DRAFT ONC Care Plan Standards Acceleration Strategy ONC
- Slides: 23
DRAFT: ONC Care Plan Standards Acceleration Strategy ONC Care Plan Task Force Date: June 20, 2016
Outline • Background: Problem Statement • Care Plan Acceleration Strategy Task Areas • Drivers: » Interoperability Roadmap » Federal Health IT Strategic Plan • Care Plan Acceleration Strategy Outcomes • Care Plan Standards Ecosystem • Care Plan Standards Based Initiatives • C-CDA Challenges • Next Steps 2
Background: Problem Statement • Interest in a comprehensive, shared, longitudinal electronic person-centered care plan is burgeoning • ONC has invested in the identification and publication of standards to support a comprehensive shared care plan (CSCP) • However, the availability of standards does not ensure the steadfast adoption and implementation of interoperable CSCPs. • Remaining barriers include: » Lack of policies to support electronic care planning across and between provider groups and patients » Limited consensus on the processes, procedures and workflow to support CSCP » Limited awareness and consensus on value of CSCPs » Variability in vendor adoption and implementation of CSCP capabilities » Consolidation and reconciliation of care plans 3
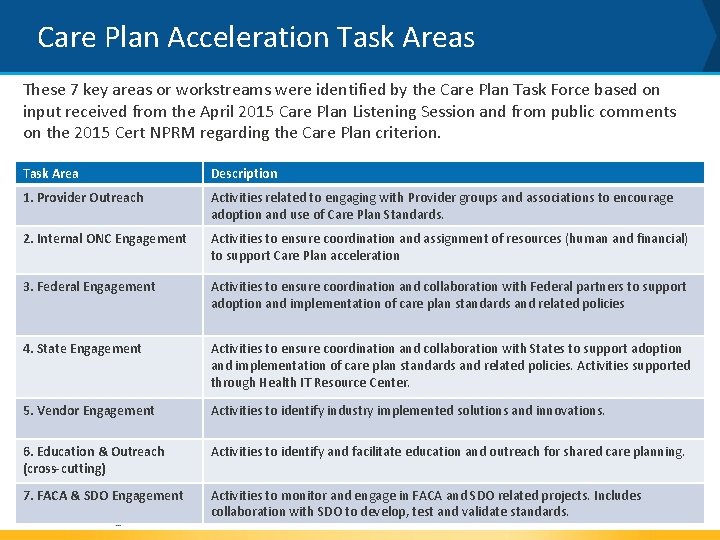
Care Plan Acceleration Strategy Task Areas • In April 2015 ONC convened one day listening session to articulate a vision for CSCPs • The session resulted in ONC identifying key task areas (or workstreams) to further support and accelerate adoption of interoperable CSCPs: » Provider Outreach » Internal ONC Engagement » Federal Engagement » State Engagement » Vendor Engagement » Education & Outreach (cross-cutting) » FACA & SDO Engagement 4
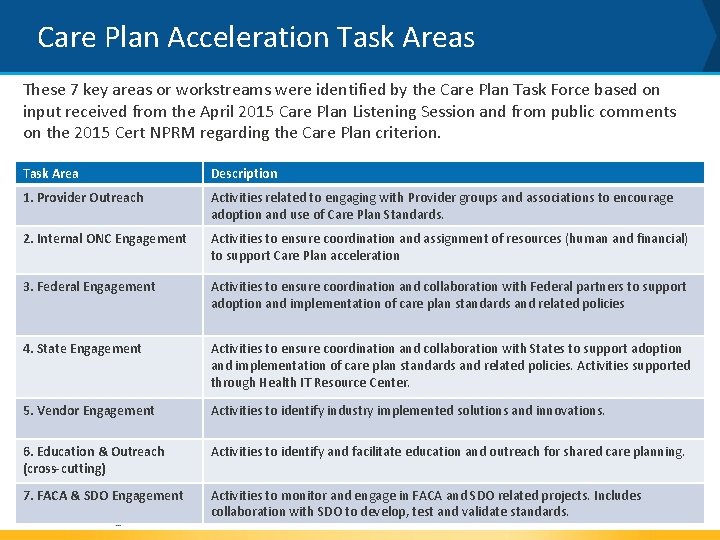
Care Plan Acceleration Task Areas These 7 key areas or workstreams were identified by the Care Plan Task Force based on input received from the April 2015 Care Plan Listening Session and from public comments on the 2015 Cert NPRM regarding the Care Plan criterion. Task Area Description 1. Provider Outreach Activities related to engaging with Provider groups and associations to encourage adoption and use of Care Plan Standards. 2. Internal ONC Engagement Activities to ensure coordination and assignment of resources (human and financial) to support Care Plan acceleration 3. Federal Engagement Activities to ensure coordination and collaboration with Federal partners to support adoption and implementation of care plan standards and related policies 4. State Engagement Activities to ensure coordination and collaboration with States to support adoption and implementation of care plan standards and related policies. Activities supported through Health IT Resource Center. 5. Vendor Engagement Activities to identify industry implemented solutions and innovations. 6. Education & Outreach (cross-cutting) Activities to identify and facilitate education and outreach for shared care planning. 7. FACA & SDO Engagement Activities to monitor and engage in FACA and SDO related projects. Includes collaboration with SDO to develop, test and validate standards. 5
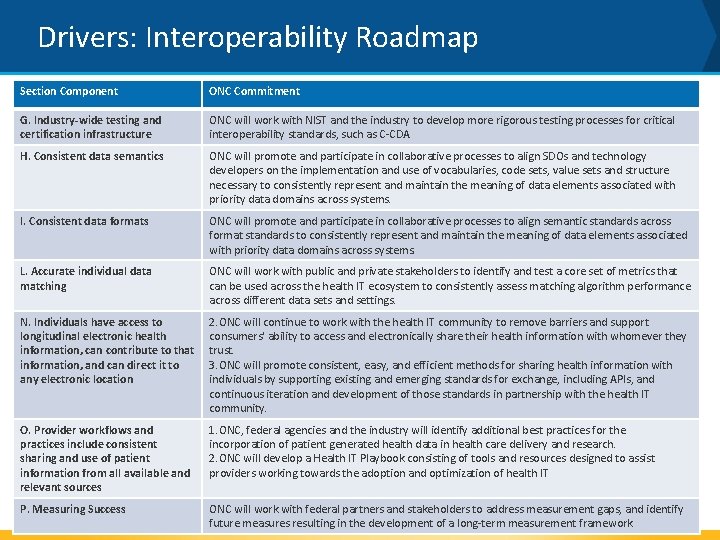
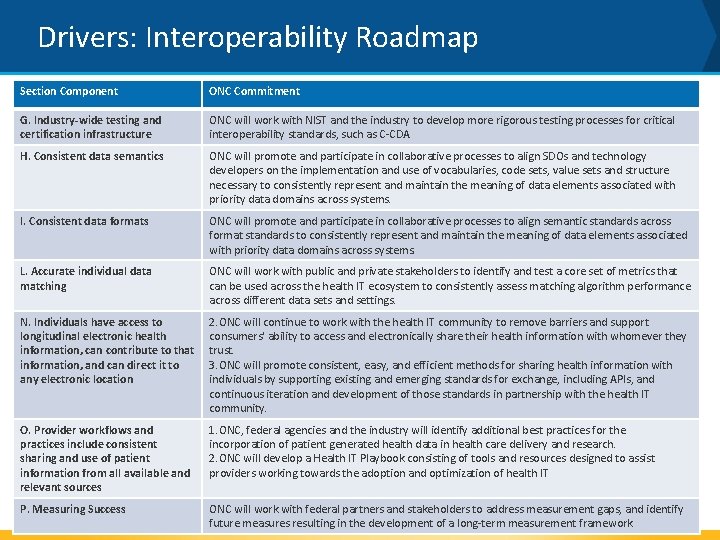
Drivers: Interoperability Roadmap Section Component ONC Commitment G. Industry-wide testing and certification infrastructure ONC will work with NIST and the industry to develop more rigorous testing processes for critical interoperability standards, such as C-CDA H. Consistent data semantics ONC will promote and participate in collaborative processes to align SDOs and technology developers on the implementation and use of vocabularies, code sets, value sets and structure necessary to consistently represent and maintain the meaning of data elements associated with priority data domains across systems. I. Consistent data formats ONC will promote and participate in collaborative processes to align semantic standards across format standards to consistently represent and maintain the meaning of data elements associated with priority data domains across systems. L. Accurate individual data matching ONC will work with public and private stakeholders to identify and test a core set of metrics that can be used across the health IT ecosystem to consistently assess matching algorithm performance across different data sets and settings. N. Individuals have access to longitudinal electronic health information, can contribute to that information, and can direct it to any electronic location 2. ONC will continue to work with the health IT community to remove barriers and support consumers' ability to access and electronically share their health information with whomever they trust. 3. ONC will promote consistent, easy, and efficient methods for sharing health information with individuals by supporting existing and emerging standards for exchange, including APIs, and continuous iteration and development of those standards in partnership with the health IT community. O. Provider workflows and practices include consistent sharing and use of patient information from all available and relevant sources 1. ONC, federal agencies and the industry will identify additional best practices for the incorporation of patient generated health data in health care delivery and research. 2. ONC will develop a Health IT Playbook consisting of tools and resources designed to assist providers working towards the adoption and optimization of health IT P. Measuring Success ONC will work with federal partners and stakeholders to address measurement gaps, and identify future measures resulting in the development of a long-term measurement framework.
