Dr Nabil khouri Integumentary System Consists of 1
Dr. Nabil khouri
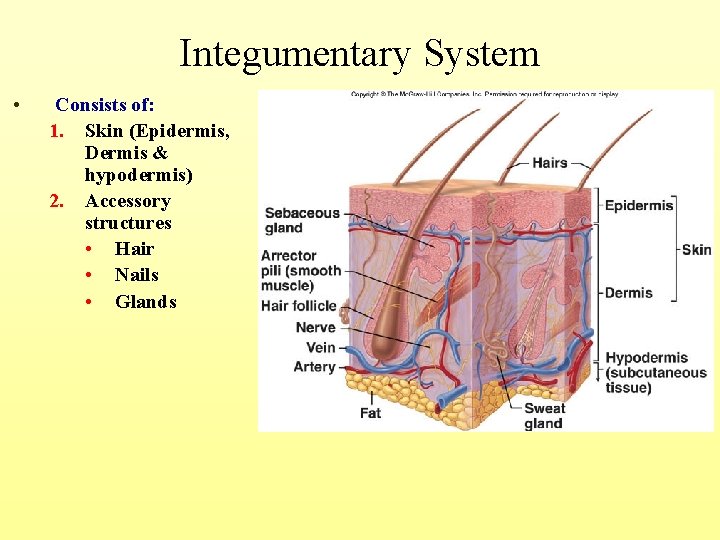
Integumentary System • Consists of: 1. Skin (Epidermis, Dermis & hypodermis) 2. Accessory structures • Hair • Nails • Glands
Functions of the Integumentary System • Protection – Chemical, physical, and mechanical barrier • Body temperature – Regulated by dilation (warming) and constriction (cooling) of dermal vessels • Sweet glands: Termo-regulation, increase secretions for body cooling • Coetaneous sensation – Receptors cells to sense touch and pain • Metabolic functions – Synthesis of vitamin D • Blood reservoir – Skin blood vessels Reservoar : store up to 5% of the body’s blood volume • Excretion – Internal Balance, Control the amount of nitrogenous wastes which are eliminated from the body in sweat – Ion balance. • Absorption - One large door for medical usage – Application.
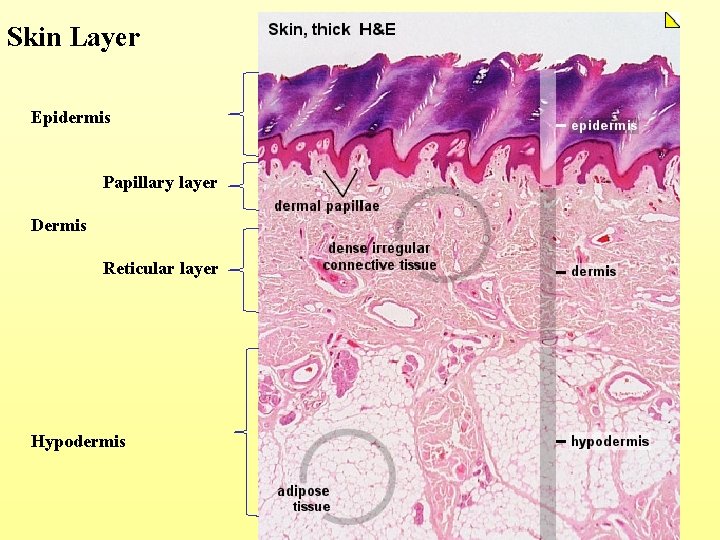
Skin Layer Epidermis Papillary layer Dermis Reticular layer Hypodermis
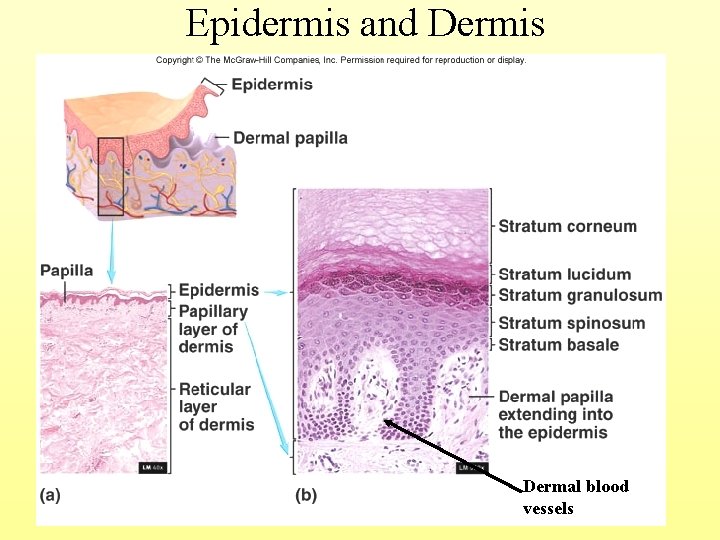
Epidermis and Dermis Dermal blood vessels
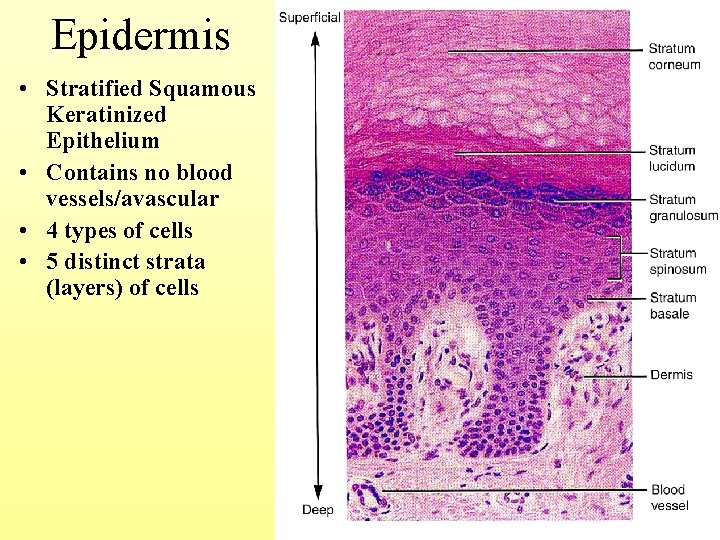
Epidermis • Stratified Squamous Keratinized Epithelium • Contains no blood vessels/avascular • 4 types of cells • 5 distinct strata (layers) of cells 5 -6

