Drug Allergyurticaria and anaphylaxis Drug related side effects






- Slides: 66
Drug Allergyurticaria and anaphylaxis 國立成功大學醫學院小兒學科 王志堯
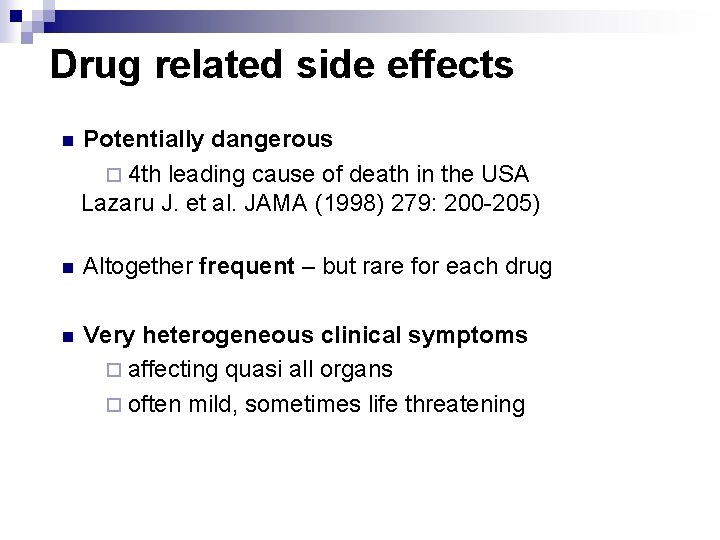
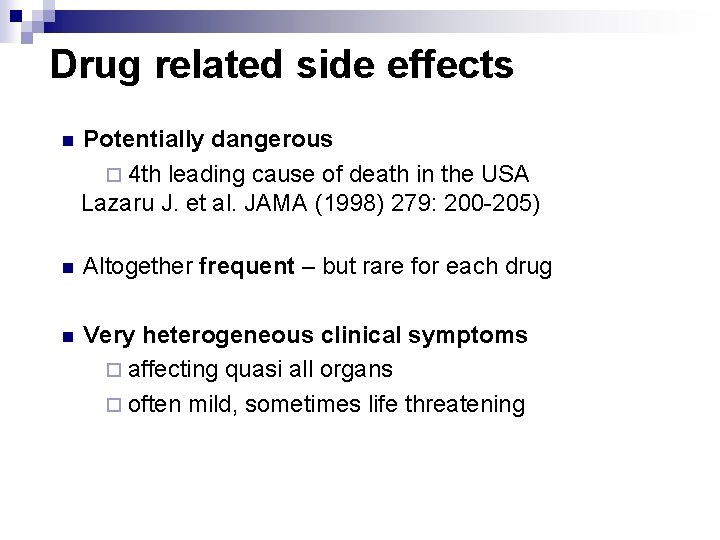
Drug related side effects n Potentially dangerous ¨ 4 th leading cause of death in the USA Lazaru J. et al. JAMA (1998) 279: 200 -205) n Altogether frequent – but rare for each drug n Very heterogeneous clinical symptoms ¨ affecting quasi all organs ¨ often mild, sometimes life threatening
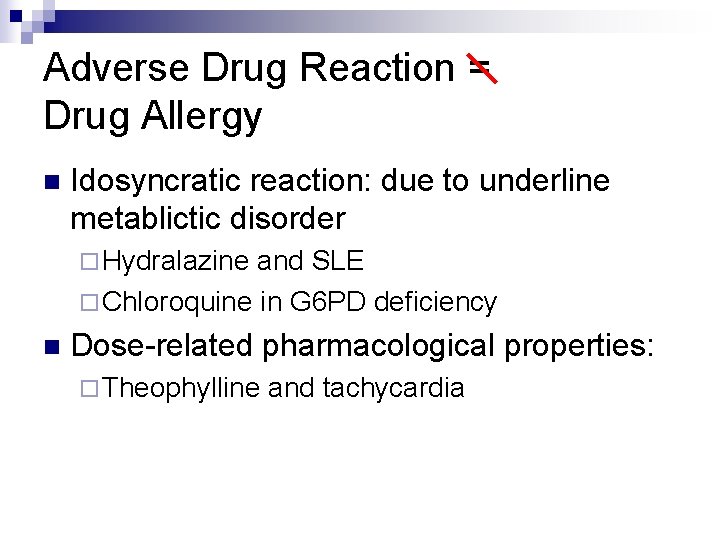
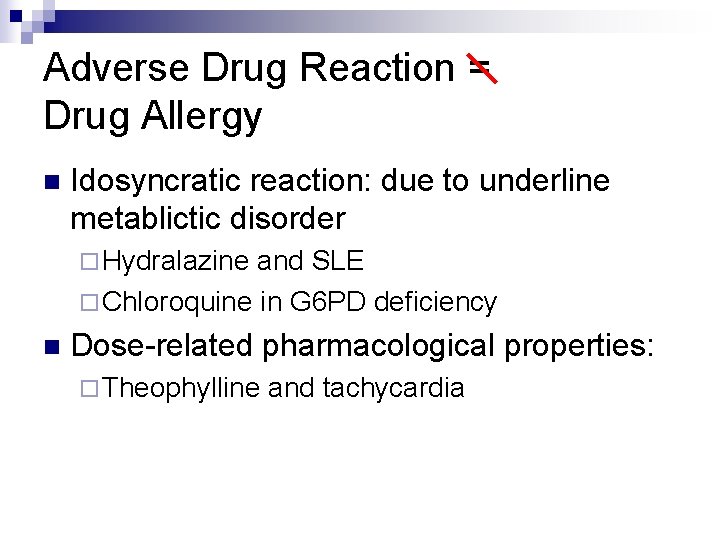
Adverse Drug Reaction = Drug Allergy n Idosyncratic reaction: due to underline metablictic disorder ¨ Hydralazine and SLE ¨ Chloroquine in G 6 PD deficiency n Dose-related pharmacological properties: ¨ Theophylline and tachycardia
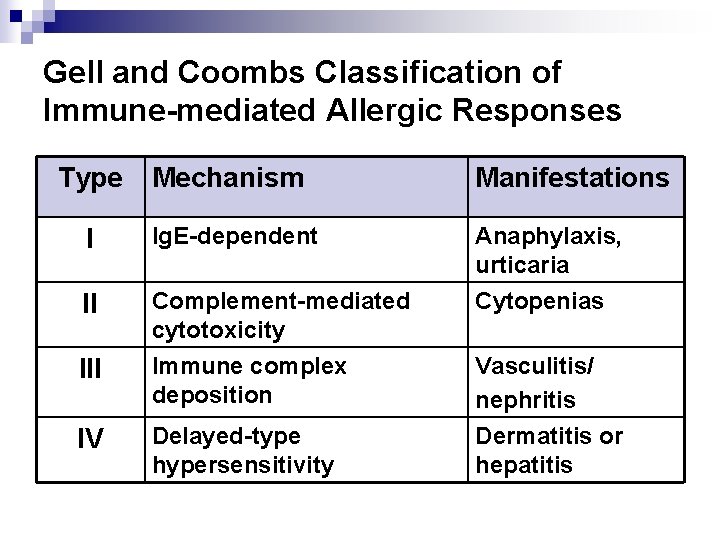
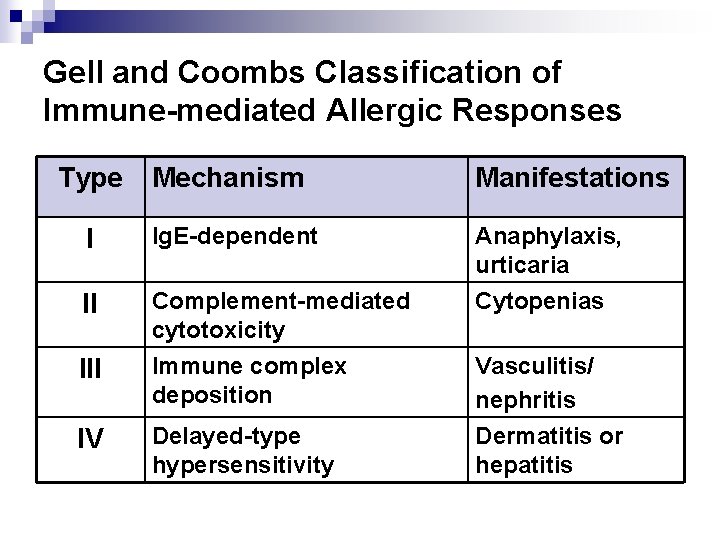
Gell and Coombs Classification of Immune-mediated Allergic Responses Type Mechanism Manifestations I Ig. E-dependent Anaphylaxis, urticaria II Complement-mediated cytotoxicity Cytopenias III Immune complex deposition Vasculitis/ nephritis IV Delayed-type hypersensitivity Dermatitis or hepatitis
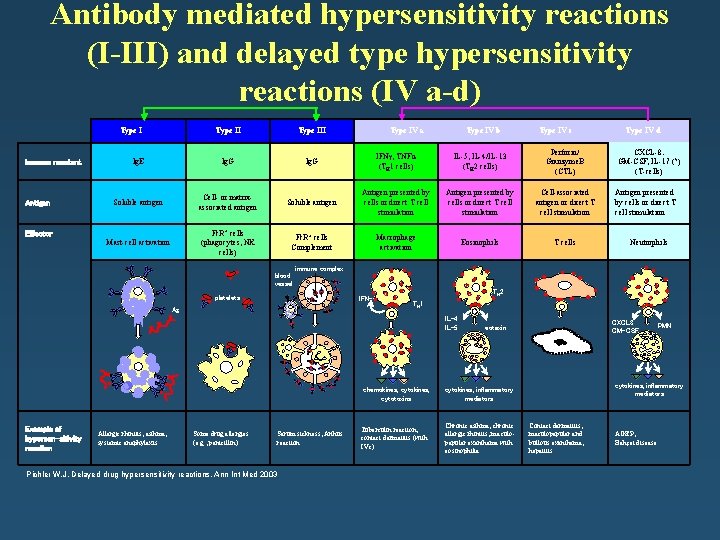
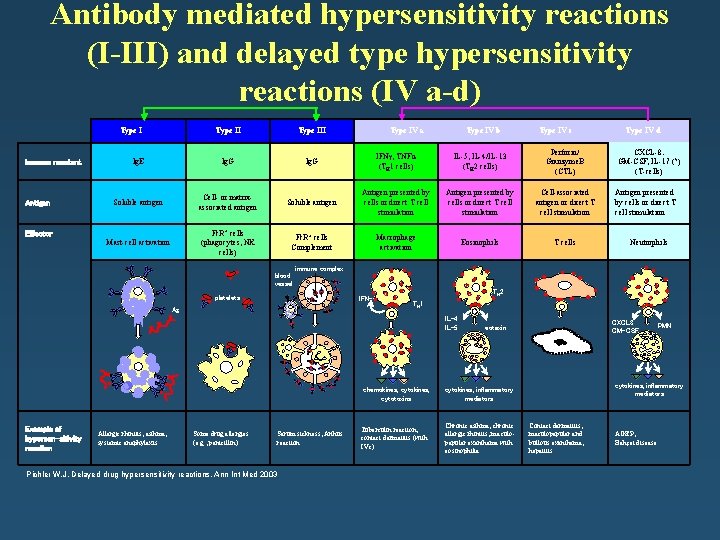
Antibody mediated hypersensitivity reactions (I-III) and delayed type hypersensitivity reactions (IV a-d) Type I Immune reactant Antigen Type III Ig. E Ig. G IFN , TNFα (TH 1 cells) IL-5, IL-4/IL-13 (TH 2 cells) Perforin/ Granzyme. B (CTL) Soluble antigen Cell- or matrixassociated antigen Soluble antigen Antigen presented by cells or direct T cell stimulation Cell-associated antigen or direct T cell stimulation Mast-cell activation Fc. R+ cells (phagocytes, NK cells) Fc. R+ cells Complement Macrophage activation Eosinophils T cells Effector Type IV a Type IV b Type IV c Type IV d CXCL-8. GM-CSF, IL-17 (? ) (T-cells) Antigen presented by cells or direct T cell stimulation Neutrophils immune complex blood vessel platelets IFN- Ag TH 2 TH 1 IL-4 IL-5 Example of hypersen-sitivity reaction Allergic rhinitis, asthma, systemic anaphylaxis Some drug allergies (e. g. , penicillin) Serum sickness, Arthus reaction Pichler W. J. Delayed drug hypersensitivity reactions, Ann Int Med 2003 eotaxin chemokines, cytotoxins cytokines, inflammatory mediators Tuberculin reaction, contact dermatitis (with IVc) Chronic asthma, chronic allergic rhinitis, maculopapular exanthema with eosinophilia CTL CXCL 8 GM-CSF PMN cytokines, inflammatory mediators Contact dermatitis, maculopapular and bullous exanthema, hepatitis AGEP, Behçet disease
