Dr Martin Connor Special Advisor Special Delivery Unit





- Slides: 46

Dr. Martin Connor Special Advisor Special Delivery Unit, DH
HMI Briefing Martin Connor 3 rd October 2011
SDU so far 1) Established as management team at start September 2) Delivery through associated partners: 1) Clinical Programmes 2) ISD 3) CPCP 4) Quality and Patient Safety 5) NTPF 3) Ministerial remit to resolve problems 4) Supporting HSE performance management through existing processes: ISD and RDOs
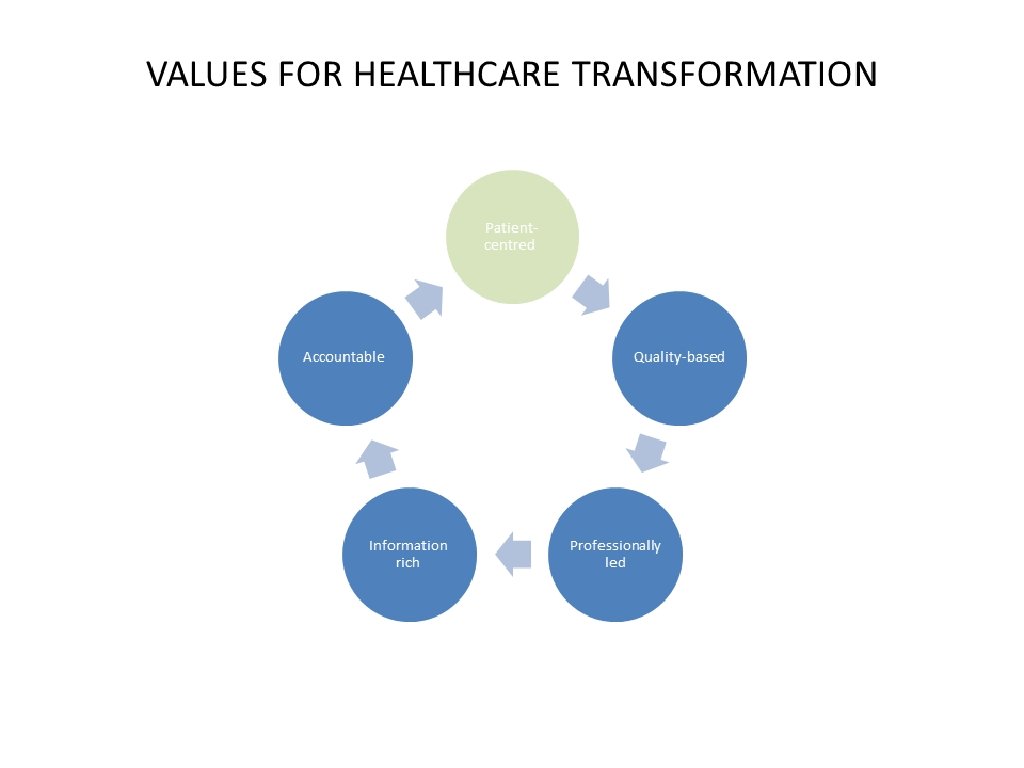
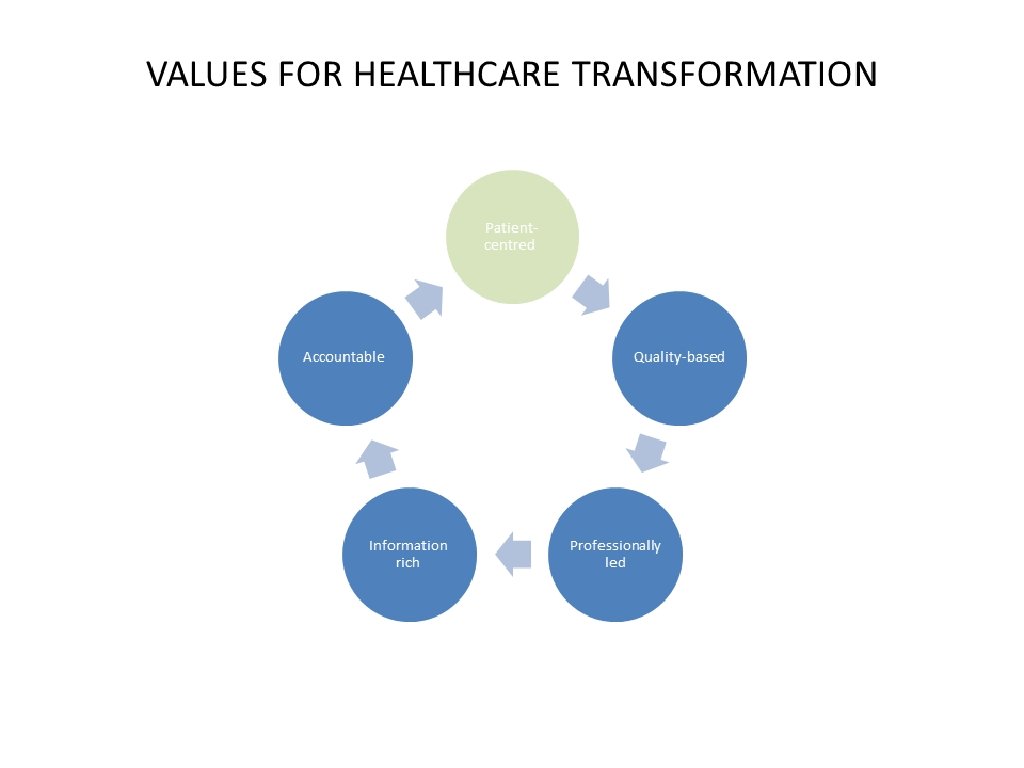
The strategy cannot be about marginal adjustment – it has to be about system transformation
Values
OVERVIEW OF SDU ACCESS STRATEGY

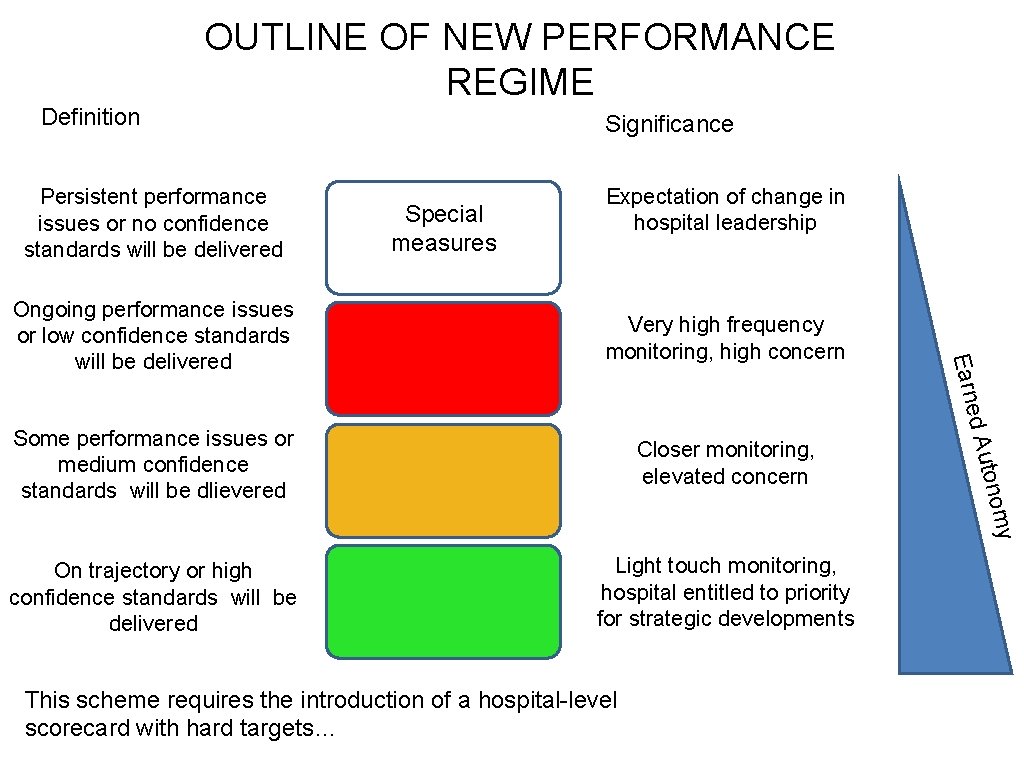
New performance management arrangements

PERFORMANCE IMPROVEMENT We hold leaders personally accountable for performance against KPIs We clarify sanctions and incentives (an essential part of the leadership challenge) WHEEL Escalation Numeric Objectives Intervention Monitoring: Frequency, Quality, Lag We start here with simplified, clearer targets that better reflect the patient journey We establish systematic, comprehensive and high frequency weekly monitoring systems