Epidermal Cells • Cell types – Keratinocytes: Produce keratin for strength – Melanocytes: Contribute to skin color (pigment melanin) – Langerhans’ cells: Part of the immune system – Merkel’s cells: Detect light touch and pressure • Desquamate: Older cells slough off • Keratinization: the prosses by which the cells die and produce an outer layer that resists abrasion and Impermeabil layer
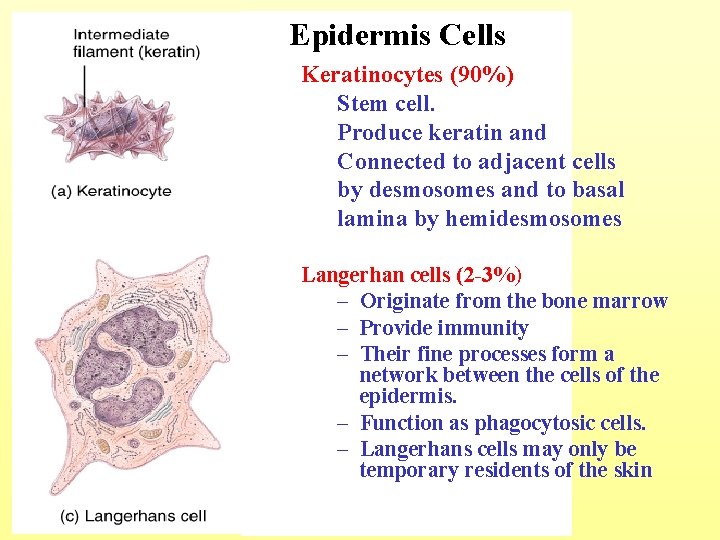
Epidermis Cells Keratinocytes (90%) Stem cell. Produce keratin and Connected to adjacent cells by desmosomes and to basal lamina by hemidesmosomes Langerhan cells (2 -3%) – Originate from the bone marrow – Provide immunity – Their fine processes form a network between the cells of the epidermis. – Function as phagocytosic cells. – Langerhans cells may only be temporary residents of the skin
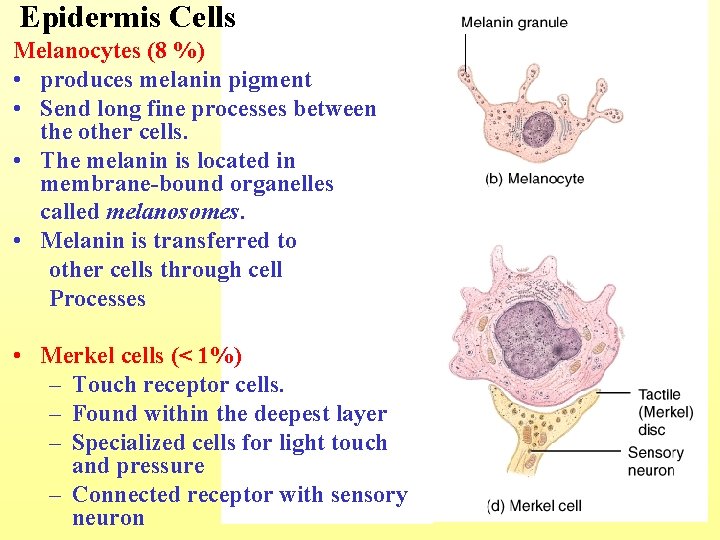
Epidermis Cells Melanocytes (8 %) • produces melanin pigment • Send long fine processes between the other cells. • The melanin is located in membrane-bound organelles called melanosomes. • Melanin is transferred to other cells through cell Processes • Merkel cells (< 1%) – Touch receptor cells. – Found within the deepest layer – Specialized cells for light touch and pressure – Connected receptor with sensory neuron
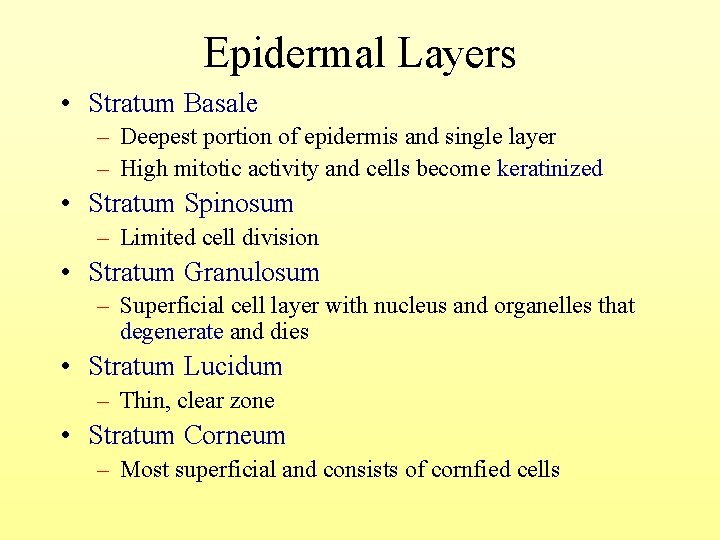
Epidermal Layers • Stratum Basale – Deepest portion of epidermis and single layer – High mitotic activity and cells become keratinized • Stratum Spinosum – Limited cell division • Stratum Granulosum – Superficial cell layer with nucleus and organelles that degenerate and dies • Stratum Lucidum – Thin, clear zone • Stratum Corneum – Most superficial and consists of cornfied cells
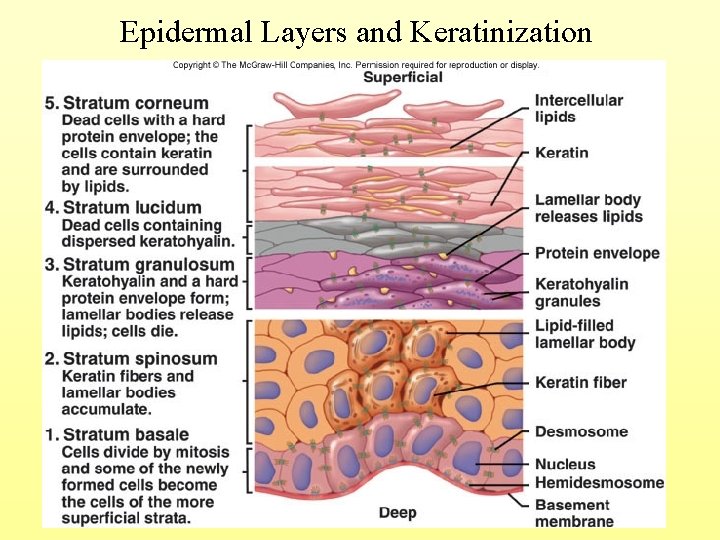
Epidermal Layers and Keratinization