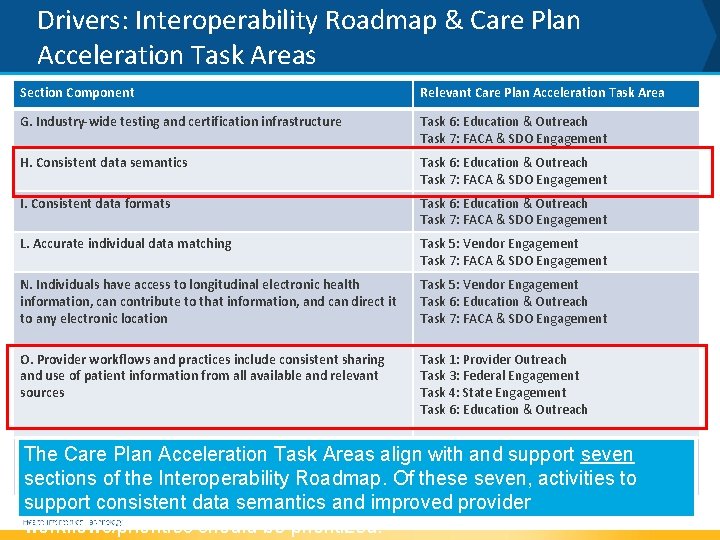
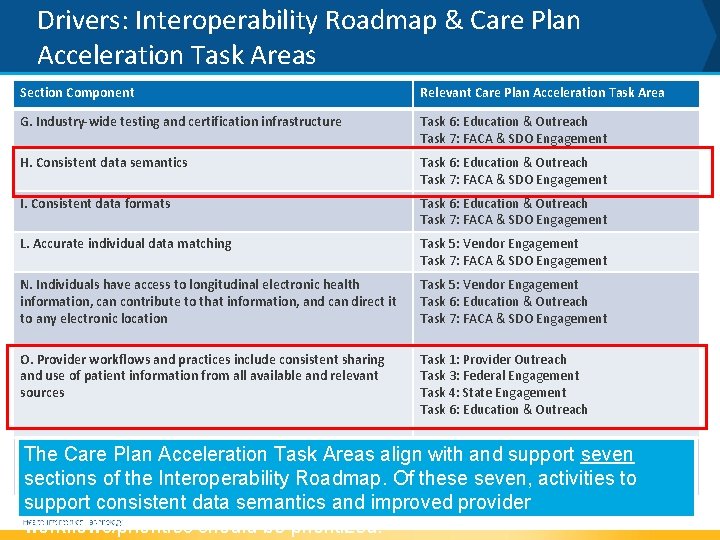
Drivers: Interoperability Roadmap & Care Plan Acceleration Task Areas Section Component Relevant Care Plan Acceleration Task Area G. Industry-wide testing and certification infrastructure Task 6: Education & Outreach Task 7: FACA & SDO Engagement H. Consistent data semantics Task 6: Education & Outreach Task 7: FACA & SDO Engagement I. Consistent data formats Task 6: Education & Outreach Task 7: FACA & SDO Engagement L. Accurate individual data matching Task 5: Vendor Engagement Task 7: FACA & SDO Engagement N. Individuals have access to longitudinal electronic health information, can contribute to that information, and can direct it to any electronic location Task 5: Vendor Engagement Task 6: Education & Outreach Task 7: FACA & SDO Engagement O. Provider workflows and practices include consistent sharing and use of patient information from all available and relevant sources Task 1: Provider Outreach Task 3: Federal Engagement Task 4: State Engagement Task 6: Education & Outreach P. Measuring The Care. Success Plan 3: Federal Engagement seven Acceleration Task Areas align. Task with and support Task 5: Vendor Engagement sections of the Interoperability Roadmap. Of these seven, activities to support consistent data semantics and improved provider workflows/priorities should be prioritized.
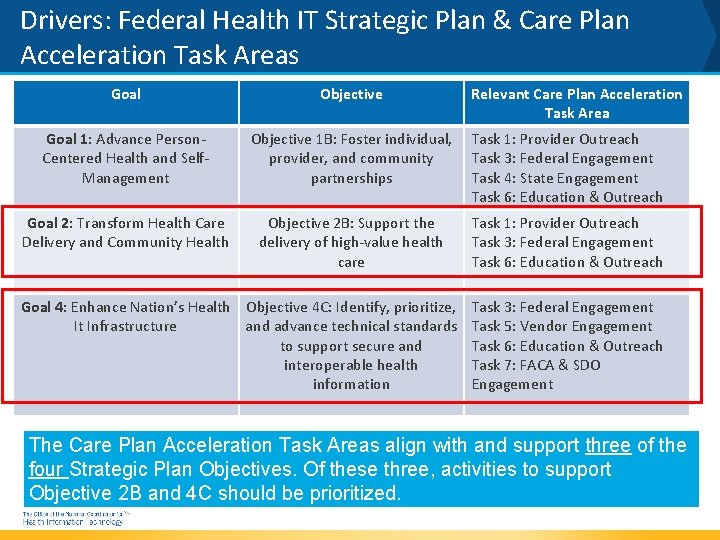
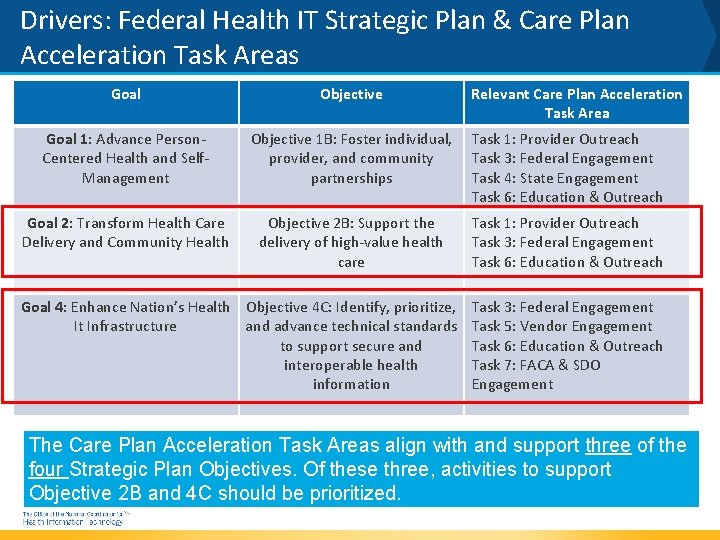
Drivers: Federal Health IT Strategic Plan & Care Plan Acceleration Task Areas Goal Objective Goal 1: Advance Person. Centered Health and Self. Management Objective 1 B: Foster individual, provider, and community partnerships Task 1: Provider Outreach Task 3: Federal Engagement Task 4: State Engagement Task 6: Education & Outreach Goal 2: Transform Health Care Delivery and Community Health Objective 2 B: Support the delivery of high-value health care Task 1: Provider Outreach Task 3: Federal Engagement Task 6: Education & Outreach Goal 4: Enhance Nation’s Health Objective 4 C: Identify, prioritize, It Infrastructure and advance technical standards to support secure and interoperable health information Relevant Care Plan Acceleration Task Area Task 3: Federal Engagement Task 5: Vendor Engagement Task 6: Education & Outreach Task 7: FACA & SDO Engagement The Care Plan Acceleration Task Areas align with and support three of the four Strategic Plan Objectives. Of these three, activities to support Objective 2 B and 4 C should be prioritized.