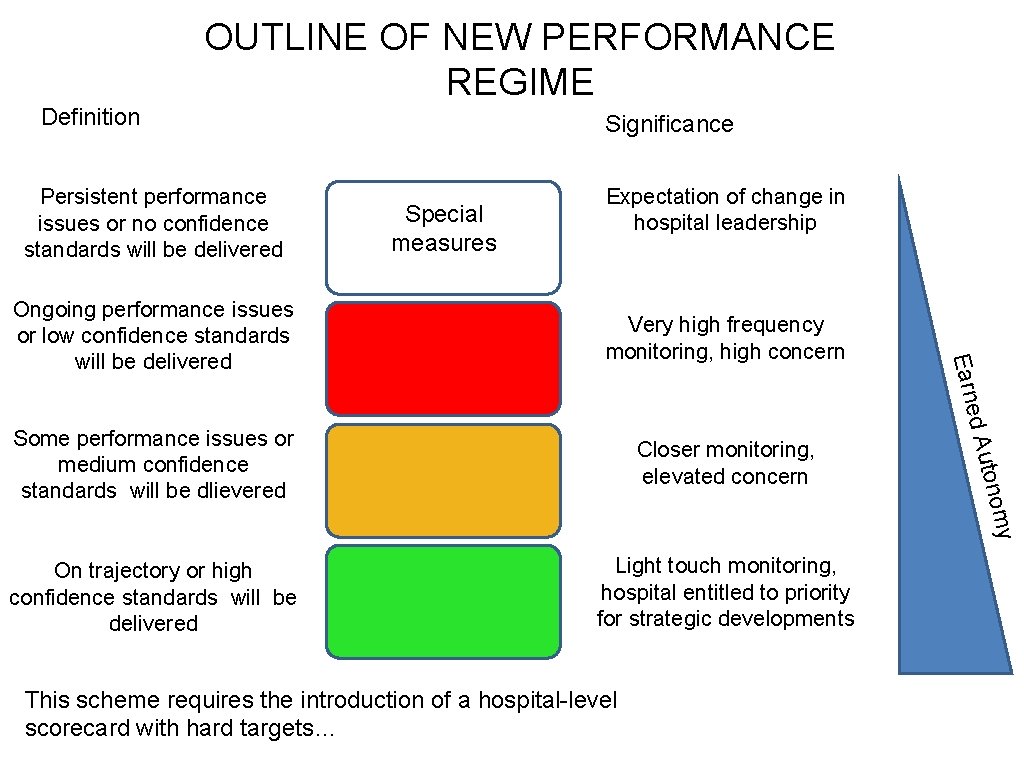
Definition OUTLINE OF NEW PERFORMANCE REGIME Persistent performance issues or no confidence standards will be delivered Significance Special measures Expectation of change in hospital leadership Closer monitoring, elevated concern On trajectory or high confidence standards will be delivered Light touch monitoring, hospital entitled to priority for strategic developments y Some performance issues or medium confidence standards will be dlievered tonom ed Au Very high frequency monitoring, high concern Earn Ongoing performance issues or low confidence standards will be delivered This scheme requires the introduction of a hospital-level scorecard with hard targets…
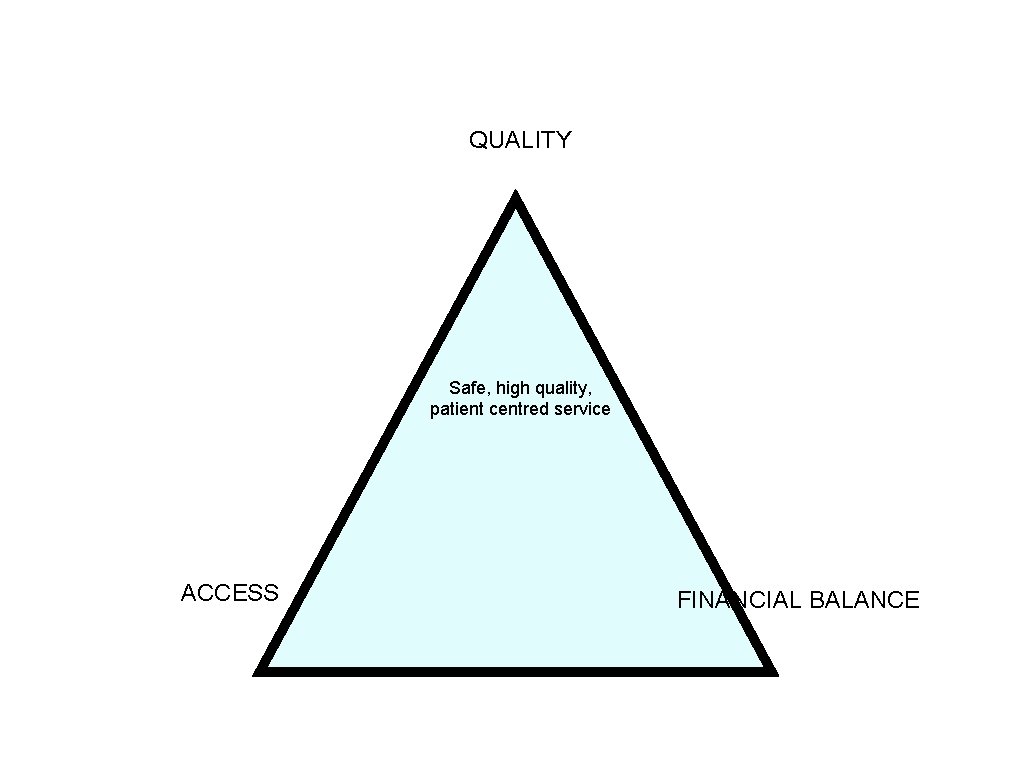
Quality, access, finance: The basis of the new scorecard
QUALITY Safe, high quality, patient centred service ACCESS FINANCIAL BALANCE

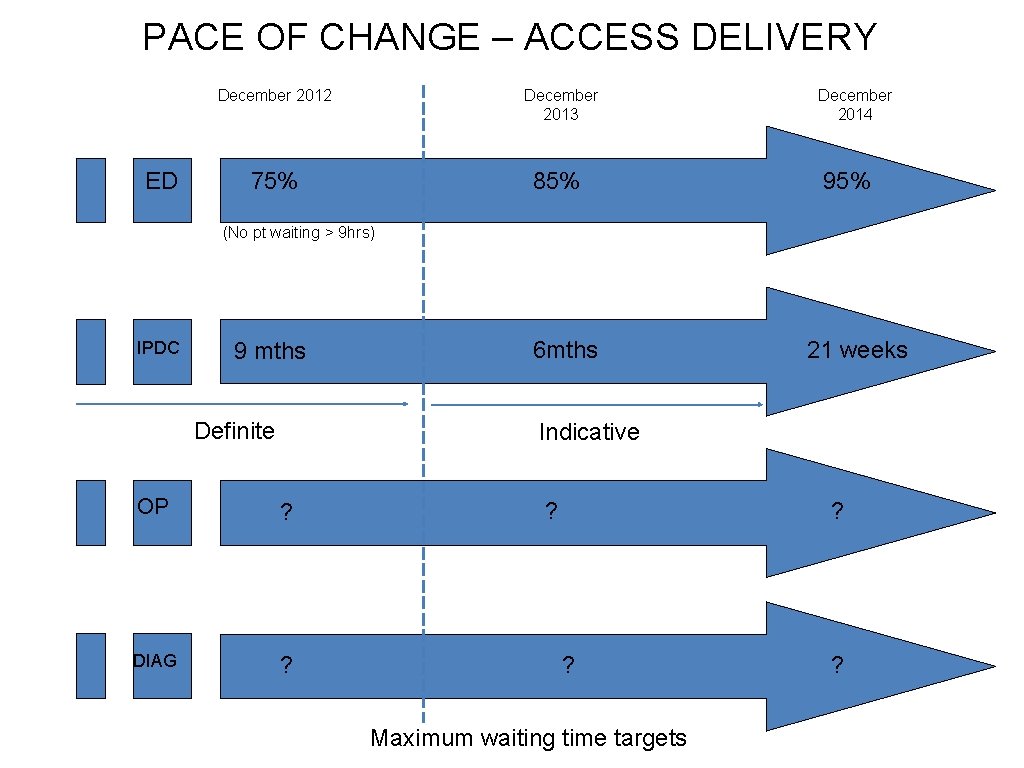
3 YEAR TARGETS
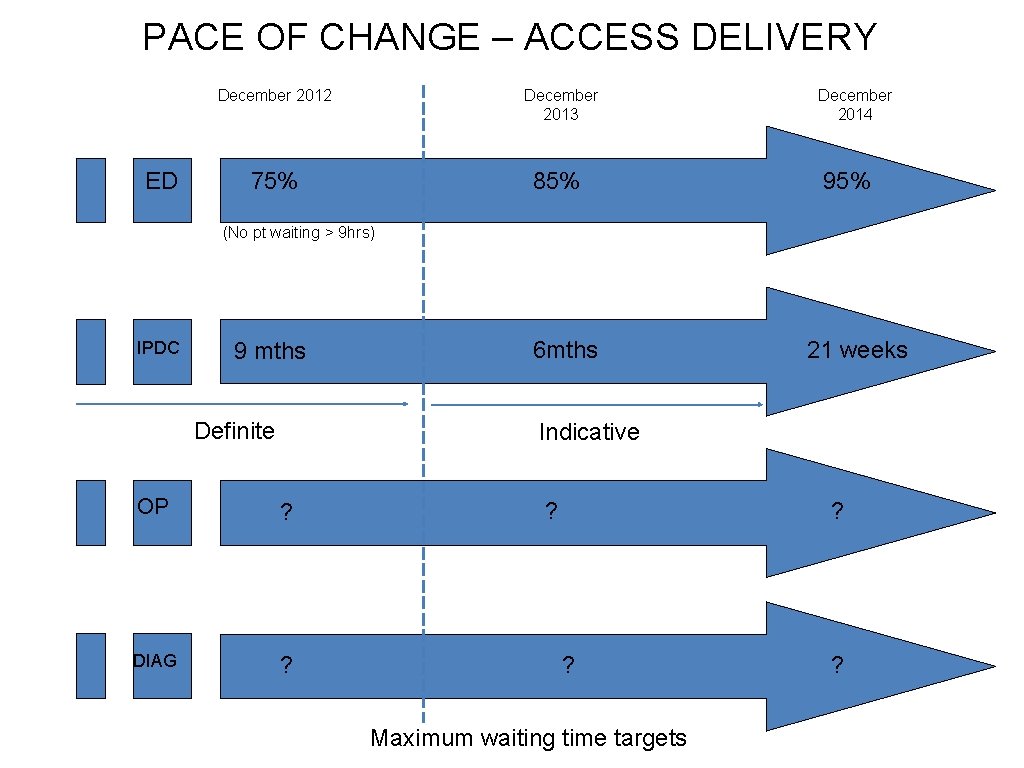
PACE OF CHANGE – ACCESS DELIVERY ED December 2012 December 2013 75% 85% December 2014 95% (No pt waiting > 9 hrs) IPDC 9 mths Definite 6 mths 21 weeks Indicative OP OP ? DIAG ? ? Maximum waiting time targets ?