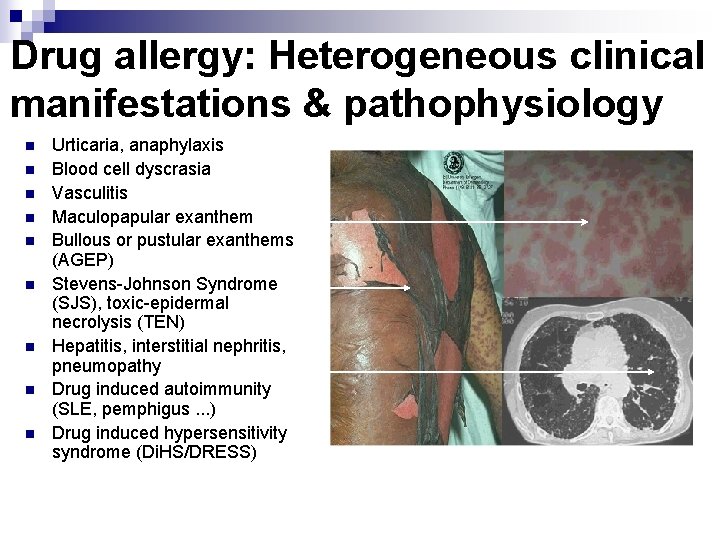
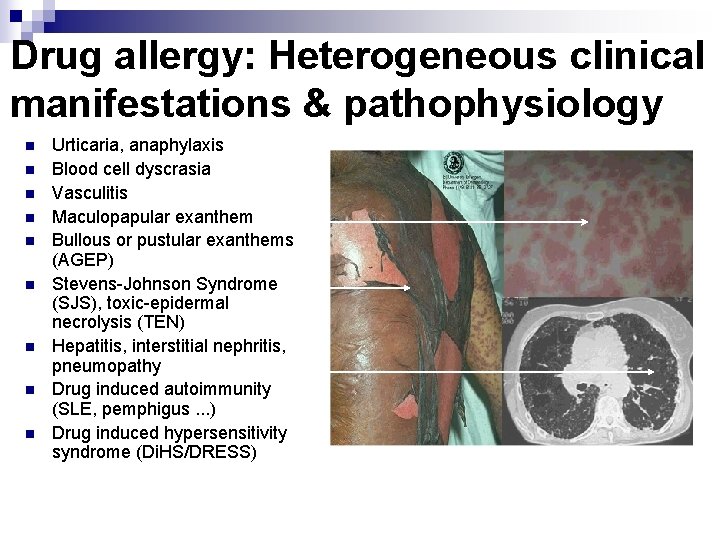
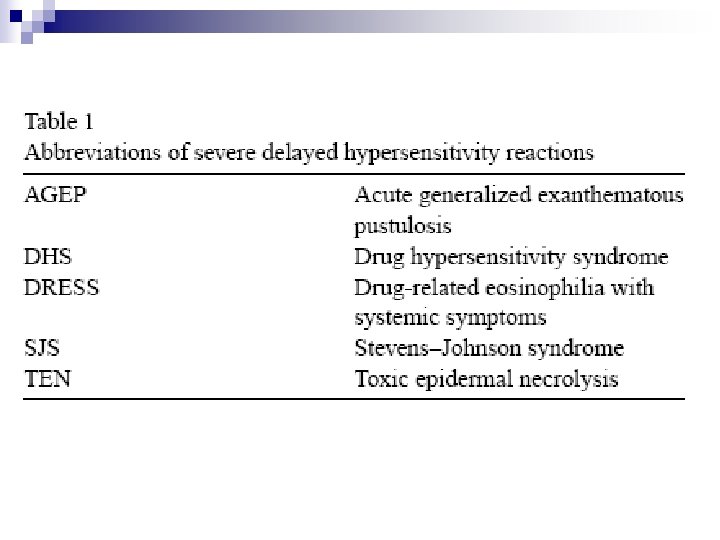
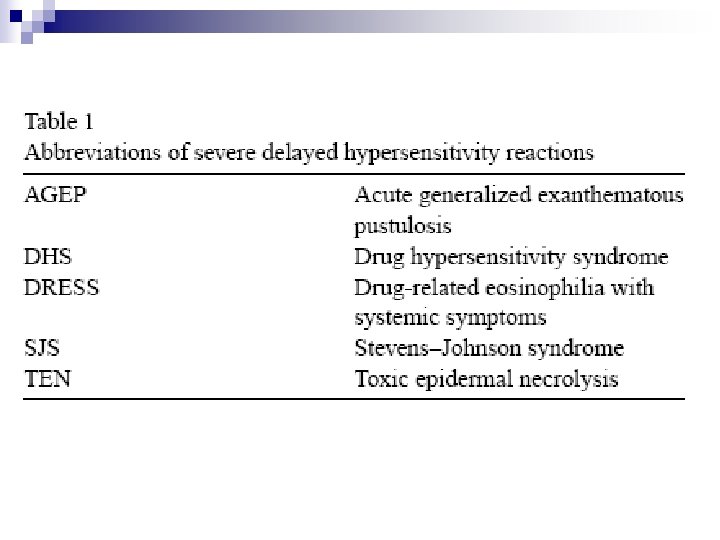
Drug allergy: Heterogeneous clinical manifestations & pathophysiology n n n n n Urticaria, anaphylaxis Blood cell dyscrasia Vasculitis Maculopapular exanthem Bullous or pustular exanthems (AGEP) Stevens-Johnson Syndrome (SJS), toxic-epidermal necrolysis (TEN) Hepatitis, interstitial nephritis, pneumopathy Drug induced autoimmunity (SLE, pemphigus. . . ) Drug induced hypersensitivity syndrome (Di. HS/DRESS)
Allergic vs non-allergic drug hypersensitivity Allergic Non-allergic Immune reactions (T-cells, Ig. E, Ig. G against a drug/metabolite with exanthema, urticaria, etc. ) n Highly specific n Dependent of structure n Can be dangerous, severe (Ig. E & T cell reactions!) n Cross-reactions to structurally related compounds n Ig. E to drug occasionally detectable (skin tests, Ig. Eserology) No immune reaction against the drug detectable, symptoms can occur at the first contact n Activation of immunological effector cells (mast-cells, basophil leukocytes, etc) n Cross-reactions due to function of drug, not structure n Skin tests and serology negative Drug provocation tests can be positive in allergic and non allergic reactions
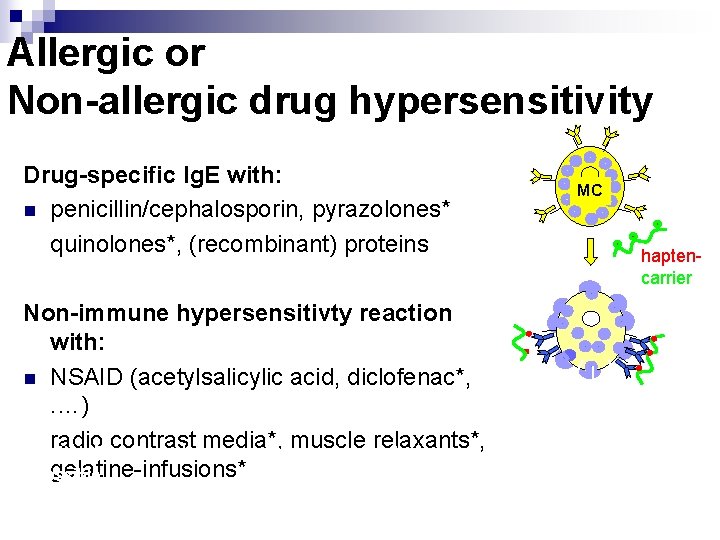
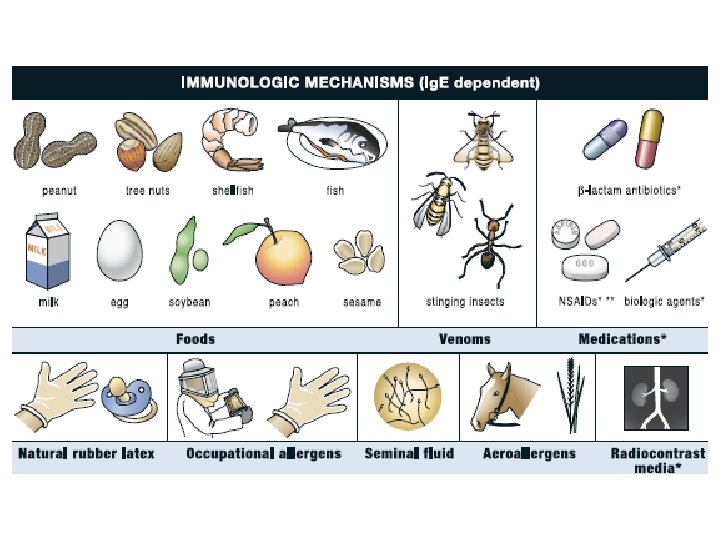
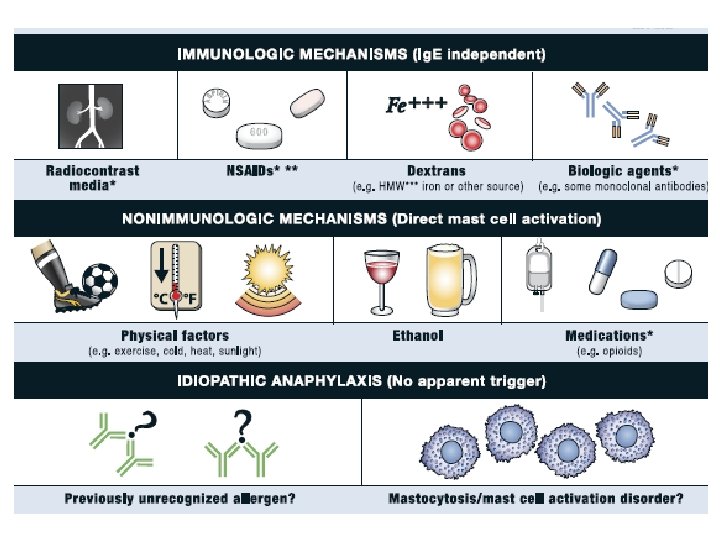
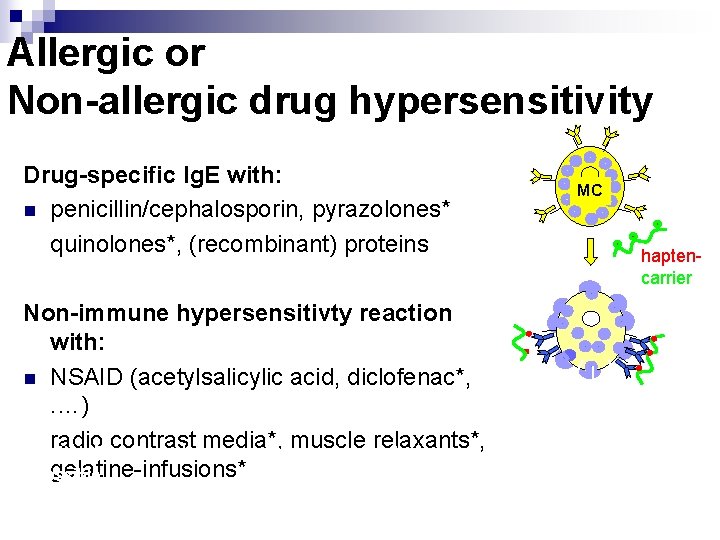
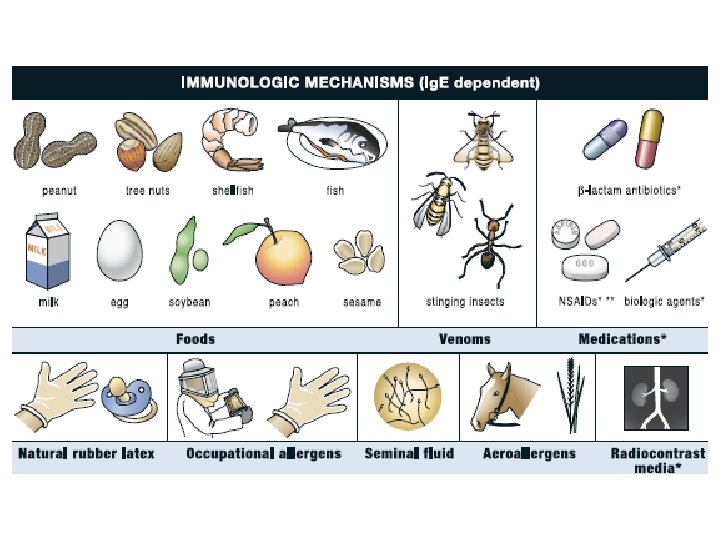
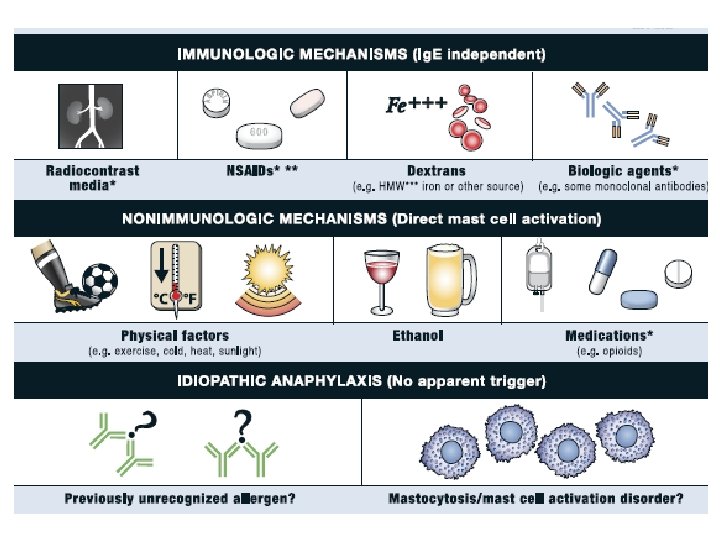
Allergic or Non-allergic drug hypersensitivity Drug-specific Ig. E with: n penicillin/cephalosporin, pyrazolones* quinolones*, (recombinant) proteins Non-immune hypersensitivty reaction with: n NSAID (acetylsalicylic acid, diclofenac*, . …) radio contrast media*, muscle relaxants*, * Both Ig. E and non-immune mediated mechanisms gelatine-infusions* possible MC haptencarrier Histamine, LT, TNFa, Tryptase, . .
