Dr Ahmed Fathalla Ibrahim DECIDUA DEFINITION 1 It
Dr. Ahmed Fathalla Ibrahim

DECIDUA • DEFINITION: 1. It is the functional layer of endometrium in a pregnant women 2. It includes the endometrium of fundus & body of uterus 3. The endometrium of the cervix does not form a part of decidua. The cervix is closed by mucous plug during pregnancy

DECIDUA • CAUSE OF FORMATION: 1. Trophoblast secretes chorionic gonadotrophins which prolong the life of corpus luteum 2. The corpus luteum of pregnancy continues to secrete progesterone 3. The increasing level of progesterone in maternal blood induces endometrial changes into decidua

DECIDUA • STEPS OF FORMATION (DECIDUAL REACTION): IMPORTANT IN DIAGNOSIS OF EARLY PREGNANCY 1. The endometrium becomes thicker & more vascular 2. The endometrial glands become full of secretion 3. The connective tissue cells enlarge due to accumulation of lipid & glycogen They are called “decidual cells”

PARTS OF DECIDUA

DECIDUA • PARTS OF DECIDUA: 1. Decidua basalis: between chorionic sac & muscle wall of uterus 2. Decidua capsularis: between chorionic sac & cavity of uterus 3. Decidua parietalis: remaining part
DECIDUA • FATE OF DECIDUA: The chorionic sac expands towards the cavity of the uterus due to the growth of fetus & enlargement of amniotic cavity: 1. The cavity of uterus is obliterated due to fusion of chorion & amnion 2. The decidua parietalis & capsularis disappear gradually 3. The decidua basalis persists to form a part of placenta

CHORION & CHORIONIC VILLI • DEVELOPMENT: During implantation, the trophoblast thickens at region of contact with endometrium & differentiates into: 1. Outer syncytiotrophoblast: a layer containing multiple nuclei in a common cytoplasm with no cell boundaries (secretes HCG) 2. Inner cytotrophoblast: a layer of mononucleated cells
PRIMARY CHORIONIC VILLI

SECONDARY CHORIONIC VILLI

TERTIARY CHORIONIC VILLI

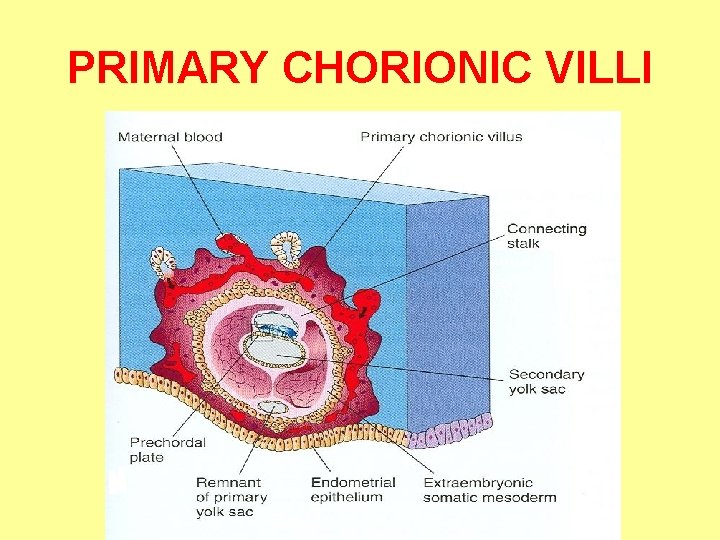
STAGES OF CHORIONIC VILLI • PRIMARY: At the end of 2 nd week, finger-like processes formed of outer syncytiotrophoblast & inner cytotrophoblast appear • SECONDARY: Early in 3 rd week, extraembryonic mesoderm extends inside the villi • TERTIARY: During 3 rd week, arterioles, venules & capillaries develop in the mesenchyme of villi & join umbilical vessels By the end of 3 rd week, embryonic blood begins to flow slowly through capillaries in chorionic villi

CHORIONIC VILLI • Chorionic villi invade & erode endometrium, maternal blood leaks & collects in spaces between villi (intervillous spaces) • Cytotrophoblast penetrates syncytiotrophoblast & extends to form a cytotrophoblastic shell that surrounds the chorionic sac & attaches it to endometrium. It prevent further penetration of decidua by syncytiotrophoblast