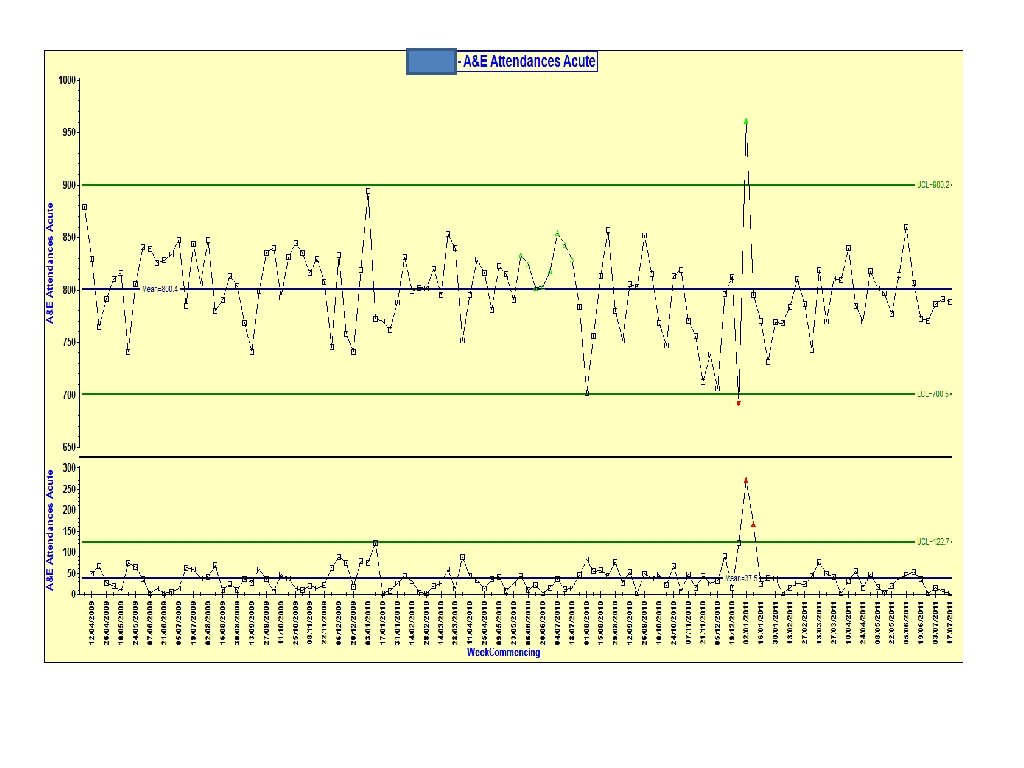
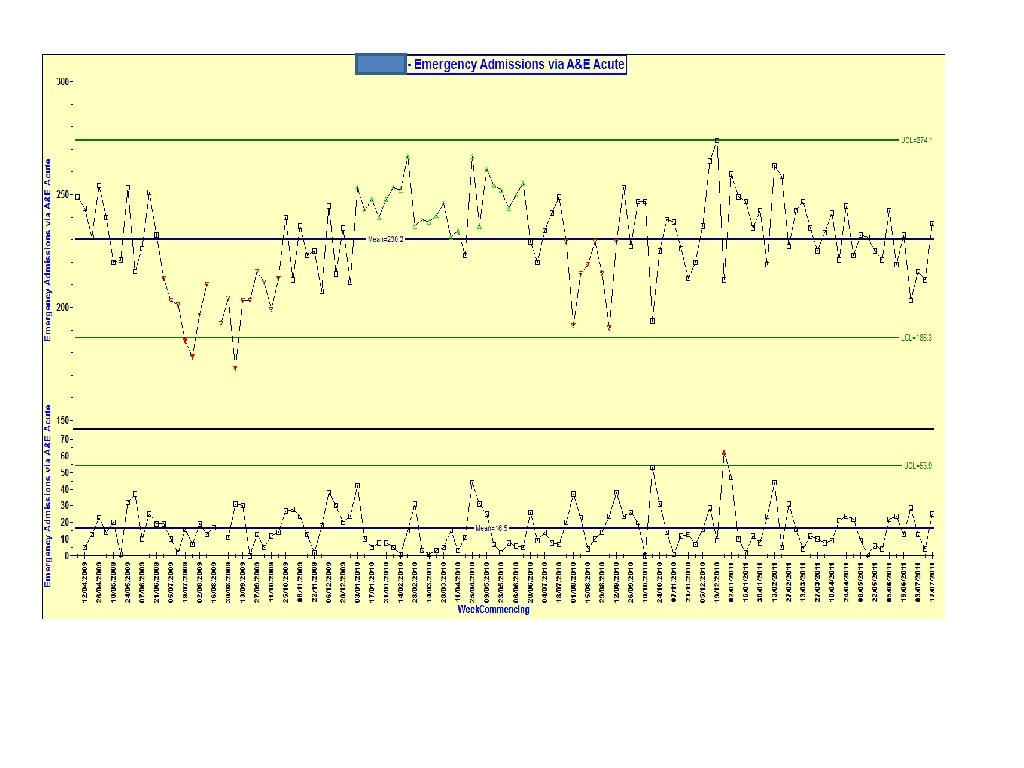
UNSCHEDULED CARE
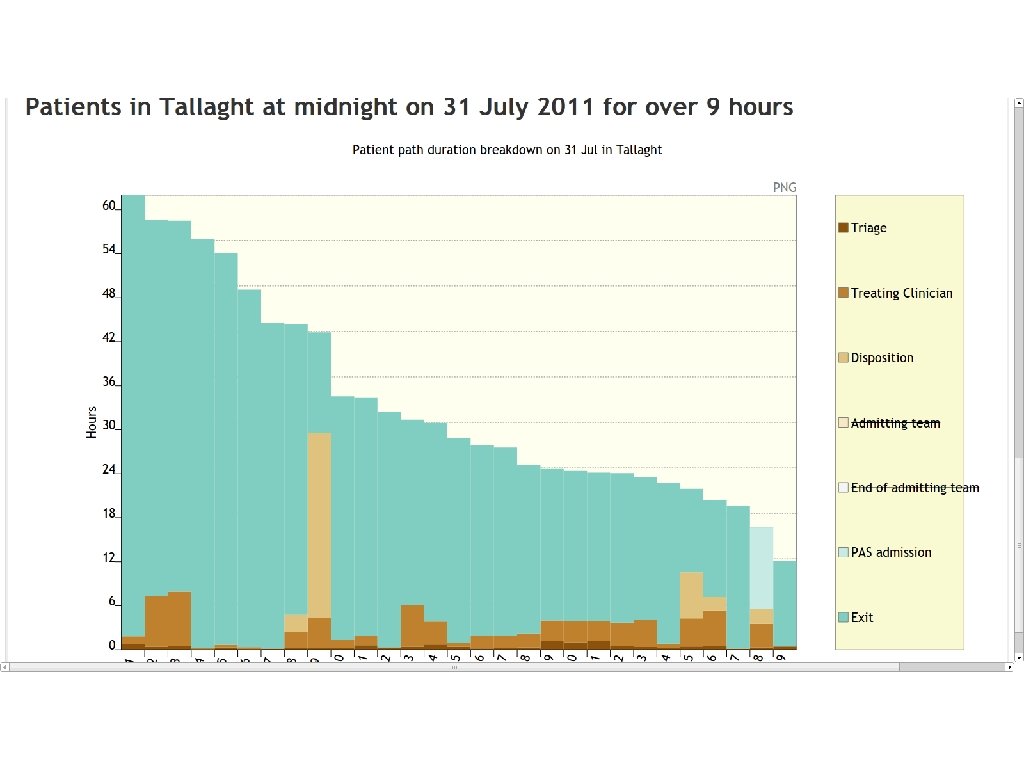
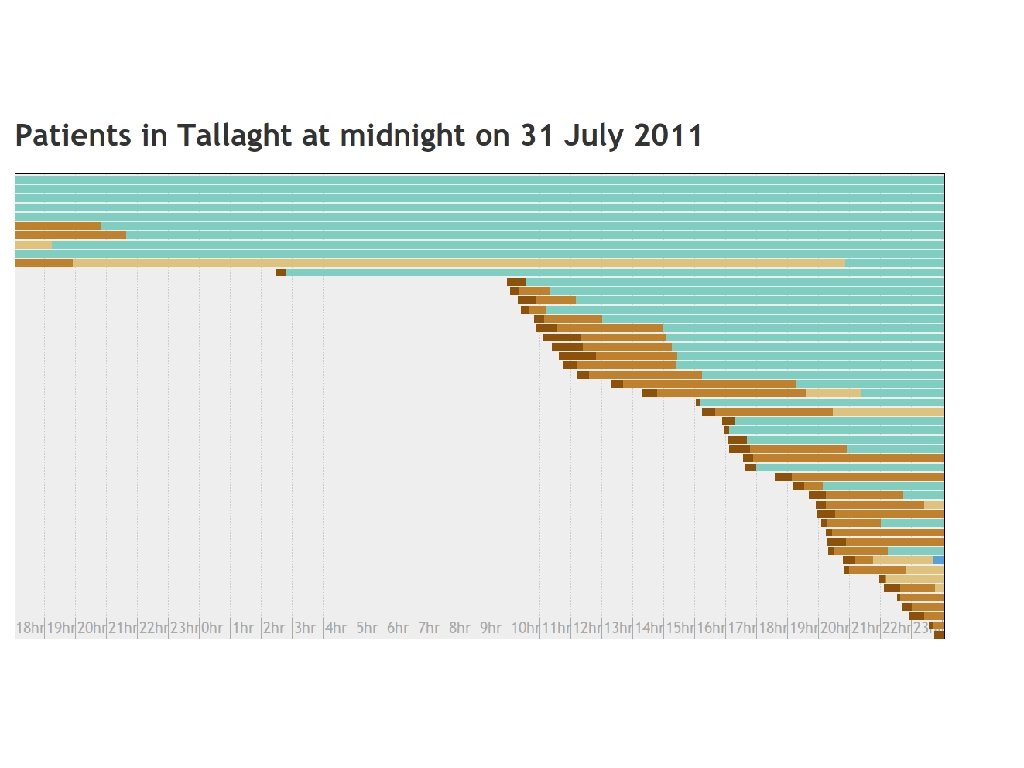
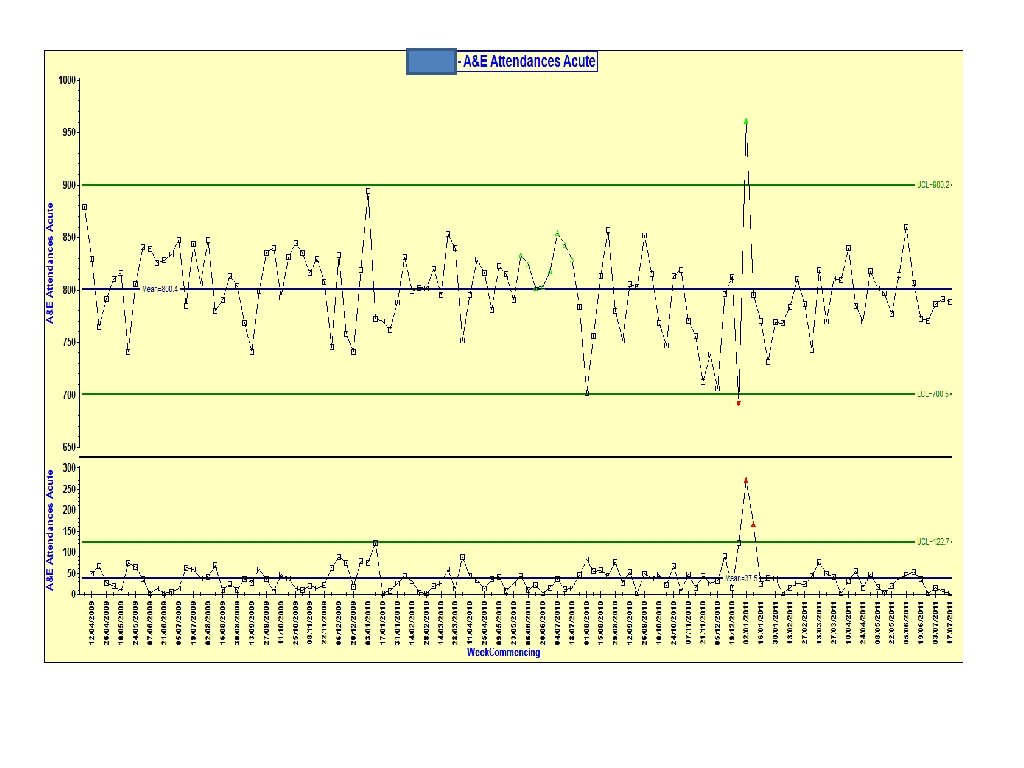
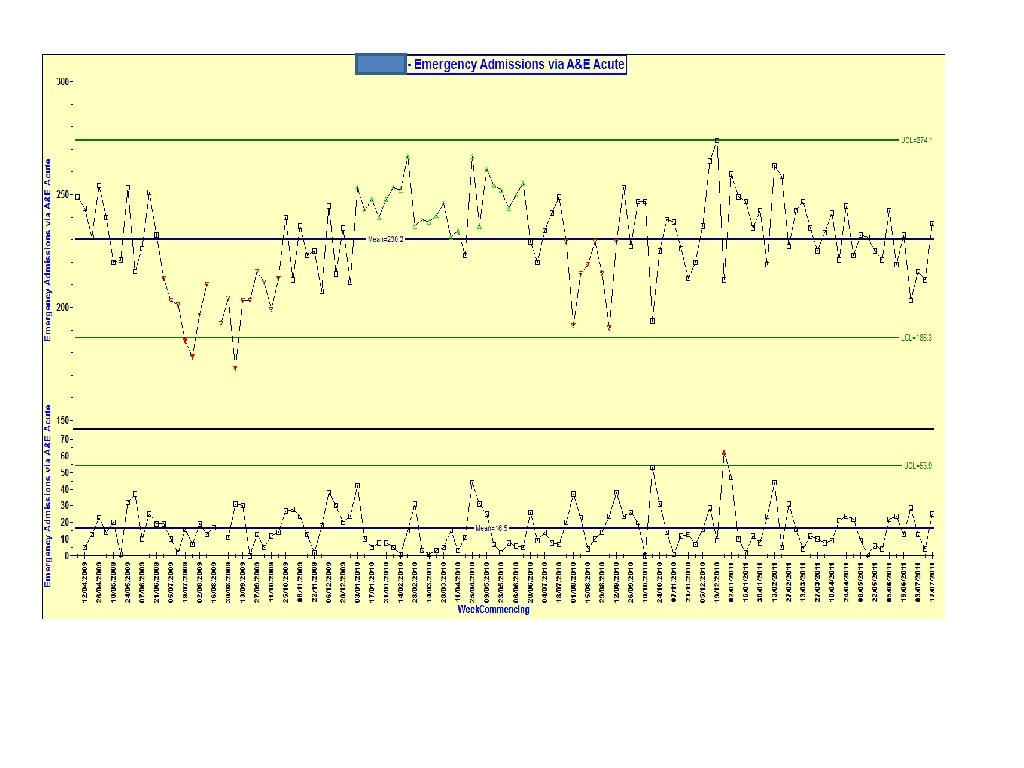
SYSTEMATIC ANALYSIS
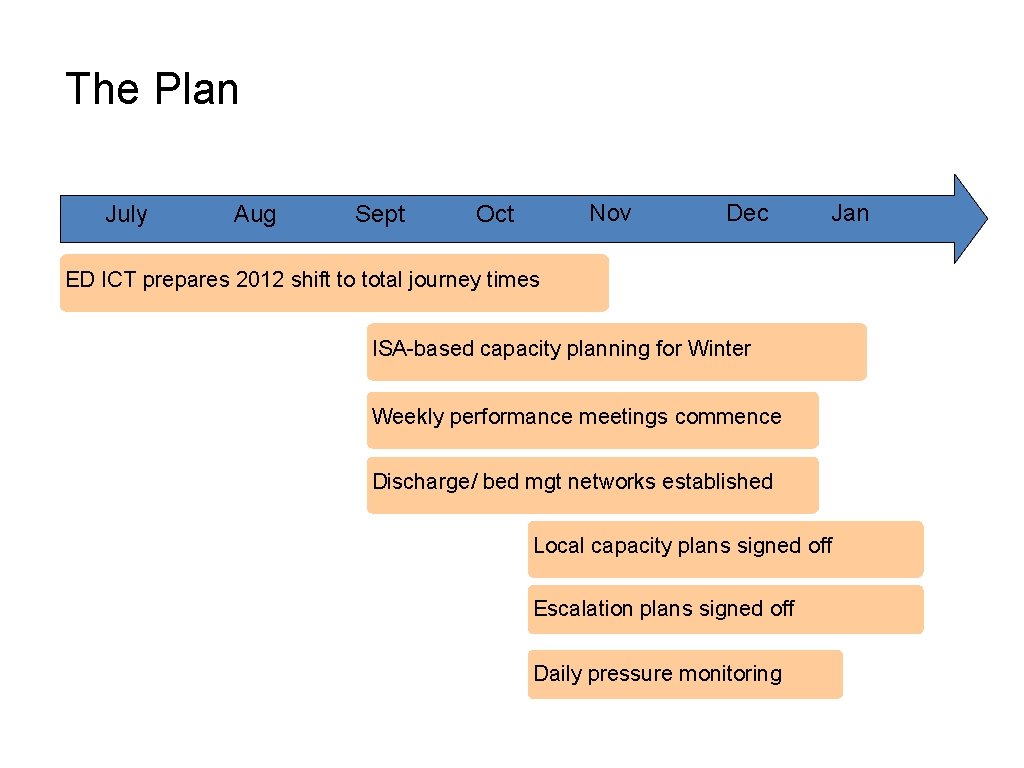
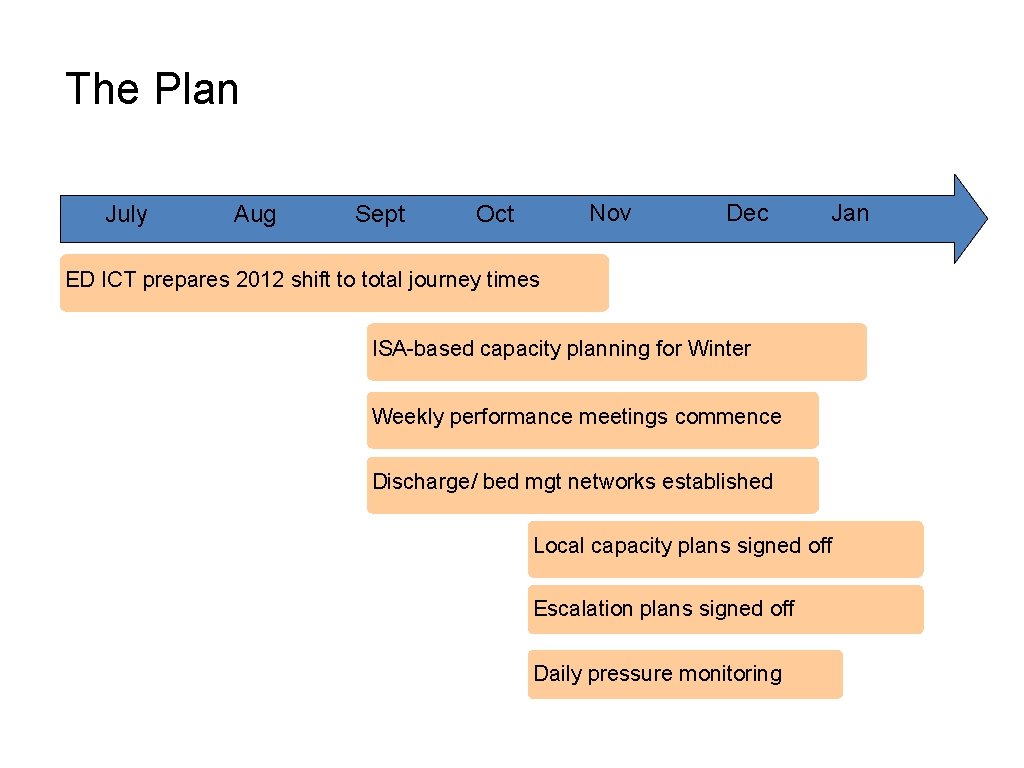
The Plan July Aug Sept Nov Oct Dec Jan ED ICT prepares 2012 shift to total journey times ISA-based capacity planning for Winter Weekly performance meetings commence Discharge/ bed mgt networks established Local capacity plans signed off Escalation plans signed off Daily pressure monitoring
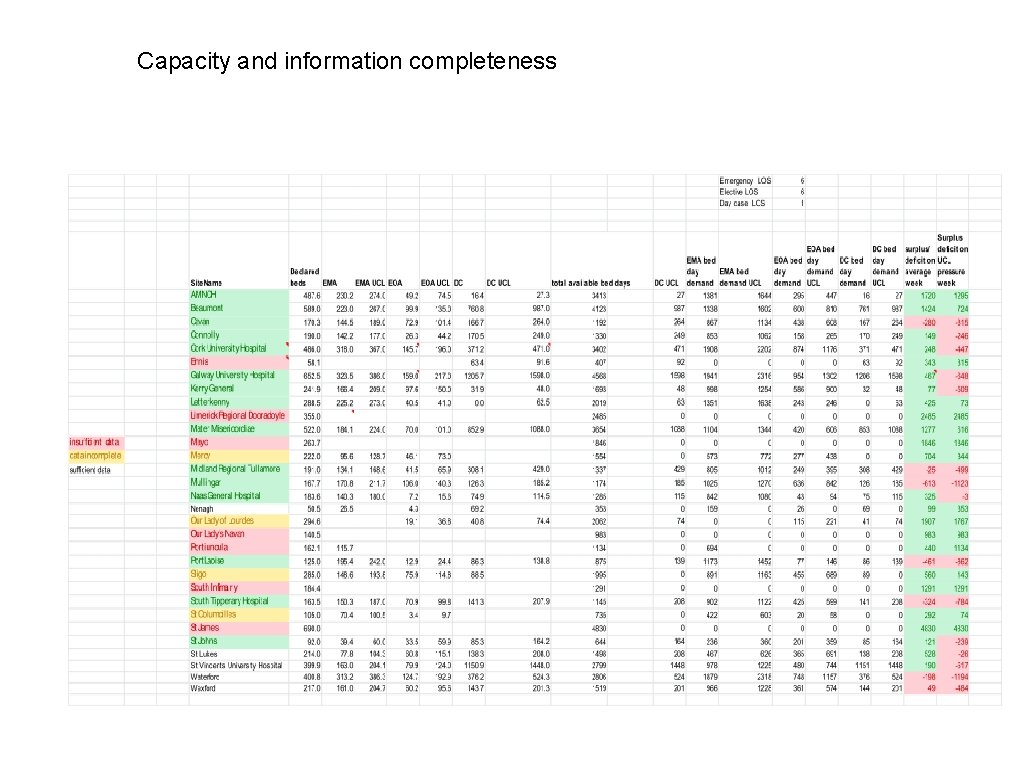
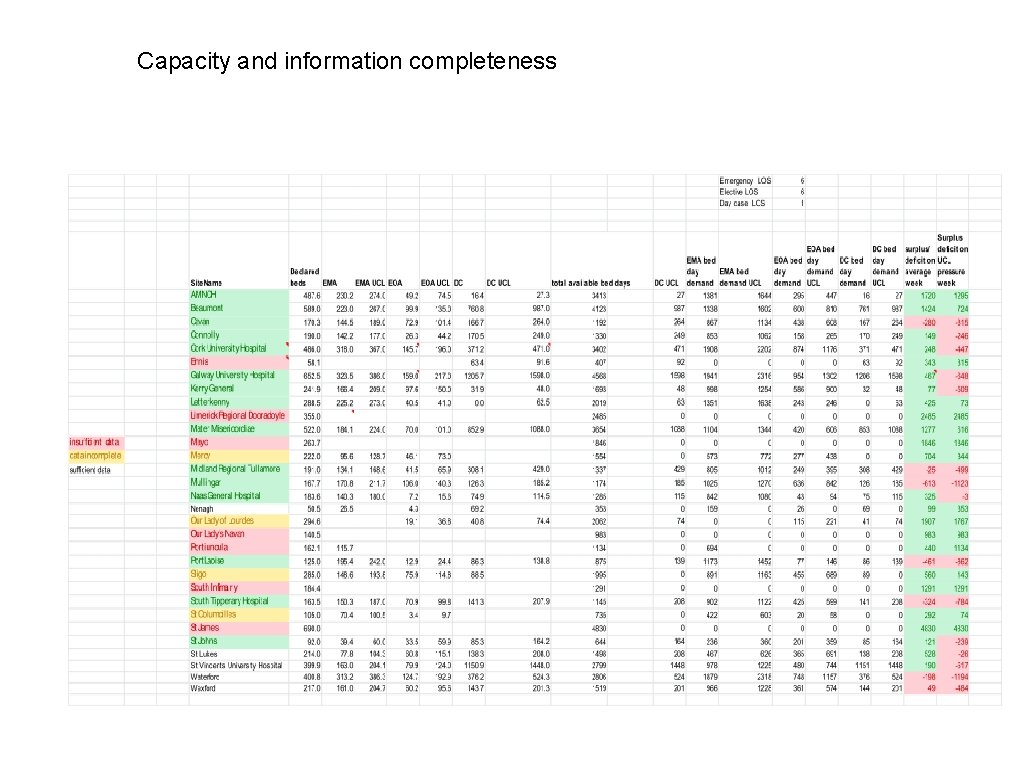
Capacity and information completeness
CAPACITY PLANNING • The capacity available each day through December and January, including medical beds and clinician rosters, discharge teams and bed managers • The availability of diagnostic support through December and January • Primary care and GP availability within