Dr Ahmed Fathalla Ibrahim DEVELOPMENT OF GONADS During

Dr. Ahmed Fathalla Ibrahim
DEVELOPMENT OF GONADS • During 5 th week: gonadal development occurs • Until 7 th week: gonads are similar in both sexes • Gonads are derived from 3 sources: 1. Mesothelium (mesodermal epithelium lining the coelomic cavity) 2. Underlying mesenchyme 3. Primordial germ cells
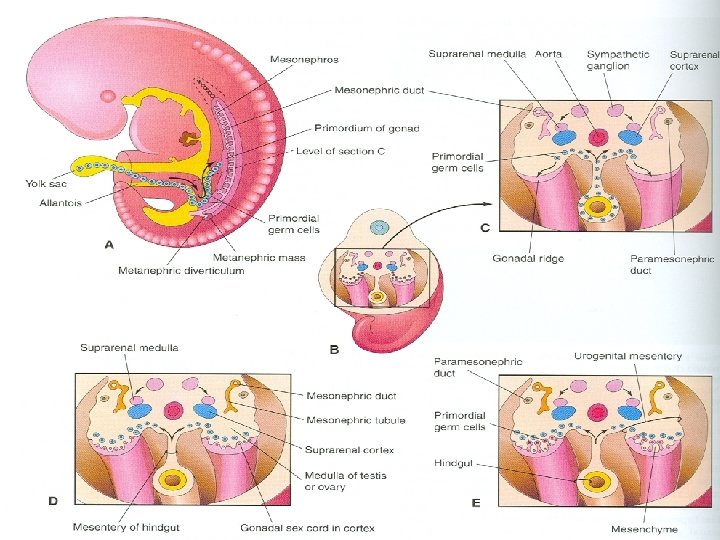
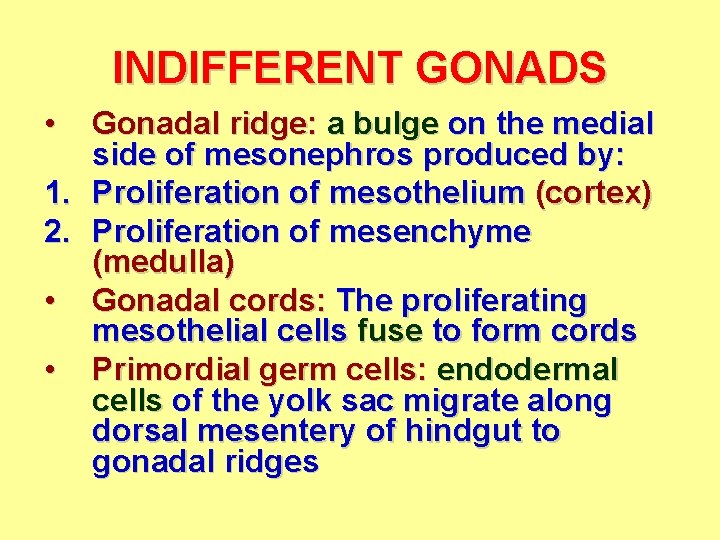
INDIFFERENT GONADS • Gonadal ridge: a bulge on the medial side of mesonephros produced by: 1. Proliferation of mesothelium (cortex) 2. Proliferation of mesenchyme (medulla) • Gonadal cords: The proliferating mesothelial cells fuse to form cords • Primordial germ cells: endodermal cells of the yolk sac migrate along dorsal mesentery of hindgut to gonadal ridges
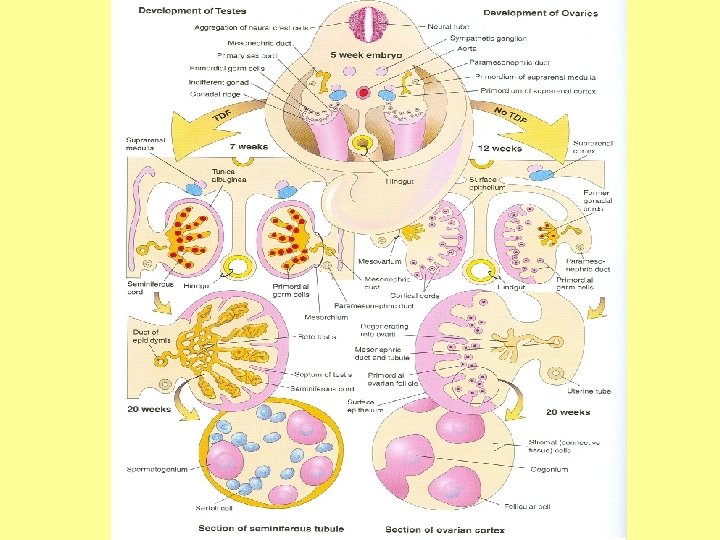
DEVELOPMENT OF TESTIS The Y chromosome has a testisdetermining factor (TDS). At 7 th week: • Regression of cortex & differentiation of medulla into testis • Gonadal cords condense & extend into medulla to form seminiferous cords • Seminiferous cords develop into: semineferous tubules, tubuli recti & rete testis
DEVELOPMENT OF TESTIS • The rete testis becomes continuous with 15 to 20 mesonephric tubules that become efferent ductules • The characteristic feature is the development of a thick fibrous capsule (tunica albuginea) that separates the enlarging testis from mesonephros
DEVELOPMENT OF TESTIS • Semineferous tubules remain solid until puberty. Its walls are composed of: 1. Sertoli cells: derived from surface epithelium of testis (mesothelial cells) 2. Spermatogonia: derived from primordial germ cells