Sub-classification of drug allergy n According to ¨ Timing of onset n Symptoms start <1 hr after administration (immediate) vs n >1 hr (often 6 hr) after application (delayed) - Immune mechanism n Gell & Coombs classification, type I-IVa-d - Combined n Immediate and Ig. E mediated n Delayed and T-cell mediated (rarely Ig. G) n Correlating the clinical manifestations with the immununological mechanisms
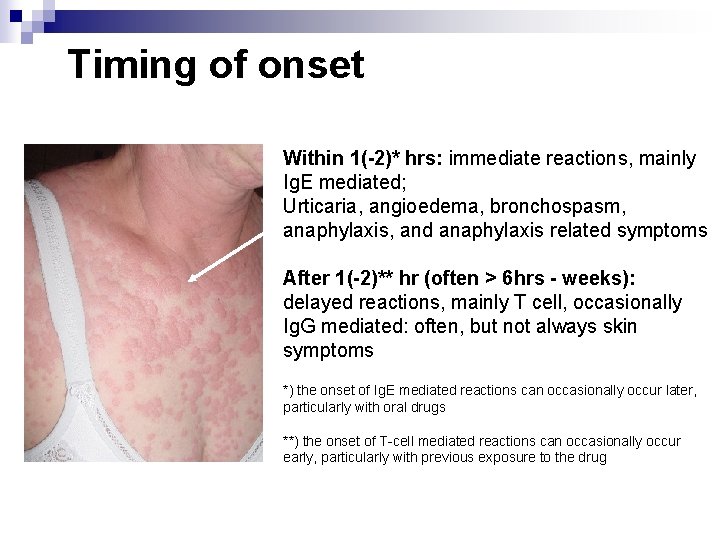
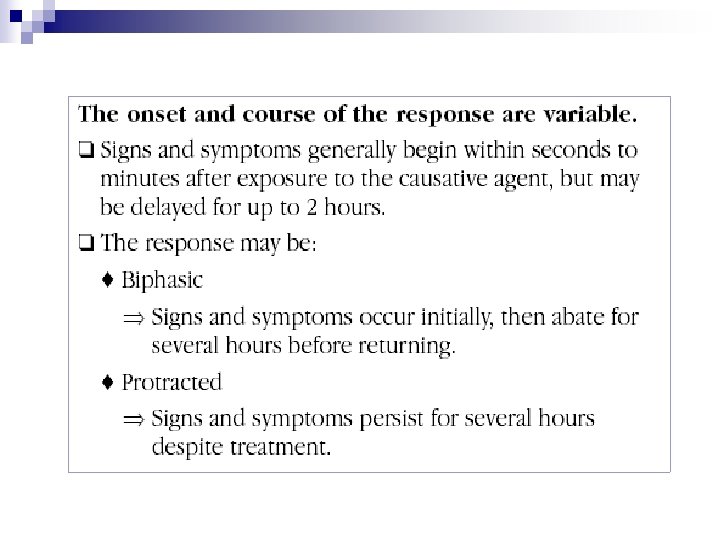
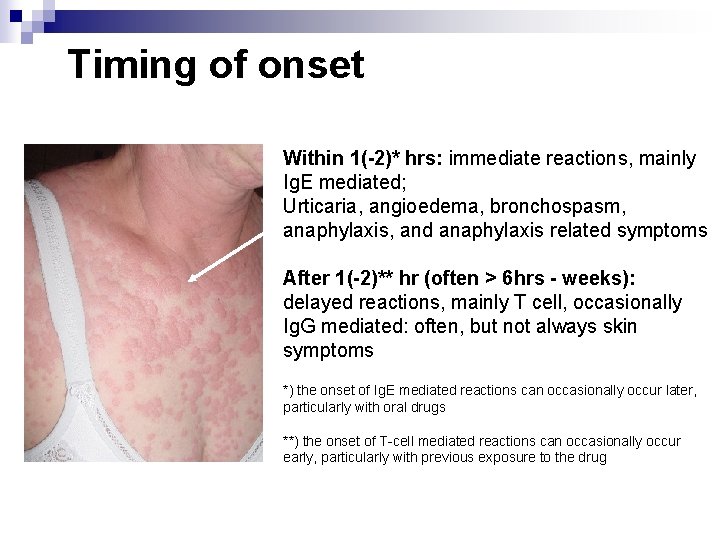
Timing of onset Within 1(-2)* hrs: immediate reactions, mainly Ig. E mediated; Urticaria, angioedema, bronchospasm, anaphylaxis, and anaphylaxis related symptoms After 1(-2)** hr (often > 6 hrs - weeks): delayed reactions, mainly T cell, occasionally Ig. G mediated: often, but not always skin symptoms *) the onset of Ig. E mediated reactions can occasionally occur later, particularly with oral drugs **) the onset of T-cell mediated reactions can occasionally occur early, particularly with previous exposure to the drug
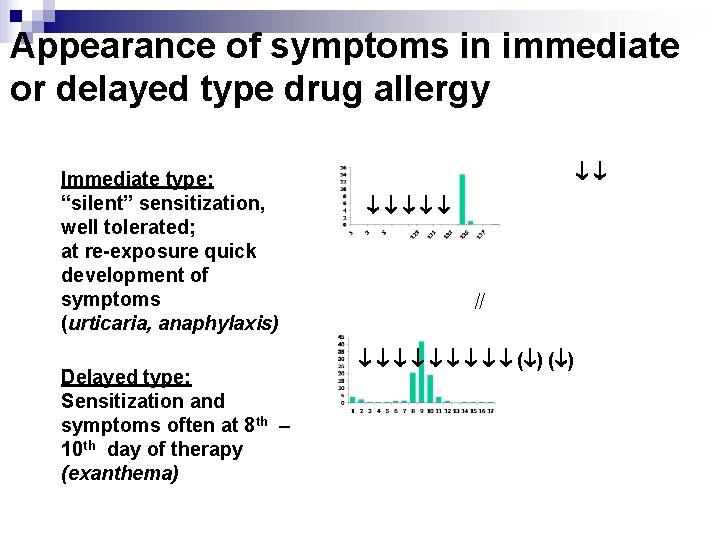
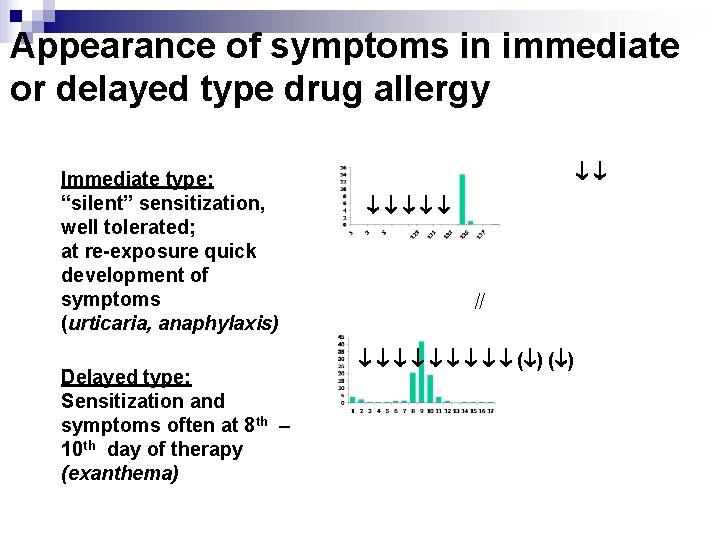
Appearance of symptoms in immediate or delayed type drug allergy Immediate type: “silent” sensitization, well tolerated; at re-exposure quick development of symptoms (urticaria, anaphylaxis) Delayed type: Sensitization and symptoms often at 8 th – 10 th day of therapy (exanthema) ( )

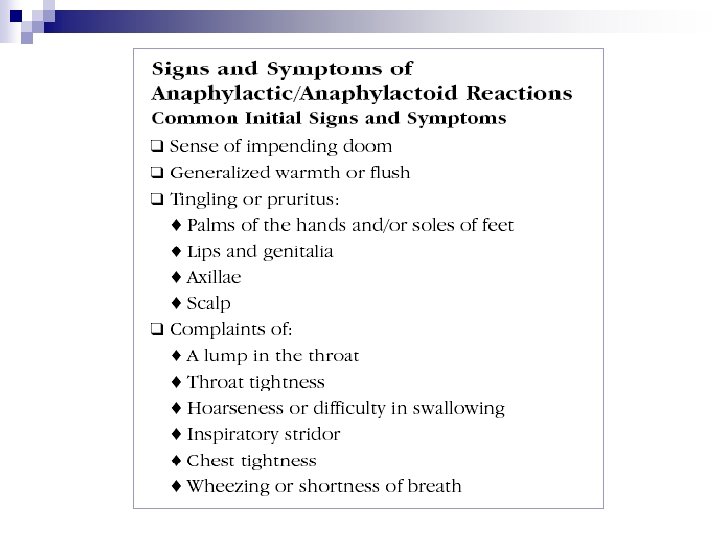
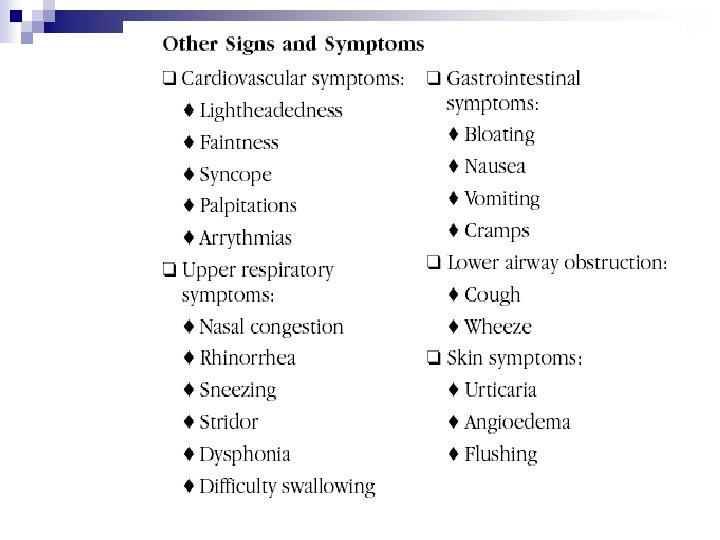
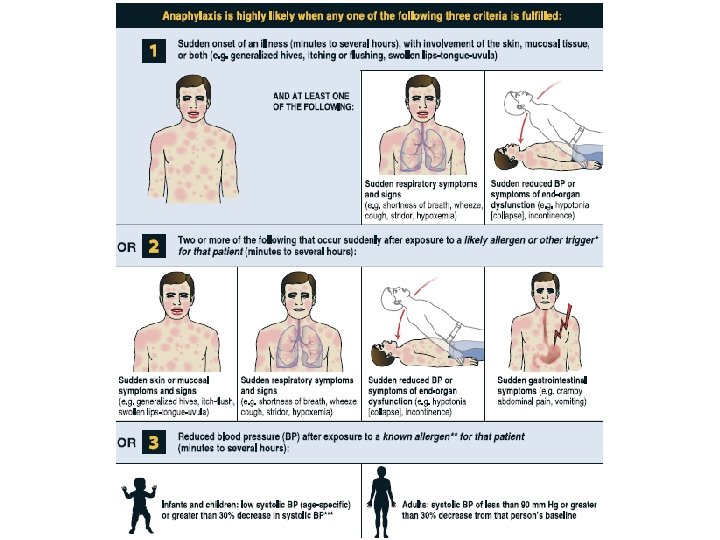
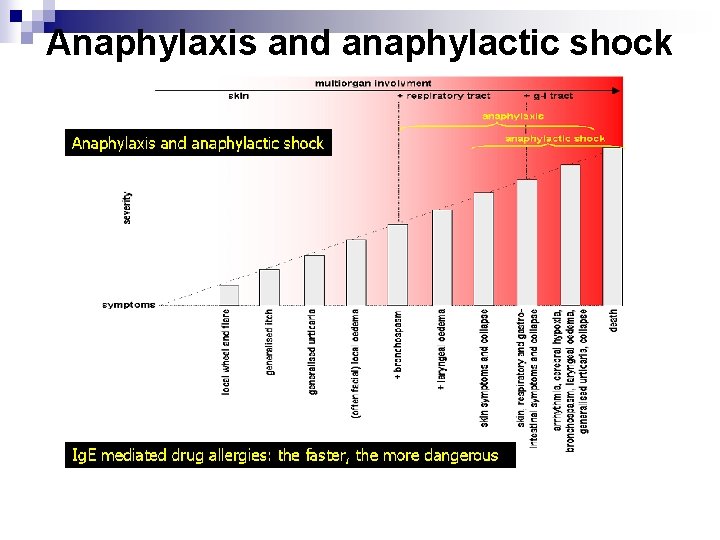
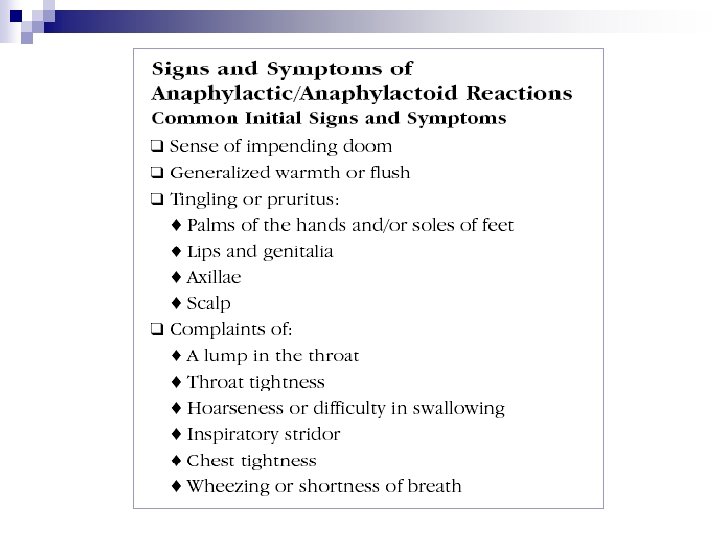
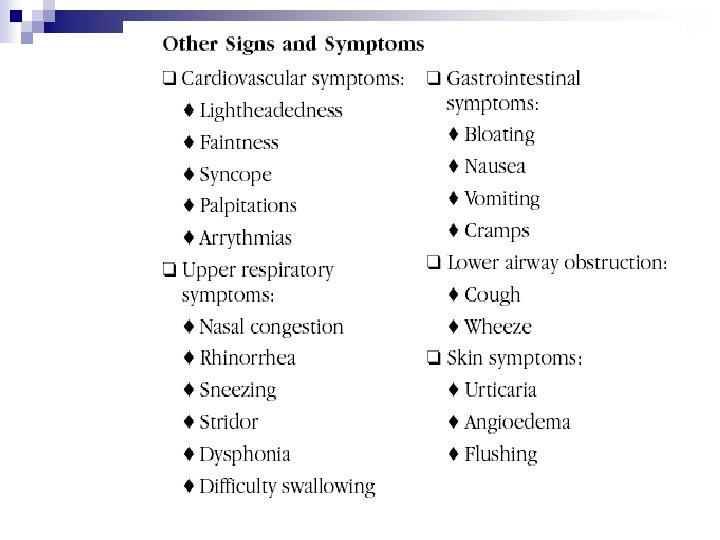
Clinical Symptoms and Signs Type I (Ig. E mediated) Allergy or non-immune hypersensitivity reaction • rapidly appearing urticaria • rapidly appearing angioedema, mostly periorbital, oral, genital swellings, with moderate pruritus, in association with generalized urticaria • gastrointestinal symptoms: cramps, diarrhoea, vomiting • anaphylaxis and anaphylactic shock
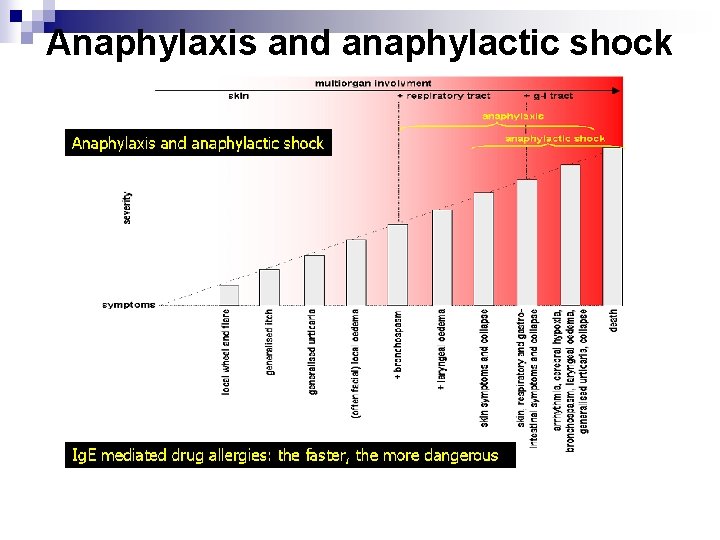
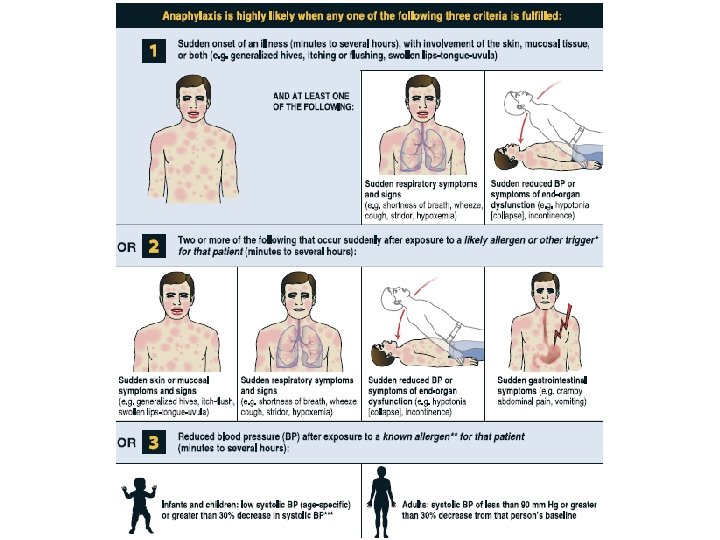
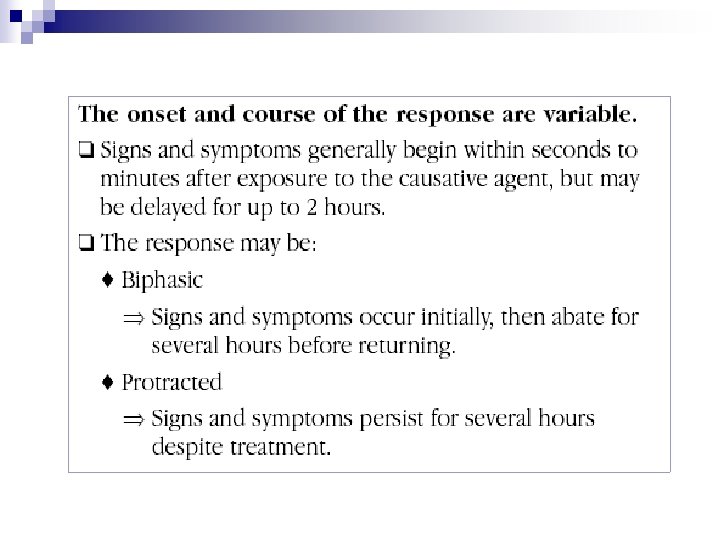
Anaphylaxis and anaphylactic shock

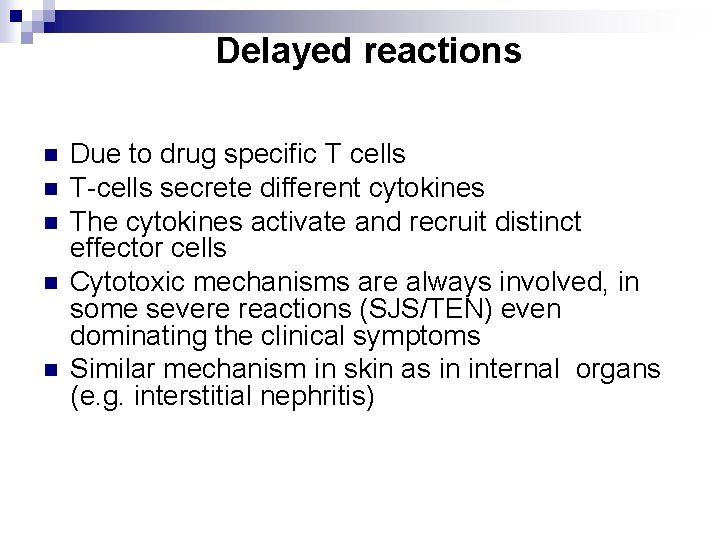
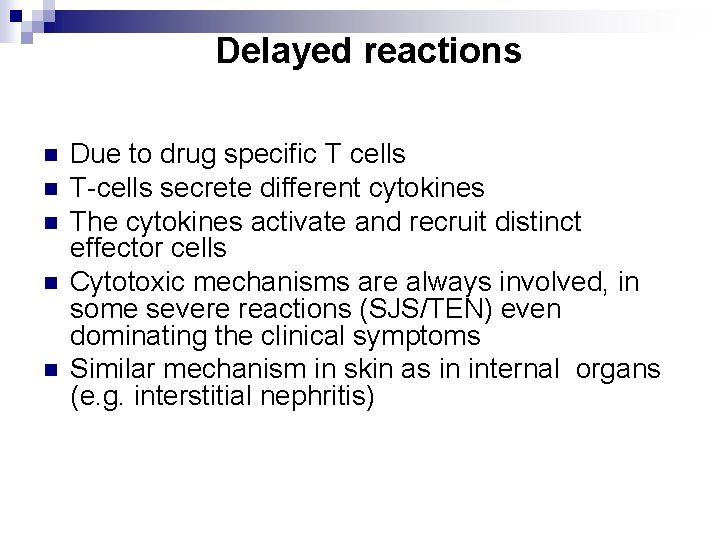