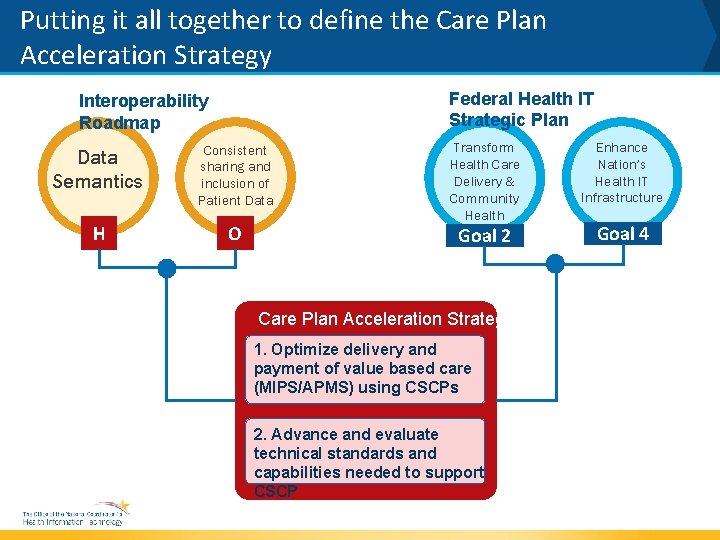
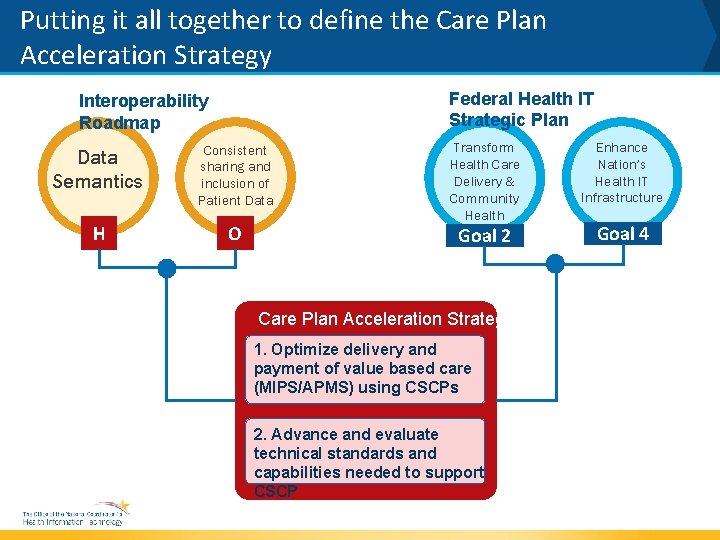
Putting it all together to define the Care Plan Acceleration Strategy Federal Health IT Strategic Plan Interoperability Roadmap Data Semantics Consistent sharing and inclusion of Patient Data H O Transform Health Care Delivery & Community Health Goal 2 Care Plan Acceleration Strategies 1. Optimize delivery and payment of value based care (MIPS/APMS) using CSCPs 2. Advance and evaluate technical standards and capabilities needed to support CSCP Enhance Nation’s Health IT Infrastructure Goal 4
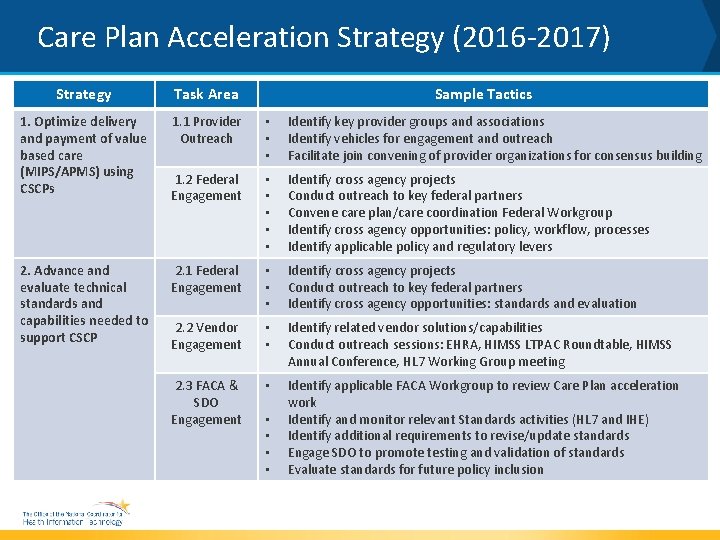
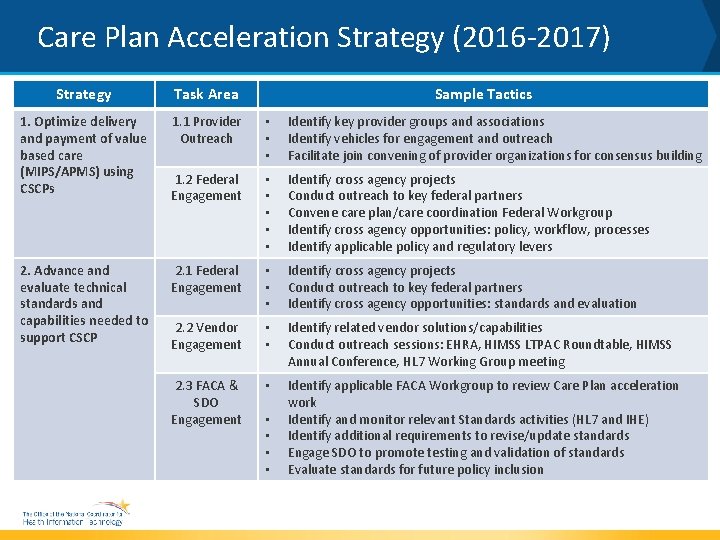
Care Plan Acceleration Strategy (2016 -2017) Strategy Task Area 1. Optimize delivery and payment of value based care (MIPS/APMS) using CSCPs 1. 1 Provider Outreach • • • Identify key provider groups and associations Identify vehicles for engagement and outreach Facilitate join convening of provider organizations for consensus building 1. 2 Federal Engagement • • • Identify cross agency projects Conduct outreach to key federal partners Convene care plan/care coordination Federal Workgroup Identify cross agency opportunities: policy, workflow, processes Identify applicable policy and regulatory levers 2. 1 Federal Engagement • • • Identify cross agency projects Conduct outreach to key federal partners Identify cross agency opportunities: standards and evaluation 2. 2 Vendor Engagement • • Identify related vendor solutions/capabilities Conduct outreach sessions: EHRA, HIMSS LTPAC Roundtable, HIMSS Annual Conference, HL 7 Working Group meeting 2. 3 FACA & SDO Engagement • Identify applicable FACA Workgroup to review Care Plan acceleration work Identify and monitor relevant Standards activities (HL 7 and IHE) Identify additional requirements to revise/update standards Engage SDO to promote testing and validation of standards Evaluate standards for future policy inclusion 2. Advance and evaluate technical standards and capabilities needed to support CSCP Sample Tactics • •