DEVELOPMENT OF TESTIS • By 6 th to 7 th week, sertoli cells produces a glycoprotein known as antimüllerian hormone or müllerian inhibiting substance (MIS) • Mesenchyme gives rise to interstitial cells (of Leydig). By eighth week, human chorionic gonadotrophin stimulates interstitial cells to secrete testosterone
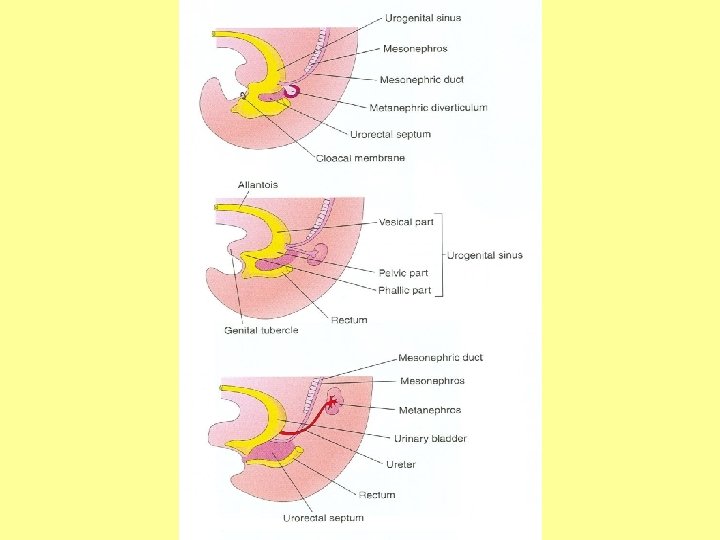
DEVELOPMENT OF MALE GENITAL DUCTS • Both male & female have two pairs of genital ducts: 1. Mesonephric (wolffian) ducts 2. Paramesonephric (müllerian) ducts • During 5 th & 6 th week, both pairs of ducts are present (indifferent state)
DEVELOPMENT OF MALE GENITAL DUCTS • Testosterone: 1. Induces masculine differentiation of mesonephric duct (epididymis, vas deferens, seminal vesicle, ejaculatory duct) 2. Induces masculine differentiation of external genitalia • Antimüllerian hormone (müllerian inhibiting substance): suppresses development of paramesonephric (müllerian) duct
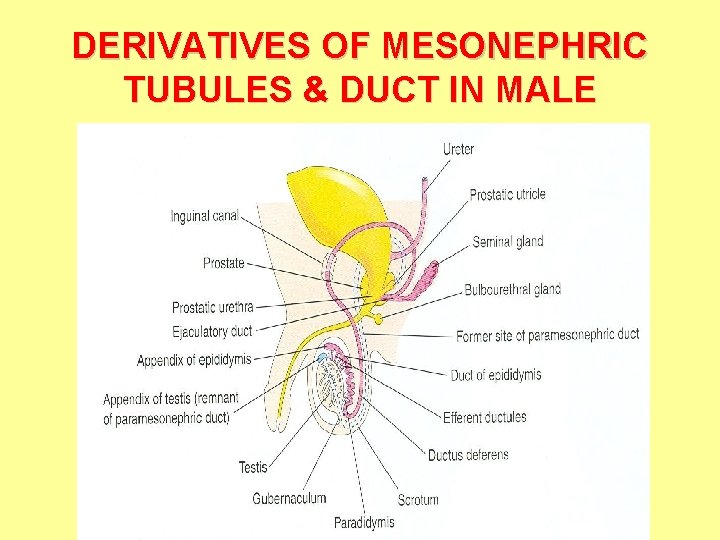
DERIVATIVES OF MESONEPHRIC TUBULES & DUCT IN MALE
DEVELOPMENT OF MALE GENITAL GLANDS • Seminal vesicles (mesodermal in origin): develops as lateral outgrowths from the caudal end of mesonephric duct • Prostate (endodermal in origin): develops as multiple endodermal outgrowths from prostatic part of urethra to form glandular epithelium. Stroma & smooth muscles are derived from surrounding mesenchyme
DEVELOPMENT OF MALE GENITAL GLANDS • Bulbourethral glands (endodermal in origin): develop as outgrowths from spongy part of urethra. Stroma & smooth muscles are derived from surrounding mesenchyme