Layers of the Epidermis: Stratum Basale • Basal cells are the stem cells of the epidermis. • The deepest epidermal layer firmly attached to the dermis • Consists of a single layer arranged in one row of columnar or cuboidal cells with intermediate keratine filaments bound by desmosomes • Rest on basement membrane. • Made of the youngest keratinocytes with Mitotic activity - Cells undergo rapid and intense division (alternate name, stratum germinativum). • The renewal of the human epidermis takes about 3 to 4 weeks. 5 -13
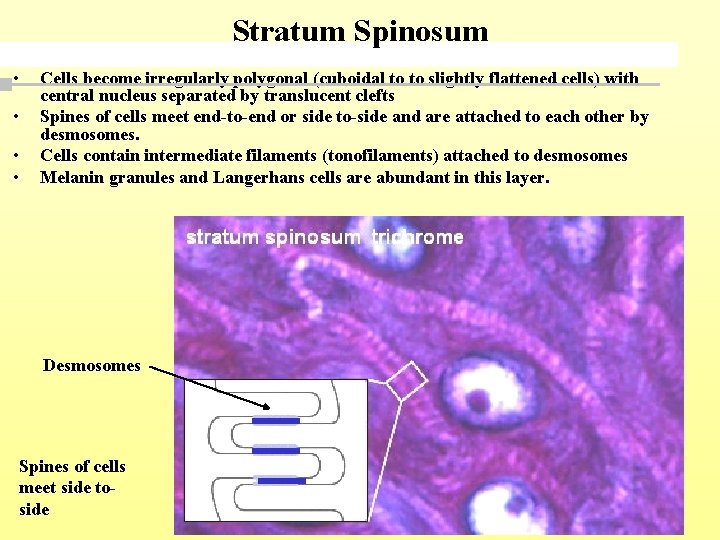
Stratum Spinosum • • Cells become irregularly polygonal (cuboidal to to slightly flattened cells) with central nucleus separated by translucent clefts Spines of cells meet end-to-end or side to-side and are attached to each other by desmosomes. Cells contain intermediate filaments (tonofilaments) attached to desmosomes Melanin granules and Langerhans cells are abundant in this layer. Desmosomes Spines of cells meet side toside
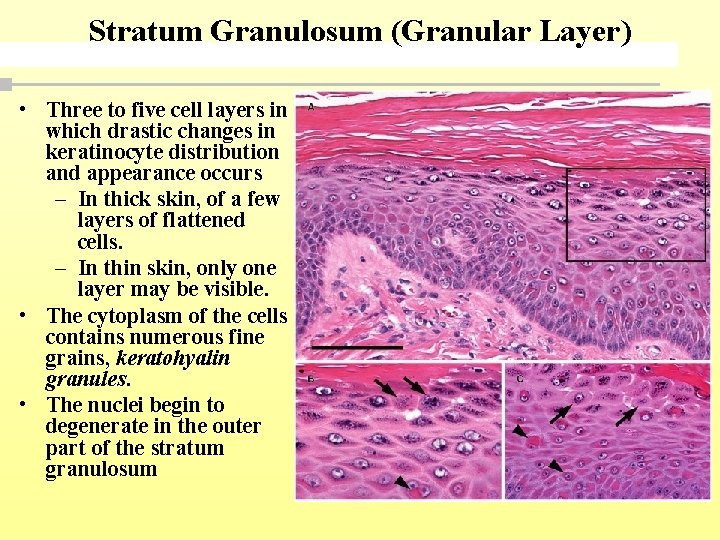
Stratum Granulosum (Granular Layer) • Three to five cell layers in which drastic changes in keratinocyte distribution and appearance occurs – In thick skin, of a few layers of flattened cells. – In thin skin, only one layer may be visible. • The cytoplasm of the cells contains numerous fine grains, keratohyalin granules. • The nuclei begin to degenerate in the outer part of the stratum granulosum
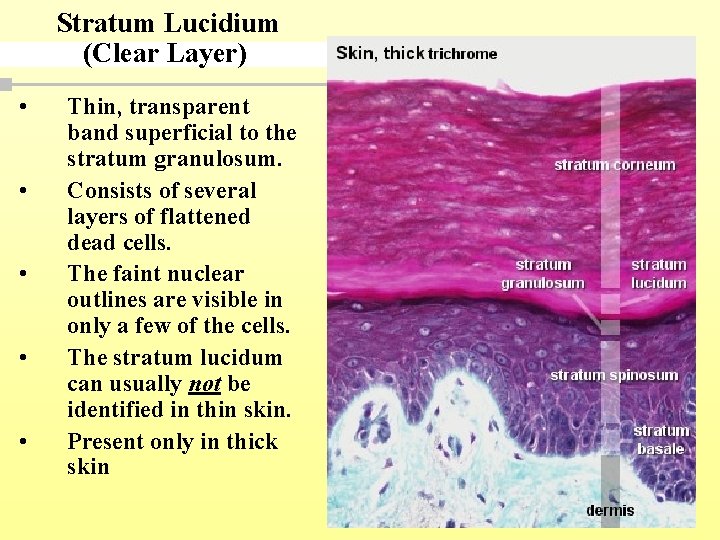
Stratum Lucidium (Clear Layer) • • • Thin, transparent band superficial to the stratum granulosum. Consists of several layers of flattened dead cells. The faint nuclear outlines are visible in only a few of the cells. The stratum lucidum can usually not be identified in thin skin. Present only in thick skin

