DRCR net Overview DRCR net DRCR net Overview

































- Slides: 59
DRCR. net Overview DRCR. net
DRCR. net Overview Ø The DRCR Network's mission is to improve the lives of individuals with retinal pathology by performing high quality collaborative clinical research that leads to a better understanding of retinal diseases and advances their treatment. The DRCR. net supports the identification, design, and implementation of multicenter clinical research initiatives focused on retinal disorders. Principal emphasis is placed on clinical trials, but epidemiologic outcomes and other research may be supported as well. 2
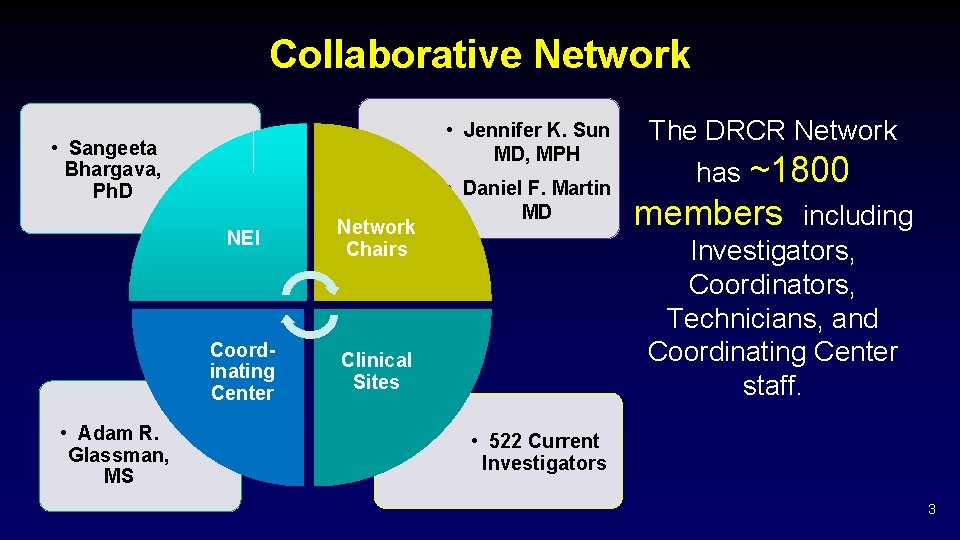
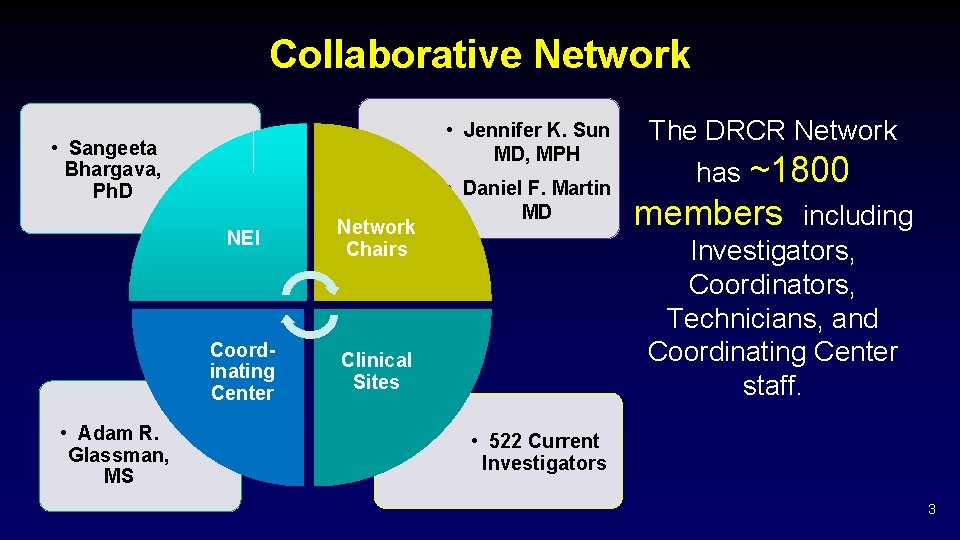
Collaborative Network • Jennifer K. Sun MD, MPH • Sangeeta Bhargava, Ph. D • Adam R. Glassman, MS NEI Network Chairs Coordinating Center Clinical Sites • Daniel F. Martin MD The DRCR Network has ~1800 members including Investigators, Coordinators, Technicians, and Coordinating Center staff. • 522 Current Investigators 3
Funding Ø National Eye Institute (NEI) and The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)sponsored cooperative agreement initiated September 2002. § Current award 2019 -2023 4

Priority Initiatives Ø Involvement of community-based practices, as well as “academic” or university-based centers. Ø Collaborate with industry to facilitate investigations and pursue opportunities otherwise not possible and to do so in a manner consistent with the Network’s dedication to academic integrity and optimal clinical trial performance. 5

DRCR. net Status (as of 2/7/19) Active Total 161 367 109 (68%) 234 (64%) 523 1, 351 1, 261 4, 787 States 37 49 Provinces in Canada 5 6 Sites (Community & Academic Centers) Community Sites Investigators Other Personnel 6

How to Join the Network Ø All retina specialists in the U. S. and Canada are welcome to apply Ø E-mail drcrnet@jaeb. org Ø Your request will be reviewed and if approved the necessary paperwork will be sent to you 7