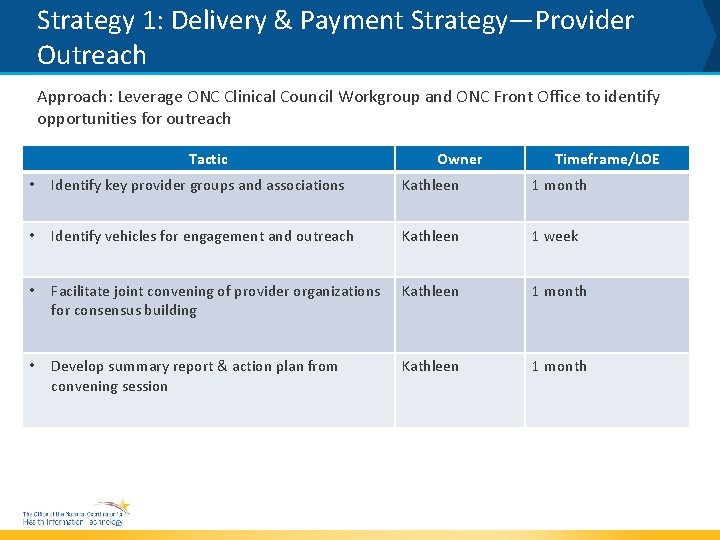
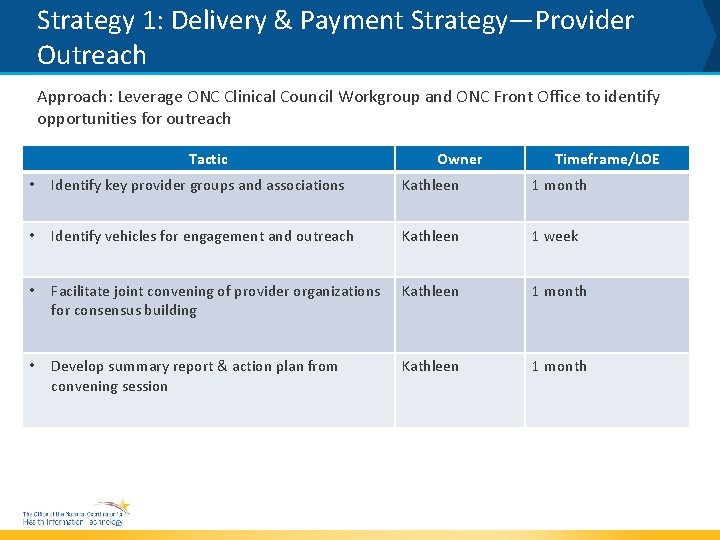
Strategy 1: Delivery & Payment Strategy—Provider Outreach Approach: Leverage ONC Clinical Council Workgroup and ONC Front Office to identify opportunities for outreach Tactic Owner Timeframe/LOE • Identify key provider groups and associations Kathleen 1 month • Identify vehicles for engagement and outreach Kathleen 1 week • Facilitate joint convening of provider organizations for consensus building Kathleen 1 month • Develop summary report & action plan from convening session Kathleen 1 month
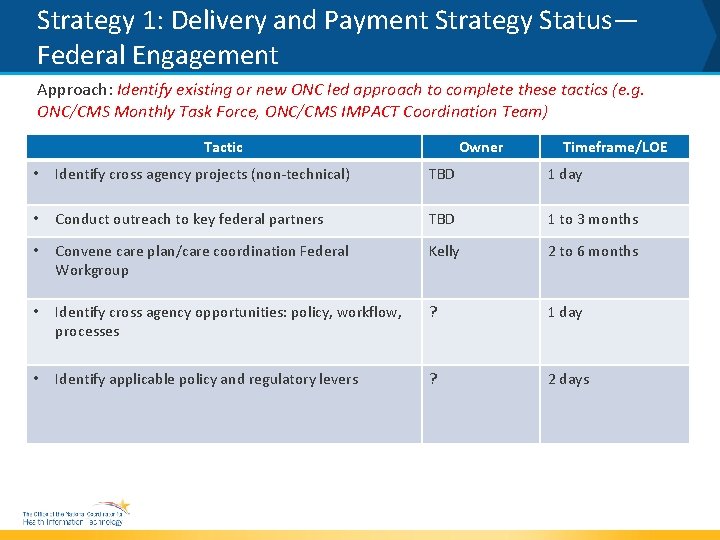
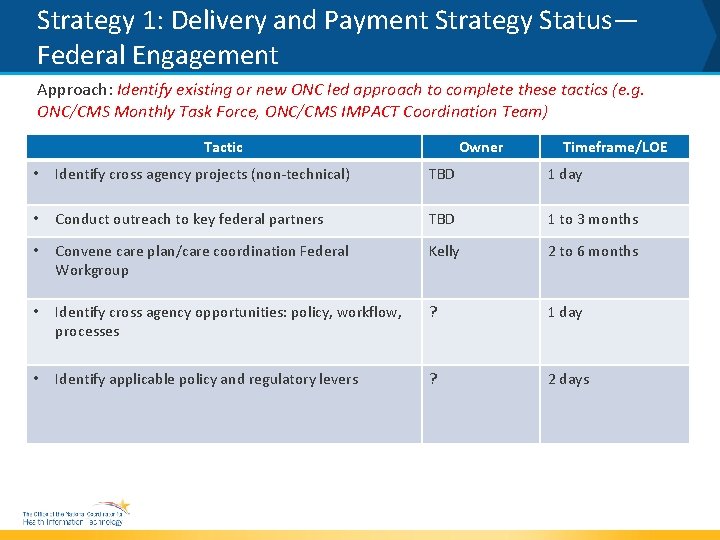
Strategy 1: Delivery and Payment Strategy Status— Federal Engagement Approach: Identify existing or new ONC led approach to complete these tactics (e. g. ONC/CMS Monthly Task Force, ONC/CMS IMPACT Coordination Team) Tactic Owner Timeframe/LOE • Identify cross agency projects (non-technical) TBD 1 day • Conduct outreach to key federal partners TBD 1 to 3 months • Convene care plan/care coordination Federal Workgroup Kelly 2 to 6 months • Identify cross agency opportunities: policy, workflow, processes ? 1 day • Identify applicable policy and regulatory levers ? 2 days
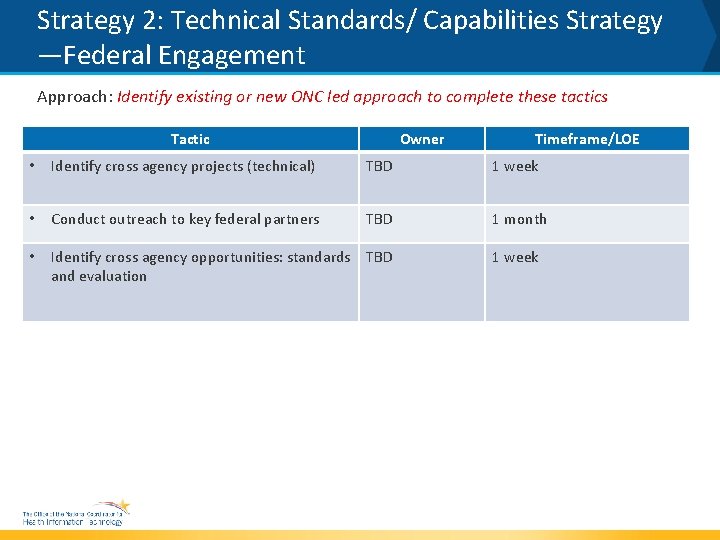
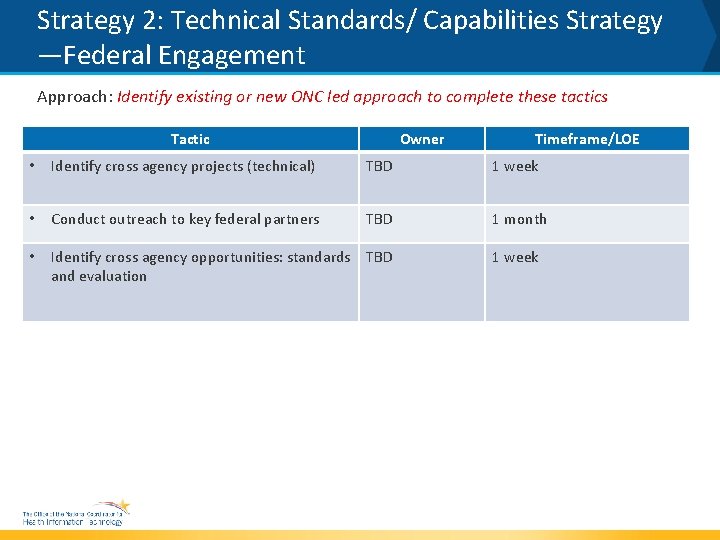
Strategy 2: Technical Standards/ Capabilities Strategy —Federal Engagement Approach: Identify existing or new ONC led approach to complete these tactics Tactic Owner Timeframe/LOE • Identify cross agency projects (technical) TBD 1 week • Conduct outreach to key federal partners TBD 1 month • Identify cross agency opportunities: standards TBD and evaluation 1 week
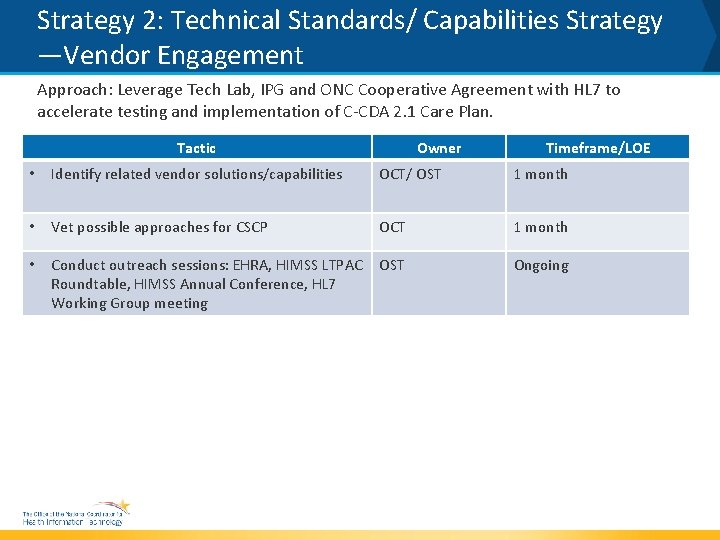
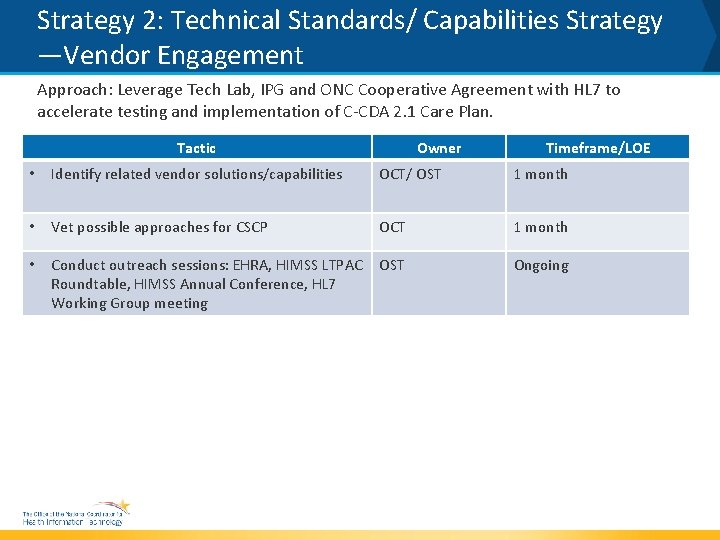