INDIFFERENT STAGE OF EXTERNAL GENITALIA • From 4 th to 7 th week, external genitalia are similar in both sexes • Differentiation begins during the 9 th week • Differentiation is complete at 12 th week
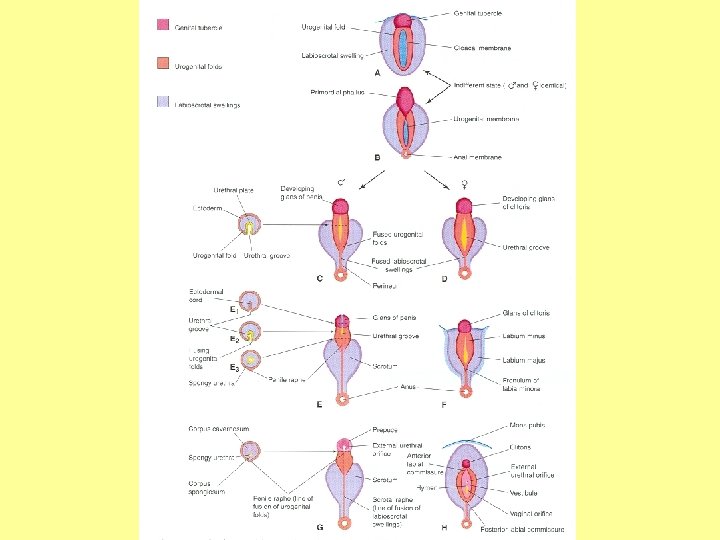
INDIFFERENT STAGE OF EXTERNAL GENITALIA • Genital tubercle: produced from proliferating mesenchyme at the cranial end of cloacal membrane. It soon elongates to form a primordial phallus • Urogenital folds: develop on each side of cloacal membrane • Labioscrotal swellings: develop on each side of urogenital folds
INDIFFERENT STAGE OF EXTERNAL GENITALIA • Cloacal membrane is divided by the urorectal septum into: ventral urogenital & dorsal anal membrane • Urogenital membrane: lies in the floor of urogenital groove which is bounded by urogenital folds. During 5 th week, the membrane ruptures to form urogenital orifice
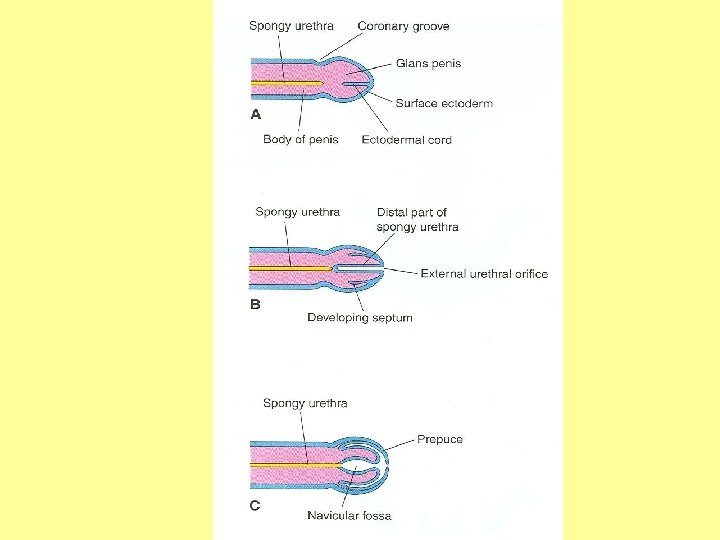
MALE EXTERNAL GENITALIA • • • 1. 2. 3. Body of penis: formed by enlarged & elongated phallus. Root of penis: formed by fused urogenital folds Spongy urethra (endodermal in origin): Proliferating endodermal cells from phallic portion of urogenital sinus (urethral plate) extend to line urogenital (urethral) groove. Fusion of urogenital folds along ventral surface of penis forms the spongy urethra Surface ectoderm fuses in median plane of penis (penile raphe) to enclose spongy urethra within penis
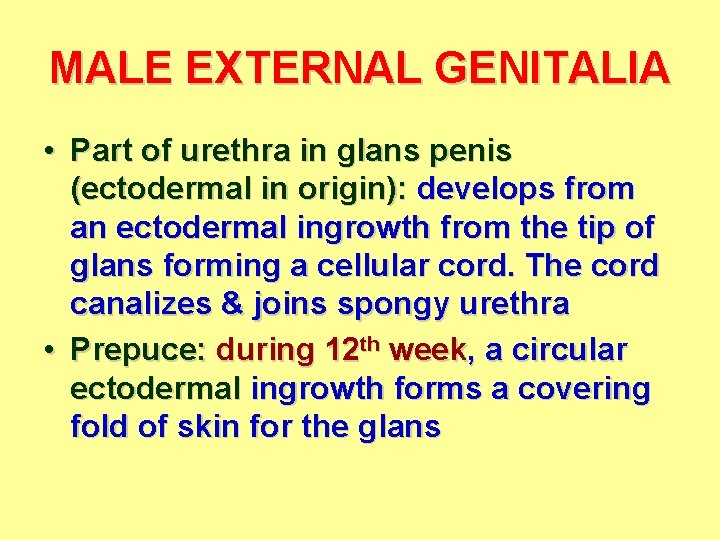
MALE EXTERNAL GENITALIA • Part of urethra in glans penis (ectodermal in origin): develops from an ectodermal ingrowth from the tip of glans forming a cellular cord. The cord canalizes & joins spongy urethra • Prepuce: during 12 th week, a circular ectodermal ingrowth forms a covering fold of skin for the glans