TYPES OF CHORIONIC VILLI • STEM (ANCHORING) VILLI: attach the chorionic sac to decidua through cytotrophoblastic shell • BRANCH (TERMINAL) VILLI: grow from the sides of stem villi, increase surface area for exchange between fetal & maternal blood
PLACENTA

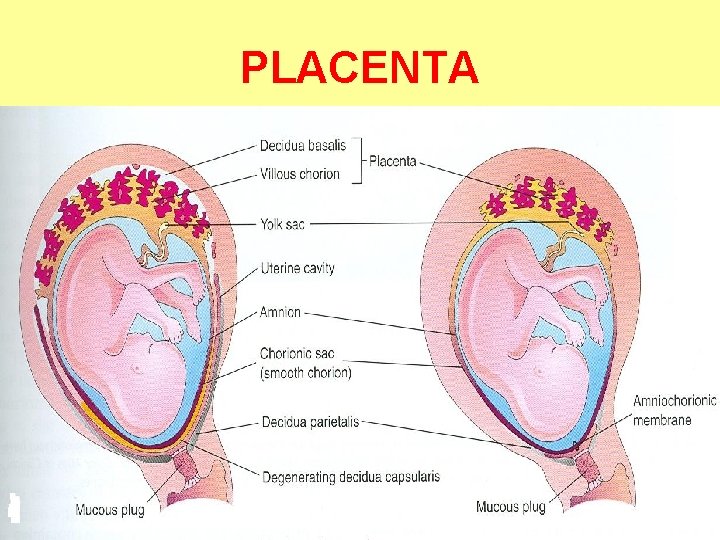
FATE OF CHORIONIC VILLI • Until the beginning of 8 th week, chorionic villi surround the whole chorionic sac, then differentiate into: 1. Smooth chorion (chorion laeve): villi in contact with decidua capsularis, degenerate & become avascular due to compression & disappearance of decidua capsularis 2. Villous chorion (chorion frondosum): large villi in contact with decidua basalis, form part of placenta

DEVELOPMENT OF PLACENTA 1. FETAL PART: VILLOUS CHORION 2. MATERNAL PART: DECIDUA BASALIS

PLACENTA A) MATERNAL SURFACE B) FETAL SURFACE

PLACENTA • • SHAPE: circular disc WEIGHT: about one-sixth that of fetus (500600 gm) • DIAMETER: 15 -20 cm • THICKNESS: 2 -3 cm • SURFACES: 1. Fetal surface: smooth, transparent, covered by amnion with umbilical cord attached near its center & umbilical vessels radiating from it 2. Maternal surface: irregular, divided into convex areas (cotyledons)

PLACENTA • The fetal part of placenta is divided into cotyledons by projections from decidua basalis (placental septa) • Each cotyledon contains 2 or more stem villi with their branch villi • By the end of 4 th month, decidua basalis is almost entirely replaced by cotyledons

PLACENTAL CIRCULATION

PLACENTAL CIRCULATION • Poorly oxygenaed blood leaves the fetus & passes through the 2 umbilical arteries to the placenta • Umbilical arteries divide into several chorionic arteries that enter chorionic villi • An arterio-capillary-venous network is formed in chorionic villi • Exchange of materials between fetal & maternal blood (in intervillous spaces) occurs across placental membrane (barrier) • Oxygenated blood returns to fetus by umbilical vein

PLACENTAL MEMBRANE • It separates fetal from maternal blood & prevents mixing of them • It is an incomplete barrier because it only prevents large molecules to pass (heparin, bacteria), but cannot prevent passage of viruses (e. g. rubella), microorganisms (e. g. toxoplasma gondii, treponema pallidum), drugs, hormones

PLACENTAL MEMBRANE COMPONENTS: • Until 20 th week: it is formed of 4 layers: 1. Syncytiotrophoblast 2. Cytotrophoblast 3. Extraembryonic mesoderm 4. Endothelium of fetal blood vessels • After 20 th week: it is more permeable to meet increased demand of fetus & is formed of 2 layers : 1. Syncytiotrophoblast 2. Endothelium of fetal blood vessels

FUNCTIONS OF PLACENTA • METABOLISM: synthesis of glycogen, cholesterol & fatty acids: source of nutrition & energy for embryo or fetus during early pregnancy

FUNCTIONS OF PLACENTA • TRANSFER: transport of substances 1. 2. 3. 4. 5. in both directions between placenta & maternal blood: Gases: oxygen, carbon dioxide Nutritional substances: glucose, aminoacids, vitamins Hormones: steroid hormones (e. g. testosterone) Electrolytes: Na+, K+, Cl. Maternal antibodies: antibodies against diphteria, smallpox, measles