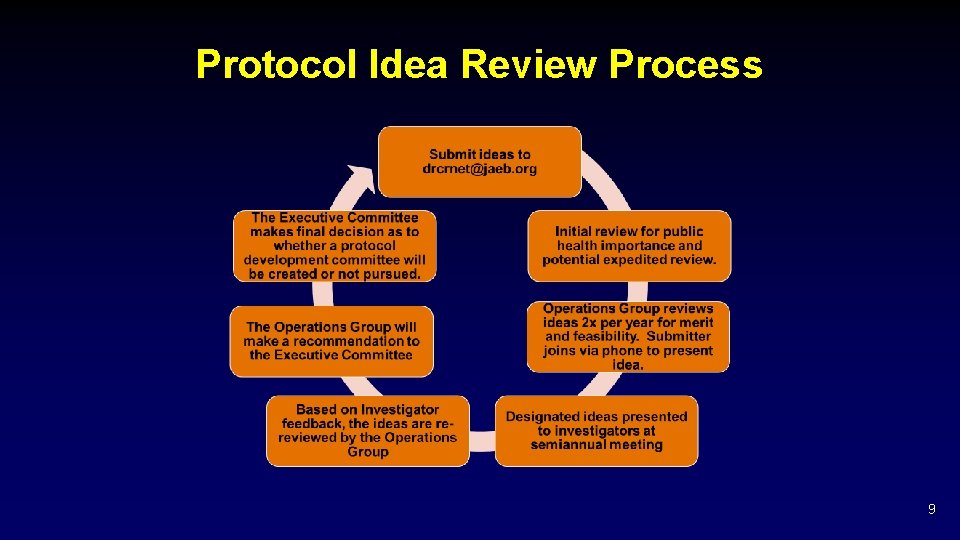
How to Submit a Protocol Idea Ø Go to the public* website: drcr. net Ø Click on Information for Investigators Ø Scroll down to Protocol Idea Form Ø E-mail form to drcrnet@jaeb. org Ø It will be reviewed by the Operations Group every six months * Forms also available on the study website 8
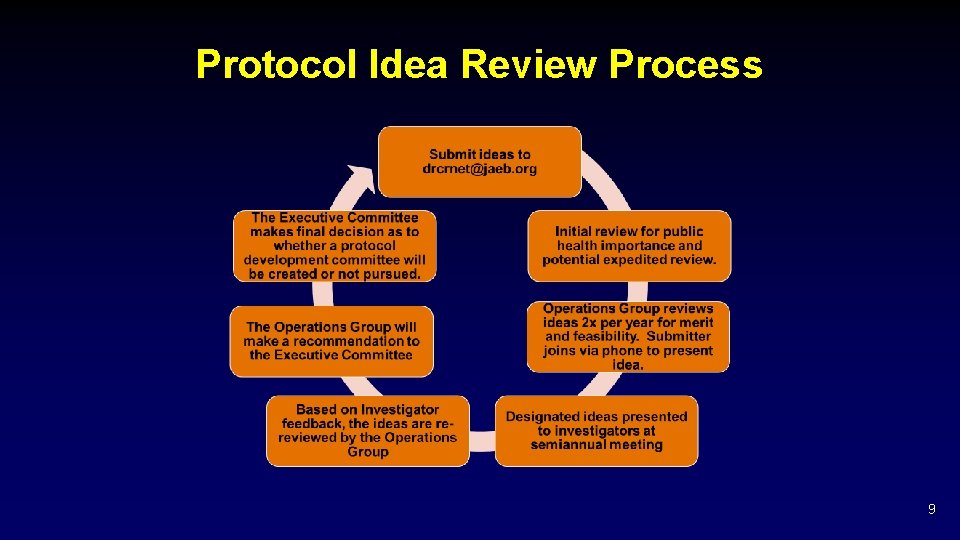
Protocol Idea Review Process 9
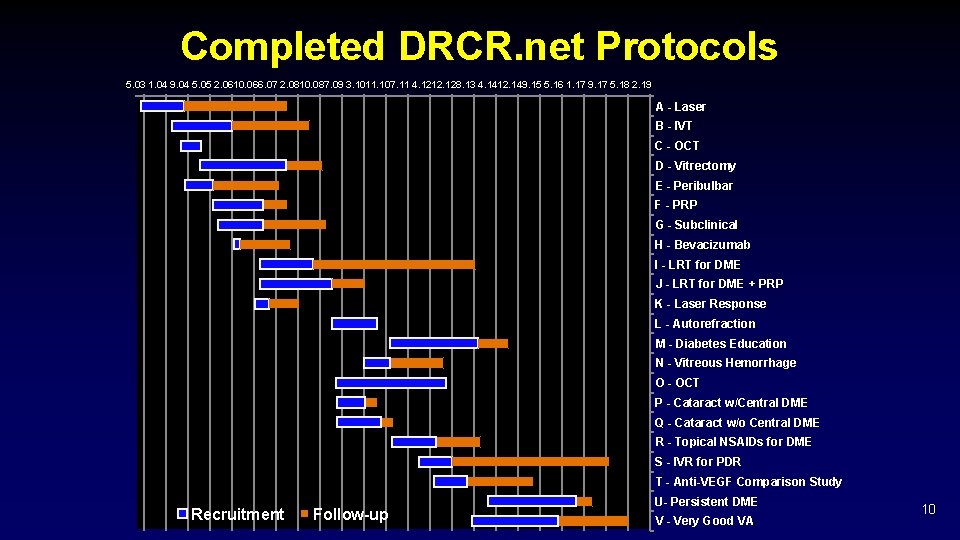
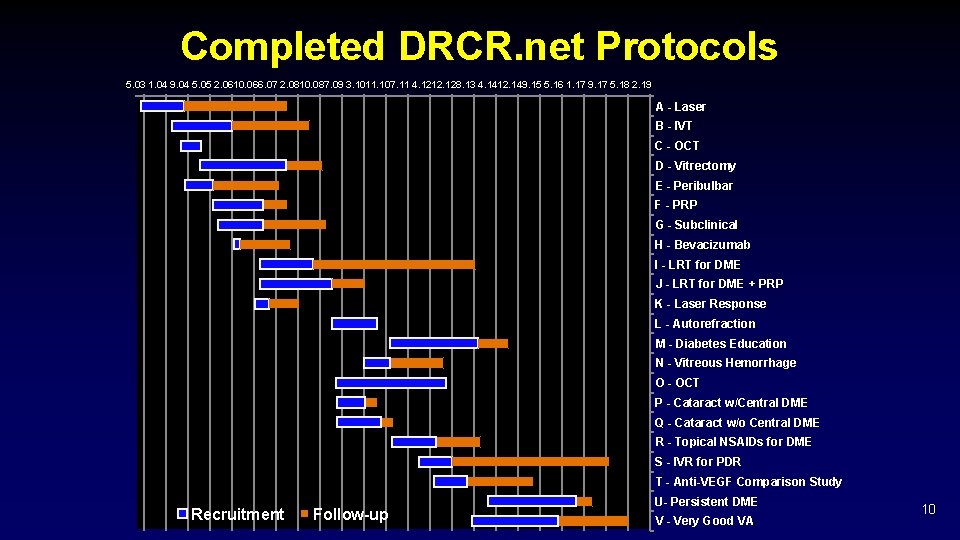
Completed DRCR. net Protocols 5. 03 1. 04 9. 04 5. 05 2. 0610. 066. 07 2. 0810. 087. 09 3. 1011. 107. 11 4. 1212. 128. 13 4. 1412. 149. 15 5. 16 1. 17 9. 17 5. 18 2. 19 A - Laser B - IVT C - OCT D - Vitrectomy E - Peribulbar F - PRP G - Subclinical H - Bevacizumab I - LRT for DME J - LRT for DME + PRP K - Laser Response L - Autorefraction M - Diabetes Education N - Vitreous Hemorrhage O - OCT P - Cataract w/Central DME Q - Cataract w/o Central DME R - Topical NSAIDs for DME S - IVR for PDR T - Anti-VEGF Comparison Study Recruitment Follow-up U- Persistent DME V - Very Good VA 10

