DSM 5 diagnostic criteria for bipolar and related
DSM 5 diagnostic criteria for bipolar and related disorders in persons with Robert. ID J. Pary NADD 2016
Acknowledgement Co-authors Lauren Charlot Sherman Fox Jessica Hellings Anne D. Hurley
Disclosures None
Aim To update evidence-based literature pertaining to the diagnosis of bipolar and related disorders in persons with ID
Historical context It is only in the past three plus decades that clinicians generally accepted the notion that a person with ID might be able to experience a mood disorder such as a bipolar disorder
Current Goal Ensure reliable assessments at the symptom level rather than developing new sets of criteria Use clear behaviorally based descriptions of possible manifestations of each DSM-5 symptom criterion
Work Group In the DSM-IV-TR (and in DM-ID), Bipolar Disorders were included in the Mood Disorders chapter In DSM 5 and DM-ID 2, Bipolar and Related Disorders comprise a separate chapter
Potential Bias To varying degrees, members of the work group believed that during the past several years the diagnosis (and subsequent pharmacologic treatment) of bipolar disorders spiked in persons with IDD
DSM 5 CRITERIA Manic Episode Criterion A A distinct period of abnormally and persistently elevated, expansive, or irritable mood AND
DSM 5 CRITERIA Manic Episode Criterion A abnormally and persistently increased goal-directed activity or energy
DSM 5 CRITERIA Manic Episode Criterion A lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary)
DSM 5 CRITERIA Manic Episode Criterion B During the period of mood disturbance and increased energy or activity
DSM 5 CRITERIA Manic Episode Criterion B three (or more) of the following symptoms (four if the mood is only irritable) are present to a significant degree AND
DSM 5 CRITERIA Manic Episode Criterion B represent a noticeable change from usual behavior:
DSM 5 CRITERIA Manic Episode Criterion B � 1. Inflated selfesteem or grandiosity
DSM 5 CRITERIA Manic Episode Criterion B � 2. Decreased need for sleep (e. g. , feels rested after only 3 hours of sleep)
DSM 5 CRITERIA Manic Episode Criterion B � 3. More talkative than usual or pressure to keep talking
DSM 5 CRITERIA Manic Episode Criterion B � 4. Flight of ideas or subjective experience that thoughts are racing
DSM 5 CRITERIA Manic Episode Criterion B � 5. Distractibility (i. e. , attention too easily drawn to unimportant or irrelevant external stimuli)
DSM 5 CRITERIA Manic Episode Criterion B � 6. Increase in goaldirected activity (either socially, at work or school, or sexually) or psychomotor agitation
DSM 5 CRITERIA Manic Episode Criterion B � 7. Excessive involvement in pleasurable activities that have a high potential for painful consequences (e. g. , engaging in unrestrained buying sprees, sexual indiscretions etc. )
DSM 5 CRITERIA Manic Episode Criterion C The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning OR
DSM 5 CRITERIA Manic Episode Criterion C to necessitate hospitalization to prevent harm to self or others OR
DSM 5 CRITERIA Manic Episode Criterion C there are psychotic features
DSM 5 CRITERIA Manic Episode Criterion D The episode is not attributable to the physiological effects of a substance (e. g. , a drug of abuse, a medication, other treatment) OR
DSM 5 CRITERIA Manic Episode Criterion D a general medical condition (e. g. , hyperthyroidism)
DSM 5 CRITERIA Manic Episode Criterion A full manic episode that emerges during antidepressant treatment (e. g. , medication, electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment Note:
DSM 5 CRITERIA Manic Episode Criterion is sufficient evidence for a manic episode and, therefore, a bipolar I diagnosis
DSM 5 Categories Bipolar I Disorder Bipolar II Disorder Cyclothymic Disorder Substance/Medication-Induced Bipolar and Related Disorder Due to Another Medical Condition Other Specified Bipolar and Related Disorder Unspecified Bipolar and Related Disorder
Diagnostic Issues between General Population and Persons with ID Rapid cycling, 4 or more episodes in a year, is more common in persons with ID than in general population Cerebral dysfunction is presumed to be a factor in the increased risk of rapid cycling
Diagnostic Issues between General Population and Persons with ID Developmental stage can affect cognitive symptoms of mania (i. e. "inflated self-esteem or grandiosity")
Diagnostic Issues between General Population and Persons with ID When cognitive symptoms are described in people with ID, content may be simplified May believe they possess more normal abilities they actually have Arrange for wedding but no girlfriend Try to buy a car but no driver’s license
Diagnostic Issues between General Population and Persons with ID Pressured speech can appear as increased vocalization (rate or volume) or gesturing in individuals who have limited expressive language
Diagnostic Issues between General Population and Persons with ID Might be completely silent during depressive episodes but vocalizes or babbles almost continuously during manic periods
Diagnostic Issues between General Population and Persons with ID Distractibility manifest as changes in ability level No longer completing daily living activities Skipping from one activity to another