Delayed reactions n n n Due to drug specific T cells T-cells secrete different cytokines The cytokines activate and recruit distinct effector cells Cytotoxic mechanisms are always involved, in some severe reactions (SJS/TEN) even dominating the clinical symptoms Similar mechanism in skin as in internal organs (e. g. interstitial nephritis)
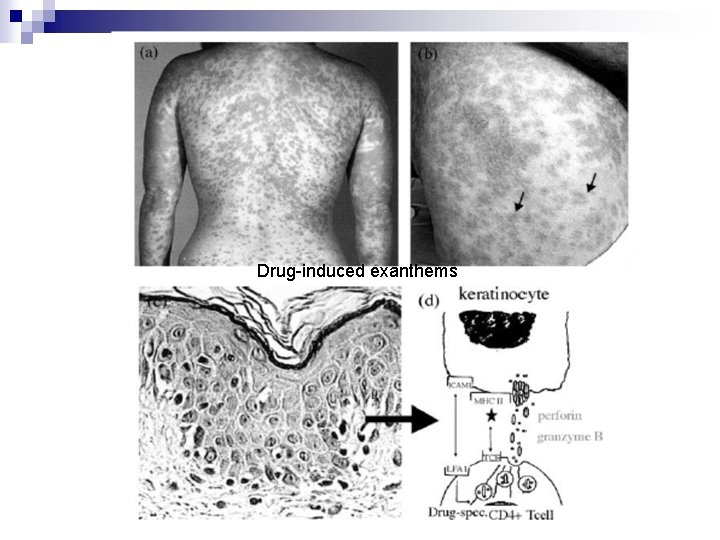
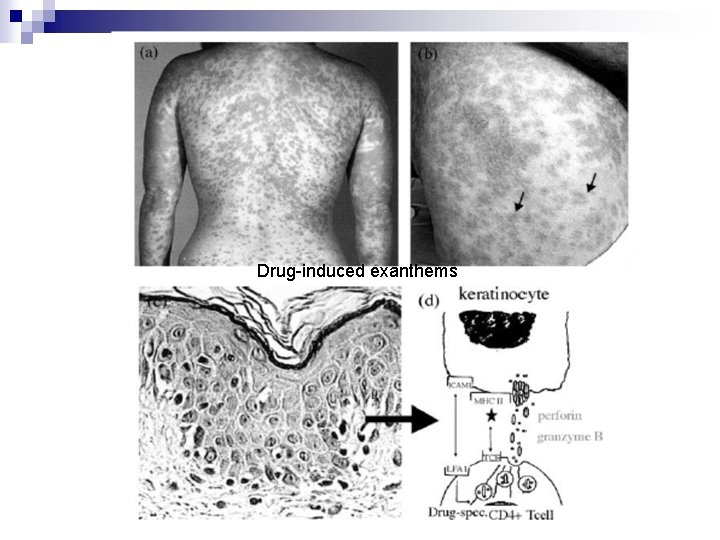
Drug-induced exanthems
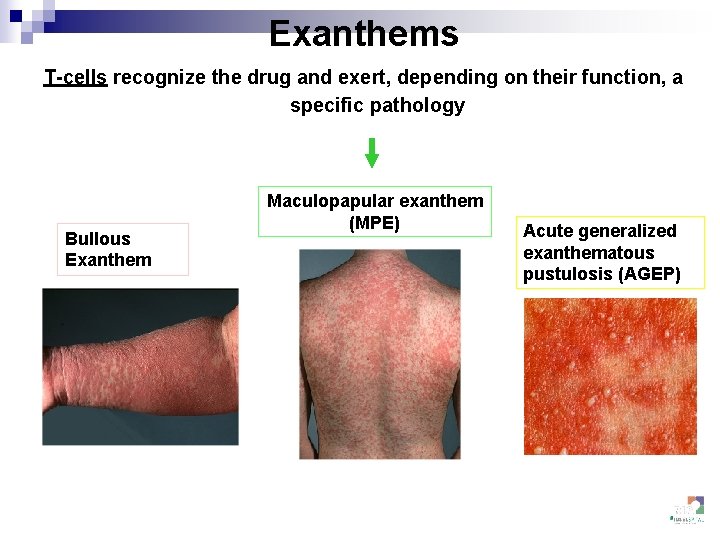
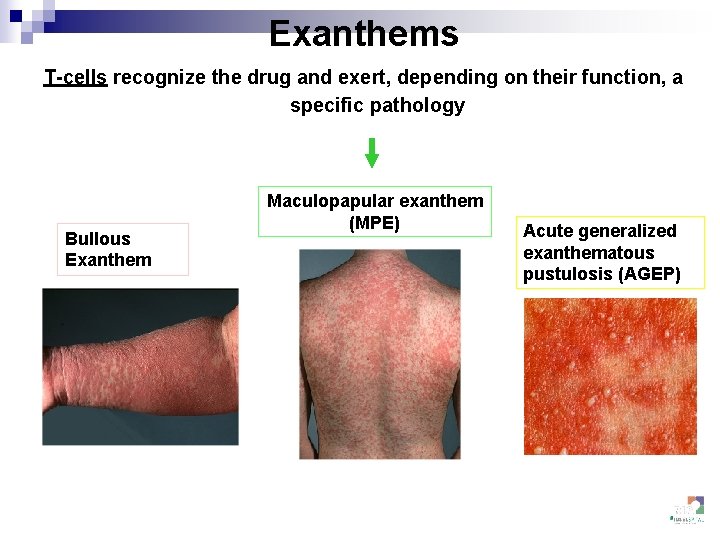
Exanthems T-cells recognize the drug and exert, depending on their function, a specific pathology Bullous Exanthem Maculopapular exanthem (MPE) Acute generalized exanthematous pustulosis (AGEP)
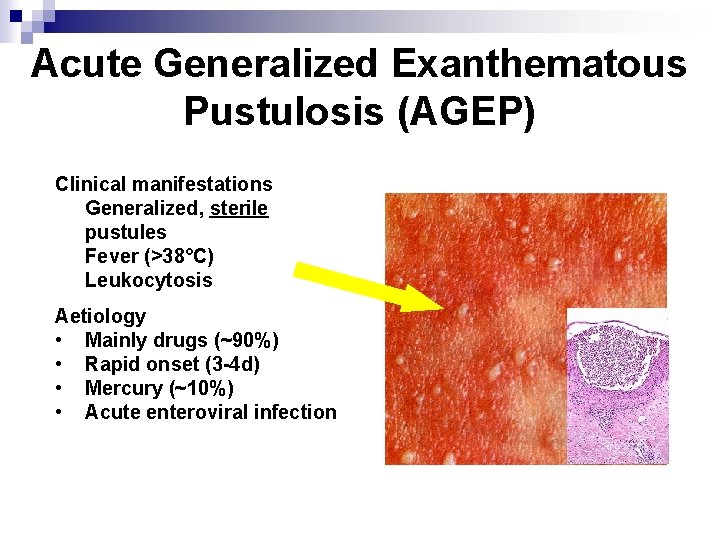
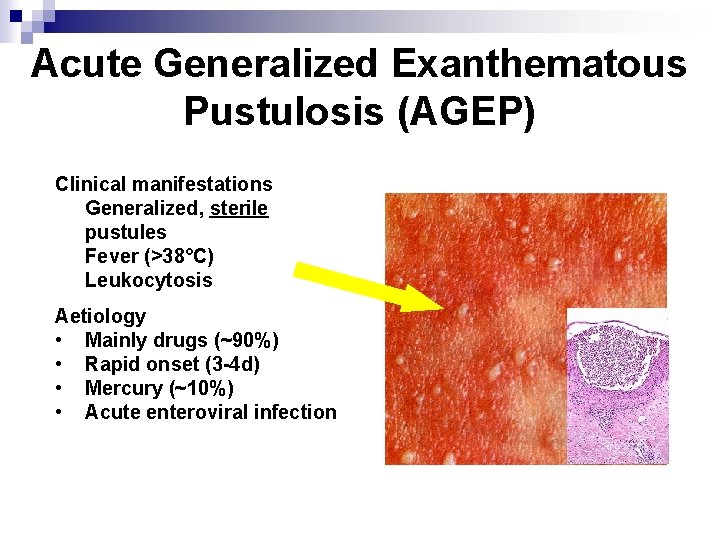
Acute Generalized Exanthematous Pustulosis (AGEP) Clinical manifestations • Generalized, sterile pustules • Fever (>38°C) • Leukocytosis Aetiology • Mainly drugs (~90%) • Rapid onset (3 -4 d) • Mercury (~10%) • Acute enteroviral infection
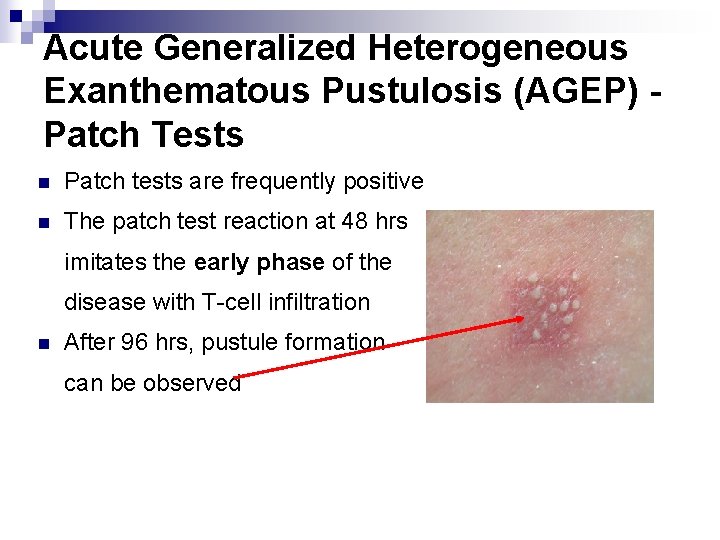
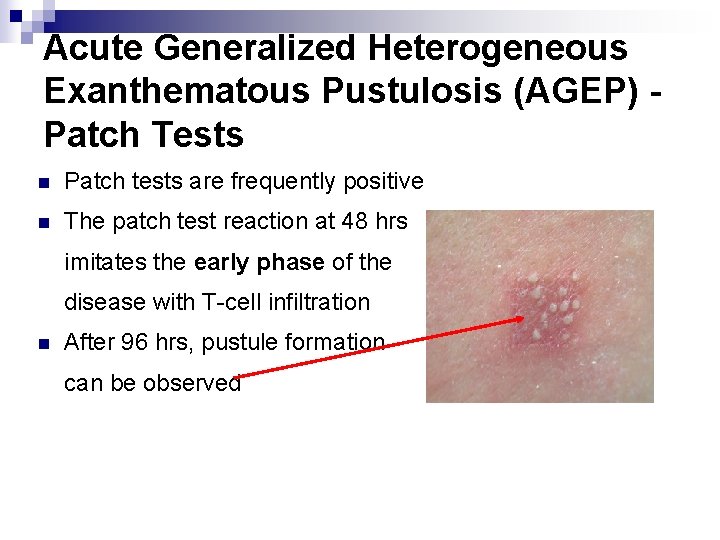
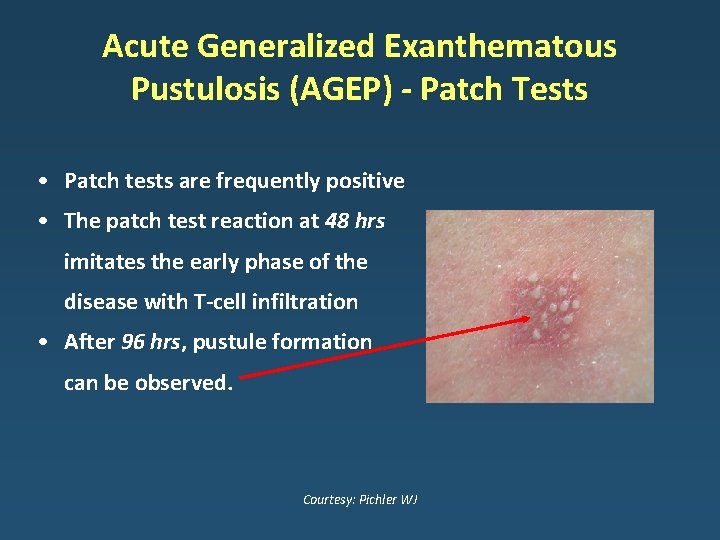
Acute Generalized Heterogeneous Exanthematous Pustulosis (AGEP) Patch Tests n Patch tests are frequently positive n The patch test reaction at 48 hrs imitates the early phase of the disease with T-cell infiltration n After 96 hrs, pustule formation can be observed



Acute generalized exanthematous pustulosis (AGEP)
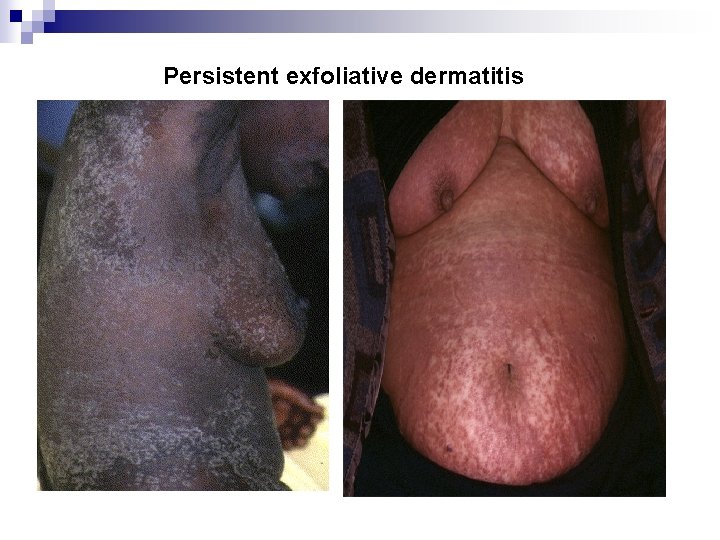
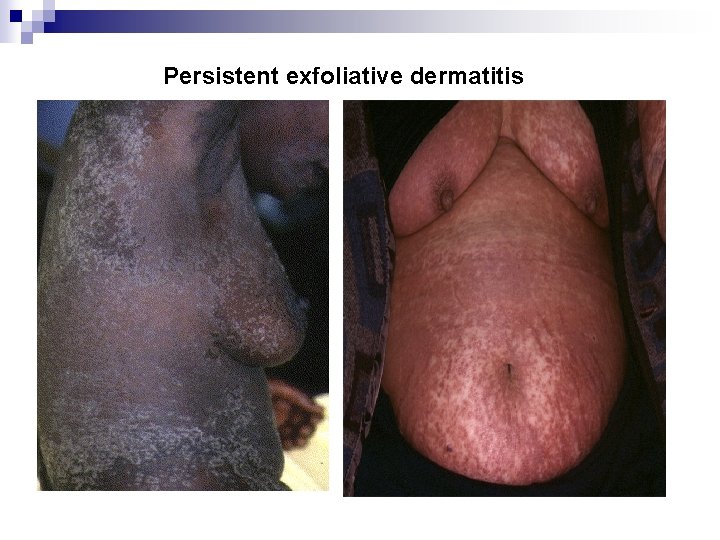
Persistent exfoliative dermatitis

Overlap SJS/TEN Fixed drug eruption
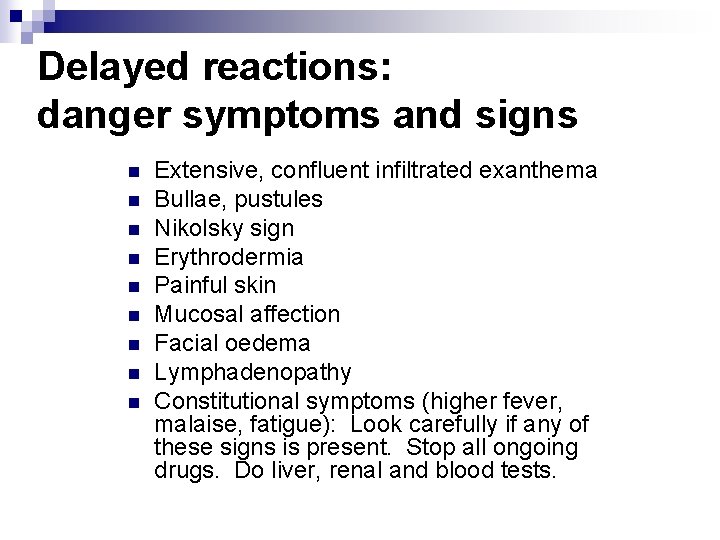
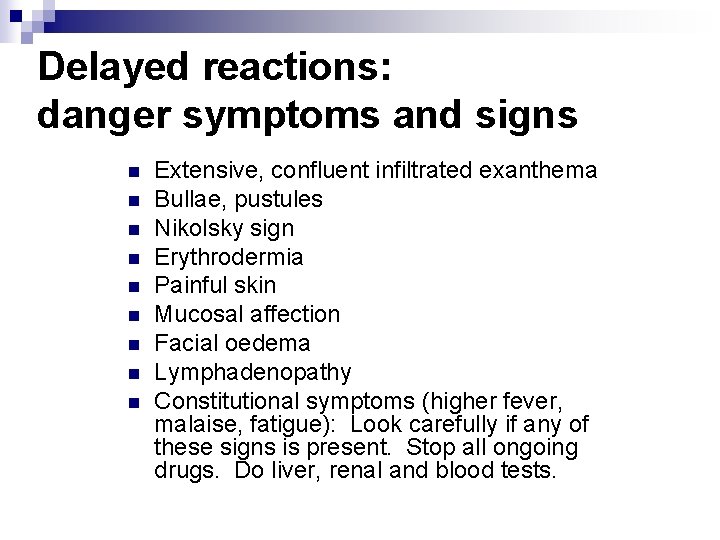
Delayed reactions: danger symptoms and signs n n n n n Extensive, confluent infiltrated exanthema Bullae, pustules Nikolsky sign Erythrodermia Painful skin Mucosal affection Facial oedema Lymphadenopathy Constitutional symptoms (higher fever, malaise, fatigue): Look carefully if any of these signs is present. Stop all ongoing drugs. Do liver, renal and blood tests.
Serious drug allergies Both immediate and delayed reactions may be potentially life-threatening Anaphylaxis (immediate reaction) is not the only life-threatening reaction
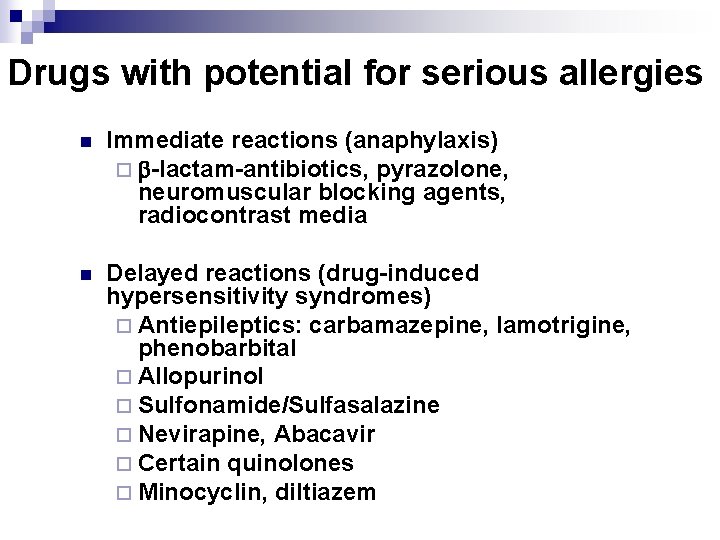
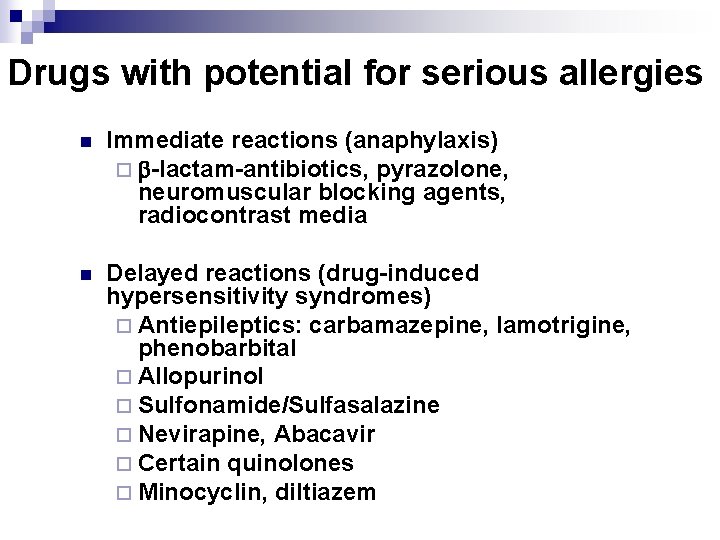