Stratum Corneum • • Outermost layer of keratinized cells (1520 layers) cells are completely filled with keratin filaments (horny cells) which are embedded in a dense matrix of proteins. Accounts for three quarters of the epidermal thickness Individual cells are difficult to observe because – (1) nuclei can no longer be identified – (2) the cells are very flat and have protein envelop – (3) the space between the cells has been filled with lipids, which cement the cells together into a continuous membrane.
Other important notes • The red coloration of the skin are due to haemoglobin in the red blood cells, which pass through the capillaries beneath the epidermis. • Yellow coloration of the skin are due to carotene, which could accumulates in fat cells found in the dermis and hypodermis. 5 -18

Thick & Thin skin 5 -19
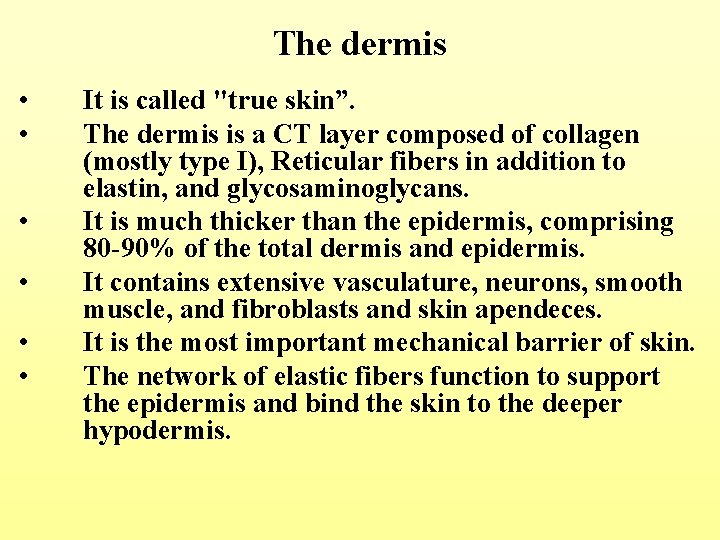
The dermis • • • It is called "true skin”. The dermis is a CT layer composed of collagen (mostly type I), Reticular fibers in addition to elastin, and glycosaminoglycans. It is much thicker than the epidermis, comprising 80 -90% of the total dermis and epidermis. It contains extensive vasculature, neurons, smooth muscle, and fibroblasts and skin apendeces. It is the most important mechanical barrier of skin. The network of elastic fibers function to support the epidermis and bind the skin to the deeper hypodermis.

Dermis – Structural strength – Two layers • Papillary layer: Superficial layer underneath epidermis - Loose connective tissue • Reticular layer: Deeper layer - Dense connective tissue; stretch marks (striae)
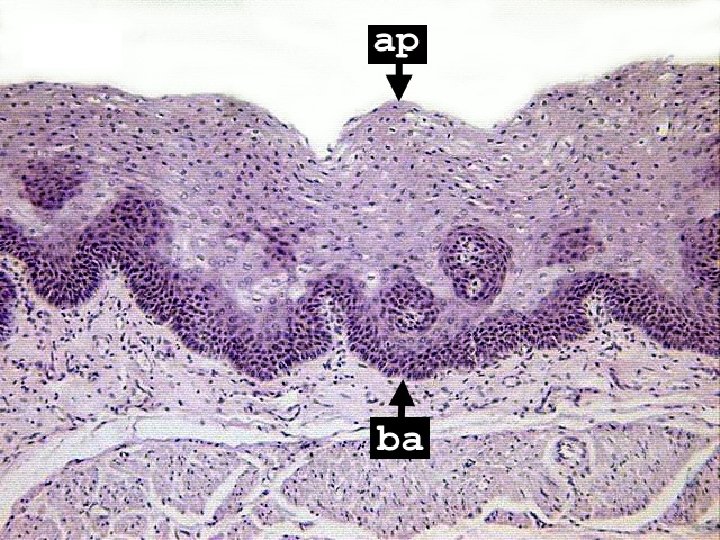
The Dermis “Papillary layer” • The papillary layer is a relatively thin layer of loose connective tissue that lies immediately beneath the epidermis. • This layer consists of loose connective tissue, cell-rich connective tissue, which fills a hollows finger–like projection at the deep surface called dermal papillae. • A key feature of this layer is the dermal ridges (dermal papillae) that extend up in ridges into the overlying epidermis and interdigitate with epidermal invaginations (epidermal ridges). • A double row of dermal papillae in finger pads produces the ridged fingerprints on fingertips. – The dermal ridges contain Meissner’s corpuscles, encapsulated nerve endings, and capillary loops that provide nutrients to the avascular epidermis. – A basal lamina supports the basal layer of the epidermis. – Collagen and elastic fibers underlie the basal lamina. – Fibroblasts, mast cells, and macrophages occupy the papillary layer. Collagen fibres appear finer than in the reticular layer.