DRCR. net Protocols Enrolling or in Follow-up 2. 12 7. 12 12. 12 5. 13 10. 13 3. 14 7. 14 12. 14 5. 15 10. 15 3. 16 8. 16 1. 17 6. 17 11. 17 4. 18 9. 18 2. 19 AA - Ultra-widefield Imaging W - PDR/DME Prevention AB - Vx for VH from PDR AC- Initial A vs B AG- Gas for VMT Recruitment Followup AH - Gas for MH Genetics Over 10, 500 DRCR. net Participants to Date 11
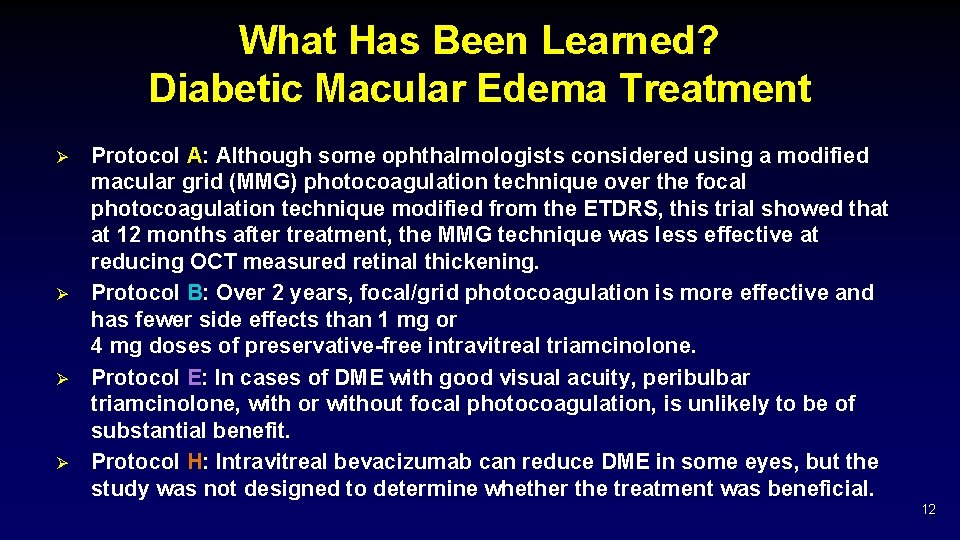
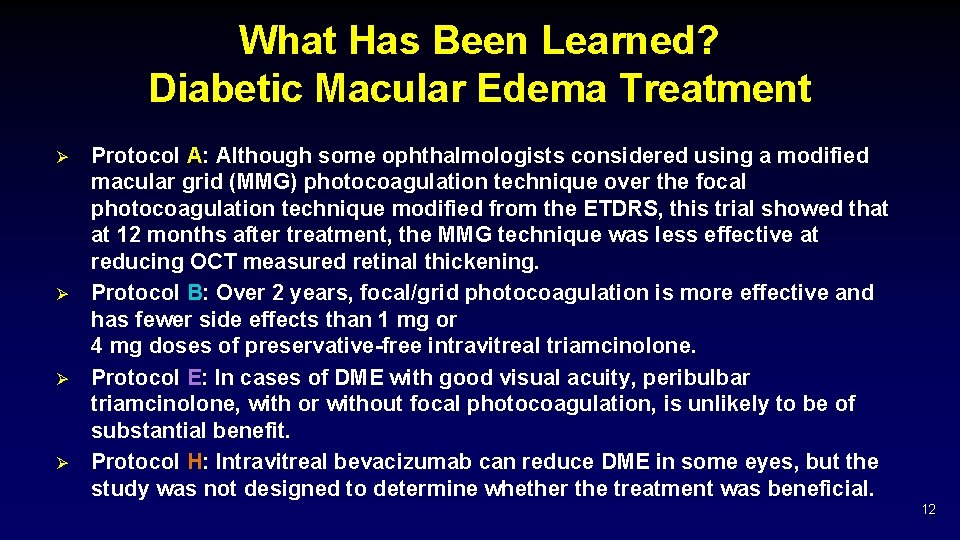
What Has Been Learned? Diabetic Macular Edema Treatment Ø Ø Protocol A: Although some ophthalmologists considered using a modified macular grid (MMG) photocoagulation technique over the focal photocoagulation technique modified from the ETDRS, this trial showed that at 12 months after treatment, the MMG technique was less effective at reducing OCT measured retinal thickening. Protocol B: Over 2 years, focal/grid photocoagulation is more effective and has fewer side effects than 1 mg or 4 mg doses of preservative-free intravitreal triamcinolone. Protocol E: In cases of DME with good visual acuity, peribulbar triamcinolone, with or without focal photocoagulation, is unlikely to be of substantial benefit. Protocol H: Intravitreal bevacizumab can reduce DME in some eyes, but the study was not designed to determine whether the treatment was beneficial. 12

What Has Been Learned? Diabetic Macular Edema Treatment Ø Protocol I: Intravitreal ranibizumab with prompt or deferred (≥ 24 weeks) focal/grid laser is more effective through 2 years in increasing visual acuity compared with focal/grid laser treatment alone for the treatment of DME involving the central macula. § Ø Focal/grid laser treatment at the initiation of intravitreal ranibizumab is no better, and possibly worse, for vision outcomes than adding laser treatment only if needed after 24 weeks or more of anti-VEGF treatment in eyes with DME involving the fovea and with vision impairment. Protocol K: Sixteen weeks after focal/grid laser for DME in eyes with a definite reduction, but not resolution, of central edema, 23% to 63% likely will continue to improve without additional treatment. 13

What Has Been Learned? Diabetic Macular Edema Treatment Ø Protocol R: At 1 year in eyes with non-central DME, this study could not identify a difference between topical nepafenac 0. 1% and placebo on OCT parameters or visual acuity. Ø Protocol T*: The 2 -year clinical trial compared 3 drugs for diabetic macular edema (DME) and found that gains in vision were greater for participants receiving the drug aflibercept than for those receiving bevacizumab, but only among participants starting treatment with 20/50 or worse vision. At one year aflibercept had superior gains to ranibizumab in this vision subgroup, however a difference could not be identified at 2 years. The 3 drugs yielded similar gains in vision for patients with 20/32 or 20/40 vision at the start of treatment. 14

What Has Been Learned? Diabetic Macular Edema Treatment Ø Protocol U: Although its use is more likely to reduce retinal thickness and increase intraocular pressure, the addition of intravitreous dexamethasone to continued ranibizumab therapy does not improve visual acuity at 24 weeks more than continued ranibizumab therapy alone among eyes with persistent DME following anti-VEGF therapy. 15