Drugs with potential for serious allergies n Immediate reactions (anaphylaxis) ¨ -lactam-antibiotics, pyrazolone, neuromuscular blocking agents, radiocontrast media n Delayed reactions (drug-induced hypersensitivity syndromes) ¨ Antiepileptics: carbamazepine, lamotrigine, phenobarbital ¨ Allopurinol ¨ Sulfonamide/Sulfasalazine ¨ Nevirapine, Abacavir ¨ Certain quinolones ¨ Minocyclin, diltiazem
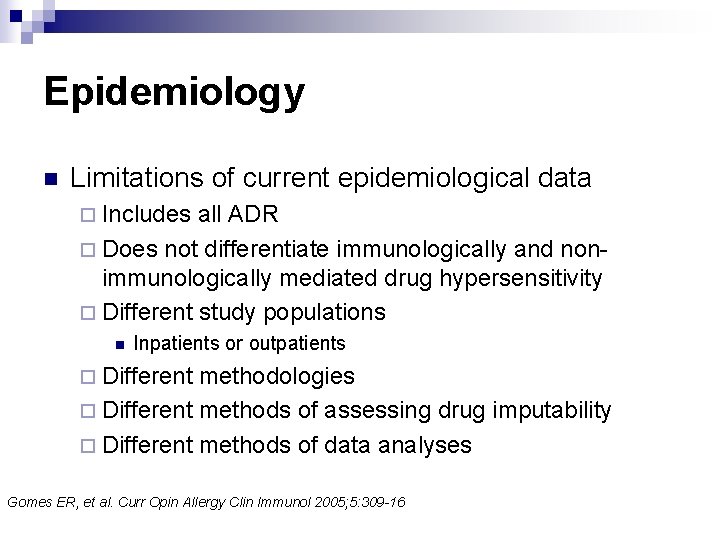
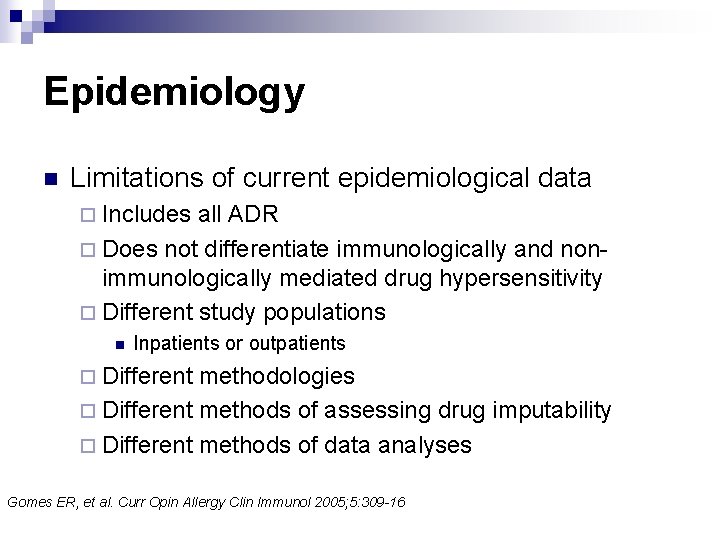
Epidemiology n Limitations of current epidemiological data ¨ Includes all ADR ¨ Does not differentiate immunologically and nonimmunologically mediated drug hypersensitivity ¨ Different study populations n Inpatients or outpatients ¨ Different methodologies ¨ Different methods of assessing drug imputability ¨ Different methods of data analyses Gomes ER, et al. Curr Opin Allergy Clin Immunol 2005; 5: 309 -16
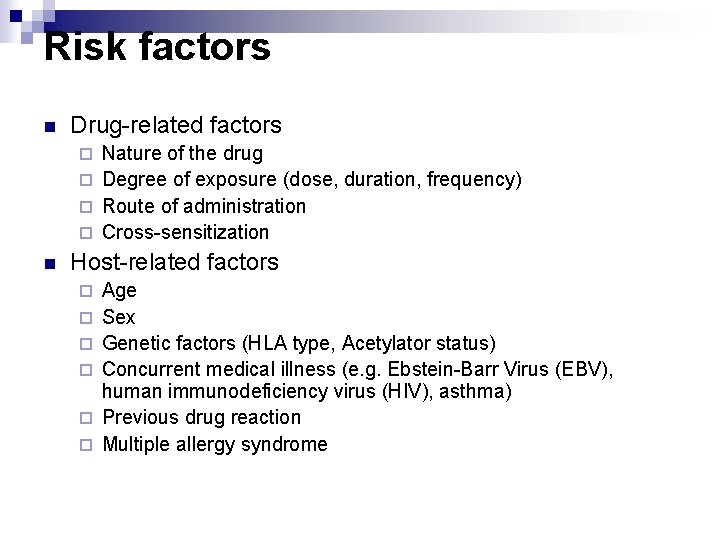
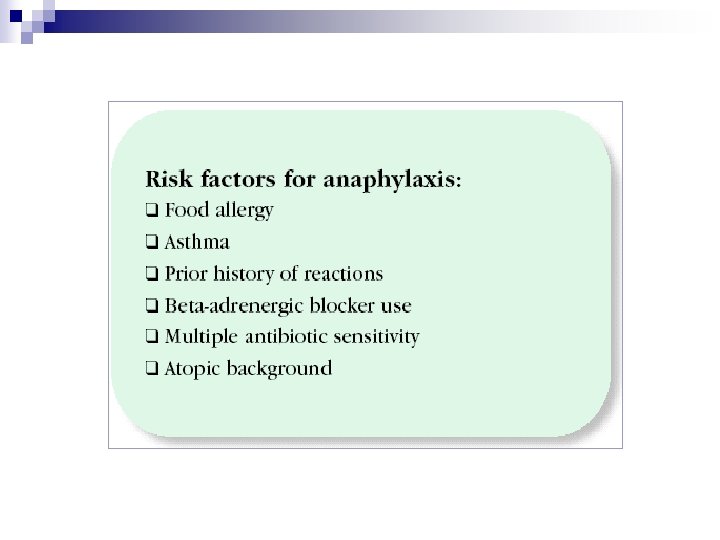
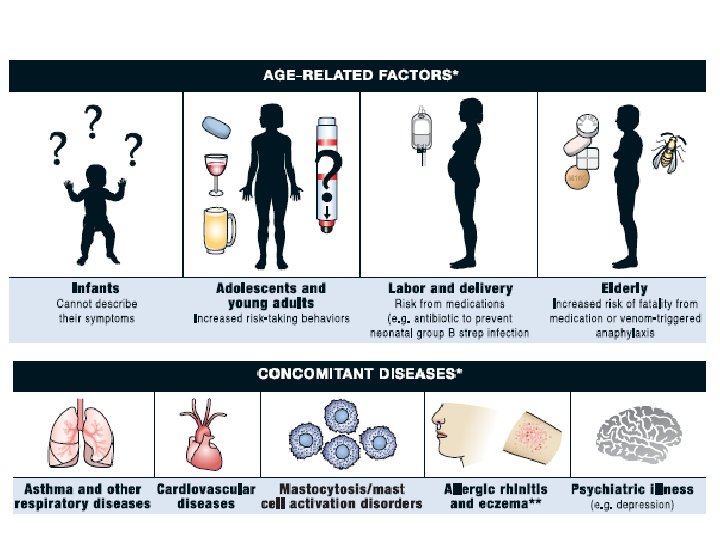
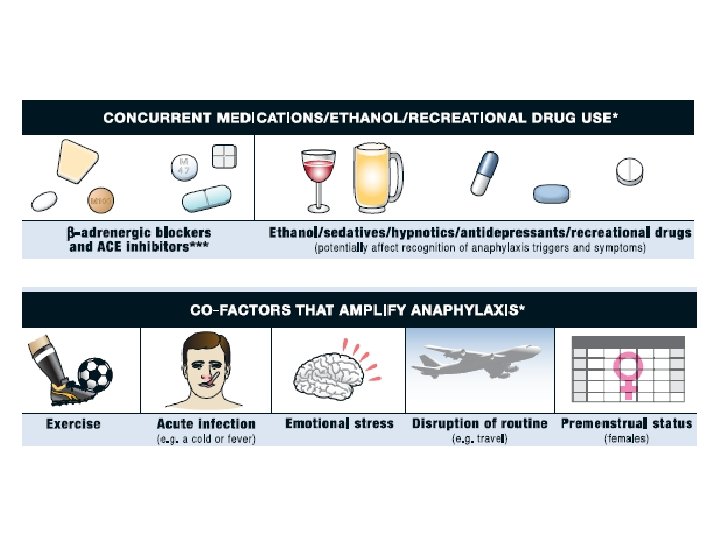
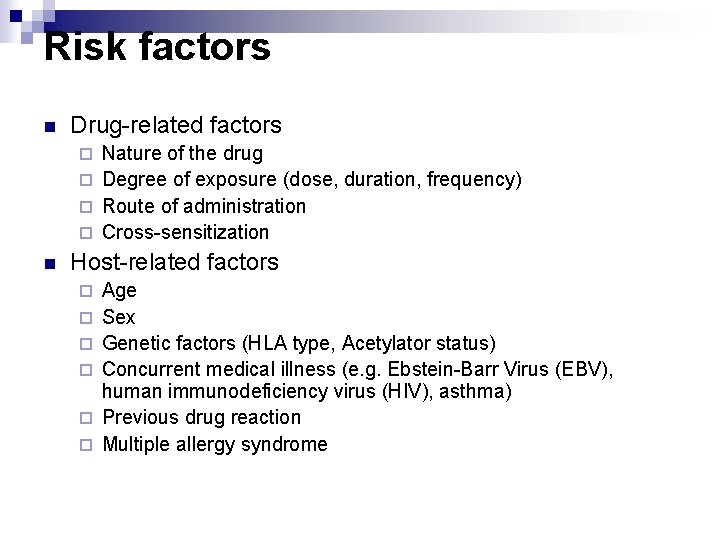
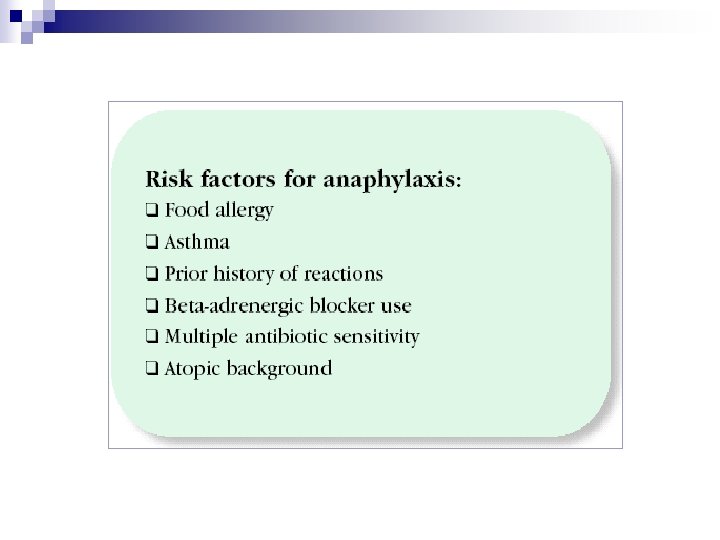
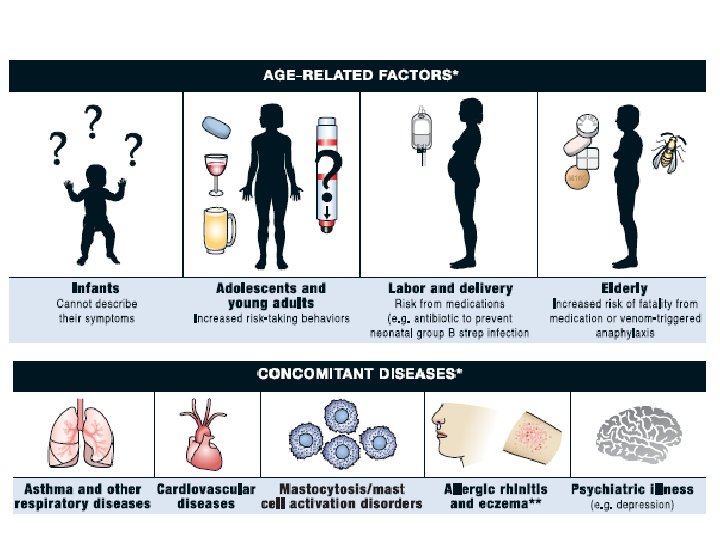
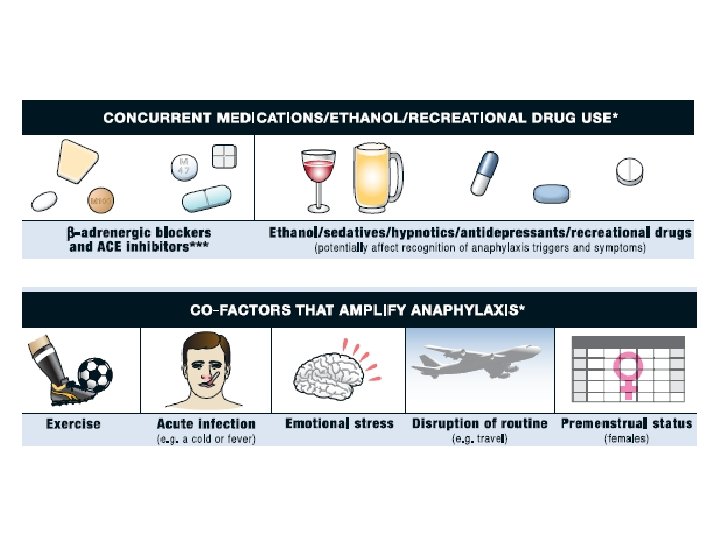
Risk factors n Drug-related factors Nature of the drug ¨ Degree of exposure (dose, duration, frequency) ¨ Route of administration ¨ Cross-sensitization ¨ n Host-related factors ¨ ¨ ¨ Age Sex Genetic factors (HLA type, Acetylator status) Concurrent medical illness (e. g. Ebstein-Barr Virus (EBV), human immunodeficiency virus (HIV), asthma) Previous drug reaction Multiple allergy syndrome
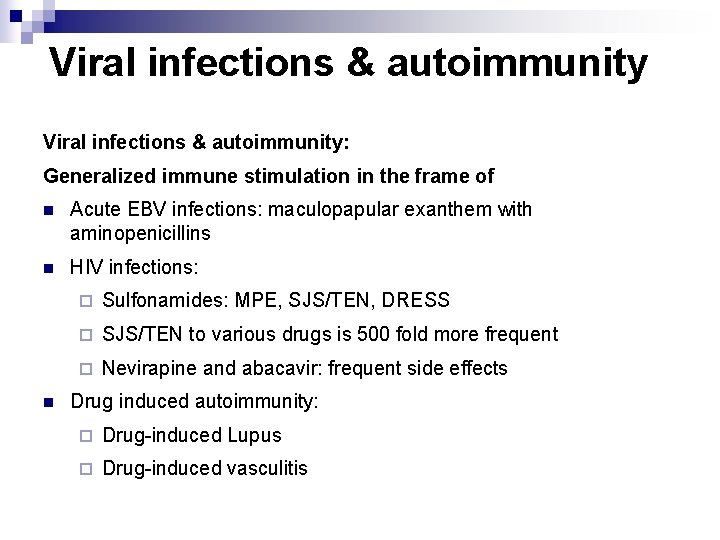
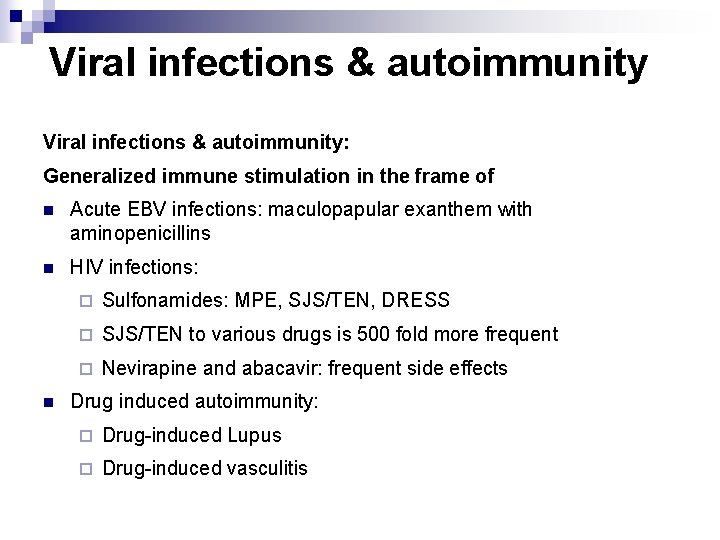
Viral infections & autoimmunity: Generalized immune stimulation in the frame of n Acute EBV infections: maculopapular exanthem with aminopenicillins n HIV infections: n ¨ Sulfonamides: MPE, SJS/TEN, DRESS ¨ SJS/TEN to various drugs is 500 fold more frequent ¨ Nevirapine and abacavir: frequent side effects Drug induced autoimmunity: ¨ Drug-induced Lupus ¨ Drug-induced vasculitis
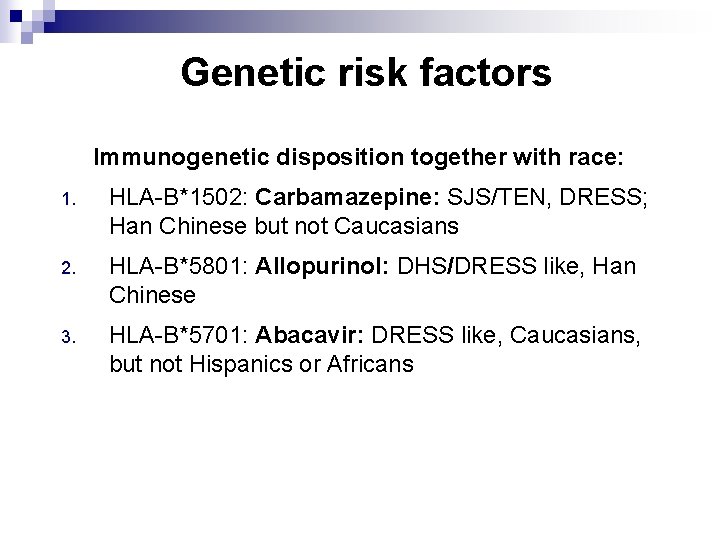
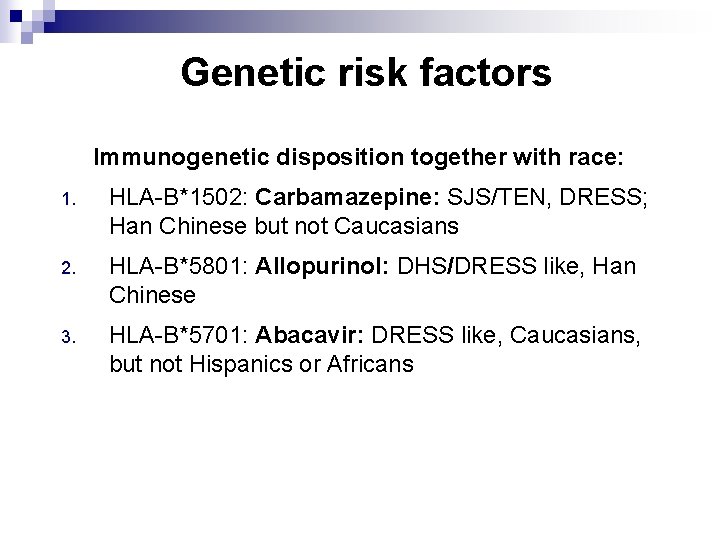
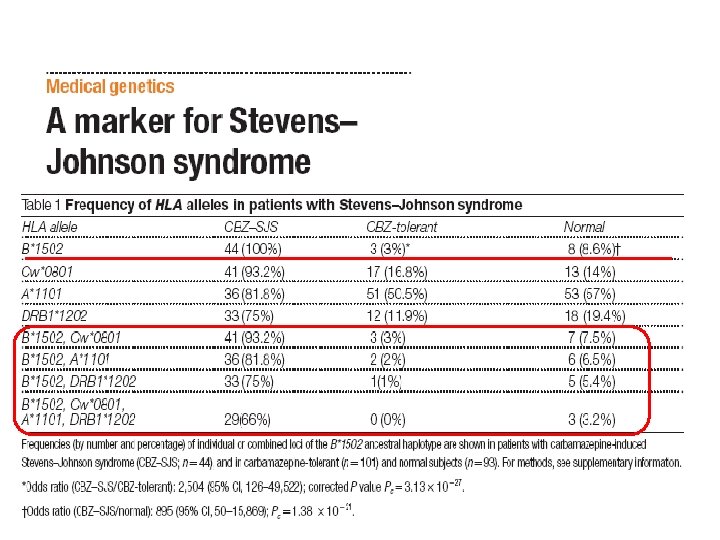
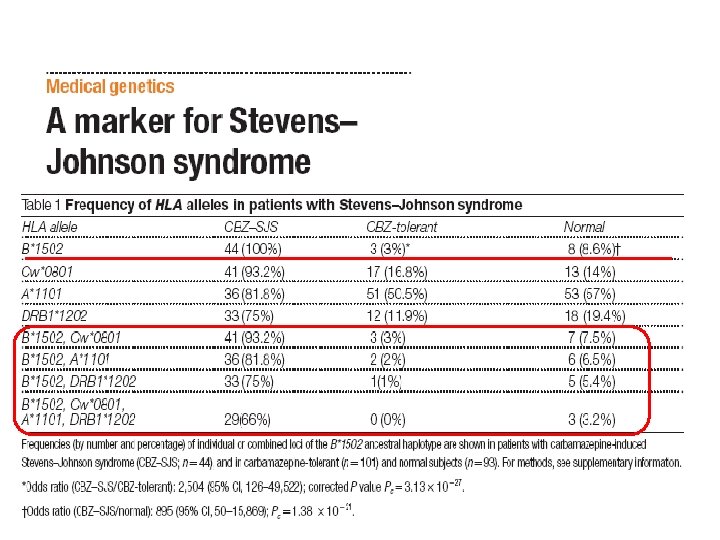