DP

The reticular layer • The reticular layer resides below the papillary layer. • The reticular layer appears dense and contains fewer cells • It is comprised of thick criss-crossing collagen fibers aggregate into bundles. These fibers form an interlacing network with direction that is parallel to the surface of the skin called cleavage (Langer's) lines. • Usually, their main orientation will follow the "lines of greatest tension" in the skin (Kraissl lines) • Elastic fibers (irregular dense connective tissue) together with relatively few cells are present
Arteries and veins of the dermis – Run through the hypodermis and branch upward to form plexuses of anatomizing vessels. – The coetaneous plexus resides at the junction of the hypodermis and dermis, and the papillary plexus resides just beneath the epidermis within the dermal papilla. • This system provides nourishment to the dermis and by diffusion to the epidermis, which is a-vascular. • The vascular system functions in thermoregulation. Blood flow is controlled by contraction of arterioles and venules they send blood through the capillary bed for heat radiation. • In some regions of skin, arterial-venous anatomizes, or shunts, can send blood directly from the arterioles to venules in order to reduce heat loss.

Receptors in Skin Classification by Location • Exteroceptors – sensitive to stimuli arising from outside the body – Located at or near body surfaces – Include receptors for touch, pressure, pain, and temperature • Interoceptors – (visceroceptors) receive stimuli from internal viscera – Monitor a variety of stimuli • Proprioceptors – monitor degree of stretch – Located in kin covering musculoskeletal organs

Classification by Modality • • • Mechanoreceptors – respond to mechanical forces Thermoreceptors – respond to temperature changes Chemoreceptors – respond to chemicals in solution Photoreceptors – respond to light – located in the eye Nociceptors – respond to harmful stimuli that result in pain • Divided into two groups • Free nerve endings “unencapsulated” • Encapsulated nerve endings
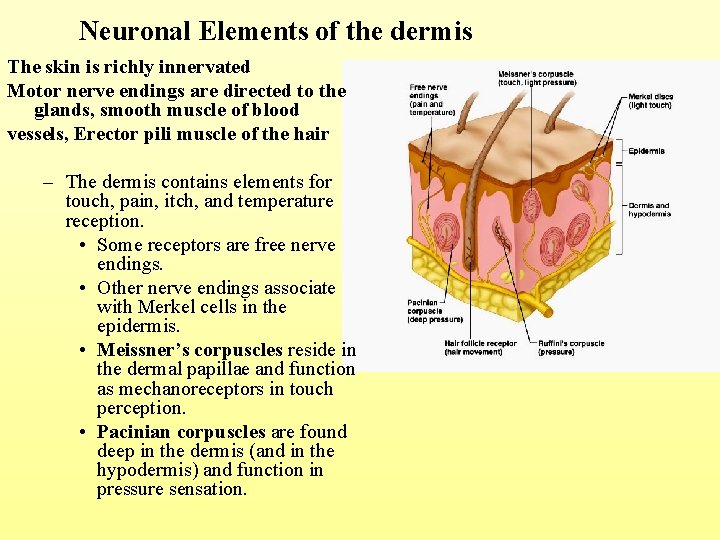
Neuronal Elements of the dermis The skin is richly innervated Motor nerve endings are directed to the glands, smooth muscle of blood vessels, Erector pili muscle of the hair – The dermis contains elements for touch, pain, itch, and temperature reception. • Some receptors are free nerve endings. • Other nerve endings associate with Merkel cells in the epidermis. • Meissner’s corpuscles reside in the dermal papillae and function as mechanoreceptors in touch perception. • Pacinian corpuscles are found deep in the dermis (and in the hypodermis) and function in pressure sensation.
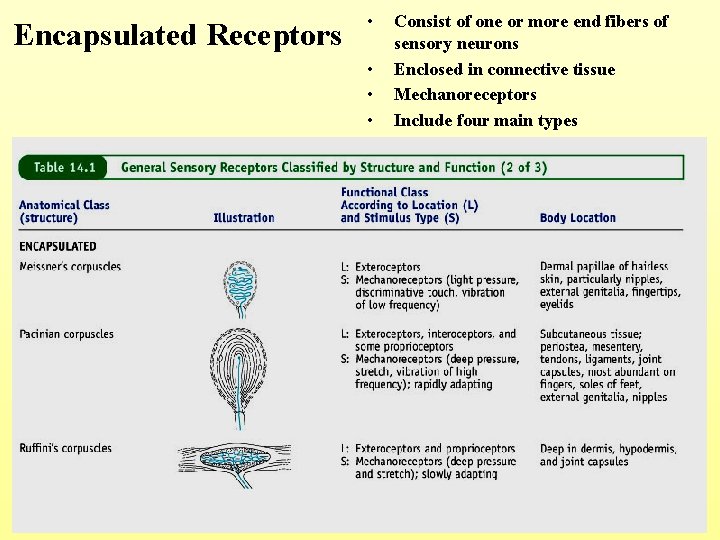
Encapsulated Receptors • • Consist of one or more end fibers of sensory neurons Enclosed in connective tissue Mechanoreceptors Include four main types 5 -30

Meissner’s corpuscle Encapsulated nerve ending in the dermal papilla of glabrous skin; light pressure and touch receptors sensitive to low frequency stimuli