Strategy 2: Technical Standards/ Capabilities Strategy —Vendor Engagement Approach: Leverage Tech Lab, IPG and ONC Cooperative Agreement with HL 7 to accelerate testing and implementation of C-CDA 2. 1 Care Plan. Tactic Owner Timeframe/LOE • Identify related vendor solutions/capabilities OCT/ OST 1 month • Vet possible approaches for CSCP OCT 1 month • Conduct outreach sessions: EHRA, HIMSS LTPAC Roundtable, HIMSS Annual Conference, HL 7 Working Group meeting OST Ongoing
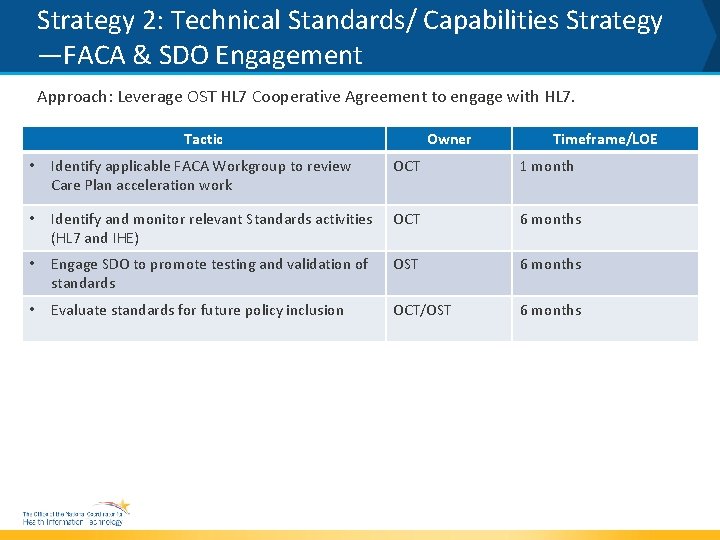
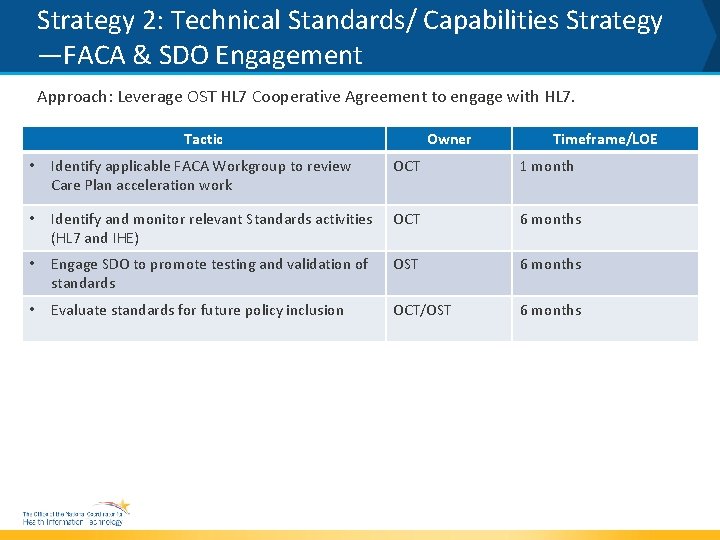
Strategy 2: Technical Standards/ Capabilities Strategy —FACA & SDO Engagement Approach: Leverage OST HL 7 Cooperative Agreement to engage with HL 7. Tactic Owner Timeframe/LOE • Identify applicable FACA Workgroup to review Care Plan acceleration work OCT 1 month • Identify and monitor relevant Standards activities (HL 7 and IHE) OCT 6 months • Engage SDO to promote testing and validation of standards OST 6 months • Evaluate standards for future policy inclusion OCT/OST 6 months
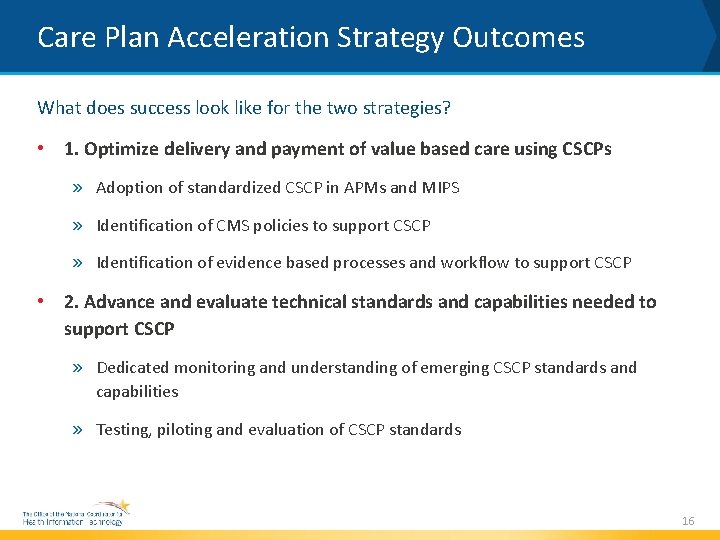
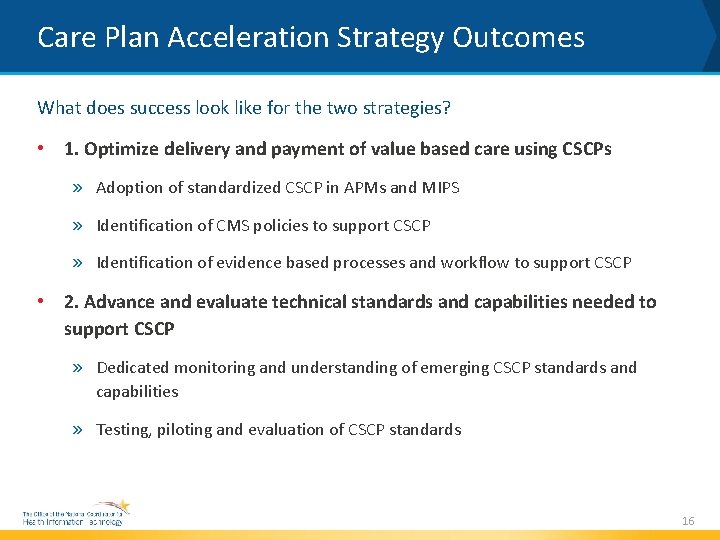
Care Plan Acceleration Strategy Outcomes What does success look like for the two strategies? • 1. Optimize delivery and payment of value based care using CSCPs » Adoption of standardized CSCP in APMs and MIPS » Identification of CMS policies to support CSCP » Identification of evidence based processes and workflow to support CSCP • 2. Advance and evaluate technical standards and capabilities needed to support CSCP » Dedicated monitoring and understanding of emerging CSCP standards and capabilities » Testing, piloting and evaluation of CSCP standards 16
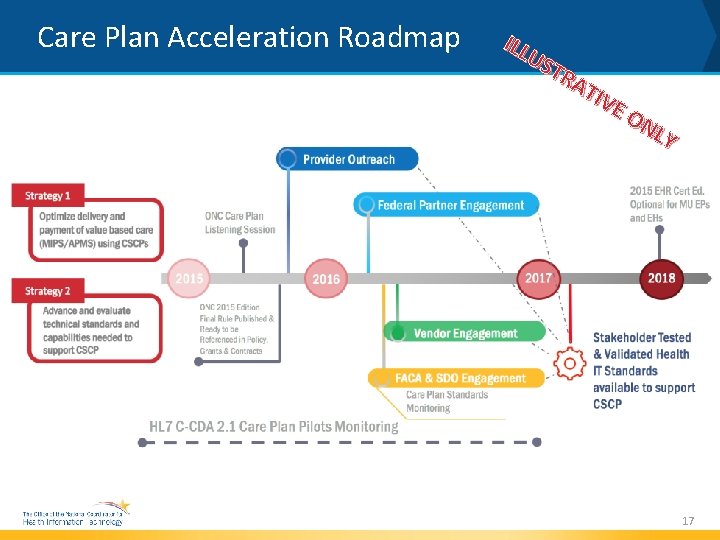
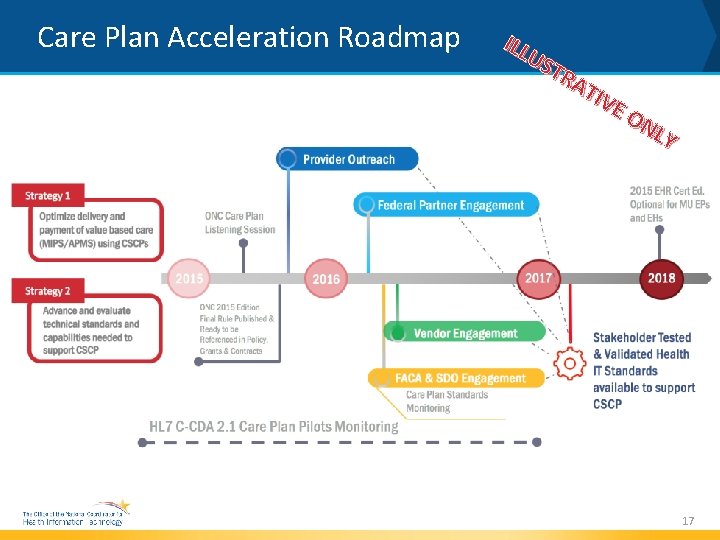
Care Plan Acceleration Roadmap ILL US TR AT IVE ON LY 17
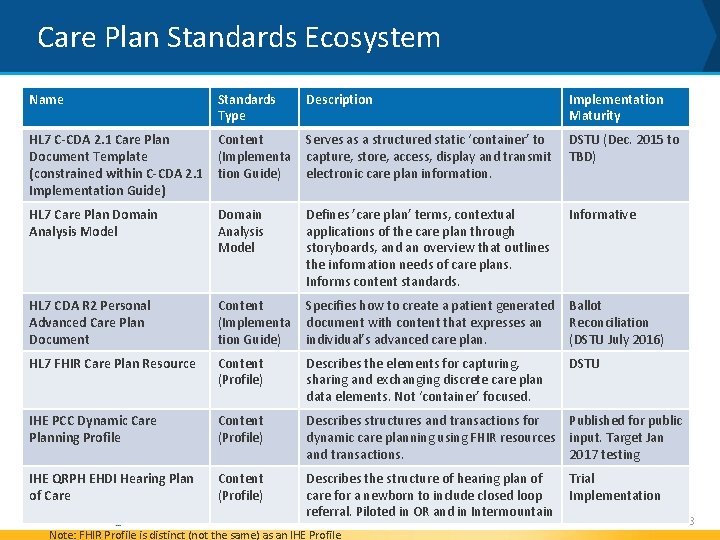
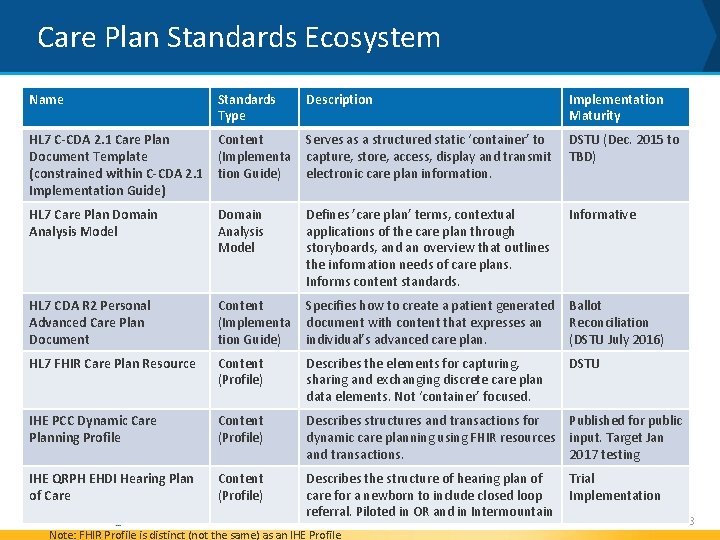
