Drugs for Heart Failure Two Major Forms of








- Slides: 33

Drugs for Heart Failure

Two Major Forms of Heart Failure 1. Heart failure with left ventricular (LV) systolic dysfunction 2. Diastolic heart failure, also known as heart failure with preserved LV ejection fraction Ø Note: In this chapter, we will focus primarily on the treatment of form #1

Heart Failure Progressive, often fatal disorder Characterized by left ventricular dysfunction, reduced cardiac output, insufficient tissue perfusion, and signs of fluid retention Affects nearly 5 million Americans

Pathophysiology of Heart Failure Inadequate tissue perfusion Volume overload Chronic hypertension Myocardial infarction Valvular heart disease Coronary artery disease Congenital heart disease Dysrhythmias Aging of the myocardium
Pathophysiology of Heart Failure Cardiac remodeling Physiologic adaptations to reduced cardiac output (CO) Ø Ø Cardiac dilation Increased sympathetic tone Water retention and increased blood volume Natriuretic peptides
Drugs for Heart Failure Diuretics RAAS inhibitors Ø Ø ACE inhibitors Angiotensin II receptor blockers Aldosterone antagonists Direct renin inhibitors Beta blockers Digoxin Other inotropic agents Other vasodilators
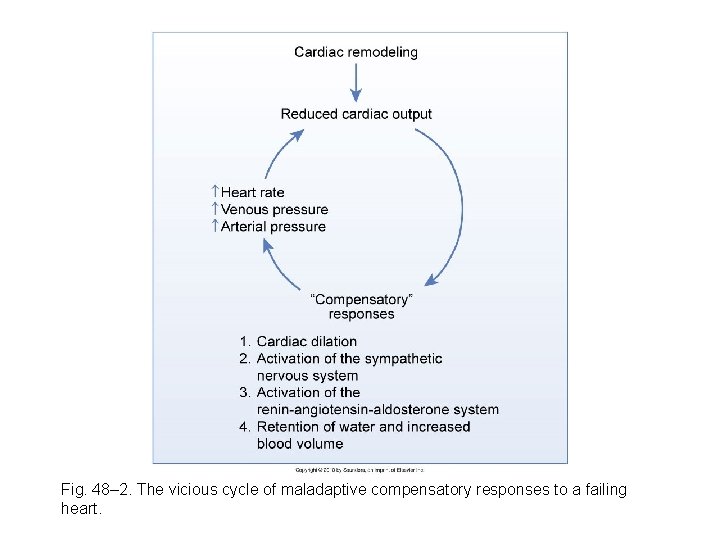
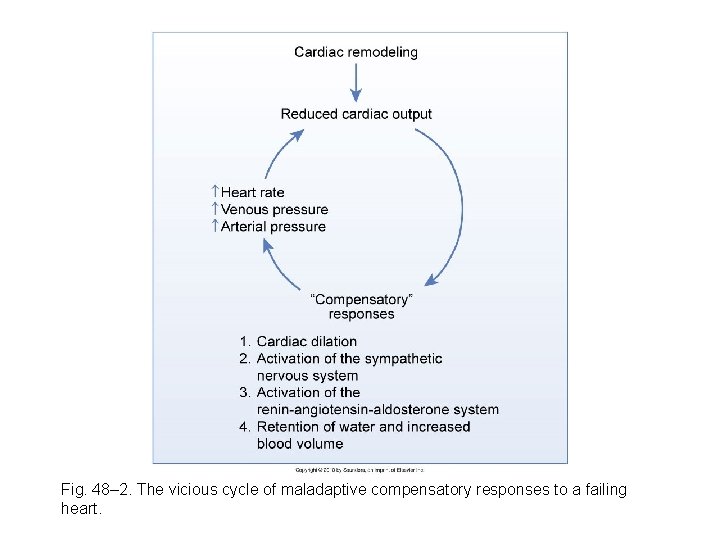
Fig. 48– 2. The vicious cycle of maladaptive compensatory responses to a failing heart.
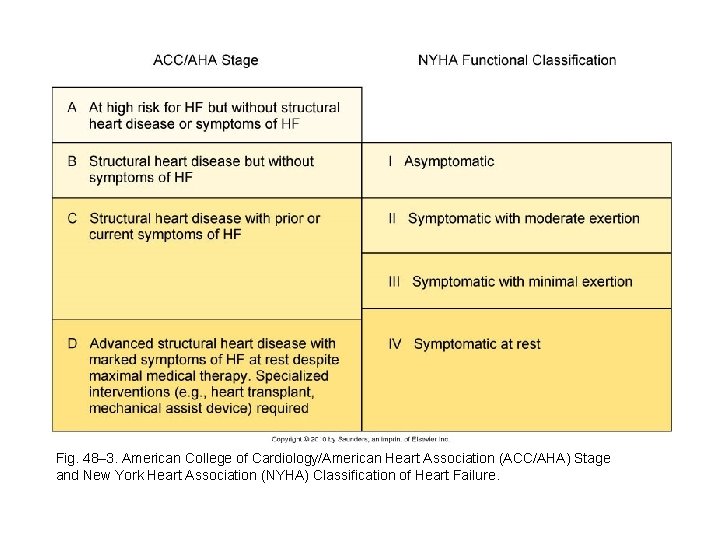
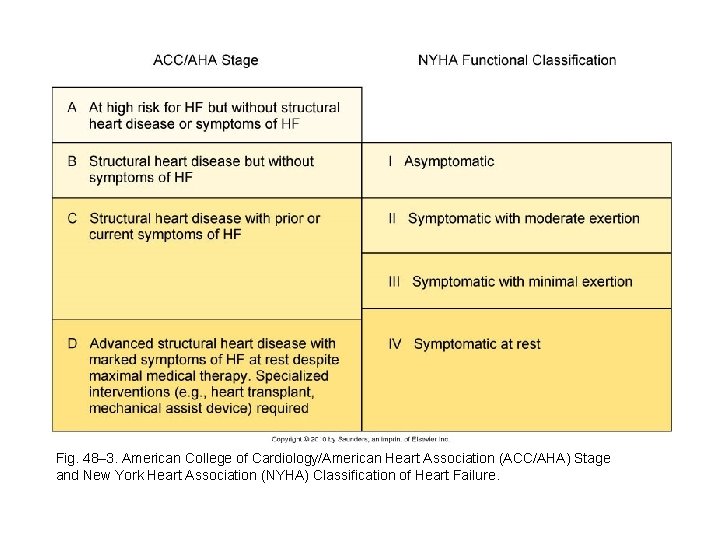
Fig. 48– 3. American College of Cardiology/American Heart Association (ACC/AHA) Stage and New York Heart Association (NYHA) Classification of Heart Failure.
Drugs Used to Treat Heart Failure Diuretics Drugs that inhibit the renin-angiotensinaldosterone system (RAAS) Beta blockers Digoxin and other cardiac glycosides Inotropic agents (other than cardiac glycosides) Vasodilators: other than ACE inhibitors and angiotensin-receptor blockers (ARBs)
Diuretics Thiazide diuretics High-ceiling (loop) diuretics Potassium-sparing diuretics
Drugs That Inhibit the RAAS ACE inhibitors Hemodynamic benefits • Arteriolar dilation • Venous dilation • Suppression of aldosterone release Ø Impact on cardiac remodeling • ACE inhibitors have favorable impact Ø