Pacinian corpuscles Axon looses myelin and passes as a single process into a concentrically layered capsule (combination of CT and Schwann cells). Found deep in the dermis and in the hypodermis; sense the vibration and pressure
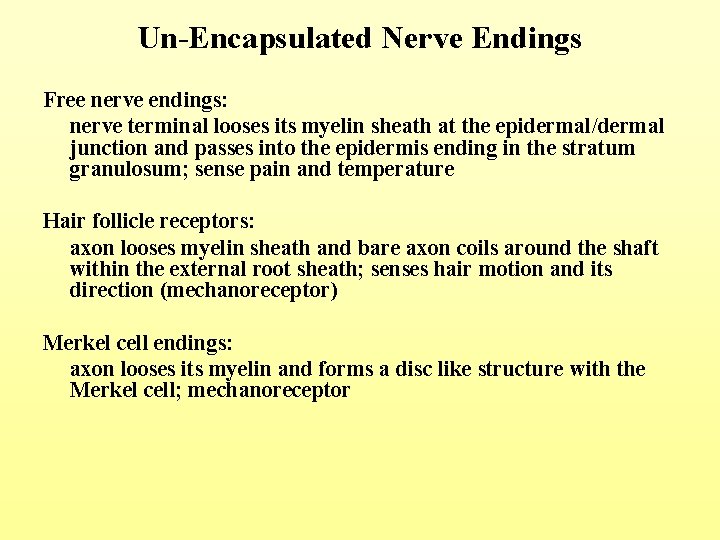
Un-Encapsulated Nerve Endings Free nerve endings: nerve terminal looses its myelin sheath at the epidermal/dermal junction and passes into the epidermis ending in the stratum granulosum; sense pain and temperature Hair follicle receptors: axon looses myelin sheath and bare axon coils around the shaft within the external root sheath; senses hair motion and its direction (mechanoreceptor) Merkel cell endings: axon looses its myelin and forms a disc like structure with the Merkel cell; mechanoreceptor
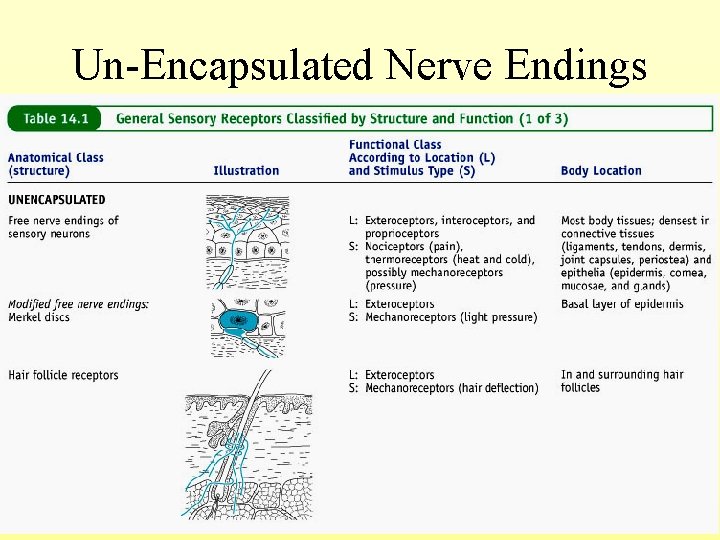
Un-Encapsulated Nerve Endings 5 -34


Hypodermis • Skin rests on this, but not a part • Also called – Subcutaneous tissue – Superficial fascia • Consists of loose connective tissue • Types of cells – Fibroblasts – Adipose (fat) cells – Macrophages • Subcutaneous fat

Epidermal appendages • Hair – Found everywhere on human body except palms, soles, lips, nipples, parts of external genitalia, and distal segments of fingers and toes • Nails • Glands – Sebaceous or oil glands – Sudoriferous or sweat glands – Mammary glands

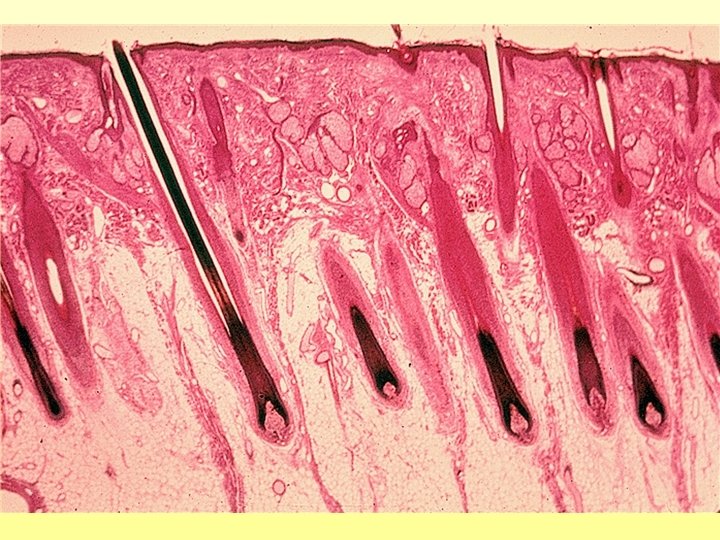
Hair (Pilus) – is composed of dead epidermal cells that have undergone a modified epidermal keratinization including the expression of specific keratin proteins that are highly crosslinked by disulfide bonds. – It is derived from hair folicles, which are epidermal invaginations that project into the dermis or hypodermis. • Two types of hair are present on humans: – Vellus (fine) hair, which is short, soft, fine, and pale – Terminal (thick) hair, which is hard, large, coarse, long and dark. » The number of hairs on all primates is similar, but most is vellus on humans and terminal on other primates.