What Has Been Learned? Diabetic Retinopathy Treatment Ø Protocol F: Results suggest clinically meaningful differences are unlikely in OCT thickness or visual acuity following application of PRP in 1 sitting compared with 4 sittings. Ø Protocol J: The addition of 1 intravitreal triamcinolone injection or 2 intravitreal ranibizumab injections in eyes receiving focal/grid laser for DME and PRP is associated with better visual acuity and decreased macular edema by 14 weeks. Whether continued long-term intravitreal treatment is beneficial could not be determined from this study. 16
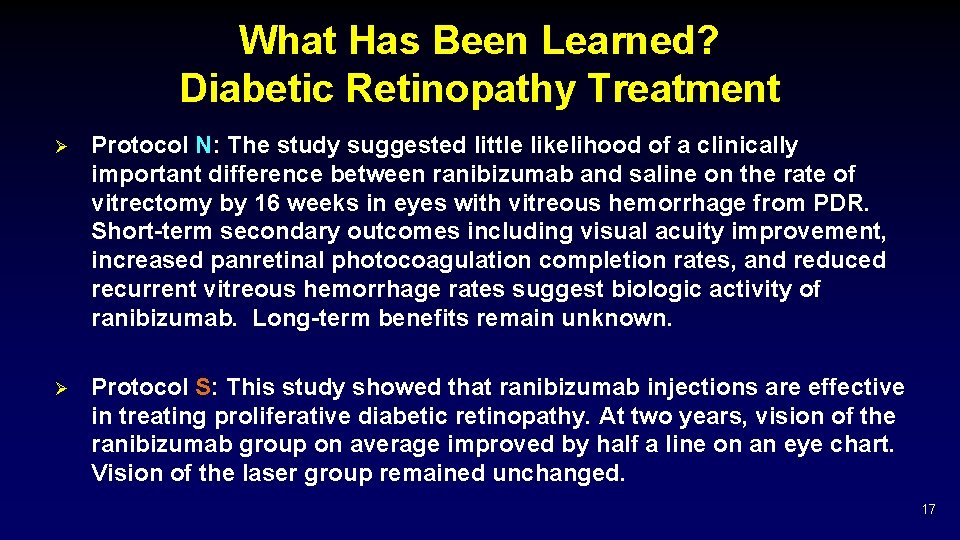
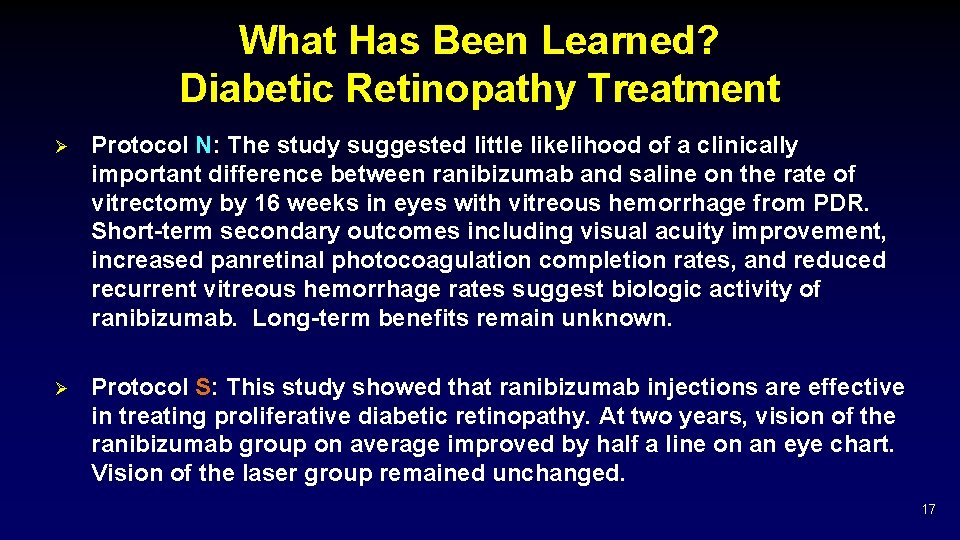
What Has Been Learned? Diabetic Retinopathy Treatment Ø Protocol N: The study suggested little likelihood of a clinically important difference between ranibizumab and saline on the rate of vitrectomy by 16 weeks in eyes with vitreous hemorrhage from PDR. Short-term secondary outcomes including visual acuity improvement, increased panretinal photocoagulation completion rates, and reduced recurrent vitreous hemorrhage rates suggest biologic activity of ranibizumab. Long-term benefits remain unknown. Ø Protocol S: This study showed that ranibizumab injections are effective in treating proliferative diabetic retinopathy. At two years, vision of the ranibizumab group on average improved by half a line on an eye chart. Vision of the laser group remained unchanged. 17

What Has Been Learned? OCT and Retinal Thickening Ø Ø Ø Protocol C: Although on average there are slight decreases in retinal thickening during the day, most eyes with diabetic macular edema have little meaningful change in OCT central subfield thickening or visual acuity between 8 AM and 4 PM. Protocol C: Reproducibility of retinal thickness in DME was better for central subfield thickness measurements than for center point measurements. A change in central subfield thickness exceeding 11% is likely to be real. Protocol G: While subclinical DME may be uncommon, this study suggests that between approximately one-quarter and one-half of eyes with subclinical DME will progress to more definite thickening or be judged to need treatment for DME within 2 years after its identification. 18

What Has Been Learned? Optical Coherence Tomography Ø Ø Protocol G: CST (central subfield thickness) on Stratus OCT™ in people with diabetes and minimal or no retinopathy are similar to thicknesses reported from a normative database of people without diabetes. CST is greater in men than in women. Studies involving comparisons of retinal thickness to expected norms should consider different mean values for women and men. Protocol O: Mean CST is ~70 µm thicker when measured with Heidelberg Spectralis OCT as compared with Stratus OCT among individuals with diabetes in the absence of retinopathy or with minimal non-proliferative retinopathy and a normal macular architecture. CST values ≥ 320 µm for men and 305 µm for women are proposed as gender-specific thickness levels. 19

What Has Been Learned? Optical Coherence Tomography Ø Protocol O: Conversion equations may be used to transform CSF values obtained on a SD-OCT to a TD scale for group comparisons. However, the CST conversion equations do not appear to predict TD values for an individual accurately enough to warrant use of these conversion equations confidently in clinical decision-making at the patient level. 20

Access to Publications and Presentations Ø Publications and Presentations can be found on the public website or on the study website (log in required) 21