MALE EXTERNAL GENITALIA • Scrotum: formed by fused labioscrotal swellings • Corpora cavernosa & corpus spongiosum: develop from mesenchyme of phallus
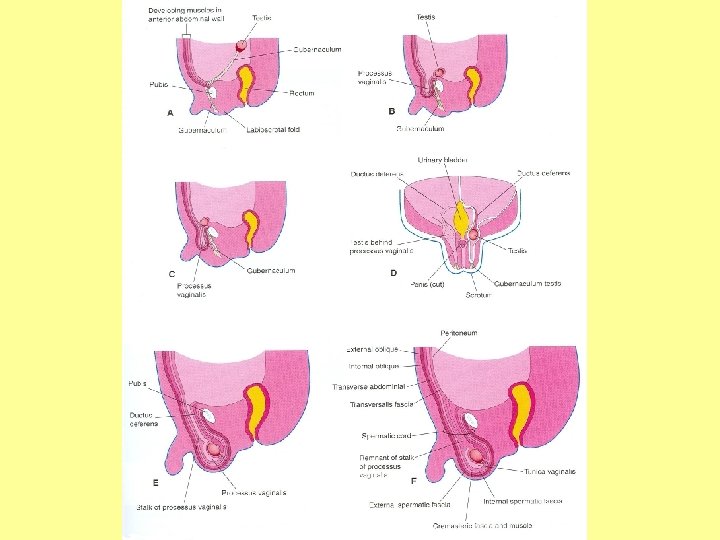
DEVELOPMENT OF INGUINAL CANALS • Develop in both sexes • Gubernaculum: a ligament attached to inferior pole of gonad, passes caudally through anterior abdominal wall at site of future of inguinal canal to become attached to internal surface of labioscrotal swellings • Processus vaginalis: evagination of peritoneum that herniates along the path formed by gubernaculum. It carries extensions of layers of anterior abdominal wall that form walls of inguinal canal (+ coverings of spermatic cord in male)
DESCENT OF TESTIS INTERNAL DESCENT: • occurs in both sexes • Gonads descend from posterior abdominal wall to deep inguinal rings (in male) or to pelvis (in female) • Completed by 26 th weeks • Causes: a relative movement resulting from elongation of cranial part of abdomen away from its caudal part (future pelvic cavity)
DESCENT OF TESTIS EXTERNAL DESCENT: • • Occurs only for testes Testes descend from deep inguinal rings, along inguinal canals, to scrotum • Begins during 26 th week and takes 2 to 3 days 1. More than 97% of full-term new born males have both testes in scrotum 2. During first 3 months, most undescended testis descend into scrotum 3. No spontaneous descent occurs after the age of 1 year
DESCENT OF TESTIS EXTERNAL DESCENT: • Causes: 1. Controlled by androgens 2. Guided by gubernaculum testis 3. Facilitated by processus vaginalis 4. Helped by increased intraabdominal pressure resulting from growth of abdominal viscera