the area over the Christmas and New Year period • Plans to provide extra capacity in ED to handle the potential for increased attendances in those areas where this has been a feature of demand in the past • Planned increases in capacity in early January to manage any increases in patient flow that occur • Home help and community service availability across the holiday period • Availability of services to support discharge across the holiday period • The availability of step-down or intermediate care beds within the locality • The availability of outpatient slots to manage patients who can be safely sent home to return for 24 or 48 hour review • The profile of elective activity to ensure that waiting time targets are met in a way that is mindful of the need to maintain unscheduled care responsiveness
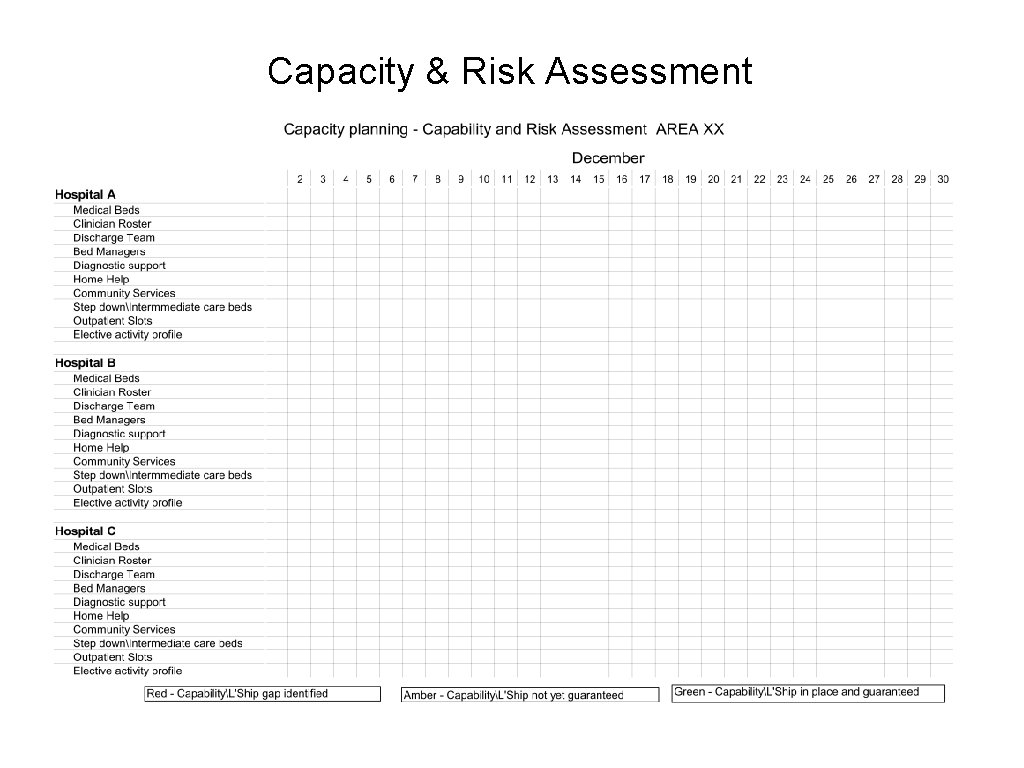
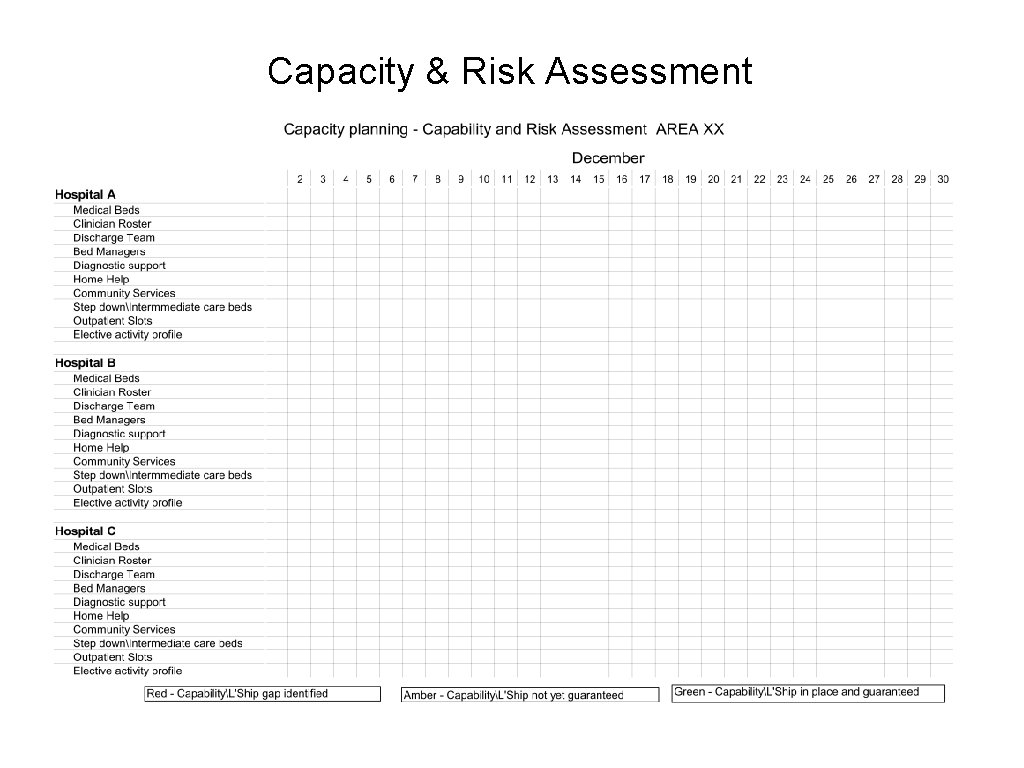
Capacity & Risk Assessment
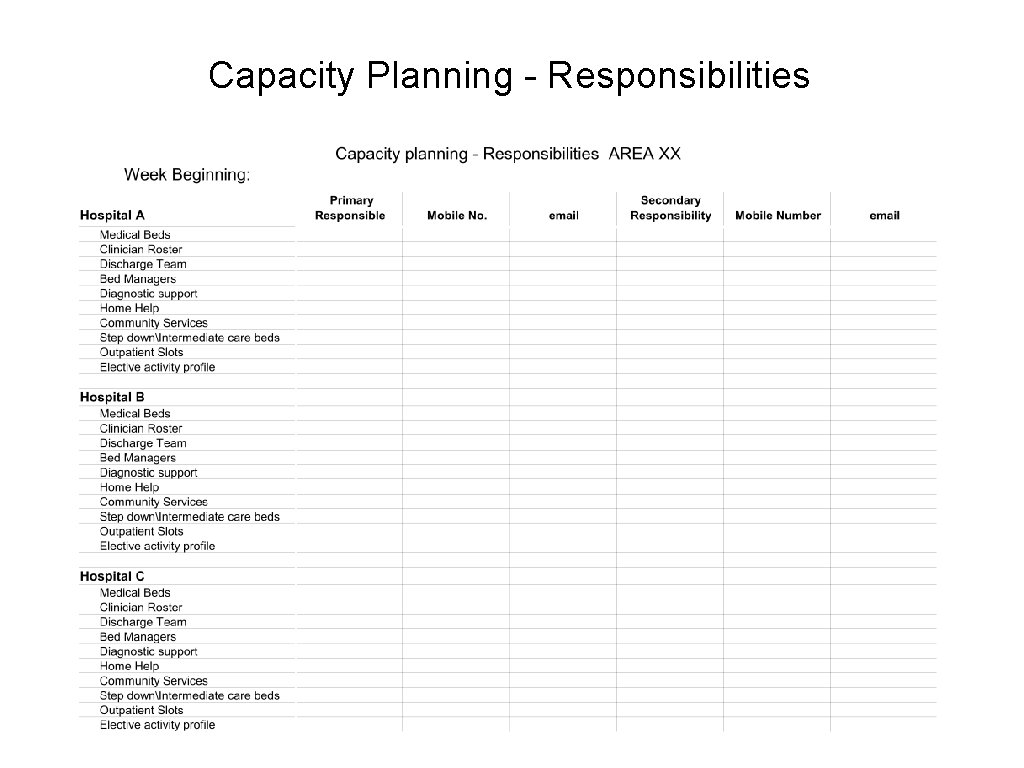
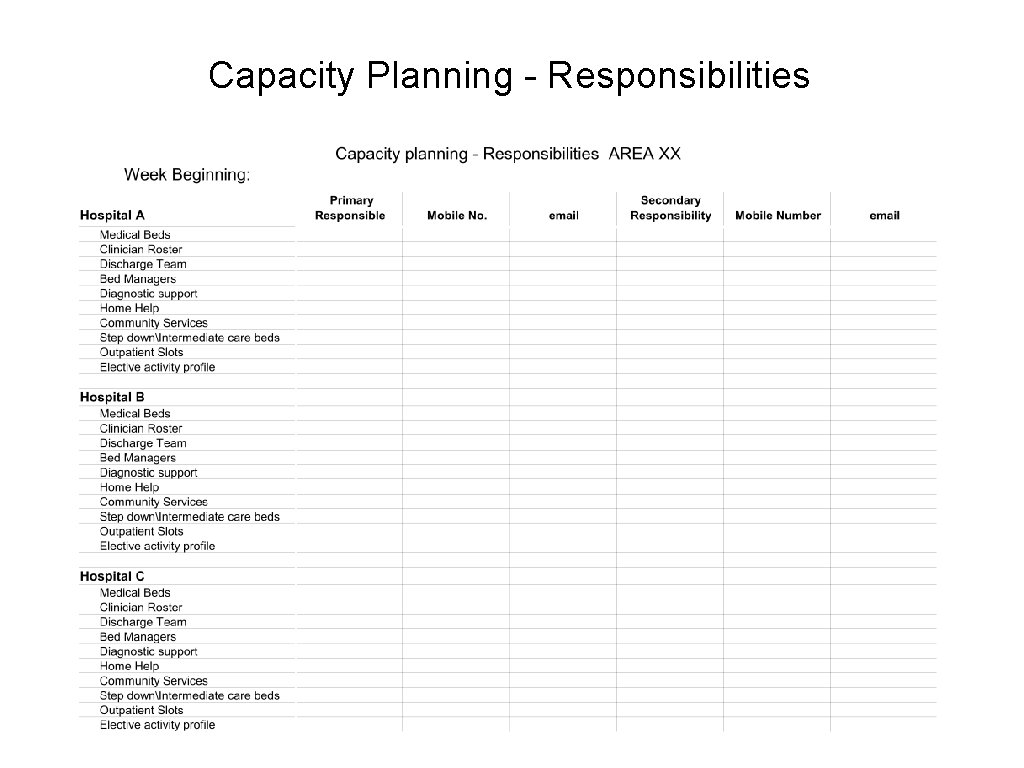
Capacity Planning - Responsibilities
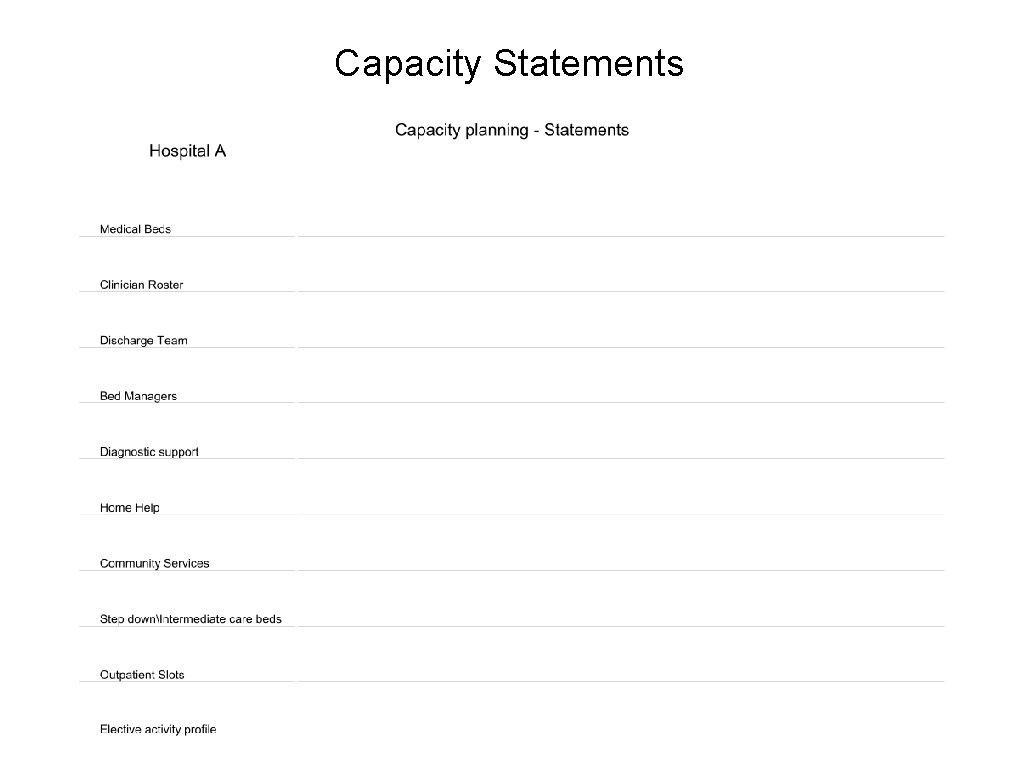
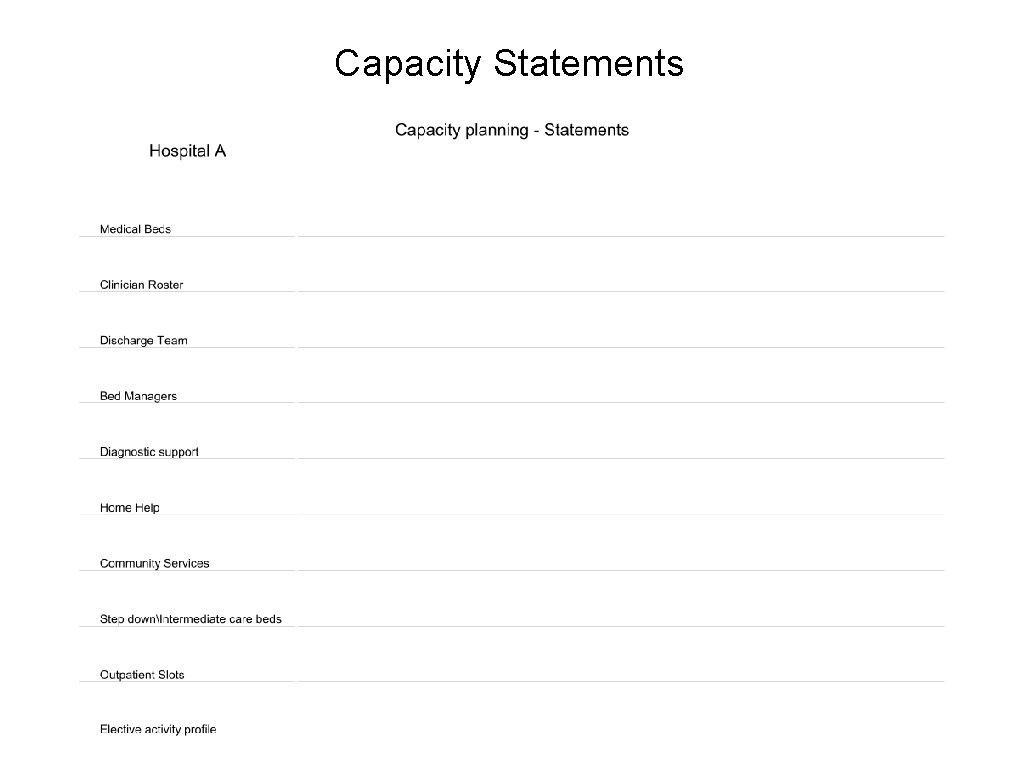
Capacity Statements