Recently Published Results 22

Protocol S Five-Year Outcomes of Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: Randomized Clinical Trial 23
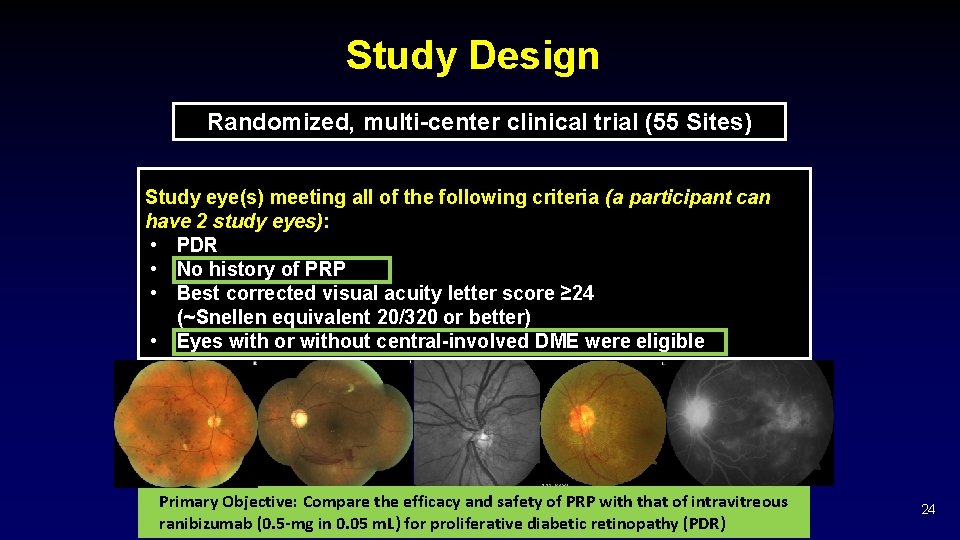
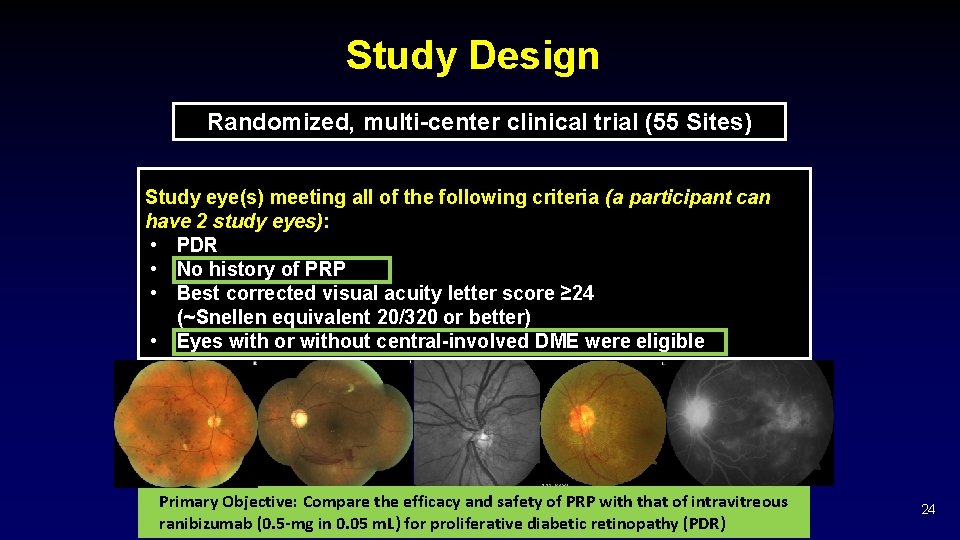
Study Design Randomized, multi-center clinical trial (55 Sites) Study eye(s) meeting all of the following criteria (a participant can have 2 study eyes): • PDR • No history of PRP • Best corrected visual acuity letter score ≥ 24 (~Snellen equivalent 20/320 or better) • Eyes with or without central-involved DME were eligible Primary Objective: Compare the efficacy and safety of PRP with that of intravitreous ranibizumab (0. 5 -mg in 0. 05 m. L) for proliferative diabetic retinopathy (PDR) 24

Conclusions: Five-Year Outcomes § § § Mean change in VA with ranibizumab similar to PRP at 5 years Loss to follow-up was relatively high in both groups Other outcomes: Favored ranibizumab: § Decreased development of centralinvolved DME with vision impairment § Decreased development of retinal detachments Favored PRP: § Fewer visits § Fewer injections Both Groups: § Substantial VA loss rare (6% in each group) § Visual field loss progressed in both groups in years 2 -5; difference between groups diminished § Vitreous hemorrhage in almost 50% of both groups 25

Protocols Currently Enrolling 26

Protocol AC Randomized Trial of Intravitreous Aflibercept versus Intravitreous Bevacizumab + Deferred Aflibercept for Treatment of Central-Involved Diabetic Macular Edema (DME) 27

Background Ø Aflibercept treatment in Protocol T resulted in better VA, on average, for eyes with worse baseline VA than bevacizumab Ø However, bevacizumab was effective for many eyes with worse VA at baseline. § Approximately 2/3 of bevacizumab-treated eyes had >10 letter improvement at 2 years § Almost half had resolution of DME at 2 years Ø Cost is an issue

Background Ø Real Life Application: § Compare starting with bevacizumab and switching to aflibercept if needed vs. starting with aflibercept? § What are the implications of insurance companies mandating this approach or patients choosing this approach? • Cost savings • Visual outcomes

Study Objective Ø To compare the efficacy of intravitreous aflibercept with intravitreous bevacizumab + deferred aflibercept if needed in eyes with CI DME and moderate vision loss. 30
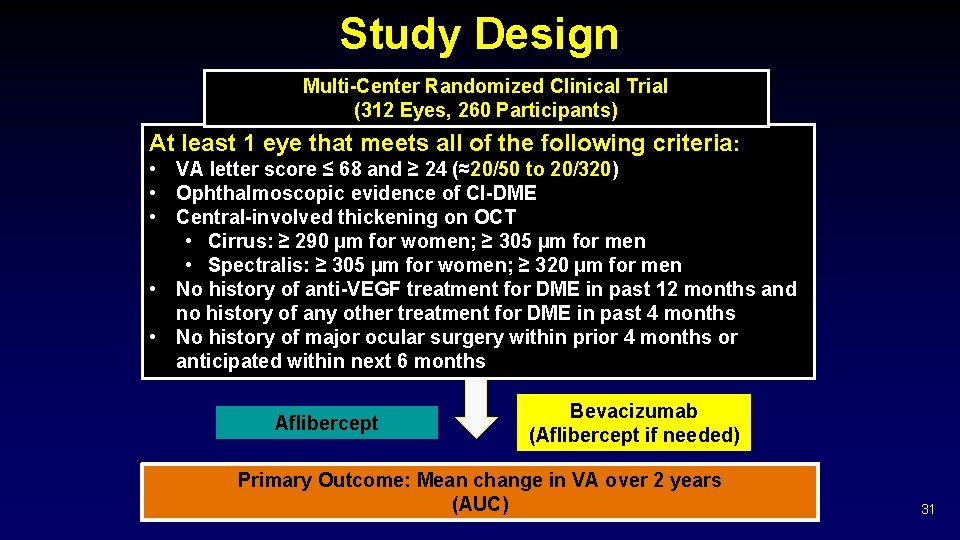
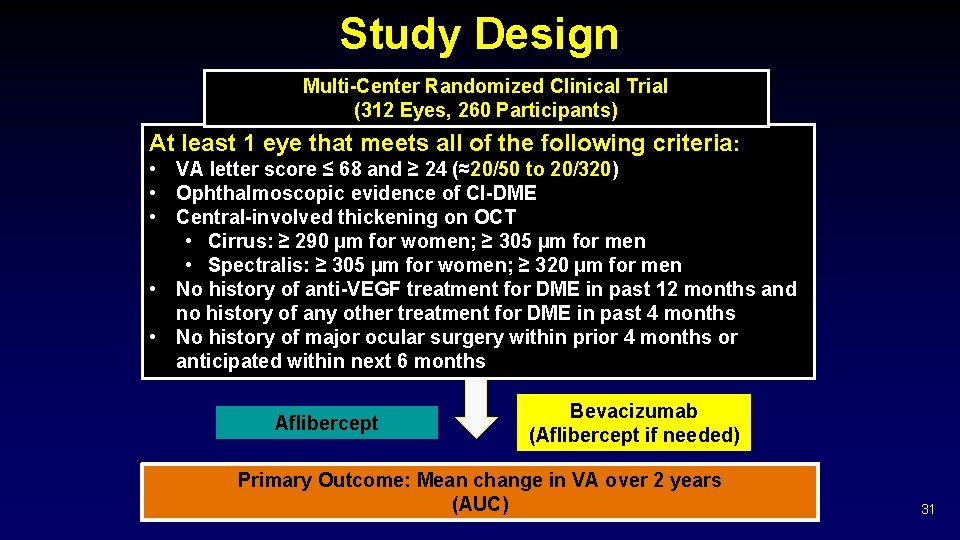
Study Design Multi-Center Randomized Clinical Trial (312 Eyes, 260 Participants) At least 1 eye that meets all of the following criteria: • VA letter score ≤ 68 and ≥ 24 (≈20/50 to 20/320) • Ophthalmoscopic evidence of CI-DME • Central-involved thickening on OCT • Cirrus: ≥ 290 µm for women; ≥ 305 µm for men • Spectralis: ≥ 305 µm for women; ≥ 320 µm for men • No history of anti-VEGF treatment for DME in past 12 months and no history of any other treatment for DME in past 4 months • No history of major ocular surgery within prior 4 months or anticipated within next 6 months Aflibercept Bevacizumab (Aflibercept if needed) Primary Outcome: Mean change in VA over 2 years (AUC) 31