Genetic risk factors Immunogenetic disposition together with race: 1. HLA-B*1502: Carbamazepine: SJS/TEN, DRESS; Han Chinese but not Caucasians 2. HLA-B*5801: Allopurinol: DHS/DRESS like, Han Chinese 3. HLA-B*5701: Abacavir: DRESS like, Caucasians, but not Hispanics or Africans
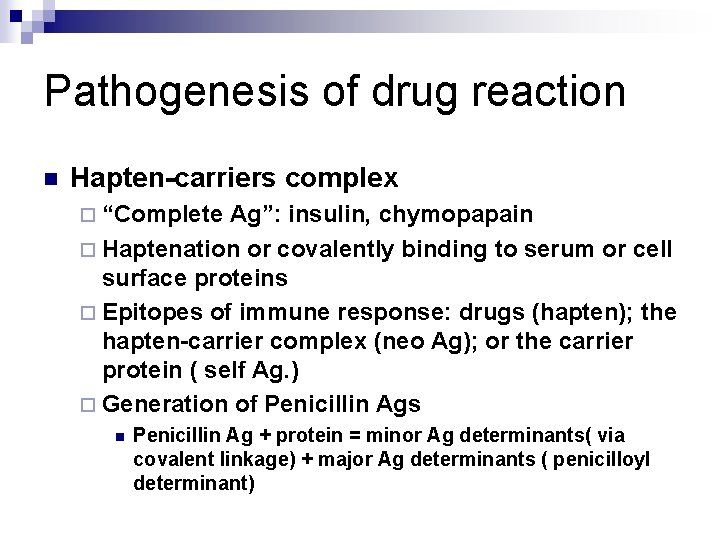
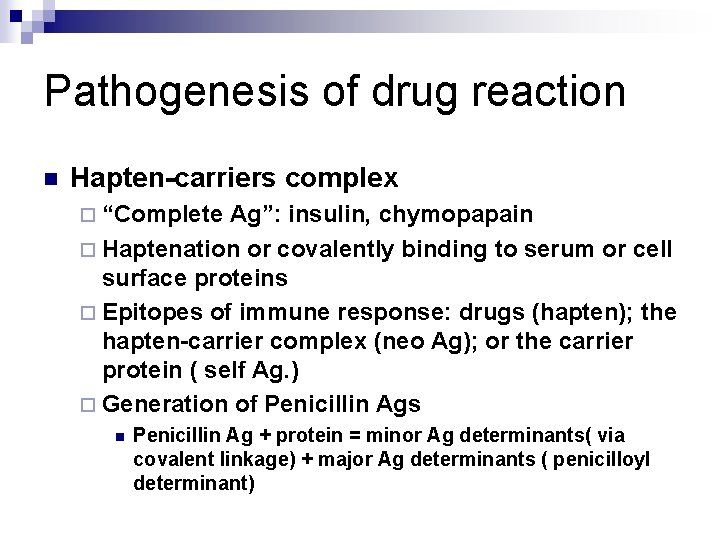
Pathogenesis of drug reaction n Hapten-carriers complex ¨ “Complete Ag”: insulin, chymopapain ¨ Haptenation or covalently binding to serum or cell surface proteins ¨ Epitopes of immune response: drugs (hapten); the hapten-carrier complex (neo Ag); or the carrier protein ( self Ag. ) ¨ Generation of Penicillin Ags n Penicillin Ag + protein = minor Ag determinants( via covalent linkage) + major Ag determinants ( penicilloyl determinant)
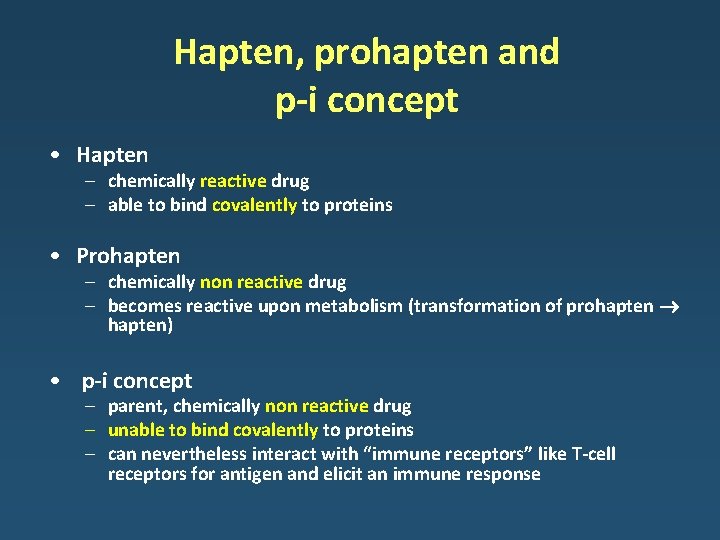
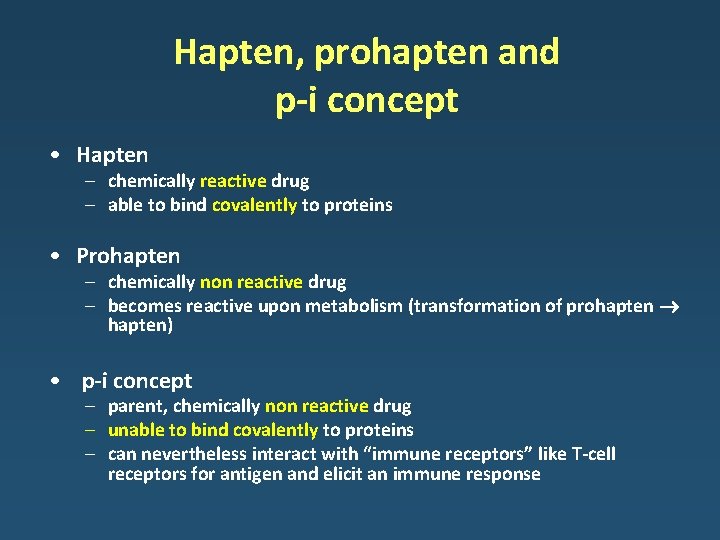
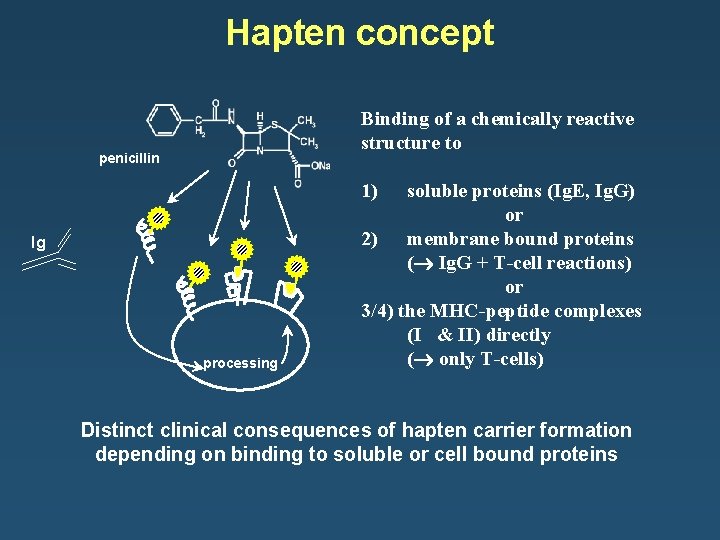
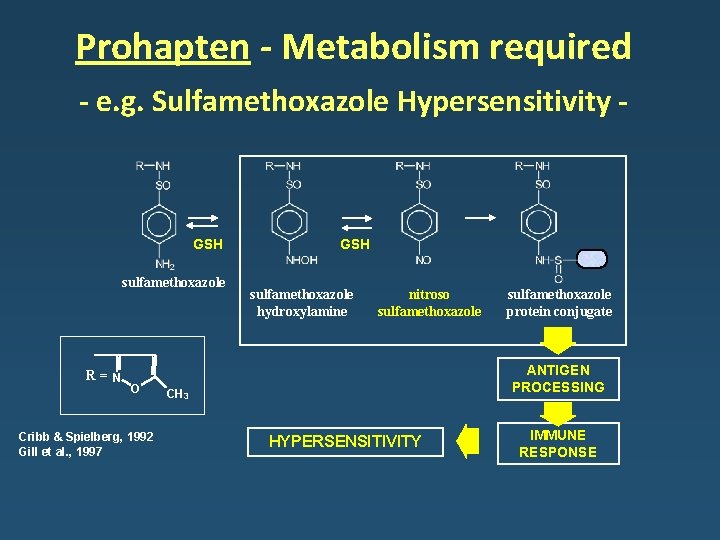
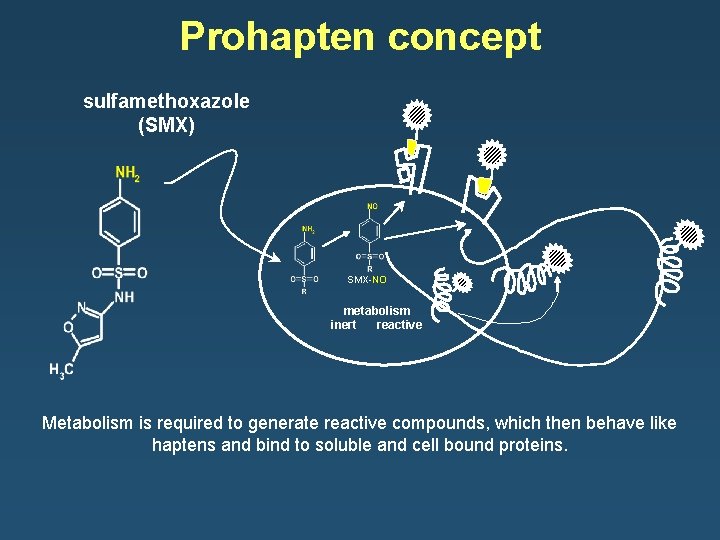
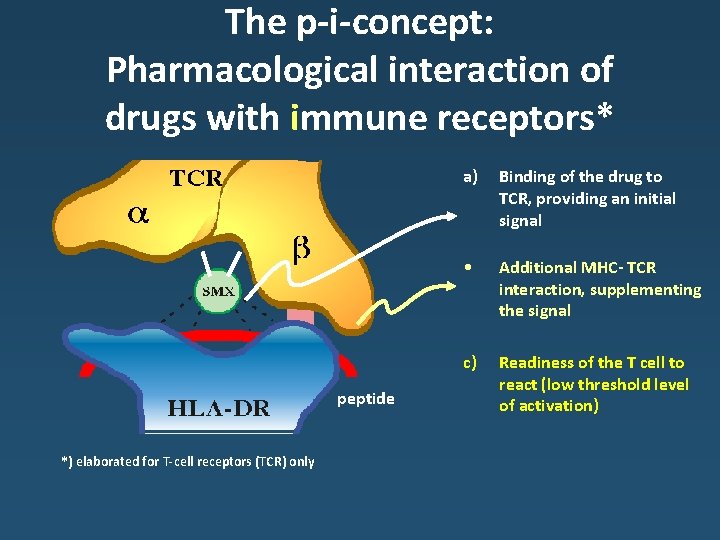
Hapten, prohapten and p-i concept • Hapten – chemically reactive drug – able to bind covalently to proteins • Prohapten – chemically non reactive drug – becomes reactive upon metabolism (transformation of prohapten hapten) • p-i concept – parent, chemically non reactive drug – unable to bind covalently to proteins – can nevertheless interact with “immune receptors” like T-cell receptors for antigen and elicit an immune response
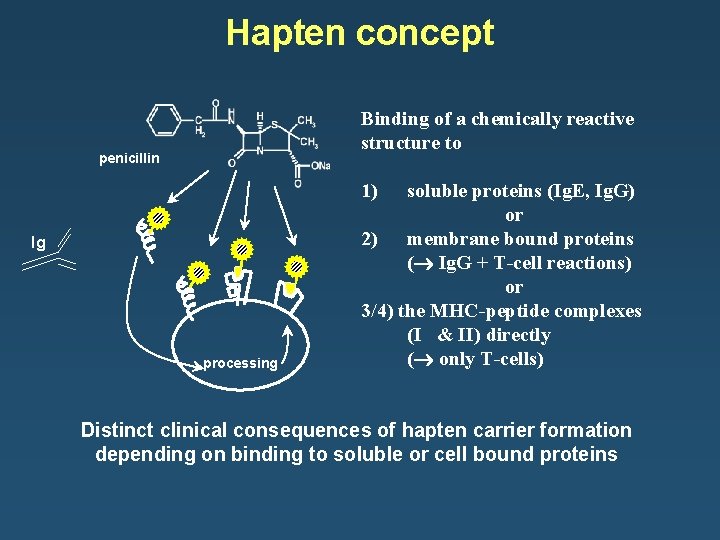
Hapten concept Binding of a chemically reactive structure to penicillin 1) Ig processing soluble proteins (Ig. E, Ig. G) or 2) membrane bound proteins ( Ig. G + T-cell reactions) or 3/4) the MHC-peptide complexes (I & II) directly ( only T-cells) Distinct clinical consequences of hapten carrier formation depending on binding to soluble or cell bound proteins
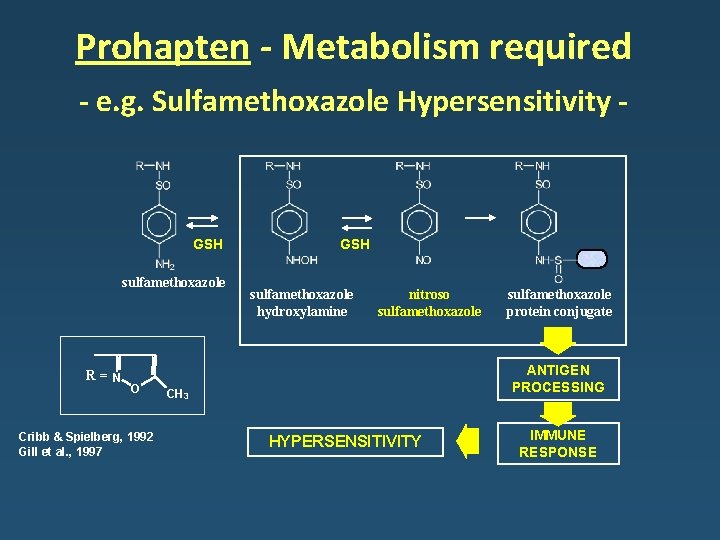
Prohapten - Metabolism required - e. g. Sulfamethoxazole Hypersensitivity - GSH sulfamethoxazole R= N O Cribb & Spielberg, 1992 Gill et al. , 1997 GSH sulfamethoxazole hydroxylamine nitroso sulfamethoxazole protein conjugate ANTIGEN PROCESSING CH 3 HYPERSENSITIVITY IMMUNE RESPONSE
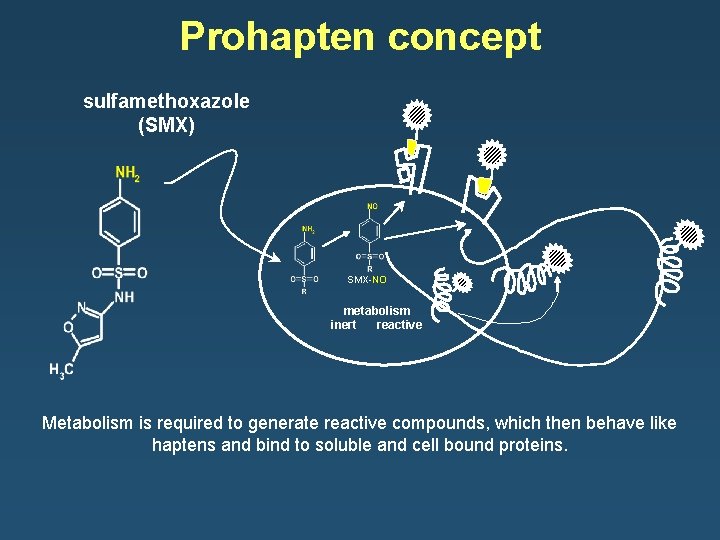
Prohapten concept sulfamethoxazole (SMX) SMX-NO metabolism inert reactive Metabolism is required to generate reactive compounds, which then behave like haptens and bind to soluble and cell bound proteins.