Care Plan Standards Ecosystem Name Standards Type Description Implementation Maturity HL 7 C-CDA 2. 1 Care Plan Document Template (constrained within C-CDA 2. 1 Implementation Guide) Content (Implementa tion Guide) Serves as a structured static ‘container’ to capture, store, access, display and transmit electronic care plan information. DSTU (Dec. 2015 to TBD) HL 7 Care Plan Domain Analysis Model Defines ’care plan’ terms, contextual applications of the care plan through storyboards, and an overview that outlines the information needs of care plans. Informs content standards. Informative HL 7 CDA R 2 Personal Advanced Care Plan Document Content (Implementa tion Guide) Specifies how to create a patient generated document with content that expresses an individual’s advanced care plan. Ballot Reconciliation (DSTU July 2016) HL 7 FHIR Care Plan Resource Content (Profile) Describes the elements for capturing, sharing and exchanging discrete care plan data elements. Not ‘container’ focused. DSTU IHE PCC Dynamic Care Planning Profile Content (Profile) Describes structures and transactions for dynamic care planning using FHIR resources and transactions. Published for public input. Target Jan 2017 testing IHE QRPH EHDI Hearing Plan of Care Content (Profile) Describes the structure of hearing plan of care for a newborn to include closed loop referral. Piloted in OR and in Intermountain Trial Implementation Note: FHIR Profile is distinct (not the same) as an IHE Profile 18
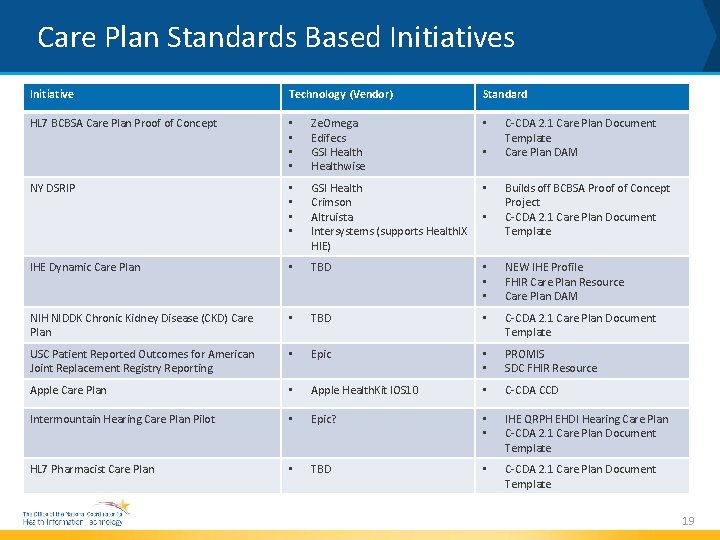
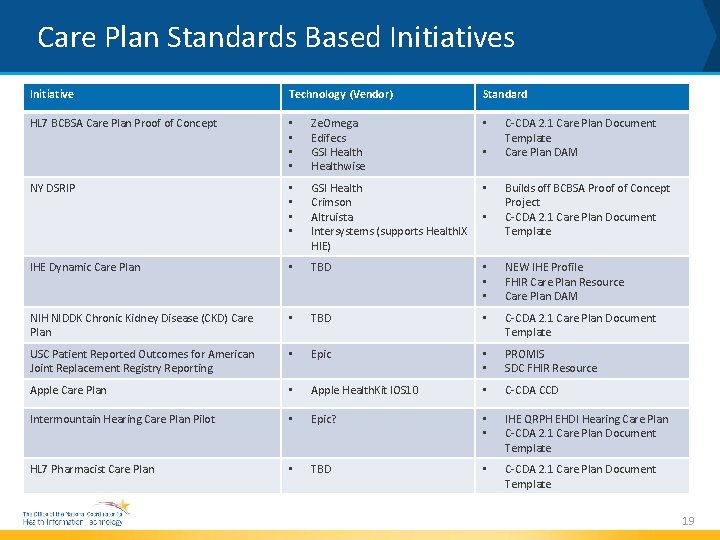
Care Plan Standards Based Initiatives Initiative Technology (Vendor) HL 7 BCBSA Care Plan Proof of Concept • • Ze. Omega Edifecs GSI Healthwise • • • GSI Health Crimson Altruista Intersystems (supports Health. IX HIE) • IHE Dynamic Care Plan • TBD • • • NEW IHE Profile FHIR Care Plan Resource Care Plan DAM NIH NIDDK Chronic Kidney Disease (CKD) Care Plan • TBD • C-CDA 2. 