Treatment Groups Aflibercept • 2. 0 -mg intravitreous aflibercept Bevacizumab (Aflibercept if needed) • Centrally repackaged 1. 25 -mg bevacizumab • Switched to intravitreous aflibercept if eye is not “successful” 32
Protocol AG Randomized Clinical Trial Assessing the Effects of Pneumatic Vitreolysis on Vitreomacular Traction 33

Study Objective Ø Primary § Ø To compare the proportion of eyes with foveal VMT (symptomatic VMA) release on OCT after PVL with gas injection vs. observation (sham injection) in eyes with VMT without an associated macular hole Secondary § To evaluate visual function outcomes at 24 weeks after gas injection is performed compared with observation. 34
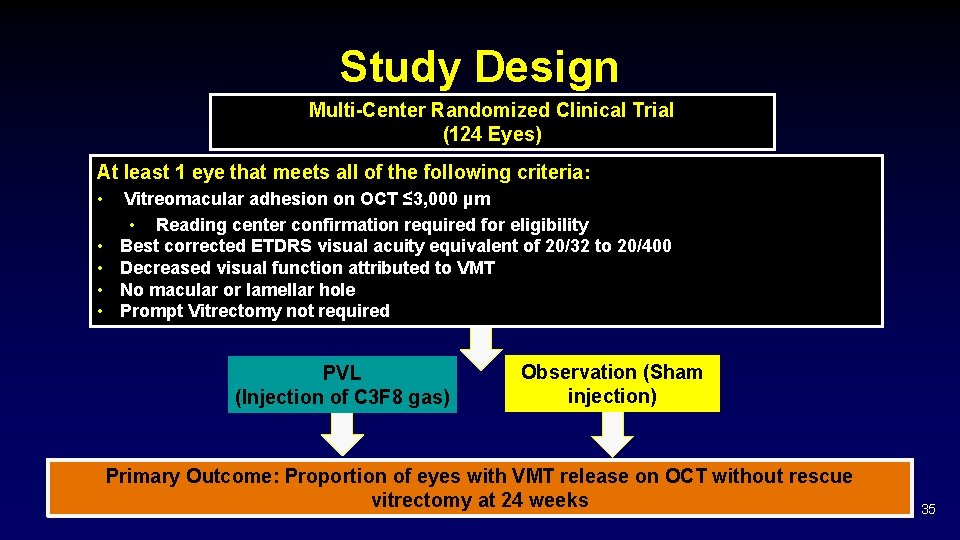
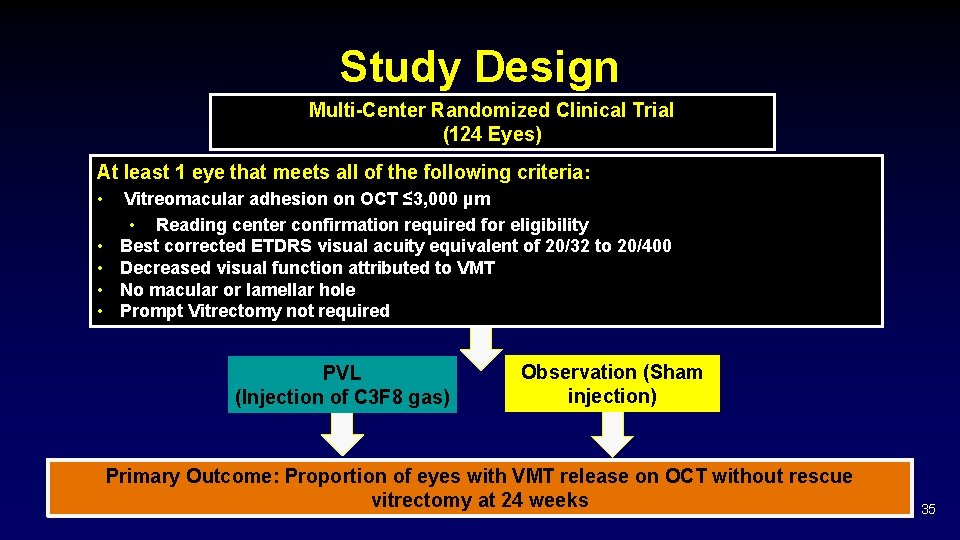
Study Design Multi-Center Randomized Clinical Trial (124 Eyes) At least 1 eye that meets all of the following criteria: • • • Vitreomacular adhesion on OCT ≤ 3, 000 µm • Reading center confirmation required for eligibility Best corrected ETDRS visual acuity equivalent of 20/32 to 20/400 Decreased visual function attributed to VMT No macular or lamellar hole Prompt Vitrectomy not required PVL (Injection of C 3 F 8 gas) Observation (Sham injection) Primary Outcome: Proportion of eyes with VMT release on OCT without rescue vitrectomy at 24 weeks 35
Protocol AH Single-Arm Study Assessing the Effects of Pneumatic Vitreolysis on Macular Hole 36
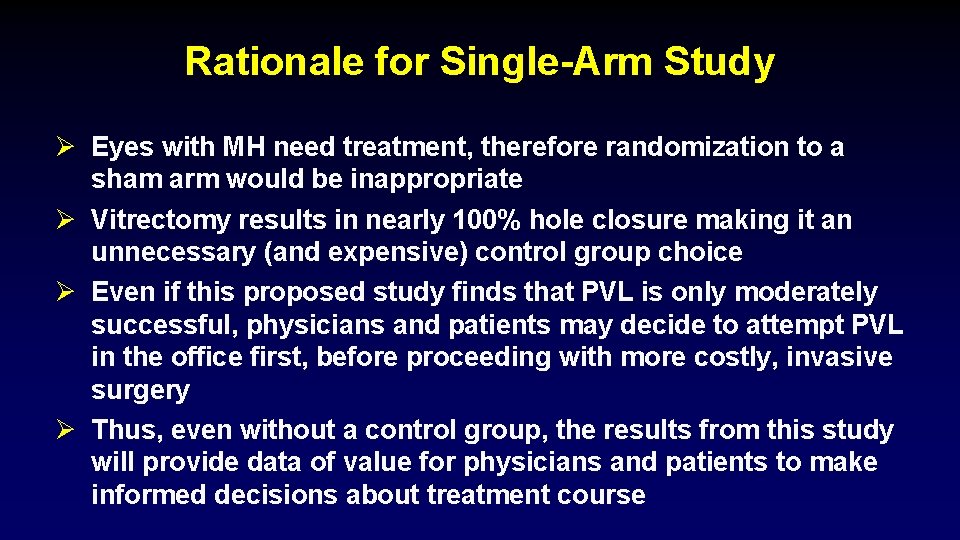
Rationale for Single-Arm Study Ø Eyes with MH need treatment, therefore randomization to a sham arm would be inappropriate Ø Vitrectomy results in nearly 100% hole closure making it an unnecessary (and expensive) control group choice Ø Even if this proposed