FUNCTIONS OF PLACENTA • SECRETION OF HORMONES: • Protein hormones: 1. Human chorionic gonadotropin (early pregnancy tests) 2. Human placental lactogen 3. Human chorionic thyrotropin 4. Human chorionic corticotropin 5. Relaxin • Steroid hormones: 1. Progesterone 2. Estrogen

ANOMALIES OF PLACENTA • ANOMALIES IN SIZE & SHAPE: normally chorionic villi persist only at site of decidual basalis: 1. Placenta membranacea: a large placenta due to persistence of on the entire surface of chorionic sac 2. Accessory placenta: a patch of chorionic villi persisted a short distance from main placenta
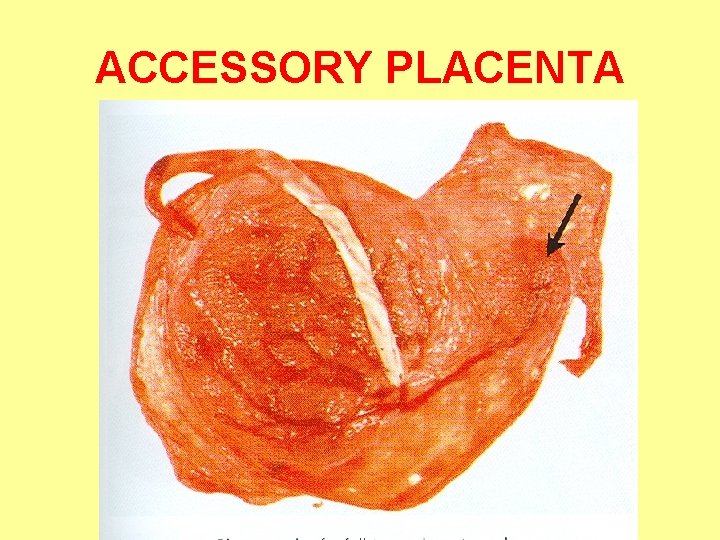
ACCESSORY PLACENTA

PLACENTA PREVIA, ACCRETA & PERCRETA

ANOMALIES OF PLACENTA • • ANOMALIES IN POSITION: Placenta previa: when blastocyst implants close to or overlying internal os of uterus late pregnancy bleeding • ANOMALIES IN EXTENSION: 1. Placenta accreta: chorionic villi extend to the myometrium 2. Placenta percreta: chorionic villi penetrate the whole thickness of myometrium & extend to perimetrium
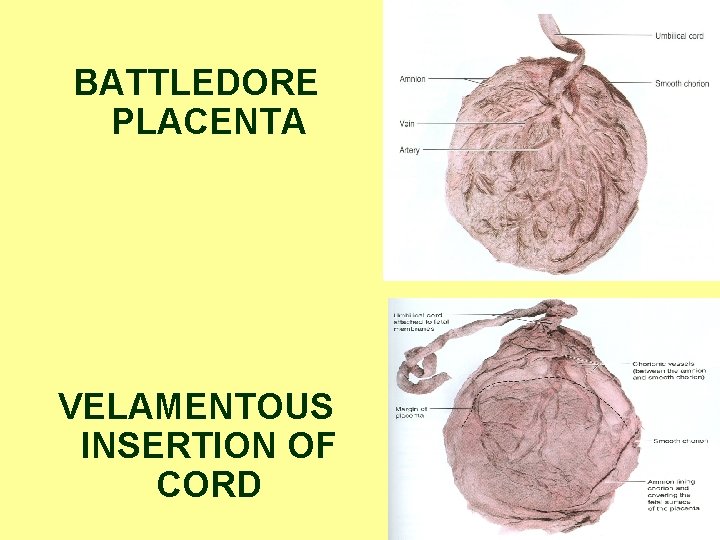
BATTLEDORE PLACENTA VELAMENTOUS INSERTION OF CORD

ANOMALIES OF PLACENTA • ANOMALIES IN ATTACHMENT OF UMBILICAL CORD: 1. Battledore placenta: the cord is attached to the margin of placenta 2. Velamentous insertion of cord: the cord is attached to the membranes surrounding placenta, umbilical vessels are liable to be ruptured
- Slides: 33