DESCENT OF TESTIS EXTERNAL DESCENT: • Associated with: 1. Enlargement of testes & atrophy of mesonephroi 2. Atrophy of paramesonephric ducts 3. Enlargement of processus vaginalis
DESCENT OF TESTIS EXTERNAL DESCENT: • Fate of gubernaculum testis: degenerates & disappears • Fate of processus vaginalis: During perinatal period: 1. The stalk normally obliterates 2. The caudal part forms the peritoneal sac surrounding the testis (tunica vaginalis)
ANOMALIES Female ducts in male: • Paramesonephric ducts develop in male • Cause: failure of development of testes & absence of müllerian inhibiting substance
ANOMALIES Hypospadius: • Most common anomaly of penis • Causes: inadequate production of androgens and/or inadequate receptor sites for hormones • External urethral orifice opens on ventral surface of glans or body of penis (80% of cases): due to failure of canalization of ectodermal cord in glans and/or failure of fusion of urogenital folds • In perineal hypospadius: labioscrotal swellings fail to fuse & the orifice is located between unfused halves of scrotum
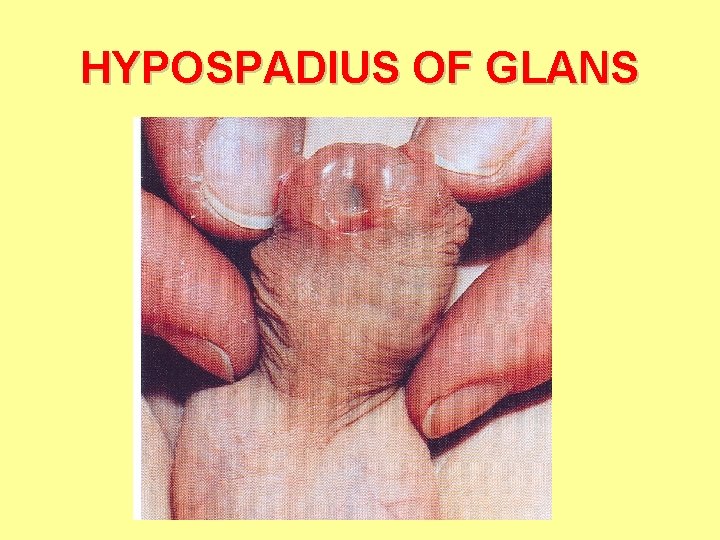
HYPOSPADIUS OF GLANS
ANOMALIES Cryptorchidism (undescended testis): • Occurs in up to 30% of premature males • Cause: deficiency of androgens • May be unilateral or bilateral • In most cases, testes descend by the end of 1 st year, if not atrophy occurs • Men with a history of cryptorchidism have an increased risk of developing testicular cancer
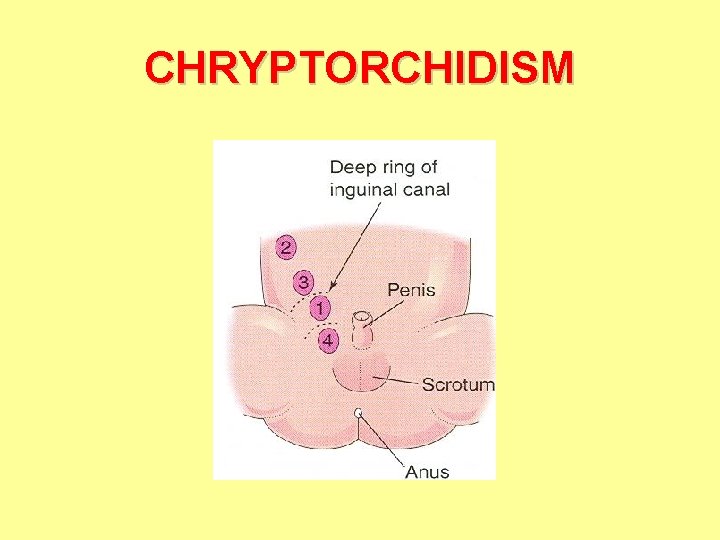
CHRYPTORCHIDISM
- Slides: 36