study finds that PVL is only moderately successful, physicians and patients may decide to attempt PVL in the office first, before proceeding with more costly, invasive surgery Ø Thus, even without a control group, the results from this study will provide data of value for physicians and patients to make informed decisions about treatment course
Study Objective Ø To obtain estimates for the proportion of eyes with macular hole closure of the inner retinal layers for eyes with VMT and full-thickness macular holes treated with PVL 38
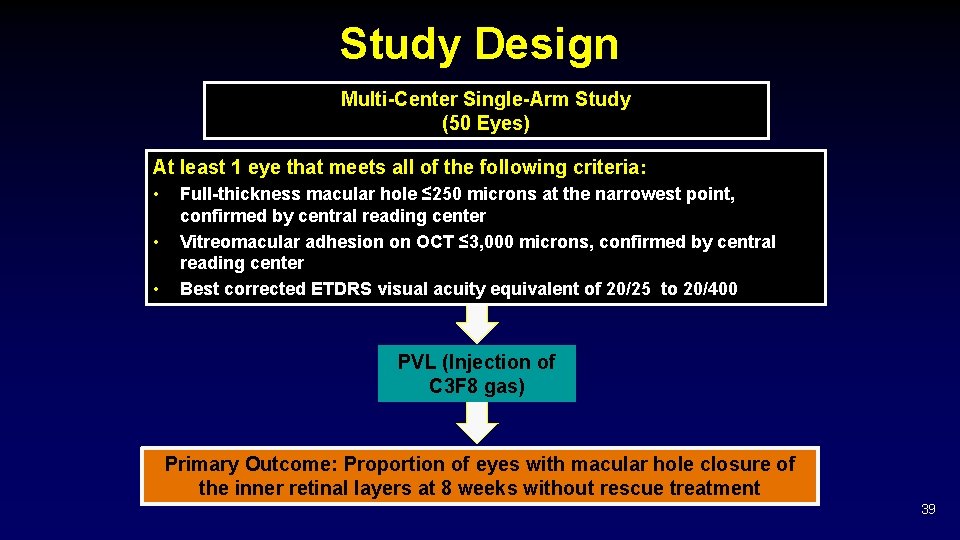
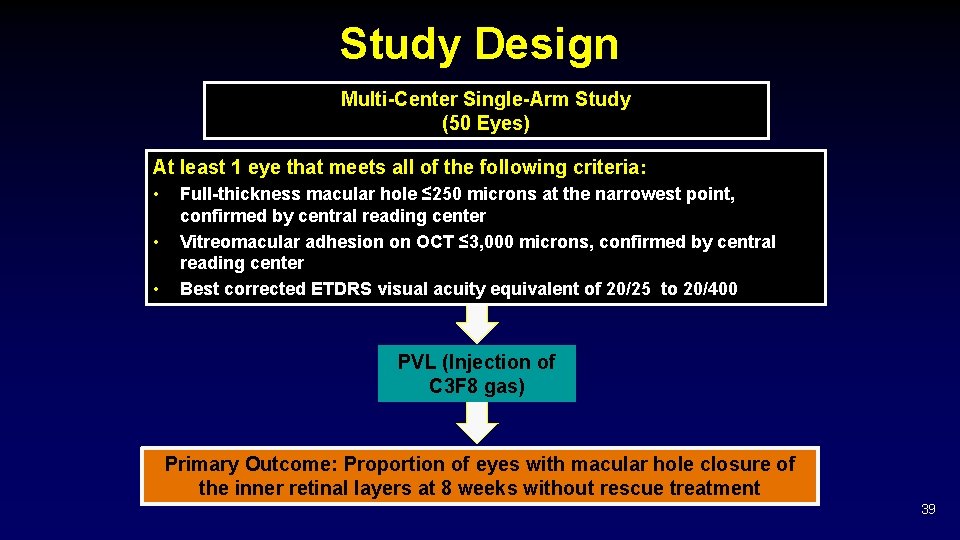
Study Design Multi-Center Single-Arm Study (50 Eyes) At least 1 eye that meets all of the following criteria: • • • Full-thickness macular hole ≤ 250 microns at the narrowest point, confirmed by central reading center Vitreomacular adhesion on OCT ≤ 3, 000 microns, confirmed by central reading center Best corrected ETDRS visual acuity equivalent of 20/25 to 20/400 PVL (Injection of C 3 F 8 gas) Primary Outcome: Proportion of eyes with macular hole closure of the inner retinal layers at 8 weeks without rescue treatment 39
Genetics Genes in Diabetic Retinopathy Project 40

Genes in Diabetic Retinopathy Project Ø Objective § § Ø Major Eligibility Criteria § Ø To create a repository of genetic material and clinical phenotype information as a resource for the research community The database may provide the opportunity to assess genetic susceptibility and resistance to DR and also variants impacting visually-important biomarkers for ME and neovascularization. Previous/current participant in a DRCR. net study Enrollment (Ongoing) § Total enrolled: 2, 396 subjects (as of 2/7/19) 41