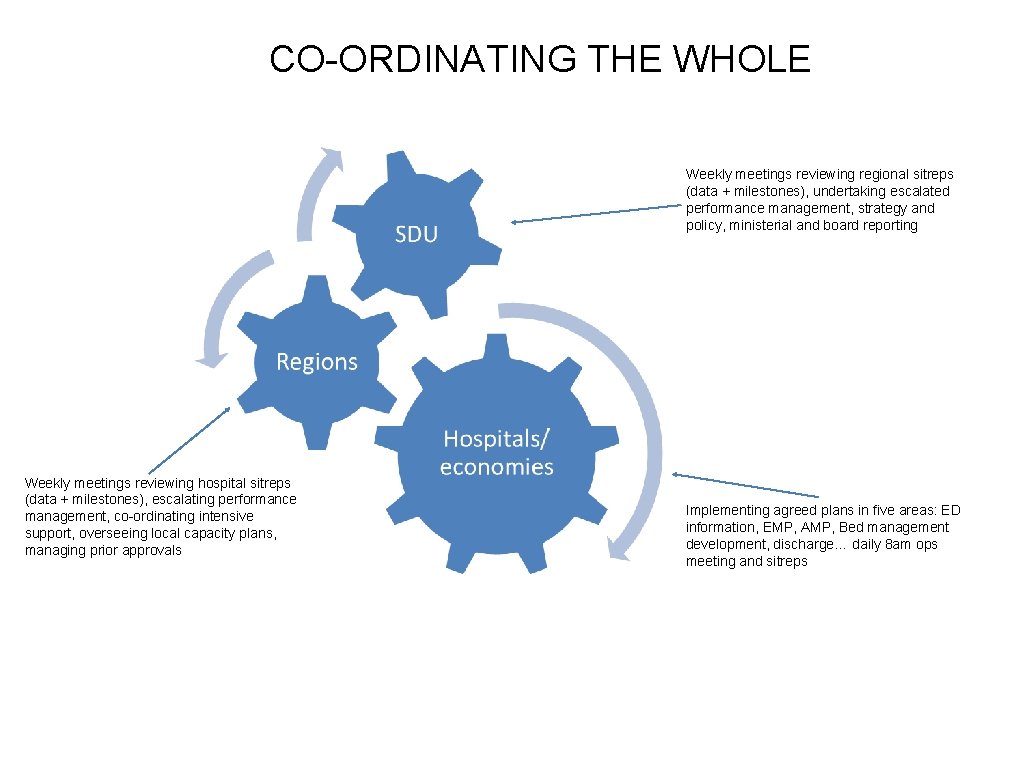
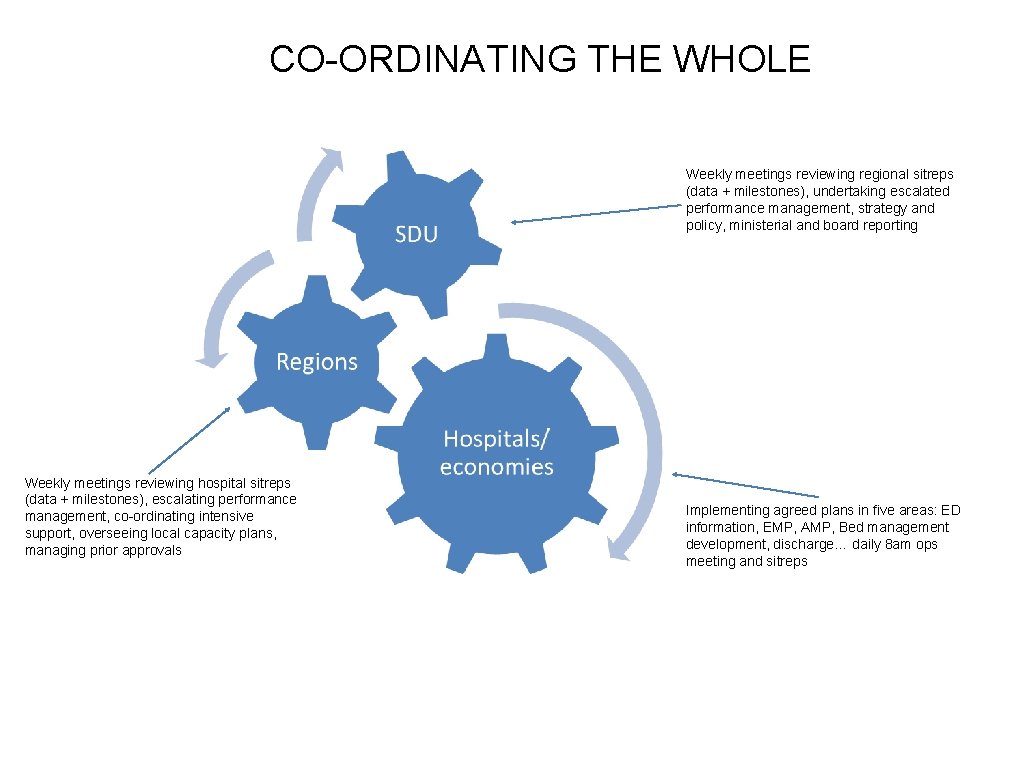
CO-ORDINATING THE WHOLE Weekly meetings reviewing regional sitreps (data + milestones), undertaking escalated performance management, strategy and policy, ministerial and board reporting Weekly meetings reviewing hospital sitreps (data + milestones), escalating performance management, co-ordinating intensive support, overseeing local capacity plans, managing prior approvals Implementing agreed plans in five areas: ED information, EMP, AMP, Bed management development, discharge… daily 8 am ops meeting and sitreps
SCHEDULED CARE: Delivering 12 months
SYSTEMATIC ANALYSIS
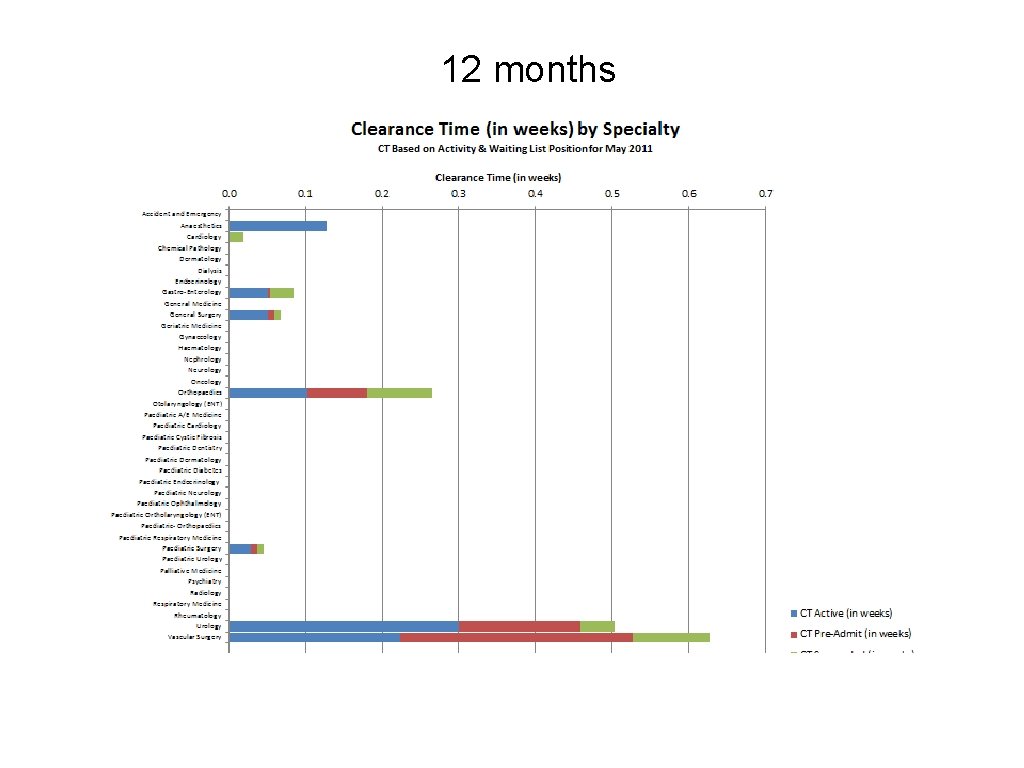
Introducing clearance times • Waiting lists are an indicator of a failure to match capacity and demand, and a failure to make good the implicit promise of treatment • By themselves , they are not a good indicator of organisational effectiveness or the risks of target delivery • If we value equity, we will want to shift the focus away from the number of patients on the list and towards the maximum waiting time