1 Care Plan Document Template USC Patient Reported Outcomes for American Joint Replacement Registry Reporting • Epic • • PROMIS SDC FHIR Resource Apple Care Plan • Apple Health. Kit IOS 10 • C-CDA CCD Intermountain Hearing Care Plan Pilot • Epic? • • IHE QRPH EHDI Hearing Care Plan C-CDA 2. 1 Care Plan Document Template HL 7 Pharmacist Care Plan • TBD • C-CDA 2. 1 Care Plan Document Template NY DSRIP Standard • • C-CDA 2. 1 Care Plan Document Template Care Plan DAM Builds off BCBSA Proof of Concept Project C-CDA 2. 1 Care Plan Document Template 19
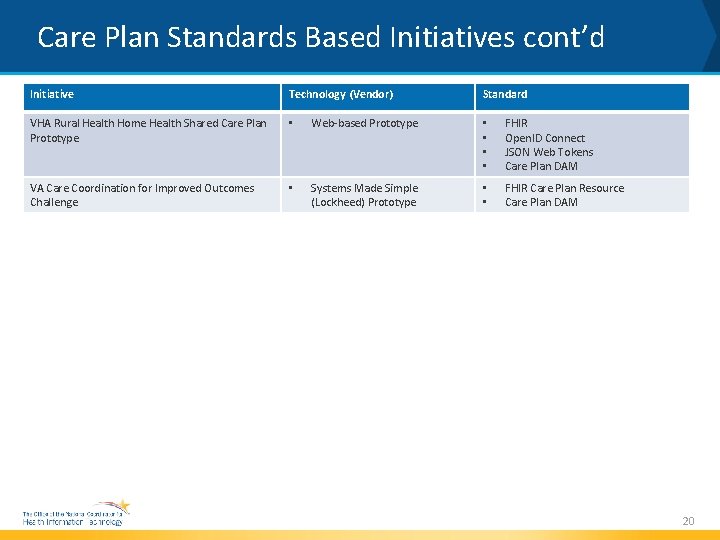
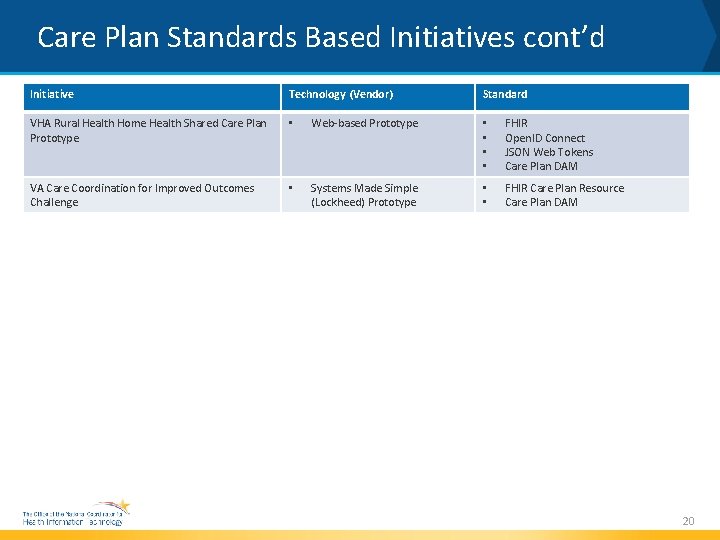
Care Plan Standards Based Initiatives cont’d Initiative Technology (Vendor) Standard VHA Rural Health Home Health Shared Care Plan Prototype • Web-based Prototype • • FHIR Open. ID Connect JSON Web Tokens Care Plan DAM VA Care Coordination for Improved Outcomes Challenge • Systems Made Simple (Lockheed) Prototype • • FHIR Care Plan Resource Care Plan DAM 20
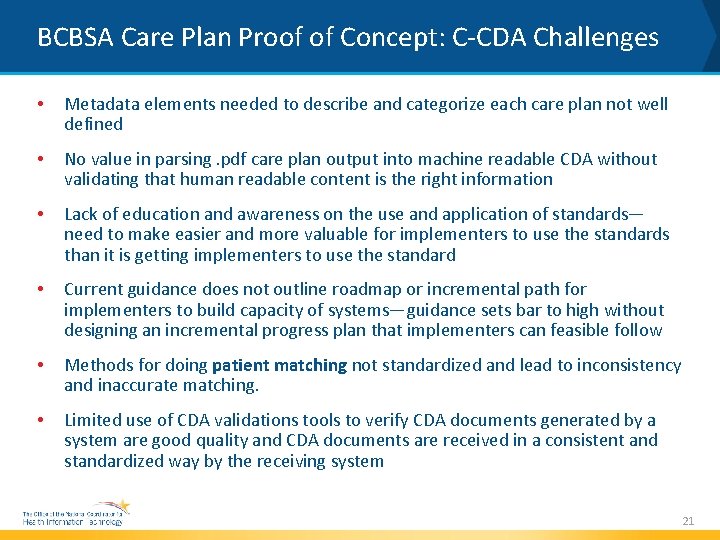
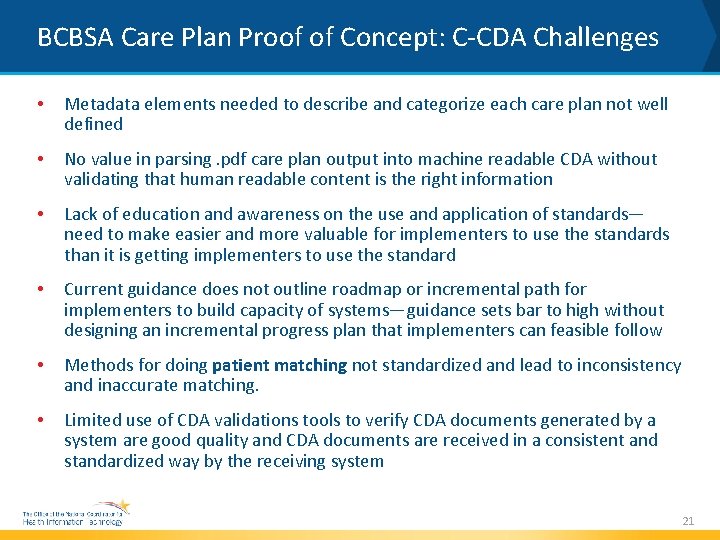
BCBSA Care Plan Proof of Concept: C-CDA Challenges • Metadata elements needed to describe and categorize each care plan not well defined • No value in parsing. pdf care plan output into machine readable CDA without validating that human readable content is the right information • Lack of education and awareness on the use and application of standards— need to make easier and more valuable for implementers to use the standards than it is getting implementers to use the standard • Current guidance does not outline roadmap or incremental path for implementers to build capacity of systems—guidance sets bar to high without designing an incremental progress plan that implementers can feasible follow • Methods for doing patient matching not standardized and lead to inconsistency and inaccurate matching. • Limited use of CDA validations tools to verify CDA documents generated by a system are good quality and CDA documents are received in a consistent and standardized way by the receiving system 21