Drugs That Inhibit the RAAS ACE inhibitors (cont’d) Ø Adverse effects • Hypotension • Hyperkalemia • Intractable cough • Angioedema • Renal failure if patient has bilateral renal artery stenosis • Can cause fetal injury
Drugs That Inhibit the RAAS Angiotensin II receptor blockers Ø Clinical trials have shown that ARBs improve LV ejection fraction, reduce HF symptoms, increase exercise tolerance, decrease hospitalization, enhance quality of life, and reduce mortality
Drugs That Inhibit the RAAS Aldosterone antagonists Spironolactone (Aldactone) and eplerenone (Inspra) Ø Current studies recommend adding an aldosterone antagonist to standard HF therapy in patients with moderately severe or severe symptoms Ø
Drugs That Inhibit the RAAS Direct renin inhibitors Benefits in HF should be equal to those of ACE inhibitors or ARBs Ø Aliskiren (Tekturna) is being tested in HF Ø Not yet approved for HF treatment Ø

Beta Blockers Action With careful control of dosage, can improve patient status Ø Protect from excessive sympathetic stimulation Ø Protect against dysrhythmias Ø Adverse effects Ø Ø Fluid retention or worsening of HF Fatigue Hypotension Bradycardia or heart block
Digoxin and Cardiac Glycosides Positive inotropic actions Ø Ø Ø Increase myocardial contractile force Alter electrical activity of the heart Favorably affect neurohormonal systems Second-line agents
Inotropic Agents Sympathomimetics Ø Dopamine (Intropin) • Catecholamine • Activates beta 1 -adrenergic receptors in the heart, kidney, and blood vessels • Increases heart rate • Dilates renal blood vessels • Activates alpha 1 receptors
Inotropic Agents Sympathomimetics (cont’d) Ø Dobutamine • Synthetic catecholamine • Selective activation of beta 1 -adrenergic receptors Phosphodiesterase inhibitors Ø Ø Inamrinone—inodilator Milrinone (Primacor)
Vasodilators Isosorbide dinitrate plus hydralazine Intravenous vasodilators for acute care Ø Nitroglycerin • Principal adverse effects Hypotension Resultant reflex tachycardia Ø Sodium nitroprusside (Nitropress) • Principal adverse effect Ø Profound hypotension Nesiritide (Natrecor) • Principal adverse effect Symptomatic hypotension
Cardiac (Digitalis) Glycosides Digoxin (Lanoxin, Lanoxicaps, Digitek) Naturally occurring compound Profound effects on the mechanical and electrical properties of the heart Ø Increases myocardial contractility Ø Increased cardiac output Ø Adverse effect • Can cause severe dysrhythmias Ø Ø
Digoxin (Lanoxin) Effects Ø Ø Ø Relationship of potassium to inotropic action Ø Positive inotropic action on the heart Increases the force of ventricular contraction Increases myocardial contractility Potassium levels must be kept in normal physiologic range Hemodynamic benefits Ø Increased cardiac output • Decreased sympathetic tone • Increased urine production • Decreased renin release
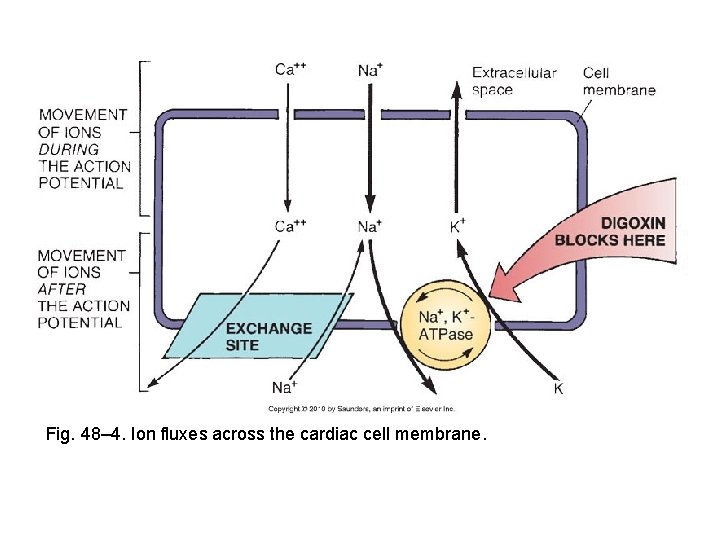