Introducing clearance times • Clearance times are a proven means of identifying the potential for the system to deliver shorter waits, at the present level of activity • They are calculated by dividing the number of patients waiting within a certain time band by the amount of elective activity completed in a period by each specialty in each hospital • They are risk-adjusted by allowing for: • A certain amount of activity to be set aside for urgent cases • A certain percentage of suspended patients that will need treatment • A certain percentage of preadmitted patients that will need treatment • The withdrawal of the NTPF activity as traditionally applied
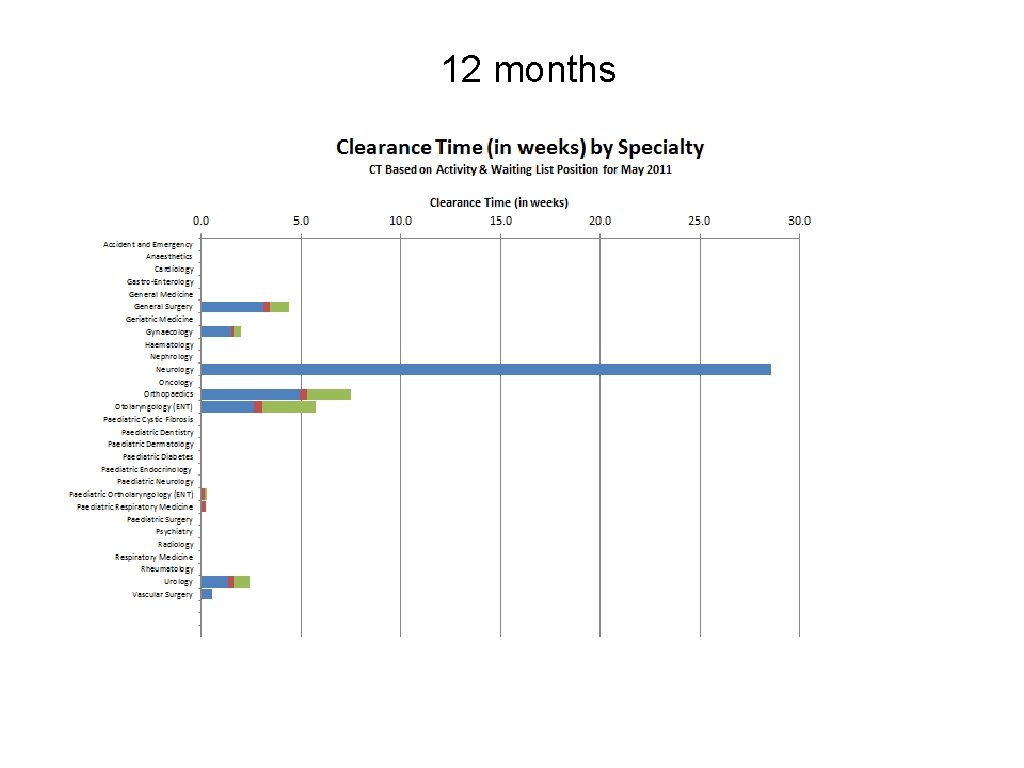
INPATIENTS
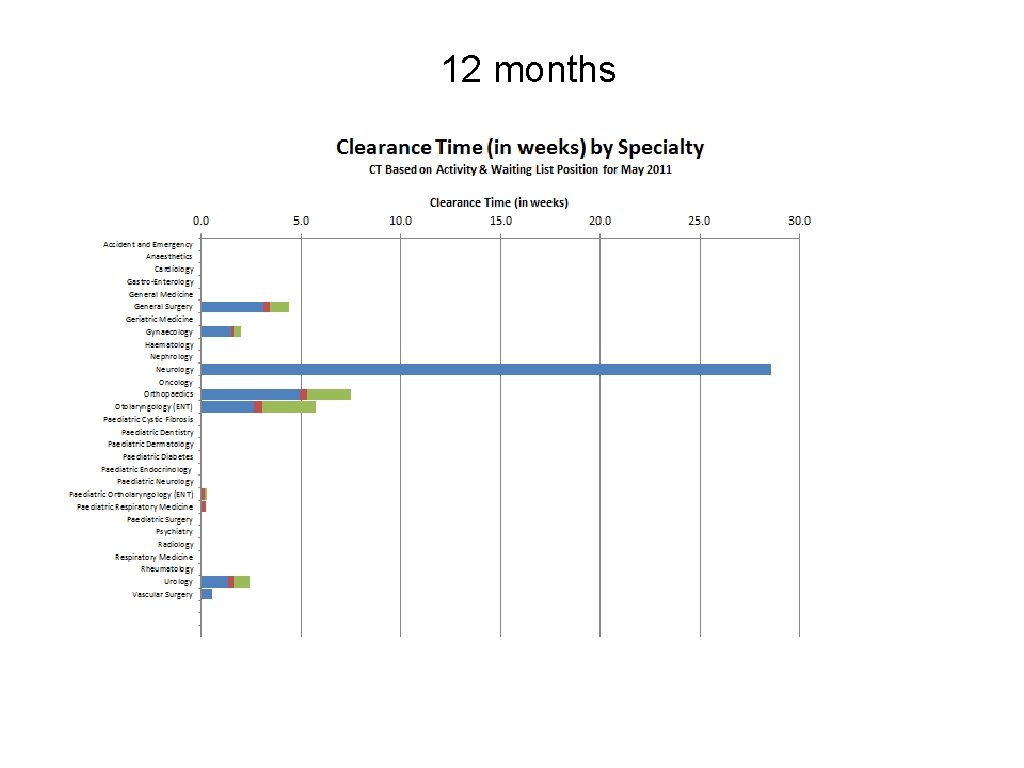
12 months
DAYCASES
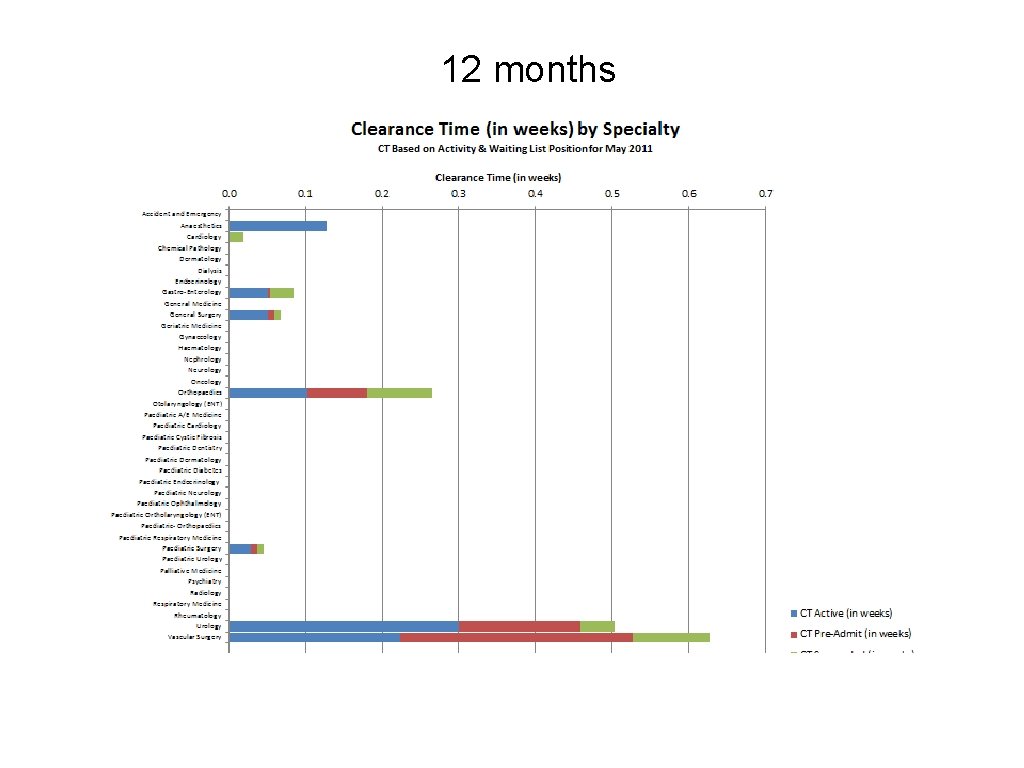
12 months
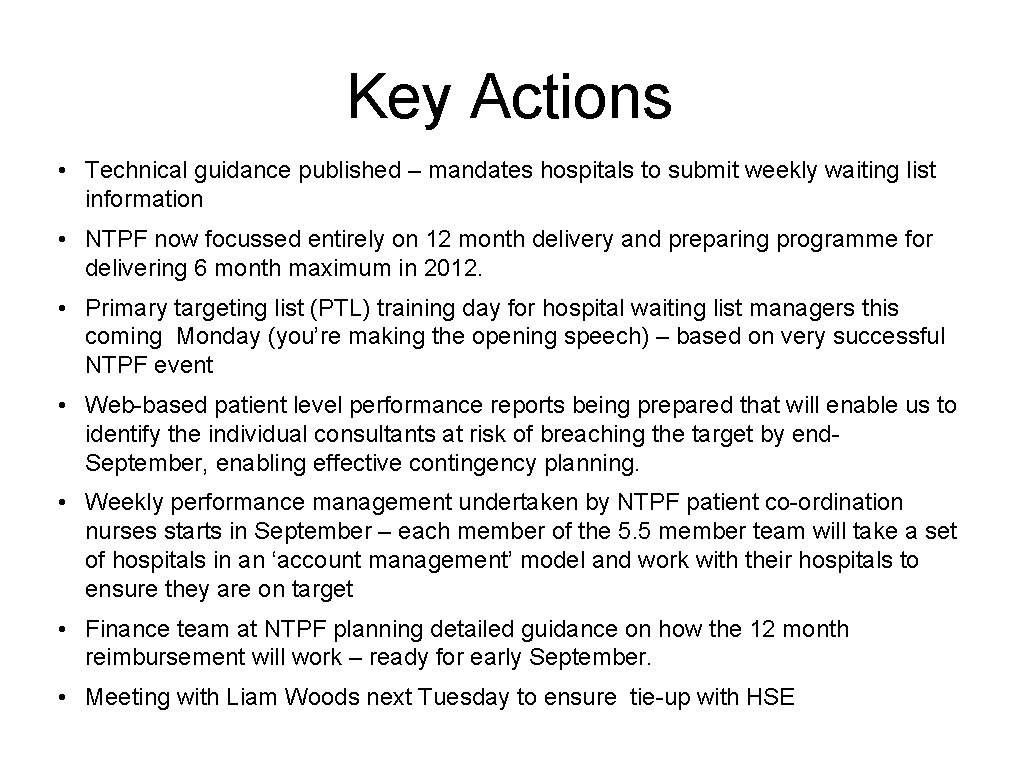
Key Actions • Technical guidance published – mandates hospitals to submit weekly waiting list information • NTPF now focussed entirely on 12 month delivery and preparing programme for delivering 6 month maximum in 2012. • Primary targeting list (PTL) training day for hospital waiting list managers this coming Monday (you’re making