Protocols Currently in Follow-up

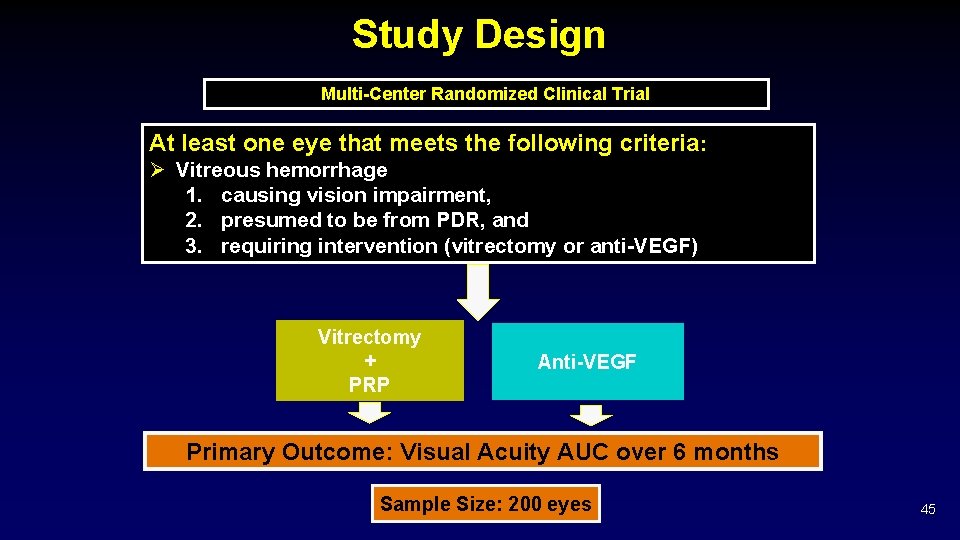
Protocol AB Intravitreous Anti-VEGF vs. Vitrectomy for Vitreous Hemorrhage from PDR

Study Objectives Ø Compare visual acuity outcomes over time for the following two treatment regimens: § § Prompt Vitrectomy + PRP Intravitreous Anti-VEGF injections in eyes presenting with vitreous hemorrhage from PDR causing vision impairment for which intervention is deemed necessary. 44
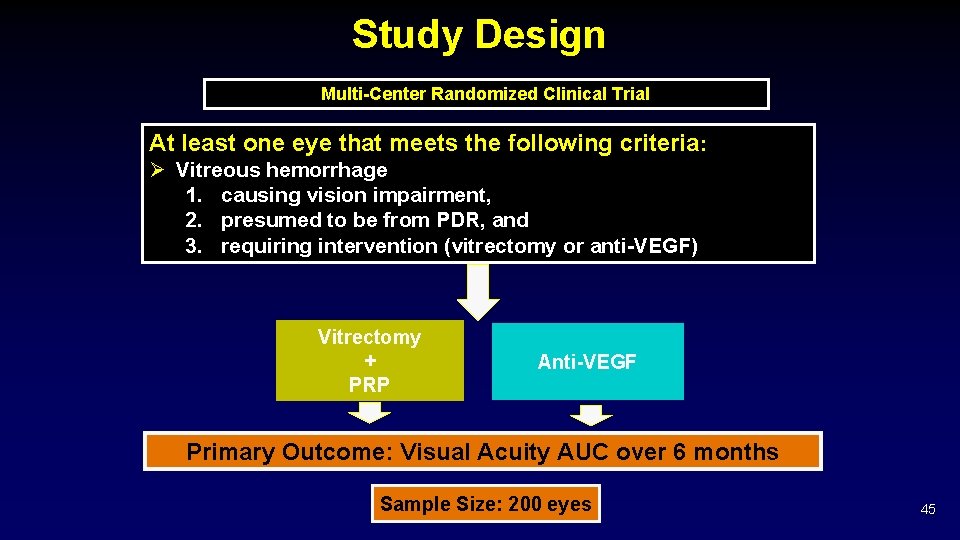
Study Design Multi-Center Randomized Clinical Trial At least one eye that meets the following criteria: Ø Vitreous hemorrhage 1. causing vision impairment, 2. presumed to be from PDR, and 3. requiring intervention (vitrectomy or anti-VEGF) Vitrectomy + PRP Anti-VEGF Primary Outcome: Visual Acuity AUC over 6 months Sample Size: 200 eyes 45
Protocol W Intravitreous Anti-VEGF Treatment for Prevention of Vision Threatening Diabetic Retinopathy in Eyes at High Risk

Primary (Short-term) Objective To determine safety and efficacy of anti-VEGF versus observation in eyes presenting with severe NPDR and no CI-DME for prevention of vision threatening outcomes (DME or PDR) Observation (sham injections) Intravitreous anti-VEGF Primary outcome: Proportion of eyes that develop PDR/PDR-related outcomes or center-involved DME causing visual acuity loss by 2 years 47
Rationale Ø The application of anti-VEGF therapy earlier in the course of disease could help to reduce future potential treatment burden in patients, at the same time resulting in similar or better long-term visual acuity outcomes. Ø If this study demonstrates that anti-VEGF treatment is effective and safe in the setting of severe NPDR, a new strategy to prevent vision-threatening complications will be available for patients. 48
Protocol T – Follow-up Extension Study A Comparative Effectiveness Study of Intravitreal Aflibercept, Bevacizumab and Ranibizumab for Diabetic Macular Edema
Study Design Observational cohort study Eligibility Criteria: Any participant, not known to be deceased, who was randomized in the Protocol T main study at clinical sites that are currently active in the DRCR. net. One follow-up visit approximately 5 years after randomization in T 50
Primary Objective Ø Descriptive analyses for the following: § § § § Types of DME treatments since last T visit Frequency of DME treatments since last T visit Treatments for diabetic retinopathy since last T visit Visual acuity outcomes at 5 years • Mean change in VA, proportion of eyes with 2 or 3 or more letter gain/loss, distribution of VA at 5 yrs DME outcomes at 5 years • Mean change in OCT, proportion of eyes with OCT < gender and machine specific cutoffs Diabetic retinopathy outcomes at 5 years APTC events occurring in participants since last T visit 51

Protocol AA Peripheral Diabetic Retinopathy (DR) Lesions on Ultrawide-field Fundus Images and Risk of DR Worsening Over Time
Objectives Ø Primary objective § To assess whether evaluation of the retinal far periphery on UWF images improves our ability to assess DR and predict rates of DR worsening over time as compared with evaluation only of the area within the 7 standard ETDRS fields. 53

Study Design Prospective, observational longitudinal study At least one eye meeting all of the following criteria: • NPDR based on clinical exam (Confirmed ETDRS level 35 - 57 on 7 -field photos) • No CI-DME on clinical exam or OCT • No history of PRP or vitrectomy • No intravitreal Tx over prior 12 mos. and not anticipated for next 6 mos. Annual Visits for 4 years Primary outcome: Relative risk of 2 or more step worsening of DR severity over 4 years in groups with and without any predominantly peripheral lesions on UWF images at baseline. 54
Recently Completed Protocols

Protocol V Treatment for Central-involved DME in Eyes with Very Good Visual Acuity

Study Design Randomized, multi-center clinical trial At least one eye meeting all of the following criteria: • Central-involved DME on OCT (Cirrus/Spectralis only)* • VA letter score 20/25 (Snellen equivalent) or better* • Minimal prior treatment for DME ** Prompt anti-VEGF Prompt laser + deferred anti-VEGF Observation + deferred anti-VEGF Primary outcome: Proportion of eyes that have lost ≥ 5 letters of VA at 2 years *Confirmed at 2 visits (screening and randomization 1 -28 days apart) **No more than 1 laser and/or 4 injections, at least 12 months ago 57
Upcoming Protocol A Pilot Study Evaluating Photobiomodulation for Diabetic Macular Edema

DRCR. net Thank you 59