of the setting Taylor resolve um problema
Taylor resolve um problema Which best explains the need for the great compromise?
Which best explains the need for the great compromise? Resolve ingredients
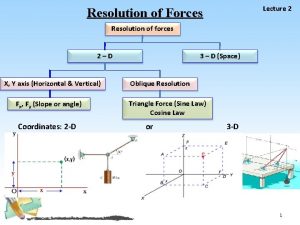
Resolve ingredients How to resolve vectors
How to resolve vectors Inherent resolve meaning
Inherent resolve meaning Tom overbye
Tom overbye 6 steps conflict resolution
6 steps conflict resolution Prudys
Prudys How to resolve the problem
How to resolve the problem Example of resolution of forces
Example of resolution of forces Tcpdump don't resolve
Tcpdump don't resolve How do the twelve tables resolve unpaid debts
How do the twelve tables resolve unpaid debts Whats a love triangle
Whats a love triangle Methods and metrics for cold-start recommendations
Methods and metrics for cold-start recommendations Ipcr adjectival rating
Ipcr adjectival rating Giving recommendations and opinions
Giving recommendations and opinions Asking and giving recommendations
Asking and giving recommendations