Hair structure • Composed of shaft and root – Shaft protrudes above skin surface – Root located below surface and base forms the hair bulb • Pigmented by melanocytes at the base of the hair
5 -40
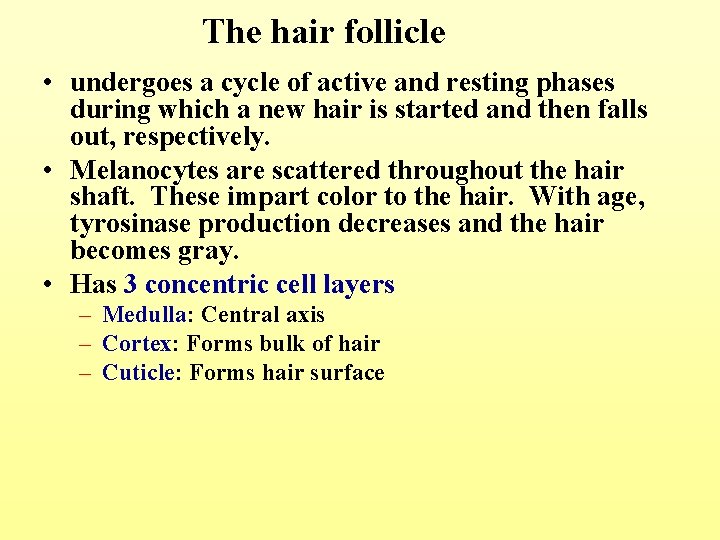
The hair follicle • undergoes a cycle of active and resting phases during which a new hair is started and then falls out, respectively. • Melanocytes are scattered throughout the hair shaft. These impart color to the hair. With age, tyrosinase production decreases and the hair becomes gray. • Has 3 concentric cell layers – Medulla: Central axis – Cortex: Forms bulk of hair – Cuticle: Forms hair surface
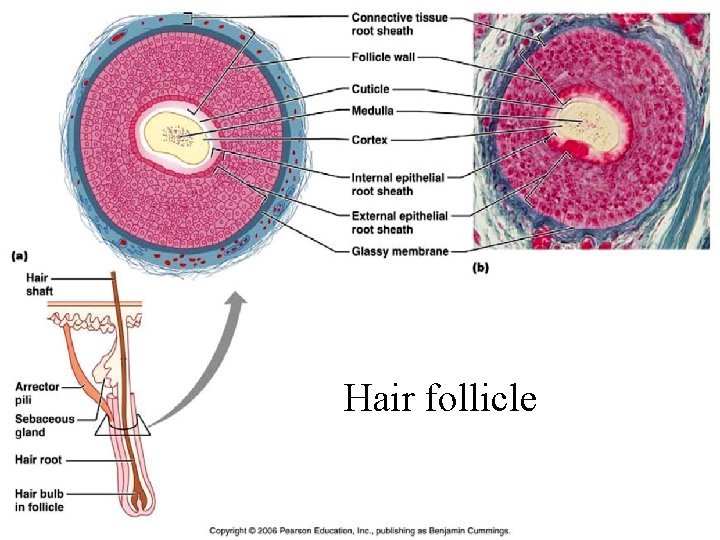
Hair follicle 5 -42
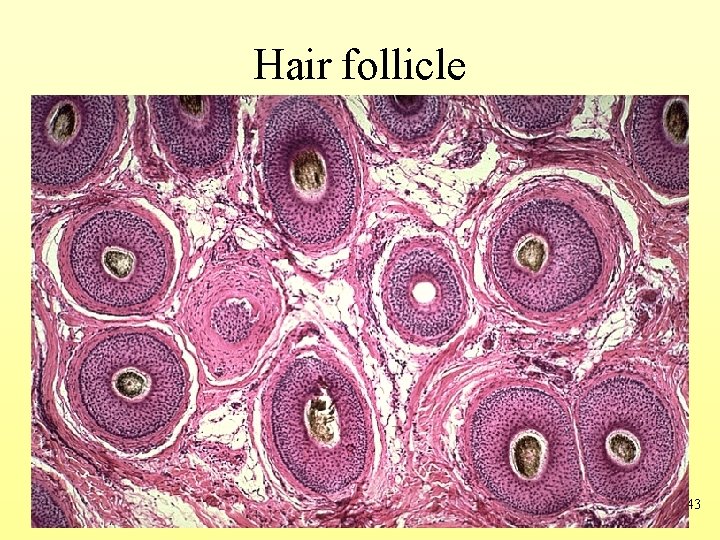
Hair follicle 5 -43

Hair Bulb • The root sheath extending from the epidermal surface into the dermis • Deep end is expanded forming a hair bulb • A knot of sensory nerve endings (a root hair plexus) wraps around each hair bulb • Bending a hair stimulate these ending hence our hairs act as Sensitive touch receptors

Hair bulb 5 -45

5 -46
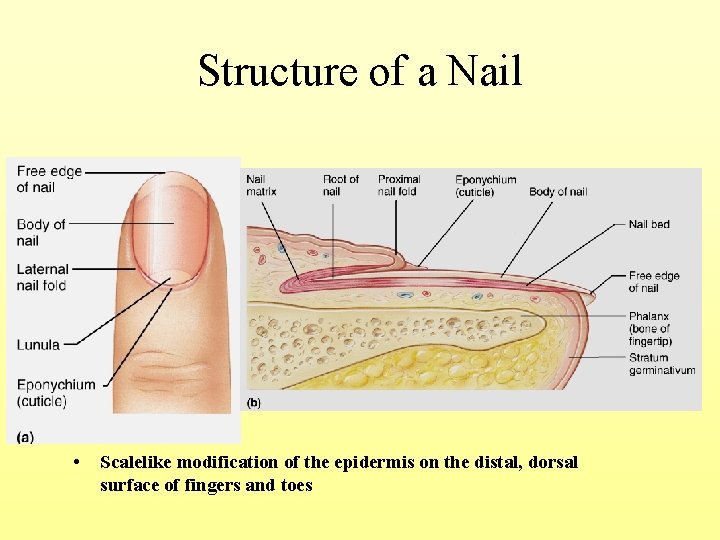
Structure of a Nail • Scalelike modification of the epidermis on the distal, dorsal surface of fingers and toes

Holocrine Seb. Gl Glands Merocrine Seb. Gl 5 -48

MODES OF SECRETORY RELEASE HOLOCRINE rare SEBUM MEROCRINE / ECCRINE secretion released, filling a dead cell Sebaceous gland Simple coiled tubular glands secretion released by exocytosis, with no loss of cytoplasm Clear & Dark released by exocytosis, with a little loss of cytoplasm APOCRINE rare