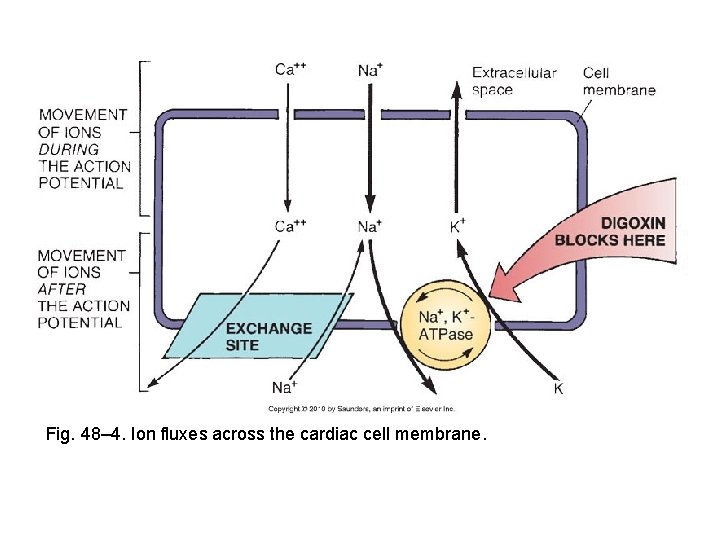
Fig. 48– 4. Ion fluxes across the cardiac cell membrane.
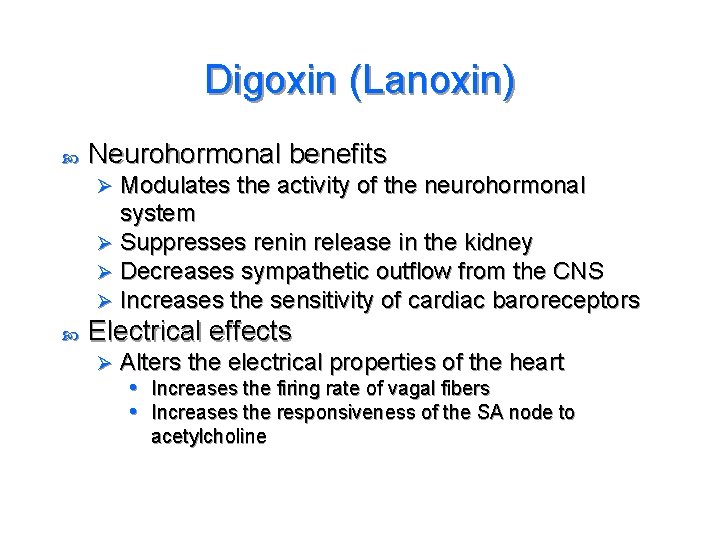
Digoxin (Lanoxin) Neurohormonal benefits Modulates the activity of the neurohormonal system Ø Suppresses renin release in the kidney Ø Decreases sympathetic outflow from the CNS Ø Increases the sensitivity of cardiac baroreceptors Ø Electrical effects Ø Alters the electrical properties of the heart • Increases the firing rate of vagal fibers • Increases the responsiveness of the SA node to acetylcholine
Digoxin (Lanoxin) Adverse effects Ø Ø Cardiac dysrhythmias Predisposing factors • Hypokalemia • Elevated digoxin level Narrow therapeutic range • Heart disease Ø Diagnosing digoxin-induced dysrhythmias Ø Managing digoxin-induced dysrhythmias
Digoxin (Lanoxin) Adverse effects (cont’d) Noncardiac adverse effects • Anorexia, nausea, vomiting, fatigue Ø Measures to reduce adverse effects • Education Ø
Digoxin (Lanoxin) Drug interactions Ø Ø Ø Diuretics ACE inhibitors and ARBs Sympathomimetics Quinidine Verapamil Pharmacokinetics Ø Ø Absorption Distributed widely and crosses the placenta Eliminated primarily by renal excretion Half-life about 1. 5 days
Management of Heart Failure Stage A No symptoms of HF No structural or functional cardiac abnormalities Hypertension, CAD, diabetes, family history of cardiomyopathy, personal history of alcohol abuse, rheumatic fever, or treatment with a cardiotoxic drug (eg, doxorubicin, trastuzumab) Ø Management directed at reducing risk Ø Ø Ø
Management of Heart Failure Stage B No signs and symptoms of HF Goal of management is to prevent development of symptomatic HF Ø Treatment is the same as for stage A with the addition of ACE inhibitors or ARBs Ø Ø
Management of Heart Failure Stage C Ø Ø Ø Symptoms of HF Structural heart disease Four major goals • Relieve pulmonary and peripheral congestive symptoms • Improve functional capacity and quality of life • Slow cardiac remodeling and progression of LV dysfunction • Prolong life

Management of Heart Failure Stage C (cont’d) Drug therapy • Diuretics • ACE inhibitors and ARBs • Aldosterone antagonists • Beta blockers • Digoxin • Isosorbide dinitrate/hydralazine Ø Drugs to avoid • Antidysrhythmic agents • Calcium channel blockers • NSAIDs Ø

Management of Heart Failure Stage C (cont’d) Device therapy • Implanted cardioverter-defibrillators • Cardiac resynchronization Ø Exercise training Ø Evaluating treatment • Based on symptoms and physical findings Ø
Management of Heart Failure Stage D Marked symptoms of HF Advanced structural heart disease Repeated hospitalizations Best solution is a heart transplant • LV mechanical assist device used until heart is available Ø Management • Control of fluid retention Ø Ø Loop diuretic, thiazide diuretic Dopamine, dobutamine • Beta blockers pose high risk for worsening HF