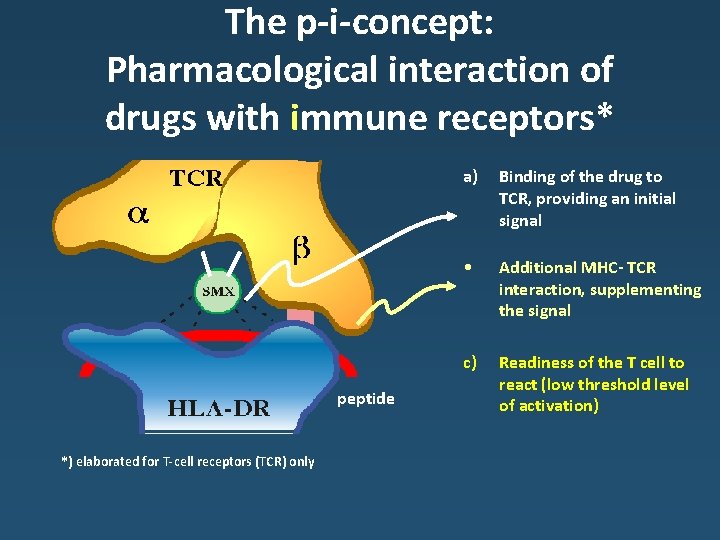
The p-i-concept: Pharmacological interaction of drugs with immune receptors* peptide *) elaborated for T-cell receptors (TCR) only a) Binding of the drug to TCR, providing an initial signal • Additional MHC- TCR interaction, supplementing the signal c) Readiness of the T cell to react (low threshold level of activation)
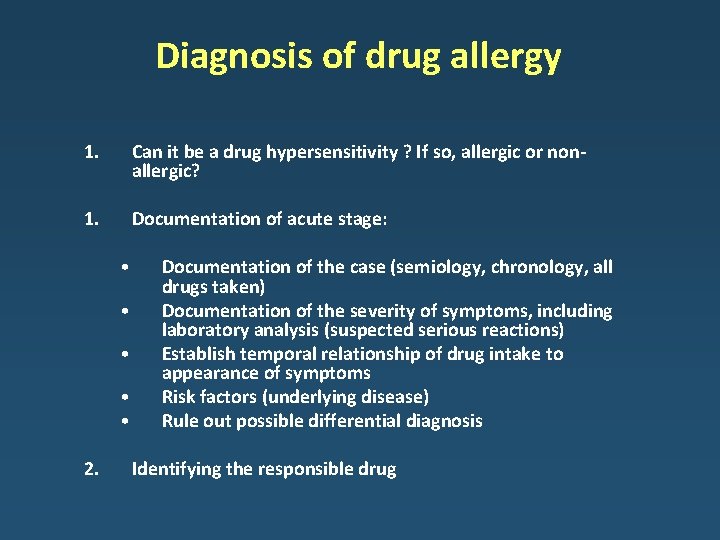
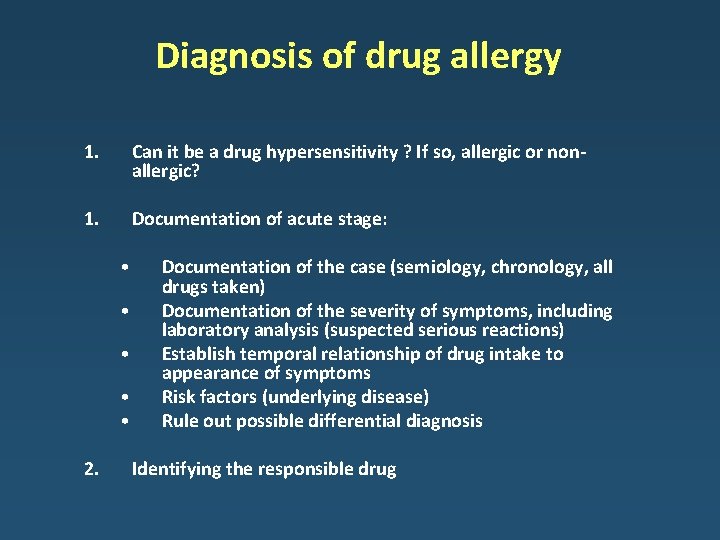
Diagnosis of drug allergy 1. Can it be a drug hypersensitivity ? If so, allergic or nonallergic? 1. Documentation of acute stage: • • • 2. Documentation of the case (semiology, chronology, all drugs taken) Documentation of the severity of symptoms, including laboratory analysis (suspected serious reactions) Establish temporal relationship of drug intake to appearance of symptoms Risk factors (underlying disease) Rule out possible differential diagnosis Identifying the responsible drug
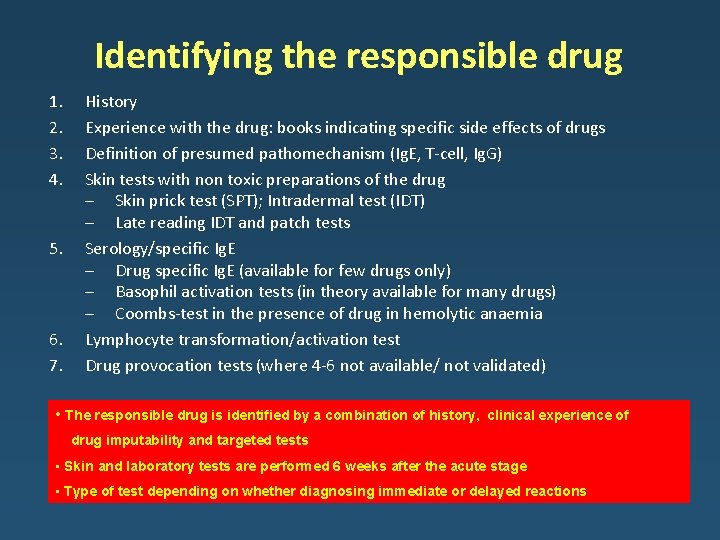
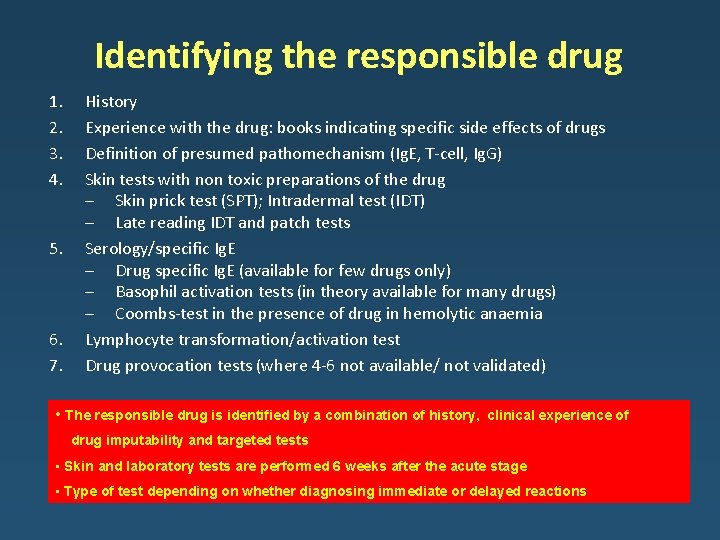
Identifying the responsible drug 1. 2. 3. 4. 5. 6. 7. History Experience with the drug: books indicating specific side effects of drugs Definition of presumed pathomechanism (Ig. E, T-cell, Ig. G) Skin tests with non toxic preparations of the drug – Skin prick test (SPT); Intradermal test (IDT) – Late reading IDT and patch tests Serology/specific Ig. E – Drug specific Ig. E (available for few drugs only) – Basophil activation tests (in theory available for many drugs) – Coombs-test in the presence of drug in hemolytic anaemia Lymphocyte transformation/activation test Drug provocation tests (where 4 -6 not available/ not validated) • The responsible drug is identified by a combination of history, clinical experience of drug imputability and targeted tests • Skin and laboratory tests are performed 6 weeks after the acute stage • Type of test depending on whether diagnosing immediate or delayed reactions
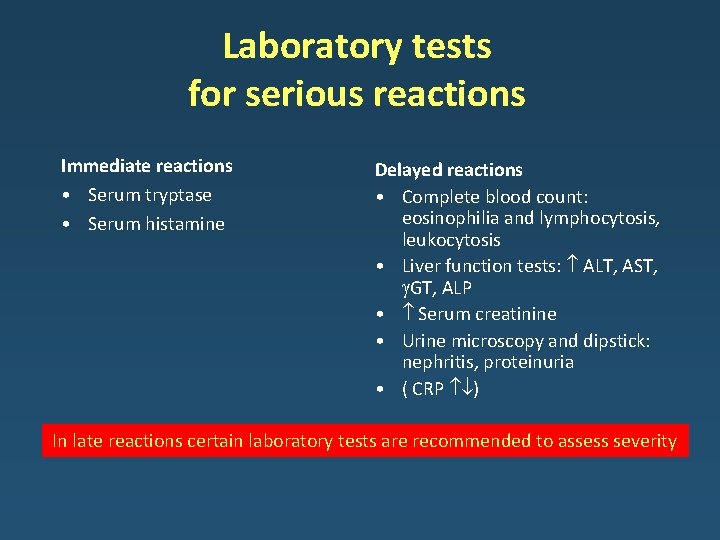
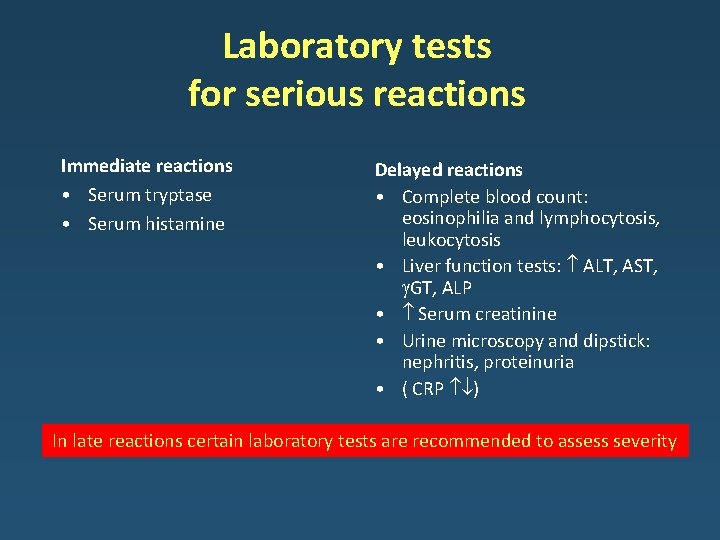
Laboratory tests for serious reactions Immediate reactions • Serum tryptase • Serum histamine Delayed reactions • Complete blood count: eosinophilia and lymphocytosis, leukocytosis • Liver function tests: ALT, AST, GT, ALP • Serum creatinine • Urine microscopy and dipstick: nephritis, proteinuria • ( CRP ) In late reactions certain laboratory tests are recommended to assess severity
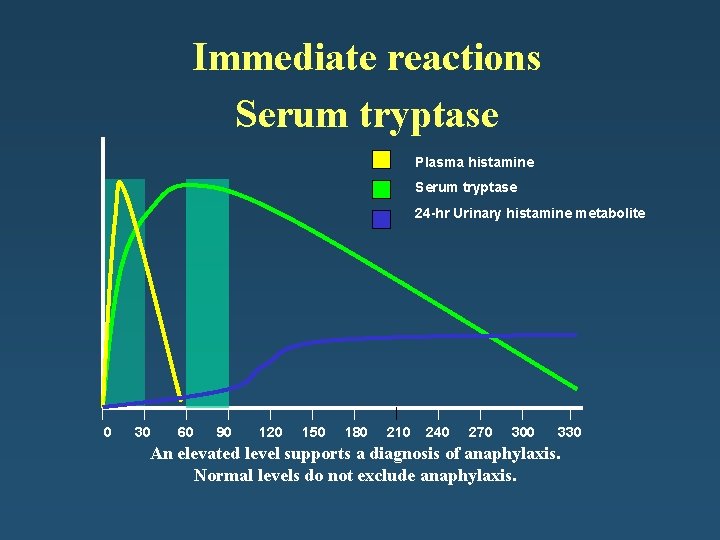
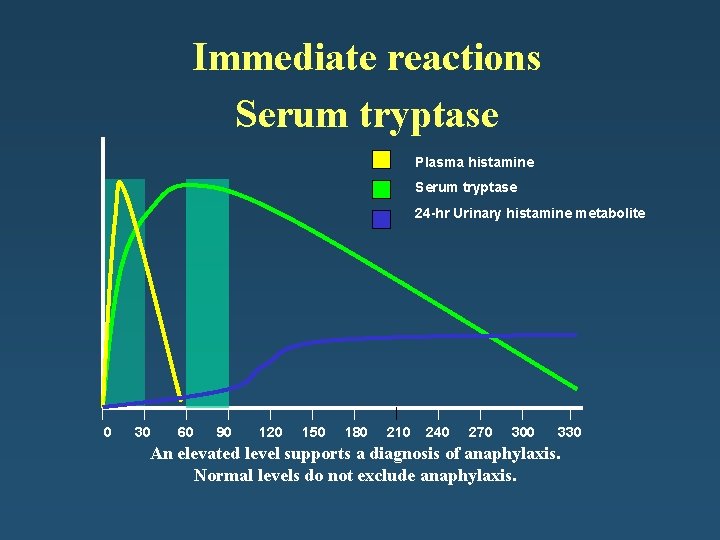
Immediate reactions Serum tryptase Plasma histamine Serum tryptase 24 -hr Urinary histamine metabolite 0 30 60 90 120 150 180 210 240 270 300 330 An elevated level supports a diagnosis of anaphylaxis. Normal levels do not exclude anaphylaxis.
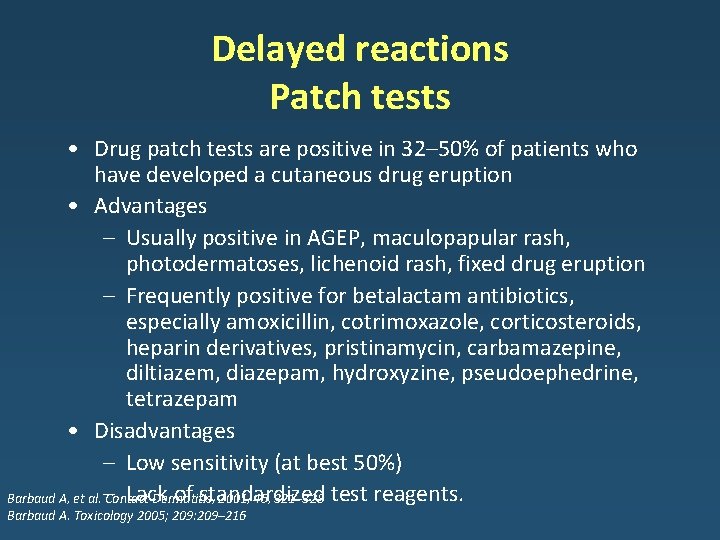
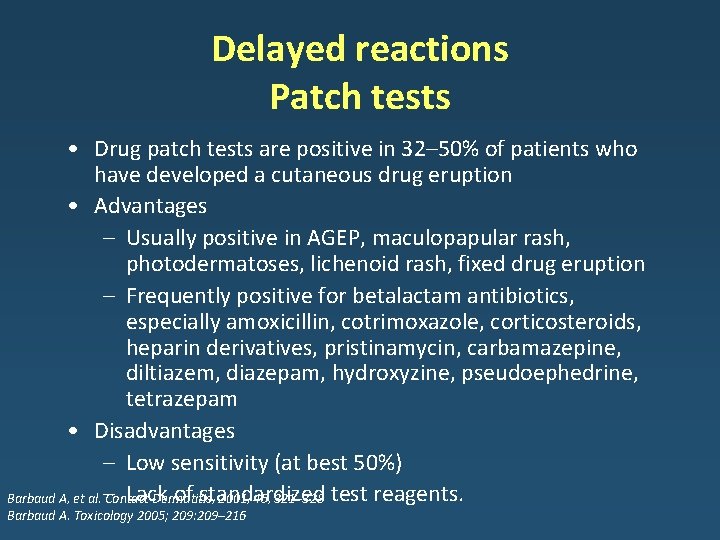
Delayed reactions Patch tests • Drug patch tests are positive in 32– 50% of patients who have developed a cutaneous drug eruption • Advantages – Usually positive in AGEP, maculopapular rash, photodermatoses, lichenoid rash, fixed drug eruption – Frequently positive for betalactam antibiotics, especially amoxicillin, cotrimoxazole, corticosteroids, heparin derivatives, pristinamycin, carbamazepine, diltiazem, diazepam, hydroxyzine, pseudoephedrine, tetrazepam • Disadvantages – Low sensitivity (at best 50%) Lack of standardized Barbaud A, et al. – Contact Dermatitis, 2001, 45, 321– 328 test reagents. Barbaud A. Toxicology 2005; 209: 209– 216