Diagnostic Issues between General Population and Persons with ID Increased energy Walking for miles Repeatedly changing clothes More frenzied baseline behaviors Rapidly piling up books or aligning objects
Diagnostic Issues between General Population and Persons with ID Occasionally, one behavior can capture several manic criteria Vigorous masturbation LASTING throughout the night • Knocked mattress off bed
Diagnostic Issues between General Population and Persons with ID Recording of challenging behaviors can fluctutate so that the pattern suggests bipolar disorder
Diagnostic Issues between General Population and Persons with ID Challenging behaviors may be consistently under or over-reported Relief staff during weekends Prolonged substitute coverage High staff turnover Staff perceived medication change
Diagnostic Issues between General Population and Persons with ID Challenging behaviors are accurately reported, but variations are due to indirect effects of: On-site visits/inspections Sporadic family or close friend contact Serious illness: housemate, family or close friend
nd 2 Mania Not ALL bipolar-like symptoms MEAN Bipolar Dx Autoimmune Endocrine Neurologic Cerebrovascular Metabolic Substance withdrawal
nd 2 Mania The authors of DSM-5 opted not to include a concrete list of medical causes because such a list is never complete Clinical judgment is critical to diagnosing bipolar disorder due to a medical condition
nd 2 Mania Any medical condition that can result in bipolar symptoms in the general population cause manic symptoms in persons with ID
Method NADD expert work group examined changes in the Diagnostic Statistical Manual 5 (DSM 5) Reviewed pertinent evidenced-based literature for persons with IDD Submitted draft for peer review Revised draft
Method – Levels of Evidence Type I: good systematic review and meta-analyses with at least one randomized control trial (RCT) Type II: a RCT Type III: well-designed interventional study without randomization Type IV: well-designed observational Type V: expert opinion, influential reports and studies

Results No type I or type II levels of evidence were found Vast majority of studies were type IV or V
Results – DSM 5 Modifications for Bipolar Disorder Criterion A is revised to include increased energy or activity as a core symptom
Results – DSM 5 Modifications for Bipolar Disorder A person, who meets both the full criteria for mania and depression, is diagnosed with bipolar disorder I The new is “with mixed features” instead of bipolar disorder I, mixed episode as in DSM-IV
Results – DSM 5 Modifications for Bipolar Disorder The third pertinent change is the introduction of the diagnostic category of disruptive mood dysregulation disorder within the depressive disorders chapter
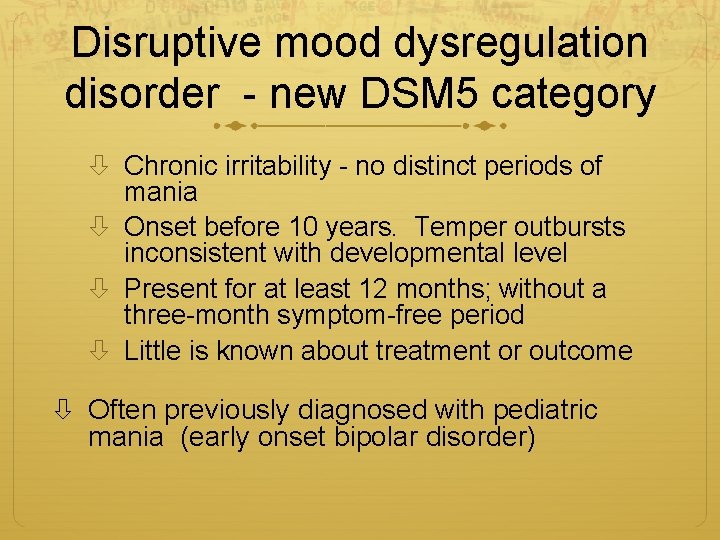
Disruptive mood dysregulation disorder - new DSM 5 category Chronic irritability - no distinct periods of mania Onset before 10 years. Temper outbursts inconsistent with developmental level Present for at least 12 months; without a three-month symptom-free period Little is known about treatment or outcome Often previously diagnosed with pediatric mania (early onset bipolar disorder)
Results In general population, 40 -fold increase in diagnosis of bipolar disorders in young people over a decade (Blader & Carlson, Biol Psychiatry 62: 107 -14 2007) Level V evidence of over-diagnosis of bipolar disorders in persons with IDD
For a reliable bipolar diagnosis in a youth with ID Clear change from previous functioning Not merely a worsening of, or fluctuation in, a condition present since early childhood
Over-diagnosis of Bipolar Disorder Individuals at risk for overdiagnosis of bipolar disorder include those with persistent irritability
Over-diagnosis of Bipolar Disorder Over-diagnosis of bipolar disorder can result in unnecessary exposure and the subsequent potential adverse effects of psychotropic medications
IASSIDD Meeting Colleagues from Europe and Australian/New Zealand did not agree that bipolar disorder was too frequently diagnosed Is over-diagnosis of Bipolar Disorder more typical of United States? North America?
DSM 5 Bipolar Disorders Systematic, prospective, wellcontrolled studies have not been conducted Using reliable means of assessing the presence of full DSM 5 criteria In representative samples of people with ID
DSM 5 Bipolar Disorders Bipolar Related Disorders have RARELY been studied Cyclothymia Bipolar II
Caution Case reports of bipolar Chromosome 22. q 11. 2 deletion (velocardiofacial or di. George syndrome) Chromsome 22 q 13. 3 deletion (Phelan. Mc. Dermid syndrome) Premature to associate any chromosomal syndromes with an increased risk for bipolar disorder
Limitation Data were not kept as to number of studies reviewed and those that were excluded from review involving persons with IDD
Conclusion Mood dysregulation disorder may provide greater diagnostic clarity for pediatric bipolar disorder The review highlights the potential over-diagnosis of bipolar and related for persons with IDD
- Slides: 60