the opening speech) – based on very successful NTPF event • Web-based patient level performance reports being prepared that will enable us to identify the individual consultants at risk of breaching the target by end. September, enabling effective contingency planning. • Weekly performance management undertaken by NTPF patient co-ordination nurses starts in September – each member of the 5. 5 member team will take a set of hospitals in an ‘account management’ model and work with their hospitals to ensure they are on target • Finance team at NTPF planning detailed guidance on how the 12 month reimbursement will work – ready for early September. • Meeting with Liam Woods next Tuesday to ensure tie-up with HSE
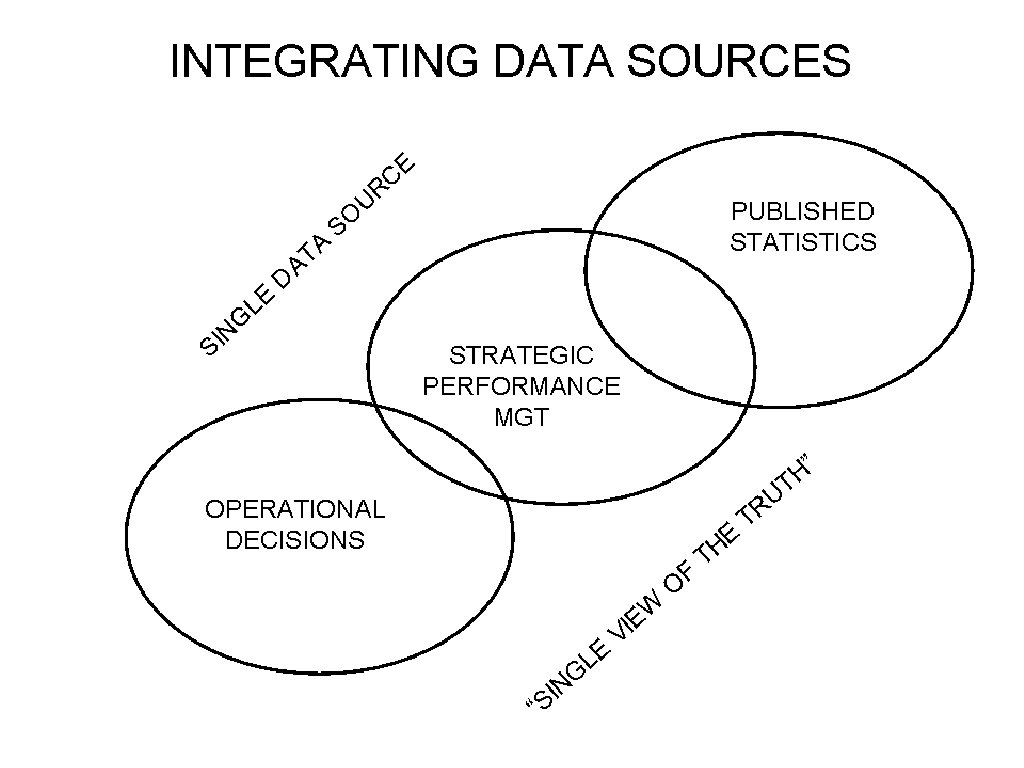
FOCUS ON INFORMATION SYSTEMS
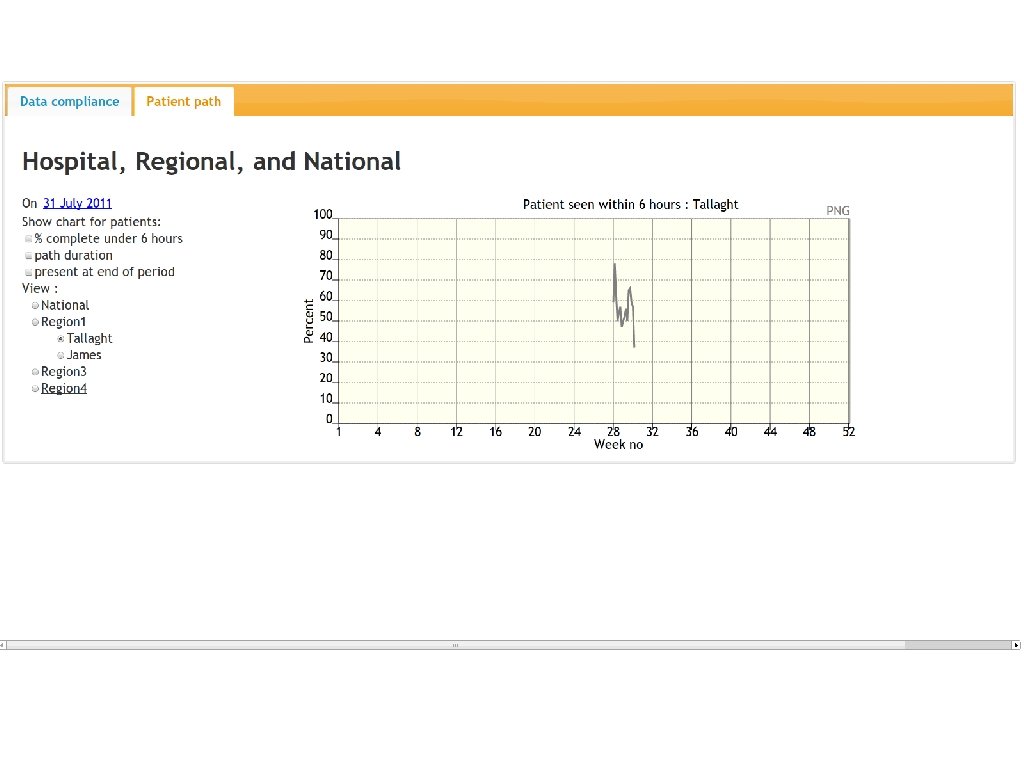
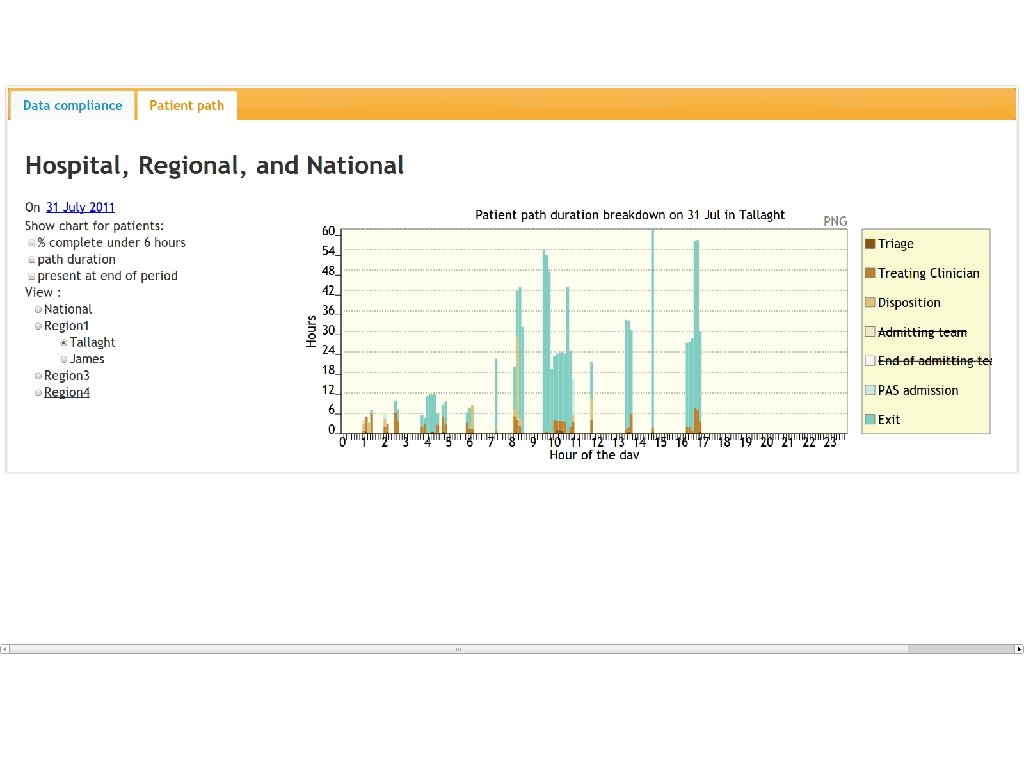
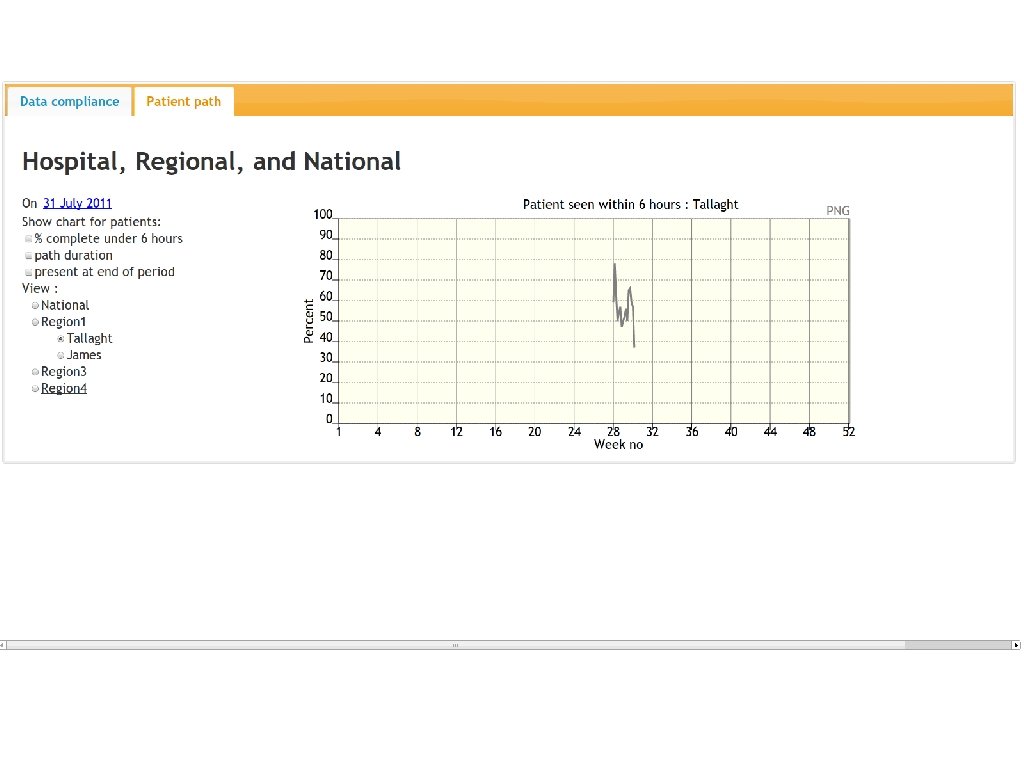
Progress • Web team now beginning to deliver product on ED and patient level tracking of surgical list by end September • NTPF now working to new agenda including their well-developed data management infrastructure for waiting lists • Development