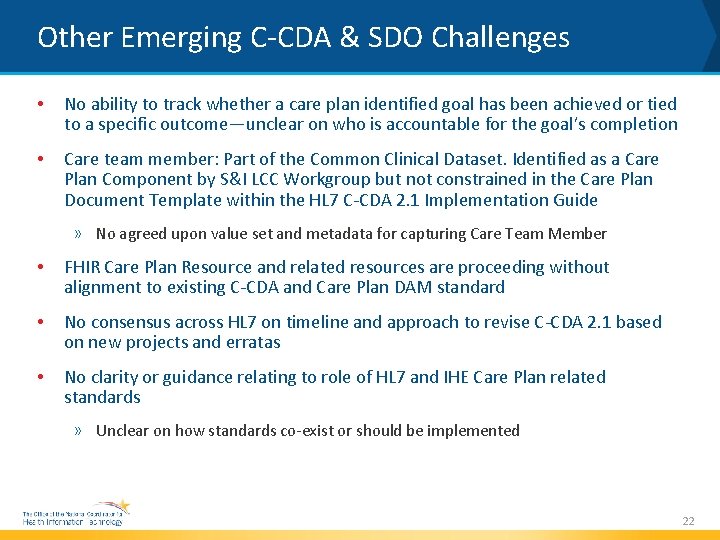
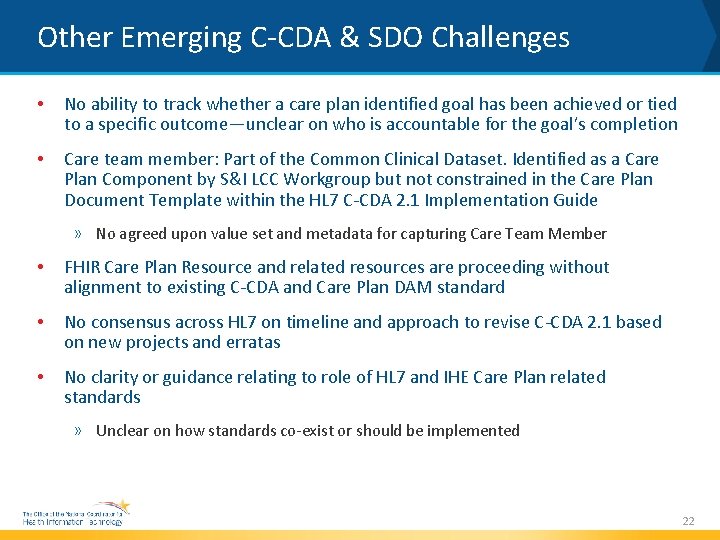
Other Emerging C-CDA & SDO Challenges • No ability to track whether a care plan identified goal has been achieved or tied to a specific outcome—unclear on who is accountable for the goal’s completion • Care team member: Part of the Common Clinical Dataset. Identified as a Care Plan Component by S&I LCC Workgroup but not constrained in the Care Plan Document Template within the HL 7 C-CDA 2. 1 Implementation Guide » No agreed upon value set and metadata for capturing Care Team Member • FHIR Care Plan Resource and related resources are proceeding without alignment to existing C-CDA and Care Plan DAM standard • No consensus across HL 7 on timeline and approach to revise C-CDA 2. 1 based on new projects and erratas • No clarity or guidance relating to role of HL 7 and IHE Care Plan related standards » Unclear on how standards co-exist or should be implemented 22
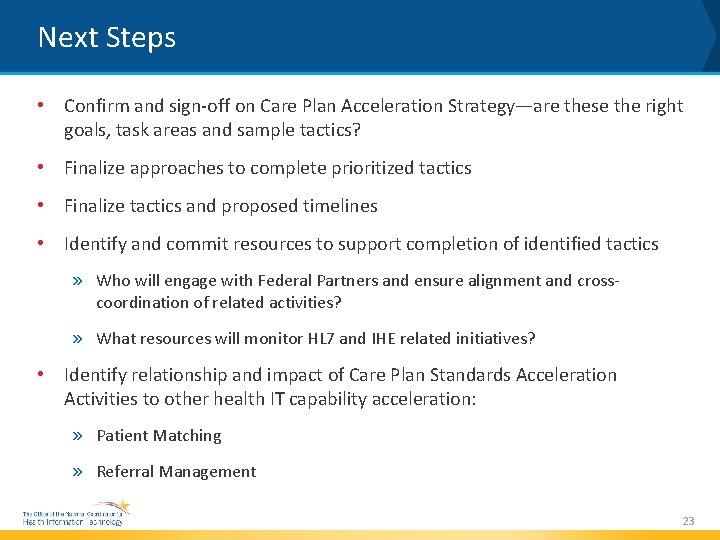
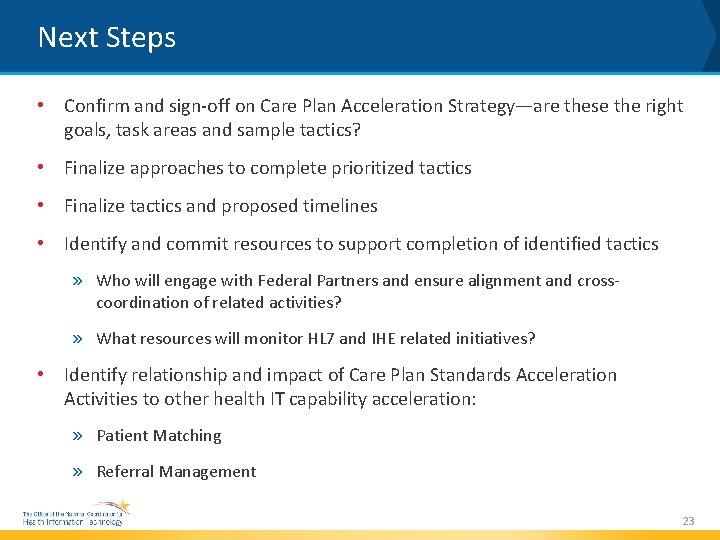
Next Steps • Confirm and sign-off on Care Plan Acceleration Strategy—are these the right goals, task areas and sample tactics? • Finalize approaches to complete prioritized tactics • Finalize tactics and proposed timelines • Identify and commit resources to support completion of identified tactics » Who will engage with Federal Partners and ensure alignment and crosscoordination of related activities? » What resources will monitor HL 7 and IHE related initiatives? • Identify relationship and impact of Care Plan Standards Acceleration Activities to other health IT capability acceleration: » Patient Matching » Referral Management 23