Skin glands 5 -50
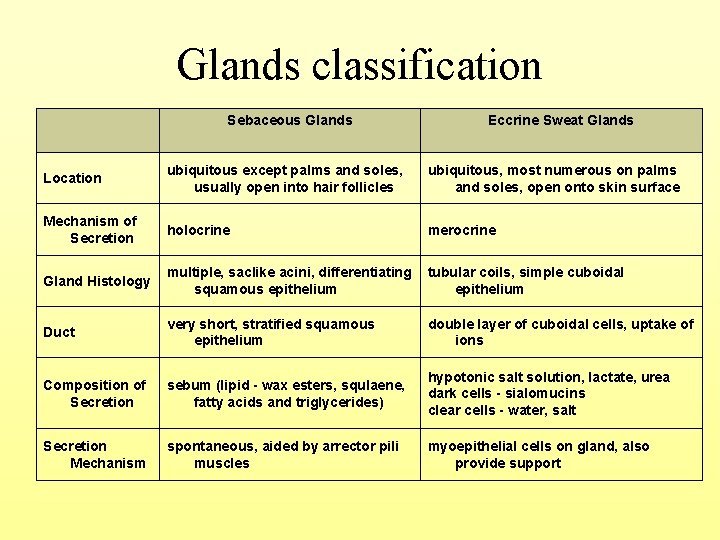
Glands classification Sebaceous Glands Eccrine Sweat Glands Location ubiquitous except palms and soles, usually open into hair follicles ubiquitous, most numerous on palms and soles, open onto skin surface Mechanism of Secretion holocrine merocrine Gland Histology multiple, saclike acini, differentiating squamous epithelium tubular coils, simple cuboidal epithelium Duct very short, stratified squamous epithelium double layer of cuboidal cells, uptake of ions Composition of Secretion sebum (lipid - wax esters, squlaene, fatty acids and triglycerides) hypotonic salt solution, lactate, urea dark cells - sialomucins clear cells - water, salt Secretion Mechanism spontaneous, aided by arrector pili muscles myoepithelial cells on gland, also provide support
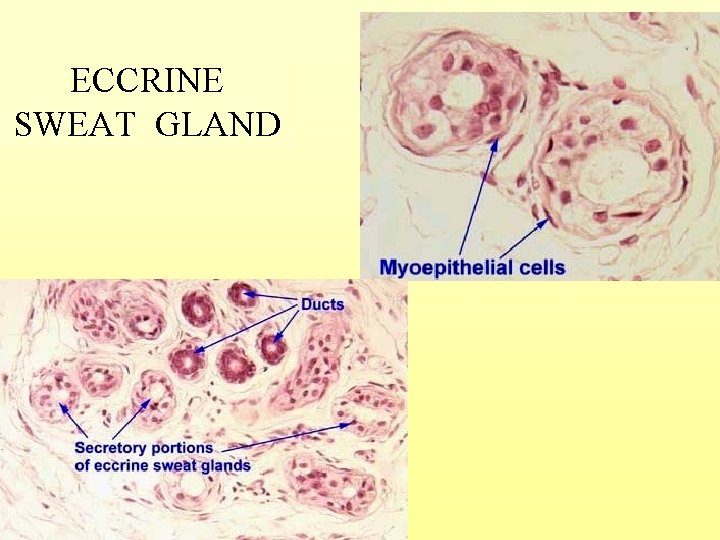
ECCRINE SWEAT GLAND
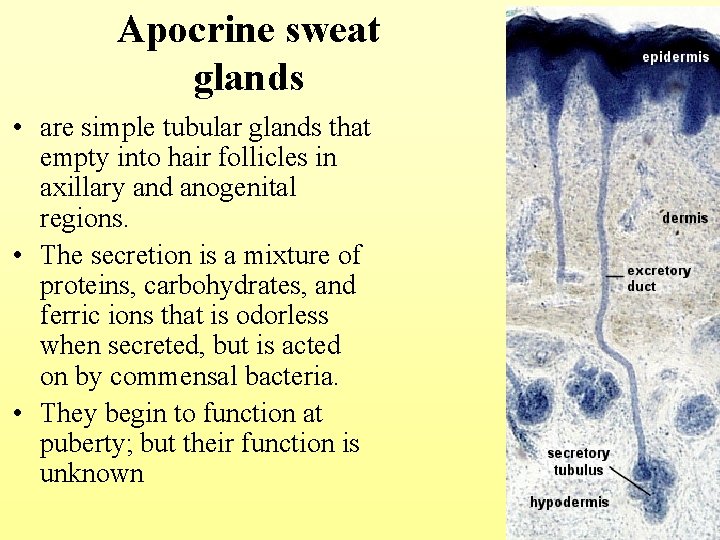
Apocrine sweat glands • are simple tubular glands that empty into hair follicles in axillary and anogenital regions. • The secretion is a mixture of proteins, carbohydrates, and ferric ions that is odorless when secreted, but is acted on by commensal bacteria. • They begin to function at puberty; but their function is unknown 5 -53
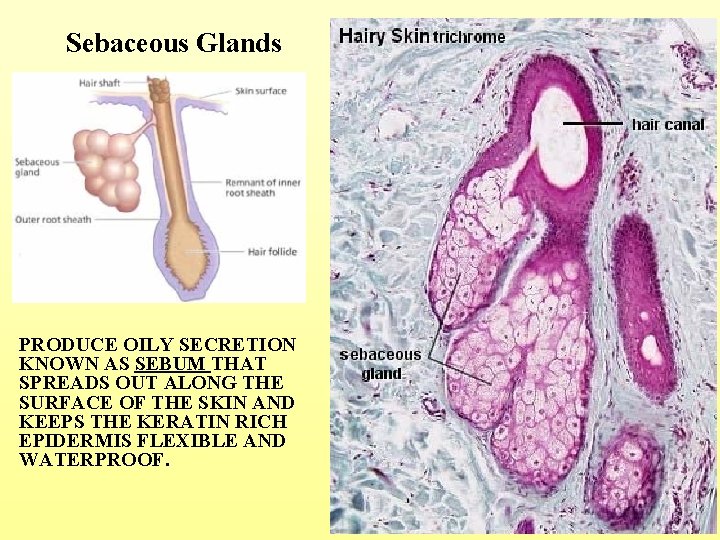
Sebaceous Glands PRODUCE OILY SECRETION KNOWN AS SEBUM THAT SPREADS OUT ALONG THE SURFACE OF THE SKIN AND KEEPS THE KERATIN RICH EPIDERMIS FLEXIBLE AND WATERPROOF. 5 -54
- Slides: 54