session completed between NTPF information dept and web team to begin project planning the web system for managing the inpatient/ daycase list – design teleconference next Wednesday
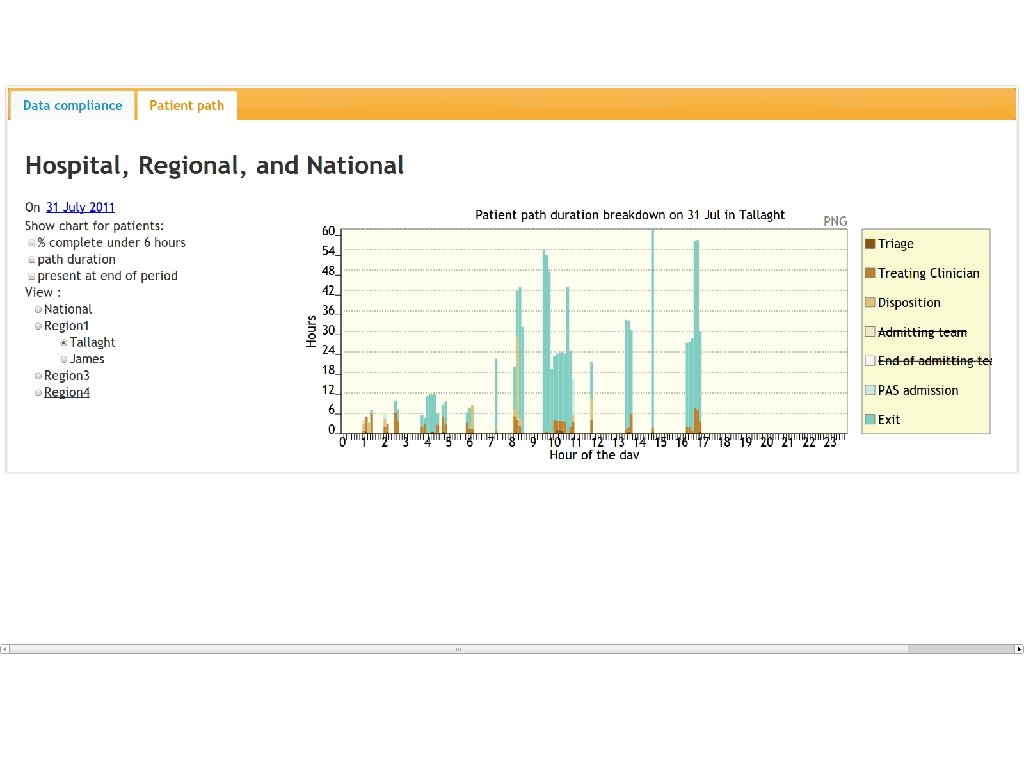
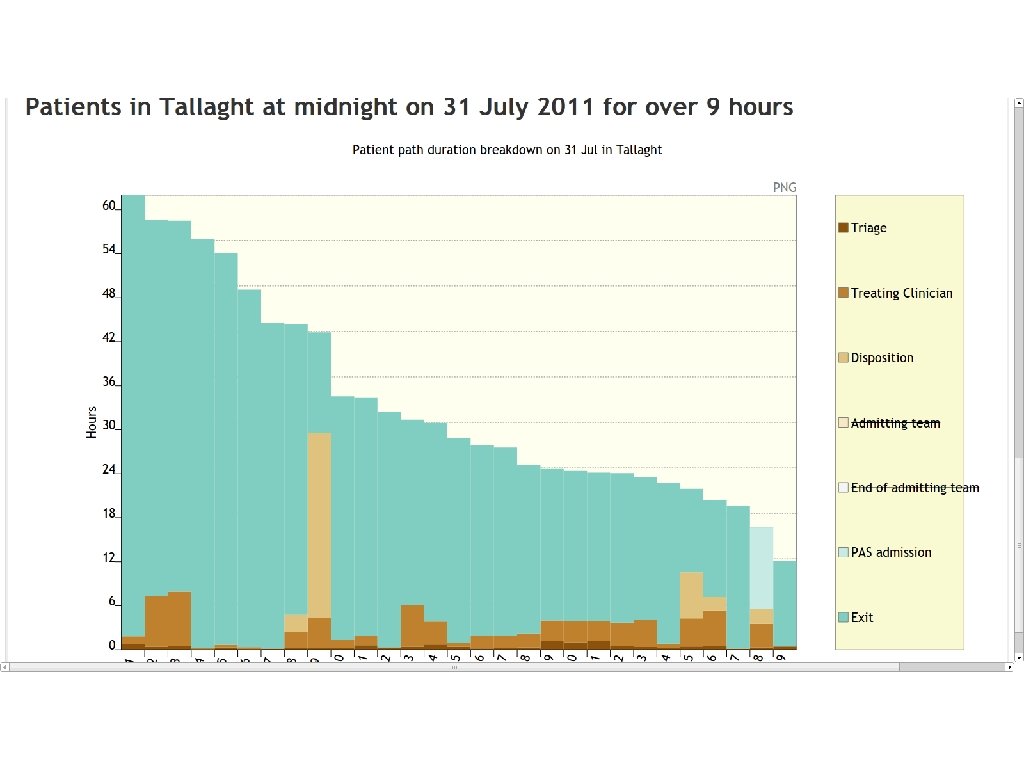
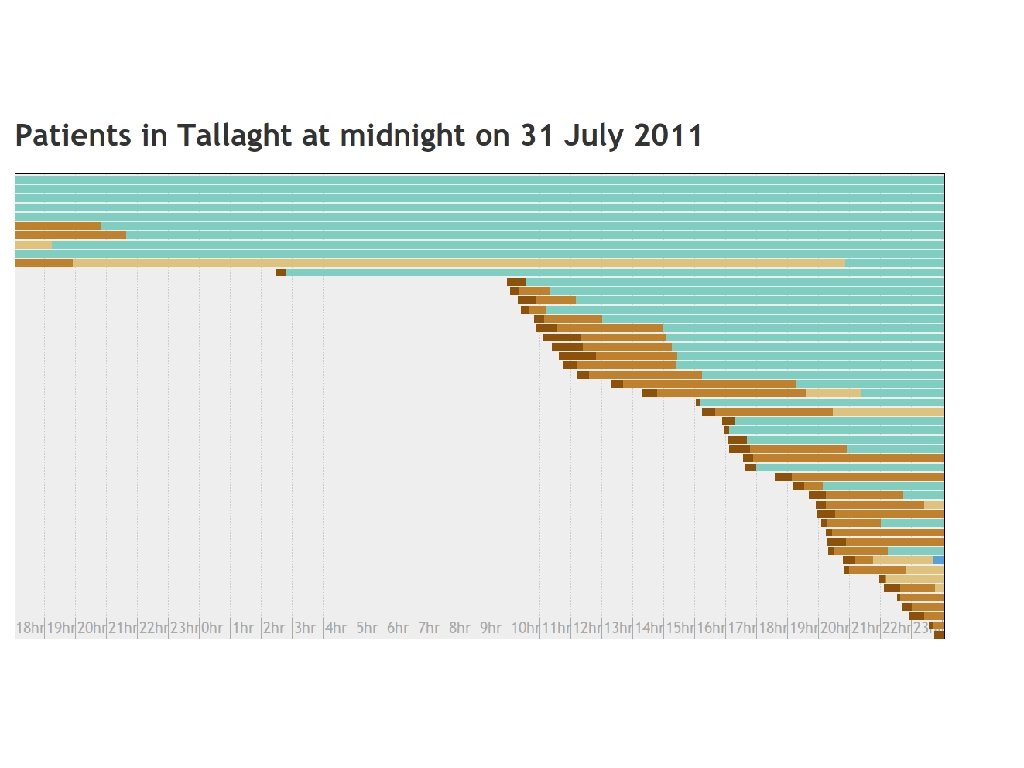
WEB-BASED DEMO

ED ICT web screen shots
Strategy
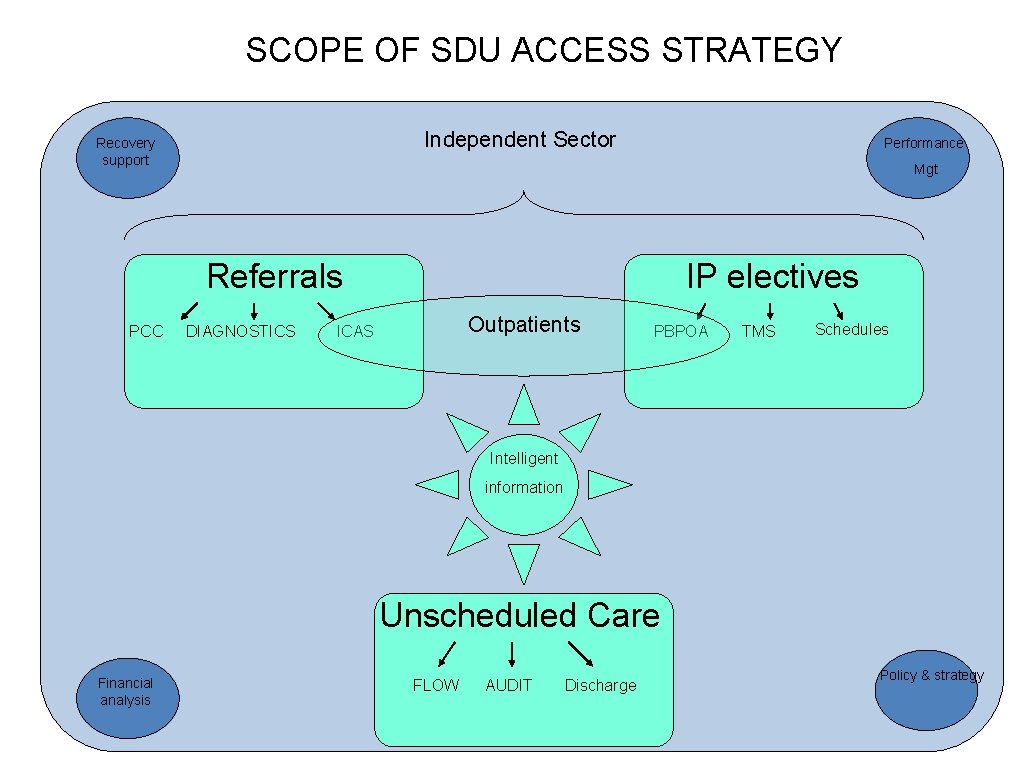
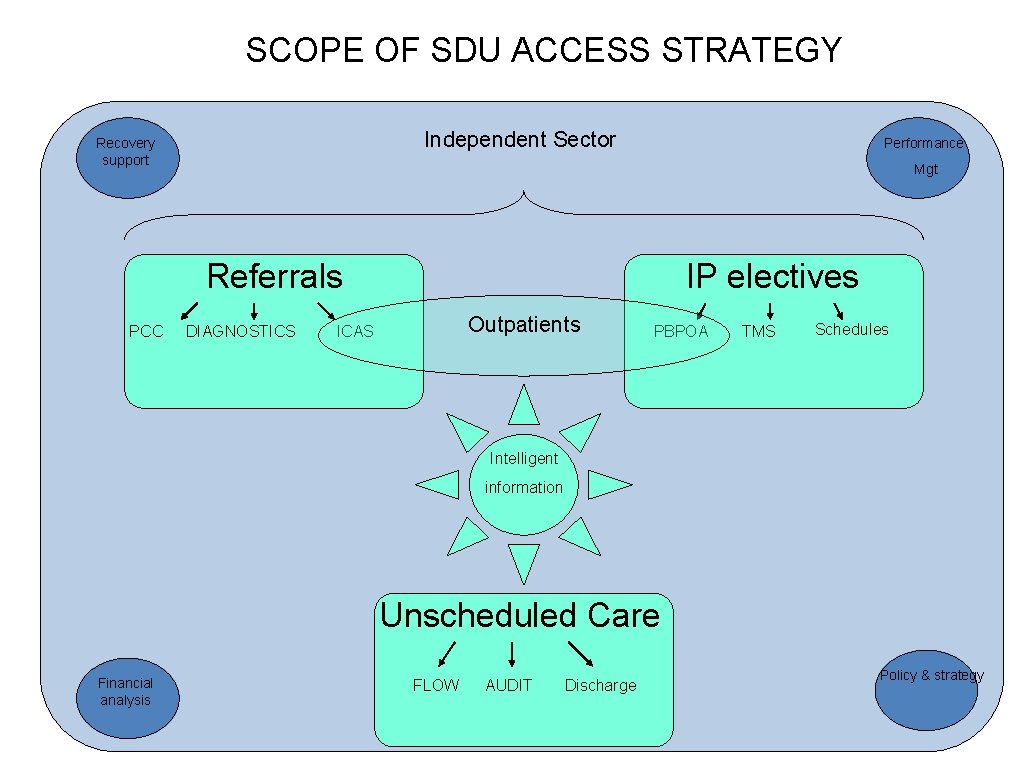
SCOPE OF SDU ACCESS STRATEGY Independent Sector Recovery support Performance Mgt Referrals PCC DIAGNOSTICS IP electives Outpatients ICAS PBPOA TMS Schedules Intelligent information Unscheduled Care Financial analysis FLOW AUDIT Discharge Policy & strategy
CONCLUSION OF PRESENTATION • Strategy definition is well underway • Team alignment amongst strategic agencies working well • New approaches developed and products starting to emerge • Execution (as always) the biggest risk: Clinical Programmes and SDU developing joint approaches to hospital-level support • Aiming for new accountability framework to commence January 2012 • New information systems give us a patient-centred view of the overall business