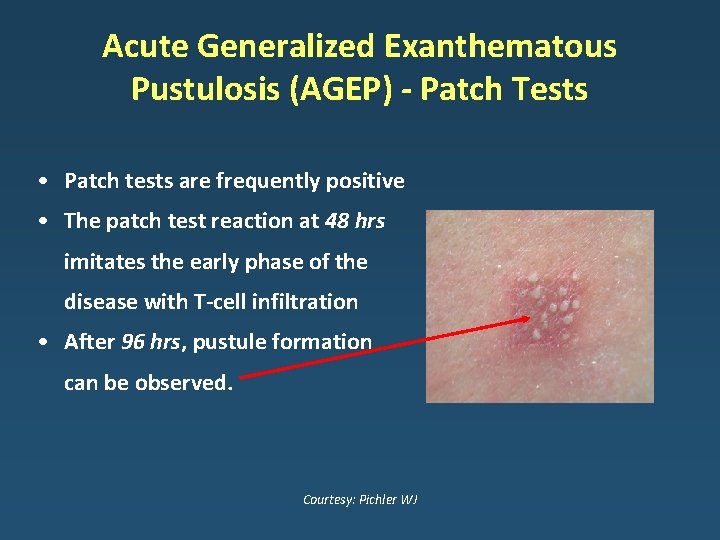
Acute Generalized Exanthematous Pustulosis (AGEP) - Patch Tests • Patch tests are frequently positive • The patch test reaction at 48 hrs imitates the early phase of the disease with T-cell infiltration • After 96 hrs, pustule formation can be observed. Courtesy: Pichler WJ
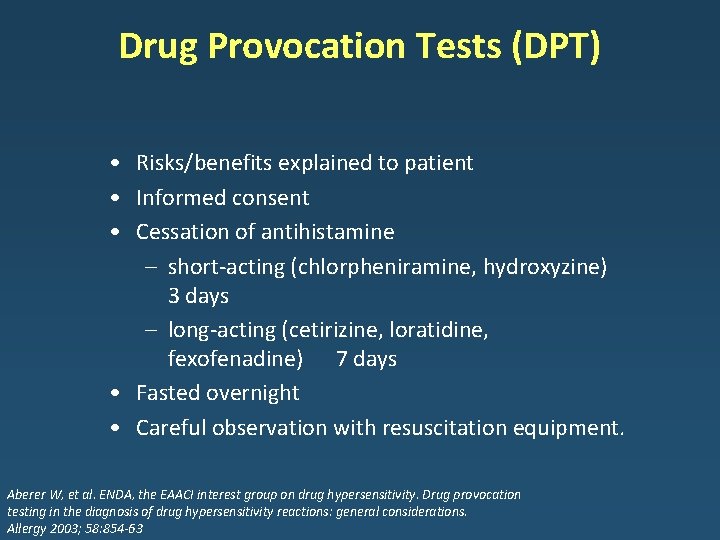
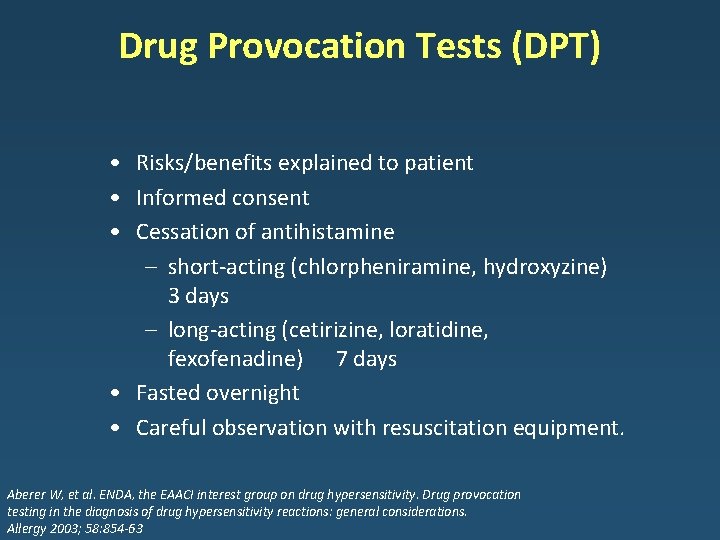
Drug Provocation Tests (DPT) • Risks/benefits explained to patient • Informed consent • Cessation of antihistamine – short-acting (chlorpheniramine, hydroxyzine) 3 days – long-acting (cetirizine, loratidine, fexofenadine) 7 days • Fasted overnight • Careful observation with resuscitation equipment. Aberer W, et al. ENDA, the EAACI interest group on drug hypersensitivity. Drug provocation testing in the diagnosis of drug hypersensitivity reactions: general considerations. Allergy 2003; 58: 854 -63
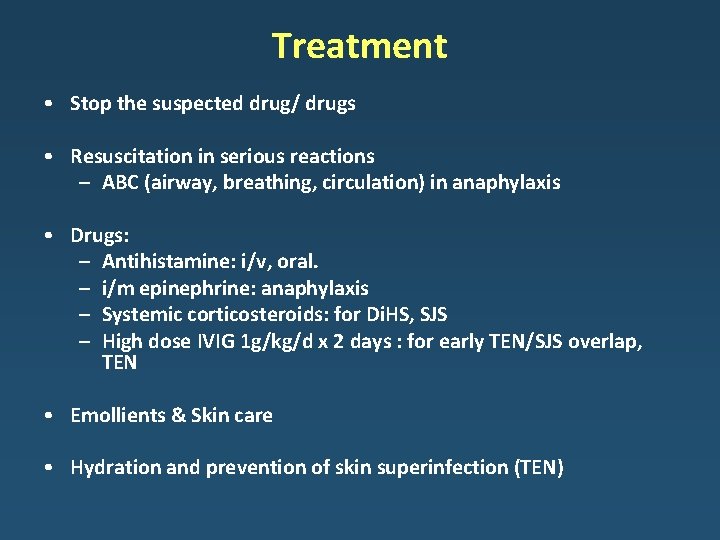
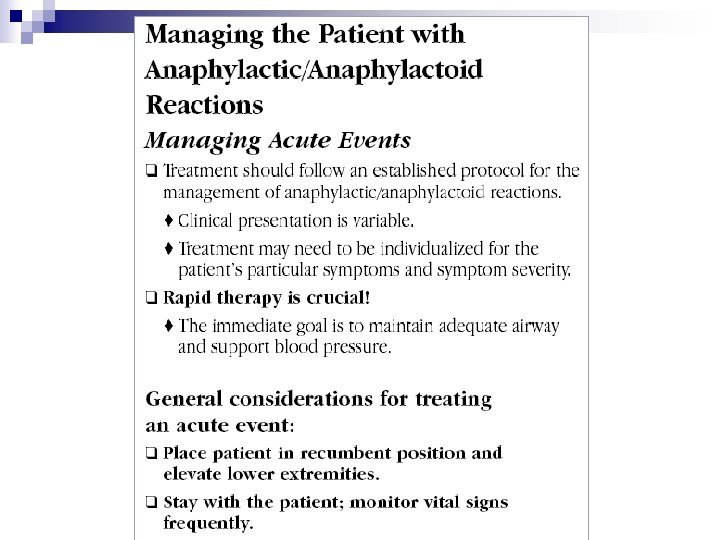
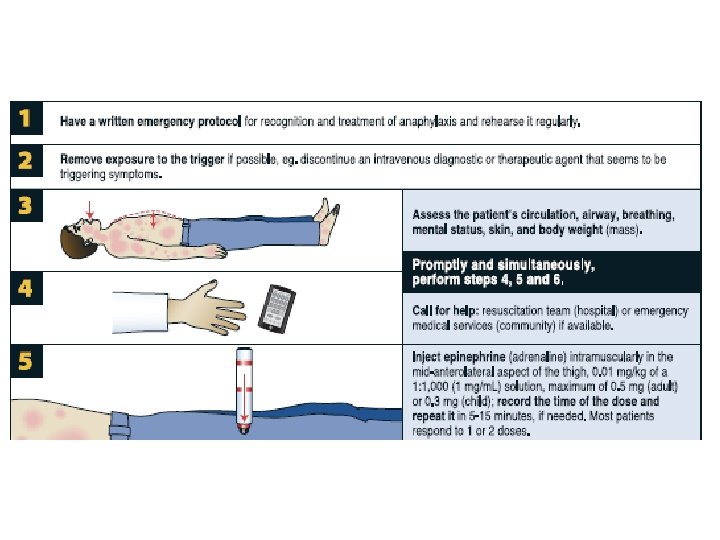
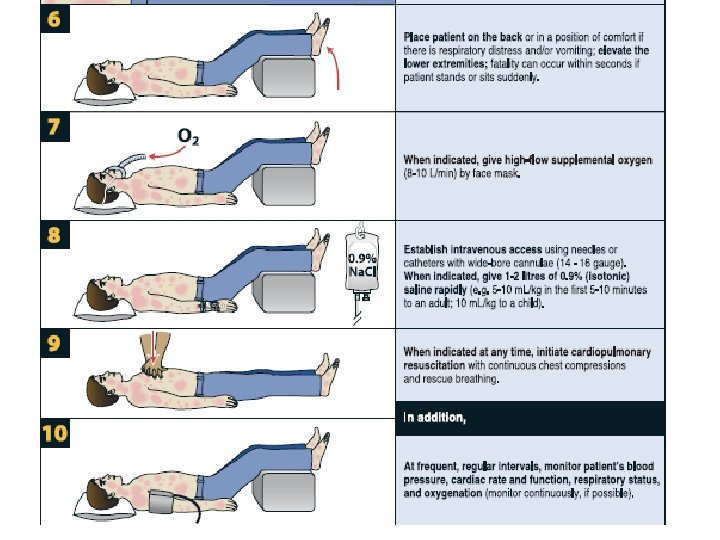
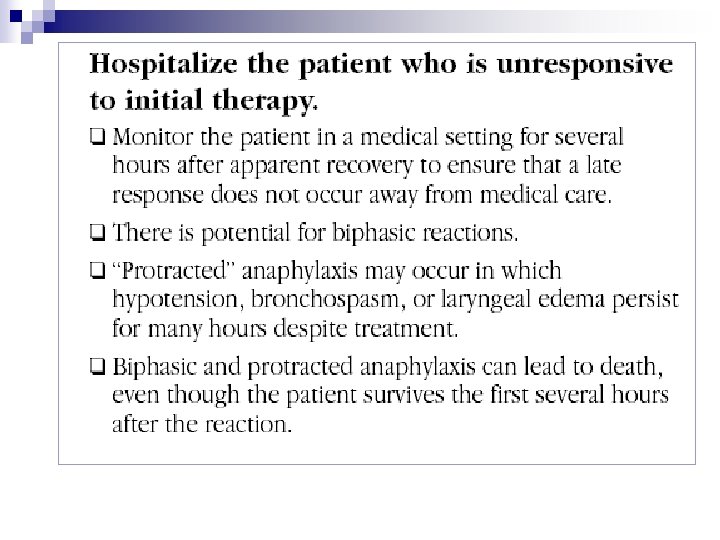
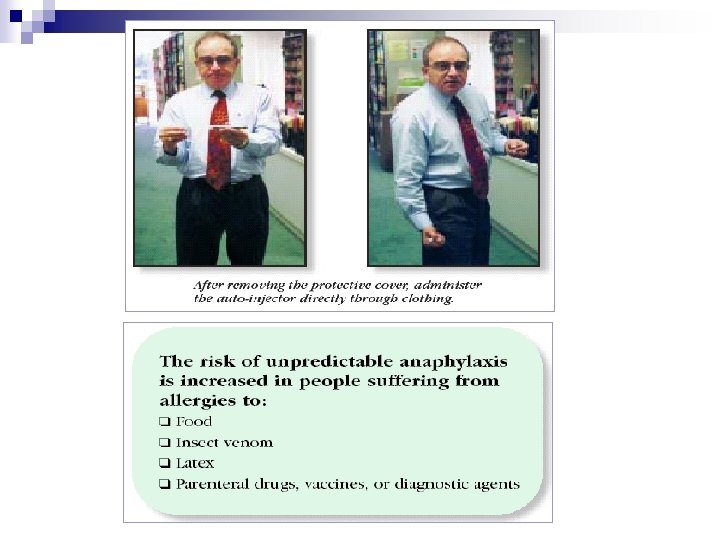
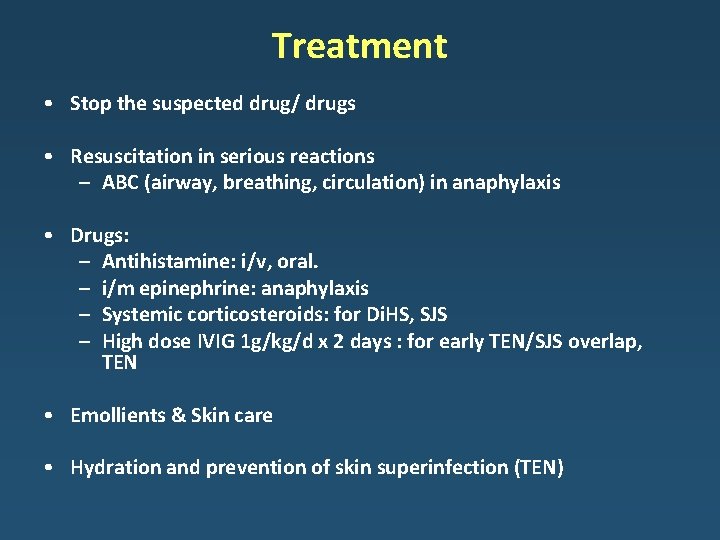
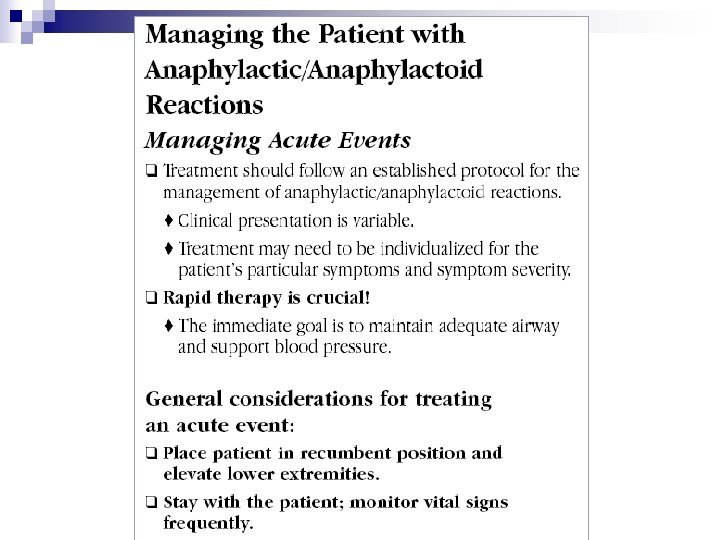
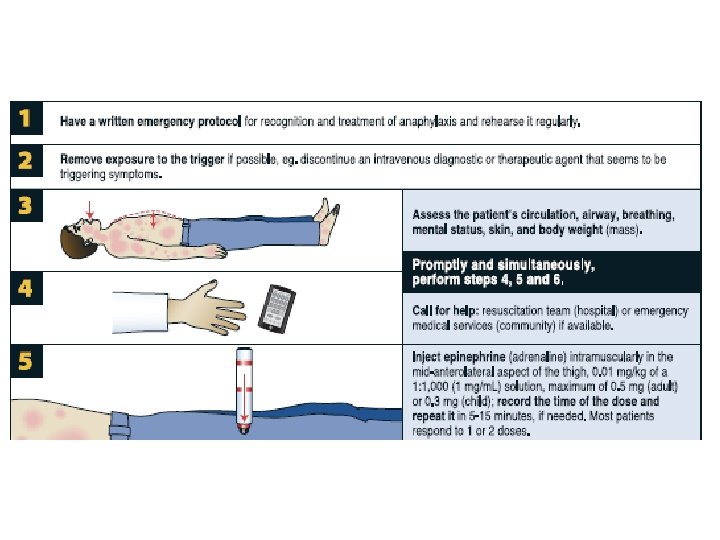
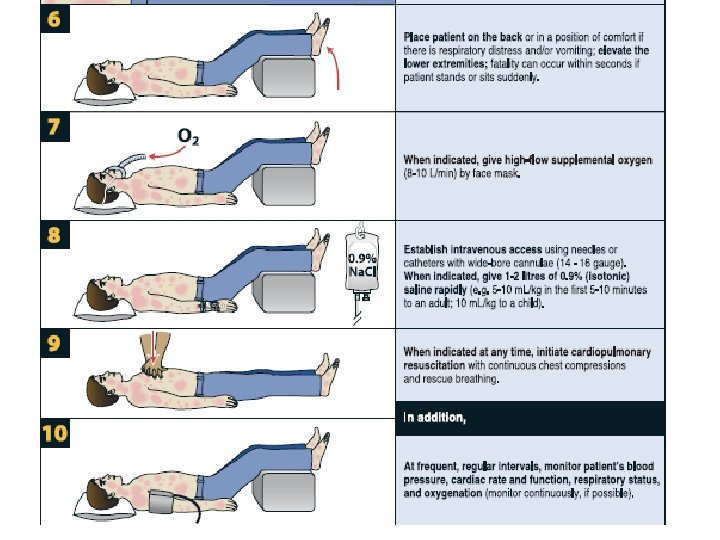
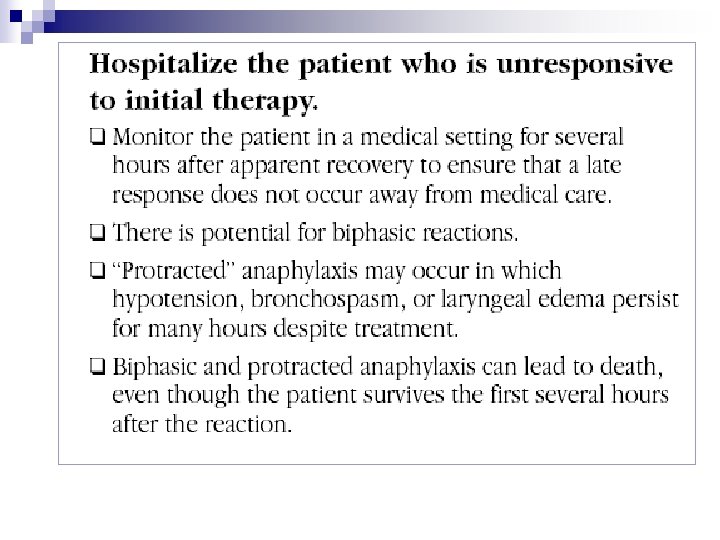
Treatment • Stop the suspected drug/ drugs • Resuscitation in serious reactions – ABC (airway, breathing, circulation) in anaphylaxis • Drugs: – Antihistamine: i/v, oral. – i/m epinephrine: anaphylaxis – Systemic corticosteroids: for Di. HS, SJS – High dose IVIG 1 g/kg/d x 2 days : for early TEN/SJS overlap, TEN • Emollients & Skin care • Hydration and prevention of skin superinfection (TEN)
Treatment • Inpatient: observation, i/v, skin care, allergist referral – Angioedema (oropharyngeal/laryngeal), anaphylaxis – Severe skin: bullous drug eruption, EM/SJS/TEN – Systemic symptoms: fever, lymphadenopathy, organomegaly – possibly > 1 implicated drug • Outpatient – Urticaria/ maculopapular rash – Fixed drug eruption – Drug allergy without systemic symptoms • When to refer to allergist – Uncertain whether the reaction was drug allergy – Uncertain which drug: need for re-evaluation and specific testing – Desensitization
Desensitization • • • Making a patient tolerant to a drug he/she is allergic to When there are no reasonable alternatives Contraindicated: SJS/TEN Not contraindicated: anaphylaxis Patient still considered allergic to the drug Rapid desensitization – immediate hypersensitivity: penicillin G, insulin • Slow desensitization – delayed hypersensitivity: allopurinol, sulphasalazine, TB drugs, SMX
Desensitization • Possible mechanisms (Ig. E-mediated reactions) – Consumption of Ig. E in immune complexes – Hapten inhibition – Mediator depletion from mast cells and basophils – Antigen specific mast cell desensitization • Recent research models – Cross-linking of inhibitory receptors on mast cells – In-vitro desensitization of human mast cells depletes syk, an upstream signal transducing molecule necessary for Ig. E signalling • Mechanism in delayed reactions unknown
Prevention • Patient Education – Potentially cross-reacting drugs – Medic Alert cards/bracelets • Pharmacovigilance – Notify local drug regulatory agencies • Electronic Medical Records